






Do you want to increase your organization’s current gift giving from $50,000 to $500,000+ in 2024?
Crescendo’s GiftLegacy Advance 2024 marketing campaign is designed to encourage nonprofits to increase Donor Advised Funds (DAFs) and IRA Charitable Rollover gifts. *
Crescendo’s marketing tools cultivate donor relationships and help you reach your fundraising goals through personalized and strategic communication.
Marketing
Engage your donors with websites, eblasts, surveys and literature
Expand your fundraising knowledge with our webinars, seminars and conference Training
We’ve used Crescendo’s system to send out systematic, effective messaging and provide information to cultivate our prospect and donor base. For the last three years, we have surpassed our annual fundraising goal of well over $50 million per year!
Kyle Paige Executive Director, Estate & Gift Planning University of MiamiSoftware
Create presentations to motivate donors and close major gifts
Manage your gift annuities program with expert support and user-friendly software Administration
* Results not guaranteed and may vary
crescendointeractive.com
Integrated Marketing for Planned Gifts 800-858-9154


5 6 7 8 13 18
Letter from the Chair
By Arthur J. (Art) Ochoa, JDCEO Corner
By Alice Ayres, MBALetter from the Journal Chair
By Bob Nolan, FAHP, CFREDiscover how AI can transform healthcare philanthropy by promoting precision, emphasizing adhering to ethical considerations, and embracing Responsible and Beneficial AI.
/ FORWARD THINKING
The team at Piedmont Athens Regional Foundation implemented a new strategy to boost giving. This shift in focus, prioritizing gratitude over alternative nationally designated fundraising occasions, culminated in the procurement of more than $86,000.
New major gift officers often feel a lack of confidence and uncertainty about navigating the major gifts process. This article explores the ways to coach your major gift officers to new heights.

Selecting physician partners can be a challenge. Try a fresh perspective when building these important partnerships.
for the Philanthropy Technology Future
By Chris CannonFrom stage to page: This article was adapted from a live presentation given at AHP’s International Conference in September 2023.
President and Chief Executive Officer: Alice Ayres, MBA
2023 AHP Journal Advisory Council
Chair: Robert Nolan, FAHP, CFRE
Members:
Murray Ancell, MS, CFRE
Mendal Bouknight
Michelle J. Collins
Sarah Fawcett-Lee, CFRE
Jolene Francis, FAHP, CFRE
Matthew Lang, CFRE
Ben Mohler, MA, CFRE, ACFRE
Andrea Page, FAHP, CFRE
Harrison Porter, CAP, CFRE
Elizabeth Rottman, CFRE
AHP Board of Directors:
Chair: Arthur J. (Art) Ochoa, JD
Vice Chair: Tammy Morison, CFRE
Secretary/Treasurer: Shawn A. Fincher
Immediate Past Chair: Randy A. Varju, MBA, FAHP, CFRE
Directors:
Julie E. Cox, FAHP, CFRE
Jeanne Jachim, MBA
Crystal Hinson Miller
Preston Walton
Published by: Association for Healthcare Philanthropy, 2550 South Clark Street, Suite 810, Arlington, VA 22202
Managing Editor: Olivia Hairfield
Business Manager: Michelle Gilbert
About Us: The Association for Healthcare Philanthropy (AHP) is the healthcare development professionals’ definitive source of thought leadership, connections to facilitate innovation, and tools to advance knowledge and elevate philanthropy. As the world’s largest association for healthcare fundraising professionals, AHP represents 7,000 members who raise more than $11 billion each year for community health services. Our mission is to inspire, educate, and serve those transforming healthcare through philanthropy.
The Journal’s Mission: Healthcare Philanthropy will be an authoritative resource for healthcare development professionals by providing a timely, informative, and insightful collection of literature that will raise the standard of individual and organizational performance. Serving as the premier forum for healthcare philanthropy literature, the Healthcare Philanthropy journal will educate, empower, and inspire development professionals and, thereby, help strengthen the case for philanthropic support and the mission of AHP.

Iam thrilled to unveil the latest issue of AHP’s peer-reviewed, scholarly journal, Healthcare Philanthropy. Within these pages, you will find a variety of insightful articles, thought-provoking perspectives, and innovative ideas that promise to captivate and inspire.
Whether you are a seasoned veteran with decades of experience or an emerging professional new to healthcare philanthropy, there is something within these pages to pique your interest. Each article offers invaluable insights and actionable strategies designed to empower and equip you for success.

Arthur J. (Art) Ochoa, JD
AHP Chair of the Board of Directors
Senior Vice President, Advancement and Chief Advancement Officer Cedars-Sinai
Allow me to highlight just a few of the contributions in this issue: delve into the transformative potential of artificial intelligence in revolutionizing fund development strategies in an article by Nathan Chappell and Betsy Chapin Taylor, FAHP. Gain invaluable insights into the art of coaching major gift officers towards unparalleled success, courtesy of Sarah Fawcett-Lee, FAHP, CFRE, and Stephanie Foster. And be inspired by a compelling case study by Steven L. Dasher, CFRE, and Nicole T. Papst, illustrating the impact of breaking with tradition and embracing innovation. We’re grateful for the authors who’ve contributed their time and knowledge to make this publication possible.
To our members, thank you for your unwavering support. I look forward to the opportunity to reconnect with you at AHP’s upcoming annual International Conference in San Diego this November. Together, we continue to forge new pathways, foster meaningful connections, and share ways to better support our communities.
Warmest regards,

In the current climate, our hospitals and healthcare institutions are navigating one of the most challenging financial landscapes in recent memory. Tightening budgets, rising operational costs, and the ever-evolving healthcare needs of our communities have placed unprecedented strain on these vital organizations. It’s within this context that the role of philanthropy becomes not just beneficial but essential.
AHP’s journal, Healthcare Philanthropy, represents one of the many ways we can come together as a community to share resources and provide support during this time. The topics in this issue look ahead to our future with technology and AI, as well as focusing on the core of what we do with a deeper look at how we can inspire our major gift officers and physician partners. I’m grateful for the authors and their contributions and support of AHP.
 Alice Ayres, MBA President and Chief Executive Officer of AHP
Alice Ayres, MBA President and Chief Executive Officer of AHP
Beyond the journal, AHP has a fantastic series of events and resources designed to equip you with the knowledge, skills, and networks needed to drive impactful philanthropy in healthcare.
In July, the Madison Institute beckons with its deep-dive educational approach, underscoring AHP’s dedication to professional growth and lifelong learning. This unique setting fosters an intimate exploration of healthcare philanthropy’s nuances, guided by leading thinkers and experts in the field.
In November, we eagerly anticipate the AHP International Conference, our flagship gathering, to be held this year in San Diego. It’s designed to supply our members with the latest tools, knowledge, and connections needed to excel and make a meaningful impact in their roles.
Beyond these gatherings, AHP remains committed to providing continuous learning opportunities. Our suite of on-demand resources, including webinars, mini-courses, and access to the On-demand Learning Hub, stands ready to support your professional journey.
As always, I look forward to connecting with you and witnessing the collective wisdom, innovation, and dedication of our AHP community come to life. Here’s to many opportunities for impactful learning and connection!

Welcome to the spring 2024 issue of the Journal of the Association of Healthcare Philanthropy! We extend our heartfelt appreciation to all the authors who have graciously shared their time, insights, and expertise in contributing articles to this publication. Your dedication to the profession of healthcare philanthropy shines through in each thought-provoking piece, and we are immensely grateful for your commitment to advancing our field.
As we explore the diverse array of topics covered in this issue, we want to take a moment to encourage all members of the Association to consider sharing their knowledge and experiences by contributing to future editions of the Journal. Whether you’re a seasoned professional with years of experience or a newcomer eager to make your mark, your perspective is invaluable. By sharing your successes, challenges, and innovative approaches, you not only contribute to the collective knowledge of our community but also inspire and empower your peers to strive for excellence in their own work.
 Bob Nolan, FAHP, CFRE Chair–AHP Journal Advisory Council
Bob Nolan, FAHP, CFRE Chair–AHP Journal Advisory Council
Executive Director of Development
Indiana University School of Public Health
The importance of increasing the knowledge and expertise of healthcare philanthropy professionals cannot be overstated. Just as professional journals have played a pivotal role in advancing other healthcare fields, such as medicine, they are equally vital in our domain. Consider, for instance, the impact of academic journals in medicine, where groundbreaking research and clinical insights published in journals like the New England Journal of Medicine or The Lancet have revolutionized medical practice, leading to improved patient outcomes, new treatment modalities, and enhanced healthcare delivery systems.
In a similar vein, the Journal of the Association for Healthcare Philanthropy serves as a platform for sharing best practices, innovative strategies, and evidence-based approaches that drive positive change and progress in our profession. By disseminating the latest research findings, case studies, and expert analyses, we empower healthcare philanthropy professionals to navigate the complexities of our field with confidence and efficacy. Together, let us continue to harness the power of knowledge exchange to elevate the standards of healthcare philanthropy and fulfill our shared mission of improving healthcare access and outcomes for all.

The advent of Artificial Intelligence (AI) presents an unprecedented opportunity to revolutionize fund development strategies through tremendous precision and personalization. While AI ethics lay the groundwork for guiding these advancements, it is essential to recognize adhering to ethical considerations alone is insufficient.
Moving beyond the foundational aspects of ethical AI, it is crucial not only for the philanthropic sector to embrace concepts beyond Responsible AI but also to ensure the simultaneous use of Beneficial AI. Ensuring Responsible and Beneficial AI not only adhere to ethical standards but also maximize the positive
impact of AI on fund development efforts by enabling more meaningful human interactions, reducing burnout among philanthropy professionals, and creating needed efficiencies.
Equally important, this dual-lens approach to measuring AI’s impact will promote a more sustainable and vibrant future for charitable giving by prioritizing the beneficial impact of AI on the organizations we serve and on those who support our efforts.
Proactively Addressing Potential Headwinds Health foundations are at an inflection point. AI will transform the practice of securing charitable investment going forward, and organizations
that fail to embrace AI and to integrate it into their practice will fall behind.
Further, a healthcare philanthropy organization that is not actively utilizing AI to optimize its fund development efforts will be remiss in its stewardship, since failing to harness innovation is a choice to underperform relative to the organization’s potential and to fall behind.
Right now, the idea of utilizing AI to advance fund development may spark questions, raise concerns, and even create fear with key stakeholders including health executives and foundation board members. Therefore, it is essential to address uncertainty, to show stakeholders how the organization will utilize appropriate ethical guardrails, and to reassure leaders the organization will hold itself to an even higher standard of Responsible AI.
An organization’s journey toward ethical, responsible, and beneficial use of AI begins with transparent conversations with leaders to strengthen their understanding of the issues and to secure their ownership of harnessing the power AI provides to fulfill the mission more efficiently and effectively.
There is also value to formally adopting a policy articulating the organization’s commitments around Ethical, Responsible, and Beneficial AI. This will provide a shared understanding of the standards with which this valuable work will be done.
Once organizational leaders are assured integrity and donor respect will remain a centerpiece of ethical and responsible practice, the organization will be positioned to pursue the significant performance and relational benefits of beneficial AI.
The application of AI in healthcare philanthropy can dramatically shift the focus from time-
consuming administrative tasks to building deeper relationships with donors. Consider the analogy of a doctor using AI to offload routine administrative tasks, thus freeing up time to engage in face-to-face interactions with patients. This not only increases the quality of care but also the accuracy of treatment plans by leveraging AI’s data-driven insights.
Similarly, in healthcare fund development, AI can automate the segmentation of donors, predict giving patterns, and identify new donor prospects–all using information that is either already in the organization’s hands or is publicly available. This allows philanthropy professionals to spend more time engaging with donors on a personal level and crafting tailored communication that resonates with each donor’s unique motivations and interests.
Precision medicine has revolutionized healthcare by treating each patient as an individual (N=1),
Ethical AI involves designing, developing, and deploying AI systems in ways that uphold moral principles, including fairness, justice, and respect for human rights and dignity. Ethical AI serves as the underpinning framework of Responsible AI (RAI).
Responsible AI (RAI) refers to the development and use of artificial intelligence technologies in an ethical, transparent, accountable way and respects privacy and human rights.
Beneficial AI (BAI) aims to ensure that AI technologies not only meet ethical standards but also actively contribute to human welfare and societal well-being, delivering tangible positive outcomes.
with treatments tailored to their genetic makeup, lifestyle, and environment. This bespoke approach has transformed modern medicine while significantly improving patient outcomes and satisfaction. In a parallel manner, AI introduces the concept of precision philanthropy to healthcare fundraising. By leveraging data analytics and AI algorithms, philanthropy professionals can now approach each donor as an individual with unique interests, motivations, and philanthropic goals.
AI tools can analyze historical contribution data, clinical activity, and other digital footprints to create a comprehensive donor profile. This supports shifting from a transactional to a custom-tailored, relationship-based approach and enables gift officers to design and propose personalized giving opportunities that closely align with each donor’s passions, whether it’s supporting cutting-edge research, enhancing patient care facilities, or funding community health initiatives.
While the advent of precision philanthropy paves the way for innovative approaches to understanding and engaging donors, the basic concepts of AI can be overwhelming, and, in some cases, dissuade organizations from deploying this transformative technology. This generic case study illustrates how any healthcare philanthropy organization can utilize predictive and generative AI to achieve unparalleled precision and personalization in its fund development efforts.
A healthcare organization should begin its AI transformation by employing predictive AI to analyze its extensive database of donor information to support better decision-making. As the name implies, Predictive AI is singularly tuned to make predictions beyond human ability. This includes looking at and making sense
of historical contribution data, HIPAA approved clinical data, engagement metrics, and digital interactions across platforms.
“Adhering to ethical AI principles is only a start. It’s imperative healthcare philanthropy raises the bar to ensure the adoption of AI is not only ethical, but also beneficial to humanity at large.”
Predictive AI algorithms sift through this data to identify patterns, preferences, and potential donor behaviors that would not likely be immediately obvious to human analysts and would take an incredible amount of time to organize and analyze manually. For instance, predictive AI can forecast which donors are most likely to respond to campaigns focused on specific healthcare initiatives, such as research into rare diseases or the expansion of community health services. Securing these insights empowers leaders to make better strategic choices and to smartly allocate limited resources such as time, budgetary investment, or stakeholder influence.
Armed with insights from predictive AI, generative AI can be used to craft personalized engagement and communication strategies. Generative AI takes into account the preferences and interests of individual donors or donor segments to create customized content.
This could range from content personalized for individual donors–such as an email campaign that speaks directly to a donor’s history and
interests or a custom-tailored annual report–as well as content designed to resonate with the broader values and goals of the donor base–such as social media content or website copy.
For example, for donors identified as being particularly interested in innovation in healthcare, generative AI could produce tailored content highlighting the organization’s efforts in adopting new technologies for patient care or research and placing the importance of that work in a greater context.
Using predictive AI and generative AI in tandem creates the ability to not only identify the most important donors or donor segments to focus on but also enables the organization to effectively automate hyper-personalized content based on a donor’s specific interests and preferences. This significantly elevates the donor experience, enhances engagement, strengthens loyalty, and increases contributions.
The health foundation should consider and address the following issues and opportunities to create a platform for ethical, responsible, and beneficial use of AI to advance philanthropy:
• Have the Right Conversations: Ensure the nonprofit board of directors is aware of, educated on, and endorses the use of AI in fund development. As the fiduciary stewards of the organization, their ownership and support are valuable and support a culture of transparency and accountability.
• Codify Commitments: Articulate the organization’s commitment to Responsible and Beneficial AI. Outline how the organization will ensure transparency, accountability, and privacy in its AI-driven initiatives. Share why AI is essential to mission fulfillment by enhancing donor engagement to maximize charitable dollars to advance healthcare outcomes.
• Update Donor Data Governance Policies: Your data governance policies guide the management, security, storage, access, and use of donor data while also ensuring data integrity and privacy. Revisit these policies to ensure these guidelines address the responsible use of AI.
• Anticipate Donor Questions: Sophisticated donors recognize AI is increasingly part of best practice fund development. So, be prepared to answer questions from donors on how their information will be used with integrity and how their privacy will be protected.
• Continue Learning: The field is continuing to evolve, so stay curious and seek out information through reputable forums, publications, and other learning content to stay up to date on emerging issues and best practices.
• Work with Responsible Partners: Ensure data partners you work with are committed to designing and using algorithms that are fair and avoid bias and discrimination. Feel free to ask questions to understand their philosophy and approach since integrity is integral.
Donors feel a stronger connection to the organization’s mission, as the outreach they receive is highly relevant and personalized. This not only results in higher contribution rates but also fosters a deeper sense of community and advocacy among the donor base.
Further, the efficiency and effectiveness enabled by AI does not replace the fundamental relationship-building role of the philanthropy officer; rather, it supports the leader’s success by enabling them to reallocate their limited time from lower-value administrative tasks to strategic, face-to-face donor interactions to nurture authentic, values-based relationships.
Returning to the agreed upon commitments the organization and its leaders adopted at the outset, it is imperative Responsible and Beneficial AI guidelines are followed throughout each step in the AI journey to ensure transparency, accountability, and privacy in its AIdriven initiatives. By doing so, it not only adheres to ethical standards but also demonstrates the tangible benefits of AI in enhancing donor engagement and advancing healthcare outcomes. This approach serves as a model for how AI can be responsibly and effectively used in healthcare philanthropy to achieve precision and personalization, setting a new standard for donor engagement in the digital age.
As we navigate the complexities of integrating AI into healthcare fundraising, it is clear the future lies in a balanced approach where technology and human interaction complement each other. By harnessing the power of Responsible
Nathan Chappell, co-founder of Fundraising. AI, head of AI at DonorSearch AI, and coauthor of “Generosity Crisis, the Case for Radical Connection to Solve Humanity’s Greatest Challenges.”
Betsy Chapin Taylor, FAHP, chief executive officer of Accordant and winner of the Association for Healthcare Philanthropy’s Si Seymour award.
and Beneficial AI, healthcare philanthropy can achieve unprecedented levels of efficiency and precision. This not only enhances the effectiveness of fundraising campaigns but also ensures donors are engaged in a more meaningful and personalized manner.
Embracing AI as a lever to elevate the organization’s impact in a way that is ethical, responsible, and beneficial unlocks the organization’s ability both to achieve its potential and to fulfill its mission more vibrantly. AI becomes not just a tool for operational efficiency but a catalyst for fostering genuine human connections.
By embracing the principles of precision philanthropy, we can ensure every donor’s contribution is maximized toward supporting the healthcare organization’s transformative work to improve patient care, advance medical research, and elevate community well-being.
As we advance, let us remember the essence of philanthropy lies in the power of human compassion and generosity. AI, when used responsibly and beneficially, amplifies this power, and opens new horizons for healthcare philanthropy to thrive. n
By shifting the focus from honoring physicians to highlighting gratitude, results were increased nearly 9x.
By Steven L. Dasher, CFRE and Nicole T. Papst
With healthcare philanthropy’s focus on grateful patient fundraising via referral programs and direct marketing acquisition (e.g., direct mail and email appeals), many hospital foundations participate in National Doctors’ Day fundraising campaigns. Although several organizations have yielded admirable results, not all experience overwhelming success.
Authors Steven L. Dasher, CFRE, and Nicole T. Papst share their success in shifting focus from honoring physicians to highlighting gratitude.
This white paper outlines one organization’s experience in prioritizing National Grateful Patient Day over other nationally designated days reserved for fundraising that many deem
Forward Thinking article sponsored by

over-saturated, such as National Doctors’ Day, Giving Tuesday, and National Nonprofit Day.
Incorporating National Grateful Patient Day into your annual fundraising strategy may boost your results and add qualified prospects to your midlevel and major giving pipelines, while allowing your entire team to experience transformational success in curating gratitude.
Fostering ideas in a supportive environment, the Association for Healthcare Philanthropy’s Huddle frequently offers fresh ways of researching fundraising opportunities and best practices. Recently, a community discussion* showcased a healthcare philanthropy organization that was attempting to move away from their Giving Tuesday solicitation model and focus on National Grateful Patient Day, September 7. Furthering this intrigue, our Donor Relations Liaison watched an AHP-sponsored webinar where participants discussed their results and strategy around this day of giving.
After bringing this idea to our team’s attention during a planning session, we decided to integrate National Grateful Patient Day into our fiscal year plan as part of our grateful patient acquisition and sustained giving strategy. Our team prioritized these efforts over a Giving Tuesday initiative and, along with National Doctors’ Day, decided to focus on identifying and cultivating patient gratitude, rather than honoring a physician or caregiver.
These efforts included a direct mail appeal with renewal, active donor, and acquisition segments; a coinciding three-part email appeal series; systemwide collaboration through multiple philanthropy departments; and brand growth (marketing). Other components included volunteer
engagement opportunities via a phone-a-thon, major gift officer engagement with prospects, and securing a match donor opportunity.
As many organizations have recently surmised, many Giving Days often utilize flashy social media strategies and heavy use of graphic design to tell a story, but the results often do not correlate with the efforts due to an over publicization in the market.
By shifting our organization’s focus from simply recognizing a caregiver to expressing gratitude, we were able to capitalize on what is at the heart of philanthropy’s role in society: providing an authentic opportunity for someone to say thank you in a meaningful way, while making a positive difference.
More than $86,000 was raised representing 110 individual gifts. Included in these results were four major gifts received in response to direct mail appeal and a gift match opportunity provided by a hospital board member. Additionally, 10 mid-level gifts were received.
While the metric, total number of gifts, is relative to the organization’s size, our team was pleased to see how many of these were representative of new donors. Fifty-six individuals were first-time donors to our organization, and 30 individual caregivers were honored.
On National Grateful Patient Day, our team hosted board members and volunteers at our facility to make phone calls to current donors, hospital board members, and auxilians. These efforts yielded more than $7,000 and allowed our volunteers the opportunity to connect directly with grateful patient donors, and to hear their compelling testimonies firsthand.
* AHP Community Huddle, “Giving Tuesday.” September 1, 2022. Accessed May 30, 2022. https://connect.ahp.org/discussion/ giving-tuesay#bm523a9838-08ae-4f0b-916c-2c39cdc03302
The concurrent email appeal amassed more than $7,800 in the two weeks leading up to September 7.
As a comparison, our organization’s Doctors’ Day solicitations raised less than $10,000 from 97 gifts, and more than 50 new donors. While half of these gifts represented support from new donors, the gift amounts and response rate from existing donors were significantly lower than National Grateful Patient Days.
Conversely, our organization’s National Grateful Patient Day results were reflective of Doctors’ Day results for our system office foundation, which has historically had more success from a Doctors’ Day appeal. Much of this has been attributed to their utilization of a donor acquisition model employed by SHARP. However, our market has failed to achieve comparable results.
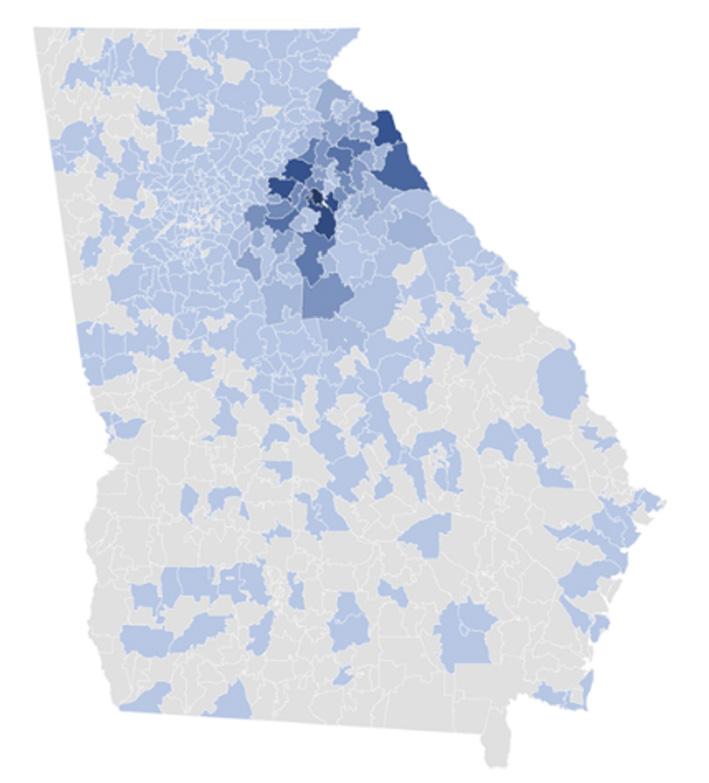
Piedmont Athens Regional is one of northeast Georgia’s largest not-for-profit hospitals and joined Piedmont Healthcare in 2016. The 427bed acute care facility serves a 17-county region with a population exceeding 607,000. The region is largely rural and centers around AthensClarke County which holds the distinction as among the poorest counties of its size nationally. Piedmont Athens Regional provided more than $204 million in uncompensated care in FY2021.
While our open rate for e-newsletters hovers just above 50%, our market hasn’t responded favorably to email solicitations in the past.
By implementing a grateful patient donor acquisition strategy and segmenting our audience by payor type (excluding Medicaid, self-pay, and charity care), patients 65+ years old, and geographically within Georgia, we were able to target a population that had previously not responded favorably. Although this strategy is similar to what we previously applied to Doctors’ Day, the notable shift is that of our message: gratitude far outweighs physician recognition.
or
helped you when you needed it most. philanthropy, we continue to transform health care and provide access to the best clinicians and one-of-a-kind experience that always puts patients first.
In gratitude,


For organizations looking to revitalize their acquisition and renewal strategies with brand alignment, National Grateful Patient Day offers an opportunity to engage with current, lapsed, and prospective donors through a marketing campaign celebrating gratitude.
Our shift in focus from honoring a caregiver with a gift to expressing gratitude for care increased our annual sustained giving results by 174%. These efforts were not simply a direct mail solicitation, but encompassed an email solicitation, major gift strategies, volunteer engagement, and an all-around full team effort including hospital and board leadership. n
Steven L. Dasher, CFRE, is executive director at Piedmont Athens Regional Foundation. As the organization’s leader, Steven has been building the team and refocusing its goals to better align with Piedmont Athens Regional’s overall strategy. This includes prioritizing major giving, implementing a sustained giving program, highlighting patient gratitude, increasing board member engagement, and eliminating underperforming fundraising events.
With his background in major giving, Steven has experience creating meaningful philanthropic opportunities for individuals, corporations, and foundations.
Nicole T. Papst is manager of sustained giving at Piedmont Athens Regional Foundation. In this role, Nicole oversees direct mail renewal and acquisition, manages employee giving, and leads grateful patient strategy.
As a fundraising professional with experience building a robust pipeline through sustained giving, Nicole enjoys creating strategies that will enhance fundraising goals and optimizing donor database management to improve tracking and analytics.


is designed to bridge a crucial gap in grateful patient and family fundraising by enhancing engagement with clinical partners. The essence of our program lies in addressing a common misunderstanding that often arises when we ask clinical partners to identify potential donors among grateful patients and families. Typically, clinical partners are advised to look for expressions of gratitude. However, the challenge surfaces because the notion of “gratitude” varies significantly between development teams and clinical staff.
For clinical partners, gratitude is perceived in its most basic form—an expression of thanks. This might include gestures such as hugs, handshakes, or verbal appreciation, which, while meaningful, don’t always signal a willingness to engage in philanthropic support. Development professionals, on the other hand, seek to identify patients and families who wish to extend their gratitude through philanthropic donations or other forms of support.
This difference in interpretation can lead to confusion and a disconnect, hindering the involvement of clinical partners in the referral process. Our Beyond Gratitude program aims to clarify this distinction, ensuring that clinical partners understand that we’re looking for signs of individuals wanting to contribute beyond a simple thank you.
That’s why our Beyond Gratitude program is unique in its foundational approach of providing clear guidelines for identifying potential donors among grateful patients and families that are looking to do more than say thank you— those seeking to go Beyond Gratitude. Our approach eliminates uncertainty and fosters a more productive partnership between clinical and development teams.
Beyond Gratitude is about unlocking the full potential of gratitude and transforming it into meaningful support for your cause. Let us help you create clarity and find those grateful patients and families that are seeking to go Beyond Gratitude.
To learn more, visit www.grahampelton.com/healthcare
How the gift of time and attention can lead to long-lasting and productive careers in philanthropy.By Sarah Fawcett-Lee, FAHP, CFRE, and Stephanie Foster
Ask any new major gift officer what weighs on them the most, and the answer will most likely be “my lack of confidence” or “I’m nervous about asking for major gifts.”
These are two of the most common responses students in the Madison Institute’s Elements of Major Gifts track express year after year. They openly share how unsure they feel about themselves and the major gifts process, and they thirst for help and guidance. Their lack of confidence is easy to attribute to inexperience, and there’s a lot that can be done to support
gift officers of all levels while they learn on the job. This requires their leaders to give the gift of time and attention, so gift officers can get the individualized help needed to be successful.
Newer gift officers may struggle to get a foothold not only because they are venturing into unfamiliar territory, but because of a lack of understanding of the big picture.
In today’s complex healthcare environment, it can be hard to grasp hierarchies and matrixed reporting, internal politics, institutional culture,
and how the demands and pressures on clinical and administrative colleagues can impact the work of the philanthropy team. A guiding hand is therefore vital.
Major gift fundraising is both an art and a science.
Being good at major gift fundraising requires a balance of strategic and nuanced thinking, strong time management and organizational skills, and an ability to create genuine connections with diverse groups of people.
Yet, how many gift officers fit that description? While one gift officer may struggle to manage and prioritize a burgeoning portfolio, another may need to refine and practice the words they use to engage clinicians as partners, or to advance relationships with potential philanthropic investors.
A gift officer may be extraordinarily talented in developing relationships but may lack organizational skills or be a poor strategist. Whatever the case, becoming competent in both the art and the science of major gift fundraising can be a long journey.
Motivated gift officers want to grow and thrive and have the tools they need to be successful. Managers who are genuinely interested in nurturing gift officers can help them avoid spinning their wheels, getting nowhere, and eventually giving up because they think it’s too hard, too scary, or too lonely to proceed.
Nobody wants to see talent go to waste. So, how can leaders support gift officers better?
Gift officers thrive when they have access to high-level information that will provide direction and context. Philanthropy leaders can elevate a gift officer’s ability to function by sharing news about the programs and service lines they are working with, as well as explaining any current
challenges or important strategic priorities for the health system.
Making sure gift officers are well-informed demonstrates trust and can boost morale. Gift officers will feel appreciated and empowered, which in turn can increase confidence.
And it also can keep gift officers safe from unintentionally doing or saying something that might hamper progress.
In healthcare philanthropy, we spend so much time building partnerships with colleagues across our health systems–including with nurses, clinicians, and administrative leaders–it only makes sense to ensure the entire philanthropy team can surefootedly navigate a complex environment. Arming gift officers with knowledge can help them align their efforts and have the greatest impact for the programs and initiatives they support.
Where possible, give gift officers a seat at the table when big topics are being discussed. For example, senior philanthropy leaders can include other members of their team in meetings with hospital presidents, service line leaders, physician leaders or trustees so they can listen and learn.
Exposing gift officers to these experiences will be an essential part of their growth as future leaders. By doing all this, senior leaders can elevate the gift officer and emphasize their significance in the organization.
Being a gift officer can be intimidating and so having the support of their peers is vitally important. From one-to-one meetings to group conversation—there are many ways to ensure new gift officers have a sounding board for ideas and can learn from others.
• Moves Meetings: For busy teams, the most efficient way to talk about prospects and portfolios is during moves meetings. However, these may not be the best venue for newer
gift officers to make themselves vulnerable and ask for advice and input.
Too often, moves meetings become “reporting out” sessions with little dialogue or inquiry. The need to get through long lists of prospects can feel like a housekeeping exercise and is not beneficial to gift officers who are trying to figure out thoughtful action steps for their prospects.
However, there are ways to structure moves meetings to draw out more discussion. Asking each gift officer to bring one or two prospects they’d like to discuss, and then inviting the whole team to listen and weigh in, can turn an everyday moves meeting into a learning lab where participants walk away with plans they can execute, and feeling enthused and inspired.
• Roundtables: If there are enough gift officers within the organization, creating a monthly virtual or in-person roundtable or idea sharing platform can provide high quality peer-topeer coaching and support. Roundtables are especially valuable if gift officers are spread out geographically and don’t see each other regularly. AHP has recently launched gift officer roundtables for its AHPrime members, which will allow people from around the country to connect with one another.
• Professional education and networking: With the abundance of virtual and inperson educational resources on offer through professional associations and consulting firms, taking advantage of webinars, publications, conferences, and seminars is often affordable and convenient. Attending educational programs is time and money well spent, even
if it means being away from the office. For example, spending a week at the Madison Institute can boost a gift officer’s productivity far better than a week of sitting at a desk, feeling stuck.
• One-to-Ones: Focused one-to-one meetings can make a huge difference in the daily work of gift officers and can build trusting relationships between the supervisor and supervisee. Using an intentional approach – free from distractions—can be effective, productive, and supportive.
These meetings allow for regular, meaningful conversation that can boost engagement. Managers should do everything they can to protect one-on-one appointments on their calendars, which sends a strong message that this time is valued.
One-to-one meetings provide a private and confidential setting to bring up and discuss challenges, and to uncover the root cause of issues. Delving into these topics can help leaders know where they might need to step in to remove barriers, clarify strategic priorities, and understand where they need to pay attention and provide support.
• Coaching: Listening and responding to gift officers, and giving them individualized attention is, essentially, coaching. Leaders who invest time in developing their team’s skills are filling the role of “coach.”
The International Coaching Federation (ICF) defines coaching as a thought-provoking and creative process that helps an individual maximize their personal and professional potential. In the relationship between a senior philanthropy leader (the coach) and a gift officer, the coach listens, identifies needs, and helps develop action plans.
Not all managers are great coaches, but there are ways to make up for this. Using all the tactics listed above, or tapping outside resources, can go a long way to developing gift officers who will have productive careers—and who can become the next generation of healthcare philanthropy leaders.
The Role of the Philanthropy Leader/ Supervisor
Effective leaders bring out the best in their team and inspire them to do more than they imagined possible. To do so, it’s important for the healthcare philanthropy leader to:
• Remove obstacles and protect the team.
• Set vision and direction.
• Ensure that gift officers are spending their time and energy in the right places.
• Identify the programs and service lines to focus on, and open doors to those clinicians.
• Frequently check in with gift officers to monitor progress and trouble shoot.
• Provide a listening ear for clinicians and respond to their needs at a leadership level.
• Help the gift officer identify their own strengths and weaknesses, and coach them accordingly.
• Reduce on-the-job stress for the gift officer, so they can be more relaxed and natural in their interactions. Putting too much pressure on gift officers can trigger behaviors that are counterproductive and can lead to unhappy donors and philanthropy partners. A happy gift officer who finds joy in their work is more likely to get results.
• Make sure gift officers can have some early wins. Balance their portfolio with a mix of loyal donors and new prospects so that the gift officer can have a range of experiences—from renewing gifts from current philanthropic partners, to qualifying and cultivating new prospects.
• Hold gift officers accountable through clear and realistic metrics but give grace when the going is tough.
For gift officers to really succeed—especially if they are new to the field or job function—it’s important for them to get focused feedback and coaching. When there’s no investment of time and attention, gift officers may be able to get by, but they won’t learn how to thrive.
The gift of time and attention should be a top priority for leaders, no matter what else is on their plate. Their primary function, after all, is to manage others. There are so many resources available that even busy leaders can ensure their team is being enriched. Putting in effort in this way can yield greater engagement, performance, retention—and ultimately drive results. n
• Be ready to show up and support the gift officer, such as attending clinician meetings or retreats, helping to educate and engage new clinician partners, or publicly validating the gift officer and the work they are doing.
Sarah Fawcett-Lee and Stephanie Foster spent a decade working together at health systems in Baltimore, Maryland–first at Mercy Medical Center, and then at MedStar Health.
Sarah Fawcett-Lee, FAHP, CFRE, is senior vice president and chief philanthropy officer at Virtua Health–the largest healthcare provider in southern New Jersey. She has spent her entire career as a professional fundraiser, including more than two decades in healthcare philanthropy. Most recently, she served as regional vice president at MedStar Health based in Maryland, where she was a member of the philanthropy executive team. Sarah was integrally involved in developing MedStar’s progressive grateful engagement program. Previously, she was vice president for philanthropy at Mercy Health Services, and director of major gifts at Sheppard Pratt Health System—both located in Baltimore.
Sarah earned a master’s degree from the College of William and Mary in Virginia, and a bachelor’s degree from the University of Hull, United Kingdom. She is a past president of the Association of Fundraising Professionals, Maryland Chapter, and has been a faculty member and assistant dean of the Madison Institute, an annual certificate program offered by the Association for Healthcare Philanthropy, since 2014.
Stephanie Foster is the founder of Fostering Philanthropy, where she provides coaching to major gift officers working in healthcare philanthropy. Stephanie has spent more than 30 years as a fundraising professional, and she has been both a coach and mentor for the last decade.
Before opening her firm, Stephanie was assistant vice president for philanthropy at MedStar Health, and director of major gifts at Mercy Medical Center—both in Baltimore, Maryland. At each of these organizations, she built robust grateful engagement programs, resulting in hundreds of impactful philanthropic investments from patients and families.

Physicians are high value partners to healthcare foundations who bring unique credibility, earned trust, and influence that ideally positions them to foster or deepen connections with patient and family donors. However, many healthcare organizations do a poor job selecting potential partners, which impedes their ability to maximize the impact of these valuable relationships.
Challenges largely stem from utilizing a selection framework that doesn’t align with what positions a physician to be successful and that is not responsive to what adds value in a donor relationship. To significantly elevate the impact of physician partnerships, it is essential to recalibrate
the selection of physician partners to align with what scientific studies and on-the-ground anecdotal evidence shows is most effective.
Many health foundations start their search for physician partners with the wrong mindset. They tend to focus on positions, titles, and clinical outcomes rather than elements that support vibrant partnership.
For example, a physician may be chosen based on being a member of the foundation board or serving as chief of staff of the hospital. While these characteristics demonstrate interest in the healthcare organization, they do not indicate
having the competencies, characteristics, or commitments to successfully fostering gratitude-based partnerships with potential donors.
Other times, physicians are chosen based upon exceptional clinical outcomes; however, someone can have deep scientific knowledge, surgical acumen, or other competencies that lead to great clinical outcomes while the same physician simultaneously demonstrates poor bedside manner or a disregard for the importance of personal relationship quality.
Finally, a physician may be both committed to the organization and have great interpersonal skills but have no alignment with the current philanthropic priorities of the healthcare foundation. Physicians are hamstrung in the ability to help when strategic priorities are not within their area of clinical practice or, frankly, consistent with what they deeply care about.
Optimizing physician selection begins with having a framework that places a primary emphasis on two things:
1. Harnessing the power of alignment between the physician’s expertise, interest, and the foundation’s current strategic funding priorities.
2. Embracing the power of interpersonal skills that foster gratitude, trust, and commitment.
High-impact philanthropy focuses on raising philanthropic funds exclusively for initiatives that are already embedded in the healthcare organization’s strategic plan, master facility plan, Community Health Needs Assessment (CHNA), and similar organization documents.
Through alignment, philanthropy is directed toward its highest and best use and is positioned to achieve the greatest impact. It naturally follows organizations should focus on
identifying physician partners whose area of clinical expertise align with the strategic funding priorities. This brings a variety of benefits:
• Securing the partnership of physicians who work within the supported clinical service line means they are best positioned to engage grateful patients and family members who have a high affinity for the case because of personal experience.
• Having an intimate understanding of the clinical work to be advanced enables a physician partner to provide expert input on the clinical case for support. Case development is also a perfect entry point to engage a physician by giving them an opportunity to share insights about a project they are passionate about while giving the philanthropy professional an opportunity to build rapport.
• Engaging physicians as advocates and expert storytellers brings credibility to the project with donors. There are valuable opportunities for physicians to share funding needs with broader audiences through board education and friends events. This provides physicians with an opportunity to gain exposure and to build a community reputation and patient base, so these education opportunities are a win-win.
• Collaborating to fund initiatives in which the physician has a mutual personal and professional interest in success elevates a physician’s ability to better serve their own patients and creates a strong incentive to help. Additionally, at a time when healthcare net operating margins only achieved a median of 1.2% last year, hospitals find dollars to reinvest in the organization tighter than ever.1 Physicians are deeply aware of the scarcity of capital, and many physicians see partnering with philanthropy is possibly the only path forward to get needed funding in the current fiscal landscape.
Ultimately, building toward having a physician partner that philanthropy leaders know and trust opens up the possibility to make them part of a prospective donor visit. When a physician is in a visit, they bring a level of credibility to the case that cannot be duplicated by other partners.
When a physician directly shares the impact philanthropy will have on patients and on their own practice, donors often express deep gratitude for the time the physician has taken to be with them and provide higher levels of charitable investment.
At CHI Memorial Foundation in Chattanooga, Tennessee, the positive impact of alignment between the philanthropic case and physician expertise has been clear. In their last two comprehensive capital campaigns, the foundation used a structure partnering a community leader with a physician leader at every level.
Each campaign was divided by campaign project rather than gift level, so, for example, a cardiac leadership team worked to achieve a specific goal for their portion of the campaign. With this focus by service line, the foundation was able to deeply engage physicians passionate about funding the project.
Both community leaders and physicians have been positively surprised by the synergy and significant success resulting from this collaboration. In the campaign quiet phase, CHI Memorial utilized physician partners in approximately 75% of donors visits—all focused on six-figure and above gifts.
In the first three months of the campaign, 100% of asks involving a physician in person with the prospect resulted in a gift. The campaign had a $15M goal over 24 months and completed with $17M raised in 18 months.
Patient and family gratitude is most often the
linchpin in a patient–physician relationship that prompts the desire to give, and gratitude is fostered by physician behaviors and commitments. Gratitude in the care environment begins when a clinician anticipates, recognizes, and responds to a patient or family member’s needs, wants, or concerns. This “perceived benefactor responsiveness” is a “significant and strong” predictor of gratitude.2
A physician can exceed a patient’s expectations by addressing social and emotional dimensions of care that make a patient feel seen, understood, validated, or cared for. Gratitude also hinges on the perceived effort and intentions of the physician rather than the physician’s expertise, credentials, or skills.3 Given a physician’s perceived efforts and intentions are key to fostering gratitude, there is merit in considering what patients perceive as the characteristics or commitments of a “good doctor.”
Patients have a basic expectation that a physician will have medical knowledge, skills, and experience and that a physician is competent, ethical, and calm under pressure. None of those elements play a meaningful factor in strengthening relationship quality.
However, dozens of studies show patients prioritize those elements that strengthen the quality of interpersonal relationship between the patient and physician and that reflect an inherent value for human beings. For example, patients want a physician to know them as a person and to show sensitivity to their emotions.
Beyond simple recognition, patients repeatedly prioritize five specific relational behaviors that reflect a value for human beings:
• Love for people demonstrated through compassion and respect.
• Kindness reflected through friendly, cheerful rapport that puts patients at ease.
• Attentive listening that aims to understand.
• Communication that is clear, understandable, honest, and polite.
• Presence showing one is engaged, interested, attentive, and available.4,5,6,7,8
High quality relationships between physician partners and patients can also be invaluable in fostering trust. When physicians fulfill patient expectations of the “good doctor” through love, kindness, listening, communication, and presence, it provides a catalyst not only for gratitude, but also for trust.4,9
At a time when trust in healthcare organizations has been dwindling, an American Board of Internal Medicine Foundation study found the public indicates a deeper sense of trust in physicians (84%) than in hospitals (72%) or in the healthcare system as a whole (64%).8
Given that 69% of donors say that trust is essential to their decision to give, engaging physician partners who can also bring a halo effect of trust offers significant value.10 Further, donor trust acts as a significant predictor of donor relationship commitment.11
Engaging physicians who embody the emotional and social dimensions of relationship quality allows a physician to do far more than just presenting the clinical case or the need for funding.
Recently, at CHI Memorial, a key physician partner met with an important prospect for the current capital campaign. This physician is an incredibly talented clinician and serves in a system leadership role. However, beyond those credentials, he also has a personal demeanor and a level of commitment that sets him apart. He is soft spoken, thoughtful, and kind and is a significant donor himself.
In advance of the meeting, the physician received a plan for the meeting along with background information on the prospect. However, the physician did more than just read it. He took the time to put himself in the prospect’s shoes and to seek to better understand the prospect, his business, and his interests as well as to uncover personal connections to the prospect’s partners.
During the meeting, the physician not only illuminated his understanding of the prospect but also demonstrated compassion and attentiveness. This resulted in the prospect engaging at a much higher level including furiously taking notes and asking probing questions. The physician’s strong emotional intelligence and acumen in building strong interpersonal relationships made all the difference in securing the prospect’s engagement and commitment.
Harnessing the power of relationship quality can also set a virtuous circle in motion. When physicians foster positive interpersonal relationships with patients, it leads to patient expressions of gratitude and loyalty that in turn support physician well-being and joy in work that in turn inspires the continuance of highquality relationships.12
Beyond the financial impact of engaging physicians in advancing mission, fostering true partnerships with physicians can also reduce burnout, decrease emotional exhaustion, and bring joy and meaning to physician partners–which is of great significance at a time when 49% of physicians say they are burned.13
This circular effect of personal relationships leading to patient gratitude that then fuels the physician’s own joy and mission is exemplified in a recent story. At CHI Memorial, a cardiologist connected the foundation to a patient who ended up making a $2.5 million gift in his honor.
When asked how he felt about the gift being made in his honor, the physician said, “It was humbling and ultimately inspired me to do more for our patients and for the community.”
The physician not only is well on the way to fully funding a program that is deeply meaningful to him but also has earned tremendous respect and accolades from his partners. Further, gratitude went both ways: the patient’s gratitude for the physician spurred a significant gift which, in turn, reignited the joy, purpose, and passion of the now grateful physician.
As healthcare philanthropy organizations continue to prioritize physician partnership as a lever to success, it is invaluable to create a framework to guide efforts to identify optimal partners.
As a philanthropy leader, engaging physicians in philanthropy can be one of the best parts of your work, but it’s also work to be undertaken thoughtfully to ensure the philanthropy organization has forged meaningful, productive partnerships with a portfolio of physicians who bring varying clinical expertise, strengths, skills sets, and personalities in order to match the right physician with the right donor for the right project.
Creating the perfect team and knowing how physicians and donors will respond to each other is a complicated puzzle that requires a philanthropy leader to be part development
Jennifer W. Nicely, CFRE, is the Foundation president for CHI Memorial in Chattanooga, Tennessee, and vice president of philanthropy for the southeast region of CommonSpirit Health. She has been an AHP member since 1998. In 2021, Jennifer was the inaugural recipient of the CommonSpirit Health Philanthropy Values Award. She can be reached at Jennifer_nicely@memorial.org.
Betsy Chapin Taylor, FAHP, is chief executive officer of the philanthropy and governance consulting firm Accordant. She has been a member of AHP since 1995 and is a former recipient of AHP’s Si Seymour award. She can be reached at Betsy@AccordantHealth.com.
officer and part psychiatrist. However, the journey always begins with a thoughtful, deliberate process to engage the right physician partners in the first place: physicians whose area of clinical expertise and interest align with the case for philanthropic support and whose interpersonal relationship building skills include demonstrations of a love of humankind, kindness, listening, communication, and presence.
This two-pronged approach provides a solid start on the process that can then be supplemented with additional considerations to further refine physician selection and to take physician relationships even further. n
1. KaufmanHall, National Hospital Flash Report, January 2024, https://www.kaufmanhall.com/sites/default/files/2024-01/KHNHFR_2024-01.pdf.
2. Emotion; American Psychological Association, 2012 vol 12 no 1 163-168, Gratitude When It is Needed Most: Social Functions of Gratitude in Women with Metastatic Breast Cancer, Sara B. Algoe, Annette L. Stanton.
3. Watkins PC. Gratitude and the Good Life: Toward a Psychology of Appreciation. Dordrecht, Netherlands: Springer Science + Business Media; 2014. DOI: 10.1007/978-94-007-7253-3, p 45-47.
4. Schattner A. Can Humanism Be Infused Into Clinical Encounters in a Time-Constrained, Technology-Driven Era? Cureus. 2022 Aug 9;14(8):e27836. doi: 10.7759/cureus.27836. PMID: 36106258; PMCID: PMC9458938.
5. Borracci RA, Álvarez Gallesio JM, Ciambrone G, Matayoshi C, Rossi F, Cabrera S. What patients consider to be a 'good' doctor, and what doctors consider to be a 'good' patient. Rev Med Chil. 2020 Jul;148(7):930-938. doi: 10.4067/S0034-98872020000700930. PMID: 33399677.
6. Steiner-Hofbauer V, Schrank B, Holzinger A. What is a good doctor? Wien Med Wochenschr. 2018 Nov;168(15-16):398-405. doi: 10.1007/s10354-017-0597-8. Epub 2017 Sep 13. PMID: 28905272; PMCID: PMC6223733.
7. Shippee ND, Shippee TP, Mobley PD, Fernstrom KM, Britt HR. Effect of a Whole-Person Model of Care on Patient Experience in Patients With Complex Chronic Illness in Late Life. Am J Hosp Palliat Care. 2018;35:104-9. Epub 20170129.
8. Surveys of Trust in the US Health Care System, American Board of Internal Medicine Foundation, May 21, 2021, p. 20, https://www. norc.org/content/dam/norc-org/pdfs/20210520_NORC_ABIM_Foundation_Trust%20in%20Healthcare_Part%201.pdf).
9. Huang CH, Wu HH, Lee YC, Li L. What Role Does Patient Gratitude Play in the Relationship Between Relationship Quality and Patient Loyalty? Inquiry. 2019 Jan-Dec;56:46958019868324. doi: 10.1177/0046958019868324. PMID: 31422704; PMCID: PMC6700843.
10. Give.org, Donor Preferences Across Household Income Brackets 2023, https://give.org/docs/default-source/donor-trustlibrary/2023_fallwinter_dtr_report_final.pdf.
11. Shabbir, Haseeb, Palihawadana, Dayananda, Thwaites, Des, 2007/03/01, Determining the antecedents and consequences of donor-perceived relationship quality—A dimensional qualitative research approach, Psychology and Marketing.
12. Layous K, Nelson SK, Kurtz JL, Lyubomirsky S. What triggers prosocial effort? A positive feedback loop between positive activities, kindness, and well-being. J Posit Psychol. 2017;12:385-398. doi: 10.1080/17439760.2016.1198924.
13. Medscape Physician Burnout and Depression Report 2024, January 26, 2024, https://www.medscape.com/slideshow/2024-lifestyle-burnout-6016865.

The future of philanthropy is likely to rely more and more on technology, but there are marginal returns to consider in the seemingly ever-expanding and increasingly expensive application marketplace. Keeping up is a challenge, as is funding in these turbulent financial times that many hospitals and systems are experiencing. Doing nothing about tech trends is not wise, but neither is jumping on every bandwagon or buying every shiny object. Making wise choices with our scarce resources is critical. In light of all of this, preparing for the technological future will help allow for more fundraising and engagement.
Exploring the future state of fundraising operations has been a common topic for me
in the last few decades. I have had the good fortune of helping dozens of the world’s leading health systems, academic medical centers, and children’s hospitals as they implement new technology. In 2023 and 2024, three technology leaders and I had been discussing the technology trends, tips, and tricks hurtling toward the sector.
Julia Gallagher, vice president of development information strategy and operations at Memorial Sloan Kettering, Will Curtis, system vice president, tech and innovation at CommonSpirit, and Matt
FROM STAGE TO PAGE:
This article was adapted from a live presentation given at AHP’s International Conference in September 2023.
Turkington, chief operating officer, at Providence Health Philanthropy, and I presented our thinking at the 2023 AHP International Conference. That session helped shape how I think about preparing for the future, starting with two nuanced realities.
On the one hand, the fundamentals sometimes remain elusive. Great tech requires data governance and quality. Accurate, complete, and timely reporting is the best indicator of a healthy tech ecosystem. Efficient processes start with behavior, not tools. Too many in the sector do not yet have mastery over the fundamentals, and all technology futures start with a strong foundation.
On the other hand, there are clear signs that technology’s role is increasingly important. Of course, we hear about artificial intelligence, AI, daily; this is an elegant technology that is increasingly important to our future. We also see more emphasis on the importance of data in decision-making and relationship-building.
Five years ago, the buzzword was CRM, as establishing a constituent relationship management system was on every leader’s mind. Five years before that, BI was the future. In these cases, these buzzwords became standards. This is because great technology that is well implemented can make us more efficient and effective, especially with high-volume activities.
More data and access, though, means more privacy protection in the healthcare sector. These issues are interrelated. Understanding these intertwined trends is vital for success and three such issues are the most relevant for philanthropy technology.
Gallagher, Curtis, Turkington, and I arrived at three tech trends that every team needs to tackle in the coming years—consumerization, computation, and compliance. Just as no
philanthropy systems team can tackle everything all at once, we acknowledge that these issues are both interrelated and not exhaustive. There are dozens of smaller or related trends that warrant exploration, but these “Three C’s,” we think, will become standards soon, too.
For over a decade, I have been writing about “the iPhone problem.” The problem is not that iPhones are somehow bad. On the contrary, they are so good that they ruin our work experience. In your pocket or next to your laptop, you have a powerful tool that helps you look up the weather, deposit checks (or transfer money to Venmo), keep up with friends via social media, laugh at kitty cats on TikTok, and on and on. Oh, and it’s your phone. And, then you head into the office, fire up the old (probably literally) work computer, and Bammo!, it’s 2007 on your screen.
Some shops have made the transition to modern technology stacks, of course. However, even the best philanthropy tech shops tend to be behind the curve compared to what is new and useful in the market.
But wait, there is some hope here. What once was certainly a 10+ year gap between our consumer lives and our work environments has been shrinking. The move to the Cloud for Software-as-a-Service tools is promising. Many are moving from a “database of record” to something closer to a real CRM ecosystem. We are starting to benefit from the availability of technology used in Fortune 100 companies with the major platform companies like Microsoft, Salesforce, and Google. Real-world BI tools like PowerBI or Tableau are increasingly available and affordable for the sector.
The key for your team is to manage expectations and adopt prioritized tech with a proven record of delivering results. Once planning and expectations are in hand, the next step is to press for more realistic funding and budgets for new, more consumer-like tech. As with most
nonprofit organizations, the typical healthcare team is underfunded. If funding does not support the vision for new technology, teams need to identify the gaps and persuade leaders to fill them.
Coined in 1965, Moore’s Law stated that the number of transistors in an integrated circuit doubled every two years, meaning that computing power (and data storage) roughly doubled every two years. Moore’s Law means that capacity has grown in parallel. Now, the power to compute complex algorithms or the storage needed to save every online click and page view have become readily available for more and more in healthcare philanthropy.
For philanthropy trends and analytic computations, the tech and tools have never been better. The innovations that Gallagher, Curtis, and Turkington are achieving with more and more capacity are impressive. Memorial Sloan Kettering (MSKCC) models donor behavior every day. Providence handles 25,000+ grateful patient records each day. CommonSpirit leverages its technology to manage dozens of fundraising teams around the country. Many others are diving deeply into the power behind Generative AI to aid work and outcomes in many ways.
The trick with this computational power is making it relevant and contextual. Data for data’s sake does not help an organization raise more money. Shoddy analytics can miss the right perspective about donor behavior. In statistics, a spurious correlation looks causal but is not; for instance, when your AI model tells you that your best future donors are your current donors, you haven’t learned much.
Too many models in the market suffer from this sort of substantial endogeneity, whereby the explanatory power of regression analysis is essentially tautological or unrelated. And no matter how powerful a model may be, if it
does not accommodate context, much of the analytics will be wrong upon closer inspection.
The most effective shops treat computational efforts as directional, not necessarily true. The more you can persuade your team that your analysis points them in the right (but not exact) direction for the next step, the more you will generate from your technology ecosystem.
With great computing power comes great responsibility…for the security of that data! Compliance in philanthropy technology means that data are secure, HIPAA, PHI, PCI, and related regulatory standards are upheld, and permissions and architecture are complete. Too many shops know the cost of a major breach in their data. Illustrating that your team did everything in its power to protect your data could be the difference between your team gaining or losing the confidence of your board, your systems users, and your constituents.
Part of compliance involves the actual steps taken, audits made, and regulations followed. Allowing for email opt-outs, for instance, aligns with the CAN-SPAM Act and is just good business. The appearance of careful practices and policies is also important. The reality is that most “controls” in the system can be readily overcome. However, doing everything according to the guidance in the industry is a healthy strategy that should keep your organization out of trouble.
Emphasis on compliance can also be useful for your team’s growth and future. While visiting a colleague in March, he told me that he has started to “put the word ‘Compliance’ in job titles” for those in gift processing because it has allowed for greater authority and better salary bands for these staff members. If you are not yet on the compliance train, data and technology governance should be your first stop. Great policies are the foundation of strong compliance. And, while it may be wise to be cautious, being
unnecessarily conservative will negatively affect your fundraising.
As with anything in the technology ecosystem, there is too much to know and do to fully prepare for the future, much less predict it. One cannot do or know it all. But each of us can start by doing the next right thing. If your philanthropy technology ecosystem future seems murky, overwhelming, or out of control, you can take steps today that will shape your environment.
Start with the fundamentals. Do you have policies and procedures for your technology and data? If not, start there. Then establish data and technology governance and the truth about your data—how accurate and complete is that data you have and what data do you need. With these fundamentals, use the governance framework to prioritize technology spending.
If technical debt—that is, costs associated with maintaining aging or inefficient systems—is a problem, start to build the business case(s) to persuade the board to fund improvements. Does your team use the system and trust your data? No amount of fancy new tools can overcome an environment with low confidence among its users.
Once you have a solid foundation, listen to stakeholders about their needs and determine what your team can handle. Remember that their expectations are now set by Apple, Google, and Amazon. This means you need to get creative in managing the gap between wish lists and budgets. Start by asking “What is low effort and high impact?” Do those things quickly, get some wins under your belt, and use the new-found confidence and trust to negotiate expectations.
Chris Cannon is the chief strategy officer at Zuri Group, a firm focused on philanthropy technology, operations, and strategy.
Cannon’s work has included authoring two fundraising books, writing AHP, CASE, AFP, and APRA articles, presenting at dozens of conferences, and counseling hundreds of clients. You can learn more about Chris at www.zurigroup.com/chris-cannon.
This article was improved via ongoing discussions with Julia Gallagher, vice president of development information strategy and operations at Memorial Sloan Kettering, Will Curtis, system vice president, tech & innovation at CommonSpirit, and Matt Turkington, chief operating officer, at Providence Health Philanthropy.
For initiatives that are high effort and high impact, like comprehensive digital transformation efforts, start planning now. For the other options—high effort/low impact and low effort/low impact—do your best to ignore them where possible.
Finally, decide where your team will land on consumerization, compliance, and computation. You might be a thoughtfully cutting-edge shop, or you might purposefully lag behind. The crucial decision is to be planful—establish a data and tech governance environment, pick your new tech wisely as you retire technical debt, and always align your tech choices with your mission and your donor’s experiences.
And always remember that technology is a means to an end. If the neat new philanthropy tech thing doesn’t help you raise more money and build better relationships, move on to the next opportunity. n


Beyond Gratitude™ is the only grateful patient fundraising model developed from individual coaching sessions with more than 2,500 doctors, nurses, and clinical professionals.
grahampelton.com/ beyond