3 minute read
Transforming Eye Care in Children with Robotic OCT
Pediatric retinal diseases, while rare, can lead to permanent blindness if not addressed promptly. Several factors can delay their diagnosis. An infant or toddler may not notice or be able to express a vision concern, especially if it impacts sight in only one eye. Young patients are also most likely to be taken first to a pediatrician’s office or emergency department, locations with limited eye screening tools.
Another obstacle: the limited use of optical coherence tomography (OCT) in pediatric ophthalmology. One of the most valuable imaging advances of the last two decades, OCT is superior to ophthalmoscopy or fundus photography in capturing subtle aspects of retinal pathology. But OCT requires the patient to remain absolutely still and focused on a fixed visual target, constraints not usually achievable with the youngest patients.
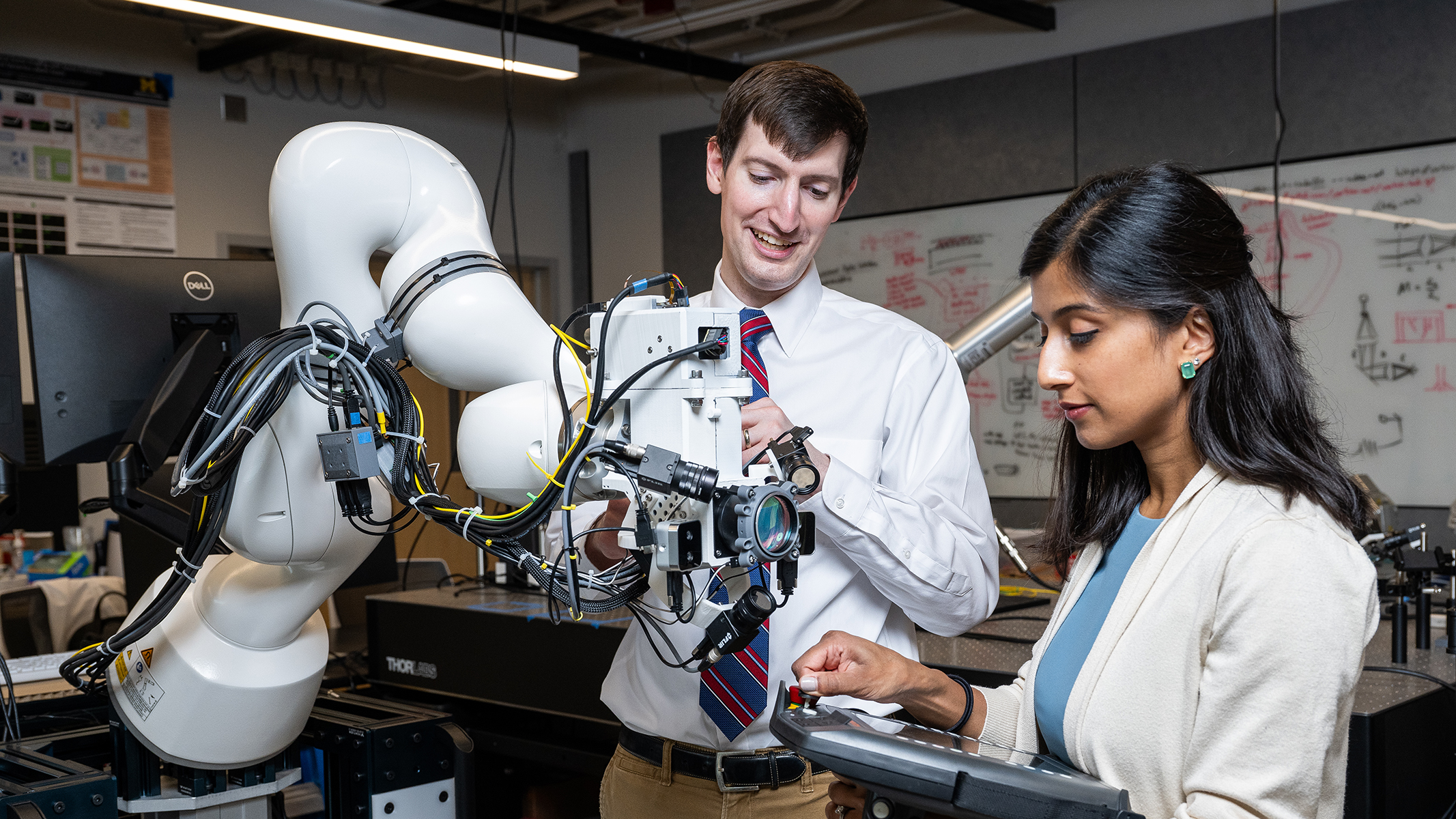
Nita Valikodath, M.D., M.S., is committed to extending the benefits of OCT to this vulnerable population. A retinal surgeon who treats patients of all ages, Dr. Valikodath is working with experts at Kellogg and Michigan Robotics to develop and test a robot-assisted OCT device that is both user- and child-friendly.

Her work builds on a contactless robotically aligned OCT (RAOCT) developed at Duke University by her Kellogg colleague Mark Draelos, M.D., Ph.D. She is funded by Kellogg’s NIH Mentored Clinical Scientist Training Grant, or K12, which supports two clinical scholars annually.
“I was first introduced to Mark’s innovations in robot-assisted OCT when we were both at Duke,”
Dr. Valikodath says, “I became convinced that a similar system could be modified for pediatric patients and revolutionize pediatric eye care. I’m delighted to have Mark as a collaborator as I pursue this project at Michigan. We share the same passion for developing innovative medical devices to improve clinical care, and it has been exciting to build our robotic OCT team.”
The device she is developing combines several key features of RAOCT, including a robotic arm and face and pupil tracking telemetry to compensate for unintended motions of the head and eye, and the ability to adapt to different patient positions (sitting, lying down) and head orientations. It will include a larger field of view of the retina, a less intimidating and more child-friendly exterior appearance, and fixation targets like colored lights or attention-grabbing images. Rigorous pilot and proof-of-concept studies will be conducted to evaluate various measures of performance, accuracy and patient acceptance.
Throughout her training, Dr. Valikodath has been inspired and mentored by several pioneers in applying advancements in telemedicine, artificial intelligence, and OCT to pediatric retina. Her most pivotal mentors have been Cynthia Toth, M.D., at Duke University, and R.V. Paul Chan, M.D., M.Sc., M.B.A., of the University of Illinois at Chicago, as well as Cagri Besirli, M.D., Ph.D., and Maria Woodward, M.D., M.S. at Kellogg.
“I’m thrilled to have this opportunity to learn from the best and grow as an independent clinician-scientist,” says Dr. Valikodath. “But I’m even more excited about how these technologies can transform ophthalmic care for kids and other vulnerable populations, guiding diagnosis and treatment in primary care and emergency settings, and bedside in inpatient and neonatal intensive care units to prevent blindness.”










