

FROM THE EDITORS-IN-CHIEF
Dear readers,
We are ringing in the new year with some new changes to PULSE. We will now be publishing two issues during the school year – don’t forget to keep an eye out for our spring publication! This issue, we are excited to present a wide range of articles (14 to be exact) with everything from opinion pieces to a spotlight piece featuring a UChicago faculty member.
We are excited to share with you an issue discussing various topics in medical ethics. How can we ensure CRISPR remains ethical? What do we make of the “husband stitch”? These are just a couple of the questions posed in this quarter’s publication.
We would like to extend a big thank you to all of our current writers, editors, and the production team for all of their hard work in making this issue possible. To our senior editors, Aymon Lone and Fareen Dhuka, thank you for stepping into these leadership positions, and we are extremely grateful to have you on the team. We hope you enjoy our issue!
With regards,
Riley Hurr and Katrina Schmitt
Writers
Aidan Choi
Alexander von Kumberg
Emnet Djibrila
Hunter Bershtein
Jahnavi Muppirala
Julian Kage
Maryam Shariff
Michelle Mejia
Miles Kaufman
Milla Dobrovolska-Ivanova
Neeharika Venuturupalli
Shaherzad Chawdree
Stacia Konow
Editors
Adam Kunz
Ally Wang
Aman Majmudar
Ashley Chen
Emily Shi
Eva McCord
Hermela Selam
Michelle Lu
Rachel Zhang
Rahul Burra
Rina Iwata
Sanaa Imami
Sophia Falk
Taran Ramchandani
Trinity Ransom
Editorial EIC
Riley Hurr
Layout EIC
Katrina Schmitt
Senior Editors
Aymon Lone
Fareen Dhuka
Managing Editor
Charlotte Clulow
Cover Design
Kim Mercado
Production
Katrina Schmitt
Riley Hurr
Fareen Dhuka
Bubbles, Tweezers and COVID-19
By Aidan Choi Edited By Aman Majmudar & Trinity RansomIn December 2020, for the first time ever in a clinical trial, liver cancer patients were treated without using chemotherapy. Instead, the researchers treated the patients using microbubble ultrasound technology, where ultrasound waves—whose high frequency we cannot hear—pop small gas-filled bubbles containing drugs at precise locations in the body. For the 15 patients who were treated with this novel technology, 93% of the tumors showed a positive response to the treatment. Better yet, the treat-
ment produced no additional side effects (unlike chemotherapy) on the patients. Due to this success, the researchers are enrolling more patients to further understand the benefits of ultrasound microbubble technology in the fight against cancer.
Besides potential cancer treatment, the technology already has a broad range of clinical uses, the most common being in gynecology to monitor a developing fetus. Ultrasound is clinically useful because it propagates through liquid mediums well, including the human body, which is roughly 70% water. One of its most innovative medical applications
is in targeted drug delivery via microbubble technology. Microbubbles, small gas-filled particles, interact with the body on a cellular level. Their gas-filled core is stabilized by an outer shell, where the drugs are loaded (Figure 1) due to the inert interior gas being a poor solvent for drug molecules. Once loaded, the microbubbles are injected into the bloodstream. When fired at by ultrasound beams, the bubbles pop like balloons in targeted areas for precise release of the payload drug.

The material of the microbubbles’ outer shell should be flexible: the easier the microbubbles can expand and contract, the easier they can release drugs. The microbubble’s ability to expand and contract while under the effects of ultrasound determines its efficacy as a drug deliverer. This explains why many microbubbles used today have a protein albumin shell rather than polymer shells that have a higher stiffness constant (material doesn’t expand and contract easily).
Under the effect of ultrasound waves at a target site like a tumor, microbubbles rapidly vibrate, expand and contract until they collapse, known as the destructibility point. Ultrasound waves collapse the microbubbles by reducing the pressure around the bubbles, creating a pressure gradient between the area near the bubbles and the rest of the surroundings. When microbubbles collapse, they produce mechanical shock waves that overcome biological barriers - which protect our organs from harmful pathogens in our bloodstream - and vortices in the direction of the barrier, known as microstreaming (Figure 2). Both the shock waves and vortices increase the permeability of the biological barriers, allowing the drugs to be planted deep within the tumor, increasing drug uptake.

Since microbubble ultrasound technology is safe and
non-invasive, it can revolutionize the field of drug delivery. One innovative application of this technology is called “acoustical tweezers.” Acoustical tweezers use two ultrasound wave beams, of different frequencies, to trap and manipulate individual microbubbles without physical contact, hence the name “tweezers.” The waves superimpose (overlap together) and cause the microbubble to vibrate. The bubble’s vibrations interact with the pressure gradient caused by the ultrasound beam to produce a force (primary Bjerknes force) on the microbubble. The forces produced by the tweezers enabled the researchers to control the movement and behavior of a single microbubble, such as when it collapsed.
“By controlling this complex process on the scale of a single microbubble, we are gathering fundamental information for promising biomedical applications,” said Dr. Diego Baresch, lead author of this research at Imperial College London. Their next step is to manipulate several microbubbles at a time and to then apply this technology to real body tissue for clinical biomedical use. Being able to manipulate individual microbubbles is a significant step as it adds yet another layer of precision to drug delivery and will allow clinicians to target only malignant cells in patients without damaging healthy body tissues.
Ultrasound microbubble technology also has the potential to treat COVID-19. Engineers at MIT are exploring the potential
“By controlling this complex process on the scale of a single microbubble, we are gathering fundamental information for promising biomedical applications.”
Dr. Diego Baresch
use of ultrasound to destroy the COVID virus. They have found that frequencies between 25100MHz (estimation of the shell’s resonant frequency f0) cause the virus to collapse and buckle in on itself in both air and liquid mediums. The virus itself has a lipid protein shell with crown shaped receptors protruding from its shell, very similar to the structure of a microbubble making this a perfect application for ultrasound technology. What remains to be explored by the researchers is the behavior of the external microscopic spikes and how the RNA material inside the virus will interact with the body once the shell fragments. If successful, non-invasive ultrasound may be used as a widespread treatment for future COVID outbreaks.
Microbubbles are being used in gene therapy to deliver genetic material such as sRNA which silences certain genes and DNA which activates genes. They are also being used to deliver proteins that can induce the growth of new vascular structures such as blood vessels. Because this technology is safe and non-invasive, it has the potential to replace drug delivery methods such as chemotherapy, which are unable to target only malignant cells and thus cause significantly harmful side effects and damage to healthy tissues.
RESEARCH
References:
Jefferson Health: First in Human Clinical Trial Shows Microbubbles may improve effectiveness of radiation therapy in patients with liver cancer, https://www.jeffersonhealth.org/ about-us/news/2020/12/human-clinical-trials-microbubbles-may-improve-radiation-therapy-liver-cancer
The Journal of Chemical Physics: On the Stability of Gas Bubbles in liquid-Gas Solutions: J. Chem. Phys. 18, 1505 (1950); https://doi. org/10.1063/1.1747520 Submitted: 31 July 1950
• Published Online: 22 December 2004 P. S. Epstein and M. S. Plesset
National Center for Biotechnology Information: Microbubbles in Imaging: Applications beyond Ultrasound, Paul Kogan, Ryan C,Gessner and Paul A.Dayton Bubble Sci Eng Technol. 2010 Jun; 2(1): 3–8. doi: 10.1179/175889610X127305 66149100
Medicine delivery via microbubbles could be made possible using sound waves: https://www. imperial.ac.uk/news/198593/medicine-delivery-microbubbles-could-made-possible/
Ultrasonics Volume 44, Pages 123-126 (Shigao Chen, Randall Kinnick, James F.Greenleaf, Mostafa Fatemi) Ultrasound has potential to damage coronaviruses, study finds: https://news.mit.edu/2021/ultrasound-coronaviruses-damage-0316
National center for Biotechnology Information: Microbubble compositions, properties and biomedical applications, https://www.ncbi.nlm. nih.gov/pmc/articles/PMC2889676/
National center for Biotechnology Information: Drug loaded Microbubbles combined with ultrasound for Thrombolysis and malignant tumour therapy:
https://www.ncbi.nlm.nih.gov/pmc/articles/ PMC6791276/#B21
Royal Society of Chemistry: Making waves: how ultrasound targeted drug delivery is changing pharmaceutical approaches:
https://pubs.rsc.org/en/content/articlehtml/2022/ma/d1ma01197a
Vesalius’ Fostering of the Inquisitive Medical Mind
 By Alexander von Kumberg
Edited By Adam Kunz
By Alexander von Kumberg
Edited By Adam Kunz
Although the Petrarchan illustration of the Middle Ages as Dark Ages is mostly contextualized and delegitimized by contemporary medieval historians, it is unquestionable that medieval Europe’s medical advances were trifling. Indeed, in the period following the fall of the Western Roman Empire in the 5th century until Francesco Petrarch’s kindling of the Renaissance in the late 14th century, medical knowledge in Western Europe was composed of antediluvian relics of incomplete classical manuscripts. Furthermore, medieval Europe was an agrarian society, with fewer than 10 percent of the population living in towns and cities. The remaining population was primarily tied to the land as serfs. Manorialism dominated Europe, entailing self-sustained archaic and stagnant socio-economic societies. Moreover, the vast majority of Europeans did not possess the means nor the time to ponder about the underlying nature of reality. Rather, most were preoccupied with surviving winters and securing salvation. Hence, any form of scientific or technological advances was severely limited. Nonetheless, there
existed small enclaves where means for prolonged thought and contemplation occurred: the monasteries. It was within the monastic tradition that medieval medical advances transpired, such as the monastic hospitals that served as centers of hospitality and care for pilgrims, paupers, the elderly, and the infirm. Furthermore, while medicine was stagnant in the West, the Arabic Golden Age was flourishing with great physicians like Ibn Sina and Abu Bakr al-Razi (latinized to Rhazes). Such physicians translated and improved upon classical texts. Thus, diverse geographical locales were the sites of most medieval medical advances. An example would be the Duchy of Apulia and Calabria, where the Medical School of Salerno – better known as ‘Salernitana’ – was founded in the ninth century – allegedly by a Christian, a Muslim, and a Jew. Even the crusades, which violently clashed West with East, led to novel discourse, as physicians that accompanied
the Latin armies began to practice, discover, and dialogue with Arabic physicians. Collections of classical, particularly Hellenic, manuscripts were united and grew in abundance, leading to great leaps in medical knowledge. Although the abundance of classical medical texts improved the practice of medicine in medieval Europe, such texts became authoritative and, in many cases, unquestioned. The dominance of classical medical discoveries led to a period of stagnation and apathy in medical circles. Yet, the Flemish physician, Andreas Vesalius overcame apathy and blind adherence to antiquated and authoritative texts. Vesalius triumphed inquisitiveness, investigation, and ultimately revolutionized the practice of medicine, forging the necessary mentality
for the scientific revolution.
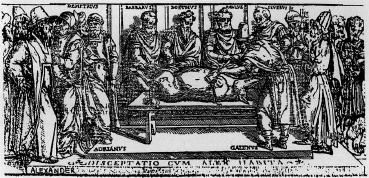
The most revered ancient physician in 16th century Europe was Galen of Pergamon. Doctors working thirteen centuries after Galen praised and feared him; his words were akin to the near infallible words of Aristotle in philosophical circles. Thus, one must understand Galen to understand the medical world that Vesalius inhabited. Galen was born in 129 AD in Pergamon, in modern day Turkey. He spent his youth traveling the Mediterranean seeking to uncover the best medical techniques of the time, and to unify, mold, and add to them. He used this abundance of knowledge to challenge the most renowned physicians of Greece, often striking fear and admiration in gathered audiences. The young physician differed from his colleagues in how he studied. While most Greek physicians pondered what caused symptoms and dialogued like their contemporary philosophers, Galen focused on anatomy. Roman law banned human dissections, and thus Galen mostly dissected non-human mammals like dogs and pigs. Despite this, Galen understood that the brain, not the heart, controlled the body (as was incorrectly suggested by Aristotle). He comprehended that arteries transported blood, and he used the patient’s pulse to signal illness. Hence, it is clear that Galen made some phenomenal discoveries. His renown
made him a physician for gladiators and ultimately emperors, having served Marcus Aurelius and Commodus. Galen considered his works to be indubitable and necessarily preserved. As a result, Galen restlessly cataloged and conserved
his millennium old ego drama through the centuries. Physicians that took a stand against Galen were ostracized and ignored. Yet, it was Vesalius who possessed the prestige and knowledge to finally topple Galen in the 16th century.
Vesalius challenged the giants of old, testing so called truths, correcting them, and propelling applications humanity onwards, not only through discoveries, but via evolutionizing the medical researcher’s mentality.

his discoveries and beliefs, allowing his works to survive longer than other ancient physicians’, this when paired with the late medieval mind’s obsession and triumph of classical ideas, meant his works were prized and utilized the most. Unfortunately, this meant Galen’s incorrect theories prevailed, such as Hippocrates’ four humours theory, bloodletting, misinformed ideas such as women having less teeth than men, and the belief that blood was created in the liver. Later physicians, despite seeing evidence of Galen’s fallibility, tried to skew results in his favor, or outright ignored any contradictions. The medical world was under the spell of Galen’s theories, echoing
Vesalius was born in Brussels, part of the Habsburg Netherlands, in 1514. He attended the prestigious Catholic University of Leuven before studying at the University of Paris for medical school. It was in Paris where the young physician learned to dissect animal and human cadavers. It was anatomy which, much like Galen, struck Vesalius as the most fascinating and key instrument to gathering medical knowledge. Luckily for him, Paris had no shortage of cadavers, particularly skeletons. It was in Paris where he was heavily influenced by the Humanist intellectual tradition and the accompanying obsession with all things classical. Indeed, Vesalius was surrounded by an academic revolution in which classical manuscripts were being retranslated at increasing rates. Vesalius’ challenging of Galen commenced early in his career, with his thesis concerning the works of the 10th century physician, Abu Bakr al-Razi, who was known to have doubts on certain Galenic principles. Perhaps it was the works of al-Razi that first propelled the young Vesalius to start questioning the Galen-centric view of human anatomy and physiology. He then traveled to the University of Padua where he received a doctoral degree in medicine and became a lecturer in surgery. The traditional medieval method of anatomical instruction relied on three separate individuals: lector
(lecturer), sector (barber/butcher), and ostensor (assistant of the professor). Vesalius refuted the labyrinthine method of hiring an assistant to guide a barber in the dissection, rather preferring to take a more hands on approach and dissecting cadavers himself while lecturing. It was in Padua, and later Bologna, where Vesalius would begin unceasingly criticizing ancient texts following self-piloted dissections. Through his endless dissections of both human and animal cadavers, Vesalius concluded that Galen had been drawing his conclusions from animals not humans. One such example was Galen’s incorrect assertion that there existed a blood vessel network at the base of the brain called the rete mirabile, which exists in sheep, or his supposed claim that the human jaw was composed of two bones. Ultimately, Vesalius transcended his contemporary society’s understanding of the human body, finally comprehending that the human was not a mere sack of humors, but an intricate
composite of physical, mechanical, and interlocking systems. Vesalius traveled to Venice in 1542 in order to prepare his epochal magnum opus, De humani corporis fabrica libri septem (Seven Books on the Fabric of the Human Body).
It can be argued that modern anatomy begins with De humani corporis fabrica libri septem. Vesalius gathered his years of medical research in this gargantuan seven volume text which includes over 300 illustrations. Indeed, his piece is not merely a textbook, but a work of art. It leased a new language to anatomy, a certain elegance and urbanity that was only made feasible by the relatively novel printing technology. Vesalius was fastidious in his overseeing of the publication process, traveling to Venice to supervise the drawings. It is most commonly believed that the illustrations were derived from the studios of painter Jan Stefan von Kalkar and the Venetian artist Titian. There, the illustrations were engraved on wood, and then sent to Basel for printing. The book is seen as a masterpiece of Renaissance printmaking just as much as it is a critical development in medical history. Fabrica, which it is commonly denoted as, is divided into seven sections cov-
ering the bones and cartilage, ligaments and muscle, veins and arteries, nerves, heart, brain, and the organs of nutrition and generation. Its pages bleed with Vesalius’ knowledge and ingenuity, with an accurate description of the skeletal system and the entire muscular system. Fabrica lays out the order of operation behind dissection, and includes a catalog of the necessary tools. The assertions of the body as a mechanical and intricate form, the rejection of humoral view, as well as the importance given to tools for scientific advances, oftentimes mark Fabrica as the beginning of modern anatomy. Furthermore, the work embodies Vesalius’ toppling of his times’ Hippocratic, Arabic, and most dominantly, Galenic absolutism. Indeed, the publication of Fabrica demonstrated that there was no proof that Galen had ever dissected a human corpse. After presenting Fabrica to the Holy Roman Emperor, Charles V, Vesalius became the imperial physician. Yet, despite his prominence,
Vesalius would need to defend his findings for the remainder of his life. Vehement defenders of Galenism, like the French anatomist Jacques Dubois, went so far as to argue that the human body physically changed since Galen, thus explaining his incorrect affirmations. Despite continuous denial and refutation, it became evident that Vesalius’ discoveries superseded and made fallible those of Galen, thus fabricating a new medical paradigm.
In 1564, Vesalius embarked on a pilgrimage to Jerusalem. The journey ended tragically. On the return, his ship was engulfed in a storm for forty days, leading to a lack of provisions and rampant sickness. The ship made landfall on the island of Zakynthos, and it is said that Vesalius died almost instantly after landfall. Despite his sudden and unexpected death at the age of 49, Vesalius had revolutionized anatomy, medicine, and science. The revolution spurred a medical renaissance. Fabrica commenced the theme of elucidating medical textbooks with accurate and detailed illustrations, which was further developed by Baroque painter Pietro da Cortona. The extraordinary discoveries made by Vesalius brought about a complete rethinking. Yet, his triumphs are not solely medical, but scientific. Indeed, Vesalius lived during the dawn of the scientific revolution, the shift from natural philosophy to science, and his discoveries and novel mentality was a necessary precept for the revolution. His unique approach was based on investigation and testing, not blind adherence. Moreover, his
story pays testament to Sir Isaac Newton’s claim, “if I have seen further, it is by standing on the shoulders of giants.” Galen was wrong in many aspects, yet he was ingenious and vital for the progression of human medical knowledge. Vesalius knew this, and he built upon a Galenic foundation. He also took the next step, proving to his contemporaries that Galen was infallible. He challenged the giants of old, testing so called truths, correcting them, and propelling humanity onwards, not only through discoveries, but via revolutionizing the medical researcher’s mentality. Ultimately, the new mentality forged by Vesalius is made incarnate in the motto of the Royal Society, “Nullius in verba” (take no one’s word for it). An inquisitorial approach to the world of nature is a necessary attribute for the scientist, and one must pay homage to those behemoths of old, like Vesalius, who introduced the mindset to the medical sphere.
References:
Andreas Vesalius (1514-1564). Andreas Vesalius (15 14-1564). (n.d.). Retrieved November 27, 2022, from https://web.stanford.edu/class/ history13/Readings/vesalius.htm
Bernard Becker Medical Library. (n.d.). Vesalius and the Invention of the Modern Body. Vesalius in Paris & The Galenic Legacy. Retrieved November 27, 2022, from http://beckerexhibits. wustl.edu/vesalius/galen-paris.html
Compier, A. H. (2012, January). Rhazes in the renaissance of andreas vesalius. Medical history. Retrieved November 27, 2022, from https://www.ncbi.nlm.nih.gov/pmc/articles/ PMC3314893/
Erjavic, N. (2018, January 10). The Embryo Project Encyclopedia. Andreas Vesalius (1514–1564) | The Embryo Project Encyclopedia. Retrieved November 27, 2022, from https://embryo.asu.edu/pages/andreas-vesalius-1514-1564
Florkin, M. (2022, November 27). Andreas Vesalius. Encyclopædia Britannica. Retrieved November 27, 2022, from https://www.britannica.com/biography/Andreas-Vesalius
Higgins, J. (2014, October 21). The Leg-
acy of Andreas Vesalius. University College Cork. Retrieved November 27, 2022, from https://www.ucc.ie/en/jennings-gallery/past/21oct2014-thelegacyofandreasvesalius/
LH;, T.-P. (2015, June). Medical renaissance. Journal of investigative surgery : the official journal of the Academy of Surgical Research. Retrieved November 27, 2022, from https://pubmed. ncbi.nlm.nih.gov/26065591/
McLean, J. (n.d.). History of Western Civilization II. The Medical Renaissance | History of Western Civilization II. Retrieved November 27, 2022, from https://courses.lumenlearning. com/suny-hccc-worldhistory2/chapter/ the-medical-renaissance/
MediLexicon International. (2022, February 8). Medieval and Renaissance Medicine: Practice and developments. Medical News Today. Retrieved November 27, 2022, from https://www. medicalnewstoday.com/articles/323533
Mesquita, E. T., Souza Júnior, C. V. de, & Ferreira, T. R. (2015). Andreas Vesalius 500 years--a Renaissance that revolutionized cardiovascular knowledge. Revista brasileira de cirurgia cardiovascular : orgao oficial da Sociedade Brasileira de Cirurgia Cardiovascular. Retrieved November 27, 2022, from https://www.ncbi.nlm.nih.gov/pmc/ articles/PMC4462973/
Polozkova, V. (2022, April 11). Andreas Vesalius: Discoveries & Accomplishments. Study.com. Retrieved November 27, 2022, from https://study. com/academy/lesson/andreas-vesalius-discoveries-accomplishments.html
Singer, P. N. (2021, December 3). Galen. Stanford Encyclopedia of Philosophy. Retrieved November 27, 2022, from https://plato.stanford.edu/entries/ galen/
Zampieri, F., ElMaghawry, M., Zanatta, A., & Thiene, G. (2015, December 22). Andreas Vesalius: Celebrating 500 years of dissecting nature. Global cardiology science & practice. Retrieved November 27, 2022, from https://www.ncbi.nlm.nih.gov/pmc/ articles/PMC4762440/
Polycystic Ovarian Syndrome: From Victoria’s Secret to Nigeria
 By Belen Flores Kuri
Edited By Ashley Chen
By Belen Flores Kuri
Edited By Ashley Chen
As the world population balloons to 8 billion people, it is unsurprising that female reproductive health and fertility are brushed under the rug. Nonetheless, approximately 6.1 million women ages 15 to 44 in the United States experience infertility and data suggests 186 million ever-married women of reproductive age in developing countries were maintaining a “child wish” . For women, infertility may be the consequence of a variety of factors, from tubal and uterine disorders to reproductive hormonal imbalances; among these, the most common is the follicular disorder polycystic ovarian syndrome (PCOS), with the condition affecting 8% to 13% of reproductive-aged women.
PCOS Pathophysiology
Although it is an incredibly prevalent endocrine disorder and has been recognized for over 70 years, PCOS has no cohesive definition or diagnosis. Despite the syndrome being named after the cysts that may form on the ovaries, this is merely an indicator rather than a cause of the condition. The low level of understanding of the syndrome, genetic factors, as well as obesity and insulin resistance, are viewed
as potential roots of its development. Similarly, the cause can also be linked to the abnormal pituitary hormone luteinizing hormone (LH) levels and androgens that impede normal ovarian function. Hence, because of the convoluted knowledge about the disease, it is most comprehensively characterized through its associated conditions and symptoms.
Symptoms
Listing and explaining the symptoms of PCOS could potentially be a whole article in itself. With the aforementioned in mind, women suffering from PCOS
are at higher risk of developing depression, anxiety, eating disorders, sexual dysfunction and often experience weight gain and obesity, hair growth and acne, diabetes, heart disease and most notably of all, menstrual irregularities and infertility. But what do we know about the potential source of the latter two symptoms?
The Government of the Menstrual Cycle
The menstrual cycle can be bro-
ken up into three main phases: the follicular phase, ovulatory and luteal, regulated by the complex interaction of, mainly pituitary, hormones. Main hormones include luteinizing (LH), follicle-stimulating (FSH) and female sex hormones: estrogen and progesterone.What on earth does this have to do with PCOS? Well, a slight imbalance in even one of these main hormones means the whole cycle can be disrupted, leading to infertility and other consequences for the body. Here is where the potential roots of PCOS take place.
Insulin Resistance and Hyperinsulinemia: the ones trying to throw a coup d’état
Regardless of weight, insulin resistance and hyperinsulinemia are prominent features among women with PCOS. Insulin resistance contributes to abnormalities in the pituitary, the production site of our menstrual cycle government and elevates the activity of hormones that convert progesterone to androsterone and eventually testosterone. In parallel, hyperinsulinemia indirectly affects the LH/ FSH ratio (an important member of our menstrual cycle government!), leading to decreased egg maturation and increased ovarian androgen production. Insulin resistance being the annoying hormonal condition that it is, is linked to adipose tissue, which in excess can create a surplus of androgens and estrogen. What seems to be the common denominator in all these attacks on the menstrual cycle government? The excess proliferation of an-
drogen, the suspect.
Suspecting Androgen
Although the true culprit or etiology of PCOS remains unknown, androgen is regarded as one of the major driving forces in the development of the signs of the disorder with 60% of patients displaying this characteristic. Surfeit production of androgens, such as testosterone can, in essence, prevent the ovaries from releasing an egg as well as enhance follicular development and dysfunctional formation of antral follicles . Such dysfunction means that the follicles mean that they are now unable to grow to a size that would be sufficient to trigger ovulation. What do all of these imbalances point towards? The overtaking of the government: menstrual irregulating, infertility, and the main form (yet not definitive) of diagnosis of PCOS: the presence of polycystic ovaries. These ovaries are enlarged and contain several fluid-filled sacs. Hence, from all the clues that have been traced since the second paragraph the Rotterdam criteria, the standardized diagnostic criteria for PCOS, can be summed in three traits: hyperandrogenism, ovulatory dysfunction and polycystic ovaries on ultrasound.
Moving past pathophysiology: Why the mystery?
At this point, it is quite safe to say that PCOS is an incredibly complicated and impactful syndrome on the quality of life of those who suffer from it. There is a myriad of journals and research articles filled with professional opinions of doctors and academics alike; however, one who ventures into the abyss of all these links would find the constant reiteration of the same words “the pathophysiology is not clear”, “the cause is unknown” … with PCOS having been discovered in 1935 the only question that remains is why? For one, there is the factor of
funding. Studies suggest that when compared to peer chronic diseases, PCOS may be relatively underfunded and unprioritized in certain healthcare systems. On the other hand, as much to do with PCOS, the discrepancies in knowledge of the condition are unclear. Is the condition just that complex as clinicians worldwide struggle or fail to formulate a diagnosis, or is there more to it? In recent years there has been a call for governments to increase their funding into PCOS, most famously in the UK with 101,910 signatures petitioning for this change and countries like the USA evaluating the need to relieve the $8 billion economic burden placed by PCOS as well as “women suffer no harmful effects from reproductive processes, and that all children have the chance to achieve their full potential for healthy and productive lives, free from disease or disability, and to ensure the health, productivity, independence, and well-being of all people through optimal rehabilitation”. Though such progress has been seen in a positive light, it is also possible to appreciate the emphasis placed not on improving the quality of life of those affected by PCOS but rather to address economics and reproduction.
Is this another gender inequality thing?
Women’s Health: Report of the Public Health Service Task Force on Women’s Health Issue was published in 1985, emphasizing how research in women’s health was imperative and how it had endangered the quality of health information available to
women and, by extension, the care received. Now, 2022 diseases of women such as pelvic-floor disorders and PCOS continue to be primarily underfunded; even with the increase seen in recent years, there has been little advance to understanding the mechanisms of these conditions. As said by Elinor Cleghorn, “the history of medicine of illness is every bit as social and cultural as it is scientific.”
It is an ‘all women’ problem
In the span of 0.44 seconds, 565,000 results show up as one enters in the Google search engine the words “PCOS celebrities”, with the likes of famous high-end personalities such as Victoria’s Beckham, actress Lea Michelle and Victoria’s Secret model Romee Strijd sharing their journeys dealing with the condition. Logically speaking, having celebrities advocate for PCOS can raise awareness and social consciousness of the syndrome’s effect. Still, narratives of weight gain and pregnancy difficulties seem to be the focal point, highlighting a very narrow demographic. In short, who else and in which manner are they being affected?
The effects of PCOS on women exceed the small boxes and clean-cut typed papers sprawled in research journals, and the impact is also social. In parts of Nigeria, prominent levels of stigma are attached to infertility, corresponding to high levels of marital problems, deprivation, violence, and neglect. Such an issue is heightened by the ongoing national crisis with non-infectious/

infectious diseases and lack of mainstream information availability about the illness, despite 13.8% to 18.1% of women in reproductive age being affected. A study with Iranian adolescents found exceedingly high-level concerns regarding their femininity and attractiveness, with similar stress levels over the future stigma of infertility being a significant source of worry in another study focusing on teens in Singapore. Similarly, in India, the perception of PCOS as a taboo disorder is widespread, with reductive discourse surrounding it because of its affiliation with infertility causing women within this context to experience feelings of seclusion and marginalization when undergoing arranged marriage pursuits. Furthermore, it may be observed how pre-existing societal pressures experienced by young teens regarding their identity and sense of societal worth are affected by this condition.
Overall, PCOS and its pathophysiology can be quite the tangled web composed of hormones, pathways, and unclear connections. However, because of the lack of information, regardless of the cause of such a situation, it is an active area of research for the betterment of the quality of lives of millions of women. Looking at the syndrome and all its
detriments to health beyond the science, it does bring into question why the main concern for so many women across the world is not only infertility but how this impediment affects their role as a female and their standing as an individual in society. Is it that we live on a planet that sees women’s worth and selfhood based on their bodies’ reproductive ability? The answer, shockingly, is unknown, but what is known is that regardless of whether the female is an average individual in Nigeria or a Victoria’s Secret model, they are both burdened by the same biological limitations of PCOS. The problem of fertility remains present—in a world of 8 billion people.
References:
(2021, 2 22). U.S Department of Health & Human Services. Retrieved from Office on Women’s Health: https:// www.womenshealth.gov/a-z-topics/ infertility
World Health Organization. (n.d.). World Health Organization. Retrieved from Health topics, Infertility: https:// www.who.int/health-topics/infertili-
ty#tab=tab_3
Teede H, Deeks A, Moran L. Polycystic ovary syndrome: a complex condition with psychological, reproductive and metabolic manifestations that impact health across the lifespan. BMC Med.2010; 8:41.
Crespo RP, Bachega TA, Mendonça BB, Gomes LG (June 2018). “An update of genetic basis of PCOS pathogenesis”. Archives of Endocrinology and Metabolism. 62 (3): 352–361. doi:10.20945/2359-3997000000049
Johns Hopkins Medicine. (2022). Health, Conditions and Diseases. Retrieved from Polycystic Ovary Syndrome: https://www.hopkinsmedicine. org/health/conditions-and-diseases/ polycystic-ovary-syndromepcos#:~:text=PCOS%20is%20a%20very%20 common,%2C%20infertility%2C%20 and%20weight%20gain.
Barbieri, MD, R. L., & Ehrmann, MD, D. A. (2022). Patient education: Polycystic ovary syndrome (PCOS) (Beyond the Basics). Wolters Kluwer UpToDate.
McLaughlin, MD, J. E. (2022). Female Reproductive Endocrinology. Retrieved from Merck Manual Professional Version: https://www.merckmanuals.com/ professional/gynecology-and-obstetrics/female-reproductive-endocrinology/female-reproductive-endocrinology
Cleveland Clinic. (2020). Controlling Your Blood Sugar Can Improve Your PCOS and Hormone Imbalance. Retrieved from healthessentials, Diabetes & Endocrinology: https://health.clevelandclinic.org/polycystic-ovary-syndrome-pill-not remedy/#: ~:text=A%20 root%20cause%20of%20PCOS, storing%20the%20glucose%20in%20cells.
Diamanti-Kandarakis E, Dunaif A (December 2012). “Insulin resistance and the polycystic ovary syndrome revisited: an update on mechanisms and implications”. Endocrine Reviews. 33 (6): 981–1030. doi:10.1210/er.20111034.
Lewandowski KC, Cajdler-Łuba A, Salata I, Bieńkiewicz M, Lewiński A (2011). “The utility of the gonadotrophin releasing hormone (GnRH) test in the diagnosis of polycystic ovary syndrome (PCOS)”. Endokrynologia
Polska. 62 (2): 120–128. PMID 21528473.
Rojas J, Chávez M, Olivar L, Rojas M, Morillo J, Mejías J, Calvo M, Bermúdez V (2014). “Polycystic ovary syndrome, insulin resistance, and obesity: navigating the pathophysiologic labyrinth”. Int J Reprod Med. 2014: 71905. doi:10.1155/2014/719050.
Ashraf, S., Nabi, M., Rasool, S.u.A. et al. Hyperandrogenism in polycystic ovarian syndrome and role of CYP gene variants: a review. Egypt J Med Hum Genet 20, 25 (2019). https://doi. org/10.1186/s43042-019-0031-4
Rodriguez Paris, V., & Bertoldo, M. J. (2019). The Mechanism of Androgen Actions in PCOS Etiology. Medical sciences (Basel, Switzerland), 7(9), 89. https://doi.org/10.3390/medsci7090089
Prizant, H., Gleicher, N., & Sen, A. (2014). Androgen actions in the ovary: balance is key. Journal of Endocrinology.
Barbieri MD, R. L., & Ehrmann MD, D. A. ( 2022). UpToDate, The University of Chicago Medical Center. Retrieved from Patient education: Polycystic ovary syndrome (PCOS) (Beyond the Basics): https://www.uptodate.com/ contents/polycystic-ovary-syndrome-pcos-beyond-the-basics#H31056296
Athanasias, D. P. (2019). What is The Difference between Ovarian Cysts and PCOS? Retrieved from London Women’s Centre: https://www. londonwomenscentre.co.uk/info/news/difference-ovarian-cysts-pcos
Williams, T., Mortada, R., & Porter, S. (2016). Diagnosis and Treatment of Polycystic Ovary Syndrome. American family physician, 94(2), 106–113.
Brakta, S., Lizneva, D., Mykhalchenko, K., Imam, A., Walker, W., Diamond, M. P., & Azziz, R. (2017). Perspectives on Polycystic Ovary Syndrome: Is Polycystic Ovary Syndrome Research Underfunded? The Journal of clinical endocrinology and metabolism, 102(12), 4421–4427. https://doi.org/10.1210/jc.2017-01415
Ismayilova, M., & Yaya, S. (2022). What can be done to improve polycystic ovary syndrome (PCOS) healthcare? Insights from semi-structured interviews with women in Canada. BMC women’s health, 22(1), 157. https://doi. org/10.1186/s12905-022-01734-w
Gibson-Helm M, Teede H, Dunaif A, Dokras A. Delayed diagnosis and a lack of information associated with dissatisfaction in women with polycystic ovary syndrome. J Clin Endocrinol Metab. 2017;102(2):604–612
Riestenberg, C., Jagasia, A., Markovic, D., Buyalos, R. P., & Azziz, R. (2022). Health Care-Related Economic Burden of Polycystic Ovary Syndrome in the United States: Pregnancy-Related and Long-Term Health Consequences. The Journal of clinical endocrinology and metabolism, 107(2), 575–585. https:// doi.org/10.1210/clinem/dgab613
Institute of Medicine. Women’s health research: progress, pitfalls, and promise. 2010. Available at: https://www.nap. edu/read/12908/chapter/1
Omagbemi, A. S., & University, B. (2022). Ovarian condition that can cause missed menstrual periods and infertility is going undetected in Nigeria. (The Coversation) Retrieved from Gavi, The Vaccine Alliance: https://www. gavi.org/vaccineswork/ovarian-condition-can-cause-missed-menstrual-periods-and-infertility-going
Saei Ghare Naz, M., Ramezani Tehrani, F., Ahmadi, F., Alavi Majd, H., & Ozgoli, G. (2019). Threats to Feminine Identity as the Main Concern of Iranian Adolescents with Polycystic Ovary Syndrome: A Qualitative Study. Journal of pediatric nursing, 49, e42–e47. https:// doi.org/10.1016/j.pedn.2019.08.010
V. Dramusic, U. Rajan, P. Chan, S. Ratnam, Y. Wong Adolescent polycystic ovary syndrome. Annals of the New York Academy of Sciences, 816 (1) (1997), pp. 194-208, 10.1111/j.17496632. 1997.tb52143
Bhavani, D. K. (2021). The PCOS discourse in India is changing, and it’s about time. Retrieved from The Hindu: https://www.thehindu.com/sci-tech/ health/pcos-awareness-month-2021-india-virtual-summit-on-stigma-wellbeing/article36222072.ece
The Calorie Counting Craze: The True Reliability of Smartwatches
By Hunter Bershtein Edited By Sophia FalkApple Watches and Fitbits: The New Health Hype

From celebrity influencers to fitness fanatics to the common college student, Apple Watches and Fitbits have become integrated into the daily lives of many. Personal fitness trackers (PFTs) are trusted to track health-related information like heart rate, step count, and energy expenditure, and tech companies promote PFTs to help people achieve their fitness goals. However, it is paramount to understand that while these devices can be helpful in monitoring exercise levels and promoting weight loss, they are not perfect. Every human body is unique, and only so much can be predicted from trivial statistics like age, height, sex, and weight. Exploring the recent research on these fitness trackers elucidates where they fall short and can better inform the public on how to best use these devices to make healthy choices. While PFTs are a helpful tool to stay on track with fitness goals for most, individuals who need very accurate measurements of vital statistics should demonstrate caution when trusting these wrist-bound devices. Experts agree that tech compa-
nies must improve the accuracy of these PFTs before fully implementing them in a clinical setting. Until then, in hospitals and sports sciences, PFTs should be used only to supplement traditional methods of vital statistics measurement, especially for people living with chronic conditions and athletes requiring precise monitoring of energy expenditure.
Heart Rate
PFTs monitor heart rate relatively accurately. A 2016 study compared PFT heart rate measurements with electrocardiograms (ECG) — a clinically accepted method to measure heart rate. Although the PFTs in this study were reasonably accurate in some cases, they proved inaccurate in others. For example, in people with sinus rhythm, ½ of PFT-measured heart rates fell within 4 bpm of the ECG-measured value, while in people with non sinus rhythm (a condition that leads to abnormal heart rate) ½ of PFT-measured heart
rates fell within 8.6 bpm of the ECG-measured value. The 2016 study also found that PFTs tend to underestimate heart rate values, particularly in the range of 75 to 150 beats per minute (bpm).
Additionally, a 2017 study comparing PFTs to ECG monitoring found that some PFTs overestimated heart rate while others underestimated this measurement. For example, the Basis Peak heart rate monitor overestimated heart rate during exercise by 8 bpm, while the fitbit underestimated the same value by 7 bpm. On top of this, two of the four personal heart rate monitors tested had suboptimal accuracy during moderate exercise. As such, while these trackers may be sufficiently accurate for daily use by most people, we must be cautious
when we consider implementing these devices in a clinical setting. This caution is especially imperative in those with abnormal heart rates and when identifying subtle psychological changes in heart rate relating to disease progression.
Sleep
In a 2019 study, wristbound devices also known as wrist actigraphy (ACT) proved somewhat inaccurate compared to polysomnographic (PSG) measures, which monitor brain waves to determine sleep. ACT sleep monitoring had lots of heterogeneity but tended to overestimate total sleep time and sleep efficiency while underestimating sleep onset latency and wake after sleep onset. These results suggest that ACT is oversensitive to sleep yet inadequate at determining when users wake up. It is also important to note that the differences between ACT and PSG were much more prominent and statistically significant in people with sleep-related disorders such as insomnia, anxiety, and depression. As such, while the common Fitbit or Apple Watch is likely fine for healthy individuals, we should exercise caution in trusting these devices for people with certain chronic psychiatric and medical conditions.
Step Count
PFTs showed mixed results in measuring step count. A 2017 study found that most PFTs were relatively accurate at recording step counts for walking but became less accurate
as speed increased. For example, the StepWatch Activity Monitor was >95% accurate at lower cadence activities but undercounted running by about 25%. Again, another 2020 study found that PFTs were relatively accurate at measuring step count for overground walking but made weaker predictions during intermittent walking and when factoring in daily activities requiring arm movement. So, while these wristbound devices are pretty good at counting steps during a typical stroll, there is definitely room for improvement.
Energy Expenditure
Energy expenditure is where PFTs lack the most. A 2019 study compared PFTs to indirect calorimetry—an accepted scientific method to estimate metabolic rate by measuring oxygen consumption and carbon dioxide production. The study found that the mean absolute percent errors (MAPEs) in energy expenditure exceeded 10% for all six tested devices, with some showing MAPEs of nearly 25%. As such, these devices cannot be relied upon by people who need to precisely track their calorie intake, especially for sports and health care.
Taking a Step Back: Making a Healthy Choice
PFTs can be a great way to increase exercise by providing a convenient means to record workouts; however, their ability to accurately measure vital health-related information has room for improvement. While these devices were better at recording heart rate and step count than sleep and energy expenditure, there was ultimately too much heterogeneity in the results to depend on these wrist-bound gadgets in situations where precise, accurate measures of vital signs and energy expenditure are required. In short, there is no problem in using an Apple Watch or Fitbit to
track a walk or lift session to stay accountable with exercise goals. However, there is a need for improvement in PFTs before they can be safely applied in clinical contexts and trusted for individuals with chronic conditions, where there is a high requirement for accuracy and precision.
References:
“Accuracy of a Wrist-Worn Wearable Device for Monitoring Heart Rates in Hospital Inpatients: A Prospective Observational Study.” Journal of Medical Internet Research, 2016. https://doi.org/10.2196/jmir.6025
“Accuracy of Wrist-Worn Heart Rate Monitors.” JAMA Cardiology, 2017. https://doi.org/10.1001/jamacardio.2016.3340
“Agreement between actigraphic and polysomnographic measures of sleep in adults with and without chronic conditions: A systematic review and meta-analysis.” Sleep Medicine Reviews, 2019. https://doi. org/10.1016/j.smrv.2019.05.001
“The accuracy of personal activity monitoring devices.” Seminars in Arthroplasty, 2019. https://doi. org/10.1053/j.sart.2017.07.006
“Validity of Consumer Activity Monitors and an Algorithm Using Smartphone Data for Measuring Steps during Different Activity Types.” International Journal of Environmental Research and Public Health, 2020. https://doi.org/10.3390/ ijerph17249314
“Validity of Wrist-Worn Activity Trackers for Estimating VO2max and Energy Expenditure.” International Journal of Environmental Research and Public Health, 2019. https://doi. org/10.3390/ijerph16173037
CULTURE
Traditional Medicine: A Way to Reimagine Modern Medicine
 By Jahnavi Muppirala
Edited By Hermela Selam
By Jahnavi Muppirala
Edited By Hermela Selam
Traditional medicine (TM) utilizes skills and practices derived from theories and beliefs indigenous to distinct cultures as tools in the prevention, diagnosis, and treatment of physical and mental illnesses. These practices incorporate plant, animal and mineral based medicines, spiritual therapies, and exercises in the treatment of disease, incorporating both medication and non-medication. The World Health Organization (WHO) has shown an increasing interest in TM, due to the global lack of access to primary healthcare (around 80% in some countries) and the dissatisfaction from side-effects of modern medicine treatments, particularly in relation to the use of chemical drugs. The most widely used TM systems include traditional Chinese medicine, Ayurvedic medicine from India, and traditional African medicine such as healing derived from the traditional values of “Botho” and “Ubuntu” in Botswana. Each of these traditional medicine systems are grounded in volumes of literature, historical records of medicinal concepts, and generational verbal teaching. Ayurvedic medicine, originating in 6000 BC, embodies a familial
and holistic approach to natural healing, directly translating to “life science.” Similarly, the incorporation of “Ubuntu” in traditional Botswana medicine prioritizes a holistic approach to health restoration considering symptoms, medication, and root causes of disease, either social or pathogenic. These social dimensions serve to avoid stigmas in medical treatment.
stances (organs, tissues), emotions, and social relationships. Books such as Huang-di Nei-jing (300-200 BC) and Shen-nongben-cao-jing (100-200 AD) describe simple medical concepts and pathways of physiological processes, the development of disease, and herbal remedies, organizing 365 medicinal herbs
Of the three major TM systems, traditional Chinese medicine (TCM) has been the most thoroughly researched, making it a promising alternative to modern medicine. TCM finds its roots in Chinese philosophy, dating back to over 3000 years. Centered around holism, TCM views the human body as an entity with its own functions influenced by the environment as well. The body is thought to be nourished by vital substances, such as Qi, which is perceived as a form of energy necessary for vitality. Analogous to a world in which components are constantly interacting in a dynamic state, good health is viewed as an internal balance between bodily sub-
into classes in accordance with their relative drug toxicity and therapeutic application. Other East Asian traditional systems such as Kampo medicine in Japan and Hanja medicine in Korea draw influence from TCM in their diagnostic and therapeutic approaches. Originally reaching the Middle East and Europe along the Silk Route, TCM spread once more to the Western world in the 17th century as trade between China and Europe surfaced. TCM has faced skepticism by mainstream medicine and has yet to be applied
CULTURE
in a Western context. However, with a recent movement towards alternative medicine, TCM has been researched out of interest in considering its role alongside mainstream medicine.
Along with many other traditional medicines, TCM finds widespread acceptance from self-reported effectiveness and therapeutic benefits. However, there is a lack of data from an evidence-based medicine (EBM) perspective which stalls the acceptance of TCM by the Western medical community. Most research has centered around TCM herbs as possible alternatives in the pursuit of pharmacological drug discovery. In particular, research has been conducted to isolate active components of herb-constituents. The two most well-known examples of clinical success have been the extraction of Artemisia annua (a TCM herb) used in artesunate to treat severe malaria and arsenic trioxide to treat acute promyelocytic leukemia.
Beginning with Artemisia annua, phytochemist Youyou Tu sought to purify and test the antimalarial agent artemisinin. Tu utilized a TCM method of high-temperature extraction to isolate artemisinin, successfully discovering the active ingredient and further removing harmful components of the herb that did not contribute to antimalarial activity. Since its successful isolation in 1972, ar-
TCM has been used in the treatment of neurodegenerative disease for more than 3000 years in Asian countries.
temisinin has become one of the leading treatments for malaria. Tingdong Zhang similarly separated the toxic and therapeutic compounds of arsenic trioxide to determine a safe dosage for intravenous delivery to maximize the effectiveness of treatment in acute promyelocytic leukemia. These two examples model the integration between modern medicine and TCM in treatment discovery. FDA clinical trials since 2011 are seeking to approve other TCM formulations, such as the Danshen dripping pill for stable angina, Kanglaite injection (coix seed oil and excipients) for cancer, and Fuzheng Huayu capsule for liver fibrosis. Apart from testing the efficacy of herbs derived from TCM, current research has shifted towards developing a neurobiological basis for the effects of TCM. Efforts have been made to determine the mechanisms underlying the effectiveness of Chinese herbal medicine (CHM) as an alternative to antidepressants. Numerous CHMs have demonstrated antidepressant-like properties, and through research, the neuroplastic mechanisms that underlie these actions have been outlined. CHMs appear to repair neuroplasticity by improving neurogenesis, synaptic spine morphology and cell signaling, glutamatergic receptor function, and neural apoptosis. Deficiency in 5 particular neurotransmitters are associated with the onset of depression: 5-hydroxytryptamine (5-HT), DA, norepinephrine (NE), acetylcholine (Ach), and GABA. Rhodiola rosea is an herb that has been found to increase 5-HT levels in Sprague-Dawley (SD) rats after 1.5, 3, and 6g/kg treatments relative to a control group. Jiao-Tai-Wan (JTW)
which is used for insomnia treatment in TCM has also been researched for its anti-depressant-like qualities. Pre-treatment with JTW (4.2 and 9.4 g/kg) in mice with lipopolysaccharide (LPS) induced depression attenuated LPS behavior and increased 5-HT and NE levels in comparison to a control group. TCM has also been used in the treatment of neurodegenerative disease for more than 3000 years in Asian countries. Its multi-target approach allows for the prevention of many complex diseases. Alzheimer’s Disease (AD) is typically characterized by dementia, aphasia, and executive dysfunction. Choline acetyltransferase (ChAT) is the key enzyme which synthesizes ACh, and acetylcholinesterase (AchE) is involved in the degradation of ACh. Normally, ChAT and AchE regulate Ach in the brain, but a decrease of Ach content is thought to be related with many clinical symptoms of AD. Typically, patients with AD require high doses of AChE inhibitors, however, this results in side effects of nausea, vomiting, and diarrhea. Further, the “single-molecule-single-target” treatment of AD has had limited success, therefore TCM may provide a new focus for AD prevention treatment and anti-AD drug development. Alkaloids are organic compounds found in plants and inhibit AchE activity. One example is Evodiamine (Evo), which when intragastrically administered to mice (100 mg/kg of Evo), showed reduced AchE activity. Further, Evo has shown anti-inflammatory properties, inhibiting glial activation and neuroinflammation
in the hippocampus which may result in typical AD side effects. One aspect for future study is the administration of TCM for AD treatment, as AD targets are distributed throughout the body. It is possible that recent nano-drug delivery systems may provide a means for TCMs to pass through the blood brain barrier (BBB) effectively. Similarly, to treat oxidative stress, mitochondrial dysfunction, and neuroinflammation in Parkinson’s Disease (PD), TCM derived compounds such as Chrysin, Cannabidiol, and β-asaron have been utilized. These TCM show antioxidative, anti-inflammatory, and analgesic properties, as well as post-transcriptional modifications at an mRNA level that need further research as they may have beneficial or detrimental effects in PD.
TM plays an ever-increasing role in the trillion-dollar global health, beauty, and pharmaceutical industries. As described, nearly 40% of pharmaceutical compositions are based on natural products originating from TM. Consequently, the industry has come to use traditional medicine as a source for bio-active agents in the preparation of syn-
thetic medicine. Often, modern medicine offers treatment divorced from the patient’s culture, family, and community, centering around the biological manifestation of the illness in comparison to its other dimensions. Consequently, many countries which face shortage of practitioners of modern medicine rely on TM which is more affordable and accessible to the wider global community. Although TCM is the most well-researched of the TM systems, there is a pressing need for more efforts to develop EBM and neurological mechanisms to validate the efficacy of other TM alternatives, showing promise of a non-invasive and comprehensive approach to disease prevention and treatment in modern medicine.
References
C.-T. Che, V. George, T.P. Ijinu, P .Pushpangadan, K. Andrae-Marobela, et al. “Traditional Medicine.” Traditional Medicine - ScienceDirect, Academic Press, 18 Nov. 2016, https://reader.elsevier.com/ reader/sd/pii/B9780128021040000020?token=4F78472EF654B2AAB 28F02D47C321F9AF59F60CCBA12DB83E2E260D4EE5E965FF5D119FB747BD426F1973749
33BE434D&originRegion=us-east-1&originCreation=20221112151337.
Traditional medicine. Traditional Medicine - an overview | ScienceDirect Topics. (n.d.). Retrieved November 27, 2022, https://www.

sciencedirect.com/topics/agricultural-and-biological-sciences/traditional-medicine
Fokunang, C N, et al. “Traditional Medicine: Past, Present and Future Research and Development Prospects and Integration in the National Health System of Cameroon.” African Journal of Traditional, Complementary, and Alternative Medicines : AJTCAM, U.S. National Library of Medicine, 2011, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3252219/#:~:text=Traditional%20medicine%20r efers%20to%20 health,illnesses%20or%20maintain%20 well%2Dbeing.
Xu, Zhiguo. “Modernization: One Step at a Time.” Nature News, Nature Publishing Group, 21 Dec. 2011, https:// www.nature.com/articles/480S90a.
Fung, F. Y., & Linn, Y. C. (2015). Developing traditional Chinese medicine in the era of evidence-based medicine: Current evidences and challenges. Evidence-based complementary and alternative medicine : eCAM. Retrieved November 27, 2022, https:// www.ncbi.nlm.nih.gov/pmc/articles/ PMC4407626/#B14
Fahim, Muhammada, Yan, Liu, Yongtao, Zhou, Hui, Yang, et al. “Antioxidative Role of Traditional Chinese Medicine in Parkinson’s Disease.” Journal of Ethnopharmacology, Elsevier, 25 Nov. 2021, https://www. sciencedirect.com/science/article/pii/ S0378874121010515.
Li, Xiaoliang, et al. “The Mechanisms of Traditional Chinese Medicine Underlying the Prevention and Treatment of Parkinson’s Disease.” Frontiers in Pharmacology, U.S. National Library of Medicine, 19 Sept. 2017, https:// www.ncbi.nlm.nih.gov/pmc/articles/ PMC5609571/.
Fang, Z., Tang, Y., Ying, J., Tang, C., & Wang, Q. (2020, August 5). Traditional Chinese medicine for anti-alzheimer’s disease: Berberine and evodi-
Aducanumab and the Accelerated Approval Program
By Julian Kage Edited By Ally WangOn June 7th, 2021, the Food and Drug Administration (FDA) announced via press release that they had approved Aducanumab, a revolutionary new drug from Biogen promising to stop cognitive decline in patients suffering from Alzheimer’s. Almost immediately, the decision was met with intense criticism from the scientific community, and three members of the advisory committee employed by the FDA to look into the efficacy of Aducanumab resigned in protest. Of the 11 members constituting the committee, which is composed of doctors from specialties related to the drug, 10 members voted against approving the medication, citing lack of evidence of the drug’s effectiveness and concern that the acceptance may spark a worrying new precedent in the world of FDA approvals.
Aducanumab, now sold under the name Aduhelm, was not approved under traditional FDA routes. Instead, it was the product of the FDA’s relatively new Accelerated Approval Program, which allows for the fast-tracked approval of drugs promising to help treat severe medical conditions that currently have little to no treatments available. The program was instituted in 1992 in response to increasing pressure

from AIDS activists in order to better combat the HIV/AIDS epidemic that was ravaging the nation. Under this new program, a drug manufacturer does not have to meet all requirements proving a novel drug’s effectiveness in a full-scale study. Importantly, the FDA does not waive these requirements, but rather approves the drug under the condition that full scale clinical trials showing the drug’s effectiveness are completed within a certain time frame, usually on the scale of years. During this time, however, the drug’s manufacturer is free to produce and sell the drug to patients. The FDA claims that Accelerated Approval does not impact the review process or how they view clinical data, but rather that it is a commitment by the agency to a shorter timeline in reviewing, prioritizing that drug’s application over others. The slew of various COVID-19 vaccines is a prime example of this. The agency rigorously reviewed clinical data and utilized external advisory committees
of some of the greatest minds in the scientific community to decide on the safety and efficacy of various vaccines. Two years later, these coronavirus vaccines are still being administered with little to no side effects reported and undisputed efficacy. When a vaccine did present potentially harmful side effects, as was the case with Johnson & Johnson’s vaccine, the FDA was quick to halt the administration of it nationwide.
Aduhelm was different. Its approval points to a deeper issue within the FDA’s Accelerated Approval Program and the power dynamic between pharmaceutical companies and the federal government. Unlike the COVID-19 vaccines and countless other drugs reviewed under the Accelerated Approval Program, in the case of Aduhelm the
FDA completely and blatantly ignored the recommendations of its advisory committee. The FDA’s approval of Aduhelm, like most Accelerated Approval Program drugs, was based on “surrogate” endpoint data: a measurement that has the potential to correlate with a real clinical result, but which is not guaranteed. Aduhelm’s endpoint data included the reduction of amyloid protein plaques on the surface of the brain, which are believed to cause cognitive decline. The relationship between amyloid plaques and cognitive decline has been mired in its own controversy as to whether it is a result or cause of cognitive decline, or if it may actually help prevent or reverse the progression of Alzheimer’s. Furthermore, the recent discovery of falsified data across some of the most influential Alzheimer’s research papers has led to increased skepticism.
Aduhelm’s approval was conditional. In its statement, the FDA acknowledged the lack of evidence showing that the drug would help patients. Now, Biogen has until 2030 to confirm the drug’s effectiveness. In the meantime, however, they have begun selling the drug at a hefty $28,200 per year (representing a 50% discount of the original price after Biogen received harsh criticism). According to the Institute for Clinical and Economic Review (ICER), Biogen’s original price tag for Aduhelm would need an 85%95% discount to meet standard
cost-effectiveness thresholds – a common metric to determine what a drug should cost, including factors such as manufacturing cost, and its effectiveness in helping patients (ICER). Biogen is taking advantage of its exclusivity in the market to generate profit from countless desperate Americans grasping at any hope to save themselves or relatives suffering from the debilitating cognitive decline of Alzheimer’s.
Aduhelm was different. Its approval points to a deeper issue within the FDA’s Accelerated Approval Program and the power dynamic between pharmaceutical companies and the federal government.
It’s easy to write this off as a one-time event, a fluke that will hopefully never happen again. However, since its enactment in 1992, ⅓ of all Accelerated Approval Program drug applications (104 of 278) have incomplete clinical trials. Of these, 70 applications were submitted after 2020. In October 2022, the FDA voted to withdraw the Accelerated Approval Program drug Makena, widely prescribed for prevention of premature births, almost a decade after its approval after its maker, Covis Pharma, failed to prove its effectiveness in subsequent clinical trials.
The Accelerated Approval Program is a necessary tool that has saved millions of Americans’ lives since its enactment. In many cases, the program has been extremely successful, but in recent years it has been taken advantage of by pharmaceutical corporations for the purpose of generating profit above all else, with Aduhelm being one of many such drugs. Biogen, the maker of Aduhelm, is currently in Phase 3 trials for another Alzheimer’s medication that they say shows promise, and which will be submitted for FDA approval in March 2023. Although analysts are debating whether their data is a “statistically
significant finding” (Bloomberg Law), they can still apply under the Accelerated Approval Program and are likely to receive approval. In its current state, the Accelerated Approval Program is failing at its goal, and the FDA is failing at standing up to large pharmaceutical companies, even going so far as to reject its own advisory committees’ findings. As Harvard Medical School Professor Dr. Aaron Kesselheim stated via Twitter after resigning from the FDA’s advisory committee over Aduhelm’s approval, “Accelerated Approval is not supposed to be the backup that you use when your clinical trial data are not good enough for regular approval” (Twitter). The FDA has instilled a dangerous precedent for future drug companies looking to quickly market their product –with potentially dangerous repercussions for patients grasping at any hope of treatment.
References:
https://icer.org/news-insights/ press-releases/in-revised-evidence-report-icer-confirms-judgment-that-evidence-is-insufficient-to-demonstratenet-health-benefit-of-aducanumab-forpatients-with-alzheimers-disease/
https://news.bloomberglaw.com/ health-law-and-business/biogens-nextalzheimer-drug-feeds-push-for-fda-approval-revamp
https://twitter.com/akesselheim/ status/1401923334347104256

INEQUITY
GeoMaps on Health and Racial Disparities
By Maryam Shariff Edited By Sanaa ImamiMore than 50% of South Side Chicago residents are forced to leave their communities in order to seek adequate healthcare (Rucker-Whitaker, 2021). Over 900,000 people make up Chicago’s South Side community, yet a majority face inadequate healthcare infrastructure and physician shortages (Rucker-Whitaker, 2021). Healthcare and racial disparities remain prevalent issues in today’s medical sphere, with Chicago serving as a prime example. The disproportionate amount of healthcare facilities and levels of access still strongly correlate to the income and insurance levels of their surrounding areas.
Although this remains a pressing issue in public health sectors, the question of how to tackle healthcare equity in terms of race still stands. While local efforts to alleviate the problem like creating tax credits and providing healthcare worker incentives have helped (Ho, 2010), a more substantial and productive approach must be taken. This can be achieved by utilizing geographical information science (GIS) visualizations to better understand small-scale public health needs and the implementation and improvement of healthcare infrastructure and quality.
Throughout the COVID-19
pandemic, researchers utilized a simple, yet effective data visualization method–the geo-map. COVID-19 outbreak statistics benefited greatly from spatial analysis and GIS to understand the pandemic. Geo-maps typically divide cases
by zip code or county level to visualize COVID-19 cases and deaths. These tools both provide data to the general public on locations of infection hotspots while simultaneously shedding light on the treatment disparities in underserved demographic groups and communities.
The use of GIS, spatial analysis, and geo-maps are not novel methods in the field of public health as organizations often produce and assess state and county-level geo-maps (Figure 1). These geo-maps utilize different social determinants of health to visually indicate barriers to healthcare. However, state and

county levels of assessment often come with limitations as levels of healthcare access vary significantly beyond these scales. The South Side of Chicago represents a key example of differences in public health characteristics from one zip code to the next. For example, Figure 2 demonstrates the significantly higher hypertension rate present within South Chicago in comparison to the North. Both North and South Chicago are placed under Cook County, however, the stark difference in healthcare statistics within the county is clear.
Chicago remains one of the most racially segregated cities in the United States due to a long and notable history of the sepa-
INEQUITY
ration of political and economic activity into geographical locations. Practices like historical redlining, contract sales, and real estate covenants continue to perpetuate racial discrimination and segregation, thus maintaining the stark racial lines between the North and South sides of Chicago. Black residents are still confined to historical lines and neighborhoods defined as “hazardous” through banks limiting access to loans (Kauffmann, 2022). Black communities still face barriers to property ownership, impeding generational wealth from remaining in “hazardous” neighborhoods (Kauffmann, 2022).
Chicago is notable not only for its racially influenced geographic division but for the stark contrast between the healthcare statistics of Black Chicagoans in comparison to the non-Black Chicagoan population. The life expectancy of a Black Chicagoan remains 9.2 years lower than the non-Black Chicagoan life expectancy of 80.6 (Duncan, 2021). Additionally, the diabetes death rate for Black Chicagoans remains 70% higher than that of non-Black Chicagoans, the homicide rate remains 9 times higher, and overwhelming
communities (Duncan, 2021).
Efforts to overcome the racial and geographical healthcare separation sprung through a multifaceted city effort, Healthy Chicago 2025, to reduce the life expectancy gap by administering aid to communities in critical need. Healthy Chicago 2025 targets hous-
public health systems. However, the Chicago Health Atlas takes a less traditional approach to tackle healthcare disparities by utilizing geo-mapping technology for public health analysis. The Chicago Health Atlas employs demographic statistics and information provided by the Chicago Health Survey to easily visualize the differences in healthcare access between the North and South regions of Chicago. The use of GIS spatial analysis provides an interactive and visual method of assessing high-risk areas in need of healthcare.

evidence points to higher occurrences of infant mortality, HIV, flu, and opioid overdose in these
ing, food access, environment, public safety, neighborhood planning, health and human services, and restructuring
Mapping indicators of health, and separating each statistic by race highlights the lower stan-
The introduction of the geo-map increased data accessibility and familiarity amongst the general population, thus paving the way for a streamlined understanding of the state of community public health.
dards of care Black Chicagoans face in comparison to their white counterparts, as well as providing insight into racial differences in healthcare treatment.
Limitations remain with researchers’ reliance on GIS and spatial visualization data to categorize complex socioeconomic situations. The first limitation lies with the differences in social determinants of health that are within a set zip code. Although zip codes are a geographically narrow and reasonable unit of analysis, dividing and characterizing public health attributes by zip code creates the assumption of equity within each region. Creating a visual tool with geographic units beyond zip code serves as a challenge since the further separation of geographic lines lacks a uniform unit for analysis. Another limitation consists of the efficiency and universality of creating similar health atlas software for other large cities in the United States. Unlike other cities, the Chicago Health Atlas collects an abundance of public health data from its Chicago Health Survey - therefore, the ability to successfully create comprehensive city-specific health surveys brings a challenge to the implementation of GIS.
Data visualization, a relatively common public health concept, serves as an essential missing step when combating healthcare and racial disparities in community areas. The geomap was effective when assessing COVID-19 spread and provided a platform to assess disparities in underserved areas and ethnic communities.
The introduction of the geo-
INEQUITY
map increased data accessibility and familiarity amongst the general population, thus paving the way for a streamlined understanding of the state of community public health. In the future, community involvement in public health affairs can extend to community-wide data collection efforts in order to aggregate public health statistics. The visualization of healthcare deserts, as well as racial disparities, serves as an important first step in combating healthcare inequity. By using GIS and geo-mapping, aid organizations, healthcare business actors, and communities have the potential to generate a better understanding of health disparities and create lasting impacts in the communities that need it most.
References:
Ahasan, Rakibul, et al. “Applications of GIS and Geospatial Analyses in COVID-19 Research: A Systematic Review.” F1000Research, F1000 Research Limited, 28 Jan. 2022, https://www.ncbi. nlm.nih.gov/pmc/articles/PMC8822139/.
Chicago Health Atlas, https://chicagohealthatlas.org/indicators/HCSHYTP?topic=hypertension-rate.
Duncan, E. Chicago Department of Public Health releases the state of Health for Blacks in Chicago, the first report of its kind focusing exclusively on the health of Black Chicagoans. City of Chicago (n.d.). Retrieved November 30, 2022, from https://www.chicago.gov/city/en/depts/ cdph/provdrs/healthy_living/news/2021/june/ chicago-department-of-public-health-releasesthe-state-of-health.html
Healthy chicago 2025. City of Chicago :: Healthy Chicago 2025. (n.d.). Retrieved November 30, 2022, from https://www.chicago.gov/city/ en/depts/cdph/provdrs/healthy_communities/ svcs/healthy-chicago-2025.html
“Heart Disease Death Rates Aged 35 and Older, Total Population.” Centers for Disease Control and Prevention, 27 Sept. 2022, https:// www.cdc.gov/dhdsp/maps/national_maps/ hd_all.htm.
Ho, K., Moy, E., & Clancy, C. M. (2010, February). Can incentives to improve quality reduce disparities? Health services research. Retrieved
Kaufmann, J. (2022, February 17). Data shows many redlining patterns in Chicago still persist. Axios. Retrieved November 30, 2022, from https://www. axios.com/local/chicago/2022/02/17/ chicago-redlining-then-and-now
Rucker-Whitaker, C. (2021, December 20). How do we close Chicago’s Health Gap? Crain’s Chicago Business. Retrieved November 30, 2022, from https://www.chicagobusiness.com/ equity/how-fix-chicagos-health-equity-problem
The Stitch that Closes Autonomy
By Michelle Mejia Edited By Rina IwataIn 2008, Angela Sanford became a mother—bringing to the world her first child. However, during the first five years since her birth, her joys as a new mother were countered by the sickening feeling that ‘something was not quite right.’

It was not until her Pap smear with Stephanie Millman, a nurse midwife, that the horrifying cause of the “excruciating pain” Sanford felt during sex was revealed. Sanford remembers how she “just started crying, saying, ‘Can you tell me what’s wrong?
Because I know something is not right’” immediately after Millman had checked on her. Her intuition was right. Sanford had received what is called the “Husband’s Stitch,” a procedure that has been practiced for many decades and continues to be performed today without the knowledge or consent of women.
What is the Husband’s Stitch?
“The husband’s stitch.” When you first hear this term, you might imagine a man sewing together a tracksuit. However, the truth of this procedure is more dire than a man learning how to sew, for the ‘tracksuit’ is the woman’s vagina. When a woman gives a vaginal birth, it is usually necessary to cut the perineum to “facilitate a smoother delivery
for the mother” (1). When the delivery is over, sutures must be performed to repair the wound. The husband’s stitch is the procedure where an Obstetrician places one or two extra sutures in a woman’s vagina after giving birth to a child. Essentially, this stitch serves no purpose to the woman and is only performed to give more sexual pleasure to the husband during intercourse. The problem is that most of the women who go through this procedure do not give consent: it is either the doctor who asks the husband for consent or the husband who asks the doctor without the consent of his wife.
This encounter itself is a violation against the autonomy of the wife, as she is significantly dehumanized.
Why The Procedure Is Not Necessary
The medical procedure of an episiotomy has existed since the 1920s. During this procedure, a surgical cut was made in the vagina to make the opening bigger for the baby to pass through. In other words, it was made to fasten the birth and prevent the perineum from rupturing by itself. It was also believed that an episiotomy would make it easier to repair the perineum (area between the anus and vulva) to make it “tighter”. This is where the “Husband’s Stitch” comes into play. However, in 2005, the Journal of the American Medical Association concluded that “Evidence does not support maternal benefits traditionally ascribed to routine episiotomy.” In 2017, Cochrane also conducted research on episiotomy and concluded that “the rationale for conducting routine episiotomies to prevent severe perineal trauma is not justified by current evidence…” and they “could not identify any benefits of routine episiotomy for the baby or the mother.” It is quite despairing that we live in a world where the medical situation of the mother does not dictate if she should receive an episiotomy or not and that it all depends on her doctor.
Hear From Her
There have been several accounts from women who have experienced this procedure. Like Sanford, they speak of how it
ETHICS
was emotionally and physically painful to experience and caused their health to decline.
Sarah Harkins, a New Orleans-based doula and lactation counselor, gave birth to her daughter in 2005. She recalls how after giving birth, the family doctor spoke to her husband and said, “Yeah, let’s go ahead and add in another stitch so we can make sure this is nice and tight.”. She says that she “was so out of it physically, emotionally, and mentally” and that the doctor asked her husband, not her, because she was “just lying there like a lump.” Harkins felt dehumanized by not being asked for consent. The family doctor had full control of the situation, and such a situation leads one to ask: why would he not place his patient first? Harkins commented:
“In the moment, I wouldn’t have used the word ‘violated’ because my brain just couldn’t process violation at the time. Now that I’ve had time to process, I have a clearer sense of what I went through and what was done to me—the injustice, to wound me in my privates, at a time when I was most vulnerable.”
the procedure. It was unfair for her to endure this during such a special time as giving birth. Her nurse midwife also expressed repugnance towards the procedure in her interview with Healthline:
“The fact that there is even a practice called the husband stitch is a perfect example of the intersection of the objectification of women’s bodies and healthcare. As much as we try to remove the sexualization of women from appropriate obstetric care, of course the patriarchy is going to find its way in there.”
The betrayal and dehumanization that have affected these women must be tremendous. As someone who is in a vulnerable position, you place your trust in a healthcare worker to help you and keep you safe. When the opposite happens, it is a very frustrating situation that nobody should endure.
“The fact that there is even a practice called the husband stitch is a perfect example of the intersection of the objectification of women’s bodies and healthcare.”
Women should not have to go through this difficult realization, especially after giving birth, a strenuous process in itself.
Similarly, Angela Sanford, now five years after her birth, realizes the horridity of her experience:
“I felt betrayed because something unnecessary was done to my body that I didn’t ask for. It was a harmful decision made without my consent. That’s not what you should get when you are in the hospital to have a baby. “
Sanford suffered the consequences of a procedure that she never consented to. It was not her fault, but even so, she still had to experience the anguish of
There are also some insights from other women on the website “On What to Expect”, which gives advice to women during the stages of pregnancy. In one of the forums called “April 2018 Babies Forum” some women shared their opinions on receiving the extra stitch.
“Oddly enough my MIL mentioned this to me (she was a L&D nurse for 30+ years, so we’re a little more open about birthing stuff together) anyways I’m having our 3rd — she said that HER doc always gave the extra stitch (without them really knowing)
she found out after the fact with her first born, from a coworker that it was a typical practice with him, she said it was in fact painful/uncomfortable for sex. She had a different doc deliver her second born and made sure not to have the extra stitch in place.... but I’m sure there are different levels of stitching and that was 35 years ago via her experience. Either way, yes I’ve heard of it, and it wasn’t a positive story.”
“I got more stitches than I needed because my tear wasn’t that bad but still needed stitches and I guess they just over estimated what was needed ... omg the pain of sex was indescribable. I waited the suggested 6 weeks postpartum but it honestly took me a good 6-8 months before I could have sex without agonizing pain. It felt like a knife ripping through my cervix. I had to do pelvic floor PT and everything. Trust your body to heal how it is supposed to.”
Both of these responses in the forum do not recommend the extra stitch and express how others and they themselves felt uncomfortable during sex after receiving this procedure. There is a clear consensus among women that this procedure is harmful. So,
why is it still being done?
The Procedure Is Still Being Done Today
The “Husband’s Stitch” is incorporated through the decision of the health provider. Women have no other option but to undergo this painful procedure since they have no choice in the matter—especially because after birth, women are exhausted and in a vulnerable position. The
National Library of Medicine researched the contribution of a provider to the risk model of performing episiotomy and concluded “The attending provider adds a significant independent effect to the episiotomy risk model,” meaning that the provider does affect the risk of a woman going through the “Husband’s Stitch.”
The most absurd part is that there is not a lot of information about the “Husband’s Stitch” on the internet. While the procedure exists, many people are not aware of it. As a result, this contributes more to the problem of allowing this procedure to exist. When searching online, it is difficult to find personal accounts from women who went through this procedure. It is quite surprising because you would think that more women would open up about their experiences. It is suspected that most women lack knowledge about the procedure and dismiss what happened to them as something normal that should happen after giving birth. This further contributes to the never ending cycle since there is little acknowledgement by the community that is being wronged by the “Husband’s Stitch.” The misinformation in the world is disheartening because it shields the fact that this procedure is indeed happening, even today.
The Last Stitch
What does it mean to be a woman? Does it mean to constantly fight against the prejudice of men? Is it to be a strong symbol for others? Is it to be caring and compassionate? Or should the question be rephrased to ask what women should not be? What should not be expected of women from men, or anyone? What should not be seen as the standard “woman”?
These questions are often brought up in today’s society when the challenges that women encounter daily are taken into account. However, most of the issues that face women, including the
“husband’s stitch”, are still left in the dark. Widespread acknowledgement and repudiation of the existence of the “Husband’s Stitch” is key in reclaiming the bodily autonomy of women.
For, a stitch cannot be undone by itself.
References:
Cromi A, Bonzini M, Uccella S, Serati M, Bogani G, Pozzo N, Ghezzi F. Provider contribution to an episiotomy risk model. J Matern Fetal Neonatal Med. 2015;28(18):2201-6. doi: 10.3109/14767058.2014.982087. Epub 2014 Nov 25. PMID: 25380033.
Hartmann K, Viswanathan M, Palmieri R, Gartlehner G, Thorp J, Lohr KN. Outcomes of Routine Episiotomy: A Systematic Review. JAMA. 2005;293(17):2141–2148. doi:10.1001/ jama.293.17.2141
Jiang H, Qian X, Carroli G, Garner P. Selective versus routine use of episiotomy for vaginal birth. Cochrane Database of Systematic Reviews 2017, Issue 2. Art. No.: CD000081. DOI: 10.1002/14651858.CD000081.pub3
Murphy, Carrie. “The Husband Stitch Isn’t Just a Horrifying Childbirth Myth.” Healthline, Healthline Media, 28 Sept. 2018, https://www.healthline. com/health-news/husband-stitch-isnot-just-myth.
Thacker SB, Banta HD. Benefits and risks of episiotomy: an interpretative review of the English language literature, 1860-1980. Obstet Gynecol Surv. 1983 Jun;38(6):322-38. PMID: 6346168.
Thacker SB, Banta HD. Benefits and risks of episiotomy: an interpretative review of the English language literature, 1860-1980. Obstet Gynecol Surv. 1983 Jun;38(6):322-38. PMID: 6346168.
“Stitches after Birth.” What to Expect, 26 Sept. 2010, https://community.whattoexpect.com/forums/march2011-babies/topic/stitches-after-birth. html.
Melatonin and Misalignment
By Miles Kaufman Edited By Taran RamchandaniIf you’ve been to Target or CVS lately, you’ve likely seen melatonin gummies up on the shelves in pretty purple bottles. These hormonal supplements have become increasingly popular, and customers’ demand for melatonin shows no signs of slowing down. There are many potential reasons for this rise in demand. Perhaps melatonin’s popularity is due to good marketing, or maybe we’re all just a little more tired than we used to be. Alternatively, falling asleep may have gotten harder as our lifestyles have become more and more misaligned with our biological clocks. Each theory likely plays a role in melatonin’s skyrocketing popularity, but I’d like to examine how the modern lifestyle is particularly misaligned with our circadian rhythms and whether melatonin supplements are an appropriate solution.
Our circadian rhythm has evolved to keep our bodies intune with the world around us. The time-keeping center of our brain uses information about how much light is present to remain synchronized with the environment. A well synchronized clock is then able to anticipate upcoming daily changes in our environment and tells the body to release certain hormones to prepare for those conditions.
Like the rest of our bodily
systems, the biological clock evolved to fit the lifestyles of our prehistoric ancestors, but modern humans have deviated from this lifestyle significantly. Most people living in today’s world experience significant circadian disruption, but by studying members of hunter-gatherer tribes, we can see what our sleep cycles might have been like before we stopped living so in-tune with our natural environments. The Hazda are a group of hunter gatherers from east Africa who live primarily outdoors. Since they depend much more on the environment, there are fewer barriers between them and the synchronization information they get from the sun. They experience less circadian misalignment as a result.
Unlike the Hazda, humans living in urbanized environments experience many factors that interfere with our biological clocks. Now that our homes are filled with incandescent light bulbs and our eyes are glued to our smartphones long after the sun has set, our internal clocks are receiving light input from
sources they were never intended to rely on. In fact cell phones emit way more blue light than are a lightbulb making nighttime smartphone usage particularly disruptive to the circadian rhythm. While staring at your phone screen late into the night may seem benign, some scientists have even classified exposure to light at night as a public health issue due to the serious health problems a misaligned circadian rhythm can cause like cancer and diabetes.
Given that the pandemic drove us indoors and drastically increased our exposure to the blue light emitted from our screens, it is no surprise that sleep quality has suffered. So how might melatonin supplements solve this problem of circadian misalignment?
Naturally occurring melatonin is produced when your

brain is not being exposed to light, and our bodies start secreting melatonin as the natural light around us starts to dim, which is typically an hour or two before bedtime. Contrary to popular belief, melatonin doesn’t actually make you sleepy, but instead binds to receptors all over the body and slows things down, preparing your body to eventually fall asleep. In our modern, artificially lit environments, we do not experience the onset of darkness at nightfall, which reduces melatonin secretion during night-time hours and hinders the body’s ability to slow down processes once it gets dark outside.
Because of this interference, many people have decided that taking supplemental melatonin before bedtime is an effective solution to compensate for the hindering effect of artificial light on melatonin production. There is plenty of evidence suggesting that melatonin supplements increase sleep quality which indicates that supplements are an effective solution to this problem.
Although taking melatonin supplements is relatively safe, melatonin is a circulating hormone that affects organs all
over the body. In fact, melatonin has noticeable effects on both appetite and seasonal affectiveness disorder that are not completely understood. It may also come as a surprise that the FDA does not regulate these hormonal supplements, and therefore dosages of these supplements are not well regulated. In fact, optimal starting doses are often a fraction of a single melatonin gummy. Additionally, melatonin may help us get to bed, but it does not realign our biological clocks with our environments, so even if one takes melatonin supplements other rhythmic hormones in their body will still be misaligned. As of today, there is no gummy you can take to mitigate the effects of artificial light exposure at night, so while melatonin may be a helpful sleep aid, it is by no means a cure for circadian misalignment.
References:
Grebow, J. Will melatonin sales continue to grow in 2021? 2021 Ingredient trends to watch for food, drinks, and dietary supplements. Nutritional Outlook. vol. 24, no. 1. Published online February 9, 2021. https://www.nutritionaloutlook.com/view/2021-ingredient-trendsto-watch-for-food-drinks-and-dietary-supplements-melatonin
Samson DR, Crittenden AN, Mabulla IA, Mabulla AZ, Nunn CL. Hadza sleep biology: Evidence for flexible sleep-wake patterns in hunter-gatherers. Am J Phys Anthropol. 2017 Mar;162(3):573-582. doi: 10.1002/ajpa.23160. Epub 2017 Jan 7. PMID: 28063234.
Touitou Y, Touitou D, Reinberg A. Disruption of adolescents’ circadian clock: The vicious circle of media use, exposure to light at night, sleep loss and risk behaviors. J Physiol Paris. 2016 Nov;110(4 Pt B):467-479. doi: 10.1016/j. jphysparis.2017.05.001. Epub 2017 May 12. PMID: 28487255.
Touitou Y, Reinberg A, Touitou D. Association between light at night, melatonin secretion, sleep deprivation, and the internal clock: Health impacts and mechanisms of circadian disruption. Life Sci. 2017 Mar 15;173:94-106. doi: 10.1016/j.lfs.2017.02.008. Epub 2017 Feb 16.
PMID: 28214594.
Martínez-de-Quel Ó, Suárez-Iglesias D, López-Flores M, Pérez CA. Physical activity, dietary habits and sleep quality before and during COVID-19 lockdown: A longitudinal study. Appetite. 2021 Mar 1;158:105019. doi: 10.1016/j.appet.2020.105019. Epub 2020 Nov 5. PMID: 33161046; PMCID: PMC8580211.
Vasey C, McBride J, Penta K. Circadian Rhythm Dysregulation and Restoration: The Role of Melatonin. Nutrients. 2021 Sep 30;13(10):3480. doi: 10.3390/nu13103480. PMID: 34684482; PMCID: PMC8538349.
Fatemeh G, Sajjad M, Niloufar R, Neda S, Leila S, Khadijeh M. Effect of melatonin supplementation on sleep quality: a systematic review and meta-analysis of randomized controlled trials. J Neurol. 2022 Jan;269(1):205216. doi: 10.1007/s00415-020-10381-w. Epub 2021 Jan 8. PMID: 33417003.
Andersen LP, Gögenur I, Rosenberg J, Reiter RJ. The Safety of Melatonin in Humans. Clin Drug Investig. 2016 Mar;36(3):169-75. doi: 10.1007/s40261015-0368-5. PMID: 26692007.
Nogueira LFR, Marqueze EC. Effects of melatonin supplementation on eating habits and appetite-regulating hormones: a systematic review of randomized controlled clinical and preclinical trials. Chronobiol Int. 2021 Aug;38(8):1089-1102. doi: 10.1080/07420528.2021.1918143. Epub 2021 May 2. PMID: 33934676.
Oren DA. Retinal melatonin and dopamine in seasonal affective disorder. J Neural Transm Gen Sect. 1991;83(12):85-95. doi: 10.1007/BF01244455.
PMID: 2018631.
On Donating Medical Technologies
By Milla Dobrovolska-Ivanova Edited By Emily ShiHospitals in the United States rely heavily on health technologies to provide patient care. Imaging technologies such as the computed tomography (CT) scan and magnetic resonance imaging (MRI) are standard, commonplace procedures used by physicians to diagnose patients and issue treatment plans. The importance of ventilators became apparent during the height of the COVID-19 pandemic when treating very ill patients. These types of technologies play a major role in both the medical systems of the United States and other high-income countries (HICs). However, hospitals in low and middle income countries (LMICs) have less access to the same types of technology. The availability of technologies in high income countries has led to a flow of donations from these coun tries to the hospitals of low-income countries. However, donations may not be the most effec tive form of increasing technological access and may indirectly worsen existing disparities. Health-related technologies

come in many forms, so it is important to make a distinction between health technology and technology for health. Technology for health relates to anything that increases the overall health of a population. It is a broad term; for example, agricultural innovations fall into this category because they can decrease malnutrition (Howitt, 2012). Health technologies, on the other hand, are specifically related to medicine. According to the WHO, health technology is “the application of organized knowledge and skills in the form of (medical) devices, medicines, vaccines, procedures, and systems developed to solve a health problem and improve quality of care and/or
High income countries have greater access to health technologies than LMICs. According to a paper by the
National Academy of Medicine, some low-income countries source 80% of their health technology entirely from donations (Compton, 2018). This disparity in access is a reason that high income countries are inclined to donate. There is an “anything is better than nothing” outlook connected to these donations (Marks, 2019); if there are LMICs that are in need of technology, some argue that it is logical to donate excess machines. However, this approach lacks a critical analysis and can have devastating consequences for the recipient country.
A vast majority of donated health technology is rendered unusable by LMIC hospitals and contributes to a buildup of waste and burden. For example, a BMJ Global Health research project found that donated medical

equipment makes up 70% of the health technology in sub-Saharan Africa, but less than 30% of the technology is functioning (Marks, 2019). The large gap between total donated technologies in relation to the number of usable donated technologies is caused by differences in infrastructure and resources.
Health technologies are almost exclusively designed in high income countries, for high income countries–they can only be successful in high income markets if they are built with the available resources in mind (Howitt, 2012). For example, consider CT scans and MRI machines, vital imaging technology. When hospitals in the United States purchase and implement newly designed, more advanced imaging technology, they often donate the older, still-functioning equipment to other countries (Daugherty, 2012). Both CT and MRI machines rely heavily on a steady flow of electricity to function. A study was conducted at the University Hospital Basel in Switzerland measured the energy consumption of 4 MRI machines and 3 CT scanners (as well as their corresponding cooling systems), and the amount of energy was found to be approximately equivalent to the energy consumed by a town of 852 people (1,107,450 kWh) (Heye, 2020). This electricity is readily available in high-income countries, but some low and middle income hospitals are located in regions where there is little, if any, access to electricity. Only around 59.1% of LMIC hospitals that provide surgical services have access to electricity, and even within
TECHNOLOGY
hospitals that do have electricity, voltage differences between countries can make equipment incompatible with electrical circuits (Marks, 2019). Technologies that function effectively in a country with a continuous flow of electricity will not succeed in an environment without consistent access to it. In compatible donations end up as waste, piling up in hospital hallways, old warehouses, and “medical equipment graveyards” (Marks, 2019).
The issues extend beyond infrastructural attributes. Low and middle income hospitals are often understaffed, and the limited healthcare professionals that they do have rarely have the training to use the donated technologies (Howitt, 2012). As stated in an article by Sally McDonald (et al.), of the University of Sydney, “Ensuring…training for healthcare workers in the use and maintenance of devices is essential prior to the donation of medical devices” (McDonald, 2019). This issue extends beyond the lack of training
equipments’ instructions. Without proper training and access to legible instruction manuals, let alone enough medical personnel, technology is useless.

It’s important to note that the characteristics of low and middle-income countries are not the only factors that lead to donations becoming waste. Donor countries must donate in a careful and ethical manner. According to a study conducted by the Catholic Health Association, where a number of donor hospitals were surveyed, “60% of donors were providing broken equipment, the sorting and disposal of which consumed valuable staff time at recipient hospitals” (Marks, 2019). This is due to difficulties and pileups of unsorted donation materials, which can also lead to the donation of expired materials guaranteed to end up as waste (CHA, 2011).
for medical workers. If a different language is spoken in the recipient country than the donating country, there will be a language barrier with regards to the
The majority of medical donations are sent out of good will, but certain donors lack good intentions altogether. Some hospitals donate loads of barely-functioning equipment as a way to “dump” technology that is considered “obsolete” for their hospitals. Some pharmaceutical organizations may receive tax breaks from donations that “fulfill corporate social responsibility targets”, whereas they would have to pay to dispose of excess materials (McDonald, 2019). Even donations sent in emergency situations out of good
will can have drawbacks. There is great difficulty regulating huge influxes of materials and distributing them properly once they have been delivered to the target nation.

After considering all of the ways in which health technologies contribute to the buildup of waste, it seems easy to believe that there are no benefits to the practice. However, if properly executed, health technology donation can decrease healthcare disparities. There are a number of existing universal guidelines with the sole purpose of increasing the efficacy of donation, and many countries have their own well-established policies.
The World Health Organization established four primary principles for all nations to follow when conducting medical donations. First, the recipient should be benefited to the greatest extent. The donating hospital or organization needs to ensure that the receiving hospitals are

truly benefitting from their donation. Secondly, the recipient’s wishes must be at the forefront of the conversation. Third, there should not be double standards associated with the quality of the donation. The same standards of quality apply to technology in the donor nation as the receiving nation. Finally, the donor and recipient should be in communication throughout the entire process, and effectively plan the donation of the goods (WHO, 2010).
Marks explores the importance of guidelines for donation in great detail. To begin, collaboration is of the utmost importance.
hospitals
“create a list of their prioritized equipment needs, including model specifications, spare parts and training require ments”, then the donating country has the responsibility to conduct a needs assessment (Marks, 2019). This ensures that the donated technology will truly
benefit the recipient hospitals. After the donations reach their destination, Marks emphasizes that a long-term relationship must be established between the donor and recipient. This will create an avenue for communication between the countries–donors can follow up on donations and send more products in the future.
Donating countries also have a responsibility to consider the economic implications of their
country is in need of a lot of wheelchairs at a certain time, international donors can supply a large amount that will meet the current need and also last for a long period of time. Consequently, the local business will suffer economically–their market will cease to exist. However, after the donated supply runs out, the local hospital will not be able to continue providing wheelchairs to patients because the local producer is out of business. This idea becomes even more important if the goal is to focus on the longterm; once donating nations stop sending technology, there needs to be an internal market for the recipient country to have access to the equipment that they have become reliant on.
Medical donations can be quite beneficial for both donor and recipient countries if the proper guidelines are followed. But perhaps there is a way to circumvent the need to adhere to strict donation guidelines with ample room for error. The Imperial College London introduces the idea of “frugal technology”. Frugal health technology is specifically designed to be sustainably used and readily available in LMICs (Howitt, 2012). Collaborating with local users to design technology using locally available resources may be a more sustainable way to improve global health than donating technologies designed specifically for high income countries. Furthermore, international partnerships need not be abandoned in this method: “One study suggests that the greatest drivers of development of frugal technology will be the multinational corporations with
TECHNOLOGY
operations in emerging markets such as India and China” (Howitt, 2012). Frugal technologies have already been implemented in some countries with great success. “The Jaipur foot is a form of prosthetic that is designed locally, affordably, and quickly, which has been implemented in 22 countries across Asia, Africa and South America” (Marks, 2019).
Improperly managed donations can have severe negative effects on lower and middle income health systems, contributing to an increase in waste and burden for recipient hospitals. However, if managed properly, they can be useful. The guidelines issued by the individual countries and the World Health Organization must be followed, with an emphasis on collaboration and longterm relationships. The primary way to improve donation quality and efficacy is to study failed donations and learn what methods do not work. This will allow future donations to be managed in a proper, more effective way. And perhaps donations do not have to be the only way to decrease the disparities in access to health technologies. In this increasingly globalizing world, designing technology specifically for low and middle income countries, with their available resources and needs in consideration, may begin to replace the need for donating medical technology altogether.
References:
Howitt, P., et al. “Technologies for Global Health”. Imperial College London, The Lancet, 2012. https://www.thelancet.com/action/showPdf?pii=S0140-6736%2812%2961127-1
Daugherty, J. “5 Tips for Donating Used Diagnostic Imaging Equipment”. Diagnostic Imaging, 2012. https://www.diagnosticimaging. com/view/5-tips-donating-used-diagnostic-imaging-equipment
McDonald, S., et al. “Medical donations are not always free: an assessment of compliance
Marks, I., et al. “Medical equipment donation in low-resource settings: a review of the literature and guidelines for surgery and anaesthesia in low-income and middle-income countries”. BMJ Global Health, National Library of Medicine, National Institute of Health, 2019. https://www.ncbi.nlm.nih.gov/ pmc/articles/PMC6768372/
“Guidelines for Medical Donations”. World Health Organization. 2010. https://www.who.int/publications/i/ item/9789241501989
UChicago Feature: Dr. Kratsios
 By Staci Konow
Edited By Michelle Lu
By Staci Konow
Edited By Michelle Lu
At the University of Chicago, we are constantly surrounded by labs conducting groundbreaking research every day. Whether it’s physicians at UC Medicine developing life-saving COVID treatments or professors discovering how to bring multiple molecules into the same quantum state, we are at the epicenter of innovative research across all disciplines. As a neuroscience major, I wanted to learn more about the research being done on campus regarding the nervous system. I had the pleasure of speaking with Dr. Paschalis Kratsios, assistant professor of Neurobiology here on campus. His research focuses on a specialized population of cells - called motor neurons. Motor neurons are essential for voluntary and involuntary movement and the Kratsios lab studies the molecular mechanisms that underlie the development and degeneration of these cells.
He started his academic career in Greece and Italy, earning his PhD in Developmental Biology from the European Molecular Biology Laboratory in 2009. He completed his postdoctoral training at Columbia University in 2016 and was faced with deciding where to take his next steps.
“I wanted to stay in academia,” he said, “and advance knowledge, [while] at the same time trying to help people with motor neuron
diseases. That is what drives me.” He applied to several universities across the world and ultimately decided to come to the University of Chicago. “I was attracted to the University of Chicago mainly because of the faculty I interacted with and the students here…I think that was the main point of coming here: to join a collaborative environment that provides expertise different from my own.”
Today, his research centers around motor neurons and circuits. His lab is unique in that they use two model organisms: the nematode C. elegans and mice. “There are very few labs in the world that use two different model organisms,” Dr. Kratsios says. “I would say that [using two model organisms] is very difficult to do and something I struggled with when I came here…but with time, we learnt to coordinate things.” Having access to the two systems allows him and his team to study neurons across systems. In C. elegans, for example, they are able to easily pinpoint specific neurons and their molecular mechanisms since the nematode only has 302 neurons and is a very well studied system. In many cases, those molecular mechanisms are
conserved in mice, so once they are identified in C. elegans, they can be further investigated in a more advanced nervous system. Though his research stays mostly in those two systems, he has not lost sight of his original passion. “A lab at the University of Massachusetts help[ed] us obtain access to motor neurons from ALS patients…we did this experiment where…we modified the expression of the protein eIF2D, a protein we had discovered in a C. elegans model of ALS.” They saw that eIF2D had the same protective effect in those patients’ neurons as they did in C. elegans. “That really taught me how powerful simple model organisms can be to discover mechanisms that are potentially of therapeutic value,” he said of the results.
Q: What is the most important question in neuroscience?
“In my mind, I find neurons to be incredibly resilient cells. The majority of them do not regenerate. They are post-mitotic
cells that do not produce progeny and stay with us for decades, some our whole lives. So for me, the most fascinating question is how do these [long-lived] cells… maintain their functionality throughout decades of life in humans? If we understand this question, then we will be able to understand what goes wrong when neurons degenerate in adults or go wrong because of disease. So I think there is a connection there that we are missing the link between sustained neuronal function for decades of life and what is the trigger for neuronal dysfunction and ultimately degeneration and disease.”
Q: What are you planning to do moving forward? In an ideal world with no restrictions, what sort of research projects would you want to pursue?

“In an ideal world, I would like to continue training the next generations of scientists. As I said, people are the most important resource [in] a research lab… but at the same time one way to make a lasting contribution for 50 of even 100 years from now is to make sure that we train the next generation of scientists and give them the values we aspire to today–to be creative in research, be ethically responsible in research, be professional and kind–all the basic fundamental things. So I would like to
keep training people and expand my lab…Right now, being at the University of Chicago, I am only working with undergrads, grad students, and post-docs, but I think that science education should start earlier. so we are currently organizing outreach programs at public high schools here in Chicago. The idea is that we would go into the classrooms and talk to students about neuroscience and our research, explaining with simple model organisms and organizing field trips to the lab. Hopefully, some of them will apply for one of the summer fellowships here that we have for high school students.”
ETHICS
The Ethics of CRISPR
 By Emnet Djibrila
Edited By Rahul Burra
By Emnet Djibrila
Edited By Rahul Burra
Intro
With every medical advancement there are always a slew of ethical questions that arise. These questions cause people to contemplate whether the application of the innovation stands with the values that society holds. These same questions surround potential new treatments involving gene editing that could possibly change the way that people prepare for parenthood. In Vitro Fertilization (IVF) has been used for over four decades, and attempting to directly modify the genome of an embryo in vitro before implantation is the next step for geneticists and researchers. With the increasing advent of the use of a technology called CRISPR, in genetics research, the sky seems to be the limit in regards to the selection and removal of certain genes in an unborn child. Currently, many prospective parents opt to receive genetic counseling and genetic testing in order to ensure that they don’t pass down any hereditary conditions. With the new technology, parents who are carriers for certain genetic diseases, or risk factors may be able to prevent their children from expressing said disease genes. However, many argue that changing the genomic sequence of a human embryo creates many further ethical issues.
Background on CRISPR
The use of Clustered Reg-
ularly Interspaced Short Palindromic Repeat (CRISPR) has represented a game changing genome editing technology. CRISPR has advanced research, allowing for efficient alterations in genes through “knocking out” (removing a gene from within the cells of an organism) or “knocking in” genes (introducing a novel gene in the genome of cells). CRISPR works by cutting DNA in very specific places, allowing for desired modifications to occur, and letting the repair processes of the DNA kick in. The CRISPR process consists of two main parts, the Cas9 or Cas13 protein that cuts the DNA, and a guide RNA that is bound to the protein and lets the Cas9 know where to cut. Scientists are able to exploit this process and add changes to genomes because once a cut is made the original sequence can be modified through deletions/insertions of base pairs or be left inactive. With this technology geneticists are able to create modifications in models of cells, and use
these models to do research in many different fields. Anything from modifying crops, to altering diseases could technically be possible with this technology. For family planning, CRISPR could potentially be used to alter traits in an embryo. Potential parents could alter traits that relate to the overall health of the child, like genes that carry alleles associated with genetic diseases.
Introduction to Ethical Questions
With the introduction of this technology, many questions begin to arise about the ethicality of these genetic modifications. Although many have the intention of using this technology to reduce the probability of passing down genetic disease, questions about the ethics of making changes to a genome purely for aesthetic
purposes have, in particular, come up (these changes to genes led to the coining of the term “designer baby”). There are many different arguments both for and against the use of CRISPR to create designer babies, but the two most prominent seem to be the principle of beneficence and the principle of nonmaleficence. The principle of beneficence is the notion that people’s actions should prevent harm whenever possible. The principle of nonmaleficence states that we should be minimizing the harm that we inflict on others. These principles can both be traced back to Hippocrates. Although the two sound extremely similar in what they are arguing, these principles could not be more different when applied to the concept of designer babies.
The Principle of Beneficence
Many who argue that designing babies is ethical tend to argue along the lines of the principle of beneficence. Utilizing CRISPR in the family planning process could potentially benefit a child in the long run. Indeed, many of the applications involving family planning and CRISPR are directly related to improving the overall quality of life. Many prospective parents utilize reproductive technologies in order to remove genes that carry hereditary disorders (ex. BRCA mutation, Cystic fibrosis, Huntington’s disease), lower the risk for diseases like Alzheimer’s and cancers,and screen for other complex diseases like Type 2 diabetes. The use of CRISPR could
ETHICS
also potentially increase life expectancy because the removal of less advantageous genes has the promise of greatly improving quality of life and leading to a healthier upbringing. According to the principle of beneficence, researchers should be doing everything possible to get this technology out to the public as a promising means of addressing increasing rates of diseases like Alzheimer’s, diabetes, and cancer and allowing people to live longer lives.
The Principle of Nonmaleficence
On the other hand, others will argue that no matter what the intention is behind wanting a designer baby, the process will do more harm than good. The technology being used is still relatively new, with the first IVF baby being born in 1978 and the first CRISPR-edited babies being born in 2018. While utilizing this technology in different animal and plant models (e.g. In laboratory mice) has been used for upwards of a decade, and is a staple in modern biological research, use in humans remains widely untested. The CRISPR-edited babies born in 2018 were indeed a result of an illegal procedure conducted by a doctor attempting to replicate a gene that reduces risk for HIV. Use of CRISPR in human embryos has still not been approved across the globe. Not only is the acute procedure of genetically modifying a human embryo with CRISPR relatively untested, there is even less conclusive data about the long term effects of employing the technology in human embryos. There is no way yet to know with certainty what the toll these modifications have on the body may ultimately be.
Closing
In addition to the ethical issues raised above, questions have also been raised
about if the use of this technology would make the overall human gene pool too homogenous, or if the desire for the perfect designer baby may be rooted in ableism. Taking into account the novelty of the technology, the main debate lies in whether or not it is ethical to give traits that are perceived to be desirable to babies in vitro. But who’s to say what is desirable? And what is our definition of desirable rooted in? The question of where we draw the line with this technology still remains ambiguous.
References:
https://www.yourgenome.org/facts/ what-is-crispr-cas9/
https://www.broadinstitute.org/ what-broad/areas-focus/project-spotlight/questions-and-answers-aboutcrispr
https://www.cancer.gov/newsevents/cancer-currents-blog/2020/crispr-cancer-research-treatment
https://sitn.hms.harvard.edu/ flash/2014/crispr-a-game-changing-genetic-engineering-technique/ https://law.stanford.
edu/2021/04/21/stanfords-hank-greelyon-crispr-people-and-designer-babies/ https://sites.lib.jmu.edu/elsi-biotech/reproductive-biotechnology/ ivf-and-designer-babies/
https://theconversation.com/thosedesigner-babies-everyone-is-freaking-out-about-its-not-likely-to-happen-103079
https://www.ncbi.nlm.nih.gov/pmc/ articles/PMC6434648/
https://explorebiotech.com/ pros-cons-designer-baby/
https://www.ncbi.nlm.nih.gov/pmc/ articles/PMC7129066/
https://crisprtx.com/gene-editing/ crispr-cas9
https://www.pewresearch.org/facttank/2018/07/17/a-third-of-u-s-adultssay-they-have-used-fertility-treatmentsor-know-someone-who-has/
https://embryo.asu.edu/pages/ethics-designer-babies
Language Barriers In Healthcare
By Shaherzad Chawdree Edited By Eva McCordIn the modern medical landscape, it is often assumed by patients that individual choices alone control one’s health; in other words, through exercising, eating healthy food, and going for regular checkups, one should be able to maintain a healthy lifestyle. However, this assumption in practice fails to hold up in the face of numerous social determinants, preventing certain groups from having access to healthy choices.
To turn to an example closest to home, these social determinants can be seen in Chicago, where life expectancies differ greatly from neighborhood to neighborhood. According to the NYU School of Medicine, there is a 30 year difference in life expectancy between Streeterville, a North Side neighborhood, and Englewood, a South Side neighborhood. These stark differences in health outcomes present in our city’s communities cannot be ignored, especially by those who work in healthcare.
According to the NIH, individuals who are affected by this are often minorities such as immigrants, refugees, and racial or ethnic minority groups. Beyond present so cio-economic disparities, these health inequalities can frequently be
traced back to language barriers between patients and healthcare providers. Patients of different ethnic and racial groups are discriminated against or cannot be understood because of their accents, vernaculars, or limited English proficiency (AAAL). The American healthcare system discriminates against these patients, preventing them from accessing the care they need.
Limited English Proficiency (LEP)

According to the U.S. Census, apmately one in five speak another language at home, with the most common being Spanish, Chinese, French, Tagalog, and Vietnamese. Among this population, more than 25 million were reported to have LEP. This means that they would have difficulty writing, speaking, or understanding English. Despite the growing LEP population, there are still major communication

barriers in healthcare. A 2019 study conducted by researchers Lisa Diamond, Karen Izquierdo, etc. investigated the quality of care LEP patients received in American hospitals. From their research, it was determined that clinicians are only required to be trained in English, excluding basic training in Spanish or other commonly spoken languages in local communities. This lack of available means of communication has led to decreased access to preventative screenings, reduced access to health information, and worse outcomes.
In contrast, studies with clinicians that speak the same native language have shown increased patient understanding, satisfaction, and better process measure values like blood pressure and LDL (Diamond, et al).
However, despite the advantages of having language-concordant care, U.S. public health

policies fail to create an equitable space for patients. Title VI of the Civil Rights Act of 1964 requires institutions that receive Federal financial assistance to make their programs and services accessible to those with limited English proficiency; however, it was unclear how the policy would implement this. In 2000, the U.S. Department of Health and Human Services Office of Minority Health took it upon themselves to create the National CLAS standard to further define what hospitals should do. CLAS—the Culturally and Linguistically Appropriate Services—requires hospitals to have language-appropriate care with qualified bilingual providers and language assistance. However, it was reported in the Medical Care Journal that the majority of hospitals do not provide vital documents in non-English language, and they mainly inform their patients in English that they have the right to receive care in their own language. The standards also explicitly discourage the use of untrained individuals and minors as interpreters, yet this continues to remain the most common way of communication for many patients. Even after the implementation of CLAS, only 13% of hospitals met all of the CLAS standards and 19% met none (Diamond, et al).
If hospitals want to adhere to CLAS guidelines and prevent language barriers from obstructing care, clinicians must be trained to serve as bilingual providers. To implement this, the medical educational system should have a standardized way of educating their clinicians
rather than loosely offering language courses that lack structure. According to a 2021 study conducted by the Journal of General Internal Medicine, 78% of the 158 medical schools 158 studied offered medical Spanish; however, only 21% met all basic standards. These basic standards were defined as having a formal curriculum, a language department faculty, post-course assignments, and giving educational credit for classes. If an incentive for credit is not given to students, it is clear that the medical educational system is putting little effort in outputting qualified bilingual providers into the health care system. Formalizing language education and training clinical language interpreters would be key in bridging the gap in communication. If action is not taken place, LEP populations will continue to suffer.
References:
Diamond, Lisa et al. “A Systematic Review of the Impact of Patient-Physician Non-English Language Concordance on Quality of Care and Outcomes.” Journal of general internal medicine vol. 34,8 (2019): 1591-1606. doi:10.1007/s11606019-04847-5
Diamond, Lisa C. MD, MPH*; Wilson-Stronks, Amy MPP†; Jacobs, Elizabeth A. MD, MPP‡. Do Hospitals Measure up to the National Culturally and Linguistically Appropriate Services Standards?. Medical Care: December 2010 - Volume 48 - Issue 12 - p 1080-1087 doi: 10.1097/MLR.0b013e3181f380bc
“LANGUAGE SPOKEN AT HOME BY ABILITY TO SPEAK ENGLISH FOR THE POPULATION 5 YEARS AND OVER.” 2021: ACS 1-Year Estimates Detailed Tables, United States Census Bureau, 2021, https://data.census. gov/table?q=B16001+&tid=ACSDT1Y2021. B16001.
Martinez, Elizabeth M et al. “Improving Equity of Care for Patients with Limited English Proficiency Using Quality Improvement Methodology.” Pediatric quality & safety vol. 6,6 e486. 15 Dec. 2021, doi:10.1097/ pq9.0000000000000486
“Minority Health & Health Disparities.” National Institute of Health, U.S. Department of Health and Human Services, https://www.niaid.nih.gov/ research/minority-health-disparities#:~:text=NIH%2Ddesignated%20U.S.%20 health%20disparity,populations%2C%20 and%20underserved%20rural%20populations.
Ortega, Pilar, et al. “Medical Spanish in US Medical Schools: A National Survey to Examine Existing Programs.” National Library of Medicine, Journal of General Internal Medicine, 29 Mar. 2021, https://link.springer.com/article/10.1007/s11606-021-06735-3.
Schencker, Lisa. “Chicago’s Lifespan Gap: Streeterville Residents Live to 90. Englewood Residents Die at 60. Study Finds It’s the Largest Divide in the U.S.” Chicago Tribune, 6 June 2019, https:// www.chicagotribune.com/business/ctbiz-chicago-has-largest-life-expectancygap-between-neighborhoods-20190605story.html.
Should the United Kingdom privatize its healthcare systems?
 By Neeharika Venuturupalli
Edited By Rachel Zhang
By Neeharika Venuturupalli
Edited By Rachel Zhang
Many in the United States (US) criticize the American healthcare system for its high expenses and unequal distribution. Nevertheless, this privatized model serves as an inspiration to healthcare systems all around the world, from the Philippines, Argentina, Columbia, Vietnam, Zimbabwe, India, Pakistan, to the United Kingdom (UK). When considering the UK in particular, their healthcare system is well-known for the equitable distribution of healthcare under the National Health Service (NHS). To provide some further background, the NHS is both publicly funded and publicly operated; it is the healthcare system which serves the four countries of the UK—England, Scotland, Wales, and Northern Ireland. The NHS is one of the world’s largest public healthcare systems and has been operating for nearly 75 years. With the exception of particular dental procedures or occasional prescriptions, the NHS is lauded for providing free healthcare services with its main source of funding being taxes. The perks of the NHS seem almost perfect— free and straightforward services,
mostly free treatments, and equally accessible centers—so why are there governing parties in the UK who wish to privatize the NHS?
For the 70th-year anniversary of the NHS, the British Broadcasting Channel (BBC) released an insightful report entitled How good is the NHS. Some of the key critiques from this assessment include substandard outcomes (when compared to other health systems in developed countries) and exceedingly long wait times for treatment. According to the BBC report, healthcare treatment, assessed by probability of death, from the NHS scores ‘worse than the average in…eight out of the 12 most common causes of death’. The NHS also ranked sixteenth for amenable mortality out of
the 18 developed countries it was compared to.
One of the biggest problems of the NHS is the long wait times. Many consumers of the NHS seem to share the similar experience of calling clinics at 8 AM, being placed on hold, and learning that the appointments for the day have been booked. It has even been expressed that finding an appointment slot is like winning the lottery—uncommon, yet people keep trying. Niki Downs, a lifelong advocate for the NHS and British resident, spoke on wait times for treatment within the NHS. Given her circumstances, Niki would be required to
wait for over a year to receive a life-saving surgical procedure. Due to this wait period, she turned towards private consultants and paid £8,000 to get her procedure done within a few months. However, it is notable that if she had chosen to wait for her procedure to be done under the NHS, she would have received treatment free of charge.
The NHS is also scrutinized for being a “bottomless pit” in the sense that the government continues to pour money into it, yet the money never seems to be enough to fix its key problems. Many who support privatizing the NHS find that it would help solve the “bottomless pit” problem, as the government would not have to continue funneling large sums of tax funds into a system that seems to demand for even more money every year. It is believed that the market would be a better regulator of money in healthcare. Theoretically, medicines in greater demand would see greater production and, as a result, a lower cost. The money to fund these medicines would also not be burdened on the government, thereby allowing

remaining publicly operated health services. However, the King’s Fund analysis reveals that, in comparison to other similarly developed countries, the UK spends an overall lower amount of money on healthcare, despite the recent increases. For the past decade, the UK has spent nearly 10% of its GDP on healthcare with little increase during this time. Other countries with large public healthcare systems, such as France and Germany, spend nearly 12% of their GDP or even higher on healthcare. An increase in the NHS budget to match that of other similar countries could greatly resolve the major issues of the NHS. Yet, members of the British conservative party continue to advocate for privatization as they believe it would be a more efficient way to provide healthcare services.
Many members of the party look towards the US as an example of a successfully privatized health system.
In order to best understand the potential implications of privatization in the UK, it is helpful to consider the benefits and drawbacks of the US’ privatized system. Individuals
primarily access the American healthcare system through insurance. Insurance can either be public or private, although there are restrictions on who can access the publicly funded insurance. Privatized insurance companies have different prices, benefits, and coverages. With all of these attributes, the costs and benefits of health insurance widely differ between person to person. Most employees and their dependents are provided health insurance by the employee’s company. Other groups (including elderly, disabled and/ or low-income) receive social services to help them with basic healthcare coverage. Despite having health insurance, many individuals still end up paying thousands of dollars for out-ofpocket services every year.
Privatization allows and encourages advancements through competition. Hospitals often compete with one another for the best technology, service, and professionals. American hospitals are known for having access to some of the most highly advanced medical technologies in the world; however, access to these hospitals is very limited

and expensive. Privatization also allows consumers to pay for better service, including decreased wait times. On average, wait times are much lower in the US than in other countries, however this service comes at a higher cost. The average wait time in an American emergency room is about 58 minutes whereas it’s at least 3 hours in the UK. Nevertheless, this wait time is often only applicable to those who are insured. American doctors are also some of the highest paid in the world with the average yearly salary being around $160,000 per year. For reference, the global average is around $85,000, and the UK average is around $115,000. Because the healthcare industry in the US is privatized, physician salaries are influenced by the market and healthcare demands. While the American healthcare system is characterized by some of the best technology, service, and professionals, it is also known to be largely inaccessible to most of the general public.
Privatizing the NHS will bring up the question of how to pay for healthcare services. This will most likely result in the creation of private insurance companies in order for individuals to afford these services. A good insurance plan is one in which these three characteristics are met: (1) it is widely used, (2) the insurance provider must not have access to the pre-existing conditions of its clients, and (3) people must not be able to choose which insurance they want. The more people covered by an insurance plan, the better the predictability of mean expenditure. Insurance coverage
also works best when it’s randomized from both ends—when providers can’t choose who they cover and individuals can’t choose the provider. Randomization is crucial when creating an insurance plan, because it keeps the insurance companies accountable for the services they’re providing while allowing them to get enough people to effectively insure them. When providers start to restrict who they cover based on pre-existing conditions, the only people insured end up being those who statistically need it the least. While it is possible for the UK to set up effective insurance companies, the process of creating these plans may take a long time. This would leave millions of British residents unable to properly pay for healthcare until insurance plans are stabilized.
While privatization in the UK has the potential to increase the quality of technology, services, and doctors, this would only be available for those who can afford it. Privatization allows healthcare to be for profit, which does not inherently keep in mind the interests of the people. Therefore, for the many people who cannot afford quality services and good insurance, they could be left with even worse health systems than before. Thus, in order to reform the NHS, it is important to allocate adequate funds to increase quality and work on better incentivizing healthcare workers to increase staff and thus decrease wait times.
References
Ward, Deborah, et al. “The NHS at 70: How Good Is the NHS?” The King’s Fund, The King’s Fund, 25 June 2018, www.kingsfund.org.uk/ publications/nhs-70-how-good-is-the-nhs.
Strick, Katie. “NHS in Crisis: Is the UK Sleepwalking into Privatisation?” Evening Standard, Evening Standard, 30 Aug. 2022, www. standard.co.uk/insider/britain-private-health-
care-boom-nhs-two-tier-system-privatisation-uk-b1017504.html.
Wickens, Charlotte. “Health and Social Care in England: Tackling the Myths.” The King’s Fund, The King’s Fund, 3 Aug. 2022, www.kingsfund.org. uk/publications/health-and-social-careengland-myths.
“Healthcare Expenditure Statistics.” Statistics Explained, Eurostat Statistics Explained, Dec. 2021, ec.europa.eu/ eurostat/statistics-explained/index. php?title=Healthcare_expenditure_statistics#:~:text=Current%20healthcare%20expenditure%20in%20Germany%20and%20France%20was%20 equivalent%20to,Member%20State%20 %E2%80%94%20see%20Table%201.
