17 minute read
A Journey in Pink - Part II: Bonna L. Nelson
A Journey in Pink Part II, Eradication by Bonna L. Nelson
Our breast cancer (BC) journey was our new full-time job. It required everything that our former careers demanded of us: planning, organizing, researching, reading, consulting with specialists, traveling to meetings and consultations, preparing notes for meetings and post-meeting reports for support teams and advocating to keep the project on time and successful. This new journey was a bit more personal and invasive, of course, including such processes as physical exams, mammograms, sonograms, MRIs, CT scans, frequent blood tests and the next step, the much-feared chemotherapy, or what I call the “eradication.”
With the new journey undertaken during the coronavirus pandemic, there was the addition of COVID-19 protection measures to be followed. Those measures still include waiting in the car until cleared to enter buildings for tests or to see doctors. Also, being asked the usual barrage of virus exposure-related questions, then wearing a mask, sanitizing hands and having temperature checked on entry and always the risk of exposure outside the safety of my home.
This phase of the Journey in Pink begins with a second consulting meeting with my wonderful University of Maryland (UM) medical oncologist, Dr. Mary DeShields, to discuss my eradication/chemotherapy plan. In our first discussion prior to surgery, Dr. DeShields had said that the number of chemotherapy treatments would range between four and sixteen, depending on the outcome of the lumpectomy and lymph node surgery.
My husband and caregiving angel, John, and I were ecstatic when we learned that the surgery outcome was very positive ~ no cancer cells in the margins of the removed tumor tissue and no cancer cells in the removed lymph nodes. For this result, Dr. DeShields awarded us with the four-star instead of sixteen-star chemo plan!
We were winners in the adjuvant therapy program to eradicate any cancer cells remaining in the body after surgery and to ensure, along with the radiation therapy to come, that chances of recurrence would be diminished. This adjuvant therapy program was determined by years of research to be the standard of care for my early-stage, triplenegative, invasive ductal carcinoma breast cancer.
Dr. DeShields also reviewed the chemotherapy drugs that she determined were best for my situation. I admit that after the news of four instead of sixteen treatments I tuned out for a while, but I did research the drugs later. I reconnected when Dr. DeShields reconfirmed that I would definitely start losing my hair within one to three weeks after the first treatment and that I should start wig shopping and looking for hats and scarves.
Dr. DeShields suggested that I undergo a port implant. Not everyone needs one, but I had a negative experience with intravenous therapy (IV). Chemotherapy must be given via an IV or a port. I agreed that the port was a better option than struggling with an IV insertion for each chemotherapy treatment, thus adding to the already stressful event. An additional reason for a port is that some strong chemo drugs can cause tissue damage around the more sensitive IV site.
The port was implanted under the skin above my heart, same-day surgery, at the UM Shore Medical Center at Easton with a local anesthetic and antibiotic. The doctor showed me the port before surgery, and I took a photo of it. It is white plastic, about the size of a quarter, and includes a
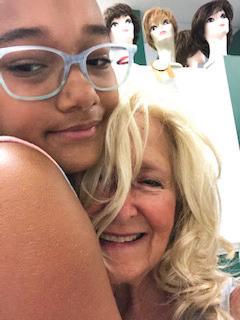
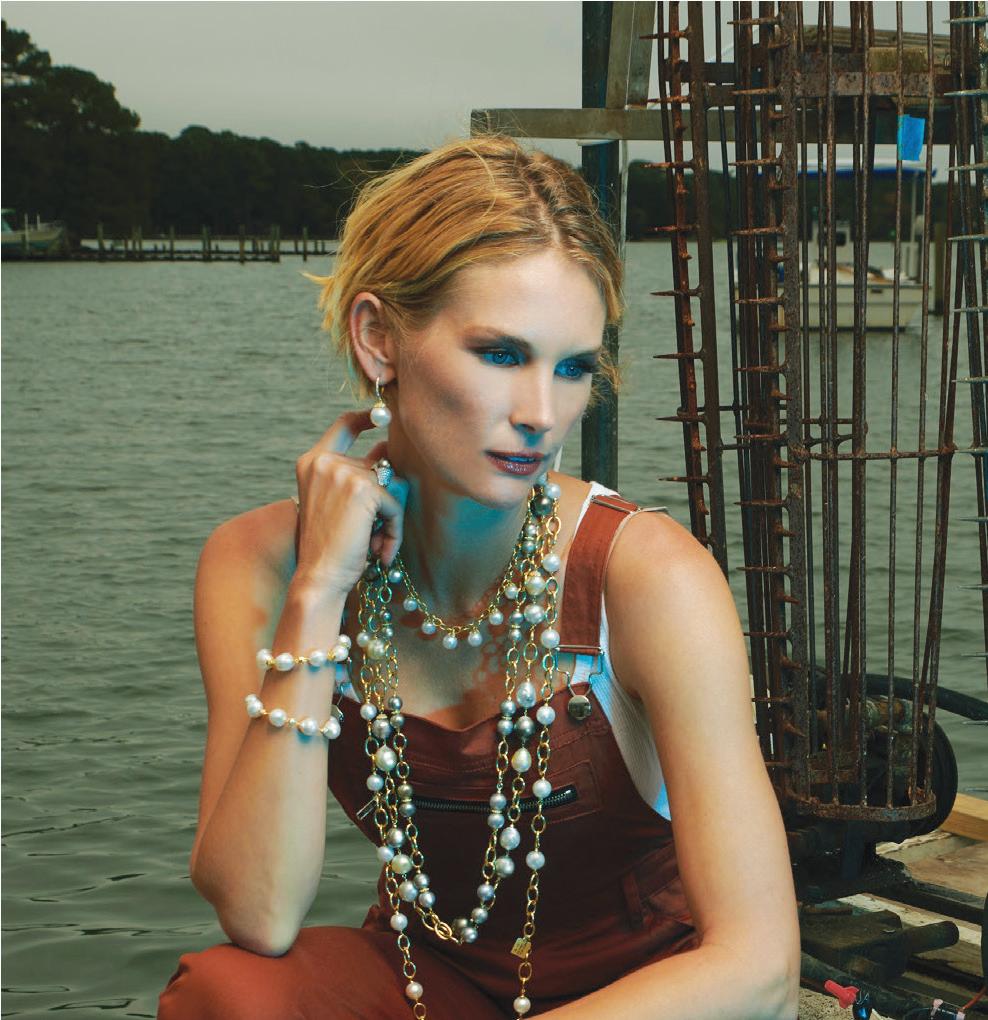
Time to start shopping for wigs and hats.
Port implanted before chemotherapy began.

white plastic tube that is threaded into a vein that loops up from the port to near the neck and back down again close to the heart.
The 1-inch incision was closed with glue. Bruising and discomfort lasted for a few days but were worth it for the comfort and convenience of chemotherapy administration that requires repeated injections of medicine at a high rate into the blood. The medicines mix better in the blood than with an IV because the port delivers medicine into a large central vein. Before each chemo procedure, I coated the port with a lidocaine cream prescribed by Dr. DeShields. This numbed the port to ready it for chemotherapy with a quick, no-pain stick. The port and catheter looks and feels strange but it gets the job done.
I enjoyed wig shopping with daughter Holly and granddaughter Bella. Holly found A Special Touch wig shop in Annapolis, which matched a wig to my own hair. Surprisingly, it was paid for by my insurance plan (one in a lifetime). I also ordered other wigs, hats and scarves online from my mother’s favorite shop, Paula Young, as well as the American Cancer Society’s not-forprofit organization, Tender Loving Care (tlc). I decided to try to have some fun with a difficult situation and bought blonde, brunette, blonde streaked, curly and straight wigs. I also ordered an inexpensive pink wig to celebrate the Pink Journey and a red wig for Christmas.
My wigs, hats, chemo beanies and scarves have brought my family, friends, medical team and me such



fun and joy! I keep them guessing about what I will wear next, and their smiles are such a reward for me. The various headcovers break the ice in every encounter.
I enjoyed a few books that covered for cancer patients to gift them the humor that brings us all healing. Also amusing is Joni Rodgers’ Bald in the Land of Big Hair.
Knowing that I had some fun headgear helped me to plan for and accept losing my hair. I found an organization on the West Coast that makes wigs out of your own hair. My hair had to be over 10” ~ it was 17”. It had to be divided into 1” rubber-banded ponytails. Holly


My hair wrapped in ponytails. Get-
the hair loss and wig experience divided it into the ponies, which with humor. One of the best was Not took two hours. Then, the family and Now... I’m Having a No Hair Day I took turns cutting off the ponies by Christine Clifford. Clifford uses and storing them in a plastic bag narrative and graphics to chart her for eventual wig making if my hair treatment, including hair loss. She didn’t grow back or for donation if achieved her goal of writing a book not needed by me.
ting ready for cutting. 26


That first cut left my hair at about 1” long. I chose to leave some bangs, side and back fringe to give me the comfort of having some hair and to have hair to show with a hat. I also streaked it with pink dye, which gave family, friends and me some cheer. I was glad we cut it a week after the first chemo because it did start to fall out after that.
I asked John to do the second cut. He electric-razored from one inch to one-half inch and scissor cut the back fringe. I have mostly retained that buzz cut and a few front fringes, though a small amount continued to fall out during and after chemo. I also lost body hair, but not my eyelashes ~ or fingernails which can be lost. I was lucky with that.
The days leading up to the first chemotherapy flew by. The tumor board, composed of the members of my oncology team as well as pathologists and other specialists, met, as they frequently do to review patient treatment plans. My post-surgery tumor tissue biopsy showed a second non-invasive tumor around the invasive tumor that was not seen on any imaging. Though the tumor tissue margins and lymph nodes were cancer free, a few members of the board thought that another excision surgery should be performed to remove more margin tissue for recurrence prevention after chemotherapy and before radiation.

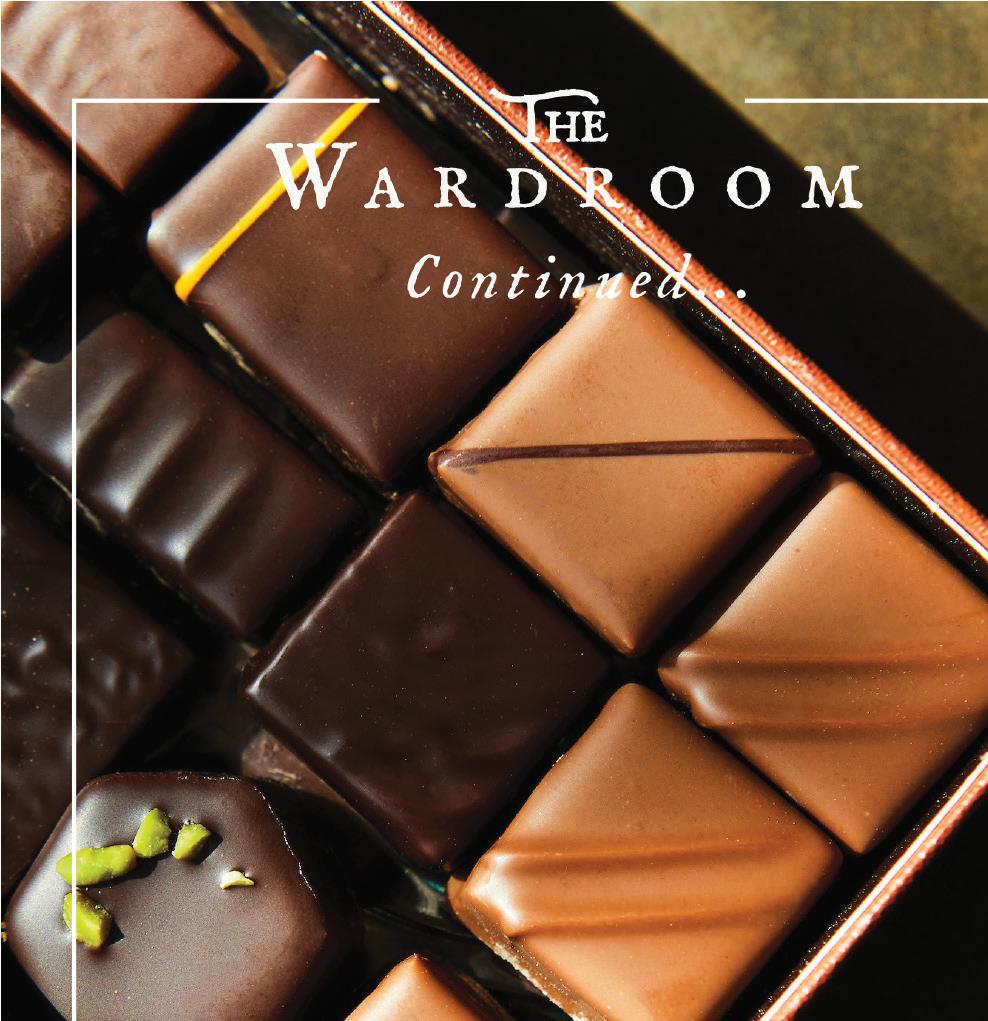
Is your bike ready to ride?
There's nothing better than that first spring ride after a long, cold winter. And there's nothing worse than heading out for your first warm-weather ride and realizing your bike needs some work. Visit us now thru Feb.28 and you’ll get: $50 off service pkgs. $130 – $199.99 $75 off service pkgs. $200 – $299.99 $100 off service pkgs. $300+
Your future self will thank you. *Sale prices available through February 28, 2021.
Not valid on prior purchases. No cash or gift card value. Service packages vary by location.
That recommendation, which was characterized by some of the doctors as “a coin toss” and “a very gray area” type of decision, and one of frequent disagreement among oncology specialists, caused me great distress. I really lost it! I had been accepting of my diagnosis, surgery, port procedure, chemo and radiation, but the thought of having another surgery in between threw me for a loop and brought on a flood of tears. While consoling me, John suggested we get a second opinion about the need for more surgery. Most of my local oncology team encouraged and supported our decision and welcomed


723 Goldsborough St. 410-822-RIDE(7433)
My brother Mike and sister Kim were very supportive.
discussing my case with another team of specialists.
My sister, Kim Smith, used connections in the medical fi eld to arrange for me to see cancer specialists at the UM Medical System, Greenbaum Cancer Center in Baltimore in early September. John and I met with Drs. Tkaczuk, Terhune and Nichols to discuss my cancer and proposed treatment plan and my concerns about the need for more surgery.
I strongly encourage readers to get a second opinion if in doubt about a decision or a doctor. You have to advocate for yourself, which I have done from the beginning. As one of my Easton doctors said you have to listen to your gut and do what you think is best for you and what feels right. If something or someone doesn’t feel right, change direction.
We were happy that we did. The Baltimore team advised against additional surgery, suggesting instead a special and fairly new radiation treatment boost that is the current national standard of care. Shorter, stronger radiation sessions were recommended in lieu of surgery for my type of breast cancer and initial surgical outcome. They agreed with my four chemotherapy treatments and the recommended chemo drugs. The key members of my local team were on board, too. Next up: chemotherapy.
During the entire Pink Journey, our spirits were lifted by the continuous support of family, friends, neigh-
Call For Availability
bors and medical teams. We appreciated receiving continuing thoughts, prayers, texts, emails, cards, calls, meals, baked goods, dinners, flowers and support during the entire process. We especially needed that wonderful support to keep our spirits up during the months of chemotherapy adventures.
To cite a few welcome supporters, my brother, Mike Herrmann, with his own medical challenges, visited and called frequently to cheer me on. Sister Kathleen Feeley, former president of the Notre Dame of Maryland University, my graduate school mentor and now good friend, also stayed in touch via email and calls. Still teaching, writing and driving at age 91, she inspires me and surprised me with a lovely in-person visit.
Sister Kathleen Feeley
With my first chemotherapy treatment fast approaching, John and I attended a very detailed three-hour chemotherapy education program 32
Leigh Mingus and Chanelle Lake, oncology nurses. prepared by Chanelle Lake, BSN, RN, Clinical Coordinator at the UM Shore Regional Health Cancer Center, where my chemotherapy was administered. Lake is also an oncology nurse (OCN) and trains and works with the other oncology nurses in the chemotherapy center next to Dr. DeShields’ office. The OCNs administer the chemo drugs via IV or port.
Lake gave us a binder filled with information, including contacts, chemo drug briefs, side effect descriptions and a glossary of terms. This resource guide also contained a list of dos and don’ts ~ no teeth flossing or whitening, cut hair after first treatment before it falls out, use an electric razor or none at all ~ all tips

Sue Sterling’s Hair Studio, Inc Happy Valentine’s Day!
Tricol Italian Hair Colour
Lowest Chemical Content & Reduced Fading Helium Hair Products
Great for Fine Hair Club Roots & DS Labs (now available)
Hair Growth Treatments - Easy to Use Call...Let us introduce you!
Sue Sterling - Owner 105 Federal St., Ste. A, Easton ◆ 410-822-6777
to protect the body while the immune system is compromised.
She walked us through the topics, answered questions and then took us to see the chemo center. It was an extremely beneficial session. She also reviewed the drugs prescribed by Dr. DeShields to take before and after chemo treatments, such as steroids and anti-nausea pills to lessen the impact of chemo side effects. Lake said that I would need a COVID-19 test and a blood test and to see Dr. DeShields before each treatment. The blood test reveals the levels of various blood components. Red and white blood cell counts and platelets are of particular interest since they are reduced by chemotherapy.
The nurse explained, as did Dr. DeShields, that chemotherapy attacks and kills any remaining cancer cells. Cancer cells grow rapidly. But chemo drugs also kill rapidly growing normal cells in the body, such as hair follicle cells, which causes the hair loss. The chemo drugs kill cells in the GI tract, the mouth, the respiratory system and other body systems, which causes the side effect distresses.
So, on treatment Day 1, I was ready. The port was lidocained, and my steroids, anti-nausea, antianxiety and allergy meds had all been taken. I had packed my BC tote bag, a gift from Holly, with a blanket, a water bottle, a neck pillow, iPad, iPhone, snacks and magazines. We had an injection waiting at home in the refrigerator for John to administrator the next day to help me with bone pain and to stimulate the bone marrow to increase production of white blood cells to prevent infection.
My ON, Leigh Mingos, RN, always called me before each treatment to review the drugs I needed to take before and after each session. She was an absolute angel during treatment, too. She let us pick our very comfortable chemo lounge cubicle, and I was lucky to always find a window seat. Looking outside at trees and people was comforting. Leigh always offered me a heated blanket, a pillow for under my knees and juice.
Nurse Leigh then put on her hazmat gear to handle the potent

chemo drugs and to take my vitals. Dr. DeShields selected two drugs for me, each administered separately: Taxotere, also known as Docetaxel (switched to Doxorubicin after two treatments due to causing tinnitus, which I still have), and Cyclophosphamide. Interestingly, many chemo drugs are made from medicinal plants. Both of these drugs cause a variety of unpleasant side effects while killing any remaining cancer cells floating around.
I think that chemotherapy is rather barbaric; it kills you while it is killing the cancer. Killing the white and red blood cells and blood platelets causes the extreme fatigue. Hair loss, as previously mentioned, occurs within one to three weeks of the first treatment, and I noticed the hair on my pillow in the morning or in the sink after brushing, as predicted. GI issues, mouth sores, joint pain, breathlessness and chemo brain are all possible. But until they come up with something better, the chemo does its job to eliminate cancer cells for many types of cancer. Even after the worst side effects, I never doubted that I needed to be “chemoed.” I trusted the scientists.
Next, Leigh painlessly inserted the chemo needle into my port and then it was time to take a breath and relax while the drug did its best work. I read, chatted with Leigh or Chanelle or John, or fell asleep, drowsy from all of the pretreatment drugs. There was no pain, much to my amazement! When the time came, Leigh removed the Docetaxel needle and inserted the one for Cyclophosphamide. Finally, she inserted a saline flush to clean the port and encourage the chemo drugs to disperse through the body. We were there for about three hours.
I believe it is important to celebrate your accomplishments. So, after each treatment, we ordered carryout for lunch. I was always famished. Once back home, I put on my “comfies” and slept for the afternoon.
Every night, I logged my side effects on the “Chemotherapy Side Effects Worksheets” found on the American Cancer Society website. I highly recommend these worksheets for observing day-to-day effects to share with the medical oncologist and ONs. They always ask about side effects, and the worksheets provide the answers so that they can make adjustments in chemo and side effect drugs and prescribe other meds to help.
My major side effects included extreme fatigue, hair loss, tinnitus, blurred vision, breathlessness on exertion, chemo brain (dizziness, spaciness, forgetfulness), mouth and throat sores, swollen ankles and feet, achy joints, red and puffy face rash, GI issues, mild nausea, mild headache, loss of taste and rubbery legs. I followed doctor’s

orders and took meds prescribed to circumvent these effects, drank more than 64 ounces of water per day to rinse the chemicals from my system, ate nutritional foods and napped frequently.
This routine was repeated three more times, three weeks apart. Each session was a little easier, as we knew what to expect. Trying to bring humor to the process, for the first session I wore a burgundy cloche hat à la Mrs. Fisher’s Murder Mysteries. We dressed for the Halloween session as Ruth Bader Ginsburg and her security detail. For the fourth and last session, wore pink and brought pink balloons and candy for the staff.
After the last session, Leigh and the other ONs danced us out from the chemo room to the lobby to the tune of Kool and the Gang’s “Celebrate,” singing and playing musical instruments, tambourines and maracas to commemorate the grand finale.
I will continue to see Dr. DeShields or her nurse practitioner, Kimberly Yvonne Brice, for followup visits, to review blood work and to manage osteopenia, found during a Dexa Bone Densitometry test, with twice-yearly injections through the port. Additionally, the ONs will need to flush the port with saline every two to three months to avoid blood clots. Kimberly Brice

To recap, on my Pink Journey we traveled from discovery in June; to surgery and healing in July; to chemo prep, port and tumor board in August; to second opinion consult, wigs and haircuts and first chemo treatment in September; to finishing chemo eradication in November. December was a time of healing before the next story, radiation treatment ~ GammaPods and Hypofractionated Beams in January. What an unexpected adventure! I am hoping that my experiences will help others to know what to expect during a similar journey.
Bonna L. Nelson is a Bay-area writer, columnist, photographer and world traveler. She resides in Easton with her husband, John.