

CONTENTS






New Zealand hosts the upcoming 54th Edition of the Annual Scientific Meeting
3 From the President
10
22 New Zealand hosts the upcoming 54th Edition of the Annual Scientific Meeting
Poor FDG metabolism - An interesting appearance of unexplainable uptake.
The Utility of 68GaPSMA Expression in Adenoid Cystic Carcinoma of the Head and Neck: A Case Study
Evaluating whether a visual grading score can be applied to the use of Gallium67-Citrate scintigraphy in the assessment of patients suspected of renal allograft pyelonephritis: a single centre retrospective audit.
Utility of Lung V/Q scans on patients with fontan circulation for diagnosing pulmonary emolisms - A Case Study
The efficacy of 18F-FDG PET/CT in the diagnosis and treatment of Erdheimchester disease - A Case Study
Evaluation of effects of bronchoscophic lung volume reduction on differential lobar function using quantitative VQ. Emphysise Study.
Using estimated GFR to determine appropriate plasma sampling time for single-sample GFR measurement.
FROM THE PRESIDENT
Welcome to the 2024 Autumn edition of the Gamma Gazette

As the 54th ASM in Ōtautahi Christchurch is just weeks away, we have taken the opportunity in this edition of the Gamma Gazette to put the spotlight on New Zealand. As the host of this year’s ASM, the Local Organising Committee share some insights about the upcoming event as well as their thoughts on Nuclear Medicine in New Zealand. We have also included some ideas on how to combine your time at the ASM with leisure and tourism!
I would like to thank our contributors to this edition of the Gamma Gazette, we have received an overwhelming number of case studies which we are thrilled to publish and share with our members. I hope this edition will encourage more members to submit articles and case studies for future editions of the Gamma Gazette. The opportunity to publish your work and share your knowledge with the Nuclear Medicine community is one of the many great benefits of being an ANZSNM member.
Lastly, I would like to remind our members to take advantage of the ASM early bird rates and register to attend before 15 March. I will be there and I look forward to catching up with you all in April.
Kia Kaha Kevin London - MANZSNM PresidentOUR CONTRIBUTORS









EDITORIAL COORDINATOR
Rajeev Chandra General Manager PO Box 6178, Vermont South, VIC 3133
T 1300 330 402
F (03) 8677 2970 gm@anzsnm.org.au
marketing@anzsnm.org.au
EVENTS & ADVERTISING ENQUIRIES SUBMISSIONS
secretariat@anzsnm.org.au
DESIGN & PRODUCTION
Enovate Studio www.enovatestudio.com
PUBLISHED IN
Autumn, Winter & Spring/Summer
CONTENT SUBMISSIONS
SCIENTIFIC SUBMISSIONS ON ALL ASPECTS OF NUCLEAR MEDICINE ARE ENCOURAGED AND SHOULD BE FORWARDED TO THE SECRETARIAT (INSTRUCTIONS FOR AUTHORS PUBLISHED AT HTTPS://WWW.ANZSNM.ORG.AU/ACTIVITIES/ GAMMA-GAZETTE-CONTENT-SUBMISSION-ANDGUIDELINES/).
LETTERS TO THE EDITOR OR POINTS OF VIEW FOR DISCUSSION ARE ALSO WELCOME.
IF ORIGINAL OR PUBLIC DOMAIN ARTICLES ARE FOUND AND CONSIDERED TO BE OF GENERAL INTEREST TO THE MEMBERSHIP, THEN THEY SHOULD BE RECOMMENDED TO THE EDITOR WHO MAY SEEK PERMISSION TO REPRINT.
THE ANZSNM GAMMA GAZETTE IS PUBLISHED THREE TIMES A YEAR. DEADLINES FOR EACH ISSUE OF THE JOURNAL CAN BE FOUND ON OUR WEBSITE ANZSNM.ORG.AU
DISCLAIMER
THE VIEWS EXPRESSED IN ANY SIGNED ARTICLE IN THE JOURNAL DO NOT NECESSARILY REPRESENT THOSE OF THE SOCIETY. THE INDIVIDUAL RIGHTS OF ALL AUTHORS ARE ACKNOWLEDGED.
THE AUSTRALIAN AND NEW ZEALAND SOCIETY OF NUCLEAR MEDICINE © 2022 COPYRIGHT IS TRANSFERRED TO THE AUSTRALIAN AND NEW ZEALAND SOCIETY OF NUCLEAR MEDICINE ONCE AN ARTICLE/PAPER HAS BEEN PUBLISHED IN THE ANZSNM GAMMA GAZETTE (EXCEPT WHERE IT IS REPRINTED FROM ANOTHER PUBLICATION)
WWW.ANZSNM.ORG.AU
Jessica Fagan Molecular Imaging & Theranostics Operations Manager - Merci Radiology, NZ Anisa Kumari Nuclear Medicine TechnologistPrincess Alexandra Hospital, QLD Site Leader Molecular Imaging - Mercy Radiology, NZ Pru Burns Unit Charge Nuclear Medicine - Capital and Coast District Health Board, NZ Dr Chong Ghee Chew MBBS FRACP FAANMS Nuclear Medicine Physician Trish Mead Team Leader, Nuclear Medicine Technologist - Auckland DHB, NZ Pippa Bresser Fellow Anatomy and Medical ImagingUniversity of Auckland, NZ Andrew Henderson Radiologist and Nuclear Medicine Specialist - Mercy Radiology, NZ

















































NEW ZEALAND BRANCH UPDATE
A year on from the devastating effects of cyclone Gabrielle, kiwis are enjoying a very welcome hot and dry, sunshine filled summer. Most of us have enjoyed some well-deserved time off and are now back to work in our busy departments.
Congratulations to our newly qualified technologists who completed the University of Auckland Postgraduate Diploma in Health Sciences (Nuclear Medicine) in November 2023:
Louisa Bruwer from Te Toka Tumai Auckland, Jaimee Field from Mercy Radiology, Auckland, Te Puawai Mower from Te Whatu Ora MidCentral District, Palmerston North. Well done to all. We are pleased to be now “growing” our own technologists in New Zealand with a very successful program run by the University of Auckland.
The ANZSNM 54 th Annual Scientific Meeting - Discover the Nucleus is being held in Ōtautahi Christchurch on the 26th-28th April 2024. The LOC are busy preparing what is promised to be an exceptional experience both in terms of an interesting program and a beautiful location. Why not make the most of this time, bring the family and enjoy some time exploring this unique part of New Zealand? If you haven’t yet registered, register now using this link: www. anzsnm2024.com.au
We are looking forward to welcoming you in April. Mā te wā.
Trish Mead - MANZSNM Branch secretary, New Zealand
WESTERN AUSTRALIA BRANCH UPDATE
After a great year with five branch meetings and a few socials, the WA Branch ended 2023 with our AGM on November 14th. SKG Radiology hosted the meeting, kindly sponsored by Siemens.
Preceding the AGM we were fortunate to have Dr Daniel Hubble present his interesting cases on “Hidden Lesions”, Erica Almedia presented “PSMA-An Unusual Finding”, Isabel Barber presented “Deception or Digestion: An investigation into the case of the full stomach”, and lastly we saw “Blinded by the Light: The Spectrum of GCA and PMR” presented by Dr Jamie Bellinge.
We are so thankful for all the volunteers who step up to present at our meetings every year and make the WA branch meetings as educational and interesting as
they are. Our first meeting was held on February 27th, hosted by Sir Charles Gairdner Hospital and sponsored by Siemens. We will also be reigniting the WA Branch Day Seminar this year, to be held in October. Discussions on the theme are already underway. Looking forward to another great year!
Rosemary
Dallen- MANZSNM Branch Secretary, Western Australia
VICTORIA/TASMANIA BRANCH UPDATE
It has been a busy few months in the VIC-TAS Branch. We finished off 2023 with our Annual Day Symposium held on Nov 18th. It was first time we had an in-person Day symposium since 2019 so it was great to see the 30+ technologists that attended. We had a great roster of speakers, some on-site and some who presented from around Australia.
The first morning session focused on the digital PET scanners and how departments are utilising the increased sensitivity and decreased scanning time. We had two speakers from MTIC (Melbourne Theranostic Innovation Centre) in Melbourne talking about the Siemens Quadra (thanks to Johanna Ingbritsen and Hugh Morgan), and then Nelson Salter from Queensland showed the abilities of the GE Omni scanner in his busy clinical department. We then heard two speakers from Tasmania: our committee member Rueben Smith who gave a great overview of Breast cancer imaging and Dr Rob Ware updated us on the new tracers in development from Cyclotek.
Another committee member, Dr Sidney Levy provided an overview of Total Body PET from a clinician/reporting doctor perspective. We finished off the morning session with two research-based talks: Dr Boon Lee presented an overview of Dosimetry of radiopharmaceuticals in clinical research, and then Prof. Paul Donnelly gave a great overview of the possibilities of using Copper-64/Copper-67 as a theranostic pairing.
After lunch we had two Radpharm presentations and one SOPA presentation. Congratulations to Yuwen Jeffries of Peter Mac and Tina Pham who will be representing VICTAS at the ASM in April.
We then had a short social function which allowed us to catch up with colleagues from around the state and

discuss topics that had come up during the day (and the committee members a chance to relax after a job well done!). A special thanks to ours sponsors for the day: MIPS, Siemens, Gamma Gurus and GMS, without whom we would have been unable to run such an event.
We started 2024 with our regular Cardiology Master Class from Dr Kim Williams in mid-January, which was well attended by people from all around Australia and a few from overseas! It was the 23rd year we have been lucky enough to hear from Dr Williams and he gave us an online presentation on “The Future of Nuclear Cardiology”. This gave him a chance to update the audience on the different ways we are now viewing the heart (including myocardial blood flow, amyloid, sarcoid) as well as the new technical innovations such as digital PET scanners and new PET tracers. A lot of these new techniques may be a long way off to most of our audience, but it is always good to hear about the possibilities.
We hope to hold a master class sometime in mid-year and our annual symposium later in the year. If any members have any topics they would like discussed or ideas for speakers we are always happy to hear from you.
Kim Jasper - MANZSNM Branch Chair, Victoria/Tasmania



SOUTH AUSTRALIA/NORTHERN TERRITORY BRANCH UPDATE
The SA/NT branch is excited to start 2024 with meetings for this year already planned and circulated.
We are changing the way in which the branch is run, after successful discussion at the AGM and Quiz Night at the conclusion of 2023. This year will see all meetings conducted online via zoom due to declining attendance of in person events. Additionally, the branch will run two social events with CPD aspects to facilitate increased involvement by members.
The SA/NT branch is extremely active, and I am looking forward to seeing this grow throughout 2024. Our first meeting was held on Tuesday the 5th of March, with


subsequent meetings throughout the following months. Last year’s AGM and Quiz night was held at The Lion Hotel and had one of our largest turnouts to date. I would like to say a large thank you to all members who continuously support the Branch, your dedication does not go unnoticed.
Alessandra Caretti - MANZSNM Branch Chair, South Australia/Northern Territory


Save the
15th Edition
Technologist Special Interest Group
ANNUAL DAY SYMPOSIUM

In collaboration with the Hunter Technologists Group

Oaks Cypress Lakes Resort, NSW



TECHNOLOGIST SPECIAL INTEREST GROUP (TSIG)





Pru Burns, Suzanne McGavin, Erin Hemingway, Emma Brook, and Prof Karen Jones TSIG Oversight Committee
TSIG OVERSIGHT COMMITTEE REPORT
Ihope you have all settled back into work after some much-deserved rest, relaxation and family time over the summer holidays.
Much of my focus right now is as Co-convenor of the 54th Annual Scientific Meeting coming up in 11 weeks! Abstracts have now closed, and we are very impressed with the quality and variety of oral and poster presentations we received from NMTs. Curium and Student Award entrants have been selected, and we are very excited to almost have the program in place. We are very proud to have included in our program two SNMMI standouts – current SNMMI Technologist Section President Dmitry Beyder, who hails from Saint Louis, and from Boston, David Gilmore, SNMMITS Director-At-Large.
As part of the ASM, we are pleased to be able to offer to our NMTs a free workshop focusing on Ultrasound guided vascular access. This technique is becoming more common throughout our departments, often undertaken by other professionals. NMTs are extremely experienced at vascular access, so the ability to add the use of point of care Ultrasound (or POCUS) into our practice is a natural step. There are still a couple of spots available, so please reach out to the ANZNSM Secretariat today if you are interested.
Our CPD&E committee hosted a webinar for International Women’s Day in collaboration with Women in Nuclear (WiN), on Wednesday 6th March, from 6pm - 7pm AEDT. This is a popular TSIG webinar, now a regular event in our calendar.
The TSIG Annual Day Symposium will be held on Saturday the 3 rd of August 2024, at the Oakes Cypress Lakes Resort, Hunter Valley, NSW. We are pleased to be able
to collaborate with the Hunter Technologists Group and provide a day symposium that allows NMT’s a closer-tohome in-person continuing education event. It's all about the networking – so make sure your plans include staying the night!
The WFA committee met on the 26th of February. Prioritisation of outcomes from the ANZSNM Workforce Symposium in 2023 continue to be our focus, with several initiatives being worked through. The WFA meet regularly with the MRPBA, and will be having discussions in person during the ASM. In March we will meet with the Australian Commission of Safety and Quality in Health Care to discuss the progress on the revision of the National Safety and Quality Medical Imaging (NSQMI) Standards.
I have a thank you, to NMT Helen Kyprianou, NMT extraordinaire from Melbourne. Helen joined the CPD&E committee with a keen focus on sharing her enthusiasm of our profession with the next generation of technologists. She invested her time completing the “Train the Trainer” course associated with the Teaching on the Run program and Helen was instrumental in taking the concept of the TSIG initiative Student Representative Council and making it a success. I wish Helen all the very best on her next adventure, and I thank her again for the positive contributions she made to the TSIG.
The TSIG AGM will be held online Tuesday 26 March 2024, please watch out for the registration details coming soon.
Looking forward to welcoming you all in April to Ōtautahi Christchurch.
Pru Burns Chair TSIG
CONTINUING PROFESSIONAL DEVELOPMENT AND EDUCATION (CPD&E) REPORT
The TSIG CPD&E Committee has some fresh faces to introduce to the Nuclear Medicine community!
Firstly, I would like to thank our outgoing members Karen Jones, Maddison Barden, Patrick Doggett and Helen Kyprianou for all the hard work and dedication they have provided while serving on this committee. Many successful webinars, symposiums and projects such as the Student Representative Council are thanks to your contributions. An Expression of Interest to join the committee was advertised in July last year which was met with an overwhelming response. Please meet our successful applicants and newest members below!
Erin Hemingway CPD&E Chair
KYM BARRY
NUCLEAR MEDICINE LECTURERKym Barry is a Nuclear Medicine lecturer at Charles Sturt University on the Port Macquarie campus. Since commencing at the university in 2016, Kym has taught students from all years and disciplines across the medical radiation sciences program, with one of her core roles being clinical coordination for nuclear medicine students.
Kym is currently a PhD candidate and has over 17 years clinical experience in nuclear medicine in a variety of settings, including large and rural public hospitals, and private practices.

ELLIE KELLIHER
NUCLEAR MEDICINE TECHNOLOGISTI graduated from the University of Newcastle in 2016, eager to apply my expertise and passion for Nuclear Medicine. My career journey has spanned diverse Queensland locations, including Mackay, Townsville, and Cairns, ultimately leading me to make Townsville my home. In 2020, I embraced a new chapter at The Royal North Shore Hospital in NSW, where I continue to expand my skills alongside cutting-edge technology. This challenging and rewarding environment fuels my passion for the field. Driven to make broader contributions, I joined TSIG to connect with like-minded professionals and work towards advancements in Nuclear Medicine. I believe in the power of collaboration to improve patient outcomes and shape the future of our industry.

SHIKHA SHARMA
NUCLEAR MEDICINE TECHNOLOGISTI started my career in Nuclear Medicine at St Vincent’s Public Hospital, Sydney in 2015 as a PDY. I enjoyed working with the team so much that I am still working at the same place! Over the last five years, I have had a chance to help make workflow changes, implement new protocols, and introduce a second PET scanner.
I also had the opportunity to complete a Master’s degree in Health Administration. I have recently accepted the Research Coordinator role in the department. I am interested in research, especially emerging theranostics agents, staff advocacy and continuing education for NMS and students in the field of Nuclear Medicine.
I hope that joining the TSIG CPD&E committee will allow me to meet like-minded Nuclear Medicine Scientists and will give me an opportunity to explore ways to help, promote and progress this field further.

ELAINE TIJA
NUCLEAR MEDICINE TECHNOLOGIST
My is Elaine Tjia and I am a Nuclear Medicine Technologist. I graduated from the University of South Australia and have close to five years of experience working at Sir Charles Gairdner hospital in Perth, Western Australia.
With the aim to provide the utmost best care to all patients, my goal is to improve my own, as well as my fellow TSIG members’ knowledge and therefore skill sets.
Through TSIG I will try my best to work towards providing the most up to date knowledge and opportunities to all its' members.
CONTINUING PROFESSIONAL DEVELOPMENT AND EDUCATION (CPD&E) REPORT
 STEPHANIE SCHULZ NUCLEAR MEDICINE TECHNOLOGIST
STEPHANIE SCHULZ NUCLEAR MEDICINE TECHNOLOGIST
I graduated from the University of South Australia in 2002, and started my Nuclear Medicine career as a PDY at the Royal Hobart Hospital. I served as the Tasmanian representative for the VIC/TAS ANZSNM Branch during my time there. I set off overseas in 2008 and worked in several large public Nuclear Medicine Departments in the UK. The knowledge and experience I gained during my time overseas has been invaluable to my future endeavours.
I returned to Australia in 2011 and worked in several private practices before settling on the Gold Coast and I have been working as a Senior Nuclear Medicine Technologist at the Gold Coast University Hospital since 2014. I have a keen interest in research and am currently involved with several large clinical trials. My goal is to enable research opportunities to be accessible to all staff, thereby promoting professional development and education within our exciting field of medicine.
STUDENT REPRESENTATIVE COUNCIL SRC REPORT
The beginning of the university year is an exciting time, as a new group of first year students commence the Nuclear Medicine program. The ANZSNM was proudly represented at university O-weeks by TSIG and SRC members. This was a great opportunity to educate students about the ANZSNM and the benefits of becoming a member. It was fantastic to meet new students and see the growing interest in Nuclear Medicine.
In planning for the year ahead, the SRC are looking forward to welcoming new members into the committee. We hope to continue to grow the committee with members across all universities and year levels, and further develop
UNIVERSITY LIAISON REPORT
Welcome to 2024. I am very honoured again to be the university liaison representative for the ANZSNM Technologist Special Interest Group (TSIG) this year. In this Gamma Gazette, I am fortunate enough to have been able to collaborate with all our universities across Australia and New Zealand to let our members know what is happening.
2024 brings some interesting news and updates about the universities, their courses and their students. One thing that came out of the 2023 Workforce Summit was working collaboratively, and the ANZSNM is looking to further this with new initiatives and collaborations in 2024 to assist with a dynamic and sustainable industry.
the roles within the group. Our key goals are to develop and present a webinar later in the year, as well as work towards increasing our online, social media and ‘on campus’ presence. Through these activities we aim to better connect with fellow students and professionals –we would love to hear about your experiences!
Jess Watson Student Representative Committee ChairThe ANZSNM TSIG is working diligently behind the scenes to represent our members and to help strengthen our Nuclear Medicine Community. Please reach out if you wish to get involved, have any news yourself or have any questions about our initiatives. As I write this, we have Expressions of interest open for the mentorship program as well as on the Student Representative council (SRC) which closes on the 17th of March. Please get in quick as we would love to have you join us.
See the website here or reach out to the secretariat or via email at tsigchair@anzsnm.org.au for further information.
Emma Brook ANZSNM TSIG University LiaisonUNIVERSITY LIAISON REPORT (Continued)

Charles Sturt University (CSU) held first year orientations for Nuclear Medicine on the 21st of Feb, with strong numbers across both campuses and interest from students in a career in Nuclear Medicine. Early numbers suggest a diverse enrolment from students around Australia, which we hope will translate to students completing placements across the country and hopefully graduates employed nationwide. Graduation ceremonies for last year's graduates are fast approaching and we wish them good luck with their new careers.
Kym Barry Lecturer Medical Radiation Science – Nuclear Medicine
The University of Newcastle (UON) graduated 27 Nuclear Medicine Scientists in December 2023. (See photo below) All graduates are now employed in Nuclear Medicine Departments across Australia.
Current enrolments in the nuclear medicine program for 2024 are: Year 1 = 65, Year 2 = 37, Year 3 = 23, Year 4 = 29. We will be organising Clinical Supervisor meetings throughout the year to discuss placement issues and assessment of clinical performance.
Our Year 4 students are on placement in Feb/March followed by the Year 3 students in March/April. Thank you to all the clinical supervisors and staff who host and support our students during their placement experiences.
Daphne James Associate Professor
EXPRESSiON OF iNTEREST
join the Student Representative Council
Are you an ANZSNM Student Member?

SCAN ME
The Australian and New Zealand Society of Nuclear Medicine (ANZSNM) Technologist Special Interest Group (TSIG) Student Representative Council (SRC) consists of two representatives from each university in Australia and New Zealand. Its aim is to engage with students who represent the next generation of technologists.
The SRC meets online 3-4 times a year, with members of the TSIG CPD & Education Commi ee and Workforce Advocacy Commi ee. As a student representative, you will increase the student voice within the ANZSNM, build professional relationships, help promote the profession to students at events and conferences, and gain experience as a ANZSNM commi ee member. Student representatives have the opportunity to participate in projects and produce media content relevant to student interests.
Most importantly, you will discover what the ANZSNM can offer and advocate what you would like the ANZSNM to do for the wider student body.
Expressions of interest or enquiries should be emailed to tsigchair@anzsnm.org.au and should include your full name, institution & year level, contact details and a short expression of interest (no more than 250 words) stating the reasons why you would like to be involved. You must be a current student member of the ANZSNM to be considered for these roles. Student membership is renewed annually and free to Nuclear Medicine Students.
Please visit the ANZSNM website to join (ANZSNM student membership).
Closing Date: Sunday 17 March 2023








UNIVERSITY LIAISON REPORT

RMIT University have a new intake of 30 Nuclear Medicine students for 2024. This number is down from 2023 and even though we had a reasonable marketing campaign we're simply not winning the battle against Medical Imaging. We need to get the word out at High School careers days, and we need to hit schools hard inside this year's 2024 National Science Week in early August which we plan to do. We have also just released our first promotional video made for the generation of today. See links below and of course add and share widely.
Instagram: https://www.instagram.com/p/C339TSdx0p7/
Facebook: https://www.facebook.com/reel/832352418654947
LinkedIn: https://www.linkedin.com/feed/update/urn:li:activity:7168429894043942913
TikTok: https://www.tiktok.com/@rmituniversity/video/7340472969187183873
We have 16 students undertaking their final 24 weeks of placement and they will graduate in early July and be ready to start work not long after. In 2nd Year we have 37 students and in 3rd Year we have 14 students.
RMIT had a very successful O-week with our new NM students. They have all been made aware that ANZSNM membership is free for students for the duration of the studying time. I have asked that the QR code be added to all slide decks for the first few weeks. We had My Linh Diep representing the ANZSNM at the O-week booth on Monday which was a great opportunity for students to ask questions.
RMIT attended the Queensland Workforce Summit in person last year - it was enlightening to be in the room and at the same time see the pain the workforce shortage is producing. RMIT University is doing all it can at present to support the industry and we are of course forever grateful for the ongoing support we receive with placements. We are looking at future initiatives to see how we could expand our reach, but it is slow going. We'd love to help out in Western Australia, Queensland and the Northern Territory and with our new Curriculum Architecture going live in 2025 we know we have a robust program to produce graduates that are ready to work. This will all come out in a media release in the months ahead. We are still going through our internal approvals, but we are very close, so please keep an eye out for this.
Mark Scalzo RMIT University

UNIVERSITY LIAISON REPORT

The University of South Australia (UniSA) held first year orientation day for Nuclear Medicine on the 21st of Feb, with the SA Branch, Lecturers and Student Representative council (SRC) working together to promote Nuclear Medicine. Thank you to Alessandro from the SA branch and Jess from the SRC for representing the ANZSNM. It was a great opportunity for students to ask questions about the industry and join the ANZSNM under the free student membership scheme.
UniSA again have had strong demand for their Nuclear Medicine course commencing in 2024. Current enrolments for first year are 40 first years, 22 second years, 13 third years and 15 fourth years. It was great to recently see the fourth years on campus for a pre-clinical workshop. This workshop involved a range of speakers and practicing of clinical skills. The workshop concluded with a mock clinic together with the radiation therapy students which was a great success. During this mock clinic we also successfully integrated use of our GE Infinia workstation – a generous donation from GE. Fourth years are currently on placement with some students receiving scholarships to help facilitate interstate and overseas placement opportunities.
UniSA continues to have strong partnerships with industry with continued involvement of industry professionals who are involved in many aspects of teaching including delivering lectures and workshops, being involved in special events, marking, curriculum advice and supervising students. The high level of industry involvement along with evolving teaching methods keeps our program contemporary. We are looking forward to the year ahead as we continue to prepare our highly motivated students for a career in Nuclear Medicine.
Katherine Guerrero
The University of South Australia


UNIVERSITY LIAISON REPORT (continued)

The University of Auckland offers a Postgraduate Diploma in Health Sciences (PGDipHSc) in Nuclear Medicine, providing a pathway to registration as a nuclear medicine technologist (NMT). Following completion of the programme, graduates are registered as practitioners in the NMT scope of practice with the Medical Radiation Technologists Board (MRTB) and qualified to work as a NMT in New Zealand. The specialisation was designed to meet the registration requirements of the MRTB for the NMT scope of practice and requires students to be concurrently employed in a clinical training position while enrolled in the specialisation to ensure they meet the clinical competencies. To accommodate the fact that many students would be training outside of Auckland, these specialisations were designed to be delivered entirely by remote learning. The programme's flexibility, being tailored towards part-time study, accommodates the diverse needs of students, allowing them to pursue their academic goals while balancing other commitments. This specialisation is the only postgraduate Nuclear Medicine study available in New Zealand leading directly to the registration of NMTs.
A little bit of history – our past
Let me take you back to Edition 34, the Spring/Summer edition of the Gamma Gazette in 2022, where Shelley Park told our story and discussed the evolution of Nuclear Medicine training at the University of Auckland. The first milestone along that journey started as a pathway to qualifying as an NMT being offered since 2014, with a suite of courses leading to registration as an NMT being introduced as part of the PGDipHSc (Medical Imaging) programme. This pathway received accreditation from the MRTB in 2017. However, the named Nuclear Medicine specialisation of the Postgraduate Diploma in Health Sciences (PGDipHSc) was only recently introduced in 2019 with another important milestone in that the named PGDipHSc in Nuclear Medicine specialisation was accredited with the MRTB. Since the last update and overview of the development of the programme, we have continued to see the programme grow and adapt in response to the ever-advancing technology and expansion in the profession.
What’s happening now? Our present
There are currently 12 students at various stages of their training working towards graduating. In 2023, we celebrated six graduates of whom two, Freya Hayden and
Te Puawai Mower received Academic Excellence Awards. These awards have been presented to academically excellent students who have completed their study and achieved the highest grade-point average over their programme.
Considering the brief history of the programme, we are proud to see its growth and refinement with a steady increase in the number of graduates across the programme as illustrated in the figure below.
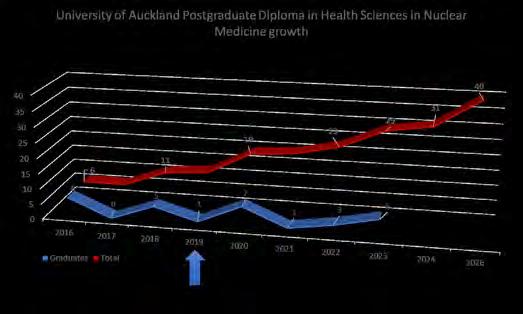
You may notice that the number of graduates fluctuates substantially every year, so it would be important to explain that students can enrol in the programme in any semester due to the flexibility in the offering of the courses within the programme. The PGDipHSc (Nuclear Medicine) programme consists of eight 15-point courses (i.e. students are required to pass courses with a total value of 120 points to be awarded the qualification). More information on the programme and courses offered can be found here
As the programme has grown and developed, we have also seen growth and change in the teaching team in the Department of Anatomy and Medical Imaging. In edition 34, you were introduced to me (Pippa Bresser), joining the University of Auckland teaching team as a full-time Professional Teaching Fellow in 2021. We have since welcomed Clare McKenzie as a part-time Professional Teaching Fellow. Clare is the team lead and clinical coordinator based in Palmerston North, Te Pae Hauora o Ruahine o Tararua | MidCentral and a committee member of the ANZSNM CPD & Education (CPD&E) Committee. We sadly also had to bid farewell to Karen Roeske who worked part time as a Professional Teaching Fellow on the programme. Karen held a pivotal role in the team involved in the development of the PGDipHSc in Nuclear Medicine.
UNIVERSITY LIAISON REPORT (continued)
Her dedication to grow the programme and her commitment to seeing students flourish and succeed in the programme will be missed. I am eternally grateful for her role in helping settle me in. We wish her well as she moves onwards and upwards on another journey in her career.
In 2023, we celebrated some important events in the Department of Anatomy and Medical Imaging which could strengthen our engagement with the ANZSNM and expand our international collaborations:
- One of our PGDipHSc (Nuclear Medicine) students, Shelley Lyford, was welcomed onto the ANZSNM TSIG Student Representative Council (SRC) further extending the reach of the SRC across universities and year levels.
- Some of our other postgraduate programmes celebrated 10 Years! Our first cohort of MRI and ultrasound students started in Semester 1, 2013 so, to celebrate 10 years of delivering postgraduate medical imaging programmes, we had drinks and nibbles on 28th March to catch up with a range of people who have helped shape and grow the programmes. In this time, we have educated 151 MRI technologists, 99 Sonographers, 76 Mammographers and 20 NMTs!
- On 29th November, the new Medical Imaging Research Centre (MIRC) was officially launched in the Faculty of Medical and Health Sciences with goals of collaboration and improving healthcare in the community. The centre will be co-directed by Professor Maurice Curtis, Associate Professor Miriam Scadeng and Dr Beau Pontré, all from the Department of Anatomy and Medical Imaging.
‘The aim is to promote collaboration to engage researchers in a network where they find expertise, and inspiration, and where work they didn't dream could be possible can become possible,’ said Professor Curtis. ‘Ultimately the purpose of the centre is to do better for our communities tomorrow than what we can do today.’
The research centre will offer expertise, equipment and mentoring for researchers at the planning stages of new projects. A working group led by the three co-directors is interested to hear from the community about what they would like to see from the centre and how best to collaborate. If you have any ideas to share, please send them to medicalimaging@auckland.ac.nz



UNIVERSITY LIAISON REPORT (continued)

Where are we going? Our future
Since many of the postgraduate courses offered at the University of Auckland are suitable to be undertaken as a one-off course (Certificate of Proficiency) for registered NMTs, Medical Imaging Technologists (MITs), Sonographers and Radiation Therapists for their continuing professional development (CPD), there is growing interest in some of the PGDipHSc suite of courses on offer. Remember, the courses are designed to be delivered fully online so you could consider doing something on offer from the comfort of your home, office or bed wherever you are in the world.
Aside from ensuring our courses are relevant and updated with the latest innovations in the profession, there are currently two exciting projects being developed in the Nuclear Medicine space. We have been engaging with the local Nuclear Medicine community on these projects in light of the much anticipated growth in the PET-CT sector in Aotearoa | New Zealand. We have been working hard to develop a Postgraduate Certificate in
PET-CT which would be attractive for our MITs and RTs in the realm of hybrid imaging. This would also be an opportunity for NMTs returning to practice or looking to upskill or refresh their knowledge. Finally, we are also revisiting and refining our course offerings in the PGDipHSc (Nuclear Medicine) programme to ensure we remain abreast of the developments and expansion in the Theranostics space. With the rapid growth in this area, it is imperative for our programme to embrace the innovations and evolution of the profession to better serve our patients. We look forward to what the future holds for our programme.
Feel free to reach out to the Medical Imaging team at: medicalimaging@auckland.ac.nz or Nuclear medicine Specialisation lead: Dr Pippa Bresser at pippa.bresser@auckland.ac.nz


hosting the 2024 Annual scientific meeting

Kia ora koutou
hello to you all
Nau mai haere mai Welcome to Ōtautahi Christchurch.



As we are weeks away from welcoming you all to Ōtautahi Christchurch, the autumn edition of the Gamma Gazette gave the local organising committee (LOC) the opportunity to showcase not only a fantastic city, but our locals and the New Zealand Nuclear Medicine community.



Since the last New Zealand Annual Scientific Meeting in Rotorua 2016, Nuclear Medicine, PET/CT and Theranostics have experienced somewhat of a boom across the motu (or perhaps more of an eruption!). With expansion by private Radiology providers across the country, spreading out into more regional sites, this is allowing improved access for our patients more than ever before. The Covid-19 pandemic provided another boost, forcing the New Zealand government at the time to fast track funding and resources to provide a public PRRT service in Auckland, as borders closed to patients needing treatment.
Showing our true can-do attitude, 2024 is the perfect time for New Zealand to host the ANZSNM ASM.
While you are in NZ this trip, we encourage you to try some Te reo Māori ("the Māori language").



Let us start with pronouncing Ōtautahi … try this Oar-toe-ta-he. It rolls o the tongue.
I decided to “interview” our NZ based LOC, and get their views and thoughts on our ASM.
While I look forward to introducing you to our place in the world, here is what the 2024 LOC have to share with you.
Ngā mihi nui!


Pru Burns, Te Whanganui a Tara Wellington













Can you share a personal experience from attending an Annual Scientific Meeting that might inspire our readers to join you in New Zealand this year?
Thanks to Covid I had not had the opportunity to attend an ASM until 2023. Attending the ASM in Adelaide left me inspired to do more and reach further. It was a wonderful opportunity to meet new peers from around Australia and New Zealand, broaden my knowledge and feel like a larger part of the Nuclear Medicine community. We often connect virtually through online platforms, but to come together in person and see such a wide range of individuals all interested and passionate in Nuclear Medicine while wanting to share, spread and grow their knowledge with others was invaluable.
I am looking forward to attending the upcoming ASM in NZ, hearing new techniques, sharing and swapping ideas with others, and reconnecting with colleagues.
Yasmin Rennie Tāmaki Makaurau Auckland

How do you feel this year's theme ‘Discover the Nucleus’ will challenge and provoke the attendees to think about their role within Nuclear Medicine?
Discover the Nucleus to me really asks two questions:
1 . What is at the heart of your practice?
Nuclear Medicine is beautiful because it is a modality that is all about discovery. It constantly challenges us to seek new ways to improve healthcare outcomes for patients. I believe this is the heart of what we do.
2.How does this connect you to the world around you?
Nuclear Medicine would not exist without the connections we make through research and collaboration. It is meetings like the ANZSNM ASM that bring like minds together and provides the space that connects the Nuclear Medicine community both locally and internationally.
Jessica Fagan, Tāmaki Makaurau Auckland

What does it mean to you to host this year’s ASM in Christchurch?
The last Christchurch ANZSNM Conference I can remember was 1988, not long after I started in Nuclear Medicine. That was such a long time ago, we are really excited that it is in our beautiful city once more, like the nucleus, Christchurch’s compact layout means everything is within a short walking distance of our magnificent new conference centre “Te Pae”. The conference theme is all about getting together and learning from each other, all of the Christchurch team are planning to be there, we have a fantastic social program and look forward to meeting our Australian colleagues.
Lynda Murray, Ōtautahi Christchurch

I wish to share two proverbs. They will mean something di erent to each of you, there is no right or wrong interpretation. Embrace them as you catch up with familiar faces, meet new ones and soak in the knowledge around you.
He rangi tā matawhāiti, he rangi tā matawhānui
A person with narrow vision has a restricted horizon; a person with wide vision has plentiful opportunities.
Ko te pae tawhiti, whāia kia tata; ko te pae tata, whakamaua kia tina.
Seek out distant horizons and cherish those you attain.
Karen Roeske, Te Whanganui a Tara Wellington


The New Zealand committee feels the timing of the meeting in New Zealand is opportune for the local nuclear medicine community and their patients. There has been a large, ongoing e ort to maintain access to quality nuclear medicine in New Zealand. The institution of a New Zealand training scheme is one example of the progress made. At the same time, there are daily reminders of the lack of resources and small workforce. At this point, the specialty stands at the crossroads in this country. There are very real concerns for its future. Now, more than ever, members of the Australasian nuclear medicine community need to support a robust, well-sta ed and equipped New Zealand nuclear medicine service. Failure, in the current climate, would have significant implications not only for New Zealand, but also for Australia and the international community.
Andrew Henderson, Tāmaki Makaurau Auckland
Christchurch-City-Canterbuy
As someone deeply involved in both the organisation of the event and the field, what part of the meeting are you most looking forward to?
It is always an awesome feeling to be part of an event with like-minded people who share the same passion for Nuclear Medicine. The meeting is an opportunity to network with friends and peers from throughout NZ and Australia, enabling the sharing and discussion of current practice and upcoming developments in Nuclear Medicine and Theranostics. This interaction can only help me improve or enhance my practice as a technologist.
Trish Mead, Tāmaki Makaurau Auckland


What are your aspirations for the future of nuclear medicine in New Zealand post-ANZSNM 2024?
Considering the exciting developments in nuclear medicine happening in New Zealand both clinically and in the higher education sector, we are going to see massive growth in the profession. We wouldn’t be able to optimise these developments without a full workforce considering the current pressures. The workforce issues are well documented and the ANZSNM is working hard with key stakeholders to address these issues. It would be imperative to grow our Nuclear Medicine training programme to ensure we are feeding the workforce pipeline and we are also working with our clinical partners to refine and enhance our current training programme to keep up to date with the evolving technology and services being o ered across New Zealand. This collaboration and networking will continue to play a pivotal role in seeing the profession grow.
Pippa Bresser, Tāmaki Makaurau Auckland


For attendees traveling to New Zealand, what experiences outside the meeting would you recommend to truly appreciate Christchurch and its surroundings?
Explore the location for the 54th ANZSNM meeting by wandering through the botanic gardens, visiting the iconic cathedral square. There is also plenty of choice, for arts, culture and adventure alike. Explore the Christchurch Art Gallery Te Puna o Waiwhetū and the Canterbury museum, enjoy breathtaking views in a hot air balloon ride, hit the road with a day trip to Hanmer springs or enjoy the culinary delights at the Arts Centre Market and Little High Eatery.
How can attendees of the ANZSNM meeting make the most of their visit to New Zealand in terms of combining professional development with leisure and tourism?
Since you are coming to Christchurch, why not take time out to see the best that the city, and the region, has to o er.
For those who are staying local, the Christchurch Attractions website has a range of activities such as city tram tours, the Christchurch Gondola, or punting on the Avon River. Their website is located at https://www.christchurchattractions.nz/
There is a wide range of dining options in the city. Along the Avon are several restaurants to choose from. Christchurch also has the Riverside Markets, with a number of restaurants on site to tempt you. Check out their website at https://riverside.nz
If you’re planning to take a few extra days to explore further afield, may we suggest checking out:
•Milford Sound
•Tekapo
•Queenstown
•Arthur Pass
•Fox Glacier
•Hamner Spring
•Mount Cook
Andrew Painting, Tāmaki Makaurau Auckland









 David Gilmore, Massachusetts College of Pharmacy and Health Sciences
Dmitry Beyder, SNMMITechnologist Section President
Dr Peter Francis Royal Childrens Hospital
Dr Ben Lawrence Auckland Hospital
Professor Andrew Scott, Department Of Molecular Imaging And Therapy, Austin Health
Helen Nadel, Standford Medicine
David Gilmore, Massachusetts College of Pharmacy and Health Sciences
Dmitry Beyder, SNMMITechnologist Section President
Dr Peter Francis Royal Childrens Hospital
Dr Ben Lawrence Auckland Hospital
Professor Andrew Scott, Department Of Molecular Imaging And Therapy, Austin Health
Helen Nadel, Standford Medicine


Friday




Friday 26th April 2024
08:00 - 12:00
Pre-Conference Symposium
13:30 - 15:30
Opening Plenary
15:30 – 16:00
Afternoon Tea
16:00 - 17:30
Concurrent Sessions
17:30 - 19:30


Venue: Miro Restaurant Christchurch
Sponsored Breakfasts
08:30 - 10:00
Plenary
10:00 - 10:30
Lowenthal Lecture
10:30 - 11:00
Morning Tea
11:00 - 13:45
Concurrent Sessions
13:15 - 14:00
Lunch
14:00-15:30
Closing Plenary




Saturday 27th April 2024
07:00 - 07:30
All for One – Walk / Run
Sponsored Breakfasts
08:30 - 10:00
Plenary
10:00 - 10:30
Pioneer Lecture

Concurrent Sessions
12:30 - 13:30
Lunch
13:30 - 15:30
Poster Session (TBC)
15:30 – 16:00
Afternoon Tea
16:00 - 17:30
Concurrent Sessions
19:00 - 23:00
Awards Dinner
Room: The Rivers Room, Ta Pae
Christchurch Convention Centre



social program
Friday 26
Welcome Reception
5:30 PM - 7:00 PM
Location: Exhibition Hall | Te Pae Convention Centre
The Welcome Reception will be held at the Te Pae Convention Centre on Day 1 of the Meeting. This is a great opportunity to network with other attendees, sponsors and exhibitors!


Friday 26
AANMS Fellow's Dinner
7:00 PM - late
Location: Miro | Christchurch
*This is available to AANMS Fellows and Members only

Saturday 27
Awards Dinner
7:00 PM - 11:00 PM
Location: The Rivers Room | Te Pae Convention Centre
Theme: Studio 54 - Step into the glamorous world of Studio 54 at our awards dinner, where attendees will be transported back to the iconic era of disco and decadence. Immerse yourself in the dazzling disco era with a night of glittering lights, funky beats, and themless style, as we celebrate the spirit of the legendary Studio 54.
Band: Girl from Mars.













what to visit whilst in nz


Exploring New Zealand presents a unique opportunity for attendees of the 2024 Annual Scientific Meeting to immerse themselves in the natural beauty and vibrant culture of this captivating destination. Beyond the event, Christchurch and its environs o er a diverse array of experiences for those eager to delve deeper into the region's o erings.




Begin your journey with a visit to the Botanic Gardens and the iconic Cathedral Square in Christchurch, providing an insightful introduction to the city and its vicinity. Dive into the realm of art and culture by exploring the Christchurch Art Gallery Te Puna o Waiwhetū and the Canterbury Museum, or elevate your perspective with a thrilling hot air balloon ride, o ering breathtaking views from above. For a relaxing interlude, a day trip to Hanmer Springs beckons with rejuvenating hot pools and picturesque landscapes.
Attendees of the Annual Scientific Meeting have the perfect opportunity to seamlessly blend professional development with leisure and tourism, embracing the best that Christchurch and the region have to o er. In addition to local activities like city tram tours and punting on the Avon River, visitors can savoUr the diverse culinary scene, from riverside restaurants to culinary markets such as the Arts












For those seeking to explore beyond Christchurch, destinations such as Milford Sound, Tekapo, Queenstown, Arthurs’ Pass, Fox Glacier, Hanmer Springs, and Mount Cook o er a diverse array of spectacular landscapes and thrilling activities to enhance their experience in New Zealand. With a harmonious blend of adventure, culture, and natural beauty, New Zealand promises to be an unforgettable destination for any traveler.




























































CASE STUDY
POOR FDG METABOLISM - AN INTERESTING APPEARANCE OF UNEXPLAINABLE UPTAKE
Remi Hillery Sunshine Coast University HospitalClinical History: The patient was diagnosed with non-small cell lung cancer (NSCLC) Stage IV T1bN1M1a in October 2021. Their medical history included hypertension, dyslipidaemia and childhood Hepatitis C (cured 2 years prior with no complications), but otherwise well. They presented for a baseline 18F-FDG PET/CT that demonstrated multiple pleural based nodules in L) hemithorax, LLL oblique fissure nodules and left hilar lymph node involvement.
Their treatment consisted of Pembrolizumab for 2 years, following which a post-treatment 18F-FDG PET/CT scan was completed, confirming no residual or recurrent disease, or new metastatic disease detected (October 2023).
Two months later, the patient begun to feel increasingly unwell, including symptoms such as oedema in legs, aches and pains, lack of energy, nausea, lack of appetite, as well as test results indicating high lactate dehydrogenase (LDH) and low albumin. Blood tests demonstrated only mildly deranged liver function tests (LFTs). Computed Tomography (CT) of the Head, Abdomen and Pelvis was completed, which demonstrated no recurrence, however generalised subcutaneous tissue and mesenteric fat stranding was detected, suggesting cardiac status or fluid overload. Echo results were normal and an ultrasound was completed to rule out deep vein thrombosis (DVT). The patient was referred to Immunology for her progressive peripheral oedema, where tests were completed to rule out Capillary Leak Syndrome.
A repeat 18F-FDG PET/CT scan was requested again two months later (February 2024) to check for recurrence. High dose prednisolone (70mg) was prescribed to treat symptoms and taken for 7 days prior to PET scan.
Procedure Results: The patient was administered with 221MBq 18F-FDG and completed a 67minute uptake prior to scanning from vertex to mid-thigh. They had a blood sugar level of 4.6mmol/L and exceeded the required 6 hour fasting requirement.
The 18F-FDG PET/CT scan demonstrated reduced uptake in the brain (compared with previous), reduced FDG metabolism in the soft tissue structures, particularly the heart musculature, liver, spleen, kidney (parenchyma) and bowel, reduced FDG in muscles and adipose tissue and diffuse mild FDG uptake in bone marrow. The PET confirmed no evidence of recurrent or new metastatic disease.
Despite the significantly decreased uptake in this scan, there was no evidence of any technical fault that would result in this scan appearance.


Case Study: Poor FDG metabolism - An interesting appearance of unexplainable uptake (Continued)
A comparison has been made between the patients most recent PET scans:

Discussion: There are various causes for decreased uptake in a 18F-FDG PET/CT scan, including age, blood glucose levels, body habitus, improper patient preparation, medications, and uptake time. Patients are asked to fast for 6 hours prior to PET/CT scan in order to achieve a euglycaemic state. Normal biodistribution of 18F-FDG includes increased uptake in the brain (due to glucose metabolism), the urinary system (as FDG is not trapped
by renal tubular cells), the liver (due to glycolysis) and myocardium (due to anaerobic glycolysis).1
The patient’s PET/CT scan demonstrated an impaired glucose metabolism, and based on the distribution of organ involvement, recommended glucose transporter regulation.
Case Study: Poor FDG metabolism - An interesting appearance of unexplainable uptake (Continued)
Glucose Transporter Regulation (GLUT and / or SGLT): Glucose transporters are membrane associated carrier proteins, with two different types: Sodium glucose linked transporters (SGLT) and glucose transporter proteins (GLUT), that move glucose from the extracellular space in the bloodstream into cells. Different GLUT isoforms are involved in regulating tissue-specific glucose uptake and metabolism in the liver, skeletal muscle and adipose tissue, to ensure homeostatic control of blood glucose levels. Impaired glucose regulation can result in abnormal use of energy substrates and is often associated with insulin resistance.2
Glucose transport is important and used in 18F-FDG PET/CT scanning to detect cancer cells, as cancer cell growth is supported by increased glucose metabolism compared with normal cells. FDG expression is described in many different cancers, including lung, due to the high metabolic rate, however, is generally absent in benign epithelial cells.3
There are limited studies that discuss potential causes of general poor glucose metabolism in 18F-FDG PET/CT scans. The patient’s treating teams suggested it may be caused by an acute insulin resistance, or less likely, as a result of her corticosteroid treatment.
Acute Insulin Resistance: Insulin resistance is the inability of insulin to sufficiently stimulate glucose uptake, predominantly in skeletal muscle and adipose tissue, or to inhibit gluconeogenesis in the liver. Hyperglycemia and insulin resistance are often a result of injury or serious illness, however, acute insulin resistance is complex and characterized by rapid onset, and may have multiple causative factors and intracellular pathways.4
Hepatic glucose production increases as a result of insulin resistance, thus reducing glucose uptake within the liver, resulting in decreased FDG uptake in the liver for these patients.5
Insulin resistance may reflect functional impairment of adipose tissue, resulting in a decreased glucose uptake.5 Muscle is a considerable site for insulin-mediated glucose disposal, where FDG is widely known to have increased uptake in muscles in a state of high serum insulin levels.6 Glucose uptake in the brain is facilitated by insulindependent glucose transporters that are widely expressed in the brain. Glucose metabolism in the brain can be assessed with FDG PET, where studies have demonstrated that patients with insulin resistance have decreased uptake in the brain.7
Corticosteroid Therapy Interference: Corticosteroids are anti-inflammatory medications often used to treat a large variety of illnesses and comorbidities; however, they can have numerous side effects. Corticosteroids reduce the insulin sensitivity in one’s body, resulting in more insulin being required to transport glucose into cells, prevent glucose from being absorbed by muscle and fat, resulting in higher glucose circulation in the blood stream.8
Corticosteroid treatment is associated with significant reduction in the intensity of FDG uptake, particularly in granulomas and myocardial tissue, regardless of dosage and duration of corticosteroid therapy.9
As the liver plays an important role in glucose regulation, patients with higher glucose levels often demonstrate increased FDG uptake in the liver. Corticosteroid treatment often results in increased glucose levels and correspondingly an increased FDG hepatic uptake.10
Case Study: Poor FDG metabolism - An interesting appearance of unexplainable uptake (Continued)
CORTICOSTEROID USE CHARACTERISTICS PRESENT IN THIS PATIENT ?
Reduced uptake in myocardial tissue Yes
Increased hepatic uptake No
Higher glucose levels No
Fluid retention Yes
Weight gain / Increased appetite No
Conclusion: No single suggested pathology or cause explained or justified the patient’s scan appearance and symptoms. The patient noted that some of their symptoms had eased since beginning steroid treatment (albumin and LDH improving), however, they noted more muscle wasting. The patient was admitted for a liver biopsy (results pending) and is booked for a Lower Limb Lymphoedema Lymphoscintigraphy scan. A team from Immunology, Renal, Hepatology and Endocrine are currently reviewing this case due to its difficult prognosis.
References
1. PrinciplesandPracticeofPET-CT.pdf
2. Glucose transporters in adipose tissue, liver, and skeletal muscle in metabolic health and disease | Pflügers Archiv - European Journal of Physiology (springer.com)
3. 18F-fluoro-2-deoxyglucose uptake on PET CT and glucose transporter 1 expression in colorectal adenocarcinoma - PMC (nih.gov)
4. Acute Insulin Resistance Following Injury - PMC (nih.gov)
5. 18F-FLUORODEOXYGLUCOSE PET/CT CAN BE AN ALTERNATIVE METHOD TO ASSESSMENT OF INSULIN RESISTANCE - PMC (nih.gov)
6. Atlas of non-pathological solitary or asymmetrical skeletal muscle uptake in [18F]FDG-PET - PMC (nih.gov)
7. Insulin Resistance Is Associated With Enhanced Brain Glucose Uptake During Euglycemic Hyperinsulinemia: A Large-Scale PET Cohort - PMC (nih.gov)
8. The effect of different types of oral or intravenous corticosteroids on capillary blood glucose levels in hospitalized inpatients with and without diabetes - ScienceDirect
9. Effect of steroids on [18F]fluorodeoxyglucose uptake in an experimental tumour model - PubMed (nih.gov)
10. Clinical implications of increased uptake in bone marrow and spleen on FDG-PET in patients with bacteremia - PMC (nih.gov)

CASE STUDY
THE UTILITY OF 68GAPSMA EXPRESSION IN ADENOID CYSTIC CARCINOMA OF THE HEAD AND NECK: A CASE STUDY
Anisa KumariNuclear Medicine and Molecular Imaging, Division of Diagnostic Radiology, Princess Alexandra Hospital (PAH), Brisbane, Queensland, Australia
Background: Adenoid cystic carcinomas (AdCC) of the head and neck are a rare epithelial tumour, it originates in the exocrine glands such as the major and minor salivary glands1. AdCC accounts for only 1% of head and neck cancers, and can occur at all ages, with median age between 50-60 years1. There is no strong genetic or environmental risk factors associated with cause of disease2. This disease can emulate broad symptoms such as painful masses or nerve paralysis 2,3 Current treatment and management options are surgical resection followed by postoperative radiotherapy and chemotherapy which is only used in the management of palliative cases1,2,3
Clinical History: A 49-year-old male patient presented with a painful mass under his right lip, initially assessed as
an infection the patient was treated with antibiotics. The patient experienced further facial numbness suggestive of a skin cancer lesion, a biopsy was taken with histological diagnosis of basal cell carcinoma. MRI revealed infiltrative growth patterns inconsistent with BCC histology, subsequently additional biopsy, and PET/CT 18F-FDG was required to confirm findings however, conflicting results of AdCC and BCC were found, and therefor 68Ga-PSMA was requested for differential diagnosis.
Method: 68Ga-PSMA was performed to confirm differential diagnosis. Patient was injected with 156Mbq of 68GaPSMA with an uptake time of 44 minutes for PET/ CT, including a dedicated head and neck and torso image. PET/MRI was conducted immediately after, with an uptake time of 78 minutes, parameters as per Table 1.
Case Study: The Utility of 68GaPSMA Expression in Adenoid Cystic Carcinoma of the Head and Neck (Continued)
Results: Both 68Ga-PSMA PET/CT and PET/MRI highlight expression of PSMA in submandibular lesion, infiltrative perineural involvement (infra orbital lesion) and uptake in right upper lip region, findings supported histology of AdCC (Figure 4) and ruled out distant metastasis. 68GaPSMA imaging confirmed diagnosis of AdCC of the head and neck and patient underwent surgery next day. Wide local excision of primary lesion on right lip with transfacial craniotomy. Pathology revealed positive margins, patient was referred for postoperative radiotherapy. As a result, 68Ga-PSMA imaging has been requested as the initial management tool for this patient's future follow up.
Discussion: The survival rate post current treatment methods decrease dramatically after 10 years to 40%1. MRI and biopsy are currently the gold standard of detecting Adenoid cystic carcinoma1,2. Due to AdCC high recurrence rate the importance of early differential diagnosis, prolonged post treatment monitoring & management1,2,3
Standalone MRI (Figure 1) in this case was unable to clearly differentiate conflicting histological results of the biopsies (BCC and AdCC) highlighting infiltrative growth patterns suggesting AdCC. 18F-FDG PET/CT (Figure 2) showed Low grade avidity in lesions (SUV max between 4.3-5.7) associated with BCC. 18F-FDG imaging was also unable to clear highlight infra orbital lesion.
Sequential 68Ga-PSMA PET/CT (Figure 3) and PET/MRI (Figure 4) was able to diagnosis and manage patient treatment outcome. This imaging pathway is unique to the PAH and provides anatomical localisation of lesions, visualisation of distant metastases and is non-invasive staging tool.
The long-term outcome of altering treatment planning based on 68Ga-PSMA should be considered for all head and neck AdCC3. A study by Klein Nulent et al., 2021 has utilized 68Ga-PSMA as an assess eligibility for 177Lu-PSMA therapy and found positive palliative treatment response3.


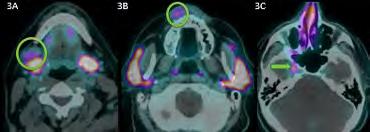

Conclusion: 68GaPSMA in conjunction with PET/MRI and PET/CT has aided in diagnosis and management of patient's disease progression and should be considered as a new gold standard for imaging AdCC of head and neck. With current treatment options of AdCC of the head and neck unsuccessful in clearing patient of disease, Theranostic applications could be considered as a future treatment option for AdCC of the head and neck.
References
1. van Boxtel, W., Lütje, S., van Engen-van Grunsven, I., Verhaegh, G. W., Schalken, J. A., Jonker, M. A., Nagarajah, J., Gotthardt, M., & van Herpen, C. (2020). 68Ga-PSMA-HBED-CC PET/CT imaging for adenoid cystic carcinoma and salivary duct carcinoma: a phase 2 imaging study. Theranostics, 10(5), 2273–2283. https://doi.org/10.7150/thno.38501
2. Klein Nulent, T.J.W., Valstar, M.H., Smit, L.A. et al. Prostate-specific membrane antigen (PSMA) expression in adenoid cystic carcinoma of the
head and neck. BMC Cancer 20, 519 (2020). https://doi.org/10.1186/s12885020-06847-
3. Nulent, T. J. W. K., van Es, R. J. J., Willems, S. M., Braat, A. J. A. T., Devriese, L. A., de Bree, R., & de Keizer, B. (2021). First experiences with Lu-177-PSMA-617 therapy for recurrent or metastatic salivary gland cancer. EJNMMI Research, 11(1), [126]. https://doi.org/10.1186/s13550-021-00866-8
CASE STUDY
EVALUATING WHETHER A VISUAL GRADING SCORE CAN BE APPLIED TO THE USE OF GALLIUM67-CITRATE SCINTIGRAPHY IN THE ASSESSMENT OF PATIENTS SUSPECTED OF RENAL ALLOGRAFT PYELONEPHRITIS: A SINGLE CENTRE RETROSPECTIVE AUDIT.
Skelton, Julia1; Katchel, Loren;1 Hillery, Remi;1 Ngai, Stanley;1 Cuscaden, Claire 1. Department of Nuclear Medicine, Princess Alexandra Hospital, Queensland, AustraliaIntroduction: Renal transplant patients are susceptible to multiple sources of infection, most commonly urinary tract infection.1 Urinary tract infections may present as cystitis, native kidney pyelonephritis or acute graft pyelonephritis (AGPN), the latter of which can be catastrophic as it may lead to impairment of graft function, graft loss and mortality.2-4 AGPN requires intensive management with weeks of antibiotic therapy and close monitoring of graft function.5 Prevalence of AGPN varies between 10-16.5%.6,7 Gallium(Ga67)-Citrate scintigraphy is able to assist clinicians in not only in identifying AGPN, but also in identifying other sites of infection and monitoring disease response following treatment.8-10 To our knowledge, there has been no visual method established to score uptake in the kidney in patients suspected of AGPN. We propose a visual grading scale describing uptake within the transplant kidney and whether this is a reliable and feasible way to confirm a diagnosis of AGPN.

Methods: We performed a single centre retrospective audit of all 67Ga-Citrate scans performed in renal transplant recipients suspected of AGPN at the Princess Alexandra Hospital between 2017 and 2023 inclusive. Planar imaging for each patient were grouped visually into four categories (Image 1): Grade 0 (no uptake seen within transplant kidney), Grade 1 (uptake seen and intensity less than physiological liver), Grade 2 (uptake seen and intensity similar to physiological liver) and Grade 3 (uptake seen and intensity greater than physiological liver). Uptake of 67Ga-Citrate within the kidney was also classified as either diffuse or focal. Single Positron Emission Computed Tomography – CT (SPECT-CT) imaging was performed to confirm additional anatomical information. Grade 2 and 3 were considered positive on scintigraphy. This scoring system was then compared to the formal report made by the radiologist or nuclear medicine physician (who also had access to all images including SPECT-CT fused images) to confirm or exclude a radiological diagnosis of AGPN.
This was the reference standard used for comparison with diagnostic testing.
Image 1: Visual Classification of radiotracer uptake in Ga67-Citrate scintigraphy (planar imaging).
Case Study: Evaluating whether a visual grading score can be applied to the use of Gallium67-Citrate scintigraphy in the assessment of patients suspected of renal allograft pyelonephritis: a single centre retrospective audit.
Results: Between January 2017 and October 2023, 278 Ga67-Citrate scans were performed at the Princess Alexandra Hospital in renal transplant patients suspected of AGPN. A total of 141 patients underwent Ga67-Citrate scans, 81 were whom were female (57%). The average age of patients at the time of scan was 55 years old and the average number of years since transplant was 7.3 years. Of 141 patients, 73 underwent more than one scan, either for new symptoms or for follow-up to assess progress or resolution while on antibiotic treatment. Ga67-Citrate scans were ordered on an inpatient (161) and outpatient (117) basis.
The most common presentations and indications for gallium scans are listed in Table 1.
Of the 278 scans, 32 (11.5%) were classified as Grade 0, 145 (52%) as Grade 1, 55 (20%) as Grade 2 and 46 (16.5%) as Grade 3. Focal uptake was seen in 109 (39%) scans and 137 (49%) showed diffuse uptake within the kidney. Of all 278 scans, 78 (28%) scans were formally reported negative for AGPN, 96 (35%) were reported as indeterminate and 104 (37%) were reported as positive. Indeterminate results were re-classified as negative for AGPN. Graph 1 illustrates the number of scans within each scintigraphy category and their corresponding radiological diagnosis. Comparing a positive diagnosis on scintigraphy (Grade 2 or 3) with the radiology report as the reference standard yielded a sensitivity of 76% (95% CI [66.5, 83.8]) and specificity of 87.3% (95% CI [81.4, 91.9]). Positive and negative predictive values were 53.4% (95% CI [43.3, 63.2]) and 95% (95% CI [93.1, 9.43]) with a disease prevalence of 16% respectively.
When patterns of uptake were focal, sensitivity increased to 78.5% (95% CI [68.2, 86.7]) and specificity increased to 87.7% (95% CI [76.3, 94.9]). Positive and negative predictive values were 54.9% (95% CI [37.6, 71.1]) and 95.6% (95% CI [93.38, 97.04]).
FORMAL RADIOLOGICAL
FOR SCINTIGRAPHY
CASE STUDY
UTILITY OF LUNG V/Q SCANS ON PATIENTS WITH FONTAN CIRCULATION FOR DIAGNOSING PULMONARY EMBOLISMS- CASE STUDY
Raelee McNab Queensland Health- Townsville University HospitalIntroduction: Fontan Circulation occurs in patients with congenital heart defects that require the corrective Fontan Procedure.
The congenital heart defect that is going to be discussed today is double inlet left ventricle in which both atriums are connected to the left ventricle with a severely hypoplastic right ventricle. Therefore not enough blood is being pumped into the pulmonary arteries and there is an unequal distribution of oxygen-rich and oxygen-poor blood in the body.
For this condition, the patient will undergo a modified Fontan procedure which includes connecting the right atrium directly to the pulmonary artery so that the atrium acts as the right ventricle, pumping the blood from the Superior Vena Cava (SVC) and Inferior Vena Cava (IVC) into the lungs to get oxygenated. Indicated in the diagram below.
One of the leading causes of mortality in patients that have undergone Fontan surgery, is thromboembolic disease due to their altered cardiac anatomy.
Cardiac History and Previous Imaging: The patient (36M) had a history of 10 corrective cardiac surgeries between the ages of 3-21 years old.
The most important surgery in the context of this case study was his modified Fontan procedure, completed at 3 years old. The procedure resulted in the right atrium being what literature states as ‘ventriclized’ and attached
directly to the pulmonary artery. (Cooke et al., 2020). Patient had been referred with complex congenital cardiac history with presentation of left sided pleuritic pain and new oxygen requirement. A Computed Tomography Pulmonary Angiogram (CTPA) was requested to determine if the patient had a Pulmonary Embolism (PE) The CTPA was completed the night before resulting in a non-diagnostic study.
This is because in a normal heart, contrast-enhanced blood is mixed with the non-contrast enhanced blood in the right ventricle, resulting in equal distribution of the contrast in the pulmonary arteries.
However, in both Fontan and modified-Fontan circulation there is no pathway from the right atrium into the right ventricle and hence there is uneven distribution and mixing of the contrast in the pulmonary arteries resulting in difficulty in bolus tracking and imaging. Hence, a V/Q scan was ordered in order to determine if the patient had an acute/chronic Pulmonary Embolism.

Case Study: Utility of Lung V/Q Scans on Patients with Fontan Circulation for Diagnosing Pulmonary Embolisms
- Case Study. (Continued)
What Fontan Circulation Patient Management means for V/Q Scans: As our physicians and technologists reviewed the referral they understood the significance of the Fontan circulation in this patient. It was determined that this patient needed to have two injections of 99mTc-Macroaggregated Albumin (MAA), one in the upper limb and one in the lower limb to be able to confidently rule in or out a PE.
This protocol of two injections is something that has been seen in literature to describe revised protocols in contrast injections for CTPA scans in patient with Fontan circulation. However in this case this was not completed in the previous CTPA. The revised protocol was that of a standard ventilation Single Photon Emission Computed Tomography (SPECT), a standard injection of 99mTcMAA into the right cubital fossa with a SPECT of the SVC Perfusion, and a standard injection of 99mTc-MAA into the left lower leg with a SPECT of the IVC Perfusion, with an additional low-dose CT scan.
During processing derived planar images were acquired along with a geometric mean was also taken fo the right and left lung perfusion, to observe if there is any preferential filling.

Patient Management: Without the use of dual injection into the upper and lower limb, a false positive diagnosis of a PE is probable and a diagnostic image is unlikely due to the uneven distribution of the contrast in the blood.
This case demonstrates not only how important nuclear medicine is in diagnosing PE in patients with unusual pathologies but also in being able to problem solve and accurately understand the patient's history impacts it may have on the pathology that is needed to be imaged.
After this scan it was confidently reported that the patient did not have any evidence of acute or chronic pulmonary emboli, and that there was also no preferential venous blood flow from the IVC or SVC into the left or right lung.
Conclusion: It is essential that all medical radiation practitioners are aware of the impact that a congenital heart efect can have on certain diagnostic scans.
The change of the protocol to account for the congenital heart defect is important for all practices to have knowledge about as it can have a large impact the patient’s care plan.

CASE STUDY
THE EFFICACY OF 18 F-FDG PET/CT IN THE DIAGNOSIS AND TREATMENT OF ERDHEIMCHESTER DISEASE: A CASE STUDY
Stephanie Schulz Department of Nuclear Medicine & PET/CT, Gold Coast University Hospital, Gold Coast, Queensland, AustraliaBackground: Erdheim-Chester Disease (ECD) is an extremely rare multisystem disorder. The underlying cause is largely unknown but thought to arise from a malignancy of the myeloid progenitor cells3. In 2016, the World Health Organization classified it as a rare type of blood cancer. Most patients are diagnosed between the ages of 40-70, but there have been cases of children and young adults reported. It affects both men and women, with a higher incidence in the male population of approximately 60%5
The disease is characterised by excessive production and accumulation of histiocytes, whose normal function is to fight infection. These excess cells infiltrate the loose connective tissue of the body and cause inflammation, resulting in thickened, dense, and fibrotic tissue which can lead to organ failure5

Some patients may experience relatively indolent disease and remain asymptomatic while others may experience more aggressive disease affecting multiple organs. Clinical signs and symptoms will differ based on the degree and number of organs involved in the disease4. Organs actively involved with ECD will take up excess FDG due to the inflammatory processes associated with histiocytic infiltration, and hence increased glucose metabolism2 There is no cure for ECD, but treatment options include targeted therapy, immunotherapy, and chemotherapy. Surgery, radiation therapy, and corticosteroids may also be used to relieve symptoms4.
Methods: A 33-year-old male presented to emergency after 4 weeks of suffering from constitutional symptoms including weight loss, diarrhoea, and fatigue. He was found to have a fever and mild tachycardia and initial blood tests showed LFT derangement, acute renal failure and pancytopaenia. Due to the patient’s drinking history, the initial diagnosis was alcohol induced pancreatitis. He was sent for an x-ray, ultrasound, and non-contrast CT of his abdomen (due to low eGFR of 28), which showed hepatosplenomegaly and bilateral renal enlargement. Initial imaging was non diagnostic for pancreatitis.
The patient was admitted, and his clinical symptoms were treated with medication and IV fluids. He was sent for a multiphase CT of his pancreas once his eGFR had improved (now 54). The CT findings showed a multisystem infiltrative condition affecting the pancreas, liver and kidneys, which was suggestive of systemic disease. Differential diagnoses included an autoimmune
Case Study: The Efficacy of 18F-FDG PET/CT in the Diagnosis and
Treatment of Erdheim-Chester Disease. (Continued)
disorder, IgG4 related disease or small vessel vasculitis. Pancreatitis and malignant infiltration were considered to be unlikely given the scan appearances. Based on these findings, the patient was referred for a renal biopsy and an 18F-FDG PET/CT scan.


Procedure: The patient fasted for 6 hours prior to an intravenous injection with 259MBq of 18F-FDG. Post void imaging was commenced 55 minutes later using a Siemens Biograph mCT PET/CT scanner. The patient was scanned according to the parameters in the table below. A low dose CT was acquired for attenuation correction purposes prior to the PET scan and a diagnostic contrast CT of the head and chest was acquired once the PET scan was completed.
TABLE
Torso: 2.5min/bed
Upper Leg: 1.5min/bed
Lower
Arterial Thorax
Chin to below liver, arms up
Post Contrast Head
Chin to top of head, arms down
Arterial Thorax
7 second delay after bolus trigger
Post Contrast Head
3 minutes post contrast administration
Case
Study: The Efficacy of 18F-FDG PET/CT in the Diagnosis and Treatment of Erdheim-Chester Disease. (Continued)
AND DIAGNOSTIC CONTRAST CT PARAMETERS
PET/CT Parameters
Diagnostic CT with Contrast Parameters
Arterial
Post Contrast Head 120 kV
Findings: The PET scan showed intense uptake in the kidneys and pancreas, moderate uptake in the right medial parieto-occipital region, and mild to moderate uptake in the spleen, portacaval and paraaortic lymph nodes and pulmonary nodules. When paired with the results of the renal biopsy which displayed histiocytic infiltration, these findings were in keeping with a diagnosis of thoracic and abdominal ECD. The patient was immediately started on interferon immunotherapy and later discharged.

The patient was admitted a month later as his clinical symptoms and blood tests were worsening. He was referred for repeat 18F-FDG PET/CT imaging as a baseline study prior to a change in treatment. The PET scan found resolution of some lesions in the lung and pancreas, a similar appearance in the kidneys with an impression of infarcts, and the spleen was now intensely avid. The patient was commenced on Cobimetinib, a targeted therapy, which is traditionally used to treat malignant melanoma4.
The patient’s symptoms and blood tests improved, and a follow up PET scan in September showed a near-complete treatment response. He reported feeling well and had put weight back on. His treating team decided to reduce his treatment dose which resulted in a flare up of his initial symptoms. His PET scan in December, showed disease recurrence, predominantly involving the kidneys and pancreas. His treatment dose was increased again, and his symptoms resolved. The patient continues to be followed up with 18F-FDG PET/CT scans.
Case Study: The Efficacy of 18F-FDG PET/CT in the Diagnosis and Treatment of Erdheim-Chester Disease. (Continued)

Discussion: 18 F-FDG PET/CT is the only imaging technique that depicts the full extent of the organs affected by ECD. Organs actively involved with ECD will take up excess tracer due to the inflammatory processes involved with histiocytic infiltration2. The physiological nature of FDG-PET imaging allows clinicians to assess active sites of disease, determine optimal biopsy sites and course of treatment, and then monitor response to treatment and whether adjustments need to be made.
ECD is notoriously difficult to diagnose, hence it is most likely under-diagnosed with approximately 1000 reported cases since it was first documented in 19305. In saying that, we currently perform surveillance scans on several patients with ECD within our department and expect that as clinicians become more familiar with the characteristics of the disease, that referrals for FDG-PET to investigate ECD will increase.
References
Prognosis for ECD had been reported as relatively poor, with a 5-year survival rate of 43% in 1996, which can be attributed to delays in diagnosis and treatment. The reported 5-year survival rate in 2023 is now 83%, proving that when diagnosed early and treated effectively, patients with ECD can live a nearly normal life4. FDG-PET as a first line imaging technique when ECD is suspected, should be highly recommended, to provide a timely diagnosis and monitor patient response to treatment.
Conclusion: 18 F-FDG PET/CT imaging has played a vital role in the timely diagnosis and treatment course of this patient. It has allowed treating physicians to determine the full extent of the disease and therefore the treatment required. Through accurately evaluating response to treatment, FDG-PET scans have also aided in the ongoing management of this patient and resulted in adjustments to his treatment course.
1. Ravindran, A. M., Picarsic, J. M., Goyal, G. M., Go, R. S., & Durham, B. H. (2023). Erdheim-Chester Disease: An Algorithmic Approach to a Diagnosis. Retrieved November 6, 2023, from Erdheim-Chester Disease Global Alliance website: https://erdheim-chester.org/news/erdheim-chester-disease-analgorithmic-approach-to-a-diagnosis/
2. Rahman, W. T., Wale, D. J., Viglianti, B. L., Townsend, D. M., Manganaro, M. S., Gross, M. D., ... & Rubello, D. (2019). The impact of infection and inflammation in oncologic 18F-FDG PET/CT imaging. Biomedicine & Pharmacotherapy, 117, 109168.
3. Robert D. Shamburek, M. (2023). Erdheim Chester Disease. Retrieved November 6, 2023, from National Organization for Rare Disorders (NORD) website: https://rarediseases.org/rare-diseases/erdheim-chester-disease/
4. Cleveland Clinic MD. (2023). Erdheim-Chester Disease. Retrieved November 6, 2023, from Cleveland Clinic website: https://my.clevelandclinic.org/health/ diseases/24668-erdheim-chester-disease
5. ECD Global Alliance (2024). Erdheim-Chester Disease. Retrieved November 6, 2023, from ECD Global Alliance website: https://erdheim-chester.org/ about-ecd/
Case Study: The Efficacy of 18F-FDG PET/CT in the Diagnosis and Treatment of Erdheim-Chester
Disease. (Continued)
Diffuse uptake patterns had the lowest sensitivity at 65% when tested independently however had the highest specificity at 89.9% (see Table 2 for CI and comparison).
TABLE 2: SENSITIVITY AND SPECIFICITY OF SCANS BASED ON UPTAKE
Discussion and Conclusion: Our results conclude that a visual grading score can be applied to Ga67-Citrate scans to assist physicians and radiologists in the diagnosis and monitoring of AGPN. Of all scans reported as positive by the radiologist, a Grade of 2 or 3 on scintigraphy was able to accurately identify positive scans in 76% of those cases. More significantly, of those reported by the radiologist as negative, a Grade of 0 and 1 on scintigraphy was able to exclude the diagnosis in 87% of patients. Scans with a scintigraphy category of Grade 0 and 1 were truly negative in 95% of cases, when compared to the radiology report. Both sensitivity and specificity increased when focal uptake was seen on planar imaging. Given the risks of contrast nephrotoxicity associated with conventional cross-sectional imaging, these results suggest that Ga67-Citrate scintigraphy and the application of our grading score may be a useful adjunct to assist clinicians with decision-making in the transplant setting.
Limitations of our audit include the use of the radiology report as the reference standard, implying an “error free” gold standard. Due to this, the accuracy of our test may have been over- or underestimated. Additionally, we grouped indeterminate results as negative as the low uptake was “of unclear significance”, according to the radiologist report. Of the 96 indeterminate scans, 41 (43%) were follow-up scans after 3 months of antibiotic treatment, and only 54 (56%) were treated as AGPN by the transplant team. Additionally, in some cases, treatment for indeterminate results was commenced based on additional factors such as positive blood cultures.
References
1 Chuang P, Parikh CR, Langone A. Urinary tract infections after renal transplantation: a retrospective review at two US transplant centers. Clinical Transplantation. 2005;19(2):230–5.
2. Lee JR, Bang H, Dadhania D, Hartono C, Aull MJ, Satlin M, et al. Independent risk factors for urinary tract infection and for subsequent bacteremia or acute cellular rejection: a single-center report of 1166 kidney allograft recipients. Transplantation. 2013 Oct 27;96(8):732–8.
3. Dupont PJ, Psimenou E, Lord R, Buscombe JR, Hilson AJ, Sweny P. Late recurrent urinary tract infections may produce renal allograft scarring even in the absence of symptoms or vesicoureteric reflux. Transplantation. 2007 Aug 15;84(3):351–5.
4. Abbott KC, Swanson SJ, Richter ER, Bohen EM, Agodoa LY, Peters TG, et al. Late urinary tract infection after renal transplantation in the United States. Am J Kidney Dis. 2004 Aug;44(2):353–62.
5. Parasuraman R, Julian K, Practice the AIDC of. Urinary Tract Infections in Solid Organ Transplantation. American Journal of Transplantation. 2013;13(s4):327–36.
6. Fiorante S, Fernández-Ruiz M, López-Medrano F, Lizasoain M, Lalueza A, Morales JM, et al. Acute graft pyelonephritis in renal transplant recipients: incidence, risk factors and long-term outcome. Nephrology Dialysis Transplantation. 2011 Mar 1;26(3):1065–73.
7. Kamath N s., John G t., Neelakantan N, Kirubakaran M g., Jacob C k. Acute graft pyelonephritis following renal transplantation. Transplant Infectious Disease. 2006;8(3):140–7.
8. Nowosinska E, Navalkissoor S, Quigley AM, Buscombe JR. Is there a Role for Gallium-67 Citrate SPECT/CT, in Patients with Renal Impairment or Who are Renal Transplant Recipients, in Identifying and Localizing Suspected Infection? World J Nucl Med. 2015;14(3):184–8.
9. Sebrechts C, Biberstein M, Klein JL, Witztum KF. Limitations of indium-111 leukocyte scanning in febrile renal transplant patients. AJR Am J Roentgenol. 1986 Apr;146(4):823–9.
10. John U, Kemper MJ. Urinary tract infections in children after renal transplantation. Pediatr Nephrol. 2009;24(6):1129–36.
CASE STUDY
USING ESTIMATED GFR TO DETERMINE APPROPRIATE PLASMA SAMPLING TIME FOR SINGLE-SAMPLE GFR MEASUREMENT
Aim: To assess whether creatinine-based estimated GFR (eGFR) can determine the most appropriate plasma sampling time to optimise single-sample measured GFR using 99mTc DTPA, as suggested in the 2018 British Nuclear Medicine Society GFR Measurement Guidelines.
Method: A retrospective review of data from 587 GFR measurements (mGFR) using 99mTc DTPA was performed, comparing the results to a prior eGFR reported on the hospital pathology system, based on the CKD-EPI equation. Comparison was also made in a smaller subset (275 studies) to other methods of estimating GFR: the Cockcroft–Gault creatinine clearance, and the MDRD eGFR. Results were assessed to determine appropriate eGFR levels to optimise the sampling time for measuring GFR accurately.
Results: eGFR as reported by the hospital pathology system showed a mean difference (±SD) of 5.84 (±12.84) mL/min/1.73 m2 for eGFR ≤90 mL/min/1.73 m2. Similar differences were obtained using the Cockcroft-Gault (3.32 ± 12.6 mL/min/1.73 m2) and MDRD (5.21 ± 12.27 mL/

min/1.73 m2) equations. eGFR >90 is reported as >90 (due to uncertainty in the estimation above this level); in these cases the measured GFR was >90 in only 106/235 cases (45.1%), again with similar results with the other equations (43.7% for C-G; 46.9% for MDRD), hence high eGFR is a poor predictor of high measured GFR, and hence cannot be used to confidently recommend a 2 h sample time in any patients. An eGFR ≥60 mL/min/1.73 m2 resulted in a mGFR ≥50 mL/min/1.73 m2 on 95.2% of cases, and is, based on these results, the most suitable cutoff for determining when a 3 h sample is appropriate. eGFR between 30 and 59 mL/min/1.73 m2 is suitable to determine a 4 h sample, as only 6.5% of measured GFR results were subsequently below 30 mL/min/1.73 m2, which is when a 24 h sample should also be performed.
Conclusion: eGFR may be used to determine appropriate sampling time for measuring GFR; this review suggests a sampling time of 3 h when eGFR ≥60 mL/min/1.73 m2, 4 h when eGFR is between 30 and 59 mL/min/1.73 m2, with a 24 h sample when eGFR <30 mL/min/1.73 m2.

CASE STUDY
EVALUATION OF EFFECTS OF BRONCHOSCOPIC LUNG VOLUME REDUCTION ON DIFFERENTIAL LOBAR FUNCTION USING QUANTITATIVE VQ (EMPHYSISE STUDY).
Chew C.1'4, Fon A.2'4, Nguyen P.3'4, Jersmann HPA.3'4, Crouch B.1, Schultz C.1,Sami Flinders Medical Centre
Background:
Emphysema is a form of chronic obstructive pulmonary disease, which is characterised by an increase in end-expiratory lung volume as a result of loss of elastic recoil of the terminal bronchioles. There is also associated pulmonary capillary destruction. There is a disproportionately worse reduction in ventilation, which results in dead space ventilation (1,2).
Patients with emphysema who are no longer responding to maximum standard medical management may benefit from bronchoscopic lung volume reduction (BLVR) using endobronchial valves (EBV). When deployed these oneway valves cause a collapse of the treated lobe with the potential benefit of improving mechanical ventilation of the other untreated lobes. This interventional treatment has been shown to result in significant symptomatic and mechanical improvement. It is a reversible treatment that is proven to be safe (3,4,5).
The current gold standard investigation to determine the target lobe to collapse with BLVR-EBV is quantitative CT (qCT). This test quantifies the proportion of each lobe that has tissue density below a Hounsfield score of -950, a threshold that defines the presence of emphysema. The target lobe is preferably the one with highest emphysema percentage. The lobe that is ipsilateral to the target lobe is preferentially substantially less emphysematous. A difference of at least 15 percentage points between the target lobe and the ipsilateral lobe is preferred, a threshold that defines “heterogenous emphysema”.
In our institution we have developed a program based on interactive data language software that allows lobar quantification of ventilation and perfusion by fusing the datasets of a VQ SPECT scan and a CT. The result is a differential lobar percentage of volume from the CT, ventilation with 99mTc Technegas® (Cyclomedica, Australia) and perfusion with 99mTc MAA (DRAXIMAGE MACROSALB®. Jubilant RadiopharmaTM , Canada). An example result is displayed in a spreadsheet in table 1a. We contend that these results on their own are not adequate to confidently assess differential lobar function and parenchymal injury. Analyses of lobar function and injury require consideration of volume, ventilation and perfusion together.
In emphysema, the increase in end-expiratory volume from loss of terminal bronchiole elastic recoil will result in a decline in lobar ventilation. The result is a drop in amount of inspired air per unit volume of the hyperinflated lobe. This reduction is represented by dividing the VENT% by the VOLUME% (lighter shaded 5th column in table 1b).
Case Study: Evaluation of Effects of Bronchoscopic Lung Volume Reduction on Differential Lobar Function Using Quantitative VQ (EMPHYSISE Study). (Continued)
In emphysema there is also pulmonary capillary destruction with loss of perfusion to diseased segments and shunting of perfusion to healthier segments. The reduction in lobar perfusion per unit volume of lung can be represented by dividing the PERF% by the VOLUME% (darker shaded 6th column in table 1b).
By multiplying the VENT%/VOL% with the PERF%/VOL% for each lobe, the product reflects the combined reduction in the concentrations of ventilation and perfusion. We have coined the term “Ventilation Perfusion Differential Index” or VQDI for this product (shaded 7th column in table 1c). The more diseased the lobe, the lower the VQDI. VQDI should mirror the lobar %emphysema in qCT.
For each voxel of a lobe, our program is capable of multiplying the quantified Technegas® activity with the quantified MAA activity. The program then sums up all voxel products within the lobe and divides the total by the volume of the lobe. The result for each lobe is compared to the sum of all lobes to be expressed as a percentage. This percentage, which we have coined the term “Ventilation Perfusion Capacity Differential Index” or VQCDI, reflects the amount of ventilated air and perfused blood per unit volume of lung parenchyma that is available for gas exchange. We contend that this is a suitable measure of lobar differential lung function (lighter shaded 5th column, table 2).
To further evaluate the efficiency of each lobe, we then divided VQCDI by the VOL%. In a heathy lobe, this ratio should be close to 1.0. In our example (darker shaded 6th column, table 2), the right lower lobe occupies 22% of total lung volume but has a VQCDI of 5%. Thus VQCDI / VOL% ratio is 0.2. In emphysema this implies that 80% of the lobe is not effectively contributing to gas exchange and could represent dead space ventilation.
Case Study: Evaluation of Effects of Bronchoscopic Lung Volume
Reduction on Differential Lobar Function Using Quantitative VQ (EMPHYSISE Study). (Continued)
TABLE 2: VQCDI AND VQCDI / VOL%.
Using our novel approach to VQ SPECT CT lobar quantification we are able to provide a pre BLVR-EBV assessment for choice of the target lobe based on the following:
VQDI: choice of lobe with the lowest value. This reflects the lobar % emphysema of qCT.
• VQDI of ipsilateral lobe: choice of target with the biggest difference in VQDI to the ipsilateral lobe. This is equivalent to seeking a 15 percentage point difference in %emphysema in qCT between the target and the ipsilateral lobes to define the presence of heterogenous emphysema.
• VQCDI: choice of lobe with the lowest value implying the least contribution to total lung function.
• VQCDI / VOL%: choice of a lobe with the lowest ratio that is well below 1.0 to indicate presence of dead space ventilation.
VOL%: choice of a lobe of substantial size. We arbitrarily chose a preference of >20%.
Emphysema, Physiology, Exercise Response (EMPHYSISE) study is a prospective multicentre trial that is being conducted at our institution. The hypothesis for this study is that BLVR-EBV treatment results in improved pulmonary ventilation, VO2max and improved pulmonary pressures and right ventricular functional parameters.
The aim of this study is to evaluate using quantitative VQ, the functional changes in the treated and untreated lobes of both lungs following BLVR-EBV in participants who were treatment responders in the EMPHYSISE study.
Method: The EMPYSISE study started recruitment in 2019 and the study is in progress.
Inclusion criteria are:
• Forced Expiratory Volume in 1 second (FEV1) <50%
• Total Lung Capacity > 100%
• Residual lung Volume > 175%
• Fissure integrity of >90% intact
• Age: >18, < 75
• Reformed from smoking for > 3 months
The exclusion criteria are:
• Co existent lung disease
• PCO2 > 60mmHg
• FEV1< 15%
• 6 minute walk test <150m
• Cardiovascular disease
• Left Ventricular Ejection Fraction <35%, MI, CVA, arrythmias
• MRI or VQ contraindicated
• Pregnancy
Participants undergo multiple investigations which include pulmonary function tests with measurements of lung volumes, cardiopulmonary exercise test, echocardiogram, cardiac MRI, St George respiratory questionnaire and 6 minute walk test.
Relevant to this study, the participants also had VQ SPECT CT lobar quantification prior to and 3 months after BLVR-EBV treatment.
Case Study: Evaluation of Effects of Bronchoscopic Lung Volume Reduction
on Differential Lobar Function Using Quantitative VQ (EMPHYSISE Study). (Continued)
The target lobe is based on a recommendation by a multidisciplinary panel consistent of interventional pulmonologists, thoracic surgeon, thoracic radiologists and a nuclear physician. Quantitative CT is used as the gold standard and quantitative VQ serves a complementary role.
Among the treatment responders, this study seeks to compare the following parameters before and 3 months after BLVR-EBV:
∆VQDI
∆VQCDI
∆ Volume %
• ∆ VQCDI / Volume %
The above comparisons were made for :
• The treated lobe
• The ipsilateral untreated lobe
• Lobes of the contralateral lung
A Mann Whitney U Rank (2 tail) test was applied. A p value of < 0.05 was considered as significant.
Treatment response was defined as:
• Lung volume reduction of >300ml
• Clinical improvement


Results:
Participants:
At the time of submission of this study, there were 22 participants recruited.
14 were excluded:
• 6 were unable or unwilling to complete tests within the trial period
• 8 had complications
4 were valve related with infection or intolerable cough
• 1 developed coincidental TB and the valves had to be removed
• 2 had collateral ventilation due to deficient fissures
There were a total of 5 participants who completed the study requirements thus far and were considered to be treatment responders. Target lobes in these participants were:
• Left upper lobe in 1
• Left lower lobe in 3
Right upper and middle lobes in 1
Target Lobes:
For the target lobes, there was a statistically significant reduction in Volume%, VQDI, VQCDI and VQCDI/Vol% (Fig 1 and Table 3)


Case Study: Evaluation of Effects of Bronchoscopic Lung Volume Reduction
on Differential Lobar Function Using Quantitative VQ (EMPHYSISE Study). (Continued)
Ipsilateral untreated lobes:
In the ipsilateral untreated lobes, there was a 52% increase in median volume% which was statistically significant (Fig 2a and Table 4).

The differential contribution to total lung function, the VQCDI, showed a 61% increase in the median value but this failed to reach statistical significance (Fig 2b and Table 4).

There was no significant change in the VQDI and VQCDI / Volume% (Fig 2c,d and Table 4)


Case Study: Evaluation of Effects of
Bronchoscopic Lung Volume Reduction on Differential Lobar Function Using Quantitative VQ (EMPHYSISE Study). (Continued)
Contralateral lung:
All parameters were not significantly changed post BLVR-EBV in the upper lobes and middle lobes of the contralateral lung. For the contralateral lower lobes there was a significant increase in volume% but the other parameters were not significantly different post treatment. (Fig 3 a-d and Table 5).

Case
Study: Evaluation of Effects of Bronchoscopic Lung Volume Reduction on Differential Lobar Function Using Quantitative VQ (EMPHYSISE Study). (Continued)



Discussion: VQ SPECT CT lobar quantification is not unique and is readily accessible from most commercial vendors. However, using our lobar quantification technique, we have devised novel indices that evaluate:
• lobar differential lung parenchymal injury with VQDI lobar differential contribution to total lung function with VQCDI
• lobar differential functional efficiency with VQCDI/ Vol%
We have used these indices to select the target lobe for treatment with BLVR-EBV. In this study we have used these indices to evaluate the functional sequelae post treatment.
Our methodology has been peer reviewed for:
• intra and interobserver reproducibility (6)
• concordance with an FDA approved commercial program (7)
concordance with qCT for BLVR-EBV target lobe choice (8)
Case Study: Evaluation of Effects of Bronchoscopic Lung Volume
Reduction on Differential Lobar Function Using Quantitative VQ (EMPHYSISE Study). (Continued)
A similar study by Pizzaro et al (9) used planar VQ quantification and showed a significant reduction in ventilation and perfusion in the treated zones. They found a significant increase in ventilation in the non-concordant zone of the contralateral lung and no significant change in the other zones. Planar quantification however lacks accuracy as the rectangular zones do not match lobar anatomy.
In our study, despite incomplete collapse of the target lobe on CT in 2 out of 5 cases (participants 4 and 5), data from our customised quantitative VQ demonstrated quantifiable changes. These were matched with robust physiological testing using other cardiopulmonary investigations as a part of the study. Thus, the functional implication of the treatment is not fully appreciated based on the structural appearance on CT post treatment.
The ipsilateral untreated lobe is expected to benefit most from improved mechanical ventilation. We found a 52% increase in median volume% which was statistically significant. There was a 61% increase in the median lobar differential contribution to lung function (VQCDI) but this did not reach statistical significance. There was no significant change in the VQDI and VQCDI/Vol%. One possible implication for the latter findings is that the increase in volume did not worsen the lobar destruction and gas trapping. Another implication is that the choice of target lobe should preference those with ipsilateral lobes that have healthier indices. The functional parameters of the ipsilateral untreated lobe is probably just as important as the target lobe itself.
In the contralateral lung there was a 25% increase in median volume of in the lower lobe which was statistically significant. In 4 of the 5 subjects the left lung was treated. Thus, this relates to the RLL. This may reflect the aerodynamic flow of the redistributed ventilation, analogous to a higher incidence of RLL in aspiration pneumonia. There were no significant changes in the other indices. There was also no significant change in all parameters in the other lobes.
The main limitation of this study is the very small sample size. The study is still in progress and preliminary results are presented. The study has been beset by a high drop out rate, which was partly due to the effects of the COVID 19 pandemic.
Conclusion: In this small preliminary study on the functional effects of BLVR-EBV treatment, we found that there was a significant functional decline in the treated lobe even when there was only a subtotal collapse that is visible on CT. In the ipsilateral untreated lobe there was a significant increase in volume. An increase in differential contribution to total lung function was also noted but this did not reach statistical significance, the small sample size maybe contributory. Of note there was no functional decline post treatment in any of the participants. In participants with treatment of a left-sided lobe there was a subsequent significant increase in volume of the right lower lobe. There was no significant functional change in all other parameters in all lobes.
Completion of the EMPHYSISE study is awaited when a more comprehensive analysis of the functional implications of BLVR-EBV treatment can be performed using quantitative VQ.
Disclosures: The EMPHYSISE study is part of Dr Fon’s PhD thesis. Funding is received from Industry Funding (PulmonX®), University of Adelaide Research Scholarship, Thoracic Society of Australia and New Zealand (SA/NT) New Investigator Award Research Grant, Thoracic Society of Australia and New Zealand (SA/NT) ASM 3-minute thesis Research Grant.
Approval of this study was granted by the Central Adelaide Local Health Network Human Research Committee (reference number: HREC/18/CALHN/389).
References
1. Lumb A. Nunn’s Applied Respiratory Physiology. 8th ed: Elsevier; 2017.
2. West J. Pulmonary Pathophysiology. 8th ed2013.
3. Klooster K. et al Endobronchial Valves for Emphysema without Interlobar Collateral Ventilation. NEJM 2015; 373 : 2325 – 2335
4. Sciurbia F. et al. A randomized study of endobronchial valves for advanced emphysema. NEJM 2010; 363: 1233 – 1244
5. Davey C. et al. Bronchoscopic lung volume reduction with endobronchial valves for patients with heterogeneous emphysema and intact interlobar fissures (the BeLieVeR-HIFi study): a randomised controlled trial. Lancet 2015; 386: 1066–73
6. El Barhoun E. et al. Reproducibility of a semi-quantitative lobar pulmonary ventilation and perfusion technique using SPET and CT. Hell J Nucl Med 2017; 20(1): 71-75
7. Chew C. et al. Validation of RAH VQ SPECT/CT lobar quantification program using a modified version of GE Q lung. Hell J NuclMed2023;26(1):9-19
8. Tee V. et al. Use of Ventilation-Perfusion Single-Photon Emission Computed Tomography to Select the Target Lobe for Endobronchial Valve Lung Volume Reduction. Respiration 2021;100(9):886-897. doi: 10.1159/000515336.
9. Pizzaro C. et al Effect of Endobronchial Valve Therapy on Pulmonary Perfusion and Ventilation Distribution. PLOS ONE | DOI:10.1371/journal. pone.0118976 March 30, 2015








Annual reports available to download with your A endoPlus mobile app.


National and overseas industry conference presentations and webinars.


Contributions from local and world experts.
Resources include webinars, case studies, online seminars and more.
Visit nucleus.anzsnm.org.au/edutrace/home

Access from any device, anywhere at any time.



VALE DR WILLIAM (BILL) BURCH
- THE INVENTOR OF TECHNEGAS
Sir Isaac Newton is attributed with having said “If I have seen a little further it is by standing on the shoulders of Giants.” It is said that he paraphrased a translation of John of Salisbury’s 1159 statement: “We are like dwarfs sitting on the shoulders of giants. We see more and things that are more distant than they did, not because our sight is superior or because we are taller than they, but because they raise us up and by their great stature add to ours.” His statement is commonly understood to be a metaphor for how knowledge grows.
Dr William (Bill) Burch, like Newton, was a physicist. He was born in Wellington, New Zealand on the 13th of November, 1938 and he lived a truly exemplary “giant’s” life. Intuitively, he understood things others never could and he built his knowledge by experimentation based on the solid foundations of his observations.
From an early age, experimentation was always part of Bill’s raison d’être. Bill was a Scorpio. And, typically of all Scorpios, he was hard working, ambitious, intuitive, a born winner and most important of all “possessed of strong intuitive powers”. Aged just 12, he ignited a tin of flashpowder which removed the skin of his hand and one of his eyebrows much to the chagrin of his mother!
While Bill did many things in his productive life, such as his time as Observatory Geophysicist to Wilkes Base in Antarctica in 1990, his passion for helping people drew Bill into nuclear medicine in various hospitals in Australia and the United Kingdom. From 1968 to 1973 Bill worked as Deputy Principal Physicist at St Thomas’ Hospital in London. During this time Bill was undertaking research for his PhD. It was an important time in his life and led to furthering his interest in nuclear medicine.
This eventually saw Bill appointed as a physicist at The Canberra Hospital in May 1973. There, George Taplin’s “Lung Imaging in Pulmonary Disease” inspired Bill on the quest to find a ventilation agent capable of producing images truly congruent with their perfusion counterpart. Bill had noticed the efficiency with which smoke particles penetrated into the alveoli of the lung and he felt that this property could be exploited to diagnose pulmonary embolism (PE). In a truly inspirational original thought, Bill began searching for a method to produce radioactive smoke! The genius in Bill’s approach was to use so little material that it is chemically insignificant and delivered significantly less radiation dose to the patient from alternative radiological procedures.
Thus, almost eight years later in 1985, one night Bill “stumbled” across Technegas. For almost 40 years Technegas has remained the pre-eminent ventilation agent in a V/Q lung scan. There are not many products that can lay claim to such longevity.
Over 4 million patients globally have had the benefit of Technegas. Countless patients’ lives have been saved through the early and accurate diagnosis of PE leading to initiating effective treatments, all thanks to Bill.
The development of Technegas must rate as one of Australia’s biggest contributions to global nuclear medicine practice up there with [ 99mTc]-phosphonates for bone scanning (Boyd, AAEC (ANSTO), 1970), filtered back-projection image reconstruction (Bracewell, ANU, 1956) and OSEM iterative reconstruction (Hudson & Larkin, Macquarie University, 1994). Just to show how advanced the Canberra group’s thinking was at the time, Chris McLaren, a technologist in the group where Bill was testing Technegas, presented a paper on V/Q lung scanning at the 1986 ANZSNM ASM using (a) Technegas, (b) SPECT for both V & Q, and (c) ventilation subtraction from the perfusion reconstructions to give a V:Q quotient image .
That is now almost 40 years ago, while the first clinical site in the US to implement Technegas is just starting in this 2nd week of 2024!

VALE DR WILLIAM (BILL) BURCH - THE INVENTOR OF TECHNEGAS (Continued)
In Bill’s own words, he wanted to make science fun and relevant especially to his younger audience. He put his words into action at Questacon in Canberra, where he was Manager of the exhibit for several years.
I met Bill for the first time at ANSTO in the 1990’s when Bill was head of the Radiopharmaceuticals Research team. Over the years, Bill had become disillusioned with the lack of foresight of the owners of the Technegas technology and he left the company. It is only in recent times that suddenly the penny has dropped and alternate applications for Technegas in pre-surgical evaluation of regional lung function, asthma, pneumonia, COPD, emphysema, right heart failure and more been explored. This point was disappointing to the hard-working individual Bill, who was always striving for excellence and an improved method to help people.
Bill and his team at ANSTO worked on research projects in diagnostic biomarkers for cancer and neurological disorders such as Alzheimer’s and Parkinson’s disease.
Those of us lucky to hear Bill’s Lowenthal Lecture at the ANZSM Annual Scientific Meeting in Darwin in 2011 learned about some of the shenanigans which accompanied the development of the Technegas generator, many of which which would not be acceptable today. Despite already being diagnosed with Parkinson’s disease, Bill delivered an unforgettable lecture which had the audience in stitches but also provided them with great insight into his thought processes.
Bill went on to meet his Maker on the 5th of December, 2023, aged 85. His life was full of achievement and devotion to the improvement of life for humanity.
Few of us will look upon Him on judgement day and be able to say, “Hey Lord, I did that. I saved hundreds of thousands of lives because of what I invented.” Bill, however, can claim this.
Ironically, Bill was afflicted with Parkinson’s Disease himself, a project he and his team at ANSTO had been researching. His usual thoroughness in understanding and research into any project he was working on would have meant that he was more aware than most of the prognosis. For the past few years of his life Bill fought the good fight. He was constantly emailing me with “thought experiments” during the COVID pandemic. He designed experiments to diagnose black lung disease and measure lung damage and recovery in long-COVID patients. This was at a time when he could not communicate verbally, but all using Technegas as the investigative agent.
It is hard to know how far the implications of Bill’s original invention will go.
I will miss his wise council, original thinking and sound advice.
Vale, my friend.
Charles F Buttigieg MSc BSc(Hons) MANZSNM
EDUTRACE - LATEST PRESENTATIONS




ARTnet Project Coordinator
The Australasian Radiopharmaceutical Trials network (ARTnet) is a collaborative network incorporating medical specialists, technologists, scientists and researchers from the field of Nuclear Medicine and Molecular Imaging with a shared interest in multicentre clinical trials that utilise radiopharmaceuticals for imaging or therapy.
Applications Close: 24 March 2024
Expression of Interest TSIG Student Representative Council
Expressions of interest are sought from ANZSNM Student members to join the Student Representative Council (SRC) working group.
Applications Close: 17 March 2024






PRESIDENT
Dr Kevin London (NSW)
Vice President
Prof Karen Jones (SA)
Immediate Past President
Dr Daniel Badger (SA)
Treasurer
Ms Suzanne McGavin (VIC)
COMMITTEE
Ms Prudence Burns (NZ)
Mr Christian Testa (VIC/TAS)
Mrs Victoria Sigalas (SA/NT)
Ms Rosemary Dallen (WA)
Mrs Prudence Burns (TSIG)
Dr Nigel Lengkeek (RPS)
Prof Andrew Scott (IRC)
SPECIAL INTEREST GROUPS/COMMITTEES
Technologists
Chair: Mrs Prudence Burns
Radiopharmaceutical Science
Chair: Dr Nigel Lengkeek
Physics
Chair: Mr George McGill
Quality and Technical Standards Committee
Chair: Dr Darin O’Keeffe
Scientific Advisory Panel
Chair: Prof Dale Bailey
International Relations Committee
Chair: Prof Andrew Scott
BRANCH SECRETARIES
New South Wales/Australian Capital Territory
Dr Kevin London (Chair)
Queensland
Ms Neena Sunny and Mr Joel Williams
South Australia/Northern Territory
Ms Alessandra Caretti
Victoria/Tasmania
Ms My Linh Diep
Western Australia
Ms Georgina Santich
New Zealand
Ms Trish Mead
Archivist
Ms Debra Huddleston
GENERAL MANAGER & SECRETARIAT
All Correspondence
Mr Rajeev Chandra, General Manager
ANZSNM Secretariat, PO Box 6178, Vermont South, Victoria 3133
Tel: 1300 330 402 | Fax: (03) 8677 2970
Email: secretariat@anzsnm.org.au
AIMS AND OBJECTIVES OF THE AUSTRALIAN AND NEW ZEALAND SOCIETY OF NUCLEAR MEDICINE
1. Promote:
• The advancement of clinical practice of nuclear medicine in Australia and New Zealand;
• Research in nuclear medicine;
• Public education regarding the principles and applications of nuclear medicine techniques in medicine and biology at national and regional levels;
• Co-operation between organisations and individuals interested in nuclear medicine; and
• The training of persons in all facets of nuclear medicine.
2. Provide opportunities for collective discussion on all or any aspect of nuclear medicine through standing committees and special groups:
• The Technical Standards Committee sets minimum standards and develops quality control procedures for nuclear medicine instrumentation in Australia and New Zealand.
• The TSIG Committee is the group overseeing the Technologist Special Interest Group (TSIG) and ensures that all projects, committees and activities of the TSIG align with the values and strategic plan of the ANZSNM. It reports directly to the ANZSNM Federal Council and oversees the two TSIG working groups: CPD & Education Working Group and Technologist Workforce Advocacy Working Group. The committee is able to form working groups to perform specific tasks as required to provide opportunities for the benefit of Technologist members of the ANZSNM after consultation with the ANZSNM Federal Council.
• The Radiopharmaceutical Science SIG and a Physics SIG that maintain standards of practice for their particular speciality and provide a forum for development in Australia and New Zealand.

