All personal information (necessary for hospital and government records) will be considered strictly confidential. It is important that you make staff aware if you have an Advance Directive / Living Will or if you have been in a hospital outside of Ontario during the past year. Hospital wrist identification bracelets are used for all patients.
1. Provincial Health Card
2. Other Health Insurance Card
3. Medications:
Bring all current prescriptions and non- prescription medications (including over the counter, herbal, etc.), in their original containers. Some medications are not supplied by the hospital and you may be required to supply your own. Any medications required during your stay will be prescribed by your doctor and will be brought to you by your nurse. Please tell your doctor and nurse if you are allergic to any medications or have any other allergies. If you have any questions about your medications, your doctor, nurse, or the hospital’s pharmacy staff will assist you.
4. Copies of your Advance Directives (e.g. Do Not Resuscitate directive) / Living Will
5. Personal Items:
You should bring only necessary personal toilet articles such as a toothbrush, toothpaste, denture cream, comb and brush, shaving items, or cosmetics. Although the hospital provides patient gowns, you may want your own easy-on-and-off pyjamas or nightgown together with a bathrobe, comfortable clothes and non-skid slippers or shoes.
Please do not bring:
• Valuable papers or documents
• Scented personal care products
• Items of sentimental value
• Jewelry or expensive clothing
• Large amounts of cash
• Alcoholic beverages or illegal substances
Please note that any patient-supplied electrical appliances may be sent to the Maintenance Department for a safety check. The hospital is not responsible

• Nurses
• Dietitian
• Discharge Planner
• Laboratory Technicians
• Diagnostic Imaging Team
• Physicians
• Occupational Therapist
• Pharmacist and Pharmacy Technicians
• Physiotherapists
• Rehabilitation Assistant
• Personal Support Workers
• Respiratory Therapist
• Social Worker
• Speech-Language Pathologist
• Student nurses and physicians
• Clergy / Pastoral / Spiritual Care
• Volunteers
The hospital is a place you come to get well, but you also can come in contact with germs that can make you feel worse. Reduce your chances of infection by taking these safety precautions:
1. Clean your hands after touching hospital objects or surfaces, before eating, and after using the washroom.
2. Ask hospital staff members to clean their hands. This should be standard practice for staff, but don’t be afraid to remind them if they forget or to ask them to wear gloves. Ask your visitors to clean their hands too.
3. Cover your cough if you are sick. If you get an infection, limit the spread of germs by sneezing and coughing into tissues that you promptly throw away, and avoid touching other people. Ask the staff if there is anything else you should do - like wear a protective mask - to prevent the spread of germs.
4. Keep an eye on bandages dressings. If a dressing on a wound or IV becomes loose or wet, let your nurse know. Also, if you have a catheter or drainage tube, tell your nurse if it becomes loose or dislodged.
5. Keep your vaccinations up-to-date. Make sure you are as protected as possible from the spread of infection. Check with hospital staff about whether it’s safe for you to receive any vaccines you might need.
6. Keep your room tidy. Do not bring too many belongings into the hospital. If your bed area becomes too cluttered, it is difficult for the housekeeping staff to clean. Patients should limit the number of personal belongings they bring with them to the hospital, such as magazines, pictures, and clothes.
Tell your friends and family not to visit if they are sick, and make sure all your guests clean their hands when they enter your room.
Cleaning Tip: Use soap and water or alcohol- based hand sanitizer under your nails, in between your fingers, and on the palms and backs of your hands. Rub for 30 seconds (the time it takes to sing “Happy Birthday” twice).

Some patients are on “isolation precautions”. This is usually done to protect the patient and others from infection. If you are in “isolation,” ask your nurse what your isolation means and what you should expect from the hospital staff or visitors. Gloves, gowns and masks are sometimes appropriate, depending on the illness.
A fall can happen to anyone in any place at any time. During your stay in the hospital, we will:
• Ask questions about how you move around or if you have had a fall before.
• Show you around your room, bathroom, and nursing unit.
• Keep your room and walkways clear and free of tripping hazards.
• Keep important things close to you so you can reach them, such as your call bell, walker, glasses, phone, and this Patient Handbook.
• Check in on you every hour to make sure you are comfortable and have what you need.
• If your patient care team concludes that you are at risk for falls, they will add special safety measures to your care plan.
To prevent falls:
• Wear non-skid shoes that fit well.
• Take your time and use your mobility aid when moving around.
• Sit upright for a few moments on the edge of your bed before standing.
• If you feel weak, sleepy or dizzy, ask your nurse for help before you get up.
• Get up slowly and make sure you feel steady before walking.
• If your patient care team has told you that you need help getting up or to walk, always use the call bell and ask for help.
Everyone wants to have the safest care possible while in the hospital.
Our staff realize this and are committed to providing you with safe, quality care. We encourage you to take an active role in your health by paying attention to the care you receive and by asking your healthcare team questions regarding your care. We want you to know that it’s OK to ask when you’re not sure:
• Have they washed their hands to prevent the spread of infection?
• Have they checked your identification before providing tests, treatments, etc.?
• Do you need help or have any questions?
Are you deciding to stay in a PRIVATE or a SEMI-PRIVATE Hospital Room?
If you are, here are some questions to ask yourself and your Health Insurance Provider.
• Am I a chronic care patient?
• Will my insurance cover the cost of my room?
• What is the daily maximum amount that my insurance will cover?
• Is there a maximum amount per stay that my insurance will cover?
• What percentage (%) of the cost will my insurance cover?
It is important for you to know the answers to the above questions, and if you are unsure, call your insurance provider. If your insurance does not cover the full cost during your stay, any portion not covered by your insurance will be your responsibility to pay.
Here at HGMH, we want all our patients to recover in a room of their choosing, and when making this choice, having full knowledge about the potential costs associated with PRIVATE and SEMIPRIVATE rooms.
Our Patient Registration Staff will make every effort to provide you with the type of accommodation you request. We will endeavor to provide patients with their requested accommodations. However, isolation cases and occupancy may prevent us from doing so.
If you have insurance coverage, please let our staff know. During your stay, you may be admitted to a mixed gender room.
Upon Admission to the hospital, you will need to review and/or sign off on the following paperwork:
• Consent form for your physician who will be looking after you;
• That you are responsible for your valuables;
• That you understand that the hospital and hospital grounds are non-smoking;
• What type of room you request and are insured for, if applicable; and
• Ministry of Health Claim form if you are a non-resident of the province of Ontario.
HGMH is pleased to provide all patients and guests free access to our public wireless network. Select HGMH-Guest under your network options on your mobile, tablet or laptop device, and read and accept the usage agreement. No password is required.



www.hgmh.on.ca

We’re excited to partner with the SD&G Library to enhance your experience during your stay. You can now access a wide range of e-books, audiobooks, educational courses, and other digital resources directly from your personal device or a borrowed device while admitted to the hospital. Enjoy exploring these valuable resources while you recover. Speak to someone from your healthcare team if you would like more information.

Every effort is made to keep the hospital as quiet as possible for you to be able to rest while you are a patient at our hospital. However, there are times when you will hear alarms and bells of various sorts going off. Staff respond to these bells as needed. You may hear messages from the overhead paging system advising of a “Code” or a “Mock Code” that is in progress. Please do not be alarmed by these bells. Our staff will ensure you remain safe during any emergency situation. They may close your door or ensure you are safely moved to a location out of harm’s way. We perform regular exercises or “mock codes” of various types,
including monthly fire drills. While these bells are loud and distracting, they are necessary to ensure our staff are well practiced and prepared to respond to an emergency situation. We thank you for your patience and understanding. More information about our various emergency response codes can be found on our website.
No one knows how much pain you are in but you. Tell your doctor or nurse when pain strikes or if it comes back again after it goes away. Talk about your pain level throughout the course of your stay.
Ask yourself and share with your nurse:
• Where does it hurt?
• When does it hurt?
• Does your pain keep you from doing things (e.g.: sleeping, dressing, eating)?
Which words describe your pain?
Aching
Bloating
Burning
Comes and goes
Constant
Cramping
Cutting
Dull
Numbing
Pressing
Pressure
Pulling
Radiating
Searing
Sharp
Shooting
Soreness
Stabbing
Throbbing
Tightness
You’re the expert on your pain
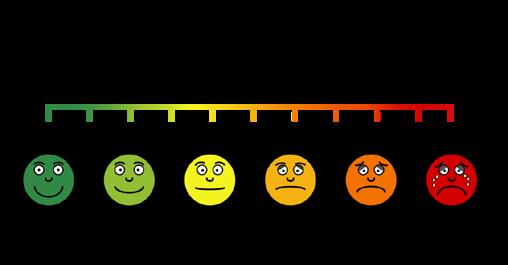
Starting to get uncomfortable? Pain medicine not working? Never let your pain level go above a 5 without speaking up!
The worse your pain is, the longer it takes to control. You may need to get more of the current pain medicine you are on or switch to a different kind of medicine
How bad is your pain on this scale?
Participating in your health care is a right and responsibility. Being active member of your health care team is one of the keys to recovery. Take part and be involved in every decision about your care. Be involved and speak up:
• Tell your nurse or doctor if something does not seem right.
• Know what time of day you normally get your medicine. If you do not receive it, tell your nurse or doctor.
• Do not be afraid to ask for more information about a medication, test or procedures.
• Write down important facts your doctors tells you, or questions you might have.
• Read all medical forms and make sure you understand them before you sign anything. If you do not understand, ask your doctor or health care professional to explain.
HGMH encourages and counts on you to participate actively in your care and welcomes your ideas to assist us in helping you.
to get relief. Don’t try to ignore painful symptoms. Managing your pain will help with your healing process. Talk to your
HELP is a patient care program that helps prevent delirium and functional decline in older hospitalized patients. Using a trained team of volunteers, HELP addresses a wide range of geriatric issues during a patient’s hospitalization by providing support to keep the patient comfortable and conducting activities to keep them mentally and physically active. This program allows patients to be discharged from the hospital as independently as possible and to prevent unplanned readmissions.
All patients 70 years of age and older, within 72 hours of admission, will be screened by the Elder Life Nurse Specialist for HELP eligibility. Should the patient meet the criteria, they will be asked to consent to participate.
Patients must be at risk for cognitive and functional decline (i.e., baseline cognitive impairment, use of a mobility device, visual impairment, hearing impairment, dehydrated). They must be able to communicate verbally or in writing.
HGMH is proud to provide the first therapeutic pool facility in a 100km radius of Alexandria. Our pool has complete wheelchair accessibility and is also equipped with a ‘water wheelchair’ for those requiring help descending into the pool.
Rehabilitation programs using the pool may be part of your care plan to support your recovery.
Patients are identified by their bracelets. Additional identification or signage may be used at the room entrances to identify violent patients or patients on isolation. If you are unsure what signage means, ask your healthcare team for clarification.
For your safety, you will be asked frequently to identify yourself or to confirm your identity prior to medication or treatments being administered.
You have access to a call bell. Call bells will be within reach of your bed and your chair. If you require assistance from your healthcare team, we encourage you to use your bell. Should you have difficulty using the call-bell that has been provided to you, please speak with your nurse about other options that are available.
There is a whiteboard located in every patient space. This whiteboard is to help provide information to the medical care team, the patient and family members.
This information is used to help with communication, patient safety and patient care quality.
Some information that can be found on this board includes:
• Treatment schedule
• The names of the staff looking after you
• Diet options
• Allergies
• Medication times
• The extension for your bedside phone
If you wish to make an external call, press 8 followed by the number you wish to call.
If you or your designated person have questions about your care, call the nursing station at extension 4126.
For questions about billing and your TV services, contact the Business Office by pressing 0.
Anyone wishing to reach you by telephone during your stay can call 613.525.2222 followed by the extension listed on the whiteboard in your hospital room.
As part of your rehabilitative process, you may be encouraged to go out on day or weekend passes. This will help the health care team to identify any problems or issues that may require further work before you are discharged. When your health care team determines that it safe to do so a gradual plan will be developed to assure safe transition.
As part of our commitment to providing the highest quality healthcare services to all members of our diverse community, interpreter services including American Sign language (ASL) are available 24/7 through LanguageLine Solutions.
All patients have the opportunity to receive visits from pastoral care volunteer services. Specially trained members of the Auxiliary attend to the spiritual needs of the patients and their families. Alternatively, should you wish to receive visits from your priest or other denominational clergy, please contact your nurse so arrangements can be made.
Should you wish to send out mail, the nursing staff will forward your correspondence to the Business Office. Regular postal fees in effect will be charged.

It is best that you do not have your own personal mail forwarded to the hospital. Please make other arrangements to have your personal mail taken care of.
Our housekeeping staff are very polite and social individuals; however, they have their daily cleaning tasks that must be completed. Please keep conversation with the housekeeping staff short. You can help our housekeeping staff keep the room clean by limiting the number of personal items in your room.
Televisions are available to rent. Ask your nurse if you wish to rent a television during your stay at our hospital. A headset must be used at all times when the television is in use so as not to disturb the rest or care of other patients.
When requesting a television rental, you will be required to sign a Patient Consent for Rental of Television form stipulating your request for TV rental and ensuring payment to the hospital for said rental. The request will be completed by the Business Office during office hours only.
Additional

Our Therapeutic Garden got its roots in 2011 with a grant from the Ontario Healthy Communities Fund through the HGMH Foundation. Over the years, the garden has more than quadrupled its original size and is used regularly by rehabilitation patients as part of their therapy. Patients participate in gardening tasks such as planting, weeding, and harvesting. This experience requires physical exercise, stimulates thought, encourages awareness of the external environment, and improves dexterity and balance. Harvests from the garden are incorporated into foods prepared in the cafeteria.
If you are interested in working in or just visiting the garden, speak to a member of your healthcare team.
Security is on site Monday to Friday from 6:30 am to 2:30 pm and every day from 10:30 pm to 6:30am.

HGMH allows visitors at any time of day. Family and loved ones play an essential role in the emotional, physical and mental well-being of our patients. We regularly revisit our visitation guidelines. Please refer to our website for the most up to date information regarding visiting hours.
It is important that you and your visitors be respectful of others in your room. Please keep the number of visitors at one time to a minimum. Visitors should not interrupt care. Hospital staff may ask visitors to leave if needed.
At HGMH, we understand that having a loved one around for our patients can be an essential part of healing. Unlike a visitor, who plays a social role for the patient, ECPs provide a patient with essential support and function as a valued member of the care team.
Visit our website for more information on ECPs or talk to a member of your health care team.
Pets are welcome at HGMH with the approval of the Primary Care Provider or Clinical Manager/designate prior to the visit. Pets must be clean, controlled and on a leash. Please ensure your pet has updated immunizations. Hospital staff may request a copy of the immunization paperwork.
should not interrupt care. Hospital staff may ask the pets and their owners to leave if needed.
Visitors are asked not to use patient washrooms for infection control purposes. Public washrooms are located throughout the hospital.

While you are visiting your loved one, you may hear warning or emergency alarms going off. Please pay attention to any messages provided via the overhead paging for an explanation of the alarm. If the emergency is just a drill, the messaging will indicate that it is a “mock” code. The most frequent drill you will hear is a “Mock Code Red” which is a fire drill. When this bell goes off, you can either stay with your loved one in their room, go to the main lobby or pool lobby, or leave the building completely. It is important to not remain in the hallways during this time. Please note that if you leave the building, you will not be able to reenter until the emergency or exercise is declared over. Depending on the situation, you may be asked to assist in moving your loved one if an evacuation is needed. More information about our various emergency response codes can be found on our website.
In Alexandria: White Rock Motel – 613-525-2362
In Cornwall: Super 8 – 613-932-8888
Ramada Inn – 613-209-0670
Best Western – 613-932-0451
First Canada Inns – 613-936-0400
In Hawkesbury: Quality Inn & Suites – 613-632-5941


First 15 minutes - Free
16 to 60 minutes - $3. After paying this fee, the pay station will indicate how much time you have left to exit the lot. You may choose to pay the full package of $ 5 if you wish to enter and exit the parking area for 24 hours.
More than 60 minutes - $5
The daily fee of $5 will allow users to enter and exit the parking area for 24 hours. You must scan the same ticket upon entering and exiting for the 24 hours to work.
There are two pay stations, one at the west exit near the pool and one near the Business Office and Emergency area. You can pay with cash, coins, debit, or credit cards at these pay stations.
Monthly parking passes (unlimited use for 30 days) can be purchased at a cost of $50 from the Business Office. Deposit required.

Star Taxi – 613-525-1422
Moon Taxi – 613-525-5252
If you need a test or specialized care at another hospital and you require an ambulance for transfer, the ambulance fees are at no charge to the patient. All other transfer services fees (provincial ambulance, non-urgent transfer service


or taxi) including to your home (including private residence, assisted living or nursing home) after discharge are the patient’s responsibility. Please ask your nurse or discharge planner for more details.
There are 2 bike racks available. One is stationed at the main entrance and the other at the pool entrance.

A 24-hour bank machine is located in the Emergency Department. Change machines can be found in the emergency room area.
Our cafeteria is located on the lower level and is open from 9:00am to 6:00pm. Hot meals are available from 12:00pm-1:30pm and 4:00-5:00pm. The food in our cafeteria is made onsite.
Sweets, sandwiches, and beverages are also available in the vending machines, located near the Emergency Department.
There are also Vending machines located near the at the Pool entrance.
Patients and visitors are served by more than 40 volunteers who maintain the Gift Shop. Light snacks and beverages, as well as a wide variety of gift items are offered for sale. Profits generated from this shop are the main fundraising source for the Auxiliary.
If you have lost an item or you would like to report a found item, please contact our Business Office at 613.525.2222 x0, located just inside the main entrance of the hospital. Remember lost items are kept for a maximum of 3 months.
A pay phone is available next to the Business Office.
A pay phone with Telecommunications Relay Services is available for persons with disabilities to use the telephone system via text telephone (TTY).


Discussions for discharge will begin early in your hospital stay, and your health care team will assist in determining the best way to meet your needs after your hospital stay. Your health care team will assist in preparing a safe discharge destination.
In your discharge plan, you will identify a safe place to live after leaving HGMH. That place may be your present home. A safe place may mean moving to another house or residence. You may want to consult with family and rehabilitation team members about a realistic plan that meets your physical, social, cognitive, and cultural needs.
You should consider what personal care and assistance you may require after you leave the hospital. If you require care, you will have to identify who your caregivers will be. They may be family members or paid personal care providers. Whoever you choose as a caregiver will need to be taught the skills necessary to properly assist you.
Discharge time for the inpatient units is 10:00am. Any costs associated with transportation to your home, retirement home, or long-term care are the responsibility of the patient or their family.
You may receive a survey in the mail. We encourage you to complete it, as your feedback helps us make improvements in the quality of care and service we provide.
If you wish to reach out to the hospital to provide feedback, please contact 613-525-2222 x4335.
Patient Accounts may be settled by mail with the prepaid return envelope provided with your bill, via the hospital’s website at www.hgmh.on.ca, or through the Business Office just inside the main entrance of the hospital. Its hours of operation are Monday to Friday from 8:00am to 6:00pm, closed on statutory holidays.
When you are getting ready to go home from the hospital or after a medical treatment, ask as many questions as you need to in order to understand:
• What treatment you received
• Whether you will have to pick up a prescription before you go home
• What kind of transportation you will need to get home
• The type of care you will need at home and if you will need someone to stay with you
• What symptoms to watch for and who to call if something does not feel right
• Whether someone will be making plans with you for home care
• What medicine you must take, how to take it, and any side effects
• What foods you should eat or avoid
• When you can go back to normal activities, such as work, school, exercise, and driving
• What follow-up appointments you will need and who will make them
You can write this information down or it may be helpful to have a family member or friend with you. They can help you to record what you should know about your care.
Your caregiver is an excellent resource and often and “expert” in your medical history. It is important to have them present (if you wish) to take notes and help with your discharge plan. Listed below are some common care responsibilities that your caregiver might assist you with:
• Personal care: bathing, eating, dressing, toileting
• Household care: cooking, cleaning, laundry, shopping
• Healthcare: medication management, appointments with your doctor, physical therapy, wound treatment, injections, medical equipment and techniques
• Emotional care: companionship, meaningful activities, conversation
Community organizations can help with services such as transportation, meals, support groups, counseling, and possibly a break from your care responsibilities to allow your caretaker to rest and take care of themselves. Finding those services can take some time and several phone calls.

Referrals to Cornwall Hospice if applicable will be organized and coordinated with the assistance of the Health Care Team.
Telemedicine is available at Hôpital Glengarry Memorial Hospital. Through this service, it’s possible you could save a drive to:
• The Ottawa Hospital
• Children’s Hospital of Eastern Ontario
• Montfort Hospital
• Queensway Carleton Hospital
• University Health Network in Toronto; or
• Other hospitals in Ontario
Telemedicine uses secure videoconference technology to provide specialized health care in our own hospital. It helps improve access to specialized medical services that are not often available in rural communities. Examples of services that can be provided at HGMH by video conference with specialized cameras and stethoscopes include:
• Pre-Operative Assessments; Mental Health Consultations; Nephrology, Cardiology, Vascular, Oncology, Hematology, Neurology, etc.
• Ask your physician when they refer you to a specialist if a telemedicine consultation is possible or ask your specialist if your next appointment can be done through telemedicine. Health care services you need can be available closer to home.



The mission of the HGMH Auxiliary is to provide volunteer services to the patients, to promote good public relations and assist the hospital in its provision of quality health care to the community. The Auxiliary is comprised of dedicated people who have given over 12,000 hours to the hospital every year. Since the Auxiliary was founded in 1966, over a quarter of a million dollars has been raised for the hospital, and an excess of one million hours of volunteer work have been contributed.
We are justifiably proud of the achievements of our incredible group of volunteers. Our top priority is the welfare of the patients, and we accomplish this by serving in many different capacities and on a variety of committees.
At HGMH, we believe that patients and families play a vital role in shaping the care we provide. Our PFAC, comprised
of recent patient and family members, is dedicated to ensuring your voices are heard and your experiences inform our services. Through collaboration, we strive to enhance the patient experience, improve communication, and foster a supportive environment for all.
If you’re interested in getting involved or learning more, please visit our website at www.hgmh.on.ca, email info@hgmh. on.ca or call 613-525-2222 X4104.
Together we can make a difference!
We take patient feedback very seriously and look at it as an opportunity to improve the services we provide. If you would like to bring a compliment or concern to our attention about the hospital’s environment, service, or the official language you were served, you can contact us in one of the following ways:
• In writing to:
Patient Relations Delegate 20260 County Road 43, Alexandria, ON K0C 1A0
• Through our websiteclick “Contact Us”
• By telephonecall 613.525.2222 x4335
All complaints, written or verbal, shall be acknowledged promptly in the official language it was received.
In 2021, HGMH was selected through an international competitive process as a pre-designated Best Practice Spotlight Organization (BPSO) through the Registered Nurses Association of Ontario (RNAO). RNAO develops and promotes the use of evidence-based best practices – interventions proven to improve health outcomes. Although HGMH staff have long followed best practices when caring for patients, new practices emerge regularly, and must be evaluated and standardized. Over three years, in partnership with RNAO, HGMH is implementing and evaluating best practices related to five areas to earn the official BPSO designation:
• Preventing Falls & Reducing Injuries from Falls
• Alternative Approaches to the Use of Restraints
• Delirium, Dementia & Depression in Older
• Adults
• Care Transitions
• Person & Family Centred Care

Accreditation Canada is an independent organization that assesses and recognizes excellence in patient care and services at health services organizations throughout Canada. HGMH undergoes an accreditation review every four years and is assessed on everything from organizational aspects like governance and leadership to hospital protocols related to the services we provide. This includes everything from infection prevention to emergency department operations to ensuring our patients and their families have a say in the hospital’s decisions.
Accreditation ensures that our hospital has the tools and processes in place to encourage collaboration toward common goals, that we have quality and safety standards that help save and improve lives, and that we support an ongoing mindset of continuous quality improvement among our entire team. HGMH completed its latest survey with Accreditation Canada in 2022, and the hospital was awarded Accreditation with Commendation for 2022-2026. This is an outstanding achievement, particularly in the midst of the COVID-19 pandemic and is evidence of the hard work and dedication of the entire hospital team to meet the rigorous standards that Accreditation Canada sets.


The HGMH Foundation works closely with Hospital staff to lead efforts to implement a wide variety of fundraising initiatives to raise critically needed funds for HGMH. Donations to honour the memory of loved ones are also welcomed.

In recognition of your appreciation, the Care Champion will receive a thank you card informing them of your gratitude and a custom-crafted Care Champions lapel pin to wear proudly and celebrate their work.
At HGMH, patient-centered care is our priority. You and your family deserve the best health care services, and we strive to exceed your expectations every day. If you were moved by the care you or your loved one received at HGMH, please consider recognizing the special caregiver through this program. This is a meaningful way to express your appreciation and an action that will have
You may also choose to make a donation to the HGMH Foundation to honour your Care Champion in which you will receive an income tax receipt. Visit our website for more information. https://www.hgmh.on.ca/carechamp/



Hôpital Glengarry Memorial Hospital is committed to protecting the privacy, confidentiality, and security of all personal health information to which we are entrusted.
The HGMH Privacy Officer is available to respond to your questions or concerns about the privacy of your personal health information. Please ask someone from your health care team for assistance in contacting the Privacy Officer.
Since latex balloons can cause allergic reactions in some people, we ask that no latex balloons be brought onto the premises.
HGMH is a designated agency under the French Language Services Act (FLSA). We are dedicated to providing our French-speaking population with access in French to the full range of quality care and services being offered. This includes access to French-speaking health care professionals as well as providing all patient materials in both official languages.
HGMH has established priorities for the identification, removal and prevention of barriers for people with disabilities. Our Accessibility Committee is accountable for ensuring that HGMH
fully complies with the Accessibilities for Ontarians Act, its regulations and related HGMH policies.
The HGMH Accessibility Plan available on the HGMH Internet site under “About Us” “Reports & Publications”
Many elements in the environment can trigger or influence health and disease. In consideration of others who may suffer from chemical sensitivities and/ or allergies, we request that you refrain from wearing scents such as perfumes, colognes, hairspray, or aftershave when at our hospital.
All hospitals in Ontario are smoke-free and vape-free. Smoking cessation therapy is available for inpatients who want to reduce their tobacco use or quit smoking.

HGMH ranks respect as one of its workplace values. Violence in any form, either directed at you or others, physically or verbally does not support the hospital’s values. It is expected that you will respect the rights of others.
If there is an injury to anyone or damage to property, this will be reported to the authorities.
Patients in hospital are at increased risk for developing blood clots related to complications from illness and decreased mobility. When you are admitted to hospital, your doctor will assess you for prevention of blood clots and may order a blood thinner. An easy way to remember the most common symptoms of blood clots are: Chest pain; Light-headedness; Out of Breath; Leg Tenderness; Leg Swelling. For more information, refer to www. thrombosiscanada.ca.
A pressure ulcer or wound is an injury caused by unrelieved pressure that damages the skin and underlying tissue. Pressure ulcers occur more frequently to people who use wheelchairs or who are in bed for long periods of time. Pressure ulcers form where bony parts of the body press against other body parts, a mattress, or a chair. They most often occur on the lower back, below the waist, hips, buttocks, heels and shoulder blades. To help prevent a pressure ulcer, avoid friction. Ask staff to make sure that you are lifted rather than dragged during repositioning. Use moisturizers and stay hydrated—dry skin breaks down more easily. Eat a well-balanced, nutritious diet and drink adequate amounts of liquids (unless your medical condition calls for limited fluid intake).

sudoku

This booklet was made possible thanks to the generous donations of our community supporters.
Disclaimer: We thank all the advertisers whose support has made this publication possible. The appearance of the advertisements in this publication should not be taken as an endorsement by our hospital of any particular goods or services and our hospital cannot be responsible for the goods and services which appear in those advertisements.