
12 minute read
Interview Spotlight: Dr. Eric Brown
from MeduCollab: Issue 1
Interview Spotlight: Novel Strategies in Combating Antibiotic-Resistant Bacteria
HANNAH SILVERMAN Bachelor of Health Sciences (Honours) Class of 2023
Advertisement
Dr. Eric Brown is a Distinguished Professor in the Department of Biochemistry and Biomedical Sciences at McMaster University and a member of the M.G. DeGroote Institute for Infectious Disease Research. A recipient of several awards in the field of molecular biology and biochemistry, Dr. Brown’s research is primarily focused on understanding the systems that drive drug resistance in superbugs. He currently serves as the Director of the Biomedical Discovery and Commercialization Program as well as the Canada Research Chair in Chemical Biology.
Can you tell us how you got started in the field of microbiology and infectious disease research?
I was a postdoctoral fellow at Harvard Medical School in Boston, and I was studying enzymes that are involved in synthesizing cell walls in bacteria. Quite honestly, I had no idea that [I] was doing something that might be useful —I was just really fascinated with how bacteria built their own cell walls. But that was a time in the early 90s where drug resistance was beginning to rear its head in the clinic, and I became aware then that the work I was doing may have some practical utility [by] way of discovering new antibiotics.
The problem of antibiotic resistance has been described as an ‘arms race’ between the scientists creating novel antibiotics and the superbugs who mutate to resist them. Since the majority of antibiotics today are just variations of the same classes discovered decades ago, how does your lab differ in its approach to antibiotic research and development?
The fundamental problem that surrounds drug resistance is that existing drugs are really just tweaks on existing chemical classes, and so there’s been a real lack of innovation in antibiotic discovery. The most recent discovery of a new chemical class of antibiotics was actually in the 80s, so [it’s] quite remarkable that there’s been so little innovation [since] that time. In my group, we’re trying to think about completely new ways of discovering antibiotics. Much of the effort that’s happened over the last 30 years or so has been rooted in fairly reductionist [and] industrial approaches to drug discovery, which in the modern era, involve genomics to discover what’s the right target, recombinant DNA technology to express and purify a target, large chemical libraries over that target, and then medicinal chemistry to make that compound better. What’s at issue there is a fundamental lack of understanding of the system as a whole, before these reductionist approaches are commenced. A lot of what we do [at my lab] is [to] try to understand the bug as a system, think about studying the whole organism in the context of drug discovery, and then letting the bugs tell us what will work best.
Antibiotic resistance has been recognized by the World Health Organization and many countries worldwide as a serious and urgent threat, making it now a research priority. Looking to the future, do you think that we will be able to continue to combat this problem effectively using antibiotics, given the rate at which bacteria are becoming multi-drug resistant?
Yes. The solution to the drug resistance problem is, in part, new antibiotic drug discovery. There needs to be stewardship measures to reduce the use of antibiotics. We need to be really mindful about the way that we treat disease. But there is always going to be a need for antibiotics. If you think about straightforward surgeries and things that we take for granted, like hip replacements and cancer chemotherapy, all of these are interventions that just require antibiotics. It’s hard for me to imagine a world where antibiotics aren’t necessary, where we’re so careful about infection and we’re so good at stewardship that we no longer need antibiotics. I think they’re here to stay. Let’s hope they’re still useful for the future.
You recently conducted some interesting research regarding the antibiotic properties and mechanisms of cannabigerol (CBG), a cannabinoid compound found in Cannabis Sativa. What do you think are the broad implications of your findings for future pharmaceutical research?
Canada kind of jumped with both feet into the legalization of cannabis, and we thought that would give us a bit of a leg up in such studies. We were inspired that the plant makes all these cannabinoids: why is it doing this? [We] don’t think it’s doing that for the sake of recreational cannabis. Our hypothesis was the plant was making these molecules for a reason, and that might be for their antibacterial, antifungal, and antipest properties. There was certainly some evidence in the literature [indicating] that was true, but we went pretty deep to reveal that there are indeed some really strong antibacterial properties of these compounds. CBG is a non-psychoactive compound that we’re interested in because these molecules have known properties that make them amenable for usage as drugs. After all, THC and other compounds are sort of famous for [their] vile bioavailability through various routes of administration, [as they] cross the blood brain barrier. These compounds themselves have unique and special properties that might make them suitable as a starting point for drugs. We think that we’ve got a long way to go. I think with a molecule like CBG, there are some toxicity issues with that compound, especially its mechanism of action. It’s a membrane-active compound, and so I think there can be some issues of host toxicity there. But it’s a really interesting starting point for a new drug.
One of your lab’s recent discoveries was finding a compound that reverses β-lactam resistance in methicillin-resistant Staphylococcus aureus (MRSA) infections. Could you elaborate on your findings, and the importance of this compound for combating MRSA infections?
Yes, this [was] a really fun project in my lab. We’ve been working in MRSA cell wall synthesis for about 20 years, interested in a particular pathway. We ran a screen for chemicals that would interfere with that aspect of cell wall synthesis. Knowing that there might be interacting pathways, it kind of gets back to my obsession with the system as a whole, and how cells are really complex in the way they respond. It turned out [that] we identified a compound that hit a pathway that was interacting [with], but quite separate from, our starting hypothesis —a gene product that was involved in helping cells respond to an assault on cell surface. It turns out that this target had a lot of really interesting effects for the bacterium. It made it difficult for the organism to make a biofilm, it slowed its growth, it halted its virulence in a worm model of infection, and it [reversed] drug resistance. This thing is a ‘Swiss Army knife’ of targets. All kinds of really interesting consequences to the inhibition of this target ensued when we found this compound. [However,] it has less than perfect physical and chemical properties in order to be a drug. In other words, we didn’t pull a [fully developed] drug out of our compound libraries here. It requires more chemistry to turn it into something that would be closer to a drug. It’s probably not work that we’ll do here, but certainly, I’m hoping that people will read our paper and be inspired by that compound and that target, and try to move that forward.
What are some of the major obstacles preventing effective antibiotic research from a scientific and societal standpoint, and how are you working to resolve them?
I touched on the science stuff earlier, in terms of these largely reductionist approaches with modern discovery. I think that’s certainly a hurdle —understanding the system, [which is] something that we’re really interested in. There’s another really interesting and quite difficult hurdle, which is economic. All drugs are paid for on a ‘per prescription’ basis. In other words, they’re paid for in terms of volume of use. If you think about it, that’s exactly the wrong thing for an antibiotic. We really want to discourage high volumes of use of antibiotics, because we know that with use comes resistance. Stewardship demands that we use as little of a drug as possible, [but] on the business side, that’s the worst possible thing for a pharmaceutical company —to come up with a drug that’s use will be restricted. If you think about it, a designer new antibiotic that’s really effective and could save a patient’s life in the ICU is one which will see very, very low volume of use. It will be used as a last resort. So one of the biggest obstacles is having to [incentivise] pharmaceutical companies to discover and develop drugs like these. There are a lot of interesting proposals [brought] before legislators and thought leaders about how to incentivise this industry, and some of the most interesting ones involve decoupling volume from value. That would be a first —to pay for the value of a drug and not the volume of a drug. It’s a really interesting problem.
Do you foresee a change in policies surrounding antibiotic usage in hospitals, now that the world is becoming more aware of this threat?
Yeah, certainly worldwide there are very different approaches to the provision of antibiotics. There are many countries in the developing world where antibiotics can be [purchased] over the counter very, very simply. It’s different here in Canada, of course, and I think we’re seeing a greater and greater emphasis on stewardship in this country. I think we’re going to see even more in the future. So [the question is] whether or not that will take the form of policy or it will become part of the culture of antibiotic use [and] prescription —more the latter, it’s difficult to come up with policies. Certainly when physicians are prescribing, they’re going to be aware of the best practices. There’s going to be greater and greater emphasis on what’s the first line, second line, third line antibiotic, when to be prescribed
“If you’re an this one, [and] when to avoid preundergraduate right scribing any at all. I think there’s now in the social going to be a culture of stewardship and best practices that is going to sciences, think about improve. But I’m not sure that there’ll health economics be necessarily strict policies around this. It’s difficult to be too prescriptive and think about about what is the right course of action policy that would necessarily in the clinic. get around the All things considered, given the pace of andifficulties in the tibiotic research now and current practices, do you think we’re on top of this fight? Do you discovery and think we’re going to be able to control superdevelopment bugs? of new I am concerned, particularly with the [fact that] antibiotics.” we’ve seen a significant departure of pharmaceuti cal effort in this area. The research intensity of phar maceutical companies really correlates to return on investment for shareholders. That’s a big concern —it really hampers our ability to deal with this. I think it is a very significant part of the lack of innovation over the last several decades in this research area. That concerns me a lot. What gives me a lot of hope is [that] there’s been no time, at least in my career, where there’s been a greater understanding of this problem. We’re seeing a lot of discussion among legislators [and] a lot of concern among governments and non-governmental organizations worldwide. If that can be translated into action, I think we’ll be in good shape, but it is a difficult problem to tackle. It’ll require multinational cooperation. That’s a realm of research that I don’t engage in and that’s really something for the social scientists to tackle. If you’re an undergraduate right now in the social sciences, think about health economics and think about policy that would get around the difficulties in the discovery and development of new antibiotics.
What’s your favorite part of working in microbiology research?
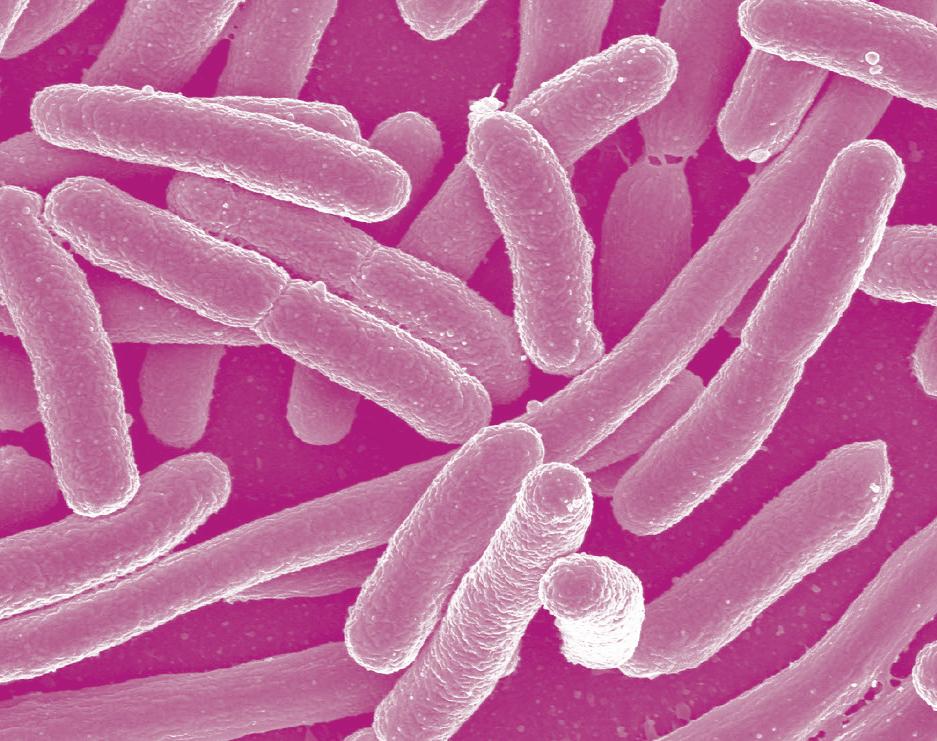
I think it’s such a great area, the model systems are really straightforward to work with. I witness the struggles of my colleagues to work with things like human stem cells and how difficult that is, and there’s just tremendous power in how simple it is to work with bacteria to do biochemistry on an organism. A doubling time [of bacteria] in the laboratory of 20 minutes is really helpful. Microbiology in general is amazing because it’s in us, it’s all around us. We kind of ignore it but there are more bacterial cells in and on the human than human cells. And increasingly, we’re recognizing how important that is and
what the role of microbial physiology is in human physiology. So, the microbes are a big part of human life. Of course, you [can] start thinking about the environment and the diversity of bacteria in the environment, from the deep oceans to the soil, and it’s just staggering to think of the microbial complexity. I think there [will be] a lot of research projects in microbes for many years to come.
What are some exciting projects happening at the M.G. Degroote Institute for Infectious Disease Research?
[The Research Institute] is a really fantastic place to work and [has] great colleagues to interact with in terms of the research area close to my heart, which is antimicrobial drug resistance. You’ve got fantastic work coming out of Gerry [Wright]’s lab in the area of natural products —he’s really interested in trying to [mimic] molecules that are made by nature to deal with drug resistance. Many of the existing antibiotics are products of bacterial metabolism, and in recent years, drug companies have [reused] these approaches. So [it’s] kind of a Back to the Future approach, but really exciting with the new technologies that are available now to deal with natural products. Laura Burrows is interested in really interesting topics that have to do with things like biofilm formation. Biofilms are a hugely important problem in bacteria being difficult to treat with antibiotics. They go into these quiescent and structured communities that are difficult to treat with antibiotics. People like Andrew McArthur are running computational, dry lab only research programs. [They] are really interested in the catalog of drug resistance chains that are out there, and it’s a staggering effort that they’ve done, for example, to build a database that’s used by people worldwide to try to understand the scale of drug resistance. Those are three examples [of what] I think are pretty cool things going on here.
Do you have any advice for undergraduate students considering a career in biomedical/infectious disease research?
Infectious disease research is really interesting, to me anyway. I think it’s something that we take for granted, when we just expect these antibiotics to work and we expect to be able to take care of infections. We’re currently going through a huge scare worldwide with the novel coronavirus that I think reminds us that the microbes are really quite capable and quite clever. I think, for undergraduates, there are a lot of opportunities here at McMaster in particular. This university has a particular strength in this research area. I think that’s something to think about in terms of projects, in terms of students thinking about spending a summer in a lab or doing a thesis project, as it is possible for students to make really significant contributions, in part due to the ease of manipulation of these model systems.









