

Georgie Oldfield MCSP Physiotherapist & Founder of SIRPA



Georgie Oldfield MCSP Physiotherapist & Founder of SIRPA


A systematic review in the BMJ: Chronic Pain affects between 35 – 50% of the UK population (Fayaz et al)



British Pain Society survey: 8 million adults in the UK report CP moderate to severely disabling

£10 billion cost to the UK economy

Back pain accounts for 40% of NHS sick leave!



Understand the psychosocial aspects

Teach coping & pain management strategies

Recommended treatments: Cognitive
Behavioural Therapy, Acceptance and Commitment Therapy and Amitriptyline
Small positive effects on catastrophising & disability, but no significant influence on pain or mood (Williams et al 2020)


**Limitations** Symptoms addressed but with a lack of awareness of the need to identify and treat the root causes

Changing thoughts and not beliefs

Aiming to manage, not resolve the pain




Studies have estimated that 85 – 90% of chronic spinal pain is nonspecific. i.e. there’s no definitive diagnosis based on scan results.

All tissues are structurally healed after 3 months

Most people with CP believe that their body structures are fragile, broken or degenerating and will never recover.
N.B. Changing these faulty beliefs is essential

Cancer

Infection

Fracture

Auto-immune disorder

Cauda Equina Syndrome

Severe mental health conditions, such as: Bipolar, Dissociative Disorder, Schizophrenia, Borderline Personality Disorder
Plus other severe or unstable mental health conditions (unless the practitioner is a mental health professional trained to work with these conditions)
Pain is a danger alarm to a perceived threat, which can be physical, psychological, social and/or emotional



In chronic pain the danger alarm is sensitized so that normal inputs are interpreted as dangerous by the brain.


Prof Lorimer Moseley
All pain is an output of the brain based on the summation of;

Sensory inputs

Emotional inputs

Fearful beliefs

Memories (previous experiences)

Expectation

Cultural norms


‘Predictive Coding constantly generates and updates a mental model of the environment. This is used to generate predictions of sensory input that are compared with actual sensory input’


Image from: Fisher et. al. British Medical Journal, January 7, 1995


There is no correlation between the pain someone experiences and the amount of structural changes found on MRI


PSB asymmetries and imperfections are normal variations—not a pathology.

There is no relationship between the preexisting PSB factors and back pain.


Findings:

Findings:
47.5% of professional basketball players had articular cartilage lesions in the knees
77% of hockey players had MRI findings of hip or groin pathologic abnormalities


Findings: The overall prevalence of intraarticular shoulder pathology detected by MRI in asymptomatic elite-level climbers was 80% Cooper JD (2022)


IASP definition: “Pain is an unpleasant sensory and emotional experience…”


2,808 employees from 28 organisations, were tracked for 2 years. Conclusions: ‘the most consistent predictors of back pain were lack of ….decision control, empowering leadership and fair leadership.’

Nursing students were studied every 6 months during their 3year training and a year later. Conclusions: ‘Other than a history of LBP, pre-existing psychological distress was the only factor found to have a preexisting influence on new episodes of LBP.’
Feyer AM (2000)



i.e. What is the risk of mental illness in relation to childhood maltreatment, based on subjective and objective reports?
Objective Measures – minimal
Subjective Reports - high

With over 17k subjects they looked at the relationship of health risk behaviour and disease in adulthood to the breadth of exposure to childhood dysfunction

Physical, sexual or emotional abuse

Physical or emotional neglect

Growing up with a family member who is addicted to a substance, mentally ill or in prison

Witnessed abuse of the Mother

Losing a parent (to separation, divorce or death)


The number of categories of ACE showed a graded relationship to the presence of adult diseases including heart disease, autoimmune disease, cancer, chronic back pain, migraines etc.

The categories of ACEs were strongly interrelated and persons with multiple categories of ACEs were likely to have multiple health risk factors later in life.
Conclusion:




History of abuse in each group: fibromyalgia, 64.7% myofascial, 61.9% facial, 50% other pain, 48.3%
Conclusions:

“Children who had experienced hospitalisation, institutional care, maternal death or familial financial hardship were more likely to be suffering from chronic widespread pain as an adult”

A study was carried out with a placebo, low-velocity, rear-end collision. They found:

Approximately 20% of subjects had whiplash symptoms, even though no biochemical potential for injury existed


4 weeks after the placebo collision, symptomatic volunteers had been predicted with 92% accuracy by the initial psychological profiles
Surviving, not thriving
Wired but tired


‘When the Body says No’ by Dr Gabor Maté


The nervous system in childhood can learn that certain emotions are dangerous and this becomes wired with an anxiety/fear pathway

Later in life the ‘dangerous’ emotion evoked in a stressful life event in adulthood can trigger a physical pain if it is repressed due to fear

The nervous system ‘decides’ reflexively that physical pain is safer than emotional and then this provides a distraction in the body

Can be due to associations, such as:






An activity – especially while stressed
Anniversaries
Places
Times of day or week etc
Person
Reactivating a memory of a sense – smell, sound etc

Beliefs – e.g. sitting for long periods will injure my back, repetitive typing will cause pain

3.
Chronic pain is not caused by damaged structures in the body, but by learned neural circuits in the brain that become sensitized
a) Increased activity in the emotional centers of the brain
Acute pain: Cortex/ nociceptive
b) A thinner DLPFC, (which normally provides down regulation to emotional centres)

Chronic Pain: Emotional
Hashmi (2013) Lamm (2011) Weich (2009) + b. Brown (2014), Lorenz (2003)




Early beliefs that pain may be permanent

Loss of hope for the future

Greater exposure to past trauma

Personality

Anticipation/expectation of pain

Young C et al. 2008, Reme S E et al. 2012, Lamm C 2011, Apkarian AV 2005, Weich K 2009, Brown CA 2014, Lorenz J 2003, Egloff N 2013


• Lifestyle factors
• Self-compassion
• Existential factors
• Healthy diet
• Life balance


• Exercise Lifestyle Education

Self-empowerment
Books
DVDs/Audios
Online Programmes
On-going personal development
Pain Reappraisal
• Beliefs
• Values
• Attitude & Mindset
• Judgements
• Personality traits
• Self-Talk

Addressing past & current unresolved emotional trauma/stress – e.g. journaling & somatic approaches
Developing emotional awareness & felt sense/ Interoception
Learning to deal with dayto-day stressors and triggers



% of participants who were pain-free or nearly pain-free post treatment (i.e. VAS 0/1 out of 10)



N.B. fMRI changes and functional improvement were largely maintained at 1-year follow-up.
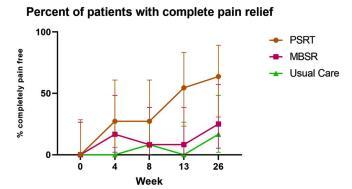

% Pain-free at 26 weeks

63.6% of the Psychophysiologic Symptom
Relief Therapy arm

25% Mindfulness Based
Stress Reduction

16.7% usual care
(53 Vets ave. age 73.5 years)



41.7% had >30% pain reduction
30% had >50% pain reduction
12.5% had >70% pain reduction

1 subject had at least 30% pain reduction


The evidence-based mindbody approach converges knowledge of pain science, trauma science, stress physiology, psychology and emotional factors.




When a whole person approach is considered and red flags have been ruled out
The root causes are addressed, rather than just treating the symptom
The predisposing, precipitating and perpetuating factors are considered and addressed



Acceptance of a paradigm shift by health professionals from the structural model to the biopsychosocial model, encompassing the emotional as well.
Willingness and readiness of the client to change beliefs and address underlying emotional causes.




‘Chronic Pain: Your Key to Recovery’ by Georgie Oldfield MCSP
SIRPA’s online Recovery Programme + Practitioner Training
Practitioner Directory
Follow the link to sign up for our weekly newsletter and the following gifts from SIRPA





A pdf of the slides from this talk bit.ly_4aIEMOl
The reference list of studies mentioned

Links to all the above plus a link to a recording of an emotional awareness strategy
Coupon code for 30% off our online recovery programme (before end of July 2024) 15% discount off our online SIRPA CPD training for health professionals/coaches (before end of July 2024)




• Asher Y et al. Effect of Pain Reprocessing Therapy vs Placebo and Usual Care for Patients With Chronic Back Pain: A Randomized Clinical Trial JAMA Psychiatry 2022;79(1):13-23
• Brinjikji et al. Systematic Literature Review of Imaging Features of Spinal Degeneration in Asymptomatic Populations, American Journal of Neuroradiology, 2015 16 Apr
• Block et al. The use of presurgical psychological screening to predict the outcome of spine surgery. Spine 2001jlu-Aug 1 (4): 274-82.
• Brown CA et al. When the brain expects pain: common neural responses to pain anticipation are related to clinical pain and distress in fibromyalgia and osteoarthritis. European Journal of Neuroscience 2014 39(4): 663-672.
• Caneiro JP et al. From Fear to Safety: A Roadmap to Recovery From Musculoskeletal Pain. Phys Ther. 2022 Feb 1;102(2):pzab271
• Castro WH et al. No stress no whiplash? Prevalence of "whiplash" symptoms following exposure to a placebo rear-end collision. International Journal of Legal Medicine. 2001;114(6):316-22
• Chan Kim et al. Association of hip pain with radiographic evidence of hip osteoarthritis: diagnostic test study. BMJ 2015; 351:h5983
• Christensen JO et al. Work and back pain: a prospective study of psychological, social and mechanical predictors of back pain severity.European Journal of Pain. 2012 Jul;16(6):921-33.21
• Cooper JD et al. Shoulder Pathology on Magnetic Resonance Imaging in Asymptomatic Elite-Level Rock Climbers. Orthop J Sports Med. 2022 Feb 11;10(2):23259671211073137
• Danese A. Objective and subjective experiences of child maltreatment and their relationships with psychopathology. Nature Human Behaviour 2020 vol 4, pages 811–818
• Donnino M et al. Psychophysiologic symptom relief therapy for chronic back pain: a pilot randomized controlled trial. PAIN Reports: September/October 2021 - Volume 6 - Issue 3 - p e959
• Elliott J et al. Asymptomatic Spondylolisthesis and Pregnancy Journal of Orthopaedic & Sports Physical Therapy, 2010 Volume:40 Issue:5 Pages:324–324
• Fayaz, A., et al Prevalence of chronic pain in the UK: a systematic review and meta-analysis of population studies. BMJ Open 20 June 2016
• Felitti V. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. American Journal of Preventative Medicine 1998 May;14(4):245-58
• Feyer AM et al. The role of physical and psychological factors in occupational low back pain:a prospective cohort study. Occupational and Environmental Medicine 2000 Feb;57(2):116-20
• Fisher JP et al. Minerva. BMJ. 1995; 310:70.
• Goldberg RT et al. Relationship between traumatic events in childhood and chronic pain. Disability and rehabilitation. Disability Rehabilitation,1999 Jan;21(1):23-30
• Hashmi JA. Shape shifting pain: chronification of back pain shifts brain representation from nociceptive to emotional circuits. Brain. 2013 Sep; 136(9): 2751
• Jones GT et al. Adverse events in childhood and chronic widespread pain in adult life: Results from the 1958 British Birth Cohort Study. Pain. 2009 May;143(1-2):92-6.
• Kaplan LD et al. Magnetic resonance imaging of the knee in asymptomatic professional basketball players. Arthroscopy. 2005 May;21(5):557-61
• Lamm C et al. Meta-analytic evidence for common and distinct neural networks associated with directly experienced pain and empathy for pain. NeuroImage 2011 54(3):. 2492-2502
• Lederman E. The fall of the postural-structural-biomechanical model in manual and physical therapies: exemplified by lower back pain. Journal of bodywork and movement therapies. 2011 Apr;15(2):131-8
• Lorenz J. Keeping pain out of mind: the role of the dorsolateral prefrontal cortex in pain modulation. Brain: a journal of neurology 2003 126(5): 1079-1091
• Lumley et al. Emotional awareness and expression therapy, cognitive behavioral therapy, and education for fibromyalgia: a cluster-randomized controlled trial. Pain. 2017 Dec;158(12):2354-2363.
• Howard Schubiner MD. Application of a Clinical Approach to Diagnosing Primary Pain: Prevalence and Correlates of Primary Back and Neck Pain in a Community Physiatry Clinic,
• The Journal of Pain, Volume 25, Issue 3, 2024, Pages 672-681
• Silvis ML et al. High prevalence of pelvic and hip magnetic resonance imaging findings in asymptomatic collegiate and professional hockey players. The American journal of sports medicine. 2011 Apr;39(4):715
• Wiech, K et al. The influence of negative emotions on pain: behavioural effects and neural mechanisms. NeuroImage 2009 47(3): 987-994
• Yarns.B et al. Emotional Awareness and Expression Therapy etc: A Randomized Comparison Study. Pain Med Vol 21, Issue 11, Nov 2020, 2811-2822