The Modern
Equine Vet www.modernequinevet.com
Vol 10 Issue 2 2020
Interpreting Antimicrobial Test Results Ask the Nutritionist? Supporting Joint Development EIV Prevalence Increasing in US Prebiotics Might Do More Harm Than Good Technician Update: Snake Bite Emergency
CHECK OUT: ASK THE NUTRITIONIST? YOUR NUTRITION QUESTIONS ANSWERED
TABLE OF CONTENTS
E. coli
COVER STORY
4 Interpreting Antimicrobial Janice Haney Carr
Test Results for Horses Cover: Medical Illustrator/ Meredith Newlove
ASK THE NUTRITIONIST?
How Can I Support Joint Health in Young Horses?............................... 3 INFECTIOUS DISEASES
Data Show Increasing Flu Prevalence....................................................... 8 DENTISTRY
Getting the Perfect Regional Block.........................................................13 TECHINICIAN UPDATE
Snake Bite—More Than Just a Pain in the Nose................................16 NEWS
Want to Help Australian Animals?...........................................................15 Prebiotics May Do More Harm Than Good.............................................19 ADVERTISERS Purina Sponsored Content.........................................3 Merck Animal Health........................................5 American Regent Animal Health/Adequan...........7
Heska..............................................................................9 American Regent Animal Health/BetaVet...........11 AAEVT............................................................17
The Modern
Equine Vet SALES: Matthew Todd • Lillie Collett EDITOR: Marie Rosenthal ART DIRECTOR: Jennifer Barlow CONTRIBUTING WRITERS: Paul Basillo • Adam Marcus COPY EDITOR: Patty Wall Published by PO Box 935 • Morrisville, PA 19067 Marie Rosenthal and Jennifer Barlow, Publishers PERCYBO media publishing
2
Issue 2/2020 | ModernEquineVet.com
LEGAL DISCLAIMER: The content in this digital issue is for general informational purposes only. PercyBo Publishing Media LLC makes no representations or warranties of any kind about the completeness, accuracy, timeliness, reliability or suitability of any of the information, including content or advertisements, contained in any of its digital content and expressly disclaims liability of any errors or omissions that may be presented within its content. PercyBo Publishing Media LLC reserves the right to alter or correct any content without any obligations. Furthermore, PercyBo disclaims any and all liability for any direct, indirect, or other damages arising from the use or misuse of the information presented in its digital content. The views expressed in its digital content are those of sources and authors and do not necessarily reflect the opinion or policy of PercyBo. The content is for veterinary professionals. ALL RIGHTS RESERVED. Reproduction in whole or in part without permission is prohibited.
SPECIAL ADVERTISING SECTION
Ask the
Nutritionist DR. ROBERT JACOBS, PH.D., EQUINE INNOVATION MANAGER, PURINA ANIMAL NUTRITION
?
Ask the Nutritionist is a monthly column featuring questions answered by PhD equine nutritionists and sponsored by Purina Animal Nutrition. Have a nutrition question you want to see featured? Email Marie Rosenthal. For clinics looking for specific nutritional advice, visit purinamills.com/ask-an-expert.
What nutritional strategies support proper joint development in young horses? Joint and bone abnormalities, collectively known as developmental orthopedic disorders (DODs), are a common growth complication in young horses. There are several nutritional strategies to support proper joint development, but it’s critical to remember that DODs are a function of many factors, including genetics, management and nutrition. A multifaceted approach may limit the incidence and severity of DODs. Here are some guidelines when thinking about young horse growth: • Plan and determine your growth goals early: rapid vs. moderate vs. slow rate of gain. • Continually monitor growth by measuring the horse’s body weight, wither height and/or hip height. Look for steady growth without the fits and starts often associated with greater incidences of DODs. FEEDING PRINCIPLES FOR YOUNG GROWING HORSES Feed a young growing horse a diet composed of forage (minimum 1% of bodyweight) and a concentrate feed formulated specifically for young growing horses. Feeds like Purina® Ultium® Growth Horse Formula, Purina® Horse Feed or Purina® Impact® Professional Mare & Foal Horse Feed are specifically formulated to provide energy for growth while supporting optimal bone growth and development. Feeding good quality forages ensures that the foal will receive the fiber necessary to develop hindgut function. However, one must account for the nutritional contribution of forage. Forage intake should be monitored and possibly restricted in faster growing foals to avoid excess calorie intake. In cases where forage alone can supply adequate calories to the young horse, a ration balancer such as Purina® Enrich Plus® Ration Balancing Horse Feed can be fed to provide the protein, vitamins and minerals necessary in the precise balance required for sound growth. When forage quality is poor, providing a complete feed, such as Purina® Equine Junior® Horse Feed is an ideal way to ensure the foal is receiving the necessary roughage plus the required energy and nutrients in the optimal ratios. If a growing horse shows signs of a DOD, start with nutrition and reduce energy intake. The goal is to reduce dietary calories without restricting necessary nutrients. Consider a ration balancer, like Purina® Enrich Plus® Ration Balancing Horse Feed to
provide essential nutrients, in addition to feeding forage to supply calories.
Here are some specific feeding strategies by life stage: NEWBORN FOAL Early in a foal’s life, the mare’s colostrum and milk supply all the nutrients it needs. Ensuring the mare eats a nutritionally balanced diet during gestation and lactation will help her to produce nutrient-rich milk, which can lay the foundation for sound foal growth. As the mare’s milk decreases in quantity and nutrients, support the nutritional requirements of growth with nutrients from other feed sources, such as Purina Ultium Growth®. WEANING Prior to weaning, ensure the foal is consuming adequate levels of a concentrate specifically formulated for growing horses to help maintain a steady growth rate. Weaning can be a stressful time and young horses may experience gastric discomfort. Feeding Purina® Outlast® Gastric Support Supplement can support proper pH of the young horse’s stomach during this stressful period. Feeding the young growing horse is an exercise in patience and planning. The goal of any feeding program should be to promote sound growth and development by providing optimal nutrition. Each foal and DOD case is unique, so create an individualized nutrition plan based on the specifics of each animal. Contact a Purina Ph.D. nutritionist for consultations through Purina Customer Service, 800-227-8941 or send us a message at www.purinamills.com/ask-an-expert.
UPCOMING TOPICS March: Foal nutrition • April: Special needs of the competition horse Have a question you want to see featured? Send them to modernequinevet@gmail.com.
ABOUT THE AUTHOR Dr. Robert Jacobs is the Equine Innovation Manager at Purina Animal Nutrition. He is responsible for conducting research aimed at better understanding how nutrition impacts various areas of equine physiology. SPONSORED BY PURINA ANIMAL NUTRITION
ModernEquineVet.com | Issue 2/2020
3
INFECTIOUS DISEASES
Interpreting Antimicrobial Test Results F O R B y
H O R S E S
M a r i e
R o s e n t h a l ,
M S
Antimicrobial resistance is not just a concern for MDs. A wide range of equine pathogens, including Salmonella, Escherichia coli and other Enterobacteriaceae, Staphylococcus, Klebsiella and Pseudomonas, are developing resistance to the drugs veterinarians use regularly to treat their patients. 4
Issue 2/2020 | ModernEquineVet.com
Because of resistance, physicians are turning more frequently to susceptibility testing to guide antimicrobial therapy choices and improve the efficacy of the drugs they prescribe to their patients. Culture and susceptibility testing is underused in veterinary medicine because of time delays and challenges in interpreting the results. However, susceptibility testing can also help guide equine therapy, K. Gary Magdesian, DVM, DACVIM, DACVECC, DACVCP, explained at the American Association of Equine Practitioners 65th Annual Convention in Denver. Just as done in human medicine, empiric antibiotic treatment can be fine-tuned once the cultures and the susceptibility results are back. Pay attention to the minimum inhibitory concentration (MIC) of an isolate, which refers to the lowest concentration of an antimicrobial that inhibits the growth of that isolate. “The lower the MIC number of a given antimicrobial, the more susceptible the isolate is,� said Dr. Magdesian, who is a professor of Medicine and Epidemiology at the University of California Davis, School of Veterinary Medicine.
Medical Illustrator: Jennifer Oosthuizen
Pseudomonas
The Science of Unique
Fenbendazole Mode of Action: Unique mode of action is what makes Panacur® (fenbendazole) so effective against the most dangerous parasites of the horse
Deep Penetration
Helps Control Parasites
Protects Cells & Organs
Effective against all stages of encysted small strongyles1
Effective against ivermectin resistant ascarids2
More attracted to the cells of the parasite than of the animal being treated3
See the Difference Scan code to watch our video and learn how Panacur® works differently than other dewormers at panacur-mode-of-action.com
2 Giralda Farms Farms • Madison, NJ 07940NJ • merck-animal-health-usa.com • 800-521-5767 2 Giralda • Madison, 07940 • merck-animal-health-usa.com • 800-521-5767 Copyright © 2020©2018 IntervetIntervet, Inc., d/b/aInc, Merck Animal Health, a subsidiary & Co.,of Inc. Copyright d/b/a/Merck Animal Health,ofaMerck subsidiary Merck & Co. Inc. All rights reserved. 18-Merck-MOA PP AD • US/EQD/0119/0001
Consult your veterinarian for assistance in the diagnosis, treatment and control of parasitism. Do not use in horses intended for human consumption. When using Panacur® (fenbendazole) Paste 10% concomitantly with trichlorfon, refer to the manufacturer’s label for use and cautions for trichlorfon. PANACUR (fenbendazole) POWERPAC equine dewormer product label. Reinemeyer CR, Vaala, WE. Larvicidal efficacy of fenbendazole against a macrocyclic lactone-resistant isolate of Parascaris equorum in foals. Proceedings of the 55th Annual Meeting of the American Association of Veterinary Parasitologists. 2010, Atlanta, GA, p49. 3 Lacey E. Mode of Action of Benzimidazoles. Parasitology Today, vol. 6, no. 4, 1990. 1 2
INFECTIOUS DISEASES
Susceptibility Breakpoints for Common Antibiotics Used in Adult Horses DRUG
SUSCEPTIBILITY BREAKPOINT
ADMINISTRATION
Chloramphenicol
≤1 µg/mL
50 mg/kg PO every 6-8 h
Enrofloxacin
≤0.25 µg/mL
7.5 mg/kg once daily1
Trimethoprim-Sulfa
≤0.5 µg/mL for trimethoprim/9.5 µg/mL for sulfonamide
30 mg/kg PO every12 h2
Minocycline
≤0.25 µg/mL
4 mg/kg PO, every 12 h
Doxycycline
≤0.25 µg/mL
10 mg/kg PO every 12 h
1. In some cases: ≤0.5 µg/mL could be targeted after administration of enrofloxacin tablets either orally or intragastrically. 2. Except for Equisul SDT, which would be 24 mg/kg PO, every 12 hours Magdesian G. AAEP Proceedings 2019, Vol. 65
Susceptible, Intermediate, Resistant: What Does That Mean? A SUSCEPTIBLE (S) ORGANISM, usually designated by S, means the antimicrobial concentrations needed to inhibit the organism are readily achieved in serum after recommended equine dosing, i.e., the antibiotic is appropriate. INTERMEDIATE (I) MEANS the antimicrobial concentrations needed to inhibit the organism may or may not be achievable in serum after recommended equine dosing, i.e, there is a chance the therapy might not work. RESISTANT (R) MEANS the antimicrobial concentrations required to inhibit the organism is higher than the achievable serum concentrates after recommended dosing, i.e, the antibiotic is inappropriate for this infection. Magdesian G. AAEP Proceedings 2019, Vol. 65
Some laboratories don’t report the MIC, but instead report whether an isolate is “susceptible,” “resistant” or “intermediate” to the tested antimicrobials. Laboratories report susceptibility breakpoints set by the Clinical and Laboratory Standards Institute. The susceptibility breakpoint is the lowest concentration of an antibiotic that inhibits bacterial growth and can be achieved in the patient after conventional dosing, Dr. Magdesian explained. These values are based on the pharmacokinetics of the individual drug, the target species and the MIC of the bacterial isolate. Feline veterinarians are always saying that cats are not small dogs when it comes to medications. The same idea can be applied to medications for horses: horses are not humans—they often have decreased bioavailability of oral medications, so the achievable serum and concentra-
tion of these drugs are different for horses than humans. This is important to keep in mind because CLSI provides veterinary susceptibility breakpoints for just a few antimicrobials for horse, so some of the results on that report from the diagnostic lab on your desk or phone might be based on the susceptibility breakpoint for human patients. This is less of an issue for IV or most intramuscularly administered equine drugs, “because the cutoff values used for susceptibility in terms of MICs would be the same or similar among horses, small animals and humans. “For example, if we're talking about IV penicillin or IV cephazolin, then the human breakpoints would apply,” he said. Because of a horse’s decreased bioavailability for many orally administered medications, the human values won’t necessarily apply, according to Dr. Magdesian. “If the diagnostic lab is using human values, the microbe could appear susceptible when in reality, the horse can't achieve those same concentrations.” A good example is cloramphenicol. For humans, the CLSI guideline is 8 µg/mL as a susceptibility break point for most bacteria, which means if the isolate has an MIC of 8 µg/mL or below, it would be considered susceptible. If the MIC is above 16, it would be considered resistant. “That's for humans. Now, can horses achieve 8 µg/mL of chloramphenicol in their plasma after oral administration? No, most horses don’t achieve such levels because of reduced bioavailability,” Dr. Magdesian said. For horses, a susceptible isolate would have an MIC of 1 or 2 µg/mL or less for chloramphenicol, because that is the plasma level that can be reached in most horses using recommended oral dosing. “If the microbe is inhibited at that concentation, then it would be considered susceptible for horses. If the microbe isn’t inhibited by that achievable concentration, then it should be considered resistant in horses,” Dr. Magdesian said. “The thing to keep in mind here is that the lab you’re using may be using human standards when they are not available for horses,” he said. “It will tell you an isolate is susceptible when in reality it isn't [for your equine patient],” he said. When in doubt call the laboratory and ask for the actual MIC, rather than just the susceptibility (S) or resistant (R) designation, especially for orally administered antimicrobials. MeV
For more information: Silley P. Susceptibility testing methods, resistance and breakpoints: What do these terms really mean? Rev Sci Tech. 2012;31:33-41. https://www.oie.int/doc/ged/D11778.PDF 6
Issue 2/2020 | ModernEquineVet.com
There’s nothing else like it. Over the past 30 years, Adequan® i.m. (polysulfated glycosaminoglycan) has been recommended millions of times1 to treat degenerative disease, and with good reason. From day one, it’s been 2, 3 the only FDA-Approved equine PSGAG joint precription available, and the only one proven to. Restore synovial joint lubrication Repair joint cartilage Reverse the disease cycle Reduce inflammation When you start with it early and stay with it as needed, horses may enjoy greater mobility 2, 4, 5 over a lifetime. Discover if Adequan is the right choice. Talk to your American Regent Animal Health sales representative or call (800) 458-0163 to order. BRIEF SUMMARY: Prior to use please consult the product insert, a summary of which follows: CAUTION: Federal law restricts this drug to use by or on the order of a licensed veterinarian. INDICATIONS: Adequan® i.m. is recommended for the intramuscular treatment of non-infectious degenerative and/or traumatic joint dysfunction and associated lameness of the carpal and hock joints in horses. CONTRAINDICATIONS: There are no known contraindications to the use of intramuscular Polysulfated Glycosaminoglycan. WARNINGS: Do not use in horses intended for human consumption. Not for use in humans. Keep this and all medications out of the reach of children. PRECAUTIONS: The safe use of Adequan® i.m. in horses used for breeding purposes, during pregnancy, or in lactating mares has not been evaluated. For customer care, or to obtain product information, visit www.adequan.com. To report an adverse event please contact American Regent, Inc. at (800) 734-9236 or email pv@americanregent.com. Please see Full Prescribing Information at www.adequan.com.
1 Data on file. 2 Adequan® i.m. Package Insert, Rev 1/19. 3 Burba DJ, Collier MA, DeBault LE, Hanson-Painton O, Thompson HC, Holder CL: In vivo kinetic study on uptake and distribution of intramuscular tritium-labeled polysulfated glycosaminoglycan in equine body fluid compartments and articular cartilage in an osteochondral defect model. J Equine Vet Sci 1993; 13: 696-703. 4 Kim DY, Taylor HW, Moore RM, Paulsen DB, Cho DY. Articular chondrocyte apoptosis in equine osteoarthritis. The Veterinary Journal 2003; 166: 52-57. 5 McIlwraith CW, Frisbie DD, Kawcak CE, van Weeren PR. Joint Disease in the Horse.St. Louis, MO: Elsevier, 2016; 33-48. Adequan and the Horse Head design are registered trademarks of American Regent, Inc. © 2019, American Regent, Inc. PP-AI-US-0222 2/2019
INFECTIOUS DISEASES
Data Show
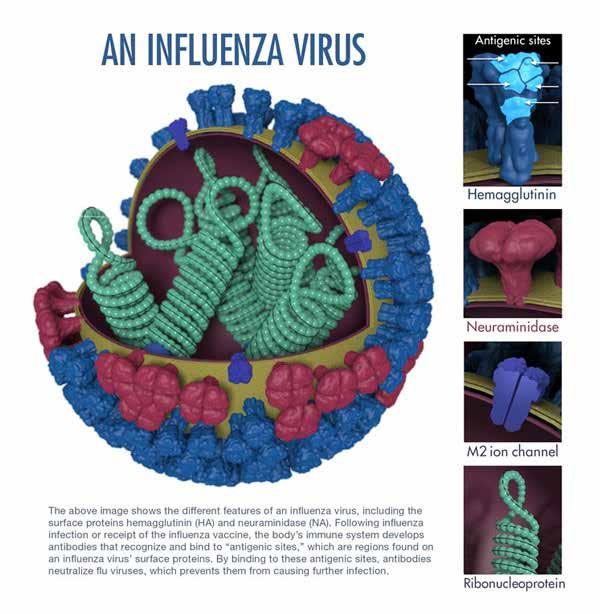
Increasing Flu Prevalence 2. Clinical signs. The most common signs associated with EIV were fever, nasal discharge and cough. Study authors emphasize that subclinical signs may occur in EIVvaccinated horses. 3. Age. Horses between 1 and 9 years old tested positive for EIV most often. 4. Breed. Quarter Horses tested positive most frequently with a lower-than-expected EIV prevalence in Thoroughbreds. 5. Use. Competition horses accounted for 42.1% of positive EIV cases followed closely by pleasure horses at 37.9%. 6. Transport. Horses with a history of recent transport were more likely to test positive for EIV. 7. Exposure. Horses living on premises with multiple affected horses were more likely to also become infected. Horses vaccinated against EIV were still at risk of contracting the virus, according to the study. In fact, of the horses with known vaccination status, 61% of positive EIV cases occurred in horses vaccinated against EIV.
Tracking an evolving target
Image courtesy of Merck Animal Health
Cases of equine influenza virus (EIV) are on the
8
rise overall since 2008, according to a new study presented at the recent American Association of Equine Practitioners (AAEP) annual convention in Denver (Figure 1). The longitudinal study examined nasal secretions from more than 7,800 horses presenting with fever and upper respiratory tract infection (URTI) from March 2008 through February 2019. The study revealed 7 key considerations for veterinarians when designing EIV vaccination and management strategies: 1. S eason. Peak EIV occurrence took place in the winter and spring months (Figure 2).
Issue 2/2020 | ModernEquineVet.com
Influenza outbreaks in well-vaccinated horses 3. generally are indicative of significant genetic changes in the influenza virus—known as antigenic drift—and inadequate protection. This theory is backed by the study, which cumulatively analyzed data on equine URTI from the Equine Respiratory Biosurveillance Program managed by Merck Animal Health in partnership with the University of California, Davis School of Veterinary Medicine. “While equine flu evolves more slowly than human flu, the antigenic drift we’re seeing means today’s EIV is significantly different from what we saw even 10 years ago,” said lead study author Wendy Vaala, VMD, DACVIM, director of Life-Cycle Management, companion animal and equine at Merck
Intraoral
•
DIGI
HY
• T
AL
E DENT
•
U IN
AL
EQ
In tra ora
AP
Equ
in e
R
NEW
lD
•
Dental DR
R ST
THE
LD WOR ’S FI
RADIOGR
Picture this… Denti Pod™ is the world’s first intraoral equine dental digital radiography detector. The elusive advantages of dental diagnostics are now readily available to you.
Denti Pod Intraoral Digital Radiography Detector 100mm x 150mm Imaging Area
You cannot practice a veterinary level of equine dentistry without dental radiology. Period. The average equine or mixed animal practice that is doing equine dentistry could, and should, easily incorporate dental radiology. If not, then I guarantee they are missing things. It is really quick, it is really easy, it is good for the bottom line, it is good for patient care, and it sets the general practitioner apart… doing better dentistry on fewer horses, while increasing practice revenue. In my opinion, dental equipment, including radiology, is the single greatest return on equipment investment in the clinical equine practice. Dentistry is a huge profit center. The initial purchase of the equipment is minor compared to what you generate long term. Jon M. GIECHE, D.V.M., FAVD EQ, Diplomate AVDC EQ (One of only eight AVD-EQ Fellows in North America!)
Introducing Denti Pod, the latest advancement in equine dental care.
As part of the revolutionary new Cuattro Hub™ portable multi-modality wireless diagnostic system, Denti Pod brings intraoral Dental DR anywhere you need it. Switch between acquisition of Dental DR, Wireless Ultrasound and Large Animal DR, all on one device, at the press of a button. Call today to schedule a demo.
www.heska.com 800.464.3752
© 2019 Heska Corporation. All rights reserved. HESKA is a registered trademark and Cuattro Hub and Denti Pod are trademarks of Heska Corporation in the United States and in other countries. Specifications are subject to change without notice. Pricing dependent on final configuration. US19AD0501
Imaging the Possibilities
INFECTIOUS DISEASES
Animal Health. “Continued monitoring is important to ensure we’re putting vaccines in the hands of
FIGURE 1. Percent of EIV(+) Cases by Year Relative to Total Case Submissions 20
15
10
5
Vaccinating for ‘flu season’
0
2008
2009 2010 2011 2012 2013 2014 2015 2016 2018 2018 2019
FIGURE 2. Equine Flu Season
Number of Horses
the veterinarian that include strains similar to the EIV circulating in horses today,” Dr. Vaala said. Analyzing samples submitted to the Equine Respiratory Biosurveillance Program, researchers identified and isolated a new influenza strain, Florida ’13, which is representative of a current circulating strain responsible for an outbreak in a large number of well-vaccinated horses. Sequencing work revealed Florida ’13 differs from Ohio ’03 (OIE recommended clade 1 isolate) by 6 amino acid changes, and all 6 of those mutations occur on the surface of the hemagglutinin glycoprotein and are in or near regions associated with antibody binding or receptor binding sites—making them critically significant.
180 160 140 120 100 80 60 40 20 0
Biosurvelillance Results Monthly Cumulative 2008-June 2019
January February
March
April
S. equi
May EHV-1
June EHV-4
July EIV
August September October November December ERAV
ERBV
Source: Merck Animal Health and University of California, Davis School of Veterinary Medicine (Nicola Pusterla). Infectious Upper Respiratory Disease Surveillance Program. Ongoing research 2008-present.
Timing of EIV vaccine administration affects vaccine effectiveness. Study data show increased flu incidence beginning in December and running through April, which is typically prior to when at-risk horses are receiving their bi-annual EIV vaccinations. Following that logic, an EIV booster in late November or early December may be more advantageous than late summer or early fall. “The data clearly point to an equine flu season,” Dr. Vaala said, “so veterinarians may benefit from critically evaluating the optimal time to administer biannual EIV vaccines. With EIV on the rise, reconsidering timing is another aspect of evolving our vaccination practices along with the virus. Even a 1 to 2-month adjustment in EIV vaccination timing could make a significant difference for the horse.” MeV Used with permission from Merck Animal Health.
AT A GLANCE: Equine Respiratory Biosurveillance Program • Comprehensive national surveillance study • Began in 2008 and continues today • Voluntary participation from 239 veterinary practices in 38 states
• Monitors: Equine influenza virus (EIV) Streptococcus equi (S. equi or strangles) Equine herpesvirus types 1 and 4 (EHV-1, EHV-4) Equine rhinitis A/B viruses (ERAV/ERBV), which were added in 2012
• Houses one of the largest collections of equine influenza isolates ever gathered in the U.S. • Managed by Merck Animal Health in partnership with University of California, Davis School of Veterinary Medicine
For more information: Vaala W, Barnett DC, James K, et al. Prevalence factors associated with equine influenza virus infection in equids with upper respiratory tract infection from 2008 to 2019. AAEP Proceedings. 2019 Vol 65. Merck Animal Health Technical Bulletin, December 2019. 10
Issue 2/2020 | ModernEquineVet.com
The only dual ingredient injectable corticosteroid approved by the FDA for use in horses
The link between RAPID ONSET and LONG-ACTING RELIEF of pain & inflammation1 BetaVet ® (betamethasone sodium phosphate & betamethasone acetate injectable suspension) is indicated for the control of pain and inflammation associated with osteoarthritis in horses. Learn more at www.betavetequine.com or call 1-800-458-0163. Please see Brief Summary of Full Prescribing Information on the following page.
INDICATION: BetaVet ® is indicated for the control of pain and inflammation associated with osteoarthritis in horses.
IMPORTANT SAFETY INFORMATION For Intra-Articular (I.A.) Use in Horses.
CONTRAINDICATIONS: BetaVet ® is contraindicated in horses with hypersensitivity to betamethasone. Intra-articular injection of corticosteroids for local effect is contraindicated in the presence of septic arthritis. WARNINGS: Do not use in horses intended for human consumption. Clinical and experimental data have demonstrated that corticosteroids administered orally or parenterally to animals may induce the first stage of parturition when administered during the last trimester of pregnancy and may precipitate premature parturition followed by dystocia, fetal death, retained placenta, and metritis. Additionally, corticosteroids administered to dogs, rabbits and rodents during pregnancy have resulted in cleft palate in offspring and in other congenital anomalies including deformed forelegs, phocomelia and anasarca. Therefore, before use of corticosteroids in pregnant animals, the possible benefits to the pregnant animal should be weighed against potential hazards to its developing embryo or fetus. Human Warnings: Not for use in humans. For use in animals only. Keep this and all medications out of the reach of children. Consult a physician in the case of accidental human exposure. PRECAUTIONS: Corticosteroids, including BetaVet ®, administered intra-articularly are systemically absorbed. Do not use in horses with acute infections. Acute moderate to severe exacerbation of pain, further loss of joint motion, fever, or malaise within several days following intra-articular injection may indicate a septic process. Because of the anti-inflammatory action of corticosteroids, signs of infection in the treated joint may be masked. Due to the potential for exacerbation of clinical signs of laminitis,
glucocorticoids should be used with caution in horses with a history of laminitis, or horses otherwise at a higher risk for laminitis. Use with caution in horses with chronic nephritis, equine pituitary pars intermedia dysfunction (PPID), and congestive heart failure. Concurrent use of other anti-inflammatory drugs, such as NSAIDs or other corticosteroids, should be approached with caution. Due to the potential for systemic exposure, concomitant use of NSAIDs and corticosteroids may increase the risk of gastrointestinal, renal, and other toxicity. Consider appropriate wash out times prior to administering additional NSAIDs or corticosteroids. ADVERSE REACTIONS: Adverse reactions reported during a field study of 239 horses of various breeds which had been administered either BetaVet ® (n=119) or a saline control (n=120) at five percent (5%) and above were: acute joint effusion and/or local injection site swelling (within 2 days of injection), 15% BetaVet ® and 13% saline control; increased lameness (within the first 5 days), 6.7% BetaVet ® and 8.3% saline control; loose stool, 5.9% BetaVet ® and 8.3% saline control; increased heat in joint, 2.5% BetaVet ® and 5% saline control; and depression, 5.9% BetaVet ® and 1.6% saline control. DOSAGE AND ADMINISTRATION: Shake well immediately before use. Use immediately after opening, then discard any remaining contents. RX ONLY References: 1. Trotter GW. Intra-articular corticosteroids. In: McIlwraith CW, Trotter GW, eds. Joint Disease in the Horse. Philadelphia: W.B. Saunders; 1996; 237–256.
BetaVet® and the Horse Head design are registered trademarks of American Regent, Inc. © 2019 American Regent, Inc. PP-BV-US-0027 5/2019
BRIEF SUMMARY OF PRESCRIBING INFORMATION (Betamethasone Sodium Phosphate and Betamethasone Acetate Injectable Suspension) 6 mg betamethasone per mL For Intra-Articular (I.A.) Use in Horses CAUTION: Federal law restricts this drug to use by or on the order of a licensed veterinarian. INDICATION: BetaVet® is indicated for the control of pain and inflammation associated with osteoarthritis in horses. DOSAGE AND ADMINISTRATION: Shake well immediately before use. CONTRAINDICATIONS: BetaVet® is contraindicated in horses with hypersensitivity to betamethasone. Intra-articular injection of corticosteroids for local effect is contraindicated in the presence of septic arthritis. WARNINGS: Do not use in horses intended for human consumption. Clinical and experimental data have demonstrated that corticosteroids administered orally or parenterally to animals may induce the first stage of parturition when administered during the last trimester of pregnancy and may precipitate premature parturition followed by dystocia, fetal death, retained placenta, and metritis. Additionally, corticosteroids administered to dogs, rabbits and rodents during pregnancy have resulted in cleft palate in offspring. Corticosteroids administered to dogs during pregnancy have also resulted in other congenital anomalies including deformed forelegs, phocomelia and anasarca. Therefore, before use of corticosteroids in pregnant animals, the possible benefits to the pregnant animal should be weighed against potential hazards to its developing embryo or fetus. Human Warnings: Not for use in humans. For use in animals only. Keep this and all medications out of the reach of children. Consult a physician in the case of accidental human exposure. PRECAUTIONS: Corticosteroids, including BetaVet®, administered intra-articularly are systemically absorbed. Do not use in horses with acute infections. Acute moderate to severe exacerbation of pain, further loss of joint motion, fever, or malaise within several days following intra-articular injection may indicate a septic process. Because of the anti-inflammatory action of corticosteroids, signs of infection in the treated joint may be masked. Appropriate examination of joint fluid is necessary to exclude a septic process. If a bacterial infection is present, appropriate antibacterial therapy should be instituted immediately. Additional doses of corticosteroids should not be administered until joint sepsis has been definitively ruled out. Due to the potential for exacerbation of clinical signs of laminitis, glucocorticoids should be used with caution in horses with a history of laminitis, or horses otherwise at a higher risk for laminitis. Use with caution in horses with chronic nephritis, equine pituitary pars intermedia dysfunction (PPID), and congestive heart failure. Concurrent use of other anti-inflammatory drugs, such as NSAIDs or other corticosteroids, should be approached with caution. Due to the potential for systemic exposure, concomitant use of NSAIDs and corticosteroids may increase the risk of gastrointestinal, renal, and other toxicity. Consider appropriate wash out times prior to administering additional NSAIDs or corticosteroids. ADVERSE REACTIONS: Adverse reactions reported during a field study of 239 horses of various breeds which had been administered either BetaVet® (n=119) or a saline control (n=120) were: acute joint effusion and/or local injection site swelling (within 2 days of injection), 15% BetaVet® and 13% saline control; increased lameness (within the first 5 days), 6.7% BetaVet® and 8.3% saline control; loose stool, 5.9% BetaVet® and 8.3% saline control; increased heat in joint, 2.5% BetaVet® and 5% saline control; depression, 5.9% BetaVet® and 1.6% saline control; agitation/anxiety, 4.2% BetaVet® and 2.5% saline control; delayed swelling of treated joint (5 or more days after injection), 2.5% BetaVet® and 3.3% saline control; inappetance, 3.4% BetaVet® and 2.5% saline control; dry stool, 1.7% BetaVet® and 0% saline control; excessive sweating, 0.8% BetaVet® and 0% saline control; acute non-weight bearing lameness, 0.8% BetaVet®and 0% saline control; and laminitis, 0.8% BetaVet® and 0% saline control.
PP-BV-US-0027_FullPg_Ad.indd 2
CLINICAL PHARMACOLOGY: Betamethasone is a potent glucocorticoid steroid with anti-inflammatory and immunosuppressive properties. Depending upon their physico-chemical properties, drugs administered intra-articularly may enter the general circulation because the synovial joint cavity is in direct equilibrium with the surrounding blood supply. After the intra-articular administration of 9 mg BetaVet® in horses, there were quantifiable concentrations of betamethasone (above 1.0 ng/mL) in the plasma. EFFECTIVENESS: A negative control, randomized, masked field study provided data to evaluate the effectiveness of BetaVet® administered at 1.5 mL (9 mg betamethasone) once intra-articularly for the control of pain and inflammation associated with osteoarthritis in horses. Clinical success was defined as improvement in one lameness grade according to the AAEP lameness scoring system on Day 5 following treatment. The success rate for horses in the BetaVet® group was statistically significantly different (p=0.0061) than that in the saline group, with success rates of 75.73% and 52.52%, respectively (back-transformed from the logistic regression). ANIMAL SAFETY: A 3-week target animal safety (TAS) study was conducted to evaluate the safety of BetaVet® in mature, healthy horses. Treatment groups included a control (isotonic saline at a volume equivalent to the 4x group); 1X (0.0225 mg betamethasone per pound bodyweight; BetaVet®); 2X (0.045 mg betamethasone per pound bodyweight; BetaVet®) and 4X (0.09 mg betamethasone per pound bodyweight; BetaVet®). Treatments were administered by intra-articular injection into the left middle carpal joint once every 5-days for 3 treatments. Injection site reactions were the most common observations in all treatment groups. Injection site reactions were observed within 1 hour of dosing and included swelling at the injection site, lameness/stiffness of the left front limb, and flexing the left front knee at rest. The injection site reactions ranged from slight swelling (in many horses on multiple days in all treatment groups) to excessive fluid with swelling, pain, and lameness (4x group only). Injection site reactions were observed most commonly on treatment days, and generally decreased in number and severity over subsequent days. The incidence of injection site reactions increased after the second and third injection (number of abnormalities noted on day 10 > day 5 > day 0). In the BetaVet® treated groups the number and severity of the injection site reactions were dose dependent. The 4X BetaVet® group had the highest overall incidence of and severity of injection site reactions, which included heat, swelling, pain, bleeding, and holding the limb up at rest. The control group and 4X group (which received similar injection volumes) had a similar incidence of injection site reactions; however, the severity of reactions was greater in the 4X group. Absolute neutrophils were statistically significantly higher in the BetaVet® treated groups as compared to the control group. Trends toward a decrease in lymphocytes and eosinophils, and an increase in monocytes were identified in the BetaVet® treated groups after the initial dose of BetaVet®. Individual animal values for white blood cells generally remained within the reference range. BetaVet® treated horses also had a trend toward increased blood glucose after the initial dose. Some individual animals showed mild increases in blood glucose above the reference range. SHAKE WELL BEFORE USING NADA 141-418, Approved by FDA For customer care or to obtain product information visit www.betavetequine.com or call 1-800-458-0163. To report an adverse event please contact American Regent Animal Health at (800) 734-9236 or email pv@americanregent.com.
A Division of American Regent, Inc. 5 Ramsey Rd. | Shirley, NY 11967
5/17/2019 9:15:15 AM
DENTISTRY
Getting the Perfect
REGIONAL BLOCK
B y
P a u l
Materials
Dr. Rawlinson prefers Tuohy needles over spinal needles for nerve blocks. “The Tuohy needles cut on the side rather than at the tip,” she said. “This allows the needle to move or push structures out of the way, since the tip is blunt. You can feel the structures that you’re going through. The needles also have 1-cm demarcations, so you can think about how deep you’re placing the needle.” Luer locks—particularly for the mental foramen and intraoral blocks—are good tools to help the clinician avoid anesthetizing his or her own eyeballs, she joked, referring to when pressure builds within a syringe resulting in non-secured needles to disengage spaying injectate into the air.
Shutterstock/Andrew Lever
Regional nerve blocks are an essential tool for dental extractions under standing sedation. They reduce the risk to the horse from general anesthesia and intraoperative hemorrhage, and can improve recovery times, according to Jennifer Rawlinson, DVM, DAVDC, Founding DAVDC-EQ. Without nerve blocks, it’s rarely possible to sedate the horse well enough to perform a safe procedure for the patient or the practitioner. “When they start head tossing—and they’re weaponized with the dental speculum in place—it’s not safe for anybody,” said Dr. Rawlinson, here at the 65th Annual AAEP Convention in Denver. “Regional and local anesthesia have markedly increased the safety and efficacy of performing dental procedures.”
B a s i l i o ModernEquineVet.com | Issue 2/2020
13
DENTISTRY
“They allow you to administer an appropriate amount of pressure without disconnection of the extension set of the syringe,” added Dr. Rawlinson, associate professor, of Dentistry and Oral Surgery, Colorado State University.
Maxillary nerve block
Nerve blocks allow for less standing sedation drugs, such as detomidine and opioids, which means there will be less of an impact on the horse’s GI tract during recovery.
Dr. Rawlinson tends to use the extraperiorbital fat body insertion technique to block the maxillary nerve as it branches from cranial nerve V. “If you inject the material into the periorbital fat pad, it will diffuse throughout the space and anesthetize the maxillary nerve without getting your needle too far into the periorbital fat pad, which is close to some critical structures,” she said. This will desensitize the ipsilateral teeth, the gingiva, and the skin, lip and nostril rostral to the infraorbital opening. There is the potential to block the lacrimal branch of cranial nerve VII, which will decrease tear production. “I tell my technician to lubricate the horse’s eyes every 30 minutes,” Dr. Rawlinson said to reduce ulceration. “You treat 1 melting ulcer in an eye, and you will never forget to do it.” She approaches the block by laying her hand along the facial crest, rather than navigating by the eye, as the position of an eye can vary slightly among breeds. By aiming for the dorsal reflection of the facial crest into the zygomatic arch, she is able to more reliably deliver the block on target. Roughly 1 to 2 cm caudal to the point of dorsal deviation is the “sweet spot” located between the maxillary tuber and the coronoid process. Place the Tuohy needle perpendicular to the skin, then advance the needle into the masseter muscle.
Materials • Sharpie and straight edge • Clippers • Betadine and saline-soaked gauze • Sterile gloves • Tuohy epidural needles (3.5”; 22 gauge and/or 6.0” length; 20 gauge)
14
Issue 2/2020 | ModernEquineVet.com
• Hypodermic needles (1.0” length; 25 gauge and/or 1.5” length; 24 gauge) • Extension set 6” luer lock • Syringe 12-cc luer lock and/ or 6-cc luer lock
“Some of the techniques that involve pointing the needle toward the backside of the eye are adrenaline provoking for me,” Dr. Rawlinson explained. “The beauty of this other technique is that you don’t have to worry that your needle is poking the eyeball.” After the needle is inserted roughly 6 cm, for an average 1,000 lb horse, a “pop” should occur as you pass through the last fascial plane on the medial aspect of the masseter muscle. After inserting the needle another 5 mm following the pop, it will be in the periorbital fat pad space. Dr. Rawlinson also stated she does not place a lidocaine bleb prior to inserting the needle. “I use the needle as a litmus test to see whether the horse is sedated enough to put a 7-cm needle into its head,” she explained. “If it reacts to the little prick of the skin, then I’m going to need to sedate it further before fully placing the needle.”
Mental foramen block
The goal of this block is to introduce the needle 1 cm into the mental foramen to block the rostral extension of the inferior alveolar nerve as it moves into the rostral aspect of the mandible to innervate the canine teeth and incisors. However, that’s not always what happens. “One study I performed found that it had a roughly 60% efficacy rate,” Dr. Rawlinson said. “One of the reasons I did the study was because I knew I was placing my block appropriately, but sometimes it just wasn’t effective.” Due to anatomical variance, there is a fairly large difference in the size of mental foramens from horse to horse. They can be extremely hard to find, much less put a needle through. “If you are having trouble placing these needles, the problem is not likely you—it’s the horse,” she said. A slow approach is often best: • Locate the position of the mental foramen, then clean and prep the site. • Prepare a 3.5-inch, 22-gauge needle attached to the extension set. • Use 2 anesthetics: lidocaine 3 mL and bupivacaine 6 mL. The lidocaine is used on the slow approach to the mental foramen, which allows the
needle to pass into the rostral mandibular canal, where the bupivacaine is deposited. • Palpate the foramen and introduce the needle roughly 1 cm caudal rostral to the foramen; deposit 0.5-1 mL of lidocaine, and wait 60 seconds. • Advance the needle to the foramen mediocaudally 1 cm, and deposit another 1 mL of lidocaine. Wait another 60 seconds. • Once through the foramen, advance the needle dorsolaterally to ventromedially roughly 1 cm into the rostral mandibular canal, and apply digital pressure to the mental foramen to stabilize the needle. • Aspirate the syringe, and slowly deposit 5 mL of bupivacaine. • Remove digital pressure, slowly remove the needle, and reapply pressure to the site for approximately 1 minute.
Inferior alveolar nerve block
The inferior alveolar nerve block anesthetizes the inferior alveolar nerve as it branches away from the mandibular nerve and travels into the mandibular foramen and the mandibular canal. The mandibular foramen is located rostrally on the medial aspect of the coronoid process, at the level of the ipsilateral mandibular occlusal surface. “This one is in a deep, dark scary place,” Dr. Rawlinson said. “You really have to go deep to access the mandibular foramen.”
The lingual nerve is also close. There is some space between the 2, but avoiding the lingual nerve will help avoid potential injuries to the tongue. To locate the mandibular foramen, extraoral landmarks can be used. “The first line I use is along the occlusal aspect of the mandibular teeth,” she said. “Draw a line with a Sharpie, then cross it with a line drawn from the lateral aspect of the mandibular condyle to the vascular notch. Where the ‘x’ occurs, that’s the spot to inject.” She will then go up from the lowest point on the mandible, perpendicular to the skin to where the ‘x’ is located. To premeasure the depth, Dr. Rawlinson will lay the needle on the lateral aspect with the tip near the ‘x’ to the most ventral aspect of the mandible. She then grasps the needle at that point—she knows that when her finger hits the horse’s skin, she’s at the depth that she wants. “On the inside of the mandible, there is a mesenteric fossa, which can be obstructive and deflect the needle,” she said. “To get around this, come 1 cm off of the ventral aspect of the mandible when you’re inserting your needle, and insert it at a 30° angle. You’ll skip over the mesenteric fossa until you contact bone.” After contacting bone, flatten the needle and scrape the tip up the bone of the mandibular foramen. “If the tip of the needle is not scraping along bone, don’t inject,” Dr. Rawlinson added. “There are a lot of things that you’ll end up anesthetizing if you’re not on bone, and bad things can happen.” MeV
Want to Help Australian Animals? For those who want to make a donation to help with the unprecedented fire damage to Australia’s ecosystem, donating to the American Veterinary Medical Foundation (AVMF) will assure that 100% of your contribution goes where it’s needed. Already, the American Veterinary Medical Association (AVMA) and the AVMF have raised $125,000 for the Australian Veterinary Association's (AVA) Benevolent Fund for distribution to veterinarians who are on the front lines providing relief to animals impacted by the wildfires. Now, VCA Charities will match up to $50,000 in additional donations made to the AVMF on behalf of the AVA Benevolent Fund. “During this deep time of need, VCA Charities and all the amazing associates at VCA Animal Hospitals
want to be there to help wildlife, pets, veterinarians and the many vulnerable communities across Australia,” said Brandon Antin, vice president of corporate affairs for VCA and a board member of VCA Charities. In total, VCA Charities has raised $150,000 and will be providing three donations to animal charities: one to support veterinarians, one to help wildlife and one to help pets. VCA Charities will match every dollar contributed to AVMF on behalf of the AVA Benevolent Fund, up to $50,000, 100% of which will be directed toward disaster relief efforts in Australia. MeV
To donate https://www.avmf.org/forms/donate-to-avmf/ use the AVMF code “Disaster Relief – AVA Benevolent Fund.” ModernEquineVet.com | Issue 2/2020
15
TECHNICIAN UPDATE
Snake Bite—More Than Just a Pain in the Nose By Kristina Rothers, CVT, VTS-EVN
Image courtesy of Kristina Rothers, CVT, VTS-EVN
On Aug. 27, 2018 a 5-yearold Quarter horse gelding presented to the Colorado State University Veterinary Teaching Hospital for a rattlesnake bite of approximately 1 hour duration. Despite the horse presenting within 1 hour of being bitten, significant swelling was already appreciable. The owners brought the horse directly to the clinic after finding him, rather than wait for the animal’s veterinarian. On presentation, the gelding’s physical examination findings were: normal rectal temperature of 100.9° F, slightly elevated pulse at 44 beats per minute, normal respiratory rate of 12 breaths per minute and normal borborygmi in all 4 quadrants. The mucous membranes were unable to be fully examined due to the swelling of the muzzle. However, color appeared a normal pink and CRT was approximately 2 seconds. His packed cell volume was 32% and the total protein was 6 g/dL. Auscultation of the heart and lungs were within normal limits. Although rare, fatal cardiac arrhythmia following envenomation is possible, so it is important to warn owners that this is a possible complication. The fang marks were identified on the muzzle, and there was a bilateral serosanguinous nasal discharge present. Airflow was detected from both nos-
trils although it was slightly decreased. Inspiratory and expiratory effort was increased due to nasal swelling. It was decided not to perform a tracheostomy at that time. However, the supplies were kept close in case the horse went in to respiratory distress. After discussing options with the owner, the owner consented to administration of antivenin, which has proved useful in horses even when given 24 hours post-envenomation. This horse had been bitten quite recently so the hope was that if we were able to administer the antivenin quickly enough the swelling would start to decrease, and he would not need a tracheotomy, which turned out to be correct in this case. A sterile, 14-gauge Mila quick catheter was aseptically placed in the left jugular vein. His weight was estimated at 500 kg. Two vials (20 mLs) of Antivenin (Venom Vet) was diluted in 1L of 0.9% sodium chloride and administered over 15-20 minutes. He was monitored for any adverse reactions; none were observed. Antivenin is an equine origin product and an anaphylactic reaction can occur. Also, anti-venom will help neutralize the toxins for approximately 48 hours; after such time, it is important to monitor the horse for signs of respiratory and/or cardiovascular distress. He was also given 500 mg flunixin meglumine IV. The owners reported that the horse’s last tetanus toxoid vaccination was in May, so a booster was not needed. The owners were anxious to take the horse home the same day so he was placed in an out-patient holding stall and monitored for several hours. After that time his respiratory effort was noticeably decreased,
Antivenin is an equine-origin product, which can neutralize toxins, but an anaphylactic reaction can occur.
16
Issue 2/2020 | ModernEquineVet.com
TECHNICIAN UPDATE
Teaching Points In this case, the owner brought the horse to us. But if an owner decides to have a veterinarian come to them and wants to help their horse before a veterinarian arrives the following recommendations can be made. 1. Try to keep the horse as quiet as possible because an increased heart rate causes higher blood flow, which results in dispersal of the poison to larger areas of the body. 2. Wash the bite with soap and water. 3. If the horse was bitten on the nose, and they see significant swelling, they can insert a cut piece of garden hose in each nostril to try and maintain an airway until the veterinarian arrives.
18
and there was a moderate reduction in the swelling in his muzzle. At that time he was discharged to the care of his owners with instructions to carefully monitor him for the next several days. The owner was told to monitor for all of the following: • any difficulty breathing, • not eating or drinking, or • decreased defecation. It was suggested that soaked feed be offered for a few days while the swelling slowly decreased. The horse was not normally fed grain, so we suggested soaking his hay as well as offering small amounts of soaked Equine Senior and offering water with a handful of sweet feed in it to encourage drinking. There are only 3 types of rattle snakes in Colorado 1. the prairie rattlesnake (Crotalus viridis viridis), 2. the western rattlesnake and 3. the massasauga. However, the western rattlesnake is found west of the Continental Divide and the massasauga is limited to the south eastern plains so we primarily see and treat prairie rattlesnake bites. The venom of these snakes is mainly hemotoxic and causes breakdown of tissues and blood vessels and impaired blood clotting. In addition, as briefly mentioned earlier, potentially fatal cardiac abnormalities have been reported in horses bitten by rattlesnakes. While the prevalence and exact cause are unknown, in 1 study it was found that 40% of the horses tested had experienced myocardial damage and 70% experienced a cardiac arIssue 2/2020 | ModernEquineVet.com
Image courtesy of Kristina Rothers, CVT, VTS-EVN
Shutterstock/nelelena
Beyond that it is important that they know what NOT to do. • Do not cut the bite area—this old practice actually may contribute to further tissue damage and increases the risk of infection. • Do not apply hot or cold compresses, either of those treatments further irritate the affected area, causing additional swelling and the risk of necrosis.
Antivenin can be useful, but it must be given within 24 hours of being bitten.
rhythmia. Cardiac failure can occur weeks to months after the bite incident and appears to be more common in horses then other species. Horses that have recovered from snake bites should be evaluated every few months for cardiac health, and owners should be watchful for signs that might suggest cardiac problems, such as shortness of breath, slow recovery after exercise, an increased effort to breathe and general weakness. Additional testing that can be done include mea-
suring troponin levels (Cardiac Troponin I or cTnI) and performing an ECG, looking for the presence of arrhythmias. Lastly, there is a Western Diamondback Rattlesnake toxoid vaccine available for horses (Red Rock Biologics, Woodland, CA). It is a conditionally licensed, inactivated Crotalus atrox Toxoid vaccine labeled for use in healthy horses 6 months of age or older. The label states that it may also provide protection against the venoms of the Western Rattlesnake (including the Prairie as well as others), Sidewinder, Massasauga and the Copperhead. Partial protection may be obtained against Eastern Diamondback as well. Vaccination schedule is a primary series of
three doses at one month intervals. Booster doses are recommended at 6 month intervals. MeV
About the Author
Kristina Rothers, CVT, VTS-EVN is an equine medicine and critical care technician at the Colorado State University Veterinary Teaching Hospital in Fort Collins, where she has worked for the last 18 years. She has an interest in colics and blood transfusions and she helps maintain the blood donor herd. In addition to her CVT, she received her specialty in Equine Veterinary Nursing in 2011. When she is not at work she enjoys showing her 2 quarter horses at breed shows.
For more information: Gaskill C. Toxin Topic: Snakebites and Horses. University of Kentucky’s College of Agriculture, Food and Environment. July 23, 2011. Gilliam LL, et al. Cardiotoxicity, inflammation, and immune response after rattlesnake envenomation in the horse. J Vet Intern Med. 2012;26(6):1457-63. Marcella K. Snakebit! AAEP.org. Accessed Oct. 12, 2019.
Prebiotics May Do More Harm Than Good Prebiotics are often added to horse feed to stabilize the horse's health to stimulate the growth and activity of certain beneficial bacteria in the large intestine. “Horses have a relatively small, non-diverse core microbiome and are therefore very susceptible to digestive disorders," explained Professor Annette Zeyner, head of the animal nutrition group at the Martin-Luther-Universität Halle-Wittenberg (MLU). However, according to the scientist, insufficient research has been conducted on whether the use of prebiotics actually does produce the desired effects. Her research group explored this question in partnership with Professor Gerhard Breves' lab from TiHo. For the study, the team investigated the effect of feeding Jerusalem artichoke meal, a typical equine prebiotic, on horses. In addition to their normal feed, 6 animals received Jerusalem artichoke meal containing high amounts of certain carbohydrates, so-called fructo-oligosaccharides (FOS) and also inulin. Another group of 6
horses received a placebo with their normal feed. The researchers then analyzed the balance of bacteria in the digestive tract of the animals of both groups. It was discovered that the prebiotics were already being fermented in the stomach by the microorganisms naturally living there—they were taking effect much too early. “The fermentation process leads to the formation of organic acids that—unlike in the large intestine—can damage the mucous membrane of the horse's stomach,” said Maren Glatter, a member of Zeyner's group and lead author of the study. However, the bacterial diversity of the entire digestive tract did increase, which probably also produces the desired protective effect. “Still, the prebiotics are probably more harmful than beneficial when used in their present form,” Dr. Zeyner said. The substances must be treated so that they arrive in the large intestine in 1 dose to have a positive effect on the intestinal bacteria living there without stimulating overactivity. MeV
For more information: Glatter M, Borewicz K, van den Bogert B, et al. Modification of the equine gastrointestinal microbiota by Jerusalem artichoke meal supplementation. PLOS ONE, 2019; 14 (8):e0220553 DOI: 10.1371/journal.pone.0220553 https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0220553
ModernEquineVet.com | Issue 2/2020
19
The Modern
Equine Vet
Reach your veterinarians wherever they are, whenever they want. FOR ADVERTISING RATES AND INFORMATION, EMAIL Matthew Todd or Lillie Collett