Paving the Way to Cures
The time is now — and Michigan Medicine is the place — for conquering pediatric brain tumors.


The time is now — and Michigan Medicine is the place — for conquering pediatric brain tumors.

Led by the collaborative efforts of C.S. Mott Children’s Hospital, Rogel Cancer Center and more than 1,500 dedicated donors, the Chad Carr Pediatric Brain Tumor Center (CC-PBTC) was established at Michigan Medicine in 2018 to pool the diverse ideas and knowledge that can solve childhood brain cancers.



The center was launched under the leadership of Valerie Opipari, M.D., former chair of the Department of Pediatrics, and Karin Muraszko, M.D., former chair of the Department of Neurosurgery, and now is under the guidance of Donna Martin, M.D., Ph.D., chair of the Department of Pediatrics, and Eric Fearon, M.D., Ph.D., director of the Rogel Cancer Center.
The center brings together unmatched expertise from across the University of Michigan (U-M) Health departments of pediatrics, radiology, neurosurgery, radiation, oncology, genetics, and pathology and U-M schools of engineering and public health — as well as renowned international collaborators.

As a national center of excellence for pediatric brain cancer, the CC-PBTC has significantly expanded Michigan Medicine’s clinical and research capacity, delivering great promise in the search for cures.
We’re already on the cusp of breakthroughs. We are doing pivotal research on diffuse intrinsic pontine glioma (DIPG) and high-grade gliomas, closing gaps in understanding their causes and mechanisms. We are also working to develop innovative treatments for DIPG and other pediatric brain tumors.
Our efforts and progress are inspired by Chad Carr, the grandson of former U-M football coach Lloyd Carr. Chad was diagnosed with DIPG three days before his 4th birthday. He endured 30 rounds of chemotherapy and a clinical trial before dying of the inoperable brain tumor at the age of 5.

The incredible contributions from our community of generous and dedicated supporters are helping us lead the way in advancing the understanding of pediatric brain tumors, improving therapies and moving us closer to finding much-needed cures.
The time is now — and Michigan is the place — for conquering DIPG, gliomas and other pediatric brain tumors.
Carl Koschmann, M.D., and Sriram Venneti, M.D., Ph.D., are co-directors of the Chad Carr Pediatric Brain Tumor Center.
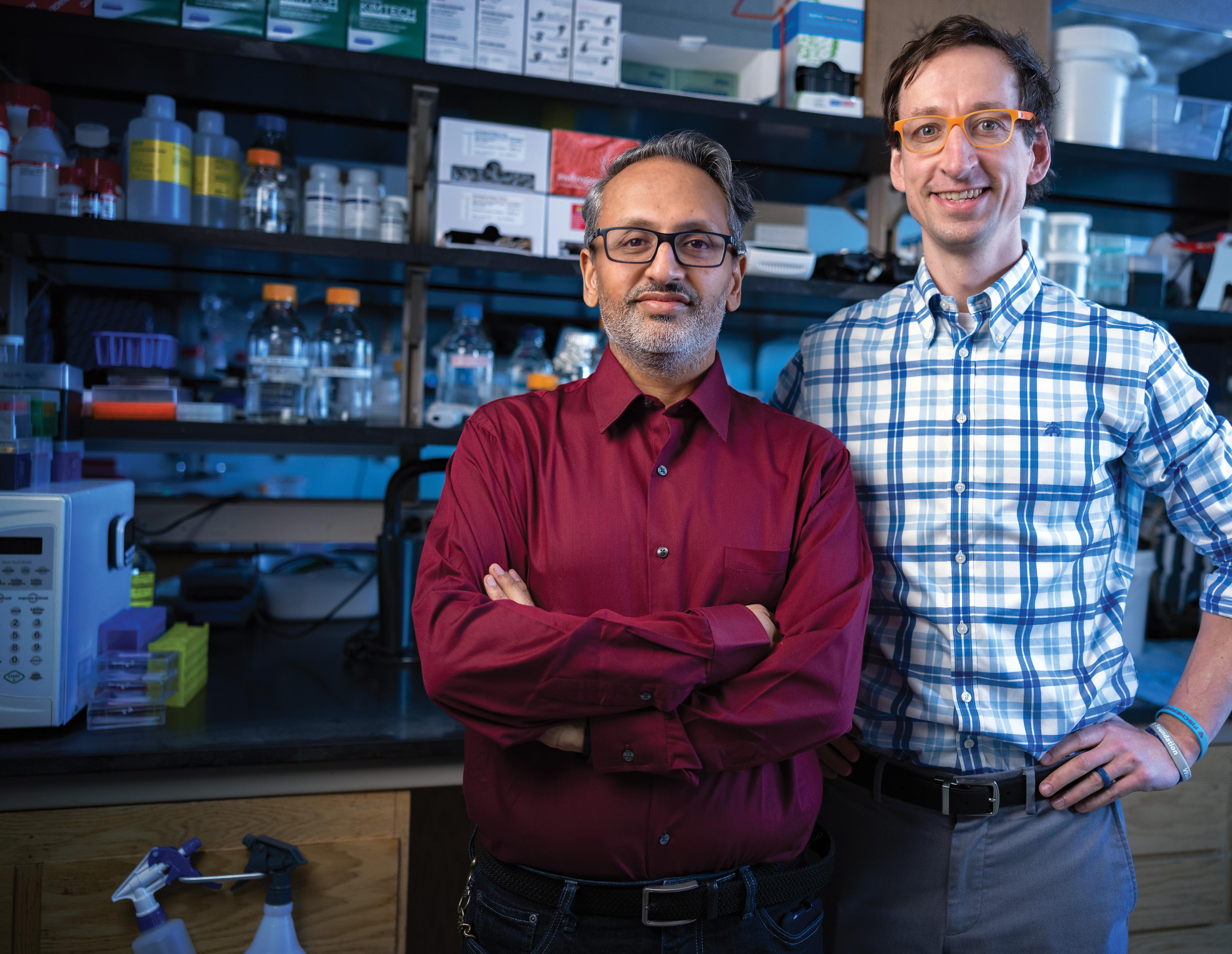
Dr. Koschmann is the ChadTough Defeat DIPG Research Professor in Pediatrics. His lab investigates molecular mechanisms by which mutations in pediatric high-grade glioma, diffuse midline glioma (DMG) and DIPG promote tumor growth and affect response to therapy.
Dr. Venneti is the Al and Robert Glick Family Research Professor in Pediatrics. His group studies mechanisms including epigenetics and cancer metabolism that drive childhood brain cancers.
Drs. Koschmann and Venneti oversee an ambitious portfolio of basic, translational and clinical initiatives for pediatric brain tumors. These efforts include recruiting the best and brightest physicianscientists and trainees, expanding leading-edge clinical trials and providing support for families receiving care at our center.
Maria Castro, Ph.D., and Pedro Lowenstein M.D., Ph.D., team up to study several aspects of pediatric high-grade gliomas, including immunotherapies, interactions between cancer cells with the tumor microenvironment, and growth and invasion patterns of cancer cells in both experimental models and in pediatric patients. Dr. Castro is the R.C. Schneider Professor of Neurosurgery and Dr. Lowenstein is the Richard C. Schneider Collegiate Professor of Neurosurgery. Their work has uncovered mutations and gene therapy strategies that could soon be used in pediatric brain tumor treatment.

Daniel Wahl, M.D., Ph.D., is an associate professor of radiation oncology and a physician-scientist specializing in central nervous system cancers. His research focuses on developing new treatments for brain tumors. His lab group is especially interested in the links between altered metabolism, DNA repair and treatment resistance in aggressive brain tumors. In the clinic, he cares for patients with malignant and benign tumors of the central nervous system.

Costas Lyssiotis, Ph.D., is the Maisel Research Professor in Oncology and an associate professor of physiology and medicine. His lab studies the biochemical pathways and metabolic requirements for tumor survival and growth. This work spans cancer metabolism, the tumor microenvironment and immunometabolism. Ultimately, his group aims to transition new information about these processes into targeted therapies for cancer and other diseases.

Meredith Morgan, Ph.D., is the Lawrence-Krause Research Professor of Radiation Oncology and associate chair for radiation and cancer biology. Dr. Morgan’s lab is focused on improving standard radiation and chemoradiation therapies by using novel agents targeting DNA damage response and repair. Her work prioritizes research with strong clinical and translational relevance, with specific areas of interest in DNA double-strand break repair, tumor immunology and experimental therapeutics.


Stefanie Galban, Ph.D., is an assistant professor of radiology. Her lab examines the mechanisms of resistance and the role of cancer stem cells in pediatric brain tumors in order to devise novel therapies. Dr. Galban’s lab has also developed imaging technologies to evaluate treatment paradigms in various mouse models of cancer, where key signaling events in high-grade gliomas can be visualized using optical imaging.
Jouha Min, Ph.D., is an assistant professor of chemical engineering. Her research aims to advance new technologies for various biomedical applications to improve patient outcomes. She integrates core concepts in chemical engineering, materials science, artificial intelligence and data science to find innovative engineering solutions to significant health problems. Her ultimate goal is to translate these new technologies for clinical use and transform care for cancer and infectious diseases.

John Prensner, M.D., Ph.D., is a pediatric oncologist who believes in using the power of science to improve treatments for children with brain tumors. He is focused on expanding our understanding of the most challenging brain cancers, including medulloblastoma, atypical teratoid/rhabdoid tumors (AT/RT) and DIPG. Dr. Prensner’s work seeks new answers in the genomes of these cancers and aspires to use these findings to transform the lives of patients.

Santhosh Upadhyaya, M.D., is a pediatric neurooncologist whose goal is to deliver leading-edge treatments to children who need a compassionate physician with a high level of expertise in this field. His research focuses on advancing treatment options by drafting and participating in clinical trials for children with brain tumors, with a special interest in AT/RT and other embryonal tumors, and ependymoma.

Andrea Franson, M.D., is a pediatric neurooncologist whose research focuses on clinical trial design, implementation and biocorrelate studies, with a particular emphasis on the development of targeted therapies. She leads numerous clinical trials locally and serves as principal investigator or co-principal investigator on several national pediatric solid tumor and brain tumor clinical trials within the Pediatric Neuro-Oncology Consortium (PNOC) and the Children’s Oncology Group (COG).

“We are very proud of the folks who are working on building our program, and the people from around Michigan and beyond who have believed in and supported the Chad Carr Pediatric Brain Tumor Center. The sky is the limit for where we can take this center from here.”
CC-PBTC pilot grants of $4.3 million (2017–2022) led to raising more than $22 million in grant funding (more than a five-fold impact)
n
2020 and 2021 funding is combined due to COVID-19 pandemic.
Since 2018, the CC-PBTC has become a highly collaborative environment, already resulting in translational discoveries that are affecting our understanding and treatment of high-risk pediatric brain tumors.

n 73.45% NIH/DOD
n
More than 70% of grant funding is from government National Institutes of Health (NIH) and Department of Defense (DOD) support $5.8M $16.2M
TOTAL = $22M
The center is inspiring breakthroughs by spurring institutional, national, and international collaborations and through innovative research, promising clinical trials and the support of unique approaches.
CARL KOSCHMANN, M.D. CO-DIRECTOR OF CHAD CARR PEDIATRIC BRAIN TUMOR CENTER
>125 papers published focused on several pediatric brain tumors including DIPG, pediatric high-grade glioma, ependymoma, medulloblastoma and atypical teratoid/rhabdoid tumor (AT/RT).
michmed.org/CCPBTCpubs
CC-PBTC hosts two dozen clinical trials for children and young adults with brain tumors, including multiple early phase studies from Children’s Oncology Group (COG) and Pacific Pediatric Neuro-Oncology Consortium (PNOC). Neurooncology care is led by Patricia Robertson, M.D., Andrea Franson, M.D., Santhosh Uphadhyaya, M.D., and Carl Koschmann, M.D.
A central nervous system targeted agent prediction (CNS-TAP) tool developed by U-M researchers is now being used to recommend precision medicine therapies in multicenter PNOC clinical trials. U-M Peds-MiOncoSeq serves as the host sequencing site for two ongoing PNOC trials for DMG/DIPG patients.
pediatric brain tumors where research, therapies and key ideas in brain tumor care are discussed. DIPG researchers from outside institutions are invited to present their work, interact with U-M researchers and foster new collaborations.
Precision medicine allows physicians to personalize care based on an individual patient’s genetic profile. Through genomic sequencing, our precision medicine clinic identifies genetic changes that could have developed a tumor, then matches drugs to target these abnormalities.



With researchers across Australia, Canada, Europe and the United States, the teams at PNOC hospitals are made up of specialists from different brain tumor treatment areas as well as nurses, social workers, psychologists and staff whose combined expertise enhances care for each patient.
The CC-PBTC was added to the PNOC in 2019, the only PNOC institution in the state of Michigan.
CBTN is the largest pediatric brain tumor biorepository in the world with more than 40 partner foundations and more than 30 member institutions. CC-PBTC is a satellite site and Carl Koschmann, M.D., is the scientific co-chair for the CBTN. U-M sequencing data and pediatric brain tumor autopsies are deposited into the CBTN in real time for collaborating researchers.
A monthly focus group that brings together U-M labs with national and international experts in
The U-M Peds-MiOncoSeq program, led by Rajen Mody, M.D., and Arul Chinnaiyan, M.D., Ph.D., offers clinical laboratory improvement amendments (CLIA) certified 1700 gene panel DNA/RNA tumor/ germline sequencing with results within two to four weeks at no cost to patients. Over 200 pediatric brain tumors have been sequenced with data deposited into the CBTN for researchers to access in real time. Results have been used to develop new predictors of response and correlative markers for tracking in liquid (cerebrospinal fluid and plasma) samples.
Where scientists and physicians are able to test the newest, move promising treatment advances, and pediatric brain tumor clinical trial offerings are aggressively expanding
The U-M Brain Tumor Bank, led by neurosurgeons Karin Muraszko, M.D., Jason Heth, M.D., and Hugh Garton, M.D., M.H.Sc., includes thousands of specimens from brain tumor patients — an enormous resource which has fueled research not only here at U-M but also for national multicenter collaborations.

U-M’s investment and expertise in genetic sequencing of tumor tissues has positioned us as one of the world’s destinations for sophisticated epigenetic analysis.

We are expanding our brain tumor tissue bank to include more and better characterized pediatric brain cancer specimens, with a goal of shedding important light on high-risk brain tumors. By expanding and further developing a pediatric brain tumor bank including all types of tumors, we will greatly improve our ability to make important discoveries and progress in uncovering novel treatments for high-risk brain tumors.

Sam was diagnosed with glioblastoma his freshman year of high school. After nearly five years of unconventional therapies, he’s enjoying life as a college senior.
During his high school commencement speech, Sam Kell told classmates why that milestone was especially meaningful for his family.
Many thought “I’d have no chance of being here tonight,” he said.
Just a few months into his freshman year, while running with the cross country team, Sam experienced double vision that prompted an MRI.
The result: brain cancer.
The next day, the then 14-year-old underwent brain surgery to remove as much of the tumor as possible. But the diagnosis remained grim: Grade IV glioblastoma — an aggressive, fast-growing brain cancer with an average life expectancy of 12–18 months.
That was in November 2015.
Today, the 21-year-old is a college senior and manager for the men’s basketball team at Oakland University in Rochester, Mich., near his family’s home.

“I’m filled with gratitude,” he says.
For nearly five years, Sam was on two experimental treatments overseen by University of Michigan Health C.S. Mott Children’s Hospital.
“Sam’s outcome is not typical,” says Carl Koschmann, M.D., Mott pediatric oncologist and researcher with the Chad Carr Pediatric Brain Tumor Center at Michigan Medicine.
“We have no experience with young adults on the treatment Sam was on. We don’t have enough data to know if either or both of these therapies contributed to his success, but he is doing well because he was up for the fight and willing to try, remaining compliant with the new therapies.”
Sam underwent DNA and RNA genomic sequencing at Mott to confirm which mutation was driving his cancer and help match him with an unconventional treatment to target that specific mutation. The sequencing results convinced doctors to treat the teen with a drug called everolimus — typically used to prevent rejection of organ transplants and in the treatment of renal cell cancer, not brain tumors.
“Cancer is part of my story, but I learned that cancer is not who I am. Even our worst enemies deserve our gratitude because they teach us so much.”
SAM KELL
In addition to the medication, Sam also opted to use a wearable device called Optune, which uses adhesive patches on the head that create low intensity, wave-like electric fields with the goal to stop or slow glioblastoma tumor cells from dividing.
The therapy, predominately used by adult patients, required Sam to shave his head every morning and hook the device on for nearly 18 hours. He maintained the intense daily routine throughout high school and through his first year of college.

Sam’s prognosis was helped by having a majority of his tumor removed by his initial surgery — leaving fewer cancer cells to grow back, Koschmann says. Still, even with a good resection, only a small minority of patients with glioblastoma survive two years.
His case was so unique that researchers detailed it in a case report published in the British Medical Journal in 2019.
Koschmann says care teams were impressed by Sam’s commitment to staying compliant with the therapies, all while keeping up with classes and playing on the basketball team at Stoney Creek High School in Rochester.
“We wouldn’t typically ask a teen to keep up with a therapy that requires shaving your head every day and using a device for 18 hours while attending high school,” Koschmann says. “But he was up for the logistics and never missed a day. We were astonished at how well he kept up with it.”
Sam’s mom, Gina Kell Spehn, says when the family researched glioblastoma and learned about expected outcomes, they knew they wanted to try something different. They were also wary of how chemotherapy might impact his quality of life.
“The results for what had been the standard of care for decades weren’t promising,” she says. “We wanted to explore all of the possibilities.”
“Sequencing Sam’s tumor helped doctors examine it from a different perspective and explore an out-of-the-box approach. For us so far, saying yes to something completely unconventional was the right choice.”
For high-risk brain tumors, which have surgical limitations because of their location, and that are resistant to the best-known therapies, there is no established standard of care proven to help the prognosis. For these pediatric cancer patients, doctors need to consider treatment that may not have ever been tried before, Koschmann says.
And stories like Sam’s are strong motivators for pushing the envelope with precision medicine. Mott was among the first hospitals in the country to use real-time sequencing in the care of high-risk pediatric tumors — and all high-risk pediatric brain tumors are now routinely sequenced through the Mi-ONCOSEQ program at Michigan Medicine.
“We’re in a relatively newer era where, instead of treating all patients with cancer the same way, we are looking at the actual fingerprint of their tumor, sequencing it to find all the genes that mutated in that tumor and providing a treatment tailored to that specific patient,” he says.
“When we have patients like Sam it’s a huge boost for our medical team to continue outside-the-box ideas in these high-risk situations. We need to keep working to advance research and make precision medicine better for patients like him.”
But because Sam’s treatment was so unconventional, there’s no precedent and little data to guide next steps.
In 2020, Sam made the tough decision to stop therapies and go into tumor monitoring.
For now, he says he’s enjoying his senior year at Oakland. He’s not sure what the future holds but, as a longtime sports fan and athlete, he has an interest in coaching.
“Cancer is part of my story, but I learned that cancer is not who I am,” he told his graduating class last spring. “Even our worst enemies deserve our gratitude because they teach us so much.”
To support the Chad Carr Pediatric Brain Tumor Center, contact:
Ann Kay
Associate Director of Development
annvkay@umich.edu
To refer a patient for a clinical trial or learn more about research, contact:

CCPBTC-CRA@med.umich.edu
michmed.org/pediatric-brain-tumors
The time is now, and U-M is the place to beat DIPG, gliomas, and other pediatric brain tumors. We have been able to make incredible progress in advancing understanding, research, and care for childhood brain tumors — all because of a generous and dedicated community of supporters.


We will continue to pursue discoveries, drive breakthroughs, and improve care to give more young patients and their families the hope, answers, and cures they deserve.
Scientific Advisory Board Members
Donna Martin, M.D., Ph.D.
Eric Fearon, M.D., Ph.D.
Valerie Opipari, M.D.
Karin Muraszko, M.D.
Faye Silverstein, M.D.
Parag Patil, M.D., Ph.D.
Alnawaz Rehemtulla, Ph.D.
Rajen Mody, M.D., M.S.
Sung Won Choi, M.D., M.S.
Andrzej Dlugosz, M.D.
Theodore Lawrence, M.D., Ph.D.
CC-PBTC Administration and Finance
Caryn Crane, Kristin Jensen, Elizabeth Bills, Falicia Modrzynski
The Regents of the University of Michigan
Jordan B. Acker, Michael J. Behm, Mark J. Bernstein, Paul W. Brown, Sarah Hubbard, Denise Ilitch, Ron Weiser, Katherine E. White, Santa J. Ono (ex officio)
University of Michigan Health Executive Officers
Marschall S. Runge, M.D., Ph.D.
Executive Vice President for Medical Affairs, Dean
Steven L. Kunkel, Ph.D.
Executive Vice Dean for Research
David C. Miller, M.D., M.P.H.
Executive Vice Dean for Clinical Affairs
Debra F. Weinstein, M.D.
Executive Vice Dean for Academic Affairs
A Non-discriminatory, Affirmative Action Employer
©2023 Regents of the University of Michigan