PROPOSED SLATE OF 2023–2025 AAN BOARD OF DIRECTORS ANNOUNCED

Vote at April 22 AAN Business Meeting
The AAN Nominations Committee, co-chaired by the late former AAN President Ralph L. Sacco, MD, MS, FAHA, FAAN, and Immediate Past President James C. Stevens, MD, FAAN, has announced the slate of nominees for AAN officer and director positions for the 2023–2025 term.
Officers:
Natalia S. Rost, MD, MPH, FAAN, FAHA, President Elect


Janis M. Miyasaki, MD, MEd, FRCPC, FAAN, Vice President


Sarah M. Benish, MD, FAAN, Secretary
Charles C. Flippen II, MD, FAAN, Treasurer
Continued on page 10 ›
Participate in 2023 Neurology Compensation and Productivity Survey
The new iteration of the Neurology Compensation and Productivity Survey will be open March 14 through May 11. This is the largest neurology compensation and productivity survey in the United States, with more than 4,000 AAN members participating in 2021. It’s important to build on the success of the last survey because the larger the data set, the higher quality it will be. Continually refined over the years, the survey is easy to take, with the ability to skip questions that aren’t relevant, and your work can be saved for you to come back to. Reminder to business administrators: you can participate on behalf of your practices and departments!
Members who complete the survey will receive access to the customizable dashboard for free—a $500 value. The cost for US members who do not participate in the survey is $500, and $1,500 for nonmembers in the US. A user-friendly dashboard allows you to filter data by subspecialty, geographic region, gender, and more. The dashboard will be available by July 2023.
Annual Meeting Abstracts Now Available

Visit
to browse the innovations and discoveries of the more than 2,600 abstracts that will be presented at the upcoming 2023 AAN Annual Meeting this April 22 to 27. These impressive findings were chosen because they represent the most innovative scientific research and cutting-edge breakthroughs in all facets of neurology.
Boston & Virtual • April 22–27
Save on Registration Before March 30
Visit AAN.com/AM today to secure your advance registration discounts for the 2023 AAN Annual Meeting. Whether you join us in person in Boston or live online, the meeting will offer an unforgettable educational and networking experience, no matter your career level or geographic location.
6 Annual Meeting Hubs Foster Collaborative Learning Through Unique Delivery Methods 21 Jones Named 2023 President’s Award Recipient 26 75 Years of Leadership of the American Academy of Neurology VOLUME 35 ISSUE 3 MARCH 2023 Continued on page 7 ›
AAN.com/AMAbstracts
Rost Benish Miyasaki Flippen
What other symptoms of Rett syndrome are asking for your attention?
PHYSICAL SETBACK
Uncontrollable hand movements increased
MOOD ALERT
Sudden episodes of inconsolable screaming lasting hours
With no FDA-approved medication for Rett syndrome (RTT), treatment is symptomatic and supportive.2,3 But there are additional challenges of daily life with RTT that are not addressed with pharmacologic treatment or therapy.

Symptoms without specific pharmacologic intervention may include:
Inattention and anxiety1
Orthopedic and mobility issues1

Breathing abnormalities (eg, hyperventilation, breath-holding, air swallowing)1,4
Nighttime behaviors (eg, screaming, laughing)5
Nonverbal communication1
Stereotypic hand movements1
References:
1. Fu C, Armstrong D, Marsh E, et al. Consensus guidelines on managing Rett syndrome across the lifespan. BMJ Paediatr Open. 2020;4(1):e000717.
2. Gold WA, Krishnarajy R, Ellaway C, et al. Rett syndrome: a genetic update and clinical review focusing on comorbidities. ACS Chem Neurosci. 2018;9(2):167-176.
3. National Institutes of Health. What are the treatments for Rett syndrome? Accessed August 1, 2022. https://www.nichd.nih.gov/health/topics/rett/conditioninfo/ treatments#:~:text=With%20therapy%20and%20assistance%2C%20people%20with%20Rett%20syndrome
4. Tarquinio DC, Hou W, Neul JL, et al. The course of awake breathing disturbances across the lifespan in Rett syndrome. Brain Dev. 2018;40(7):515-529. 5. Wong K, Leonard H, Jacoby P, et al. The trajectories of sleep disturbances in Rett syndrome. J Sleep Res. 2015;24(2):223-233.
Rett syndrome is a rare, heterogeneous, neurodevelopmental disorder.1,2
Looking beyond the symptoms that currently have pharmaceutical treatments may greatly impact care.
© 2022
Inc.
is a registered trademark of
rights reserved.
Together with caregivers, you can help identify more opportunities for collaborative and comprehensive care. Learn more at RettDialogue.com
®
Acadia Pharmaceuticals
Acadia
Acadia Pharmaceuticals Inc. All
RETT-0066 01/23
Minna, living with Rett syndrome Caroline, Minna’s mother and caregiver
The Mission of the AAN is to promote the highest quality patient-centered neurologic care and enhance member career satisfaction.
The Vision of the AAN is to be indispensable to our members.
Contact Information
American Academy of Neurology
201 Chicago Avenue Minneapolis, MN 55415
Phone: (800) 879-1960 (toll free) (612) 928-6000 (international)
Email: memberservices@ aan.com
Website: AAN.com
For advertising rates, contact: Michael J. O’Brien II
Account/Relationship Manager
Wolters Kluwer
Phone: (978) 578-4514
Email: Michael.Obrien @ wolterskluwer.com
March Highlights
7
Add the 2023 Exhibit Hall to Your Boston ‘Must Do’ List
Set to kick off with an Opening Luncheon on Sunday, April 23, and run through Wednesday, April 26, this year’s Exhibit Hall promises to be four days of the meeting you won’t want to miss!
8
New Brain & Life Book: Navigating the Challenges of Concussion
The latest volume in the Brain & Life® Books series, co-authored by AAN member Michael S. Jaffee, MD, FAAN, has been published.
25
Self-advocacy, Positivity Guides Leadership Graduate to New Heights
Christine Doss Esper, MD, is quick to attribute recent impressive career successes, at least in part, to skills—and confidence—she gained through her experience in the AAN’s Women Leading in Neurology (WLN) program.
AAN Chief Executive Officer: Mary E. Post, MBA, CAE

News Briefs
Stay Updated on Extended Telehealth Flexibilities
Editor-in-Chief: Melissa W. Ko, MD, MBA, CPE, FAAN

Managing Editor: Angela M. Babb, MS, CAE, APR
Editor: Tim Streeter
Writers: Ryan Knoke and Sarah Parsons
Designer: Siu Lee
Email: aannews@ aan.com
AANnews® is published monthly by the American Academy of Neurology for its 38,000 members worldwide. Access this magazine and other AAN publications online at AAN.com.
The American Academy of Neurology ’s registered trademarks and service marks are registered in the United States and various other countries around the world.
“American Brain Foundation” is a registered service mark of the American Brain Foundation and is registered in the United States.
The inclusion of advertisements and/or promotions of Sponsors and other Internet sites or resources that offer content, goods, or services on the Website does not imply endorsement of the advertised/promoted products or services by AAN.
Many of Medicare’s pandemic telehealth flexibilities, including place of service and audio-only, were extended through December 31, 2024, in the Consolidated Appropriations Act, 2023. This legislation supersedes many of the regulations stipulating that telehealth flexibilities would last only through the duration of the federal public health emergency related to COVID-19. For a breakdown of these updates, visit AAN.com/telehealth
Permanent Standard Time Endorsed
The AAN has endorsed the American Academy of Sleep Medicine position statement supporting the benefits of permanent standard time for optimal brain health. The position statement calls for abolishing seasonal time changes in favor of a fixed, national, year-round standard time. Visit AAN.com/advocacy/position-statements to learn more.
AAN Member Services Wins National Award
The AAN won the 2023 National Customer Service Association Service Team of the Year award for its Member Services team. The awards recognize teams and organizations that consistently go the extra mile to provide the best in service to their customers.
AANnews · March 2023
Brain Health Initiative Plays to AAN’s Public Education Strengths
Over the past year, the AAN has begun to lay the foundation for an expansive plan to closely examine brain health and serve as the leading authority of unbiased neurologic information and public education in the field. Towards that end, the Committee on Public Engagement, under the leadership of David A. Evans, MBA, chair, and Natalia S. Rost, MD, MPH, FAAN, FAHA, vice chair, has been hard at work developing the framework for a multi-year initiative to address brain health through the lifespan. The framework, divided into five epochs, focuses on brain function in specific years of life, each led by a member of the committee:
Fetal Epoch
Brenda Banwell, MD, FAAN
Brain health begins with neural development and is influenced by maternal, placental, environmental, and genetic factors. From birth through the early years of development, environmental enrichment, food security, educational opportunities, and a healthy familial microenvironment not only promote cognitive and emotional development, but also strongly mitigate early life genetic or acquired central nervous system injury. The advent of prenatal and newborn screening for treatable neurologic diseases is creating a new field of “preventive child neurology,” best exemplified by the availability and dramatic impact of gene therapy for infantile spinal muscular atrophy. Strong partnerships between maternalfetal medicine, neonatology, geneticists, and child neurologists will be essential to meet this changing landscape, including the need for new training programs in fetal-neonatal child neurology. Brain health begins at home, and families have great potential to enrich their children’s brain health.
Adolescence Epoch
Rana R. Said, MD, FAAN
The cornerstones of brain health in childhood, adolescence, and young adulthood include factors that extend beyond early life and also arise during these specific periods of growth and development. Important areas of focus include schools and education programs for children of all developmental abilities, including those with complex health care needs. Partnerships with colleagues and organizations focused on the health and well-being of children are vital. As we look at the global needs of children and adolescents, areas of focus will include interventions for conditions such as sleep, migraine, depression, and anxiety, with scalable programs tailored to meet the needs of all in this age epoch and address issues of resource distribution as a social determinant of health. Research and public policy are two arms of these initiatives, including direct-to-public messaging to understand the importance of brain safety, effects of sleep disruption, the impact of nutrition on brain health, toxins’ effects on the developing brain, and the mental health crisis.
Adulthood Epoch
Linda M. Selwa, MD, FAAN

In the adult age group, it is critical to develop and maximize healthy behaviors that prevent longer term illness and injury and to optimize the intellectual, social, and physical well-being supported by a healthy brain. We plan to focus our efforts on prioritizing discovery of preventive strategies to mitigate the effects of vascular disease, genetic predispositions, trauma, and toxins on the brain; advocating for reduced cost and equitable access to treatments or interventions that prevent disability and disease; enhancing the education of the public in existing healthy brain strategies; and establishing preventive brain health as a neurologic discipline.
Maturity Epoch
Sarah Song, MD, MPH, FAAN
The maturity age epoch has the job of looking backwards while moving forwards. We recognize three things: First, brain health and brain wellness are truly multifactorial, and to address them, partnerships with other disciplines and organizations will be key. Second, layered over every effort toward brain health is the need to address health equity. And finally, we must strike a balance between screening and prevention of medical conditions affecting brain health with treatment and rehabilitation of the sequelae caused by not addressing brain health. As a result, our recommendations center around innovative research strategies and building upon larger cohort studies; considering contributing issues in public policy such as nutrition, the environment, and mental health; and signaling the necessity of preventive care through publicizing brain health issues while recognizing the need to support caretakers, extend rehabilitation policies, and train the next generation of diverse neurologists.
Senescence Epoch
Daniel José Correa, MD, MSc, FAAN
True brain health must include consideration of quality of life (QOL) and the quality of end-of-life care (QEOL) in late life. These concepts are not only essential for the senescence age/“platinum” epoch,
4 A ANnews • March 2023 PRESIDENT'S COLUMN
Avitzur
but must be integrated into all life stages. As we advance brain health efforts to improve care and longevity, we also seek to support the hopeful increase of super-agers in our society. As a result, our recommendations center around expanding current research strategies to include QOL and QEOL; supporting public policy related to research and resources for the community to improve QOL; and adapting public and professional health education for these efforts. Future work will require continued feedback and collaboration across specialties and community advocacy organizations.
The team, along with many other experts in brain health, presented their work at the Brain Health Summit held on September 15, 2022, in Washington, DC. Multiple organizations attended, including patient organizations such as the Alzheimer’s Association, ALS Association, and LEAD Coalition, and specialty organizations including the National Institutes of Health, American Heart Association, and American Academy of Family Physicians. Earlier in the week, US Reps. Earl Blumenauer (D-OR) and Morgan Griffith (R-VA), successfully introduced a congressional resolution to designate September 15, 2022, as "National Brain Health Day."
As editor-in-chief of Brain & Life® for the past several years, I have witnessed the evolution of a remarkable compendium of material focused on wellness for the neurologic community and the general public alike.
We have amassed a large number of resources at BrainandLife.org and integrated existing AAN patient education onto the website. The Brain & Life® Books series has produced helpful educational materials for patients and caregivers, like the recent Navigating the Challenges of Concussion by Michael S. Jaffee, MD, FAAN.
Over the past year, the Brain & Life podcast has interviewed people living with neurologic conditions, celebrity advocates, as well as physicians and other experts on their experiences, sharing their stories and advice with an increasingly growing listenership. Episodes have included a two-part series on brain health for women and multiple segments on multiple sclerosis, Alzheimer’s disease, migraine, Parkinson’s disease, myasthenia gravis, and more. There are often suggestions to improve lifestyle, including how to use diet, exercise, and mindfulness to achieve wellness. To learn more, listen, and share with your patients, visit Brainandlife.org/Podcast and follow wherever you get your podcasts.
If you want to learn more about the AAN’s Brain Health Initiative, the 75th AAN Annual Meeting in Boston will feature a HeadTalk on Sunday, April 23, at 1:00 p.m. entitled, “A Global Brain Health Conversation.” Representatives from the World Federation of Neurology and the European Academy of Neurology, with whom we plan to collaborate in the future, have been invited to participate. The Innovation Hub at the Annual Meeting will bring you a presentation by Mr. Evans;
Dr. Rost; Justin T. Jordan, MD, MPH, FAAN; and Joel A. Salinas, MD, FAAN. They will discuss what’s next for the AAN’s Brain Health Initiative on Wednesday, April 26, from 11:30 a.m. to 12:30 p.m. As we continue this work over the next few years, we will be sure to keep you posted. In the meantime, please join me at the 75th AAN Annual Meeting in Boston to hear more.
Finally, it is my pleasure to announce that a new fund has been established to help support the Academy’s upcoming work in brain health. The Ralph L. Sacco, MD, Memorial Fund for Brain Health was recently launched with a generous bequest from Dr. Sacco, who served as AAN president between 2017 and 2019. Members are invited to donate to the fund in memory of Dr. Sacco at AAN.com/Sacco. Dr. Sacco dedicated his career to stroke prevention and the amelioration of brain health. He is the only neurologist to have served as both president of the AAN and president of the American Heart Association. It was his vision for our two organizations to work together, as he believed we could achieve new heights by joining forces.

It was on March 13, 1948, that the AAN was incorporated in its home state of Minnesota. As we take pride in our rich history and accomplishments, from founder Dr. A.B. Baker to Dr. Ralph Sacco, we are invigorated by ambitious projects like the Brain Health Initiative that build upon our successes and lift us toward an exciting future.
Orly Avitzur, MD, MBA, FAAN President, AAN oavitzur@aan.com @OrlyA on Twitter
A ANnews • March 2023 5
I enjoyed every interaction I had with Dr. Sacco. This conversation with him and Ann H. Tilton, MD, FAAN, took place at the Potamkin Award reception during the 2019 Annual Meeting.
Annual Meeting Hubs Foster Collaborative Learning Through Unique Delivery Methods
Step outside the traditional classroom and into the world of unconventional learning with the 2023 Annual Meeting Hubs. Eight focused areas provide deeper dives into your area of interest and opportunities to engage in collaborative learning, gain actionable tools for your patients and career, and find your community. From silly to inspiring, and interactive to introspective, Hubs provide creative programming you can't find anywhere else, and fun opportunities to document reconnections with old friends in one of the photo areas. This year’s Hubs include Academic, Innovation, Leadership University, Practice and Policy, Trainee and Educator, Research, Wellness, and the always popular HeadTalks.
Hub Spotlight
Trainee and Educator Hub
Access information and resources to connect trainees and educators through interactive panel discussions and games and career track exploration. Meet a mentor and create lasting connections with your peers through formal and informal networking opportunities. Look for:

Daily group networking sessions and neurology games
One-on-one and group mentoring opportunities
Award recognition
Programming to include:
Finding A Great Mentor / Being a Great Mentee
Everything You Want to Know About the Residency In-service Training Examination (RITE®)

A.B. Baker Award for Lifetime Achievement in Neurologic Education Presentation

Academic Hub
Engage in discussions about all aspects of an academic neurology career and department through interactive presentations, conversation corners, networking spaces, and mentoring opportunities. Find content tailored to anyone in an academic neurology department, from department chairs to medical students. Look for:
Stage talks focusing on the dynamic and emerging needs of academic neurology through career development; leadership; building community; supporting research, practice, and teaching; and addressing challenges with benchmarks and budgets
Conversation Corners offering discussion and connection with one or two experts on a specific topic
Networking spaces facilitating ongoing conversation after scheduled programming to connect new acquaintances and reconnect old friends
Learn more about 2023 Annual Meeting Hubs at AAN.com/AMHubs
Boston & Virtual • April 22–27
EVENTS
Add the 2023 Exhibit Hall to Your Boston ‘Must Do’ List
Participate in 2023 Neurology Compensation and Productivity Survey
continued from cover
New this year, the survey captures additional information for those practicing in the full-time telehealth model and for those delivering care in the inpatient setting.
Visit AAN.com/benchmark from March 14 through May 11 to complete the survey and ensure access to a wealth of data that can help you in your work.
Who benefits from completing the 2023 Neurology Compensation and Productivity Survey?
While planning your week in Boston, be sure to put the Exhibit Hall on your “must do” list. Set to kick off with an Opening Luncheon on Sunday, April 23, and run through Wednesday, April 26, this year’s Exhibit Hall promises to be four days of the meeting you won’t want to miss!

In addition to offering a wide array of opportunities to meet, mingle, and learn from pharmaceutical and medical device industry representatives, you’ll also find opportunities to:
Connect with other health organizations throughout the Association Neighborhood
Gather career resources and more in the Career Fair Recruiter Neighborhood
Discover cutting-edge technologies and therapies in the Emerging Technologies Neighborhood
Learn about pipeline products, new notable companies, and more at the Emerging Neurologic Care Presentation Stage
Welcome the return of the Innovation Hub with physician talks, paint and wine, and VR
Preview the latest products and services at Vendor Booths
Grab a free cup of joe and mingle at the Exhibit Hall Buzz Cafes
Keep your devices charged in the comfort of the Exhibit Hall Charging Lounges
In addition, the Exhibit Hall will feature these special social and networking events:
Opening Luncheon
Sunday, April 23, 11:30 a.m.–1:00 p.m.
Exhibit Hall Networking Crawl
Monday, April 24, 4:00 p.m.–6:00 p.m.
Innovation Hub Talks & Events
Sunday, April 23, 12:00 p.m.–4:00 p.m.
Monday, April 24, 11:30 a.m.–5:30 p.m.
Tuesday, April 25, 11:30 a.m.–4:00 p.m.
Wednesday, April 26, 11:30 a.m.–4:00 p.m.
US Neurologists and Advanced Practice Providers in All Organizational Settings
Benchmark key compensation metrics with your peers
Explore salaries using subspecialty data
Identify productivity, wRVU and $/wRVU benchmarks
Find teleneurology, telestroke, and other on-call services and reimbursement rates
Discover the teleneurology volume your colleagues provide
Learn benchmarks for full-time telehealth practice model
Review metrics for those providing inpatient care
Identify how other academic departments are funded
Gauge demand for neurologic services using total patient encounters and appointment wait times
Discover the proportion of time your peers spend in clinical and non-clinical activities
Evaluate key practice and department metrics filtered by your same organizational setting
Business Administrators in all Organizational Settings
Benchmark neurologist and neurology APP compensation and productivity
Compare salary by subspecialty
Benchmark on-call rates and duties
Gauge demand for neurologic services using total patient encounters and appointment wait times
Benchmark your salary against other business administrators
Review ancillary services to find new opportunities for your organization
Find out average size of other practices and their use of APP employee mix
Discover the payer mix for neurologic practices
A ANnews • March 2023 7 PRACTICE
How You Can Recognize Private Payer E/M Downcoding
Have you ever noticed lower reimbursement than what you expected from a private payer? In recent years, several private payers have announced downcoding programs for evaluation and management (E/M) services, the rationale being to reduce potentially inappropriate use of upper-level E/M services visits. Some payers use an algorithm-based program that assigns the E/M level based on diagnosis codes. While payers do provide updates to providers when they are implementing programs associated with downcoding (normally in the payer newsletters), the AAN wants to provide members with tips on how to identify downcoding:
Review your provider remittance or explanation of benefits. The payer may not change the actual coding on the claim, but the payment will be that of the level their program determined to be appropriate.
Familiarize yourself with advice codes. The following codes signal downcoding:
CO150: Payer deems the information submitted does not support this level of service
M85: Subjected to review of physician evaluation and management services


N610 Alert: Payment based on appropriate level of care
CARC 186: Level of care change adjustment
Payments are less than anticipated rates based on allowable.
If you notice downcoding, it is recommended to review the claim submitted to confirm if a lower level was appropriate. If you find the records don’t reflect the downcoding, you have the option to appeal the claim. When appealing, it is important to provide excerpts from the CPT E/M documentation guidelines or the payer’s medical policy to support your appeal.
Other tips to consider if your claim is downcoded:
The use of independent certified coders to evaluate the claims and medical records in questions may be beneficial and provide substance to any appeal.
Some of the information that supports the code level might not be in the progress note itself but on procedure sheets. These forms are sometimes overlooked when submitting records to a payer.
If you have any questions or would like more information, contact practice @ aan.com
New Brain & Life Book: Navigating the Challenges of Concussion
The latest volume in the Brain & Life® Books series, Navigating the Challenges of Concussion, has been published. The book is co-authored by AAN member Michael S. Jaffee, MD, FAAN, with Donna K. Broshek, PhD, ABPP-CN, and Adrian M. Svingos, PhD.
“Navigating the Challenges of Concussion helps patients and their families to sort through the noise and conventional wisdom to better understand the current state of knowledge of this common injury and its effects,” said Jaffee. “Armed with the knowledge and stories outlined in this book, individuals who have suffered a concussion can know what to expect in their recovery and how to lay the groundwork for improved postinjury outcomes. Moreover, as knowledge about concussion evaluation and management changes at a rapid pace, this book also keeps health care providers abreast of the latest clinical guidelines and encourages them to understand the patient experience more fully. The book addresses acute management as well as approaches to those with persisting symptoms and concerns for long-term sequelae. This is a soup to nuts guide that illuminates this condition for patients, caregivers, and health care providers alike.”

“I’m enthusiastic about having Concussion join the family of patient-oriented volumes in the Brain & Life Books series,” said David C. Spencer, MD, FAAN, editor of the series. “The Brain & Life Books series is designed to inform, guide, and connect with readers using understandable, non-technical language. Nowhere is this more needed than when someone has experienced and is recovering from a concussion. Over the years, concussion has been widely misunderstood and often discounted as minor or trivial. In Navigating the Challenges of Concussion, Dr. Jaffee uses clear language to dispel myths and guide patients and families using the best available evidence-based information on management and recovery while helping to avoid common pitfalls—and always with a reassuring hand on your shoulder.”
Navigating the Challenges of Concussion can be purchased online and from all major booksellers.
For more information, visit BrainandLife.org/Books
8 A ANnews • March 2023 PRACTICE
Spencer Jaffee
ADVOCACY
Capitol Hill Report
Capitol Hill Report presents regular updates on legislative and regulatory actions and how the Academy ensures that the voice of neurology is heard on Capitol Hill. It is emailed to US members twice monthly and is posted at AAN.com/view/HillReport. Below are some recent highlights.
ISSUE IN FOCUS
Reducing the administrative burdens faced by neurologists is a long-standing priority for the AAN.
The AAN works to address administrative burdens across multiple fronts to ensure that clinicians can spend more time on patient care and less on administrative tasks. Prior authorization (PA) in particular is often cited as a top concern among AAN members. PA is one of the most time-consuming and expensive administrative requirements preventing physicians from spending more time with patients. Over 90 percent of clinicians reported that PA requirements have a negative impact on patient clinical outcomes and 82 percent of clinicians reported that issues associated with PA can lead to patients abandoning a recommended course of treatment. A recent member survey indicated that AAN members believe addressing administrative burden associated with PA should be the AAN’s top priority for 2023.
On January 30, the AAN submitted comments to CMS urging the agency to implement a number of critical reforms to improve oversight of Medicare Advantage (MA) plans’ usage of PA. These comments are a critical element in several years of efforts to pressure CMS to address the growing PA burden in MA. The AAN was deeply disturbed by April 2022 findings from the Department of Health and Human Services Office of Inspector General relating to inappropriate PA denials which found that some PA requests were denied by MA plans, even though the requested services met
Medicare coverage guidelines The AAN strongly believes that Medicare beneficiaries enrolled in MA plans have the same access to covered services as those covered under Medicare Fee-for-Service. Key reforms contained in this proposed rule include: strengthening of evidentiary standards plans must use when developing PA policies, requiring greater alignment of MA PA policies with those in Medicare FFS, restrictions on the use of PA when patients transition between plans, and changes impacting reviewers of adverse decisions.
The AAN will continue its efforts to reduce PA-related burden and is currently working to draft additional comments to CMS in support of proposals advancing interoperability and improving the electronic exchange of health care data to streamline prior authorization processes. The AAN recognizes the importance of codification in legislation of important policies that prevent overly burdensome barriers to care. Last Congress, the Improving Seniors Timely Access to Care was one of the most widely supported bills, with 327 House and 53 Senate co-sponsors. The bill is likely to be reintroduced this Congress, pending reevaluation of the cost estimate from the Congressional Budget Office. AAN staff are keeping a close eye on this and other key legislative developments related to prior authorization.
A ANnews • March 2023 9
Proposed Slate of 2023–2025 AAN Board of Directors
Directors:
Wayne E. Anderson, DO, FAHS, FAAN
Jennifer Bickel, MD, FAAN*
Gregory J. Esper, MD, MBA, FAAN*
Larry B. Goldstein, MD, FAAN, FAHA
Lily Jung Henson, MD, MMM, FAAN
Shannon M. Kilgore, MD, FAAN
Jeffrey C. McClean II, MD, FAAN*
Bruce I. Ovbiagele, MD, MSc, MAS, MBA, MLS, FAAN
José H. Posas, MD, FAAN*
*New to the Board
The current President Elect, Carlayne E. Jackson, MD, FAAN, will begin her term as President on April 28, 2023. The current President, Orly Avitzur, MD, MBA, FAAN, will then serve on the Board of Directors as Immediate Past President. The following additional directors will serve as ex officio directors beginning on April 28:
Bruce H. Cohen, MD, FAAN, Chair, Advocacy Committee/ex officio
Brad C. Klein, MD, MBA, FAAN, Chair, Medical Economics and Practice Committee/ex officio
José G. Merino, MD, MPhil, FAHA, FAAN, Editor-in-Chief of
Neurology ®/ex officio
Maisha T. Robinson, MD, MSHPM, FAAN, Chair, Member Engagement Committee/ex officio
Mary E. Post, MBA, CAE, Chief Executive Officer/ex officio, non-voting
The Academy is comprised of two legal entities, the AAN and the AAN Institute. Most of the elected members of the AAN Board of Directors also serve ex officio on the Board of Directors of the AAN Institute, which includes an independent secretary-treasurer and additional members who serve in ex officio capacities. The AAN Institute Board of Directors will include the following additional members:
Brett M. Kissela, MD, MS, FAHA, FAAN, Secretary-Treasurer
Paul M. George, MD, PhD, FAAN, Chair, Science Committee/ex officio
Lyell K. Jones, Jr., MD, FAAN, Chair, Quality Committee/ex officio
José G. Merino, MD, MPhil, FAHA, FAAN, Editor-in-Chief of Neurology ®/ex officio
Joseph I. Sirven, MD, FAAN, Chair, Education Committee/ex officio
Mary E. Post, MBA, CAE, Chief

continued from cover
Executive Officer/ex officio, non-voting
The slate of nominees will be presented to the voting membership for approval during the AAN’s 2023 Business Meeting on Saturday, April 22, from 4:00 p.m. to 4:30 p.m. ET during the Annual Meeting. The voting members present at the AAN Business Meeting also will be asked to vote on approving the following Bylaws amendments for the AAN. Voting members are Fellows (FAAN) and Neurologists, and Honorary and Senior members who had voting privileges in their most recent previous category of membership.
Adding the Chair of the Diversity, Equity, and Inclusion Committee to the AAN Board in Article IV, Section 1
Replacing all mentions of “Executive Director” with “CEO” throughout the Bylaws
Replacing “Chairman” with “Chair” in Article IV, Section 5
A complete copy of the proposed AAN Bylaws amendments is available at AAN.com/AmendedBylaws
For more information, contact Karen Kasmirski, Senior Governance Coordinator, at kkasmirski @ aan.com
Meet the AAN and AAN Institute Boards of Directors Nominees
Officers
President
Carlayne E. Jackson, MD, FAAN, is professor of neurology and otolaryngology at the University of Texas Health Science Center San Antonio (UTHSCSA), where she serves as chair of the Department of Neurology and holds the Edna Smith Dielmann Distinguished University Chair. She has served as president elect of the AAN since April 2021.
Jackson is a graduate of Texas A&M University, where she received a Bachelor of Science degree in chemical engineering. She obtained her medical degree at UTHSCSA, where she subsequently completed her neurology residency training and
clinical neurophysiology fellowship. She has obtained board subspecialty certification in both clinical neurophysiology and neuromuscular medicine. She is a graduate of the Executive Leadership in Academic Medicine (ELAM) program sponsored by Drexel University College of Medicine.
Jackson serves as medical director for the South Texas ALSA Center of Excellence and the South Texas MDA Clinic. She is a member of the Western ALS Study Group, Northeast ALS Research Group, and the Muscle Study Group. She has participated in over 70 multicenter clinical trials in the areas of ALS, muscular dystrophy, and myasthenia gravis and has published over 260 abstracts, journal articles, and book chapters.
Jackson previously served as the chair of the AAN Meeting Management Committee and Board Planning Committee in
10 A ANnews • March 2023
MEMBERSHIP
addition to her role as secretary on the Executive Committee of the Board of Directors. She has also previously served the AAN as a member of the Science Committee, Meeting Management Committee, Leadership Development Committee, and the Board of Directors. She was a member of the Continuum® editorial board from 2007–2017. She co-chaired the ALS Measurement Development Panel and co-authored the ALS Practice Parameters. She has actively participated on the Education Subcommittee and the Neuromuscular Topic Work Group. Jackson participated in the Palatucci Advocacy Leadership Forum in 2013 and has been a delegate to Neurology on the Hill. She has served as a mentor in the Emerging Leaders Program, the Diversity Leaders Program, Women Leading in Neurology, and the Transforming Leaders Program and received the AAN Leading in Excellence Mentorship Award in 2017.


President Elect
Natalia S. Rost, MD, MPH, FAAN, FAHA, is chief of the stroke division at the Massachusetts General Hospital Department of Neurology and professor of neurology at Harvard Medical School. A cum laude graduate of Boston University School of Medicine, she also holds a Master of Public Health degree from Harvard School of Public Health. Rost trained in neurology and vascular neurology at Massachusetts General Hospital and Brigham and Women's Hospital residency and fellowship programs.
Rost is internationally recognized for her expertise in vascular neurology, neuroimaging of cerebrovascular disease, and big-data science applications to personalized clinical outcome prediction in acute stroke. A clinician-scientist at the helm of the ambitious research program dedicated to reducing global burden of stroke-related cognitive and functional disability, Rost is currently the MGH Research Scholar and Principal Investigator of DISCOVERY (www.discoverystudy.org), an innovative national clinical research network funded jointly by the National Institute of Neurological Disorders and Stroke/National Institute on Aging (U19NS115388) to address post-stroke cognitive impairment and dementia in diverse US populations.
Rost is the author of numerous peer-reviewed publications, book chapters, and co-author of the MGH Handbook of Neurology. She is the recipient of the 2012 Michael S. Pessin Stroke Leadership Award from the American Academy of Neurology, 2017 MGH Neurology Department’s Ray Adams Clinical Mentor Award, and 2021 Leading in Excellence Through Mentorship Award from the AAN Leadership Program. She is a Fellow of the American Academy of Neurology and American Heart Association, former president of the Boston Board of the American Heart Association (2014-2016), scientific chair of the 2022 NINDS Alzheimer’s Disease-Related Dementias Summit, and she serves as associate editor of the journal Stroke
Among her professional accomplishments, Rost is particularly proud of her career-long service to the American Academy of Neurology, where she currently serves as chair of the Science Committee and vice chair of the Committee on Public Engagement, including her key leadership role in the AAN’s Brain Health Initiative.
Vice President
Janis M. Miyasaki, MD, MEd, FRCPC, FAAN, is a graduate of the University of Toronto medical school, neurology residency program, and movement disorders fellowship. From 1994 to 1998, she was a community neurologist. In 1999, she became faculty at the University of Toronto, assuming the roles as director of education for neurology for four hospitals, ward chief, member of the board of trustees for the University Health Network; president of the Medical Staff Association; president of the Canadian Movement Disorders Group; deputy physician-in-chief, Toronto Western Hospital; and associate clinical director of the Movement Disorders Centre at Toronto Western Hospital from 2001 to 2013. In 2007, Miyasaki initiated the first neurologist-led palliative care for movement disorders in the world.

Since 2014, Miyasaki joined the University of Alberta and is currently division director neurology, Department of Medicine and Zone Section Head Neurology, Edmonton Zone; and co-director of the Neuropalliative and Advanced Symptom Management Clinic. She is an active clinical researcher, holding grants, mentoring young researchers in movement disorders, physician wellness, and equity (Scopus h-index 52). She is the first director of Equity, Diversity, and Inclusion for the Department of Medicine at the University of Alberta.
Her AAN activities began in 2000 through writing a guideline on Parkinson's disease. Since that time, she has worked on the Practice Committee, Technology and Therapeutics Subcommittee, Practice Improvement Subcommittee, Patient Safety Subcommittee, and Education Committee, Business Innovation Subcommittee, Physician Wellness and Burnout Work Group, Wellness Subcommittee, and numerous task forces. Miyasaki has been a member of the Board of Directors from 2011–2017, AAN treasurer from 2017–2021, and vice president of the AAN from 2021–2023.
Secretary
Sarah M. Benish, MD, FAAN, is currently the physician co-chief for M Health/ Fairview Neuroscience service line. She is an associate professor of neurology at the University of Minnesota and is also the division head for general neurology. She enjoys her clinic time as a general neurologist. Over her career, she has
A ANnews • March 2023 11
Continued on page 12 ›
MEMBERSHIP Proposed Slate of 2023–2025 AAN Board of Directors
developed an interest in treating headache patients but continues to enjoy caring for all neurologic diseases.
Prior to joining the University of Minnesota, she was a physician owner/partner at Minneapolis Clinic of Neurology, one of the largest physician-owned, single-specialty neurology clinics in the country. She spent seven years on its board of directors and was treasurer for one year. During her decade with this clinic, she learned a lot about the business of medicine and what it takes to survive in the days of modern medicine and payment reform.
Benish began her involvement with the AAN as a member of the inaugural class of the Emerging Leaders Forum. She has served on the Practice Committee, Quality Committee, Data Analytics Subcommittee, and Registry Subcommittee.
Treasurer
Charles C. Flippen II, MD, FAAN, is the Richard D. and Ruth P. Walter Professor of Neurology faculty member of UCLA Goldberg Migraine Program at the Ronald Reagan UCLA Medical Center, vice chair for Education in the Department of Neurology and associate dean of the Center for Continuous Professional Development at the David Geffen School of Medicine at UCLA (DGSOM).
Flippen is a diplomate of adult neurology of the American Board of Psychiatry Neurology (ABPN) and of headache medicine of the United Council of Neurologic Subspecialties. He is a member of the American Headache Society, International Headache Society, Fellow of the American Neurological Association, and Fellow of the American Academy of Neurology, where he serves as treasurer of the AAN.
In addition to his AAN activities, Flippen represents the ABPN on the Neurology Residency Review Committee of the Accreditation Council of Graduate Medical Education and

2023–2025 AAN Board of Directors
Wayne E. Anderson, DO, FAHS, FAAN, is a neurologist subspecialty certified in headache and pain medicine. Since childhood, he knew he wanted to be a physician and work with the brain but did not know which path to take: psychiatry, neurology, or something related such as neuroradiology. However, after a few medical school rotations, it became clear: neurology.
After residency at University of California, Davis, he worked in both solo and group practice models, including a hybrid private practice within a hospital-based neurology center. The different
continued from page 11
serves on several intramural committees in the DGSOM.
Flippen is also active within the general Los Angeles community through his service as a board member of 100 Black Men of Los Angeles, member of Sigma Pi Phi Fraternity, Delta Xi Boulé, and member of Alpha Phi Alpha Fraternity, Inc.

Immediate Past President
Orly Avitzur, MD, MBA, FAAN, is a practicing neurologist with offices in Tarrytown and Carmel, New York. She is a former chair of the AAN Medical Economics and Management Committee, the Practice Management and Technology Subcommittee, and the Audit Committee. She is editor-in-chief of Brain & Life®, the AAN's patient and caregiver magazine and website. Avitzur is a medical writer and has written for Neurology Today ®, the official news source of the AAN, reporting on trends and innovations in the practice of neurology since 2001. Her stories have included broad coverage of technology in clinical care; the evolution of the health care regulatory environment; the neurology pipeline; equity, diversity, and inclusion; and, most recently, neurologists on the front line during the COVID-19 pandemic.
For 10 years, Avitzur served as a health editor for Consumer Reports, and as its medical director from 2015-2018. She is the recipient of several APEX writing awards and the 2009 AAN Journalism Fellowship award. She attended Johns Hopkins University for her undergraduate studies and during medical school at the Pennsylvania State University, Avitzur received the Merck Award for Academic Excellence. She is a clinical instructor at Yale University School of Medicine in New Haven, CT, where she completed her neurology residency, and a clinical assistant professor at New York Medical College in Valhalla, NY. She received her Master of Business Administration from the University of Connecticut.

practice models offered a unique understanding of the benefits and challenges of both employed and private practices.
He has been actively engaged in Academy projects, participating on the Practice Committee, eLearning Subcommittee, Advocacy Engagement Subcommittee, and in several work groups. He has represented the American Academy of Neurology in joint work groups in other specialties, including the American Board of Anesthesiology exam writing committee and the American Academy of Ophthalmology workforce on vision and concussion. A graduate of both the Palatucci Advocacy Leadership Forum and the Transforming Leaders Program, he is dedicated to the field of neurology
12 A ANnews • March 2023
and is passionate about ensuring the future of the profession. In addition to advocacy programs such as Neurology on the Hill, current projects include promoting awareness of the importance of neurology through public education.
Jennifer Bickel, MD, FAAN, is the chief wellness officer for Moffitt Cancer Center in Tampa, FL, where she is charged with creating system change to improve professional well-being through an operational emphasis on meaningful, essential work; a culture that promotes well-being; and through tailored support programs. She is also a professor of oncologic science at the University of South Florida. She serves as the chair of the American Academy of Neurology’s Wellness Subcommittee and as a member of the National Academy of Medicine’s Action Collaborative on Clinician Well-being and Resilience. She attended medical school at the University of Missouri-Kansas City and completed her neurology residency at University of Kansas Medical Center.
As a headache medicine specialist, Bickel served at Children's Mercy Hospital in Kansas City, MO, until 2021 as chief of the headache section and as the headache medicine fellowship director. Her clinical program provided comprehensive care to children and adolescents with headaches including injections, infusions, medical acupuncture, mental health support, and clinical research. As a neurology educator, she has been active in many areas, including holding roles as the course director for medical neuroscience and as the SIGN advisor at University of Missouri-Kansas City. As faculty of the American College of Healthcare Executives, she leads seminars for health care administrators on how to prioritize clinician well-being within health care operations.
Bickel has been active in the AAN for over a decade, beginning with participating in the Palatucci Advocacy Leadership Forum in 2012 and in following years as advisor and faculty. Additionally, neurology advocacy includes serving on the BrainPAC Executive Committee, attending Neurology on the Hill, and leading grantsupported community outreach programs. In 2016, she became involved in AAN education through a focus on undergraduate education and the medical student pipeline. Currently, she is a member of the Education Committee. In 2017, she graduated from the AAN’s Transforming Leaders Program and later served as project advisor and physician liaison for the program. Since 2017, she has been a member of the Editorial Advisory Board for Neurology Today®. As the chair of the AAN Wellness Subcommittee, she also serves on the Member Engagement Committee.

Gregory J. Esper, MD, MBA, FAAN, is professor of neurology at Emory University School of Medicine and is a general neurologist. He earned his medical degree at Vanderbilt University, completed neurology residency at Washington

University in St. Louis, and finished a clinical neurophysiology fellowship and a clinical research fellowship in electrical impedance myography with Dr. Seward Rutkove at Harvard University's Beth Israel Deaconess Medical Center. He earned his MBA from Emory’s Goizueta Business School in 2009. Esper was recently recognized in Emory’s Physician Group Practice as a Diamond Provider, earning 99-percentile patient satisfaction ratings.
Esper serves Emory Healthcare as associate chief medical officer, a role that promotes systemwide standardization in clinical workflows across the growing 11-hospital academic health system with over 220 outpatient sites. He is the vice president of Lean Promotion, in which he leads Emory’s systemwide initiative for lean transformation. He is the medical director for Emory’s Connected Care systemwide telehealth program. He also serves as vice chairman of clinical affairs for the Emory Department of Neurology. Esper enjoys an appointment as affiliated professor of business administration at Emory University and is a member of Goizueta Business School’s corporate advisory board.
Esper currently serves the American Academy of Neurology as the chair of the Health Services Research Subcommittee, as a member of the Medical Economics and Practice Committee, and as a member of the Academic Committee. He is a member of Vizient’s Risk Adjustment Committee and Neuroscience Quality and Accountability Steering Committee. He recently served as a member of the American Association of Medical College’s COVID-19 Clinical Guidance Repository Working Group. He publishes and lectures on such topics as telemedicine, lean implementation in health care, health care reform, value-based care, medical economics, leadership, and talent management. He is passionate about health services research and envisions a nationally connected landscape for neurology-related discovery that defines the impact of health care reform on neurologists and how neurologists continue to add value to the US health system as health care evolves.
Esper is married to Dr. Christine Doss Esper, who herself is associate professor of neurology at Emory University and a movement disorders specialist. They have three children who enjoy sports, music, and TikTok. Esper is a violinist and a singer who enjoys opera, musical theater, and Byzantine chant.
Larry B. Goldstein, MD, FAHA, FAAN, is professor and chair of the Department of Neurology, associate dean for Clinical Research, co-director of the Kentucky Neuroscience Institute, co-director of the UK Neuroscience Research Priority Area, and interim director of the UK-Norton Healthcare Stroke Care Network at the University of Kentucky. Goldstein received his BA in 1977 from Brandeis University and MD from Mount Sinai School of Medicine in 1981. His subsequent professional training included an internship and neurology residency at Mount Sinai Medical
A ANnews • March 2023 13 Continued on page 14 ›
Proposed Slate of 2023–2025 AAN Board of Directors
Center (1981–1985) and a research fellowship in cerebrovascular disease at Duke University (1985–1987).
Goldstein advanced at Duke to the rank of professor of neurology and director of the Duke Stroke Center until moving to the University of Kentucky in 2015.

Goldstein’s clinical and scholarly work focuses on stroke and related disorders. He has published over 820 peer review journal articles, reviews, editorials, book chapters, abstracts, and other professional papers. His research spans strokerelated laboratory-based studies, clinical trials, quality of care and care delivery studies, as well as clinical effectiveness and epidemiological investigations. He serves as a reviewer for multiple professional journals as well as national and international granting agencies. He is a member of the editorial boards of Stroke, Cerebrovascular Diseases, the Journal of Stroke and Cerebrovascular Diseases, and Cardiology Today. He has chaired or been a member of several national guideline writing committees.
Goldstein has been a member of the AAN Quality Standards Subcommittee (2005–2007), the Practice Committee (2007–2015), the Stroke Systems Work Group (2007–2017), the Education Committee (2017–current), the Joint Audit Committee (2017–2012; vice chair 2019–2021), Neurology Chair’s Work Group/Subcommittee (2018–current), Health Policy Subcommittee (2019–current), and is an AAN Media Expert (2019–current). He has been a member of the Board of Directors of the American Heart Association (2002–2004, 2008–2011), as well as having multiple leadership roles within the organization. He was also appointed to the FDA Peripheral and Central Nervous System Advisory Committee (2005–2009; 2014–2019) and served as advisor or panel member for several other FDA committees in addition to the CMS Medicare Evidence Development & Coverage Advisory Committee (2013–2015), and as a member of the National Committee for Quality Assurance Advisory Committee.
Goldstein received the AAN’s G. Milton Shy Award (1979) and numerous other national and state awards. He was awarded the Order of the Long Leaf Pine, North Carolina’s highest civilian honor, by the governor in 2015 for his service to the state related to improving stroke care.
Lily Jung Henson, MD, MMM, FAAN, is the chief executive officer of the Piedmont Augusta Hub in Augusta, GA. Prior to that she served three years as the CEO of Piedmont Henry Hospital in Stockbridge, GA. She formerly served as the chief medical officer at Piedmont Henry as well as the former chief of neurology of the Piedmont Healthcare System in Atlanta, GA. Prior to her move to Atlanta in 2015, Henson served as the vice president of medical affairs of Swedish Ballard Hospital in Seattle, WA,
continued from page 13
after her tenure as the inaugural chief of staff of Swedish Issaquah Hospital.
Henson has been a neurologist with 30 years of practice with a focus on multiple sclerosis and a principal investigator in many clinical trials involving MS disease-modifying therapies. She was an associate professor of neurology at the University of Washington Medical School.

Henson attended the Honors Program in Medical Education at Northwestern University in Chicago, where she obtained her BS and MD degrees. She completed her neurology training at the University of Washington in Seattle. She went on to get a certificate of medical management and a Master of Medical Management through Tulane University’s School of Public Health and Tropical Medicine. She is a 2016 ACHE Thomas Dolan Executive Diversity Scholar. She is a fellow of the American College of Healthcare Executives and a past regent-at-large of District 2.
Henson is the former chair of the board of directors of the Hands of Hope Clinic in Stockbridge, GA. She served on the national board of directors of the National Multiple Sclerosis Society, the board of managers of Fast Forward, and was a board trustee of the Georgia Chapter and the Greater Northwest Chapter of the NMSS. She also served as the chair of BrainPAC of the American Academy of Neurology, the advocacy editor of the AAN’s website, and as vice chair of the AAN Government Relations Committee.
Shannon M. Kilgore, MD, FAAN, serves as the deputy associate chief of staff for education at the Veterans Affairs Health Care System in Palo Alto, CA. In addition to her education role, her clinical focus is in primarily movement disorders, though she also directs stroke care at VA Palo Alto. With a keen interest in medication safety and fairness in pharmaceutical pricing, Kilgore represents neurology on the Medical Advisory Panel to Pharmacy Benefits Management, which determines the formulary for the Department of Veterans Affairs.
Kilgore obtained her Bachelor of Arts in psychology from the University of Texas at Austin, and her Doctor of Medicine from the University of Texas Health Science Center at Houston/McGovern Medical School. She then completed her neurology residency and fellowships in both cerebrovascular disease and movement disorders at Stanford. She brought this unique combination of experience to the VA, where she has taught medical students, neurology residents, and geriatrics fellows in both outpatient and inpatient settings, as a clinical associate professor, affiliated of Stanford’s Department of Neurology. At Stanford, she serves as the site director for the neurology residency program and as a member of the Clinical Competency Committee.
14 A ANnews • March 2023 MEMBERSHIP
Kilgore has maintained a long-held passion in combining both education and advocacy. She served on the ACGME Review Committee for Neurology twice, both as a resident/ fellow, and again as a full member, vice-chair, and chair. She has continued work within the ACGME on multiple Milestones committees. Having represented the AAN at the American Medical Association (AMA) since 2004, she was elected to the AMA’s Council on Medical Education in 2019, allowing her to advocate for medical students, residents, international medical graduates, and practicing physicians to the various accreditation/ certification/licensure and oversight bodies within medicine. In this capacity, she now represents the AMA to the Accreditation Council for Continuing Medical Education Board of Directors.
Kilgore also serves the Academy on the Editorial Board of Continuum: Lifelong Learning in Neurology ® and the Education Committee, overseeing the Program Accreditation Work Group. She has also been a member of the Government Relations Committee and has served on multiple task forces. A member of the 2014–2015 Emerging Leaders Forum class, she now enjoys giving back to the AAN as a mentor within the various AAN Leadership Programs.
Jeffrey C. McClean II, MD, FAAN, is currently chair of the Department of Medicine at Brooke Army Medical Center (BAMC), the largest, busiest hospital in the Department of Defense health system. Previously, McClean was deputy chair for the BAMC Department of Medicine, and prior to this he served four years as the program director of the only neurology residency in the US Air Force (USAF). He is an associate professor of neurology with the Uniformed Services University of the Health Sciences (USUHS). He is also the neurology chief consultant to the USAF surgeon general, providing guidance for a network of neurology clinics across the country and overseas.
McClean obtained his undergraduate degree from Harvard College in 1999 and his medical degree from USUHS in 2005. After finishing his neurology residency at Wilford Hall Medical Center in 2009, he completed a fellowship in neuromuscular medicine at Harvard (Brigham & Women’s Hospital and Massachusetts General Hospital) in 2010.
His engagement with the AAN began with his participation in the Emerging Leaders Forum in 2013–2014. He has served on the Member Engagement Committee, Digital Strategy Subcommittee, Diversity Leadership Subcommittee, and Nominations Committee. He is a member of the Brain & Life® Editorial Board and was a founding co-editor of Equity, Diversity, and Inclusion for Neurology® He is vice chair of the Leadership Development Committee; chair of the Inclusion, Diversity, Equity, Anti-racism, and Social Justice Subcommittee; and previously served as chair of the AAN Special Commission on Racism, Inequities, and Social Justice. McClean is also a member of the Alpha Omega Alpha Honor Medical Society and an AOA Leadership Fellow.

Bruce Ovbiagele, MD, MSc, MAS, MBA, MLS, FAAN, is professor of neurology and associate dean at the University of California, San Francisco, as well as chief of staff at the San Francisco Veterans Affairs Health Care System. Prior to these roles, he served for six years as professor of neurology and chair of the department of neurology at the Medical University of South Carolina. His primary research involves the translation of evidencebased interventions into clinical practice and community settings to improve stroke outcomes for underserved and vulnerable populations in the United States and around the world. He currently leads several NIH-funded studies of stroke in the US and sub-Saharan Africa. Ovbiagele has published over 600 peer-reviewed articles (h-index 87) in the areas of stroke prevention, epidemiology, risk factors, and outcomes, and has edited five textbooks. His work has been recognized with several awards including the Michael S. Pessin Stroke Leadership Award and Robert Wartenberg Lecture award from the AAN; Penn Award from the American Neurological Association; Mridha Humanitarian Award from the American Brain Foundation; Feinberg Award and Stroke Council Award from the American Stroke Association; Haddock International Impact Award and Distinguished Scientist Award from the American Heart Association; and Meritorious Achievement Award from the National Medical Association.
Ovbiagele has been a member of the AAN since 1998. He has been privileged to serve on several committees and subcommittees including the Clinical Research Training Fellowship Award Committee, Clinical Research Subcommittee, Minority Scholars Subcommittee, and Education Committee. He was a Neurology on the Hill participant in 2008, Palatucci Advocacy Leadership Forum graduate in 2009, and Minority Scholars Visiting Professor to Morehouse School of Medicine in 2011. He has served as director of stroke courses at both the Annual Meeting and Fall Conference, faculty chair/guest editor for a Continuum® issue, and abstracts reviewer for the AAN Annual Meeting. He presently directs the Health Equity for Neurologists course at the Annual Meeting. Ovbiagele is a member of the AAN’s Media Expert Panel.
Ovbiagele chaired the International Stroke Conference (2016–2018), served as an associate editor of Stroke (2020–2022), and is the current editor-in-chief of the Journal of the American Heart Association. He is an elected member of the National Academy of Medicine and Association of American Physicians; as well as an elected fellow of the World Academy of Sciences, World Stroke Organization, American Association for the Advancement of Science, Royal College of Physicians (London), and Royal Society of Public Health.

A ANnews • March 2023 15 Continued on page 16 ›
Proposed Slate of 2023–2025 AAN Board of Directors
José H. Posas, MD, FAAN, is a sports neurologist at Ochsner Health in New Orleans, LA. He serves as the Ochsner Neurology Residency Program Director, the Neurology Department Chief Diversity Officer, as well as serving on the Ochsner Health Physician Diversity Council. He is assistant clinical professor of the Ochsner Clinical School/ University of Queensland Medical School program.

He has been passionate about equity, diversity, and inclusion (EDI) efforts and was formally recognized as such since graduating from the AAN Diversity Leadership Program in 2017. Posas has previously contributed to the AAN EDI Joint Coordinating Council and mentored the student-run Neuro Equity Coalition. Accomplishments at his institution include having EDI efforts front and center for quality improvement initiatives and giving talks to physician leads systemwide and across the state of Louisiana. He is a founder of El PODER, which is a future physician shadowing and observer opportunity to marginalized and minoritized individuals at the high school and collegiate level. At the AAN, he is proud to serve as chair of the Underrepresented in Neurology SynapseSM Group, chair of the Innovation Hub, and active member of the IDEAS, eLearning, and Pipeline Subcommittees. Posas is the face of the AAN’s NeuroPanels and thrilled to be able to connect experts in their various subject matters in a less formal manner to learners at the graduate level and beyond to complex, subspecialty concepts for non-subspecialist. He plays Dungeons and Dragons with other AAN members mostly for fun, and at times for BrainPAC. He has a penchant for bowties and sneakers, is an avid coffee drinker, and purveyor of puns and dad jokes.

Posas went to Louisiana State University Health Sciences
School of Medicine in New Orleans to complete his medical degree. He completed his neurology residency at the University of Miami at Jackson Memorial Hospital in Miami, FL, where he was administrative chief in his senior year of training. He completed fellowship in sports neurology at Kerlan Jobe Orthopaedic Clinic in Los Angeles, where he was the inaugural Sports Neurology Fellow.
Ex Officio (voting)
Bruce H. Cohen, MD, FAAN, is the director of the NeuroDevelopmental Science Center and Director of Scientific Affairs and Clinical Trials of the Rebecca D. Considine Research Institute at The Children’s Hospital Medical Center of Akron, and professor of pediatrics and professor of integrative medical sciences at Northeast Ohio Medical University. He holds the Phillip H. Maynard Chair in NeuroDevelopmental Sciences. Cohen attended Washington
continued from page 15
University, graduating summa cum laude with a BA in chemistry. He attended the Albert Einstein College of Medicine of Yeshiva University.
Following pediatric training at The Children’s Hospital of Philadelphia, he did his neurology training at the Neurological Institute of New York, before returning to Children’s Hospital of Philadelphia for a fellowship in pediatric neuro-oncology. He spent the next two decades at The Cleveland Clinic, serving as a pediatric neurologist, neuro-oncologist, and practicing neurogenetics before moving to Akron Children’s Hospital in 2011 to pursue work in clinical trials. His clinical practice is centered on caring for children and adults with mitochondrial disorders, neurogenetic illness, and brain tumors, and he has a busy clinical research practice. His administrative responsibilities dovetail into his academic and practical interests in health care economics and health care delivery models.
Cohen’s academic career initially involved clinical trials for treatment of brain tumors in infants and children, and then transitioned in the emerging field of mitochondrial medicine. He also developed an interest in health care economics and practice management in the early 1990s. Cohen has served as chair of the Child Neurology Section of the American Academy of Neurology, chair of the Practice Committee of the Child Neurology Society, and chair of the Coding Subcommittee of the Medical Economics and Management Committee of the AAN. He has served as secretary-treasurer, and currently serves as president of the Child Neurology Society. In 2010, he joined the AAN’s CPT team and became the lead advisor to the CPT Panel from 2016–2022. In 2021, he took on two new additional roles within the AAN: chair of the Advocacy Committee (which includes all the subcommittees covering the legislative and regulatory work) and a seat on the Board of Directors. Cohen has participated in the education of dozens of neurology residents and fellows; led over a dozen international symposia; organized and conducted investigator-initiated clinical trials in brain tumors, neurofibromatosis, and mitochondrial disorders; and has authored 130 peer-reviewed manuscripts and delivered 670 invited lectures.
Brad C. Klein, MD, MBA, FAAN, is a full-time practicing neurologist with additional certifications in headache medicine and electromyography in his private practice at Abington Neurological Associates, Ltd., in Abington, PA. He has been a participant, principal, and/or coordinating investigator in numerous clinical trials and further serves as the practice’s chief financial officer. He is also the director of the Abington Headache Center, Abington-Jefferson Health, and a clinical professor of neurology at Thomas Jefferson University (TJU).

16 A ANnews • March 2023 MEMBERSHIP
He received his medical degree from Sidney Kimmel Medical College, previously known as Jefferson Medical College, at TJU in Philadelphia, concurrently with his Master of Business Administration degree at Widener University. He completed his neurology residency and headache fellowship at Thomas Jefferson University Hospital.
During Klein’s residency, he graduated from the Palatucci Advocacy Leadership Forum and founded the Pennsylvania Neurological Society, serving as its first president. Through his tenure, he provided multiple testimonies to the state legislature and was an advisor on multiple legislative bills. Thereafter, he served in a number of other state and national leadership roles, including treasurer of the Alliance for Headache Disorders Advocacy, chair of the Practice Management Committee of the American Headache Society, and Governor-appointed member of the Pennsylvania Health Care Cost Containment Council.
Within the AAN, Klein has served as a member of the Practice Management and Technology Subcommittee, Health Services Research Subcommittee, Benchmark Survey Work Group, Solo and Small Practice Work Group, Meeting Management Committee, many education topic work groups, as well as chair of the Medical Economics and Practice Committee.
He has been the recipient of numerous local, regional, and national awards, including “Patient’s Choice Award,” and Castle Connelly’s “Top Doctor.”
José G. Merino, MD, MPhil, FAHA, FAAN, is a professor in the department of neurology at Georgetown University Hospital, where he is also co-vice chair for education. Merino studied medicine at the Universidad Anáhuac in Mexico City and obtained a Master of Philosophy degree on the history of medicine from the University of Cambridge in England. He trained in neurology and psychiatry at the Albert Einstein College of Medicine and in stroke at the University of Western Ontario. He has worked as faculty and clinical staff of the Section of Stroke Diagnosis and Therapeutics of NINDS, the University of Florida, Johns Hopkins Medicine, and the University of Maryland. His clinical and research interests focus on the management of patients with acute stroke. Merino has been engaged in editorial pursuits throughout his career. He has been a member of the editorial board of Stroke, the Revista Mexicana de Neurociencia, and science editor of AAN.com. Most recently, he was the US research editor of The BMJ from 2012 until 2019.
He has served the AAN as a member of the Science Committee, Nominations Committee, Meeting Management Committee, Leadership Development Committee, and immediate past chair of the Diversity Leadership Subcommittee. Currently, he is editor-in-chief of Neurology ® journals, is a member of the editorial board of the AAN’s Brain & Life® en Español, and is chair of the Publication Committee.

Maisha T. Robinson, MD, MSHPM, FAAN, is an assistant professor in the Department of Neurology at Mayo Clinic in Florida, with a joint appointment in the Department of Internal Medicine. Upon joining the staff of Mayo Clinic, she established the clinic’s first neuropalliative care program and she currently serves as the chair of the Division of Palliative Medicine and as the program director for the Palliative Medicine Fellowship.
Robinson earned her undergraduate degree from Princeton University and her medical degree from Tufts University School of Medicine, subsequently completing a residency in neurology at Mayo Clinic in Minnesota, where she served as chief resident. She pursued a fellowship in hospice and palliative medicine at Memorial Sloan Kettering Cancer Center and returned to Mayo Clinic in Florida for a neurohospitalist fellowship. She was awarded a postdoctoral fellowship in health services and health policy research through the Robert Wood Johnson Foundation Clinical Scholars Program at UCLA, during which she earned a Master of Science degree in health policy and management and engaged in research focused on the intersection of neurology and palliative medicine. Robinson has spoken nationally and internationally on neuropalliative care, she edited a book titled Case Studies in Neuropalliative Care, and she is a member of the American Board of Internal Medicine Approval Committee on Hospice and Palliative Medicine.

Within the AAN, Robinson was selected for the inaugural cohort of the Emerging Leaders Forum and she has participated in the Palatucci Advocacy Leadership Forum. She has served as vice chair of the Meeting Management Committee, chair of the Medical Student Diversity Subcommittee, vice chair of the Pain and Palliative Care Section, and a member of the Leadership Development Committee, Diversity Leadership Subcommittee, Nominating Committee, and Medical Advisory Board of Brain and Life® magazine. She has also served as a mentor in the Emerging Leaders Program and in the Women Leading Neurology Program.
Ex Officio (non-voting)
Mary E. Post, MBA, CAE, is the chief executive officer of the American Academy of Neurology, the world’s largest association of neurologists with more than 38,000 members. Leading a team of more than 200 staff with locations in Minneapolis, MN, and Washington, DC, Post is responsible for the AAN achieving its mission of promoting the highest quality patient-centered neurologic care and enhancing member career satisfaction, as well as the AAN’s vision of being indispensable to its membership.

A ANnews • March 2023 17 Continued on page 18 ›
Proposed Slate of 2023–2025 AAN Board of Directors
Post began her position as CEO of the AAN in April 2020. She is the fourth CEO since the AAN was established in 1948. Post was selected for the role based on her extensive experience leading a major nonprofit medical specialty organization as well as her broad prior experience at the AAN, where she served for 16 years in many leadership roles, including as deputy executive director.
Post is a Certified Association Executive (CAE), the highest credential in the association management industry. She also holds a Post-Master’s Certificate in organizational leadership, a Master of Business Administration Degree in human resources, and a Bachelor of Science Degree in business administration. She has over 25 years of experience in the nonprofit medical specialty industry.
Post has led meaningful, sustainable, programmatic, operational, and financial growth within organizations while increasing value for stakeholders and creating an awardwinning, resilient culture.
In Post’s most recent position as the executive director for the
continued from page 17
American Board of Anesthesiology (ABA), she established a strong and collaborative partnership with its board of directors and 700 volunteer physicians to innovate and transform the organization’s programs.
Under Post’s leadership, the ABA became the first US medical specialty certifying board to successfully implement an Objective Structured Clinical Examination (OSCE) into the ABA’s initial certification program. In 2014, the ABA also reimagined its Maintenance of Certification in Anesthesiology Program (MOCA) and incorporated learning and assessment of knowledge into its physicians’ daily practice through MOCA Minute®
Post also led collaboration with the Accreditation Council for Continuing Medical Education (ACCME) and the CME community to link the ABA’s assessment with relevant CME programs. This collaboration positioned the ABA as a nationally recognized leader and demonstrated the benefits of partnering with other organizations to provide value to physicians.
2023–2025 AAN Institute Board of Directors
The AAN Institute Board of Directors will include the following additional members.
Secretary-Treasurer
Brett M. Kissela, MD, MS, FAHA, FAAN, is professor and chair of the Department of Neurology and Rehabilitation Medicine and senior associate dean for clinical research at the University of Cincinnati College of Medicine and Chief of Research Services for UC Health. Since 2008, he has been co-director of the Stroke Recovery Center at Drake and a member of the University of Cincinnati Stroke team since 2000. He is fellowship-trained in vascular neurology and has extensive clinical trial experience in acute stroke treatment, prevention, and recovery trials.
He is an internationally recognized expert on causes, outcomes, and recovery of stroke, with a special interest in the impact of diabetes on stroke and factors that influence stroke outcomes. He also participates in a variety of stroke recovery projects that look to improve recovery with the use of innovative techniques and devices. Honors and awards include the Cincinnati Business Courier's Forty Under 40 Award, Michael S. Pessin Stroke Leadership Prize from the American Academy of Neurology, Alpha Omega Alpha membership, National Medical Honor Society, Phi Beta Kappa, UC Faculty Senate Award, American Heart Association 2018-2019 Gold Standard Board Award (highest since the program’s inception), and has continuously been named as one of the Best Doctors in America (national surveys from Woodward-White and Best Doctors, Inc.).

Ex Officio (voting)
Paul M. George, MD, PhD, FAAN, serves on the faculty at Stanford University as a vascular neurologist in the Department of Neurology and Neurological Sciences. He is a physician-scientist focused on caring for neurology patients and improving neural recovery therapies. As faculty, he helped create a multi-disciplinary stroke recovery clinic at Stanford.
George received his undergraduate degree in Biomedical Engineering at Tulane University. He then pursued his graduate studies earning a Master from Johns Hopkins University and a doctorate from the Massachusetts Institute of Technology. He attended medical school at Harvard University before completing his residency and fellowship at Stanford University, where he served as chief resident. He has spoken nationally and internationally on stroke and neural recovery―a topic for which he has received national research funding and written numerous articles and reviews. George is also involved in Stanford’s neuroscience graduate program, serving on the admission and DEIB committees, and teaching the first-year Responsible Conduct of Research course.

18 A ANnews • March 2023 MEMBERSHIP
His lab applies bioengineering tools to better understand the brain’s recovery after stroke. His research group develops novel bioactive materials to interact with the nervous system. By modulating the recovering brain with these tools via electrical stimulation and stem cell therapies, his lab can decipher pathways of neural recovery. His lab then works to create translational therapeutics from these discoveries. With the AAN, he was selected as a member of the inaugural class of the Emerging Leaders Forum. He has also served as a member and vice chair of the Science Committee and chair of the Research Program Subcommittee. He is proud to continue his AAN involvement as the current chair of the Science Committee.
Lyell K. Jones, Jr., MD, FAAN, is a consultant, professor, and vice chair (education) of neurology at the Mayo Clinic in Rochester, MN. Jones received his undergraduate and medical degrees from Wake Forest University before completing his neurology residency and neurophysiology fellowship at the Mayo Clinic, where he has been a member of the consulting staff since 2009. Jones’s clinical and research focus is in neuromuscular medicine, particularly neurodegenerative, infectious, and autoimmune neuromuscular disorders.
Health care quality and value have been the central focus of Jones’s health system leadership roles. He currently serves as Mayo Clinic’s enterprise medical director of contracting and payer relations, overseeing Mayo Clinic’s commercial contract portfolio as well as its Strategic Contracting team. In his role as chair of Government Program Strategy at Mayo Clinic, he has led systemwide implementation of novel care models such as the Mayo Clinic Accountable Care Organization, an MSSP covering more than 60,000 lives. He is a former medical director for the Mayo Clinic Office of Patient Experience and chair of Payment Model Operations. Jones has served on numerous national committees, and as the chair of the American Academy of Neurology Quality Committee he oversees development of neurology practice guidelines, quality measures, and implementation of the Axon Registry ®. He currently serves on the Boards of Directors of the AAN Institute and the Mayo Clinic ACO.

Prior to joining the staff at the Mayo Clinic, Jones served in the Unites States Air Force at Wilford Hall Medical Center in San Antonio, TX. In his education leadership capacity at Mayo Clinic, Jones developed a Neurology Residency Health Disparities Initiative (NeuroHDI) and created an award-winning Neurology Residency Wellness Program. He is the current editor-in-chief of Continuum: Lifelong Learning in Neurology ®. He has been recognized with the AAN Program Director Award, the ACGME
Parker J. Palmer Courage to Teach Award, and has been inducted into the Mayo Clinic Teacher of the Year Hall of Fame.
Joseph I. Sirven, MD, FAAN, is professor of neurology and chair emeritus of the Department of Neurology at the Mayo Clinic in Arizona and currently practicing at Mayo Clinic in Florida. He is editor-in-chief of Brain & Life® en Español and on the editorial board of the English language Brain & Life®. He is currently chair of the AAN Education Committee. Previously, he served as director of education for Mayo Clinic Arizona with oversight over all educational activities at the Mayo Clinic Arizona campus, including medical student rotations, residencies, fellowships, PhD candidates, nursing, allied health, and continuing medical education programs.
In addition to being a neurologist, Sirven is a certified aviation medical examiner and a consultant to the Federal Aviation Authority (FAA) on pilot and passenger health. Sirven is a professor of practice in the College of Health Solutions at Arizona State University, where he teaches science of health care delivery to both undergraduate and graduate students. He previously served as chair of the AAN Education Conference Subcommittee and served on the Board of Directors for the American Brain Foundation. He was the previous vice chair of the Epilepsy Section of the American Academy of Neurology, chair of the Communication Council for the American Epilepsy Society, and former chair of the Professional Advisory Board for the Epilepsy Foundation.
Sirven is a bilingual Cuban American and served as chief medical contributor for NBC Latino, the English language website for Latinos by NBC News. He is currently host of “What’s Health Got to Do with It?” on WJCT-NPR North Florida. Previously, he served as the medical commentator for KJZZ radio in Phoenix, the NPR affiliate for Phoenix and Tucson Arizona, in addition to KTBS TV 3.
Sirven has published extensively on epilepsy and its treatment. He is editor of nine textbooks including Clinical Neurology of the Older Adult, the American Epilepsy Society’s Introduction to Epilepsy, Clinical Epilepsy, An Atlas of Video EEG Monitoring, Case Studies in Epilepsy, The Social Determinants of Health in Epilepsy and Epilepsy. He is currently a Neurology Core Clerkship director for Mayo Clinic College of Medicine and Dartmouth Medical School.

A ANnews • March 2023 19



















© 2022 Reata Pharmaceuticals, Inc. All Rights Reserved. US-NNU-2100006 05/2022 References: 1. Fogel BL, Perlman S. Clinical features and molecular genetics of autosomal recessive cerebellar ataxias. Lancet Neurol. 2007;6(3):245-257. 2. Indelicato E, Nachbauer W, Eigentler A, et al. Onset features and time to diagnosis in Friedreich’s Ataxia. Orphanet J Rare Dis 2020;15(1):198 3. Parkinson MH, Boesch S, Nachbauer W, Mariotti C, Giunti P. Clinical features of Friedreich’s ataxia: classical and atypical phenotypes. J Neurochem. 2013;126(suppl 1):103-117. 4. National Institute of Neurological Disorders and Stroke. Friedreich Ataxia Fact Sheet. Updated November 15, 2021. Accessed March 16, 2022. https://www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Fact-Sheets/Friedreichs-Ataxia-Fact-Sheet. *There may be additional uncommon symptoms. Get helpful resources and the latest FA information at ThinkFA.com.
FA is a severe disease that relentlessly progresses to loss of ambulation and independence in
all patients, identifying these early signs is crucial.3 Falls1 (gait ataxia) Imbalance1 (proprioception loss) Reflex loss1 (areflexia) Sensation loss1 (sensory neuropathy) Tiredness4 (fatigue) falls imbalance re ex loss tiredness sensation loss falls imbalance re ex loss tiredness sensation loss falls imbalance re ex loss tiredness sensation loss falls imbalance re ex loss tiredness sensation loss falls imbalance re ex loss tiredness sensation Think FA FIRST when you see any combination of these symptoms*: Initial symptoms of FA can be vague and overlap with other conditions.2,3 However, FA is the most common inherited ataxia. 4 Will you recognize it when you see it?
Because
nearly
FACT:
signs of Friedreich’s
Loss of balance is one of the early
Ataxia (FA), but it may not be this obvious.1
Jones Named 2023 President’s Award Recipient
AAN President Orly Avitzur, MD, MBA, FAAN, has honored Elaine C. Jones, MD, FAAN, with the 2023 President’s Award. Avitzur praised Jones, who “has been a dedicated member of the AAN for the past 27 years, during which time she has chaired the Government Relations Committee and the Coding and Payment Policy Subcommittee; served on the board of directors as well as numerous committees, work groups, task forces, and sections; and led the Gender Disparity Task Force. Her dedication to the AAN since her involvement in 1996, and to global volunteerism since 2011 when she first traveled to Port Au Prince, has been exceptional. She helped develop a network of neurologists who went to Haiti and trained local medical doctors and team members on how to care for neurologic patients, improving the management of stroke, Parkinson’s disease, migraine, and epilepsy. She returned regularly for eight years, volunteering her time to grow adult and child hospital services, and after being unable to travel in person, she continued to support the local Haitian medical community via telehealth.
“She has been a consummate advocate in neurology, and her generosity of service and altruism has earned the universal admiration of the many colleagues who have worked with her
 Jones
Jones
over the years. I am honored to present her with the 2023 President’s Award.”
Jones stated, “I am extremely honored to receive this year’s AAN President’s Award. However, it is thanks to the opportunities provided by the AAN that I am even eligible for this award. Early on in my career I stumbled on the AAN’s new program for leadership training, the Palatucci Advocacy Leadership Forum, and I immediately discovered the nurturing and family environment that the AAN offers. I always assumed professional organizations were meant for academic and scientific experts, and someone like me in a solo, private practice just went for the educational opportunities. However, it is clear the Academy supports all members of the neurological community with advocacy, business resources, and life/wellness needs, along with the excellent educational opportunities. The roles I have held at the Academy and the friendships I have made have truly enhanced my professional and personal lives. I am grateful to the Academy for supporting me and allowing me to get involved in the advancement of neurology both in the US and abroad.”
Support Our AAN Members in Türkiye and Syria
According to these principles, the AAN should engage in assisting neurology communities during times of humanitarian need when the event directly impacts neurologists and their care of neurology patients and be guided by humanitarian principles of humanity, neutrality, impartiality, and independence.
Coming together as a neurology community in times of need to help one another and deliver on our mission to provide the highest quality patientcentered neurologic care is what makes the AAN a truly exceptional organization.
Thank you for supporting our colleagues in Syria and Türkiye during these difficult days and being a part of our neurology community.
Sincerely,
Orly Avitzur, MD, MBA, FAAN President, AAN oavitzur@aan.com @OrlyA on Twitter
With more than 250 AAN members in Türkiye and Syria, we acknowledge the incredible devastation caused by this week’s earthquake and the ensuing hardship our AAN members are facing providing neurologic care in this region. While we continue to learn more about how the AAN can support our members in Türkiye and Syria during this time, we would like to encourage other AAN members to consider making a donation to the International Federation of Red Cross and Red Crescent Societies or other reputable charities. In recognition of the many humanitarian needs across the world, the AAN recently adopted guiding principles for how the AAN consistently responds to global events requiring humanitarian assistance.
A ANnews • March 2023 21 MEMBERSHIP
Attend Health Care Equity Symposium at Annual Meeting
Inclusion is the reason the AAN was founded. To be an organization that is the home for all neurologists. It is what makes us stronger. To support our goal of being a fully inclusive, deliberately diverse, and anti-racist organization and our core values of Inclusion, Diversity, Equity, Anti-racism, and Social Justice (IDEAS), we are excited to share progress and updates with you.
CESC: 21_NeuroByte Ad—Half Page Horizontal> AN Placed in AANnews

In today’s world, the reality is that access to quality health care varies greatly depending on race, gender, socioeconomic status, and many other factors. Join us at the Health Care Equity Symposium at the 2023 Annual Meeting as we explore ways we can eliminate the disparity gap. This event, from 1:00 p.m. to 4:30 p.m. on Monday, April 24, includes the Cheryl A. Jay Keynote Lecture, panel discussions, recognition and presentations from the winners of the Health Care Equity Research Award, and opportunities to engage with peers on topics relating to health care equity. This session will feature the third annual Cheryl A. Jay Keynote Lecture, honoring the gifted clinical neurologist who was passionate about social justice in health care and serving the underprivileged. This year, the Cheryl A. Jay Keynote
8.25 x 5.25 +0.125 bleed, 4C
Lecture will be presented by Olajide A. Williams, MD, MS, a professor and chief of staff of the department of neurology at the Columbia University Vagelos College of Physicians and Surgeons. A specialist in the treatment of stroke and cerebrovascular diseases, Williams is also an attending physician at New York-Presbyterian Hospital and a clinical neurologist at Columbia University Irving Medical Center. He attained his medical degree from the University of Lagos, Nigeria, and completed his neurology residency and neuromuscular fellowship training at The Neurological Institute of New York. He also holds a Master of Science degree from the Columbia University Mailman School of Public Health. Williams is a worldrenowned leader in stroke disparities and community-based behavioral intervention
research. He is founder and chair of Hip Hop Public Health, an internationally recognized organization that creates and implements multimedia public health interventions that target and engage young people in the health of their families and communities. He is a principal investigator of multiple NIH investigator-initiated awards, including a Center for Stroke Disparities Solutions in New York. An influential clinicianeducator, in addition to teaching courses on clinical practice and neuroscience to VP&S medical students Williams is actively engaged in addressing health care disparities and promoting greater diversity and inclusion in academic medicine.

BYTE-SIZED
Videos on a variety of topics in neurology Free with membership at AAN.com/NeuroBytes MEMBERSHIP
LEARNING
Williams
Recipients of IDEAS Grants and Award Announced

Five AAN members have been recognized for their efforts in championing the goals of IDEAS in their academic institutions or communities. Learn more about the individual grants and award at AAN.com/tools-resources/diversity-officers
AAN IDEAS Innovator Grant
These grant funds support projects, events, and activities that foster IDEAS within academic neurology departments or the communities they serve. They are designed for those with new, untested, and innovative approaches to fostering IDEAS with little or no prior experience in implementing IDEAS-related projects.

2022 winners are Em Harrington, MD, PhD, of The Ohio State University, for the project “Developing sexual and gender minority educational resources for neurology”; and Mihir Kakara, MD, of the University of Pennsylvania, for the project “Addressing gaps in disability inclusion.”

The recipients each receive a $2,000 prize, recognition by the AAN, and the opportunity to present their project virtually to the Diversity Officers Subcommittee.
AAN IDEAS Project Grant
These grant funds support projects, events, and activities that foster IDEAS within academic neurology departments or the communities they serve. They are designed for those who have experience and are already working in the IDEAS space within their academic neurology departments.
2022 winners are Pamela McDonnell, MD, of The Children’s

Hospital of Philadelphia for the project “Helping Spanishspeaking families activate their electronic patient portal”; and Aileen Antonio, MD, of Hauenstein Neurosciences, Trinity Health Saint Mary’s, for the project “Sleep apnea education for the Asian American minority communities in West Michigan.”
The recipients each receive a $2,000 prize, recognition by the AAN, and the opportunity to present their project virtually to the Diversity Officers Subcommittee.
IDEAS Changemaker Award
This award is for an AAN member who has made a meaningful contribution within their academic institution by increasing diversity, equity, and inclusion efforts within the neurology department.

2022 winner Roy H. Hamilton, MD, MS, FAAN, FANA, receives a $1,000 prize and complimentary registration to the 2023 Annual Meeting to make a 30-minute presentation highlighting work being done.

A ANnews • March 2023 23
Follow and subscribe to our new podcast! BrainandLife.org/Podcast
Hamilton
Kakara McDonnell
Antonio
Harrington





MEMBERSHIP Self-advocacy, Positivity Guides Leadership Graduate to New Heights
Not only was Christine Doss Esper, MD, recently promoted to associate professor of neurology, Emory University School of Medicine, Division of Movement Disorders, in Atlanta, GA, but in 2022, she was elected chair of the AAN’s Women’s Issues in Neurology Section and chair of the International Parkinson and Movement Disorder Society Telemedicine Study Group. She is quick to attribute these impressive career successes, at least in part, to skills—and confidence—she gained through her experience in the AAN’s Women Leading in Neurology (WLN) program.

“I am a different person today because of the WLN program, and it gave me an essential set of skills to grow further professionally and personally,” explained Esper. During one of her first WLN sessions, her coach, Joanne Smikle, PhD, emphasized the applications of self-leadership, and her discussion on self-advocacy and self-promotion really spoke to Esper. “It is important to own your journey, understand the value that you bring, and thoughtfully advance your brand,” she said. “This can be particularly challenging for women in academic medicine, and likely results in many lost opportunities. It is very easy to get stuck in the mundane dayto-day activities of research, patient care, charting, etc., but we need to change our perspective and assess our overall intention with our professional life. I learned how to reframe the factors necessary for professional success, which allowed me to decide how to apportion my time towards pursuits that promote growth and team development while simultaneously creating new opportunities that benefit our patients and our people.”
Another pillar of self-leadership that the program taught Esper is how to actively reject pessimism. “Medicine is increasingly challenging as physician burnout mounts and the workforce crisis grows,” she said. “However, it is essential to minimize wasting time and energy on the negatives, what ifs, and blaming others. We learned to believe in ourselves and be the change that we want to see in the world. Others gravitate towards positivity, and many will join and follow progressive, confident, and optimistic leaders in their journeys.”
WLN also creates a unique and powerful opportunity for its participants to network—"an action that cannot be overemphasized,” according to Esper. “While judicious selection of tasks, projects, and endeavors is critical, I have learned that being open, outgoing, engaging, and helpful will beget more
high-value opportunities,” she said. “As you engage in these new endeavors, you meet new colleagues, make new friends, and generate productive outcomes. What initially was ‘work’ is less burdensome and is much more enjoyable with camaraderie.”
Esper is equally grateful for her WLN mentor, Cynthia Comella, MD, FAAN. “She is a beacon for women in neurology and a true trailblazer in the field of movement disorders. Her guidance this past year has been priceless, and I would love to pay this forward to other female neurologists.” Esper’s recent election as chair to the AAN Women’s Issues in Neurology Section puts her in a unique position to tackle some of these challenges, “and Regina Troxell, MD, vice chair of the section, and I are establishing working groups to tackle many of these issues."
Added Esper, “I cannot thank the AAN enough for this opportunity!”
The empowering and inspirational Women Leading in Neurology program is designed to help mid-career participants tackle gender disparities head-on, create a peer network with other women AAN members, and advance to the top levels of leadership in their fields and within the Academy.
Learn more about AAN Leadership Development Programs at AAN.com/Lead
The 2022-2023 Women Leading in Neurology program is supported in part by AbbVie; Alexion, AstraZeneca Rare Disease; Alnylam; argenx; Bristol Myers Squibb; Harmony Biosciences; Impel Pharmaceuticals Inc.; MERZ Therapeutics; and Supernus Pharmaceuticals, Inc.
AANe-news. Because Your Time Is Valuable.
Sent to your email address the second and fourth Wednesday of each month, AANe-news™ delivers the latest top headlines and resources from the Academy so you can quickly scan and connect directly with the information you need to know.
Another members-only solution from your AAN.

A ANnews • March 2023 25
Esper
75 Years of Leadership of the American Academy of Neurology
The AAN has been fortunate to have been led by these individuals who built upon the work of their predecessors to grow our organization into one that seeks to be indispensable to its 38,000 members by promoting the highest quality patient-centered neurologic care and enhancing member career satisfaction.
AAN Presidents
1948–1951
A.B. Baker, MD, FAAN
1963–1965
Joseph M. Foley, MD, FAAN
1951–1953
Pearce Bailey, MD, FAAN
1965–1967
Charles A. Kane, MD, FAAN


1953–1955
Howard D. Fabing, MD, FAAN
1955–1957
Walter O. Klingman, MD, FAAN




1967–1969
Richard P. Schmidt, MD, FAAN
1969–1971
Sidney Carter, MD, FAAN
1957–1959
Francis M. Forster, MD, FAAN


1971–1973
Joe R. Brown, MD, FAAN
1959–1961
Augustus S. Rose, MD, FAAN

1961–1963
Adolph L. Sahs, MD, FAAN








1973–1975
Gilbert H. Glaser, MD, FAAN




1975–1977
Robert A. Fishman, MD, FAAN
1977–1979
Robert J. Joynt, MD, FAAN
1979–1981
Dewey K. Ziegler, MD, FAAN
1981–1983
Maynard M. Cohen, MD, FAAN
1983–1985
Nelson G. Richards, MD, FAAN
1985–1987
Melvin Greer, MD, FAAN
1987–1989
Theodore L. Munsat, MD, FAAN
1989–1991
Lewis P. Rowland, MD, FAAN
26 A ANnews • March 2023 MEMBERSHIP
1991–1993
Roger N. Rosenberg, MD, FAAN






1993–1995
Jack P. Whisnant, MD, FAAN
1995–1997
Kenneth M. Viste, Jr., MD, FAAN
1997–1999
Steven P. Ringel, MD, FAAN
2003–2005
Sandra F. Olson, MD, FAAN

2015–2017
Terrence L. Cascino, MD, FAAN
2005–2007
Thomas R. Swift, MD, FAAN



2007–2009
Stephen M. Sergay, MB BCh, FAAN
2009–2011
Robert C. Griggs, MD, FAAN
1999–2001
Francis I. Kittredge, Jr., MD, FAAN
2011–2013
Bruce Sigsbee, MD, FAAN
2001–2003
Stanley Fahn, MD, FAAN
AAN Executive Leadership
1951–1960
Doris McKinley, Executive Administrator
1960–1964
Thomas D. Swedien, Executive Administrator
2013–2015
Thomas A. Pedley, MD, FAAN

2017–2019
Ralph L. Sacco, MD, MS, FAHA, FAAN

2019–2021
James C. Stevens, MD, FAAN
2021–2023
Orly Avitzur, MD, MBA, FAAN

1964–1983
Stanley Nelson, CPA Executive Secretary (1964–1966), Executive Director (1966–1983)





1983–1998
Jan W. Kolehmainen, Executive Director
1999–2020
Catherine M. Rydell, CAE, Executive Director and Chief Executive Officer
2020–present
Mary E. Post, MBA, CAE Chief Executive Officer


A ANnews • March 2023 27
DO YOU THINK OCCASIONAL SEIZURES ARE ACCEPTABLE? WHAT WOULD YOUR PATIENTS SAY?











































































































ONCE-DAILY XCOPRI® (cenobamate tablets) CV is indicated for the treatment of partial-onset seizures in adult patients.1
IMPORTANT SAFETY INFORMATION and INDICATION for XCOPRI® (cenobamate tablets) CV

CONTRAINDICATIONS

























































































































































































































































































XCOPRI is contraindicated in any patients with known hypersensitivity to the compound or any of the components of the drug product.



XCOPRI is contraindicated in patients with Familial Short QT syndrome.

WARNINGS AND PRECAUTIONS



Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS): Also known as Multiorgan hypersensitivity, has been reported in patients taking antiepileptic drugs, including XCOPRI. DRESS has been reported, including one fatality, when XCOPRI is titrated rapidly (weekly or faster titration). No cases of DRESS were reported in an open-label safety study of 1339 partial-onset seizure patients when XCOPRI was initiated at 12.5 mg/day and titrated every two weeks. This finding does not establish that the risk of DRESS is prevented by a slower titration; however, XCOPRI should be initiated at 12.5 mg once daily and titrated every two weeks. DRESS typically, although not exclusively, presents with fever, rash, and/or lymphadenopathy, in association with other organ system involvement. Eosinophilia is often present. If such signs or symptoms are present, the patient should be evaluated immediately. XCOPRI should be discontinued immediately and not restarted if an alternative etiology for the signs or symptoms cannot be established.
QT Shortening: XCOPRI can cause shortening of the QT interval. Caution should be used when administering XCOPRI and other drugs that shorten the QT interval as there may be a synergistic effect on the QT interval that would increase the QT shortening risk.
Suicidal Behavior and Ideation: Antiepileptic drugs (AEDs), including XCOPRI, increase the risk of suicidal thoughts or behavior in patients taking these drugs for any indication. Patients treated with any AED for any indication should be monitored for the emergence or worsening of depression, suicidal thoughts or behavior, and/ or any unusual changes in mood or behavior. Advise patients, their caregivers, and/or families to be alert for these behavioral changes and report them immediately to a healthcare provider.
Neurological Adverse Reactions: XCOPRI causes dose-dependent increases in the neurologic adverse reactions including, dizziness, diplopia, disturbance in gait and coordination, somnolence, and fatigue.

Prescribers should advise patients against engaging in hazardous activities requiring mental alertness, such as operating motor vehicles or dangerous machinery, until the effect of XCOPRI is known.
Withdrawal of AEDs: As with all antiepileptic drugs, XCOPRI should generally be withdrawn gradually because of the risk of increased seizure frequency and status epilepticus. But if withdrawal is needed because of a serious adverse event, rapid discontinuation can be considered.

—Chrissy, real XCOPRI patient
Individual results may vary. Watch her story
"I'm not giving in, I’m striving for ZERO seizures."
REFERENCES: 1. XCOPRI [package insert]. Paramus, NJ: SK Life Science, Inc. 2. Krauss GL, Klein P, Brandt C, et al. Safety and efficacy of adjunctive cenobamate (YKP3089) in patients with uncontrolled focal seizures: a multicentre, double-blind, randomised, placebo-controlled, dose-response trial. Lancet Neurol. 2020;19(1):38-48.
In 2 clinical studies of patients taking XCOPRI:
Up to 55% reduction in 28-day seizure frequency1
The primary outcome:
Median percentage reduction in 28-day seizure frequency (double-blind period).
55% XCOPRI 400 mg/day (n=111; P<0.001)*
55% XCOPRI 200 mg/day (n=109; P<0.001)*
*Statistically significant compared with placebo.
36% XCOPRI 100 mg/day (n=108; P=0.006)*
24% placebo (n=106)
During the maintenance phase of a clinical study:

As many as 1 in 5 patients experienced ZERO seizures with XCOPRI1,2
Prospectively defined, secondary outcome:

Percentage of patients achieving 100% seizure reduction during the 12-week maintenance phase (Study 2).
The most common adverse reactions in patients receiving XCOPRI (≥10% for XCOPRI and more frequently than placebo) include somnolence, dizziness, fatigue, diplopia, and headache.1
Discover the possibility of ZERO seizures at XCOPRIHCP.COM
MOST COMMON ADVERSE REACTIONS
In adult adjunctive therapy placebo-controlled clinical studies, the most common adverse reactions that occurred in XCOPRI treated patients (incidence at least 10% and greater than placebo) were somnolence, dizziness, fatigue, diplopia, headache.
DOSING CONSIDERATIONS
Dosage adjustment of XCOPRI or other concomitant medications may be necessary.
• Consider gradually reducing phenytoin dosages by up to 50% during initial titration.
• Consider reducing dosages of phenobarbital and clobazam as needed when used concomitantly with XCOPRI. When XCOPRI and carbamazepine or lamotrigine are taken concomitantly, consider increasing dosages as needed of carbamazepine or lamotrigine.
• Consider increasing dosages as needed of drugs which are CYP2B6 and CYP3A substrates and decreasing dosages as needed of drugs which are CYP2C19 substrates.
• Effectiveness of hormonal oral contraceptives may be reduced when administered concomitantly with XCOPRI. Women should use additional or alternative non-hormonal birth control.

Dosage reduction of XCOPRI may be considered in patients with mild to moderate and severe renal impairment. XCOPRI use is not recommended in end-stage renal disease.
The maximum recommended daily dose is 200 mg for patients with mild or moderate hepatic impairment. XCOPRI use is not recommended in patients with severe hepatic impairment.
DRUG ABUSE
XCOPRI is a Schedule V controlled substance.
INDICATION

XCOPRI is indicated for the treatment of partial-onset seizures in adult patients.



STUDY DESIGNS1:
The efficacy of XCOPRI as adjunctive therapy in partial-onset seizures was established in 2 multicenter, randomized, doubleblind, placebo-controlled studies in adult patients (Study 1 and Study 2). Patients had partial-onset seizures with or without secondary generalization and were not adequately controlled with 1 to 3 concomitant antiseizure medictations. Study 1 (N=221) compared XCOPRI 200 mg/day with placebo. Study 2 (N=434) compared XCOPRI 100 mg/day, 200 mg/day, and 400 mg/day with placebo. The double-blind treatment period consisted of a titration phase (6 weeks) and a maintenance phase (6 weeks for Study 1 and 12 weeks for Study 2). In both studies, patients were started on a higher starting dosage and/or faster titration than the Prescribing Information recommendation. The primary outcome was median percentage reduction in 28-day seizure frequency during the double-blind treatment period.
© 2022 SK Life Science, Inc., a subsidiary of SK Biopharmaceuticals Co., Ltd. PM-US-XCOP-0680 03/22
P lease see Brief Summary of full Prescribing Information on the following pages.
BRIEF SUMMARY OF FULL PRESCRIBING INFORMATION INDICATION AND USAGE
XCOPRI is indicated for the treatment of partial-onset seizures in adult patients.
CONTRAINDICATIONS
XCOPRI is contraindicated in patients with:
• Hypersensitivity to cenobamate or any of the inactive ingredients in XCOPRI
• Familial Short QT syndrome
WARNINGS AND PRECAUTIONS
Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS)/ Multiorgan Hypersensitivity
Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS), also known as multiorgan hypersensitivity, has been reported in patients taking XCOPRI. DRESS has occurred, including one fatality, when XCOPRI was titrated rapidly (weekly or faster titration). No cases of DRESS were reported in an open-label safety study of 1339 partial-onset seizure patients when XCOPRI was initiated at 12.5 mg once daily and titrated every two weeks. This finding does not establish that the risk of DRESS is prevented by a slower titration; however, XCOPRI should be initiated at 12.5 mg once daily and titrated every two weeks. DRESS typically, although not exclusively, presents with fever, rash, lymphadenopathy, and/or facial swelling, in association with other organ system involvement, such as hepatitis, nephritis, hematological abnormalities, myocarditis, or myositis sometimes resembling an acute viral infection. Eosinophilia is often present. This disorder is variable in its expression, and other organ systems not noted here may be involved. It is important to note that early manifestations of hypersensitivity, such as fever or lymphadenopathy, may be present even though rash is not evident. If such signs or symptoms are present, the patient should be evaluated immediately. XCOPRI should be discontinued immediately and not restarted if an alternative etiology for the signs or symptoms cannot be established
QT Shortening
In a placebo-controlled study of the QT interval, a higher percentage of subjects who took XCOPRI (31% at 200 mg and 66% at 500 mg) had a QT shortening of greater than 20 msec compared to placebo (6-17%). Reductions of the QTc interval below 300 msec were not observed. Familial Short QT syndrome is associated with an increased risk of sudden death and ventricular arrhythmias, particularly ventricular fibrillation. Such events in this syndrome are believed to occur primarily when the corrected QT interval falls below 300 msec. Nonclinical data also indicate that QT shortening is associated with ventricular fibrillation. Patients with Familial Short QT syndrome should not be treated with XCOPRI Caution should be used when administering XCOPRI and other drugs that shorten the QT interval as there may be a synergistic effect on the QT interval that would increase the QT shortening risk.
Suicidal Behavior and Ideation
Antiepileptic drugs (AEDs), including XCOPRI, increase the risk of suicidal thoughts or behavior in patients taking these drugs for any indication. Patients treated with any AED for any indication should be monitored for the emergence or worsening of depression, suicidal thoughts or behavior, and/or any unusual changes in mood or behavior.
Pooled analyses of 199 placebo-controlled clinical trials (mono- and adjunctive therapy) of 11 different AEDs showed that patients randomized to one of the AEDs had approximately twice the risk (adjusted Relative Risk 1.8, 95% CI:1.2, 2.7) of suicidal thinking or behavior compared to patients randomized to placebo. In these trials, which had a median treatment duration of 12 weeks, the estimated incidence rate of suicidal behavior or ideation among 27,863 AED-treated patients was 0.43%, compared to 0.24% among 16,029 placebotreated patients, representing an increase of approximately one case of suicidal thinking or behavior for every 530 patients treated. There were four suicides in drug-treated patients in the trials and none in placebo-treated patients, but the number is too small to allow any conclusion about drug effect on suicide.
The increased risk of suicidal thoughts or behavior with AEDs was observed as early as one week after starting drug treatment with AEDs and persisted for the duration of treatment assessed. Because most trials included in the analysis did not extend beyond 24 weeks, the risk of suicidal thoughts or behavior beyond 24 weeks could not be assessed.
The risk of suicidal thoughts or behavior was generally consistent among drugs in the data analyzed. The finding of increased risk with AEDs of varying mechanisms of action and across a range of indications suggests that the risk applies to all AEDs used for any indication. The risk did not vary substantially by age (5-100 years) in the clinical trials analyzed.
Table 1 shows absolute and relative risk by indication for all evaluated AEDs.
Table 1: Risk of Suicidal Thoughts or Behaviors by Indication for Antiepileptic Drugs in the Pooled Analysis
Events Per 1000 Patients
The relative risk for suicidal thoughts or behavior was higher in clinical trials in patients with epilepsy than in clinical trials in patients with psychiatric or other conditions, but the absolute risk differences were similar for epilepsy and psychiatric indications. Anyone considering prescribing XCOPRI or any other AED must balance this risk with the risk of untreated illness. Epilepsy and many other illnesses for which AEDs are prescribed are themselves associated with morbidity and mortality and an increased risk of suicidal thoughts and behavior. Should suicidal thoughts and behavior emerge during treatment, the prescriber needs to consider whether the emergence of these symptoms in any given patient may be related to the illness being treated.
Neurological Adverse Reactions
Somnolence and Fatigue
XCOPRI causes dose-dependent increases in somnolence and fatigue-related adverse reactions (somnolence, fatigue, asthenia, malaise, hypersomnia, sedation, and lethargy). In Study 1 and Study 2, 31% of patients randomized to receive XCOPRI at 100 mg/day, 36% of patients randomized to receive XCOPRI at 200 mg/day, and 57% of patients randomized to receive XCOPRI at 400 mg/day reported at least one of these adverse reactions, compared to 19% of patients who received placebo. Somnolence and fatigue-related adverse reactions were serious in 0.4% of XCOPRI-treated patients compared to no patients who received placebo and led to discontinuation in 2% of XCOPRI-treated patients compared to 1% of patients who received placebo.
Dizziness and Disturbance in Gait and Coordination
XCOPRI causes dose-dependent adverse reactions related to dizziness and disturbance in gait and coordination (dizziness, vertigo, balance disorder, ataxia, nystagmus, gait disturbance, and abnormal coordination). In Study 1 and Study 2, 21% of patients randomized to receive XCOPRI at 100 mg/day, 31% of patients randomized to receive XCOPRI at 200 mg/day, and 52% of patients randomized to receive XCOPRI at 400 mg/day reported at least one of these adverse reactions, compared to 18% of patients who received placebo. Dizziness and disturbance in gait and coordination adverse reactions were serious in 2% of XCOPRI-treated patients compared to no patients who received placebo and led to discontinuation in 5% of XCOPRI-treated patients compared to 1% of patients who received placebo.
Cognitive Dysfunction
XCOPRI causes adverse reactions related to cognitive dysfunction related-events (i.e., memory impairment, disturbance in attention, amnesia, confusional state, aphasia, speech disorder, slowness of thought, disorientation, and psychomotor retardation). In Study 1 and Study 2, 6% of patients randomized to receive XCOPRI at 100 mg/day, 6% of patients randomized to receive XCOPRI at 200 mg/day, and 9% of patients randomized to receive XCOPRI at 400 mg/day reported at least one of these adverse reactions, compared to 2% of patients who received placebo. No cognitive dysfunction-related events were serious in XCOPRI-treated patients or in patients who received placebo. Cognitive dysfunction related adverse reactions led to discontinuation in 0.4% of XCOPRI-treated patients compared to no patients who received placebo.
Visual Changes
XCOPRI causes adverse reactions related to visual changes including diplopia, blurred vision, and impaired vision. In Study 1 and Study 2, 9% of patients randomized to receive XCOPRI at 100 mg/day, 9% of patients randomized to receive XCOPRI at 200 mg/day, and 18% of patients randomized to receive XCOPRI at 400 mg/day reported at least one of these adverse reactions, compared to 2% of patients who received placebo. No visual changerelated events were serious in XCOPRI-treated patients or in patients who received placebo. Visual change led to discontinuation in 0.5% of XCOPRI-treated patients compared to no patients who received placebo.
Risk Amelioration
Prescribers should advise patients against engaging in hazardous activities requiring mental alertness, such as operating motor vehicles or dangerous machinery, until the effect of XCOPRI is known. Patients should be carefully observed for signs of central nervous system (CNS) depression, such as somnolence and sedation, when XCOPRI is used with other drugs with sedative properties because of potential additive effects.
Indication Placebo Patients with Events Per 1000 Patients Drug Patients with
Relative Risk: Incidence of
Incidence
Placebo Patients Risk Differences: Additional
Patients Epilepsy 1.0 3.4 3.5 2.4 Psychiatric 5.7 8.5 1.5 2.9 Other 1.0 1.8 1.9 0.9 Total 2.4 4.3 1.8 1.9
Events in Drug Patients/
in
Drug Patients with Events Per 1000
S:6.875" S:9.875" T:7.75"
Withdrawal of Antiepileptic Drugs
As with most antiepileptic drugs, XCOPRI should generally be withdrawn gradually because of the risk of increased seizure frequency and status epilepticus. But if withdrawal is needed because of a serious adverse event, rapid discontinuation can be considered.
ADVERSE REACTIONS Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions and for varying durations, adverse reaction frequencies observed in the clinical trials of a drug cannot be directly compared with frequencies in the clinical trials of another drug and may not reflect the frequencies observed in practice.
In all controlled and uncontrolled trials performed in adult partial-onset seizure patients, XCOPRI was administered as adjunctive therapy to 1944 patients. Of these patients, 1575 were treated for at least 6 months, 710 for at least 12 months, 349 for at least 24 months, and 320 for at least 36 months. A total of 658 patients (442 patients treated with XCOPRI and 216 patients treated with placebo) constituted the safety population in the pooled analysis of placebo-controlled studies in patients with partial-onset seizures (Studies 1 and 2). The adverse reactions presented in Table 2 are based on this safety population; the median length of treatment in these studies was 18 weeks. Of the patients in those studies, approximately 49% were male, 76% were Caucasian, and the mean age was 39 years.
In Study 1 and Study 2, adverse events occurred in 77% of patients treated with XCOPRI and 68% treated with placebo. Table 4 gives the incidence of adverse reactions that occurred in subjects with partial-onset seizures in any XCOPRI treatment group and for which the incidence was greater than placebo during the controlled clinical trials. The most common adverse reactions that occurred in XCOPRI-treated patients (incidence at least 10% and greater than placebo) were somnolence, dizziness, fatigue, diplopia, and headache.
The discontinuation rates because of adverse events were 11%, 9%, and 21% for patients randomized to receive XCOPRI at doses of 100 mg/day, 200 mg/day, and 400 mg/day, respectively, compared to 4% in patients randomized to receive placebo. The adverse reactions most commonly (1% or greater in any XCOPRI treatment group, and greater than placebo) leading to discontinuation, in descending order of frequency, were ataxia, dizziness, somnolence, diplopia, nystagmus, and vertigo.
* Reported as an adverse reaction; see Laboratory Abnormalities for ALT changes from collected laboratory values
Laboratory Abnormalities
Hepatic Transaminases
In Study 2, there was a post-baseline elevation of alanine aminotransferase (ALT) to greater than 3 times the upper limit of normal (ULN) in 1 (0.9%) patient treated with 100 mg XCOPRI, 2 (1.8%) patients treated with 200 mg, and 3 (2.7%) patients treated with 400 mg, compared to no patients who took placebo. The maximum ALT elevation was 7.6 times ULN in patients treated with 400 mg XCOPRI.
Potassium
In clinical studies, there was a post-baseline elevation of potassium values greater than 5 meq/L (upper reference range) in patients treated with XCOPRI. In Study 1, there were 17 (17%) patients treated with XCOPRI 200 mg compared to 8 (7%) patients who took placebo with normal baseline potassium values who had at least one post-baseline maximum value greater than 5 meq/L. In Study 2, there was a dose-related distribution where at least one post-baseline potassium value was greater than 5 meq/L, occurring in
Studies in Patients with Partial-Onset Seizures with XCOPRI Frequency in Any Treatment Arm Greater Than 1% Over Placebo XCOPRI Placebo 100mg200mg400mg Adverse Reaction n = 108 % n= 223 % n=111 % n=216 % Cardiac Disorders Palpitations 0020 Ear and Labyrinth Disorders Vertigo 1161 Eye Disorders Diplopia 67152 Vision Blurred 2240 Gastrointestinal Disorders Nausea 6693 Constipation 2480 Diarrhea 1350 Vomiting 2450 Dry Mouth 1130 Abdominal Pain 2210 Dyspepsia 2200 Infections and Infestations Nasopharyngitis 2453 Pharyngitis 1200 Urinary Tract Infection 2502 Injury, Poisoning and Procedural Complications Head Injury 1020 Investigations Alanine Aminotransferase Increased* 1140 Aspartate Aminotransferase Increased 1130 Weight Decreased 2010 XCOPRI Placebo 100mg200mg400mg Adverse Reaction n = 108 % n= 223 % n=111 % n=216 % Metabolism and Nutrition Disorders Decreased Appetite 3151 Musculoskeletal and Connective Tissue Disorders Back Pain 4253 Musculoskeletal Chest Pain 2100 Nervous System Disorders Somnolence 19223711 Dizziness 18223315 Fatigue 1214247 Headache 1012109 Balance Disorder 3591 Gait Disturbance 1381 Dysarthria 2170 Nystagmus 3760 Ataxia 2362 Aphasia 2140 Asthenia 0131 Dysgeusia 2020 Memory Impairment 2120 Migraine 0020 Sedation 1120 Tremor 0311 Psychiatric Disorders Confusional State 2230 Euphoric Mood 0020 Irritability 1020 Suicidal Ideation 2100 Renal and Urinary Disorders Pollakiuria 0100 Reproductive System and Breast Disorders Dysmenorrhea 1210 Respiratory, Thoracic and Mediastinal Disorders Hiccups 0110 Dyspnea 0300 Skin and Subcutaneous Tissue Disorders Pruritus 2100 Rash Papular 2000
Table 2: Adverse Reactions in Pooled Placebo-Controlled Adjunctive Therapy
159532_Xcopri_Brief Summary_6.875 x 9.75 live area.indd 2 4/21/20 1:06 PM S:6.875" S:9.875" T:7.75" TUZI20CDPR0043_M26_HCP_Jrnl_Ad_Single_Page_BS_FM.indd 2 7/10/20 9:44 AM
Table 2: Adverse Reactions in Pooled Placebo-Controlled Adjunctive Therapy Studies in Patients with Partial-Onset Seizures with XCOPRI Frequency in Any Treatment Arm Greater Than 1% Over Placebo (Cont.)
8.3%, 9.1%, and 10.8% of the patients treated with XCOPRI 100 mg, 200 mg, and 400 mg, respectively, compared to 5.6% of patients who took placebo. Two patients had a maximum potassium value of 5.9 meq/L.
Other Adverse Reactions
Gastrointestinal disorders: There was an incidence of appendicitis in the overall clinical trial safety population of 2.9 cases of appendicitis/1000 patient-years of exposure that is in excess of the expected background rate in the general population.
Adverse Reactions Based on Gender
No significant gender differences were noted in the incidence of adverse reactions.
DRUG INTERACTIONS
Effect of XCOPRI on Other Drugs
Other Antiepileptic Drugs
Lamotrigine and Carbamazepine
XCOPRI decreases plasma concentrations of lamotrigine and carbamazepine. Because of a potential for reduced efficacy of these drugs, increase the dosage of lamotrigine or carbamazepine, as needed, when used concomitantly with XCOPRI.
Phenytoin
XCOPRI increases plasma concentrations of phenytoin. Because of a potential 2-fold increase in phenytoin levels, gradually decrease phenytoin dosage by up to 50% as XCOPRI is being titrated.
Phenobarbital and Desmethylcobazam
XCOPRI increases the plasma concentrations of phenobarbital and desmethylclobazam, the active metabolite of clobazam. Because of a potential for an increase in the risk of adverse reactions from these drugs, consider a reduction in dosage of phenobarbital or clobazam, as clinically appropriate, when used concomitantly with XCOPRI.
CYP450 substrates
CYP2B6 and CYP3A4
XCOPRI decreases plasma concentrations of CYP2B6 substrates and CYP3A substrates. Because of a potential for reduced efficacy of these drugs, increase the dosage of CYP2B6 or CYP3A4 substrates, as needed, when used concomitantly with XCOPRI.
CYP2C19
XCOPRI increases the concentration of CYP2C19 substrates. Because of a potential for an increase in the risk of adverse reactions from these drugs, consider a reduction in dosage of CYP2C19 substrates, as clinically appropriate, when used concomitantly with XCOPRI.
Oral Contraceptives
XCOPRI decreases plasma concentrations of oral contraceptives. Because of the potential for reduced efficacy of oral contraceptives, women should use additional or alternative non-hormonal birth control while taking XCOPRI.
Drugs that Shorten the
QT Interval
XCOPRI can shorten the QT interval; therefore, caution should be used when administering XCOPRI and other drugs that shorten the QT interval.
CNS Depressants and Alcohol
Concomitant use of XCOPRI with other CNS depressants, including alcohol, may increase the risk of neurological adverse reactions, including sedation and somnolence.
USE IN SPECIAL POPULATIONS
Pregnancy
Pregnancy Exposure Registry
There is a pregnancy exposure registry that monitors pregnancy outcomes in women exposed to antiepileptic drugs (AEDs), such as XCOPRI, during pregnancy. Encourage women who are taking XCOPRI during pregnancy to enroll in the North American Antiepileptic Drug (NAAED) Pregnancy Registry by calling the toll-free number 1-888-233-2334 or visiting http://www.aedpregnancyregistry.org/
Ris k Summary
There are no adequate data on the developmental risk associated with the use of XCOPRI in pregnant women.
In animal studies, administration of cenobamate during pregnancy or throughout pregnancy and lactation resulted in adverse effects on development (increased embryofetal mortality, decreased fetal and offspring body weights, neurobehavioral and reproductive impairment in offspring) at clinically relevant drug exposures
In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2-4% and 15-20%, respectively. The background risk of major birth defects and miscarriage for the indicated population is unknown.
Data
Animal Data
Oral administration of cenobamate (0, 10, 30, or 60 mg/kg/day) to pregnant rats during the period of organogenesis resulted in increased embryofetal mortality, reduced fetal body weights, and incomplete fetal skeletal ossification at the highest dose tested, which was associated with maternal toxicity. There was a small increase in visceral malformations at the high dose; however, teratogenic potential could not be fully evaluated because of the high rate of embryofetal deaths, which resulted in an inadequate number of fetuses examined. Maternal plasma exposure (AUC) at the no-effect dose for adverse effects on embryofetal development (30 mg/kg/day) was less than that in humans at the maximum recommended human dose (MRHD) of 400 mg.
Oral administration of cenobamate (0, 4, 12, or 36 mg/kg/day) to pregnant rabbits during the period of organogenesis resulted in increased embryofetal mortality at the highest dose tested, which was associated with maternal toxicity. Maternal plasma exposure at the no-effect dose (12 mg/kg/day) for adverse effects on embryofetal development was less than that in humans at the MRHD.
When cenobamate (0, 11, 22, or 44 mg/kg/day) was orally administered to female rats throughout pregnancy and lactation, neurobehavioral impairment (learning and memory deficit and increased auditory startle response) was observed in the offspring at all doses and decreased preweaning body weight gain and adverse effects on reproductive function (decreased numbers of corpora lutea, implantations, and live fetuses) were seen in the offspring at the high dose. Maternal plasma exposure at the lowest effect dose (11 mg/kg/day) for adverse effects on pre- and postnatal development was less than that in humans at the MRHD.
Lactation Risk Summary
There are no data available on the presence of cenobamate in human milk, the effects on the breastfed infant, or the effects of the drug on milk production.
The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for XCOPRI and any potential adverse effects on the breastfed infant from XCOPRI or from the underlying maternal condition.
Females and Males of Reproductive Potential Contraception
Women of reproductive potential concomitantly using oral contraceptives should use additional or alternative non-hormonal birth control.
Pediatric Use
Safety and effectiveness in pediatric patients have not been established.
Juvenile Animal Toxicity Data
Cenobamate was administered orally to juvenile rats from postnatal day (PND) 7 to 70. To maintain consistent plasma drug exposures, doses were increased during the dosing period, up to 120 and 80 mg/kg/day in males and females, respectively. Adverse effects included mortality, delayed sexual maturation, neurological (decreased grip strength) and neurobehavioral (learning and memory deficits) impairment, decreased sperm count, decreased brain weight, and ocular histopathology. Recovery from these effects was observed following discontinuation of dosing. Overall, a no-effect dose for adverse effects on postnatal development was not identified. At the lowest doses tested, plasma cenobamate exposures (AUC) were less than that in humans at the maximum recommended human dose (MRHD) of 400 mg.
Geriatric Use
Clinical studies of XCOPRI did not include sufficient numbers of patients aged 65 and over to determine the safety and efficacy of XCOPRI in the elderly population. In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.
Renal Impairment
XCOPRI should be used with caution and dosage reduction may be considered in patients with mild to moderate (CLcr 30 to less than 90 mL/min) and severe (CLcr less than 30 mL/min) renal impairment. Use in patients with end-stage renal disease undergoing dialysis is not recommended.
Hepatic Impairment
XCOPRI should be used with caution and in patients with mild to moderate (5-9 points on Child-Pugh assessment; Class A or B) hepatic impairment. In these patients, the maximum recommended dosage is 200 mg once daily and additional dosage reduction may be considered. Use of XCOPRI in patients with severe hepatic impairment is not recommended.
159532_Xcopri_Brief Summary_6.875 x 9.75 live area.indd 3 4/21/20 1:06 PM S:6.875" S:9.875" T:7.75" TUZI20CDPR0043_M26_HCP_Jrnl_Ad_Single_Page_BS_FM.indd 3 7/10/20 9:44 AM
DRUG ABUSE AND DEPENDENCE
Controlled Substance
XCOPRI contains cenobamate and is listed as a Schedule V controlled substance.
Abuse
Abuse is the intentional, non-therapeutic use of a drug, even once, for its desirable psychological or physiological effects. In a human abuse potential study conducted in recreational sedative abusers (n=39), single doses of XCOPRI (200 mg and 400 mg) were compared to placebo. XCOPRI at single doses of 400 mg produced responses on positive subjective measures such as “Drug Liking,” “Overall Drug Liking,” “Take Drug Again,” and “Good Drug Effects” that were statistically greater than the responses produced on these measures by placebo. In this study, euphoric mood occurred at greater extent with XCOPRI (400 mg) (8%) than with placebo (0%). Phase 1 multiple ascending dose studies in healthy subjects showed rates of euphoria and feeling drunk of about 3% and disturbance in attention of about 5% in subjects who received supratherapeutic doses of cenobamate, but these adverse events were absent in the placebo group. In Phase 2 and 3 studies in subjects with epilepsy, euphoric mood, confusional state, and sedation occurred at low rates in subjects who received XCOPRI (0.5-2.5%).
Dependence
Physical dependence is a state that develops as a result of physiological adaptation in response to repeated drug use, manifested by withdrawal signs and symptoms after abrupt discontinuation or a significant dose reduction of a drug. Clinical studies in healthy subjects indicate that XCOPRI may cause physical dependence and lead to a withdrawal syndrome characterized by insomnia, decreased appetite, depressed mood, tremor, and amnesia. XCOPRI should be withdrawn gradually
OVERDOSAGE
There is limited clinical experience with XCOPRI overdose in humans. There is no specific antidote for overdose with XCOPRI. In the event of overdose, standard medical practice for the management of any overdose should be used. An adequate airway, oxygenation and ventilation should be ensured; monitoring of cardiac rate and rhythm and vital signs is recommended. A certified poison control center should be contacted for updated information on the management of overdose with XCOPRI. There are no data on the removal of XCOPRI using dialysis.
PATIENT COUNSELING INFORMATION
See FDA-approved Medication Guide and Patient Counseling Information section is the Full Prescribing Information.
Manufactured for: SK Life Science, Inc.
Paramus, NJ 07652
Phone: 1-866-657-5574
© 2019 SK Life Science, Inc.
XCOPRI® is a registered trademark of SK Life Science, Inc. or its affiliates and protected by U.S. Patent 7,598,279
S:6.875" S:9.875" T:7.75" T:10" TUZI20CDPR0043_M26_HCP_Jrnl_Ad_Single_Page_BS_FM.indd 4 7/10/20 9:44 AM
EDUCATION UCNS Certifies New Diplomates in Autonomic Disorders

The United Council for Neurologic Subspecialties has certified nine new diplomates in the neurologic subspecialty of Autonomic Disorders. Demonstrating their expert knowledge in their subspecialty, these physicians now hold the distinction of being UCNS diplomates after passing the 2022 UCNS Autonomic Disorders Certification Examination. There are now 61 UCNS diplomates who are certified in Autonomic Disorders. The next UCNS Autonomic Disorder Examination will take place in 2024. To see the list of new diplomates, visit “News” at UCNS.org
Applications Now Open for Neurocritical
Care Certification Examination
The application period is now open for the United Council for Neurologic Subspecialties Neurocritical Care certification examination. The application deadline is June 1, 2023, and the five-hour, 200-multiple-choice question examination is scheduled to take place online the week of November 13 through 17, 2023, with virtual live proctoring.
The 2023 examination schedule is:
Application period: March 1–June 1
Extended application deadline ($500 fee applies): June 15
Examination registration period: August 1
Examination week: November 13–17
Visit UCNS.org/NCCcertification for more information on eligibility and to apply.
AMERICAN BRAIN FOUNDATION
April 26 Commitment to Cures Gala to Celebrate Breakthroughs

Join your friends and colleagues at the beautiful new Omni Boston Hotel at the Seaport—conveniently located across the street from the Boston Convention and Exhibition Center—on Wednesday, April 26, at the 2023 AAN Annual Meeting in Boston for Commitment to Cures, the annual gala that galvanizes the neurology community around the crucial need to raise awareness and support for brain research.
The evening of stories, entertainment, and honorees will be emceed by Jim Cramer, migraine advocate and host of CNBC’s “Mad Money.” The event will begin with a cocktail reception at 6:00 p.m. ET followed by a seated dinner and program at

7:00 p.m. ET, that will feature inspiring stories from people living with brain disease and updates on our latest research studies. Musician Peter Frampton will also receive the Ambassador Award for elevating public awareness of inclusion body myositis, and Josep Dalmau, MD, PhD, FAAN, and Vanda Lennon, MD, PhD, will receive the Scientific Breakthrough Award for their groundbreaking research in autoimmune neurology.

The 2022 gala in Seattle was the Foundation’s most successful to date, raising over $874,000 for brain disease research. Over the years, the Commitment to Cures Gala has hosted many special guests, including actor and comedian Seth Rogen and his wife, Lauren Miller Rogen; Sidney Crosby; Emilia Clarke; Khloé Kardashian; Cindy McCain, and others.
Tickets can be purchased when you register for the AAN Annual Meeting or at AmericanBrainFoundation.org/C2C2023 All ticket sales and proceeds go to funding brain research.
34 A ANnews • March 2023
Cramer
Frampton Dalmau Lennon
DATES & DEADLINES
MARCH
March 1
Applications Open: UCNS Neurocritical Care Certification UCNS.org/NCCcertification
March 5–7
Neurology on the Hill AAN.com/NOH
March 13
Happy 75th AAN Anniversary!
March 28
Application Deadline: Palatucci Advocacy Leadership Program AAN.com/PALF
March 30
Advanced Registration/Hotel Deadline: 2023 Annual Meeting AAN.com/AM
APRIL
April 1
Application Deadline: UCNS Neurooncology Certification UCNS.org/NOcertification
April 6
April 22–27
75th AAN Annual Meeting: Boston and Live Online AAN.com/AM
April 22
AAN Business Meeting in Boston AAN.com/AM
MAY
May 1
Application Deadline: UCNS Clinical Neuromuscular Pathology Certification UCNS.org/CNMPcertification
May 3–4
March 14
Neurology Compensation and Productivity Survey Begins AAN.com/Benchmark
NCC: 21 Career Center Ads Ad—Half Page Horizontal> AN Placed in AANnews 8.25 x 5.25 +0.125 bleed, 4C
Registration Opens: AAN Summer Conference AAN.com/SummerConference
April 12
Applications Open: Emerging Leaders, Diversity Leadership, and Practice Leadership Programs AAN.com/Lead

Virtual Career Fair Careers.aan.com
May 18
Neurology Compensation and Productivity Survey Deadline AAN.com/Benchmark
and
From first job to career shift, get access to the latest openings, candidate CVs, and timely resources to seal the deal. Go right to the top at Careers.AAN.com!
Where the Top Jobs
Top Talent Connect!



















© 2022 Reata Pharmaceuticals, Inc. All Rights Reserved. US-NNU-2100006 05/2022 References: 1. Fogel BL, Perlman S. Clinical features and molecular genetics of autosomal recessive cerebellar ataxias. Lancet Neurol. 2007;6(3):245-257. 2. Indelicato E, Nachbauer W, Eigentler A, et al. Onset features and time to diagnosis in Friedreich’s Ataxia. Orphanet J Rare Dis 2020;15(1):198 3. Parkinson MH, Boesch S, Nachbauer W, Mariotti C, Giunti P. Clinical features of Friedreich’s ataxia: classical and atypical phenotypes. J Neurochem. 2013;126(suppl 1):103-117. 4. National Institute of Neurological Disorders and Stroke. Friedreich Ataxia Fact Sheet. Updated November 15, 2021. Accessed March 16, 2022. https://www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Fact-Sheets/Friedreichs-Ataxia-Fact-Sheet. *There may be additional uncommon symptoms. Get helpful resources and the latest FA information at ThinkFA.com.
loss of ambulation and
Falls1 (gait ataxia) Imbalance1 (proprioception loss) Reflex loss1 (areflexia) Sensation loss1 (sensory neuropathy) Tiredness4 (fatigue) falls imbalance re ex loss tiredness sensation loss falls imbalance re ex loss tiredness sensation loss falls imbalance re ex loss tiredness sensation loss falls imbalance re ex loss tiredness sensation loss falls imbalance re ex loss tiredness sensation
FA FIRST when you see any combination of these symptoms*: Initial symptoms of FA can be vague and overlap with other conditions.2,3 However, FA is the most common inherited ataxia. 4 Will you recognize it when you see it?
Because FA is a severe disease that relentlessly progresses to
independence in nearly all patients, identifying these early signs is crucial.3
Think
FACT:
signs of Friedreich’s
Loss of balance is one of the early
Ataxia (FA), but it may not be this obvious.1




























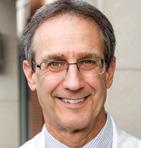
































 Jones
Jones