5 minute read
Top news
‘Poop pills’ as good as colonoscopy to treat C. difficile
STOOL CAPSULES COULD BE THE MAGIC PILL FOR TREATMENT OF THE DANGEROUS INFECTION
Advertisement
ORIGINAL STORY
CBC, NOVEMBER 2017
PHOTO BY
LAUGHING DOG PHOTOGRAPHY
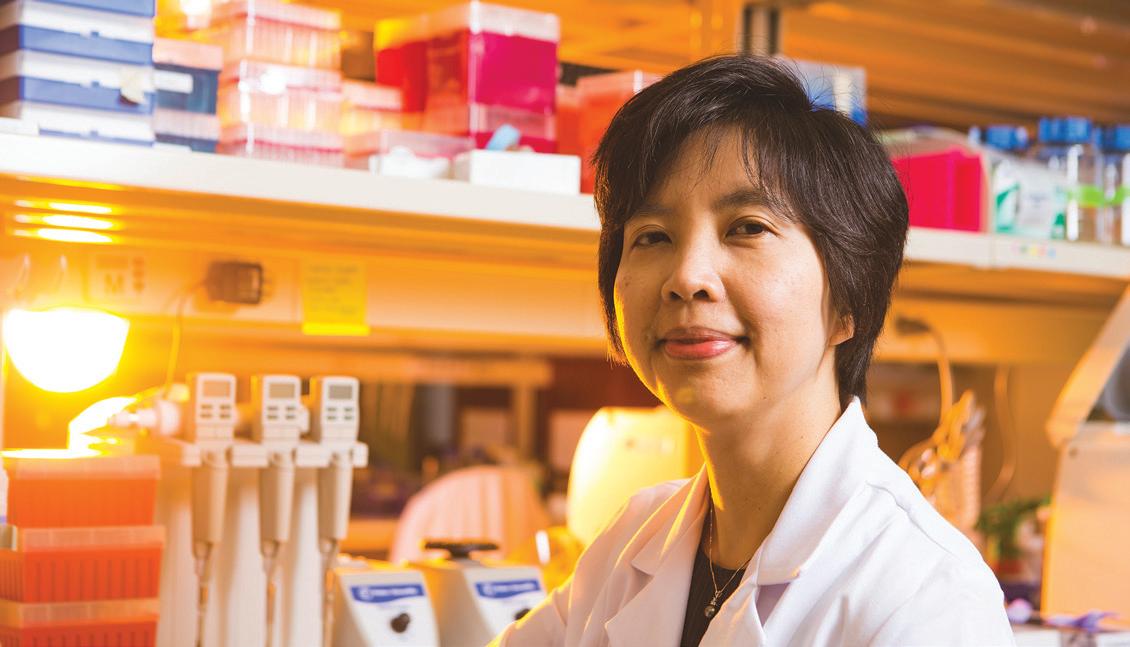
Dina Kao’s study shows capsules were 96-per-cent effective in treating C. difficile.
WHEN IT COMES to treating Clostridium difficile (C. diff) with a fecal microbiota transplant—yes, human poop—swallowing a frozen capsule appears to have far less of an “ick factor” and works as well as delivering the therapy via colonoscopy, University of Alberta researchers say.
C. diff is a potentially fatal infection of the gut marked by severe diarrhea and abdominal pain. Outbreaks in hospitals and long-term care facilities are notoriously challenging to eradicate.
A study led by U of A associate professor and gastroenterologist Dina Kao (’94 BSc, ’99 MD, ’08 MSc) found that while both methods resulted in a 96-per-cent success rate in treating C. diff, the capsules have many advantages: They are noninvasive, less expensive and can be administered in a doctor’s office without the patient being sedated.
Kao believes administering fecal microbiota transplant using capsules—a delivery mode in which fecal matter from donors is refined, then frozen—could help broaden the use of fecal transplants for treating C. diff. microbiota transplant,” Kao said, noting that using the capsules instead of colonoscopy could save the health system at least $1,000 per patient. “From a health-care perspective, I think it becomes a no-brainer,” said Kao. “Why would we be delivering a transplant by any other route?”
The research was funded by Alberta Health Services and the University Hospital Foundation and published in the Journal of the American Medical Association.

ORIGINAL STORY
CTV NEWS, FEBRUARY 2018
IN A STUDY published in the American Journal of Hypertension, researchers from the U of A have found that up to 70 per cent of readings from home blood-pressure monitors are “unacceptably inaccurate.”
Funded by the University Hospital Foundation, Jennifer Ringrose (’98 MSc), co-author Rajdeep Padwal and their team tested dozens of in-home blood-pressure monitors.
“High blood pressure is the Number 1 cause of death and disability in the world,” said Ringrose. “We need to make sure that home blood-pressure readings are accurate.”
Docs should think twice before prescribing marijuana
ORIGINAL STORY
CTV NEWS, FEBRUARY 2018
A NEW MEDICAL guideline published in the medical journal Canadian Family Physician says there is limited evidence to support the reported benefits of medical marijuana for many conditions. It adds that any benefit could be balanced or even outweighed by the potential harm.
“While enthusiasm for medical marijuana is very strong among some people, good quality research has not caught up,” said project leader Mike Allan, director of evidence-based medicine in the U of A’s Department of Family Medicine.
The guideline was created by a committee of 10 doctors, allied health professionals and a patient, after U of A researchers performed an indepth review of clinical trials. It was peer reviewed by 40 others, including doctors, pharmacists, nurses and patients.
Meet the newsmakers

JENNIFER RINGROSE ’98 MSc – Women and Children’s Health Research Institute
RAJDEEP PADWAL Mazankowski Heart Institute, Department of Medicine Division of General Internal Medicine MIKE ALLAN Director – PEER (Patients, Experience, Evidence, Research) Director – Evidence Based Medicine, Department of Family Medicine PETER LIGHT Dr. Charles A. Allard Chair – Diabetes Research
Director – Alberta Diabetes Institute, Department of Pharmacology ANITA KOZYRSKYJ Professor –Department of Pediatrics, Division of Pediatric Respirology, Pulmonary and Asthma
Whoa! Sunlight could actually shrink your fat cells
ORIGINAL STORY
READER’S DIGEST, JANUARY 2018
WINTER ALWAYS SEEMS to bring on weight gain, even if we resist Christmas baking and stick to our workout routines. A study in Scientific Reports, led by U of A pharmacology professor and director of the Alberta Diabetes Institute Peter Light, may show why.
Light and his team put some fat cells under lamps giving off blue light (the shortest visible light to come from the sun) for four hours and kept other samples in the dark. After two weeks, the fat-cell groups showed remarkable differences.
The blue light-treated fat cells had fewer lipid droplets—organelles that store fat—than the cells that didn’t get any light. What’s more, the lipid droplets in the light-treated cells were also smaller than the ones in the placebo group.
While more studies are needed and the researchers haven’t pinned down why light affects fat storage, the study authors believe blue light might tell your body how to store fat. During the winter, when daylight is short, your body is programmed to store fat; with more sunlight in the summer, your body burns it off again.
The researchers hope the findings could lead to weight-loss innovations, but warn not to try shedding pounds just by spending extra time in the sun.
Funding partners

Canadian Institutes for Health Research
University Hospital Foundation Alberta Innovates
Juvenile Diabetes Research Foundation
Alberta Diabetes Foundation
American Diabetes Association
Edmonton Civic Employees Charitable Assistance Fund
Firefighters Burn Trust Fund Dr. Rod Eidem Diabetes Research Fund
Deutsche Forschungsgemeinschaft
C-section in overweight moms increases risk of obesity in kids through changes in babies’ gut bacteria
ORIGINAL STORY
NEW YORK TIMES, FEBRUARY 2018 OVERWEIGHT MOTHERS ARE more likely to have overweight babies and the gut bacteria the babies inherit may in part be to blame, according to a study led by U of A professor of pediatrics Anita Kozyrskyj.

Published in JAMA Pediatrics and funded by AllerGen, Alberta Innovates and the Canadian Institutes of Health Research, the study reports that overweight mothers are more likely to have a caesarean section. Babies born by C-section to those mothers have different gut bacteria from those in babies born to normal-weight women and are more than five times as likely to be overweight.
There is no single probiotic that can undo changes in gut bacteria of infants after a C-section, says Kozyrskyj, and “if a C-section is unavoidable, there is no easy answer.” But typically, she adds, “breastfeeding is effective in helping to prevent infants from becoming overweight.”










