




4. Introduction
UEA Pro-Vice Chancellor Professor Charles ffrench-Constant
6. Our Year in Review
We look back on the successes of both UEA Health and Social Care Partners and our partners
11. Fuelling Breakthroughs
Learn more on the six funded projects from our 2023/24 UEA Health and Social Care Partners Research Capacity Building Funding Call
12. CELDA
Care Experience Improvements for People with Learning Disability and/or Autism
13. FACES
Impaired Facial Emotion Communication in Parkinson’s Disease
14. PARROT
Polypharmacy Assessment, Review, and Rationalization for Optimal Treatment
15. RESULTS
Access to Results: Acceptability of immediate access to test results via a hospital patient portal
16. RIPPLE
Improving Climate Psychological Preparedness for Coastal Communities
17. WEIGHT
Observational Study Exploring the Timing of Postnatal Neonate Weight Measurements
18. Scholarships
Learn more about the seven funded Scholarship projects from our 2023/24 UEA Health and Social Care Partners Scholarship Programme
19. Review of Research Policy Linked to NMAHP-Led Research
20. Worldwide Cataract Surgery Rates
21. Physical Activity (PA) for Hospitalised Stroke Patients
22. Developing the Pilot NMAHP
Embedded Researcher Role
23. Paediatric Genomic Research and Testing Engagement in Community Paediatrics and Underserved Communities
24. Local Enablers and Barriers to NMAHPs Completing Research-Based Awards
25. The 7-Day Decision Point Model for Multidisciplinary Teams Supporting Patients with Femoral Fracture
27. Impact Case Studies
Read about the Impact Case Studies from previous UEA Health and Social Care Partnership-funded projects
28. The Better Sleep Programme
A six-month scoping exercise to develop a business case and plan of work for a wider project
33. Point-of-Care 3D Medical Printing
3D printing has revolutionised many industrial sectors, improving productivity and creating products that were not possible using traditional manufacturing methods
37. PPI & Scoping Review for GP at Front Door of Accident & Emergency Services
GP at Door of A&E services are now 16 routinely deployed in our acute hospitals across Norfolk and Waveney
44. Technology to Support Change
The TOSCA project ran a series of focus groups to understand the views of young people with complications of obesity around using technology to support their journey within the Complications from Excess Weight (CEW service)
51. Brain Injury Discharge Information Project
The project aims to quickly develop an online patient-facing portal that will provide personalised gold-standard information about recovery following mild traumatic brain injury
55. Co-production of promising interventions to support multiple behaviour change in socially deprived communities
CHARMING is a project to co-produce interventions supporting multiple behaviour change in socially deprived communities
62. mHealth for patients with Peripheral Arterial Disease
‘Walk-A-Cise’ seeks to develop and implement a new mobile app aiming to improve the health of patients with Peripheral Arterial Disease (PAD)
69. Assessing the Social Needs and Wellbeing of Young People with PreExisting Mental Health needs postCOVID-19
ANSWERS will see researchers work with young people to better understand how they have been affected by the pandemic
79. Care Experience Improvements for People with Learning Disability and/or Autism
CELDA aims to enhance the quality of care for individuals with learning disabilities and autism
88. Our Partners and Associate Partners
As we present this UEA Health and Social Care Partners Impact Case Report to our esteemed members of the management and executive boards, it is essential to underscore the critical importance of health and social care in the East Anglian and North East Essex regions.
Over the last five years, the landscape of our healthcare system, particularly the NHS, has undergone significant transformations, driven by evolving societal needs, technological advancements, and, most profoundly, the global COVID-19 pandemic

The NHS, a cornerstone of our society, has faced unprecedented challenges and opportunities during this period. The pandemic tested our resilience, adaptability, and commitment to providing exceptional care, regardless of the circumstances
As we navigated through this crisis, the importance of an integrated health and social care system became more apparent than ever Our region, with its unique demographic and geographic characteristics, has played a pivotal role in shaping and responding to these changes.
Both the East Anglian and North East Essex regions has demonstrated
remarkable innovation and collaboration in the face of adversity
The NHS, alongside local authorities and community organisations has made significant strides in addressing the immediate needs of our population while laying the foundation for a more sustainable and responsive future
The integration of health and social care services, the adoption of digital health solutions, and the emphasis on preventive care have become key elements in our strategic approach
This report reflects on the journey of the past five years, capturing the challenges, achievements, and lessons learned.
It also outlines the path forward as we continue to navigate a post-pandemic world, where the demand for efficient, equitable, and high-quality care is greater than ever
The insights and strategies presented here are not just about maintaining the status quo but are about driving forward a vision of a more resilient and compassionate health and social care system.
As we look to the future, it is imperative that we recognise the evolving needs of our population and the critical role that health and social care will play in ensuring the well-being of our communities
The decisions we make today will shape the future of healthcare in our region, and it is with this in mind that we welcome you to the UEA Health and Social Care Partners’ Research Impact Report.

Professor Charles ffrench-Constant Pro-Vice-Chancellor
Faculty of Medicine and Health Sciences
It’s been a fantastic year for research and collaboration. We take a look back to celebrate the UEA Health and Social Care Partnership’s successes. Click the titles to view the news article from our website.
We hosted a 3D medical printing workshop in December, to progress discussions to establish an innovative regional 3D medical printing facility that has tremendous potential to transform patient care.
UEAHSCP launches new website
UEA Health and Social Care Partners launches it new website, reflecting on its ambitious tone for our regional research partnership
AbiliTec team awarded NHS EnglandEast of England funding
Members of our AbiliTec team were awarded funding from NHS EnglandEast of England to provide a practicebased evaluation of telerehabilitation services for people after stroke and their carer ’ s in the region
We hosted our Research Sandpit at the Thomas Paine Study Centre
Our twice-yearly Research Sandpits helps researchers turn great ideas into fundable projects.
We opened our Research Capacity Building Programme Funding Call Every year we accept applications for the UEA Health and Social Care Partners Research Capacity Building Programme Funding Call, where project leads from our partner organisations can apply for seedcorn funding to help build capacity and capability for collaborative practiceled research


We sat down with Tim Clarke, Brioney Gee and Bonnie Teague to share their insights and discuss the Working on Worries study The team was awarded seed corn funding from UEA Health and Social Care Partners alongside an NIHR ARC EoE implementation fellowship to develop training resources and sessions to upskill school staff to deliver a programme for parents and carers to support their child’s mental health
The Carer Support Nurse initiative, which received early facilitation by UEA Health and Social Care Partners to secure external funding for its evaluation, was honoured with a regional award in the NHS Parliamentary awards This new evidence-based role provides personcentred assessment and support to unpaid/family carers to help them in their caring role by supporting their own health and their skills in caring.
On the 12th of July we celebrated connecting and innovating by hosting our Collaborate to Innovate Conference at the Enterprise Centre, co-hosted with the Citizens Academy.

UEA Health and Social Care Partners has awarded funding of nearly £130,000 towards six regional research projects which tackle challenges across local health and social care services, such as enhancing care across learning disabilities and autism services, optimising patient access to digital test results, and improving mental health preparedness in coastal communities facing climate change impacts
OOBP project publishes journal 2022-2023 UEAHSCP Scholarship
Receipient Rene Gray, along with his team in the Out of Bed Project, have been published in the BMJ Journal.
The power of collaboration
We spoke to Dr Simon P Hammond on how collaboration has shaped research and continued to be a powerful tool for learning
The CHarMINg Project evidence briefings
The CHarMINg Project co-produced interventions supporting multiple behaviour change within socially deprived communities.
Jeremy Dearling joined us to discuss the importance of citizen-led research
Jeremy spoke to us about his experiences within PPI and its relevance to help practice-led research projects.
CESSATION Study Published in British Paramedic Journal
Female Ambulance Staff Experiences of Menopause Transition (CESSATION)
published a qualitative study of female ambulance staff experiences of the menopause transition CESSATION received funding from UEA Health and Social Care Partners and College of Paramedics
Q&A with Dr. Paul Everden, North Norfolk Primary Care
Dr Everden takes the time to speak with us about the PPISCOREV project and how the positive effects of GP Front Door has had on Emergency Departments and the plans for the future of the project
Point of Care 3D Printing Workshop at the Quadram Institute
On 5 February we hosted a Point of Care 3D Printing Workshop at the Quadram Institute, Norwich Research Park. The aim of the workshop was to help to better understand the clinical, research, and training potentials for a proposed 3D printing in the East of England
New £1.1 million grant to improve wellbeing of teens in
Dr Simon P Hammond, lead of UEAHSCP’s Looked After Children’s Mental Health Research Network (LANTERN), which initially received UEAHSCP funding for £5,000, has been granted £1 1 million for a project looking at the use of Life Story Work (LSW) for teenagers in care
Morag Farquhar leads popular webinar about the Carer Support Nurse project
On 15 February 2024, Professor Morag Farquhar led an engaging webinar to disseminate the findings from the Carer Support Nurse project; over 100 delegates signed up to the webinar
Giving GPs cameras to photograph skin complaints could help slash wait times for hospital appointments according to a new service evaluation from the University of East Anglia The evaluation was funded by UEA Health and Social Care Partners.

On 22 March, the CELDA project team, a receipient of the 2022/23 Partnership Funding Call, hosted their online event; Care Experience Improvements for people with a Learning Disability and / or Autism
On 27 March, Dr Guy Peryer, lead of UEAHSCP's Palliative Care research group, hosted a community-focused event aimed at strengthening communities' palliative care provision
Oral Presentation at the RCN International Nursing Research Conference
The award-winning Carer Support Nurse initiative has been selected to present at the RCN International Nursing Research Conference 2024 in September.
The Carer Support Nurse initiative received facilitation by UEA Health and Social Care Partners to secure external funding for its evaluation, went on to win a regional award in the NHS Parlimentary Awards in 2023.
Health Innovation East is one of 15 regional Health Innovation Networks that support the introduction of innovative technologies, devices, and care pathways to transform health and care
Melissa Taylor is one of UEA Health and Social Care Partner’s Scholarship Awards recipients, will deliver an oral presentation in Istanbul, Turkey


UEAHSCP has awarded funding of nearly £130,000 towards six regional research projects which tackles challenges across local health and social care services, such as enhancing care across learning disabilities and autism services, optimising patient access to digital test results, and improving mental health preparedness in coastal communities facing climate change impacts.
The funding, made possible by our partner organisations, will serve as a catalyst for researchers to cultivate innovative ideas that target pressing issues across regional health and social care services, with a particular focus on projects that align with our partners’ most important research priorities:
Population health management, reducing inequalities and supporting prevention
Improving mental health
Management of long-term conditions and multimorbidity
Improving integrated urgent and emergency care
Learning disability and autism
Workforce development and sustainability
Digital technology to transform care delivery
Read more about the six projects on pages 12-17
CELDA aims to enhance the quality of care for individuals with learning disabilities and autism.
It focuses on creating a risk assessment tool for identifying at-risk homes, identifying key improvement areas in the learning disability care market, collecting
Lead Researcher
Victoria Bunting
Business Change Lead and Social Worker, Norfolk County Council
Lead Organisation
Norfolk County Council
Collaborators
NHS Norfolk and Waveney Integrated Care Board
Norfolk Safeguarding Adults Board
Norfolk Community Health and Care
NHS Trust

Impaired Facial Emotion Communication in Parkinson’s Disease
A Robust Qualitative Approach to Better Understand its Impact on Psychosocial Well-being, and Creation of an Information Support Resource for Clinicians and Loved Ones
FACES aims to comprehend the impact of impaired facial emotion communication in Parkinson’s Disease (PD) and offer valuable support.
Through interviews with individuals with PD and their loved ones, the project seeks to uncover experiences and strategies to mitigate challenges in recognising emotions.
Validation of findings and creation of a patient-led guidance resources will provide insights for clinical staff and loved ones, enhancing social-emotional communication
The project aims to share its outcomes in the influential journal Health Psychology, contributing to a broader understanding of PD-related issues and support strategies
Lead Researcher
Abigail Webb
Research Associate (ESNEFT) and Clinical Research Fellow (University of Suffolk)
Lead Organisation
East Suffolk and North Essex NHS Foundation Trust
Collaborators
University of East Anglia
University of Suffolk Parkinson’s UK

PARROT focuses on enhancing medication management for complex care and frail inpatients receiving care at ESNEFT.
By establishing a specialised pharmacy service, the project aims to assess medications using evidence-based tools, deprescribing when suitable, and optimising medication to enhance patient safety
The project's objectives include evaluating incidents of polypharmacy (the use of multiple medicines), identifying inappropriately prescribed medications, documenting interventions made, and measuring the resulting reduction in medication
Throughout the study, patients will be monitored to collect data, feedback, and ensure their well-being, contributing to a comprehensive service evaluation that aims to enhance patient care and safety
Throughout the study, patients will be monitored to collect data, feedback, and ensure their well-being, contributing to a comprehensive service evaluation that aims to enhance patient care and safety.
Emma Travers
Assistant Chief Pharmacist, East Suffolk and North Essex NHS Foundation Trust
Lead Organisation
East Suffolk and North Essex NHS Foundation Trust
Collaborators
NHS Norfolk and Waveney Integrated Care Board
University of East Anglia


Access to Results: Acceptability of immediate access to test results via a hospital patient portal
RESULTS focuses on investigating the acceptability of providing patients with immediate access to their test results through a hospital patient portal.
Through a cross-sectional survey, qualitative interviews, and the design of an implementation strategy, the project aims to understand patient perspectives, identify barriers and enablers, and if found to be acceptable, create a plan for effectively rolling out immediate test result access
This initiative seeks to enhance patient engagement and streamline healthcare delivery by exploring acceptance of this digital approach.
Lead Researchers
Dr Zarnie Khadjesari
Associate Professor, University of East Anglia
Dr Adulis Beyenne
Clinical Information Officer, West Suffolk NHS Foundation Trust
Lead Organisation
West Suffolk NHS Foundation Trust
Collaborators
University of East Anglia

Mental ill-health is a significant issue in coastal communities and these communities also experience disproportionate climate related risks such as flooding and erosion, leading to worsening the health inequalities
RIPPLE aims to enhance climate psychological preparedness in coastal communities by collaborating with local partners and residents
The project seeks to understand longterm mental health challenges faced by coastal populations and develop prevention strategies
Objectives include creating an awareness baseline for climate change impacts, measuring household preparedness using the Psychological Preparedness for Disaster Threat Scale (PPDTS) assessment, and identifying at-risk households
By addressing psychological well-being and preparedness, RIPPLE aims to empower coastal communities to navigate climate-related challenges more effectively and foster resilient communities
Lead Researchers
Bernice Dixie
Road Safety Communities Team Leader, Norfolk County Council
Jane Locke Prevention Policy Manager, Public Health, Norfolk County Council
Lead Organisation
Norfolk County Council
Collaborators
NHS Norfolk and Waveney Integrated Care Board
Norfolk and Suffolk NHS Foundation Trust
University of East Anglia
East Suffolk Council
Great Yarmouth Borough Council
North Norfolk District Council
Coastal Partnership East

WEIGHT focuses on piloting neonatal weight measurements within the first five days after birth to inform future studies.
The project's objectives are to locally assess neonatal weight loss/gain, determine sample size requirements for a larger multi-centre study, evaluate study feasibility and recruitment, establish a maternity Public and Patient Involvement (PPI) group, and network with regional Trusts for collaborative research
The pilot data will establish a baseline and inform the larger study's design, aiming to determine the optimal day for neonate weight measurements postbirth.
This comprehensive research holds local and national significance in improving long-term health outcomes, supporting breastfeeding, and enhancing maternal mental health
Lead Researcher
Steph Roberson Infant and Feeding Specialist, Specialist Midwife, East Suffolk and North East Essex NHS Foundation Trust
Lead organisation
East Suffolk and North Essex NHS Foundation Trust

Collaborators
West Suffolk NHS Foundation Trust University of Suffolk
Our Scholarships enable practitioners from our Partner organisations to apply for funding to support specific research activites, including undertaking literature reviews, mentoring to support research design and development, and impact dissemination activites.
UEA Health and Social Care Partners allocated £16,189 of the Partnership income to fund research scholarships This allows employees of the Partnership organisations to support the research capacity and facilitate success in attracting research grants and other funding
The focus is on supporting practitioner led research whose duties are to undertake, or support people who conduct research in the key themes of UEA Health and Social Care Partners as listed in the UEA Principles.
The UEA Principles U int be an ma pr de su en We pr
Population Health Management, reducing inequalities and supporting prevention
Improving Mental Health
Management of long-term conditions and multimorbidity
Improving integrated urgent and emergency care
Healthy ageing
Learning disability and Autism
Workforce development and sustainability
Advances in technology and medical science to improve care delivery
Children, Young People and Family health and wellbeing
Palliative and End of Life Care
Cross-cutting themes include economic evaluation, organisational and system transformation, and coproduction methodologies
Read more about the seven Scholarships on pages 19-25

National healthcare policy aims to grow and support the conduct of research for the benefit of patients and staff in the UK.
The purpose of policy itself is to drive practice in clinical organisations and to enable leadership, implementation and translation of both research activity and consequent results into clinical practice
There is a gap which is not yet understood between the intentions of policy and the ability to undertake Nursing, Midwifery and Allied Health Profession (NMAHP)-led research successfully or at all
There is an anecdotal perspective that policy which is in place favours medics over other professions, however this too has not yet been explored
To date, a review of research policy linked to NMAHP-led research is absent from the literature. Exploring the history of healthcare policy and content could enable some understanding of the dichotomy between the intentions of policy and its impact in practice The view is this work is the foundation to future workforce related research
Contact Claire Whitehouse Senior Nurse for NMAHP Research, James Paget
University Hospitals NHS Foundation Trust


This Scholarship plans on conducting a comprehensive literature review examining the cataract surgery rates around the world.
Cataract surgery is the most crucial surgical procedure to reduce preventable blindness around the world, however some countries are falling behind in cataract surgical rates
There is currently no such paper that is up-to-date, and comprehensive, examining cataract surgical rates in countries around the world.
By identifying which countries have fallen behind in cataract surgical rates, there governments can then be informed this and further investments in eye surgical services can be made
This will help ensure that all individuals around the world have equitable access to eye care
Contact Ethan Waisberg
F1 Foundation Doctor, The Queen Elizabeth Hospital King’s Lynn NHS Foundation Trust
Despite the widely known benefits of physical activity (PA) for hospitalised stroke patients, the majority of their time is spent sedentary. This is damaging both in terms of reduced recovery opportunity, and due to the long-term risks of sedentary behaviour such as risk of further cardiovascular events, including recurrent strokes.
Both recovery opportunity and reduced cardiovascular risk are essential for patients. Faster and better functional recovery has implications to reduce length to stay and care needs at the point of discharge. Similarly, there is a specific focus in the recent national stroke guidelines to reduce risk factors for recurrent strokes, and yet PA is a modifiable risk factor which the hospital environment currently does not reduce sufficiently
Furthermore, there is an even greater need to increase patient PA levels, as recent national guidelines recommend that stroke patients with a motor impairment, should receive a minimum of 3 hours therapy/day and be “supported to remain active for up to 6 hours a day” Due to the current workforce demands, this presents a huge challenge to staff and patients alike The current funding for sufficiently trained staffing will require a significant increase, however, this is likely to take time
Instead, research is focusing on modifying the environment and use of current resources, however, recent studies still suggest limited improvement
There is a need to further explore the factors that enable and prevent PA for acute stroke patients, and although studies have explored issues from either the patient, visitor or staff perspective, there is a current gap in the existing capturing their combined perspectives This needs to be fully explored to understand the best way to then design, implement and embed meaningful change to improve patient care and meet best practice standards
Contact Rachel Dance
Senior Stroke Physiotherapist, James Paget University Hospitals NHS Foundation Trust

In contribution to achievement of the NHS Long Term Plan, Health Education England Research and Innovation Strategy, National Institute for Health Research (NIHR) strategy and AHP Faculty Research Strategy 2022 the James Paget University Hospitals NHS Foundation Trust have innovated by designing the NMAP-ER model (recently published in the BMJ Leader with Newcastle Upon Tyne Trust and ImpACT Research Group, University of East Anglia.
This innovation has two pilot posts at each site (2x James Paget University Hospitals NHS Foundation Trust, 2x Newcastle) There is emerging evidence that patients have better outcomes where hospitals are research active (Ozdemvir, 2018) and staff satisfaction and wellbeing are increased where they are involved in research activities (Boaz, 2015) We believe in a positive research ethos and leading from the front in therapies with this innovation is one route to achieving our vision of becoming a centre of excellence for NMAHP research

NMAHPs are underrepresented in their involvement with research, and this is attributed to a lack of confidence, competence, and opportunity to engage in research.
This Scholarship will seek to provide evidence and support for the benefit of having a NMAHP embedded researcher role with protected time to engage in research and to increase confidence, competence, and opportunity for the individual but also the wider department
Contact Rene Gray
Physiotherapist and Embedded
Researcher, James Paget University Hospitals NHS Foundation Trust

Genomic medicine has the potential to revolutionise Paediatric practice. Currently the results of the 100,000 Genomes project are shaping efforts to commence a newborn genome screening in the United Kingdom, and this is being done through consideration of ethical and logistical frameworks.
Tackling inequalities and inequities in delivering genomic medicine is crucial for ensuring the utility of the datasets generated, and for maximising patient and wider-community benefits For patients with rare diseases, where obtaining a diagnosis in itself is an intervention for the family, a lack of awareness and access to genetic research studies or to clinical genetics will adversely impact health outcomes
Therefore, it is important to evaluate the literature that exists around barriers and solutions to undertaking genetic tests such as whole genome sequencing, in regional Paediatrics settings. There are
no unifying frameworks for engaging underserved communities in genetic research projects, and there is a scarcity of evidence around the perceptions regarding genetic testing and research participation, of parents or caregivers for children affected by rare diseases.
Improving our understanding of challenges and potential solutions to increase engagement of diverse communities in Paediatric genetic testing projects will aid rare disease diagnosis through projects such as NIHR BioResource. In turn, increasing the diversity of genomic datasets will improve our ability to understand the pathogenicity of genetic variants and offer counselling to families in the future
Dr Thiloka Ratnaike Paediatric Registrar,
East Suffolk and North Essex NHS Foundation Trust and Clinical Lecturer, University of Cambridge
NMAHP led research is beginning to come under the spotlight and its ability to take place successfully in clinical organisations has been written about in the literature for the past decade.
Time, funding, resource, and support are four key reasons cited regularly as barriers to conducting NMAHP led research activity, alongside lack of research skill and knowledge
For the past 3 years, the James Paget University Hospitals NHS Foundation Trust NMAHP-RES has actively sought to support staff and managers to apply for clinical academic fellowships and internships offered regionally
Whilst we have a 100% retention rate on the programmes for all fellows and interns, we have yet to deep dive into their experiences
We are keen to take a 100% pass record as only one measure of success in this regard rather than assuming we are doing everything right
Exploring the real-world experiences of our fellows, interns and their managers will provide them with the opportunity to share their own learning, challenges, and celebrations, which we might be able to apply to future cohorts.
Contact Emma Stimpson Project Manager, Nursing, Miwifery and Allied Health Professions Research and Evaluation Service, James Paget University Hospitals NHS Foundation Trust

Femoral fracture incidence is increasing yearly due to an ageing population. This is even greater in regions such as Norfolk and Waveney with an above average elderly and frail population.
Femoral fracture requires surgery to fix to allow an early return to walking and function but there are high levels of mortality and long-term disability associated to this major injury
There are national best practice standards that have the objective to improve the outcomes following surgery for this fracture This includes time to a dedicated specialist ward, time to surgery and time to being mobilised after surgery
There is also a need to ensure patients have a clear pathway from admission to be able to have the best chance of returning home as soon as possible This requires the input from the whole multidisciplinary team including surgeons, nurses, occupational therapist, and physiotherapists.
At the James Paget University Hospitals NHS Foundation Trust, the therapy team have developed an MDT approach to improve the involvement of patients at an earlier stage of their acute journey and reduce acute length of stay
This approach includes early occupational therapy assessment, joint therapy sessions and setting a criterialed decision point in the first week after surgery
This “7-day decision point” model has improved MDT communication and working and reduced acute length of stay for our femoral fracture patients
It is hoped to be able to share this good practice to a wider audience within the Norfolk and Waveney Integrated Care Board but also further afield to improve patient care and outcomes
Contact Melissa Taylor Specialist Occupational Therapist and Orthopaedic Therapy Team Leader, James Paget University Hospitals NHS Foundation Trust


“I think it’s a testament to the Partnership, where across the region there is a strong commitment to developing both the capacity and capability of the workforce to undertake practice-led research and innovation, which UEAHSCP has a supporting role in.”
Carrie Jackson
Former Research Director of UEA Health and Social Care Partners

An Impact Case Study is a detailed analysis that showcases the tangible outcomes and effects of a particular intervention, program, or initiative within a specific context or region.
In the realm of health and social care, an Impact Case Study focuses on demonstrating the real-world improvements or changes brought about by health and social care interventions, policies, or practices
Across Norfolk, Suffolk, and North East Essex, these case studies play a crucial role in assessing the effectiveness of various initiatives and identifying areas for improvement.
By analysing data, testimonials, and other evidence, Impact Case Studies help stakeholders understand what works well and what needs adjustment or further investment.
They contribute to the continuous improvement of healthcare systems and practices in the region by highlighting successes, identifying challenges, and informing future decision-making processes
They play a vital role in driving positive change and ultimately contribute to the enhancement of health and well-being within the region
The Better Sleep Programme (TBSP) was a six-month scoping exercise to develop a business case and plan of work for a wider project. The wider project aims to roll-out training and supervision in sleep interventions in order to improve access effective help for young people in this area (ages 14 to 25) with mental health difficulties, as well as to support and promote further clinical research.
The focus is on making it easier for young people to access help for sleep difficulties across the wider health and social care system, spanning prevention and early intervention, community support and urgent and emergency care (including CYP crisis prevention) and incorporating NSFT, primary care, social care and Voluntary, Community and Social Enterprise (VCSE) services.
The aim is to also increase awareness of the importance of sleep in young people’s mental health and to make it easier for professionals, young people and their families to access appropriate resources and online support where this is already available.
It is hoped that the wider project will help improve understanding of this underresearched area by providing a platform to host additional research projects as well as reporting on the clinical outcomes of the intervention itself
Young people experience high levels of sleep difficulties that significantly affect their mental health Despite this, sleep difficulties are rarely addressed within mental health services
The Better Sleep Programme has adapted Cognitive-Behavioural Therapy for Insomnia (CBT-I) to be suitable for young people with mental health difficulties
After showing positive outcomes in secondary mental health services, the Norfolk and Waveney Integrated Commissioning Board have funded TBSP to improve access to help with sleep across the wider youth mental health system
The Better Sleep Programme provides training and supervision to mental health professionals from services across Norfolk and host workshops to increase awareness around the role of sleep in mental health. The aim is to embed this intervention into routine practice, allowing young people in Norfolk timely access to first-line NICE recommended treatment for insomnia
The project relies heavily on digital solutions to achieve this ambitious target whilst working with multiple organisations across a wide geographical area
The ambition of The Better Sleep Programme (TBSP) is to have an effective intervention for sleep difficulties offered in routine clinical practice This needs to be widely available and easily accessed The Better Sleep Programme uses digital solutions to make this a reality
After showing effectiveness and feasibility within secondary mental health services, they undertook a 6-month scoping project with over 30 local mental health providers Similar to recent research findings, they found a high level of sleep difficulties, a low level of provision and services keen for further training
The implementation of a sleep intervention into a mental health system is novel The strategic approach involves:
An accreditation programme for therapeutic practitioners (two days of online training and six months of online supervision)
A half-day online skills workshop for wider staff groups alongside a selfhelp guide they have developed Projects to adapt the intervention for more specialist clinical populations and Improved access to digital resources and information
Their overall ambition is to improve the awareness of the role of sleep and the availability of effective interventions across youth mental health services
nationally. Raising awareness of the work is central to this, as is disseminating their findings and widening access to the online training and digital resources TBSP has developed Ultimately, they want access to sleep interventions to become part of routine clinical practice
Sleep difficulties are particularly prevalent in young people and are welldocumented as a risk factor contributing to all forms of mental health difficulties (Hertenstein et al , 2019)
Results from the 2022 NHS survey show that 34% of 7-16yr olds struggle with their sleep three times a week and this prevalence increases to 72 3% in those experiencing mental health difficulties In those aged 17-25yrs these sleep difficulties rise to 64% and reach 89 5% in 17-25yr olds struggling with mental health difficulties

Recent research has found that insomnia precedes the onset of mental health difficulties (Hertenstein et al , 2019; Orchard et al., 2020) and that treating insomnia can improve mental health, however treating mental health difficulties does not show the same reduction in insomnia Moreover, insomnia has been shown to increase the risk of developing mental health difficulties such as anxiety, psychosis and depression (Hertenstein et al., 2019; Harvey et al , 2008) Targeting sleep can therefore improve outcomes in both sleep and wellbeing and is often viewed as a more accessible intervention by young people.
Not only does insomnia increase the likelihood of mental health problems, it also contributes to higher risk behaviours such as suicidality, self-harm and impulsivity (Glenn et al , 2021; Liu et al , 2017; Wong et al , 2011) Therefore, it is vital to treat sleep difficulties to reduce mental health symptoms and risk of young people acting on their thoughts
Cognitive Behavioural Therapy for Insomnia (CBTi) is recommended as the first line of treatment for insomnia (NICE, 2024) This therapeutic intervention typically consists of psychoeducation, sleep scheduling, stimulus control, sleep hygiene, cognitive restructuring, and relaxation training (Davidson, 2019; NICE, 2024) Research has demonstrated that CBTi is as effective as sedating hypnotics in the short term and supersedes these in the
long term (Smith et al., 2002; Okajima et al , 2011) Furthermore, research has demonstrated the therapeutic interventions’ efficacy in both young people with mental health difficulties and those without (Muench et al , 2022) However, in secondary mental health services, CBTi is seldom considered, and mental health treatment is typically the only focus (Hertenstein et al , 2022)
To summarise, research to date demonstrates high efficacy of CBTi for sleep problems in individuals with mental health difficulties, but it is yet to be rolled out nationally as an intervention offered in youth mental health services.
At the start of the project, TBSP set a target to train 180 practitioners across two years and have currently trained 137 in less than one year They have provided workshops to 130 professionals to date The training feedback has been extensively positive with 100% of attendees reporting that they would recommend the training
To date, TBSP has outcome data collected for 94 young people Interim analyses indicate high baseline levels of insomnia and significant improvements being seen in sleep and wellbeing after six sessions of sleep work They have found 68% of service users no longer reaching clinical threshold for insomnia and 35% scoring below the clinical range on wellbeing measures (compared to 80% and 93% scoring above respectively at baseline)
The meaning of this change is captured in positive feedback and quotes from service users:
“It works!” “So good to see the impact it makes on [my] sleep but also mood and wellbeing,” (service user)
“I don't think about sleep anymore, it just happens naturally It's never on my mind” (service user)
Beyond the measures collected, practitioners report drawing on their new skills in their work with ‘many/most’ of the young people they are working with
They estimate at least 1000 young people will already have benefitted from more informed help with their sleep to date
Disturbed sleep plays a critical role in the
onset and maintenance of mental health difficulties
TBSP are seeing a high level of need around sleep in young people accessing mental health services with medication being the main treatment offered
Preliminary findings suggest that The Better Sleep Programme has led to improvements in sleep and psychological wellbeing for young people in Norfolk and Waveney
Increasing the availability of this first-line NICE recommended offer should help to reduce costs associated with medication use in young people
TBSP recommend continuing to fund projects like The Better Sleep Programme to ensure:
THRESHOLD
N = 64 N = 31
Ongoing training and supervision for existing services to maintain current provision
Continued support and adaptations for specialist services including case studies to guide implementation
Further workshops to increase knowledge and awareness in the wider system
Ongoing development of resources for young people with different presentations and needs
Continuation of data collection to monitor effectiveness
TBSP also recommends further research is needed, such as:
Randomised controlled trials (preferably single blind) to determine the effectiveness of a CBTi-based intervention vs a singular mental health intervention
Use of CBTi in children under 14years old
More screening options to detect sleep difficulties early on
Researching the impact of psychological interventions for sleep in inpatient settings
Publications
Rollinson, R , Price, I , Gee, B , Lyons, J , Carroll, B , Wilson, J , & Clarke, T (2021)
Low-intensity sleep intervention in a youth mental health service: a case series analysis Behavioural and Cognitive Psychotherapy, 49(1), 62-75
https://www cambridge org/core/journal s/behavioural-and-cognitivepsychotherapy/article/abs/lowintensitysleep-intervention-in-a-youth-mentalhealth-service-a-case-seriesanalysis/9E814C18943D46A72A1A02CF 4227F2D4?
utm campaign=shareaholic&utm mediu m=copy link&utm source=bookmark
Rollinson, R , Cole, A , Gee , B , Tofan, I , Graham, A , Hatton, J , Lyons, J , Reeve, S., Wilson, J., Beardsworth, K., Clarke, T. (2024) Delivering a sleep intervention across an NHS youth mental health service using non-expert practitioners: a service evaluation Early Intervention in Psychiatry (In submission).
The Norfolk and Waveney Integrated Commissioning Board (ICB) funded TBSP to improve access to effective help with sleep across the wider youth mental health system.
For more information on The Better Sleep Programme, please visit our website
The research was supported by UEA Health and Social Care Partners (UEAHSCP)
The views expressed are those of the author(s) and not necessarily those of the University of East Anglia or UEA Health and Social Care Partners
The Point-of-Care 3D Printing Service (POC3DP) research group were awarded two grants from the UEA Health and Social Care Partners in 2022 and 2023 to conduct evaluation and proof-ofconcept research on setting up a regional point-of-care medical 3D printing service to serve all regional NHS hospitals.
POC3DP (Project 1) is a scheme to set up a 3D-printing service to produce surgical equipment tailored to individual needs, in one of the region’s hospitals, as well as setting up an offsite research and development 3D Printing suite
It is hoped that this project could help patients receive treatment more quickly and help reduce costs within the NHS
The BEAT project (Project 2) aims to develop the clinical application and implementation of 3D printing technology to transform quality of care for breast cancer patients, which may be extended in its application to other cancer patient care in the near future
The project aims to build regional 3D technology awareness and UEA-NNUH joint research capability in clinical applications of 3D printing to improve quality of care.
The POC 3DP research group were
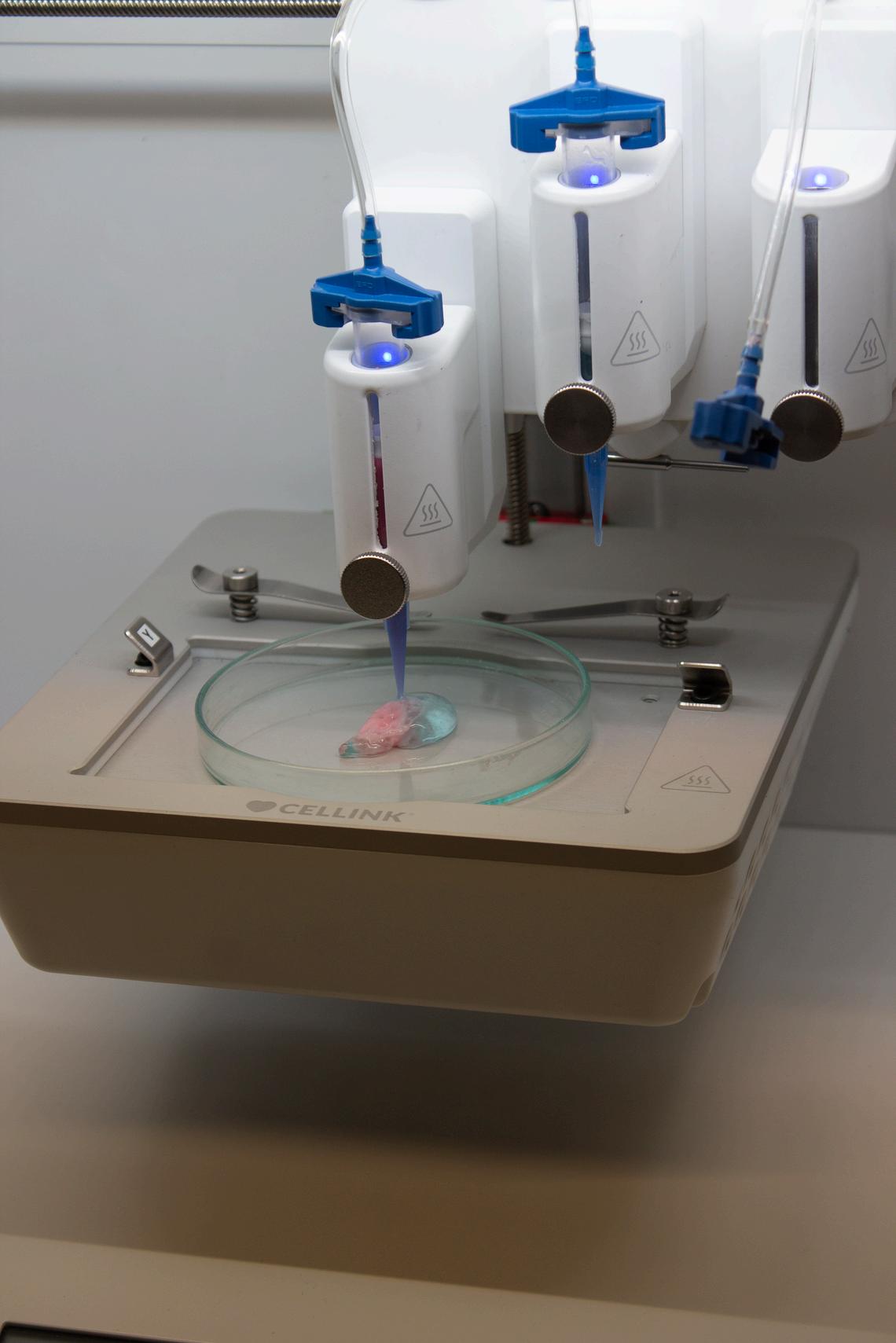
awarded two grants from the UEAHSCP in 2022 and 2023 to conduct evaluation and proof-of-concept research on setting up a regional point-of-care medical 3D printing service to serve all regional NHS hospitals Project 1 aimed to engage with the regional NHS trusts and evaluate the level of interests in using POC medical 3D printing to improve patient care
At the end of the project 1, the team discovered that currently some types of surgeries have already been using medical 3D printing but outsource the service with high cost and slow turnover time. Another important finding from the engagement activities is that many surgeons who are not currently using medical 3DP are interested in introducing it to their practice
Due to these two key outcomes, they designed and developed the project 2 with the intension of using it as a proofof-concept demonstration to how POC medical 3D printing could improve the speed and quality of surgeries and produce cost-saving for NHS and improve quality of care for patients
The team used the breast reconstruction surgery as the case study and developed a workflow of how to effectively utilise POC medical 3D printing to significantly improve the quality and efficiency of breast reconstruction surgery
create customised products that were not possible using traditional manufacturing methods
In the UK healthcare sector, 3DP has been used by NHS hospitals for over 15 years and now over 50 NHS Trusts around the country already have inhospital point-of-care (POC) 3DP services that enable the delivery of significantly more personalised, faster and cheaper treatment for patients.
However, currently hospitals in the Norfolk, Suffolk and North-East Essex region do not have any such POC 3DP service. Project 1 aimed to evaluate the level of interest from the regional trusts on hosting a regional POC 3DP service
Using POC 3DP service can provide significant cost-saving Using breast reconstruction surgery as an example (project 2) In the NNUH, approximately 200 PMBRs are performed each year using autologous tissue from other parts of patient’s body
3D Printing (3DP) is an Additive Manufacturing method that can rapidly
Without the assistance of 3DP, currently the surgeons use a ruler to do crude measurements. This leads to multiple surgical procedures being required to reach symmetry to allow functional as well as psychological completeness Shaping the breast at each surgery can take at least 2-3 hrs. Each surgical procedure requires general anaesthetic with 1-2 days hospital stay and 2-4 weeks recovery accounting for a significant cost both for the patient and the NHS
(estimated hospital bed costs £300/night and theatre costs £1500/ hour) 3D technology could significantly reduce the time required for all steps of the procedure and improve the accuracy of breast volume estimation and shaping
The key findings of Project 1 are:
There is a definite appetite for pointof-care 3D printing across numerous departments in the NHS
Appetite is typically strongest in more junior doctors with more experience, clinicians are often stuck in their ways and resistant to change
Reconstructive, Orthopaedic, Radiologist and breast reconstructive surgeons appear to be the most interested in the new technology
There are a wide range of potential applications of 3D printing within the NHS ranging from simple anatomical models (which currently make of the majority of existing point-of-care 3D printing lab workload) to more complex cutting guides and biocompatible implants
Cost savings are primarily reduced theatre time due to improved surgical planning and preparation
Also cost savings associated with bringing jobs on site
Funding is a big hurdle because the NHS is under-funded
Other 3D printing suites have been funded through charity or by capital bid
The key findings for Project 2 are:
By working closely with the surgeon, a new workflow on how to integrate the 3D technology, including imaging and 3D printing, were developed for breast reconstruction surgery:
Point-of-Care 3D Scan-to-Print Workflow
Patient attends the appointment 3D model processing
1-2 hours
Printing 3D breast mould
24-48 hours
Delivering breast mould to surgeon
Modifying mould design
Patient attends the appointment 5-10 mins
24-48 hours
Delivering breast mould to surgeon
The cost-saving can be generated from;
Reduced Theatre time
Minimise/avoid repeated correction surgery
Shortened patient recovery time
Recommendations for commissioners and future research are:
A point-of-care 3D printing service
should be set up with the Norwich and Norfolk University Hospitals
NHS Foundation Trust, under orthopaedic lab
An internal lead to champion and continue to build the business case
Engage more surgeons from different disciplines to strengthen the business case
Discuss with the hospital charity and Trust Innovation/Capital fund for funding support for setting up the service
For more information on The Point-of-Care 3D Medical Printing research group, please visit our website

General Practitioner (GP) at Door of Accident & Emergency (GDAE) services are now routinely deployed in acute hospitals across Norfolk & Waveney. They aim to assess patients when they first arrive at Accident & Emergency (A&E) and signpost those who do not need urgent care towards other more appropriate care services to help reduce pressure on A&E.
Because many GDAE service users are likely to be in ‘hard-to-reach’ demographics, this project will see researchers working closely with citizens to design face-to face interviews that will help the project better understand the often-under-represented perspectives of those who have sought help from the GDAE service pathway
Researchers aim to produce a short format survey that is suitable (sensitive, respectful, informative) for administering to service users on site at point they are receiving the service
PPISCOREV is led by the James Paget University Hospitals NHS Foundation Trust and University of East Anglia
Media often report stories about the
pressures on Accident and Emergency Departments (A&E), due to the number of visits and the waiting time for patients To reduce these pressures, primary care clinicians were deployed in or near A&Es.
They wanted to map these services and assess their use around the UK In addition, they wanted to develop research to understand why people attend A&E for health problems rather than their GPs or other medical services
A systematic review suggests that providing GP services at or near A&E (GPAE) has done little to reduce the pressures on this service
Conversations with members of the public revealed why patients may not go to their own GP and provided insight for the development of future research to evaluate the use of GPAE
People seeking unscheduled health care at A&Es has been growing at a pace that exceeds population growth (Baker 2017)
Many interventions to improve patient flow and to meet service performance targets have been tested and continue to be trialled in the NHS.
One example is embedding primary care clinicians - general practitioners (GPs) or nurse practitioners (NPs) -- into care pathways available to A&E attenders.
This has become widespread practice in the NHS GP at Door of A&E (GPAE) services are now routinely deployed at hospitals across the UK.
Some GP services are located on the site of A&E, and some are close by. Patients attending A&E are assessed by a clinician who allocates them to the GPAE service or usual A&E care
of studies about primary care professionals (GPs or NPs) delivering treatment in A&Es, to assess the effectiveness and cost-effectiveness of the interventions in the UK. These included studies of primary care services that treat patients within or near to hospital A&E departments
Secondly, the project team began conversations with members of the public to understand why patients use A&E rather the GP services and to help to develop future research

If eligible for GPAE care they are allocated to a GP or NP consultation ‘slot’ This should be the same as if they had attended their own registered GP surgery
It is important to evaluate the effectiveness and cost-effectiveness of the GPAE interventions and, importantly, to understand why patients opt for A&E rather than their own GP services
The project team undertook two strands of research Firstly, a systematic review
Visiting A&E can be stressful and so it is important to gain insight from members of the public, known as patient and public involvement, so that the methodology and questions are approached sensitively to avoid perceived stigmatism about their decision to attend A&E rather than their own GP
A systematic review of 20 eligible studies (see reference list of included studies below) showed diversity in design, delivery and evaluation Broadly, the evidence suggested that primary care clinicians providing treatment in or near A&Es had little effect (good or bad) on clinical outcomes or economic evaluations Clinicians had mixed opinions about the effectiveness of putting primary care services in or near A&Es Some clinicians liked the opportunity to share knowledge with other clinicians, but others were concerned about patient safety and the rationale for the system.
Patients were generally satisfied with the healthcare they received but seemed unaware of the different care pathways or that they had been streamed into one or the other None of the studies had addressed the reasons for patients attending A&E instead of their own GP, thus showing a gap in the research, which they plan to follow up.
Three focus groups were held in different areas of Norfolk (urban and rural) to gain different perspectives from people of different age, gender, and socio-economic status The PPI sessions provided clear direction about how to approach patients, gain their consent to participate in the research, and how to broach questions to ensure they felt comfortable answering.
In seven studies, PPI members guided the research (design, tool development, analysis, theory development, dissemination)
Various descriptions were used for GP services such as inside/integrated; inside/parallel; outside/onsite; outside/offsite and for streaming patients, such as front door streaming; streaming inside the emergency department; no primary care streaming; combined streaming pathways.
Ten studies provided details of outcomes for GPAE pathways Most patients were
seen or treated within four hours, but those in A&E waited longer than those in primary care streams Overall, patients received fewer investigations in the primary care stream, but those in A&E received more prescriptions of common drugs
Most studies showed that a larger number of patients left before being seen in A&E compared to primary care services There were no adverse outcomes reported but some clinicians felt that caution may limit which patients are streamed to primary care services
Most patients were satisfied with the care they received, irrespective of whether they received medical attention in A&E or primary care services. Reasons for dissatisfaction with the A&E were due to duration of visit, facility cleanliness, time to discuss healthcare, involvement in decision making and privacy
Clinicians had mixed views about primary care services in or near A&Es. There were concerns about the need for the service, its governance, and the working environment. Perceived barriers and facilitators of primary care in or near A&Es, included staff engagement, governance, space, recruitment, training, funding, and service demand Clinicians felt more time might be given to A&E patients that really needed the service, but some were concerned about potential safety for some patients.
Of the three studies that presented cost as shown in the systematic review, existing evaluations provide little evidence that primary care services in or near Emergency Departments offers any system advantages for clinical outcomes, or cost savings
This may be due to diversity of models and how they were evaluated It is essential to include process evaluations in future studies to understand how GP services in or near A&Es can improve the system and patient care
The models identified should be properly compared to evaluate effectiveness and cost effectiveness by systematically collating data on patient outcomes, adverse outcomes, and patient experience Such research would provide a solid evidence base for development of future GPAE
The review also identified a gap in knowledge about why patients attend A&E instead of their own GP.
This is important and should be thoroughly addressed to identify perceived issues within the health service and provide a system that effectively delivers care
We hope to secure funding to undertake comprehensive interviews, based on our PPI work, to fill this gap in knowledge about the use of A&E.
The PPISCOREV team believe from the PPI that many patients may decide that attending A&E with a chronic and nonemergency health problem is the only sensible option when other health care services are hard to access
But there is no robust dataset to document the healthcare decisionmaking that low acuity attenders have taken
Their recommendation is therefore to conduct qualitative research, based on the PPISCOREV team’s PPI findings asking patients about their decision making around A&E attendance

References in Narrative
Baker, C (2017, Feb 21) "Accident and Emergency Statistics: Demand, Performance and Pressure." 6964. Retrieved Feb 27, 2023, from https://researchbriefings files parliament uk/documents/SN06964/SN06964 pdf
References of Studies Included in Systematic Review
Ablard S, O’Keeffe C, Ramlakhan S, et al (2017) Primary care services co-located with Emergency Departments across a UK region: early views on their development Emergency Medicine Journal 34(10): 672-676
Aldus CF, Pope I, Brainard JS, et al (2022) Feasibility and evaluation of an emergency department-based GP streaming and treatment service Journal of Evaluation in Clinical Practice DOI: 10 1101/2022 05 13 22275043 1-10
Anderson H, Scantlebury A, Leggett H, et al (2021) Factors influencing streaming to general practitioners in emergency departments: a qualitative study International Journal of Nursing Studies 120: 103980
Brant H, Voss S, Morton K, et al (2021)
Current provision of general practitioner services in or alongside emergency departments in England Emergency Medicine Journal 38(10): 780- 783.
emergency departments: an exploration of patient choice, preference and satisfaction Emergency Medicine Journal 24(4): 260-264
Coleman P, Irons R and Nicholl J (2001) Will alternative immediate care services reduce demands for non-urgent treatment at accident and emergency?
Emergency Medicine Journal 18(6): 482487
Dale J, Green J, Reid F, et al. (1995)
Primary care in the accident and emergency department: II Comparison of general practitioners and hospital doctors British Medical Journal 311(7002): 427-430.
Dale J, Lang H, Roberts JA, et al (1996) Cost effectiveness of treating primary care patients in accident and emergency: a comparison between general practitioners, senior house officers, and registrars British Medical Journal 312(7042): 1340-1344.
Edwards M, Cooper A, Davies F, et al (2020) Emergency department clinical leads’ experiences of implementing primary care services where GPs work in or alongside emergency departments in the UK: a qualitative study BMC Emergency Medicine 20(1): 1-10
Chalder M, Montgomery A, Hollinghurst S, et al. (2007) Comparing care at walkin centres and at accident and
Edwards M, Cooper A, Hughes T, et al (2022) The effectiveness of primary care streaming in emergency departments on decision-making and patient flow and safety–A realist evaluation. International
Emergency Nursing 62: 101155.
Edwards M, Cooper A, Hughes T, et al (2021) A classification of primary care streaming pathways in UK emergency departments: Findings from a multimethods study comprising crosssectional survey; site visits with observations, semi-structured and informal interviews. International Emergency Nursing 56: 101000
Gaughan J, Liu D, Gutacker N, et al (2022) Does the presence of general practitioners in emergency departments affect quality and safety in English NHS hospitals? A retrospective observational study BMJ Open 12(2): e055976
James D, Kithany H, Robbins A, et al. (2019) G327 (P) Children and young people seen in a co-located primary care hub; an observational study In: Royal College of Paediatrics and Child Health, Birmingham UK, Paediatrics: pathways to a brighter future BMJ Publishing Group Ltd
Jones D (2011) How GPs can help reduce inappropriate attendance Emergency Nurse 19(4). Leigh S, Mehta B, Dummer L, et al (2021) Management of nonurgent paediatric emergency department attendances by GPs: a retrospective observational study British Journal of General Practice 71(702): e22e30
McCarron M, Burgess K and Gibbs S (2019) G339 (P) An evaluation of
primary care streaming in a tertiary paediatric emergency department. Royal College of Paediatrics and Child Health Birmingham UK: BMJ Publishing Group Ltd.
Salisbury C, Hollinghurst S, Montgomery A, et al (2007) The impact of co-located NHS walk-in centres on emergency departments. Emergency Medicine Journal 24(4): 265-269
Scantlebury A, Adamson J, Salisbury C, et al (2022) Do general practitioners working in or alongside the emergency department improve clinical outcomes or experience? A mixed-methods study BMJ Open 12(9): e063495.
Uthman OA, Walker C, Lahiri S, et al (2018) General practitioners providing non-urgent care in emergency department: a natural experiment BMJ Open 8(5): e019736.
Ward P, Huddy J, Hargreaves S, et al. (1996) Primary care in London: an evaluation of general practitioners working in an inner city accident and emergency department Emergency Medicine Journal 13(1): 11-15
The research was funded by UEA Health and Social Care Partners (UEAHSCP) and the National Institute for Health and Care Research Health Protection Research Unit (NIHR HPRU) in Emergency Preparedness and Response, a partnership between the UK Health

Security Agency (UKHSA), King’s College London (KCL) and the University of East Anglia (UEA) The views expressed are those of the author(s) and not necessarily those of the funders
Some Key Publications/Further Reading
Hull et al "Population and patient factors affecting emergency department attendance in London: retrospective cohort analysis of linked primary and secondary care records." British J. Gen. Practice 68 668 (2018): e157-e167
Ismail et al "Reducing inappropriate accident and emergency department attendances: a systematic review of primary care service interventions " British J Gen Practice 63 617 (2013): e813-e820.
Lloyd-Rees J "Supporting frequent attenders to reduce their visits to an emergency department " Emergency Nurse 29.3 (2021).
McCartney M " An economist explains why healthcare can’t be treated as a market " BMJ 358 (2017)
Morris et al. "Calculating the proportion of avoidable attendances at UK emergency departments: analysis of the Royal College of Emergency Medicine’s Sentinel Site Survey data " Em Med J 35.2 (2018): 114-119.
TOSCA ran a series of focus groups to understand the views of young people with complications of obesity around using technology to support their journey within the Complications from Excess Weight (CEW) service. This study aims to collate data on young people’s perceptions and preferences regarding the role and usability of technology designed to support behavioural change.
The project aims to improve Healthy Futures CEW clinic service provision across England by developing a costeffective evidence-based intervention to support adolescents with health change behaviour in an easily accessible way which works for them.
Complications of Excess Weight (CEW) clinic patients (aged 10-16 years) and their adult family members took part in focus groups and co-design workshops.
Groups explored young people’s health priorities, the barriers and facilitators of health behaviour change, and codesigned ways in which technology could be used to support young people in overcoming these barriers to achieve their health goals. They were facilitated by a cross-disciplinary team of clinicians, academics and technology innovators
38 individuals (19 adolescents, 19 family members) participated
Mental health, sleep and peer support were identified as the domains in which CEW patients would most benefit from additional support; participants believed technology could be helpful in providing this support
Participants expressed a preference for technology able to individually tailor content to the young person ’ s needs, including relatable peer-produced content
The need for support for both the young person themselves and their family members was highlighted
There is potential for digital technology to be used to support the holistic health priorities of young people receiving specialist care in CEW clinics.
TOSCA plans to use the findings of this study as the basis to begin developing innovative approaches to the use of technology to support this high-need group
The growing prevalence of childhood obesity is among the most important threats to public health globally increasing the risk of a wide range of noncommunicable diseases, including cardiovascular diseases, diabetes, musculoskeletal disorders and certain types of cancer (1,2)
In England, 22.7% of children aged 10/11 years were living with obesity in 2022/23, with 5 7% classed as severely obese (3) This equates to more than 2.5 million children eligible for specialist treatment according to the National Institute for Health and Care Excellence (NICE) guidance (4)
optimal care for young people experiencing severe obesity, a key objective of the pilot clinics was to contribute to generating evidence on the most promising interventions and service models for this cohort (6)

The NHS Long-Term Plan committed to improving the care available to children and young people experiencing health complications related to excess weight.
As part of this commitment, 21 new CEW clinics located across England were commissioned in 2021 (5) CEW clinics provide specialist biopsychological care, delivered by a multidisciplinary team comprising consultants, nurses, and allied health professionals Given the limited evidence-base for what constitutes
During their treatment, young people under the care of a CEW clinic are encouraged to make multiple behavioural changes to improve their health, such as increasing activity, changing dietary patterns and taking regular medication.
However, adolescents face multiple barriers to successful and sustained behavioural change (7) Whilst CEW clinicians aim to support young people and their families to overcome these
barriers, this support is only provided during scheduled clinic appointments
Digital technology is now an integral component of almost all young people’s lives (8) As such, increased use of digital technology may enable CEW clinics to offer their patients accessible ongoing support between appointments to increase the likelihood of successful health behaviour change
Systematic reviews of technology-based interventions for overweight and obesity in adolescents have found some evidence of short-term improvement in dietary behaviours and physical activity (9), and significant reductions in body mass index (BMI) (10-12)
However, while short-term engagement with technology-based behaviour change interventions is often good, this engagement tends to decrease over time (13-15), likely limiting their impact (16) Further, despite the acknowledged importance of involving intended end users in the development of digital health technologies (17), most currently available digital weight-management interventions were not developed with the involvement of patients or healthcare professionals (18).
This study aimed to explore the views of young patients and their family members on the potential for digital technology to enhance the support offered by CEW clinics to adolescents with severe obesity Research questions they sought
to address included:
(a) What are the most important unaddressed health priorities for adolescent CEW clinic patients from the perspective of patients and their family members?
(b) What do adolescent CEW clinic patients and their family members perceive to be the key barriers and facilitators to health behaviour change, and to what extent do they believe that digital technology could assist in overcoming barriers?
(c) What preferences do adolescent CEW clinic patients, and their family members have for the design and delivery of digital technology to support health behaviour change?
In total, 19 young people and their family members were supportive of the idea of increased use of digital technology by CEW clinics to facilitate access to additional support to address currently unmet needs.
However, participants expressed the view that this support should be an adjunct to, not a replacement for, faceto-face support provided by clinicians.
This view aligns with the evidence-base as there is currently little evidence for the effectiveness of digital interventions for paediatric obesity as standalone interventions outside of comprehensive package of support (20)

Participants identified three domains in which they would particularly benefit from increased support: mental health, sleep, and peer support
Improved mental health, sleep and increased social support (both from peers and family members) were also seen as facilitators of wider health behaviour change, as well as overcoming financial barriers and balancing the benefits of technology against the negative impacts of excessive screentime
participants in the current study overlap with this identified in a Canadian study of adolescents with severe obesity receiving multidisciplinary clinical care (15) This study highlighted three factors that impact behaviour change across lifestyle domains: perceived controllability, the impact of mental health and social relationships and interactions
In line with the current study, the Canadian team identified both mental health and sleep as important priority areas for young people living with obesity and concluded that “lifestylebased interventions for behaviour change should evolve to emphasise outcomes beyond weight status to include mental health as a primary intervention focus and outcome ”
All three domains prioritised by the participants as unmet needs were seen as areas where technology could facilitate the provision of additional support
Existing digital interventions were viewed as potentially helpful but current awareness and utilisation of digital resources is low
Many of the barriers and facilitators of health behaviour change refer to by
Participants expressed enthusiasm for the creation of a platform bringing together digital resources tailored to the needs of individual technology to connect young patients and their family members with others with similar experiences was also supported
In line with previous research (7,12), the findings of this study make clear the role of family support in the success or failure of adolescents’ health behaviour change efforts As such, any digital technology developed in this area must take into account the needs and preferences of not just the young patient but their wider family support network.
This study highlights the potential for digital technology to be used to provide young people experiencing health complications related to obesity with additional support to make behavioural changes to improve their health
The findings suggest that such technology-based interventions should focus on the outcomes beyond weight, provide individually tailored content and support the needs of the wider family, not the young patient alone, to maximise their impact
Technological support should be offered as an adjunct to multidisciplinary clinicbased interventions and may require ongoing clinician support to ensure engagement is maintained over time for potential benefits to be realised.
Future studies need to look at the barriers young people have identified in enabling them to move forwards with becoming healthier. Mental health, lack of peer support and poor sleep were all highlighted by young people and their families.
1 Di Cesare M, Sorić M, Bovet P, Miranda JJ, Bhutta Z, Stevens GA, et al The epidemiological burden of obesity in childhood: A worldwide epidemic requiring urgent action Vol 17, BMC Medicine BioMed Central Ltd ; 2019
2. World Health Organization. Obesity and overweight [Internet] 2021 [cited 2024 Jan 4] Available from: https://www.who.int/news-room/factsheets/detail/obesity-and-overweight
3 Office for National Statistics National Child Measurement Programme, England, 2022/23 School Year [Internet]. 2023 Oct [cited 2024 Jan 4] Available from: https://digital nhs uk/dataand[1]information/publications/statistical /national-child-measurementprogramme/2022-23-school-year
4 National Institute for Health and Care Excellence. Obesity: clinical assessment and management [Internet] 2016
Available from: www.nice.org.uk/guidance/qs127
5 NHS England Complications from Excess Weight (CEW) clinics for children [Internet] 2022 [cited 2024 Jan 4]
Available from: https://www england nhs uk/getinvolved/cyp/specialist-clinicsfor[1]children-and-young-people-livingwith-obesity/
6. National Institute for Health and Care Research HSDR Commissioning Brief 2022 Evaluating new models of care for children and young people with excess weight and related complications
7 Kebbe M, Perez A, Buchholz A, McHugh TLF, Scott SS, Richard C, et al Barriers and enablers for adopting lifestyle behavior changes in adolescents with obesity: A multi-centre, qualitative study. PLoS One. 2018 Dec 1;13(12).
8 Office for National Statistics Internet users, UK: 2020 [Internet] 2021 Apr [cited 2024 Jan 4] Available from: https://www.ons.gov.uk/businessindustry andtrade/itandinternetindustry/bulletins/ internetusers/2020
9 Rose T, Barker M, Jacob C, Morrison L, Lawrence W, Strömmer S, et al A systematic review of digital interventions for improving the diet and physical activity behaviors of adolescents. Journal of Adolescent Health 2017;61(6):669–77
10 Alotaibi M, Alnajjar F, Cappuccio M, Khalid S, Alhmiedat T, Mubin O Efficacy of Emerging Technologies to Manage Childhood Obesity Diabetes, Metabolic Syndrome and Obesity. 2022;15:1227–44
For more information on the Technology to Support Change Project, please visit our website
11. Kouvari M, Karipidou M, Tsiampalis T, Mamalaki E, Poulimeneas D, Bathrellou E, et al Digital Health Interventions for Weight Management in Children and Adolescents: Systematic Review and Meta-analysis Vol 24, Journal of Medical Internet Research JMIR Publications Inc ; 2022
12 Azevedo LB, Stephenson J, Ells L, Desmet A, O’malley C, Chai LK, et al The effectiveness of e[1]health interventions for the treatment of overweight or obesity in children and adolescents: a systematic review and meta-analysis Obesity Reviews 2022;23(2):e13373
13 Hawkes RE, Miles LM, Ainsworth B, Ross J, Meacock R, French DP Engagement with a nationallyimplemented digital behaviour change intervention: Usage patterns over the 9month duration of the National Health Service Digital Diabetes Prevention Programme. Internet Interv. 2023 Sep 1;33
14. Lipschitz JM, Pike CK, Hogan TP, Murphy SA, Burdick KE The Engagement Problem: a Review of Engagement with Digital Mental Health Interventions and Recommendations for a Path Forward Vol. 10, Current Treatment Options in Psychiatry Springer Science and Business Media Deutschland GmbH; 2023. p. 119–35.

15. Yardley L, Spring BJ, Riper H, Morrison LG, Crane H, Curtis K, et al Understanding and Promoting Effective Engagement with Digital Behavior Change Interventions Am J Prev Med 2016;51(5):833– 42
16 Tu AW, Watts AW, Chanoine JP, Panagiotopoulos C, Geller J, Brant R, et al Does parental and adolescent participation in an e-health lifestyle modification intervention improves weight outcomes? BMC Public Health 2017 Apr 24;17(1)
17 Partridge SR, Redfern J Strategies to engage adolescents in digital health interventions for obesity prevention and management Healthcare 2018 Sep 1;6(3).
18 Rivera J, McPherson A, Hamilton J, Birken C, Coons M, Iyer S, et al Mobile apps for weight management: A scoping review. JMIR Mhealth Uhealth. 2016 Jul 1;4(3)
19. Wickham CA, Carbone ET. Who’s calling for weight loss? A systematic review of mobile phone weight loss programs for adolescents. Nutr Rev. 2015 Jun 1;73(6):386–98
20 Rivera J, McPherson AC, Hamilton J, Birken C, Coons M, Peters M, et al UserCentered Design of a Mobile App for Weight and Health Management in Adolescents with Complex Health Needs: Qualitative Study. JMIR Form Res 2018 Jan 1;2(1)
The Brain Injury diScharge infOrmatioN (BISON) project was led by UEA in collaboration with James Paget University Hospitals NHS Foundation Trust and The Queen Elizabeth King’s Lynn Hospitals NHS Foundation Trust, along with community partners including Headway Norfolk & Waveney and the Norfolk and Waveney Acquired Brain Injury Network.
This initiative aimed to address the inconsistency and inadequacy od discharge information for patients with mild Traumatic Brain Injury (mTBI) across NHS Trusts in the East of England
Despite the high incidence of mTBI and its potential progression to PostConcussion Syndrome (PCS), which can severely impair quality of life, existing discharge processes varied significantly in quality and accessibility
BISON developed a concussion information leaflet in partnership with Headway for their Concussion Awareness Campaign and a prototype for a web-based portal that provides symptom-dependent personalised guidance for mBTI patients These resources aimed to empower patients with accessible information to manage their recovery effectively.
However, the landscape of concussion management is rapidly evolving, with several competitors developing more refined solutions
By the project’s end, it was acknowledged that alternative apps and tools in the market, such as Concussion
Tracker App developed by the Canadian company Complete Concussions, provided more comprehensive and userfriendly options
Traumatic Brain Injury (TBI) is a global health problem with approximately 27 million new cases worldwide each year
In England and Wales approximately 1.4 million people present to A&E departments annually following a head injury. Mild TBI (mTBI) account for 8095% of all TBIs
Although most individuals with mTBI recover fully, there is an estimated 25% who develop persistent severe effects lasting more than one year, a condition known commonly as Post-Concussion Syndrome (PCS).
Individuals may have a wide variety of life-limiting neurocognitive symptoms including extreme fatigue, sleep disorders, memory and attention deficits.
In 2019, the Concussion Action Programme (CAP) Research Group produced a UEA Health and Social Care Partners-funded scoping review of the mBTI Provision in the East of England
A key finding was a large variation in both content and quality of discharge information provided following attendance at A&E within regional NHS Trusts
It was recommended that discharge information following mild traumatic brain injury (mBTI) should be regionally consistent and accessible, including making it available online, across all NHS Trusts
Whilst guidelines exist for return to play/study within the sports medicine community, this specialist information is not accessible to the average person.
Until recently, the standard advice was to rest and wait for the brain to recover on its own This advice is not in line with current guidelines as they now understand that progressive activity is beneficial for brain recovery
If patients are provided with accessible return to activity information on discharge, they will be empowered to promote recovery safely and will know when to seek help should they not recover at the expected rate

The UEA Health and Social Care Partners funded report on mild traumatic brain injury provision in the East of England made the following key recommendations:
Discharge information following mild Traumatic Brain Injury (mBTI) should be regionally consistent and accessible, including making it available online, across all NHS Trusts
Implement an automated follow-up process for discharged mBTI patients to identify any post-injury sequelae
Conduct research in the area of PCS following mBTI, specifically focusing on early identification and management
Written information (including red flags to watch out for and basic return to study information) should be given to students and their parents or carers following a head injury incurred at school
Concussion or head injury training should be made mandatory for all physical education teachers to complete
Investigate the need for a specialised regional concussion clinic
BISON’s aim was to employ a usercentred design strategy to develop a mBTI discharge information portal for patients who are discharged from the A&E.
Elizabeth King’s Lynn Hospitals NHS Foundation Trust in addition to PPIE representatives from Headway
Their initial work with these groups led to the production of a concussion information leaflet for Headway’s Concussion Awareness Campaign
BISON next developed a first prototype for a web-based portal symptomdependent personalised guidance for mBTI patients to use on discharge from the A&E, the Ambulance Service or their GP The portal implemented goldstandard return to activity guidance developed in the sports medicine community
Following the 2021 Parliamentary Inquiry into Sport Concussion, the government responded by commissioning a set of guidelines for concussion management in grassroots sport These guidelines were implemented into the portal.
Toward the end of the project, the BISON project learned that the team led by Laurence Geller – appointed following the inquiry as ministerial advisor on concussion – had made the decision to promote a Canadian company who designed the “Concussion Tracker App”. Comparing the two approaches, their PPIE group had a strong preference for the app-based solution.
They engaged with clinicians from James Paget University Hospitals NHS Foundation Trust and The Queen
Concussion is a fast-paced space and there are now a few applications on the market with completing solutions from

companies including Complete Concussions, Return-2-Play, Podium Analytics, and a new Cambridgedeveloped app soon to be on the market Of the three, in the BISON team’s opinion Complete Concussions is currently the best solution.
The next step in this programme of research is to focus on the management of concussions in the University student and staff populations Research at Loughborough University shows that university students express limited knowledge of concussion and undertake risky behaviours
Support across and within university campuses is variable. Some institutions have online concussion resources (e g Cambridge), and better access to medical clearance enabling quicker return to activity (e g Nottingham)
However, no UK HEI has yet fully engaged with the concussion agenda
The vision is to develop the gold standard for concussion support within UK HEIs and then roll this out to other sectors
Click here to read the UK Concussion Guidelines for Non-Elite (Grassroots) Sport.

CHARMING is a project to co-produce interventions supporting multiple behaviour change in socially deprived communities.
It focuses on the ‘big four’ behaviours:
Unhealthy diets
Smoking Physical inactivity
Excessive alcohol consumption
Service users, practitioners, researchers and policy makers will identify best practice and reach consensus on promising interventions.
It is hoped that healthcare practitioners and others who support multiple behaviour change are better able to reach those who can benefit the most, use evidence-based approached and empower people to make positive changes for their health and well-being.
People in affluent communities live on average 19 years longer in good health than people in low-income communities. This is largely due to behavioural risk factors, e g : dietary behaviours, physical activity, and smoking
These risk factors cluster, especially in communities of high socio-economic disadvantage
The CHARMING project aimed to identify and co-produce promising approaches to support multiple behaviour change in these communities.
They spoke with 42 stakeholders (e g : local government, community organisations, NHS) and held group conversations with 36 people with lived experience of self-managing behaviour change in difficult circumstances
They found that the cost-of-living crisis and poverty greatly affected capability and opportunity to make positive changes in health behaviours
Communities mentioned siloed services and lack of trust in health professionals and current services.
They wanted empathy and being asked what matters most to them to facilitate behaviour change; behaviour change support embedded in enjoyable, sociable activities; creative approaches to

encourage informal conversation; and sequential behaviour change support CHARMING recommended that commissioners reduce silos between services, offer more behaviour change support in communities and strengthen VCSE
They recommend that researchers coproduce, with communities, promising approaches to supporting multiple behaviour change, which are asset-based and holistic, using non-traditional methods (e.g.: creative and social).
Unhealthy diets, tobacco smoking, physical inactivity, and excessive alcohol consumption (‘the big four’) are responsible for ~50% of the population attributable fraction of years of life lost in the UK (Steel et al , 2018), with a large economic impact.
People in communities of high socioeconomic disadvantage are much more likely to engage in all four unhealthy behaviours (King’s Fund, Clustering of Unhealthy Behaviours over Time, 2012)
Behavioural risk factors largely explain the 19-years difference in healthy life expectancy and two times higher years of life lost from all causes between lowincome and the most affluent communities (Marmot Review Ten Years On, 2020, Steel et al , 2018)
People in the most deprived areas spend nearly a third of their lives in poor health; worsened by the Covid-19 pandemic (King’s Fund, What is Happening to Life Expectancy in England? 2021)
In communities of high socio-economic disadvantage, behavioural risk factors
can present as coping mechanisms to mental ill health and markers of distress and poverty (Hanson et al , 2019)
It has been known for 10+ years that unhealthy behaviours cluster, but still do not know how best to support multiple behaviour change (NICE, Public Health Guideline 49, 2014).
In “Tackling Multiple Behaviours” (2018), the King’s Fund reported “academic evidence on how best to tackle multiple unhealthy behaviours remains weak more can be done at national level to invest in research in this area but the quickest win is to support local areas providing these services to learn and self-evaluate in practice”
Therefore, the CHARMING project aimed to identify promising interventions to support multiple behaviour change among people living in communities of high socio-economic disadvantage.
They held conversations with 42 stakeholders from multiple agencies and group conversations with 39 people with lived experience in community assets
CHARMING identified the following key themes from the conversations with the communities and the stakeholder organisations which support them:
The cost-of-living crisis and poverty reduce people’s capability and opportunity to make positive
changes in health behaviours.
People are unable to prioritise their health given crisis circumstances; support by current services does not reach them
Key barriers to multiple behaviour change (see figure below based on conversations with stakeholders and communities, respectively):
Wider socio-economic determinants (e.g.: poverty).
Lack of face-to-face contact, appropriate guidance, and access for at-risk people within health/community services
Environmental barriers, both physical and social
Personal barriers: low self-esteem, mental health, lack of knowledge and skills
Insufficient behaviour change support for people not at crisis.
Communities lack trust in health professionals and current services
Services are siloed, without collaboration or integration
Signposting and referring to support are insufficient and sometimes confusing
Build trust and foster empowerment
Show empathy and understanding. Ask what matters most
Discuss how behavioural change could help the person achieve what they value
Offer financial incentives.
Set achievable goals and build on success
How to support multiple behaviour change
People want sequential support
Dietary behaviours and physical activity go together.
‘Starter behaviour’ varies across people
Highlight positive consequences of changing start behaviour (e g : better mood, energy, saving money, role model) which may enable further change
Embed healthy behaviour change support in enjoyable, sociable activities – not targeting a problem behaviour directly
Have fun, try something new, use creative approaches to encourage informal conversation
Harness the social element: doing things with others to sustain engagement
One-to-one supplemented with group sessions

Stakeholders also mentioned other behaviours (not shown) which impact on the ‘big four’, e.g., gambling, substance use.
Community consultations also highlighted the role of conflicting priorities and a sense of being overwhelmed by the thought of changing health related behaviours, manageable goals were often described as the most effective ways to change behaviour.
The project has generated multiple recommendations for commissioners and researchers which are outlined below. In addition, CHARMING has formulated recommendations for community and clinical practice which can be found by visiting the CHARMING project’s webpage
The recommendations for commissioners are:
More integrated and holistic behaviour change support
Reduce silos between services: offer integrated behaviour change support, a ‘one-stop’ shop.
Use a person-centred (wrap around) approach instead of a service centred approach.
Focus on one behaviour first, based on what matters most to the person
Reduce silos between services: offer integrated behaviour change support, a ‘one-stop’ shop
Focus on one behaviour first, based on what matters most to the person
Train the workforce in starting a supportive conversation around behaviour change
Signposting and referring to support is insufficient
More behaviour change support in communities
Strengthen the role of community hubs as support networks.
Train the workforce in starting a supportive conversation around behaviour change
Offer group-based support in communities, supplemented with 1:1 support
Reduce silos and strengthen VCSE
Strengthen integration and collaboration between services
Commission community-based, holistic, person-centred behaviour change support.
Provide sufficient longer-term funds to support VCSE in delivery
1
2
Use a person-centred (wrap around) approach instead of a service centred approach
3
4
5
6
7
8
Strengthen the role of community hubs as support networks
Offer group-based support in communities supplemented with 1:1 support
Reduce the burden of VCSE by increasing access to funding and resources
Strengthen integration and collaboration between services
9
The recommendations for future research are:
Co-produce promising approaches to supporting multiple behaviour change
Co-produce interventions in multiagency partnerships
Develop holistic interventions providing person-centred support.
oIncorporate trauma informed approaches
Sequential rather than parallel behaviour change
Incorporate strength-based approaches to foster hope and empowerment
More research into community assetbased interventions
Embed interventions into enjoyable activities with a social element.
Deliver interventions in existing community assets
Use group-based approaches plus 1to-1 support
Use fun and creative approaches.
Development and evaluation of holistic and asset-based interventions, using nontraditional methods
Pilot and evaluate non-traditional methods (e g : creative and social) to increase research engagement
Develop and evaluate holistic and asset-based interventions for multiple behaviour change
Develop relevant and meaningful outcome measures
Co-produce and deliver interventions in multi-agency partnerships and existing community assets 2 Develop holistic interventions which deliver person-centred support for multiple behaviour change
1
The CHARMING project’s outputs have been well received by their partners and have informed conversations about commissioning around preventative services and interventions, for example: Suffolk County Council
The CHARMING project has directly informed research funding bids. They were awarded an NIHR-funded Programme Development Grant [NIHR205176] called CHERISH, which identifies, pilots and evaluates nontraditional approaches (e g : creative and social), in partnership with community organisations
Insights from the CHARMING project have also informed a stage 2 bid for an NIHR Programme Grant for Applied Research (under review) of MedEx, a community-based eating behaviour and physical activity intervention to maintain cognition and reduce dementia risk, in terms of engaging communities of high socio-economic disadvantage in behaviour change research
For more information on The Co-production of Promising Interventions to Support Multiple Behaviour Change in Socially Deprived Communities Project, please visit our website

WALKACISE seeks to develop and implement a new mobile app aiming to improve the health of patients with Peripheral Arterial Disease (PAD).
Exercise therapy is a key component to support people with PAD. This research project aims to increase the adoption of a new mobile phone app which uses GPS tracking to monitor patients’ walking distance, allowing healthcare professionals to analyse results and track improvements over time. This data enables clinicians to provide more individualised support to people with PAD due to an enhanced understanding of an individual’s maximum walking distance.
Patients with cramps in their legs when they walk often have a poor blood supply termed peripheral arterial disease. The first-line treatment option for this condition is exercise therapy to improve the blood supply.
NICE guidelines recommend supervised exercise therapy, however this is very poorly provided in the NHS with only 40% of hospitals having a programme, and only 25% attending even when they do
A new method of delivering exercise
therapy is needed to make it more accessible The Walk-a-Cise mobile phone application enables remotely monitored exercise therapy, that patients can undertake at a time and place convenient to them. Using GPS tracking, walking distances can be accurately measured, and monitored by their healthcare professional.
This project has expanded the use of the prototype Walk-a-Cise app across the East of England, and also enabled both patient and public input, and stakeholder input into the design and development of the new version of the app, which is now UKCA marked, registered with MHRA, and being further spread across the NHS
Every year over 6000 people lose a leg due to blocked blood vessels. Typically there are signs of blocked blood vessels much earlier than this, and with the right lifestyle changes this can be prevented.
Early treatment including blood thinning medications, cholesterol lowering tablets and stopping smoking can help to prevent this disease progressing, however in order to improve the blood supply to the leg patients need exercise therapy.

Exercise therapy is hard These patients get cramps in the calf muscle when they walk, due to a build up of lactic acid For new blood vessels to develop patients need to walk through that pain as much as possible
Unfortunately, most hospitals do not have an exercise therapy programme In Norfolk and Norwich University Hospitals NHS Foundation Trust, they have an exercise therapy programme, however this covers the whole region, include patients who attend The Queen Elizabeth Hospital King’s Lynn NHS Foundation Trust and James Paget University Hospitals NHS Foundation Trust. This means patients would have to travel
up to 50 miles each way to attend, and therefore only a quarter of patients actually come This situation is the same throughout the UK, therefore the NHS is not providing the recommended care to the majority of their patients
The efficacy of supervised exercise therapy to improve walking distances, functional status and Quality of Life has been established A Cochrane review of 21 studies revealed that supervised exercise therapy improves maximal walking distances by approximately 120 to 210 metres when compared with home-based exercise therapy and walking advice
A network meta-analysis also showed that supervised and home-based
exercise therapy improved daily physical activity levels
When comparing endovascular revascularisation and supervised exercise therapy there was no statistical difference between these groups, suggesting that supervised exercise therapy is as good as endovascular revascularisation, especially in long term outcomes
Despite the encouraging evidence supporting SET, it is an underutilised tool with low availability, uptake and adherence
In a recent US study only 1 3% of those diagnosed with peripheral arterial disease were enrolled to supervised exercise therapy and only 5 1% successfully completed the program
A survey conducted in 2021 revealed only 4.8% of vascular units have access to SET in the UK and only 22% meet NICE recommendations with patient uptake rates around 25%.
Funding is a key barrier for the lack of accessibility (94.3% in the 2016 survey), followed by a lack of suitable staffing, facilities and expertise.
Patient-specific barriers that may prevent a patient from partaking include compliance (affected by travel arrangements, inconvenience, and cost), lack of motivation, trivial improvements and medical co-morbidities (such as
Tracking-based technologies have been studied for patients with peripheral arterial disease previously.
This includes using Smart Watches, and mobile phones Walk-a-Cise undertook a recent meta-analysis which identified 15 studies using either Smart Watches or free apps
Analysing that data statistically through a meta-analysis identified that these technologies increased patient walking, defined as 6-minute walk test, claudication onset time, peak walking time, maximum walking distance, and through scores on the walking impairment questionnaire and quality of life.
However, these apps and watches will not work outside of small clinical trials due to lack of healthcare professional
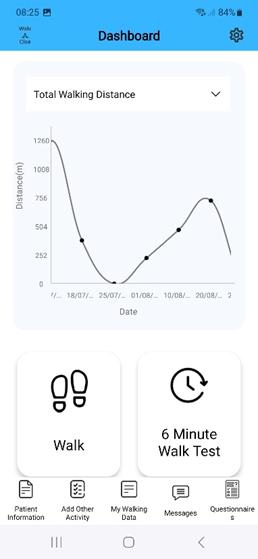

connectivity, and reproducibility on a large scale.
The Walk-a-Cise app has been used in Norfolk and Norwich University Hospitals NHS Foundation Trust, and early uptake data identified overall 66% of eligible patients were enrolled GPS walking distance was significantly lower than GPS distance (202.63m v 509.37; p=0 0002)
Walking distance has significant implications in decision making regarding surgical intervention in these patients
Over the duration of use of the app, participants increased their walking distance by a mean difference of 163 43m Some barriers to uptake were identified including lack of availability on Apple phones (now addressed), and 26% didn’t have a smartphone
The Walk-a-Cise mobile phone application has undergone significant development, through further funding from Innovate UK, based on the patient and public involvement and stakeholder groups undertaken during the UEA Health and Social Care Partnership funding.
The app has also been rolled out to additional hospitals, with these hospitals now being updated to the new version of the app, and further dissemination to the wider NHS
Feedback suggested converting the app into a treatment rather than monitoring platform The main components of this included not only ensuring GPS accuracy, but also including a wider range of walking outputs, such as claudication onset distance, claudication onset time, total walking distance, and maximum walking distance. In addition, Walk-a-Cise has developed a 6-minute walk test Each of these outputs are commonly published in the literature and used for monitoring purposes
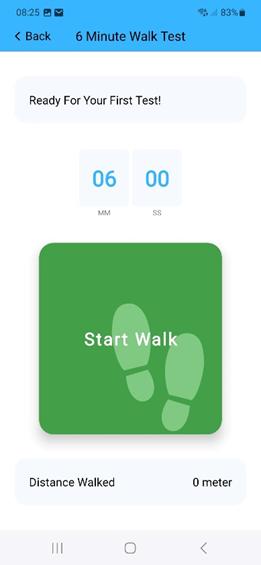
The app now also includes a communication platform so that patients can contact their healthcare professional directly, avoiding unnecessary delays should they deteriorate, enables input of other exercise activities, and can connect with the users Smart Watch
The component that transforms the new app into a treatment, and therefore required registering with MHRA and obtaining Class 1 UKCA mark status was the development of bespoke animated
exercise classes. Animations were developed based on national guidelines, with Jon Dunleavy at the Norwich University of the Arts leading, and codesign being undertaken alongside the Vascular Society Peripheral Arterial Disease Special Interest Group These are at 5 levels of difficulty, with patients able to work through these until they reach the appropriate level for them
Animations were developed based on national guidelines, with Jon Dunleavy at the Norwich University of the Arts leading, and co-design being undertaken alongside the Vascular Society Peripheral Arterial Disease Special Interest Group.
The Walk-a-Cise mobile phone application is now ready for uptake throughout the NHS, and the next stage is to monitor uptake and outcomes on an individual hospital level, and spread throughout the UK and beyond
The Walk-a-Cise mobile phone application is now ready for widespread adoption At present this is undertaken at a hospital level, where patients have already got significant peripheral arterial disease warranting referring to a vascular surgeon
They believe that intervening earlier in the pathway will further reduce the need for referral, and reduce the need for invasive surgical intervention. They team would therefore like to trial the app within the community, working with Integrated Care Boards to enable GPs to refer to the app directly with oversight from community support such as leisure centres and health hubs
Walk-a-Cise are developing the app further to include additional patient groups, such as paediatric obesity and cardiology, where remote exercise therapy can also be used as part of their treatment plan.

A national clinical trial utilising the Walka-Cise app is being developed to compare the app to supervised exercise therapy and home-based exercise therapy
Key Publications
https://www nice org uk/guidance/cg147/ chapter/Recommendations#managemen t-of-intermittent-claudication
www.ncbi.nlm.nih.gov/pmc/articles/PMC 6513337/
www ejves com/article/S10785884(18)30923-7/fulltext
https://pure coventry ac uk/ws/portalfile s/portal/29651511/Binder5 pdf
www ncbi nlm nih gov/pmc/articles/PMC 9941040/

For more information on the mHealth for Patients with Peripheral Arterial Disease Project, please visit our website
ANSWERS is an observational cohort study, aiming to collect early comprehensive mental health and social determinant information across multiple timepoints with 250 representative young people with pre-existing mental health needs across Norfolk and Suffolk.
The information collected will provide ANSWERS with data about what is important to young people, what helps and impacts their mental wellbeing from social needs and neighbourhood perspectives, and how this relates to their health service use. ANSWES will also plan to assess if this routine collection and understanding of service user health and socioeconomic factors supports system-wide MH organisations with policy and delivery during COVID19 recovery.
Adolescence and early adulthood are periods that are developmentally critical for mental health This is influenced by external global factors such as the COVID-19 pandemic and anxiety around climate change The ANSWERS project included a literature review, the collatioN of national and local data from the
perspectives of young people, their families and healthcare professionals, and focus groups with young people in Norfolk and Suffolk to synthesise views and experience on what supports their mental health and that of young people more broadly
Results show that young people identify many strategies that they do independently to protect and maintain their mental health and are aware of needing to support each other
Young people asked for more mental health awareness in schools, for therapeutic input to be more individualised, and they valued being truly listened to and heard by professionals. The pros and cons of on-line vs inperson mental health advice and support was discussed
Adolescence to young adulthood is an important period of development, characterised by biological, cognitive, psychosocial, and emotional changes alongside expected key life transitions such as continuing education and starting employment

This presents a critical period for the onset of mental health disorders (Kessler) Young people today face many challenges for their mental health, including exposure to global news and a huge amount of information (both factual and speculative) via an increasingly connected world afforded by the Internet.
Recent world-events, including the COVID-19 pandemic, the war in Ukraine, and concerns about climate change are known to have impacted mental health (Singh, singh, van Nieuwenhuizen, meherali) To support young people, it is important to understand what factors positively impact their mental health and wellbeing
Exploring young people’s perspectives on their mental health will allow a more person-centred knowledge of how best to support them
ANSWERS’ study aims to understand the perspectives of young people on what helps their mental health since the peak of the CVOID-19 pandemic The bracket of young people is defined for this report as ages 11-25 years old, as per the UK (14)
ANSWERS kept a broad scope for these discussions (encompassing services, community activities, social networks, and personal coping strategies) to gain a holistic view of the avenues to which young people turn to help their mental health
Existing qualitative data on what helps young people’s mental health during and since the pandemic, from the perspectives of young people, their families and their healthcare professionals was collated Firstly, through a scoping review searching data within the UK, followed by the collation of data local to Norfolk and Suffolk.
The scoping review searched PsychINFO, Embase, MEDLINE, and CINAHL searching within the timeframe of 01/03/2020 – 19/07/2022 using search strings of mental health, youth, qualitative methodology and COVID-19 Eleven studies fit criteria (1-4, 6, 7, 9, 1012, 15) The following themes emerged of what young people found helpful during and since the COVID-19 lockdown:
Young people turned to mental health services, where online provisions of services offered consistency, structure, and connection; allowing people to engage to the extent they were most comfortable with and for some, removing access barriers (1, 4, 9)
Some young people reported accessing mental health support from educational facilities or the workplace, in the form of staff offering practical support such as deadline extensions and wellbeing leave, as well as wellbeing check-ins and increased awareness of mental health (7)
Lockdown afforded the opportunity for
families and friendship groups to have more open, direct, and sensitive conversations, which fostered better connections (3, 6, 7, 9). This acted as a support mechanism for young people’s wellbeing For those living at home, some young people felt that they were feeling closer with family due to the time lockdown enabled them to spend together (6, 7, 9, 10, 15)
Young people also turned to technology to help cope, maintaining a sense of social connectedness, and accessing support networks (3, 6, 7, 11, 15)
Young people participated in self-care practices such as prioritising more time to focus on their wellbeing, relaxation, self-reflection, controlled breathing, mindfulness, and meditation (4, 6, 7, 9, 15)
Additionally, young people reported better sleep during lockdown and linked this key lifestyle factor to their mental health (4, 6, 7).
The collation of local secondary data from published reports prepared by third-sector organisations, health support and council bodies (that gathered qualitative data from perspectives of young people), their families or mental health professionals resulted in the following themes:
School Staff: Young people wanted to be listened to by staff in
education, for staff to respect and value minorities’ rights, and to be approachable to that they felt able to ask for advice or support. Young people expressed wanting more mental health awareness being raised in schools including busting myths that contribute to stigma
School Structure: Young people suggested changes to school structure such as later starts and breaks between lessons would benefit their mental health via reduced sleep deprivation and time to process what they’ve learnt and clear their minds
Support to Support: Young people wanted to get more help and advice on how to support peers with their mental health.
Technology: Regarding accessing support, young people cited their preference as being a blend of human interaction initially, followed by technology
To better understand the perspectives of young people in Norfolk and Suffolk about strategies for supporting their mental health and wellbeing, ANSWERS spoke to 10 young people who had accessed or attempted to access formal support for their mental health across 3 focus group discussions.
Discussion topics were informed from the outcomes of the literature scoping review and secondary data review Groups were video/audio recorded, transcribed and analysis thematically
Participants were recruited through MAP, an NHS peer participation group and Headucate Data was collected from 10 participants 3 participants were aged 11-15, 7 were aged 16-25 2 participants were males and 8 females (from observational data)
Themes are presented below (corresponding quotations in Appendix 1):

From the perspectives of young people, “wellbeing” as a concept was defined as distinct from mental health in that wellbeing encompasses more aspects of their mental health including physical health
A theme of having knowledge/awareness emerged, including insight into the definition of wellbeing for young people as being the concept of having selfawareness of how they feel and what to do if they don’t feel okay
Young people reported enjoyable activities (such as going on walks, interacting with pets) helped their mental health through the self-reported mechanisms of grounding, bringing joy and comfort
Within this, being outside was a helpful strategy for supporting their mental health by bringing a sense of freedom, not feeling trapped and giving space to breathe.
Creativity was recognised as helpful through facilitating young people to process the things that they’ve experienced and the vast quantity of news/information they take in, as well as being a form of expression Journalling was recognised as being helpful through similar mechanisms (processing and selfexpression) with an added emphasis on not having to hide anything.
Young people reported that they chose to seek formal help when they experienced an extended period of no improvement in how they felt or if others in their life raised concern Barriers to seeking help included young people thinking they must be self-harming or suicidal to seek help, exacerbated cultural messages that it is weak to seek help or minimising messages from adults towards young people which confuse what is normal and what warrants help
Emphasis was given to the impact of being properly listened to as an individual and having input that feels tailored to them individually rather than being treated as though they are the same as others (for example, just because they have the same diagnosis)
Being given the choice of remote and inperson therapeutic input was recommended to combine the strengths of both (cited as human connection and accessibility, respectively) Young people asked for support managing overexposure to information and how to help their peers with their mental health Educational staff were identified as playing a big role in mental health support
A collated from the literature review, documentation review and focus group
work, results show that young people have many strategies that they use on a personal level to maintain their mental health and wellbeing, including creativity and use of outdoor spaces
Emphasis was put on these techniques giving them the space to think, process and express themselves. This feels
Young people valued being properly listened to and reported that currently school staff can be minimising of their struggles.
Mental health awareness training and basic mental health skills may be indicated for education staff to better support young people and to facilitate healthy and open interactions about wellbeing

amount of information they are exposed to (through school and the Internet, and their peers)
The findings indicate that educational staff having mental health awareness and ability to support with mental health would be valued. This was present in the national data and local secondary data as well as the local primary data collected via focus groups
Use of technology for formal support was also present across all three models of data, with the consensus being that there is space for both, with timing and choice being critical to feeling empowered
Therapeutic input was valued most when it started with face-to-face to build rapport and create human connection, with technology coming in later as helpful
for being able to stay consistent despite practical barriers Overall, focus group data emphasised wanting to be given the choice between modes, given that preference varies on individual circumstance
Local young people identified the need for help with how to support their peers with their mental health as well as help to know how to navigate consuming and caring about the worldwide information afforded through the Internet (identified from both secondary data and primary data)
Young people showed a sense of caring and wanting to be able to help in these areas, which may impact their wellbeing when they feel helpless to change or impact these situations
Future research would benefit from continuing to engage young people to ascertain what their perspectives are on their mental health in a post-COVID-19 world and how to best support them from their perspective.
Research on young people’s mental health would benefit from further focus groups with young people on a larger scale to include a more representative sample, learn more about peer support strategies, and work with schools, health services and other support systems to support increased mental health awareness and communication training
1 Cummings, A (2023) The views of mental health professionals who use digital methods to support careexperienced young people Practice, 35(2), 121-136
2 Critchley, E , Cuadros, M , Harper, I , Smith-Howell, H., & Rogish, M. (2021). A parent-sibling dyadic interview to explore how an individual with Autism Spectrum Disorder can impact family dynamics Research in Developmental Disabilities, 111, 103884
3 Dedryver, C C , & Knai, C (2021) ‘It’s Easily the Lowest I’ve Ever, Ever Got to’: A Qualitative Study of Young Adults’ Social Isolation during the COVID-19 Lockdowns in the UK. International journal of environmental research and public health, 18(22), 11777
4 Dewa, L H , Crandell, C , Choong, E , Jaques, J., Bottle, A., Kilkenny, C., ... & Aylin, P (2021) CCopeY: a mixedmethods coproduced study on the mental health status and coping strategies of young people during COVID-19 UK lockdown Journal of Adolescent Health, 68(4), 666-675.
5. Kessler, R. C., Berglund, P., Demler, O., Jin, R , Merikangas, K R , & Walters, E E (2005) Lifetime prevalence and age-ofonset distributions of DSM-IV disorders in the National Comorbidity Survey
Replication Archives of general psychiatry, 62(6), 593-602.
6. Marques, S. S., & Braidwood, R. (2021). Impact of the coronavirus lockdown on older adolescents engaged in a schoolbased stress management program: changes in mental health, sleep, social support, and routines Children & Schools, 43(4), 198-208
7. McKinlay, A. R., May, T., Dawes, J., Fancourt, D , & Burton, A (2022) ‘You’re just there, alone in your room with your thoughts’: a qualitative study about the psychosocial impact of the COVID-19 pandemic among young people living in the UK BMJ open, 12(2), e053676
8. Meherali S, Punjani N, Louie-Poon S, Abdul Rahim K, Das JK, Salam RA, Lassi ZS Mental Health of Children and Adolescents Amidst COVID-19 and Past Pandemics: A Rapid Systematic Review
Int J Environ Res Public Health 2021 Mar 26;18(7):3432
9. Mindel, C., Salhi, L., Oppong, C., & Lockwood, J (2022) Alienated and unsafe: Experiences of the first national UK COVID‐19 lockdown for vulnerable young people (aged 11–24 years) as revealed in Web‐based therapeutic sessions with mental health professionals Counselling and psychotherapy research, 22(3), 708-724.
10 Rogers, G , Perez‐Olivas, G , Stenfert Kroese, B., Patel, V., Murphy, G., Rose, J., & Willner, P (2021) The experiences of mothers of children and young people with intellectual disabilities during the first COVID‐19 lockdown period Journal
of Applied Research in Intellectual Disabilities, 34(6), 1421-1430
11. Scott, S., McGowan, V. J., & Visram, S. (2021) ‘I’m Gonna Tell You about How Mrs Rona Has Affected Me’ Exploring young people’s experiences of the COVID-19 pandemic in North East England: A qualitative diary-based study. International journal of environmental research and public health, 18(7), 3837
12 Shoesmith, E , Shahab, L , Kale, D , Mills, D S , Reeve, C , Toner, P , & Ratschen, E (2021) The influence of human–animal interactions on mental and physical health during the first COVID-19 lockdown phase in the UK: A qualitative exploration International Journal of Environmental Research and Public Health, 18(3), 976
13 Singh, G , & UthayakumarCumarasamy, A (2022) Cost of living crisis: a UK crisis with global implications–A call to action for paediatricians BMJ paediatrics open, 6(1).
14 The YIACS Model Youth Access (https://www.youthaccess.org.uk/ourwork/championing-our-network/yiacsmodel#:~:text=Our%20members%20are %20rooted%20in,housing%20and%20so %20much%20more)
15 Thompson, J , Spencer, G , & Curtis, P (2021) Children's perspectives and experiences of the COVID‐19 pandemic and UK public health measures Health
Expectations, 24(6), 2057-2064.
16 van Nieuwenhuizen A, Hudson K, Chen X, Hwong AR. The Effects of Climate Change on Child and Adolescent Mental Health: Clinical Considerations
Curr Psychiatry Rep 2021 Dec 7;23(12):88 Singh, G , Xue, S , & Poukhovski-Sheremetyev, F. (2022).
Climate emergency, young people and mental health: time for justice and health professional action. BMJ paediatrics open, 6(1)
Acknowledgements
The research was funded by UEA Health and Social Care Partners (UEAHSCP).
The views expressed are those of the author(s) and not necessarily those of the University of East Anglia or UEA Health and Social Care Partners
Appendices
Appendix 1
Quotes corresponding to each theme
Definitions
“For me personally, wellbeing is about being OK, feeling OK, mentally, physically and emotionally, I put all three of that on to well-being.”
“feeling OK and knowing what to do if you aren't feeling OK”
the walking gives a sense of feeling free, more able to breathe and not having to think”
“I think the aspects of grounding that these activities bring it just like brings you back to kind of yourself because it's so easy to lose yourself doing just constant assignment after assignment, task after task So just coming back in like, I don't know, like just having like 5 minutes playing with your dog is like you ' re just like, oh, like, this is what makes me happy This is what- who I am This is, you know, I think that's just important aspect to hold on to To keep motivated about just doing life.”
“I write poetry and lyrics as of way of communicating and processing and and I'm very bad at it but I dance like try to dance whenever I can to maintain my physical health and my mental health and again to really help me make sense of what is going on around me and and process it”
Accessing formal support
“I just had had no information on [mental health and when to seek support] at all I didn't know what was normal. I thought it had to be, like, at the level where you ' re contemplating suicide before you sought support, I thought it was only reserved for extreme cases ”
Experiences of support
Helpful personal strategies
“for me my dog is a source of comfort,
“the ones that [a]re helpful activly listen to what your saying [sic] … the unhelpful ones just brush it off and direct you

elsewhere and they act really disinterested”
[response to question: what message would you give to those in charge of the mental health services] “that not everybody is the same, two people have have anxiety but it doesn’t mean they act the same way. ”
Recommendations for support “Being forced to be in person / online isn’t always great, an option would be preferred”
“One of my closest friends developed anorexia … and I had no idea what that was I had no idea how to deal with it I was just absolutely clueless and without, you know, trying, you know, without being told about these sorts of things and how- what you can do to help and how you talk to people in a way that's non-judgmental and listening and the importance of all of that, it’s just so important because I was just a terrible friend to her for that year Because I just didn't know what to do. And I think that happens in a lot of cases because you just don't know what to do When you ’ re not, you haven't been told, you know.”
For more information on the Assessing the Social Needs and Wellbeing of Young People with Preexisting Mental Health Needs Post-COVID-19 Pandemic Project, please visit our website
The CELDA study investigated the poor care received by people with learning disabilities and/or Autism in residential care homes which subsequently closed, alongside the trauma that the staff supporting them experienced whilst supporting these closures.
Since June 2020, the Learning Disability service at Norfolk County Council has seen the closure of over 20 residential homes for people with a Learning Disability in Norfolk (approximately 100 vulnerable adults being affected by this).
Over half of these have been due to poor care and intervention from the Care Quality Commission or Norfolk County Council. Several of these closures have been traumatic, with individuals receiving “inhumane treatment” and other alleged abuse taking place
The staff managing these closures have had to support individuals in the care environments who have been the victims of, at minimum, poor care or have experienced abuse of some form
This study used focus groups to investigate the challenges of closing a
care home using a debriefed participant cohort and a non-debriefed cohort
A debriefing occurs in teams and is a discussion of the events in the workplace to assist learning (Evans et al., 2023).
They give staff an outlet for their emotions. As there is an inconsistent practice of using debriefing for home closures, it was considered prudent to collect data surrounding the wellbeing and emotional outcomes of those who had been debriefed vs those who had not been debriefed to add to this body of work and potentially create long-term protocols within Norfolk County Council related to debriefing practices
The debriefs have always been held in person and are Multi-Disciplinary; Norfolk County Council, Care Quality Commission, Norfolk Community Health and Care NHS Trust and the Norfolk and Waveney Integrated Care Board staff have been invited and included in the sessions
They have been led by a qualified social worker, usually a senior manager who has used the refined template at the end of this chapter
Thirteen participants, six who had undergone a debrief (the debriefed participants) and seven who had not (the non-debriefed participants), engaged in focus groups to compare and contrast the impact of such sessions and how they may have been beneficial for the participants
Two focus groups explored the multifaceted challenges surrounding home closures, delving into emotional and logistical dimensions They found common ground in experiencing feelings of guilt, worry, and frustration stemming from the intricacies of care home closure processes.
Notably, both groups shared a sense of constant burnout and stress, exacerbated by the relentless cycle of care home closures However, the nondebriefed group highlighted an additional layer of pressure: the burden of juggling
multiple responsibilities, leading to feelings of inadequacy and trauma among staff
Logistical hurdles emerged prominently, with both groups identifying sudden moves for residents and poor communication with care providers as major obstacles. The non-debriefed group also flagged resource strain exacerbated by the cost-of-living crisis and the ongoing impact of COVID-19. They highlighted how external factors compounded the challenges of closures, making the situation notable tougher compared to before
Interestingly, discussions about workload intensity only surfaced in the nondebriefed group, revealing how closurerelated stressors directly impacted daily responsibilities Participants discussed the overwhelming amount of work and the subsequent inability to maintain a


healthy work-life balance, exemplified by the constant distraction of urgent emails, even during focus group discussions
Despite these differences, both groups recognised the utility of debriefs in navigating the emotional toll of closures
While the non-debriefed group emphasised the need for compulsory debriefs to address time constraints and enhance staff retention, the debriefed group advocated for regular debriefs as a crucial tool to process emotions and foster a sense of collective purpose
They found debriefs to be invaluable in acknowledging the impact of secondary traumatic stress (STS) and reaffirming their shared commitment to the home closure process and wellbeing of the vulnerable adults they supported
The two focus groups provided nuanced insights into the challenges posed by home closures, shedding light on both shared experiences and different perspectives.
Both groups advocated for mandatory debriefs.
Only the non-debriefed participants noted the impact a home closure had on their pressure and workload recognising the cumulative impact of this and of secondary traumatic stress on staff teams means that debriefs could have a long-lasting impact on staff wellbeing and capabilities
Reduced expectations around quality of care
Practitioners experiencing secondary traumatic stress
Practitioners supporting care environments to improve care
More research is required into the impact that poor care has on visiting professionals such as social workers and community nurses
The future research should consider the impact of witnessing poor care on the expectations these professionals have for caring environments
More research is also required into the best way to support professionals when care homes close, especially where abuse and neglect have been experienced by those living in the service
The long-term impact of secondary traumatic stress is well evidenced and further research into the efficacy of the use of debrief is required
Increased safeguarding referrals
Practitioners observing poor care
Practitioners advocating for people
Health and social care leaders should consider implementing debriefs for care home closures as standard practice to better support their staff’s wellbeing and professional development
It would likely have positive impacts on retention, but further research would be required in this area
It would likely have positive impacts on retention, but further research would be required in this area This is the template used in the debrief session with health and social workers It can also be adapted for others:
For more information on the Care Experience
Improvements for People with Learning Disability and/or Autism Project, please visit our website
Introductions
Recognise trauma and facilitation –reference secondary traumatic stress
Disclaimer about self; qualifications, not therapist, etc
MIND: ‘Secondary’ means that although the original (primary) trauma happened to someone else, the impact it’s having in your life is traumatic for you It doesn’t mean it’s any less significant than any other kind of PTSD, or any easier to deal with Repeatedly witnessing or hearing about traumatic events in the course of your job is also sometimes called ‘secondary trauma’, although this experience is increasingly thought of by professionals as an original (primary) trauma
Recognise not a lessons learnt –no formal outcomes for the session
Recognise people may criticise themselves or others – the only appropriate response to this is “ we can’t be perfect every time” today is not about managing and performance, it is to recognise the illogical nature of emotions and how they do not align with the performance or worth of an individual
Personal trauma increases risk of secondary trauma
Trauma, including secondary, is opportunity for growth –vicarious post traumatic growth
No judgement session
Session is not recorded, is for professional development only; any key actions taken away by facilitator
Word association game: World Cloud
Group work: strengths of the incident/home closure
Group work: worries of the incident/home closure
Group work: What do you like about your job?
Group work: What do you like about the people you work with?
Resilience outside of work: How are we bringing joy to ourselves
Resilience outside of work: What nice thing are you doing this weekend?
A qualitative study was conducted to investigate the poor care received by people with learning disabilities and/or Autism in residential care homes which subsequently closed, as well as the trauma that the staff caring for them experienced whilst supporting these closures
Although the care provided to those with Autism or learning disabilities in residential care homes is poor on a national level, the care has been seen to be particularly poor in care homes in the county of Norfolk.
The graph below displays the ratings of services for people with a learning disability or Autism (Care Quality Commission, 2023).
Out of all the areas included in this data extract, Norfolk had the highest percentage of services rated ‘inadequate’ at 30%, compared to regions like Cambridgeshire at 5% and Suffolk at 4%
This is a graph showing the ‘Ratings of services for people with a learning disability or Autism’ It displayed the ratings of services for people with a learning disability or Autism (Care Quality Commission, 2023)
East of England (859 locations, 811 rated)
Bedford (58 locations, 52 rated)
Buckinghamshire (54 locations, 49 rated)
Cambridgeshire (67 locations, 65 rated)
Central Bedfordshire (37 locations, 33 rated)
Essex (201 locations, 196 rated)
Hertfordshire (137 locations, 127 rated)
Luton (24 locations, 24 rated)
Milton Keynes (34 locations, 30 rated)
Norfolk (118 locations, 110 rated)
Peterborough (26 locations, 31 rated)
Southend-on-Sea (34 locations, 31 rated)
Suffolk (54 locations, 54 rated)
Thurrock (21 locations, 21 rated)
Data extracted on 8th August 2023.
Please note that Care Quality Commission is currently addressing a data issue affecting core service ratings.
It is likely to affect this analysis but there is a small risk to some ratings may be missing
Since June 2020, over 20 learning disability residential homes in Norfolk have been closed due to poor care These closures have been traumatic, with residents receiving indigent care involving claims of abuse (Lambert House – Care Quality Commission, n d , Heathers – Care Quality Commission, n.d.).
Before these closures, press articles were released which discussed the “inhumane treatment” being received by the residents of the homes (Shocking Inspection Uncovers Hidden Abuse at Care Home, 2020; Soanes 2023, Shocking Figures Show One in 10 Norfolk Care Firms Under Watchdog Sanctions, 2023, Warning That Norfolk’s Care Crisis Has Yet to Peak, 2023)
An article from April 2023 stated that Norfolk County Council statistics suggested that care standards in Norfolk were far worse than those in other areas of England (Shocking Inspection Uncovers Hidden Abuse at Care Home, 2020)
CELDA conducted a thematic analysis of ten Care Quality Commission care home reports from 2020-2023 where the care provider had closed due to poor-quality care environment, often led by Care Quality Commission intervention.
The purpose was to:
Better equip Norfolk County Council’s staff to support care providers to improve the quality of care for people with a learning disability and/or Autism
Investigate whether there were any commonalities in what caused these care homes to fail
Understand the context of the participants involved in the study were working in
The analysis resulted in four themes of poor care:
Poor overall culture within the home
Lack of support for staff and managers
Unfit environment to provide good quality care
Ineffective systems in place to provide good quality care
It ultimately found that similar themes of mismanagement over staff and processes occurred in all ten homes; that these issues directly affected those living in the care home and impacted on the staffs’ ability to support people safely and effectively
Based on the thematic analysis themes, a risk matrix was developed for services that may be at risk of providing poor care CELDA believes that the use of this matrix will allow visiting professionals to assess risk more objectively and score it to the same criteria, leading to earlier identification of need and support to improve. Development of risk matrix includes the sub-codes and codes found in the thematic review turned into real world scenarios that practitioners may see whilst visiting care providers
The risk matrix will allow for quick recognition of the quality of the care received by the people living in the service It will allow the service to map out where the difficulties are quickly and signpost to potential improvements.
This can be used by all health and social care professionals and practitioners visiting care homes
Hopefully, it will be utilised nationally as a tool for care providers in the future
More research is required into the efficacy of the risk matrix for how it can assess and predict risk in care environments The risk matrix is backed by this research and professional experience, but it requires more testing in real-world situations
A criticism of this research is the lack of expert by an experienced voice. Service users were not included in this research and further research into their experiences of poor care is required and what insights they could add to further develop the risk matrix
References
Evans, T R, Burns, C , Essex, R , Finnerty, G , Hatton, E , Clements, A J , Breau, G , Quinn, F., Elliott, H., Smith, L. D., Matthews, B , Jennings, K , Crossman, J , Williams, G , Miller, D , Harold, B , Gurnett, P., Jagodzinski, L., Smith, J., Milligan, W , Markowski, M , Collins, P , Yoshimatsu, Y., Turull, J. M., Colpus, M., Dayson, M L and Weldon, S (2023) A systematic scoping review on the evidence behind debriefing practices for the wellbeing/emotional outcomes of healthcare workers, Frontiers in Psychiatry, 14: pp. 1-10.
Care Quality Commission (2023) Quality issues in services for people with Learning Disabilities and Autistic people, Learning Disabilities Network, 16th August 2023
Lambert House - Care Quality Commission (n d ) www cqc org uk Retrieved May 24, 2024, from https://www cqc org uk/location/1120440841/inspection-summary
Heathers - Care Quality Commission (n d ) www cqc org uk https://www cqc org uk/location/1119626780
Shocking inspection uncovers hidden abuse at care home (2020, April 22) North Norfolk News. https://www northnorfolknews co uk/ne ws/22796468 shocking-inspectionuncovers-hidden-abuse-care-home/
Shocking figures show one in 10 Norfolk care firms under watchdog sanctions (2023, April 24) Eastern Daily Press https://www.edp24.co.uk/news/234692 92 care-home-standards-norfolk-sparkcounty-council-concerns/
Warning that Norfolk’s care crisis has yet to peak. (2023, January 10). Eastern Daily Press
https://www edp24 co uk/news/232330 94.warning-norfolk-yet-reach-worstpoint-care-crisis/

Our consortium of partners are organisations in the public, independent and voluntary sector committed to leading sustainable change in health and social care services.
East Suffolk and North Essex NHS Foundation Trust
James Paget University Hospitals NHS Foundation Trust
NHS Norfolk and Waveney Integrated Care Board
NHS Suffolk and North East Essex Integrated Care Board
Norfolk and Norwich University Hospitals NHS Foundation Trust
Norfolk County Council
Norfolk and Suffolk NHS Foundation Trust
The Queen Elizabeth Hospital King's Lynn NHS Foundation Trust
University of East Anglia
West Suffolk NHS Foundation Trust
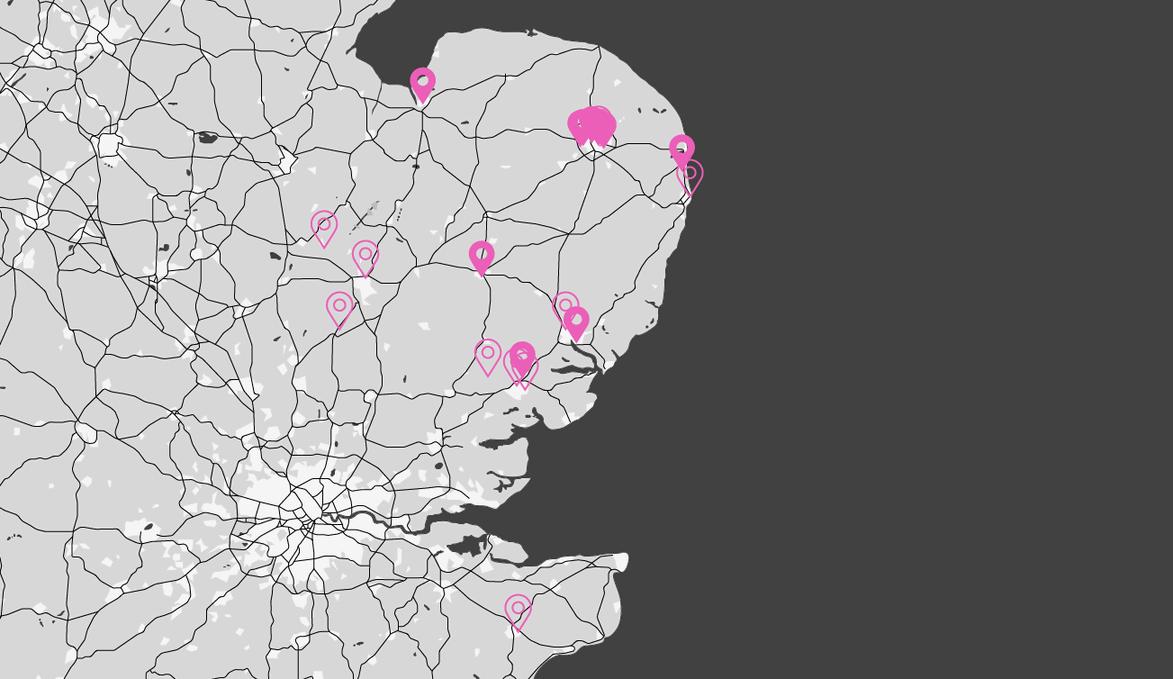
Benefits of Associate Membership
We have strong collaborative networks with a wide range of research funding bodies, and organisations working together across our region to improve health and care services
We have a wealth of expertise at our fingertips to enable you to gain access to and support from leading academics, researchers and practicioners as well as sharing and cascading best practice, new evidence and innovations
We hold frequent webinars, conferences and events to connect people with ideas to people who can help develop these into real world projects with impact
Our Associate Members
Cambridgeshire Community Services NHS Trust
Community360
East Coast Community Healthcare CIC
East of England Ambulance Service NHS Trust
Eastern ARC
Health Innovation East
Health Tech Enterprise
Healthwatch Essex
Integrated Care 24
Norfolk and Suffolk Culture Board
Norfolk Community Health and Care NHS Trust
Norfolk Green Care Network
Suffolk County Council
We welcome inquiries from community and voluntary sector organisations applying either as individual organisations or as consortia.
Get in touch with the team today to see how we can support your research ueahscp@uea.ac.uk or visit our website www.ueahscp.com.


