ZIRCONIA RESTORATIONS : EVOLUTION AND INNOVATION


 By Dennis J. Fasbinder, D.D.S.
By Dennis J. Fasbinder, D.D.S.

ALL CONTENTS © 2020 SPEAR EDUCATION 4 6 12 14 16 18 20 22 24 25 8 CONTENTS ZIRCONIA RESTORATIONS: EVOLUTION AND INNOVATION
Introduction
Zirconia Mircostructure
Monolithic Restorations
Strength
Esthetics
Zirconia Surface Wear
Conclusion
References
About the Author
About Spear
INTRODUCTION
Interest in ceramic materials has continued to increase over the past few decades as higher strength ceramics have afforded expanded clinical applications. Optimal goals for ceramic materials would be to deliver superior esthetics, with predictable, cost effective fabrication, and long-term durability.
Glass ceramic materials have consistently provided enamel-like appearance; however, they are also brittle materials. Clinical research has consistently reported that the primary failure mechanism of glass ceramics is chipping and fracture.
(Pjetursson, 2007)
While there is a wide range of material options available for crowns, a survey of more than 1,700 dentists in the National Dental Practice-Based Research Network indicated that monolithic zirconia is the most common choice of material for a posterior crown. (Makhija et al 2016) Several factors were suggested as influencing the shift toward monolithic zirconia crowns, including increased patient demand for esthetic restorations, the cost effectiveness of zirconia, and that zirconia has significantly greater strength than glass ceramic materials and offers the additional advantage of allowing for more conservative tooth preparations.
Zirconia was initially introduced for clinical use as a more esthetic core material compared to metal. Early zirconia crowns were veneered with feldspathic porcelain to improve the esthetic appearance of the crown because zirconia is relatively opaque with a higher value. However, the chipping of the veneer porcelain led many dentists to be discouraged with its use. One meta-analysis of single crowns with a zirconia core reported a 91.2% survival rate, which was significantly lower than that of metal-ceramic crowns at five years.
(Sailer 2015)
Full-contour, monolithic zirconia crowns are preferred due to the simple fact that the surface of a full-contour zirconia crown is resistant to chipping or fracture. (Lawson, Burgess 2014) They also exhibit high flexural strength, allow for more conservative dental preparation, and minimize wear to antagonist dentition. (Albashaireh, 2010; Grin, 2013)
While zirconia is often presented as a single material, different formulations have evolved with considerably different polycrystalline structures and physical properties. An understanding of the various types of zirconia materials will aid in making informed clinical decisions to promote the desired clinical outcome for the case.

ZIRCONIA RESTORATIONS: EVOLUTION AND INNOVATION 5
ZIRCONIA MICROSTRUCTURE
Zirconium is a soft, silver-colored metal recovered as a mineral called Zircon (ZrSiO4). It is mined primarily from large deposits in Australia and South Africa and shipped to plants for processing. The mined Zircon is purified, and metal oxides are added to the refined powder such as yttrium to stabilize the metastable crystal form, aluminum to prevent water corrosion, and other coloring components. The Tosoh Corporation in Japan supplies the vast majority of the raw zirconia powders for dental manufacturers. So essentially almost all dental zirconia materials are fabricated from the same zirconia raw material. (Helvey 2017)
Zirconia is a polycrystalline material that does not contain glass particles even though it is commonly described as a “ceramic” material. Although the various brands of zirconia may be manufactured from the same raw zirconia powder, the quality and properties of a specific brand of zirconia are a function of the processing of the raw materials by the manufacturer to minimize porosity, enhance density, and ensure a homogenous material.
Zirconia is referred to as metastable since it can occur in three different crystalline phases depending on temperature and pressure parameters.
(Zhang 2018) Zirconia exists in the monoclinic phase in its naturally occurring state at room temperature and pressure. A uniform monoclinic zirconia would not be of use in dentistry since it has poor strength properties. At an elevated temperature of ~1170° C the monoclinic phase transforms into the tetragonal phase.
The tetragonal phase can be stabilized at room temperatures by adding small amounts of additives, called dopants, to the zirconia. Yttria has become the most effective dopant in amounts of 3 weight% to 5 weight% that is equivalent to 3 mol%. The third phase of zirconia transforms at temperatures above 2,300° C into the cubic phase. A greater amount of yttria is required to stabilize it (> 9.3 weight%) at room temperature resulting in compositions 5 mol% (about 50% cubic phase).
(Helvey 2017)
Compared with other dental ceramics, 3 mol% zirconia has higher flexural strength, fracture toughness, and hardness, mainly derived from the mechanism called “transformation toughening.”
(Pittayachawan 2009)
The tetragonal phase accounts for the high strength properties of 3 mol% zirconia. As a result of externally applied stresses, such as a crack initiation, the energy at the leading edge of the crack causes the tetragonal crystals to locally phase shift to monoclinic crystals.
The monoclinic crystals are volumetrically larger than the tetragonal crystals and this expansion results in a localized compressive force applied to the leading edge of the crack. The compressive forces essentially prevent the crack from propagating. This t > m transformation, or transformation toughening, is a major contributor to the high strength of zirconia and its ability to resist fracture under loading.
While the term “full contour zirconia” is often used to describe a monolithic, high strength, tooth-colored material, there is considerable variation in zirconia. The original zirconia materials introduced prior to ~2014 were 3 mol% that were 90%-100% tetragonal polycrystals and had very high strength properties. However, it tends to be relatively opaque, with a high value, and less esthetic than glass ceramics for matching natural tooth structure.
It generally requires a porcelain veneer to create the desired esthetic outcomes. Examples of these include: Lava Zirconia (3M), BruxZir (Glidewell), Cercon (Dentsply Sirona), and IPS e.max ZirCAD MT (Ivoclar Vivadent). (Zhang 2018)
The challenge for manufacturers of 3 mol% zirconia was to improve the esthetic appearance of the material while maintaining the desired high strength properties. This fostered the introduction of “anterior zirconia” or “translucent zirconia.” Development of translucent zirconia has included techniques such as increasing the amount of yttria, reducing the c oncentration of alumina, eliminating porosity by sintering at higher temperatures, reducing the crystalline grain size, and increasing the amount of cubic phase in the material.
(Zhang 2018)
ZIRCONIA RESTORATIONS: EVOLUTION AND INNOVATION 7
The challenge for manufacturers of 3 mol% zirconia was to improve the esthetic appearance of the material while maintaining the desired high strength properties.
Two early initiatives to improve translucency of these materials were to significantly reduce the amount of alumina dopant added and reducing porosity by sintering at higher temperatures. These improvements paved the way for monolithic full-contour zirconia restorations. Material examples of this were Lava Plus (3M), Vita YZ HT (Vita), BruxZir Full Strength (Glidewell), Katana HT/ML (Kuraray Noritake), and InCoris TZI (Dentsply Sirona). (Zhang 2018)
This modest improvement in the appearance of zirconia still limited its application in full contour restorations to posterior teeth with lower esthetic demands.


 Figures 1-3: CEREC zirconia crowns (3 mol%) delivered for teeth #19 and #20.
Figures 1-3: CEREC zirconia crowns (3 mol%) delivered for teeth #19 and #20.
The most recent attempt to increase the translucency of zirconia is to significantly increase the cubic crystalline phase to >25% and stabilize it with 5 mol% yttria. (McLaren 2017) The cubic crystalline phase decreases light scattering that occurs at grain boundaries and the zirconia appears more translucent.
However, this approach also reduces the flexural strength and fracture toughness because stabilized cubic zirconia does not transform at room temperature. (Zhang 2016) This results in a 35%-40% reduction of the flexural strength compared to 3 mol% zirconia. Recently introduced zirconia of this type include Lava Esthetic (3M), Katana Zirconia UTML/STML (Kuraray Noritake), BruxZir Anterior (Glidewell Laboratories), and ArgenZ Anterior (Argen Corp.). (Zhang 2016, McLaren et al 2017)



ZIRCONIA RESTORATIONS: EVOLUTION AND INNOVATION 9
Figures 4-6: Pre-operative #3 with stained, caries under ceramic crown replaced with full contour polished Katana zirconia crown (5 mol%).
As the composition of zirconia materials has evolved, it can be helpful to consider some sort of general classification system to provide a basis to understand differences in materials. One simple categorization of zirconia materials is based on the mol% of yttria. (Burgess 2018) 3 mol% zirconia are the early zirconia materials that are 85-90% tetragonal phase with flexural strengths in excess of 1100 MPa. They are also relatively opaque with a high value that limits the esthetic applications.
4 mol% zirconia has about 25% cubic phase with improved translucency and flexural strengths in the 750-900 MPa range. 5 mol% zirconia has about 50% cubic phase with significantly increased translucency. The flexural strength is further decreased to the 650-800 MPa range.
At this point, one may be thinking that this may be more information on zirconia structure than really needed. This categorization obviously reveals the changing physical properties of different types of zirconia is directly related due to the different proportions of the polycrystalline phase. There can be considerable variation in material properties within each category as yttria is actually measured in tenths of a mole percent.
However, the trend in improving the translucency of the zirconia is evident moving from 3 mol% to 5 mol%. A similar trend is also noted in the decreasing physical strength properties from 3 mol% to 5 mol% zirconia.
The changing physical properties of different types of zirconia is directly related due to the different proportions of the polycrystalline phase
The Gateway to Great Dentistry
Dentistry’s Most Innovative Online Learning Resource

PATIENT EDUCATION
Make chairside case presentation more engaging with our new tablet app, or stream animated videos to your lobby monitors via Fire TV Stick and Apple TV — options designed to empower even the most hesitant patient to take ownership of their oral health.
CLINICIAN EDUCATION
Increase your skills and earn continuing education credits on your own schedule with more than 1,500 clinical and practice management lessons presented by dentistry’s most respected clinicians.
TEAM TRAINING AND MEETING RESOURCES
Utilize tools designed for your front office, hygienists and assistants. When your staff understands and communicates the value of the dentistry you provide, patients are better informed and more receptive to accepting treatment.
SPEAR TALK
Connect with thousands of like-minded colleagues in a safe, supportive, clinicianonly environment meticulously monitored by Spear faculty and contributing authors to find answers to any clinical or practice challenge.
Membership to Spear Online provides your entire practice team with:
Discover how Spear Online impacts your entire practice: 855.625.2333 | online@speareducation.com | speareducation.com/spear-online
MONOLITHIC RESTORATIONS
The primary advantage of early zirconia materials was superior strength compared to other restorative materials. However, the high value and relative opaque appearance of 3 mol% zirconia did not offer the esthetic appearance required for more anteriorly positioned restorations.
Bilayer restorations consisting of a high strength, relatively opaque zirconia core with a more translucent porcelain veneer became preferred for improved esthetic results. But clinical research has reported that the chipping/ fracture of the veneering porcelain is a significant problem. (Sailer 2015) The introduction of translucent zirconia materials offered an opportunity for monolithic esthetic restorations and avoid the potential for surface chipping/fracture of veneered zirconia crowns. (Lawson, Burgess 2014)
Zirconia restorations are fabricated with a CAD/CAM process regardless of the impression technique used to record the tooth preparation. Zirconia blanks (pucks or blocks) are available from manufacturers in a partially fired or pre-sintered state. This allows for easier machining of the volume shape of the computer designed restoration with very good margin fidelity. A post-machining oven sintering process at very high temperature, ~1,350° C to 1,500° C, is required to fully sinter the zirconia. The oven sintering process results in a volumetric shrinkage of zirconia between 21% and 24%.
Manufacturers bar code the zirconia blanks to record the specific shrinkage percentage of the blank. The bar code is input to the design software to mathematically expand the design by the blank shrinkage factor. The milled restoration is obviously considerably larger than the desired final restoration. The milled restoration volumetrically shrinks to the correct volumetric size during oven sintering to create the fully crystallized zirconia restoration.
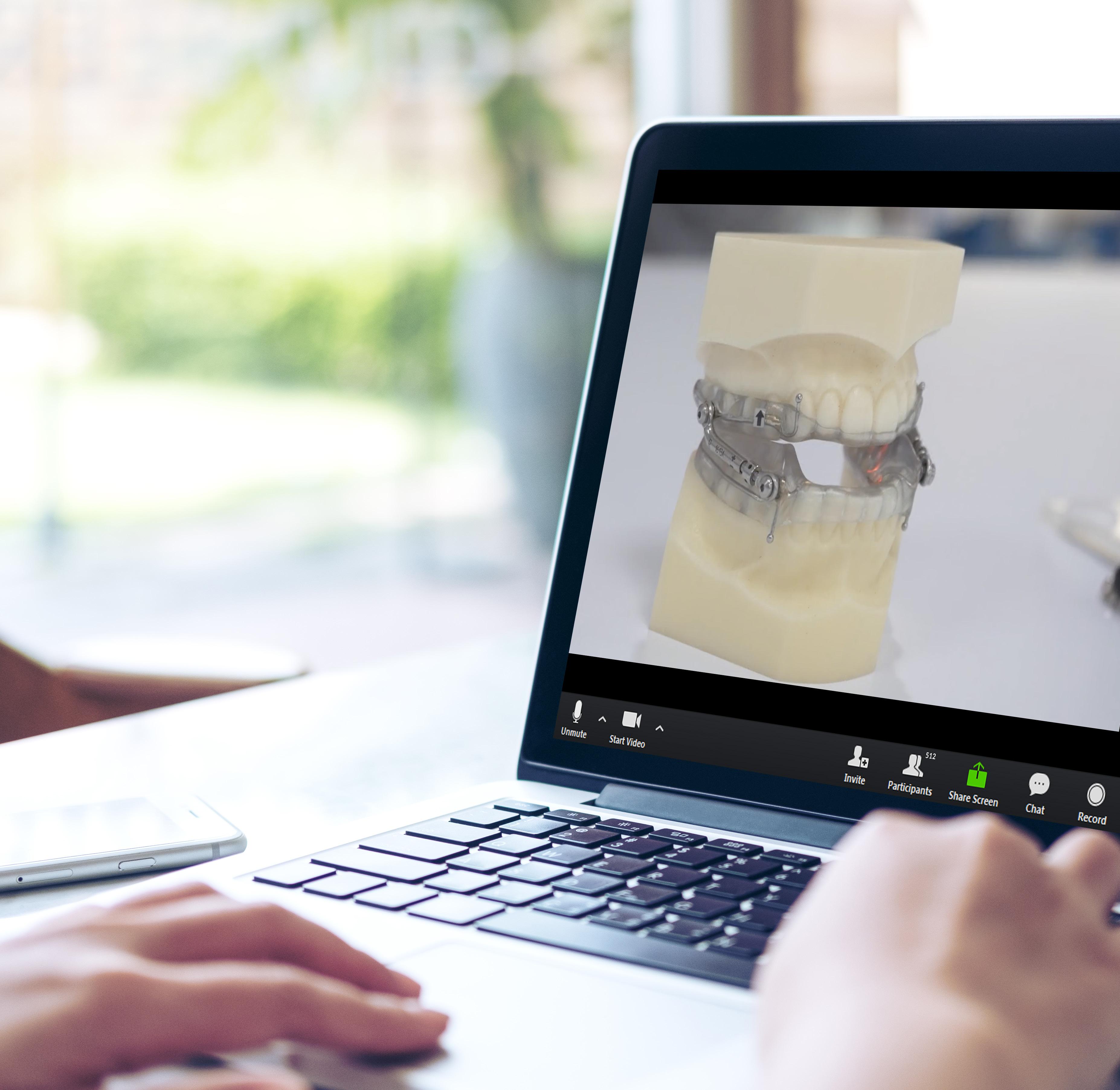
Virtual Seminars- Engage in the Campus Experience Online with the Entire Team
New format provides the same dynamic CE content as campus seminars – but with online flexibility
The new virtual Spear Seminar format allows you to refine your clinical skills following the same lessons that you would at the Spear Campus in Scottsdale — but from anywhere, as a safe online alternative to large-attendance campus events.
Experience the same clinical dental CE seminars as you would in Scottsdale, but in the safe and comfortable atmosphere of home – in shorter hours, with more opportunity to connect with faculty and share on-demand recordings with your practice team.
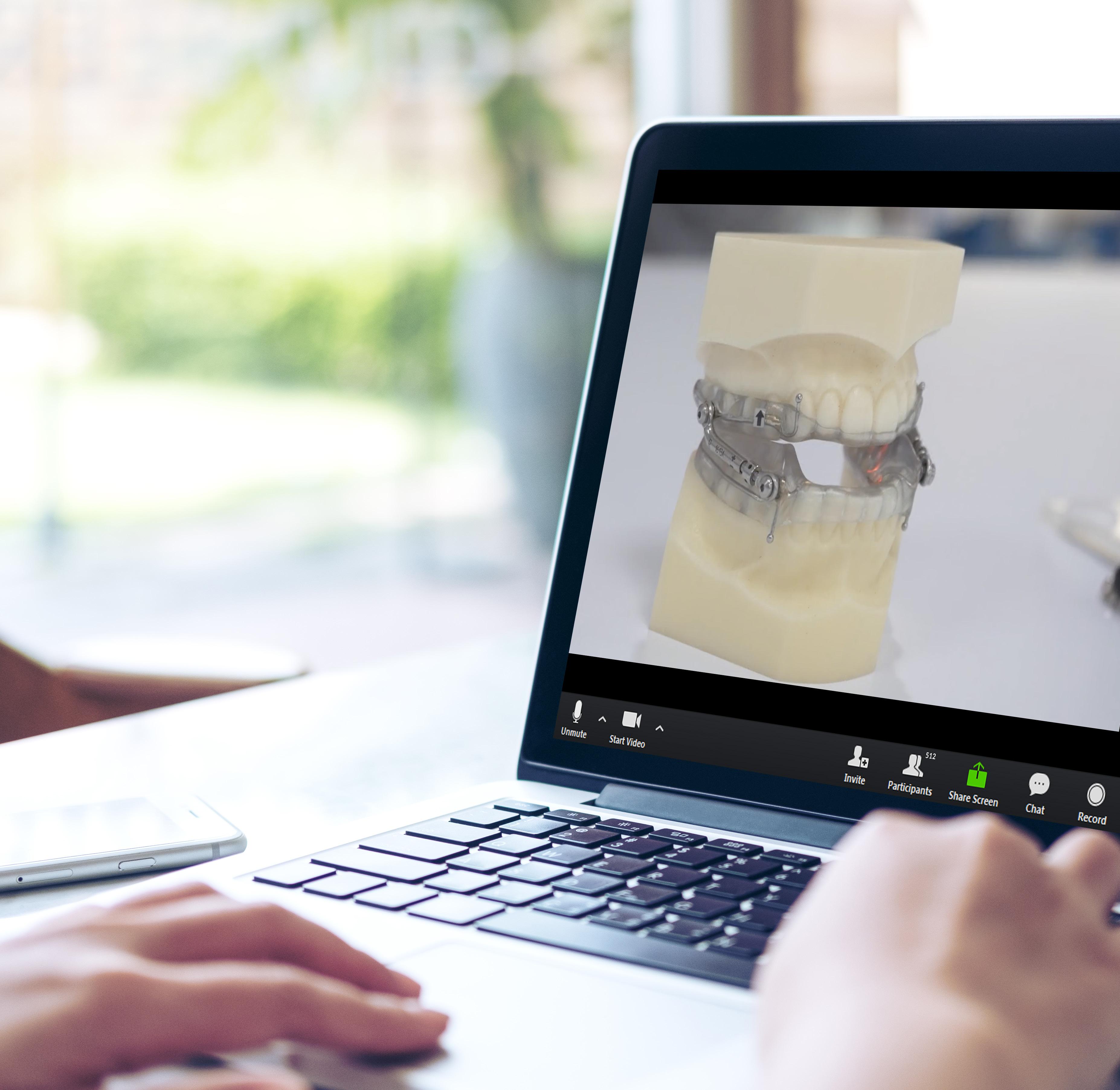
What would your practice team like to accomplish next? New dates are now available.
Register for the Spear Seminar that addresses your clinical needs and works with your schedule at SPEAREDUCATION.COM/VIRTUAL-SEMINARS
STRENGTH
Material strength is often compared by flexural strength and fracture toughness as it may be rationalized that higher strength may reduce the potential for chipping and fracture. The veneering porcelain on the surface of porcelain fused to metal (PFM) crowns has a flexural strength in the range of 90-100 MPa.
High strength ceramics such as lithium disilicate or zirconia-reinforced lithium silicates have flexural strengths in the range of 350-475 MPa with a fracture toughness of 3.2 to 3.5 MPa/m2. Zirconia (3 mol%) has a flexural strength in excess of 900 MPa and a fracture toughness of 5.5 to 7.4 MPa/ m2. The significant increase in strength of zirconia is perceived to be an advantage for longevity, however this still needs to be supported by long-term clinical evidence.
The strength of the ceramic material is often cited as a critical element in the success of the restoration. A laboratory study illustrates an important point about material strength. (Nakamura 2015) The minimum occlusal reduction for 3 mol% zirconia is generally 1.0 mm and for 4 mol% zirconia 1.2-1.5 mm thick due to the reduced flexural strength. The fracture rate of monolithic zirconia crowns (Lava Plus) were compared to lithium disilicate crowns (e. max Press) at different axial (0.5, 0.7, and 1.0 mm) and occlusal thicknesses (0.5, 1.0, and 1.5 mm).
Axial reduction did not significantly influence the fracture rate of either type of crown. However, there was a significant difference in the strength of the monolithic zirconia crowns based on the occlusal thickness. Reducing the occlusal thickness of the crowns resulted in a significant decrease in fracture resistance. This illustrates that one must consider the minimum thickness or volume of material required to maintain the desired strength of a material.
In essence, strength is a conditional property, meaning it depends on an adequate thickness or volume to have the reported strength. Use of the material without regard to its recommended dimensional thickness does not ensure the expected level of material strength and may compromise the clinical outcome.
A study done by investigators at the American Dental Association compared the flexural strengths of zirconia from dental laboratories. (Liao 2018) Dental laboratories were asked to submit two zirconia samples. One sample was of the laboratory’s anterior (high translucency) zirconia and one sample from the laboratory’s posterior (low translucency) zirconia.
Posterior zirconia samples had a mean flexural strength of 492 + 199 MPa and anterior zirconia samples had a mean flexural strength of 563 + 136 MPa. The authors speculated that the variation in flexural strengths was due to differences in zirconia materials, differences in processing techniques or a combination of both.
While the small sample size from each dental laboratory was not statistically significant, the results lend credence to the importance of material and processing relative to expected strengths of zirconia materials.
ZIRCONIA RESTORATIONS: EVOLUTION AND INNOVATION 15
Strength is a conditional property, meaning it depends on an adequate thickness or volume to have the reported strength
ESTHETICS
The translucency of a material is an important contributor to its potential esthetic applications.
When light strikes a polycrystalline material (zirconia), a portion of the light is reflected away from the surface, a portion is transmitted through the material, and a portion is scattered or absorbed into the bulk of the material. The amount of light that is transmitted is a measure of translucency and is related to the reflectivity of the surface with smoother surfaces reflecting more light. It is also related to how much light is scattered as it passes through the material with more scattering causing a more opaque appearance.
Light scattering occurs as it passes through a material and it changes direction. This may be caused by impurities, defects, different crystalline phases, and grain boundaries. To make monolithic zirconia more translucent and aesthetic, the light scattering from the zirconia must be significantly eliminated. (Kontonaski 2019)
One disadvantage of 3 mol% zirconia is that the larger grain size of the tetragonal crystalline particles leads to greater light scattering and less translucency. (Sulaiman 2015) The lack of translucency also limits 3 mol% zirconia chameleon effect of absorbing surrounding tooth color as well as more translucent glass ceramic restorations.
The increased zirconia opacity also lends a brighter appearance to the zirconia crown. It can be somewhat problematic to decrease the value of the crown with surface stains and glaze. And the increased opacity of the zirconia also prevents the cement color from influencing the final shade of the crown. The addition of a higher proportion of cubic crystalline phase in translucent or anterior zirconia (5 mol%) effectively reduces the grain sizes and decreased scattering of the light, which allows more light to be transmitted, improving the translucency.
Translucency of ceramic materials has been well documented in laboratory studies. One study measured the translucency of zirconia core materials compared to lithium disilicate ceramic in equal thicknesses. The translucency of zirconia copings was significantly less than that of the lithium disilicate glass-ceramic control as one would expect of 3 mol% zirconia.
(Balidissar 2010)
A more recent study compared the translucency of lithium disilicate ceramic (IPS e.max CAD HT) to four different high translucency zirconia in 0.5 mm, 1.0 mm, 1.5 mm, and 2.0 mm thick specimens. (Church 2017) Lithium disilicate had significantly higher translucency than translucent zirconia materials at similar thickness. The translucencies of the zirconia materials were fairly similar at each thickness, however translucency significantly decreased for each zirconia material at each increase in thickness.
These results are consistent with the general perception that zirconia is a more opaque material than glass ceramics at the same thickness. But ceramic materials are recommended to be 1.5 mm thick occlusally while zirconia materials are recommended to be 1.0 mm thick occlusally. The authors noted that at clinically recommended thicknesses, the translucency parameters of the translucent zirconia materials were not only similar to those of the lithium disilicate ceramic material but also comparable to the translucency parameters reported for 1.0 mm of dentin or enamel.
ZIRCONIA RESTORATIONS: EVOLUTION AND INNOVATION 17
Light scattering occurs as it passes through a material and it changes direction. This may be caused by impurities, defects, different crystalline phases, and grain boundaries.
ZIRCONIA SURFACE WEAR
Occlusal surface wear is often perceived as a function of material hardness. Basically, the harder the material, the greater the opposing abrasive wear potential. Zirconia is a very hard material that has been thought to be very abrasive to opposing tooth structure. However, wear is actually a function of material smoothness. (Miyazaki 2013)
Any material surface magnified enough will appear as a series of peaks and valleys rather than a mirror-like surface. The peaks act as abrasive areas for the opposing dentition. The smoother the material surface, fewer peaks as it were, the less abrasive wear against the opposing dentition. The clinical goal for zirconia would be to create a smooth surface to prevent abrasive wear of the opposing dentition.
There are several points of view as to the optimum technique to create a smooth zirconia restoration. Oven firing a ceramic glaze to the zirconia may create a smooth surface since the ceramic glaze will flow across the valleys of a rough surface, self-leveling into a smooth surface once it is fired. However, the glass-containing glaze is a thin layer of about 100 microns and will wear over time in function. This would expose a potentially rough surface of the zirconia, possibly leading to abrasive wear of the opposing dentition.
For this reason, it has been recommended to polish the occlusal surface of the zirconia prior to glazing it. This would remove the peaks and valleys and maintain the smooth surface in spite of the wear of the glass-containing glaze layer. Polishing proximal surfaces may not be as critical due to the lack of functional wear on these areas.
A second point of view holds that even if the surface of the zirconia is polished, it will also wear, resulting in the same surface profile as if the glaze were applied and degraded during function. However, zirconia is relatively resistant to wear due to its high fracture toughness.
Surface wear of materials generally involve some degree of degradation of the material as it is slowly worn down through microfractures of the material surface. Zirconia has a high fracture toughness, preventing these microfractures of the surface, and thereby maintaining its rough and potentially abrasive surface once the glaze has been worn away.
Laboratory studies have demonstrated that polished monolithic zirconia has the least abrasive surface and sandblasted and glazed zirconia causes the highest functional abrasion of the opposing enamel. (Stawarczyk 2013, Mitov 2012) Additional studies have reported that polished monolithic zirconia is less abrasive compared to classic veneering ceramic (Jung 2010, Park 2014) or lithium disilicate.
(Rosentritt 2012)
A second aspect of the surface finishing is concerning an occlusal adjustment of a zirconia crown post-cementation. Any adjustment to the occlusal surface of the zirconia must be repolished to return the smooth surface to the restoration. Failure to do so may result in abrasive wear of the opposing dentition. (Sabrah 2013, Chong 2015)
Most of the evidence for the wear caused by zirconia is a result of laboratory studies with simulated occlusal function systems. One recent systematic review of clinical studies related to the antagonist enamel wear of monolithic zirconia posterior crowns included five clinical studies after review of 198 potential publications. (Gou 2019)
The results reported by these studies varied widely but in general the antagonist wear due to zirconia was similar to that of natural teeth and less than that of metal-ceramics. Additional long-term clinical research is needed to confirm these findings for newer translucent zirconia.
ZIRCONIA RESTORATIONS: EVOLUTION AND INNOVATION 19
CONCLUSION
The evolution of full contour zirconia illustrates the continued effort to improve the material for expanding clinical applications. The high strength properties of the initial 3 mol% zirconia are very desirable to clinicians since it prevents the most common failure of glass ceramics: chipping and fracture.
It may be an advantage in high-stress clinical situations with potentially limited inter-arch space to create the occlusal reduction required for glass ceramic restorations. However, the esthetic properties required improvement. Newer zirconia materials continue to improve the translucency and esthetic outcomes. However, it is also obvious that there is a significant difference in the ensuing physical properties of newer zirconia formulations.
Physical properties and laboratory studies do not provide sufficient evidence of clinical success. But the differences in physical property values between 3 mol%, 4 mol%, and 5 mol% zirconia offer reasonable evidence that they should not be considered equivalent materials. Clinical evidence needs to be collected to provide insight as to the optimum applications of these materials.
ZIRCONIA RESTORATIONS: EVOLUTION AND INNOVATION 21
REFERENCES
Pjetursson BE, Sailer I, Zwahlen M, Hämmerle CHF. A systematic review of the survival and complication rates of all-ceramic and metal-ceramic reconstructions after an observation period of at least 3 years. Part I: Single Crowns. Clin Oral Implants Res 2007 Jun;18 Suppl 3:73-85. doi: 10.1111/j.16000501.2007.01467.
Makhija SK, Lawson NC, Gilbert GH, Litaker MS, McClelland JA, Louis DR. Dentist material selection for single-unit crowns: Findings from the National Dental Practice-Based Research Network. J Dent 2016;55:40-7.
Sailer I, Makarov NA, Thoma DS, Zwahlen M, Pjetursson BE. All-ceramic or metalceramic tooth-supported fixed dental prostheses (FDPs)? A systematic review of the survival and complication rates. Part I: Single crowns (SCs). Dent Mater. 2015 Jun;31(6):603-23. doi: 10.1016/ j.dental.2015.02.011.
Lawson NC, Burgess JO. Dental ceramics: a current review. Compend Contin Educ Dent 2014 35(3):161-166.
Albashaireh, ZSM. Ghazal M, Kern M. Two-body wear of different ceramic materials opposed to zirconia ceramic. J Prosthet Dent 2010 104:105–113.
Grin, J.D. Combining monolithic zirconia crowns, digital impressioning, and regenerative cement for a predictable restorative alternative to PFM. Compend. Contin. Educ. Dent. 2013, 34, 212–222. [PubMed]
Helvey GA. What is in your zirconia? Compendium Apr 2017, 38(4): 213-217.
Zhang Y and Lawn BR. Novel Zirconia Materials in Dentistry. Journal of Dental Research 2018 Vol. 97(2) 140–147.
Pittayachawan P, McDonald A, Young A, Knowles JC. Flexural strength, fatigue life, and stress-induced phase transformation study of Y-TZP dental ceramic. J Biomed Mater Res B Appl Biomater 2009 88:366–77.
Zhang F, Inokoshi M, Batuk M, Hadermann J, Naert I, VanMeerbeek B, Vleugels J. 2016. Strength, toughness and aging stability of highly-translucent Y-TZP ceramics for dental restorations. Dent Mater. 32:e327–e337.
McLaren EA, Lawson N, Choi J, Kang J, Trujillo C. New high-translucent cubicphase–containing zirconia: clinical and laboratory considerations and the effect of air abrasion on strength Compend Contin Educ Dent. 2017 Jun;38(6):e13-e16.
Burgess JO. Zirconia: the material, its evolution, and composition. Compendium Oct 2018, Vol 39, Spec issue 4, pgs 4-8.
Nakamura K, Harada A, Inagaki R et al Fracture Resistance of monolithic zirconia molar crowns with reduced thickness. Acta Odontol Scand 2015; 73(8):602-608.
Liao Y, Lukic H, McLees J, Boghosian A, Megremis S. Survey of flexural strength consistency of zirconia specimens from multiple dental laboratories. J Dent Res 97 (Spec Issue A): abstract #1302, 2018
Kontonasaki E, Rigos AE, Ilia C, Istantsos T. Monolithic zirconia: An update to current knowledge. optical properties, wear, and clinical performance. Dent J. 2019 Sep 2;7(3):90. doi: 10.3390/dj7030090.
Sulaiman TA, Abdulmajeed AA, Donovan TE, et al. Optical properties and light irradiance of monolithic zirconia at variable thicknesses. Dent Mater. 2015;31(10):1180-1187.
Baldissara P, Llukacej A, Ciocca L, Valandro FL, Scotti R. Translucency of zirconia copings made with different CAD/CAM systems. J Prosthet Dent. 2010;104(1):6-12.
Church TD, Jessup JP, Guillory VL, Vandewalle KS. Translucency and strength of high-translucency monolithic zirconium oxide materials. Gen Dent 2017 Jan/Feb: 48-52.
Miyazaki T, Nakamura T, Matsumura H, et al. Current status of zirconia restoration. J Prosthodont Res 2013;57:236-261.
Stawarczyk B, Ozcan M, Schmutz F, et al. Two-body wear of monolithic, veneered and glazed zirconia and their corresponding enamel antagonists. Acta Odontol Scand 2013; 71: 102-112.
Mitov G, Heintze SD, Walz S, Woll K, Muecklich F, Pospiech P. Wear behavior of dental Y-TZP ceramic against natural enamel after different finishing procedures. Dent Mater. 2012 Aug 1;28(8):909–18.
Jung YS, Lee JW, Choi YJ, et al. A study on the in-vitro wear of the natural tooth structure by opposing zirconia or dental porcelain. J Adv Prosthodont 2010; 2: 111-115.
Park JH, Park S, Lee K, et al. Antagonist wear of three CAD/ CAM anatomic contour zirconia ceramics. J Prosthet Dent 2014;111:20-29.
Rosentritt M, Preis V, Behr M, et al. Two-body wear of dental porcelain and substructure oxide ceramics. Clin Oral Investig 2012;16:935-943.
Sabrah AH, Cook NB, Luangruangrong P, et al. Full-contour Y-TZP ceramic surface roughness effect on synthetic hydroxyapatite wear. Dent Mater 2013;29:666-673.
Chong BJ, Thangavel AK, Rolton SB, et al. Clinical and laboratory surface finishing procedures for zirconia on opposing human enamel wear: A laboratory study. J Mech Behav Biomed Mater 2015;50:93-103.
Gou M, Chen H, Kang J, Wang H. Antagonist enamel wear of tooth-supported monolithic zirconia posterior crowns in vivo: A systematic review. J Prosthet Dent. 2019 Apr;121(4): 598-603. doi: 10.1016/j.prosdent.2018.06.005. Epub 2018 Dec 1.
ZIRCONIA RESTORATIONS: EVOLUTION AND INNOVATION 23
AUTHOR ABOUT THE
Dr. Fasbinder is currently the Director of the Computerised Dentistry Program and a clinical professor in the Department of Cardiology, Restorative Sciences and Endodontics, University of Michigan, School of Dentistry. He is board certified in general dentistry and maintains a part-time private practice in Ann Arbor, Michigan.
Dr. Fasbinder directs the Computerised Dentistry Unit at the University of Michigan School of Dentistry that is dedicated to research and education on CAD/CAM dental systems. The CompuDent Unit has been a leader in education and research with the chairside CAD/CAM systems and digital impression systems since 1993 resulting innumerous publications.
Dr. Fasbinder is a frequent speaker on ceramic-based dentistry and digital dental systems at meetings and conferences in North America and abroad.
Dennis J. Fasbinder, D.D.S.

Based in Scottsdale, Arizona, Spear Education is an innovative dental education company that includes the following practice-building, member-based services:
Spear Online
The “Gateway to Great Dentistry” includes more than 1,500 video lessons spanning restorative, esthetics, occlusion, worn dentition, treatment planning and more. But access is not only for dentist continuing education. Membership provides the entire office team with staff training, team meeting and patient communication tools — like the Patient Education platform and native apps, in addition to “Conversation Essentials” video vignettes — to align the entire practice on patient care.
Spear Study Club
Involves small groups of peers that meet locally as many as eight times a year to collaborate on real-world cases, improve their clinical expertise and discuss growing practice profitability. Spear has the largest network of study clubs, with active clubs in more than 40 states and six countries.
Spear Practice Solutions
The technology-enabled business and clinical solutions platform blends custom education, personalized coaching and real-time analytics to help your practice reach its full potential.
Spear Campus
Thousands of dentists visit Spear’s scenic Scottsdale campus annually for seminars and workshops. Members attend sessions in a state-of-the-art, 300-person lecture hall and receive hands-on training in Spear labs.
Spear Faculty Club
Designed as a prestigious community of doctors who share the journey to Great Dentistry with others. While all Faculty Club members demonstrate a commitment to continued learning, professional growth and providing the best patient care, many also serve as Visiting Faculty and mentor attendees during campus seminars and workshops.
25


 By Dennis J. Fasbinder, D.D.S.
By Dennis J. Fasbinder, D.D.S.