
12 minute read
TELEHEALTH THRIVES
HEALTH
USATODAYSPECIALEDITION
Advertisement
GETTY IMAGES
Telehealth Thrives in Trying Times
Pandemic spotlights the advantages of remote health care
By Robin Roenker
Center (UMMC) — one of two federally visits per day. By the end of 2020, the percent of Medicare-covered primary designated National Telehealth Centers UPMC health care system was handling care visits were conducted via telehealth . F THE COVID-19 PANDEMIC has of Excellence — performed 16,938 15,000 telehealth visits daily . Two months later, in April, telemedicine
Iany sort of silver lining, it may be telehealth visits in 2019. In 2020, UMMC The telemedicine boom was aided by represented 43.5 percent of Medicarethat it has helped telemedicine go providers conducted more than 165,000 new, temporary flexibility regarding the covered primary care appointments. mainstream. visits via telemedicine, a roughly 874 types and manner of services that can be By June, the number of patients using
When most of the country went percent increase . provided via telehealth , while still being telehealth to replace canceled in-person into lockdown last March, telehealth The story is the same throughout the eligible for coverage by Medicare and appointments was more than four times became many physicians’ primary means country. Prior to COVID-19, the University Medicaid services. the rate of telehealth appointments in of connecting with patients. of Pittsburgh Medical Center (UPMC) In February 2020, before the fed-
The University of Mississippi Medical typically conducted 250 telemedicine eral provisions went into effect, just 0.1
CONTINUED
USATODAYSPECIALEDITION

HEALTH
USATODAYSPECIALEDITION

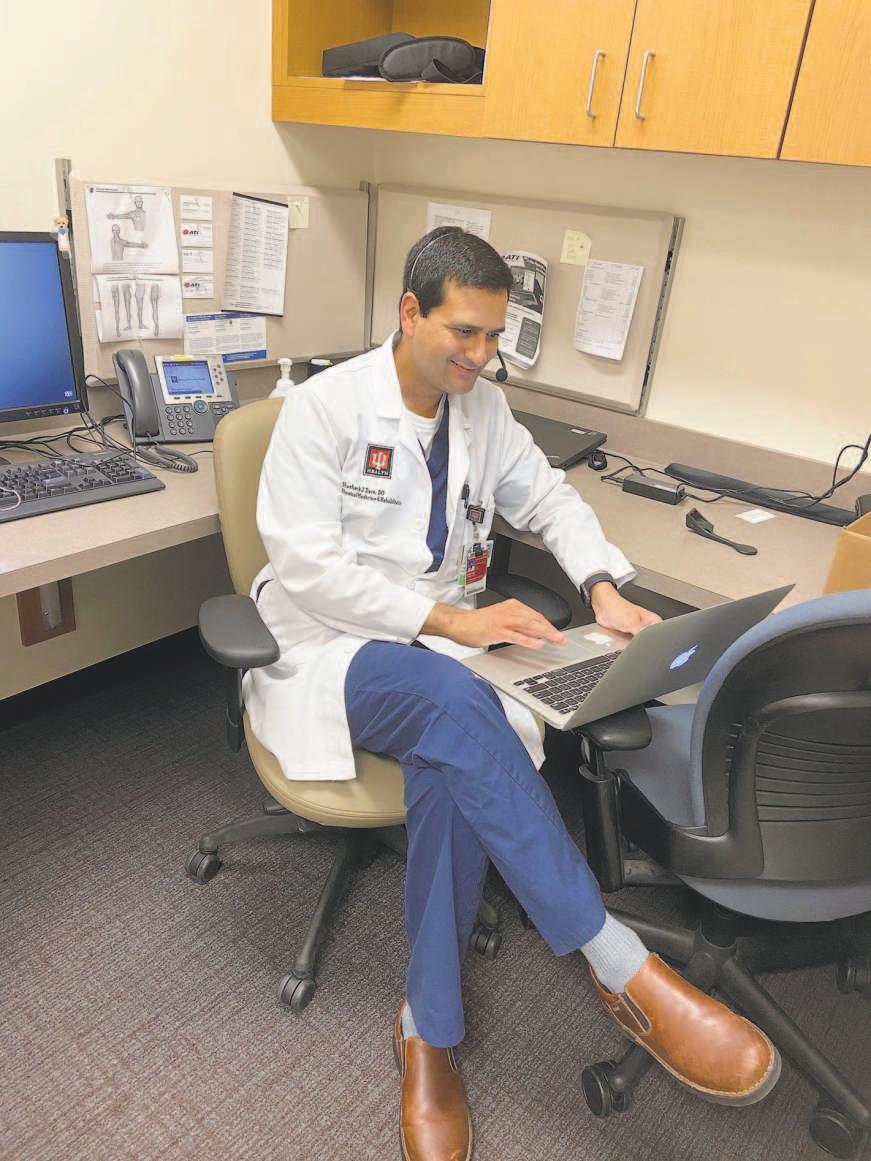
INDIANA UNIVERSITY HEALTH Dr. Shashank Dave, a physical medicine and rehabilitation physician at Indiana University Health, says patients are often more at ease during telehealth appointments.
UNIVERSITY OF PITTSBURGH MEDICAL CENTER By the end of 2020, the University of Pittsburgh Medical Center system was conducting 15,000 telehealth visits daily.
2019, according to a McKinsey & Co. study.
“Prior to the pandemic, the utilization of telemedicine by consumers and physicians was actually quite low,” says Ann Mond Johnson , CEO of ATA (American Telemedicine Association) , which is lobbying to make many of the coronavirus-related telehealth provisions permanent. “From our vantage point, the pandemic served to accelerate things. We saw 10 years’ growth in 10 weeks.” CONVENIENT OPTION
For patients like Brady Conway, a 27-year-old from St. Clairsville, Ohio, who has autism and epilepsy, telehealth has been a godsend.
Prior to the pandemic, Conway’s mother, Jerri McCombs , had to take an entire day off from her job as a nurse to drive him to his behavioral health appointments at UPMC Western Psychiatric Hospital in Pittsburgh, roughly 70 miles away . The trip was agitating for Brady, who is nonverbal, and he was often physically disruptive in the waiting room and during appointments. “It was always stressful, and he was all over the place,” McCombs says.
Without the commute, Conway’s doctors were able to see his more typical behavior in his home environment. “Telehealth should, honestly, always be the solution for this population,” McCombs says.
Janet Strauch of Greenfield, Ind., found even routine checkups to be more convenient and less stressful using videoconferencing.
“Telehealth saves me at least an hour in commute time, and I actually felt like I got more one-on-one time with the physician to really focus and discuss my personal case,” says Strauch, who used telemedicine for the first time during the pandemic to address orthopedic pain in her spine. Immune suppressed due to medications she is taking, Strauch says telemedicine allowed her to stay on top of her follow-up care without unnecessary risk of exposure to COVID-19.
“There are so many advantages to telehealth for appointments that don’t require an in-person procedure,” says Dr. Shashank Dave , a physical medicine and rehabilitation physician at Indiana University Health who is treating Strauch. “There’s ease of use, decrease in travel time. Plus, I’m able to see patients in their normal, natural environments. And I think that helps patients feel more relaxed and at ease during appointments.”
EQUAL ACCESS
Beyond its convenience, telemedicine makes health care more equitable by delivering access to primary and specialized care in rural areas that often have few providers.
In Mississippi, it allows UMMC specialists — including cardiologists, dermatologists, allergists and psychiatrists — to provide care to patients throughout the state. Telehealth also
CONTINUED
USATODAYSPECIALEDITION


HEALTH
USATODAYSPECIALEDITION
USE THIS 43.5
PERCENT PULLOUTS
XXXXXXXXXXXXXXX Leadin goes here asdfasdfasdfasg fsdfdfasdf asdf asdf asdf asdf asdf asdf asdf asdf. asdf asdf asdfa sdfasdfg sdfgsd asdfasdfasdfasdfas.
Dr. Will Campbell, a cardiologist, and Marlene Holloway, a registered nurse care coordinator, meet with a patient via videoconference.
provides physicians with a cutting-edge tool for preventative care. Remote patient monitoring from UMMC Telehealth , for example, connects rural Mississippians with chronic conditions, including diabetes and heart disease, with health care providers who can help monitor and manage their symptoms.
Behavioral health is another area in which telehealth usage is growing . While platforms to remotely deliver mental health care existed well before COVID-19, “some providers were a little bit resistant to adopting them. It’s a different way of practicing,” says Dr. John Torous , director of the digital psychiatry division at Beth Israel Deaconess Medical Center in Boston. “COVID has been a catalyst (for adoption). I think most patients have been very excited to use telehealth.”
JMIR Mental Health , an academic journal for which Torous serves as editorin-chief , recently published research showing that, of surveyed patients who used telepsychiatry during the pandemic, more than 80 percent had an overall positive experience with remote care — whether via video or telephone — and 63.6 percent said it has been as effective as their in-patient sessions .
To achieve telehealth’s full potential, providing reliable, high-speed internet access to every community must be a priority, advocates say.
“We are a rural community, and the (internet) bandwidth in some of these areas is very slim,” says Dr. Danette McAlhaney , a family medicine specialist in Bamberg, S.C., who has been providing telehealth visits for four years. “At times, we’ve had to do audio visits only, because we aren’t able to do video visits for those areas.”
And while McAlhaney doesn’t think telemedicine should replace every in-person visit, she knows it serves an important role in bringing high-quality care to her patients.
“It’s a good add-on service,” she says. “It has its time and its place.”
— ANN MOND JOHNSON, CEO, American Telemedicine Association
UNIVERSITY OF MISSISSIPPI MEDICAL CENTER
USATODAYSPECIALEDITION

HEALTH
USATODAYSPECIALEDITION
Stress and Strain
Study indicates a link between COVID-19 and mental health
By Fiona Soltes
S THE COVID-19
APANDEMIC reaches the one-year milestone, many people have reported experiencing some degree of coronavirus-related stress or anxiety. And those issues may be more acute for those who’ve had the disease.
Researchers in the U.K. analyzing electronic health records of nearly 70 million Americans — including more than 62,000 COVID-19 patients — found that 18.1 percent of people infected with the coronavirus were diagnosed with a psychiatric disorder within 90 days of infection. Further, those who had received a mental health diagnosis within the previous year were slightly more likely to contract the coronavirus, and a similar number of coronavirus patients (1.6 percent) received an initial dementia diagnosis within 90 days of contracting COVID-19. The study was published last November in The Lancet Psychiatry journal.
James C. Jackson , assistant director of the ICU Recovery Center at Vanderbilt University Medical Center, fi nds the results interesting but “not at all surprising. It’s what we would expect, and what we have seen historically in other contexts.”
Mental health concerns such as depression, post-traumatic stress disorder (PTSD) and cognitive impairment are prominent for many non-COVID intensive care survivors, he says. With COVID-19, mental health concerns may be related to the overall experience or the illness itself. “There’s no doubt, for some percentage of individuals with COVID, that their brains are affected in ways that are either fundamental or peripheral,” Jackson says. The common symptom of loss of smell, for example, is neurological .
Kristin Addison-Brown , a clinical neuropsychologist in Jonesboro, Ark., says COVID-19 often has pulmonary aspects; prolonged periods of low oxygen can trigger dementia and other mental challenges. There’s also potential overlap between depression and prolonged fatigue commonly associated with COVID-19.
As for a prior mental illness diagnosis being a risk factor for COVID-19, Jackson and Addison-Brown say these people may be engaging in unhealthy behaviors — or not engaging in healthy ones — that would affect that risk. Someone with an anxiety disorder, for example, may feel unable to wear a mask. Another who is depressed may not visit the doctor, exercise or eat healthy foods. Someone with dementia may forget to adhere to pandemic hygiene and safety protocols .
Socioeconomic status can also play a role , as fi nancial uncertainty can increase stress and limit access to care.
It may not matter whether a mental health diagnosis or illness comes fi rst. Until there’s evidence otherwise, Jackson says, traditional treatments for depression, PTSD and anxiety could still be helpful. There may be nuances, but someone shouldn’t avoid seeking care.
With depression and anxiety in general, ruling out underlying causes like thyroid issues or other physical disturbances fi rst is important, Addison-Brown says. After that, it can be “treating the symptom, because that’s what’s causing the distress for the individual.”
Patients should start by contacting their primary care physician, she says, and discuss whether a diff erent level of care is needed. It’s time to seek help, Addison-Brown says, when mental health challenges affect day-to-day functioning or cause signifi cant distress.
Both Jackson and AddisonBrown found the study’s link between dementia and COVID-19 notable. Here, an underlying cause may be more important in determining the right treatment.
The link to dementia, Jackson says, could include those with an underlying but not-yet-expressed condition, or those with diminished cognitive reserve . These patients — especially the elderly, frail and otherwise vulnerable — may have been on the verge of dementia prior to a COVID-19 diagnosis.
GETTY IMAGES
USATODAYSPECIALEDITION


USATODAYSPECIALEDITION

USATODAYSPECIALEDITION

USATODAYSPECIALEDITION
HEALTH
CALM

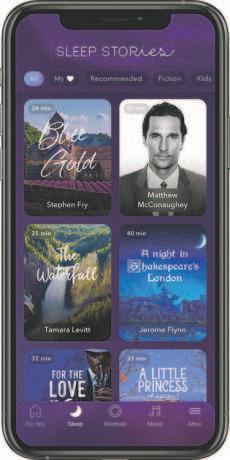
CALM with a daily meditation designed to reduce anxiety in a week.
Turns out I’m not alone in getting a new work benefi t to help manage stress. Data shows the rate of people experiencing anxiety and depression has tripled during the pandemic , says Darcy Gruttadaro , director of the Center for Workplace Mental Health with the American Psychiatric Association Foundation . And employers are realizing they need to off er more mental health benefi ts, she says.
“Emotional health, mental health, physical health — there are more and more studies showing that they all have an impact on performance, productivity and retention,” Gruttadaro says. “We also know ... stress impacts physical health. That’s costly for employers.”
Calm and Headspace , another popular meditation app, have seen big usage spikes. Daily downloads of Calm have doubled since the pandemic started , according to a company spokesperson. Since March 2020, Headspace has experienced a 500 percent increase in requests from companies looking for ways to support employees’ mental health .
“We currently have more than 1,500 companies, such as Starbucks, Adobe, GE, Hyatt and Unilever, who off er Headspace for Work to help employees take care of their minds, build more productive cultures and foster higher-performing organizations,” says Megan Jones Bell , chief strategy and science off icer at Headspace.
Some of the app’s most popular features are live group meditations, sleep music and exercises to curb stress and anxiety, she says. On Election Day, Headspace saw a 965 percent increase in unique users from the week before .
It even released a special “Politics Without Panic” selection of exercises , which Jones Bell says were “designed to help people handle the mix of emotions they were experiencing.”
A 10-minute meditation known as the “Daily Calm” is one of Calm’s most popular features, along with bedtime sleep stories for grown-ups and kids.
Gruttadaro, whose center off ers resources to employers looking to promote mental health, says she’s also seeing more organizations access its training guides and other tools during the pandemic. “If there’s one tiny silver lining with this pandemic, it’s that (the stigma surrounding mental health) is starting to fade a bit,” she says. “People are starting to recognize that all of us are vulnerable.”
Mindfulness and meditation apps can help people relax and focus, Gruttadaro says, which is likely why they’re becoming a popular benefi t for employers. Burnout can lead to turnover, which isn’t good for a company’s bottom line. “We want to retain our high performers,” she says.
I’ve been using Calm multiple times each week, mostly tuning in to short, on-demand meditation exercises focused on gratitude or releasing anxiety. If I’m short on time, I take a few moments to view one of the app’s serene scenes, such as snow falling or the northern lights. Even if I don’t have time to access the app, I’m now able to recall the breathing exercises repeated in many of the meditations.
One hurdle to employee adoption is the concern that tapping into mental health resources off ered at work could harm one’s career. I have wondered if my employer can see how I’m using the Calm app. Do they receive reports showing those of us who might be dealing with anxiety, stress or sleep problems?
Calm did not respond to multiple requests for comment about whether they share user data with the companies that pay for subscription plans. Jones Bell says Headspace doesn’t share any personalized data with employers. “The metrics are provided in the aggregate, so they don’t receive details about specifi c actions any individual employee takes within the Headspace app,” she says.
Company leadership can play a big role in helping employees feel comfortable using any new mental health benefi ts they might be off ering, Gruttadaro says. “That opens the door to people thinking, ‘Well, if the leaders are using it and the senior management folks are using it, then it’s OK for me to use it, too.’”
HEADSPACE


HEADSPACE
USATODAYSPECIALEDITION










