40 minute read
Understanding a Public Health Epidemic
“Arecent study published by the Centers for Disease Control and Prevention (CDC) highlighted the issue of insufficient sleep,” the journal Sleep Science reported in 2018. “It was concluded that more than a third of American adults are not getting enough sleep on a regular basis. As a consequence of these findings, the CDC declared that insufficient sleep is a ‘public health epidemic’.”
Sleep deprivation can result from insomnia and other sleep disorders, as well as various medical and mental health conditions. We also seem to be, as sleep scientist Matthew Walker says, “the only species that deliberately deprive themselves of sleep for no apparent gain. Many people walk through their lives in an underslept state, not realizing it.”
Insufficient Sleep Syndrome (ISS) is a disorder caused by chronic voluntary sleep deprivation to the point of being unaware of the need for sleep. Sacrificing sleep for work, school, social activ- ities, entertainment, web-surfing, and having “too much to do” are behaviors that can lead to ISS. Symptoms include hypersomnia (excessive daytime sleepiness), fatigue, irritability, low energy, distractibility, and difficulty with concentration and attention.

People can also experience these effects after just one night of sleep loss, which quickly weakens the immune system, motor skills, and reaction time. A few days of short sleep can trigger changes in mood, anxiety, and weight. This is called acute sleep debt, which can be recovered if corrected soon enough.
4. (REM, or rapid eye movement sleep for 10-60 minutes)
“Sleep deprivation is an illegal torture method outlawed by the Geneva Convention and international courts, but most of us do it to ourselves.”
- Ryan Hurd, in" Dream Like a Boss”
All four stages form a sleep cycle. A person typically goes through four to six cycles every night. Failure to complete enough cycles and stages, especially deep sleep and REM sleep, can have profound consequences on brain functioning, physical health, and emotional wellness.
Chronic sleep debt is a different story. Trying to catch up on weekends isn’t enough to make up for “burning the candle on both ends'' during the week. The body is remarkably resilient, but once ISS becomes a person’s baseline, the risk of chronic disease and premature death becomes very real. The Sleep Research Society found that people who get “irregular-insufficient” sleep had a 42% higher mortality risk compared to those who get “regular-optimal” sleep. Enough hours of sleep on a regular basis are needed to support the sleep stages, which are:
“As a species, we have the flexibility to function on less than optimum sleep. We are not going to stop functioning, but sleep deprivation comes at a price.”
According to the National Sleep Foundation, “During sleep, the body and mind go through various restorative processes, including repairing and rejuvenating cells, consolidating memories, processing emotions, and cleansing toxins from the brain. Good sleep can help you regulate your emotions better as well as improve cognitive skills like learning and attention.”
-Malcolm von Schantz, Chronobiology Professor
Prioritizing sleep is vital for physical and mental health. People in the insufficient sleep category who embrace that reality and make some basic lifestyle changes will reduce their risk for disease and premature death. Those who are sleep deprived due to medical conditions, mental health disorders, or insomnia should consider seeking help from a doctor or clinician.
1. (light sleep for 1-7 minutes)
2. (light sleep for 10-25 minutes)
3. (deep sleep for 20-40 minutes)
The world is waking up to the importance of sleep, which will hopefully avert what is becoming a public health nightmare.
According to the Centers for Disease Control & Prevention (CDC), “there is no precise number of minutes or hours of sleep at night that guarantees you will wake up feeling totally refreshed.” That’s because the quality of your sleep is also important. However, there is an optimum range of hours needed for the sleep stages to run their course, and children and adolescents require more sleep time than adults since their brains and bodies are still developing. The CDC has found that, “based on your age and lifestyle, what’s recommended for you likely falls within a certain range.” Here are the current age-specific guidelines:

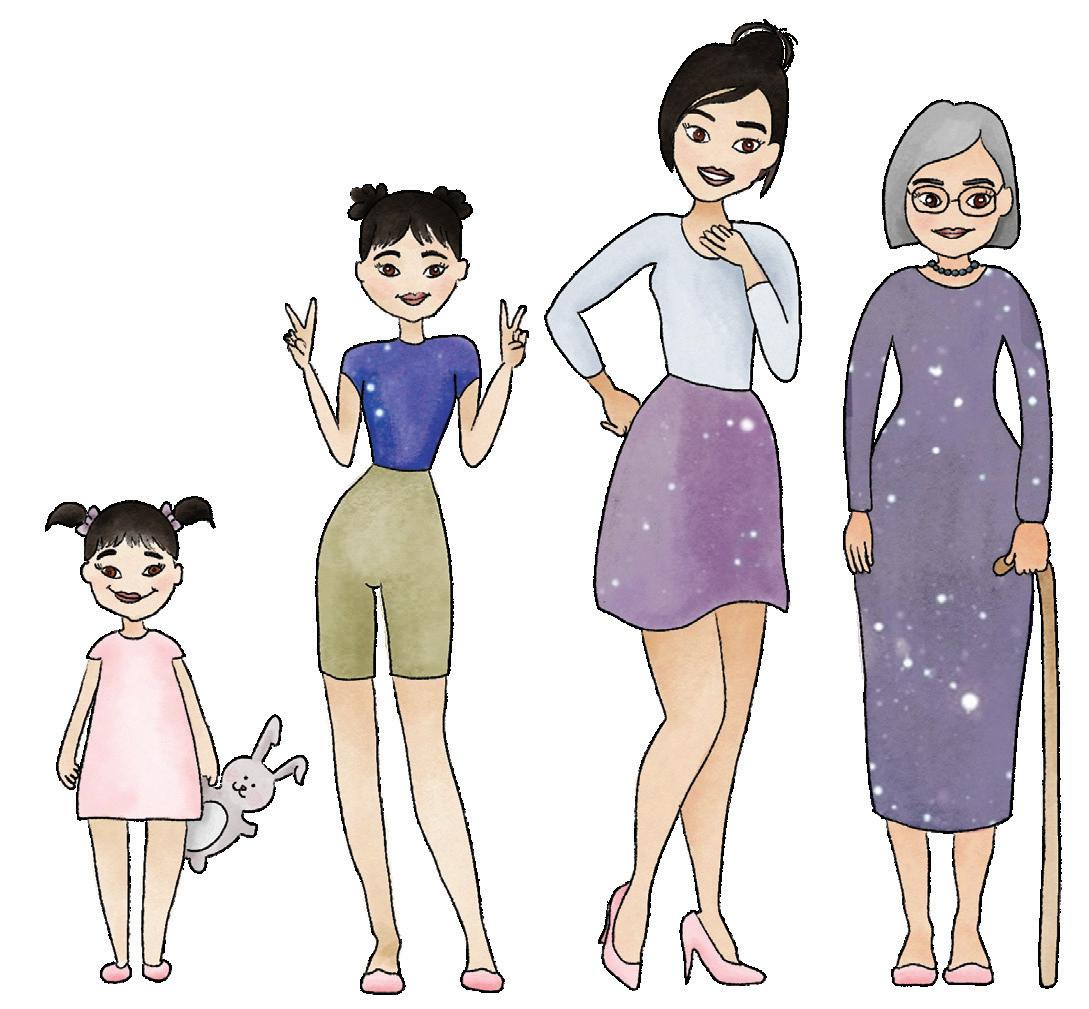
Newborns (0-3 months): Between 14 and 17 hours of sleep. This includes daytime naps, since newborns rarely sleep through the night.
Older infants (4-12 months): Between 12 to 16 hours, including naps.
Toddlers (1-2 years): Between 11 and 14 hours, including naps.
Preschoolers (3-5 years): 10 to 13 hours, including naps.
School-age kids (6-12 years): 9 to 12 hours each night.
Teenagers (13-17 years): 8 to 10 hours nightly. We note here that 76% of Utah teens are getting less than 8 hours a night on a regular basis. This is partly because of their natural hormonal delay in circadian rhythms, which pushes the need to sleep about two hours later.
The National Sleep Foundation, backed by medical organizations such as the American Academy of Pediatrics, has stated that policies focusing on adequate sleep for teens provide “a wide range of potential benefits to students with regard to physical and mental health, academic achievement and public safety.”
Adults (18-64 years): 7 (minimum) to 9 hours of nightly sleep. The need to nap for adults could indicate inadequate quantity and quality of sleep, or a medical condition that should be investigated.
Older adults (65 and older): 7 to 8 hours
Between 1% to 3% of the population have a genetic mutation that makes them “natural short sleepers”, meaning they can sleep 6 hours a night or less without any apparent harmful effects. The rest of us, however, will be happier and healthier if we find and stick with our sweet spot, according to the age categories above.
Expert Advice from the Pediatric Sleep Council
What is sleep training?
-Dr. Sonia Rubens
Just like so many areas of development, children typically need help learning how to self-soothe to sleep. This process is often referred to as “sleep training.” Although there are multiple approaches, sleep training typically involves helping your child learn how to fall asleep and return to sleep on his/her own. Sleep training does not have a one-size-fits-all approach. You will want to use an approach that works best for you and your family. Regardless of the method you choose, there are some things that are consistent across most sleep training approaches.
In addition, whatever approach you use, being consistent is key. You don’t want to keep your little one guessing when it comes to where, when, and how they will sleep. Although there are exceptions (e.g., vacations, visitors, holidays), try to keep the sleep experience as consistent as possible for your baby.
First, sleep training involves setting the stage for sleep by creating a consistent bedtime routine. This helps signal to your little one that it is time to wind down and fall asleep. Bedtime routines should be about 15-20 minutes (a little longer if it includes a bath) and might involve such things as a feeding, diaper change, putting on pajamas, reading a book, and singing a song. These things can vary from family to family, though. It is never too early to start a bedtime routine; it is something you can start doing even before you work on other aspects of sleep training. A similar routine can also be used before naps.

Second, sleep training involves helping your baby learn to fall asleep on their own. Once you have cued your baby that it is time for bed through the bedtime routine, the next step is to put him in his bed while awake. What happens next depends on your baby and how you wish to approach this part of sleep training. Some families choose to use a gradual approach to this step. For example, you can leave the room and slowly increase the amount of time between when you check on your baby. Another way is to stay with your baby in his room and gradually move yourself farther away over successive nights. Other families decide from the start to give their baby long stretches to figure out how to fall asleep by themselves.
Regardless of the approach you take, it is important to know that for babies who are given a lot of love and attention during the day, letting them cry while they learn to fall asleep has no negative impact on their development. In fact, babies who learn to get a good night’s sleep tend to be really well adjusted, happy children!
Third, sleep training involves helping your child learn to fall back to sleep on their own during the night if they happen to wake during the night (which all babies do naturally). Oftentimes, once they learn to fall asleep on their own at the start of the night, that skill transfers to the rest of the night regardless of how many times they may wake during the night. For other babies, you may need to do some sleep training during the night once they have mastered the skill at the start of the night. Balancing how to respond to night wakings and the need for night feedings is something to discuss with your baby’s health care provider when you are working on sleep training.
What are the top 4 sleep training myths?
-Dr. Melisa Moore
1) If you sleep train, you have to let your baby cry it out -There are many ways to approach helping a baby learn to sleep through the night, and the specific techniques we recommend depend on the age of the child and parent or family preferences. There are many options that are based on the same behavioral approach. I don’t know of any sleep professional who would recommend letting a baby cry all night long.
2) Waking through the night is abnormal -We all have sleep cycles, and at the end of each one, our brains wake up. That means that we all wake several times per night, and we don’t even know it! Your baby might be signaling you that they are awake because they are used to settling down a different way (rocking, nursing, etc.) and might need some help to return to sleep.

3) Sleep training is easy -Sleep training is hard to do, even if it’s what you do for a living. Reach out to friends and family and even supportive social media (avoid anything that makes you feel guilty). It helps to keep your eye on the prize: better sleep for the baby and for you.
4) Sleep training has to take place at bedtime and all through the night -No way! I hardly ever recommend doing sleep training all at once. I usually suggest implementing behavioral changes only at bedtime, especially at first. During night wakings (which are likely) just do whatever it takes for everyone to get as much sleep as possible. If your baby can’t fall asleep independently (go from being wide awake to asleep on his or her own, without having an adult in the room) at bedtime, it’s highly likely your baby will keep signaling you when he or she is awake throughout the night.
Dr. Rubens and Dr. Moore are members of the Pediatric Sleep Council, which was created to provide accurate and up-to-date information on sleep in young children for parents and caregivers. These questions and answers are just a sampling of the valuable information found on their website: babysleep.com.
Clean up your Bedtime
The National Institutes of Health define sleep hygiene as “a set of behavioral and environmental recommendations intended to promote healthy sleep.” continue reading on next page...
Many of these practices are common sense; others are supported scientifically or are being researched to find out how and why they matter. As you review these suggestions, are there some that you could easily start today (or tonight)? Try them for a few weeks and see if it makes a difference in the quantity and quality of your sleep.
Make sure your bedtime is early enough to get 7-9 hours of sleep (see page 8 for age-specific guidelines).
Go to bed and wake up at the same time every day. Try to be consistent, even on weekends and vacations.
Physical activity during the day promotes better sleep at night, even if it's just 30 minutes. Exercising outdoors in the morning adds sunlight exposure, which helps regulate circadian rhythms. A survey by the National Sleep Foundation showed that people who spent 3-5 hours a day outdoors reported the best sleep.
Have consistent mealtimes. Your appetite and circadian rhythms are closely linked, and sleep can be affected by irregular or skipped meals, and large meals at night. Try to eat your last meal 2-3 hours before bedtime.
Avoid caffeine in the afternoon and evening, and alcohol before bedtime.
Light exposure has a strong effect on sleep. Bright, natural light exposure within an hour after waking) helps you wake up in the morning; dim light and darkness (about two hours before bed and through the night) help you fall asleep.
Avoid exposing yourself to media or conversations that heighten your emotional state close to bedtime. Briefly write down any nagging thoughts (ideas, worries, upcoming events, etc.) that are keeping you awake to get them on paper and out of your head.
Create a routine that helps you relax. Bedtime rituals (warm bath or shower, meditation, dimming lights, reading, etc.), especially when done in a certain order, signal the mind and body that it’s time for sleep. Create a routine that works for you, too.
Don’t go to bed unless you’re sleepy; if you don’t fall asleep after about 20 minutes, get up and do something quiet (no electronics) until you feel sleepy enough to try again.
The temperature in your bedroom should be on the cool side, around 60 to 68 degrees Fahrenheit. Wear layers, socks, or extra blankets as needed to keep your body warm enough.
Do you have a comfortable bed? Mattress preference includes temperature, firmness, size, and who you share it with. Finding a mattress that is sleep-friendly for you is worth the effort and investment. The same goes for pillows, sheets, and blankets.
Only use your bed for sleep and related activities.
Blue light causes more alertness than warmer tones and has been shown to promote wakefulness even at bedtime. Over 50% of American adults report staring at electronic screens within an hour of going to bed, making this the sleep hygiene rule we break the most. Take a break from all devices with screens at least 60 minutes before bedtime. For a truly restful sleep, make your bedroom screen-free; that includes TVs, computers, phones, tablets, and laptops. Charge them overnight in another room and use a simple alarm clock to wake up if needed.
Sound matters. Do you need your room quiet, or does some sound help you get to sleep? Certain neutral sounds (like a fan) can be soothing and mask background sounds that disrupt sleep. White noise played from sound machines or apps contains all audible frequencies and seems to help some people sleep better, using sound machines or device apps.
If you’re already doing some of these, congratulations! If you miss a day or “relapse” into old habits, just resume your efforts as soon as you can. Make your sleep hygiene as important as your personal hygiene!
By Shana Chavez SWUPHD Clinical Assistant

What is snoring?
Snoring refers to the noise that sometimes occurs as we breathe while sleeping and is typically caused by narrowing of the upper airway. The sound it creates can range from soft whistling to loud rumbling or snorting. It happens when the tissues at the back of the throat, which naturally relax during sleep, vibrate together as air passes through.

How common is it?
Almost all of us snore at times, even babies and children. According to Johns Hopkins University, nearly half of all adults snore occasionally, while one-fourth of us are chronic snorers. Based on information collect- ed by the National Sleep Foundation, snoring happens more often in men than women.
Why do we snore?
There are many reasons why someone might snore. Occasional bouts of snoring might simply be due to nasal congestion that comes with a cold or seasonal allergies, making it more difficult to breathe through the nose. Some other reasons that might cause or worsen snoring include:
Anatomy – Conditions that can restrict proper airflow include larger than normal tonsils or adenoids (lymphatic glands located high in the throat), a deviated septum (when the thin wall separating the nostrils is off-center), an elongated uvula (the fleshy piece of tissue that hangs at the back of the throat), or a naturally low or thick soft palate (the soft tissue located toward the rear of the roof of the mouth).
Sleep position – Snoring is generally more frequent or louder when back-sleeping, since gravity contributes to the relaxing of tissues in the back of the throat.
Being overweight – Snoring is more common in individuals with a body mass index (BMI) greater than 25.
Pregnancy – Women in late pregnancy are more likely to snore because of hormonal changes which can cause swelling of nasal tissues.
Sleep deprivation – Not getting enough sleep can contribute to snoring because throat tissues relax more deeply when we’re overly tired.
Using alcohol or sedatives – Drinking alcohol or taking medications that have a sedating effect - especially when used closer to bedtime - can further relax the throat, increasing the frequency and severity of snoring.
Age – snoring becomes more common as we get older because muscles, including those of the throat and tongue, become weaker.
Heredity – A family history of snoring means you are more likely to snore also.
What can you do to reduce snoring?
Be active and get regular exercise; losing excess weight can lessen snoring. If you generally sleep on your back, switch to side-sleeping which allows for a more open airway. Eliminate alcohol intake or avoid it in the hours before bedtime. Quitting smoking may also reduce snoring, as well as improve overall health.
Some other things to try include elevating the head of your bed by three or four inches or swapping out your pillow for one that better supports your head and neck. Over-thecounter nasal strips can help open nasal passages. If you have a cold or seasonal allergies, treating nasal congestion can ease snoring.
When is snoring something to worry about?
While snoring is common and not normally a cause for concern, chronic snoring, especially when accompanied by other symptoms, may indicate something more serious. Snoring can sometimes be associated with obstructive sleep apnea, a condition where breathing stops and starts many times throughout the night due to limited airflow. This pattern of irregular breathing interrupts the normal respiratory process of taking in oxygen and removing carbon dioxide (waste gasses). Untreated sleep apnea can lead to additional health issues like high blood pressure, heart attacks, strokes, and type 2 diabetes. The American Heart Association reports that one in five adults has at least mild sleep apnea. Other symptoms often associated with this condition include:
• Restless nights (tossing and turning)
• Feeling excessively tired during the day or falling asleep during meetings or other daytime activities
• Gasping or choking during the night
• Waking in the mornings with dry mouth, sore throat, or headache
• Being told that your breathing pauses during sleep
• Nighttime chest pain
• Unexplained irritability or moodiness
• Trouble concentrating
• Loud snoring that is disruptive to others
Sleep apnea, while rare, can occur in children also. In addition to some of the previously mentioned symptoms, children may exhibit behavioral issues and poor attention span. It’s advisable to mention any chronic snoring in children to their doctor as it could indicate an issue with the tonsils or adenoids.
Again, snoring can be completely normal. However, if your snoring concerns you or a partner, or if you’re experiencing other symptoms, a visit to your physician for further evaluation is warranted. Your doctor can help in diagnosing any possible sleep disorders and recommend a treatment plan.
Sleep Disorders & Insomnia

“A third of US adults report that they usually get less than the recommended amount of sleep. Not getting enough sleep is linked with many chronic diseases and conditions—such as type 2 diabetes, heart disease, obesity, and depression—that threaten our nation’s health. Not getting enough sleep can lead to motor vehicle crashes and mistakes at work, which cause a lot of injury and disability each year. Getting enough sleep is not a luxury—it is something people need for good health. Sleep disorders can also increase a person’s risk of health problems. However, these disorders can be diagnosed and treated, bringing relief to those who suffer from them.”
-Centers for Disease Control & Prevention (CDC)
The current percentage of adults in the US getting insufficient sleep (less than 7 hours in a 24 hour period) is 32.3%. The percentage in Utah is slightly lower, at 30.9%. Some of us are in that category by choice or habit, while others are involuntarily deprived of sleep by medical conditions.
We talked to Robert Pearson, MD, at Serenity Sleep Center in Cedar City, Utah to find out more about sleep disorders and how to treat them. Dr. Pearson is an otolaryngologist and surgeon with over 28 years experience in the medical field and additional board certification in sleep medicine.

How do you become a “sleep doctor”?
Dr. Pearson: By certification through the Board of Internal Medicine and a one-year fellowship in sleep medicine. Any doctor that wants to specialize in sleep medicine takes the same test, whether you’re an otolaryngologist, pulmonologist, neurologist, or psychiatrist.
What is the most common sleep disorder you treat?
90% of sleep issues I deal with are related to sleep apnea, which is abnormal ten-second or longer pauses in breathing during sleep. This results in tiredness during the day and can cause snoring at night. Apnea worsens medical problems like atrial fibrillation (Afib), high blood pressure, or congestive heart failure. The coexistence of sleep apnea and Afib is very high, so if we treat the apnea, a lot of times the Afib will go away. It’s estimated that about 20% of the adult population has some level of sleep apnea.
What causes sleep apnea?
Most of the time it’s the tongue falling back and obstructing the airway when throat muscles relax during sleep. This is called obstructive sleep apnea and can be influenced by your genetic anatomy, weight, and age. Central sleep apnea is less common and occurs when the brain fails to tell the body to breathe.
How is sleep apnea diagnosed?
When symptoms suggest apnea, a sleep study is recommended. This is where the patient spends the night in a sleep lab for a polysomnography, which monitors 14 different functions including heart and brain activity, sleep stages, air flow, muscle tone, limb movement, oxygen levels, and respiratory effort. Some people need to take a little bit of medication to help them sleep, although we only need about two hours of actual sleep time to determine the presence of sleep apnea.
Another option is a home sleep study, which we do a lot of. Two nights are needed for a home study to get reliable data since it’s unattended by staff. The information gathered from a home study is reasonably accurate, although the gold standard is still polysomnography. Unfortunately, the type of test is often determined by what insurance will cover.
How is sleep apnea treated?
A machine that provides continuous positive airway pressure (CPAP) is very effective in treating peo- ple with moderate to severe obstructive sleep apnea. A CPAP provides mild air pressure through a hose connected to a mask or nose piece to help you breathe better at night.
Although CPAP technology and comfort have improved usage over the years, some people just can't tolerate it. Although not as effective, there is a mandibular advancement device (MAD) that can be worn at night which pulls the jaw forward, creating more space in the back of the throat for the airway. There can be some jaw and teeth discomfort, and it’s important to involve your dentist to make sure alignment isn't affected. The MAD is considered effective first line therapy for people with mild to moderate sleep apnea, and can work with severe cases as an alternative.
There is also a newer surgical implant treatment that has a high efficacy rate for people who can't tolerate a CPAP. A nerve stimulator the size of a pacemaker is inserted in the upper chest under the skin and wired to an electrode in the jaw, which connects to a nerve that moves the tongue. Activated by remote control, the process allows some time to get to sleep, then works by stimulating the tongue to move forward with every breath taken, opening the airway for proper breathing.
A patient with central sleep apnea may need to use a BIPAP, which provides pressure for both inhaling and exhaling, similar to a ventilator.
What other sleep disorders do you find?
Restless leg syndrome can be diagnosed with a sleep study. This is when the legs have uncomfortable sensations with the urge to move them after you lie down to go to bed.
A sleep study can also detect REM sleep behavior disorder. While most people are in a natural state of paralysis while dreaming during the REM (rapid eye movement) stage, this disorder causes verbal and physical responses to dreams; flailing, kicking, or jumping up.
More rare is narcolepsy, or attacks of sleep that come during the day, and accompanying cataplexy, which causes muscle weakness when experiencing intense emotions like laughter or anger. Narcolepsy diagnosis needs both a nighttime and daytime study. Sleep bruxism, or nighttime teeth grinding, is primarily handled by dentists, who can observe signs of tooth wear during check ups. Solutions may include a mouthguard worn at night. Bruxism often diminishes if a patient is receiving treatment for apnea.
continue reading on next page...
What about insomnia?
Insomnia is a very common condition and there are lots of reasons for it. A sleep study does not help diagnose insomnia; we do that based on patient history. It can be a challenge to treat. We can help people understand how sleep works and educate on sleep hygiene; I also recommend keeping a sleep diary. There are medications, but people are variable in their response and finding one that works is a process of trial and error. There are also side effects and long term risks of addiction and dementia. I think it’s best to use sleep medications intermittently - just take them on weekends, for example - which prolongs their efficacy and is safer over time.
I deal with physiology and surgical issues and treatments, but so much of insomnia is behavioral related. I definitely recommend cognitive behavioral therapy for insomnia (CBT-I); studies show that this treatment has at least equally positive results as medications, without the side effects. A therapist can also discover if the insomnia might be linked to depression, bipolar disorder, PTSD, or other conditions,so I often refer patients to mental health providers. It’s hard to find any local therapists that specialize in CBT-I, however, and a lot of insurances don’t cover it, so I know some patients who find online providers.
“Insomnia is a common sleep disorder that can make it hard to fall asleep, hard to stay asleep, or cause you to wake up too early and not be able to get back to sleep. You may still feel tired when you wake up. Insomnia can sap not only your energy level and mood but also your health, work performance and quality of life. At some point, many adults experience short-term (acute) insomnia, which lasts for days or weeks. It's usually the result of stress or a traumatic event. But some people have long-term (chronic) insomnia that lasts for a month or more. Insomnia may be the primary problem, or it may be associated with other medical conditions or medications.” -
Mayo Clinic
What’s your take on melatonin supplements?
Light triggers the production of melatonin in our bodies, which increases throughout the day to a certain level that helps flip the switch to help us fall asleep. Taking a melatonin supplement doesn't work like a sleeping pill; it won't make you drowsy in 20 minutes. Taken earlier, it may help promote sleep by adding to your natural melatonin, but there’s a debate that chronic use could actually suppress your body’s melatonin. So it’s probably best to use it intermittently, although no one actually knows what the right dosage should be.

There are other processes and chemical pathways affecting sleep. Narcolepsy is linked to the absence of hypocretin, a chemical that also helps suppress body movements during REM sleep. Adenosine is a sleep-related chemical which is part of a process that is disrupted by caffeine intake. There's a lot we’re still trying to work out about the complex world of sleep.

What else do you recommend?
Stick to a bedtime schedule and avoid a lot of stimulation right before bed, like eating and exercise. Set the mood for sleep with lower lights. Use glasses that block blue light from screens or alter the device’s display settings for evening use. Or just read a book as opposed to a screen. Blue light exposure is especially a problem with the younger population, who tend to be on video monitors, computer screens, tablets, and phones later into the evening, stimulating wakefulness. Again, exposure to artificial blue light too late and too often interferes with the production of melatonin, a hormone that facilitates sleep onset. I recommend everyone get off screens at least a couple hours before they go to bed. Apnea, narcolepsy, and insomnia all cause tiredness during the day, but the single most common cause is sleep deprivation; we schedule and occupy ourselves to the point we don't have enough time to get adequate sleep. Our bodies need that 7 to 9 hours of sleep to get the full benefit of all the necessary sleep stages every night. Most people get better sleep when put on CPAP machines, but when CPAP patients still show only 5 to 6 hours of sleep it’s often because they’re simply not going to bed early enough to get the hours in. There's lots of data that shows an increase in health problems and mortality if we don't give ourselves enough sleep. Making sleep a priority has to become a habit.
The Promise of Cognitive Behavioral Therapy for Insomnia

By David Heaton, LCSW HEALTH Editor
Cognitive behavioral therapy for insomnia (CBT-I) is now recognized as the most effective non-drug treatment for people with insomnia and is often more effective than medications in the long term. CBT-I has an average treatment effect of at least 50% improvement that tends to last and even improve over time.

What is CBT?
Cognitive Behavioral Therapy is a model of psychological treatment originating in the mid-20th century that explores how cognition (your thoughts), emotions (your feelings), and behavior (your actions) are linked. An underlying principle is that you can use reasoning to choose how you perceive and react to the events and challenges of life. Instead of being a victim of your own irrational beliefs, you can become empowered with the realization that you can control your emotions, thoughts, and actions. This can be challenging, so many people seek help from therapists to guide them through CBT techniques for specific problems.
CBT is the most researched form of psychotherapy and was the first model tested with strict, evidence-based criteria typically used in the health field. The American Psychological Association states that “CBT is an approach for which there is ample scientific evidence that the methods that have been developed actually produce change.” CBT effectively treats depression, anxiety, PTSD, phobias, OCD, eating disorders, addictions, relationship problems; even chronic pain and tinnitus, among other problems.
What is CBT-I?
CBT-I is a cognitive behavioral model specifically designed to treat insomnia, pioneered over 30 years ago by clinical psychologist Arthur J. Spielman. He insisted that insomnia was not just a symptom of other mental and physical health disorders, but could be its own condition requiring specialized attention. A tribute published in the Journal of Clinical Sleep Medicine after Dr. Spielman’s death in 2015 stated that his “main legacy is that he fundamentally changed the way clinicians think about insomnia, and then followed up by changing the way they treat it.”
CBT-I uses several different approaches in treatment, including assessment, education, thought restructuring, behavior- al training, and motivational techniques. It is a brief treatment that is typically provided to individuals or groups in 6-8 sessions, although it has effectively been done in 2-3 sessions, depending on client needs.
How do I find a CBT-I provider?
There are currently some challenges to accessing CBT-I, the first being a shortage of practitioners. Physicians rarely have the capacity to provide it or may be unaware of CBT-I, relying instead on medications as a first-line treatment for insomnia patients.
The CBT-I model is best suited for psychologists and mental health therapists as providers, although the Center for Deployment Psychology observes that “many clinicians are experienced with some of the components of CBT-I but very few have been found to routinely use the full, evidence-based complement of assessments, interventions, and outcome measures in a systematic manner.”
Another limitation is health insurance, which would usually cover CBT-I for insomnia only if caused by diagnosed depression or anxiety. Out-of-pocket cost for therapy, including CBT-I, would run at least $100 per session, which may discourage some people.
What are some solutions?
• Once physicians become aware of the value of CBT-I, they would need community providers to refer insomnia patients to. Otherwise, online or self-help resources are the only options.
• Awareness of the model and Increasing demand for CBT-I services may motivate local therapists to get trained. Many clients with depression, anxiety, and PTSD disorders have some form of insomnia. Trained therapists could provide CBT-I treatment to their insured clients who have those diagnoses. In the meantime, some therapists offer other models to treat insomnia which can still be helpful.
continue reading on next page...
• Group therapy can usually be offered at a lower rate than individual treatment, so CBT-I groups could provide a more affordable option for the uninsured.
• Advancements in technology have made CBT-I therapy available virtually and digitally, enabling people with insomnia to get help where there are no local in-person resources.
• Self-help. Working with a trained professional can help insomnia sufferers with motivation and setbacks, especially if there are also issues with trauma or clinical depression. However, for those of you who are ready to apply CBT-I principles on your own, there are now books, online courses, and apps that can help you learn and apply them. For starters, here are some of those techniques:
Psychoeducation

“Knowing is half the battle”. Learning about how sleep works and why it’s important can help motivate you to make changes in your bedtime habits. Hopefully the articles in this magazine can help with that. Becoming familiar with good sleep hygiene (see page 12) is also a core component of CBT-I; introduce and merge with the other techniques.
Get a baseline
Start a sleep log to track your sleep efficiency. This is how long you’re actual- ly asleep in bed, which should be at least 85%. You calculate sleep efficiency by taking the total time in bed (in minutes) and subtracting the time it took to fall asleep along with any time awake during the night. Divide that number by the total time in bed then multiply by 100.
Example: you went to bed at 11:00pm last night and got up at 6:30am this morning. That’s 7 ½ hours, or 450 minutes. You think it took about half an hour to fall asleep and you remember waking up twice during the night and being awake for about 10 minutes each time. That’s 50 minutes. 450-50=400 minutes of actual sleep. Dividing 400 by 450 equals .89, multiplying by 100 to get 89%, which is in the healthy range.
Track your sleep efficiency for two weeks (some smartwatches and fitness trackers can do this for you). Figure the average to use as a baseline going forward. Continue monitoring your sleep quality as you try CBT-I techniques, noting what is helping (or not). You can discontinue tracking once your sleep has improved to your satisfaction.
Cognitive restructuring
People with insomnia often develop inaccurate thoughts and beliefs about sleep that lead to behaviors that make sleep worse, which further reinforces the negative thoughts. For instance, someone with insomnia is worried about falling asleep so tries to go to bed too early and spends hours in bed experiencing increasing panic about not being able to fall asleep, which in turn actually makes it harder to sleep.
Cognitive restructuring attempts to disrupt this harmful cycle by examining, challenging, and changing the irrational thoughts and beliefs.
Here are some examples of restructuring thoughts:
• Irrational thought: “I haven’t slept for days!” Reality: I may have had poor sleep recently, but I’ve actually slept for at least a few hours every night of my life. New thought: “My body makes sure I always get some sleep. I’m looking forward to improving my sleep hygiene to make it even better.”
• “I can’t sleep, I’m going to be a wreck tomorrow!” vs. “I’ll just get up and read until I get tired. I’ll be fine in the morning. I’ll probably sleep better tomorrow night!’
Stimulus control
If your bed becomes associated with anti-sleep behaviors like eating, working, studying, or watching screens, it may switch from a restful stimulus to a stressful one. Repair this by:
• Using the bed only for sleep and related activities.
• Leave the bed and do something non-stimulating if you’re struggling to fall asleep for more than 10 minutes, then go back to bed when you’re tired.
• Set an alarm for the same time every morning.
• Avoid taking daytime naps.
Sleep restriction
This technique builds on stimulus control, dissociating bedtime from negative experiences while building “sleep pressure” to stabilize sleep cycles.
Using a sleep log to get an average of how much time you are actually sleeping each night (see “Get a baseline” above), you are then only allowed to be in bed for that many hours while keeping the same waking time. If you’re usually in bed for 8 hours but tend to lay awake for around 2 of those hours, you’re only sleeping 6 hours. So, you would start by going to bed at 1am if you have to be up by 7am.
A word of caution; you will likely not sleep through the whole 6 hour period at first (in this example), and naps are not allowed, so you will be dealing with the effects of sleep deprivation for a week or two. You should use caution when driving or operating heavy machinery if you’re feeling sleepy during the day. This technique is also not recommended for people with certain medical conditions, like seizures or bipolar disorder.
When you’re sleeping most of the 6 hours, you would add another 15-30 minutes and go to bed a little earlier every week or so, continuing the process until you are sleeping better through the night and feeling rested during the day.
Relaxation training
These techniques can enhance your natural relaxation response while decreasing the anxiety and racing thoughts that often come with being unable to sleep. They can become part of your bedtime routine when you lie down at night.
• Breathing exercise involves taking slow, deep breaths, which have a calming effect on your heart rate, anxiety, and stress. A suggested pattern is to inhale through the nose for 4 seconds, hold for 7, then exhale through the mouth for 8 seconds. Repeat six times.
• Progressive muscle relaxation is the process of tensing and relaxing your muscle groups, moving from the toes to the head (or vice versa) as you lie comfortably in bed.
• Guided imagery is the practice of envisioning an actual or imaginary calming scene, then taking time to become aware of the sights, sounds, and sensations you might experience there. Some people combine visualization with breathing and muscle relaxation. Music or a recorded voice narrator can be used as well.
• Biofeedback uses technology to monitor brain waves, heart rate, breathing, and temperature. When connected to these devices, you can use relaxation techniques to watch your body’s stress readings decrease in real time, reinforcing your ability to control your reactions to stress. Office visits for biofeedback or home-use devices can be pricey, but you can use an inexpensive pulse oximeter on your finger to watch your heart rate decrease as you try relaxation exercises.
• Meditation: Learning to focus attention through meditation has shown to reduce stress and anxiety while increasing relaxation. Practicing forms of meditation during the day that involve movement, like yoga or Tai Chi, promotes mindfulness skills that will help your approach to sleep as well.
Things to consider
Don’t get discouraged if CBT-I doesn't work right away. It can take time to learn and practice new skills. You might experience some sleep deprivation at first when implementing stimulus control and sleep restriction, but this should soon resolve as your body adjusts to a more consistent schedule. Some people find it helpful to track their progress over time in order to see small improvements that can encourage them to continue treatment.
The success of self-initiated CBT-I techniques will largely depend on your ability to make them a daily priority. Sleep logs, sleep hygiene, and reprocessing automatic thoughts need daily attention to be the most helpful.
Medications
Jeffrey Rossman, PhD, notes that “Although sleep medication can be an effective short-term treatment for insomnia, some patients experience side effects such as amnestic episodes, cognitive impairment, and morning hangover.” He continues, “whereas sleeping pills mask the symptoms of insomnia, CBT-i promotes a genuine learning process that restores the body’s natural sleep mechanism.” Still, patients who are taking sleep medications should consult their doctor before weaning off or discontinuing them.
Other uses
CBT-I shows potential for working with short-term insomnia and people who are struggling with insomnia due to pregnancy, PTSD, and cancer recovery.
DIY CBT-I resources
The Department of Veterans Affairs offers their own app, called CBT-I Coach, that is appropriate for non-veterans and veterans alike. CBT-I Coach is a free, self-help mobile app to guide you through developing and maintaining good sleep habits.
The VA also has a web-based CBT-I program that can be used on devices or computers, called SleepEZ , found at veterantraining.va.gov/insomnia.
There are a variety of CBT-I based online programs available for purchase, from the Cleveland Clinic’s 6-week Go! To Sleep program ($40 at clevelandclinicwellness.com ) and the Conquering Insomnia program by Dr. Gregg Jacobs ($50 at cbtforinsomnia.com ) to more expensive options costing several hundred dollars.
While they can be used on their own, these resources are not intended to replace therapy.
Standard Time vs. Daylight Saving Time

By Eric Suni Guest Columnist
The United States started daylight saving time in 1918 and has implemented and repealed it at various times since then. It was created primarily to reduce energy consumption and promote commerce.
Yes, daylight saving time started again on March 12 and ends on Nov. 5, 2023. For much of the United States, daylight saving time is a part of our lives again — despite efforts to legislate out the time change. On March 15, 2022, just days after clocks were adjusted to “spring forward,” the U.S. Senate passed the Sunshine Protection Act, which would abolish clock changes in favor of daylight saving time year-round.

By establishing a stable time, the new law would prevent sleep disruptions that occur from biannual clock changes. Switching to per- manent daylight saving time, however, could interfere with quality sleep. Groups such as the American Academy of Sleep Medicine as well as many experts, oppose permanent daylight saving time and prefer the idea of permanent standard time.
Daylight saving time reduces exposure to morning sunlight, which makes it harder to wake up in the morning. More light in the evening may make it harder to fall asleep at night. In addition, the shift in the timing of daylight exposure can affect the body’s internal clock, which follows a 24-hour schedule known as a circadian rhythm.
So is daylight saving time becoming permanent or ending permanently any time soon? Not necessarily, as the Sunshine Protection Act still requires approval by the House and President Joe Biden. That didn’t occur with the 2022 version of the bill. But in March 2023, not long before the clocks changed again, Sen. Marco Rubio, R-Florida, reintroduced it to the Senate, with a similar bill also introduced in the House. Either bill would bring major shifts in our clocks, daylight exposure, and sleep if it were to become law.
A new study by the American Academy of Neurology says that the November time change may be the one that hurts. The analysis of 30,000 Ca- nadian adults found that in the week following the changing of clocks in the fall, people experienced the following:
• 115.2% increase in difficulty falling asleep
• 102.8% increase in excessive daytime tiredness, or hypersomnia
• 64% increase in difficulty staying asleep
• 34% increase in sleep dissatisfaction
Although dozens of states have considered legislation to end clock changes, only federal action can establish permanent daylight saving time in the United States. Legislators in some states that would move to permanent daylight saving time, if federal action allows it, are now second-guessing that move. States may be able to opt out of daylight saving time (as Hawaii and most of Arizona already do), choosing permanent standard time.
So far, there has been no significant action on the Senate or House bills to make daylight saving time effective year-round. As it stands, daylight saving time will end again on Nov. 5, 2023.
Excerpted from Latest Updates: What’s Happening With Daylight Savings Time? www.sleepfoundation.org. Used with permission.
Currently, daylight saving time begins the second Sunday in March at 2:00 am (clocks skip forward one hour) and ends on the first Sunday in November at 2:00 am (clocks turn back one hour).
Utah passed legislation in 2020 calling for permanent daylight saving time if federal law allows them to do so, as long as at least four out of ten other western states make the move as well. Seven are now on board, so the law is now awaiting Congressional approval.