THINGS







For centuries, people have suspected a full moon in the sky to cause mysterious changes in people. Now, psychiatrists at Indiana University School of Medicine have found deaths by suicide increase during the full moon.
“We wanted to analyze the hypothesis that suicides are increased during the period around full moons and determine if high-risk patients should be followed more closely
during those times,” said physician Alexander Niculescu, Ph.D.


Niculescu and his team looked at data from the Marion County coroner’s office in Indiana about suicides that took place from 2012-2016. They found deaths by suicide significantly increased during the week of the full moon, with people over age 55 showing an even higher increase. They also looked at the time of day and months that suicides took place,
finding 3 p.m. to 4 p.m. and the month of September to be peak times for suicides.




The team recently published their findings in Discover Mental Health.










“From a clinical perspective and a public health perspective, we found some important take-home messages in this study,” Niculescu said. “Highrisk patients should possibly be followed more closely the week of the full moon, during late afternoons and perhaps the month of September.”


Niculescu and his team previously developed blood biomarker tests for other mental health conditions (anxiety, depression, and post-traumatic stress disorder) and for pain. Using blood samples previously taken by the coroner from some of the people, the team was able to see which biomarkers were present.



“We tested a list of top blood biomarkers for suicidality that we identified in previous studies,” Niculescu said. “The biomarkers for suicidality that are predictive of death by suicide during full moon, peak hour of day and peak month of the year compared to outside of those periods appear to be genes that regulate the body’s own internal clock, so called ‘circadian clock’. Using the biomarkers, we also found people with alcohol-use disorder or depression may be at higher risk during these time periods.”








Niculescu said the increased light from the full moon could be what leads to the increase in suicides during that period. Ambient light plays a major role on the body’s cir-







cadian rhythm, which is the natural 24-hour cycle our bodies follow to regulate when we are asleep and when we are awake. Moonlight could be impacting people at a time when it should be darker.





“The effect of ambient light and body clocks in suicide needs to be studied more closely, along with how people sleep and their exposure to light,” Niculescu said. “Changes in light can affect vulnerable people, in conjunction with other risk factors.”
As for the other two peak periods for suicides, Niculescu said the peak of suicides from 3 p.m. to 4 p.m. could be related to stressors throughout the day as well as a decrease in light beginning to occur that day, causing a lower expression of circadian clock genes and cortisol. And in September, many people are experiencing the end of summer vacations, which could cause stress, as well as seasonal affective disorder effects, as daylight decreases during that time of year.
“Our work shows the full moon, fall season and late afternoon are temporal windows of increased risk for suicide, particularly in individuals who suffer from depression or alcohol use disorders,” Niculescu said.

In the future, Niculescu hopes to study if exposure to screens at night contributes to increased suicidality in people, especially younger people.

“Some people have a full moon in their hand every night,” Niculescu said. “It’s an area we absolutely need to study further.”




At ECMC, each of us—from doctors, nurses, support sta , and specialists—is focused on not just healing the community but supporting each other at every turn. Our commitment to our employees starts with a rewarding work environment and continues through to our professional development programs. Whether you’re just starting out or you’re a seasoned healthcare professional, ECMC is


Have you tried all forms of treatments, injections or even considered surgery?

My name is Dr. Milioto of WNY Pain Relief. My office specializes in treating those who have tried it all and had no relief. We have created a unique treatment THAT ACTUALLY GETS TO THE ROOT OF YOUR PROBLEM WITHOUT DRUGS, INJECTIONS OR SURGERY.



At WNY Pain Relief we help Rehabilitate a variety of chronic symptoms and conditions:









Spinal symptoms:
• Bulging, herniated or degenerative discs






• Stenosis
• Pinched nerves

• Muscle spasms
• Radiating pain from neck or back into hands, legs or feet


Neuropathy Symptoms:



• Numbness
• Tingling
• Burning
• Hot or cold feeling in hands or feet
• Pins/needles feeling in hands and feet

• Restless or tired legs
WNY Pain Relief

offers Specialized treatment protocol unlike any other in Buffalo utilizing and offering:


• Spinal Decompression
• Class IV Therapeutic Laser


• Infrared Light Therapy


• Neuropathy Therapy
• Weight Loss
• Hydromassage
• Balance
•

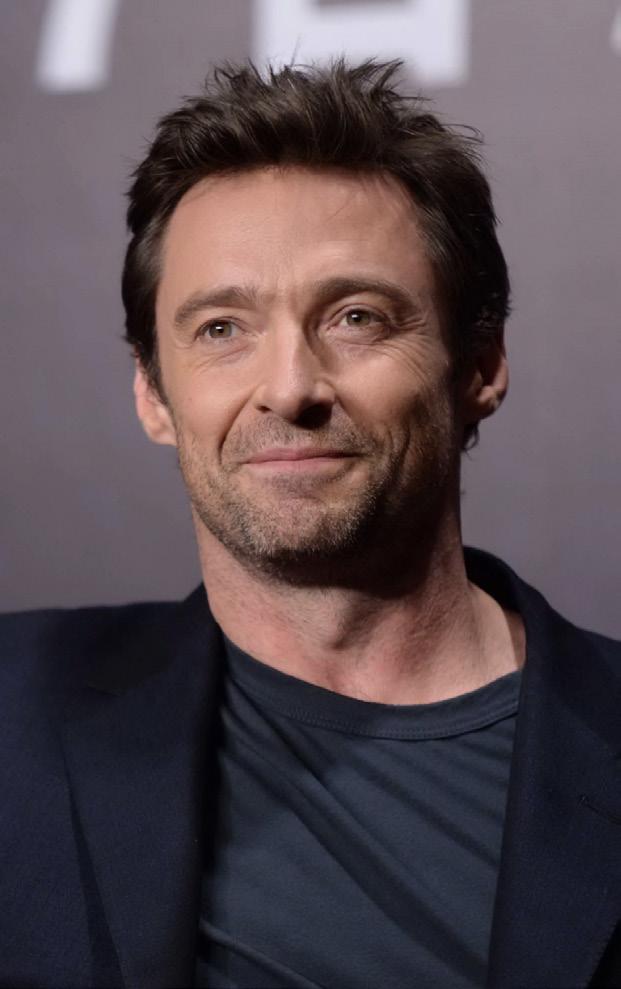
Actor Hugh Jackman is offering a warning about sun damage and skin cancer after having two biopsies.
Jackman was recently wearing a bandage on his nose in a video posted to his Twitter account.
"I just went to my doctor... and she just saw little things — could be or could not be basal cell, in her opinion. She doesn't know," Jackman shared. "Summer is coming for those of us here in the northern hemisphere. Please wear sunscreen. It's just not worth it no matter how much you want to tan. Trust me, trust me, trust me."
Basal cell carcinoma is common and not as potentially harmful as some other types of skin tumors, such as melanomas. It's the type of skin cancer that President Joe Biden had removed after a recent physical.
Jackman, 54, urged people to wear sunscreen. He previously was treated for basal cell carcinoma in 2013, 2014 and 2016.
Jackman reminded viewers that UV exposure in youth can leave a legacy of skin cancer decades later.
"This is all stuff that happened 25 years ago and it is coming out now," he said, pointing to the bandage on his nose. "Put some sunscreen on — you'll still have an incredible time out there."
About eight of every 10 skin cancers are basal cell carcinoma, according to the American Cancer Society.
According to the American Academy of Dermatology (AAD), people can protect themselves by wearing a broad-spectrum sunscreen that protects against UVA and UVB rays, preferably with an SPF of 30 or higher every day. Wear it even on cloudy days, the AAD says.
Avoid tanning beds and sun lamps. If possible, stay out of the sun between 10 a.m. and 2 p.m., when the sun's rays are strongest. Seek shade.
Q: As an anesthesiologist, what kind of interactions do you have with patients?
A: Our interventional pain management practice actually utilizes minimally invasive pain-blocking techniques to help disrupt the pain cycle, which helps make day-to-day activities less difficult for patients and effectively restores quality of life. We evaluate each patient to help understand the underlying problem and to create an individualized treatment plan. That may involve surgery, nerve-blockers or an implantable drug delivery system as a last resort. These are all part of the treatment processes. We offer a variety of interventional procedures and injections to help reduce or eliminate pain symptoms and reduce reliance on opioids. We also offer on-site imaging.
Q: What kinds of conditions do you treat?
A: I implement a comprehensive approach in order to diagnose and treat acute chronic pain generated from the spine, peripheral joints, as well as the head and face. Some of these conditions include arthritis, chronic pain, coccydynia, complex regional pain syndrome, degenerative disc disease, myofascial pain, occipital neuralgia, radiculopathies, sacroiliac joint disease, scoliosis, spinal stenosis, spondylosis, as well as trigeminal neuralgia.
A: When a patient comes to us we really want them to already be on a multi-modal pain management regimen that is not opioid. We work on the WHO pain scale ladder and use non-opioid medications for control of neuropathic and nociceptive pain. Nociceptive pain is pain due to inflammation, and neuropathic pain is pain related to nerve conditions. So we use medication that works on different receptors. So for nociceptive pain, for example, we prescribe Tylenol and NSAIDs [i.e. aspirin, ibuprofen], which help reduce inflammation. For neuropathic pain, we control pain using duloxetine, which is actually a psych med that’s also used for pain control, and a number of other medications for pain control. If the patient does not feel optimal pain control using non-opioid, multi-modal pain regimens, then we go to injections. Injections aren’t optimal right off the bat, so they’re a secondary approach. If that doesn’t work, then we do imaging and see what interventional procedures might work.
Q: Generally speaking, are these temporary interventions or ongoing?
A: It depends on the patient. For example, there could be patients with really severe stenosis that would definitely require surgical intervention to relieve pain. For example, for central stenosis we do epidurals to help them with pain control. If they still aren’t achieving the pain control results they want, then at that point we refer them to a surgeon for evaluation. So we essentially are here so that not every patient who needs pain control is going for surgery.
Q: Are there any risks that come with suppressing pain?
A: When a patient comes to our practice, we do all of the imaging because, prior to inserting a needle into the spinal cord, I always take MRIs of the spine as needed and analyze it before inserting the needle, so we know everything that’s going on with the body. So the chances of missing anything are very rare.
Q: What got you interested in anesthesiology and pain management?
A: In anesthesiology we do take care of pain, but the patient is sleeping and we don’t get to have a follow-up and really get to know the patient. With pain management, we get to follow up, see how they’re
doing in their day-to-day, how they function in society. That gives me a lot of contentment in my practice.
Q: What kinds of new pain management techniques are emerging?
A: I am highly trained in cutting edge technologies such as doing spinal cord stimulator trials, dorsal root ganglion trials and peripheral nerve root stimulator placement.
Q: What is a spinal cord stimulator?
A: A spinal cord stimulator works for masking pain signals before they reach the brain. A stimulator device delivers electric pulses to electrodes placed over the spinal cord. I do spinal cord stimulator trials that involve placing temporary leads into the back and connecting them to an external battery. No incisions were made during the trial. This is not a surgery. The leads are placed using a small needle. The indications for spinal cord stimulator trial include failed back surgery syndrome, chronic painful peripheral neuropathy, complex regional pain syndrome and diabetic neuropathy. It only takes a half an hour to an hour to put in.
Q: How diverse are your patients age-wise?
A: I’m actually the only person in my practice who sees young kids. For me, age is no barrier. My youngest patient is 16. Usually with young kids, they’ll come in with an injury related to contact sports. And I’ll usually help them with injections that will help them be more active in the sport. My oldest patient is 94. With older patients is often cervical stenosis or lumbar stenosis, joint pain, arthritis.
Q: For patients who are on or are trying to get off opioids, is there a particular protocol for helping them?
A: We don’t actually prescribe any medication; we’re interventional. But when a patient comes to me, I always evaluate their pain regimen and try to make recommendations to primary care about how we can tweak it and target different receptors without opioids. Once all these things are covered, then we can consider opioids. Opioids are always as-needed, they can never be a scheduled medication. They’re the last resort, not the first. With a multi-modal approach I think we’re moving in the right direction to save our society from the opioid crisis.
Name: Harpreet Dhiman, D.O.
Position: Anesthesiologist and clinical assistant professor at the University at Buffalo. Affiliated with UBNS (Neurosurgery — University at Buffalo)
Hometown: Delhi, India
Education: Received her Bachelor of Science degree from the University of Pittsburgh, her medical degree from Touro College of Osteopathic Medicine (New York City). Did her residency training in anesthesiology at Albany Medical Center, and pain fellowship with SUNY Upstate Medical Center

Affiliations: Catholic Health System; Kaleida Health System

Organizations: American Board of Anesthesiology
Family: Married
Hobbies: Painting
Pregnancy rates in the United States suffered a steep decline during the last decade, new government data shows.
The overall U.S. pregnancy rate fell by 12% between 2010 and 2019, according to figures released in April by the U.S. National Center for Health Statistics (NCHS).

The pregnancy rate among women aged 15 to 44 was 85.6 per 1,000 in 2019, down from 97.3 per 1,000 in 2010, the report found.
A drop in unintended pregnancies and teen pregnancies contributed to the overall decline in pregnancy
rates.
Pregnancies among teens declined by more than half (52%) during the 2010s, added the researchers, who were led by Lauren Rossen.
Likewise, unintended pregnancies experienced a 15% decline, falling from 42.1 per 1,000 in 2010 to 35.7 per 1,000 in 2019.
The drop in pregnancy rates is reflective of the overall decline in U.S. birth rates that has been going on since the mid-2000s, said Phillip Levine, a professor of economics at Wellesley College in Massachusetts.
“The report is not terribly
surprising,” said Levine, who was not involved with the study. “We know that birth rates have been falling pretty dramatically, beginning around 2007.”
The pregnancy rate is calculated from three components: live births, lost pregnancies and abortions, the NCHS said. These are compared to the total female population.
Abortions experienced a heavy decline of 17% during the 2010s, while lost pregnancies and live births increased by just about 3%, the NCHS report noted.
An increasingly larger proportion of women in their childbearing years simply aren't getting pregnant at all, Levine said.
Many potential explanations have been suggested as reasons why young adults aren't having kids, Levine said — financial pressures like rising housing costs and student debt, a decline in religiosity, greater access to contraception, the decision to delay childbearing.
Levine argues that none of those explanations really seem to work, and that the falling pregnancy rate appears to be due to a larger societal shift regarding family priorities.
“If it's the case that people decide they're going to have their first baby at 30 instead of 25 or something like that, that would reduce the birth rate in the short term but eventually it would catch up, right? That doesn't seem to be happening. There's a reduction in childbearing over women's entire childbearing years. By the end of their reproductive period, they're having fewer children than they used to,” Levine said.
Texting and driving can be
deadly. Holding your phone in your hand to talk and surfing the internet while behind the wheel is dangerous, too.
This is widely known, but a new survey finds that about half of all respondents still use an electronic device most or every time they drive.
“I'd say it's not as much surprising as it is frustrating,” said Adam Snider, a spokesman for the non-
profit Governors Highway Safety Association (GHSA), which wasn't involved in the study but issued a news release after it was released.
“Distracted driving is something that is incredibly pervasive.”
In the survey, conducted by the Insurance Institute for Highway Safety (IIHS), more than 2,000 licensed drivers were asked how much they agreed with dozens of statements designed with the Health Belief Model
in mind.
That model is described as a behavioral change theory developed to understand why some people don't adopt a certain health behavior. It's usually applied to illness or disease prevention, according to the study.
“I think the results from this study really help shed some light on the reasons why” people are still using their phones in their cars, said lead author Aimee Cox, a research associate with the IIHS.

Cox said that appears to include “the need or the perceived need to respond to family or friends, the need for information, all these things that modern cellphones have really allowed us to do without thinking about it.”
While distracted drivers are using their phones while driving because they don't want to miss a call from their kids, for example, it's also their family members who they say could motivate them to put the phones down.
“I think that provides a really unique opportunity to where if we can encourage that open and safe communication and dialogue, we can have teen drivers and kids encouraging their parents to practice safe driving behaviors and vice versa. I think it needs to go both ways,” Cox said.
Distracted drivers killed at least 3,000 people in 2020, according to a statement issued by GHSA CEO Jonathan Adkins. That was 8% of all traffic deaths.
Another 400,000 people are injured each year, Snider said, but it may very well be higher, because it can be hard to prove that distracted driving caused a crash.
Cats constantly licking and chewing because of a skin condition called feline allergic dermatitis may benefit from a new generic treatment approved by the U.S. Food and Drug Administration.
The FDA approved Modulis for Cats on March 29, making it the first generic cyclosporine oral solution for cats with skin conditions resulting from this allergic dermatitis.

The immunosuppressant drug tamps down the allergic process that causes cats with this condition to be itchy.
The medication contains the same concentration and dosage of cyclosporine as an approved brand-name drug, Atopica for Cats. That medication was approved in August 2011.
Cats with this condition can be intensely itchy. They may lick, chew and scratch at their skin and hair.
This can cause them to develop other skin issues, including miliary dermatitis, lesions known as eosinophilic plaques and hair loss.
Cats need to be at least 6 months old and weigh 3 pounds to use the medication, which is only available from a veterinarian.
People who administer this to their cat should avoid accidentally ingesting the drug. Don’t eat, drink, smoke or use smokeless tobacco while handling it, the FDA advised.
Wash your hands after giving Modulis for Cats to your pet. People with known hypersensitivity to cyclosporine should avoid contact with the product, the FDA warned.
The medication is sponsored by Provetica, LLC, based in Lenexa, Kan. It comes in three sizes.
The trustees of the Medicare hospital trust fund have projected the fund will be depleted by 2031. Incoming Medicare taxes after that will be insufficient to rebuild a reserve. Thanks to the InflationReduction Act, which fixes monthly insulin costs at $35 and authorizes Medicare to negotiate a few drug prices effective 2026, the fund would have been depleted three years sooner in 2028. So that begs the obvious question: if the projected savings in insulin costs and a dozen or other drugs can push the depletion date out three years, why not let Medicare negotiate all drug prices? Answer: the drug lobby.
COVID19 and newer strains. Most commercial insurance premiums increased for the very same reasons.
Artificial intelligence, like ChatGPT (Generative Pretrained Transformer), is being met by providers with the same guarded optimism and trepidation as the now firmly entrenched electronic medical record.
But unlike the electronic medical record, which was slowly and painfully incorporated into healthcare over several years, chatbots will become an integral part of healthcare seemingly overnight.
Google’s chatbot scored 85% on a practice medical licensing exam. Another chatbot scored 90% on a law bar exam.
As with the electronic medical record, if AI is not used properly, there are concerns over privacy, equity, safety and quality. Proponents of chatbots in healthcare see win-win scenarios for providers and
patients.
Chatbots will relieve providers and their support staff of several menial administrative tasks, thereby freeing them to spend more time with their patients and critical clinical issues.
Industry experts believe AI will increase access, improve the patient experience, lower costs and prevent many heretofore frustrated physicians and nurses from leaving healthcare altogether.
Basically, chatbots can: automatically refill prescriptions; provide basic, necessary medical information; check symptoms; assist with coverage and claims; instantly respond to queries; recommend wellness programs; provide medical assistance; and schedule appointments. And all this 24/7.

According to a survey of 31,000 full time physicians by Doximity, the average physician compensation declined 2.4% last year. (It went up 3.8% in 2021.) The decline occurred despite a predicted MD shortage, a significant rise in operating costs, and MD burnout. According to the AMA, when adjusted for inflation, Medicare reimbursement declined 22% between 2001 to 2012. (Commercial carriers tend to follow suit.)
According to Doximity, the highest paid specialties are:
• Neurosurgery, $746,000
• Thoracic surgery, $668,000
• Orthopedic surgery, $605,000
• Plastic surgery, $539,000
• Oral and maxillofacial surgery, $538,000
• Vascular surgery, $534,000
• Cardiology, $527,000
• Radiation oncology, $516,000
• Gastroenterology, $486,000
• Radiology $485,000.
Even though 90% of us have health insurance, many are saddled with increasingly higher deductibles and co-pays as employers continue to shift more of the costs to employees. Not surprisingly, most consumers are clueless about their benefits and out-of-pocket costs until they are confronted with a health crisis. Healthcare in our country is confusing, frustrating and terribly expensive. Healthcare debt is still the No. 1 reason for bankruptcy. A recent survey of over 1,000 consumers by a national consulting firm revealed:
• Over 50% of respondents are concerned about their ability to pay for a major healthcare event;
• 65% said they are not able to afford a new $250 a month expense to manage a chronic condition and related medications;
• 64% said they would delay or skip necessary care if they were unsure of their ultimate out of pocket responsibility.
Ironically, putting off care to save money can result in even higher costs to patients as symptoms not treated early worsen over time until there is an acute medical crisis. This non adherence eventually impacts quality, outcomes, productivity and even provider burnout. Hospitals have been slow to display mandatory pricing information on their websites. Once in compliance, this should help consumers calculate what their insurance will pay and then what they will owe out of pocket for selected procedures.
According to an analysis by the Robert Wood Johnson Foundation, health insurance premiums on the federal exchange increased about 3.4% this year. The enhanced subsidies provided by the federal government resulted in record breaking enrollment. The number of insurance companies on the exchange increased to 232. Premiums on the exchange actually dropped 2.2% from 2019 through 2022. The reasons for the 3.4% increase this year are: high inflation beginning last year; uncertainly over enhanced income-based subsidies (the Inflation Reduction Act eventually continued the enhancement through 2025); the end of continuous coverage requirements through the pandemic; uncertainty over the lingering impact of
Uber has been providing non-emergent medical transport (NEMT) since 2018. Uber’s newest venture is delivering prescriptions, over-the-counter drugs and healthy foods. Providers will use the same Uber platform they already use to arrange rides for their patients. Patients who lack their own transportation are more likely to be non compliant by missing medical appointments or by not taking their meds. Uber ride and prescription delivery services are becoming more popular with providers under value-base, contracts which reward providers for positive patient outcomes.

Health Affairs analyzed over 3,700 hospital webpages and found just about all of them incurred at least one third-party data transfer. Specifically, 98.6% had at least one third-party data transfer and 94.3% had at least one third-party cookie. The median number of third-party transfers was a whopping 16. The leading culprits were Alphabet 98.5%; META 55.6%; Adobe 31.4%; and ATT 24.6%. Angry consumers, feeling their privacy has been violated, have filed individual and class action lawsuits against hospitals for sharing their personal information with these website trackers.

The Affordable Care Act mandates that insurers offer free preventive services including screening for breast cancer, cervical cancer, diabetes and vision testing for preschoolers. Inexplicably, judge Reed O’Connor, the same judge who tried to kill the entire hugely popular act in 2018, has ruled that some of the mandated free preventive services are illegal. Really? Who brought this suit? Just about every commercial carrier has vowed to continue with free preventive services because it saves lives and money in the long run.
George W. Chapman is a healthcare business consultant who works exclusively with physicians, hospitals and healthcare organizations. He operates GW Chapman Consulting based in Syracuse. Email him at gwc@gwchapmanconsulting.com.

U.S. Pain Foundation: 50 million Americans live with long-term pain that ranges from distracting to disabling
 By Jane Schmitt
By Jane Schmitt
Pain management is a critical part of the local healthcare scene and that’s welcome news to people with chronic conditions affecting them not only physically but psychologically, too.
It’s time to get your life back, said chiropractor Christian Milioto of the Western New York Pain Relief & Integrative Wellness Center.
“People are looking for hope,” he said. “They’re looking for help.”
Milioto and other practitioners seek to provide some relief for pain-weary individuals who want to feel better and improve their quality of life. That’s no easy task, but this region offers lots of resources in the form of freestanding wellness clinics, rehabilitation facilities, therapy practices and specialty divisions of hospitals and health systems.
Pain is your body’s way of telling you that something is wrong, most likely due to injury, illness or disease. Pain that doesn’t go away over time or with treatment is classified as chronic and can lead to fear, anxiety, depression, limited mobility, lost independence, reduced productivity
and feelings of isolation.
An estimated 50 million Americans live with long-term pain that ranges from distracting to disabling, according to the nonprofit U.S. Pain Foundation.
“When painful symptoms first arise, patients and their healthcare providers work together to see if they can identify and address the underlying cause,” the foundation says on its website. “For many conditions and injuries, however, there is no precise medical or surgical cure. As time passes, in addition to other diagnoses or even without an identifiable cause, patients may be diagnosed with chronic pain. Treatment goals will then shift from resolving the pain to reducing and managing it.”
One size doesn’t fit all Americans spend billions of dollars a year on pain-relief treatments and care including medication, injections, therapy and exercise. The treatment approach is never one-sizefits-all and often is multidisciplinary, according to Cathy Hoy-Patterson,
A monthly newspaper published by Local News, Inc. Distribution: 25,500 copies throughout more than 1,500 high-traffic locations.
public health educator for the Niagara County Department of Health.
“You have to find what works best for you,” she said.
This spring, the department’s nursing division and the county Office for the Aging offered a free chronic pain self-management workshop at the North Tonawanda Public Library. The six-week program outlined a so-called toolbox, including cognitive behavioral therapy, to boost self-efficacy for people struggling with the physical and emotional impact of pain.
“We explain to people that they go to their doctor and (generally) spend 15 minutes with that doctor every couple of weeks. But they have 24/7, the rest of their lives, to manage their condition,” Hoy-Patterson said. “So let’s find some tools that work best for them.”
She added: “This workshop is not focused on medication; we do not prescribe anything. The philosophy is to increase self-efficacy.”

Developing communication skills is an important component.
“Often people are frustrated and they’re in pain and don’t how to communicate with their doctor and family members,” she said. “We can help them with that.”
Experts note that effective pain management doesn’t necessarily mean eliminating all the aches and hurts. Oftentimes it’s about gaining an increased understanding of what’s going on in the body and achieving quality of life despite the pain.

At the Western New York Pain Relief & Integrative Wellness Center, Milioto focuses on treating senior citizens whose struggles include neuropathy, herniated discs, spinal stenosis and pinched nerves. His work is inspired by his grandmother, who has dealt with rheumatoid arthritis, stenosis and osteoporosis.
Treatments offered at the center in Cheektowaga include spinal decompression, therapeutic laser, infrared light therapy, electroanalgesia therapy, chiropractic, hydromassage


Christian Milioto holds a doctor of chiropractic degree (DC) and practices at Western New York Pain Relief & Integrative Wellness Center. “There’s never been a day where I walked into my clinic and wasn’t excited. It’s helping people to get their lives back, but doing it safely, naturally and effectively,” he says.

and whole-body vibration.
“I love what I do. There’s never been a day where I walked into my clinic and wasn’t excited,” Milioto said. “It’s helping people to get their lives back, but doing it safely, naturally and effectively.”
Common culprits include:
•Autoimmune disorders (i.e., arthritis, fibromyalgia)
• Traumatic injury
• Lasting pain from surgical procedures
• Cancer
• Neuropathy
Good
Editor & Publisher: Wagner Dotto
Writers: Deborah J. Sergeant, Jim Miller, Gwenn Voelckers, Anne Palumbo, Brenda Alesii, Ernst Lamothe Jr., George Chapman, Christ Motola, Jane Schmitt, Mike Costanza
in
or in

The Oxford English Dictionary defines contentment as "the state of being happy and satisfied."
This dictionary definition sounds like a nice way to feel, doesn’t it? Oh, if we could just snap our fingers and be content with who we are and what we have.
Wouldn’t life be grand?
I’ve had the privilege of meeting and talking with a lot of women and men who live alone, and our conversations often turn to the subject of contentment: how to find it, how to keep it, and how to find it again once it has been lost.
Those on their own often feel a lack of something in their lives, and many have trouble letting go of a craving for things to be different.
I know. I’ve been there.
For years after my divorce, I had trouble seeing the good in myself and in my life. But with time, intention and practice, I was able to stop yearning for what I didn’t have and start appreciating what existed right in front of me.
It all began with an important first step — taking a hard look at myself.
While I’m no expert in survey design, I created the simple non scientific quiz below to help you assess where you are on the road to contentment.
Your results may light a new and
hopeful way forward.
Circle the choice that best answers the questions below:
1. If asked, can you readily name your own positive personal qualities? How many come to mind?
A. 5 or more.
B. 1 to 4.
C. Nothing really comes to mind.
2. How would you describe your home?
A. Very “me” — I’ve made it my own.
B. It’s fine. I keep meaning to redecorate, but I never get around to it.
C. My home looks as tired as I feel.
3. How would you describe your success in letting go of old ways of thinking and of negative thoughts or behaviors that keep you anchored in the past?
A. I live in the present; it’s full steam ahead!
B. I still wallow in self-pity from time to time.
C. I can’t let go of regrets and obsess about the past.
4. Could you imagine planning a trip by yourself and traveling alone to a new or familiar destination?
A. In a heartbeat.
B. Maybe someday.
C. I can’t imagine traveling solo.
Gary Mervis has a philosophy that life’s most important dates: are the day one is born and the day one finds life’s purpose.
For Mervis, a Pittsford resident, his purpose crystallized when his youngest daughter, Elizabeth, called “Teddi,” was diagnosed at age 9 with a malignant brain tumor. Three years and many surgeries and treatments later, Teddi lost her battle to the disease.

Mervis cited loneliness as his daughter’s biggest challenge, realizing she was the only child in her elementary school dealing with a deadly disease. That sad chapter in his family’s life motivated Mervis to create a safe haven for kids and in 1982 Camp Good Days was born. The purpose? To provide kids with cancer and other life challenges the opportunity to come together in a
residential camping experience to be with the only ones who could truly understand what they were going through: other ill children. Currently, campers range from children to even adults battling diseases.
In Good Health spoke with Mervis about his enduring legacy and how his daughter continues to influence his life to this day.
Q. At the time of Teddi’s diagnosis, you were working for the New York State Assembly and coaching football at St. John Fisher University. How did your life change during that terrible time?
A. My daughter’s illness and death put me on a new path. I had spent 23 years as a staff member in the State Assembly, but even though it’s usually the mom who becomes the primary caregiver in situations like this, I decided to take a leave of
5. Does going alone to a café for a cup of coffee or grabbing a bite to eat at a local restaurant feel comfortable — even enjoyable?
A. I do it all the time.
B. Occasionally, but I feel self-conscious.
C. I’m just not ready.
6. Do you exercise, get enough sleep, and stay on top of health screenings?
A. Of course!
B. A little, but I could do more for myself.
C. Sadly, I’ve neglected my health and fitness.
7. How often do you pamper or reward yourself by taking some time just for you or by purchasing that little something special you’ve had your eye on?
A. As often as I can.
B. I tend to put others’ needs before my own.
C. I can’t remember the last time I pampered myself.
8. Can you imagine your life without a special someone on your arm?
A. I would enjoy sharing my life with someone special, but I could also be perfectly content with my "family of friends."
B. Maybe, but not for long; I feel incomplete without a "one and only."
C. Life doesn't feel worth living when I'm not in love.
Calculate your total points using this scale:
3 points for each A answer
2 points for each B answer
1 point for each C answer
8 points: Contentment may feel elusive at the moment-beyond your
absence. Never in my wildest imagination did I think I’d find myself waiting for my daughter to come out of surgery, a seven-and-a half craniotomy followed by weeks of radiation and chemo. It gave me a reason to find a vehicle to help others.
Q. How did you take that first step for such a massive undertaking?
A. At the time, there were no computers, cell phones, none of the technology we have today. One morning, we were watching the “Today“ Show and they had a story about ill children going on nature hikes and enjoying time swimming and having fun. I wanted Teddi to have that opportunity, so I called the “Today” show, talked to a reporter, who referred me to a pediatric oncologist in Michigan. I was able to track him down and he explained that this camp activity was rare and a new concept. There was nothing like this in Western New York. I was able to contact people I knew from my job in state government along with two hospital administrators, who learned of hundreds of children with cancer. Camp Good Days opened in 1979 and Teddi passed away in 1982. She went to two camps. She was my inspiration and the camp is my memorial to her.
Q. Who does Camp Good Days help and what is your primary area of service?
A. We are located in Branchport, on the shores of Keuka Lake and across from the state park. Most of our campers come from Buffalo,
grasp. But it can be found. You may benefit from talking with a professional counselor or spiritual adviser. Help and encouragement might also be found in grief support groups and other gatherings — in person or online — that offer emotional support and practical advice.
9-15 points: You experience feelings of contentment, but you know there’s more to be found. Continue to stretch yourself. Reach out to others. And “try on” healthy pursuits outside your comfort zone. Success and achievement breed contentment. You might also find inspiration and a needed jump-start in workshops, lectures, and retreats devoted to personal growth and development.
16 points: Good for you — what you have is precious. Being content with yourself opens up all kinds of possibilities. It enables you to feel peace and joy, whether you are alone or in a committed relationship. It is an invaluable inner springboard on which you can launch all things imaginable!
Gwenn Voelckers is the founder and facilitator of Alone and Content, empowerment workshops for women and author of “Alone and Content,” a collection of inspiring essays for those who live alone. For information about her workshops, to purchase her book, or invite her to speak, visit www. aloneandcontent.com
Rochester, Syracuse and Utica, but we’ve had children attend from 36 different countries experience the magic of Camp Good Days.
Q. What is the cost to attend?
A. It is free! Despite a lot of ups and downs over the years, we’ve been able to keep our heads above water financially. These kids and parents spend a lot of time in hospitals. I never want a family already struggling with a cancer stricken child to worry about money or worry about choosing between paying their mortgage versus sending their kid to camp. All programs have been free of charge since 1979.
Q. Can you use more volunteer help?
A. Yes, volunteers are our biggest need right now. Please call for information on volunteering at 1-800785-2135 or at our website: www. campgooddays.org.
Does it sometimes feel like your young picky eater is turning every meal and snack into an epic power battle — and you're just not sure how to get them the nutrition they need?
If so, you're not alone.
According to an article published recently in the journal Pediatrics, up to 50% of kids may be described as "picky eaters." And while there's no one agreed-upon definition of picky eating, in general, if your child or adolescent is particular about the food they eat at least some of the time, you may have a picky eater on your hands.
“I think all parents have said at one time, 'My kid is such a picky eater!'” clinical psychologist Rachel Busman said in a recent Child Mind Institute article. “It's very normal for kids to go through stages where they're a little more picky, especially when they are trying to assert their autonomy.”
Experts at the institute note that picky eating is one of the most “common complaints” of parents. Here, they and other child experts weigh in on the topic with five top tips for parents of picky eaters:
1.Grocery shop and cook together
Involving your child in grocery
shopping can help extend their picky eater food list to include novel items, Busman explained. When they are shown a wide variety of food flavors and options, it can open their eyes to new tastes and textures they might enjoy.
Similarly, if you scroll through recipe books or websites together and pick a new dish or dessert to create, it helps make eating different foods a fun adventure instead of a battle.
Cleveland Clinic registered dietician Jennifer Hyland notes that forcing kids to eat food they don't like can make them doubt their own body signals surrounding hunger, especially when they're toddlers.
“Forcing food can cause your child to distrust their own appetite and lead them to believe that they can't regulate their own hunger cues,” she explained in an article. Instead, allow them to eat until they're full — even if that means some vegetables are left on the plate. This also helps ensure that eating food doesn't become associated with stress and anxiety.

3.Have meals as a family
Both Hyland and the pediatricians at Healthychildren. org recommend eating together as a family, to help create a positive vibe
ore American children have autism than previously thought, the U.S. Centers for Disease Control and Prevention reports.
It also finds that the COVID-19 pandemic delayed diagnosis for many, which could have lasting impact.
Data from 11 communities in the Autism and Developmental Disabilities Monitoring Network, which tracks the number and characteristics of children with autism and other developmental disabilities, revealed that at age 8, about one in 36 children has been identified with autism spectrum disorder (ASD).

That's 2.8% of 8-year-olds, according to an analysis published in March in the CDC's Morbidity and Mortality Weekly Report.
A previous estimate, done in 2018, pegged prevalence at one in 44 children, or 2.3%.
A second report found that
progress in early detection of autism among 4-year-olds in the same 11 communities slowed during the early months of the COVID-19 pandemic.
They were less likely to be screened or identified with ASD than current 8-year-olds were at the same age.
“Disruptions due to the pandemic in the timely evaluation of children and delays in connecting children to the services and support they need could have long-lasting effects,” said physician Karen Remley, director of CDC's National Center on Birth Defects and Developmental Disabilities.
“The data in this report can help communities better understand how the pandemic impacted early identification of autism in young children and anticipate future needs as these children get older," Remley said in an agency news release.
Who was diagnosed with ASD also changed, the report revealed.
Prevalence of autism in Asian,
around food. They also suggest cooking the same meal for everyone at the table and including at least one food in each meal that your picky eater enjoys, if possible.
“Try your best to cook the same meal for the whole family. The child may not eat all of it, but it's important that you present it, and that you set an example of trying these foods yourself,” Hyland explained.
Teaching your child that unwanted food is still safe food is important, according to the Child Mind Institute. For instance, they may need to be shown that the tomato they are repulsed by isn't actually full of bad germs just because they don't like it.
One way to demonstrate this is to teach your child to offer unwanted food to others at the table. When your picky eater sees other family members enjoying it, they're more likely to understand that it's safe to eat.
You may have thought that a
good meal presentation was only for formal restaurants, but as it turns out making foods into fun shapes and including a variety of colors in your meals can help make them appealing to kids.
Hyland recommends offering your picky eater something they can shake onto their food if they don't want it, to make it “more exciting.” Additions like herbs, seasonings or seeds can help turn an unwanted item into a winner.
“Sprinkles also go a long way,” said Hyland. “Sometimes it really is as simple as that.”
The Cleveland Clinic also notes that a child may try a food between 10 to 20 times, on average, before they like it. This means that your patience and persistence in re-offering previously rejected foods to your picky eater can really pay off.
Hyland explained that, “The most important thing a parent can do with a choosy eater is to be consistent and not give up.”
Black and Hispanic children was at least 30% higher in 2020 than 2018. Among white children, ASD prevalence rose 14.6% over the period.
This was the first time that the percentage of 8-year-old Asian or Pacific Islander, Hispanic or Black children identified with autism was higher than in white children. For
white children it was 2.4%, compared to 3.3% for Asian and Pacific Islander children; 3.2% for Hispanic children, and 2.9% for Black children.
Public health experts noted that the shifts may reflect improved screening, awareness and access to services among historically underserved groups.




New study shows instant noodles may be harmful to reproductive and cardiovascular health
By Amanda Jowsey


Quick, cheap and filling food is oftentimes our go-to as Americans. Life demands our constant effort and attention, so we often let the nutritional choices we make fall by the wayside.
Instant noodles, notoriously



eaten in excess by financially starved young adults, can be found in almost every pantry.
New research published in the “Journal of Nutrition” shows that this beloved meal-like snack can have some alarming adverse health effects.
The study, done by the Baylor College of Medicine, shows that eating instant noodles, like Ramen, two or more times a week, is linked to an increased risk for cardiometabolic syndrome, which raises the risk of heart disease, diabetes and stroke.
These results were more prevalent among women, most likely due to biological differences in sex hormones and metabolism.






More alarmingly, it shows that the bisphenol A (BPA) present in the polystyrene foam packaging of some brands of these products may be causing hormonal imbalances in women.



BPA interferes with the way hormones, specifically the sex hormone estrogen, sends messages throughout the body. BPA can essentially mimic estrogen and interact with estrogen receptors, leading to changes that can contribute to cancer development and progression.











BPA is shown to interfere with enzymes essential to produce estradiol, the primary form of estrogen in the body during reproductive years. One recent Harvard study found a connection between fewer fertile eggs in women who had higher levels of BPA in their urine.


Thinking about all the young female college students eating packs and packs of these on a budget has frightening implications. Are we all just destined for reproductive harm or cancer?
Baylor’s primary investigator on the study, physician Hyun Joon Shin, said that the study indicates how important it is for us to make conscious and informed choices about the food we put into our bodies.




“This research is significant since many people are consuming instant noodles without knowing possible health risks,” Shin said. “My hope is that this study can lay a foundation for future research about the health effects of instant noodle consump-


tion.”






Emily Wood, dietitian and plantbased nutrition coordinator from Niagara Falls, has more than 14 years’ experience with a specialty in plantbased nutrition. She works for the T.
Colin Campbell Center for Nutrition Studies, part of Cornell University in Ithaca and has a passion for helping others deepen their knowledge of plant-based nutrition and offering support for those focused on this area of their health-related practices.


She’s also a mom of three and shared her best tips for avoiding the health risks associated with overly processed and packaged foods like instant noodles.
“Plan ahead. Planning decreases your chance of eating something out of convenience that is unhealthy and reduces food waste. I always have a grocery list on the counter, so as I think of dinner ideas or run out of staple foods, I put it right on the list,” she said. “Also, the biggie and probably most obvious, minimize eating out as much as possible. Eating out is not only more expensive than ever, but [according to an article in Nutrients Magazine,] a higher rate of eating out of the home is linked to poorer diet quality, higher intakes of fat, sugar, and sodium, and lower intakes of fiber and micronutrients.”
The CDC recently released some helpful tips for eating healthy on a budget. The top two suggestions: Meal planning and sticking to fresh, frozen, or canned goods instead of prepackaged instant-ready food which is more expensive and provides less nutritional value.
Using meal planning apps and shopping apps like Instacart can also be helpful. Even if you don’t purchase through the app, it’s still helpful to have a visual reminder of options while you’re prepping for the week.
My cheese-loving friend has sworn off cheese for a while, saying it’s “too caloric, too fatty, too tempting.”
She’s not the first to go on a cheese moratorium, and I get it: cheese can be all those things. But not always. There are healthy cheeses to be had and recommended ways to eat them.
Swiss cheese, in fact, is one of the healthier cheeses, a designation bolstered by its appearance on nearly every healthiest-cheese list out there.
Why does Swiss cheese make the coveted cut?

Let’s begin with why Swiss cheese is the cheese for you if you’re watching your salt intake. With only 52 mg of sodium per slice, Swiss cheese has significantly less sodium than most other types of cheese. Considering that the American Heart Association recommends no more than 2,300 mg of sodium a day, you’ll barely make a dent with a few slices of Swiss. Make the same sandwich with American cheese, however, and you’re looking at 900 mg.
Swiss cheese also has more vitamin B12 than any of its peers—a whopping 36% of your daily requirement. An essential vitamin, B12 helps the body produce energy, maintain nerve health and lower blood pressure. Unfortunately, many people— from older adults to vegetarians—are deficient in this important vitamin.
Incorporating a slice or two of Swiss cheese into your weekly diet can help keep your B12 levels up.
Much like milk, Swiss cheese serves up healthy doses of protein, calcium and phosphorous, three nutrients that contribute to the development and maintenance of strong bones. But unlike many milk products, Swiss cheese is super low in lactose, making it a great cheese option for people with lactose intolerance.
On the downside, Swiss cheese has 5 grams of saturated fat per slice, which is about a quarter of the recommended daily amount. Although some research indicates there may be no link between saturated fat and heart disease, experts still advise limiting your intake.
On the plus side, Swiss cheese’s full flavor, along with its slow-to-digest proteins and fats, may help thwart the urge to overindulge.
Anne Palumbo is a lifestyle columnist, food guru, and seasoned cook, who has perfected the art of preparing nutritious, calorie-conscious dishes. She is hungry for your questions and comments about SmartBites, so be in touch with Anne at avpalumbo@aol.com.


Serves 6-8
1½ tablespoons olive oil
3 cups sliced mushrooms
10-oz box frozen chopped spin-

ach
½ cup chopped onion
1 clove garlic, minced
5 large eggs
½ cup milk
1-2 teaspoons Dijon mustard
1 teaspoon thyme
½ teaspoon salt
¼ teaspoon coarse black pepper
1½ cups shredded Swiss cheese
The majority of Swiss cheese made in America, often called baby Swiss, is only aged for about a month, while traditional Swiss cheese is aged from two months to many years. Because of the shorter aging, baby Swiss has smaller holes, tastes slightly sweet and nutty, and is great for melting. Traditional Swiss, on the other hand, is more expensive, has larger holes, and tastes sharp and tangy.
Preheat oven to 350F. Thaw and squeeze moisture from spinach. Lightly coat 9-inch pie pan with cooking oil; set aside. Heat oil in large nonstick skillet over medium heat. Add mushrooms and cook for 4 minutes, stirring frequently. Add onion and garlic and cook for 4 minutes more, stirring often, until tender. Turn down heat if mixture starts to burn. Remove from heat, transfer to medium bowl and let cool. Gently mix in spinach.
In large bowl, whisk eggs, milk, mustard, thyme, salt, and pepper. Fold in the mushroom mixture and cheese. Transfer to prepared pie pan and bake until set, about 50 minutes. Let stand for 10 minutes. Slice and enjoy!
We are grateful for your commitment and compassion that you give each and every day. Thank you for all you do!
716.686-8000 HospiceBuffalo.com


While nationwide the temperatures are trending upward and we are experiencing brighter forecasts, we are also seeing an increase in spring and summer allergies.
Around 50 million people suffer from allergies in the U.S., according to the American College of Allergy, Asthma and Immunology, which makes it a very common ailment.
“Allergies run a very wide spectrum from simply a runny nose and stuffiness to serious problems like asthma and other ailments that can be fatal,” said physician Stanley A. Schwartz, division chief of allergy, immunology and rheumatology at University at Buffalo department of medicine. “That is what makes allergies something that people must pay attention to. Something that may be as small as a food allergy can be life-affecting because there are people who die from peanut allergies because of anaphylactic shock.”
Schwartz, who is also a distinguished professor of medicine and pediatrics at the Jacobs School of Medicine and Biomedical Sciences,

discusses five aspects of allergies.
Allergic reactions can cause symptoms such as runny nose, sneezing, congestion, itchy or watery eyes and post nasal drop. In addition, some people experience scratchy throat and fatigue. Allergies also affect your sleep. Allergies can make it difficult to breathe, leading to sleep apnea, snoring, and other sleep disorders.
“People used to feel like every allergy season was worse than the previous. But that was just perception because they were just dealing with their current suffering,” said Schwartz. “However, now with global warming and with the spring season starting earlier, it is distinctly obvious that allergy seasons are getting worse and longer with each year.”
Allergies are treated in various ways ranging from over-thecounter medication such as antihistamines, decongestants and nasal
Spring allergies can be brutal, and many — but by no means all — sufferers reach for synthetic medications to combat their symptoms.
Many others want something more natural, however.
“These allergies cause unpleasant symptoms such as runny noses, sneezing, itchy eyes and nasal congestion,” said physician Jo Reed, an expert in allergy, asthma and immunology from Ochsner Health in Louisiana.
“Of course, you can take various synthetic medications for allergies, but many sufferers prefer to use
natural remedies,” Reed said in an Ochsner news release.
Here, Reed offers some options:
An herb known as butterbur is one option, according to several scientific studies. In one, Swiss researchers found butterbur is a strong antihistamine that can control hay fever.
“It also does not cause drowsiness, unlike some over-the-counter allergy medications,” Reed said.
• Green tea contains a substance that can block certain allergic responses in the body, according to studies by Japanese scientists. It may reduce sneezing and itchy eyes.
• Spicy food, including cayenne
sprays to severe case solutions such as, allergy shots or immunotherapy.
Immunotherapy treatment involves a series of injections of purified allergen extracts, usually given over a period of a few years.
“Nasal sprays must be used regularly for it to be effective. If you are not consistent and only use them when you have allergy symptoms starting, it will not work the way it needs to,” said Schwartz.
Your physician will help you take steps to identify and avoid your allergy triggers. This is generally the most important step in preventing allergic reactions and reducing symptoms.
Allergy shots are given once a week for six months. Schwartz said it is typically done when allergy season is over so a patient can build tolerance. Then slowly the allergy shots are given once a month.
“This all has to be done in a doctor’s office because there is always a risk of any allergic reaction. Allergy shots over a period of time have been proven to be quite successful. It can help you become desensitized to the symptoms,” said Schwartz. “It has
pepper, could help. It contains capsaicin, known to reduce nasal congestion. Also, allicin, found in garlic, is an anti-inflammatory that can reduce swelling and inflammation.
• A neti pot, with its long, thin spout, can help clear clogged sinus passages. Fill the pot with warm, sterile water and salt before tilting your head back and allowing the solution to enter your nasal passages through a nostril. Continue until the solution flows out of the other nostril.
Seasonal allergies can cause dryness in your nose and sinuses, leading to congestion and swelling.
“One great way to counteract the dryness is to use a humidifier,” Reed said. “This device releases water vapor into the air and helps moisturize your dry nasal and sinus passages, resulting in less congestion and
Schwartz, allergy,been known to be as high as 97% effective.”
If you think you have seasonal allergies, talk to your doctor. Experts can help you establish your triggers along with possible treatment options. Creating your personal blueprint will help you follow and manage your allergies. An allergist can provide a skin test, which involves the patient being pricked with small amounts of proteins found in common allergens. If you’re allergic, the patient develops a raised bump or hive at the test location of the skin.
“One of the reasons why we recommend people come to our offices is because there are a lot of misconceptions and people start to misdiagnose,” said Schwartz.
Seasonal allergies, sometimes called hay fever, can lead to various reactions with substances in the air such as pollen, falling through the sky. While the timing and severity of an allergy season vary across the country, there are many following climate factors that contribute to how bad your symptoms might be, including trees, grass and ragweed pollen that thrive during cool nights and warm days.
“Allergies happen throughout the year with weather playing a large factor. It can lead to pollen issues and there is no way to turn it all off and on,” said Schwartz.
Respiratory allergies are various and run the gamut from light to severe. Because of that range there are misconceptions about what can cause allergies including the decision to purchase a pet.
“One of the things people come in is thinking that if they get a special hypoallergenic animal then they don’t have to worry about their allergies. However, the animal’s hair has nothing to do with allergies,” he added. “It is the animal’s saliva.”
discomfort.”
• Eucalyptus oil, from the leaves of eucalyptus trees, has been found in studies to reduce inflammation-caused allergies. Add a few drops to a bowl of steaming water and breathe in the vapors.
Your vacuum should have a high-efficiency particulate air filter, so you can rid your home of pollen with regular cleaning. These filters effectively minimize the amount of symptom-causing pollen inside your house.
You can also wear protective clothing to reduce your pollen exposure when outside, Reed advised. Slip on sunglasses, a wide-brimmed hat and long pants to keep pollen from getting on your skin. Remember to remove your clothes at the end of the day and shower to remove any pollen.
The pandemic exacerbated the longstanding shortage of bedside nurses. Tougher conditions, supply scarcity, employee illnesses and many sicker patients prompted many hospital nurses to quit the profession or move into a non-hospital role in nursing.
In addition, waves of retiring nurses have also affected the number of hospital nurses, meaning both that fewer nurses are in hospitals and also that as these individuals age, like their contemporaries, they will need more healthcare.
Deb Palmeri, clinical service manager at Visiting Nursing Association of WNY in Cheektowaga, has noticed that patients receive shorter care and upon discharge, less education.

“They don’t know about their healthcare needs, like ostomy care,” she said. “They’re not getting the education on their disease processes as much anymore. Our patients are coming home pretty sick.”
She thinks this points to the nursing shortage causing truncated care by necessity.
To properly care for patients, many hospitals temporarily reduced capacity or paused services. Some are still not operating at full capacity, as that would place the patient-to-nurse ratio at unsafe levels. Some also use agencies dispatching travel nurses, which seems a bit like a shell game to Martha Kershaw, who holds a doctorate in education, and is a registered nurse and associate professor of nursing with Daemen University in Amherst. When nurses shift from hospital systems to traveler positions with agencies, they may make four to five times their previous salary.
But the additional cost to hospitals and increased retention “has caused in some places, the number of travelers to decrease,” Kershaw said.
One of the barriers to placing more nurses within the healthcare system is a lack of slots for nurses’ clinical hours. Kershaw said that during the pandemic, many organizations did not want additional new people within their facilities. But the school’s new acute care program has helped develop nurses in high demand and since the pandemic restrictions have lifted, “they’re definitely looking for students to come in,” she said.
A lack of nurses at long-term care facilities further worsens the nursing shortage problem at hospitals, as sick people who need short-term rehabilitation or long-term care have no place to go and must therefore stay at the hospital longer, filling beds needed by still sicker people.
The enrollment rates at many schools have decreased as coverage of the nursing shortage has made more people aware of the challenges of nursing.
“Some of the aspects of COVID-19 could have steered people away from nursing because of the fear of the unknown and the quick transition of maintaining home life and work when COVID-19 came,” said Jacob Fisher, Fisher, who holds a Ph.D., is a master’s trained nurse, and works as assistant dean of nursing and faculty with Trocaire College in Buffalo. “People know about the emotional-mental piece of nursing during COVID-19 and working short- staffed. These also played a big role.”
He hopes that continuing to
develop relationships with healthcare organizations can help them cultivate long-term employees. He also suggests that summer internships and other experiences can bring potential nursing students to organizations to learn what nursing is all about.
“Today, part of that relationshipbuilding is what will be the best for the employees,” Fisher said. “It’s a fit with outside life. Some organizations offer sign-on bonuses and agreements where they don’t have to work weekends or holidays. Healthcare has to be modifiable with current times and is equitable for everyone. We have to figure out needs of the employees.
“Helping bolster the student experience early on can help with the shortage.”

Jennifer Schwytzer, nationally licensed master social worker and owner of KINDfulness Coaching, has recognized that part of this concept relates to the emotional makeup of nurses. Drawn to the profession by their sense of empathy, “nurses are more prone to compassion fatigue and burnout with exposure to trauma, high mortality rates, staff shortages and long hours,” she said.
Schwytzer serves clients throughout Western New York and specializes in mental health and selfcare among healthcare workers.
The fast-paced world of hospital
nursing leaves little time to process stress and trauma during the workday and little energy to do so afterwards. Schwytzer said that this can lead to burnout without nurses even knowing what happened.
She added that many members of the Millennial age group values work/life balance more than previous generations, which can lead to disillusionment with the nursing career during a time of high demand such as during the pandemic.

“The COVID-19 era has accelerated nursing shortages, which for those that stay as nurses means they may have more patients, less help, more hours or overtime and high levels of stress,” Schwytzer said. “This screams burnout.”
She encourages healthcare workers to fight burnout.
• “Identifying your feelings and thoughts early on can help to put a halt to burnout symptoms. A common framework that therapists or coaches may use teaches you that your circumstances don’t change, but the way you frame your thoughts and feelings can significantly impact your actions and behaviors. Getting a handle on how you think and view your environment can significantly impact the job you do.
• “Learning to set healthy boundaries, knowing what you are willing to do and not willing to do also helps. Sometimes saying no can be so important, especially in the nursing profession: ‘No, I can’t take an extra shift; I know I need a break today.’ Keeping boundaries and respecting others’ boundaries fits into this suggestion as well.
• “Try to learn not to take things so seriously. Everything is not about us. Recognize that you can provide support and assistance without taking on someone else’s trauma or problem. It is not always up to you to solve or fix. That may be out of our control and recognizing what is in and out of our control is key.
• “Believe that others can save themselves. We cannot fix or heal someone that does not want to be healed and sometimes this is a really hard concept to allow in.
• “Self-care is so easy, yet we have such a hard time doing it because there just isn’t enough time or energy. Everyone has the same 24 hours in the day; you can take care of you. It’s a choice you make and if you need help figuring out how to integrate the things you love and enjoy into your day, ask for help. It’s crucial to eliminating burnout from your life and job.”
Cafeteria workers. Receptionists. Pharmacists. Janitors. Administrators. Physical therapists.
Much has been made of burnout among doctors and nurses, but a new survey has found high rates of work fatigue in nearly every type of job associated with health care.
Physicians, nurses, clinical staff and non clinical support workers in health care all are experiencing substantial levels of burnout, according to a report published recently in the Journal of General Internal Medicine.

For example, the percentage reporting burnout was very similar between nurses (56%), clinical staff (54%), doctors (47%) and non clinical staff (46%).
“Every member of the health care team is really critical to patient outcomes and patient experiences of care,” said lead researcher, physician Lisa Rotenstein, an assistant professor of medicine at Harvard Medical School. “It’s just really important for us to remember that as we are trying
to optimize both patient outcomes and experiences for our workforce.”
For this study, Rotenstein and her colleagues surveyed workers at 206 large health care organizations between April and December 2020, at the height of the pandemic.
The participants included more than 15,000 physicians and 11,000 nurses.
But researchers also surveyed more than 5,000 clinical staff such as pharmacists, nurse assistants, therapists and social workers, as well as more than 11,000 non clinical staff including housekeeping, administrators, lab technicians and food service workers.
In addition to high levels of burnout, the researchers also found that many workers intended to leave their jobs within two years - nurses (41%), clinical and non clinical staff (32%) and doctors (24%).
Substantial numbers also reported work overload, including 47% of nurses and clinical staff, 44% of
By Deborah Jeanne SergeantUB
nurse Christopher Palumbo always wanted to make a difference in others’ lives through healthcare. While attending college, he learned more about nursing and realized that was the right path for him.
“What drew me to it is the holistic approach,” he said. “We don’t just take care of the pathology of the disease, but mind, body, soul and spirit to give patients the best total care.”
The North Tonawanda resident started nursing school in 2018 at UB and passed the board examinations in 2022. He started working in the cardiac ICU at Mercy Hospital as a bachelor’s trained nurse that summer. But Palumbo isn’t done with school yet. He started the nurse practitioner program at UB in August 2022.

What has surprised him the most during the transition from student to full-time nurse is the amount of autonomy nurses possess in certain settings. Nurses are far more than pillow fluffers and temperature takers (although providing comfort and checking vitals are both important).
“You are not just there to do busy work,” Palumbo said. “You have to know the devices and medication and equipment. You have to make a lot of decisions on your own. A lot of providers give you orders to make the decision as you see fit. In a lot of cases, you’re the one making the decisions with orders given.”
He has also felt surprised at the amount of information he had to know, both to become a nurse and to stay up to date while working as a nurse.
“There’s so much to learn,” Palumbo said. “You have to put in the work outside of your three days a week at the hospital to research
and the things you’re working with. Things are constantly changing, and new research comes out that shows something is not the best way to do things. You really have to be willing to go with that change and learn. Even with the technology and charting systems we have change.”
One very positive change has been the shift away from stigmatizing men in a female-dominated field. Palumbo said that he feels honored to work in an industry largely populated by women, but still encounters unusual reactions from patients.
“I’ll walk into a room and they’ll think I’m the doctor but I’m with a female doctor,” he said. “They think she’s the nurse. It’s awesome to change that and educate the patients that females aren’t only nurses; they’re also doctors.”
As a new nurse, one of his biggest day-to-day challenges has been feeling confident at work, yet humble enough to realize that he can learn from mistakes and move forward, because “you want to do everything right, but you won’t get everything right,” he said.
The part of nursing he most enjoys is interacting with patients and families from different cultures and backgrounds. He likes learning more about others and why people do different things.
After he finishes his four years at UB, he wants to work as a nurse practitioner in critical care and eventually help educate new nurse practitioners.
“It’s an amazing field,” Palumbo said “The more nurses we can get into it, the more voices to go to legislators to make changes and get laws passed for staffing and protection for nurses. And the more people who receive excellent care.”
non-clinical staff and 37% of doctors.
Even though the survey was conducted during the height of the pandemic, Rotenstein suspects that things haven’t improved for health care workers in the subsequent years.
“Some of the stresses have persisted as we have moved into a new
phase of the pandemic,” Rotenstein said. “There are staffing shortages. There are patients who have delayed care because of the COVID pandemic, and so now we’re seeing an increase in demand for health care. Oftentimes, health care workers are being asked to do more with less.”
Chris Palumbo on Nursing:
‘It’s an amazing field’
Sophia Overton serves as clinical nursing instructor at UB. Overton’s route to her current role is rather serpentine.
She had always wanted to work as a nurse since she was 14. She completed an LPN vocational program while in high school but worked a few different jobs instead. Although she “took a few turns in life,” she returned to the career two decades later at age 36.
Her company was laying off employees, which caused her to think, “What do I want to do now?”
That contemplation took her back to her original plan: to become a nurse. She completed her associate degree at Niagara Community College, her BSN and master’s degree at Daemen, and is currently enrolled in UB’s program for psychiatric mental health nurse practitioner, which she anticipates completing in 2026.
“I want to reach my fullest capacity,” Overton said. “The LPN was just a steppingstone to a bigger place in life.”
In the meantime, she has worked in several roles, including hospice nurse, long-term care, school nurse, registered nurse case manager, a correctional staff nurse, a quality support nurse investigator, a behavior health nurse and clinical nurse educator.
Much has changed in healthcare since her early introduction to it as a teen. Most of all, the technology and equipment has changed, such as mercury thermometers common during her teen years to the electronic thermometers used now.
The nurse-to-patient ratio has also changed, from 20 patients to much lower levels, which she equates to improving patient care. The care itself has also shifted to patient-centered care.


Although it’s never too late to improve oneself, Overton wishes that she had stayed the course as a younger person, with the same focus
she had at 14.
“I think now I would’ve been in a different position,” she said. “However, I don’t regret the twists and turns in life because of all the lessons I have learned. I can share that with upcoming, future nurses.”
She also wants everyone in healthcare to treat others “equally and respectfully,” she said. “Give quality care to everyone. There are so many biases and prejudices and racism in healthcare, and I would like to see that just eliminated.”

Despite the challenges of the field, she wants more high school students to consider nursing as their career because of how rewarding it is and because of the opportunities nursing can provide in numerous arenas.
Overton would like to see greater representation of people of color among nurses, not only for equity’s sake, but also so more patients can receive care from people who look like them. Better representation can also help reduce cultural misunderstandings between patients and providers.
According to the American Association of Colleges of Nursing, Blacks comprise 13% of the population, but only 10% of bachelor’s trained nurses.
Someday, Overton hopes to work with underserved populations, focusing on diabetes care and mental health.
“So many Black and Hispanic people deal with mental health issues and have diabetes,” she said. “Around 75% of people with depression have diabetes. That care should come together, not remain separate. I want to open an integrative practice. We don’t really have one in the city of Buffalo.”
In her spare time, she enjoys watching plays, visiting museums, and in her travels, viewing Frank Lloyd Wright architecture.
The shortage of nurses to work in hospitals pre-existed the pandemic. However, the health crisis made the problem worse. The nursing shortage has affected independent practices similarly.
“We are having a hard time hiring nurses,” said Deb Palmeri,




clinical service manager at Visiting Nursing Association of WNY in Cheektowaga. “We aren’t hearing from applicants.”
The pandemic has made home healthcare a less desirable field for nurses than it used to be. Palmeri said that patients of home healthcare

are sicker than they used to be, as hospitals push to discharge patients sooner than they used to.
Increase in violence against nurses has made the field more stressful, especially in non institutional settings like home healthcare (although violence against hospital nurses is up).
“There’s a lot of family dynamics you don’t see in the hospital,” Palmeri said. “In the hospital, it’s a controlled environment. They’re struggling to get around. We walk into the home for short-term intermittent care. Is it safe for us to be in the home?”
Palmeri also said that several VNA nurses experienced burnout during the pandemic and segued to less stressful roles such as case management for insurance companies.
Palmeri does not believe better pay is necessarily the answer to the nursing shortage.
To attract more nurses, VNA offers sign-on bonuses and has tried to offer more Monday through Friday daytime shifts to provide better work-life balance, but that’s impossible to offer all employees because patients need care outside of banking hours. Offering weekend-only shifts or 10- or 12-hour shifts for fewer days per week fits some employees’ needs better.
VNA is also more widely publicizing its need for nurses by posting on social media, hosting open houses, and participating in college job fairs. Still, out of the near dozen students in clinical rotation who began at VNA in July 2020, only two are left, as they “found homecare isn’t for them,” Palmeri said. “It can be challenging as a young nurse. Most have gone other paths in their nursing profession, so that’s encouraging.”

Martha Kershaw, doctorate in education, and is a registered nurse and associate professor of nursing with Daemen University in Amherst, She said that although the nursing shortage includes private healthcare organizations, it’s more dire at hospitals because “work-life balance is a big thing, and the younger generation is definitely looking for it. There are many areas for nurses to work like hospitals, community, wellness centers, as educators, and in schools as nurses. But from what I’m seeing
there’s a need across the board for nurses.”

Daemen is trying to increase the number of enrollments in its nursing school and find more nurse educators. Without sufficient educators, an educational institution cannot train new nurses.
Jacob Fisher, P.h.D., is a master’s trained nurse, and assistant dean of nursing and faculty with Trocaire College in Buffalo, thinks that independent practices could retain and recruit more nurses by mimicking what large organizations are doing like providing sign-on bonuses and developing more flexible schedules.


“They maybe can’t offer as high of a sign-on bonus, but the expectation of the schedule is part of the package,” Fisher said. “An educational assistance can help them in obtaining a higher level of nursing. Part of that is helping them see how they fit into the organization now and how can the organization help them to get to their end path, like a BSN.”
Many large healthcare organizations reimburse or pay upfront for employees’ education, but with a stipulation that they work for them for six months to three years, depending upon the organization and the level of education. Although this brings many more nurses into the workforce, it also keeps away from choosing small, independent practices and instead working in the larger healthcare systems, such as those operating larger hospitals and the freestanding offices owned by the same healthcare systems. The strategy is often successful in keeping nurses in the same organizations for years after they have fulfilled their obligation.
Fisher wants to see more healthcare organizations work with each other in collaboration — even if as business they’re competitors — and with educators as well.
“This can meet the needs of students so they’re ready to enter the workforce,” Fisher said. “Most of our grads stay in the Western New York area. We tell our students every day in clinical that it’s an on-the-job interview. They may want you to join them when you’re done with school, or a nurse assistant position could segue into a nursing position once you have the credentials.”
People who want to work as a nurse have many pathways to receive their credentials.
Unlike many careers, nursing doesn’t have to cost a lot to enter. Many people begin nursing in entry-level work, such as a certified nurse assistant.
“That’s typically offered as a free program by teaching hospitals and other organizations,” said Molli Oldenburg, doctorate of nurse practitioner and global initiatives coordinator and family nurse practitioner program coordinator at UB.

These programs typically run for four to 12 weeks.
Many organizations offer tuition in part or in full to become a licensed practical nurse, a credential that requires a yearlong program.
“It’s typically a vocation educa-
tion,” Oldenburg said. “I completed mine while in high school and did half days at BOCES for two years. If you did it full-time, you could do it in a year.”
The next level is a registered nurse, an associate degree program that requires a two-year program, often offered at community colleges, followed by a state exam before receiving licensure.
Since 2017, registered nurses are required to complete a bachelor’s degree (BSN) within 10 years, which is a four-year program (including the two years to complete the registered nurse program).
Healthcare organizations “mostly cover the cost to go back to get your bachelor’s if you’re already working there with your associate,” Oldenburg said.
The next level is the advanced practice registered nurse, or master of science in nursing. This could include a nurse practitioner, clinical nurse leader, clinical nurse specialist, certified registered nurse anesthetist or certified nurse midwife.
“They’re more in a provider role diagnosing, treating and prescribing,” Oldenburg said.
Beyond these levels are the non clinical specialties such as doctor of nurse practitioner, which enables people to serve as a nurse administrator, nursing informaticist, nurse educator, or nurse researcher.
“Most hospitals and unions that nurses join offer some payback for this education, but it’s mostly funded by nurses,” Oldenburg said.
With each level comes a higher level of responsibility, scope of practice and salary.
“The options of what you can do are endless as a nurse practitioner,” Oldenburg said. “You can work in whatever you’re trained to work in as long it’s in your scope of practice. It’s been discussed that they’re require all NPs to be doctorate prepared and eliminate the master’s level. There’s discussion that will happening. Other health sciences like pharmacy and physical therapy have moved to that. It’s something I do believe will happen to keep up and be equal to other healthcare roles. It offers more ability for NPs to bring research and evidence-based care to practice and improve care to in patient and out patient. It improves education in academia.”
Area institutions like UB and Daemen try to stay abreast to needs among healthcare providers to grow existing programs or if needed, begin new ones.
“One of the things we noticed
Molli Oldenburg, a nurse practitioner, is the global initiatives coordinator and family nurse practitioner program coordinator at UB. is a need for acute care nurse practitioners,” said Martha Kershaw, who holds a doctorate in education, and is a registered nurse and associate professor of nursing with Daemen University in Amherst. “We’ve had a program for that approved and we started admitting students this semester. They could meet the need in hospitals in any hospital setting for hospitalist, ICU and ER.”
Seeking more education can only help nurses in furthering their careers in the future, especially in management education, or leadership roles. At the master’s level, nurses can specialize in areas of interest so they can command higher wages and practice more independently. But the DNP may not mean greater wages when practicing at the clinical level, but as a steppingstone to teaching or administrative roles.


Dr. Boyle is a fellowship-trained, experienced surgeon who has performed numerous joint replacements and joint revision surgeries, helping patients recover their mobility and reduce or eliminate pain. Dr. Boyle will do a comprehensive review of your individual condition and provide a course of treatment – including surgical and non-surgical options – specifically tailored to your unique needs.
There’s more need than ever before for well-educated and highly trained nurses. Trocaire is ready to help you get the skills you need to thrive in the high-paying world of healthcare. Let us help you get started.

 K. Keely Boyle, MD Specializing in Lower Extremity Joint Replacement and Reconstruction
K. Keely Boyle, MD Specializing in Lower Extremity Joint Replacement and Reconstruction


Every baby born in a hospital receives a newborn hearing exam. Unfortunately, the next time that the person’s hearing is considered is typically once a significant degree of hearing is lost.
Signs of hearing loss vary by age.

In infants, tugging on the ears, irritability and general discontent can be symptoms of an ear-nosethroat related illness that could cause damage to hearing unless address promptly.
“Parents may notice language delay for preschool-aged children,” said Karen Martin McMahon, audiologist and owner of Hearing Health Center in Buffalo. “Teachers would notice inattentiveness at PreK.”


School-aged children may seem to not listen in school, keep the TV or other devices loud or seem confused when given directions that are age-appropriate in complexity.
Parents would notice the child
might be turning the television higher than what they feel would be normally appropriate.
“At home, there may be issues with conversation,” McMahon said. “Parents may receive teacher complaints about poor grades or inattentiveness.”

For adults, it’s typically other adults who signal a hearing problem is present, as they must repeat themselves or deal with the excessive radio or TV volume. Some less obvious signs he included are not hearing the crickets at night or the birds during the day. Dizziness or ringing in the ears (tinnitus) can also indicate a hearing problem.
“The clarity of conversation is usually an issue,” McMahon said. “There’s difficulty in hearing in the presence of background noise. People feel like others are mumbling or conversation is muffled. Ringing in the ears — tinnitus — can be a sign of




hearing loss. The same things apply for older adults.”
Losing hearing can cause different and significant problems across the lifespan. For children, diminished hearing can interfere with language acquisition, learning and developing social understanding.
“Some hearing loss is reversible if you catch it soon enough,” said Salvatore Gruttadauria, audiologist and owner of Diversified Hearing & Balance Centers in Buffalo. “Some viral conditions affect the ear and cause sudden hearing loss. Many wait because they think it’s wax in the ear. There’s only a short window of time to have that done. Audiologists aren’t medical doctors, but the hearing test is a window into the health of the ear. A hearing test isn’t just to see whether you can hear, but is your hearing system healthy? Does it need any medical intervention?”
For school-aged children who
have lifelong hearing loss, early intervention can help them stay abreast with their schoolwork. Neglecting hearing issues can cause them to fall behind.
Working adults should also promptly address hearing issues. Otherwise, their work and income may suffer.
“Studies do indicate that people with an untreated hearing loss actually have a decreased income over people who don’t have a hearing loss,” Gruttadauria said. “If they say ‘What?’ a lot are thought of as not being as smart or as capable. That’s not necessarily true. It can affect their work performance and their overall income.”
For people working in environments such as construction or agriculture, not hearing well can compromise their safety because they don’t realize what they’re missing. It can also result in loss of work for some occupations such as professional truck drivers.
For older adults, letting hearing loss go too long can increase the risk of cognitive impairment.
“A study shows that untreated hearing loss is the single most modifiable factor to decrease your risk of dementia,” Gruttadauria said. “You can do something about it: provide hearing aids to mitigate the risk. As we get older, safety can be a concern, like hearing the smoke alarm. Or hearing when people call or come to the door. If people can’t hear well on the telephone, that can cut people off socially.”
Waiting can also make acclimating to hearing aids more challenging as the brain has to relearn how to process sounds again. Untreated hearing loss can also increase the risk for falls.
Unfortunately, it can take many people a long time to discover and treat hearing loss — the average time is seven years. Gruttadauria said that many people feel shocked to discover that they have a hearing loss. As with many areas of health, the sooner a problem is identified and addressed, the better.

What’s the best way to go about choosing an assisted living facility for my 86-year-old father? Since mom died last year, his health has declined to the point that he can’t live at home anymore but isn’t ready for a nursing home either.
If your dad needs help with things like bathing, dressing, preparing meals, managing his medications or just getting around, an assisted living facility is definitely a good option to consider.
Assisted living facilities are residential communities that offer different levels of health or personal care services for seniors who want or need help with daily living.


There are nearly 29,000 assisted living communities (also called board and care, supportive-care or residential-care facilities) in the U.S. today, some of which are part of a retirement community or nursing home. Most facilities have anywhere between 10 and 100 suites, varying in size from a single room to a full apartment. And some even offer special memory care units for residents with dementia.
To help you choose a good assisted living facility for your dad, here are some steps to follow.

• Make a list: There are several sources you can turn to for referrals to top assisted living communities in your area including your dad’s doctor or nearby hospital discharge planner; friends or neighbors who’ve had a loved one in assisted living; or you can do an online search at Caring.com.


• Do some research: To research the communities on your list, put a call into your long-term care ombudsman. This is a government official who investigates long-term care facility complaints and advocates for residents and their families. This person can help you find the latest health inspection reports on specific assisted living facilities and can tell you which ones have had complaints or other problems in the past. To find your local ombudsman visit LTCombudsman.org.
• Call the facilities: Once you’ve identified a few good assisted living facilities, call them to see if they have any vacancies, what they charge and if they provide the types of services your father needs.


• Tour your top choices: During your visit, notice the cleanliness and smell of the facility. Is it homey and inviting? Does the staff seem respon-
sive and kind to its residents? Also be sure to taste the food, and talk to the residents and their family members, if available. It’s also a good idea to visit several times at different times of the day and different days of the week to get a broader perspective.
On your facility visit, get a copy of the admissions contract and the residence rules that outline the fees (and any extra charges), services and residents’ rights, and explanations for when a resident might be asked to leave because their condition has worsened, and they require more care than the facility can provide.
Also, find out their staff turnover rate, COVID-19 infection-control procedures and if and when medical professionals are on site. To help you rate your visit, Caring.com offers a checklist of questions that you can download and print at Caring.com/ static/checklist-AL-tour.pdf.
• How to pay: Monthly costs for assisted living ranges anywhere from $2,500 to $6,000 or more, depending on where you live, the facility you choose, and the services provided. Since Medicare does not cover assisted living, most residents pay outof-pocket from their own personal funds, and some have long-term care insurance policies.
If your dad has limited financial resources and can’t afford this, most states now have Medicaid waiver programs that help pay for assisted living. Or, if he’s a veteran, he may be able to get funds through the VA’s Aid and Attendance benefit. To find out about these programs, ask the assisted living facility director, or contact his local Medicaid office (see Medicaid.gov) or the regional VA benefit office (800–827–1000).

Assisted living facilities are residential communities that offer different levels of health or personal care services for seniors who want or need help with daily living.
Michael Slattery just loves putting miles on his bicycles.
“I average about 5,000 miles a year,” says the deputy town supervisor of the town of Chili.
The married, 57-year-old grandfather plans to put his love for cycling to use for worthy causes on May 8, when he sets out on an over 1,800 mile jaunt down the Eastern Seaboard to raise money for three nonprofits.



The money Slattery brings in will go to the Pirate Toy Fund, the National Center for Missing and Exploited Children and Honor Flight Rochester.
Slattery plans to start his trip in Charlotte and head south, rolling through Penns ylvania, Maryland, Virginia, North and South Carolina and Georgia before ending up in Florida 25 days later. Along the way, he’ll stop at the Alexandria, Virginia headquarters of the National Center for Missing and Exploited Children (NCMEC) as part of his fundraising efforts.
NCMEC, the largest and most influential nonprofit child protection organization in the U.S., helps find missing children, strives to decrease child sexual exploitation and tries to
prevent child victimization.
“We lead the fight to protect children, creating vital resources for them and the people who keep them safe,” says Edward Suk, executive director of NCMEC’s New York branch.
Slattery says the deaths of two young women, 20-year-old Fairport resident Lisa Eisman and 17-yearold Brittanee Drexel of Chili, made NCMEC’s fight particularly important to him. Both young women died violently.
Eisman was Slattery’s cousin. She and her college roommate, who were students at the State University College at Buffalo, were beaten to death in 1985 while hitchhiking to Fort Lauderdale on spring break. Drexel disappeared in 2009 while on a trip to Myrtle Beach. Slattery coached her for a time when she was on the team Chili Soccer.
“My daughters grew up with Brittanee,” he says. “For me, it’s personal.”
NCMEC aided the search for Drexel.
“We had our local and national case management team involved in cultivating leads with law enforcement,” Suk says. “We also handled
targeted poster distribution, and media outreach through our media team.”
Raymond Moody, Drexel’s killer, was convicted of kidnapping, murder and first-degree sexual in late 2022. He was sentenced to life in prison on one charge and 30 years each on the other two charges. Slattery plans to visit the place where Drexel’s remains were found while en route to Florida, and to visit NCMEC’s Washington offices as part of his fundraiser.
Slattery’s upcoming journey south is just one of the rides he’s taken to raise money for NCMEC. Just last year, he participated in The Ride for Missing Children, NCMEC’s annual fundraiser. Mounting his bike, he pedaled through Buffalo, Rochester, Syracuse, Utica and Albany, covering about 100 miles in each city.
Since 1995, the Pirate Toy Fund has headed to hospitals and other locations in the greater Rochester area to distribute new toys to needy children free of charge. As Slattery pedals along to raise money for the nonprofit, he’ll have a friend at his back—literally. Otto Harnischfeger, the Pirate Toy Fund’s executive director, will follow him down the road in an RV, providing aid.
“I can’t believe he’s doing it,” Harnischfeger says of his good friend. “I ride five minutes and I’m sore. I want to get off the bike.”
Harnischfeger has known the Slattery family since he became
friends with Raymond Slattery, Michael’s father, when the two were on the Rochester Police Department.
“It’s a caring family, they really are,” Harnischfeger says.
The money Slattery raises on his long-distance ride should be welcome.
“Our first year we gave out 300 toys,” Harnischfeger says. “Last year, we gave out over 36,000 toys free of charge, all because of the good nature of the Rochester community.”
In addition to raising money for the Pirate Toy Fund, Slattery sits on the nonprofit’s board of directors.
Six times a year, about 60 veterans and their helpers, called “guardians,” head out of Rochester for a weekend in the nation’s capital, courtesy of Honor Flight Rochester.
“Honor Flight Rochester provides airplane trips for veterans to travel together to see their memorials in Washington DC to receive that long-delayed thank-you that they’d not received many years ago,” says Richard Stewart, the nonprofit’s president and CEO.
The trip to the nation’s capital includes hotel accommodations, tours of the World War II, Korean War and Vietnam War memorials and other important sites and a gala dinner in honor of those who once served their country. The veterans travel free, but their guardians, who are usually family members or friends, have to cover part of the cost of the trip.
Slattery says he plans to stop in Washington this May to accompany an Honor Flight Rochester group as it visits memorial sites. After that, he’ll have lunch with them and get back on his bike.
“I plan on leaving Washington in the early afternoon, so I can get in about 30 miles or so,’ Slattery says.
Honor Flight Rochester, an all-volunteer organization, spends about $500,000 a year on its services to veterans, and is supported by donations. Stewart says the nonprofit is able to cover its current costs, but will have to fund new trips to Washington in the future.
“We have a fly-list of 1,000 veterans,” Stewart says. “If we don’t have money, we don’t fly.”
Slattery’s ride south is just his latest effort to help his community.
He has also raised money for other nonprofits, including Camp Good Days & Special Times, which offers residential camping programs and recreational and support activities to children who are affected by cancer or sickle cell anemia and their families. In addition, Slattery sits on the Chili Town Board.
“It’s a passion for me,” Slattery says. “I enjoy giving back.”
The father of two grown daughters and grandfather of four children recently retired from the Monroe County Department of Transportation, where he was the highway maintenance manager.
For more information about Slattery’s upcoming ride or do donate to his fundraiser, go to: michaelscharityride.com.
For more information on the nonprofits for which he plans to raise money, go to: www.missingkids.org/ footer/about/newyork, www. piratetoyfund.org or https://honorflightrochester.org.