

Gut Reads
Gut Reads
GI Books by
GI Authors
GI Books by GI Authors
ACG POSTGRADUATE COURSE Attend an upcoming
2024
2024 ACG’s Functional GI and Motility Disorders School & Southern Regional Postgraduate Course
December 6–8, 2024
Renaissance Nashville Hotel, Nashville, TN
2025
2025 ACG’s NEW Esophagus School & Western Regional Postgraduate Course
January 24–26, 2025
Mandalay Bay, Las Vegas, NV
2025 ACG’s IBD School & ACG/FGS Annual Spring Symposium
March 7–9, 2025
Naples Grande Beach Resort, Naples, FL
2025 ACG/LGS Regional Postgraduate Course & Women Leading with Guts Course
March 14–16, 2025
DoubleTree by Hilton, New Orleans, LA
2025 ACG’s Endoscopy School & Eastern Regional Postgraduate Course
June 6–8, 2025
Washington Marriott Metro Center, Washington, DC
2025 ACG’s Functional GI and Motility Disorders School & Midwest Regional Postgraduate Course
August 22–24, 2025
Marriott Indianapolis Place, Indianapolis, IN
2025 ACG’s NEW Esophagus School & ACG/VGS/MASGNA Regional Postgraduate Course
September 5–7, 2025
Williamsburg Lodge, Williamsburg, VA

ACG Weekly Virtual Grand Rounds
REGISTER NOW: gi.org/ACGVGR
Plus our monthly webinar series focused on career-based topics!



FEATURED CONTENTS
TRAINEE HUB
Dr. Alicia Muratore and Dr. Eric Shah interview Dr. Sachin Jain to glean essential lessons for GI fellows on leveraging nonfinance business skills when delivering clinical care.
PAGE 15
GUT READS: GI BOOKS
BY GI AUTHORS
Reviews of recently published consumer-friendly GI books by GI authors, and recommended non-GI reads from ACG leaders and rising stars.
PAGE 19
ACG PERSPECTIVES
GI advanced practice providers share a glimpse of what their "typical day" looks like.
PAGE 37

ACG members and GI practices continue to face mounting financial and reimbursement pressures. Complex coding and documentation requirements only add to these burdens. The ACG Practice Management Committee is pleased to announce the new member benefit: professional coding and documentation assistance for ACG members, tailored to your individual practice’s questions and needs.

Arlene Morrow, CPC, CMM, CMSCS, is now available to answer your questions!
ACG members will receive an answer and guidance within a few business days.


“What’s even better is inviting people who have never tried your culture’s meals before, and seeing the delight in their eyes as they take their first bite ” —Joseph Sleiman, MD, "Culinary Connections: Fusion
of Flavors for Fall" PG 31
6 // MESSAGE FROM THE PRESIDENT
Dr. Jonathan Leighton on the importance of the human experience in medicine
7 // NOVEL & NOTEWORTHY
Recent member accomplishments, ACG resources for education and grantwriting, community outreach efforts, in memoriam remembrances & more
8 // GI EYE
A tribute featuring photos taken by the late Michael Gallitelli of the ACG extended family
15 // TRAINEE HUB
Guidance for GI fellows on bringing nonfinance business skills into GI practice
19 // COVER STORY
GUT READS: GI BOOKS BY GI AUTHORS
GI physicians review recently published books by GI authors, plus recommended reads on non-GI topics from ACG leaders and rising stars
31 // ACG PERSPECTIVES
31 CULINARY CONNECTIONS
ACG foodies share a fusion of flavors for Fall
37 A DAY IN THE LIFE OF APPS IN GI GI advanced practice providers offer a look at their "typical day"
43 SPOTLIGHT ON INNOVATION: IUS
Advances in the use of intestinal ultrasound (IUS) for monitoring and managing IBD
47 NORTH AMERICAN GI TRAINING GRANT
Dr. Yuying Luo shares her experience training in DGBI in the Netherlands
49 // INSIDE THE JOURNALS
50 AJG
A new ACG Clinical Guideline on Focal Liver Lesions by Frenette, et al., and the special issue of the Red Journal on obesity
50 CTG
Acute and Long-Term Effects of AppDelivered Heartfulness Meditation on Psychological Outcomes and the Endocannabinoid Signaling System in Cyclic Vomiting Syndrome by Venkatesan, et al
50 ACGCRJ
Sirolimus Use in Refractory Crohn's Disease by Siu, et al
51 // REACHING THE CECUM
51 ACG GUIDELINE HIGHLIGHTS: ALCOHOLASSOCIATED LIVER DISEASE
A visual summary of ACG's 2024 Clinical Guideline on Alcohol-Associated Liver Disease by Jophlin, and Singal, et al
52 PATIENT HANDOUT: NUTRITION IN IBD
Diet considerations for the management of inflammatory bowel disease
#ACGfoodie Dr. Joseph Sleiman making Culinary Connections by sharing a meal with friends
ACG MAGAZINE
MAGAZINE STAFF
Executive Director Bradley C. Stillman, JD
Editor in Chief; Vice President, Communications Anne-Louise B. Oliphant
Manager, Communications Becky Abel
Art Director Emily Garel
Senior Graphic Designer Antonella Iseas
BOARD OF TRUSTEES
President: Jonathan A. Leighton, MD, FACG
President-Elect: Amy S. Oxentenko, MD, FACG
Vice President: William D. Chey, MD, FACG
Secretary: Nicholas J. Shaheen, MD, MPH, MACG
Treasurer: Costas H. Kefalas, MD, MMM, FACG
Immediate Past President: Daniel J. Pambianco, MD, FACG
Past President: Samir A. Shah, MD, FACG
Director, ACG Institute: Neena S. Abraham, MD, MSc, MACG
Co-Editors, The American Journal of Gastroenterology:
Jasmohan S. Bajaj, MD, MS, FACG
Millie D. Long, MD, MPH, FACG
Chair, Board of Governors: Dayna S. Early, MD, FACG
Vice Chair, Board of Governors: Sita S. Chokhavatia, MD, MACG
Trustee for Administrative Affairs: Irving M. Pike, MD, FACG
TRUSTEES
Jean-Paul Achkar, MD, FACG
Brooks D. Cash, MD, FACG
Jill K. J. Gaidos, MD, FACG
Seth A. Gross, MD, FACG
David J. Hass, MD, FACG
James C. Hobley, MD, MSc, FACG
Aasma Shaukat, MD, MPH, FACG
Neil H. Stollman, MD, FACG
Renee L. Williams, MD, MHPE, FACG
Patrick E. Young, MD, FACG
CONNECT WITH ACG
youtube.com/ACGastroenterology
facebook.com/AmCollegeGastro
twitter.com/amcollegegastro
instagram.com/amcollegegastro bit.ly/ACG-Linked-In
CONTACT
IDEAS & FEEDBACK
We'd love to hear from you. Send us your ideas, stories and comments. ACGMag@gi.org
CONTACT ACG
American College of Gastroenterology 11333 Woodglen Drive, Suite 100 North Bethesda, MD 20852 (301) 263-9000 | gi.org
DIGITAL EDITIONS
GI.ORG/ACGMAGAZINE




American College of Gastroenterology is an organization with an international membership of over 19,000 individuals from 86 countries. The College's vision is to be the preeminent organization supporting health care professionals who provide compassionate, equitable, high-quality, state-of-the-art, and personalized care to promote digestive health. The mission of the College is to provide tools, services, and accelerate advances in patient care, education, research, advocacy, practice management, professional development and clinician wellness, enabling our members to improve patients’ digestive health and to build personally fulfilling careers that foster wellbeing, meaning and purpose.
CONTRIBUTING WRITERS




Mahasen Akram Elshaer, MRCP, UK
Dr. Akram Elshaer is an Egyptian gastroenterologist who currently practices at the King Fahad Military Medical Complex in Saudi Arabia.
Hanna Blaney, MD, MPH
Dr. Blaney is a transplant hepatology fellow at Georgetown University Medstar Health.
Justin G. Brandler, MD
Dr. Brandler is a gastroenterologist at Virginia Mason and is a member of the ACG Institute’s 2023-2024 Emerging Leadership Program cohort.
Darren M. Brenner, MD, FACG
Dr. Brenner is a Professor of Medicine and Surgery at Northwestern University Feinberg School of Medicine. He currently serves as the ACG Governor for Illinois and is a member of the ACG Research Committee




Michael T. Dolinger, MD
Dr. Dolinger is an Assistant Professor of Pediatric Gastroenterology at the Icahn School of Medicine and Mount Sinai Kravis Children’s Hospital. He leads the Henry and Elaine Kaufman intestinal ultrasound program at the Susan and Leonard Feinstein inflammatory bowel disease Center at Mount Sinai.
Bara El Kurdi, MD
Dr. El Kurdi is Assistant Professor of Medicine at Virginia Tech Carilion School of Medicine in Roanoke, VA. He is a member of the ACG Innovation & Technology Committee and Legislative & Public Policy Council.
Scott L. Gabbard, MD, FACG
Dr. Gabbard is a gastroenterologist at the Center for Esophageal and Swallowing Disorders at the Cleveland Clinic Foundation Ohio. He is Chair of ACG’s Patient Care Committee and serves on the Research Committee.
Michael P. Gallitelli
The late Michael P. Gallitelli, who unexpectedly passed away at age 54 on July 5, 2024, was the husband of long-serving ACG Vice President of Meetings & Exhibitions Elaine McCubbin Gallitelli. A U.S. Navy veteran, avid sports fan, and passionate environmental advocate, he delighted in capturing the simple beauty of the world around him.



Sachin Jain, MD, MBA
Dr. Jain is President and CEO of SCAN Health Plan. He also serves as Adjunct Professor of Medicine at Stanford University School of Medicine.
Noa Krugliak Cleveland, MD
Dr. Krugliak Cleveland is an Assistant Professor of Medicine at the University of Chicago Pritzker School of Medicine.
Jonathan A. Leighton, MD, FACG
ACG President Dr. Leighton is Professor of Medicine at Mayo Clinic Arizona. He also chairs Mayo Clinic Arizona’s Office of Joy and Well-being.

Victoria Louwagie, DMSc, MS, PA-C, DFAAPA
Victoria Louwagie is a Physician Assistant at the Mayo Clinic Health System in Mankato, MN, and Assistant Professor of Medicine at the Mayo Clinic College of Medicine and Science. She currently serves on the ACG Advanced Practice Providers Committee.

Yuying Luo, MD
Dr. Luo is Assistant Professor of Medicine at Mount Sinai West & Morningside in New York, NY, and the recipient of a 2023 North American International GI Training Grant.




Alicia Muratore, MD, MBA
Dr. Muratore is a GI fellow at University of North Carolina at Chapel Hill and a Harvard Business School alumna
Monica R. Nandwani, DNP, RN, FNP-BC
Monica Nandwani is Director of Advanced Practice at Stanford Health Care in California. She is the current Chair of the ACG Advanced Practice Provider Committee.
Katherine E. Scholand, MD
Dr. Scholand is Assistant Professor of Medicine at the University of North Carolina at Chapel Hill and is a member of the ACG Women in GI Committee.
Eric D. Shah, MD, MBA, FACG
Dr. Shah is an Associate Professor in the Division of Gastroenterology and Hepatology at the University of Michigan and director of the Michigan Medicine GI Physiology Laboratories. He currently serves as Chair of the ACG FDA Related Matters Committee and is a member of the Legislative & Public Policy Council and Research Committee.




Joseph Sleiman, MD
Dr. Sleiman is an Advanced IBD Fellow at the Digestive Disease Institute of the Cleveland Clinic Foundation. He currently serves on the ACG Training Committee.
Amy L. Stewart, FNP-C
Amy Stewart is a nurse practitioner at Capital Digestive Care in Washington, DC. She is currently the lead APP for Capital Digestive Care’s Metropolitan Gastroenterology Group and is a sub-investigator at Chevy Chase Clinical Research.
Raseen Tariq, MBBS
Dr. Tariq is currently a GI fellow at Mayo Clinic on the NIH-sponsored T32 track, graduating in December 2024, and is a member of the ACG Innovation & Technology Committee.
Jason J. Thomas, DPAS, MPAS, PA-C
Jason Thomas is an Associate Professor at Seton Hill University and Physician Assistant at Independence Health in Latrobe, PA. He currently serves on the ACG Advanced Practice Providers Committee.

Amanda B. Wilhite, MPAS, PA-C
Amanda Wilhite is a Physician Assistant at Houston Methodist Gastroenterology Associates in Houston, TX.
KEEPING THE “WHY” AHEAD OF THE “WHAT”
By Jonathan A. Leighton, MD, FACG
WHILE IT IS CRITICAL THAT WE CONTINUE TO DEAL WITH the headwinds facing medicine, it is also important to remember why we went into medicine in the first place…to care for our patients, address their medical problems, and hopefully improve their outcomes. But sometimes we forget that the patient experience may be as important as the treatment of their ailments. It is important to realize the service we provide is not only about technology and diagnostics but also about how we interact with our patients. I would suggest that our new North Star should take us from the best healthcare experience to the best human experience. If you ask a physician what constitutes a quality experience, they may appropriately focus on technical expertise, outcomes, and safety. But if you ask a patient the same question, they often emphasize access, responsiveness, and communication. A great patient experience is judged by the patient. It takes into account all of their senses. It includes relationships and processes. I believe that delivering a great patient experience is no longer an option, but a necessity—especially in the competitive environment we live in. It is my belief that we need to see the human experience through the eyes of our patients. That human experience is characterized by teamwork, belonging, trust, and hope.
I am reminded of a Beryl Institute study in 2015 which found that 99% of consumers felt that their experience was somewhat or extremely important, and 95% felt that their participation in decision-making was also somewhat or extremely important. And I do believe this is true. For our patients, service delivered is as important as the clinical outcomes we are trying to achieve. By providing outstanding service to our patients and their caregivers, we as clinicians have the power to distinguish ourselves from all others. We should never let the things we do replace the reasons we do them. It is about the care we provide and the promises we make. Above all, it is how we respect and treat each other in delivering those promises.
As Medical Director of the Office of Mayo Clinic Experience for seven years, I have a unique perspective on the importance of experience in the lives of our patients and their families. Our most important metric is “Likelihood to Recommend” because it represents more than an expression of satisfaction with our patient’s care or even meeting expectations. It reflects the extent to which providers have met their patients’ needs, including peace of mind, compassionate and coordinated
care, communication, hope, and trust. Likelihood to recommend inversely correlates with the number of service problems a patient encounters in their visit and, therefore, it is critical that we address service lapses.
In a world where the healthcare environment is extremely uncertain with unpredictable change, increasing competition, increasing regulatory issues, and declining reimbursement, it is clear that patients have preferences on where they receive their care. As we clinicians struggle to keep up with science, changing technologies, and economic challenges, it can be difficult to maintain the patient experience. Yet, economic trends are driving patients’ increasing involvement in choosing care providers.
In the end, there is one clear imperative: earning and retaining patient loyalty is the right thing to do and can provide that competitive edge. Providing a good experience and likelihood to recommend are driven by factors that are within control of clinicians and their practices. In addition, these factors are completely consistent with the values that inspire professional pride among physicians, allied health staff, and other personnel.
As gastroenterologists and hepatologists, we are all committed to quality. And when we speak about quality, we should be concerned not only about safety and outcomes but also service to our patients. I believe most of us understand the importance of value and efficiency in addressing the challenges before us so that we can deliver better service to our patients. Studies have shown in the outpatient setting that if we redesign our practices based on system standards, improve efficiency, and delegate administrative tasks, we can potentially increase time savings by up to 30%. In addition, there are studies suggesting that poor quality can translate into significant financial burdens because our staff are working on fixing mistakes rather than
accomplishing a new task. Patients want to connect with their medical team in a way that makes them feel understood. There are data that show positive and statistically significant associations between patient experience metrics and favorable clinical outcomes. There is also evidence that workforce engagement and patient experience influence an organization's financial performance. Finally, we know that practices that emphasize safety and quality of care are correlated with the engagement level of their workforce; and we know more satisfied employees lead to more satisfied patients. An employee-driven model of care should be energized and innovative, team-based, and systemssupported. The future success of our healthcare organizations and independent practices depends on our ability to change and provide increasing value to our staff and our patients.
These are indeed challenging times, but it is important to always remember the reason we went into healthcare…to improve the lives and wellbeing of our patients. I believe there are three key areas to focus on if we are going to be successful: relationships, workflow and processes, and communication. Building relationships is critical to enable patients to feel more confident in their healthcare team, especially by demonstrating concern for their medical problems. Workflows and processes must be efficient and demonstrate teamwork and coordinated care. Finally, communication is critical, especially about medications, wait times, and delays and instructions for follow-up care.
Remember, what put us where we are today may not be enough to keep us there tomorrow. Healthcare is deeply personal, and medicine is an art. Patient-centered care should always be reliable and timely. We need to create a welcoming environment that enhances the human connection and fosters lasting relationships. Focusing on the patient and delivering on the promise of the best human experience will always be the right thing to do.
“It is my belief that we need to see the human experience through the eyes of our patients.”

—Jonathan
Note wor thy Note wor thy
NOVEL & NOTEWORTHY
FEATURES KUDOS on new jobs, recommendations for great educational videos and podcasts, and new resources for grant writing from the Research Committee.
Reports of ACG members in action in the community come from Tauseef Ali, MD, FACG, and the Association of PakistaniDescent Gastroenterologists of North America in Oklahoma City, OK, and from Trustee James C. Hobley, MD, MSc, FACG at the Kappa Alpha Psi fraternity gathering in Shreveport, LA. McMaster University hosted a training for GRADE reviewers, while representatives of the U.S. Food and Drug Administration (FDA) met with members of the FDA Related Matters Committee at the College’s Headquarters in North Bethesda, MD.
With in memoriam tributes, the College celebrates with fondness and respect the lives and contributions of Daniel Pelot, MD, MACG, and Jerome H. Siegel, MD, MACG.
AN EYE FOR THE WORLD’S BEAUTY
It is an honor for ACG MAGAZINE to publish photographs by Michael P. Gallitelli posthumously. A member of the extended ACG family, Michael passed away unexpectedly on July 5, 2024, at the age of 54. He was the beloved husband of Elaine McCubbin Gallitelli, ACG’s Vice President of Meetings and Exhibitions, a member of the ACG staff since 2002. Michael was well known to many of the ACG staff and the ACG Board of Trustees. He traveled with Elaine to Board meetings over the years and got to meet many in the ACG leadership.

About the Photographer
In leaving the world, Michael left the tremendous gift of his photographs. He did not start out as a photographer but found his passion for recording the striking and beautiful places he saw during the hikes that he and Elaine enjoyed in their relationship. They traveled all over the country and Canada and loved exploring new places together.
At first, he got an inexpensive camera, but as his hobby grew into a passion, Michael’s skills as a photographer evolved, and his camera equipment got an upgrade. Even when shooting with his phone, he had an incredible knack for capturing the perfect moment. He was a quiet observer with a keen sense of timing and a gift for small details and grace notes.
In his hikes and travels, and even in his own backyard, he took photos of birds and animals, gorgeous landscapes,

inviting vistas, and misty mountains. His photos reveal a strong sense of composition and a clear ability to capture moments of serenity and beauty. He had wide ranging interests and an incredible sense of curiosity about the world – this curiosity and his skills of close observation are evident in his photos.
Michael’s family displayed his work with love and pride at his memorial service on July 19 in Union, New Jersey.
Born and raised there, he resided in New Jersey for most of his life. Recently, he and Elaine had moved to Maryland and purchased a home in a more rural area where he enjoyed grilling, feeding the backyard birds, and savoring the peace and quiet the area provided.
Michael served in the U.S. Navy from 1989 until 1997, performing duties worldwide including posts in Hawaii and London, UK. He was very proud of his military service and often talked about


how it was the best time of his life.
An avid sports fan, he was devoted to the New York Rangers, Tottenham Hotspurs, New York Red Bulls, and New York Mets.
Before his death, Michael was attending college and working on a degree in environmental science. He was passionate about climate change and improving the planet for his children and for future generations.

He is survived by Elaine; two sons, Brandon and Lucas; his father, Peter; brother Joseph; and sisters, Corinna and Jolie. He is predeceased by his mother, Kathleen, and brother, Keith.
Michael was a dedicated father, a loving husband, and a kind, funny, authentic, friendly, and honorable man. His boundless sense of humor and the silly songs he created for those he loved will be missed by everyone who knew him.
Michael Gallitelli died far too young, but while he was alive, he loved deeply and well, and he saw the world’s beauty with clarity and grace –touching so many lives and leaving this world a better place.
[ACROSS THE UNIVERSE]

Lisa B. Malter, MD, FACG, is now the chair of the ACG Education Universe editorial board, the College’s CME portal (education.gi.org). In this role, she oversees the development of content and collaborates with the ACG Educational Affairs Committee. She wears another important hat as course co-director of IBD 101, a one-day primer for first-year GI fellows sponsored by ACG and NYU Langone Health where Dr. Malter is Professor Medicine at NYU Grossman School of Medicine.
[UNC NEWS]


Starting in July, Nicholas J. Shaheen, MD, MPH, MACG, assumed the role of Director of The North Carolina Translational and Clinical Sciences Institute (NC TraCS) at The University of North Carolina. After a 12-year tenure as Division Chief for UNC GI & Hepatology, he takes on this new role while continuing to fulfill his responsibilities as senior associate dean for clinical research. Millie D. Long, MD, MPH, FACG, will serve as Interim Chief of GI & Hepatology. Dr. Long is the CoEditor-in-Chief of The American Journal of Gastroenterology
[LISTEN UP]

Brains & Guts: The GI Innovation Podcast In each episode, Toufic Kachaamy, MD, FACG, and Vladimir M. Kushnir, MD, FACG, interview gastroenterology innovators and inventors to unpack their successes, pitfalls, and learnings. The goal? Empower individual gastroenterologists with the knowledge and skills to explore ideas and apply the innovator’s mindset to everyday practice.
Listen on the ACG website: gi.org/journals-publications/brains-guts
Listen on your favorite podcast platform: Apple Podcasts, Google Podcasts, Spotify

Toufic Kachaamy, MD, FACG

[MILITARY MIGHT]
ACG’s Military Governor, John G. Gancayco, MD, FACG, stepped down this summer after seven years of service as the GI fellowship program director at the San Antonio Uniformed Services Health Education Consortium (SAUSHEC). Dr. Gancayco helped train 42 GI fellows over the years. David T. Dulaney, MD, has been named as the incoming program director. The future is bright for Army & Air Force GI!
[EVIDENCE MASTERS]
[WHAT TO WATCH]
ACG Virtual Grand Rounds – In case you missed them, check out these recent talks on the ACG Education Universe. Login required to a free account at education.gi.org

How to Bring Farm to Table into GI Training and Practices
Thursday, June 20, 2024
Faculty: Madhuri Badrinath, MD; Alexis Bejcek, MD; and Christina Tennyson, MD
Watch: education.gi.org/presentations/universe_17588
Enhancing Diversity in Clinical Trials
Thursday, July 18, 2024
Speaker: Belen A. Tesfaye, MD | Moderator: Shajan Peter, MD, FACG
Watch: education.gi.org/presentations/universe_17591
Scoping Out Solutions: Actionable Steps for GI Clinician Well-Being
Thursday, September 19, 2024
Faculty: Jonathan A. Leighton, MD, FACG; Jeffrey P. LaFond, MD, FACG; and Keith W. Jones, MA Watch: education.gi.org/presentations/universe_17618
GRADE Team at McMaster – The newest members of the ACG GRADE team completed training at McMaster University in June. Joy W. Chang, MD, of the University of Michigan, Po-Hung (Victor) Chen, MD, PhD, FACG, of Johns Hopkins University, Jennifer M. Kolb, MD, MS, of UCLA, and Andrew M. Moon, MD, MPH, FACG, of the University of North Carolina at Chapel Hill completed training to certify them as expert methodologists in guideline development. Led by Grigorios I. Leontiadis, MD, PhD, FACG, the group spent three intense days studying GRADE (Grading of Recommendations, Assessment, Development, and Evaluations), a transparent framework for developing and presenting summaries of evidence that provides a systematic approach for making clinical practice recommendations.

Nicholas J. Shaheen, MD, MPH, MACG
Millie D. Long, MD, MPH, FACG
John G. Gancayco, MD, FACG and David T. Dulaney, MD
Vladimir M. Kushnir, MD, FACG
Left to Right: Jennifer M. Kolb, MD, MS; Andrew M. Moon, MD, MPH, FACG; Joy W. Chang, MD; and Po-Hung (Victor) Chen, MD, PhD, FACG
[FDA INTERFACE]
FDA Meeting at ACG Headquarters – On May 17, 2024, the FDA-Related Matters Committee hosted three physician leaders from the FDA at the ACG's office in North Bethesda, Maryland. They discussed the evolving challenges and opportunities in new drug approvals and clinical study design, as well as the joint ACG-FDA Fellowship, which grants first- or second-year fellows with

[CRC MONTH IN JULY]
The Association of Pakistani-Descent Gastroenterologists of North America (APGNA) held its Annual Summer Convention and hosted a colorectal cancer awareness walk for attendees. Tauseef Ali, MD, FACG, organized the meeting, which featured a talk by ACG Trustee Aasma Shaukat, MD, MPH, FACG. Other APGNA and ACG members involved included Arif M. Muslim, MD, FACG; Muhammad Anis Memon, MD;

[GRANT GUIDANCE]
The ACG Research Committee created new grant writing resources for those applying for the 2025 Clinical Research Awards. If you have questions, are new to grant writing, or need a refresher, watch videos, read grant tips, and explore other resources including a tutorial with a checklist for success as well as pearls and pitfalls for ACG grant applicants.
Visit: gi.org/grant-writing-resources | Apply: gi.org/research-awards
Deadline: December 2, 2024 at 11:59 pm ET for 8 categories supported by the ACG Institute for Clinical Research & Education
[VISITING PROFESSORS]
The Edgar Achkar Visiting Professorship (EAVP) is a signature offering of the ACG Institute for Clinical Research & Education. Since 2014, EAVP has provided GI training programs with visiting professors for lectures, small group discussions, panel discussions, and one-on-one visits with trainees and faculty. A source of inspiration, mentoring, and clinical education, almost every GI training program in the United States has hosted an EAVP visit. Starting in 2021, the program offers a Visiting Scholar in Equity, Diversity & Ethical Care under the auspices of the ACG Institute’s Center for Leadership, Ethics & Equity (LE&E Center).



Visiting Scholar in Equity, Diversity, & Ethical Care University of South Florida, Tampa, FL – April



Left to Right: Erica Lyons, MD, Associate Director for Therapeutic Review, Division of Gastroenterology, OND, CDER; Amanda Cartee, MD, FACG, Vice Chair, FDARelated Matters Committee; Eric Shah, MD, MBA, FACG, Chair, FDA-Related Matters Committee; Jessica J. Lee, MD, Division Director, Division of Gastroenterology, OND, CDER; Juli Tomaino, MD, Deputy Division Director, Division of Gastroenterology, OND, CDER; Renee Williams, MD, MHPE, FACG, ACG Trustee.
Lin Chang, MD, FACG (UCLA) Westchester Medical Center, Valhalla, NY –March 6
Rachel B. Issaka, MD (Fred Hutchinson Cancer Center)
4
Francis A. Farraye, MD, MSc, MACG (Mayo Clinic Florida) Texas Tech University El Paso, Virtual – April 4
Millie D. Long, MD, MPH, FACG (UNC Chapel Hill) UMass Chan Medical School Baystate Health, Springfield, MA – April 10
Victor Chedid, MD, MS (Mayo Clinic Rochester) Visiting Scholar in Equity, Diversity, & Ethical Care University of Alabama at Birmingham, Birmingham, AL – April 11
ACG Institute Director Neena Abraham, MD, MSc (Epid), MACG (Mayo Clinic Arizona) AdventHealth Orlando, Orlando, FL – April 25-26
Transplant hepatologist Dr. Omar A. Haq of Dallas, TX, with his best friend, Tauseef Ali, MD, FACG, at the APGNA meeting.
[AT KAPPA ALPHA PSI]
In May, ACG leaders attended the Kappa Alpha Psi Southwest Province meeting in Shreveport, Louisiana, beginning a partnership to help improve colorectal cancer awareness and screening rates. ACG Trustee James C. Hobley, MD, MSC, FACG, and Immediate Past President Daniel J. Pambianco, MD, FACG, shared the data on the crucial importance of early screening – especially among Black American men – and gave attendees recommendations on how to spread awareness in their communities. U.S. Rep. Troy Carter (D-LA) also challenged each of his fraternity brothers to encourage 10 family members and friends to get screened.

[IN MEMORIAM]
Jerome H. Siegel, MD, MACG (March 2, 1932 – July 28, 2024)

Dr. Jerry Siegel, a friend, mentor, and teacher to so many, passed away July 28, 2024. He was native of Atlanta, Georgia. He graduated as a pharmacist and then received a degree in chemistry from the University of Georgia. In 1960, Dr. Siegel graduated as Alpha Omega Alpha from the Medical College of Georgia. He completed his internship in Allentown, Pennsylvania, and followed that experience by serving as a flight surgeon in the U.S. Air Force. After completing his military service, he began his residency in medicine and gastroenterology at the VA Hospital in the Bronx and Columbia Presbyterian Medical Center in New York, New York. He was mentored by Dr. Henry Colcher and Dr. Charles Flood. After residency, he entered private practice in Atlanta, Georgia. He left private practice in 1973 and was accepted by Professor Sheila Sherlock as a research fellow in gastroenterology and hepatology at the Royal Free Hospital, University of London. He became involved in ERCP and introduced colonoscopy to that institution.
In 1975, Dr. Siegel accepted an appointment at the New York Medical College as training director of the fellowship program. He honed his endoscopic and ERCP skills and became one of a few gastroenterologists in the United States performing ERCPs. He garnered his experience with sphincterotomies when he worked with Laszlo Safrany in Muenster, Germany. Dr. Siegel accepted fellows from other programs for advanced training; then, in 1989, he began one of the first advanced fellowship programs in therapeutic endoscopy in North America.
His practice, based at Doctor's Hospital/Beth Israel North, was a regional referral center for ERCP. He ran the first live endoscopy courses in New York in ERCP there and trained many fellows and visiting gastroenterologists in the intricacies of the procedure. He was well known as a traveling endoscopist, with temporary privileges at 40 hospitals in the tri-state area. He would come as needed to assist with ERCP when no other expert options were available, traveling with duodenoscope and accessories to hospitals that had neither. His private practice in 2010 contained six interventional endoscopists –unequaled in the United States.
Dr. Siegel was a Clinical Professor of Medicine at the Icahn School of Medicine at Mount Sinai. He published 123 peer-reviewed articles, 130 abstracts, 14 requested peer-reviewed articles, and 27 chapters in textbooks. In 1991, he published a single-author textbook on ERCP, which remains a standard today. He participated in symposia and live demonstrations throughout the United States, Canada, Europe, South America, China, Japan, and India. He taught and trained gastroenterologists in Vietnam.
Dr. Siegel was elected ACG Governor for Manhattan from 2005 to 2011 and served on the College’s National Affairs Committee (2008-2011). He was on the editorial boards of Gastrointestinal Endoscopy, The American Journal of Gastroenterology, and other journals. In 2004, he was designated a Master of the College (MACG).
Jerry and his wife of 62 years, Beverly, resided in Manhattan. They have a daughter, Dori; a son, Brian; and four grandchildren with strong family ties to Atlanta. He was a truly extraordinary physician, teacher, friend, and colleague who will be deeply missed.
[IN MEMORIAM]
Daniel Pelot, MD, MACG, Irvine, CA (November 5, 1934 - November 29, 2023)

Daniel Pelot, MD, 89, was born in South Carolina and passed away in Huntington Beach, California, on November 29, 2023.
Dr. Pelot was a Professor of Medicine at UC Irvine Medical Center for over 40 years. His research interest was in chemoprevention of colon cancers and colorectal adenomas. After an undergraduate degree from Savannah State, he graduated from medical school at Howard University in 1966. He trained at Los Angeles County-USC Hospital, volunteered at the Los Angeles Veterans Administration Hospital, and served for decades on the faculty and staff of UCI Medical Center. Over the years, Dr. Pelot mentored medical students, residents, and fellows, and was highly engaged with colleagues. His research, writing, speaking, and teaching took him from humble roots to big cities and internationally to China and Australia. He joined the College in 1976, was elected Governor for Southern California (B) from 1986 to 1992; and served as ACG Trustee from 1993 to 1999. After service on the Board of Trustees, he continued his loyal engagement and service with terms on the Professional Issues Committee (1998-2005), the Archives Committee (1998-2004), and the Awards Committee (2005-2011). In 2005, Dr. Pelot was honored as a Master of the College (MACG).
Dr. Pelot was a devoted husband to Ann for nearly 50 years. Ann Pelot had the distinction of being the first woman to be awarded a PhD in mathematics from Georgetown University in 1968. She taught at the university, college, and community college levels in Southern California. He is survived by daughters Michele R. Pelot, MD, an anesthesiologist at Cedars-Sinai Medical Center in Los Angeles; Denise Danielle Pelot, JD, an attorney in Boston; grandchildren Aidan and Olivia; and many nieces and nephews.
Dr. Pelot’s legacy includes commitment to family, hard work, dependability, and service. His repertoire of jokes, combined with a gentle manner and concern for others, will be sorely missed by all who turned to Dan for counsel, especially his beloved family.
Daniel J. Pambianco, MD, FACG; Kevin T. Marks, MD; U.S. Rep. Troy Carter (D-LA); James C. Hobley, MD, MSc, FACG
Learn About



TRAINEE HUB
Bridging Business and Medicine: Essential Lessons for GI Fellows
IT HAS BEEN SAID THAT “HEALING IS AN ART, MEDICINE IS A PROFESSION, BUT HEALTHCARE IS A BUSINESS." Many, if not all, physicians enter medicine with the goal to provide excellent clinical care to patients. To obtain this goal, medical schools and post-graduate training programs have traditionally focused on teaching learners the pathophysiology, diagnosis, and treatment of various disease processes. However, many, if not all, physicians will encounter an experience in which their ability to implement good clinical care is impeded not by a lack of clinical knowledge, but rather a lack of management or implementation of knowledge. To be able to provide the excellent clinical care we desire, physicians need to learn the skills and knowledge to navigate the business side of the healthcare system.
For many, business skills evoke thoughts of financial statements and accounting. While it is true that financial literacy is important to running a gastroenterology practice, both in private practice and academic settings, business skills extend far beyond financial literacy to include leadership, ethics, management, marketing, strategy, and operations.
Alicia Muratore, MD, MBA and Eric Shah, MD, MBA, FACG
“Physicians who understand strategic thinking will be able to identify opportunities for growth, differentiate their practice, and stay ahead of industry and patient needs.”
We interviewed, Dr. Sachin Jain, a prominent physician and figure in the health care industry, who emphasized that these non-finance skills are the real game-changers in delivering clinical care. Below we will focus on specific skills that are not just beneficial – but essential – to GI fellows navigating the complex healthcare landscape.
Beyond the Basics: The Power of Soft Skills
1.Leadership Skills: Managing Your Team
Effective leadership is pivotal in medicine, and especially in gastroenterology, where we lead diverse teams of nurses, technicians, staff, and physicians. Soft skills like leadership and team management are often learned through practical experience rather than formal education. While medical training emphasizes clinical expertise, there is limited structured training in leadership and organizational behavior. Given that all physicians will go on to become leaders of teams in some capacity, a formalized education on this topic is needed (Rotenstein, et al., 2018). Physicians are already educated on ways to communicate effectively with patients to explain their health problems, recommend treatments, and help patients understand their care. However, the medical curricula should also be expanded to include leadership skills, including the ability to coordinate teams, provide mentorship and feedback, and develop interprofessional communication. These skills are important no matter which type of practice a gastroenterologist enters, as all
physicians will find themselves in some type of leadership position (Bhavsar-Burke & Dilly, 2023).
In academia, researchers need to be able to foster collaborative environments and set clear goals among team members. Department chairs and leaders need to facilitate open communication amongst colleagues and across departments. In private practice, physicians can improve clinic operations by enhancing staff morale and teamwork through more effective leadership. Providers can develop leadership training programs for clinical staff to empower them to take on leadership roles within the practice.
2.Leadership and Accountability: Maintaining Ethics
All physicians have taken the Hippocratic Oath, committing to uphold specific ethical and medical standards. Physicians are taught about this code of ethics through discussions on patient care and professionalism. However, few, if any, teachings are provided on navigating complex ethical dilemmas or managing corporate responsibilities within healthcare practices and organizations. Some of these ethics are already incorporated into medical teaching and training by nature of exposure. For example, many physicians will have conducted some sort of research during their training and thus have been taught research ethics to ensure studies are conducted ethically and transparently.
However, physicians are less likely to have received formal training on ethics on the system side: for example, establishing departmental or practice codes of conduct. These codes shape the expectations and culture of the group and can drastically impact staff behavior and incentives. Furthermore, education is needed about how to ensure proper compliance, such as how to implement regular audits of billing practices. Perhaps most importantly, it is
paramount that physicians who enter these leadership roles maintain their ethical commitment to patients, or risk conflict of their responsibility to the corporation vs. responsibility to the patient (Jain, 2024).
3.Entrepreneurial Management: Innovating in Healthcare
Physicians receive limited formal training in entrepreneurial management during medical school and residency. While some may develop entrepreneurial skills through experience in research or leadership roles, there is often a gap in understanding business principles and innovation strategies applicable to healthcare delivery. Classes in entrepreneurial management encourage innovative thinking and problem-solving. For gastroenterologists, this means being open to new technologies, treatment methods, and care models that can improve patient outcomes. Physicians with this type of knowledge can be proactive in identifying opportunities for improvement within their practice and can implement change. In academia, knowledge of entrepreneurial management can help physicians to secure grant funding by identifying innovative research ideas. Many academic centers have innovation labs or groups that physicians can formally participate in to further innovate their research. Physicians can also learn to collaborate with industry partners to commercialize research findings and generate revenue. Importantly, physicians should understand the financial implications that may come from developing ideas and technologies while employed in various settings.
Innovation within private practice settings can be seen in developing new service lines or sub-specialty clinics to meet community needs by identifying gaps in healthcare service and implementing innovative solutions to reach those needs. Gastroenterologists should be aware of innovation resources that may be available to them. Many academic
hospitals will have access to innovation centers. For example, the University of North Carolina has one called Innovate Carolina, while University of Michigan has the University of Michigan Center for Innovation. These programs connect physicians with a wide variety of team members and resources to bring research and ideas to fruition.
4.Marketing: Communicating Value to Patients
Marketing in healthcare is not just about advertising, it is about understanding and meeting patient needs. How patients arrive to a gastroenterology practice is evolving. In addition to referrals from providers, patients are searching for their own gastroenterologists. Additionally, given the access to health-related information, patients are much more informed. This changes how physicians and healthcare networks need to market themselves to attract and retain more patients.
In addition to word of mouth, physicians now need to consider their online visibility and presence. First and foremost, physicians should continue to provide good, high-quality care. However, they then need to determine how to make referring providers and patients aware of that care. Education on marketing can help physicians achieve that goal. Physicians should be educated on how they can create a strong and recognizable brand for themselves as well as for their practice.
Physicians should be educated on digital marketing: how to utilize social media, search engine optimization, and online advertising to reach potential patients. Additionally, physicians should be taught tools to cultivate patient engagement. This could be through developing strategies to engage with patients through newsletters, educational content, and patient portals.
5.Strategy: Navigating the Digestive Healthcare Landscape
Strategic planning is key to success in gastroenterology. Business skill strategy courses can help teach
“A physician who understands operations management can significantly enhance the efficiency, effectiveness, and quality of care provided in their practice.”
physicians about competitive advantage and long-term planning. The clinical landscape is vastly different now than it was 20 years ago and will be extremely different 20 years from now. There are ever-evolving technologies, shifting regulatory environments, and changing patient demographics. Physicians who understand strategic thinking will be able to identify opportunities for growth, differentiate their practice, and stay ahead of industry and patient needs. Physicians can create vision and strategy that incorporate new advanced diagnostic tools, expanding service lines, or strategic partnerships. Physicians in academia can implement a strategic plan to secure research funding or forge interdisciplinary partnerships to strengthen academic endeavors.
6.Operations Management: Optimizing Efficiency
Effective operations management is essential for gastroenterologists to know and understand. A physician who understands operations management can significantly enhance the efficiency, effectiveness, and quality of care provided in their practice. In a gastroenterology practice this means understanding how to streamline workflows, reduce wait times, and utilize electronic health records effectively. It can also enable physicians to be able to design better patient flow process, enhance the efficiency of endoscopic procedures, and ultimately improve patient outcomes. Many physicians already think about and perform this type of work, largely as quality improvement projects or as part of their routine practice discussions. However, there are many specific skills and knowledge that could be taught that would provide even further insights and benefits. For example, physicians could learn about time-driven activity-based costing (TDABC), which is a practice that
assigns cost based on actual time and resources consumed by activities, offering a more precise and practical approach to managing and reducing costs.
Integrating these key business principles can enhance how we as gastroenterologists approach and deliver care in many ways.
Conclusion
Medical school provides us with a foundation in pathophysiology and clinical science, but we often enter the clinical workforce without a substantial understanding of public policy and management frameworks that influence our ability to implement effective clinical care. Incorporating business school teachings into gastroenterology practice—whether in academic or private settings—can enhance leadership, innovation, and patient care. Formal education for these topics should take place across the continuum of medical education from medical school, through residency and fellowship, and into post-training continuing education. These teachings can be implemented formally through didactics in medical school and training conferences, specialized retreats, or asynchronous online programs. Some examples already exist which include Mayo’s Resident Leadership Academy and Brigham and Women’s Management and Leadership Track. However, these programs are for selected cohorts within each residency, and all trainees would benefit from expanding these offerings to the class at large. Individuals can be sponsored to attend Harvard Online’s Healthcare Leadership classes which offer courses on business strategy and economics in today’s healthcare landscape.
“Medical school provides us with a foundation in pathophysiology and clinical science, but we often enter the clinical workforce without a substantial understanding of public policy and management frameworks that influence our ability to implement effective clinical care. Incorporating business school teachings into gastroenterology practice—whether in academic or private settings—can enhance leadership, innovation, and patient care.”
By leveraging these skills and understanding core business principles, gastroenterologists can navigate the complexities of modern healthcare delivery and lead the way in providing high-quality, patientcentered care.
Special thanks to Dr. Sachin Jain for his valuable insights on the importance of business skills in healthcare.
Bibliography
1. Bhavsar-Burke, I., & Dilly, C. K. (2023b). How to become a leader as a fellow. Gastroenterology, 165(2), 329–332. https:// doi.org/10.1053/j.gastro.2023.05.002
2. Jain, S. H. (2024, June 4). The doctor in the Corporation. Forbes. forbes.com/sites/sachinjain/2024/05/23/the-doctorin-the-corporation/
3. Rotenstein, L. S., Sadun, R., & Jena, A. B. (2018a, October 17). Why doctors need leadership training. Harvard Business Review. hbr.org/2018/10/why-doctors-need-leadershiptraining
About

Alicia Muratore, MD, MBA, is a gastroenterology fellow at University of North Carolina at Chapel Hill and she is a Harvard Business School alumna. She is passionate about leveraging business insights to enhance healthcare delivery and operational efficiency.

Sachin Jain, MD, MBA, has served as a medical educator at Harvard and Stanford with expertise in healthcare delivery innovation and healthcare reform, as well as CEO of the groundbreaking healthcare industry organizations CareMore Health System and the SCAN Group and Health Plan.

Eric D. Shah, MD, MBA, FACG, is an Associate Professor in the Division of Gastroenterology and Hepatology at the University of Michigan. He is director of the Michigan Medicine GI Physiology Laboratories. He also conducts medical innovation research with a focus on the development of new medical technologies and rigorous costeffectiveness and health economics studies to maximize value and access to care.
Resources
Leadership Development Opportunities from the ACG Institute for Clinical Research and Education
The ACG Institute offers leadership programs for gastroenterologists across the career span through its Center for Leadership, Ethics & Equity. The application portal for 2025 programs is open from September 16, 2024 to November 15, 2024, and all the leadership courses will convene from June 6 to 8, 2025.
Emerging Leadership Program
The Emerging Leadership Program provides the opportunity for U.S.based ACG Trainee members in their 3rd or 4th year of GI fellowship training to develop, build, and maintain success as future leaders. Participants will learn about communication, negotiation, change, and time management, and promoting equity, diversity, and inclusion. Info: gi.org/emerging-leadership
Early Career Leadership Program
The Early Career Leadership Program (formerly the Young Physician Leadership Scholars Program) develops future leaders in clinical gastroenterology by providing leadership and policy training to U.S.-based ACG member physicians who have completed one full year of practice after their terminal GI or hepatology fellowship and are in their first five years of clinical practice. Info: gi.org/early-career-leadershipprogram
Advanced Leadership Program
The Advanced Leadership program provides mid-career physicians (10-20 years post-fellowship completion) who are U.S.-based ACG members the opportunity to further develop comprehensive leadership skills.
Info: gi.org/advanced-leadership
Clinical Research Leadership Program
This unique interactive program provides ACG clinician investigators with the skill set to start, grow and maintain success as research leaders. Participants learn research leadership skills to maintain a successful independent research program. The program is for earlyto mid-career clinical investigators who are ACG member physicians (between 2-15 years out of fellowship training), are working in the U.S., and have active or recent funding as a Principal Investigator or Co-Principal Investigator.
Info: gi.org/clinical-researchleadership-program
Gut Reads
Gut Reads
GI Books by GI Authors
GI Books by GI Authors
With Special Recommendations for Leadership Reads and Fun Fiction
With Special Recommendations for Leadership Reads and Fun Fiction
AACG CELEBRATES THE PUBLICATION OF SEVERAL NEW BOOKS for the consumer audience written by GI experts. These authors’ dedication extends beyond the clinic, the endoscopy suite, or the lab to using the written word to educate patients interested in their digestive health. In putting the spotlight on these authors, the goal is to bring attention to their creativity and commitment and to highlight new works that might be useful with GI patients.
Beyond the world of consumer books, ACG MAGAZINE is sharing reading recommendations for your professional development, as well as fun fiction for the simple pleasure of a good read. The ACG Institute’s Advanced Leadership Program participants and faculty suggested a leadership or personal development book that has been influential and important in their leadership journey. The fiction readers among the Advanced Leadership group also shared a book recommendation just for fun, relaxation, or inspiration that colleagues might enjoy. Their varied and thoughtful selections are certain to provide fascinating possibilities for your reading list.
New Books by GI Authors Reviewed by ACG Members
Austin Lee Chiang, MD, FACG
Gut: An Owner’s Guide
Reviewer: Scott L. Gabbard, MD, FACG
Kate M. Scarlata, MPH, RDN & Megan E. Riehl, PsyD
Mind Your Gut: The Science-Based, WholeBody Guide to Living Well with IBS
Reviewer: Darren M. Brenner, MD, FACG
James H. Tabibian, MD, PhD, FACG
Digestive Problems Solved: A Patient's Guide to Expert Insights and Solutions
Reviewer: Katherine E. Scholand, MD
Xiao Jing “Iris” Wang, MD
Boo Can’t Poo
Reviewer: Justin G. Brandler, MD
Gut:
An Owner’s Guide (The Body Literacy Library), DK Publishing, 2024
Author: Austin Lee Chiang, MD, FACG Reviewer: Scott
L. Gabbard, MD, FACG

In Gut: An Owner’s Guide, Dr. Austin Chiang provides a comprehensive review of clinical gastroenterology aimed at the savvy patient. Dr. Chiang discusses GI function, common diseases and their pathophysiology, and various aspects of gastrointestinal testing. The book is complete with many illustrations that truly add to the learning. I was especially impressed with the chapter focusing on maintenance of a healthy GI tract – proper nutrition and hygiene, lifestyle changes are described in a very informative manner.
This book is a wonderful resource for our patients who wish to dig deeper than the “one-pager” articles that we often print out in clinic. This resource has the potential to answer many of the questions that my patients ask on a routine basis. The author is engaging and writes in an easy-to-understand style.
This book would also serve as a nice introduction to gastroenterology for any budding gastroenterologists in high school or college; there is a fantastic amount of useful information contained in the pages.
On a personal note, I have read a few chapters to my two sons on some nights instead of their typical bedtime book – the chapter on poop got two thumbs up from both boys!

About Dr. Austin Chiang
Dr. Chiang is Assistant Professor of Medicine and Director, Endoscopic Bariatric Program, at Thomas Jefferson University in Philadelphia, PA. He also serves as Chief Medical Social Media Officer at Medtronic. He is a well-known health social media creator and when he is not writing books, seeing patients,
making Tik Toks, or traveling for his work for Medtronic, he is a violinist and fierce champion for LGBTQIA+ visibility in medicine and in the world.

About Dr. Scott Gabbard
Dr. Gabbard is a gastroenterologist at the Center for Esophageal and Swallowing Disorders at the Cleveland Clinic Foundation in Cleveland, OH. He is Chair of ACG’s Patient Care Committee where he oversees the development and dissemination of ACG patient education materials and collaborates on podcasts with Gastro Girl. This is his second book review for ACG MAGAZINE (2023 Issue 2 bit.ly/ gabbard-book-review-gut-feelings). When he is not reviewing books, he is reviewing clinical research grant applications as a member of the ACG Research Committee.
Mind
Your Gut: The
ScienceBased,Whole-BodyGuide to LivingWellwith IBS, Hachette
Books, 2024
Authors: Kate Scarlata, MPH, RDN and Megan Riehl, PsyD
Reviewer: Darren M. Brenner, MD, FACG

Mind Your Gut, by Kate Scarlata MPH, RDN, and Megan Riehl, PsyD, is a well-written and highly informative text providing both seasoned practitioners and lay-people alike with concise, simple strategies for integrating evidence-based nutritional and behavioral interventions into the care of individuals with irritable bowel syndrome. They have taken a nononsense, evidence-based approach to treating IBS while concurrently dispelling many of the perpetuated myths and misconceptions in the lay person literature.
The book is designed to walk the reader step-by-step through nonpharmacologic approaches to treating
IBS. It begins with an overview of the interplay between the gut-brain axis, defining in simple terms how these systems interact and explaining how behavioral and nutritional interventions are beneficial in reducing symptom burden. Dr. Riehl provides techniques for gradually integrating home-based cognitive behavioral therapy and/or gut-directed hypnosis into personal care. Ms. Scarlata then walks the reader through the role of food in the development of IBS symptoms, providing dietary and lifestyle recommendations for identifying and eliminating food triggers in a healthy and safe manner. The book is laden with simple, poignant self-help tips (“Brain Bites,” “Gut Game Changers,” “Digestible Details”) which summarize and emphasize key strategies. The resources section provides a wealth of extra information, including charts and tables to help guide behavioral strategies, IBS-safe sample menus and recipes, and links to websites for further validated approaches.
The authors are realistic, conceding that natural treatment of IBS is not a one-size-fits-all process. However, they provide so many options that through trial and error, individuals should be able to identify their own set of techniques for symptom benefits. Most importantly, the recommendations provided by these two authoritative authors are steeped in science— something missing from many similar texts in this space. In summary, I give this book my highest recommendation, noting that this is a resource which should be incorporated into the clinical practice of anyone treating individuals with IBS.

About Ms. Kate Scarlata: Kate Scarlata MPH, RDN, is a gut health and nutrition expert with more than 30 years of experience. She is a New York Times best-selling author who specializes in food intolerance, including the low FODMAP diet. She is the author of an invited "How I Approach It" Red Section article, Low FODMAP Diet: What Your Patients Need to Know. The American Journal of
“Dr. Tabibian does an excellent job describing the role of stress and other psychological factors on gastrointestinal function and explaining various therapies including cognitive behavioral therapy, gut-directed hypnotherapy, and diaphragmatic breathing.”
Gastroenterology 114(2):p 189-191, February 2019. DOI: 10.1038/s41395-018-0274-6. Read: bit.ly/ScarlataAJG

About Dr. Megan Riehl: Megan E. Riehl, PsyD, is a GI Psychologist and Clinical Associate Professor at the University of Michigan. She has lectured extensively on psychogastroenterology. Dr. Riehl is clinical program director of the GI Behavioral Health program at Michigan Medicine where she has a full-time clinical practice, leads GI behavioral health trainings, and provides peer consultation. She is currently on the National Board of Trustees for the Crohn's and Colitis Foundation.

About Dr. Darren Brenner: Dr. Brenner is a Professor of Medicine and Surgery at Northwestern University Feinberg School of Medicine. His clinic and academic pursuits focus on disorders of gut-brain interaction (DGBIs) with particular focus on irritable bowel syndrome, constipation, opioid-related bowel disorders, and fecal incontinence. He currently serves as the ACG Governor for Illinois and is a member of the ACG Research Committee.
Digestive
Problems Solved: A Patient's Guide to Expert
Insightsand Solutions, Springer, 2023
Authors: James H. Tabibian, MD, PhD, Adventist Health, Glendale, CA
Reviewer: Katherine E. Scholand, MD, University of North Carolina at Chapel Hill
Digestive Problems Solved: A Patient's Guide to Expert Insights and Solutions by Dr. James H. Tabibian is an introduction

to the world of gastrointestinal diseases for patients. The book walks through the basics of gastrointestinal function, navigating the healthcare system, the normal steps of an evaluation, and when to seek a second opinion. It prepares patients for the questions their doctor is likely to ask, including a discussion on alarm symptoms and evaluation of potential triggers of digestive problems. The book also discusses the nuances of the various causes when a treatment regimen is not working. It also touches on topics patients are often curious about, such as probiotics, various diets, and the microbiome. Each section has additional reading resources for the patient who is interested in learning more from reliable sources, such as the NIH or various GI journals.
The highlight for me was the sections on disorders of gut-brain interaction and treatment options. Dr. Tabibian does an excellent job describing the role of stress and other psychological factors on gastrointestinal function and explaining various therapies, including cognitive behavioral therapy, gut-directed hypnotherapy, and diaphragmatic breathing.
This book would be a good recommendation for patients experiencing ongoing gastrointestinal symptoms with limited relief and unresolved questions. It will help to educate them on the basics of their gastrointestinal tract as well as the next steps to take and questions to ask. I see the book as a tool to create more well-informed and empowered patients.

About Dr. James Tabibian: Dr. James Hagop Tabibian is a Gastroenterologist and Advanced Endoscopist at Adventist Health Glendale and the Medical Director of Interventional GI. Prior to joining Adventist Health in 2023, he was a Health Sciences Clinical Professor in the Geffen School of Medicine at UCLA and Director of Endoscopy at Olive View-UCLA Medical Center. Dr. Tabibian is an excellent home chef who is dedicated to delicious meals and healthy eating. As one of the “ACG Foodies,” his recipe for Tabbouleh Salad was published in in ACG MAGAZINE in 2023. Explore: bit.ly/TabibianTabbouleh

About Dr. Katie Scholand: Dr. Scholand is Assistant Professor of Medicine at UNC who has a particular interest in gastrointestinal motility disorders. She finished her GI fellowship at the University of Colorado in 2023. Dr. Scholand is a member of the ACG Women in GI Committee. She enjoys spending time with her family and watching South Carolina Gamecocks sports.
Boo Can’tPoo, Mayo Clinic Press, 2024
Authors: Xiao Jing “Iris” Wang, MD and Rocio Ledesma, Illustrator Reviewer: Justin G. Brandler, MD, Virginia Mason Franciscan Health, Renton, WA

Constipation is a highly prevalent global condition which can lead to impaired quality of life. As an adult neurogastroenterology and motility specialist, I see countless constipated patients in clinic who suffer
from symptoms related to maladaptive behaviors developed in childhood.
Many could have benefited decades previously from a relatable, evidencebased children’s story for the ensuing battle with their bowels. Cue Boo Can’t Poo, written by dear friend and colleague from Mayo Clinic, Dr. Xiao Jing “Iris” Wang!
Using an approachable narrative about a little ghost named “Boo,” this simple yet effective board book empowers both children and their caregivers with practical strategies for tackling their turd troubles. I was quite impressed how Dr. Wang was able to integrate so many evidence-based behavioral recommendations seamlessly into lyrical prose that actually rhymed organically! Boo Can’t Poo uniquely strikes a Bristol 4 type balance of substance and style.
Hear what my co-reviewers had to say (spoiler alert!):
Isaac (7): “I like that he breathes because it’s good for helping poop go down more easily and not having to push really hard…I liked that he told his parents that he couldn’t poop because they give you really good ideas…and I like that he drank some water…and I like that he puts his knees up…and I like it that there’s faces on the poops. And my Dad laughed about what I just said.”
Joseph (4): “I like it, Daddy!”
Norah (8 months): “Bpppptthhhh!” *Bubbles in mouth*
The Brandler family gives Boo Can’t Poo a two green kiwi thumbs up!

About Dr. Wang: Dr. Xiao Jing “Iris” Wang is Assistant Professor of Medicine and a consultant in the Division of Gastroenterology and Hepatology at the Mayo Clinic in Rochester, MN, where her research interests include disorders of the gut-brain axis and she studies the motility and function of the GI tract. Dr. Wang is a member of the ACG Training Committee, the ACG Educational Affairs Committee, and is a Co-Chair of the ACG GI Circle. She is an alumna of the ACG Institute’s Early Career Leadership Program in 2022 and completed the Clinical Research Leadership Program in 2024. When she is not caring for patients or writing children’s books, she is a marvelous baker known for her delicate macaroons.

About Dr. Brandler: Dr. Justin Brandler is a gastroenterologist at Virginia Mason with an interest in neurogastroenterology and motility. He completed his fellowship at the University of Michigan in 2022 and is a member of the ACG Institute’s 2023-2024 Emerging Leadership Program cohort. Dr. Brandler is noted for his commitment to the importance of empathy in the patientdoctor encounter and chronicled his efforts to understand the patient experience and develop empathy by undergoing a series of common tests and procedures in GI. His “GI Empathy Initiative” experience was published in ACG MAGAZINE in 2022. Explore: bit.ly/ GI-empathy-initiative
“ Boo Can’t Poo uniquely strikes a Bristol 4 type balance of substance and style. ”


Brandler Family book reviewers in action. Photo Credit: Sarah Brandler.
Listen to Learn More
Jacqueline Gaulin (AKA Gastro Girl) recorded podcast conversations with the authors of our featured new books.
Listen to interviews with the authors:
Kate Scarlata and Dr. Megan Riehl gastrogirl.com/podcast/how-do-i-livewell-with-ibs
Dr. Austin Chiang gastrogirl.com/podcast/ your-gut-health-fact-vs-fiction
Dr. James Tabibian gastrogirl.com/podcast/whats-wrongwith-my-gut
Dr. Xiao Jing "Iris" Wang gastrogirl.com/podcast/how-do-i-talk-tomy-child-about-constipation
Check out the rest of the Gastro Girl podcast series, some of which were produced in collaboration with the ACG Patient Care Committee Listen: gastrogirl.com/podcasts
Leadership Reads & Fun Fiction
Explore this list of book recommendations to enhance your professional life and add to your reading list of fun fiction. Crowdsourced from among the distinguished participants in the 2022 and 2023 cohorts of the ACG Institute’s Advanced Leadership Program, this varied list includes meaningful insights and thought-provoking picks to inspire your next read.

How
to
Know A
Person, The Art of Seeing Others Deeply and Being Seen Deeply by David Brooks (Random House, 2024) Wisdom is not just about knowing. It is about deep listening and relating. It is about allowing the other side to be seen and to be vulnerable. This book presents principles that lead towards more authentic communication and connection. A key to more effective leadership.

Rami Abbass, MD, MBA, FACG Partner, University Gastroenterology Associates; Assistant Medical Director, The Endoscopy Center at Bainbridge, Solon, OH

For Leadership books, I have two classics. First, How to Win Friends and Influence People by Dale Carnegie (Simon & Schuster, 1936). It seems like these are simple concepts, and should be intuitive, but very
helpful in talking to people in general, which is useful for any leader. Also, knowing which battles to win on our end vs. letting others win. How to Win Friends and Influence People really should be read by every person on this planet and should even be recommended in school!

Second, The Law of Success by Napoleon Hill (Tribeca Books, 1928). Also an old book, but the concepts within are quite useful, from making sure you have a “definite chief aim” in life, to guidance on initiative and leadership, as well as the importance of enthusiasm for the work we do, concentration, co-operation, and creating a habit of doing more than paid for that ultimately leads to even gains that we may not have expected!

Fun read: Covenant of Water by Dr. Abraham Verghese (Grove Press, 2023). This is an amazing story spanning generations in a beautiful state of India called Kerala (personal input: where I grew up and this brought me back
memories) and features a medical condition that took an inspiring young woman to become a neurosurgeon to decipher it in her family members.

Bincy P. Abraham, MD, MS, FACG Professor of Clinical Medicine, Houston Methodist Academic Institute; Professor of Clinical Medicine, Weill Cornell Medical College; Adjunct Professor of Clinical Education, Texas A&M University, College of Medicine; Director, Gastroenterology Fellowship Program, Houston Methodist; CoDirector, IBD Advanced Fellowship Program; Distinguished Professor and Director, Underwood Center -Fondren Inflammatory Bowel Disease Program; Houston Methodist Gastroenterology Associates, Houston, TX

Leadership Read: The book Act Like a Leader, Think Like a Leader by Herminia Ibarra (Harvard Business Review Press, 2015) helped me refocus my leadership efforts to lead with greater impact. It challenged my outdated perception of a successful leader, allowing me to evolve my leadership style. It also encouraged me to diversify my network and helped me remain comfortable asking, “What can we do?” when hitting a wall or when someone says something is impossible. This is a powerful reframe that gets me unstuck when a leadership challenge arises.
How to Win Friends and Influence People really should be read by every person on this planet and should even be recommended in school!

For fun fiction, I recently finished Kristin Hannah’s book, The Women (St. Martin’s Press, 2024). It is an engrossing and captivating telling of combat medicine from the perspective of a Vietnam War surgical nurse. After reading the book, I discussed it with a friend, a combat veteran who served in Iraq as an Emergency Medicine physician. She assured me the author accurately recounted the harrowing day-to-day activities of those who ensured soldiers and sailors got home to their loved ones and the oftenforgotten psychological toll of combat medicine on the nurses and doctors who served.

Neena S. Abraham, MD, MSc (Epid), MACG Professor of Medicine, Mayo Clinic Arizona; Director, ACG Institute for Clinical Research & Education

Crucial Conversations: Tools for Talking When Stakes are High, Third Edition, Joseph Grenny, Kerry Patterson, Ron McMillan, Al Switzler, Emily Gregory (McGraw Hill, 2021). This book has significantly enhanced my ability to lead and inspire my team. The book's insights into managing high-stakes conversations have been crucial in addressing sensitive issues, mediating conflicts, and fostering a culture of open communication and trust. By applying its strategies, I've been able to guide my team through challenging situations, ensure alignment on goals, and facilitate collaborative problemsolving. This has not only improved team morale and cohesion but also strengthened our collective ability to deliver high-quality patient care.

Tauseef Ali, MD FACG Medical Executive Director, SSM Health Digestive
Care and SSM Health Crohn's and Colitis Center, Oklahoma City, OK

I really enjoyed Sally Helgesen's book, How Women Rise (Hachette Books, 2018) (and loved meeting her at the Scrubs & Heels summit in 2023!). She reviews 12 habits professional women often have that can hold them back from achieving their career goals. I recognized myself in several of the real-life case scenarios she uses to illustrate these habits, and it was almost shocking to finally become aware of some self-limiting behavior, whether it is expecting others to spontaneously notice our hard work and reward our contributions or failing to enlist allies from day one of the job and to leverage relationships. But more importantly, Helgesen encourages and guides a shift in mindset and behavior to put forward our leadership potential and offers actionable steps to achieve professional growth. One piece of advice that particularly resonates with me is: "Do not put your job before your career" –don't limit yourself to perfecting the task at hand, think bigger and forward, then pursue opportunities that will position you for a future of growth and success!

Aline Charabaty, MD, FACG Associate Professor of Medicine, Johns Hopkins School of Medicine, Division of Gastroenterology & Hepatology, Washington, DC; ACG Governor for Washington, DC

Leading Change by John Kotter (Harvard Business Review Press, 2012) outlines the common cause of failure when implementing change and lays out eight concrete processes to
implement change step by step. I have been using these strategies in my recent projects and find them very useful. Helping team members clearly see the vision and future empowers everyone on the team to make the change successful. Change by top-down approach, without team engagement, rarely works.


Chien-Huan Chen, MD, PhD, FACG Professor of Medicine; Associate Director of Clinical Affairs; Director of General Gastroenterology; Director of Patient Safety and Quality; Director of Small Bowel Endoscopy, Washington University School of Medicine in St. Louis How to Raise Successful People: Simple Lessons for Radical Results by Esther Wojcicki (Mariner Books, 2019). I started reading this book to get tips on parenting, but it ended being a very motivating leadership book for me. It is written by Esther Wojcicki, a high school journalism teacher at Palo Alto High. She discusses her novel and innovative teaching methods that she has used for decades to build confidence, grit, and leadership qualities in high schoolers and her daughters. This book has taught me the importance of Trust, Respect, Independence, Collaboration, and Kindness which she calls "TRICK" in developing one's leadership model. Self-control and responsibility are important values not only for children but for anyone in any stage of life, especially a leader. This book has taught me that failure is not something to be afraid of, rather something to be expected as a part of learning. In fact, there is no learning without failure. Delayed gratification and self-control are qualities that help one build grit, and yes, grit
is teachable and buildable at any stage of life. This book stresses the importance of 'not dictating' and the value of collaboration and the impact of modeling for everyone around us, all things that we discussed in the leadership course.

I thoroughly enjoyed reading Lessons in Chemistry: A Novel by Bonnie Garmus (Doubleday, 2022). This is a story about a highly intelligent woman scientist in the early 1960s, who had to carve her way through the masculine world of scientific research. The fearless path that she takes to achieve her research goals and to make sure that she is noticed for her intellect, knowledge, and hard work and not just her pretty looks is something to admire. Her resilience and grit as she navigates the male-dominated world is truly inspiring. Though it is fiction, this book actually teaches leadership qualities through its protagonist.

Swapna Gayam, MD, FACG
Associate Professor of Medicine; West Virginia University Medicine, Morgantown, WV

A definite must-read from my perspective is Give and Take by Adam Grant (Penguin Books, 2014). Adam Grant is a social psychologist at Wharton. The book speaks to how those in leadership who focus on developing people and helping other individuals achieve their true potential, tend to be the most successful and impactful in organizations and in achieving their goals as well as personal and professional satisfaction. Giving to others is a gift that never stops reaping rewards for everyone.

David J. Hass, MD, FACG
Associate Clinical Professor of Medicine, Yale University School of Medicine; Medical Director, PACT Gastroenterology Center, a Partner of HHCMG, Orange, CT



Full Steam Ahead! by Kenneth H. Blanchard & Jess Stoner (MJF Books, 2011). Goofy name, but it is really short and about how to write a good vision statement.
Leadership and SelfDeception by the Arbinger Institute (Berrett-Koehler Publishers, 2018). A great read about how to identify in yourself where you might fall into traps about being an effective leader.
For fun but also about leadership: Eleven Rings: The Soul of Success by Phil Jackson (Penguin Books, 2013). He was the coach of the Chicago Bulls during their amazing six championships in eight years and then with the LA Lakers and winning more championships there. It is about leadership, dealing with superstar athletes, sports, and how to stay sane.

Sunanda V. Kane, MD, MSPH, FACG
Professor of Medicine, Mayo Clinic, Rochester, MN; ACG Past President (2018-2019)

Exceptional Leadership: 16 Critical Competencies for Healthcare Executives, 3rd Edition, Carson F.Dye and Andrew N.Garman (ACHE Management Series, 2024). This is an outstanding book describing 16 important
and practical leadership competencies organized into four cornerstones: (1)Well-cultivated Self Awareness; (2)Compelling Vision; (3) Masterful Execution; and (4) A Real Way with People. Each chapter follows a similar format: a competency is defined; how effective leaders use that competency; misuse and overuse of that competency; and how to improve in that competency.
I recently read this book cover to cover in a Change Management course and this book, along with Kotter's classic Leading Change from 1996, are essentially the only two leadership change management books one needs to master this topic. These books complement each other well. I will refer back to Dye and Garman's book Exceptional Leadership for years to come; there is so much leadership wisdom in those pages.

Costas H. Kefalas, MD, MMM, FACG
President, Akron Digestive Disease Consultants, Inc., Akron, OH; ACG Treasurer

I would like to suggest Jonathan Livingston Seagull by Richard Bach (Macmillan, 1970) as a leadership read. This book has been influential in my leadership journey.
Jonathan Livingston Seagull is a story about a seagull who is not content with simply following the flock. He is determined to learn how to fly faster and higher than any other seagull. In his journey, he discovers the importance of self-discovery, perseverance, and the pursuit of excellence.
I was inspired by Jonathan's determination and willingness to challenge the status quo. He taught me that true leadership is about more than just getting the job done. It's about inspiring others to reach their full potential and to never give up
on their dreams. I highly recommend Jonathan Livingston Seagull to anyone who is looking for a book that will challenge them to think differently and to strive for greatness.

For fun fiction, I highly recommend A Gentleman in Moscow: A Novel by Amor Towles (Penguin Books, 2016). This beautifully written novel tells the story of Count Alexander Rostov, a former aristocrat who is forced to live in a hotel by the Bolshevik Tribunal. Despite his circumstances, Rostov maintains his dignity and grace, and his story is both heartwarming and inspiring.

Sumana Moole, MD Merus Gastroenterology & Gut Health LLC, Suwanee, GA

I would suggest Amy Edmondson’s books, Teaming (JosseyBass Pfeiffer, 2012) and The Fearless Organization (Gildan Media, 2020). Both books are fantastic examples of leadership activities that result in increased efficiency, accuracy, and support for an organization’s mission. Here is a link to a video summarizing The Fearless Organization. I was in the audience at the AAMC meeting for this presentation and many people were blown away by the lecture. I cannot summarize how impressive this concept is, thus the reason for sharing the video. See vimeo.com/373045969.

For leisure and inspirational reading: When Breath Becomes Air by Paul Kalanathi (Random House, 2016, Pulitzer Prize Finalist). The book is a story about living while dying shortly after residency training.

Abraham Verghese’s book Cutting for Stone (Vintage, 2010) is a wonderful story of an immigrant, humanity, medicine, and a family saga of Africa and America. Cutting for Stone comes from the original Hippocratic Oath that cautions against this practice due to the high risk of death to remove bladder stones.
Honorable Mentions:
• Atul Gawande, Being Mortal (Metropolitan Books, 2014) The effects of aging and how we compensate for the changes.
• John Barry, The Great Influenza (Penguin Books, 2005) The great flu of 1918, which parallels COVID.
• Robert M. Edsel and Bret Witter, The Monuments Men (Center Street, 2009) Saving the priceless works of art in Europe during World War II.

James D. Morris, MD, FACG Assistant Dean for Graduate Medical Education and VA Affairs; Professor of Medicine, LSU Health, Shreveport, LA
of the time when her child had lice, managing that crisis while traveling. I both laughed and cried reading that, recalling when my middle child, who was a toddler at that time, came home from daycare with lice, spreading it to me, pregnant at the time with our daughter. The weeks of mayonnaise treatments, lice combs, and obsessive washing followed by a lifetime of tea tree oil behind my children’s ears and putting the fear of God in them of trying on hats resulted. This book made me realize with that example and many others that I was not alone in these challenges while simultaneously working, leading, and parenting. A key take-away from this book is that at times in women’s lives (or anyone’s life) when they may think about leaning out (such as before a maternity leave, other leave of absence), those are the times to “lean in” given it will make the returnto-work more enticing if there is a fantastic new path ahead.

Leadership books: There are so many fantastic leadership books that have been influential such as How Women Rise, Crucial Conversations, and many others that have been detailed elsewhere in this review. Here are a few I will call out.

Lean In: Women, Work, and the Will to Lead by Sheryl Sandberg (Knopf, 2013). This was a book I read years ago, and its impact was profound. It was one of the early books to highlight women in leadership and C-suite positions. As women who aspire to leadership, we often observe others and marvel at how they make it look so easy at times, leading with fluidity and grace. Sheryl Sandberg keeps it real and is candid about some of the day-to-day challenges she faced, many of which we have as well. I remember her detailed recollection
Athena Rising by W.Brad Johnson and David G. Smith (Harvard Business Review Press, 2019) is an incredible read. Its goal is to share “How and Why Men Should Mentor Women.” Following the #MeToo movement, so many male colleagues raised concerns about mentoring women, for fear that they would be the target of such harassment accusations. This, unfortunately, added even more barriers to women finding mentorship. This book is a no-nonsense guide for men on addressing those concerns, while highlighting the ever-important role that men can play in the career advancement of women. In a specialty like GI that is so male-predominant, the success of women in GI is heavily dependent on the mentorship and sponsorship by our male colleagues. This book is great for men and women alike. I have also been fortunate enough to hear these authors speak, and they are fantastic! Sharp, witty, and spot on!
Fiction Reads: “Hello, my name is Amy Oxentenko, and I have a book hoarding addiction.” Laugh as you may, but it is true! I LOVE to read, and my nightstand has a stack of books so high that I want to read such that they now also fill the top drawer of my nightstand. Nooks and e-readers are convenient for travel, but nothing beats the feel of a book in the hand. I literally have a library at home, organized by author, genre, etc. I could write a book – on my love of books.

My favorite recent author is Freida McFadden, who tends to write psychological thrillers. Each of her books has an unexpected plot twist that you do not see coming, akin to Gone Girl. She has dozens of titles, but some of my favorites are The Housemaid (Poisoned Pen Press, 2024), The Wife Upstairs (2020), Never Lie (Thorndike Press, 2024) and The Coworker (Poisoned Pen Press, 2023). Other authors who write psychological thrillers that I enjoy are Ruth Ware, Mary Kubica, and Harlan Coben.
For the runners out there, a few mustread books (which are actually great as audio books while running) include: Finding Ultra by Rich Roll (Harmony, 2012), Good for a Girl by Lauren Fleshman (Penguin Press, 2023), and The Longest Race by Kara Goucher (Gallery Books, 2023).

Amy S. Oxentenko, MD, FACG Professor of Medicine; Vice Dean of Practice, Mayo Clinic, Rochester, MN; President-Elect, American College of Gastroenterology
of the “10,000-hour rule.” While some of us are naturally good at something, most of us need to commit the time and effort to excel in our fields.
Fiction: I recommend author Anne Holt whose detective mysteries read like the TV show Law and Order. Love the setting in Norway.

Remarkably Bright Creatures by Shelby Van Pelt (Ecco, 2022). Even though this is a fictional work, there are so many takeaways to life that I loved the ups and downs of the book, beautifully written.

Shireen A. Pais, MD, FACG Advanced Physicians and Surgeons, Valhalla, NY


How Women Rise: Break the 12 Habits Holding You Back from Your Next Raise, Promotion, or Job by Sally Helgesen (Hachette Books, 2018) and Lead: How Women Claim Their Authority by Ellen Snee (She Writes Press, 2021).
Both of these books inspired me to continue on my own professional development and how to be strategic.

Nimisha K. Parekh, MD, MPH, FACG, AGAF Clinical Professor of Medicine; Director of Inflammatory Bowel Disease, Digestive Health Institute; Associate Dean of Faculty Development, University of California Irvine

Nonfiction: Malcolm Gladwell's Outliers: The Story of Success (Little, Brown and Company, 2008). This book introduces the concept

Leadership book: True North, Emerging Leader Edition: Leading Authentically in Today’s Workplace by Bill George and Zach Clayton (Wiley,
2022). At its heart, it is a book about following your internal compass, the idea that true leadership comes from being authentic with a strong sense of self – understanding one’s strengths and weaknesses and being honest about them. Exceptional leaders lead with purpose and integrity and surround themselves with a support team of mentors, peers, and family members who help guide them along the way. It is about aligning your leadership style with your values and beliefs and sticking with them even in tough situations.

Fun book: The Wager: A Tale of Shipwreck, Mutiny and Murder by David Grann (Doubleday, 2023). It is the story of the HMS Wager, its shipwreck off the coast of Patagonia in 1741, the crew’s survival, a mutiny, a rescue, and the inquiry with contrasting accounts of the events when they returned to England.

Murtaza “Kittu” Parekh, MD, MPH Raleigh Endoscopy Center, Raleigh, NC

Two leadership books that go hand-in-hand by Simon Sinek: Start with Why (Portfolio, 2011) and Leaders Eat Last (Portfolio, 2017).
For each aspect of our lives, understanding and communicating the "why" is important – and even more so in leadership positions. In medical care, creating a shared decision-making environment with patients entails not just explaining the possible evaluation/ medical plan in terms of the "what" and "how," but also the "why." From a personal side as a parent of teenagers, explaining the "why" of decisions to teenagers can lead to deeper
understanding and fruitful discussions. For those "non-readers," you can check out the TED talk or podcast!


Leaders Eat Last (Portfolio, 2017). Servant leadership.
My experience has taught me that taking risks, not being afraid to make mistakes, and jumping in before you feel ready are the best ways to learn and grow!
Fun read: The Henna Artist, Alka Joshi (MIRA, 2021). A captivating story of a woman in Jaipur, India, in the 1950s going through life with curveballs thrown in, adapting to each with grace – that's life!

Bryan G. Sauer, MD, MSc, FACG
Professor of Medicine, University of Virginia, UVA Health, Charlottesville, VA

As a parent and a leader, I loved Hidden Potential: The Science of Achieving Greater Things by Adam Grant (Viking, 2023). There are many pearls in this book, and I share two that spoke to me: “Character is your capacity to prioritize your values over your instincts.” Our values are our compass and as a parent, teacher, and leader, this resonated with me.
“Becoming a creature of discomfort can unlock hidden potential in many different types of learning. Summoning the nerve to face discomfort is a character skill— an especially important form of determination. It takes three kinds of courage: to abandon your triedand-true methods, to put yourself in the ring before you feel ready, and to make more mistakes than others make attempts. The best way to accelerate growth is to embrace, seek, and amplify discomfort.” – Adam M. Grant, Hidden Potential: The Science of Achieving Greater Things

Shivakumar Vignesh, MD, FACG Professor, Internal Medicine; Banner MD Anderson Cancer Center, University of Arizona College of Medicine-Phoenix; Adjunct Professor, MD Anderson Cancer Center, Houston, TX

Whistling Vivaldi: How Stereotypes Affect Us and What We Can Do by Claude M. Steele (W. W. Norton & Company, 2011). This book was recommended to me after I made a comment on the lack of proactivity in a medical student compared to their peers. What I truly appreciated is that this work is grounded in research around "stereotype threat." This book offers insight into how individual performance can be impacted positively or negatively by certain stereotypes and was quite eyeopening, to be honest. I highly recommend it.

Renee L. Williams, MD, MHPE, FACG
Associate Professor of Medicine and Associate
Chair for Health Equity, NYU Langone Health; ACG Trustee
Charles “Tremendous” Jones, renowned author and leadership consultant, once said, “You will be the same person in five years as you are today except for the people you meet and the books you read.” I could not agree more! The books below profoundly impacted me. I hope you find them useful on your journey as well.

From Strength to Strength: Finding Success, Happiness and Deep Purpose in the Second Half of Life by Arthur C.Brooks, (Portfolio/ Penguin 2022). Brooks, the William Henry Bloomberg Professor of the Practice of Public Leadership at Harvard’s Kennedy School, aims this book at ambitious strivers who have succeeded mightily in the first half of their lives. (Sound familiar…?)
Brooks’ goal is to teach the reader that the skills for success in the second half of life are markedly different than in the first. To succeed, we need to shift from reliance on fluid intelligence, which starts to fade in our 30s, to crystallized intelligence (i.e., wisdom). As we seek a life which is both enjoyable AND meaningful, we should become less self-absorbed, more willing to dare, and increasingly focused on legacy values rather than resume values.

Demon Copperhead by Barbara Kingsolver (Harper Collins, 2022). This Pulitzer Prizewinning novel explores the influence of place, perception, and poverty on everything from an individual boy’s journey to manhood to the opioid crisis in America. At turns both comic and confounding, there is never a dull moment!

Patrick E. Young, MD, FACG Professor of Medicine, Uniformed Services University of the Health Sciences, Bethesda, MD; Director of the Digestive Health Division, Walter Reed National Military Medical Center; ACG Trustee

Douglas G. Adler MD, FACG Director, Center for Advanced Therapeutic Endoscopy (CATE) at Centura Health-Porter Adventist Hospital, Salt Lake City, UT

The Little GI Book: An Easily Digestible Guide to Understanding Gastroenterology (Slack Books, 2020)

William J. Bulsiewicz, MD, MSCI
The Plant Fed Gut Mt. Pleasant, SC Fiber Fueled (Avery, 2020)

The Fiber Fueled Cookbook (Avery, 2022)

Emeran Mayer, MD Director, UCLA Gail and Gerald Oppenheimer Family Center for Neurobiology of Stress Professor, Psychology Medicine Co-Director, CURE: Digestive Diseases Research Center Professor, Physiology

Interconnected Plates: A Mediterranean-Inspired Gut Healthy Cookbook (Friesens Corporation, 2023)

The Mind-Gut-Immune Connection: Understanding How Food Impacts Our Mind, Our Microbiome, and Our Immunity (Harper, 2023)


Roshini Rajapaksa, MD Clinical Associate Professor, NYU Grossman School of Medicine
Gut Renovation (William Morrow, 2022)
ACG VIRTUAL GRAND ROUNDS
Weekly on Thursdays at 12 pm and 8 pm ET
Live Presentation by an ACG Expert Plus Q & A #GIhomeschooling











































Even as all aspects of practice have changed due to COVID-19, your need to stay up to date on clinical GI does not stop. ACG is committed to your professional education. Our goal is to help the GI community embrace #GIhomeschooling with quality speakers and presentations.
ACG has launched Virtual Grand Rounds weekly on Thursdays at 12 pm and 8 pm ET. Each week an expert faculty member will present live on a key topic followed by Q & A.
Learn More and Register: GI.ORG/ACGVGR
Culinary Connections:
by Vani Paleti, MD; Alexander Perelman, DO & Christina Tennyson, MD
Fusion Flavors for Fall of
WELCOME TO A FUSION OF FLAVORS THIS FALL FROM OUR AMAZING ACG FOODIES CONTRIBUTORS. Get ready to enjoy the fusion of flavors from cultures across the world. Food not only nourishes our body, but it also brings us together through the stories we share, and the connections we make that nourish our mind and soul.
Culinary connections become memories that bring a big smile when we get a whiff of that smell or taste of that flavor, bringing back flurries of warm memories of good times.
What are we waiting for? Let's dive into Dr. Blaney’s one-pot lentil stew, Dr. Elshaer’s recipes for Egyptian street foods, Kitchari and Hawashi, and Dr. Sleiman’s Shish Barak dumplings. Enjoy!
— Alex, Christina, and Vani

JOSEPH SLEIMAN, MD
Cleveland Clinic Foundation, Cleveland, OH
Cooking for others is undoubtedly the biggest pleasure for an Arab child maturing into adulthood. We may hate it at first, but something about remembering your culture of hospitality, welcoming a big crowd into your house, and sharing stories (sometimes gossip) as you share a wellcooked meal, just brings back an untapped joy for many of us.
What’s even better is inviting people who have never tried your culture’s meals before, and seeing the delight in their eyes as they take their first bite. It’s the closest to being back in your grandmother’s kitchen trying her dishes for the first time.
While some dishes are more daring than others, Shish Barak is the one that everyone loves to eat, but hates to
SHISH BARAK
Ingredients:

–
make. It is a delicious Middle Eastern homemade meat-stuffed dumpling cooked in yogurt and has roots in Iranian and Armenian cultures. Think of it as the ravioli of the Middle East, but the stuffing is minced meat, and the sauce is yogurt-based.
However, I recently found a hack through a Syrian Canadian cook’s Instagram page (@breakingbreadwithbayan), and it changed the game for me! I know a bunch of friends might very well revoke my Arab title for this hack, but hear me out!
Instead of making, rolling, and shaping her own dough, she used wonton wrappers. They are essentially made of flour, water, and salt, the same ingredients as Shish Barak dough! The only difference is that the wonton wraps are rolled a bit
thinner and might be a bit bigger than traditional dough, but that’s a sacrifice I’m willing to make to get the dish on the table in a fraction of the time and effort! Everything else has the same texture and taste. And trust me, your partners/guests won’t know the difference. Of note, you can also use dumpling wrappers which are round and end up looking closer to the Shish Barak traditional dough shape.
Since trying this hack, I am now sworn to only making it this way, so give it a try. Thank you, Bayan’s Kitchen, for this hack. <3
And yes, different villages made it slightly differently (or, according to them, better), and that’s the beauty of it. This is the most barebones version to start with.
DUMPLING VERSION | SERVES 4-6 PEOPLE (BECAUSE ARABS DON’T COOK FOR ONE)
Steps:
• 400g wonton or dumpling wrappers
Filling
• 1 Tbsp olive oil
• 1 lb. ground beef (you can try vegan protein alternatives too)
• 1 medium onion, diced finely
• 1 tsp salt
• 1/4 tsp black pepper
• 1 tsp 7-spice
• Optional: Roasted Pine Nuts
Yogurt Sauce
• 1.5 L plain yogurt
• 1.5 Tbsp cornstarch
• 2 tsp salt
• 1 cup cold water
• 3 Tbsp olive oil
• 6 garlic cloves, minced
• 1 Tbsp dried mint
• Optional: Roasted Pine Nuts
1. Cook the ground beef in olive oil until no longer pink, then add the onion and cook until softened. Add salt, pepper, and 7-spice, and cook until the liquid is all gone. Set aside until cooled completely. Optional: you can add roasted pine nuts, parsley, paprika, or other flavors to taste, usually according to how your mom/aunty tells you they do it back home.
2. Place ½ Tbsp (not more, trust me) of the meat mixture into the center of each wonton wrapper. Dip your finger into water and rub it against each edge of the wrapper. Fold over the wrapper to the opposite edge and pinch the seals shut, forming a wedge shape. Then wet the remaining corners and fold over the wrapper one more time. Press firmly to seal. Make sure to keep both the wonton wrappers and the filled dumplings covered with a towel or plastic wrap while you’re working so they don’t dry out and crack.
3. Bake in a single layer at 375°F for 10-15 minutes or just until it begins to turn golden. Set aside.
4. While waiting, whisk together plain yogurt, cornstarch, salt, and water in a pot until smooth, then turn on the heat and whisk continuously until it comes to a boil. Do NOT stop whisking until it comes to a boil or the yogurt will split. Then, lower the heat to low and add the baked dumplings.
5. Sauté the minced garlic and dried mint in olive oil until slightly browned and fragrant. Add to the yogurt. Add salt to taste. Let it all simmer for 5-10 minutes or until the dumplings are plump. Top with toasted pine nuts or almonds and serve with green onions and enjoy.














MAHASEN
AKRAM ELSHAER, MRCP, UK
King Fahad Military Medical Complex, Saudi Arabia
My interests are preparing healthy foods for my family, swimming, and running. My best moment is watching my family or my friends smile after preparing a delicious meal. I have two popular street Egyptian foods to share: Hawashi and Koshari.
About Hawashi: Hawashi is popular particularly in Cairo and Alexandria (where they call it Baladi). It is basically dough (or pita) stuffed with a mixture of ground beef that is seasoned with tantalizing warm spices, onions, garlic, hot peppers, and fresh herbs. Legend has it that one butcher by the name of Ahmed AlHawash in Cairo’s Tawfeek Souq came up with this sandwich back in the early
HAWASHI AND KOSHARI
Hawashi Ingredients:
• 4 pieces pita bread, cut in half
• 1 Tbsp Mediterranean olive oil
• 1 lb. ground beef
• 1½ tsp kosher salt
• 1/2 tsp freshly ground black pepper
• 1/2 cup finely chopped yellow onion
• 3 Tbsp finely chopped parsley
• 1 Tbsp chopped Calabrian chilies, optional
• 1/2 tsp ground cumin
• 1/2 tsp garlic powder
• 1/4 tsp ground coriander
• 1/4 tsp ground allspice
• 1/2 tsp smoked paprika
• 1/8 tsp ground cardamom
• 1/8 tsp ground cinnamon
Steps:
• The ground meat should be heated until well done at least 250 degrees for 25 minutes.
• Enjoy with pita bread
1970s and gave it his name. The idea has traveled throughout parts of Africa and the Middle East (in Lebanon, another version of this sandwich is called Arayes).
The Origins of Koshari: Though no one knows for sure where Koshari came from, most people in Egypt believe that Kitchari— an Indian dish of lentils and basmati rice— may have inspired the beloved Egyptian meal. It’s possible that Indian soldiers, who arrived with Britain’s occupation of Egypt in the late 1800s, brought Kitchari with them. Some say the dish has Italian influences, too, as Egyptian Koshari has two distinctly Italian staples: pasta and tomato sauce. To make the dish their own, Egyptians drizzled Da’ah, a tangy garlic and vinegar sauce, and Shatta, a spicy chile and garlic sauce, onto it. Today, variations of Koshari, including Mujaddara or Mejadra—a similar meal of basmati rice, black lentils, and caramelized onions—are eaten throughout the Arab world.

HANNA BLANEY, MD, MPH
Georgetown University
Medstar Health, Washington, DC
I grew up in a small town in Arizona with a mother who is a phenomenal cook. Despite working full time, she would make my family delicious and nutritious meals daily and we would sit together nightly as a family of four to enjoy our meal. While my mother grew up in the northeast eating mostly Italian- and French-inspired food, she became an adventurous chef and expanded to make us from-scratch meals inspired by Mexican to Chinese cuisine.
With her as my model, I have always loved cooking and putting together my own recipes. When I was in 4th grade, I created a recipe for a fruit
Koshari Ingredients:
• 3/4 cup brown lentils
• 4 cups water
• 3/4 cup uncooked long grain rice
• 1 cup elbow macaroni
• 2 Tbsp vegetable oil
• 2 large onions, chopped
• 4 cloves garlic, minced
• 1 15.5 oz. can diced tomatoes
• 1/4 tsp red pepper flakes, or to taste
• Salt and pepper to taste
Steps:
1. Combine the lentils and water in a large saucepan. Bring to a boil, then simmer over medium heat for 25 minutes.
2. Add the rice to the lentils, and continue to simmer for an additional 20 minutes, or until rice is tender.
3. Fill a separate saucepan with lightly salted water and bring to a boil.

4. Add the macaroni and cook until tender, about 8 minutes. Drain.
5. Meanwhile, heat the vegetable oil in a large skillet over medium heat.
6. Add onion and garlic; cook and stir until onion is lightly browned.
7. Pour in the tomatoes and season with red pepper flakes, salt, and pepper.
8. Simmer over medium heat for 10 to 20 minutes.
9. In a large serving dish, stir together the lentils, rice, and macaroni.
10. Mix in the tomato sauce until evenly coated.







tart inspired by several recipes from my mother’s Gourmet magazine and The Joy of Cooking. I sent the recipe into our state’s newspaper and it was published a few weeks later! Since then, I have enjoyed coming up with recipes (and almost never use measuring spoons), with most turning out pretty well. While I will occasionally follow recipes, I often create my own after being inspired by a meal.
Prior to medical school, I had the opportunity to travel extensively and enjoy many cultural foods. Coming home from these trips, I would experiment with new spices, trying to replicate the flavors of my travels. In medical school, I married into a multicultural family, and we have since blended the foods of Central America and the Middle East.
eating as best we could. From my trips to India, dal became a staple, as did my father’s southwestern pinto bean recipe. Out of necessity and convenience, legumes became a central part of our diet.
As a gastroenterologist and hepatology fellow serving many lower-income patients with obesity and MASLD, I have worked to incorporate lifestyle interventions, including encouraging my patients to experiment with legumes. I have shared recipes for lentil soups as well as “frijoles sin grasa,” with several of my patients successfully incorporating legumes into their diets.
We would like to hear from you if you have personal connections with GI & gastronomy. Contact ACG magazine staff by email at acgmag@gi.org to share your story with the ACG community. You can also tweet using #ACGfoodies to connect with the community.
While in medical school and married to a then surgical resident, we did our best to stretch out our budget while
As a busy fellow mom married to an equally busy surgeon, nutritious, easy, and tasty meals are a must. One-pot meals with minimal prep and minimal clean up are even better. The meal I will share with you has become a staple for our family as it can be thrown together with food from the pantry as well as can help us clean out our refrigerator. Bonus: Leftovers make for a fantastic lunch!
ONE POT LENTIL STEW FOR BUSY NIGHTS
Ingredients:
• 1 Tbsp of olive oil
• 1 Tbsp cumin (or more, to taste)
• 1 tsp paprika (or more, to taste)
• 1 6 oz. can tomato paste
• Garlic (2-3 cloves, diced)
• 1 lb. lentils
• 6-7 cups of water or vegetable broth
• 5-6 dried dates or apricot (diced)
Steps:
1. In a large pot over medium heat, heat up olive oil.
2. If you are adding in fresh vegetables like carrots or zucchini, add them in here and sauté for a few minutes.
3. Then, add the tomato paste, garlic, cumin, and paprika and stir.
4. Once the spices become fragrant, pour in the water or broth and add the lentils.
5. Bring to a boil.
6. Add dates or other dried fruit and then let the lentils simmer for 20 minutes.
• Optional: A dash of coriander and/or cinnamon
• Optional: Veggies (carrots, zucchini, spinach)
• Optional: Kalamata olives
For Serving
• Greek yogurt
• Lemon (zest and juice of 1/2)
• Salt, to taste
7. If you want to add something like spinach, stir the spinach in at the last stage.
8. Finish with the juice of ½ lemon, consider a drizzle of olive oil.
9. For a topping, stir lemon zest into the Greek yogurt and enjoy!









Learn from successful GI innovators and unpack learnings and pitfalls
process






When Victoria Louwagie, a Physician Assistant with Mayo Clinic Health System, invited members of the ACG Advanced Practice Providers Committee to share a “day in the life” with ACG MAGAZINE, her fellow APP colleagues delivered brilliantly, sharing diverse and wide-ranging experiences. While there is no “typical day” among the group, there are clear themes and commonalities.
APP Committee Chair Monica Nandwani summarized it best, “Every day is different with each day offering unique opportunities for collaboration with a wide range of individuals, a variety of challenges, and different avenues for new learning and contribution.”
Across the U.S. and spanning different clinical settings, these reflections from ACG APP members reveal vibrant and varied professional experiences and a deep commitment to improving digestive health. While some have academic roles and administrative responsibilities, all have unique and valuable perspectives on the role of APPs in the GI care team.
No Such Thing as Typical: A DAY IN THE LI FE OF APPS IN GI



VICTORIA LOUWAGIE, DMSC, MS, PA-C, DFAAPA
Physician Assistant, Mayo Clinic Health System, Mankato, MN; Assistant Professor of Medicine, Mayo Clinic College of Medicine and Science
At Mayo Clinic Health System, we embrace clinical care, education, and research. I have been afforded the amazing opportunities to participate and lead in each of these arenas. Within this growing GI practice, typically my workday is mostly driven by providing digestive healthcare for patients within my community. For over a decade as a PA in GI, with physician collaboration, I have provided expert GI care in the clinic, to hospitalized patients and to outreach locations.
I am actively involved in pre-NP/PA education. I never say “no” to a pre-NP/ PA student shadower! Come see, firsthand, the best professions. (See “Nurse Practitioner #1 in Best Job, Career Rankings, Salary, Reviews and Advice; U.S. News Best Jobs” and “PA Named #2 Best Health Care Job by U.S. News & World Report - AAPA.”)
I also find great fulfillment in providing medical education to graduate students. Several times a year, the Mayo Clinic Health System Division of Gastroenterology accepts graduate-level NP/PA students for their elective clerkship/rotation. Precepting students has been shown to increase clinicians' connections and engagement in their work, and I could not agree more. These students keep me up-to-date on the most current evidence-based practices. I am fortunate to be the Director for the Mayo Clinic PA Program Adult and Pediatric Medicine Gastroenterology Block. Through modern GI medical education and curricula, these students learn about digestive health utilizing small group, hands-on learning and virtual reality simulation to enhance critical thinking. APPs can provide exceptional GI care. I also serve as an NP/PA Supervisor providing administrative support to 14 NP/PAs. It has been incredibly satisfying to welcome new graduate NP/PAs into the profession and watch them grow into practitioners
Victoria Louwagie, DMSc, MS, PA-C, DFAAPA; Monica R. Nandwani, DNP, RN, FNP-BC; Amy L. Stewart, FNP-C; Jason J. Thomas, DPAS, MPAS, PA-C; and Amanda B. Wilhite, MPAS, PA-C.
“Every day is different with each day offering unique opportunities for collaboration with a wide range of individuals, a variety of challenges, and different avenues for new learning and contribution.”
who practice to the top of their scope of practice and transform patients’ lives. I tell many of the APPs I support, “Life can be hard, it does not get easier. You just get better at doing hard. The same is true with practicing medicine. You get better at doing hard things.” I have been able to partner with physician and operational leaders to ensure professional optimal collaboration. My leadership approach has been grounded in servant leadership, underscored by professionalism, transparency, and compassion. I have been able to balance putting people first and keeping the strategic goals of the organization in sight.
Research is also a passion of mine. I will admit at first it was challenging to break into original research. There were


many lessons learned along the way. I would highly encourage APPs to find a mentor who may guide them. Mentorship has been the linchpin to much of my professional success and personal satisfaction. My research has focused mostly on interdisciplinary teams, mentorship, and postgraduate APP career development. It has been an honor to have been an invited speaker on the national stage (AAPA) about the impact of APRN/PA mentorship, and on the international stage (Karolinska Institute Stockholm, Sweden) displaying modernized PA digestive disease education. Being involved in professional societies has been rewarding,


APP Committee and Education Subcommittee. I have been able to connect with GI APPs across the U.S. The ACG Education Subcommittee has relentlessly aimed to provide accessible GI education to APPs through the APP Training Modules and the ACG Education Universe.
There are seasons of life. Seize them. You cannot do it all, all the time. Make the most of opportunities, seek them out and lean in. Learn to also know when to say “no.” Find your tribe that supports you, encourages your growth, and gives you peace.

MONICA R. NANDWANI, DNP, RN, FNP-BC
Director of Advanced Practice, Stanford Health Care, Stanford, CA; Chair, ACG Advanced Practice Provider Committee
What is your typical day like? Do you have a “typical day”?
Every day is different, with each day offering unique opportunities for collaboration with a wide range of individuals, a variety of challenges, and different avenues for new learning and contribution. In my role as an APP Manager, I'm involved with many of our advanced practice providerspecific programs, including our APP Onboarding and Wellness Champion initiatives. Additionally, I serve as the APP representative on a range of organization-wide committees and offer support to our APP Shared Governance Council. My days often involve engaging with APPs and multidisciplinary team members. Together, we focus on supporting APPs so we can take the best care of our patients, optimizing workflows, ensuring we meet regulatory standards, and providing relevant practice updates, with the goal of continuous improvement.
How do you spend your time and interact with patients?
Although my clinical duties have lessened since I transitioned to a leadership role, staying active clinically is a priority for me. It allows
Clockwise from top left: Have you met the future? PA Louwagie has. Victoria Louwagie with pre-PA students who attended the “Become
PA: Pre-PA Workshop” as part of the 2024 AAPA National Conference in Houston, TX. Victoria Louwagie in the new Mayo Clinic Health System Mankato bed tower that opened May 2024, expanding inpatient GI and hepatology care within southern Minnesota. Victoria Louwagie mentors and precepts pre-NP/PA students and NP/PA students several times a year. NP/PA students during their elective clerkship may spend up to four weeks with the Mayo Clinic Health System GI team. These NP/PA students are quickly integrated into the provider team and are afforded the opportunity to deepen their GI knowledge. Victoria Louwagie in clinic with a staged “patient.”




What are the biggest challenges and/ or areas for growth in your role?
One universal challenge is adapting to continual change. It's a considerable part of my role to deliver clear and concise messages to a variety of audiences about updates, changes, or new information. Enhancing my ability to tailor my messages to effectively resonate with all individuals in these varied groups is an ongoing area of growth for me. Another challenge is finding ways to engage and support APPs in today’s health care climate, which is marked with increased clinician workload, rising patient complexity, and continuously evolving technology.
What are the biggest lessons and insights from your career and/or current role that might help other GI APPs as they progress in their professional life?
me to continue to fuel my passion for gastroenterology, maintain a connection with our patients, and stay updated with the latest developments and changes in clinical practice impacting APPs and patient care. Even though I'm not currently engaged in full-time clinical work, I prioritize contributing to the field and my profession by serving as a member of various professional organizations and serving as current chair of the American College of Gastroenterology Advanced Practice Provider Committee.
What is the team dynamic in your role and how do you characterize your relationships with supervisors and colleagues?
I consider myself very lucky to work with a diverse, dynamic, highly skilled, and supportive team where everyone brings a unique perspective and has different strengths. The team I work with strives to create an environment that fosters growth, respect, inclusivity, and appreciation. I find my role engaging as I get to work with APPs across different areas of the organization. For example, in one recent committee meeting, we had APP members
who worked in different service lines and in different settings across our institution (inpatient, outpatient, adult, pediatric) collaborating towards a shared goal of promoting APP wellbeing. I am a firm believer that the people we work with greatly impact our job satisfaction. I'm genuinely thankful not only to enjoy my work but also the people I work with – with an extra bonus of working in a beautiful part of the country with wonderful weather!
What are the most rewarding and satisfying aspects of your role?
I find it rewarding to be able to have an impact on APP professional practice, professional fulfillment, and well-being through the programs and initiatives that I support in my current role. This can be challenging given the many demands on clinicians, the current health care landscape, and the inherent stressors of our work – but I am fortunate to work with a leadership team and in an organization that prioritizes supporting its APPs.
One of the biggest lessons I’ve learned throughout my career is the importance of building your network – within and outside of your organization, within and outside of our specialties, and across disciplines. Your network can open doors and provide opportunities where you might not have thought possible or even known about. There is such an incredible community of APPs from whom we can learn from and gain valuable insights. Cultivating mutual support and lifting each other up is crucial to moving our professions forward. Whenever there's a new opportunity, my first thought is always towards colleagues who could benefit and excel in that scenario. We are each other’s greatest champions!

AMY L.
STEWART, FNP-C Capital Digestive Care, Washington, DC
When thinking about a typical day in my life – a few key concepts come to mind – patient care, collaboration, and decision making. On an average clinic day, I see about 12-14 patients (every 30 minutes). I enjoy having the time to spend with patients that we both need
Clockwise from top left: Monica Nandwani presenting to visiting Dutch NP students about advanced practice providers in the U.S. Health Care System. Monica Nandwani presenting a poster on Advanced Practice Provider Shared Governance at a Nursing Leadership Conference. Monica Nandwani presenting at APP Onboarding to new hire Advanced Practice Providers. Monica Nandwani presenting at the 2023 ACG Annual Meeting and Postgraduate Course on the topic, “What Your APP Can Bring to Your Practice.”





work with your group to figure out how to do more of that. Look for a mentor (inside or outside your practice) who challenges you, supports you, and is your biggest cheerleader. My physician mentors in my group have been instrumental in my career development and my APP mentors outside my group have held the door open for me (shout out to Kim Kearns, NP!).

JASON J. THOMAS, DPAS, MPAS, PA-C
Associate Professor, Seton Hill University
Physician Assistant, Independence Health, Latrobe, PA
What is your typical day like? Do you have a “typical day”?
for a therapeutic relationship. My patients often tell me after a visit it’s the first time they’ve felt “heard” in their medical care. I do carry my own panel of patients as well as co-manage some with my physician colleagues.
One of my favorite parts of my role is the collaboration between APPs and MDs at our practice. While I see patients independently, I do often collaborate with my physician colleagues. I feel lucky to be part of a group where my clinical decisions and contributions to the practice are respected and valued; and, most days, we have fun at work.
I wear many hats at my practice – I am the lead APP for my division of 24 physicians/6 APPS and manage the clinical and prior auth teams for our in-office infusion center which infuses 400+ patients each month. One day a week, I see the infusion patients at the time of their infusion for a short check-in, order labs as needed, coordinate health maintenance, etc.
I perform high resolution anoscopy for anal cancer screening/changes from HPV, and one day a week is spent in the
procedure room (about 8 HRAs/day). I share this practice with my colleague and mentor Jessica Korman, MD – and highly recommend that GI APPs find a unique skillset! Whether you want to learn hemorrhoid banding, take care of a specialty population – the profession needs you, your expertise, and you can truly practice at the top of your license. I stay busy outside of clinic being involved with industry on advisory boards and as a speaker, as well as lecturing at national conferences (this year alone at AANP, GHAPP, AIBD IBD Institute, and TSGE). My passion is for APP education and networking to build our strengths as individuals and as a profession. My work on the APP Committee for the ACG has been incredibly rewarding. Involvement in societies and with industry help to “keep my cup full” and I have truly found joy in APP Education through speaking of all kinds.
My advice to other GI APPs is to find your “why!” This profession has a high propensity for burnout. Figure out what it is that brings you joy, and
One of the great aspects of my career is that each day brings unique experiences and challenges. Since 2019, I have responsibilities as a clinical physician assistant practicing in community gastroenterology for Independence Health System in Latrobe, PA, and as an associate professor at Seton Hill University, Greensburg, PA, in the physician assistant program.
During my academic days, my time is balanced between class preparation, program meetings, teaching lecture and laboratory courses, serving on University Committees, and tending to student needs, such as advising or discussing course material to help them succeed as PA students.
My clinical days, which are currently one day per week, allow me to keep my skills current and serve many patients for whom I have provided care for over two decades. I also have the ability to see patients who develop urgent needs and collaborate with many of our health system’s outstanding physicians and advanced practice providers. My practice is office-based, given my availability, but I should note that our practice’s advanced practice provider panel includes three full-time nurse practitioners and two full-time physician assistants who provide exceptional care to our patients in both the inpatient and outpatient settings.
Clockwise from top left: Empathetic listening and shared decision making during a patient visit. Amy Steward discussing a patient in clinic with her colleague and friend Dr. Ramsey Daher. Amy Stewart leading a team meeting with the infusion clinical and prior authorization team at Chevy Chase office of Capital Digestive Care. Amy Stewart performing high resolution anoscopy (HRA). Capital Digestive Care IBD Providers at the Crohn’s and Colitis Foundation Take Steps Walk. Left to Right: Dr. Kirsti Campbell; Dr. Erica Cohen; Dr. Sam Kallus; Amy Stewart NP; Dr. Sam Muench; Dr. Zach Borman; Kristin Attiogbe, NP; and Dr. Jessica Korman.


While our community-based practice is based on general gastroenterology and hepatology, I have a special interest in caring for patients with inflammatory bowel disease, functional gastrointestinal disorders, and chronic liver disease management.
How do you spend your time and interact with patients?
Being that our practice is communitybased, I take much pride in getting to know patients well. They are much more than a chief concern to me, and they are defined by their individuality rather than their medical issues. Other providers have commented to me that they appreciated such information being included in my documentation, such as their current occupation and other personal characteristics that may influence their health. I love to listen to patients and let them tell their stories. My role as an associate professor has really driven home to me that patients will tell you what is ailing them if you let them speak and then ask thoughtful, meaningful questions in response. I also enjoy patient education. Explaining the workings of the human body, how diseases happen, and how medications work are really vital components of the advanced practice provider role.
What is the team dynamic in your role and how do you characterize your relationships with supervisors and colleagues?
In both the academic and clinical settings, I have been fortunate to be

surrounded by supportive colleagues, supervising physicians, and support staff for as long as I’ve been working. Many of them have become great friends, which really helps everyone function at their optimum level when patients and students need us.
What are your clinical and administrative duties? What is the balance here?
Within our PA program, I teach several courses in the classroom and laboratory. Additionally, PA educators have significant responsibilities in program development, curricular assessment, and student advising that consume a lot of time. At Seton Hill University, I serve on the committee for mission and faculty and on the Faculty Athletics Support team for the Women’s Softball program. Within the clinical setting, in addition to seeing patients, I regularly monitor patient laboratory and radiographic findings, respond to concerns, answer questions, and renew medications electronically.
What are the most rewarding and satisfying aspects of your role?
Within the clinic, the biggest reward is providing a means for a patient to heal and become capable of returning to the highest possible quality of life for the longest amount of time. Hearing that a patient felt that you cared about them always brings me joy. The same can be said for my academic position. Watching the transformation of students as they grow from inexperienced college students to extremely knowledgeable and caring
providers is an amazing thing to be involved in. Knowing that I had even a small part in that is very fulfilling.
What are the biggest challenges and/ or areas for growth in your role?
Balancing all that comes with being an educator and trusted clinician can be very difficult. Add to that the commitment of having a family (wife Amanda, daughters Clare and Nora), and it can be quite challenging. I would say the biggest challenge is being the best that I can be in all three areas and not feeling like I’m letting anybody down. If I could choose one thing to become better at, it would be to become a more efficient multi-tasker.
What are the biggest lessons and insights from your career and/or current role that might help other GI APPs as they progress in their professional life?
I was fortunate to gain my first employment with a private GI practice (Dr. Bill Provance and Dr. Doug Klions) 20 years ago. Looking back, what they provided me was invaluable. In essence, they guided me through what now many would consider an APP GI fellowship. They invested time and resources to teach me GI and many pearls that have proven their worth time and time again. I would advise new GI APPs to look to the people, not the prestige, position, or prizes when they are looking to launch a career in GI.

AMANDA B. WILHITE, MPAS, PA-C
Physician Assistant, Houston
Methodist Gastroenterology Associates, Houston, TX
What is your typical day like? Do you have a “typical day”?
A typical day for me on Monday/ Tuesday is all day clinic with my physician. Wednesday/Thursday/ Friday, I have my own clinic all morning that sometimes runs into the early afternoon. For the remainder of the day, I complete my clinic notes in addition to managing our EPIC inbox. This entails answering all our patient
From left: Jason Thomas in the Seton Hill PA Program History & Physical Examination Laboratory. Jason Thomas with Douglas E. Klions, MD, a long-time ACG member, in the clinic in Latrobe, PA and his ACG Social Media Acumen for outstanding work launching and growing the ACG APP Facebook group. Jason Thomas with wife Amanda and daughters Clare (14) and Nora (11).


advice messages, addressing all lab results (including all labs that we get from our infusion patients), signing off on orders/therapy plans, medication refills, etc. In addition, I will also do any other needed tasks such as scheduling/ performing peer-to-peer conversations and writing letters of medical necessity.
How do you spend your time and interact with patients?
I like to spend quality time with my patients and make sure all their questions/concerns are answered before the visit is over, even if that means we run over the allotted clinic time. I never want a patient to feel rushed in their visit and want to make sure they leave feeling more knowledgeable about their disease state and treatment plan.
What is the team dynamic in your role and how do you characterize your relationships with supervisors and colleagues?
My team consists of my supervising physician, two infusion nurses, one licensed vocational nurse (LVN), one medical assistant (MA), and a procedure scheduler. We have worked together for the past nine years and all have a very close relationship. We have developed an efficient system in how we run our practice, and each person knows their designated duties/ roles. I correspond directly with patients regarding their lab results/ patient triage messages and answer any questions/concerns they have. If patients need anything additional such as medication approvals/refills,

vaccines, referrals, procedure scheduling, follow-up appointments, etc., then I will delegate these tasks to my medical assistant, nurse, and scheduler.
What are your clinical and administrative duties? What is the balance here?
As far as clinical duties, I assist my supervising physician in clinic two full days a week and then have my own clinic three days a week. Either before, after, or in between clinic patients, I am working on EPIC inbox tasks including signing orders, therapy plans, medication refills, addressing lab results, answering staff and patient advice messages.
What are the most rewarding and satisfying aspects of your role?
Since all the patients I take care of have inflammatory bowel disease, the most rewarding part about my job is when a patient tells me that I have helped give them their life back and they are able to do normal daily activities without being tied to their house/the bathroom.
What are the biggest challenges and/or areas for growth in your role?
As far as future growth in my role, I hope to officially become certified in doing intestinal ultrasound when there is an official certification program for APPs.
What are the biggest lessons and insights from your career and/or current role that might help other GI APPs as they progress in their professional life?
In order to have longstanding job satisfaction, I think it is vital for all APPs to work with a physician who genuinely respects them and completely trusts in
them to care for the patients in their practice. It is also vital for APPs to establish from the beginning what they want their role in the practice to be and to ensure that they get as much autonomy as they feel comfortable with.
Amanda B. Wilhite, MPAS, PA-C during a typical day as a Physician Assistant at Houston Methodist Gastroenterology Associates.

Spotlight on Innovation: ADVANCEMENTS IN INTESTINAL ULTRASOUND
with Dr. Noa Krugliak Cleveland & Dr. Michael Dolinger
ABOUT

Noa Krugliak Cleveland, MD
Dr. Krugliak Cleveland is an Assistant Professor of Medicine at the University of Chicago Pritzker School of Medicine who specializes in IBD.

Michael T. Dolinger, MD
Dr. Dolinger is an Assistant Professor of Pediatric Gastroenterology at the Icahn School of Medicine and Mount Sinai Kravis Children’s Hospital. He leads the Henry and Elaine Kaufman intestinal ultrasound program at the Susan and Leonard Feinstein Inflammatory Bowel Disease Center at Mount Sinai.
INTRODUCTION
In the realm of gastroenterology, technological advancements continually redefine patient care and clinical practice. One such innovation making significant strides is intestinal ultrasound (IUS), a non-invasive, point-of-care tool for monitoring and managing inflammatory bowel disease
(IBD). To delve deeper into this cuttingedge technology, we had the privilege of speaking with Dr. Noa Krugliak Cleveland and Dr. Michael Dolinger, leading experts in the field on behalf of the ACG Innovation & Technology Committee.
They share insights into the implementation and impact of IUS, the challenges encountered, and the transformative potential of this technique. This conversation not only highlights the practical aspects of integrating IUS into clinical practice but also highlights the importance of continuous learning and collaboration in the medical community.
1. Could you provide an overview of intestinal ultrasound and elaborate on what inspired its introduction at your institution?
Noa Krugliak Cleveland, MD
Intestinal ultrasound (IUS) is a noninvasive, point-of-care monitoring tool for the management of patients with inflammatory bowel disease (IBD). Using sonographic waves and scanning the abdominal wall, the clinician and patient
can visualize both the colon and small bowel and identify evidence of both active inflammation and signs of chronic disease, as well as diseaserelated complications such as bowel strictures, fistulae, and abscesses.
Unique to bowel ultrasound, it is not invasive, preferred by patients over all our current endoscopic, serologic, and stool tests, and it is highly responsive to change. In patients with active severe colitis, response to IV corticosteroids can be seen as early as 24 hours and when looking at all therapies, this can be seen as early as two weeks. Crohn’s data demonstrate sonographic response as early as 4-12 weeks. IUS without radiation or bowel preparation can be done as often as needed and can also assess for deeper levels of healing, such as transmural healing, an emerging treatment target in Crohn’s disease.
I was first exposed to IUS by my mentor Dr. David Rubin. I shortly thereafter sought training from the International Bowel Ultrasound Group. Once I started utilizing IUS in clinic, it
Raseen Tariq, MBBS and Bara El Kurdi, MD
“IUS without radiation or bowel preparation can be done as often as needed and can also assess for deeper levels of healing, such as transmural healing, an emerging treatment target in Crohn’s disease.”
was evident that this tool is completely practice-changing. It allowed for tighter control, more objective real time data, and far more information on the patient’s state of the disease during the clinic visit. I knew that this is an opportunity to change the care we provide for patients at the University of Chicago. This subsequently led to the recruitment of another IUS-trained fellow to join us as a pediatric faculty member, Dr. Amelia Kellar; and later also to promote training of a number of our own IBD faculty. We currently have seven fully trained clinicians who perform IUS and two who are currently in training.
Michael Dolinger, MD
I began training in Intestinal Ultrasound in 2019 through an educational curriculum for certification developed by the International Bowel Ultrasound Group. The reason I had begun training is due entirely to my mentor, Dr. Marla Dubinsky. At the beginning of my second year of fellowship, I had a research meeting, and we discussed my career goals and aspirations. I explained I wanted to do meaningful research that impacted patients and advanced the field of IBD. Almost immediately, Marla asked me if I wanted to go learn ultrasound and bring it back to the patients of Mount Sinai and lead efforts to implement it into IBD care in the United States on a larger scale. Without hesitation, and without knowing what intestinal ultrasound actually was, I said yes. Less than a few months later, I traveled overseas to Copenhagen to begin training in IUS, not knowing how much this would impact patients. Quickly during training, I realized the vision that Marla had for IBD patients and improving care by utilizing intestinal ultrasound in the United
States. We could use IUS as a better, non-invasive monitoring tool to guide treatment optimization and better triage when more invasive procedures were needed to impact IBD care and improve outcomes for patients with a better tool to foster shared understanding along the way.
2. What were the pivotal steps and challenges encountered during the integration of intestinal ultrasound into clinical practice at your institution?
Noa Krugliak Cleveland, MD
The most critical step to integrating IUS into our IBD center was getting my colleagues who have not been trained in IUS to trust this tool, to trust me, and to see for themselves the benefit it has to our IBD practice. This took some time, but after about a year, I began receiving regular referrals from my IBD colleagues, as well as internal faculty who wished to train in IUS themselves. The second pivotal step in building our Intestinal Ultrasound Program was receiving philanthropic support from a grateful patient. This allowed for hiring support staff, which was critical to approaching the program in a holistic way and attending to the clinical operations, research, and educational needs of our program. Over time, training my staff has made me and our clinicians more efficient and allowed us to maximize our educational efforts, hosting trainees from all over the world, as well as building a large research database and receiving grant support for our work.
Michael Dolinger, MD
There were almost too many pivotal steps and challenges to count. To list a few, obtaining a high quality ultrasound machine for regular use in the clinic; integrating the ultrasound as a point-of-care tool into our electronic medical record and PACS; partnering with radiology and surgical colleagues; developing a mastery level skillset without any direct supervision or guidance; incorporating intestinal ultrasound into the IBD center clinic work flow, reimbursement, and sustainability models; and teaching our IBD providers the best way to use intestinal ultrasound in their practice. These were all large hurdles that were overcome with great problem solving led by our entire IBD team and Marla Dubinsky, not just myself.
3. How did you and your team acquire the necessary training in intestinal ultrasound? Additionally, could you recommend any resources or programs for professionals interested in adopting this technology?
Noa Krugliak Cleveland, MD
The training curriculum is offered through the International Bowel Ultrasound Group (IBUS-group.org).
The training is currently comprised of three modules: Module 1 is a twoto three-day training course with hands-on experience; Module 2 is a four-week hands-on training with an IUS expert for a total of minimum 40 exams; and Module 3 is a didactic session with a knowledge-based test at the end. This curriculum is being changed with integration of an electronic learning platform to improve the scalability of the curriculum and to allow for competency measures
“We could use IUS as a better, non-invasive monitoring tool to guide treatment optimization and better triage when more invasive procedures were needed to impact IBD care and improve outcomes for patients with a better tool to foster shared understanding along the way. ”
to be assessed. We have secured funding from the Helmsley Charitable Trust to support training throughout the U.S. over three years. The next training program is scheduled to be in Houston in 2025 (go to IBUS-group.org to learn more).
There are additional educational programs and webinars offered though IBUS, as well as the new organization we founded in North America, the Intestinal Ultrasound Group of the U.S. and Canada (iUSCAN), which members can attend. This includes IBUS and iUSCAN’s joint teleconference called “IUSMonthly,” which is held once a month and where IBD cases managed utilizing IUS are presented. This has been very well attended by both novice sonographers, along with our field’s most senior experts from all over the world.
Michael Dolinger, MD
There is currently one unified international training and certification program, developed by IBUS and available on their website. I currently lead efforts, thanks to a grant from the Helmsley Charitable Trust, within IBUS to change the curriculum to meet the growing demand for high quality intestinal ultrasound including the development of an e-lLearning platform for training. I would recommend becoming a member of IBUS and exploring all of the education and training curriculum they have to offer. Myself, Noa Cleveland, and Kerri Novak have also co-founded the intestinal ultrasound group of the United States and Canada (iUSCAN) which is an its infancy but will lead educational curriculums in North America (iuscan.org). For now, IUS monthly, a webinar series on the second Tuesday of each month developed by Michael Winter, serves as an excellent forum for education for those interested or beginning their journey in intestinal ultrasound.
4. In your experience, how do new techniques typically emerge in the medical field, and how do you navigate the process of transforming an idea for using an old technology in a new, innovative way?
Noa Krugliak Cleveland, MD
The answer is really in the stem of the question: IUS is really an old technology that is utilized in an innovative way. I
“Intestinal ultrasound solves a problem by being a noninvasive test that has the potential as a tight control monitoring tool to directly monitor inflammation in the bowel to guide decision making for better outcomes.”
believe the key to the emergence of IUS today is in both the technologic progress of U.S. systems and imagery, but more importantly, our field being at a place where we understand that time is of the essence in management of IBD, and faster and more accurate objective data is key to prevent progression and to change outcomes in patients. The timing of reintroducing bowel ultrasound in this era of treat-to-target and disease modification has allowed for this successful uptake and great interest.
Michael Dolinger, MD
New techniques and innovative ideas emerge in the medical field to solve problems. Currently, many IBD patients do not achieve remission and must undergo many invasive tests which may or may not be so helpful. Intestinal ultrasound solves a problem by being a non-invasive test that has the potential as a tight control monitoring tool to directly monitor inflammation in the bowel to guide decision making for better outcomes. There is no secret to bringing something new into the mainstream of clinical practice against the inertia of current standards of care. It takes an immense amount of hard work, multifaceted effort, persistence, and dedication from individuals and teams of individuals.
5. For institutions considering the adoption of innovative technologies like intestinal ultrasound, what guidance would you offer on the evaluation, acquisition, and implementation processes?
Noa Krugliak Cleveland, MD
The first step is presenting the role of IUS in clinical practice and in providing patients with the highest level of care. Presenting a financial plan is helpful and important as well. This is not only an investment that pays for itself, but also a revenue generating tool.
You can refer to our guide on credentialing, published in The American Journal of Gastroenterology (bit.ly/AJG-IUS-Dolingeretal). This publication details all that is needed for billing and a sample IUS template note. Once there is leadership commitment for both investment in the training and equipment needed, ideally two IBD clinicians in your practice should go through the training curriculum. This will allow for a team to be working towards competency and also building the infrastructure for documentation and billing of IUS.
Visiting other IUS expert centers is another important step in integrating IUS into your
“I believe the key to the emergence of IUS today is in both the technologic progress of U.S. systems and imagery, but more importantly, our field being at a place where we understand that time is of the essence in management of IBD.”
practice. This allows clinicians to see the different clinical flows and IUS infrastructures, continue to learn new skills, to exchange ideas, and to foster collaborations. It is key for the clinician performing IUS to stay humble, accurate in their reporting and interpretation, and describe any limitations of an exam. This is crucial for colleagues to gain both trust in IUS as a monitoring tool and trust in the clinician performing it. Lastly, pay it forward and become both a training center as well as a clinical trial site to advance both education and research. The ultimate goal is to get IUS to all patients with IBD in order to improve their lives.

To join iUSCAN, open this QR code with your cell phone camera
Michael Dolinger, MD I would tell institutions to listen to their patients. Patients often want their providers to listen, and they want their team to continue to push the boundaries to improve care. Once you listen to your patients, it’s about acting upon those wants and learning. Taking steps that are forward-thinking and not waiting for the status quo to change is imperative. Leadership within institutions needs to be supportive of ideas that have the potential to improve IBD care without
knowing if they will be successful. To take risks and change care is the only way to move forward. I would ask them to take a long-term view, not seek an immediate return on investment, but think about the new long-term for clinical care, potential for research, and inherent value being an innovative leader may provide to your organization.
RESOURCES
Guide to Intestinal Ultrasound Credentialing, Documentation, and Billing for Gastroenterologists in the United States, Michael Todd Dolinger, MD, MBA; Noa Krugliak Cleveland, MD; David T. Rubin, MD, FACG; Marla C. Dubinsky, MD, FACG
Read: bit.ly/AJG-IUS-Dolinger-etal
ABOUT

Bara El Kurdi, MD
Dr. El Kurdi is Assistant Professor of Medicine at Virginia Tech Carilion School of Medicine in Roanoke, VA. He finished his GI fellowship at UT Health San Antonio in 2023. He is a member of the Innovation & Technology Committee and ACG’s Legislative and Public Policy Council.

Raseen Tariq, MBBS
Dr. Tariq is currently a GI fellow at Mayo Clinic on the NIH-sponsored T32 track, graduating in December 2024, and is a member of the ACG Innovation & Technology Committee.
LESSONS LEARNED:
1. IUS has potential to transform IBD care at the bedside level.
2. Mentorship is at the heart of the innovation process. Mentors who support their mentees by providing opportunities for personal growth pave the way for technological advancement.
3. Old technology adaptation is not without challenges.
4. Although the regulatory pathway for repurposing of old technology maybe easier, provider trust, institutional investment, reimbursement, time preference, and knowledge gap are major challenges that can hinder the adaptation of old technologies for innovative purposes.
5. New techniques involve skills which require training. Building the infrastructure for training providers is essential for the growth and survival of such techniques.
6. When approaching your institution for investment in new technology, it is essential to do your homework. Be ready to discuss:
a) the technology’s impact on patients/community; b) a financial plan/ reimbursement pathway; and c) a plan for implementation/ integration once you have institutional buy-in.
TRAINING AT A NETHERLANDS CENTER OF EXCELLENCE FOR DGBI AND MOTILITY DISORDERS

I had the honor of being awarded the 2023 ACG North American International GI Training Grant to travel to Maastricht University Medical Centre (MUMC), a tertiary academic center in the Netherlands. My clinical and research interests include disorders of gut-brain interaction (DGBI) such as irritable bowel syndrome (IBS) and functional dyspepsia (FD) and defecatory disorders.
DGBIs are highly prevalent globally, affecting about 40% of the global population (including the United States) with associated negative impact on quality of life for patients and economically on the healthcare system. Integrated DGBI care (with dietitians and gastropyschologists) is now recognized as the most optimal model for improving patient outcomes. I had the privilege to learn
“DGBIs are highly prevalent globally, affecting about 40% of the global population (including the United States) with associated negative impact on quality of life for patients and economically on the healthcare system.”
from the neurogastroenterology and motility team at MUMC who have established a center of excellence for DGBI and motility disorders and are referred patients from across the Netherlands and neighboring European countries.
There is a tremendous need for collaborative and innovative research to generate new ideas for treatment modalities, change the paradigm of care and deliver better outcomes for patients with DGBI globally. I thoroughly enjoyed the chance to immerse myself in a different healthcare and hospital system; for example, I was reminded again of the indelible importance of social determinants of health on both a population and individual patient level (e.g., universal healthcare, easy access to affordable public transport, and minimally processed foods).
Yuying Luo, MD, Icahn School of Medicine at Mount Sinai, New York, NY, ACG North American International Training Grant to Maastricht University Medical Center

Additionally, I had the opportunity to participate in research meetings and hear about the plethora of ongoing research projects using novel methodologies and devices, observe the patient recruitment process for ongoing studies, and learn from their multidisciplinary team on the workflow and treatment approach for complex patients. I especially appreciated learning about MUMC’s patient hotel model1 where patients with suspected complex GI motility disorders stay in a nearby hospital hotel (to avoid an inpatient stay and improve patient satisfaction) with carefully coordinated testing and clinical visits on consecutive days. There are many things I took away from both the clinical and research perspective that I hope we can apply to our practice and projects.
I am incredibly grateful to the American College of Gastroenterology for providing this unparalleled opportunity for early career gastroenterologists; to my mentors and fellowship program at Mount Sinai for their support over the years (including Dr. Laurie Keefer and Dr. David Greenwald for their support for this grant and Dr. Bhavana Rao for encouraging me to apply); to Dr. Daniel Keszthelyi, chief of gastroenterology and hepatology at MUMC for thoughtfully coordinating my visit; and to all the staff and students at MUMC for being gracious hosts.
REFERENCE
1. Masclee GM, Masclee AA, Kruimel JW, Conchillo JM, van Vliet J, Keszthelyi D. Using a Patient Hotel: Perceptions of the Quality of Care by Patients Undergoing Analysis for Gastrointestinal Motility Disorders in the Netherlands. J Patient Exp. 2022 Mar 28;9:23743735221089453. doi: 10.1177/23743735221089453. PMID: 35372681.


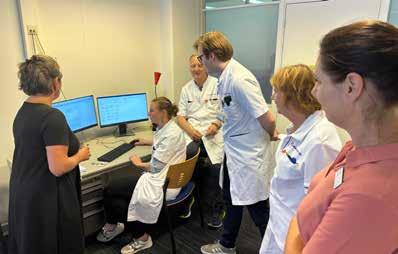
Photo page 47: Dr. Daniel Keszthelyi and Dr. Yuying Luo. Photo top right: Fresh fruits and vegetables available in the hospital.


Inside the JOURNALS























A NEW ACG CLINICAL GUIDELINE on commonly diagnosed asymptomatic liver lesions by Catherine T. Frenette, MD, et al. published in July in The American Journal of Gastroenterology offers evidence-based approaches to the initial evaluation and management of these incidental findings. The authors address clinical dilemmas about whether further workup is necessary and which imaging modality should be used and make management recommendations.

In CTG, investigators assessed the impact of a secular, guided meditation technique delivered by a free app on cyclic vomiting syndrome in 30 patients who completed the six-week study. The authors believe this is the first study to show endocannabinoid-boosting effects resulting from a psychological intervention.
ACG Case Reports Journal continues its monthly “Behind the Case” podcast series with a fascinating conversation on a retrospective case series of four patients treated with sirolimus for refractory Crohn’s disease at the Mayo Clinic Florida.
[THE AMERICAN JOURNAL OF
GASTROENTEROLOGY]
ACG Clinical Guideline: Focal Liver Lesions
Catherine Frenette, MD; Mishal Mendiratta-Lala, MD; Reena Salgia, MD; Robert J. Wong, MD, MS, FACG; Bryan G. Sauer, MD, MSc, FACG; Anjana Pillai, MD, FACG. The American Journal of Gastroenterology 119(7):p 1235-1271, July 2024. DOI: 10.14309/ajg.0000000000002857
With the continued dramatic rise in the widespread role of imaging in diagnosis and management of patients, there is a resultant rise in detection of asymptomatic incidental liver lesions. Gastroenterologists and hepatologists often see these patients in consultation and make recommendations for management of multiple types of focal liver lesions (FLLs), including hepatocellular adenoma, focal nodular hyperplasia, hemangioma, and hepatic cystic lesions including polycystic liver disease. Malignancy is important to consider in the differential diagnosis of FLLs. The guideline includes a flow chart of recommendations.
READ: bit.ly/ajg-frenette-et-al

Obesity Special Issue
In June, AJG published a special issue exploring obesity. Co-Editors-in-Chief
Jasmohan S. Bajaj, MD, MS, FACG and Millie D. Long, MD, MPH, FACG imagined the issue as a “crossroads between the multiple specialties involved in studying obesity pathogenesis.” They also recognize the evolving role of GI specialists as “hubs for obesity management” in an editorial that prefaces the issue.
READ: bit.ly/ajg-june-2024-obesity
[ACG CASE REPORTS JOURNAL]
Sirolimus Use in Refractory Crohn's Disease
Rex K. Siu, MD, MSc; Christian Karime, MD; Jana G. Hashash, MD, MSc; Jami Kinnucan, MD; Michael F. Picco, MD, PhD; Francis A. Farraye, MD, MSc. ACG Case Reports Journal 11(6):p e01368, June 2024 DOI: 10.14309/crj.0000000000001368
Authors at Mayo Clinic Florida’s IBD Center retrospectively identified and reported clinical outcomes for four patients prescribed sirolimus for treatment of refractory Crohn’s disease. Despite a median sirolimus therapy duration of 524 days and some therapeutic benefits, all patients discontinued therapy due to adverse effects. These findings suggest that while sirolimus may have clinical utility, its role may be limited by treatmentderived adverse effects.
READ: bit.ly/acgcrj-siu-et-al-sirolimus
[CLINICAL & TRANSLATIONAL GASTROENTEROLOGY]
Acute and Long-Term Effects of App-Delivered Heartfulness Meditation on Psychological Outcomes and the Endocannabinoid Signaling System in Cyclic Vomiting Syndrome
Thangam Venkatesan, MD; Cecilia J. Hillard, PhD; Lina Ayar; Saranya Arumugam, MBBS; Stacey Culp, PhD; Mahima Vyas; Kebire Gofar, MD, MPH; Ana Petrova, MD; Olafur S. Palsson, PsyD. Clinical and Translational Gastroenterology 15(7):p e00711, July 2024. DOI: 10.14309/ ctg.0000000000000711
What Is Known
An integrative healthcare model incorporating heartfulness meditation (HFM) and a care coordinator can improve psychological outcomes and health-related quality of life in cyclic vomiting syndrome (CVS).
The independent effects of HFM in CVS and the underlying mechanism are not known.
What Is New Here
HFM delivered through an app improves psychological outcomes, such as mood, state and trait anxiety, psychological distress, sleep, and health-related quality of life.
HFM is the first psychological intervention shown to boost circulating endocannabinoid concentrations, which play a role in the regulation of stress, nausea, and vomiting.
READ: bit.ly/ctg-venkatesan-et-al
HEARTFULNESS MEDITATION IN CVS

ACGCRJ Associate Editor Dr. Himesh Zaver is joined by Dr. Jami Kinnucan, Dr. Francis A. Farraye, and Dr. Rex K. Siu to discuss their case, "Sirolimus Use in Refractory Crohn's Disease," published in the June 2024 issue.
LISTEN: bit.ly/acgcrj-podcast-sirolimus

ACG GUIDELINE Highlights
Alcohol-Associated Liver Disease (ALD)
Loretta L. Jophlin, MD, PhD; Ashwani K. Singal, MD, MS, FACG; Ramon Bataller, MD, PhD, FACG; Robert J. Wong, MD, MS, FACG; Bryan G. Sauer, MD, MSc, FACG; Norah A. Terrault, MD, MPH, FACG; and Vijay H. Shah, MD, FACG
Epidemiology

Diagnosis

Treatment for AUD and ALD

The spectrum of ALD ranges from steatosis to steatohepatitis to cirrhosis. Can also present as alcohol-associated hepatitis (AH) which can lead to ACLF
Primary Risk Factors
Secondary Risk Factors

Amount and duration of ETOH use
1) Women are at risk ( body fat and ETOH dehydrogenase)
2) Metabolic syndrome
3) Smoking
Screening for ETOH: Use AUDIT to identify AUD (higher scores have linear relationship with mortality!)

Biomarker CDT (Blood) EtG (Urine) EtS (Urine) Peth (Blood)
Use motivational interviewing Pharmacotherapy is effective!
The 5 “A” model ETOH use with a NNT of 7.

For Alcohol-Associated Hepatitis (AH):
1) Use the NIAAA diagnostic criteria as a guide.
Prednisolone or prednisone 40 mg daily x 4 weeks is recommended.
Options to consider in a multidisciplinary setting:
1) Naltrexone
2) Acamprosate
3) Baclofen
4) Gabapentin
5) Topiramate
2) Use MELD score to stratify disease severity and when to start steroids (MELD>20)
3) Calculate Lille score at day 4 or 7. If >0.45 steroids should be discontinued.
AH = alcohol-associated hepatitis
ACLF = acute-on-chronic liver failure
ALD = alcohol-associated liver disease
AUD = alcohol use disorder
CDT = carb
D = day
EtG = ethyl glucuronide
ETOH = alcohol
EtS = ethyl sulfate
FIB-4 = Fibrosis-4
DOI: 10.14309/ajg.0000000000002572


ALD-related deaths were increasing prior to 2020 and accelerated during the pandemic.
Public policy matters! ETOH taxes associated with ALD mortality
4) Diabetes

5) Gastric bypass anatomy (RYGB direct dumping of ETOH into jejunum in setting of ETOH dehydrogenase)
6) Having other chronic liver diseases
Screening for Fibrosis: Use noninvasive tests such as FIB-4 and transient elastography
Underlying inflammation and steatohepatitis may lead to an overestimate of liver stiffness with elastography.
Nutritional Support
Considerations
Supplement thiamine, B12, and zinc
Caloric intake goal of 35 kcal/kg/d with 1.2-1.5 g/kg/d of protein
If <21 kcal/kg/d start enteral support.
When interpreting FIB-4, consider that ETOH use can reduce platelet count!

Zinc deficiency is an independent predictor of 28 day mortality

Feeding tubes are safe in patients with EV without active bleeding and no recent banding

4) Pentoxifylline is not recommended.
5) Consider 5 days of NAC infusion as an adjuvant to steroids for severe AH.
6) Severe AH unresponsive to medical management needs early LT evaluation.
QUICK-Trans study show no significant difference in rate of relapse between early vs standard liver transplant (>6 mo sobriety)
Kcal = kilocalorie
Kg = kilogram
LT = liver transplant
MELD = Model for End-Stage Liver Disease
NAC = N-Acetylcysteine
Loretta L. Jophlin, MD, PhD; Ashwani K. Singal, MD, MS, FACG; Ramon Bataller, MD, PhD, FACG; Robert J. Wong, MD, MS, FACG; Bryan G. Sauer, MD, MSc, FACG; Norah A. Terrault, MD, MPH, FACG; Vijay H. Shah, MD, FACG The American Journal of Gastroenterology 119(1):p 30-54, January 2024.
NIAAA = National Institute on Alcoholism and Alcohol Abuse
NNT = number needed to treat
Peth = phosphatidylethanol
RYGB = Roux-en-Y Gastric Bypass
Concept and Content: Erica Duh, MD, UC Irvine | Reviewer: Loretta L. Jophlin, MD, PhD READ THE GUIDELINE: bit.ly/alcohol-liver-guideline
“Patients with ALD suffer from 2 disorders – one of liver disease and the other of AUD”
Disulfiram
NUTRITION IN INFLAMMATORY BOWEL DISEASE (IBD)
Understanding Nutrition in IBD: Information for Patients & Caregivers from the American College of Gastroenterology
WHAT IS IBD?
Inflammatory Bowel Disease (IBD) is a long-term (chronic) inflammation of tissues in your digestive tract which includes the conditions ulcerative colitis (UC) and Crohn’s disease (CD).
DIET AND NUTRITION CAN AFFECT HOW PEOPLE WITH IBD FEEL. Certain foods (“trigger foods”) may make you feel worse, and avoiding those may help to manage your symptoms. Meeting your nutritional needs is very important, and you may need to talk with your doctor or a dietitian to make sure that your body is getting the nutrients it needs to work well.
There is no “one-size-fits-all” diet that works for everyone with IBD!
Some IBD patients can tolerate certain foods, while others cannot. IBD is an autoimmune condition and there is no single diet or medication that can help IBD completely. Some diets may help you manage your condition, although many people combine diet and medication to find what works best for them. Talk to your doctor about IBD and nutrition, and do not begin any exclusion diets without talking to your doctor or dietitian first.
SOME DIET OPTIONS FOR PATIENTS WITH IBD
Mediterranean Diet
• Whole grains, fruits, and vegetables
*Note: Patients with narrowing in their intestines (strictures) may need to avoid high-fiber foods
• Fats from fish, olive oil, nuts, and seeds
• Protein from low-fat dairy, poultry, fish, shellfish, or legumes (beans, peanuts, and peas)
• Less red meat, especially for patients with UC
• Avoid ultra-processed foods with high sugar and salt (junk foods)
Specific Carbohydrate Diet (SCD)
• Eliminates sugars, starches, and grains
• Shown to decrease IBD symptoms, and may decrease inflammation
Crohn’s Disease Exclusion Diet
• Eliminates sugars, red meat, dairy, and wheat
• May help control mild Crohn’s disease for short periods of time
• Important to regularly test for low protein, vitamin D, vitamin B12, folate, and iron
• A therapy called “exclusive enteral nutrition” may be helpful in CD in both children and adults.
QUESTIONS TO ASK YOUR DOCTOR
• Are any of my nutritional levels low? Which ones, and what tests are needed?
• Do I need to take any vitamins/minerals to help?
• Is it safe to drink alcoholic beverages or sugary drinks (soda, energy drinks, or electrolyte drinks)?
• Should I get help from a registered dietitian?
ACG Patient Information: gi.org/topics/inflammatory-bowel-disease
Find a Gastroenterologist: gi.org/patients/find-a-gastroenterologist
Learn About



