































An advanced reporting system specifically designed to do a particular task, a job that would be a lot tougher to do without it.
Now the right tool for advanced value analysis & supply utilization management is here: The customizable Utilizer® reporting engine is designed to help you quickly and effortlessly uncover and resolve savings while meeting the quality challenges in your supply chain.
This unique system is built on a powerful reporting engine that has shown countless successes in the real world of supply utilization and value analysis management.

By Robert W. Yokl
327-4820 ryokl@ValueAnalysisMagazine.com www.ValueAnalysisMagazine.com
ryokl@ValueAnalysisMagazine.com
Copyright 2025 SVAH Solutions. All rights reserved. Reproduction, translation, or usage of any part of this work beyond that permitted by Section 107 or 108 of the 1976 United States Copyright Act without permission of the copyright owner is unlawful. For permission, call, fax, or e-mail Robert W. Yokl, Managing Editor. Phone: 610-327-4820
E-Mail: ryokl@valueanalysismagazine.com for approval to reprint, excerpt, or translate articles.


Robert W. Yokl, President, SVAH Solutions


How do you know when to start, stop, or continue with a value analysis review? There should be valid reasons why you are going to perform a value analysis review, why you may stop it midstream, or why it must continue out to a final resolution. These are valid issues that VA/supply chain team members deal with every day.
Today I am talking about “Start, Stop, Continue” conundrum. If you get this dynamic right, you will do big things and get great results for your health system. If you get it wrong, you have just wasted a bunch of time with little or no results to show for it. The strategy here is to get it right more than you get it wrong.
You Have to Prove that a Value Analysis (VA) and/or Cost Management (CM) Review is Necessary – Today, you are going to need the buy-in from your department heads and managers to even review a product or service in their areas. They do not even want to discuss change without proof that the needed change is real, so make sure you have proof. Pretend you are in their shoes and try to punch holes in your proof. Make it bulletproof and you can make big things happen.
Lip Service from Start to Finish in a VA/CM Project is Part of the Game – Those department heads and managers are going to do everything they possibly can to try to put the brakes on your efforts or even dispel the results you find in your VA/CM projects. You are going to have to expect the lip service and roll with it. The good part about the lip service is that they are going to offer up valid points and reasons that are worth their weight in gold. Then, you can research them and validate/invalidate them without losing a beat.
One of Our Long Time Mantras –“Don’t Stop at the First Savings You Find” – Let’ s face it, you will always find initial/quick savings on just about any VA/CM project you work on, but we have found over our decades of experience that there is always much more.
Robert W. Yokl


“He knew how to read the room (hospital) and is now the COO of that very large and prestigious hospital.”
Organizational Inertia is Very Real in Healthcare – Nobody wants to have their VA/ CM project drag on and feel as though it is stuck in neutral or just taking small baby steps. What I learned from some very skilled Quality and VA Managers over the years is that some hospitals and health systems have a pace at which they work. The more complex the VA/CM study, the slower their pace might be. This inertia usually rears its head on areas that involve changes to entire clinical areas such as changes to oxisensors, IV products, procedural areas, etc.
Learn to Read the Room (Hospital) - I remember a value analysis project that I worked on with a large community hospital and the Director of Value Analysis. Together we were able to uncover a $200K savings opportunity through our analysis. All clinicians agreed on the major savings opportunity, but it would require the entire hospital (nursing, anesthesia/OR, etc.) to change the way they set up their IV sets. The Director of VA then made a bold statement and said that they would only implement the changes on the nursing staff which would net $130K in savings and leave the OR team alone. He basically said that hospitals like his can only take so much change at once and he would bank the savings and address OR down the road. He knew how to read the room (hospital) and is now the COO of that very large and prestigious hospital.
– So much great work is put into VA/CM projects but after the project has been completed, the VA/CM project managers move on to the next project. VA/CM project managers need to build follow-ups into their process to ensure that their good work does not fall back into old habits or that previous products do not creep back into the departments where you enacted the changes. Plus, if the results weren’t achieved, you can then easily re-implement those changes and regain the results. It just makes sense to perform the savings validation. Otherwise, what good is saying you saved money when the organization really didn’t?
I could go on and on with the things that are just part of the school of hard knocks that do not have to be in healthcare value analysis and cost management projects. The key is having the awareness that these things could happen on any given value analysis or cost management project, but they don’t have to make you stop in your tracks or get thrown out of kilter. Learn to anticipate these and you will be unstoppable!


Danielle Miller, Healthcare Data Specialist, SVAH Solutions
Pricing strategies alone are becoming less effective in managing healthcare supply chain costs, and healthcare organizations will need to explore other avenues for savings to fill the gaps. Supply utilization management is a key approach to achieving this, focusing on optimizing resource use rather than just controlling pricing, standardization, and compliance. By addressing inefficiencies in supply spending, such as feature-rich products and services, hospitals can achieve savings of 7-15% of total non-salary budget. Effective supply utilization management can improve both financial performance and patient outcomes, making it essential for healthcare organizations to adopt this strategy as a core aspect of their approach.
Clinical supply utilization management (CSUM) and value analysis (VA) are distinct processes in the healthcare supply chain, though they complement each other when combined. VA focuses on evaluating lower-cost alternatives, managing contracts, and solving problems related to products and services. However, it lacks robust tracking systems for ongoing progress. CSUM, on the other hand, tracks the utilization/consumption of products and services based on patient metrics, providing clear insights and data on cost trends, which helps identify areas for improvement.
When CSUM data reveals rising costs, VA can then step in to find solutions. CSUM provides actionable, volume-based insights that help supply chain and VA teams strategically target cost-saving opportunities, making it more effective than VA alone. Integrating CSUM with VA offers substantial savings (5% to 12% of total non-salary budget) and improves the ability to track progress, making the process more data-driven and actionable.
Clinical supply utilization management refers to the process of overseeing and optimizing the use of resources within a hospital, such as orthopedic soft goods, pacemakers, pharmaceuticals, dressings, surgical gloves, etc. The goal is to ensure that these resources are utilized efficiently, reducing waste and unnecessary expenses while ensuring that patient care remains top priority.
Effective supply utilization management involves a systematic approach to monitoring, controlling, and forecasting resource usage, so hospitals can balance demand with availability, prevent shortages, and minimize waste. With a data-driven approach, hospitals can align utilization/consumption with patient care needs without compromising quality or safety.
Cost Reduction: Supply utilization management is key to controlling supply chain costs, as traditional methods like price negotiation have limits. Misaligned use of products, services, and technologies can cost organizations 26% more than their peers and hurt financial performance. Inefficiencies, such as overuse of items like IV catheters, often overshadow savings from pricing. Managing supply expenses requires attention to price, standardization, value analysis, and utilization. Ignoring these aspects can result in significant financial losses.
Danielle Miller
Improved Patient Care: Efficient resource utilization ensures that necessary treatments, equipment, and staff are available when needed most. Proper management prevents shortages of critical supplies or delays in care, improving patient outcomes.
Optimizing Operational Efficiency: Managing hospital supply utilization/consumption effectively ensures that resources are allocated where they are most needed, thereby improving overall hospital workflow. This can lead to faster turnaround times, smoother patient care, and a reduction in operational bottlenecks.
Benchmarking with Data Analytics: Many healthcare organizations are using value analysis analytics to identify savings in their supply chain, but few are using comparative analytics to benchmark and detect real-time utilization issues compared to peers. This is important because simply tracking supply spend doesn't provide enough insight to influence clinician behavior, which is crucial for driving change. By sharing comparative analytics with stakeholders, organizations can capture attention, encourage receptiveness to recommendations, and support practice adjustments to improve supply chain performance. For example, a study on examination gloves may reveal discrepancies in usage that lead to productive discussions about underlying causes, such as policy non-compliance or overuse. Without comparative analysis, these conversations and necessary changes won’t happen, limiting the potential for savings. To maximize savings, organizations should go beyond tracking spend and start benchmarking across a wide range of purchasing categories.
Effective benchmarking can unlock significant savings on hospital supply expenses, but many healthcare supply chain/value analysis professionals don't implement it properly. To achieve real impact, benchmarking needs to be done at the SKU (stock-keeping unit) level, using data from local, regional, or national partners, or through specialists with the necessary data. This approach makes the benchmarking process more effective and impactful.
Employee Education and Engagement: Ensuring that all hospital staff understand the importance of supply utilization/consumption management is key. Training staff on how to reduce waste, optimize resource usage, and follow established protocols for inventory management can lead to significant improvements in consumption practices across departments.
Automatic and Ongoing Monitoring: Regular audits of resource utilization patterns can help identify areas of inefficiency. By closely monitoring utilization/consumption trends, hospitals can proactively make adjustments, leading to better control over hospital resources.
To avoid unnecessary costs and preserve savings, hospitals must focus on effective supply utilization management. This involves optimizing resources, improving operational efficiency, and maintaining high-quality patient care. By using technology, data analytics, and streamlined processes, hospitals can reduce waste and ensure essential resources are available. In a climate of rising costs and increasing pressures, supply utilization management remains a crucial strategy for financial stability and patient well-being.


STAY CONNECTED HERE

J. Hudson Garrett Jr., Ph.D., MSN, MPH, MBA, FNP-BC, IP-BC, PLNC, VA-BC, BC-MSLcert MSL-BC, CPHRM, LTC-CIP, CPPS, CAE, CPHQ, CVAHPTM, CMRP, CPXP, CDIPC, FACDONA, FAAPM, eFACHDM, FNAP, FACHE, FAPIC, FSHEA, FIDSA, FAHVAP
Karen Niven, MS, BSN, RN, CVAHPTM, FACHDM, FAHVAP


In today’s dynamic healthcare landscape, the pursuit of improved clinical and operational outcomes has become paramount. The increasing complexity of healthcare demands that organizations continually refine their approaches to delivering care. A strategic method that is gaining prominence is healthcare value analysis a process that evaluates the balance between cost, quality, and outcomes to ensure that every healthcare dollar is spent wisely. Central to this approach is the need for rapid competency development among staff, the establishment of highly reliable processes, and the integration of innovative healthcare products and services.
Healthcare value analysis is a systematic evaluation of clinical products, services, and processes to determine their overall value relative to their cost. This method is not merely about cost-cutting; it’ s
about maximizing value. It involves critical decision-making processes to determine which products and services will drive better patient outcomes, streamline operations, and reduce waste. In an era marked by rising healthcare costs and ever-increasing patient demands, value analysis helps organizations focus on interventions that offer the highest return on investment not only financially, but also in terms of patient safety and quality of care.
One of the key elements of healthcare value analysis is the speed at which healthcare professionals are brought up to speed with new competencies. Rapid changes in medical technology, treatment protocols, and regulatory requirements necessitate that healthcare workers continuously upgrade their skills.
Accelerating competency is critical for several reasons:


“In an era marked by rising healthcare costs and ever-increasing patient demands, value analysis helps organizations focus on interventions that offer the highest return on investment—not only financially, but also in terms of patient safety and quality of care.”
1. Enhanced Patient Care: When healthcare professionals quickly acquire new skills, patient care becomes more efficient and effective. For example, training in new surgical techniques or updated diagnostic procedures directly contributes to better outcomes.
2. Operational Efficiency: A workforce that is agile and adaptable is more capable of managing complex workflows and integrating new technologies. This leads to more streamlined operations, reducing delays and errors that can adversely affect patient outcomes.
3. Staff Satisfaction and Retention: Investing in rapid competency development also boosts morale. Staff feel valued when their professional development is prioritized, leading to lower turnover rates and a more experienced, knowledgeable workforce.
Modern educational tools, simulation-based training, and just-in-time learning modules have emerged as effective methods to shorten the learning curve. These approaches allow healthcare professionals to quickly grasp and implement new practices, ensuring that the delivery of care remains at the cutting edge.
Process reliability is the backbone of quality healthcare delivery. In the context of value analysis, building highly reliable processes means standardizing procedures, minimizing variability, and continuously monitoring performance to ensure consistency. The following strategies are essential:


checklists, and evidence based guidelines that ensure every patient receives care based on best practices.
2. Continuous Quality Improvement: Establishing a culture of continuous quality improvement involves regular audits, feedback loops, and the use of data analytics to identify and address process deficiencies. This iterative approach ensures that processes remain robust even as new challenges arise.
3. Leveraging Technology: Innovative technologies such as electronic health records (EHRs), computerized physician order entry (CPOE), and predictive analytics are instrumental in creating reliable processes. These technologies help in tracking performance, identifying trends, and preemptively addressing issues before they escalate.
4. Engaging Frontline Staff: The insights of frontline healthcare workers are invaluable. By involving them in process improvement initiatives, organizations not only benefit from practical insights but also foster a culture of accountability and continuous learning.
Highly reliable processes reduce variability in care delivery, leading to fewer adverse events, improved patient safety, and enhanced operational efficiency. As healthcare organizations invest in these processes, they create a resilient system capable of adapting to changes and sustaining improvements over time.
Innovation in healthcare is more than just a buzzword; it is a critical driver of improved clinical and operational outcomes. Innovative products and services can transform traditional healthcare models by introducing more efficient, effective, and patient-centered solutions. Consider the following areas where innovation is making a significant impact:
1. Digital Health Solutions: Telemedicine, mobile health applications, and remote monitoring devices have revolutionized patient care. These technologies not only extend the reach of healthcare services but also enable real-time monitoring and management of chronic conditions, reducing hospital readmissions and improving overall health outcomes.
2. Advanced Medical Devices: Innovations in medical devices from minimally invasive surgical instruments to state-of-the-art imaging systems have enhanced the precision and safety of various procedures. These advancements lead to shorter recovery times, reduced complications, and higher patient satisfaction.
3. Data Analytics and Artificial Intelligence (AI): Leveraging big data and AI allows for predictive analytics that can foresee patient deterioration, optimize resource allocation, and personalize treatment plans. These technologies support proactive rather than reactive care, ultimately saving lives and reducing costs.
4. Value-Based Care Models: Innovative service delivery models, such as value-based care, shift the focus from volume to value. By aligning financial incentives with patient outcomes, these models encourage healthcare providers to focus on quality over quantity, leading to improved patient care and cost efficiencies.
5. Interoperability and Integration: Integrating various digital platforms and ensuring that healthcare systems can communicate seamlessly enhances care coordination. This interoperability is essential for timely decision-making and holistic patient management, as data from different sources can be synthesized to create a comprehensive view of a patient’s health.
To truly capitalize on the benefits of healthcare value analysis, organizations must embed it into their strategic framework. This integration involves:
• Leadership Commitment: Senior leadership must champion the value analysis program, allocating necessary resources and fostering a culture of continuous improvement.
• Cross-Functional Collaboration: Effective value analysis requires collaboration among clinicians, administrators, IT specialists, other stakeholders, and supply chain experts. This multidisciplinary approach ensures that all aspects of patient care and operational efficiency are considered.
• Performance Metrics: Establishing clear metrics to assess both clinical and operational outcomes is essential. Data-driven decisionmaking enables organizations to measure the impact of their initiatives and adjust strategies as needed.
• Continuous Innovation: Organizations must remain open to adopting new technologies and practices. A commitment to innovation ensures that the processes remain current and are continuously improved upon.


“Innovation in healthcare is more than just a buzzword; it is a critical driver of improved clinical and operational outcomes.”
Healthcare value analysis represents a transformative approach in the ongoing quest for improved patient outcomes and operational efficiency. By accelerating competency among healthcare professionals, establishing highly reliable processes, and leveraging innovative products and services, organizations can create a robust framework for delivering high-quality, cost-effective care. As the healthcare environment continues to evolve, embracing these strategies is not only beneficial but essential. The future of healthcare lies in the seamless integration of value analysis into every facet of service delivery, ensuring that care remains patient-centered, efficient, and sustainable for generations to come.
For more information or to join the Association of Healthcare Value Analysis Professionals (AHVAP), visit www.ahvap.org.



Dr. Garrett is the Executive Director and Executive Vice President for the Association of Healthcare Value Analysis Professionals (AHVAP) and an Adjunct Assistant Professor of Medicine in the Division of Infectious Diseases at the University of Louisville School of Medicine.

Karen is the Senior Director of Clinical Value Analysis at Premier, Inc and serves as the President of the Board of Directors for the Association of Healthcare Value Analysis Professionals (AHVAP).
Shannon Hillyer, RN, BSN, CRNI, Director of Global Customer Solutions, Medical Delivery Systems
Eric
Flynn,
RN,
BSN, Director of Critical Care/Vascular Access, Raleigh General Hospital
Beth Forman, DNP, MSN, RN, CPPS, Assistant Chief Nursing Officer, Raleigh General Hospital

Vascular access is a critical component of medical care that allows for the delivery of fluids and medications to patients through the insertion of a peripheral or central vascular access device (VAD) into a blood vessel [1, 2]. Hundreds of millions of VADs are inserted in the United States alone each year [3]. Given the frequency of vascular access in healthcare settings, there may be a high opportunity for risk if not managed properly. Complications arising from catheters have been reported in up to 42% of patients, including common issues such as phlebitis, infiltration, occlusion, extravasation, and catheter related bloodstream infections (CLABSIs). These complications can also lead to significant increased costs for healthcare facilities [4].

Inconsistencies in policy, practice, training, and device selection may contribute to poor vascular access outcomes[5]. Given these challenges, healthcare facilities frequently implement quality improvement initiatives to enhance their vascular access protocols and the quality of training provided to practitioners. An in-depth assessment can be a useful first step in addressing a facility’ s specific needs to drive sustainable improvement of policies, practices, and standardization of products across the institution.
This case study covers the facilitation of a comprehensive vascular access management (VAM) assessment at Raleigh General Hospital, and the subsequent quality improvement initiatives which refined vascular access practices to minimize risks. We aim to share both best practices and lessons learned from the VAM process at Raleigh General to serve as guidance for facilitation of these processes in other institutions nationwide.
Raleigh General Hospital (RGH) is a 300-bed full-service institution located in Beckley, West Virginia. RGH is owned by Lifepoint Health, a healthcare delivery network which oversees 62 acute care hospitals and other healthcare facilities in non-urban communities across the country. RGH is home to the highest-rated hospital emergency department in southern West Virginia and offers a diverse portfolio of inpatient and outpatient services to nearly 13,000 patients annually [6].
Similar to many hospitals and health systems across the US, Raleigh General had experienced historic challenges with vascular access care related to provider assignments, internal policies and protocols, and devices used across the facility [7, 8]. RGH leadership therefore sought out a device vendor (BD, Franklin Lakes, NJ) to gain a better understanding of problems with the current standard of care. The BD team conducted a VAM assessment in collaboration with the RGH stakeholders, which is a uniquely integrated approach to vascular access care, combining clinical practice assessments, device portfolio considerations, and expert clinical training/education.
At RGH, the VAM assessment included a review of clinical charts, an evaluation of the rationale behind line placements, documentation of the number of needlesticks required prior to success, as well as an overview of other hospital performance metrics. Furthermore, BD conducted on-site interviews with hospital staff to gain insight into the current vascular access processes, including challenges for staff and leadership. Daily monitoring took place to observe patient care quality and safety throughout the VAM assessment process. This included observations of line conditions, dressing states, and infusions to identify inconsistencies in line selection, including in difficult venous access (DVA) patients. This thorough evaluation initiated a multi-year partnership between RGH and BD, and revealed opportunities to improve vascular access practices related to personnel utilization, in-house policies and protocols, and device utilization to improve outcomes for the facility.

Vascular Access Personnel: Various staff members played a role in vascular access at Raleigh General prior to the VAM assessment. Bedside nurses were responsible for peripheral IV placements, while physicians, including a dedicated vascular surgeon, managed all central line insertions. However, there was limited knowledge among staff regarding different vascular access options, resulting in above-average central line utilization.


In addition, RGH faced shortages of personnel qualified to assist in line insertions and maintenance. As a result, beginning in 2022 RGH contracted a third-party line placement company to manage all peripherally inserted central lines. In this process, in-house nurses would contact the thirdparty service for line placement, and a specialized nurse was dispatched to RGH within 24 hours of the request. The reliance on external contractors contributed to challenges such as delays to line placement, delayed patient discharges, inappropriate line usage, increased expenses, and unimproved infection rates. The persistent challenge with the third-party coincided with outreach to BD, and the relationship with the third-party was terminated around the start of the assessment.
Techniques and Policies: The VAM also assessed daily practice for inserting and maintaining lines compared to best practices. Of particular focus were items such as proper site selection and adherence to antiseptic techniques. For minimizing infection risk and ensuring device longevity, peripheral intravenous catheters should be placed in the forearm, hand, or upper arm, and central VADs in the chest or upper arm. During the VAM, variations from site selection were observed, in part due to unique clinical or patient situations.
Another key step in reducing infection is maintaining aseptic techniques to keep the VAD free of contaminants. The VAM observed some deviation from best practice recommendations, as well as opportunities for re-education to strengthen adherence to these protocols.
Technology and Products Utilized: Lastly, the VAM paid particular attention to the use of vascular access products and devices at RGH. The assessment highlighted a lack of VAD standardization, particularly in midlines, peripheral IVs, and peripherally inserted central catheters (PICCs). There was a wide variety of redundant VADs available for provider use that could
potentially lead to inconsistencies in device and component selection. The lack of standardization created issues with device compatibility, impacting workflow efficiency and increasing training requirements on the hospital floor.
In addition, for DVA patients, advanced techniques such as ultrasound guidance can be a valuable tool to facilitate vascular access. However, few RGH clinicians were trained in this technique, thereby limiting the process that would yield the best clinical outcomes.
In total, the above factors contributed to a vascular access practice characterized by heavy reliance on central lines, lower than recommended dwell times, and above-average CLABSI rates at the time of the initial VAM assessment. However, the assessment helped set a baseline and the findings informed the development and pilot of various initiatives in the following years, aiming to refine vascular access practices and improve patient outcomes.

“Contrasting with a generalist approach, the implementation of vascular access teams with specialized experts is associated with higher first-time insertion rates, contributing to enhanced patient satisfaction and reduced institutional costs.”

Marsha Jamison, CNO at Raleigh General, established core objectives for enhancing patient care and operational efficiency based on the findings of the assessment. These included reducing central line usage to only when deemed necessary, decreasing infection rates, improving patient satisfaction, and minimizing blood contamination for frontline nursing staff. These key objectives guided the development of three main initiatives that followed the VAM assessment.
A key initiative following the assessment was the formation of a vascular access team (VAT). These teams, comprised of vascular access specialists with advanced knowledge and skills in VAD insertion and management, are a crucial tool to optimizing patient outcomes. Contrasting with a generalist approach, the implementation of VATs with specialized experts is associated with higher first-time insertion rates, contributing to enhanced patient satisfaction and reduced institutional costs [3].
The establishment of a VAT at RGH marked a significant step towards assuming full internal accountability for vascular access management. This in-house team, composed of three nurses under the Director of Critical Care/Vascular Access, was carefully selected based on their expertise in care,
technical proficiency, and critical thinking abilities. The VAT received specialized training, including a comprehensive week-long training session led by a BD field educator specializing in catheter insertions. After the VAT became proficient in their initial PICC line training, the field educator returned to RGH to teach on additional line insertions, including midlines, to leverage vessel visualization and ensure optimal line matching for patients. The VAT focused on vascular access management and education following the completion of their training. Alongside completing all vascular access consultations and VAD insertions, the VAT team performed daily rounds and monitored patients’ lab results to detect any signs of infection. The VAT remained committed to maintaining high-level knowledge on both vascular access and infection control throughout the facility via continuous education efforts.
During their routine rounds, the VAT encountered various vascular access challenges which they leveraged as educational opportunities for hospital staff. This involved:
• Providing technique corrections to ensure proper device usage.
• Advising appropriate site selection.
• Building comprehensive dressing kits to optimize patient care and outcomes.
• Facilitating trainings on the hospital floors for frontline nursing staff.
• Collaborating with the education department to integrate the new vascular access practices into new-hire training sessions.
Throughout the entirety of the VAT education process, the BD field educator facilitated ongoing communication and support with the device supplier, ensuring adherence to product best practices and protocols. By dedicating these resources to in-house vascular access expertise, RGH could better align with hospital quality metrics, evolve vascular access practices, and provide comprehensive education for providers.
In parallel with VAT development, the CNO, ACNO, and Director of Critical Care/Vascular Access sought to enhance hospital policy by implementing evidence-based protocols and best practices in vascular access. One of the first policy changes instituted stricter criteria for central line usage. These criteria required provision of rationale for both the placement and continued utilization of central lines, ensuring that lines were only inserted when deemed appropriate and were promptly removed when no longer necessary. The goal of this change was to address inconsistencies in patient care practice. For instance, patients being discharged with PICC lines must now meet specific requirements to ensure appropriate line utilization.
The CNO, ACNO, and Director of Critical Care/Vascular Access strived to achieve first-time insertions and zero CLABSIs. Additional protocols aimed to standardize hospital policies to improve patient outcomes and lower the overall rate of central line utilization. For example, despite the
CLABSI rate falling below national averages, the CNO instituted a policy to conduct root cause analyses on any infections that did occur to understand how to prevent them in the future. These facility-wide policy changes were designed to not only improve patient outcomes but also enhance patient satisfaction and minimize discomfort through improving first-time insertion rates and reducing needlesticks.


Leadership and the VAT worked tirelessly to ensure compliance with these new guidelines. Some providers were hesitant to accept the new changes due to their longstanding clinical practice of central line usage. However, leadership across the facility and BD worked closely to ensure a smooth transition. To encourage uptake of policies, educational sessions were organized by the BD team to guide physicians through the vast breadth of capabilities and applications of VADs. RGH nursing leadership facilitated an open and transparent dialogue to convey the need and evidence for policy changes. Lastly, the VAT initiated daily hands-on monitoring and rounds to ensure line patency and oversee the transition.
Leadership at RGH sought to harmonize the inconsistencies in device and material use that may have contributed to poorer outcomes. The lack of standardization had previously disrupted workflow, as significant time was spent locating compatible components. Leadership and the VAT collaborated to standardize the brands of supplies to reduce the risk of device mismatch. RGH adopted standardized midline catheters, IV catheters, PICCs, and needleless connectors based on the field educator’s recommendations. This standardization effort also involved the adoption of improved peripheral intravenous lines to minimize blood exposure to providers, along with the introduction of a positive pressure needle-free connector. This assisted in minimizing infection risk by reducing the amount of blood reflux into the needle-free connectors. The new practices for device selection prioritized the patient’s best interest and optimized clinical outcomes.
Despite these successful efforts to narrow device variation, a setback occurred when a preferred device, known for its superior clinical outcomes, was removed from the hospital’s supply chain due
to cost considerations. Nursing leadership advocated for the reinstatement of the preferred device by using compelling data that highlighted its effectiveness. Nursing leaders’ transparency and expertly guided efforts resonated with hospital leadership and despite its higher associated costs, the preferred device was made available to ensure that providers could continue delivering optimal patient care.
The implementation of these new initiatives resulted in direct improvements at RGH. The impact was observable through improved patient outcomes, heightened workflow efficiency, a favorable cultural transformation, and positive economic outcomes.
Together, all of these interventions contributed to enhancing patient outcomes. The VAT provided a remarkable improvement in response times for line placements due to their accessibility and proximity to the patients. Unlike the previous third-party service, where line placement could take up to 24 hours, the VAT ensured placement within just one hour of consultation, which eliminated unnecessary discharge delays. Additionally, there was a decrease in multiple device utilization due to VAD standardization efforts. The effectiveness of these changes was particularly evident through the significant reduction of CLABSI incidents within the first two years of implementation. In addition, the reduced infection rates and fewer needlesticks enhanced overall patient satisfaction and comfort, shown in positive patient feedback given to the VAT.
The newly adopted policies at RGH prompted a remarkable transformation in staff culture and workflow despite the initial reservations. The supply standardization policies facilitated an easier decision-making process that allowed staff to readily choose compatible devices. Besides having access to standardized devices, the hospital staff were also now equipped with the necessary training and knowledge to select the appropriate lines for insertion, thereby enhancing overall hospital efficiency. This new working culture emphasized the importance of having skilled and actively involved vascular access staff.
In response to this cultural shift and increase in responsibilities for vascular access care, nurses felt a greater sense of ownership over clinical decisions. There was a notable increase in ownership among hospital staff to enhance patient care and reduce infection rates, a sentiment celebrated through a regularly distributed nursing newsletter. This led to improved outcomes for patients and heightened satisfaction among nurses themselves. Furthermore, this fostered a culture of continuous learning by not only boosting performance but also cultivating a sense of engagement and investment among employees dedicated to delivering exceptional patient care.
While the primary goal of the VAM assessment was to pinpoint opportunities for clinical enhancements, RGH leadership noted several economic impacts from the resulting initiatives. Though not precisely quantified, the reduction in CLABSI rates led to substantial cost savings for RGH through avoiding infection treatment costs. Furthermore, discontinuing the use of the third-party agency, which charged the hospital per line inserted, contributed to additional savings while simultaneously improving efficiency and staff ownership by enabling RGH providers to independently select VADs, place, and maintain the lines. The hospital’s adoption of standardized materials and devices facilitated refined purchasing practices and further enhanced financial benefits across the organization.


“With clear priorities and the best interest of patients and providers in mind, leadership were unwavering in their support for large improvement efforts such as the formation of the VAT.”
Enhancing patient outcomes through specialized care has transformed clinical and operational processes at RGH. Initiating the process with a hands-on assessment has proven to be instrumental in identifying areas of improvement and implementing targeted solutions. The success observed from the initiatives following the VAM has provided invaluable learnings, which will serve as the foundation for future improvements as RGH’ s collaboration with BD continues.
The success of these initiatives can be attributed in part to the consistent efforts of the CNO, ACNO, and Director of Critical Care/Vascular Access. Having support from leadership is paramount for provider success and delivering quality care, and the effective leadership from RGH fostered a culture of trust, transparency, and collaboration, empowering employees to take initiative and overcome challenges. With clear priorities and the best interest of patients and providers in mind, leadership were unwavering in their support for large improvement efforts such as the formation of the VAT.
Additionally, their transparency throughout the decision-making process facilitated clear communication and discussion between leadership and staff. Leadership ensured that nurses understood the “why” behind the changes and the benefits for patients to help address the initial pushback. Emphasizing a mutual goal, patient well-being, aligned everyone’s effort to a common cause. RGH’s leadership remained committed not only to ensuring a smooth transition for providers but also to fostering the development of leaders and advocates at the bedside.


Encouraging staff ownership at RGH was crucial to develop employees’ sense of autonomy, accountability, and pride in the quality of their patients’ care. For RGH, staff ownership helped to cultivate continuous improvement in clinical workflow and enabled employees to expand their responsibilities. The quality improvement implementations were a pivotal step in empowering staff members to take the lead in vascular access initiatives.

The active involvement of frontline staff throughout the VAM process yielded numerous benefits. Encouraging nurse ownership over their patients’ vascular access care resulted in improved decisionmaking, reduced unnecessary lines, and enhanced patient care. Ensuring that all team members were educated and knowledgeable about relevant protocols fostered an environment conducive to positive change. By engaging the workforce and making them feel like leaders in the process, there has been a notable shift in ownership and commitment at RGH. Looking ahead, it is crucial to recognize that building a culture where nurses feel highly utilized and motivated enables them to embrace significant cultural shifts.
Evidence-based practice is essential to ensure the delivery of high-quality, effective, and safe services. By integrating evidence from literature in conjunction with clinical expertise, RGH made informed decisions to enhance clinical care.
RGH’s commitment to data-driven improvement was integral to improving care quality. This commitment entailed ongoing data monitoring, regular assessment of practices, and openness to implementing additional changes. The VAT team monitoring labs for every PICC line following insertion allowed for the collection of real-world data to serve as reference points in providing best practices and avoiding infection. By refining protocols and incorporating data monitoring, RGH ensured compliance with internal quality metrics, facilitating continuous improvement in patient care.
Building on the initial successes, RGH remains committed to continuous evolution and improvement of vascular access practice. Following the initial VAM assessment, RGH and BD have continued their collaboration, as seen through additional follow-up assessments to track progress, implementation of additional protocols and VADs, and commitment to continuous education to refine vascular access practice at RGH. These regular assessments have allowed the teams to identify new ways to strengthen vascular access care at RGH, and show the benefits of continuous evaluation and close collaboration between providers and device vendor.
Improving vascular access management requires a thorough assessment of all pieces of the current standard of care. In this case, the VAM assessment served as an invaluable tool, offering insights that helped minimize clinical complications, ensure the proper selection and maintenance of devices, and refine protocols for care delivery. By systematically evaluating and improving upon these aspects, healthcare providers can enhance patient safety and optimize outcomes.


“Despite facing initial resistance, the successful implementation of new teams, protocols, and devices underscores the adaptability and resilience of this healthcare organization.”
The comprehensive VAM assessment led to the establishment of a vascular access team, protocol refinement, and product standardization at Raleigh General Hospital. All these initiatives aided in reducing hospital-wide infection rates and enhancing patient quality of care. In illustrating these points, this case study serves as a compelling example of the transformative impact that well-designed quality improvement initiatives can have on a facility. By partnering with a vendor and taking a holistic approach of first identifying challenges in current practice, BD and RGH were able to develop evidence-based, actionable solutions to evolve standard of care.
Despite facing initial resistance, the successful implementation of new teams, protocols, and devices underscores the adaptability and resilience of this healthcare organization. Through effective leadership, clear communication, and a commitment to patient-centric care, RGH providers embraced necessary changes to enhance patient outcomes and satisfaction. As such, this case study underscores the importance of assessing current practices to seek continuous improvement in healthcare delivery.
Research and editorial support was provided by Halit O. Yapici, MD, MBA, MPH, Nick Bettencourt, BS, and Julia Bogart, BSPH of Boston Strategic Partners (funded by BD).



1. Kelly, L.J., The family of vascular access devices. Journal of Infection Prevention, 2009. 10 (1_suppl): p. S7-S12.
2. Moureau, N.L. and E. Alexandrou, Device Selection, in Vessel Health and Preservation: The Right Approach for Vascular Access, N.L. Moureau, Editor. 2019, Springer International Publishing: Cham. p. 23-41.
3. Carr, P.J., et al., Vascular access specialist teams for device insertion and prevention of failure. Cochrane Database Syst Rev, 2018. 3(3): p. CD011429.
4. Morrell, E., Reducing Risks and Improving Vascular Access Outcomes. J Infus Nurs, 2020. 43 (4): p. 222-228.
5. Morrow, S., et al., Vascular access teams: a global outlook on challenges, benefits, opportunities, and future perspectives. Br J Nurs, 2022. 31(14): p. S26-S35.
6. Hospital, R.G. Raleigh General Hospital. [cited 2024 May 17]; Available from: https://www.raleighgeneral.com/
7. Acito, M., et al., Strategic Integration of Technology and Practice Model Enhances the Standard of Care for Inpatient Blood Draws. Nurse Leader, 2024.
8. Selchow, J., K. Alsbrooks, and S. Salmon, Innovative Needle-Free Device Drives Evolution in Standard of Care for Inpatient Blood Draws, in Healthcare Value Analysis AND Utilization Management Magazine. 2023.



Anne
Marie Orlando, RN, MBA, RCIS, CVAHP, Senior Director, Clinical Programs at Blue.Point Supply Chain Solutions; Treasurer, Association of Healthcare Value Analysis Professionals
In today’s healthcare environment, value analysis (VA) teams face mounting pressure to balance ever-increasing costs with maintaining or improving clinical outcomes. To tackle this, value analysis teams rely on data and lots of it. Afterall, data is the cornerstone of any successful VA program. Collecting accurate and timely data lays the groundwork for evidence-based decisions. Without data, teams cannot identify trends, benchmark performance, or measure the impact of their initiatives. However, data alone is not enough. When improperly organized or presented, it can overwhelm stakeholders or lead to analysis paralysis. To extract meaningful insights, data must be contextualized and organized into tools that promote clarity and action. Dashboards serve an important role in this process, and they can elevate efforts to drive sustainable, impactful change. An effective dashboard will not only visualize data but also provide a roadmap with actionable insights.
A well-built dashboard is a powerful tool for real-time or near real-time monitoring of key performance indicators (KPIs). It provides a snapshot of performance, allowing teams to quickly identify successes and areas needing intervention. Dashboards are highly visual, often featuring charts, graphs, and filters that allow users to drill down into specific data points. Key benefits of dashboards include:
• Real-Time/Near-Time Monitoring: Teams can track ongoing performance and quickly respond to deviations or emerging trends. Dashboards are ideal for monitoring real-time or short-term performance.
• Custom Views for Stakeholders: Dashboards prioritize visualization and quick insights. They can be tailored to meet the needs of different audiences from VA to supply chain to clinical leaders.
• Simplified Decision-Making: Visualizing complex data in an intuitive format accelerates understanding and action.
• Enhanced Collaboration: Dashboards provide a clear framework for evaluating success, ensuring all stakeholders are aligned and accountable. It encourages collaboration by presenting data that is easy to understand and relevant to diverse stakeholders. Dashboards enable real-time discussions.
• Proactive Problem-Solving: Dashboards’ real-time data empowers teams to act quickly on emerging issues, such as supply chain disruptions or budget overruns.
• Demonstrating ROI (Return on Investment): Dashboards provide tangible evidence of value analysis initiatives, making it easier to secure buy-in from leadership.
To maximize the impact of a dashboard, value analysis teams should define key metrics that align with organizational goals, such as infection rate reduction, cost savings, or patient/staff safety. Consistency and accuracy must be ensured by standardizing data sources and using reliable, unified information. Tools should be tailored to stakeholders by developing views that address the unique needs of different audiences. Finally, these dashboards should be regularly updated and iterated to remain relevant as organizational priorities evolve.
In value analysis, data is the foundation, but tools like dashboards transform it into actionable insights. Numerous third-party tools are available to unlock the potential of data, while more advanced organizations may opt to develop solutions on their own. By using dashboards for real-time monitoring, organizations can ensure their efforts drive meaningful and measurable improvements. This will not only enhance decision-making but also promote accountability, transparency, and collaboration across the organization. In an era where healthcare faces increasing complexity and financial pressures, investing in these tools is a critical step toward achieving sustainable success.
Anne Marie Orlando, RN, MBA, RCIS, CVAHP, Senior Director, Clinical Programs at Blue.Point Supply Chain Solutions; Treasurer, Association of Healthcare Value Analysis Professionals
Anne Marie has been a critical care nurse for over 19 years with a leadership foundation in the Interventional Cardiology and Interventional Radiology space. During her supply chain tenure, Anne Marie held a dual role of Supply Chain and Clinical Resource Director where she operationalized many clinical initiatives while maintaining fiscal accountability. At the GPO level, Anne Marie served as the Director of Clinical Services for Yankee Alliance supporting member value analysis teams and their work with clinical utilization. Anne Marie is currently the Senior Director, Clinical Programs for Blue.Point Supply Chain Solutions supporting value analysis teams in the use of the Blue.Point platform focusing on aligning product utilization and standardization with evidence-based practice.




Robert W. Yokl, President, SVAH Solutions




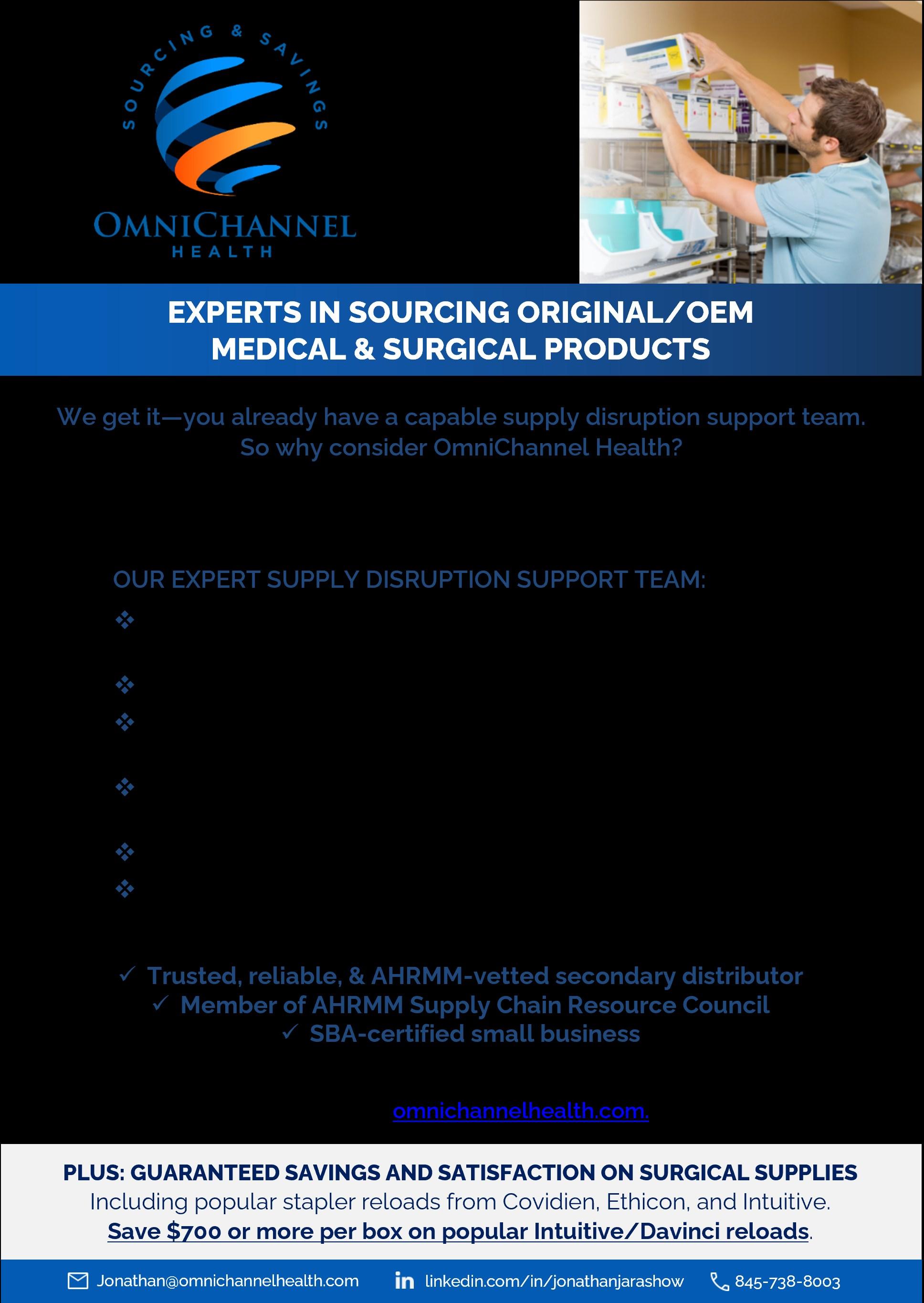
Third-party suppliers are here to stay in healthcare. They not only help you fill the holes in procurement but can also bring significant savings with equal or even the same products that you normally buy. This just makes sense in today’s healthcare marketplace where we have seen major issues with everything from IV solutions, lab products, and even simple things like evacuated containers. This list could be endless, so it is wise so start to line up your third-party vendors to help your healthcare organization be prepared in case of an emergency.
If a critical instrument is not available for a surgical case, that may cause the case to be delayed or even cancelled. Surgical time is premium time at healthcare organizations so you really must make sure that everything is available, but if you are missing one of the bread-and-butter instruments that the surgeon must have, you may not have much choice but to delay/cancel the case. Supply chain, the masters of alternatives, must start to incorporate more alternatives beyond their normal calls to other health systems or various national distributors which leads to adding third-party vendors into the mix.
Robert W. Yokl
Who doesn’t like to have an ace in their bullpen that they can call on to get them out of a jam when it comes to product availability in a pinch? That is what your third-party suppliers should be. Product availability is paramount as nothing gets done without certain products. You can’t bill for a case if your surgeon must cancel their procedure because some innocuous instrument that has always been in stock is suddenly not.

“Our clients know the value of having relationships with third-party vendors, especially when dealing with things like robotic devices.”
When it comes to any shortage of products, it will not only be hitting your organization but more than likely your entire region or even nationally. If you already have a relationship with a third-party vendor, they can help you a lot more easily than if you are starting the relationship from scratch in crisis mode. Let’s face it, you are probably not going to be high on the priority list without having that relationship in place because your third-party vendor will have to take care of his partner clients first. You can avoid these instances altogether by developing partnerships with third-party suppliers now versus at the time of crisis. It is always better to be proactive rather than reactive.
Everyone knows that robotic cases are more costly than most other cases, but what’s worse is that you may be missing a vital instrument, staples, or a suture device that can jeopardize your case. That is why many of our clients welcome not only one third-party supplier, but some have two or three for certain categories. They know the value of having relationships with third-party vendors, especially when dealing with things like robotic devices.
Saving money on OEM (Original Equipment Manufacturer) products is also a benefit to consider, as pricing can be very challenging and you want to get more savings on board wherever possible. Most third-party suppliers offer products that they can discount beyond what a group purchasing organization or custom contract with the OEM can cover. This may take a bit more time to facilitate in order to get more savings but will likely be no different than the time you spend working on implementing and changing products with your current portfolio.
Robert W. Yokl


With all the positives outlined in this article, you may be thinking that it is not all shiny and rosy with any vendor and wondering how working with third-party suppliers could be any different. I’m not sure this is a negative but there is a bit of competition with third-party vendors. If you develop a relationship with multiple third-party suppliers, you will learn the strengths and weaknesses of each one. Imagine you have a go-to vendor to get the best price on robotic devices and a secondary that may not have the best price but is close and always has available products when you need them. With already built relationships you can safely test the waters and have your value analysis teams validate every device to ensure that nothing goes awry. It is better to do these evaluations when you’re not under any timeline duress.
There are numerous benefits to partnering with third-party vendors. If you already have a few successful partnerships, I encourage you to keep exploring the areas where you can take advantage of this growing opportunity for savings and available products when the time comes. Of course, if you have had limited exposure to third-party suppliers, now may be the best time to explore the possible savings and products available for your own healthcare supply chain organization. It is beneficial to develop these relationships now.

Robert W. Yokl, President, SVAH Solutions




Clinical supply utilization management (CSUM) is not a one-time event but instead is a fluid and ever-changing system to track everything in your supply chain using patient volume centric metrics to ascertain where savings, problems, and quality improvements are. Most organizations think of supply utilization as spend management, but it is really about consumption, overuse, waste, inefficient use, life cycle shortfalls, and feature-rich products. The fluidity of CSUM is because of the ebb and flow of the month-by-month and year-by-year healthcare supply chain spend to patient volume dynamics. It is ever changing, and a new savings opportunity pops up every month when you update your data. In essence, it is the gift that keeps giving major savings.
CSUM has been a wonderful system for me and my clients over the past 15 years since we implemented our CSUM solutions with savings on average being 5% to 11% of total supply budget. CSUM is comparable to the days when a hospital or health system finally broke down and joined a GPO, then implemented the contracts and realized millions of dollars in savings. The savings have continued for them up to this day, although they are no longer as high due to market conditions.
Robert W. Yokl
CSUM is similar to implementing a GPO contract because most health systems are currently doing little to nothing about their CSUM enterprise-wide, so there will be huge savings right from the get-go. I remember one health system client we started working with on CSUM initiatives that saved $2 million in only four areas of opportunity. That was only four opportunities, and they had hundreds more.
Every time you update your data, whether it be monthly or quarterly, you will find as we do that something has changed and some products’ cost per metric is skyrocketing, but at least now you know this and have proof that this is happening. Every month when we update our client’s data, we find so many savings opportunities that we have to be strategic in what we recommend is a good savings opportunity at that time. You want to be in this place too and have more savings than you need so you can pick and choose the right opportunities and the right time.

“

Having the best price is great but if you are using 23% to 42% more Cath Lab Balloons (Balloon Cost Per Cath Lab Case), IV Sets (Cost Per Adjusted Patient Day), or CRM Devices
(Average Cost Per Implant), then you are losing real bonafide savings by ignoring that this is happening.”
Price and standardization are undoubtedly a factor of supply utilization but at best you can maybe affect up to 20% of the total cost of a product or service, whereas with CSUM you have more of the product pie to go after - even up to as much as 100% if you eliminate a product you don’t need. It will show you that you are running too high in some areas and will put firm numbers to the actual opportunities you need to work towards to reduce costs further.
Some think that if they get the best price and standardization that they don’t need to worry about things like supply utilization because they have the best pricing and thus feel that they have the best overall costs. That cannot be further from the truth because there are two simple aspects to product procurement that dispute that idea. First, you have rich products that have rich features. If you are using the Rolls Royce of any product category and only really require the Ford or Chevy model, then you are going to have higher costs on those products. If you own a BMW, you know that the maintenance costs alone, not to mention the payments, will be much higher than owning a Kia or Honda that will still get you to where you need to be and will probably have more features than that base model BMW you overpaid for. It’s the same with healthcare supply chain products, and there are hundreds of them within most categories that we need to get right.


Robert W. Yokl
Second, which I have found most important in my 33 years of performing value analysis reviews, is the quantity of products you use. Having the best price is great, but if you are using 23% to 42% more Cath Lab Balloons (Balloon Cost Per Cath Lab Case), IV Sets (Cost Per Adjusted Patient Day), or CRM Devices (Average Cost Per Implant), then you are losing real bonafide savings by ignoring that this is happening. Wouldn’t you want to know what categories are running amuck by using real datacentric methods, key performance indicators, and multiple benchmarking methods to truly identify savings opportunities forever?

Somebody must manage the CSUM program, and we have found that your VA managers and teams are the perfect fit for this. They will require more training so that they understand the dynamics they are dealing with, but once you have that in place and get a few wins under your belt, you will be off finding savings on an ongoing basis. VA does not have cost savings reporting tools dedicated to them and let’s face it, the VA process is spot-on to drill down to the root cause and then implement solutions to achieve the next level of big savings.
There is a starting point to everything and CSUM is no different in that you need a starting point to start tracking from and measuring your peaks and valleys that will help you uncover areas of needed cost and quality improvements. I highly recommend that you utilize a database for CSUM as we have found that is the best for reporting this information out. Data will need to be cleaned and validated as well but it is not as difficult as you might think, and the big savings juice is definitely worth the squeeze. If you have any questions, reach out to me at ryokl@svahsolutions.com.
The good news is that you still have time to lead your organization down the CSUM road and start to capture this low-hanging fruit that has been sitting there forever because you did not realize the value of the big savings it could bring about. CSUM not only points you to big savings but also tells you where you are achieving best practice level cost and quality results which are highly valuable. These are just a few of the advantages of CSUM. Once you start your program, you will wish that you had implemented one sooner. There is no time like the present to start planning out your CSUM program.




Robert W. Yokl, President, SVAH Solutions




Value analysis begins and ends with the customer, and it is ever more important to learn as much as possible from our customers, stakeholders, and experts on our VA projects. You must be a good interviewer to bring out not only what your customers want or need but then also be able to translate that to real value analysis functional requirements, life cycle value, reliability, and quality. Remember, value analysis is the study of function and the search for lower cost alternatives with equal or better quality/reliability. You just can’t rely on what is requested on a piece of paper or on what product they have been using for the past few years to give you all your answers. You must go directly to the source which is your customers, stakeholders, and experts.
I remember a few years back when I was sitting in a conference room at a client hospital because our linen utilization reporting discovered that the Emergency Department was using too many bath blankets by over 300% more per month. The ED using more bath blankets was not in dispute for this meeting so it was important we find out why and what could be done about this. But this was not just
Robert W. Yokl
a meeting with the ED Manager and/or Director. We also had the ED Chairperson who heard about our outrageous linen utilization report that stated that her department was using 300% more bath blankets, and I could tell by the look on her face that I was in for a fight.

“Prepare your questions ahead of time so that you can ask smart, well-thought-out questions that are worthy of your customers’ and stakeholders’ time they are sharing with you.”

Instantly, the ED Chairperson started the meeting and promptly tried to squash the excessive usage of bath blankets with the fact that they were so busy in their ED and were so unique that they required more bath blankets than most other Emergency Departments. Basically, she was not going to let this discussion go any further, but I was determined to interview both the Chairperson and the ED Manager on this topic. As soon as the ED Chairperson finished talking, I asked one question. “What are you using to elevate patients’ limbs in the ED?” All eyes turned to the ED Manager, and she said, “We use bath blankets and as a matter of fact, we use two or three per elevation sometimes.” Next, I turned to the Environmental/Housekeeping Data Analyst (yeah, they were so big they had an analyst in Environ.) and asked him what the difference in cost was between laundering a towel and a bath blanket. He said that they could use up to eight towels before equaling the cost of laundering one bath blanket. Bingo! Everyone realized that they should be using towels for elevation instead of bath blankets. Two questions and a big savings!
You May Only Get One Shot for a VA Interview - Make it Count
Hospitals are a busy place, and if you are going to set up a time to interview a key customer or stakeholder, you better be prepared to ask all your questions because you may only get that one chance. Yes, prepare your questions ahead of time so that you can ask smart, well-thought-out questions that are worthy of your customers’ and stakeholders’ time they are sharing with you. This will also force you to craft valid questions to ask your key customers and stakeholders as sometimes you want to just talk about the product they are requesting or that is causing a problem. Remember, healthcare is a busy place, and you cannot expect them to provide you with all the nuanced details of their use patterns, outcomes, and problems with a product unless prompted to with a good question.
You cannot expect to be a subject matter expert in many of the product, service, and technology projects that you work on in VA as it would be impossible to acquire that much experience. You don’t have to be a subject matter expert. All you need to do is find out who knows the most about that
Robert W. Yokl
product, service, or technology within the organization or even outside your organization for them to be your resident expert. Recruit your resident expert who hopefully does not have any bias one way or the other of the changes that could be made with your VA project but instead wants the project to succeed. Then you will work with your resident experts to find out everything about your product or service and they will assist you in crafting the questions you want to ask in your interviews with the key customers and stakeholders.

Once you do have an interview with your key customers and stakeholders, you want to rely on that information to build your functional requirements or brainstorm for solutions to the problem that is the reason for your VA project. You will need to validate what your customers and stakeholders provide for you and the best person to do that with is your resident expert. They can point you in the right direction to find out more facts or be able to speak for the information provided to you by the key customers and stakeholders during your interviews.
I learned a long time ago from a trainer that followed the Barbara Walters style of question asking where she always seemed to get those close-to-the-vest celebrities, statesmen, and even Presidents talking like none other. She frequently used questions like, “Can you explain to me? Can you describe for me? Tell us about…, etc.” These are powerful questions that will get your customers to open up to you like you never thought possible. “Dr. Jones, can you explain to me exactly what is not working right with your current surgical energy instrument versus the instrument you are requesting in your new product request?” It is powerful to ask the right questions!
VA interviewing may be one of the most difficult skills to master because there is no training for being a good interviewer when it comes to VA projects. Just because you have open communications with your key customers and stakeholders does not mean that they are going to offer up everything you need to produce a viable VA project result. It is your job as a VA Practitioner to seek out the answers to the tough questions but first you must craft the right questions in order to be successful. Master this skill and there is nothing you can’t uncover in your VA projects moving forward!
Mark Copeland, Vice President, Sales, 3T Medical Systems, Inc.



I hear an underlying current of frustration and anger from vendor reps across the country all the time.
“Value analysis committees are trying to keep new products out of hospitals.”
“Value analysis committees just reject everything unless it’s cheaper.”
“Value analysis committees hate vendor reps.”
Hmmmm, value analysis committees HATE vendor reps?
Ah yes, I call this attitude the “Aluminum Foil Hat” theory of the “Why can’t I get my new product requests approved in health systems?” line of questioning. I hear it constantly.
My colleagues and friends in medical device sales and marketing, please allow me to pop the “nobody likes us” balloon: VACs do not hate you. VACs do not even know who you are.
VACs do not hate you. VACs do not care about you at all.
But VACs do hate your new product requests.
Because value analysis committees are not searching for your product. I know it may be counter-intuitive, but VACs are constantly searching the web, Googling “cool new med tech” to see what’s out in the great big medical device world.

“Most VAC packs are just advertisements telling me how great the product is and how to buy...no context.”

Nope, value analysis committees are looking to solve the health system’s PROBLEMS. Or align with the health system’s STRATEGIES. Or at least improve patient care AND save some money. Or time. Or reduce staffing requirements. They aren’t looking for YOUR product. They are looking to improve the health system’s outcomes (patient care) and bottom line (financial), while strengthening the health system’s position versus competition (strategy).
Yes, value analysis committees could make the new product request process a little more transparent…to their clinical teams. More clarity would certainly be appreciated by doctors and nurses.
But VACs do not owe the medical device industry anything. Ask yourself this: Do YOU owe the cable company an explanation as to why you will not switch to them? They send me brochures all the time by snail mail. These brochures are just lousy marketing pitches talking about their product, without understanding if I am happy, frustrated, or even interested in learning more. I pay no attention to the brochures and pitch them on the way in from the mailbox…and I’ll bet you do too.
Certainly, I feel no obligation to explain to Comcast my decision-making algorithm. I feel no obligation to Comcast at all. Nor do you, I am willing to wager.
So why do we expect a VAC to feel like they owe US any explanation, much less “like us?”
I read 3-5 VAC packs a week, submitted by medical device vendors. Most are just advertisements telling me how great the product is and how to buy. These VAC packs mirror the brochures I receive from Comcast. Lots of words and promises no context and no idea whether I even need Comcast.
Shoot, I am trying to cut the cord, not use a different cable company at a cheap introductory price so that I can be locked into a long-term, high-priced contract with automatic price increases built in. And have their service team traipsing through my house? No, I’m good, thank you very much….
Copeland
But we in the medical device industry insist on asking clinical champions to take valuable time and risk political capital to get OUR PRODUCT approved in the VAC’s hospital. There’s NOTHING about the value to the health system. Just a bunch of words and phrases in Latin telling me about some clinical “problem” that VAC do not even know exists.
If I am on the VAC, there is a good chance I’m a businessperson, supply chain leader, or healthcare administrator. I am not a doctor or nurse. I would not know cardiac aFib from a fibular strut. I need context and an explanation from a requesting doctor or nurse that shows me WHY we are even looking for something new, HOW much it costs, WHAT we hope to accomplish if we buy it, and WHO will use it if we do end up approving the new product.
My advice to every rep, product manager, VP of Sales, and founder with whom I consult is to describe:

If you do these five things, your VAC pack will now be talking about the benefits to the REAL customer (the ASC, hospital, or health system).
If your champion (the requested doctor or nurse) does the same thing, your approval rates will skyrocket. Sure, you may have to coach your champion to understand the larger picture of the needs of the ASC/ hospital/health system, but once you do, your champion will be more empowered and enthusiastic to support a new product request.
As you get better and more experienced at having new product requests submitted as “new solutions to current problems,” you ’ll find your products are more and more welcome in health systems.
You might even get a hug from a value analysis committee member!
Nah, just kidding. There are no hugs in value analysis.
But there are big wins and big benefits to thinking of the value analysis committee less like “the enemy” and more like me when I get a cable company brochure in the mail.
I don’t hate the cable company. I just see no need to bring them into my house.
VACs do not hate you or your company. They just don’t see a need to bring your product into their house.
Mark Copeland





Mark Copeland is a 28-year healthcare sales professional with the last 20 spent in startup medical device companies.
His company, 3T Medical Systems Inc, manufactures and sells innovative medical devices to health systems globally, and Mark teaches companies how to present their new product requests in a way that meets the value analysis requirements.
Contact Mark at mcope67@gmail.com for more information, or visit ValueAnalysisExpert.com.
mcope67@gmail.com (717) 579-8144


Leslie Sullivan, RN, CMRP, CVAHP



When Bob Yokl reached out to me to write this article for HCVA&UM Magazine, he challenged me to write a forward-thinking article that truly has the vision for the future of healthcare value analysis teams. In agreeing to write this article I also challenged Bob back and asked if the readers were looking for immediate next steps to take, or if the readers want a true forward-thinking, real-world, data-centric vision for VA teams of the future. Bob agreed with my thinking and asked for the real-world vision that you are seeing here.
Innovation, artificial intelligence, DEI, change management, education, and collaboration. You have heard the chatter unless you’ve been cast back in time. It’s been getting louder as we recover from the pandemic, and with the start of 2025, it’s become a near-deafening roar from the crowds. What you hear is a historic generational shift, bringing significant changes to the workplace and the dynamics of healthcare over the next 10 years. Getting familiar with the who, the when, and the why will be pivotal in understanding the impacts your teams will face and whether your current processes will be sustainable by 2035. There’s a ton of overwhelming noise out there right now.
In this two-part series, we’ll tune in on who the players are, how the game is changing, and considerations for ensuring your VA teams are bringing home the wins in the future.
Alas, your organization has finally decided to adopt a formal VA process. You're gathering industry recommendations to get a team in place, or maybe you fall on the other end of the spectrum where you ’ve finally curated the perfect VAT(s), robust with engaged physicians, highly experienced clinical leaders with board certifications, infection prevention and quality improvement nurses with advanced degrees, and maybe even C-Suite representation. The members have an astonishing number of years of education and hands-on experience. Great!... But…
Will your team of MVPs and selection processes be sustainable or make sense in the next 10 years? If you ’ve given a confident “YES!”, we want to talk. If your answer is “NO”, you ’re already a step in the right direction. If you haven’t thought about it until now or just don’t know, most VA leaders are likely to have a response, so you're in good company and got here with perfect timing.
The first step to answering this complex question is knowing who the generational players are, their statistics over time, and their general attributes. Because an endless amount of information is available on the subject, slight deviations occur in the data. The table below provides a high-level approximation of the past, present, and future workforce spanning over 30 years. We’ll look at the colors like a heatmap, red being the hottest and most critical shifts.
*Source: EY Analysis – United States Bureau of Statistics
Each generation has been identified with attributes that characterize the group as a whole. The following list is not comprehensive and does not suggest that individuals cannot share core values from outside their generational cohort. However, our perspectives are developed by societal exposure throughout our lives. For instance, a Baby Boomer may have a strong commitment to justice and equality due to experiencing the civil rights era, yet most are accustomed to traditional and in-person organizational structures and have been for over 50 years.
Baby Boomers Senior leadership positions
Generation X Middle management
Generation Y (Millennials)
Expected to dominate senior leadership roles
Generation Z Rising to significant positions
Alpha Generation Future workforce (14% in 2035)
Prefer clear hierarchies and formal structures
Achieving goals, high-quality work, adaptable, independent
Purpose-driven work, inclusive culture
Entrepreneurial, innovative, dynamic environments
Adaptable, tech-savvy, collaborative, innovative
Professional accomplishments, quality healthcare, long-term employment
Financial security, long-term employment, practical, skeptical
Align careers with values, support positive societal contributions
Diversity, inclusion, global citizenship
Comfort with technology, creativity, social consciousness
Practices, processes, and standards in the healthcare supply chain and value analysis have largely been shaped by the experiences and perspectives of Baby Boomers, along with the increasing integration of Generation X viewpoints. Over the past several decades, their use of hierarchical structures, organizational commitment, and goal-achieving ambitions significantly contributed to industry reliability and resilience. However, as we approach substantial generational shifts, it is essential to re-evaluate current practices.
The demographic transition will see Millennials and Generation Z assuming more prominent leadership and decision-making roles within the healthcare sector. They seek opportunities for growth, learning, and acquiring new skills. Their innovative outlooks and strong affinity for technology and digital advancements are expected to drive transformative changes. Both generations strongly commit to diversity and inclusion inside and outside the workplace. They prefer environments that encompass not only racial, gender, and ethnic diversity but also various perspectives and backgrounds. Organizations prioritizing policies promoting equal opportunities and cultivating a culture where all voices are acknowledged and valued are more likely to retain these young professionals.
The healthcare industry has been preparing for a labor shortage for years. Most institutions have recognized the critical impact this will have on patient outcomes. Thus, homing in on their recruitment efforts to attract post-Gen-X talent and retention strategies like sign-on bonuses, tuition reimbursement, and offering benefits that promote mental well-being. Let’s not forget about DEI initiatives and how they will impact your future VA teams.


“Incorporating varying perspectives helps contribute a wide range of experiences and viewpoints, resulting in more comprehensive solutions, better prepared to adapt to changing market conditions, and improving organizational outcomes.”
Adopting DEI initiatives intersects with health equity and is essential for aligning health system brands with the future workforce's values, attracting and retaining diverse talent while fostering inclusiveness. Diverse and inclusive teams enhance cultural competency, improve patient care, reduce bias, drive innovation, and improve financial performance. Health equity ensures that care is administered equitably, leading to better patient outcomes and reduced disparities.
Healthcare organizations have an ethical duty to reflect the diversity of their communities and provide equitable care. The same goes for your VA teams. Incorporating varying perspectives helps contribute a wide range of experiences and viewpoints, resulting in more comprehensive solutions, better prepared to adapt to changing market conditions, and improving organizational outcomes.
I challenge you to assess your teams/committees at their current state. Do you have members from emerging generations? Can your members represent the communities they serve? It’s impossible for even the largest institutions to represent every population but using the criteria below will give you a guide.
Leslie Sullivan
Due to the sensitive nature, it is strongly advised to use only information that is made publicly available, that your participants have openly shared, and/or that is visibly apparent.
If you choose to make notes, keep them private and avoid using names.
Consider a tallying approach or YES/NO.
If your organization is actively working on improving DEI efforts and/or has a DEI officer, reach out for guidance.
Category
Race/Culture
Organizational Title Tech Specialist/ Analyst Mgr/Sup/ Coord Director Executive/ C-Suite/ Senior
published bio’s. Don’t ask!)
Leslie Sullivan


In part two of the series, we’ll take a deeper dive into establishing your VA succession plan and discuss the steps you should be taking now to ensure a smooth transitional shift.
Covering
• Training Gaps and Opportunities
• Mentoring/Internships
• Recruiting Vs. Appointing
• Technology/Innovation
• VA Beyond the Hospital Walls


Leslie Sullivan, RN, CMRP, CVAHP, has been a registered nurse for 19 years, building her clinical and leadership foundation in the ER and Procedural Endoscopy spaces.
She transitioned from the bedside to begin her Supply Chain and Value Analysis journey in 2018. Since then, she has delivered transformative solutions that streamline operations, reduce costs, and improve patient outcomes. Her passion and commitment to building relationships through authenticity, transparency, and empathy have been key to her success in the healthcare industry.


