
6 minute read
SAVINGS VALIDATION
Why Validation of Your Savings is Now Mission Critical for All Healthcare Organizations
Robert T. Yokl, President/CEO, SVAH Solutions
The Healthcare Financial Management Association tells us that that your free-standing hospital, multi-hospital system, or IDN’s payment systems are evolving from fee-for-performance to value-based purchasing, readmission restrictions, and bundled payments. This prediction should also mean a paradigm shift for your supply chain expense management strategies, tactics and techniques.
State of Supply Chain Expense Management
To understand the reason there is a need for change in how a healthcare supply chain department assesses, measures, and monitors the financial results of their GPO and custom contracts, you need to understand the state of supply chain contract expenses savings reporting today. Our studies show that 100% of the savings from these contracts are reported to senior management, but less than 28% are ever verified. Thus, we have discovered that as much as 64% is lost due to not monitoring, tracking, or verifying these savings. Luckily, 36% of this reported savings does hit the mark as not all savings goes off track but it is hard to tell this if you are not continually auditing your savings.

Just imagine if 100% of the savings that were reported were actually saved. We estimate that 64% more savings would hit your healthcare organization’s bottom line. Isn’t that what we are all striving for - bigger and more sustainable savings yields?
Savings Validation

Robert T. Yokl
Little or No Accountability for Your Vendors
When was the last time you checked to see if the savings improvements that were promised by a vendor occurred? Not often enough, according to our own extensive multi-year research. Almost daily, our automated supply expense savings auditor* uncovers that a savings that was promised by a vendor and then reported to a hospital, system, or IDN’s senior management either didn’t happen or increased a hospital, system, or IDN’s supply chain expenses.
Promises Are No Longer Good Enough
It is rare that a vendor takes responsibility for missing a savings or quality target they have estimated in their proposals because they aren’t held accountable by anybody to do so. However, more and more of your hospital, system, or IDN’s contracts with third parties will be “at risk” agreements. Meaning, if your healthcare organization misses their financial and quality targets in these contracts, they will be held accountable and could lose money on these deals. Isn’t it time we, too, hold our vendors to these same standards?
Creating a Culture of Accountability
The first order of business in creating a culture of accountability is to know your reimbursement formulas from your third-parties’ agreements for your cases, procedures, and tests. This way, you can determine if your vendors are in the ball park with their offers.
Next, memorialize your suppliers’ offers, promises, and guarantees into your vendor agreements. For instance, if a vendor is guaranteeing a savings of $222,000 within twelve months in their proposal, show it as a guarantee and list the penalty for missing their promised savings goals.
Finally, track, trend, and analyze the in-use cost of the product, service or technology, at least quarterly, under your new contract to determine if the supplier has met their guarantee. Without this last step, you have no basis for holding your vendors accountable for their offers, promises, and guarantees. This paradigm shift is mission critical for your healthcare organization to survive and thrive in the 21 st century.
Are You Ready to Ensure Your Savings Hits the Bottom Line 100% of the Time?
Every supply chain professional loses sleep over where to find more price, standardization, and supply utilization savings for their healthcare organization’s survival. Yet, what these same individuals don’t realize is that there are hundreds of thousands or even millions of dollars being lost annually because of not validating savings after implementation. When are we going to plug the holes on these mission critical supply chain expenses?
Utilization Management

Purchase Cost is the Tip of the Iceberg!
What Happens After the Right Product, at the Right Price, at the Right Time is Delivered to the Right Person?
Robert T. Yokl, President/CEO, SVAH Solutions
We all assume that when we buy a product, service or technology for our customers that it is used as intended, is appropriate, and has no added cost to it. The fact is, SVAH’s experience over the last 15 years in the new discipline of Clinical Supply Utilization Management is that anything can happen and does when you aren’t there to observe it. Here are six specific things that we have documented that routinely happen when you hand off these products, services and technologies to your customers:
Usage Patterns Change: All of a sudden, your volume or usage increases on a product by 20% over a three-month period without explanation. How would you know this is happening?
Users use the wrong product for the wrong patient care function: A four-port PICC Line is used when only a two-port PICC line is functionally required. This could represent thousands of dollars a year in unneeded and unnecessary expenses for your hospital, system or IDN.
Policies change, or users stray from procedures: Changing your bed linens daily vs. every other day, which is your hospital’s official policy, will increase your linen utilization cost by 50%. Just imagine the hundreds of other policies that are changed when users decide that they have a better way of doing things.
Products have quality issues and failures: Just the other day, a value analysis manager told us that she uncovered that every other lancet device that her hospital system was buying was defective and costing her healthcare system twice as much for months. Generally, you only hear about 1 in 10 quality issues or product failures before they become very costly to your healthcare system. This may seem like small dollars but everything adds up to big dollars if no corrective action is taken.
Utilization Management

Robert T. Yokl
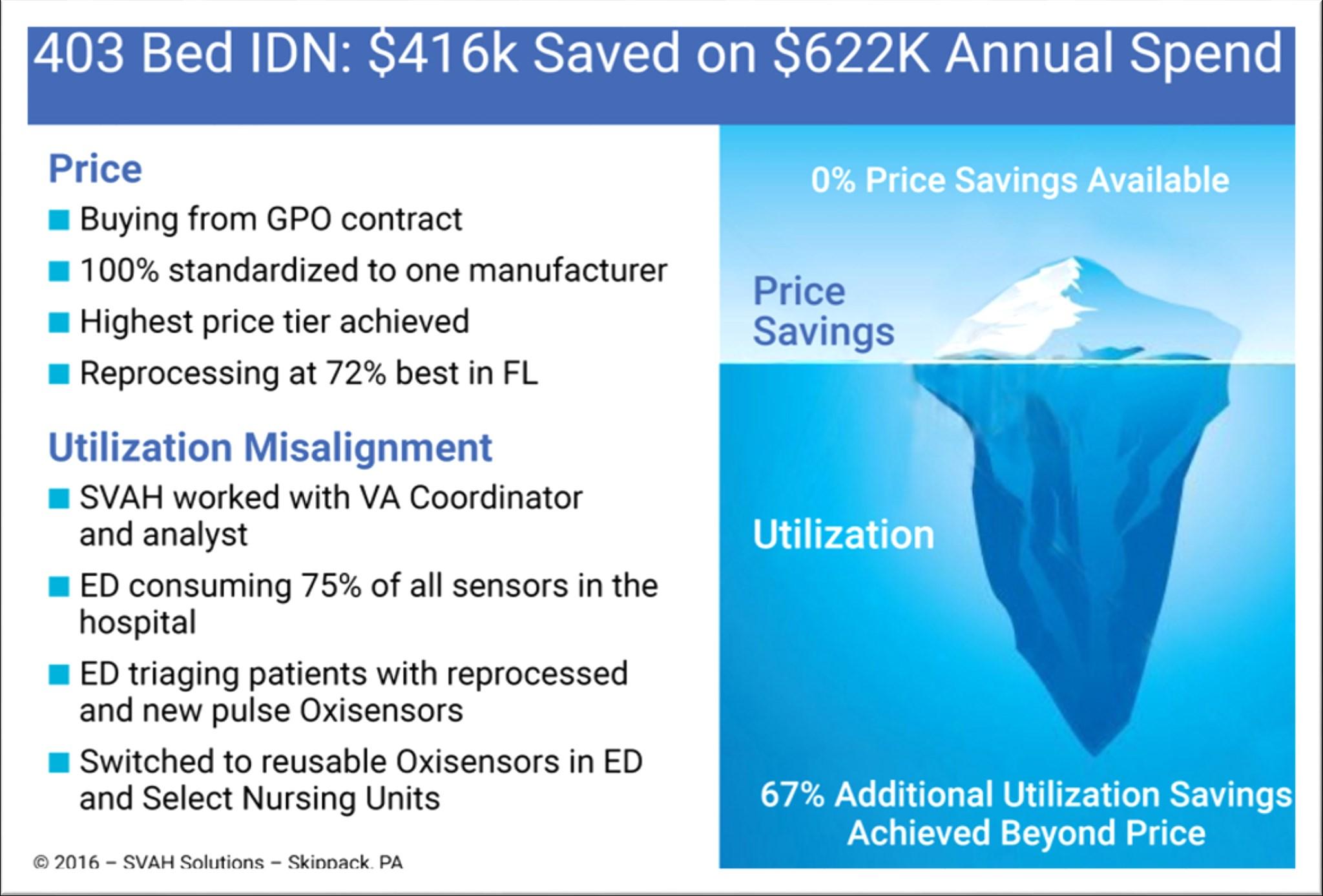
Figure 1—Pulse Oxisensor Utilization Misalignment Example
© 2019—SVAH Solutions, Skippack, PA
Wasteful and inefficient bad habits: Using more than two pairs sterile gloves (double gloving), even though the procedure you are performing only requires one pair of sterile gloves, or, taking specific supplies (scissors) from a suturing kit and wasting the rest of the contents.
Vendors upsell their product lines to end users: Too often, when a vendor or manufacturer receives complaints about a product, (e.g. trays, electrodes, gloves) you are buying from them, they will substitute a higher cost product to solve a quality issue without compensating your hospital for the higher price item. This will then be reflected in higher utilization costs for this product. This happens more often than you realize.
It is hard to argue that things change and people change over the course of weeks, months, and years. So, why should it be any different with the products, services, and technologies you are buying for your customers? That’s why you need to have a Clinical Supply Utilization Management System* in place to monitor, control, and when necessary, eliminate these utilization misalignments. That’s what elimination of variation is all about.


