LOOP IN THE

SPEECH
PATHOLOGY WEEK Communication through art
SALLY JOUSTRA 40 YEARS OF SERVICE
SHORT NOTICE ASSESSMENT
Langmore Centre’s achievement
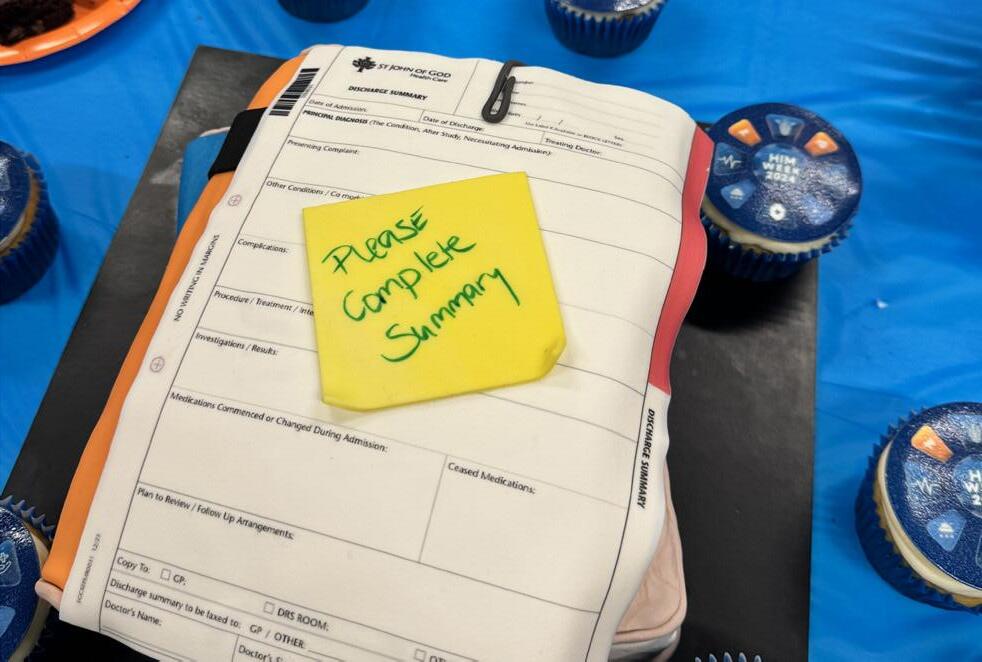
CELEBRATING THE BERWICK AUXILIARY



SPEECH
PATHOLOGY WEEK Communication through art
SALLY JOUSTRA 40 YEARS OF SERVICE
SHORT NOTICE ASSESSMENT
Langmore Centre’s achievement
CELEBRATING THE BERWICK AUXILIARY

Dear caregivers and VMOs,
As we step into a new quarter, I want to take a moment to connect with each of you and share some important insights regarding the current landscape of private health care in Australia.
Many of our patients are facing increasing financial pressures, a reality compounded by rising living costs and economic uncertainties. We recognise that these challenges can lead to difficult decisions regarding their health care options. As a team dedicated to compassionate care, it is crucial that we understand and address these concerns with empathy and support.
In light of this, I’m excited to share our new self-funded campaign designed to enhance patient accessibility. This initiative will focus on providing surgical care with transparent out-of-pocket costs, allowing us to reach more individuals in need. In particular, those without private health insurance. Patients can avoid long public waiting lists and have their surgeries scheduled more quickly, all while choosing their preferred doctor.
Even in difficult times, we see hope and goodness. As we celebrate Foundation Day, we are reminded of the countless contributions made by our long-serving caregivers. Your commitment and compassion are the backbone of our organisation and inspire us to strive for excellence every day.
Our commitment to providing high-quality health care remains unwavering. I encourage all of you to continue fostering open communication with our patients and their families. By listening to their concerns, we can better tailor our services to meet their needs and ensure they feel valued and supported.
Thank you for your dedication and hard work. Together, we can navigate these challenges and continue to provide exceptional care to our community.
Warm regards,
Lisa Norman General Manager, South East Melbourne Hospitals

Berwick After Hours Hospital Co-Ordinator Sally Joustra celebrates 40 years of service in 2024.
Sally began at Berwick Bush Nursing Hospital in 1984 and on Foundation Day, 2024 she reminisced on her time nursing in the Berwick community:
“Forty years, wow. It’s amazing how much the hospital has changed and yet remained the same. When I started at Berwick Bush Nursing Hospital in 1984 it was 24 beds: eight medical, eight surgical, and eight maternity. Four nursing staff were rostered for a morning shift: three RNs and one EN. A workload not possible without strong teamwork. Healthcare computers were non-existent, nor were automated tools such as BP machines and oxygen probes. Local teenagers were employed as the supper girls. Being a communityowned hospital, there was a feeling of a supportive family. Fellow workers became my network of advice and camaraderie as I was the new girl on staff and later a new mum.
Many staff were children of employees, myself included. My son Scott became the third generation of our family to work at Berwick. The hospital evolved into Berwick Hospital Incorporated, and the hospital logo, ‘I Will Survive’, was seriously challenged. We had some very scary years, and we certainly embraced hope as we struggled financially. Finally, our prayers were answered when St John of God purchased the hospital in 2010.
The staff were very concerned that the holistic care and community ethos would be lost. But we need not have worried as the core values of St John of God were the strengths we needed to shape the future and have continued into the lovely 202-bed hospital we have today.

Being a person who uses humour as a default setting, I could tell many stories. The copious medical, personal and professional dramas and anecdotes of the hospital were the most valuable to me. However, the time the hospital entered a float in the City of Casey street parade and the time we rescued a staff member’s cat from the ceiling space was a special highlight, and organising a wedding in labour ward with 10 minutes’ notice. The baby was born half an hour later!
People ask me why I have been here so long. My answer is best described as a paraphrase from Paul’s first letter to the Corinthians. St John of God Hospital may be a shiny new blue hospital and specialist centre with all kinds of clever technology. It may have an evergrowing roster of attending medical officers and wellqualified staff.
It may be part of a huge and well-respected organisation, and it may only be 700 metres from home. But without love, it is nothing.
I wish to thank everyone I have worked with over the years in all the very many departments of the hospital for being wonderful friends and co-workers. I also wish to thank my husband Norm for being my home support. It has been a great privilege and a true pleasure to be here with you all. To have shared so many years of my life with you. Thank you.” - Sally Joustra
Thank you Sally for the role you have played in shaping the health care we provide to our patients today and for your leadership and experience. We are richer for having you as part of our team.

St John of God Health Care’s (SJGHC) south east Melbourne hospitals are pleased to welcome Dr Jonathan Barrett, Director of Medical Services.
Jonathan is a specialist Physician and Intensivist.
Prior to joining SJGHC he was Director of ICU at Epworth Richmond, Deputy Director at Cabrini Malvern and worked at Holmesglen Private Hospital in ICU and at Monash Casey ED as a Consultant. He has completed his Master of Public Health and continues to actively teach at undergraduate and postgraduate levels and is a college examiner for the College of Intensive Care.
Jonathan also has an interest in quality and safety and has worked with the Australian Commission on Safety and Quality in Healthcare. As a member of the Comprehensive Care Committee, he was involved in taking this national standard from concept to implementation. He continues to work with ACSQHC on the National Sepsis Program.
With an interest in research and leading teams to innovation, Jonathan’s primary focus is on improving patient care and outcomes. He has led teams and commenced new services during his private appointments and public appointments at Monash Health.
Jonathan commenced with St John of God Health Care on 5 August 2024 and also works at Casey ED as a Consultant.
To contact Dr Jonathan Barrett, please email jonathan.barrett@sjog.org.au



On 16th July as part of NAIDOC Week celebrations, the SEM HMC gathered with members of the Reconciliation Working party and Elders and leaders from local Aboriginal services, Bunjilwarra and Nairm Marr Djambana.
They were able to celebrate the SJGHC Reconciliation Action Plan and discuss the local response and commitment to ongoing Reconciliation. Partnership agreements were signed by both services which soldified the shared commitment to moving forward in collaboration together.
Jillian West, a Bunurong woman, lead Welcome to Country and shared some of the local stories that are important to the local Bunurong/Boon Wurrung people.
July,Aug, Sept 2024
Congratulations to all nominees and winners of Caregiver of the Month. Thank you for your hard work and commitment to the Values of St John of God Health Care.
Langmore
Cara Tattersall (Art Therapist) for compassion
Frankston
Team award for Granada Ward:
Therese Kandetski (Enrolled Nurse) for justice
Jacob Goodingham (Enrolled Nurse) for compassion
Berwick
Leah Ebanks (Registered Nurse) for excellence
Team award for 2 East Medical Unit for compassion and excellence:
Dr Cam McLaren (Oncologist)
Anna Salan (Enrolled Nurse)
Robyn Cooksey (ANUM)
Margarita Nguyen & Brenda Grant (Pastoral Practitioners)
Dr Hossein Kasiri (Palliative Care Physician)
Juliet Auger (Care Coordinator),
Jo Wilson (Cancer Care Coordinator)
Langmore
Kim D’Silva (RN, Mental Health) for compassion
Frankston
Karissa Monks (Admin Clerk) for excellence
Berwick
Day Oncology Team for excellence

Langmore
Emina Music (Registered Nurse) for excellence
Frankston
Cheryl Kishere and Angela Smith (Environmental Services Assistants) for respect
Berwick
Jasmine Rossborough (Consulting Medical Receptionist) for excellence
St John of God Langmore Centre successfully achieved Short Notice Assessment in late August.
Congratulations to the Langmore team on this outstanding result. We met all the requirements of the National Standards, with no recommendations made.
Two assessors from the Australian Council on Healthcare Standards (ACHS) were onsite over the 2 days. They were very impressed with thehospital, caregivers, VMOs and excellent and professional patient care provided.
When an assessor asked a patient about their time at Langmore, they said they were, “receiving wonderful care at Langmore and felt safe to be here”. Internally, we have outlined opportunities for improvement which we will focus on and monitor. It


is important for us to implement these improvements and ensure they are embedded into our systems and processes to enhance patient safety.
I would like to the Langmore team for their hard work and dedication in preparing for Short Notice Assessment. It was a whirlwind two days and everyone played a vital part in achieving this successful outcome. Well done to the Langmore team!
Eveline Soon
Clinical Governance Manager
St John of God South East Melbourne Hospitals



St John of God Frankston Rehabilitation Hospital
Linda was working as a partner in her own law firm when she suffered a stroke. She was initially unable to speak any words.
During rehabilitation at SJG Frankston, Linda was especially drawn to the Art Therapy program offered.
Through her art she found she was able to communicate how she was feeling, and combined with intensive speech therapy she began to recover her ability to express herself with words.
In her commentary on her art works, Linda recalled her experience of losing the ability to communicate verbally.
“When I forgot how to say my children’s names, the loss of my language was a devastation beyond imagination,” she said. “Abruptly, I unexpectedly found myself in a strange existence of being conscious but having no memory of words, names, places, people, animals and everything. I felt like a ghost.”
Linda was keen to engage in art therapy processes initially as a mindfulness activity to assist in her ability to relax, focus and re-develop cognition. Lorin Randall,
Art Therapist at SJG Frankston said, “Art Therapy accesses right brain and is predominantly non-verbal where the emphasis is on the process of creating, not the outcome.”
Linda went on to immerse herself in creative processes where a series of expressive artworks emerged from the impulses and influences she was experiencing.
“With each artwork she completed I would encourage her to take time to reflect on her thoughts and processes (conscious or unconscious), and to journal a short narrative about each piece. The result was an extensive collaboration of expressive, creative art works that depicted her emotional and physical journey of rehabilitation and recovery,” said Lorin.
Linda expressed the process saying, “When I can’t find my words or remember, painting helps me. It all comes together when I do art!”
The combination of speech and art therapy helped Linda to communicate her way.
By Deb Cunningham, Speech Pathologist


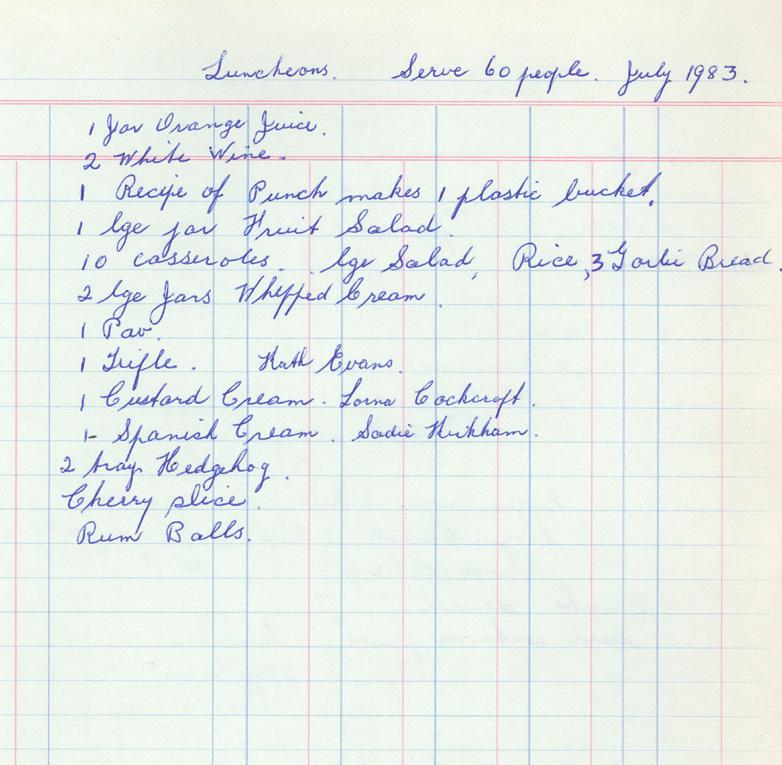
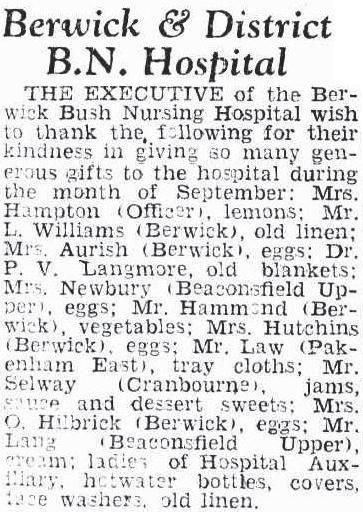
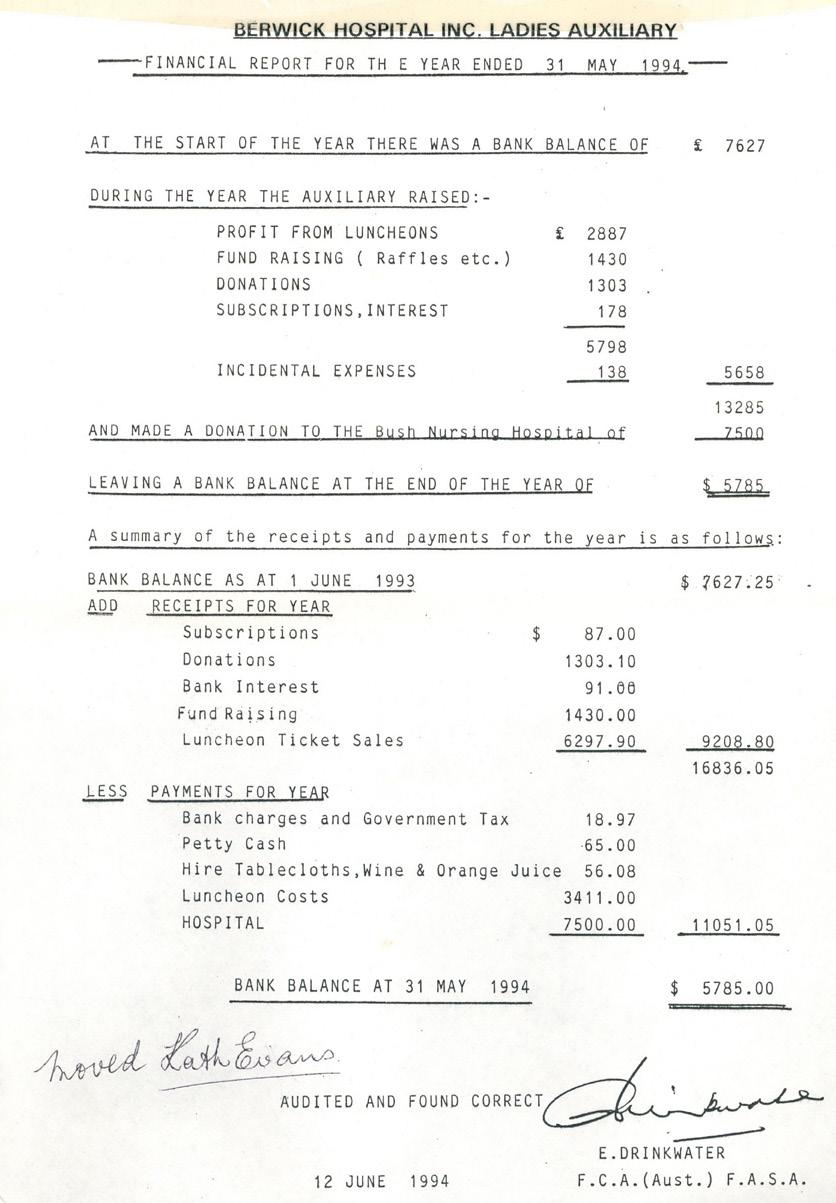
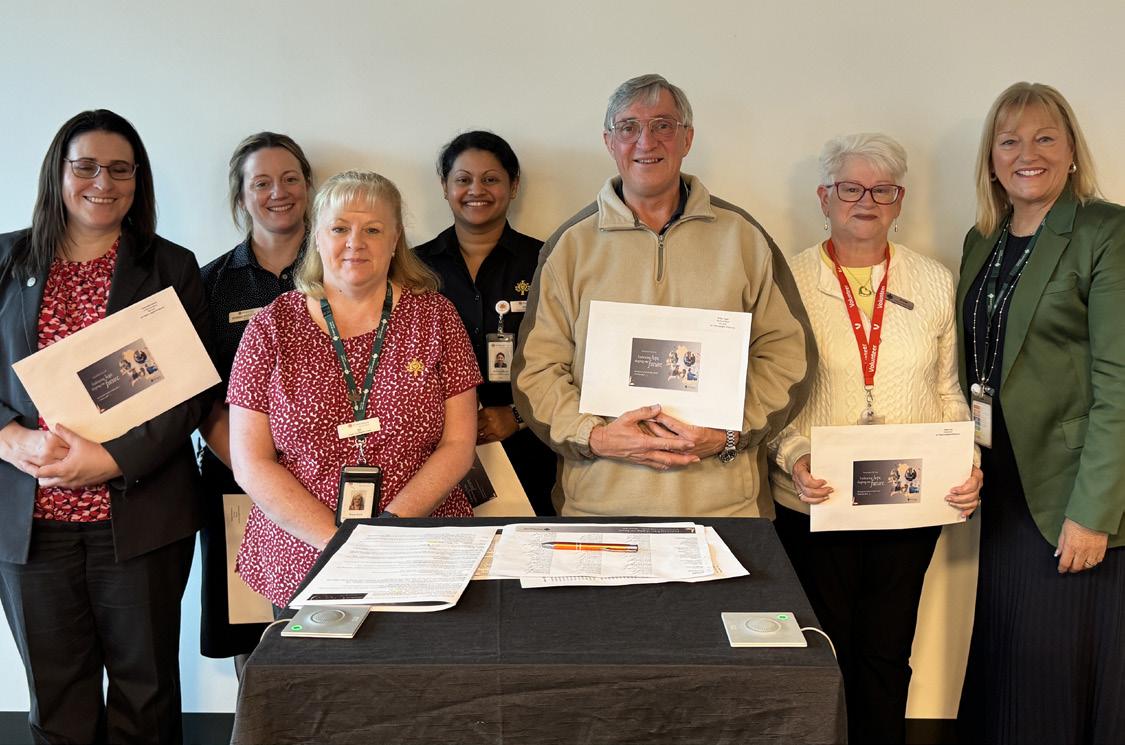
The Auxiliary has raised hundreds of thousands of dollars in the 72 years they have been operational. These funds have been used to buy equipment, improve facilities, upskill caregivers and to support the hospital in times of financial hardship over the years.
We are proud of the amazing work that this wonderful team of selfless volunteers does and we are incredibly grateful for the impact they make.


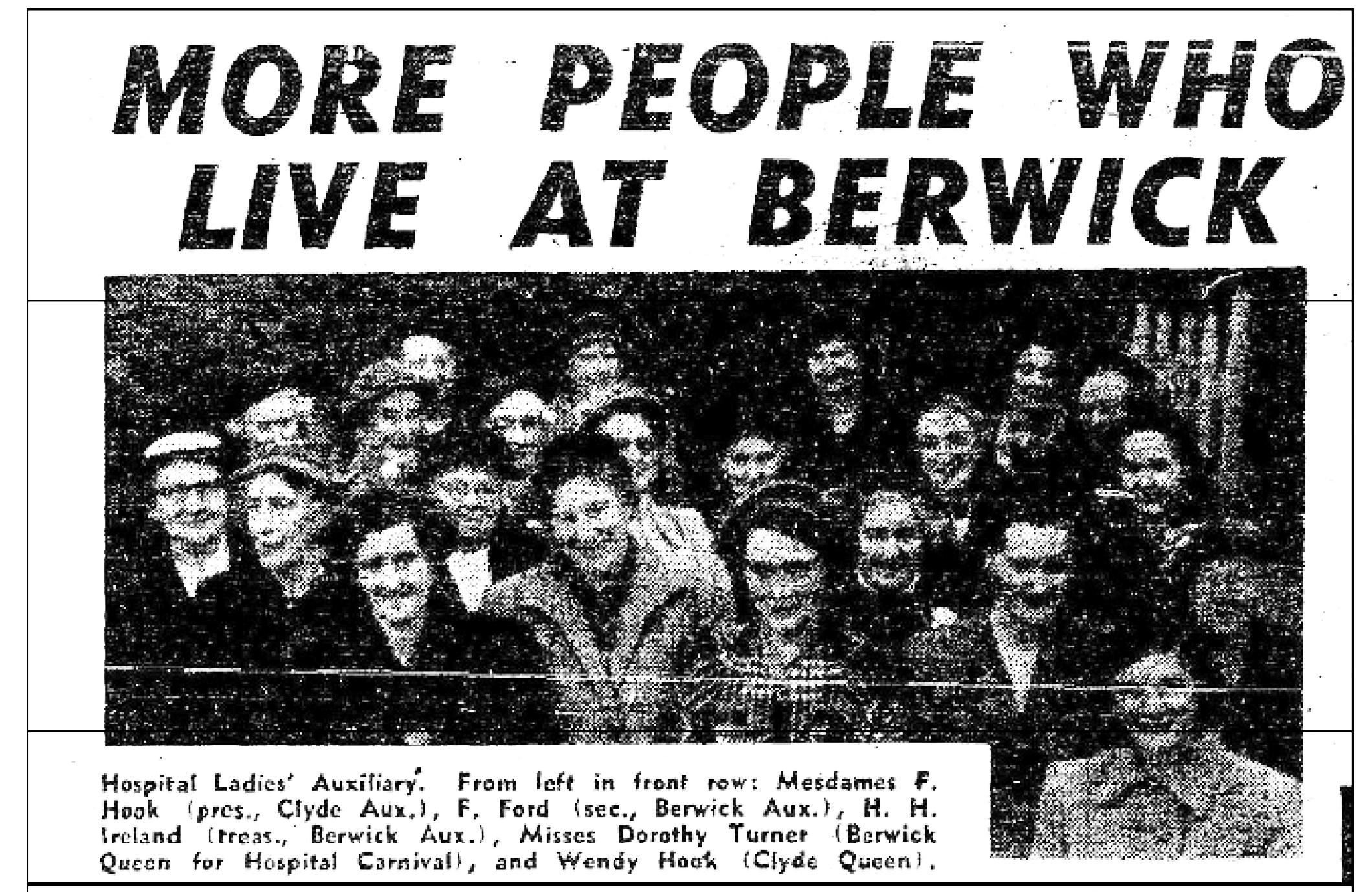




Maura, Kathy, Kosanka and Bill volunteer in outpatient rehabilitation at St John of God Berwick Hospital and each one speaks about how much they love volunteering in this area and how awesome the Allied Health caregivers are to volunteer alongside. They journey with caregivers supporting patients as they complete six to eight weeks of a rehabilitation program.
Let’s hear from the allied health caregivers about how awesome this team of volunteers are and the difference they make to caregivers, patients and the vibe of this service.
“Most importantly volunteers provide a cheerful smile and engaging conversation that increases client morale allowing them to get even more out of their rehabilitation,” Katelyn, Exercise Physiologist
“It’s always lovely to have that familiar warm smile and conversation in the groups for not only the patient’s, but the staff also,” Jo-Anne, Cardiac Rehabilitation Nurse
“Your love, care and support has been invaluable not only to the patients but also to all the caregivers,” Alicia, Outpatient Rehabilitation Physiotherapist.
Boom! Outpatient rehab have that special equation that gives best outcome for all involved - the patients, caregivers and volunteers.
Volunteers are part of the team, clear in their role, needed, and appreciated. When all this comes together, I gotta say it makes my heart sing. This is what we


work together to achieve in all aspects of volunteering with St John of God as we uphold the values of respect, hospitality, justice, compassion and excellence in all that we do to provide the very best in patient experience and outcome.
Maura, Kathy, Kosanka, and Bill you truly are worth your weight in gold. Treasured and valued. Thank you for your contribution and dedication to St John of God South East Melbourne.
Erica
Proposch
Coordinator of Volunteers

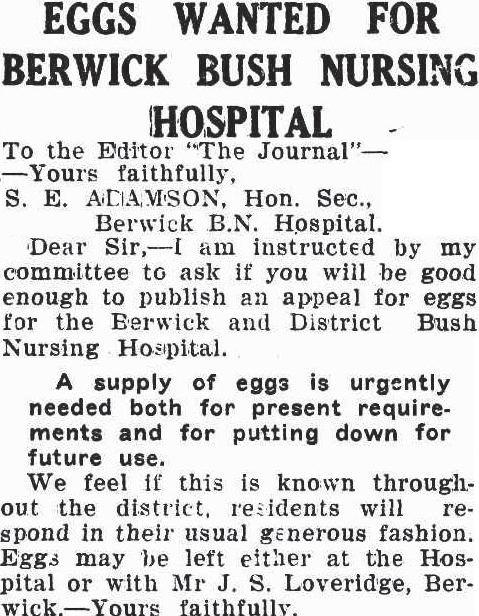
An egg shortage. Sound familiar?
While our supermarket shelves are currently bare of eggs, we reflect on this Dandenong Journal article from November 1939 when it seems the community were in a similar situation!
29 November, 1939 Dandenong Journal
Berwick Day Oncology Unit successfully went live with CHARM on Tuesday, 27 August- the first site for the group-wide rollout.
CHARM Evolution is a cutting-edge oncology electronic medical record system that supports every step of cancer care. It offers safe, secure access to patient health records and treatment plans from anywhere, helping our caregivers make informed decisions before and during patient treatment.
This seamless launch was the result of months of careful planning and preparation by the hospital and project teams. The success would not have been possible without the dedication and hard work from CHARM Project Nurse Monika Whitehead, along with leadership support from Nurse Unit Manager Lisa Marchetti, VMO CHARM representatives, and St John of God South East Melbourne’s Hospital Management Committee.
Lisa Norman, CEO St John of God Berwick and Frankston Hospitals & General Manager South East Melbourne, praised the project team, “The CHARM Project Team, with their deep understanding of the clinical environment, made implementation easy by providing exceptional support and effective solutions to ensure the best outcomes are achieved.”
What CHARM means for caregivers:
• Better Communication: It enhances collaboration among the oncology and haematology team, allowing everyone to stay on the same page and streamline patient care.
• Improved Patient Care: CHARM brings together all aspects of treatment, from medication management to scheduling, ensuring everything runs smoothly.
• Up-to-Date Protocols: It allows caregivers to access the latest, evidence-based treatment protocols.
• Increased Safety: With CHARM, medication and patient safety is a top priority, especially when it comes to lifetime dosing limits, aligning with Australian standards.
What CHARM means for patients:
• Better Coordination: Patients will benefit from improved teamwork among their care providers, leading to more efficient scheduling and treatment.
• Cutting-Edge Care: Patients can rest assured they’re receiving the latest evidence-based treatments.
• Enhanced Safety: CHARM boosts safety throughout the cancer treatment journey.
• As part of our digital roadmap, CHARM is one of the key initiatives aimed at improving the delivery of our compassionate, person-centred care.
As one of the initiatives included in our Digital Roadmap, CHARM is a key step toward improving the compassionate, person-centred care we’re known for.
“CHARM gives us confidence that we’re providing the right treatment to our patients. Our infusion services offer complex treatment regimens to those facing some of the most challenging times in their lives. CHARM helps us uphold our commitment to delivering excellence in patient care,” Lisa said.
What’s next?
The CHARM Project will continue to roll out across the remaining seven oncology services, with Murdoch scheduled to go live in mid-November. Before that, a system-wide upgrade will bring CHARM to its latest version, introducing new features and ensuring up-todate cyber security. This upgrade is expected to be implemented with minimal impact on current users at Subiaco and Berwick.

St John of God Berwick Hospital has installed a memorial wall within their tranquil outdoor chapel courtyard to acknowledge and pay tribute to deceased caregivers, volunteers and founders.
The memorial wall was a concept initiated by Theatre Technician, Rex Flannery and supported by the hospital’s management team. Plaques have been installed in memory of the deceased caregivers, with each of their names engraved.
“I thought it would be lovely to honor our caregivers who have passed by having this memorial for all our current caregivers to have somewhere to reflect and a quiet space to remember their work colleagues,” explained Rex.
St John of God Berwick Hospital takes immense pride in its culture and living its Values each and every day. All staff are referred to as ‘caregivers,’ a term reminding individuals of the role they play in patient care and the hospital experience. Providing the best patient experience is a collaborative effort which encompasses each and every staff member- from cleaners, to doctors, to administration professionals. It is this sentiment that captures the value of each individual who chooses to work with the hospital and the importance of the contribution they make.
Director of Mission Integration, Rhonda O’Connor explained, ”We fondly remember those who have been


part of our hospital community and who have made a valued contribution. We look forward to installing memorial walls at both St John of God Langmore Centre and St John of God Frankston Rehabilitation Hospital in the near future.”
On Thursday 29th August 2024, Rex and his fellow theatre technician, Leanne Bluett placed the first flowers at the memorial wall. Rex reflected, “I am pleased to say the wall plaques are now in place.”


St John of God Berwick Hospital (SJGBH) has recently launched an innovative new service that puts patients in touch with specialist emergency doctors without leaving home. Operated in conjunction with My Emergency Doctor, this telehealth service is designed to help individuals facing urgent, but non-lifethreatening medical concerns, especially when a visit to the ED seems like the next step and their regular GP isn’t available.
By opting for this virtual service, patients are able to avoid the lengthy wait times that often come with in-person ED visits. Instead, they can connect with a doctor quickly, get expert advice and potentially start treatment much faster. If hospital admission is required, a direct pathway to St John of God Berwick Hospital may be organised. Referrals for diagnostic tests such as pathology and radiology, medical specialists and allied health professionals can also be arranged.
My Emergency Doctor is an emergency telemedicine service which provides access to an Australian qualified emergency specialist doctor 24 hours a day, 7 days a week. The service does not require an appointment, and doctors will talk to patients via a phone or web-based video call.
To access the service, patients pay a $220 fee reimbursable by SJGBH if the consultation results in direct admission. This is half of the cost of attending other local private emergency departments, with the convenience of being able to access care from home.
The service commenced in May 2024 and within the first 3 months a total of 37 calls were received, with 38% of patients being directly admitted to SJGBH. The average patient age was 55 years, with a range between 2-89 years. 27% of patients were 75 years and older, demonstrating that age is no barrier to utilising technology. Pain was the most common presenting complaint, in particular back pain.
The response from both general practitioners (GPs) and patients has been extremely positive. SJGBH CEO, Lisa Norman says that GPs recognise the value of the service in ensuring their patients can access care out of surgery hours. The first patient to utilise the service was recommended by a local GP who was impressed by the process in providing access to urgent care for her patient.
For many patients, avoiding a public emergency department when possible is highly desirable. This has been the case with multiple patients undergoing chemotherapy. When facing issues post-treatment, they have been able to connect with My Emergency Doctor and arrange direct admission to the hospital. This eliminated the need to wait in an ED and the risk of exposure for these immunocompromised patients. Bypassing the emergency department waiting room can also be important for people who find attending an ED stressful or triggering.
Patient feedback has been positive. Jeremy Stork used the My Emergency Doctor service to arrange a consultation for his elderly mother-in-law, Pat. “Pat had terrible swelling in her legs and was in a lot of pain. She lives in an aged care facility and is very frail. It’s extremely difficult to get her into the car for medical appointments, let alone wait in an ED,” he said.
“We connected with My Emergency Doctor via Pat’s iPad while she rested and talked with a doctor who was able to assess her and arrange direct admission to the hospital that night. It was a real game-changer for us and meant Pat began treatment much sooner.”
St John of God Health Care’s Virtual Care Strategy recognised issues for private patients seeking easier access to private health care services without a GP or public emergency department doctor referral. The initiative is one of the first steps in providing better navigation into the private health care system for patients.
To learn more or access My Emergency Doctor: www.sjog.org.au/berwickonlinedoctor























40 Years
Sally Joustra
30 Years
Fiona Jackson
20 Years
Tracey Murphy
Lisa Geeson
Justine Wilkinson
15 Years
Suzanne Mitchell
Jacqueline Davidson
Gaynor Stanford
Sheena John
Carol Plunkett
Reynaldo Claveria
Fiona Ingram
Rebecca Jamieson
Joanne Lotherington
Ying Lu
Varun Sikka
Jennifer Cornell
Anna Macente
Cheryl Titcher
Leesa Penn
Jincy John
Elsamma Mathew
10 Years
Gayle Brown
Alma Lim
Claire Burge
Bianca Ball
Olivia Poliwodzinski
David Hedges
Helen McCulloch
Meena Handunge
Sarah Barker
Nisha John

Manju Abraham
Ricky Fagan
Diane Ginns
Samantha Masters
Eugenia Ramos
Jacqueline Miller
Monika Whitehead
5 Years
Sonya Robinson
Ashwinder Kaur
Leanne Mastin
Shincy Mathew
Jen Laverman
Riza Siscar
Margaret Lennon
Natalie Shores
Leslie Leahy
Georgie Walters
Sincy Mathew
Sheenam Soni
Trichia Kim
Natalie Benn
Jo Goncalves
Melinda Meehan
Leanne Elton
Mona Patel
Rebecca Kenner
Joy Aninon
Leonie Harding
Adrianna Barbu
Ryan Nestoriwsky
Evon Ebrahim
Navreen Kaur
Michelle Lisao
Jade Elumba
Miquaeel Khan
Darryl Ferber
Belinda Pane
Lia Power
Kathryn Bottern
Alicia Chan
Sharon Quinn
Virginia Suarez
Justin Keppel
Emily Goodman
Stella George
Hanna Reyes
Romil Fortinez
Jinu Anthony
Lincy Innocent
Tori McCarthy
Prasanna Perera
Emily Le Fleur
Era Singh
Erin Valentine
Jessica Kitson
Samantha Grigg
Krystal Pratt
Anna Flynn
Kelly Nekritin
Maddie Linke
Chloe Brown
Sinead Scanlon
Caitlin Kennedy
Jake Lau
Tara McGrath
Andrew Yeoh
Harpreet Kaur
Aji Flower
Marivic Funilas
Sophie Raimbert
Yenny Torres Romero
Fissaha Gobena
Angela Worley
Tas Iqbal
Kate Asker
Rene Sandeman
Rini Varghese
Dione Johnstone
Julie Andrews
Jackie Moroney
Nicole Faoro
Reid Hiskins
Rebecca Parr
Emily Kelly
Teagan Burrough
Kate Raymond
Hiyasmin Facundo


Priscilla Singh
Casey Merrigan
Solly Joseph
Helen Malhotra
Vern Lu
Bindu Chacko
Fabiola Tuck
Tashia Wijesundera
Sneha Philip
Chamani Samaratunga
Lakshmi Mudaliar
Malinda Kirkpatrick
Myrna Magsino
Yifen Wang
Tresa George
Miguel Geocaniga
Sheldon Senora
Nadia Abdul Razak
Janelle Ward
Ira Orola
Christina Viney
Adam Larche
Jeanille Terrington
Sinto Dominic
Sue McRae
Jess Jess

20 Years
Marie Ducane (Retired)
James Chan
15 years
Sean Sandilands
Bruce Shirazi
Anju Soosairaj
Dierdree D’Silva
Jais John
Jennifer Shurdington
Edwina Dunstone
Cheryl Harrison
10 Years
Sophy Thannimoottil
5 Years
Sonia Godson
Joy Canete
Karen Ward
Debbie Warr
Joseline Pandiyamakkil
Augustine
Deanna Cordner
Natalie Angelopoulos
Jade Campbell
Sue McKenna

20 Years
Tammy Pearse
15 Years
Belinda Walker
Georgia Mermigas
Karen Jordaan
Glen Draper
10 years
Ronita Thompson
Darlene Van Slooten
Nina Dahima
Berman Adjam
5 Years
Nihitha Roy
Seethal Babu
Chloe Bell
Joanne Cummins
Rosanna Santos
Diriba Ticha
Marie Juglall
Michelle Dzwairo
Casey Merrigan
Zechariah Alagbe
Jennifer York
Stephanie Wong
Fiya Francis

10 Years
Helen Jones
Anne Lee
Glenys Parker
Brian Toohey
5 Years
Maura Beard
Margaret Droudge
Annette Kirby
Chris Jones
Margery McRae
Jim Weir

Foundation Day celebrates the establishment of the Sisters of St John of God in Wexford, Ireland in 1871. We honour the many Sisters who have since followed in their footsteps providing care for the disadvantaged throughout the world, especially the Sisters who served here in Australia and laid the foundations for the St John of God Health Care that we are all part of now.
Over the last 153 years, the Sisters have exemplified strength, courage, hope and an unwavering commitment to action, even in the face of adversity. This has shaped who we are today – one of the nation’s largest Catholic health care providers with a dedicated network of 16,500 caregivers across 26 hospitals and services in Australia and New Zealand caring for more than 400,000 patients and clients every year.
Eight Sisters arrived in Australia from Ireland in 1895, responding to an invitation from Perth’s Bishop Matthew Gibney to help care for the sick. By 1900 there were 17




Sisters from both Ireland and Australia. Of this group, seven were among the first trained nurses in Western Australia.
It is truly special to trace a connection back to this moment in history and reflect on the impact that the Sisters have had on health care in Australia. We are privileged that each of us has been entrusted by the Sisters to continue the ministry they founded. We carry forward their spirit of courage and lessons of hope in our own lives.
We are deeply grateful to each of you for the care you provide to our communities. Congratulations, as well, to our long-serving caregiverswo received their Length of Service Awards and the new leaders who were commissioned –thank you for your commitment.










In September St John of God Health Care launched a new marketing campaign to raise awareness of the option to self-fund private hospital care and provide patients with the key information they need.
The majority of private hospital admissions across Australia continue to be funded by private health insurance. However, St John of God Health Care has seen an increase in enquiries about self-funding private hospital admissions over the past 12 months.
While self-funding has always been an option in our private hospitals, we have enhanced processes to ensure patients can access the information they need to self-fund their care, including:
• Establishing a dedicated team for self-funding enquiries in our National Patient Admissions Centre with a dedicated 1300 phone number
• Engaging with specialists to ensure their practices know how to support patients with information on costs associated with self-funding (including SJGHC, medical practitioner and diagnostic fees)
• Making specialist doctors who regularly treat selffunded patients searchable via Find a Specialist on our website.
St John of God Health Care’s self-funded pathway is a stepping stone for people who don’t want to be on public waiting lists but aren’t covered by private health insurance.
To support this we will be launching a new marketing campaign that will go live on 16 September across Facebook, Instagram, Google and Spotify.
Self-funded care offers the same comprehensive care in St John of God Health Care’s private hospitals as an insured patient would receive, with:
• Quick access, avoiding public hospital waiting lists
• Choice of specialist and continuity of care from the initial consultation through to surgery, in hospital and after discharge

• A range of payment options including lump sum and payment plans.
Market research conducted for SJGHC showed that only 43 per cent of people without private health insurance were aware that self-funded hospital care was an option so, to help people understand the possibilities, we now have a dedicated patient information line for enquiries: 1300 940 199.
Doctors who treat self-funded patients are listed on our Find a Specialist search: sjog.org.au/specialists
Read our self-funded care guide at sjog.org.au/self-funded
If patients don’t have private health insurance, or the adequate level of cover, they may choose to pay (or self-fund) the procedure themselves, out of their own pocket.
This campaign aims to educate the community about their options. Rather than finding themselves on a long public waiting list, patients may choose to self-fund and have their procedure fast-tracked in a private hospital with their choice of doctor.
It is hoped that this strategy may welcome a new cohort of patients to St John of God Health Care, helping us to meet community need and to increase activity.



