A PUBLICATION FOR EMPLOYEES OF STANFORD HOSPITAL & CLINICS
ISSUE SEVEN / SPRING 2014
THE STANFORD NURSING EFFECT LIFE FLIGHT & E2 GOOD WORKS
from the CEO
PAGE TWO News and Notes From Around SHC...
Dear Colleagues, I am especially pleased to introduce you to this issue, which is focused on the amazing nurses of Stanford Hospital & Clinics. Our more than 2,000 nurses are the lifeblood of our organization and truly distinguish Stanford. They are a continued source of knowledge, care, courage, inspiration, support, kindness and compassion for the tens of thousands of patients we see every year. Moreover, their roles at Stanford are constantly expanding, as nurses become leaders in management, technology, quality, safety, research and other areas. In this issue you will also gain inspiration from our nurses in stories about what they do in their free time, such as volunteering on medical missions around the globe, or running 26.2 miles, swimming 2.4 miles and biking another 112 miles in an Ironman triathlon, for “fun.” Simply put, we would not exist without our esteemed group of nursing professionals, and I thank all of them for everything they do for our patients, and for us, every day.
Sincerely, AMIR DAN RUBIN PRESIDENT & CEO
Health Matters, a Stanford Medicine Community Day, will be held May 10 from 9 am to 2 pm at the Li Ka Shing Center. The event, which is free and open to the public, explores the latest advancements in medicine and the health topics that matter most to you and your family. To register, or for more information, please visit healthmatters.stanford.edu … Twenty years ago this June, a patient with cancer that had spread to her brain became the first person treated with a new radiation delivery device some had dubbed “Adler’s Folly.” Officially known as a CyberKnife, the device was designed by Stanford neurosurgeon John Adler to treat brain cancer that couldn’t be surgically removed. That first patient has been followed by more than 200,000 others worldwide … The Outpatient Center in Redwood City will once again be the site for free skin cancer screenings to the community on Saturday, May 31, from 8 to 11:30 am. Last year, more than 350 screenings were given … The Stanford Ear Institute is
scheduled to open in late June, sharing a building with the Byers Eye Institute on Watson Court. The SEI will provide multidisciplinary care for a wide variety of ear problems, including hearing loss, ear infections, ear tumors and balance disorders. “The new center is a joint effort between the adult and children’s hospitals to bring together all hearing and balance specialties into a single setting to create a smoothly integrated pathway for patients to receive all services in one location,” said Robert Jackler, MD, Otolaryngology Department Chair … Stanford will open another new primary care site this summer. Stanford Primary Care, Los Altos is scheduled to open in July at 960 N. Antonio Road, adding to the hospital’s current lineup of faculty practices which includes Portola Valley and Hoover Pavilion … Wondering what it takes to build an 824,000-squarefoot hospital? Tours of the future Stanford Hospital construction site take place each Thursday from 3 to 4 pm. Sign up at futurehospital. org/construction-tours.
STANFORD HOSPITAL PEOPLE IS PUBLISHED BY
SHC OFFICE OF COMMUNICATIONS GARY MIGDOL EDITOR, DIRECTOR OF INTERNAL COMMUNICATIONS KATIE LIPOVSKY, COMMUNICATIONS SPECIALIST ASHLEY GEORGIAN MEDIA RELATIONS MANAGER GRACE HAMMERSTROM CONTRIBUTING WRITER JAMES LARKIN DIRECTOR OF CORPORATE COMMUNICATIONS/PR SARA WYKES CLINICAL AFFAIRS WRITER NORBERT VON DER GROEBEN PHOTOGRAPHY
Send comments and story ideas to communications@stanfordmed.org
2
STANFORD HOSPITAL PEOPLE / ISSUE SEVEN 2014
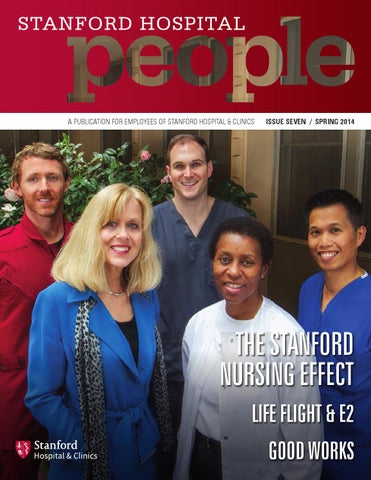
ON THE COVER: RNs’ impact at SHC is visible in many ways. Here’s a sampling (L to R) – Jonathan Gardner, Life Flight; Joan Forte Scott, administration; Jake Robinson, D1; Robinetta Wheeler, Wound and Ostomy; and Joel Jay Baluyot, OR.
C E L E B R A T I N G N A T I O N A L N U R S E S W E E K M A Y 6 – 12
THE STANFORD
NURSING EFFECT
New Skills, Advanced Education, Quality Improvement and Research Broaden the Nursing Team’s Contribution to Modern Medicine
M
ORE THAN 100 YEARS AFTER THE FIRST STAN FORD HOSPITAL BEGAN
ACCEPTIN G PATIEN TS, MODERN
NURSING AT STANFORD IS A PROFESSION DEFINED BY
A BROAD AND DEEP DIVERSITY OF ROLES AND RESPONSIBILITIES FAR BEYOND THOSE EARLY YEARS. As we celebrate National Nurses Week this month, we honor the
2,000-strong body of Stanford nurses. They are women and men whose RNS KATIE STEPHENS (L) AND KISHORE PARMER (R) ON B3. STEPHENS, WHO CAME TO SHC AS A TRAVELING NURSE, WAS RECENTLY NAMED ASSISTANT PATIENT CARE MANAGER FOR B1.
CONTINUED ON PAGE 4
STANFORD HOSPITAL PEOPLE / ISSUE SEVEN 2014
3
CONTINUED FROM PAGE 3
care for patients is respected and recognized. These professionals, with knowledge-backed compassion and patient care skills, conduct research that improves the quality of care. They lead collaborative, multidisciplinary groups toward new services. Many have earned advanced certification in their care specialties; many have earne advanced degrees. It would be easier to say where they are not contributing than to do a quick tally of those contributions. What characterizes nursing at Stanford is support for knowledge. Elvie Wohlers, RN, after 33 years in North ICU, handled the transformation of medicine from paper to digital and pursued validation of her experience. In 2012, she was one of 279 nurses in the United States who earned an advanced care certificate in cardiac surger . The year before, she was one of North ICU’s Magnet champions, working with her colleagues to prepare for the visit of Magnet appraisers gauging whether the hospital was worthy to be recognized for a second time with nursing’s most prestigious award. It was. It’s a status only earned by 7 percent of health care organizations in the United States. That support for knowledge is what Katie Stephens,
“ I noticed a huge difference in the amount of support nurses received here. I felt my manager trusted me, my personal opinions and my decision-making.” to fix that, with the full support of her manager and th unit’s physicians. respiration—and found a way to fi that, with the full support of her manager and the unit’s physicians. At Stanford, it’s easy to see those broader, deeper roles for nurses. Kim Pardini-Kiely, BS, MS, the hospital’s vice president for quality and effectiveness, quickly found in her first nursing job that she enjoyed caring for patients an teaching them, too. When her nurse manager took time off for maternity leave, Pardini-Kiely was asked to fill tha job. “I got the bug for management and for improvement,”
RN, who began at Stanford as a traveling nurse liked
she said. She looks around at Stanford’s nursing team
so much that she stayed. She was recently named
and sees “a cadre of experienced leaders we are lucky to
as an assistant patient care manager for B1. When
have. Here we have an opportunity to move beyond the
she arrived, she said, “I noticed a huge difference in
typical assumptions.”
the amount of support nurses received here. I felt my
Some of that assumption breaking is now organized by
manager trusted me, my personal opinions and my
David Pickham, RN, MS, PhD, at Stanford nearly a year
decision-making.” She was part of a patient safety
as its director of transdisciplinary research. His job, he said,
team in B3/C3 that saw a problem with identification o
is to “gather everyone around the table so everyone’s voice
deterioration in patients’ respiration— and found a way
is heard, sharing knowledge and information informed
CLARISSA OWENBY HAS BEEN A NURSE ON B2 FOR 18 YEARS
4
STANFORD HOSPITAL PEOPLE / ISSUE SEVEN 2014
ELVIE WOHLERS HAS WORKED THE PAST 33 YEARS FOR NORTH ICU.
NURSES
BY THE NUMBERS
by each person’s background.” The group he wants to gather will include not only nurses, but also every other nonphysician in the hospital. Nurses led many research
NUMBER OF RNS AT SHC
projects at Stanford before Pickham arrived. Now their
NURSE PRACTITIONERS
2,094 137
reach and impact will expand. “Together,” Pickham said, “we inform each other.” Lisa Meyer, RN, began as a bedside nurse who volunteered to dive into the information technology of electronic medical record systems without even knowing how to turn on a laptop. Now she is the director of the hospital’s inpatient systems and services. Her team designs and builds EPIC’s EMR based on the workflow of all thos who care for patients. “We are transforming the care system in everything from follow-up phone calls to video visits,” she said. “Nurses are part of that because they are at the bedside every day.”
RNS WITH AN ADVANCED DEGREE
RNS WITH ADVANCED CERTIFICATION
RNS WITH A BSN OR HIGHER
INVOLVED IN LEADERSHIP COUNCILS
373 807
1,681 227
“A lot of nursing has been a soft science,” said Joan Forte Scott, MBA, BSN, RN, who transitioned from bedside nurse through an impressive list of management responsibilities. Now, she is administrative director
GLOSSARY OF TERMS
of patient and community engagement. “Finally, we’re demonstrating that those soft aspects of care have a quantifiable and significant impact on health and heali
.”
For all the changes in technology and organization, however, Wohlers said the human component is still the same. “Sensitivity,” she said. Clarissa Owenby, RN, believes other behavior matters, too. “First and foremost,” she said, “listening to the patient.” D1’s Jake Robinson, RN, had trained as an EMT and paramedic in preparation for a career as a firefight . He’d never considered nursing. “I did not see myself as a compassionate person,” he said, “until I started nursing.”
VAT—Value Analysis Team A hospital-wide program that includes teams from Patient Care Services and others, tasked with finding savings opportunitie in purchasing, utilization, and procurement and acquisition.
HATS—Handle All Transfers Safely SHC’s Safe Patient Handling Program teaches coaches, nurses, and caregivers best practices for lifting and moving patients.
Magnet The highest honor for nursing excellence; SHC was first designate as a Magnet hospital in 2007 and was re-designated in 2012.
Role-Based Practice A professional practice model designed for nurses to re-examine one’s own practice behaviors against best practice standards.
Professional Practice Model A schematic model that describes how nurses practice, collaborate, communicate and develop professionally to provide the highest quality care.
Shared Leadership Councils SHC’s model for shared decision-making, the Shared Leadership Council structure is composed of several councils from all areas of nursing practice and the interdisciplinary team. LISA MEYER BEGAN HER CAREER AS A BEDSIDE NURSE BUT IS NOW SHC’S DIRECTOR OF INPATIENT SYSTEMS AND SERVICES.
STANFORD HOSPITAL PEOPLE / ISSUE SEVEN 2014
5
FOCUS ON...
LIFE FLIGHT Celebrating 30 Years of Airborne Transport It was May 1984. A 70-year-old woman critically injured in a car accident in Santa Cruz County became Stanford Life Flight’s inaugural mission. With that flight Life Flight became the first helicopte emergency services program in the Bay Area; and Stanford Hospital and Clinics became the first medical center in thi region to have its own helicopter and air medical transport team. Thirty years and many thousands of flights late , Life Flight has an enviable history to celebrate this month. It can also boast one of the most experienced crews, whose attitudes explain why Life Flight is still going strong. “We are always moving forward,” said David Bevin, RN, a 20-year veteran. “There is always some new technology.” To be considered for this crew requires years of experience, clinical qualification and interpersonal skills. The team maintains its expertise through ongoing
6
STANFORD HOSPITAL PEOPLE / ISSUE SEVEN 2014
TWO OF SHC’S LONG-TERM LIFE FLIGHT NURSES ARE GERALYN MARTINEZ (L) AND DAVID BEVIN (R).
“ A patient wrote me a very nice letter to say thanks … because I leaned over her and said ‘You’re going to be OK. You’re going to make it at Stanford.’” training and continuing education. Most of the nurses have advanced certifications; several have graduat degrees. “It’s a very collaborative, team-centered approach,” said Geralyn Martinez, RN, a 24-year veteran Life Flight nurse, “and it’s very intense.” That technology Bevin mentioned touches almost every part of what Life Flight does. It now has a faster, larger helicopter than its first model, wit medical equipment that is compact, lightweight, and rugged. Stanford’s Life Flight is the only program in Northern California able to transport critically ill cardiac patients. Its helicopter is now equipped with instrument-aided and night flight vision goggles to aid visibilit and improve safety.
“Stanford has always been regarded as one of the premier programs in the state, if not the country,” said Life Flight’s program manager, Michael Baulch, RN, JD. “We’ve seen the technology change over time, but Stanford has kept its focus on safety and on the best use of this very expensive asset.” Beneath all the technology and specialized training, however, remains the power of a calming voice. “A patient wrote me a very nice letter to say thanks,” Bevin said, “because I leaned over her and said, ‘You’re going to be OK. You’re going to make it to Stanford.’ ”
DID YOU KNOW? Life Flight may launch as many as three times a day for an average of 700 flights annuall
FOCUS ON...
E2 Compassionate Care for Complex Patients To an outsider, E2 would probably look like any other nursing unit: It has a nursing station within sight of white boards that chronicle the room number, the patient initials and the names of each patient’s care team. On this unit, however, a calculated quiet rules the public space. No call lights ring: nurses remain in patient rooms. E2 is the hospital’s medical/surgical/neuro/ trauma/liver transplant ICU. Its intense activity happens behind the sliding glass doors of each patient’s room. E2, with 33 beds, has such a low ratio of patient to nurse (1:1 or 1:2) that 170 nurses are needed to cover two shifts for the 24/7 critical care given to its patients. Those in the most critical condition may have up to three or four nurses caring for them. To maintain continuing care, E2’s float nurses move from room to room t give breaks to staff nurses, to help with emergencies, and to accompany patients to CT, MRI and Cath-Angio.
CYNTHIA PARKE (L) AND MAUREEN FAY (R), E2 UNIT MANAGER.
Delivering the highest level of care possible for these patients also means that E2 has its own pharmacy and pharmacist; its own set of advanced equipment, prepped to go; and carts set up for those procedures typical for patients in this type of unit.
“ I feel blessed to be here. The teamwork is spectacular. I like the complexity of the situations we have to decipher.” Maureen Fay, RN, MSN, is E2’s patient care manager. She is relatively new to the patient care manager job but by no means new to nursing. She is following a family tradition: her grandmother, mother-in-law and grandmother-in-law are all nurses. She also knows the unit well: She was one of E2’s assistant patient care managers for more than eight years and a staff nurse on E2 for more than three years. She was drawn to critical care early on, she said, “because patients were complex and you
DID YOU KNOW? PERCENTAGE OF E2 NURSES IN UNIT FOR OVER 10 YEARS:
40%
PERCENTAGE OF E2 NURSES IN UNIT FOR OVER 20 YEARS:
20%
can actually do things that make a difference right away.” “I feel blessed to be here,” said Elizabeth Borgueta, RN, part of the unit for six years. “The teamwork is spectacular.” She, like other E2 nurses, is not afraid of the medical challenge that E2’s patients represent. “I like the complexity of the situations we have to decipher,” said her colleague Stephanie Flowers, RN, part of the unit for 10 years. STANFORD HOSPITAL PEOPLE / ISSUE SEVEN 2014
7
SHC’S GOT TALENT Iron Woman Growing up with a twin brother, Merriam Young, MS, RN, played sports from a young age and competed successfully in swimming in high school. Five years ago, she took her affinity for athletics to a higher level. She starte running half marathons and quickly transitioned to competing in Ironman triathlons. After just six months of training, Young completed a 70.3-mile half Ironman (1.2-mile swim, 56-mile bicycle ride and 13.1-mile run). “After that I was hooked,” she says. “They say that triathlons are addicting—and it’s true!” When her trainer and good friend suggested they do a full Ironman—2.4-mile swim, 112-mile
“ I did not believe I could ever complete that distance. It was the most amazing experience of my life.” bicycle ride and 26.2-mile run—she was quick to decline. “I did not believe I could ever complete that distance,” she recalls. Her friend’s persistence and her own competitive nature won out. At the peak of her training schedule,
Destined to Dance BMT nurse Chariss Ilarina, RN, says she was destined to dance. Her parents, both members of dance troupes in their native Philippines and in the U.S., instilled a love of dance in their daughter, enrolling her at dance school at age five. As a young girl, she studied and competed in tap, ballet, and jazz, before trying Russian folk ballet. “That was my first experience with folk dance, and I found more strength in it than classical ballet,” she says. In high school, Ilarina joined the Likha Pilipino Folk Ensemble of San Francisco, a nonprofit organization that spreads Philippine culture through music and dance. She was made a soloist early on and given a lot of principal roles.
8
STANFORD HOSPITAL PEOPLE / ISSUE SEVEN 2014
Young worked out for two to three hours, fiv days a week, and all day on the weekends, while working full time as the director of Clinical Inpatient Access. She completed her first Ironman in June 2012 in 15:51:5 . “It was the most amazing experience of my life,” she says. Last November, Young finished her second Ironman in 13:35:2 , putting her in the top 10 percent in the world in her age group. After completing that race, she swore off the full Ironman but is already reconsidering. “I never say never.”
“ Working as a nurse with hematology/ oncology and bone marrow transplant patients has taught me to hold on to the things I love to do.”
“I found a love and passion for folk dance with Likha,” says Ilarina. Sixteen years later, she is a company dancer/performer and artistic dance lead. She has toured domestically and internationally with the dance company in ethnic folk dance festivals in Malta, the Philippines, Brazil, the Netherlands, France, Italy, Greece and
most recently Peru, where Likha won overall “Best Dance” and “Ms. Festival.” As a young woman, Ilarina was on a natural trajectory to pursue dance as a career but chose nursing instead. This decision continues to fuel her passion for dance. “Working as a nurse with hematology/oncology and bone marrow transplant patients has taught me to hold on to the things I love to do.”
KUDOS January Service Spotlight Award JENNIFER SEMEDO When Jennifer Semedo noticed an accident blocking the Woodside Road exit on Highway 101 in Redwood City, she knew patients headed to the nearby Stanford Medicine Outpatient Center might be stuck in the accident-related traffic. Semedo, a clinica clerical coordinator at the Dermatology Clinic, worked with the front desk staff to notify patients of the accident and to give them alternate directions to the Outpatient Center. One couple the staff reached had already left home for an appointment at the clinic. The couple was impressed that Semedo and the rest of the team had been so proactive and thoughtful: The team also had rescheduled the patient’s appointment. “They should be acknowledged for their excellent performance and outstanding actions,” wrote the patient in a letter to SHC.
February Service Spotlight Award KRISANNE HANSON, WENDOLYN DAVIS AND PATRICK MAGINOT Krisanne Hanson, Wendolyn Davis and Patrick Maginot were honored as February’s Service Spotlight award winners for providing an excellent guest experience. Krisanne was helping a woman with directions at the hospital when she learned that
the woman was waiting for a family member and she had forgotten to bring formula for her baby. Hanson walked with her to the gift shop and spoke with Davis, a sales associate. Davis made several phone calls to find the formula but could not locate it. Hanso turned to Maginot, a Patient Services Manager in the Food Services Department. He found the exact formula the woman needed and, in less than 20 minutes, delivered it to her.
February Patient Safety STAR Award MARY BAILEY, RN Known by her colleagues on D1 as a role model, Mary Bailey is a caring and conscientious nurse. She was honored as February’s Patient Safety STAR Award winner. While reviewing a patient’s clinical documentation, she recognized that a significan medical condition was not being addressed in the patient’s care. She took immediate action. Her critical decision-making skills helped to ensure the patient’s safety. Bailey’s actions made a significant difference to the patien and his family. It is clear that she takes pride in the nursing care she delivers. Her quick response is evidence of the dedication Bailey has for her patients.
March Patient Safety STAR Award SHANNON HILDEBRAND, RN, AND JUNE TILTON, RN Shannon Hildebrand and June Tilton are known as excellent patient care providers by their
colleagues on E3. They were honored with the Patient Safety STAR Award in March. By being proactive, Hildebrand and Tilton averted a medical disaster and saved a patient’s life. Hildebrand alerted Tilton after she noticed a subtle post-op change in a patient’s lab results and physical assessment. Together, they brought their concerns to the treating team. Working with the team of doctors, they started treatments, stabilized the patient and expedited a transfer to a higher level of care. The clinical skill, communication and advocacy they demonstrated in this situation show how dedicated they are to their patients.
March Service Spotlight Award ALINA WRIGHT, RN When a patient told Alina Wright that he was going to walk to the grocery store, she felt compelled to help. The patient said he planned to walk from the hospital to the store and then back to his hotel in South Palo Alto. As a nursing coordinator in Head and Neck Medical Oncology, Wright knew that the patient suffered from physical disabilities that would make the long walk difficult. After he shift, she took him to the grocery store and drove him back to his hotel. “Our patients suffer so much, to relieve the patient for one moment was all I could do,” said Wright. “That is why I became a nurse, and that is why I work at Stanford.”
Patient Satisfaction SHC hit an all-time high by reaching the 95th percentile in the most recent likelihood to recommend scores complied by the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS). Six other areas also received their highest ever ranking, including overall hospital rating (83rd percentile), pain management (78th), nurse communication (77th), MD communication (72nd), cleanliness (64th),
and call light responsiveness (63rd). Discharge information had its highest rating since 2010 (77th). Stanford was also honored as an Outstanding Patient Experience Award winner for 2014. Only 15 percent of hospitals nationally received this designation, which is based on how a hospital’s patients responded to the HCAHPS survey for visits occurring between April 2012 and March 2013. STANFORD HOSPITAL PEOPLE / ISSUE SEVEN 2014
9
GOOD WORKS In the Community Making a Difference When Esther Yu, BSN, RN, arrived at Stanford Hospital three years ago, she became instantly recognizable by her decorative ID badge. Yu had fashioned flowers made out of recycled medicatio lids and clipped them to her ID. When colleagues and patients began asking her to make pieces for them, she enlisted the help of fellow nurse Chris Tucker, RN, to meet the demand. The crafty duo also sent 150 handcrafted magnets to the kids at Camp Kesem, a program run by Stanford University students for children with a parent or guardian with cancer. As nurses in the Infusion Treatment Area, they raised awareness of the camp with their patients whose children could benefit Yu is also actively involved in San Francisco’s Freedom House, a shelter for victims of human traffickin . As an advocacy volunteer, she builds awareness of the services offered to such victims and helps raise funds for the organization. “When I think of young girls whose futures are taken away, I feel like I have to do something,” says Yu. A three-week trip to West Africa last summer solidifie her commitment to helping others. She went as part of a medical mission with the Mercy Ship, dispensing malarial treatments in villages. “If what I do can make a difference in even one person’s life, I do it,” she says. “I believe everyone should have an equal opportunity for success in life. When they can’t, I feel the need to help them get there.” 10
STANFORD HOSPITAL PEOPLE / ISSUE SEVEN 2014
ESTER YU, RN, TRAVELED TO WEST AFRICA RECENTLY TO HELP PROVIDE MALARIAL TREATMENTS IN LOCAL VILLAGES.
“ If what I do can make a difference in even one person’s life, I do it. I believe everyone should have an equal opportunity for success in life. When they can’t, I feel the need to help them get there.” Military Medical Missions A sharp uniform. A prestigious career. A good paying job. Those qualities drew Evelyn Barte, RN, to a career in the Armed Forces of the Philippines as a young woman in the Philippines. After graduating from nursing school, Barte was commissioned and served as a military nurse for 18 years, including several months in the Vietnam War. When she immigrated to the United States in 1989, she maintained her ties to the Philippine military forces, volunteering to continue serving her home country as part of a retired officers medical league Every two years, Barte travels with this group to countries in Asia and Africa for four to six weeks to serve on medical and surgical missions. More recently, she volunteered with separate organizations so she could return to the Philippines to help after the
typhoon. In one of these missions, Barte traveled by helicopter and then walked for miles to provide health education and consultations in villages in the most remote regions of the Philippines. “I volunteered to stay and help in my own country,” she says. “It was sad, but very rewarding to help. The people are so appreciative. When they show their smile to you, it’s so rewarding. It’s a priceless accomplishment.” Barte came to Stanford in 2000 and works as a per diem nurse in the Infusion Treatment Area to accommodate her travel schedule and charitable work. She also volunteers at several parishes in San Francisco, feeding the homeless and mentoring children.
EVELYN BARTE, RN, SPENT 18 YEARS AS A MILITARY NURSE.
At SHC Reducing Length of Stay Length of stay among surgical heart valve patients at Stanford Hospital varied greatly due to lack of standardization in the care delivery process. When the cardiovascular leadership team asked nurse coordinator Sophia Loo, RN, to lead an improvement effort, she put together a multidisciplinary team that included nurses, physician assistants, physical therapists, respiratory therapists, case managers, pharmacists, dietitians, physicians and surgeons. The group began meeting weekly in February 2013.
SOPHIA LOO, RN, HAS LED AN IMPROVEMENT EFFORT TO REDUCE PATIENT LENGTH OF STAY.
They dissected the entire valve care process and developed a care path to synchronize the timing of care delivery from postoperative state to discharge. From the care path, Loo created an activity checklist to track and document a patient’s progress toward daily goals, focusing on out of bed to chair, ambulation, incentive spirometer and pain management. The checklist hangs from a patient’s bed in the ICU and on a white board on the floor s it’s visible to the entire caregiving team, including the patient and family members. Patient rooms are also
marked with a pink sign, “Patient ON Valve Care Path.” “Having a checklist increased the visibility of these activities,” says Loo. “Patients like the step by step progression outlined on the checklist.” Since implementing the care path last June, total length of stay dropped from 13.4 days in 2012 to 10.6 days. Post procedure length of stay decreased from 11.8 to 9.4 days during this same period. The direct cost per case decreased by two percent. The program was expanded to all cardiac patients this March.
Improving Patient Satisfaction Just nine months into her new job as the assistant clinic manager for the Pain Management Clinic, Ann Cullen, MS, RN, took on a new challenge—leading the clinic’s team through a Rapid Performance Improvement Workshop (RPIW) to improve patient satisfaction. A multidisciplinary team representing all areas of pain management focused on three indicators of patient satisfaction: care providers giving clear follow-up instructions; care providers explaining the problem or condition; and the staff working well together to provide care for the patient. “Every member of the team was fully participatory and extremely engaged,”
“ Every member of the team was fully participatory and extremely engaged” . says Cullen, who was SOS-certified in her previous position at Stanford. She’s excited to bring a systems approach to improving the patient experience in her new department. The group’s first intervention was t implement hourly rounds. A staff member now walks through the waiting and exam areas to check on patients, offer them water and update them on waiting times. The team also created a visibility wall that providers huddle around each morning. It lists providers in the clinic each day, their assigned medical assistant, and their next available appointments. To ensure that patients understand their follow-up care, the team developed standardized, clear instructions for patients to take home. Providers review these instructions with patients in the exam room and answer patients’ questions before they check out. As a continuous improvement process, Cullen will actively monitor and refine these interventions an check Press Ganey scores to gauge the success of the effort.
ANN CULLEN, RN, LEADING HER TEAM’S RPIW TO IMPROVE PATIENT SATISFACTION.
STANFORD HOSPITAL PEOPLE / ISSUE SEVEN 2014
11
300 Pasteur Drive Stanford, CA 94305
From Tibetan Refugee to SHC Nurse Dechen Dolkar was born and raised in a Tibetan refugee settlement in Bhutan, and schooled in India. Her path to becoming a nurse and practicing at Stanford took many turns. When the Chinese invaded Tibet in 1959, and after His Holiness the Dalai Lama fled his country with the hop of returning, many Tibetans, including Dechen’s parents and extended family, escaped. The couple first went to nearby Nepal, but when Chinese force invaded their town, they fled to Bhutan, where the settled amid hundreds of other Tibetan refugees. That is where Dolkar’s childhood began. But her first childhood memories came much late , she says, when she was sent to India to attend one of the many Tibetan schools established by the Dalai Lama in the early 1960s. Dolkar spent much of her young life in the northern part of India, a several-day journey from her home. When both of her parents died, she and her brother and sister grew up separately—Dolkar in a Tibetan foster home in India, where she completed high school and college, her brother in a monastery and her younger sister in Bhutan with relatives. In 1993, a cousin in the U.S. sent Dolkar an invitation to visit and changed the course of her life forever. By then, she knew she wanted to study nursing, so she applied for a student visa and received an RN from the College of Marin and a BSN at Sonoma State University. After graduation, she worked at UCSF in the Neuro ICU
and came to Stanford Hospital in 2004, where she is a nurse on the E2 ICU. Today, Dolkar shares her time between nursing and maintaining ties to her Tibetan culture. There is a large community of Tibetans in the Bay Area, she says, and Dolkar is an active member of the Tibetan Association of Northern California (TANC), an organization that seeks to preserve the Tibetan culture and to promote self-rule in Tibet. Dolkar serves as chair of the association’s health promotion committee. As she points out, many Tibetans living in the Bay Area do not have health insurance. Their primary concern is for their family here and sending money home to others. “It is a stressful life here for a lot of Tibetans, and many have high blood pressure,” she says. To help the Tibetan community manage their health, the health promotion committee holds a health fair twice each year. Dolkar and other nurse volunteers conduct blood pressure and blood sugar screenings, seek the consult of volunteer nurse practitioners and physicians, and educate members on nutrition, exercise, smoking cessation and other lifestyle choices. The group also makes follow-up calls to individuals with borderline to high blood pressure to answer questions and to see that they receive necessary medical care through clinics for uninsured and low-income families. Although Dolkar left her immediate family behind in India and Bhutan, she says that Tibetans here in the U.S. treat each other as extended family. “In our culture, you help whoever you can in your extended family,” says Dolkar. “The Buddhist culture is ingrained in us. Being kind to others is part of our culture.”