SECTION REPORT CRITICAL CARE MEDICINE
Mind the Gap – Utilizing the pCO2 Gap in Shock Resuscitation Gerard Heath, MD and Gina Hurst, MD
A
bstract
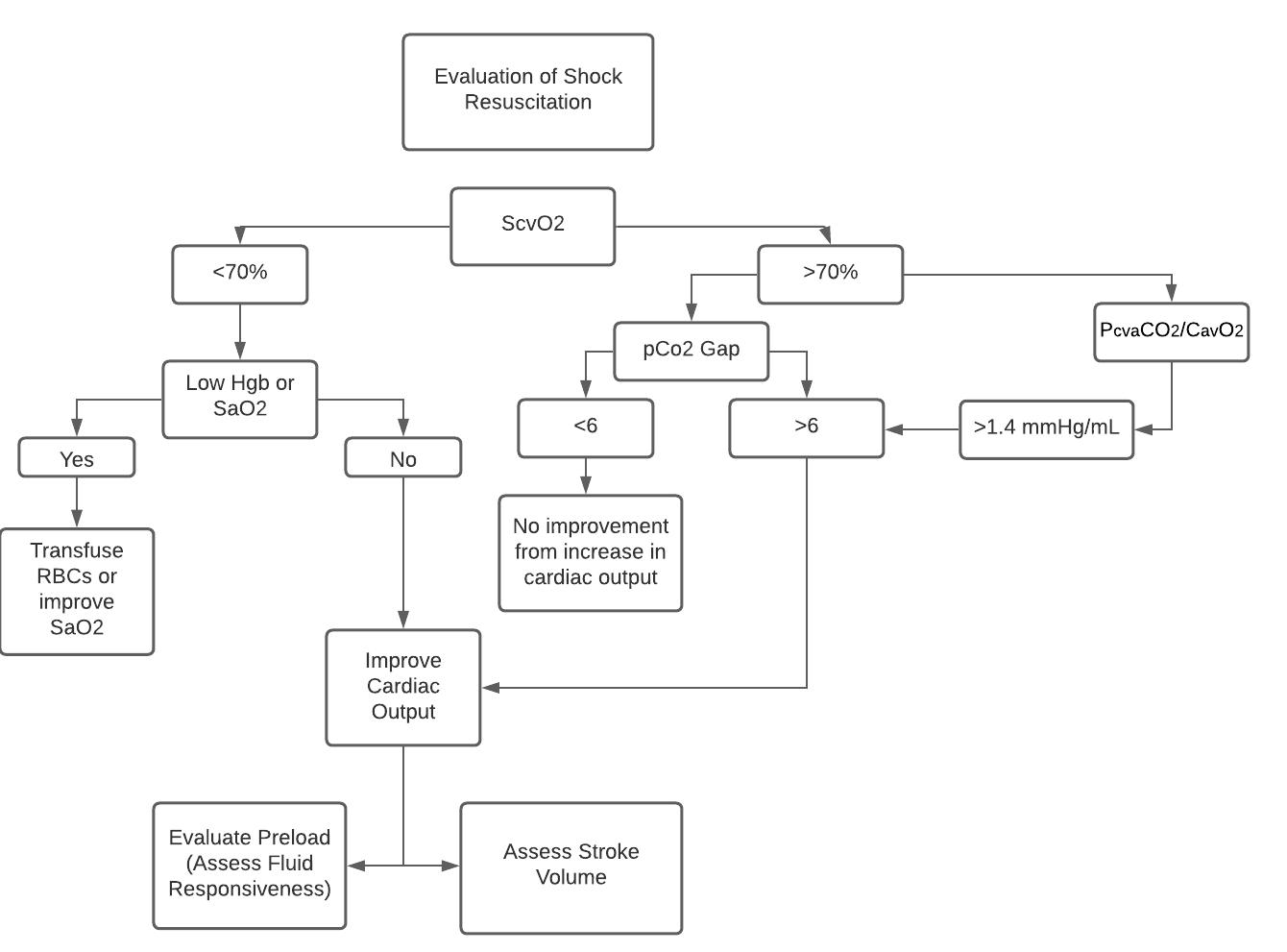
The successful management of acute circulatory shock relies upon the correction of several hemodynamic and O2-derived parameters informed by our understanding of oxygen delivery (DO2). These metrics, while important, have limitations, and O2-derived parameters may be confounded by physiologic derangements in the shock state. In this review, we hope to discuss how the observation of the partial pressure of carbon dioxide (pCO2) within the cardiovascular system may be incorporated into resuscitative assessment. In the setting of otherwise normalized hemodynamics and ScvO2, an elevated pCO2 gap, which is the difference between central venous and arterial pCO2, offers prognostic insight and has the potential to identify under-resuscitated patients who may benefit from an increase in cardiac output to achieve effective resuscitation.
Shock Resuscitation Early-Goal Directed Therapy (EGDT) established the importance of a methodical approach to septic shock management, with ongoing monitoring of resuscitation efforts and the restoration of identifiable hemodynamic endpoints.1 This protocolized approach highlighted several important physiologic parameters to optimize including central venous pressure, mean arterial pressure, and central venous oxygen saturation. Of these parameters, the central venous oxygen saturation (ScvO2), is of particular importance as many patients in shock have reduced ScvO2 levels. This abnormality indicates a derangement in oxygen delivery or consumption correlating with an increased risk of mortality.2-5 As with all resuscitative endpoints, contextual interpretation
30
COMMON SENSE SEPTEMBER/OCTOBER 2021
is key. In the setting of shock, underlying tissue damage and microcirculatory derangements may cause oxygenated arterial blood to shunt to the venous system with little oxygen extraction, leading to normal ScvO2 levels despite ongoing, or worsening, tissue hypoxia.6,7 This clinical scenario may be associated with either a normal or elevated lactate as an ongoing measure of hypoperfusion. Determining additional opportunity for resuscitative intervention in these cases can be clinically challenging. Throughout this article we hope to explore the utility of “the pCO2 gap” in evaluation of shock resuscitation, where the pCO2 gap is identified as the difference between arterial and central venous partial pressure of carbon dioxide.
CO2 Biochemistry Refresher To understand the application and limitations of the pCO2 gap in shock resuscitation, it is important to have a basic understanding of carbon dioxide production and elimination within the human body. Under oxygen-rich conditions, the tissues in the body produce high-energy molecules, namely ATP, through oxidative phosphorylation, leaving behind CO2 as a waste product. Under conditions of tissue hypoxia, the production of ATP results in the creation of lactate and also generates hydrogen ions which are then buffered by bicarbonate to produce CO2. In a shock state, anerobic metabolism predominates leading to an increase in CO2 production which then is transported to the lungs and expelled in the process of respiration. Note: Differences exist beyond the scope of this article between the partial pressure of CO2 and concentration of CO2 in the bloodstream, as well as between central venous pCO2 and mixed venous pCO2, but the use of central venous pCO2 for calculation of the pCO2 gap has been established as valid experimentally and the relationship of pCO2 and cCO2 is roughly linear over the physiologic range (Markota).
Understanding Venous vs Arterial pCO2 and the pCO2 Gap
Arterial pCO2 is primarily driven by gas exchange while venous pCO2 is driven by both tissue CO2 production, determined by the respiratory quotient, and venous outflow. Venous outflow can be thought of as directly related to cardiac output, or the blood flow supplied to physically move the CO2 from the periphery to the lungs where it is then expelled. The relationship of venous pCO2 and cardiac output has been established experimentally and the two are inversely related according to the Fick equation.4 In essence, when cardiac output is not adequately matched to metabolic demand, CO2 tends to accumulate in the venous system, while arterial pCO2 remains primarily determined by respiration, thus increasing the pCO2 gap between venous and arterial measurements.8 Under normal conditions, the pCO2 gap is rarely greater than six and this number has been established as a clinically significant alerting the clinician to the possible need for further cardiac output augmentation.9-11 An increased pCO2 gap has also shown to exist in all forms of shock and is not specific to septic shock or any single phenotype.4,10,12-16
Evidence for the pCO2 Gap in Clinical Practice Two questions remain to be established for the utilization of the pCO2 gap in shock resuscitation. The questions are as follows: How can we be sure that an elevated pCO2 gap primarily indicates inadequate cardiac output? What impact can its implementation make in the care of critically ill patients? While the focus thus far has been on venous hypercarbia being related to poor venous outflow, one could imagine an accumulation of CO2 in the venous system being a direct result of increased anerobic metabolism and hypoxia at the tissue level. However, animals subjected to hypoxia without ischemia did not develop
>>