6 minute read
Necessity Sparks Acceleration of Educational Innovation
School leveraged technology, experiential learning methods to bolster academic offerings despite pandemic disruptions
For years, a core component of the University of Rochester School of Nursing’s Accelerated Bachelor’s Program for Non-Nurses (ABPNN) involved sending students out into the greater Rochester area to get their first community health experience. Assigned to work with the school’s many community partners, they fanned out across the city where they often encountered patients challenged by the social determinants of health, such as racism, poverty, literacy, and transportation.
The community health component of NUR 377, the advanced medical-surgical nursing course, was both among the most challenging and most impactful experiences in a student’s 12-month undergraduate journey.
But in the spring of 2020, the school’s academic leadership team knew that big changes were necessary for the course. And they had to happen fast.
As COVID-19 began to surge throughout the country, shutdowns began to take effect, travel was restricted, and faceto-face interactions were discouraged. If COVID disruptions meant students were unable to go out into the Rochester community, they would miss out on a meaningful portion of their education.
Rochester would have to come to them.
In a matter of weeks, faculty and members of the school’s Educational Innovation Team (EdIT) did just that. With students starting the summer semester from their homes – some as far away as California – EdIT transformed the course, developing synchronous (real-time) and asynchronous (on-demand) content that allowed students to replicate the in-person experience of past semesters. From thousands of miles away, UR Nursing students could explore Rochester neighborhoods using interactive maps and windshield surveys (iPad videos taken while driving city streets that catalog the shops and services available to residents in a particular area). They accessed the lived experiences of residents by interviewing CEOs and program directors on video calls. And they sharpened their skills by simulating telehealth visits through remote interactions with standardized patients.
Flipping the community health component on its head was a massive undertaking, but much of the groundwork for the transition had been laid before anyone had ever heard of COVID-19. Over the past few years, the School of Nursing had already made strategic investments in its education technology infrastructure and had begun to implement changes to curricula and the methods in which students were educated. The stewards of the school’s educational mission placed a greater emphasis on student engagement, leveraging technology, and the further integration of clinical and classroom experiences.
“We had already been preparing the workforce for a changing environment, and the pandemic served as an accelerant to that,” said Lydia Rotondo, DNP, RN, CNS, FNAP, associate dean for education and student affairs. “That’s the silver lining of COVID-19. It accelerated and pushed us to more fully implement our innovations.”
That was particularly true of NUR 377, where the biggest changes were implemented in a matter of two to three weeks.
“We really needed to creatively identify alternate learning experiences,” Rotondo said. “We leveraged everything we had to make this work, and the efforts – large and small – of our faculty were remarkable.”
“We had to pivot so quickly we couldn’t do everything we wanted to do all at once. But we were able to bring the Rochester community to wherever our students were and then further refine that experience for the fall semester,” added Tara Serwetnyk, MS, RN, NPD-BC, a teaching associate and the education innovation coordinator for the school. “We took something that was already good and made it better.”
“What really stands out to me is that we ate, slept, and breathed this for about two weeks,” said Kaitlyn Burke, MNE, RN, CCRN-CNE-cl, instructor of clinical nursing and member of EdIT. “Everything really came together nicely considering what little time we had to put it together, but it has continued to evolve and expand.”
The makeover of NUR 377 was just one example of how the school – hastened by the pandemic – has re-imagined its academic environment due to the expanding literature on best practices for student learning and course design, as well as evolving educational requirements for nurses to effectively practice in complex and collaborative environments.
While the school’s academic programs were never put on hold, students shifted out of the in-person classroom setting back in March. Instruction was delivered remotely for classroom courses, but most labs and clinical training continued in person, though in smaller sizes. Helen Wood Hall saw its
maximum capacity cut by 75 percent and student gathering places such as the student lounge, atrium and Evarts Lounge were closed, while some classrooms, meeting rooms, and other public spaces were reconfigured to ensure appropriate physical distancing.
Faced with these obstacles, the school’s faculty, instructional designers, and simulation experts drew heavily on its iROC (Redefining Our Classroom) program, which focuses on optimizing technology to foster student engagement through an active and collaborative approach to education. Developed in 2018, it places a strong emphasis on hands-on learning and using digital tools such as iPads, video-conferencing, and simulation to facilitate learning, enhance critical-thinking skills, and improve clinical judgment.
The revised community health component of NUR 377, which still immerses students in a community organization but gives them different tools with which to understand it, perfectly embodies the school’s shift in academic philosophy. While health care professionals were learning to navigate technologies in order to help treat their patients through telehealth, so too were UR Nursing students. Telehealth visits in NUR 377 allowed students to triage standardized patients who presented themselves as being COVID-positive in a safe environment where their occasional mistakes could do no harm. That simulation experience was invaluable, said Megan Su, ’20N, an August ABPNN grad, who is now a COVID-19 case investigator in California. “Never did I imagine I would be in a position where I would be tracing and investigating the spread of COVID in the community and applying my knowledge and experience from my Community Health course to provide resources and guidance to patients diagnosed with COVID,” she said. “All the trials and tribulations of 2020 serve as a reminder that we’re not alone, we’re resilient, and we’re stronger together. I feel so lucky and grateful to be in the nursing profession, and I couldn’t have done it without the guidance of my amazing instructors at UR.” “One of the great things from my perspective was that students not only learned more about the community, but they were also exposed to telehealth visits, which are relatively new for health care in general, but really new to nursing,” Burke said. “It really gave students a great opportunity to talk and work with patients in a secure setting.”
Many of the enhancements ushered in by the pandemic will remain part of the curriculum moving forward. UR Nursing faculty have built longstanding relationships with dozens of community partners across local counties, and when it is safe to do so, they’ll resume the process of embedding students in those organizations. But, recognizing the shift health care is taking from hospital-based care to community-based care, the School of Nursing is also working on developing a community health course for the beginning of the accelerated program and integrating community health material in all courses across three semesters, rather than back-loading all of the content into a culminating course at the end of the year.
“We’re itching to get students back into the community – we don’t want to take that away from them,” said Serwetnyk, noting that these experiential learning opportunities will benefit students long after the current crisis wanes.
“There’s still a lot of value in what we created.”
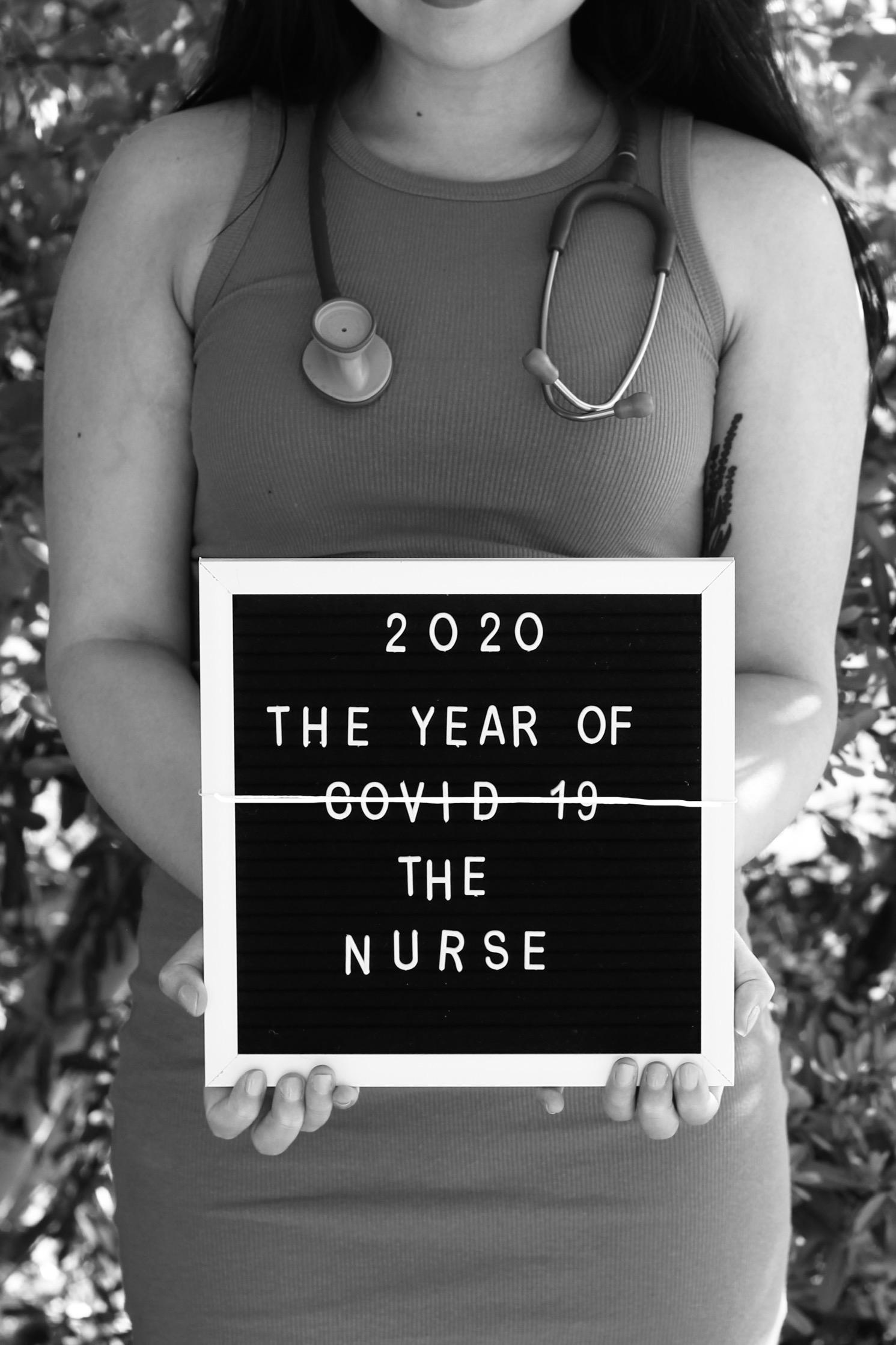
Megan Su, an August 2020 graduate of the Accelerated Bachelor’s Program for Non-Nurses who is now a COVID-19 case investigator in California, is one of the students who directly benefited from some of the innovative curricular changes that expanded out of necessity during the pandemic.






