The
the Association of Salaried Medical Specialists | ISSUE #139 | JUNE 2024 WORKING ON OUR MENTAL HEALTH MINISTER MATT DOOCEY TALKS WORKFORCE PLANS P.06 CME OFF BALANCE WHAT IS TE WHATU ORA DOING TO MAKE CME EASIER TO TRACK P.12 SMOKE AND MIRRORS ASSOCIATE MINSTER OF HEALTH TALKS TOBACCO REFORM REPEAL P.16
Magazine of
ISSUE #139 JUNE 2024
This magazine is published by the Association of Salaried Medical Specialists and distributed by post and email to union members.
Executive Director: Sarah Dalton
Magazine Editor: Andrew Chick
Journalist: Matt Shand
Designer: Twofold
Cover Image: Shutterstock
The Specialist is produced with the generous support of MAS.
WANT TO KNOW MORE?
Find our latest resources and information on the ASMS website asms.org.nz or follow us on Facebook and Twitter.
Also look out for our ASMS Direct email updates.
If you have any feedback on the magazine or contribution ideas, please get in touch at asms.org.nz
PREFER TO READ THE SPECIALIST ONLINE?
We have listened to your feedback and are aware that some members prefer not to receive hard copies of the magazine.
If you want to opt out of the hard copy, just email membership@asms.org.nz and we can let you know via email when the next issue is available to read online.
ISSN (Print) 1174-9261
ISSN (Online) 2324-2787
The Specialist is printed on Forestry Stewardship Council® (FSC®) certified paper.
Proposed position for FSC logo and text. Please align to bottom of this margin.

The Specialist talks with the first Minister of Mental Health Hon Matt Doocey about emergencies, workforce and filling his boots.

The Specialist speaks to Associate Minister of Health Casey Costello about why she believes repealing world-leading legislation will still allow New Zealand to be smokefree by 2025.
UPFRONT 02 The more things change, the more they stay the same 03 Rates, recruitment, meetings and ministers IN BRIEF 33 Anatomy of a health crisis 34 Overcoming phobias with virtual reality 34 In the media 34 Branch Officers Hui 35 Mental health groups call for urgent investment in open letter to Minister 35 Moral injury amongst the wards 36 Paid union meetings for Te Whatu Ora staff 36 New National Secretary selected 36 Kenepuru clarification 06 The flying doctor 08 ASMS ELECTION: Results | Cliff notes | Seeding change 12 Off balance FEATURES 20 Ashes in my mouth 22 Where there’s smoke… 23 Flatline for transparency 26 Patients and penguins 28 Medal-winning medicine 30 Passing the test 04 PROFILE: MATT DOOCEY Working on our mental health
16 PROFILE: CASEY COSTELLO Smoke and Mirrors
JUNE 2024 PAGE 1
THE MORE THINGS CHANGE, THE MORE THEY STAY THE SAME
KATIE BEN, ASMS PRESIDENT

Kia ora! It is a privilege to write my first column as the new National President of ASMS, and an honour to bring my own flavour to the leadership of the National Executive.
We face continued change in our health service, within our localities, and within our hospitals.
The ASMS National Executive is, likewise, changing. We have a new set of executive members, following the retirement of some very long-standing members.
We have started our journey towards embodying our Toi Mata Hauora identity, and welcome Rudi Johnston and Mark Lawrence to the team as our first Māori representatives.
Welcoming the new invariably means saying farewell to those who have left. It is with much gratitude that I thank our retiring executive members Julian Fuller, Seton Henderson and Nathalie de Vries for their hard work, imagination and contribution to the governance of ASMS over many years.
I would also like to thank Julian Vyas for his mahi over the last three years and I am grateful for his continued involvement as our immediate past president.
In amongst all the change, however, much remains the same.
We still try to hold together a health service that is understaffed and under resourced. We still try to hold governments to account for a fully accessible public health service which serves the needs of all New Zealanders in equitable ways.
We, again, face bargaining this year as we strive to improve the terms and conditions for all our members.
What will I bring to the kōrero? I bring a passion for fairness, justice, and for equity. No doctor left behind! I drive towards a transparent and fair remuneration system across the health sector. A system where no one group benefits to the detriment of their colleagues.
This will take time and energy, and I ask for your patience while we work on unravelling the web of different conditions that have developed around the country.
I bring a strong ethical focus, and a drive for equity of health outcomes for all New Zealanders regardless of demographic or socioeconomic background.
And what do I ask for from you? To keep the conversation flowing. To let us know how things look in your workplaces and where ASMS can help. To show up to the local meetings and engage with management on the local issues that matter to you.
Please continue to be a part of the ASMS narrative and to contribute to the collective cohesion that underpins all we do.
Over the next three years, I hope to continue the work of my predecessors to keep ASMS an engaged, responsive union with the interests of its members at its heart.
This cannot be done without the assistance of all the amazing staff at ASMS and the hard work of Sarah Dalton our Executive Director.
It is thanks to these people that what is important – our dedication to our members and the health system – will not change, and that those changes which are needed, will happen.
I look forward to our ongoing relationship, and to being a part of this fantastic organisation.
Let us know how things look in your workplaces and where ASMS can help.”
PAGE 2 THE SPECIALIST
RATES, RECRUITMENT, MEETINGS AND MINISTERS
SARAH DALTON, EXECUTIVE DIRECTOR
First, I would like to thank the nearly 2,500 Te Whatu Ora members who took time complete our claims development survey in May. We are sifting through the data and will present our findings at the paid union meetings being held across the country between June 29 and July 25.
More information about those meetings is available on page 36 of this issue and on our website at asms.org.nz/events. We will also email each member about the meetings in their district closer to the time.
If you can’t make it in person, we will also run online meetings on 25, 26 and 30 July.
Winter rates
As we head into winter it’s great to have national minimum rates agreed for additional duties. These are an extension of and an improvement on the previous winter rates agreement. Please be proactive in seeking their application. If your service is down on SMO and/or RMO numbers, make sure these rates are approved.
While they are not the best response to shortstaffing, they are a recognition that you are working short.
All of your extra work burden needs to be documented, and it needs to be acknowledged and remunerated.
We know that the longer-term solution is based on improved retention and recruitment based on improved data and planning. But we also know that Te Whatu Ora is not there yet.
Meeting with ministers
Encouragingly, in terms of that planning, we have had clear signals from the Minister of Health that he wants to see more medical students, more trainees with more opportunities to train, and an SMO workforce that is appropriately supported to provide the training and supervision those future specialists need.
It’s early days, but following ASMS’ meeting with Dr Reti in late May we will be going back seeking rapid (and funded) development of improved and increased training pathways.
We have also met with the new Minister of Mental Health. Matt Doocey is taking his role seriously, which is just as well. As the recent open letter from the college of psychiatrists (co-signed by ASMS) makes clear – the specialty faces a range of extremely challenging workforce pressures right now.
Working together
ASMS is also proactively partnering with other unions – in particular, NZNO – where there are shared concerns around staff and patient safety. We have work underway at Kenepuru Hospital

and expect to develop a shared approach to the various health and safety issues at MidCentral.
We are also deeply concerned about public service cuts. Following on from austerity measures that saw downward pressures on pay and conditions over the last several years, they make it even more difficult to retain and recruit staff.
Contrary to the rhetoric, we have countless depressing examples of cuts to frontline health services, clinical roles that are not being filled, agreed service-sizing increases that are not making it into current budget cycles, and a lack of commonsense, timely approaches to succession planning and securing recently qualified specialists.
We will keep working hard to push back against this short-sighted penny-pinching, but it will be an uphill battle. When these issues impact on you, make sure your local industrial officer is looped into key discussions. We are in a better position to help when we know what’s going on.
Kia kaha koutou — and I’ll see many of you at the paid union meetings in July.
Contrary to the rhetoric, we have countless depressing examples of cuts to frontline health services.”
JUNE 2024 PAGE 3
WORKING ON OUR MENTAL HEALTH
Triple one calls could see fire, police, ambulance and mental health as emergency options if Minister for Mental Health Matt Doocey’s plan comes to fruition.
“I think it’s about time we had a fourth option,” he says. “You could get triaged by a crisis counsellor who might be able to support you or deescalate you over the phone. Based on your situation, you might have police or mental health respond to the call.”
Pilot programmes run in Wellington have shown the concept has some promise.
“There was a 30 per cent reduction in emergency department presentations [for mental health] and a 30 per cent reduction in admissions that following month for the individual.
“If you call 111 at the moment with a health issue you get an ambulance. If you call with a mental health issue you get a criminal justice response, which is a police officer.
“We’re lucky to have police filling this role, but if we look at what is happening in the United Kingdom at the moment, the Metropolitan Police issued instructions they will no longer attend mental health callouts.
But the Minister acknowledges the key challenge to this or addressing any mental health issue in New Zealand is workforce.
“I think our mental health and addictions services are in a fragile state,” he says.
“I think we need to support them to become more sustainable. There is an increasing demand for mental health and addiction services. That’s why, for me, we’ve got to shift the focus towards prevention and into early intervention.
“I hear the workforce tell me they are up for that. If we start shifting towards prevention and early intervention, we can make a real difference.”
Doocey sees his role as the first Minister for Mental Health is to create the infrastructure to curb the growing workforce vacancy rates, improve equity of access and find ways to keep the workforce in New Zealand.
“Workforce is the biggest issue,” he says. “That is the priority for me.”
“I visited a community adolescent service that has a 50 per cent vacancy rate. This is the reality – people cannot be seen in a timely manner or get stuck on waiting lists.”
While other ministries have established infrastructure, mental health does not.
“I’m having to set that up for the first time,” Doocey says.
“I am very fortunate to know Dr Shane Reti well and we work well together.
“We don’t want to take the $2.4 billion mental health infrastructure out of the wider health plan. Then things become more siloed. We’re building up the systems that are part of Vote Health but the exciting part is the crossdepartment work – what are we doing about mental health in the Department of Corrections or Ministry of Education – we are saying ‘How can we work together to actually add more value to what mental health is providing in your areas?’ Then we can join this up with a whole of government health strategy.”
The Minister sees establishment of a workforce plan, specific to mental health, as a key piece of work.
“It kind of beggars belief that we’ve got this far in mental health without a mental health workforce plan,” Doocey says.
“Because there was no plan, new roles ended up cannibalising existing workforce roles, so the workforce was just spread, and large, clear gaps eventuated.
“I’m in the planning stage now to have a specific mental health workforce plan targeted to reducing vacancy rates.
“Currently we are looking at about a 19 per cent vacancy rate for Health New Zealand psychiatry roles. I think psychology is about 12 or 13 per cent. We need to make sure that, when we look at our overall training plan, it should focus on how it reduces vacancy rates.”
“We need to grow a locally trained workforce. In clinical psychology we only train 50 a year. That is a constraint. I am working with the Tertiary Education and Skills Minister to see how we work with universities to open up that funnel and increase the number of clinical placements. I think we can increase that to 100 and then keep increasing it.”
But how does he plan to get those trained in New Zealand to stay in New Zealand to work?
“Terms and conditions are going to be absolutely vital,” he says.
“One of the biggest conditions we need to sort at the moment is there are too many professionals covering vacant roles. That leads to burnout. We have some ability to cover roles through migration and I think we should ensure people want to come to New Zealand to work. But I do not see skilled migration as the silver bullet.”
PAGE 4 THE SPECIALIST
The Specialist talks with the first Minister of Mental Health Hon Matt Doocey about emergencies, workforce and filling gumboots.
Doocey says the current restrictions on who can be selected for clinical placements is causing people to leave psychology.
“There will be about 400 people who graduate and have undergraduate degrees in psychology, and if they miss out on those 50 places the data shows they disappear,” he says.
“We are working with universities to form a new registration system to pick these people up and put them in new roles within the health system. We need to do things differently. I am going to trial new stuff.”
Getting “money out of the Beehive” and into community organisations and NGOs will form part of the long-term strategy once the plan has been established, but he admits that “announcing money is the easy part”.
“The trap the last Government fell into [with its $1.9 billion investment into mental health] is that announcing the money did not mean the services will be grown on the ground.
“When it came to finding the workforce to open those new services, that’s where things fell over. The issue with the $1.9 billion was it was said to be for mental health but, if you unpack it, a large portion wasn’t. Yes, it went to other departments – the state abuse enquiry, housing and corrections – and that is fine, but people were disappointed it did not go directly to mental health services.”
Since taking the job Doocey has made his own spending announcements. Most recent is a $24 million investment into the charity I Am Hope, founded by Mike King, to provide youth counselling sessions.
How will this be different?
“What we’ve said is we actually need to get money out of the Beehive as a large portion of the last Government’s money got trapped in bureaucracy,” Doocey said.
“We need to get the money into the grassroots organisations that are already delivering.
“There is real potential to upscale the NGOs and community services. When you look at Gumboot Friday, as an example, Mike King has around 400 professionals accredited and vetted on his platform that are available to go and now he can add another couple of hundred.
“Now he’ll be able to scale up, literally overnight, to increase that by another 15,000 young people accessing that service.”
Doocey says he will measure his success in the role by the appetite from future governments to keep the ministerial position alive.
“The measure will be that when there is a change in government, because governments come and go, the incoming government will say, ‘that worked’. I’ve been of the view you need to have a dedicated minister who has the time and energy to get into the detail of the issue of mental health and help drive it forward.”

It kind of beggars belief that we’ve got this far in mental health without a mental health workforce plan.”
– MATT DOOCEY
PROFILE
JUNE 2024 PAGE 5
I want to see greater engagement with members and actively seeking members’ opinions and feedback on the wider ASMS strategy, particularly around bargaining and the SECA.”
– KATIE BEN

THE FLYING DOCTOR
MATT SHAND, JOURNALIST
PAGE 6 THE SPECIALIST
OF WORKING IN PUBLIC HEALTH.
Ensuring assisted dying is as dignified as possible is a particular driver for newly elected ASMS
President Katie Ben. And flying is one of her passions.
“I voted against the assisted dying bill. Not because I do not agree with the concept, but because I did not agree with the legislation around it,” Ben says.
“After it passed, I knew that – if it was going to happen – I would provide it so I was comfortable with how it was being done for my patients.”
Every few weeks Ben makes a trip to the West Coast, which would normally be a fiveto six-hour drive but, due to owning her own aeroplane, can be made in just under two hours.
“The drive is long. I thought it would be better to fly. I have always had a passion for flying, which I have done for 25 years.
“There are a lot of similarities between being an anaesthetist and flying an aeroplane.
“Also, being 5,000 feet up is extremely good for my mental health, clarity and stress. And it allows me to bring a needed service to the isolated West Coast and be with people at a critical time.”
Ben says the experience of assisting people in their final stage of life’s journey is extremely humbling.
“You get to hear the fantastic stories and you get to see people in their home, surrounded by life. Not in a day-stay situation,” she says.
“You are reminded they are husbands, grandads, wives, mothers, and grandmothers and have had the most amazing journeys. It is a strong reminder that patients were not always 85-year-

olds dying of cancer but people who led strong, interesting, and amazing lives.”
Ben says the legislation around who can administer assisted dying and what checks need to be undertaken before the procedure is administered need to be strengthened.
“I always have initial conversations with the patient and then speak to their wider medical network, such as GPs and oncologists, to get an understanding of where the decision to end their life comes from and if it is a surprise to those professionals.
“At the moment there is no requirement to do that.”
Her passion for rights goes beyond the patient to the health practitioners.
“It’s not my quote but we [senior medical officers] are the team of 5,000 looking after the team of 5 million,” she says.
“Mental health and the wellbeing of our medical workforce are very important, and we need to encourage doctors to talk more to manage our high-pressure work.
“One of the reasons I put my hand up to be a branch president all those years ago was to be part of a change, and I’ve put my hand up now to continue being part of the change as ASMS President. I think I can bring a lot to the role.
“I first joined ASMS in 2009 after arriving from the United Kingdom. I remember being asked if I had joined the union yet and I asked if I should.
I was wary coming from England where the unions are not held in such high regard as they are here.”
Ben first became a branch officer in Nelson and has sat on the National Executive representing Region 4 for the last six years.
“I am at the stage of my life and career where I feel I can really make an impact in the role of ASMS President,” she says. “Having the last three years on the Executive has allowed me a lot of time to grow and learn how things are done.
“A lot of what I want to achieve is already on the agenda for ASMS to complete. Things like streamlining the meetings and creating more objective outcomes measuring the work ASMS does and including members in those discussions.
“I want to see greater engagement with members and actively seeking members’ opinions and feedback on the wider ASMS strategy, particularly around bargaining and the SECA.
“I want to see continued work promoting a safe public health system for everyone and hold the Government to account to provide this.
“Striving for equity of outcomes and levelling the field in terms of terms and conditions for SMOs across the country should be a priority. We do not want to see access to health care for patients restricted by geographical or economic barriers.”
MAIN IMAGE: ASMS PRESIDENT KATIE BEN TAXIS TO THE RUNWAY AT NELSON AIRPORT AMID HER UNUSUAL COMMUTER VEHICLE. RIGHT: ASMS PRESIDENT KATIE BEN SAYS FLYING IS A WAY TO UNWIND FROM THE STRESS
JUNE 2024 PAGE 7
ASMS ELECTION RESULTS
THE 2024 ASMS NATIONAL EXECUTIVE ELECTIONS HAVE BEEN COMPLETED.
The Executive is made up of 13 members. The President and Vice President are elected nationally. Two representatives of Te Mauri Taurite are selected at a national hui, and two representatives are selected regionally by each of four regions. The immediate past President fills the final place.




• Region 1: Te Tai Tokerau; Waitematā; Te Toka Tumai; Counties Manukau
• Region 2: Waikato; Hauora a Toi; Lakes; Tairāwhiti; Taranaki
• Region 3: Whanganui; MidCentral; Te Matua a Māui; Wairarapa; Capital, Coast and Hutt Valley
• Region 4: Nelson Marlborough; Waitaha; Te Tai o Poutini; South Canterbury; Southern
New President Katie Ben and Vice President Sylvia Boys were elected unopposed. Mark Lawrence and Rudi Johnson were selected at the hui-ā-motu in Tauranga in February (see page 10 for details).
All the regional executive positions required an election, and the results were as follows:


REGION 1
Received a total of 508 valid votes.
The successful candidates: Andrew Ewens and Keat Lee (both Waitematā)


REGION 3
Received a total of 317 valid votes. The successful candidates: Kai Haidekker (Te Matua a Māui) and Tanya Wilton (Capital, Coast and Hutt Valley).


REGION 2
Received a total of 246 valid votes. The successful candidates: Felicity Dumble (Waikato) and Andrew Robinson (Lakes).


REGION 4
Received a total of 320 valid votes.
The successful candidates: Tom Morton (Nelson Marlborough) and Geoff Shaw (Waitaha).
The overall turnout was 22.84 per cent, with 1,398 valid votes cast from 6,119 eligible members. Julian Vyas is the immediate past President of ASMS.
KATIE BEN
L TO R: ANDREW EVANS, KEAT LEE
L TO R: FELICITY DUMBLE, ANDREW ROBINSON
L TO R: KAI HAIDEKKER, TANYA WILTON
L TO R: TOM MORTON, GEOFF SHAW
SYLVIA BOYS MARK LAWRENCE
INAUGURAL MĀORI REPRESENTATIVES
ASMS ELECTION PAGE 8 THE SPECIALIST
RUDI JOHNSON
As doctors we are respected members of the community and can act as community champions .”
– SYLVIA BOYS
CLIFF NOTES
MATT SHAND, JOURNALIST
Newly elected national Vice President and Counties Manukau ED doctor Sylvia Boys thinks it’s time for doctors to speak up.
Self-described “bottom of the cliff” doctor Sylvia Boys says it is time doctors use their collective voice to speak up for a system in crisis and secure safety nets at the top of the cliff – to aid patient and practitioner alike.
Boys is ASMS’ new vice president and says her experience working in the United Kingdom during her OE in 1997 shaped her commitment to doctors unions. This led to her becoming a branch president in Counties Manukau, before joining the National Executive last triennium.
“Coming from the UK I saw first-hand the mess that occurs when doctors work without having their rights protected,” she says.
“There is often an aversion to doctors speaking up for themselves, and it is important we use our collective voice, and strength, to ensure New Zealand does not succumb to the same pitfalls as the UK did.”
“Doctors play a critical role advocating for the public health system,” she says. “This will require work outside the bargaining table.
“I think there is a lot ASMS can achieve for doctors and patients, but we must be cognitive of our sphere of influence.
“At present, our main sphere of influence is collective bargaining and remuneration and, unfortunately, contract negotiations are not the ideal place to address the day-to-day issues SMOs face.
“It is certainly one lever we can use but, when we are dealing with a crisis, more is needed. We are faced with very real SMO burnout and despair. We must use all our levers to push the employer for better work conditions and to support clinicians to do their jobs effectively or we will see a cycle of SMOs leaving.”
Boys also has a degree in population health and wants to see more measures taken by government to increase social health as well as limit the commercial determinants of harm.
“We are not prepared for the increased ageing of our population,” she says.

“Preventable diseases put a lot of pressure on the already stretched health system. We have seen the current Government repeal smoking legislation, which would have curtailed a product that does amongst the most harm. As a result, we will be faced with more preventable disease and pressure on our health system.”
Boys advocates for doctors to use their voices, both through ASMS as part of the union and as respected individuals within their communities, to advocate for change.
“As doctors we are respected members of the community and can act as community champions,” she says.
“It will be great for SMOs to get involved, visit their MPs when able, and let the power brokers know the real story as to what is occurring in health care workplaces.
“I want to see members empowered to speak up and fight back against the culture and stereotype of the ‘stoic doctor’– silent and suffering through. We need people to hear about the shortages and prevent the active dissuasion that Te Whatu Ora undertakes.
“This will have real benefits to patients long term.”
JUNE 2024 PAGE 9

SEEDING CHANGE
MATT SHAND, JOURNALIST
ASMS’ election of two Māori representatives to the National Executive is set to sow the seeds of cultural safety and representation for future generations of Māori doctors.
At ASMS’ annual conference last year, changes were ratified that embedded the principles of Te Tiriti o Waitangi in the union’s constitution.
This year ASMS held its inaugural hui-ā-motu at Maungatapu Marae (Ngāti Hē) in Te Moana a Toi-te-Huatahi Bay of Plenty on 23 and 24 February. At the hui, Te Mauri Taurite elected two representatives for the National Executive.
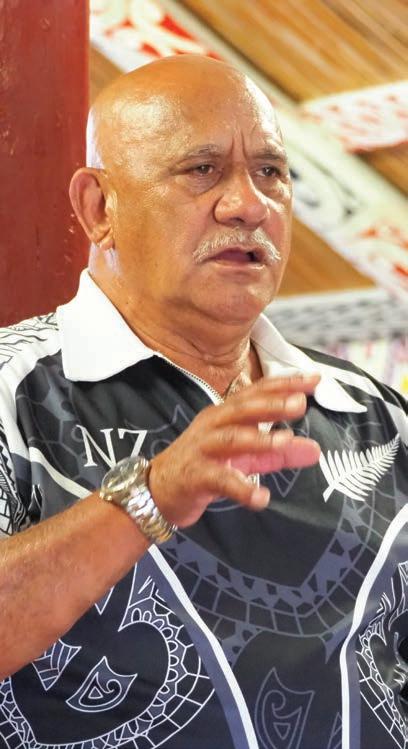
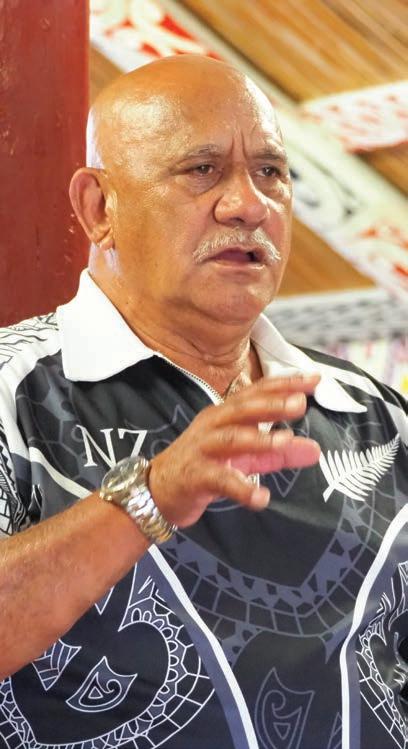
Māori doctors and dentists from across the country attended the hui, electing psychiatrist Mark Lawrence and dentist Rudi Johnson by unanimous vote.
The hui was an opportunity for connection through whakawhanaungatanga – the building of relationships, collaboration on the strategic direction of Te Mauri Taurite, and celebration of te ao Māori, tikanga, te reo and waiata.
In reflecting on their journeys, several members spoke about the importance of the University of Auckland’s Māori and Pacific Admission Scheme (MAPAS) and the University of Otago’s Te Kauae Parāoa policy, which recognise the need for Aotearoa to have a health workforce that reflects the population it serves.
Many spoke of their mentors who had supported them through navigating the challenges of medical school.
“Medical school was not a happy time,” newly elected Māori representative Lawrence says.
“I didn’t feel like I deserved to be there, so getting through was tough.”
Because of this experience, establishing culturally safe structures within unions and professional groups that represent doctors and dentists is something he thinks is particularly relevant to support future generations of SMOs.
“It is important to conduct this work now as about 20 per cent of medical students are now Māori,” Lawrence says.
“What ASMS has done is create a co-governance structure and a strong commitment to Te Tiriti o Waitangi. Not just giving it lip service. This action gives Māori the authority to have their own voice and to determine their direction.
“It will take five or ten years for the impact of this governance shift to filter through to the next generation of Māori doctors and, in the meantime, we will give a strong voice on their behalf.”
Fellow Māori executive member Rudi Johnson echoes this sentiment. She refers to the inaugural Māori executives as being kaitiaki of the position and responsible for keeping it in trust.
ASMS ELECTION PAGE 10 THE SPECIALIST
TOP: ASMS KUIA MARAMA REWETI-MARTIN. BOTTOM: ASMS KAUMATUA TE PONA MARTIN.

“It is exciting to be here at the start of this change,” she says.
“I see our role as a placeholder for the wave of Māori doctors who are about to come through the ranks and deserve to have their voice heard in a safe space.
“Toi Mata Hauora is carving a way forward regarding cultural competency that will assist everyone. We have a kaumatua and awareness of tikanga. Positions like this, and the voice it brings, go a long way to normalising health care as a career.
“When I grew up, being a doctor just was not in the realm of possibility. I had labourer parents –shearers – and it did not seem achievable.
“I want future tamariki to see medicine as a normal opportunity that can be explored and entered into.”
Following the election, members wasted no time talking strategy and establishing workplans that will benefit Māori members. The meeting was facilitated by ASMS’ Kaumatua and Kuia, Te Pona Martin and Marama Rewiti-Martin, who also composed and gifted ASMS a waiata ahead of the hui. (See side panel “Te Mauri Taurtie”.)
Lawrence says the change in government means ASMS, and others, need to take a stronger role in public health and equity advocacy.
“The National Party has already talked about scrapping MAPAS, the very programme which
enabled many Māori doctors at the hui to enter medical school.
“It highlights how decisions made today make generational change, the Hui-a-Motu would have had far less attendance had MAPAS not existed.
“We [all doctors] are struggling with similar issues, from lack of beds to a lack of colleagues,” Lawrence said.
“We must find ways to tackle these issues.”
ASMS Executive Director Sarah Dalton says the election of ASMS’ first two Māori executives represented a “momentous day” for ASMS and is the culmination of years of work from staff.
“When I was interviewed for the job as Executive Director, I said I wanted to bring equity kaupapa to the forefront,” she says. “I consider by giving me the job the Executive also agreed.
“It has not been easy. Change never is easy. But this measure goes a long way towards our goal of always trying to leave ASMS better than when we found it.
“As unions we love to celebrate how we can achieve more when we stand together than when we stand as individuals. Here we plant the seeds for future change.
“Seeds that will grow ASMS into a stronger union, a collective union and a stronger voice for Māori health professionals for generations to come.”
LEFT: ASMS STAFF COMMEMORATE THE ELECTION OF MARK LAWRENCE AND RUDI JOHNSON AS INAGURAL ASMS MĀORI REPRESENTATIVES.
BELOW: ASMS ARE WELCOMED ON TO MAUNGATAPU MARAE IN TAURANGA.

TE MAURI TAURITE
Tū mai ana Te Mauri Taurite
Hei raukura o Toi Mata Hauora e Tauawhi ana, poipoi rawa ana Kia whai hua mai, te toiora e
Chorus
Pūmau ki te aroha
Pūmau ki te oranga
Pūmau ki te manawanui e
Pūmau ki te aroha
Pūmau ki te oranga
Pūmau ki te manawanui e
Pūmau ki te manawanui e
Pūmau, Toi Mata Hauora e
Translation
Te Mauri Taurite stands
As members of Toi Mata Hauora
Who embrace and nurture all To achieve wellbeing
We hold fast to aroha And wellbeing
We are dedicated and committed
We support and are supported by Toi Mata Hauora – ASMS
JUNE 2024 PAGE 11

OFF BALANCE
MATT SHAND, JOURNALIST
The management of CME is a bugbear for many ASMS members. What is Te Whatu Ora doing to make process easier for SMOs to manage?
Every year approximately $50 million is paid to senior medical officers across New Zealand through continuing medical education (CME) funds.
Despite being such a large sum of money, the systems for managing and accessing this entitlement are often ad hoc and not nationally consistent. Some districts still rely on manual spreadsheets and paper trails to track balances.
This, in turn, leads to errors. As a result, some SMOs have been short-changed their entitlements, and ASMS industrial officers are constantly helping sort this out.
CME is a vital tool for ensuring SMOs can remain up-to-date in training, expand their skillset and build networks. ASMS regards it as a part of future-proofing the existing workforce. Any measure that makes it harder to access and use should be stopped.
Difficulty accessing CME, or even finding out current balances, is a common talking point at Joint Consultative Committee (JCC) meetings across the country.
“Accessibility problems take two forms,” ASMS Industrial Director Steve Hurring says.
“One is managers taking an overzealous approach to what is covered by CME and what constitutes a reasonable expense.
“Often managers mistakenly apply public sector business travel rules which are far more restrictive, not realising that CME is a contractual entitlement, not a discretionary one, and is intended to cover all reasonable expenses associated with CME without arbitrary caps on expenditure.
“The other problem with access is the extremely poor management of the claims process, poor record keeping, and poor access to information about leave balances. There is wide variation across the country in this area as well.”
In Wellington in March 2023, unlawful deductions of CME were detected and raised. They occurred when CME accumulation was changed when New Zealand’s borders were closed in response to Covid-19.
“During bargaining for the last MECA, the then DHBs indicated they intended to reduce the CME accumulation limit back from five years to three years on the basis that the ‘borders were open’,” ASMS Senior Industrial Officer Ian Weir-Smith says.
“They did subsequently concede that CME balances over the three-year limit would not be forfeited and could still be used. However, new funds would not accrue where the balance was over the three-year accumulation.”
Despite this, Weir-Smith observed issues at Capital, Coast and Hutt Valley district, where staff who had more than the $48,000 accumulation had their balances unilaterally reduced back to $48,000.
“It was an unlawful deduction, and it was only sorted after ASMS got involved with management,” Weir-Smith says.
“CME is always an issue industrial officers have to assist with. It is commonly on our members’ minds.
“[In Wellington] we had the issue resolved, but it is unfortunate in a time we are trying to retain our health care professionals that these types of things keep cropping up.
“The process to resolve the issue took time and left many members feeling undervalued. Bearing in mind the lack of visibility of things like CME balances and the communication in making the unilateral deductions, it leaves members feeling distrustful of the process and the accuracy of the records.
“The perception of being short-changed is very real.”
Another area where SMOs can be left feeling short-changed occurs when calculating their leave days and where their
PAGE 12 THE SPECIALIST
Te Whatu Ora inherited 28 separate systems that support the paying of our 90,000 staff and management of their various leave entitlements –most of which aren’t fit-for-purpose...”
– TE WHATU ORA
working day is longer than the CME applied to cover it.
“Te Whatu Ora needs to get the message that CME leave is for 10 working days leave, not necessarily just 80 hours as it is often calculated,” Weir-Smith says.
“The term ‘working days’ is important. It is not for eight hours of a day. If you work a 10- or 12-hour shift, then you may be using 10–12 hours of CME for your day of leave. If the leave is only provided based on 80 hours that would reduce your CME by 20 per cent or more.”
Last year at a meeting at Capital, Coast and Hutt Valley it was confirmed this practice will be changed and any leave lost will be added to affected staff.
Hurring says ASMS has made progress in recent years to create more consistency over what CME covers.
“It is now understood that annual leave can be taken alongside CME,” Hurring says.
“Te Whatu Ora now accepts that costs arising from childcare, which would otherwise prevent participation, can be covered by CME too.”
On the Te Whatu Ora-ASMS work programme is the development of a national CME policy to replace the 20 district ones.
“This should eliminate the misinterpretation problems currently experienced by members in a number of districts,” Hurring says.
“Getting started on this work has been waiting confirmation of the permanent medical leadership positions, which should be in place this month.”
With more than $50 million spent each year, it seems odd no better system has been developed and measures that have been made are not rolled out further.
“In some cases, the CME system is just a spreadsheet that is manually updated. There is a lot of potential for that system to have inputting errors and a lack of accountability should it ever be questioned,” Hurring says.
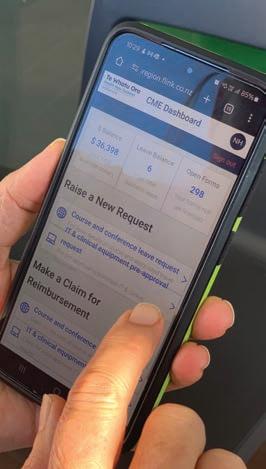
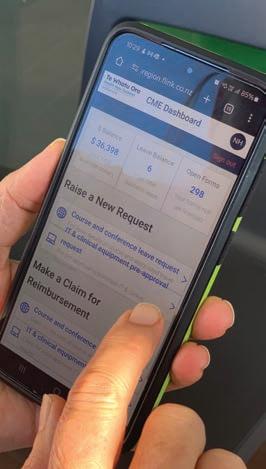
Some districts have been proactive in resolving the issues. Waitematā district used part of its capital expenditure budget to produce an appbased system to allow doctors to manage their CME applications on their phones or devices.
The app started operating in 2020. Project manager at Waitematā Nicolette Hansen says the app was developed in response to staff requests.
“Staff requested a simplified, electronic process for applying for and claiming CME and other leave types,” she says.
“We identified some issues which an e-process would help address around the management of CME leave.
“It used to be very paper based. SMOs were getting fed up with having to submit paper records for everything. In some cases, they would hand in pages of receipts following trips away. They wanted something electronic and something they could access from more places.”
The app digitises the CME process, enables receipts to be uploaded from a phone and adds automatic updates to CME balances and entitlements. This allows leave applications and expenses to be logged from any location where a device has internet.
“You could sit in the Koru Lounge waiting for your flight and log the taxi trip that got you to the airport in real time,” Hansen says.
“The app also adds transparency. You can see what you have spent your CME balance on. See your applications and approvals and budgets.”
The app also makes life easier for auditing purposes and end-of-year reports. However, the app is not yet fully integrated and cannot automatically update payroll.
“If we could get the app to speak to payroll it would make things a lot better long term,” Hansen says.
There are also long-term plans to give the app more functions. “Nurses have continuing professional development as well as psychologists.
We are looking to see if we can tweak the app so they can use it.”
Other districts are starting to take notice. Counties Manukau; Capital, Coast and Hutt Valley; and Northland are now investigating if the app can be rolled out with their systems.
Hansen says a strength to the app-based system is it can be altered to reflect the current collective agreement terms and conditions with relative ease.
“We were able to update the CME app to make the changes from hours to days as stipulated in the Single Employer Collective Agreement,” she says.
“As well as the changes to the amount that can be accrued.”
However, there is no current plan to have the app roll out at a national level.
“National-level changes take time and it is a matter of priority,” Hansen says.
A Te Whatu Ora spokesperson says a range of CME management systems are used across New Zealand and they are still considering how to best support effective management of CME across the medical workforce.
“Te Whatu Ora inherited 28 separate systems that support the paying of our 90,000 staff and management of their various leave entitlements – most of which aren’t fit-for-purpose for our requirements in 2024 and need investment,” they said.
“We have commenced a detailed review of these systems, which is expected to be completed in the next few months. We will then be able to make informed decisions about these systems, including how best to support effective management of CME for our medical workforce over the long term, and work through the changes needed.
“Our goal to modernise Health NZ’s payroll systems and processes includes a reduced reliance on manual inputs wherever possible. The app you refer to still requires some information to be entered manually by the payroll team.”
JUNE 2024 PAGE 13
Smoke and mirrors


16 PAGE 14 THE SPECIALIST
Ashes in my mouth
Patients and penguins 22 20 23
Where there’s smoke…
Flatline for transparency

Medal-winning medicine Passing the test 26 28 30

JUNE 2024 PAGE 15















MATT SHAND, JOURNALIST
The Specialist speaks to Associate Minister of Health Casey Costello about why she believes repealing world-leading legislation will still allow New Zealand to be smokefree by 2025.
Reducing the supply of cigarettes will not reduce demand for cigarettes, Associate Minister of Health Casey Costello says.
Costello also says proposed measures to reduce the number of suppliers of nicotine products would make it too hard, or too costly, for people to buy nicotine products.
At times, our interview is confusing, as speaking points seem to clash with each other.
Official advice given to Costello also mentioned the repeal of the smokefree legislation would likely bring an increase in tax revenue, suggesting reducing supply would have reduced sales.
In contrast, increased sales will equal more tax but also equal more consumption to generate that tax revenue – as a result an extra $1.5 billion over four years will be earned by the Crown thanks to sales of nicotine products. The coalition Government agreed to repeal legislation put in place by the previous Labour Government in 2023 that was heralded as a game-changing move to reduce cigarette harm in New Zealand. The repeal is being handled by
Associate Minister of Health and New Zealand First list MP Casey Costello.
The repeal sees the removal of the commitment to a ‘Smokefree Generation’, a limit on the amount of addictive nicotine that could be added to cigarettes, and a reduction in the number of retailers of tobacco from 6,000 to 600.
Costello says the portfolio “fell onto her lap”.
She says she is still committed to further reducing smoking rates and achieving the Smokefree 2025 goal of daily smoking rates of less than 5 per cent for all population groups. However, it is unclear how repealing stricter measures will help achieve those results.
Costello won’t stake her job on New Zealand reaching the Smokefree 2025 target but promises to “go back to the drawing board” should repeal not work out.
“It was in our coalition agreement. It was logical as it was something we felt strongly about,” Costello says.
What made New Zealand First want to see a change?
“Basically, the practicality of it,” Costello says. “There’s no evidence to say it [the smokefree legislation] was going to achieve what it hoped to achieve.”
“The other component was that it was fundamentally based upon the fact that if we reduce supply it will reduce demand.
“Anybody who works in enforcement around addiction knows that reducing supply is not a demand reducer. What we had to do was recognise that what was being done [before the new Smokefree laws were enacted] was incredibly effective.
“We had achieved the greatest smoking reduction in the last two years, so what we were doing was working and none of the things repealed were in place.
“The reality is we’re down to the hardcore, addicted smokers. We are down to 285,000 daily smokers. Not young people taking up smoking but long-term smokers that are addicted. We need to work on programmes that are going to target them and provide suitable interventions to quit smoking.”
PROFILE
PAGE 16 THE SPECIALIST
Why not do both? Why don’t you do that [targeted intervention] and have the increased legislative measures?
“So, we know vaping was working. So, we were going to go down from 6,000 retailers to 600. So we were limiting access to vaping for those who had successfully quit smoking. We recognise it is lower socio-economic groups, the marginalised communities of Māori and Pasifika that are the hardcore smokers. And we’re going to say, ‘Okay we’re reducing the retailers down to 600.’ In cities that might mean a 10-minute drive and in rural areas you would be driving 60 minutes. I was dealing with people who are talking about how they know they need to quit smoking but they will give up food and petrol to smoke.
“Limiting supply is not going to limit demand. We must deal with demand. That’s what we’re trying to do and go back to the fact that what we were doing was working. We had 100,000 people quit in the last two years and we didn’t have to do anything more.
“In response to ‘why not do both’, this is about getting the best bang for your buck as to what we’re trying to achieve. When you go out to the quit smoking groups that are working in the community, they are saying what is working. For some of them, they are asking that vaping be supplied as a quit smoking tool. You know, they are talking about the things they know are working. One of the huge drops in Māori women smoking was due to a vaping programme.”
You say reducing supply will not reduce demand. Clinicians could argue the removal of the addictive substance, the nicotine, would spell the end of tobacco addiction. Would that not help people transition away from cigarettes and into these vape products?
“It’s like if you are an alcoholic and saying I’ll give you low alcohol beer so that’ll mean you won’t need to drink proper alcohol,” she said.
“Now the same logic applies if they’re addicted to nicotine. They want the nicotine hits if they are not getting the nicotine hit, and that goes to the black market discussion that goes back to ‘if you want to get it you’ll get it’.
“What we want is to get rid of the addiction. This idea of denicotisation was all unproven, theoretical, and yet those dealing with the quit

It’s like if you are an alcoholic and saying I’ll give you low alcohol beer so that’ll mean you won’t need to drink proper alcohol.”
– ASSOCIATE MINSTER OF HEALTH CASEY COSTELLO
JUNE 2024 PAGE 17
ASSOCIATE MINSTER OF HEALTH CASEY COSTELLO.

smoking groups, they say people will try a different way to get the nicotine hit so we need to wean them off nicotine.”
It’s not completely evidence-free. There are case studies overseas showing smokers stopped smoking cigarettes in two weeks once nicotine was removed.
“When we discussed this with ASH [Action for Smokefree 2025], they said it [denicotisation] was not the way to go. Denicotisation is not a proven tool.”
(See ‘Ashes in my mouth’ page 20 for ASH’s response to this claim.)
So, you say there was no evidence this would work, what is the evidence that not doing this will work?
“I’m saying what we were doing was working and we want to do more of it.
“We want to provide the quit smoking tools, and at the time vaping wasn’t one of the quit smoking products we were providing, but when you talk to the people at the coalface, they’re saying vaping could work.
“We know in the UK, they actually had vaping shops in the hospitals to stop them from smoking at that point, but we weren’t doing that. We weren’t allowing vaping to be used as a product.
“So, there’re things that we thought you could look at without putting in all of this stuff and actually look at a more targeted response.”
But if denicotisation of cigarettes went alongside your campaign to have vaping products more available – with nicotine – would you not see the transition where one would move from one to the other?
“Like they will go to a black market cigarette – which are readily available…”
Where is your information about this black market coming from? If that is the logic, should we not just make all drugs legal to prevent a black market starting?
“The differential is we’re talking about a product that’s legal; we’re not talking about a product that is illegal now and we’re trying to control it. We’re talking about a perfectly legal product that has been around forever and I’ve had numerous discussions about all this and the, ‘Oh, there is no evidence of a black market,’ and the study [unsure which] produced is an analysis of rubbish to say there was no black market because no illegal cigarette packets were found.
“Well, the Chinese cigarettes that get into this market are in paper packets. We had an extra $10 million investment into customs just to curb black market tobacco. The people that are actually out in the communities can tell me where you can buy black market cigarettes and which shops sell them. We know they are getting in. There’s no way customs is stopping all of it.
“We know they’re out there so this idea, you know, there is no black market is just not true.”
PROFILE PAGE 18 THE SPECIALIST
We were going to go down from 6,000 retailers to 600. So we were limiting access to vaping for those who had successfully quit smoking.”
– ASSOCIATE MINSTER OF HEALTH CASEY COSTELLO
I read the KPMG report that is produced for the tobacco industry, and it says there has been a reduction in illicit tobacco use in New Zealand by 10.1 per cent…
“What we’re seeing at the border [illegal tobacco] has virtually doubled in the last five years I think.”
So, are we going to stop those measures?
The extra funding [to curb illegal tobacco], is that going to continue?
“We’re still wanting to control that but, again, let’s focus on reducing demand, which is what we’re keen to achieve.”
The briefing given to you by the Ministry of Health was quite strong. It says Smokefree 2025 will not be possible anymore. Do you accept that criticism?
“I mean that was the advice given. We didn’t speak to the Ministry of Health in isolation. ASH was one example of an organisation we spoke to…”
Who else did you speak to?
“Well, I met with everybody. Cancer Society… I mean there are a whole lot of organisations that have strong views in the space. We kept going back to the fact that what we were doing was working. We needed to ensure we continued down that path. We wanted to introduce more targeted programmes to the communities that were most adversely affected by smoking addiction.”
What will those programmes be?
“Well, if you look at quit smoking groups, the community groups that go out and meet with them, that was about having more of a range of products [that replace cigarettes].”
“So that was the direct engagement from one of the quit smoking groups. They’re in a bus, meeting the communities at shopping malls and sports grounds, and they’re going out to the
communities and actually going into the home and providing intervention there at health centres. You know, I would much rather have seen those targeted initiatives better funded, the advertising campaigns and funding for those programmes.
“And then the other component was increasing the penalties and really looking at the whole regulatory regime.”
So the penalties – increasing fines etc. Who is going to be enforcing that?
“At the moment there is this funding for 16 dedicated, and there are 39 other, health enforcement officers that are working in this space. So that’s the enforcement. Part of this work is actually to look at this whole regulatory regime and how enforcement has been done.
“We’re also looking at how stores display. So the vaping stores at the moment look like Smiggle stores. They are very attractive and all bright and shiny. We want to actually do a review of the regulations that were already in place. We’re doing a whole review about that; not just who licenses but actually the whole regulations around how they were written and how easy they are to enforce. Because there’s no point increasing penalties if it’s too hard to do the enforcement in the first place. So, we’re looking at that whole component.”
Doctors deal with the effects of smoking harm on a daily basis. With the health workforce so stretched, and now with curtailed measures to reduce the harm done, do you have any concern the removal of legislation will cause more harm to the health system and increase wait times?
“Well, what I can say is if we don’t see the reduction we have continued to see then, absolutely, we have to look at everything. If we’ve changed nothing and those reductions don’t occur, then yes, we are back to the drawing board. But
we’ve got to put everything in place that was in place to receive the reductions we have received or changed and will continue to push.
“That’s why, you know, we’ve said repeatedly we are committed to the 5 per cent target, and there’s a range of enforcement and supports and community initiatives that can be put in place to continue to push us there.”
So, in 2025 if we don’t get to 5 per cent, what happens? Do we bring in these ideas again?
“I mean we look at everything. My view is we’ve achieved this with what’s in place and we’re trying to do that without a whole new regulatory restriction regime that I think would have unfortunate, unintended consequences.
“I just want to reach the communities struggling the most – my family is all up North and I’m just looking at the retailer reduction. I know numerous locations that, if they lost the local store, they would have to drive 30 minutes to buy cigarettes.
“I think we want the same target, we just have a different approach.”
Are you concerned that vaping is just tobacco 2.0? A lot of tobacco companies are pivoting towards it. It has an addictive component. Are we going to be hit with a wave of vapeaddicted people?
“I mean, nicotine remains an addictive product. Yes. But at this point, we’re talking about degrees of harm. We want to keep it out of the hands of young people. Unfortunately, vaping got ahead of us. Vaping had us before we knew what to do with it. And we’ve been in catch-up mode ever since. But there’s no denying it. It’s played a part [in reducing smoking numbers]. And it is, you know – as much as we talked about it being a bit on the balance of things – it’s less harmful than smoking.”
JUNE 2024 PAGE 19
It would concern me if ASH is stating that denicotisation is not evidence-based.”
– PROFESSOR JANET HOEK
ASHES IN MY MOUTH
MATT SHAND, JOURNALIST

A leading anti-smoking group is being criticised by public health experts as being “illogical and ignorant” about advice given to Associate Minister of Health Casey Costello regarding the repeal of anti-smoking legislation.
In an interview with The Specialist (page 16), Associate Minister of Health Casey Costello said anti-smoking group Action for Smokefree 2025 (ASH) was asked whether removing nicotine from cigarettes would reduce smoking rates. ASH replied that “it was not the way to go. Denicotisation is not a proven tool.”
Costello also says ASH advocated for greater access to vape and vape products to combat smoking rates and their advice included increasing the range of flavours available to make them more appealing.
ASH says it provided a briefing to the incoming minister but did not have any meetings with NZ First, or Casey Costello, prior to the release of the coalition agreements outlining the repeal of tobacco laws.
“It was very clear that stopping the repeal was extremely unlikely,” ASH Chief Executive Ben Youden says.
“We therefore took a tactic to seek discussions about what was planned, and could be retained, reformed or modified in the repeal process.”
Youden confirms ASH does not oppose the repeal of the law to remove nicotine from cigarettes.
“Nicotine is better managed through regulation, rather than primary legislation as a means to better mitigate and react to unknown impacts on what was, in essence, a de-facto ban of cigarettes,” he said.
ASH also confirmed it labelled nicotine removal from cigarettes as “theoretical”.
“Given no jurisdiction has ever implemented this policy, this is simply a fact,” Youden says.
“The evidence to justify the policy was and is theoretical as it is based on an ‘expert elicitation’ process, not on any empirical data. We have a duty to be honest about the limitations of the evidence, especially if the real-world consequences (good and bad) are unknown.”
Public health experts and academics instead point to clinical trials where removal of nicotine in cigarettes showed a large impact on people’s desire to quit and success at doing so.
Co-director of ASPIRE Aotearoa Professor Janet Hoek says clinical trials show once nicotine is removed from cigarettes there may be a slight increase in smoking as the people try to obtain their usual nicotine dose; however, people quickly realise that will not be possible and then reduce their smoking and become more interested in quitting, more likely to try and quit, and more successful in their quit attempts.
“It would concern me if ASH is stating that denicotisation is not evidence-based,” she said.
“There are clinical trials from Aotearoa and from the US that point to the powerful impact denicotisation would have on smoking prevalence. There is strong support for this
PAGE 20 THE SPECIALIST
Nicotine is better managed through regulation, rather than primary legislation as a means to better mitigate and react to unknown impacts on what was, in essence, a de-facto ban of cigarettes.”
– BEN YOUDEN

policy from people who smoke, and qualitative studies also point to this measure’s likely effect.”
ASH says they presented alternatives to the ‘smokefree generation’ proposal, which would have seen it become illegal to sell cigarettes to people born after a certain year, favouring an R21 age limit.
They also argued for greater access to vaping and vape products to assist in quitting.
“We also proposed reform for vaping, including better protections for children balanced with more appropriate and consistent access and advice to adults who smoke,” Youden says.
“Vaping has clearly contributed to a profound downturn in smoking in recent years and is massively reducing smoking harms.
“ASH has advocated both to [previous Minister of Health] Verral and Costello for the removal of disposables vapes that kids use, better regulation of the sales environment and fixing the regulator.”
ASH also echoes sentiments from Costello about how measures to reduce supply do not decrease demand.
“Smoked tobacco is addictive, and withdrawal and addiction do not disappear if the substance and preferred form of delivery are removed.
“Reducing it to ‘demand’ is an oversimplification of substance use and addiction.
“Consumption may well reduce, as might use, but demand is also linked to withdrawal and need to alleviate symptoms – both physical and psychological.
“By way of example, the relapse rates of those who have been in smokefree prisons is almost 100%. It is our understanding and experience in nicotine addiction that inform our views.”
Anti-smoking advocates are confused at the stance ASH has taken on the issue and question the relevance of the organisation.
Health Coalition Aotearoa co-chair Lisa Te Morenga says ASH runs the risk of losing its social licence with its advocacy stance.
“This briefing they have given to the ministers defies their own logic and pro-vaping stance,” she says.
“They believe vaping is the best thing to stop smoking but are standing in the way of legislation that would actively encourage people to vape more to satisfy their addiction to nicotine, especially if nicotine was removed from cigarettes.
“It makes no sense, and it is a real shame they have opened the door for this smoking repeal to occur by giving bad advice to decision makers.”

JUNE 2024 PAGE 21

WHERE THERE’S SMOKE…
MATT SHAND
As tobacco companies globally pivot to the sale of non-combusted nicotine products, the coalition Government’s decisions around smokefree legislation will not threaten the profitability of selling nicotine.
In 2023 Phillip Morris International made $35.2 billion in revenue, a 10.7 per cent increase from the previous year.
More specifically, from the profit generated by that revenue, about 40 per cent was generated by ‘smoke-free products’ such as nicotine pouches (snus) and products which heat tobacco rather than combust it.
Smoke-free products are becoming very big business. Phillip Morris recently spent more than $16 billion to acquire the company Swedish Match, which produces oral nicotine products in what Phillip Morris described as a bid to “enable us to provide access to a broader range of better alternatives for those adult smokers who would otherwise continue to smoke”.
In this context, documents leaked to Radio New Zealand in March 2024 about the negotiation of the coalition agreement between National, ACT
and New Zealand First talk about providing excise tax freezes on cigarettes and zero excise tax for “less harmful smoking products” such as heated tobacco products and oral tobacco products.
The leaked documents say, “We need to treat this for what it is. Addiction. Not punish people for it but help them out of it.”
The same documents also label nicotine as “only as dangerous as caffeine”.
This approach accepts further nicotine addiction as the answer to smoking addiction. Vapes, oral tobacco and heated tobacco products all rely on highly addictive nicotine in order to get people to use them repeatedly.
Daily vaping and e-cigarette rates in New Zealand have risen 1,000 per cent over the last nine years, from 0.9 per cent to 9.7 per cent of the adult population. This 8.8-point increase is greater than the 7.7-point decrease in the daily smoking rates over the same period. The result is a net gain in nicotine addiction, an addiction that may continue to grow as the popularity of e-cigarettes grows.
Data on smoking quit rates in New Zealand underlines the power of nicotine addiction. Figures released alongside the announcement to repeal smokefree legislation showed
that, over the last decade, 158.6 per cent of smokers – 867,000 adults – stopped smoking. Even more impressively, 225.1 per cent of the youth population – or 177,000 young people –successfully quit smoking.
Figures greater than 100 per cent are possible because people quit more than once, primarily due to the addictive nature of nicotine.
Once nicotine is removed from cigarettes, experts say there is an initial increase in consumption as people try to smoke more, to consume more nicotine. But, with the stimulus gone or so low it cannot be absorbed into the blood stream, the desire to smoke quickly reduces.
Globally, there is a push from tobacco companies to have nicotine labelled “as harmless as caffeine” and establish that it is “not the nicotine but the combustion of cigarettes” that causes harm.
The subsequent Government decision to repeal a limit on nicotine in cigarettes shows a recognition of this view.
So far, vaping has shown itself to be less lethal than cigarettes. But it was not too long ago when cigarettes were promoted for their ‘health benefits’ and stress-relieving qualities, and even had endorsement by doctors and medical professionals.
OPINION PAGE 22 THE SPECIALIST
They cannot pick and choose what information they release for the sake of spin.”
– SARAH DALTON
FLATLINE FOR TRANSPARENCY
MATT SHAND, JOURNALIST

Te Whatu Ora wrapped the results of its first nationwide staff Pulse Survey up in red tape, taking a year to release the full findings. Now they are embarking on a second survey. Have they learnt anything?
Evasive manoeuvres, cover ups and broken promises have plagued the release of Te Whatu Ora’s first Pulse Survey, with Official Information Act (OIA) requests exposing a disturbing trend of Te Whatu Ora not releasing information promptly.
Te Whatu Ora is the most complained about agency to the Ombudsman when it comes to fulfilling obligations under the OIA, with 92 complaints about the handling of requests in the six months prior to March 2024.
The Pulse Survey 1.0 was completed in February 2023, but it took more than a year to gain access to region-by-region breakdowns – even after promises made in senior executive meetings, including by Chief Executive Margie Apa and Chief People Officer Andrew Slater, to share the results with ASMS.
The Specialist resorted to the OIA to obtain the results and eventually received them after substantive delays and about 36 pages of redactions from the documents.
The main target of the redactions is the information from the frontline captured in staff comments about issues.
According to further documents released under the OIA, the release process was plagued with delays and stalling tactics, despite the information being easy to access.
“Te Whatu Ora executives need to understand they run a publicly funded organisation that demands greater transparency for the general public and their employees,” ASMS Executive Director Sarah Dalton says.
“They cannot pick and choose what information they release for the sake of spin. The delayed release of the Pulse Survey report is paying lip service to the phrase ‘transparency’ without doing it.”
Delay tactics breed mistrust
The timeline of the OIA request to release the Pulse Survey sheds light on questionable tactics by Te Whatu Ora when it comes to releasing information.
JUNE 2024 PAGE 23

ASMS sent an OIA request on 28 November 2023. The maximum time an OIA request can take is 20 working days. However, the Act specifically mentions that this is a maximum, and the information should be provided “as soon as reasonably possible”.
By 30 November, every single Pulse Survey result was compiled. On 22 December, Principal Advisor to the Chief People Officer asked for an update, stating, “The info has been with your office since 4 December … if you’re able to expedite this that would be great.”
On 16 January an extension was requested to the OIA request, with a response due on 14 February.
It was not until 3 March, after the newly extended deadline was missed, that the information was sent through to ASMS and released publicly via the Te Whatu Ora website. The redacted information appears to be comments from members submitted as part of the report, which are broken down into districts.
Released information makes mention of these comments as being part of 28 separate reports with full breakdowns of comments, but these have not been obtained by The Specialist
Transparency is more than a buzzword
Minutes from executive leadership meetings, released alongside Pulse 1.0 data, highlight concern that comments left by staff, including SMOs, “will appear in the media after they are communicated with employees”.
“We recommend responding with our approach of owning the results and being transparent.”
Despite this, there was a lengthy wait for results to follow.
These notes also mention the free-text responses were negative. “It is clear from the free-text responses that at an organisation level people don’t feel universally listened to, valued or respected. Many of the free-text responses are quite confronting to read where people variously describe themselves as undervalued, distressed, overworked, stressed, fatigued and fed up.”
The authors recommended communicating the results, bad as they were, to ensure trust is built with stakeholders.
“This requires honesty about where we need to improve while encouraging a constructed, solutions-focused narrative,” the report read.
A communication plan was drafted and distributed with the results, which double downed on this sentiment.
“There is a need to carefully plan the release of results and initiate action planning at a national level to ensure Te Whatu Ora is seen to follow through on its commitment to transparency and finding solutions to challenges facing our workforce.”
The communication plan includes telling the engagement story “on our terms”.
Media lines were prepared by the communications team if requests were made for verbatim comments from the survey.
Staff were advised to say, “One of our top priorities is to maintain the privacy and anonymity of our people, and the integrity of our survey process for the future. To ensure this, verbatim comments are being carefully managed and used for action planning and improvement purposes, rather than being shared in their entirety, without the context needed to draw meaningful conclusions.”
Some comments obtained by The Specialist show that lack of anonymity was not a particular
PAGE 24 THE SPECIALIST
risk and raise the question whether the blanket removal of comments was more about avoiding the airing dirty laundry.
Some comments included:
“I would like to see Te Whatu Ora value its employees. Often working short staffed without so much as a thanks, appreciation or any support…”
“Iwouldliketoseemanagementowntheir part of the responsibility that we are feeling burnt out and tired. Ours seem to think it’s all our own fault and that we have to fix it ourselves, with no input from them. They also don’t check in on those of us with issues to make sure we are improving.”
“Clear communication especially between management to staff. Everything feels secretive and we do not get consulted until a decision has already been pretty much made. Management do not take the time to find out what is involved in our day-to-day work before making these big decisions which impact us greatly.”
“The survey was gathered using public funds and so should be available to the public,” Dalton says. But efforts at meetings with Te Whatu Ora executives to gain access were initially met with unfulfilled promises and pushback.
In a National JCC meeting Te Whatu Ora Chief Executive Margie Apa asked, “What would you [ASMS] do with the information?” and questioned if it would be given to media.
“The evasive manoeuvres are what is frustrating in this case,” Dalton said.
“Te Whatu Ora engaged with staff during this process and will not share those results without spinning the narrative. If they want to be a transparent workplace they should start walking the walk.
“If you don’t like what people are talking to you about, change the things you do, not what you tell people.”
Te Whatu Ora responds
Te Whatu Ora says it stands by its decision to withhold information in pages 48–79 in their response to the OIA request.
“There was no indication to participants in the survey that such comments could be released
for public use and there is also a possibility that some comments may be attributed to an identified individual based on the content of their comments.
“The release of direct quotes would potentially inhibit the full and unrestricted participation of our staff in future surveys,” their response reads.
Executive staff said the results of Pulse 1.0 provided a list of 1,550 things that needed to be followed up on, with about 90 per cent of those now completed, including quick wins.
Quick wins or quick spins?
The Specialist has been able to obtain a spreadsheet of actionable opportunities identified by Te Whatu Ora from a selection of the free-text comments in the first Pulse Survey.
The table logs 1,370 responses, as well as the district and services they originate from. All are then categorised as ‘opportunities’ (988), ‘quick wins’ (207) or ‘red flags’ (175). They are then all listed as something Te Whatu Ora is actioning, with the vast majority completed and just 20 ‘in progress’ and 23 ‘not started’.
Red flags almost all related to either bullying, favouritism or poor management. Canterbury; Capital, Coast and Hutt Valley; and Waikato had the largest number of red flag responses. Responses to all red flags are marked as completed, but many of the actions were simply to report the redacted response back to the respective service.
Other responses were to declare the problems – including concerns about psychological safety at work – “not a red flag”. Some responses to bullying noted they “believe this position is overstated” and others said that the issue was “identified as a national priority” and left it there.
On the ‘quick wins’, again, feeding back responses to a service was a common indicator of a job done. One issue about a faulty lock was deemed quickly won with “investigating to see if there have been requests to fix a lock”. One completed quick win simply asked, “Can this be addressed?” while another stated “Go forth and do it” to a request for equipment that wasn’t broken.
About a fifth of quick wins proposed better communication as a solution, but perhaps the most troubling was a completed quick win in Canterbury that stated it was “not a quick win”.
A fresh pulse but no local breakdown released
Te Whatu Ora has recently completed its second Pulse Survey with some high-level results shared in May.
These generally show improvements and a higher level of engagement.
However, lack of resources continues to plague the workforce, with just 40 per cent of all respondents saying they have the resources to perform their job well (up 7 per cent from the first Pulse Survey).
Of similar concern is reduced support for the statement ‘The changes our organisation is making will enable us to better meet the needs of our communities’, which fell from 56 to 51 per cent.
However, most categories showed an improvement across the two surveys of between 2 and 5 per cent. On average, 63 per cent agreed or strongly agreed.
However, a fuller breakdown, including a district and an occupational analysis, has been requested and, so far, not provided.
As context from the first Pulse Survey, while 33 per cent overall agreed their team had the resources they needed to perform their roles well, the one breakdown by profession that The Specialist has seen shows only 13 per cent of SMOs and 19 per cent of RMOs agreed with the statement. Equally, while 15 of 16 questions have 50 per cent or more support overall in Pulse 1.0 and 2.0, the professional breakdown from the first survey found SMOs were only net positive for 5 of the 16 questions.
ASMS believes these concerns are at the core of the causes for the industrial action taken against Te Whatu Ora in 2023. The details of the new results will show what, if anything, is changing. “We hope we can see fewer blank pages and more change within Te Whatu Ora,” says Dalton.
JUNE 2024 PAGE 25
PATIENTS AND PENGUINS
MATT SHAND, JOURNALIST

What is it like practising medicine at −58 degrees centigrade? The Specialist speaks to Emily Adam, who was stationed at Antartica’s Scott Base over the summer research season.
Being an outdoors enthusiast, Emily Adam set her sights on pushing boundaries in her personal and professional life. That passion eventually led to her pushing against the boundaries of life on Earth, practising medicine in Antarctica.
“Every day I just look out the window and feel amazed at how pristine it is,” Adam says.
“It’s just beautiful but, at the same time, it is a reality check. Even though it looks like a beautiful, sunny day, the temperature outdoors may be down to −58 degrees with the wind chill.
“It’s surreal.”
As the lone doctor on Scott Base, Adam is responsible for the wellbeing of the crew and visiting researchers, with about 300 people passing through the base each year.
That will involve acting as a GP as well as, at times, radiographer, medical risk assessor, councillor, epidemiologist, telehealth specialist, physiotherapist and medical trainer – many roles that would normally have nurses and allied health staff to assist.
The job also involves a lot of regular stocktaking and predicting what medicines to order in advance so as not to run out.
Adam’s background in the outdoors, as well as experience in prehospital emergency care, worked well to prepare her for the job on Scott Base.
“I enjoy many different outdoor activities and have always been involved in community organisations,” she says. “These include surf lifesaving and LandSAR [Land Search and Rescue].
MAIN IMAGE: KIS3 TENTS ON THE ANTARCTIC ICE. PAGE 26 THE SPECIALIST

“I always wanted to get down to Antarctica, and I thought I would put forward my medical and outdoor experience and let them determine if I was a good fit for the job.”
The timing worked out for Adam. Scott Base was undergoing an upgrade, which saw the population swell during the 2023/2024 summer season.
After completing her application and passing her psychometric testing, it was not long before Adam was packed into a Royal New Zealand Air Force Hercules and flown to her new posting in Antarctica.
“A big part of the job is screening new arrivals to the base for any infectious conditions,” she says.
“Anything that gets in down there tends to spread very rapidly, and there are limited-to-no isolation facilities.
“You also perform health checks for those going out into the field. We have science groups heading out hundreds of kilometres away from the base, and you have to ensure they are healthy to go and remove what elements of risk you can.”
Much of that sees Adam preparing 300 medical kits on the base and providing training to people leaving the base. The possible risks vary incredibly from expedition to expedition.
“It’s about figuring out what each specific expedition is doing and what are the risks they may face,” she said.
“For example, one group was heading up Erebus, so we had to think about altitude sickness and extraction plans. Another group was working with penguins, which carries a potential risk of exposure to avian influenza, which is spreading across Antarctica, or, if they are working with penguin guano, the risk of gastroenteritis and dehydration, which is already a large risk due to the lack of humidity in Antarctica.”
Another aspect of the role is ensuring equipment is working and not damaged by the harsh winter conditions.
“There are monthly checks for certain kits and equipment,” she says.
“You need to check all the oxygen cylinders because the lack of humidity can make the seals on the cylinders brittle quite quickly.”
What appealed to Adam was being a doctor in a small, tight-knit community.
“It gives you a very holistic experience of health care,” she says.
“You are living and working with all your patients, so you know them on a very personal level. They are your friends, and you carry lots of respect for them.
“Secondly, you are working all by yourself. There is no allied health to support you. It makes you a well-rounded doctor.”
While being the only doctor on the base, the other staff who work at Scott Base are usually well trained, and it is not uncommon for others on the base to hold various health care qualifications. In an emergency, the US base McMurdo Station, about 3 kilometres away, has other medical staff, more equipment and a small hospital.
“They are very good neighbours,” Adam says.


A key challenge is dealing with the isolation that comes from living 3,000 km away from New Zealand for 6–12 months at a time, and the difficulties of living in confined spaces.
“You have to adjust to the lack of privacy. Everyone has at least one roommate,” she said. “It is fascinating how the base is run.
“We get all our water from reverse osmosis, so you are limited in how you use it. Showers are for three minutes and there are also lots of restrictions on what soaps and other chemicals can be used, as we have to preserve |the environment. Even the type of toothpaste you have is scrutinised.
“The chefs do an amazing job, but fresh food is obviously not readily available. You await the arrival of the plane as it means some fresh food has landed.”
Isolation and the lack of family connection is another thing to manage.
“It can be quite difficult, particularly as it gets closer to the end of the year,” Adam says.
“People miss their kids, and it can get quite difficult around occasions like Christmas for some. Being away from people you love is always one of the hardest challenges.”
Adam says she would love to return to Antarctica sometime but that is not in her immediate plans. For now, she wants to continue her training and look for opportunities when they present themselves.
Medical professionals wanting to work in Antarctica can register an Expression of Interest with Antarctica New Zealand. https://jobs.bfound.net/Jobs/145974?CoId=1582
JUNE 2024 PAGE 27
TOP: SCOTT BASE. BOTTOM: DR EMILY ADAM SAYS BEING STATIONED AT SCOTT BASE AS THE LONE DOCTOR WAS A CHALLENGE.
DOCTOR SUSAN BEABLE.

Thirty medical professionals will travel with the New Zealand Olympic team to Paris this year to support approximately 200 athletes.
MEDALWINNING MEDICINE
MATT SHAND, JOURNALIST
Doctor Susan Beable wanted to compete at the Olympic Games but never quite made it.
Now she uses her medical expertise travelling with New Zealand’s Olympic team ensuring athletes have the best chance at achieving glory at the Games.
“I feel I am representing my profession on the international stage and that feels really great to me,” she says.
“It is special to be at the greatest moments in sports.”
As Deputy Director of Health for the New Zealand Olympic Team, Beable has worked with the New Zealand Olympic team since the Glasgow Commonwealth Games in 2014, and has travelled to every event since, excepting Tokyo 2020.
“My background is in women’s health and sport performance advantage initiatives,” she says.
“In my role I do a lot of women’s health clinics and my research interest has been depression amongst athletes. We do a lot of safeguarding to ensure protocols are in place for mental health, women’s health, and equity for women in sports and sports treatment.”
Part of this is ensuring athletes have regular medical screening and mental health assessments to ensure continued monitoring.
“We have found that after the Games people can have a bit of a crash,” Beable says.
“This is regardless of the results or even performance. Over the last two Games there has been a very big push on this [mental health].
“I conducted research in 2017 confirming there is a link between high performance sport and depression rates. I think, historically, we didn’t do as good a job as we could in this area.”
Beable says athletes are people and are just as likely to have depression as the general population. But unique stressors, such as spending so much time away from family, coupled with the singular focus the Olympics bring, has consequences.
“My research shows financial stress is also a large concern,” Beable says.
“This is a new stressor not shown in our earlier surveys, which shows the effect of cost of living. Athletes are now considering their ‘Plan B’. Should I continue to cycle or go out and get a job?”
Beable also assists women athletes leading up to and during the Games.
“We’ve always had a strong, education-focused approach about optimising energy availability and undoing some of the ‘myths’ we see in terms of nutrition and disordered eating,” Beable says.
“Period management is part of preparation beforehand so that, hopefully, when we get to the Games everything goes seamlessly.”
The worst part of the job is working with athletes who have suffered an injury or setback that will jeopardise their chances of competing in the Games.
“The worst thing is where someone sustains an injury at training once they are over there or injures themselves the week before the Games,” she says.
PAGE 28 THE SPECIALIST


“When you know they are just not going to make the Games, that’s always a hard conversation to have. I try to remove the word ‘athlete’ and put the word ‘patient’ in my brain regardless of whether we are at the Games. What is best for the patient’s health must trump competition.”
To combat these difficult conversations there is an ongoing education programme the medical team routinely undertake, including discussions about the real risk of injury, the protocols involved and the need to report issues early.
“We try to make our role as doctors not about the [sporting] outcome,” she says.
“It is always nice to see one of the athletes who’s had a bit of a tough journey make it onto that podium.”
Chief Medical Lead for the Olympic team Bruce Hamilton says treating Olympic athletes is “high stakes medicine”, with small decisions in care, treatment and wellbeing having drastic consequences.
His role is to select the medical team that will make sure athletes have their best chance of making the starting line. Sometimes this involves supporting them when they cannot, with a view to the next Olympic Games.
“It is when the job gets tricky,” he says.
“A decision like [benching] an athlete has huge, life-changing results for the athlete and their Olympic experience. But our priority is to the athlete’s health, so it can happen from time to time. Sometimes it is a clear decision and sometimes
we’ve had athletes compete with conditions we thought would be very challenging.”
Hamilton has a long career in medicine but started off gaining a degree in physical education. His choice of practising medicine in sport has seen him travel across the world from Australia to the United Kingdom, Qatar and finally back to New Zealand to lead the Olympic team’s health unit.
“In this role I work with our team of physiologists, nutritionists and psychologists and ensure our team is delivering all it can for the Olympic athletes,” he says.
“There will be about 200 athletes travelling for the Games but about 450 all up once you include the support staff and others. We have a team of 30 professionals travelling with the team, including five doctors.”
Hamilton says preparation for an event like the Olympics takes a dedicated team of health care professionals, with the work starting about two years prior to the Games’ commencement.
“A lot of the work has already taken place leading up to the Games. Then it is more about preventing illness and preventing infections. We’ve got a strong focus on mental health this time around and it’s becoming a big focus.
“We will support good behaviour and make sure our mantra of ‘report early’ is well known.”
In the lead up to the Games, athletes will undergo periodic health evaluations ranging from ECG readings, cardio-workups and mental health checks. “That gives us the baseline,” Hamilton
says. “If things are identified we act. We use a combination of public and private health care to obtain our treatment. A lot of athletes are insured and so have access to private health care to speed urgent things along.”
Hamilton says the addition of doctors like Beable has been part of a greater recognition of broader skill sets of general physicians, including psychology and a greater focus on women’s health.
“It has been a real challenge for us in the past,” he said. “Now we have a women’s health doctor come in and focus primarily on women’s health concerns.
“The type of medicine we do has many similarities with the work of general practitioners in that it is low frequency but comes with high expectation as part of a multidisciplinary approach to health care.”
The health care shortages in the public health system also have impacts for the Olympic Games, and the team is constantly looking for willing specialists to assist.
“We are always in need of psychologists and specialists to be part of the team,” Hamilton says.
“There are lots of ways to get involved, and most people do not think about it until the Games come along. But all the work is done in the lead up.
“There are lots of ways to get involved. For example, this year the surfing is in Tahiti and we need to arrange to have a team doctor sent there with the team and that could be from a range of specialties.”
ABOVE: CHIEF MEDICAL LEAD, BRUCE HAMILTON. LEFT: CANOE SLALOM ATHLETE FINN BUTCHER PADDLES DOWN A WHITEWATER COURSE. PHIL WALTER – GETTY.
JUNE 2024 PAGE 29
PASSING THE TEST
DR CHAO-YUAN CHEN

Who is responsible for keeping track of patients test results, especially when a patient’s care is being transferred between clinicians?
At the Medical Protection Society (MPS), we get lots of questions from members asking whose responsibility it is to follow up on a test result. Missed test results, or important results that are not acted on, adversely affect health practitioners, patients, and health systems. MPS has always advised that the safest medicolegal approach is to practise in a way that assumes the responsibility for following up a test result lies with the clinician ordering the test. However, for many aspects of our complex health system, there are moments where a patient’s care is transferred whilst important investigations are ongoing with results pending. These moments, where the transfer of care occurs, are key points where results may be missed or not actioned, with resultant morbidity and, in some cases, mortality.
A particularly high-risk scenario involves a patient undergoing an investigation in a different setting to the one they are being transferred to, and that investigation revealing incidental findings that are not acted upon. These cases occur as the subject of Health and Disability Commissioner (HDC) investigations such as in Case 21HDC00619.1 In this instance, a patient presented following an injury to a public hospital ED in 2018, had an x-ray and CT and was discharged two hours later with a diagnosis of shoulder soft tissue injury with follow-up GP review. The formal CT report finalised two days later showed a soft tissue mass in the patient’s neck and recommended ENT review and follow-up MRI. The reporting radiologist noted in his report that this was discussed with the patient’s GP, who would organise follow-up. Three ED discharge
summaries were copied to the patient’s GP, with the third discharge summary containing the formal radiology report. The patient’s GP stated to the HDC that because there were no changes to the first two discharge summaries, he filed the third discharge summary without reviewing this as he thought it was a duplicate.
The patient presented to her GP a few days later as recommended by the ED and there was no mention of the CT. She presented to an accident and medical clinic two years later in 2020 for an unrelated matter and was informed of her CT neck result. The patient advised her GP, and this was the first time action was taken for the patient’s neck mass. The patient was subsequently diagnosed with metastatic squamous cell carcinoma. In his response to the HDC, the patient’s GP stated that he had no recollection of a phone call from the radiologist as he would have taken care to act on this.
The HDC found the patient’s GP to have been in breach, taking into account that the while the GP had no recollection of a call from the hospital, three discharge summaries were sent out with the last one containing this finalised CT report.
This case illustrates that the common practice of copying a patient’s GP into a pending result without a clear handover of results risks missing important results, potentially leading to a poor outcome.
In April 2024, Te Whatu Ora (Health New Zealand), Manatū Hauora (Ministry of Health), and Te Aka Whai Ora (Māori Health Authority) issued the Transfer of Care and Test Results Responsibility,2 which conveys the primary principles for the follow-up of results when care is transferred.
PAGE 30 THE SPECIALIST
A particularly high-risk scenario involves a patient undergoing an investigation in a different setting to the one they are being transferred to, and that investigation revealing incidental findings that are not acted upon.”
The document cites the MPS casebook article titled ‘Handling Test Results’3 and provides a comprehensive framework to address medicolegal aspects related to the management of test results in health care settings, emphasising the reduction of risk during care transitions. This document signals clear expectations from health system leaders and will therefore be considered an expected standard by our regulatory authorities; notably, the document has since been circulated by the Medical Council of New Zealand.
The four principles set out in the document establish clear responsibilities for health practitioners regarding the management of test results:
1. Responsibility of the Requestor: The clinician who orders a test retains primary responsibility for the results. This responsibility persists even after the patient’s care is transferred, unless there is an explicit and documented agreement transferring responsibility to another party. This principle aims to ensure that all pending tests at the time of transfer are managed properly, with a clear indication of responsibility for actioning results.
2. Communication and Delegation:
Effective communication and explicit agreements are mandatory when test results are shared with other clinicians. If another clinician is expected to act on results, this expectation must be communicated clearly and documented through a handover process. This process should involve closed-loop communication to confirm that the responsibility has been accepted by the recipient.
3. Duty of Care for Copied Clinicians: If a clinician is copied on results, particularly abnormal ones, they share the responsibility to ensure that appropriate actions are taken. This principle underlines the shared duty of care among health care providers to act in the best interest of the patient, guided by clinical judgment and the specifics of the clinical context.
4. Agreement on Monitoring and Follow-up: Regular monitoring and followup responsibilities must be explicitly agreed upon between referring and receiving clinicians. This includes defining the scope of responsibility for ongoing tests, which should be agreed upon and documented.
The medicolegal implications of these principles are profound, highlighting the importance of meticulous documentation and communication between health care providers. Accountability and the potential for criticism arise if these protocols are not followed, particularly when adverse outcomes result from mismanaged test results.
It is important to recognise the need for clear protocols and systems within health care organisations to manage test results efficiently and safely. All health care providers involved in the processing and management of test results must be adequately trained and aware of their specific responsibilities.
Systems and local procedures
Given the varied environments in which health care is provided, robust information technology infrastructure and local procedures need to be established that align with these principles. Systems should be designed to ensure that test results are clearly communicated to the responsible clinician, and there should be defined protocols for escalating issues when necessary. For example, some emergency departments specifically roster staff to review all formal radiology results and act on any significant results because, as noted above, |tests ordered in the emergency setting risk being missed, or significant results not followed up. It is important that each different department devise plans and strategies to follow up results that are ordered – since copying in the GP as the means of following up a test result is an ineffective method for requesting follow-up without direct handover and communication between clinicians. Indeed, Transfer of Care and Test Results Responsibility explicitly advises
against this practice unless there is clear communication and documentation of a handover.
It would be helpful to discuss with the patient what test results are outstanding and to ask them to specifically see a particular clinician if follow-up is required. For example, if a patient’s renal function requires follow-up post discharge from hospital, it would be helpful to advise them to get the blood test and see their GP with the results as well as communicating this follow-up plan with the GP. This way, the patient can be included in the follow-up process for their own health. Involving the patient in the process is protective for everyone concerned.
In conclusion, the principles outlined by Te Whatu Ora, Manatū Hauora, and Te Aka Whai Ora set a clear standard for the management and follow-up of test results across health care transitions. The HDC case described underscores the vital importance of clear communication and adherence to these guidelines to prevent similar outcomes.
By reinforcing the responsibility of the clinician who orders the test and the importance of ensuring explicit communication for test followup, these principles aim to safeguard patient wellbeing and enhance the overall effectiveness of health care delivery. As health care environments and technologies evolve, it is important that all involved parties remain vigilant and proactive in integrating these principles into daily practice, thereby ensuring all abnormal tests are acted upon and minimising the risk of a poor outcome.

1 Health & Disability Commissioner. 2023. CT scan results missed on discharge summary. https://www.hdc.org.nz/ decisions/search-decisions/2023/21hdc00619/
2 Health New Zealand | Te Whatu Ora. 2024. Transfer of Care and Test Results Responsibility. https://www.tewhatuora. govt.nz/publications/transfer-of-care-and-test-resultsresponsibility/
3 King S. 2015. Handling Test Results. MPS Casebook. https://www.medicalprotection.org/newzealand/ casebook-may-2015/handling-test-results
JUNE 2024 PAGE 31
Anatomy of a health crisis
Overcoming phobias with virtual reality
In the media
Branch Officers Hui
Mental health groups call for urgent investment in open letter to minister
Moral injury amongst the wards
Paid union meetings for Te Whatu Ora staff
New National Secretary selected
Kenepuru clarification

PAGE 32 THE SPECIALIST
IN BRIEF
NEWS FROM AROUND THE MOTU
ANATOMY OF A HEALTH CRISIS
ASMS’ latest report – Anatomy of a Health Crisis – brings together a range of data sources to assess the condition of Aotearoa’s public hospital services. Much of the data is previously unpublished and, following on from ASMS’ 2019 report Hospitals on the Edge, paints a picture of continuing deterioration.
In the last 10 years, people attending emergency departments has increased 22.5 per cent and the number of potentially life-threatening events (triage levels 1–3) has increased 51.1 per cent compared to less serious events.
By the end of 2022/2023, triage levels 1–3 accounted for almost two thirds of all ED presentations.
The flow-on effect of these changes can be seen: Acute inpatient discharges have increased by 24 per cent between 2014 and 2023, while non-acute discharges decreased by 1 per cent.
Director of Policy and Research Harriet Wild says the trends shown in the data indicate elective services are being displaced by a combination of budget constraints and the rising number of complex, acute cases.
“The widening gap between population growth rates and public hospital discharge rates contributes to growing unmet need for elective treatments and, for those who can afford it, growing use of private health care,” she says.
“Rising unmet need is also evident for mental health and addiction (MHA) services.
“The proportion of adults reporting high and very high levels of psychological distress skyrocketed by 72.5 per cent between 2016/17 and 2022/23. Meanwhile, the number of clients accessing MHA services increased by only 10.4 per cent between 2016/17 and 2021/22, and the workforce grew by just 5 per cent between 2017/18 and 2021/22.”
The reports show MHA staff vacancy rates have more than doubled between 2018 and 2022, and nearly 20 per cent of psychiatrist positions were vacant in 2022.
Unpublished Te Whatu Ora forecasts of public and private employment for psychiatrists show a per capita decline until 2033. Unpublished Medical Council data also shows a shift towards private employment.
“This shift to private practice has significant implications for the provision of planned care, on top of an already chronically understaffed SMO workforce,” Wild says.
“Based on a national survey of clinical directors, and accounting for access, quality, safety and unmet need, Aotearoa has a shortfall of approximately 1,140 public hospital SMO FTEs.
“The shortages mean access to hospital specialists across many specialties is declining. Te Whatu Ora data shows more than 68,000 patients were waiting more than four months for a first specialist assessment as of December 2023.
Anatomy of a health crisis
By the numbers
“That’s a 55 per cent increase in 12 months and an almost six-fold increase since (pre-Covid) September 2019.”
Beyond this, the report identifies the number of patients deemed unwell enough to exceed clinical thresholds for a commitment to be treated but who do not receive treatment within four months increased 600 per cent between July 2019 and September 2023, from 4,685 to 29,266.
“As access to hospital specialists declines, growing numbers of patients are left in limbo under the care of their GPs, adding further to the pressures on access to primary care services, as well as to the risks of patients’ condition deteriorating and their quality of life worsening,” Wild says.
“In Aotearoa, self-reported unmet need for GP services over a 12-month period is estimated by the New Zealand Health Survey at 34.3 per cent of the adult population. Limited official data shows a further 5.1 per cent adult unmet need for a hospital specialist.”
Unmet need drives up economic costs
While the specific economic costs of unmet health need are unknown, the broader economic costs of ill health are large. Costs outside of the health system were conservatively estimated by Treasury in 2010 to be between 2.7 and 7.6 per cent of GDP (about $10 billion to $30 billion today). The upper end of that range exceeds the annual Vote Health in the Government’s Budget.
“To assess the efficacy of a country’s health system, you need to know how many people have a need for health treatment that is not being met,” Wild says.
“The information presented in the ASMS report indicates Aotearoa New Zealand’s unmet health need is far more serious than comparable countries and warrants urgent investigation.
“Chronic workforce shortages, long waiting lists and cost-barriers to health care won’t be fixed until governments widen the policy lens on health and recognise that investing in wellbeing is also an investment in the economy.”
The full report is available at https://asms.org.nz/wp-content/ uploads/2024/04/ASMS-Anatomy-of-a-Health-Crisis-210416.pdf
JUNE 2024 PAGE 33
OVERCOMING PHOBIAS WITH VIRTUAL REALITY
Tackling phobias through virtual reality (VR) has seen a Christchurch startup land a major contract with the National Health Service in England.
oVRcome uses VR to help people tackle phobias – anything from spiders to flying. But now it is being used to help eliminate that anxiety of attending medical procedures, particularly for people with autism.
“The NHS came to us and said they have a problem of non-attendance from autistic people,” oVRcome chief executive Adam Hutchinson says.
“They worry about the procedure, the environment and often will just stay home instead of getting their treatment.
“Our technology allows them to experience what it will be like, how the interaction will unfold and prepare themselves for what it will be like when they arrive. This reduces the anxiety and stress of the unknown.”
People using oVRcome put on a headset which surrounds them in the local hospital environment. Procedures are filmed beforehand with a 360-degree camera, allowing the user to look around the room and witness the procedure being performed.
Patients can access a VR library via their smartphone.
“Users are offered an onboarding session to see how to use the headsets. Then they are lent a headset so they can try them out in the comfort of their own home,” Hutchinson said.
“The pilot with the NHS, which has been co-designed with members of the autistic community, will feature up to a hundred participants and is set to launch in August.

“The contract comes off the back of a small trial held in the UK in 2023, which displayed promising results.”
Hutchinson says the VR exposure therapy creates safe, immersive experiences for users and has many applications with vulnerable populations.
The technology was tested locally at Otago University through a clinical trial and showed a 75 per cent reduction in phobia symptoms after six weeks of using the oVRcome app. The phobia reduction technology is now used in 35 countries.
“Our goal with oVRcome is to make treatment for anxiety disorders easy and accessible for anyone who needs it, anywhere in the world,” Hutchinson says.
“The opportunity to design and develop our programme with users, for users, means that we can use this technology meaningfully and to its maximum impact.”
IN THE MEDIA: COMMITMENT TO HIRING CANCER SPECIALISTS QUESTIONED
Health New Zealand says it is working hard to recruit cancer care specialists but ASMS says the workforce data it is working form is “patchy and only partially reliable”.
“I have people in tears about the toll it’s taking on patients, and the toll it’s taking on their colleagues,” ASMS executive director Sarah Dalton told Stuff.
Stuff reported Minister of Health Shane Reti as saying he was confident recruitment efforts were adequate.
Dalton replied there is a lack of transparency from public health leaders about staffing constraints.
In March, Stuff made a request under the Official Information Act (OIA) to Te Whatu Ora for an overview of its recruitment activities for oncology-related services, broken down by district, for the past four years.
Recruitment campaigns for radiation oncology staff and radiologists were run at a cost of $29,039 in 2020. Recruitment campaigns for medical physicists, radiologists, medical oncology, haematology, and radiation oncology staff in 2021 cost $94,596.
Campaigns for radiation therapist and radiation oncologist roles in 2023 cost $94,466. Between January and March this year, $64,704 was spent on campaigns for the same roles.
Te Whatu Ora said the figures were for its own international recruitment centre and for Kiwi Health Jobs, an online platform that Te Whatu Ora jointly owns with the New Zealand Blood Service.
Te Whatu Ora unable to provide a districtlevel breakdown of recruitment spending for oncology-related services.
BRANCH OFFICERS HUI
The annual ASMS Branch Officers hui will be held on 21 June in the Oceania Room at Te Papa in Wellington.
This will be the first workshop since the conclusion of triennial branch officer elections earlier this year.
The hui will cover a range of important information for branch officers including an update on the development of claims for Te Whatu Ora bargaining, new research on the IMG workforce in New Zealand, and a review of the 2024 government Budget. There will also be education around the role of branch officers, particularly for people new to the role.
All branch officers who have not yet made travel arrangements are encouraged to contact sharlene.lawrence@asms.org.nz for assistance arranging travel to and from the event.
PAGE 34 THE SPECIALIST
MENTAL HEALTH GROUPS CALL FOR URGENT INVESTMENT IN OPEN LETTER TO MINISTER
An alliance of mental health organisations is urging the Minister for Mental Health Matt Doocey to invest in the Aotearoa New Zealand’s mental health system in an open letter.
The letter comes in response to the Government’s omission of mental health and addiction as priority areas in their Budget Policy Statement.
Around 260,000 New Zealanders live with moderate-to-severe mental illnesses and the demand for mental health services is steadily rising.
The 2018 He Ara Oranga Report of the Government Inquiry into Mental Health and Addiction found that “in addition to the human costs, the annual cost of the burden of serious mental illness, including addiction, in New Zealand is an estimated $12 billion or 5 per cent of gross domestic product.”
Dr Hiran Thabrew, Chair of Tu Te Akaaka Roa ¬ RANZCP New Zealand National Committee said we can’t afford to neglect mental health in the upcoming Budget.
“The most vulnerable are falling through the cracks because our system does not have the capacity to give them the support they desperately need.
“New Zealanders are struggling to access help in a system that is often disjointed, chronically understaffed and under resourced. How is that conducive to effective and therapeutic mental health care?

“On the other end is a workforce faced with immense stress, burnout and exhaustion due to heavy and unsustainable workloads.
“With dedicated funding for mental health and addiction, we can provide life-saving support to people with mental illnesses and addiction issues, reduce strain on our workforce and public health systems, and empower New Zealanders to lead fulfilling lives.
“There is also a strong economic case for investment in mental health – better mental health improves productivity, educational and professional outcomes, physical health, and overall wellbeing.
“We encourage the Coalition government to prioritise mental health care for our communities in the upcoming budget through targeted and sustained investment,” Dr Thabrew said.
Jodie Bennett from Changing Minds said, “We were very disappointed in the omission of mental health as a priority area in the latest Budget Policy Statement. This is an oversight our lived experience community expects answers on as a matter of priority.”
John Moore, CEO of Yellow Brick Road, said, “By investing in preventative wellbeing services and family and whānau focussed services we can reduce the number of individuals and whānau in crisis. Family and whānau are the largest provider of mental health support, by funding whānau focussed services we can support them to provide that care more effectively and keep themselves well at the same time.”
MORAL INJURY AMONGST THE WARDS
Moral injury stemming from caring for people about to die, and the flow-on effects to medical professionals’ mental health, is being explored in a PhD by Doctor Sinead Donnelly.
In the process of writing her thesis, Donnelly interviewed 93 doctors about traumas experienced in their work.
“I was really taken aback by all the challenges our doctors face. The moral injury that comes from not feeling there was the means to provide adequate care for someone who was dying stays with people,” Donnelly says.
“First-year doctors have to battle with this often. From ethical issues raised by families asking them to up the morphine as they want it over, through all that comes with a patient at the end of their life.
“The PhD looks at ways we can support junior doctors through this process. After hearing senior doctor stories, there are some that date back 20–30 years that still sit with them and affect them.”
Donnelly says the attitude that doctors have had to adopt in the current workforce crisis is likely contributing to the ongoing moral injury faced by doctors treating terminally ill patients.
“Doctors tell me the job is broken,” she said.
“You just have to roll up your sleeves and keep going. It is a moral injury.
Surgeons talk about intraoperative deaths on the table and the distress that it causes them. They have to sew the person up, speak to the family and there is no space to actually debrief themselves.
“There is this culture of staying in your armour and to keep soldiering on. One surgeon said we cannot care and cope. The system does not allow us to do both.
“There are so many stories now affecting so many people.”
Donnelly asked her interview subjects to consider what might work to support doctors through treating patients who pass away.
“It was not, we need lectures on self-help and ethics,” she says.
“It was about taking time. Taking a moment for the doctors to acknowledge a human being has died and that is a sad thing. Acknowledge if the passing was terrible and if it is causing distress. This is where the senior doctors need to step in, remove their armour and speak with the juniors. If a senior doctor sees how difficult a situation it is, it will validate a junior doctors’ feelings.
“It does not have to be a long time, just a moment to debrief.”
Unfortunately, Donnelly says the workforce shortages and pressures on doctors to see patient after patient make this almost impossible.
“Management of hospitals needs to acknowledge the humanity of its doctors and that they do extraordinary things.”
JUNE 2024 PAGE 35
DR SINEAD DONNELLY
PAID UNION MEETINGS FOR TE WHATU ORA STAFF
In the build-up to the renegotiation of ASMS’ largest collective agreement with Te Whatu Ora, ASMS is holding paid union meeting up and down the country in late June and July.
There will be 29 in person meetings, followed by three online meetings at the end of July. The meetings will include a presentation from either ASMS Executive Director Sarah Dalton or Industrial Director Steve Hurring, including the results of the online member survey run in May and a discussion of developing claims.
2,400 members competed the ASMS online survey.
At time of print the following dates and times for paid union meetings had been provided to Te Whatu Ora.
• Wairau – Thursday 27 June, 1-3pm
• Nelson – Monday 1 July, 11.30am-1.30pm
• Whangarei – Tuesday 2 July, 2-4pm
• Auckland – Thursday 4 July, 10am-noon
• Greenlane – Thursday 4 July, 2-4pm
• Middlemore – Friday 5 July, 10am-noon
• West Coast – Friday 5 July, noon-2pm
• Taupo – Monday 8 July, noon-2pm
• Lower Hutt – Tuesday 9 July, 10am-noon
• Rotorua – Tuesday 9 July, noon-2pm
• Tauranga – Wednesday 10 July, noon-2pm
• Wairarapa – Wednesday 10 July, 3-5pm
• Palmerston North – Thursday 11 July, 2-4pm
• Hamilton – Thursday 11 July, 2-4pm
• Whanganui – Friday 12 July, noon-2pm
• Whakatane – Friday 12 July, noon-2pm
• Christchurch – Monday 15 July, noon-2pm
• Hillmorton – Tuesday 16 July, 9.30-11.30am
• Burwood – Tuesday 16 July, 12.30-2.30pm
• Hastings – Tuesday 16 July, 2-4pm
• Timaru – Wednesday 17 July, 1.45-3.45pm
• New Plymouth – Thursday 18 July, noon-2pm
• Invercargill – Thursday 18 July, noon-2pm
• Queenstown – Friday 19 July, 12.30-2.30pm
• North Shore – Monday 22 July, 10am-noon
• Waitakere – Monday 22 July, 2-4pm
• Dunedin – Monday 22 July, 2-4pm
• Porirua – Tuesday 23 July, 2-4pm
• Gisborne – Wednesday 24 July, noon-2pm
• Wellington – Thursday 25 July, 10am-noon
Latest dates, times and locations will be available on the events page of the ASMS website. www.asms.org.nz/events
Following the conclusion of the in-person meetings, three online unpaid meeting will be held.
• Thursday 25 July, 5pm
• Friday 26 July, 5pm
• Tuesday 30 July, 5pm
Email events@asms.org.nz to express interest in any of the three online meetings and you will be sent a link closer to the date.



NEW NATIONAL SECRETARY SELECTED
Following the first meeting of the new National Executive, ASMS has a new National Secretary.
ASMS Executive Director Sarah Dalton says now it is a particularly good time to acknowledge the fantastic contribution of immediate past National Secretary Nathalie de Vries.
“Secretary is a key role with responsibility for record-keeping for all Executive meetings and, perhaps most dauntingly, presenting the annual report and audited accounts to Annual Conference each year,” says Dalton. “Nathalie did an impeccable job, being the face of that major accountability function at Conference and I wish her all the best in her new role as CMO for Whanganui district”.
While the roles of President and Vice President are elected directly on a national basis by the membership, the role of National Secretary is appointed by the members of the Executive from amongst their ranks.
The National Secretary for the 2024-27 terms is Region 1 executive member Andrew Ewens
KENEPURU CLARIFICATION
Following feedback from members, The Specialist believes it is important to make a clarification about in feature in the magazine’s last edition.
‘Kenepuru Hospital and the postcode lottery’ looked at ongoing threats to the future after-hours service of the Kenepuru Accident and Medical Clinic (KAMC).
It incorporated data around admissions to Kenepuru Hospital and presentations to KAMC. The story did not sufficiently clarify that admissions data is not only from the KAMC and that the figures are only a proxy for KAMC admissions overnight. In particular the spike of admissions between 7am and 8am could reflect admissions from other parts of the hospital.
BY THE NUMBERS: KENEPURU HOSPITAL AND THE POSTCODE LOTTERY The proposal late last year to close Porirua’s after-hours service at Kenepuru Hospital highlights the problems of the postcode lottery when comes to health care, and how lack of investment only exacerbates these issues. Late last year the threat of injunction from ASMS halted Te Whatu Ora’s plan to close its after-hours service at Porirua’s Kenepuru Te Whatu Ora collective agreement including the principles Te Whatu Ora’s proposal was close the accident and medical TeWhatuOrasaidtheyweremakingthemovebecauseof lackof However, they failed to consult with employed staff, the community, and unions before making their proposal. ASMS Executive Director Sarah Dalton minced no words with Te Whatu Ora management during meeting November where unions were told about the decision. “You have not consulted with our members, which is in breach of our collective agreement,” she said. “As result, we will be seeking an injunction to this decision immediately.” Afewdayslater,ASMSwastoldthat newlocumagencyhadbeen foundand,as result,Kenepuru’safter-hoursservicewouldhave temporarystayofexecution.Forhowlongwas,andremains,unclear. Wellington – about 30–35-minute drive. While Kenepuru does not have an ED, being open night prevents some patients having visit the EDs in Wellington or the Hutt Valley. As well as the 60,000 residents Porirua, Kenepuru serves the 55,000 people of the Kāpiti region further north more like 60-minute drive from Wellington Hospital. Ministerial briefing papers obtained under the Official Information Act (OIA) show other options to bring registrars from Wellington Hospital Kenepuru were declined because Wellington was already short-staffed and oversubscribed. Regional Hospital KAMC [Kenepuru Accident and Medical Clinic] overnight as it is service that already under significant and one of the lowest compliances with SSED [Shorter Stays Emergency Departments] the country,” the document reads. “Ontopofthat,theEDrosterwillhaveupto vacanciesbyDecember andaverages to unfilledshortnoticegapsperdayalready.” Dalton says this is an example of “blinkered thinking” when comes to patient demand. “The patients who cannot be seen at Kenepuru Hospital will inevitably turn up at Wellington Hospital, which is already oversubscribed and facing long wait times. “WeshouldbelookingatwaystoalleviatethedemandonWellington Whetherthatisbykeepingtheafter-hoursopenorinvestingin anotherED reduceWellington’sload. ADMISSIONS AROUND THE CLOCK We should be looking at ways to alleviate the demand on Wellington Hospital, and Kenepuru could play a large part in doing that.” 1,000 TimeofDay Midnight 2pm 4pm 6pm 8pm 10pm 1pm 3pm 5pm 7pm 9pm 11pm 24 30 1675 862 511 724 434 313 251 237 144 59
PAGE 36 THE SPECIALIST
NATHALIE DE VRIES ANDREW EWENS
ASMS SERVICES TO MEMBERS
As a professional association, we promote:
• the right of equal access for all New Zealanders to high quality health services
• professional interests of salaried doctors and dentists policies sought in legislation and government by salaried doctors and dentists.
As a union of professionals, we:
• provide advice to salaried doctors and dentists who receive a job offer from a New Zealand employer
• negotiate effective and enforceable collective employment agreements with employers. This includes the collective agreement (MECA) covering employment of senior medical and dental staff in DHBs, which ensures minimum terms and conditions for more than 5,000 doctors and dentists, nearly 90% of this workforce
• advise and represent members when necessary
• support workplace empowerment and clinical leadership.
ASMS JOB VACANCIES ONLINE
Check out jobs.asms.org.nz a comprehensive source of job vacancies for senior medical and dental specialists/consultants within New Zealand hospitals and health services.
CONTACT US
Association of Salaried Medical Specialists
Level 9, The Bayleys Building, 36 Brandon St, Wellington
Postal address: PO Box 10763, The Terrace, Wellington 6140
P 04 499 1271
E asms@asms.org.nz W www.asms.org.nz
FOLLOW US /asms.nz /ASMSNZ
Have you changed address or phone number recently? Please email any changes to your contact details to: asms@asms.org.nz
If you have reason or need to seek a reduction or waiver to your annual subscription, please write to us. Our constitution allows for this in certain circumstances. Emails should be addressed to sarah.dalton@asms.org.nz
ASMS STAFF
Kettley
Director Sarah Dalton COMMUNICATIONS
Communications Advisor
Chick
Advisor Matt
INDUSTRIAL
Director Steve
Industrial Officers
Kris
Industrial Officers David
Chan
Adam
Jenny
Sarah Thompson Kirsty
POLICY & RESEARCH Director of Policy and Research Harriet Wild Principal Policy Advisor Virginia Mills Health Policy Analyst Lyndon Keene Industrial Research Advisor Louie Hancock SUPPORT SERVICES Manager Support Services Sharlene Lawrence Finance and Technical Support Advisor Vanessa Wratt Membership Officer Saasha Manson
Services Administrator Danni Mackay
Executive
Senior
Andrew
Journalist/Communications
Shand
Industrial
Hurring Senior
Ian Weir-Smith
Smith
Dixon
Craigie
Chapman
Macnab
Support
MAS is a membership-based insurance and investment company for New Zealand professionals. We offer a range of general insurance, life insurance, income protection and KiwiSaver options to protect everything that’s important to you and your family.
The MAS Retirement Savings Scheme is recognised by Te Whatu Ora Health New Zealand and the Royal New Zealand College of General Practitioners as a workplace savings option. The MAS Retirement Savings Scheme is also a recognised Overseas Pension Scheme for UK pension transfers.
Find out more at mas.co.nz or call us on 0800 800 627.

MAS is a proud supporter of ASMS