
5 minute read
COVER: Advancing
BIOMEDICAL ENGINEERING FACULTY JULIE SUTCLIFFE AND RANDY CARNEY are making big strides in cancer research. With a combined $6.5 million in new grants from Stand Up to Cancer and the National Institute of Health’s National Cancer Institute, Sutcliffe and Carney are pioneering new technology that will help treat and diagnose cancer earlier and more effectively, saving more lives.
“It’s feasible that in our lifetimes, cancer will be a manageable disease, but we need these new technologies to figure out how to do that,” said Carney.
Advertisement
ADVANCING Cancer
Research at UC Davis
By Noah Pflueger-Peters
Photo above: Professor Julie Sutcliffe (left) and UC Davis School of Medicine collaborator Rick Bold, M.D. at the UC Davis Comprehensive Center in Sacramento. (Julie Sutcliffe/UC Davis)
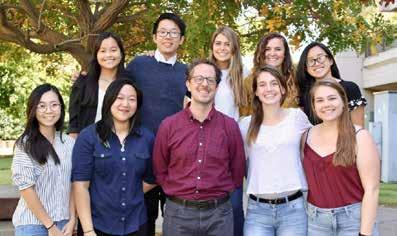
Photo below: The Carney Lab in 2019. (Randy Carney/UC Davis)
IMAGING TOOLS TO TREAT PANCREATIC CANCER
Professor Julie Sutcliffe is using her expertise in cancer imaging and diagnosis to develop a new, effective treatment for pancreatic cancer. After developing a therapeutic from a radioactive imaging tool, her team received $4 million from Stand Up to Cancer to bring their UC Davis-made drug to clinical trials to help patients suffering from the disease.
Pancreatic cancer is often asymptomatic until very late stages and the pancreas itself is very dense, making it impossible to deliver drugs directly to the source. The only true treatment is surgically removing part or all of the pancreas, but the surgery can’t be done if the cancer has spread—or metastasized—to other parts of the body. The goal, then, is to find and eradicate the metastasized tumors to make the surgery an option for more patients.
“If you can’t have surgery because you have metastatic disease, then we’re going to use this therapy to treat that metastatic disease first so they can operate,” she said.
UC Davis School of Medicine developed radioactive isotopes in their lab that bind to receptors that only exist on metastasized pancreatic cancer cells. These isotopes allow them to accurately image the disease using a PET scanner— something some experts didn’t think was possible.
When, in 2018, Stand Up to Cancer and the Lustgarten Foundation called for proposals that fast-tracked therapeutics for pancreatic cancer, the team took the challenge in stride to turn their diagnostic tool into a treatment.
“When they said to us ‘you have a year to develop a therapeutic,’ we said, ‘ok, game on,’” she said. “If I change the one radioactive isotope on my diagnostic, I now have a radionuclide therapy [tool] that I can use to treat.”
The team received $1 million in 2018 to develop the tool and conduct initial tests. After finding success, the team submitted an Investigational New Drug (IND) application to the Food and Drug Administration for the therapeutic that is currently under review. The additional $4 million will allow them to conduct clinical trials.
“We’ve got all the preclinical data, we have the toxicology package and we make the drug in my lab,” she said. “So now not only does UC Davis have this first-in-human diagnostic, but they will also have a first-in-human therapy that was homegrown out of our lab.”
Sutcliffe stresses the importance of her team, both in her lab and at the UC Davis School of Medicine. The team brings together chemists and biologists in her lab with surgeons, pathologists, radiation oncologist and nuclear medicine physicians who all contribute expertise and experience to all aspects of developing this new treatment.
“It’s team science,” she said. “Imagine the people power it took to get from an idea through to preclinical modeling to enough data to get an IND application in a year. My team is so diverse and I need all of them.”
A NEW GOLD STANDARD FOR EARLY-STAGE CANCER DIAGNOSIS
Assistant professor Randy Carney and his lab are on a mission to find new tools to diagnose very early-stage cancer. His new five-year, $2.5 million project funded by the NIH National Cancer Institute seeks to develop next-generation nanotechnology to identify traces of cancer in blood, saliva or sweat samples to find the disease earlier and save more lives. as extracellular vesicles. Exosomes are tiny nanoparticles in bodily fluids that were once thought to be cellular waste, but actually carry genes, proteins and lipids from their cell of origin, including cancer cells. However, there may be one cancer vesicle out of trillions in a given sample, so the team needs to both find and highlight them.
“When the cancer cell spits it out, it’s like a needle in a haystack,” said Carney. “So the core of our project is to try to distinguish those tumor vesicles from the healthy ones.”
To do this, the team plans to engineer gold nanoparticles with targeting molecules to literally light up the cancer exosomes. The team has identified five cancer-associated proteins to focus on for their initial tests and made five corresponding types of gold nanoparticles that bind to each of these proteins. Each nanoparticle lights up differently when the team shines a light or weak laser on them.
The nanoparticles also allow them to sense these exosomes with high chemical sensitivity—the more nanoparticles they have bonded to a cancer exosome, the more they know about its chemical makeup. This could lead to new insights not only about cancer, but also about exosomes’ composition and distribution in different samples.
“A really realistic secondary goal is to start to be able to get answers to questions that we didn’t even know to ask,” he said. “It’ll be kind of an enabling technology in that way.”

The team will begin by collecting data from advanced-stage cancer patients to learn which markers and patterns correspond to different types and stages of cancer. Because this type of work is new, Carney expects that tests will reveal new insights about how cancer progresses that can be used to find and diagnose the disease earlier on, which is key to saving more lives.
“The technology is hard to translate to real patient outcomes, but it has great promise and it’s super exciting to try to use it successfully,” he said. “It’s super inspiring for a whole group to be working on something that’s so directed and has a great potential outcome.”
Top Photo: Biomedical engineering professor Julie Sutcliffe.
Bottom Photo: Biomedical engineering assistant professor Randy Carney. (Reeta Asmai/UC Davis)










