10 minute read
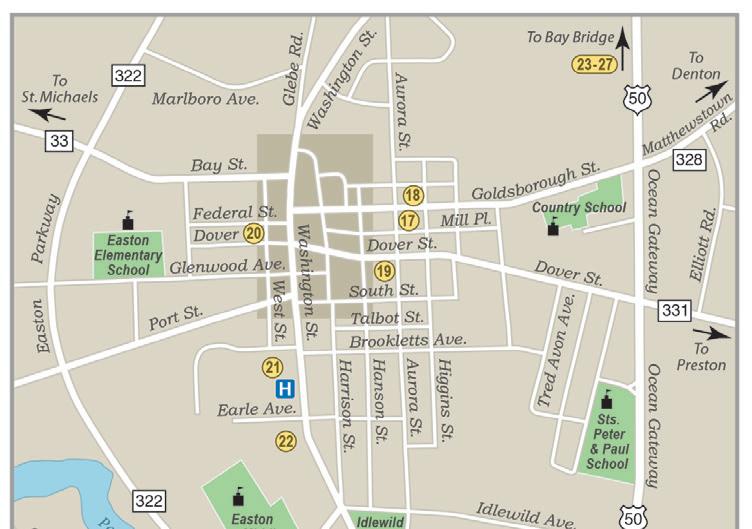
Easton Map and History
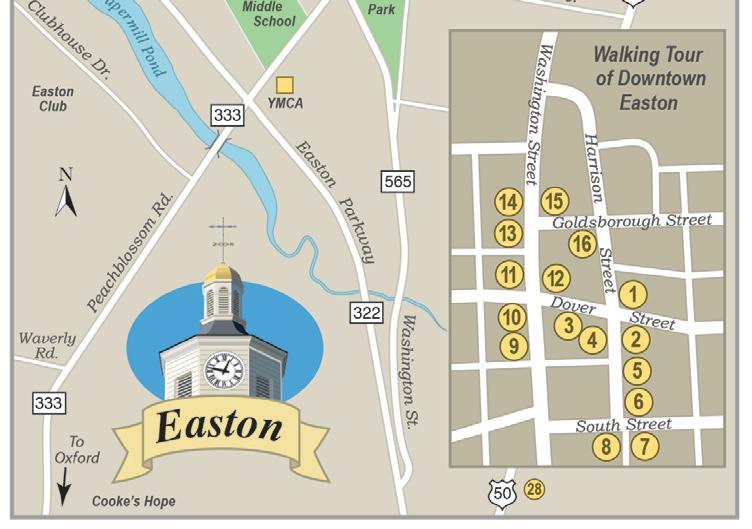
The County Seat of Talbot County. Established around early religious settlements and a court of law, Historic Downtown Easton is today a centerpiece of fine specialty shops, business and cultural activities, unique restaurants, and architectural fascination. Treelined streets are graced with various period structures and remarkable homes, carefully preserved or restored. Because of its historical significance, historic Easton has earned © John Norton distinction as the “Colonial Capitol of the Eastern Shore” and was honored as number eight in the book “The 100 Best Small Towns in America.” With a population of over 16,500, Easton offers the best of many worlds including access to large metropolitan areas like Baltimore, Annapolis, Washington, and Wilmington. For a walking tour and more history visit https:// tidewatertimes.com/travel-tourism/easton-maryland/.
develop, optimize and monitor oncology patient treatment plans and provide calculations, measurements and oversight for plan implementation of dosage of radiation beams, avoiding critical structures such as heart and lung. They are critical to the accuracy of the radiation plan.
The medical physicists apply principles and theories of physics to all aspects of medicine. Using computer software, they help to plan radiation treatments for cancer patients, applying external radiation beams from high-energy machines such as the LINAC and GammaPod. They also design equipment installations and ensure through inspections and
Spring into Spectacular

21 Goldsborough St., Easton 410.763.9262 dragonfl yboutiquemd

Madhi, GammaPod clinical trial researcher.

Monica Penwell Associate Broker
101 N. West Street, Easton, MD 21601 Cell: 410-310-0225 Office: 410-822-2001 monicapenwellrealtor@gmail.com

testing that the equipment functions properly.
RTs administer radiation treatments using computer systems to operate equipment like the GammaPod and LINAC. In accordance with the treatment plan developed by the RO, dosimetrists and medical physicists, the RTs position the patient and the equipment and monitor for accuracy of dosage and for quality assurance using computers and closed-circuit television monitors.
The lead-and-concrete walls of the LINAC room shield the high-energy X-rays so that no one outside the room is exposed. Since I was with them for 15 days of treatment, I interacted with the RTs the most. They were always supportive and informative, not really anonymous shapes floating around the room! The actual radiation treatment was only fi ve minutes ~ the proper positioning of me and the machines took much longer. Additional X-rays and scans had to be taken each week for continued accuracy.
The oncology NPs and nurses that I saw weekly with Dr. Nichols answered questions about treatments and side eff ects, and monitored my overall health and vital signs during treatment. My nurses also gave me advice and soothing creams to help with skin burns from treatment.
I am thankful for my team of medical and technical specialists
with whom I spent 16 days. I am thankful for their knowledge, expertise, compassion and support during the radiation sessions and in examinations after treatment. I am thankful for their careful attention to the planning and accuracy of the positioning of the machines and me to produce a successful outcome of killing any remaining cancer or precancerous cells in the breast without doing harm to surrounding tissue and organs.
Radiation Therapy 101: According to the Mayo Clinic and the Centers for Disease Control, radiation is energy that comes from a source and travels through space at the speed of light. This energy has an electric field and a magnetic field associated with it and has wave-like properties, electromagnetic waves.
Radiation kills cancer and precancer cells to help prevent recurrence in the affected breast. Recurrence can take place months or years later due to cancer cells left behind after a lumpectomy that removes only the tumor and a small amount of surrounding normal breast tissue. Lumpectomy combined with chemotherapy and radiation therapy is referred to as breast conservation therapy. I like the sound of that: breast conservation. Even better, I like the hope of no recurrence!
Radiation for any stage of breast cancer uses high-energy X-rays, protons, gamma rays or other particles to kill cancer cells. Rapidly growing cells such as cancer cells are more susceptible to the effects of radiation therapy than are normal cells. Radiation is painless and invisible.
External radiation is accomplished by a machine delivering the radiation from outside the body to the breast. It is the most common type of radiation therapy used for the breast. External beam radiation therapy of my entire affected breast was accomplished with the LINAC, which customizes high-energy Xrays or electrons to conform to the area being treated while sparing surrounding tissue. It features several built-in safety measures to ensure it will deliver the volume and dosage as prescribed by the RO.
Additionally, Dr. Nichols chose to administer my radiation rapidly, using hypofractionated radiotherapy. According to Yale Medicine, faster isn’t always better, but in the case of radiation therapy for some cancers, accelerating radiation courses can help patients recover sooner. It

Silicone cups used to immobilize the breast for GammaPod radiation.
reduces the course of radiation sessions in half. I had three weeks of treatment, instead of the usual six or seven, with higher doses or fractions of radiation precisely delivered to the aff ected breast in order to leave surrounding tissue, organs and muscle untouched.
Having fewer treatment sessions usually means fewer unpleasant side eff ects such as skin irritation, fatigue and nausea and fewer trips to the cancer center, thus improving quality of life. For me, that meant fewer trips to Baltimore, mild fatigue and skin irritations, which the team treated with cream and told me would heal over time.
Aside from the travel to Baltimore, which was our choice, radiation was much easier on my body than chemotherapy, which kills fast-growing cells in the whole body, thus the hair loss, mental fog, GI issues, hearing and vision issues, major fatigue, etc., but was so necessary to destroy remaining cancer cells in the body.
I started my radiation treatments with what Dr. Nichols called a “boost” on the fairly new GammaPod radiation device developed and invented by two professors/doctors at the UM School of Medicine and now used in the UMGCCC. The GammaPod uses stereotactic radiation therapy specifi cally designed to highly target the aff ected breast area without damaging skin, healthy
breast tissue or major organs. This new, ultra-precise form of radiation therapy uniquely delivers a high dose of radiation while the patient lies face down with the breast immobilized, as opposed to on the back with traditional radiation therapy.
Approved by the FDA in 2017, the GammaPod treatment begins with a fitting session to immobilize the breast by placing it in a series of silicone and plastic breast cups, followed by a CT planning scan, followed by the treatment. Air is pumped out of the breast cups prior to treatment.
After talking to Dr. Nichols about the GammaPod, signing up for the clinical trial of the breast cups and conducting my own research on the technology, I was excited to finally see it and begin. Dr. Nichols treated the first patient to use the GammaPod machine, and UMGCCC was the first center in the U.S. to offer the new technology. It was exhilarating to step onto the ledge attached to the upright table and place my cup-enclosed breast into the hole, where it was locked into place. The table lowered slowly and gently to a horizontal position, and the breast dropped away from the chest wall and away from heart and lungs for treatment.
It felt like a ride in an amusement park. Nurses and RTs stood nearby, adjusted my face-down position
25% Off with this LUCKY ad!
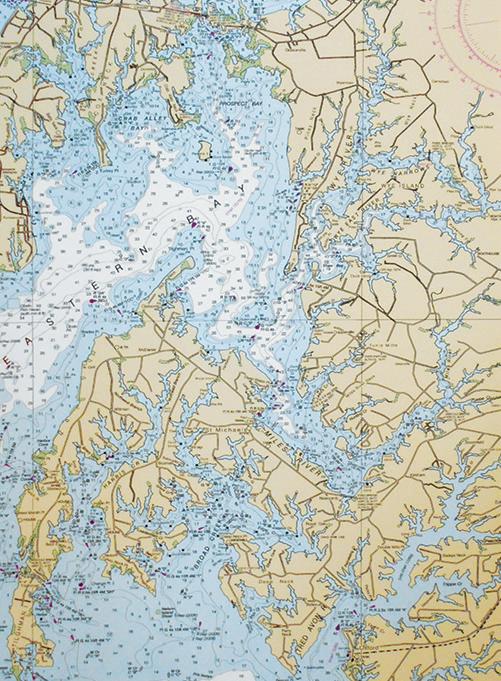

Chart Your Way to the BEST CUSTOM FRAMING!
Beautifully Framed Charts and other Décor
410-310-5070 125 Kemp Lane, Easton
Plenty of Off-Street Parking

Journey in Pink time I will answer questions and be examined and photographed. and then left the GammaPod room For 16 days, we packed lunches, to the observation room while the both to eat healthily and to avoid radiation treatment occurred. I adding to my COVID-cancer weight could not feel or hear anything. After gain. We kept a special calendar treatment, the reverse occurred. The to gleefully mark off the days. My table returned to a vertical position. Johnny “Angel” drove us to BaltiI stepped off and was escorted to a more and back. We spent about six private room where Terri, my NP, hours a day, including the drive, removed the cups, which was a big parking, security checks, waiting, “ouch” for me. I developed blisters, a COVID checks, changing, positionrash and skin irritation in concentric ing (including aligning with the circles from the silicone breast cups, original Maori markings), treating, a common occurrence. I was given changing and returning. cream to apply and was assured it My primary side effects are skin would all heal without scars. irritation and darkening and mild
It is hoped that the GammaPod fatigue. Naps are my friends. John treatment will eliminate the need for walked the hospital halls and steps surgery and chemotherapy in early- while I was in treatment. I am hoping stage breast cancer patients. This is that one day I will regain my strength fantastic news, as it would decrease and endurance and on a follow-up overtreatment of women with small, appointment will walk those halls early-stage breast cancer. I am hop- and steps with him. ing for that outcome and am happy to As Joan Lunden said in her breast be participating in a trial of a breast cancer memoir, Had I Known, “… conserving therapy that may help there are no short cuts in the battle women avoid surgery and chemo in against cancer. I was willing to do the future. whatever it took to get to the fin-
During my preparation and ish line.” Me, too! John and I did treatment, Karen Warmkessel, UM whatever it took to get to the end of Media Relations Specialist Karen Warmkessel took photos for me during my preparation and treatment. Before and after the treatment the clinical trial researcher, Madhi Qutab, took photographs for the study and asked me questions pertinent to the trial. The trial will run for three years, during which The RTs and nurses bid farewell. 54


our eight-month battle with breast cancer.
On the last day of radiation, the RT crew congratulated me. Dr. Nichols, Sarah and Lori examined my skin, thought it looked better and set my next month’s appointment, and Madhi took more photos for the study. We said our good-byes and thanks. I gave everyone a pink breast cancer ribbon pin and copies of the January Tidewater Times with my fi rst pink journey article.
Lori gave me a radiation graduation certificate and made a PA announcement. “Code Sunshine,” she said. She told me to ring the bell in the lobby to indicate completion of treatments. John was there as I came out, cell phone ready to take photos. To my surprise, many of my team of nurses and RTs came out and formed a line to applaud, say farewell and take a photo with me. Holding back tears, trying to smile, wishing we could hug, we said our good-byes.

Finito, ringing the bell ceremony. John and I celebrate.
What comes next? Healing, follow-up doctors’ appointments, reflecting, processing, revising my bucket list, determining how to pay it forward, giving back, living the rest of my life, writing the fourth part of my pink journey…
Cancer changes your life, often for the better. You learn what’s important, you learn to prioritize, and you learn not to waste your time. You tell people you love them. ~Gilda Radner
Comedian, actress, writer, died of ovarian cancer at age 42, author of the cancer memoir It’s Always Something
Bonna L. Nelson is a Bay-area writer, columnist, photographer and world traveler. She resides in Easton with her husband, John.