
11 minute read
HEALTH & WELFARE Articles on Tetanus in a Dachshund, 39 & Me - Genetics, Heartworm Resistance
from DCA Newsletter Winter 2020
by twc910
Welcome to the “Health and Welfare”segment of the Newsletter.It is hoped that DCA members will submit ideas for this section of the magazine as well as articles about experiences pertaining to the healthcare of their dogs that will be of interest to other readers.
Please send ideas, suggestions and articles to the Dachshund Club of America Newsletter Editor.
This is a story about Thorn, a patient of Drs. Portner and Berkowitz of the Emergency and Critical Care team along with Dr. Tracy, our Neurologist and Dr. Lewis, our veterinary Dentist. Submitted by Trudy Kawami
About Thorn:
Thorn presented to Dr. Portner of the Emergency and Critical Care team on referral from another emergency and specialty hospital for treatment of suspected Tetanus infection. At the time of presentation, he was a 20 week old, intact male, dachshund puppy who had sustained a fall from the couch 5 days prior. The day after the fall he was a little lethargic and then progressively started to become more and more stiff throughout the weekend. Thorn was seen at another emergency and referral hospital, but was referred to us at NorthStar VETS for continued treatment and care under the expertise of our Emergency and Critical Care doctors.
Tetanus:
Tetanus occurs when spores from the bacterium Clostridium tetani. Spores are very hardy and can be found commonly in the environment, especially in soil and can survive for years under certain conditions. When spores are introduced into a wound that provides an anaerobic environment, allowing the spores to become vegetative, and produce tetanospasmin, the toxin responsible for the severe neurologic clinical signs that we see. Clinical signs usually develop within 5 to 10 days from the inoculating wound, but up to 18 days has been reported.
Tetanus in dogs is very uncommon (even more uncommon in cats) because dogs and cats have a natural resistance to the effects of tetanospasmin; localized clinical signs are more common than generalized tetanus, likely owing to this inherent resistance. It takes nearly 200 times the amount of toxin for a dog to be affected than a human and 3,600 times the amount of toxin for a cat. Thorn presented with very classic signs of generalized tetanus including severe trismus, and we could only open his mouth a couple of millimeters, his ears

were erect and pinned to the top of the head (some patients will also show a ridgeline in the skin longitudinally between the ears), stiffness leading to a sawhorse type stance and his tail held straight out, he had a lateral strabismus (eyes looking outward instead of looking straight ahead) and constricted pupils, and his third eyelids were elevated because the muscle behind the eye was retracting the globe.
Thorn’s progress:
Thorn was admitted to the Intensive Care Unit and watched very closely while he was supported through his illness. Treatment with antibiotics, most specifically metronidazole, was started to begin treatment for C. tetani infection. We monitored his blood gases and electrolytes and blood sugar along with his vital signs very closely, ready to provide ventilator support if he was unable to maintain his breathing well enough on his own. After a few days of treatment, including the administration of Tetanus Antitoxin, we were able to open his mouth a few more millimeters and identified the source of his infection: a fractured deciduous tooth. The tooth was extracted by Dr. Lewis of our Dentistry and Oral Surgery team and a gram stain of the bacteria from the tooth showed
Emergency and Critical Care service at NorthStar VETS “tennis racket” shaped bacteria most consistent with Clostridium bacteria, confirming our diagnosis.
We were prepared to begin nutritional support for Thorn with either a nasogastric feeding tube or intravenous nutrition, but thankfully, Thorn began opening his mouth enough to begin eating on his own if fed in very small amounts. It was a painstaking process to feed him such small amounts at a time, but even though he could barely move from stiffness, he would begin tremoring and wagging his tail, very excited about being able to eat. Thorn spent 9 days in the hospital with his family coming to visit him every day. Once he was able to eat enough on his own and maintain his own body without intravenous support, his family was able to take him home and continue his supportive care and recovery there. Dr. Portner rechecked Thorn the next day and he was even more relaxed at home, only becoming stiff when stimulated, but he was able to sleep comfortably and even started being able to urinate outside when he was carried out and held up in the grass.
Thorn was rechecked again 1 week later with Dr. Tracy and he was continuing to show considerable improvement. With some support, he was able to start taking some steps and was eating well at home. Dr. Berkowitz contacted Thorn’s family one month after he first showed signs of problems and they reported: “He is amazingly fine! Completely normal, thanks to you and your staff.” We are so happy with Thorn’s progress and he will go on to live a

Robbinsville, NJ, Maple Shade, NJ, Brick, NJ Joshua Portner, DVM, DACVECC – Medical Director, Maple Shade
Dr. Portner grew up in Southern New Hampshire. He obtained his bachelor’s degree in Biology/All-College Honors from Canisius College in Buffalo, New York, and his veterinary degree from Tufts University School of Veterinary Medicine in Massachusetts in 2004. After graduation from Tufts University, Dr. Portner completed a rotating internship in small animal medicine and surgery at Alameda East Veterinary Hospital in Denver, Colorado, and went on to complete his residency in Emergency and Critical Care at Ocean State Veterinary Specialists in Rhode Island in July of 2008. In 2009, Dr. Portner passed the specialist certification examination and became board certified in Emergency and
normal, happy life with a terrific family. ! Even after all that treatment as a pup, and dog is now a FCH with at least one Absolute under is belt AND has sired a litter.


Critical Care Medicine.
Dr. Portner has special interests in mechanical ventilation, nutrition for critical patients, and transfusion medicine. Along with membership in the Veterinary Emergency and Critical Care Society (VECCS), American Veterinary Medical Association (AVMA), and the New Jersey Veterinary Medical Association (NJVMA), he has also been a member of the International Veterinary Academy of Pain Management (IVAPM) and the International Sled Dog Veterinary Medical Association (ISDVMA), as well as several state associations. During his residency, he was a member of the Rhode Island Disaster Response Team, which is an organization responsible for providing medical care to sick and injured animals during a state of emergency.
Steven Berkowitz, DVM Dr. Steven Berkowitz attended St. Georges University and did his clinical year at the University of Illinois. Berkowitz joined NorthStar VETS after serving as the Chief of Emergency and Critical Care at another specialty hospital.
Prior to that, he completed a three-year residency in Emergency and Critical Care medicine at the Oradell Animal Hospital in Paramus, NJ. His residency was completed at one of only a few recognized veterinary trauma centers in the United States. Prior to his residency, he was a staff Emergency Veterinarian at Animal Specialty Center in Yonkers, NY as well as serving as an emergency doctor at Animal Emergency and Referral Associates in Fairfield, NJ for 3 years. Dr. Berkowitz can be seen on seasons 5 and 6 of “Animal Precinct” on Animal Planet, which was filmed during his internship at The Bergh Memorial Animal Hospital of the ASPCA in New York City.
Dr. Berkowitz has special interest in the management of metabolic and endocrine derangements, trauma, as well as management of the septic patient.
39&Me

From the AKC CHF Website, October, 2020 Originally published in the Canine Chronicle
By Caroline Coile
And herein lies one problem with genetic testing: dog owners, and even dog breeders, too often don’t know what it means. And it’s not really their fault. Thirty years ago all we had to know was the difference between genotype and phenotype, and dominant and recessive. We thought that if we could identify every carrier through test breedings, and remove them from the gene pool, we could purge our dogs of hereditary illness. We fantasized about DNA tests that might one day allow us to actually “see” a dog’s recessive genes. And when that first test happened, and then another, and another, breeders set out to do just that. They removed every carrier they could identify, and in so doing created a genetic bottleneck that reduce their breed’s genetic diversity and allowed other heretofore unknown or insignificant diseases to come to the forefront.
With more knowledge of our dog’s genes came the need for more knowledge on how to use this knowledge.
Now we have hundreds of DNA tests, and predictably, even more misunderstanding when it comes to their use. Which is why the hot-off-thepress AKC Canine Health Foundation’s white paper, Review of the State of Genetic Testing–a Living Resource, is something everyone who has ever even uttered the phrase “DNA test” should read. And since it’s free, and online at www.akcchf.org/educationalresources/library/articles/CANINE_ GENETIC_TESTING_07-282020_FINAL_withlinks. A pdf, you can read it while you’re waiting for groups, or waiting for your next progesterone test results. And it’s written so that no matter what your level of expertise, you can start at the basics and work up, or skip around and just check out the newer parts.
As for our friend asking the questions, she could have read several sections concerning genetic tests and breed specificity. Among other things, she would have found out while several companies offer multiplex tests that will test for the presence of alleles associated with as many as somewhere around 175 disorders in certain breeds, they have limitations that far too many dog owners don’t understand: • Far more than 175 (or 200, or 300) genetic diseases exist in dogs. Being clear of 175 of them doesn’t mean your dog is“cleared of every genetic disorder.” It’s just cleared of every disorder on that test panel. • Many disorders are probably polygenic in nature (that basic was explained earlier in the paper, but basically it means a trait depends on the interaction of alleles at several loci), and some have variable penetrance or expressivity (again explained elsewhere, but basically variable penetrance means that the trait doesn’t always manifest, and variable expressivity means the trait may manifest to different degrees), and either may depend on alleles at other loci or environmental factors.
Despite a vast amount of research on hip dysplasia, for example, we still have no DNA test for it because it’s not a simple case of
Mendelian inheritance. • An allele that causes a disease in one breed may not cause it in another. For example, the presence of an allele at a different locus may also be needed for the disease to manifest.
That’s the case for one of the current witch hunts, the “allele for degenerative myelopathy” (DM). In several breeds, dogs with two mutant copies in the SOD1 gene are at increased risk of DM. Yet in other breeds these mutant copies have no effect on DM susceptibility, probably because another as yet unidentified mutant allele must also be present. The homozygous SOD1 mutation is necessary, but not sufficient, for DM, yet people are having their dogs tested for the
SOD1 mutation in breeds in which DM never occurs, and probably can’t occur. Then they’re either removing dogs from the breeding population or bragging that they are clear, continued page 14...
(July 14, 2004 –October 15, 2020)
• #1 Dachshund All Coats/All Systems 2008 • 12 BISS wins including 2008 DCA Host Show • 7 All-Breed Bests in Show • Two-time Westminster BOV Winner • 2009 Westminster Hound Group 4
“This bitch not only possesses the basic elements of head and body makeup that make for an excellent representative of the breed but she conveys the essence of the breed as an athletic bold and courageous hound while retaining the allure and charm of femininity. She offered a perfect balance of bone and substance wrapped in excellent coat texture which when put in motion thrills and excites.”
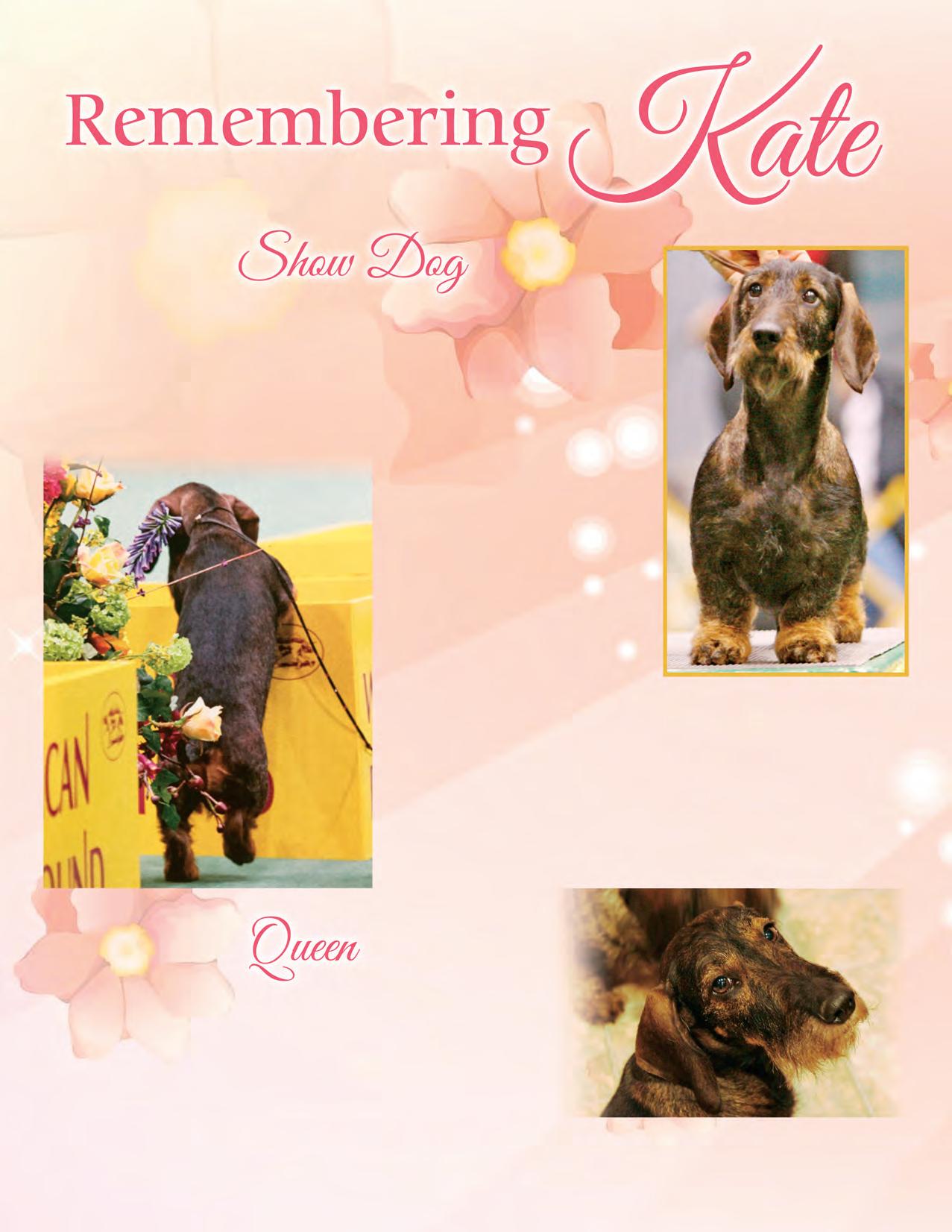
Dr Donald Sturz–2009 Westminster BOV Judge (DoxieDigest 2009)
• Demanding and loving • She filled every day with her presence • Lived her life on her own terms until the very end








