Self Administration Manual Welcome to

This administration manual is intended to provide guidance to you and your employees in the areas listed in the Table of Contents on the following page.
TABLE OF CONTENTS
1.Contact Information 2.Website Login 3.Enrollment Information 4.Explanation of Benefits and Appeals Process 5.Monthly Invoices and Month End Reports 6.Enrollee Questionnaires and Forms 7.SBC Guidelines 8.Miscellaneous
CONTACT INFORMATION
Sales and Retention Department
Company representatives* should contact the Sales and Retention Department to request new enrollment packets and any other issues not listed below.
Phone: 330-363-6390
Fax: 330-454-7845
Service Center
Company representatives and employees should contact the Service Center for questions regarding benefits that your plan covers or an outstanding claim. An AultCare Service Representative is available Monday through Friday 7:30 am to 5:00 pm.
Phone: 330-363-2050 / 855-270-8497
Fax: 330-363-7717
Billing Department
Company representatives may contact the Billing Department with questions in regards to monthly invoices.
Phone: 330-363-6360
Fax: 330-363-5012
Member Services/Eligibility Department
Company representatives may contact the Member Services/Eligibility Department with enrollment questions.
Phone: 330-363-6360
Fax: 330-363-7746
Email: aultcareeligibility@aultcare.com
Visit our website at www.aultragroup.com
representatives are individuals authorized to request information on behalf of the company.
*Company
WEBSITE LOGIN
Attachment #1: Employer Account Registration Guide
Attachment #2: File Retrieval Guide
Attachment #3: Member ID Card Retrieval Guide


AULTRA
WEBSITE EMPLOYER GUIDE
Employer Account REGISTRATION GUIDE
Welcome
Welcome to our Aultra family. Whether you are a new client, or have been with us for many years, we are proud to assist you managing your employer account.
We have created an area on www.aultragroup.com designed just for you. You can use the online account to retrieve monthly reporting and invoices send us files, view your group’s eligibility, order ID cards, and more.
To get started, you and each authorized representative, must register for a secured, online account. Once you have created an online account, use this document to learn how to retrieve files from your online account.
If you have questions, you can contact your Account Coordinator, Account Executive, or for technical assistance, email the Aultra Web Team at AultConnect@AultCare.com.
Helpful links:
• Frequently Asked Questions
• Website How to Guides
Thank you, Your Aultra Team

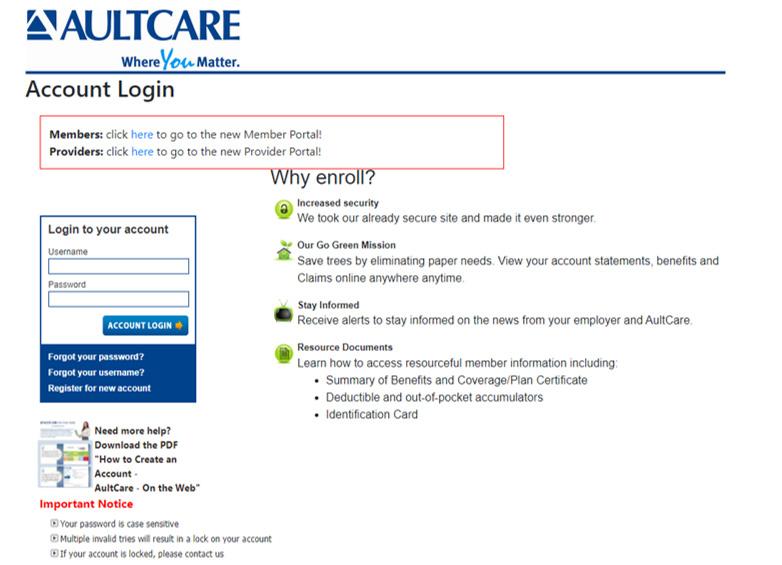
CREATING YOUR EMPLOYER LOGIN ON THE AULTRA WEBSITE

• Open a web browser and go to www.aultragroup.com.
• Click the Account Login button towards the middle of the page.
1
• Then click on the “Register for a new account” link.

• Select “Employers” as your “Membership Type” and click on the “SIGN UP NOW” button.

AULTCAREEMPLOYERACCOUNTREGISTRATIONGUIDE
Select “Employers” as your “Membership Type” and click on the “SIGN UP NOW” button.

2
1. Select “I Agree” to agree with the “Terms of service” outlined on this page.
2. By entering your name next to the “By” textbox, you are signing your signature.
Step # 1
You must agree with our “Terms of Service” before you can create an account with us.
Click on “CONTINUE” button to proceed.
1. Select “I Agree” to agree with the “Terms of service” outlined on this page.
2. By entering your name next to the “By” text-box, you are signing your signature.
Click on “CONTINUE” button to proceed.
Step # 2
Enter the following information
Your first name
Your middle initial
Your last name

A phone number where we can reach you
The title of your position at your company
Click on “CONTINUE” button to proceed.

Step # 2
Enter the following information

• First Name
• Middle Initial
• Last Name
• A phone number where we can reach you
• The title of your position at your company
Click on “CONTINUE” button to proceed.
AULTCAREEMPLOYERACCOUNTREGISTRATIONGUIDE
3
STEP #3
1. Enter the 9 digit Tax ID number of your company (without the dash)
2. Enter the name of your company
3. Enter the street address, city and state of your company
Adding Group Numbers
1. Enter the Group Number of your company
2. Click “Add” button
3. The Group Number will then appear in a list box underneath
4. If you need to add more groups, repeat the steps in this section
the following information: for your account enter a username, the system will tell you if it is already taken or not. If the is already taken, please choose and enter a different username. for your account password that you choose should consist of: characters least one uppercase character and one lowercase character least one number
Optional
If you already know someone at Aultra (e.g Account Coordinator), you can help us expedite the verification process for your employer account by supplying the following ”optional” information:
1. Enter your phone number
2. Enter the name of the person you know at AultCare;
Click

2. Enter the name of the person you know at Aultra; (e.g., Group Account Coordinator)
email address enter correct email address. We will use this email to communicate with you.
Click on “CONTINUE” button to proceed.
security questions with answers select your security questions carefully. We will ask you these questions if you forget username and/or password. CONTINUE” button to proceed.
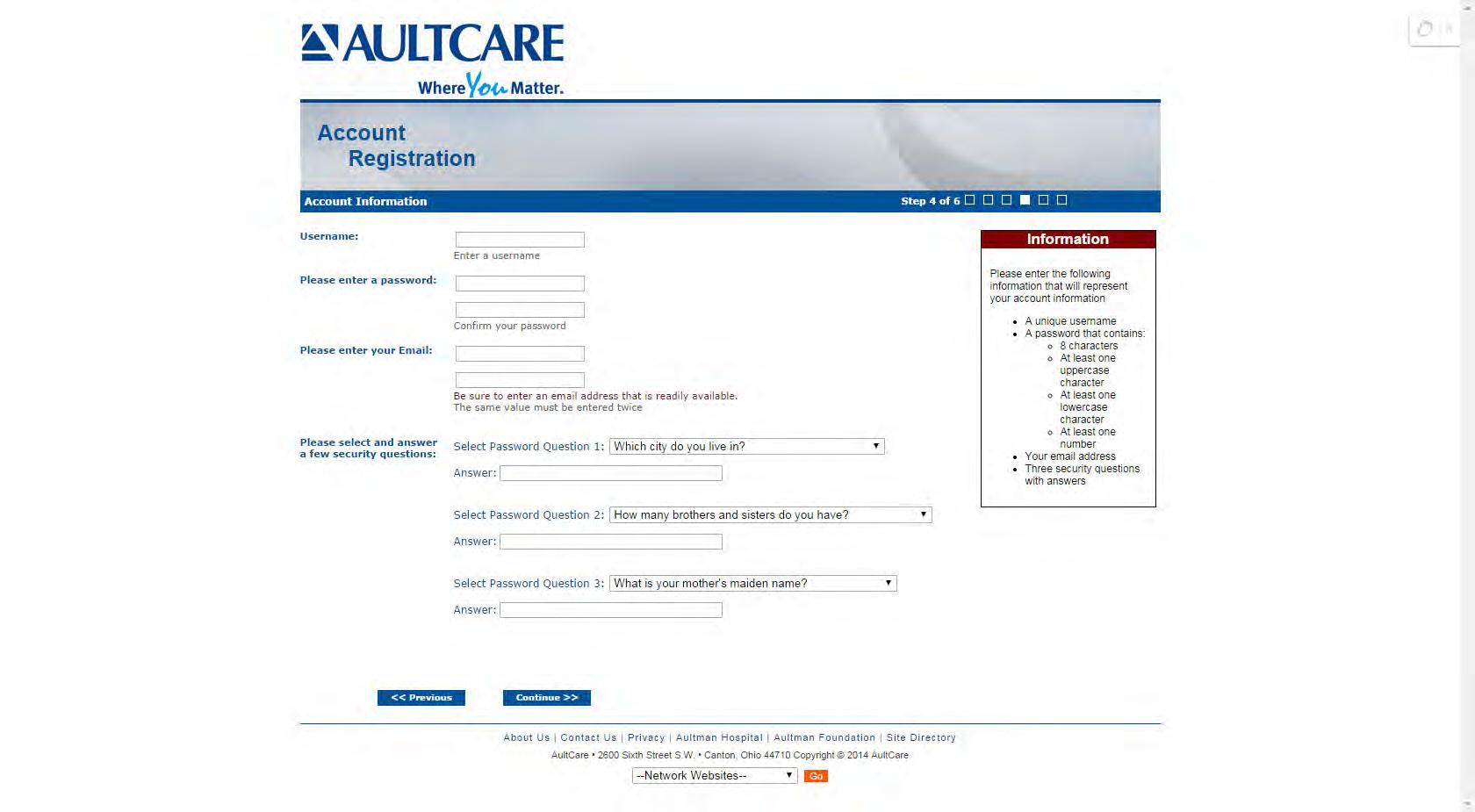
STEP # 4
Enter the following information:

Username for your account
When you enter a username, the system will tell you if it is already taken or not. If the username is already taken, please choose and enter a different username.
8
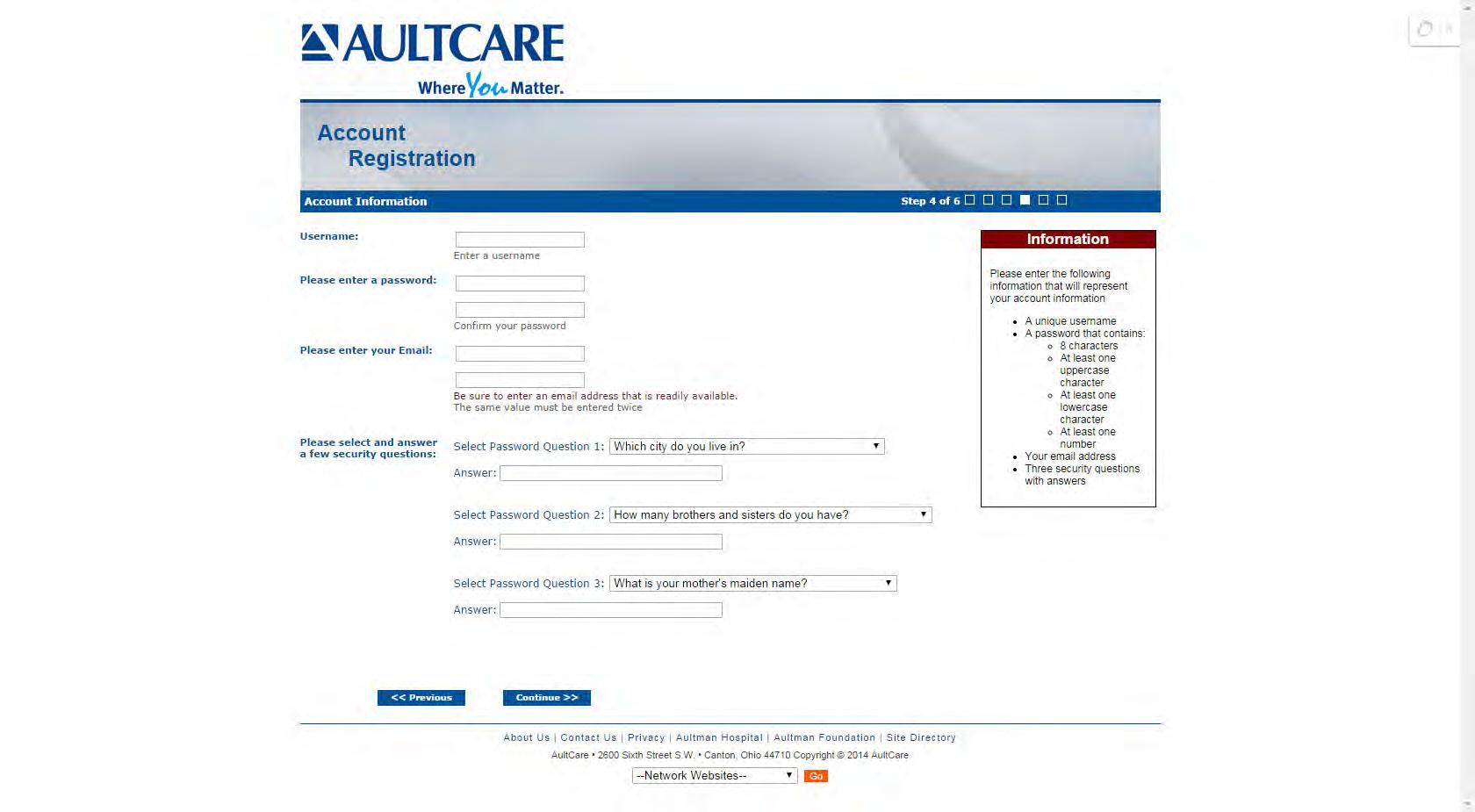
Password for your account
The password you choose should consist of:
» 8 characters
» At least one uppercase character and one lowercase character
» At least one number
Your email address
Please enter your email address. We will use this email to communicate with you.
Three security questions with answers
Please select your security questions carefully. We will ask you these questions if you forget your username and/or password.
Click on “CONTINUE” button to proceed.
(e.g.
Group
on
CONTINUE” button to proceed.
“
AULTCAREEMPLOYERACCOUNTREGISTRATIONGUIDE 9
4
Step #
Reason for requesting access
Select your reason(s) for requesting access. You can select more than one reason.

2. SFTP IP Addresses
If you will be using secure FTP transfer in addition to our website , please list the IP address(s) that will be used.
3. Authorization to represent your company Select “I Agree” to state you are an authorized representative of the company you are applying for this account.
Sign your name electronically by entering your name in “ By ” textbox.
Optional on this page
If you need to send us a message or have a question, enter it in the comments box.
Click on the “CONTINUE” button to proceed.

5 1.
5
an authorized
AULTCAREEMPLOYERACCOUNTREGISTRATIONGUIDE
I, John Smith, am
representative of X Company.
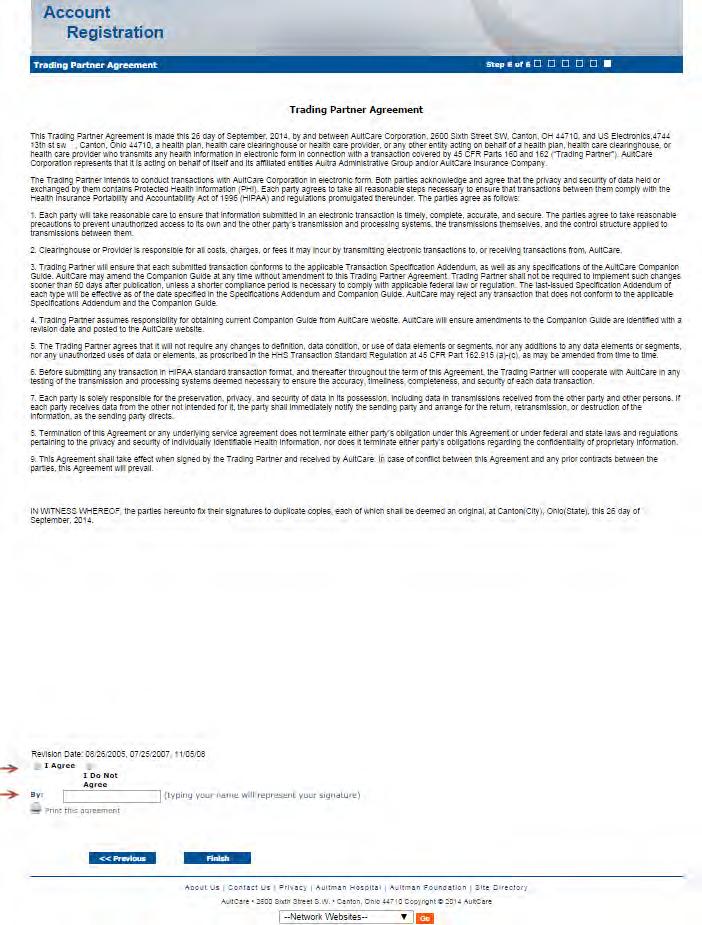
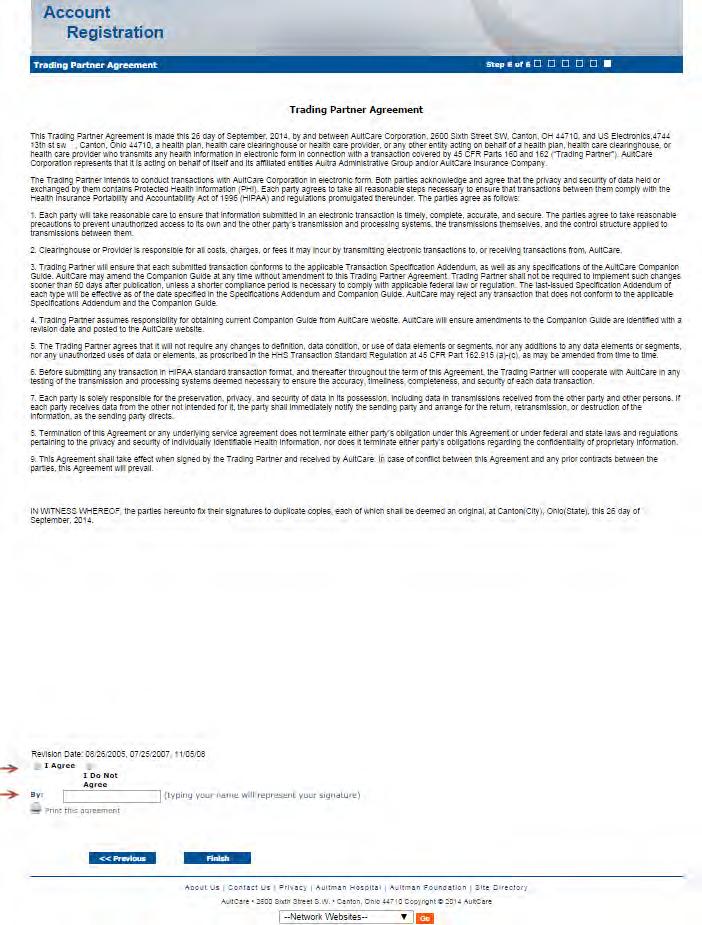
Step # 6
This is the final page of your account registration process. You must agree to the Trading Partner Agreement specified on this page. You can print this agreement by clicking on “Print this agreement.”
From this page:
1. Select “I Agree” to agree to the “Trading Partner Agreement” outlined on this page.
2. Indicate your approval by entering your name in “By:” textbox.
Click on the “FINISH” button to proceed.

Upon successful completion of your account registration, you will see the following message:
12
Thank you for the submission of your registration request. You will receive an email advising on the next steps to complete the process.
What to expect next?
• Upon completion of the registration process, you should receive an email stating the registration process has been completed. (Note: At this time, your account is not active yet)
• We will review the application and finish with the account setup process.
• When your account setup has been completed, you will receive an email informing you your account has been set up and is ready for use. (Note: At this time, the process is complete, and you will be able to login to our website)
If you have questions, you can contact your group coordinator, or for technical assistance, email the Aultra Web Team at aultconnect@aultcare.com
6


Aultra EMPLOYER FILE AND ID CARD RETRIEVAL GUIDE

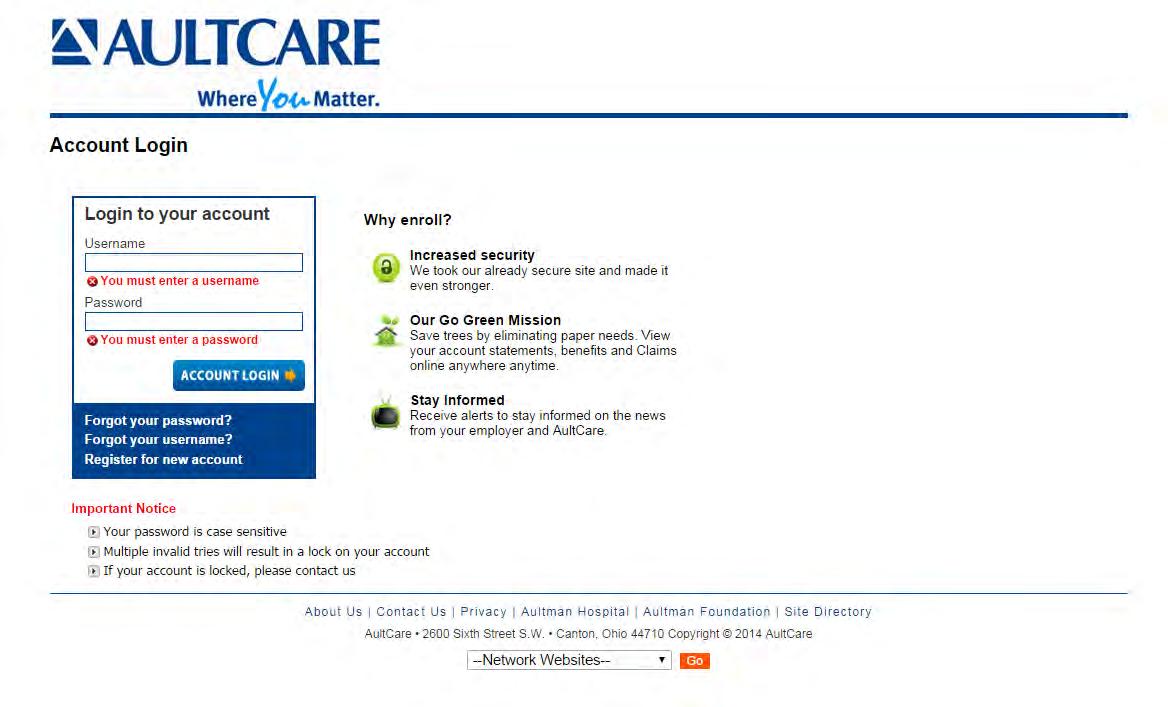
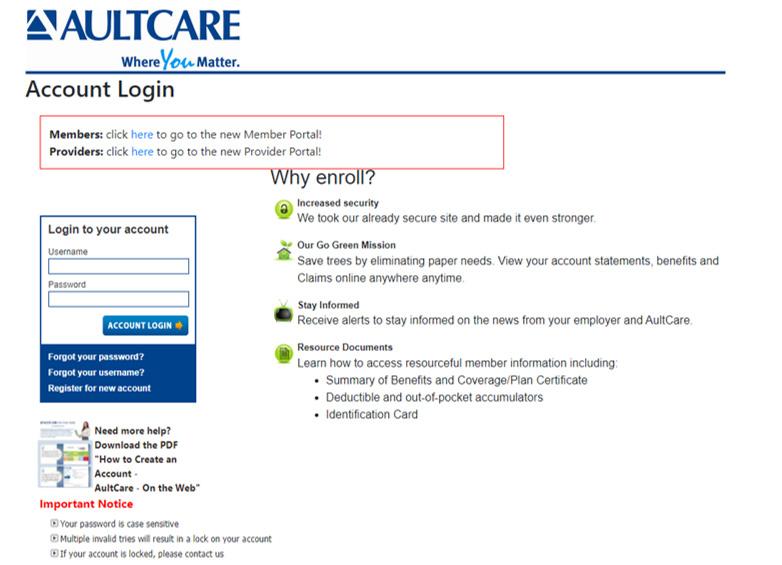
1. Visit www.aultragroup.com.
2. Select Employer Resources and click Account Login

3. Enter your username and password. Click Account Login to access your account.
4. You must have an online account to retrieve files. Select Register for new account if you do not have an account.
.
How to retrieve your monthly files on the Aultra website
1

My Dashboard
Once you are logged into your account, your dashboard will appear. All links associated to your account will be displayed. In the screenshot below, three main areas have been identified.
• Location A lists the last three (3) files Aultra has posted for you. These are on your dashboard so you can easily view these files.
• Location B is a link. This link will take you to your Secure FTP Center. The FTP Center allows you to download all files Aultra uploaded to your account. This is where you can upload files to Aultra.
• Location C is a link similar to Area B. It will take you to the same place and files as Location B.

2

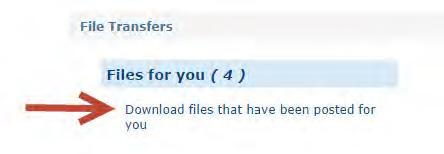
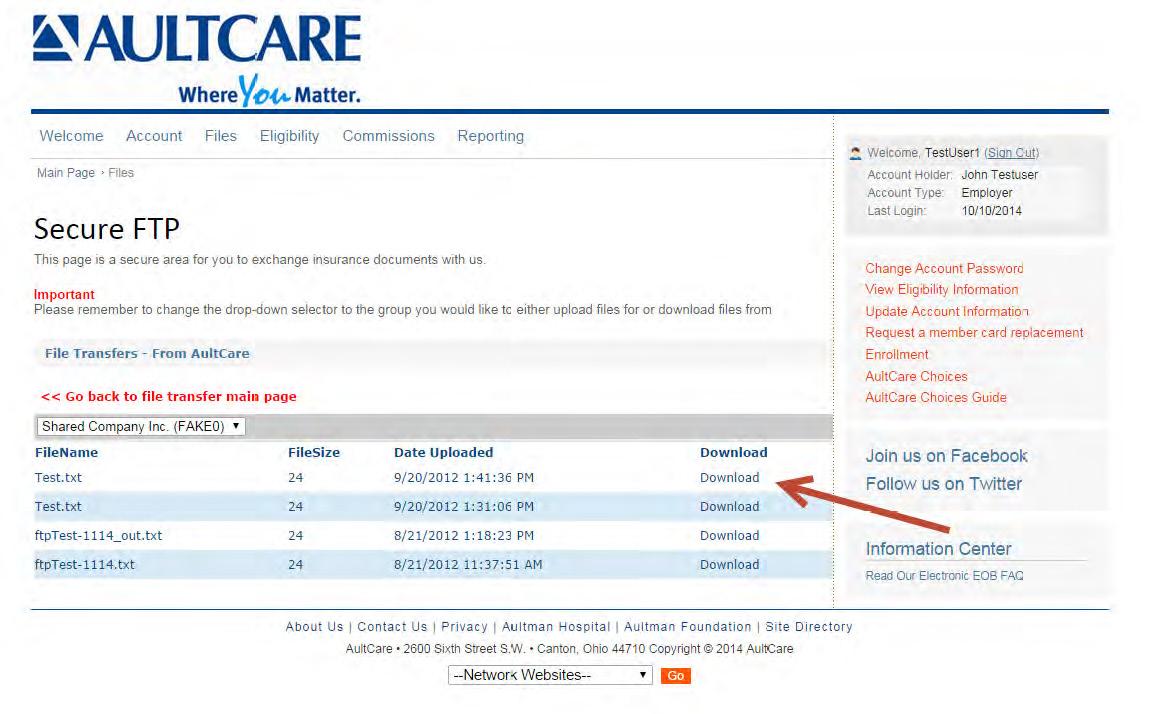
Secure FTP Center
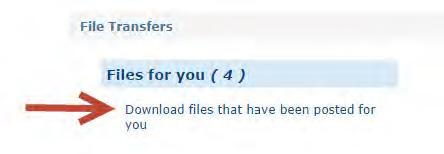
When you click on the Files link from your dashboard (Location C in the example) you will be directed to the Secure FTP Center (see image below). You will see two links: Files for you and Files from you.
VIEWING YOUR FILES
Files for you
This link will show all of the files Aultra uploaded to your account. Retrieve your files by clicking on this link. The number displayed is the number of available files.
UPLOADING FILES TO SEND TO AULTRA
Files from you
This link will take you to a page where you can upload files to Aultra.

3
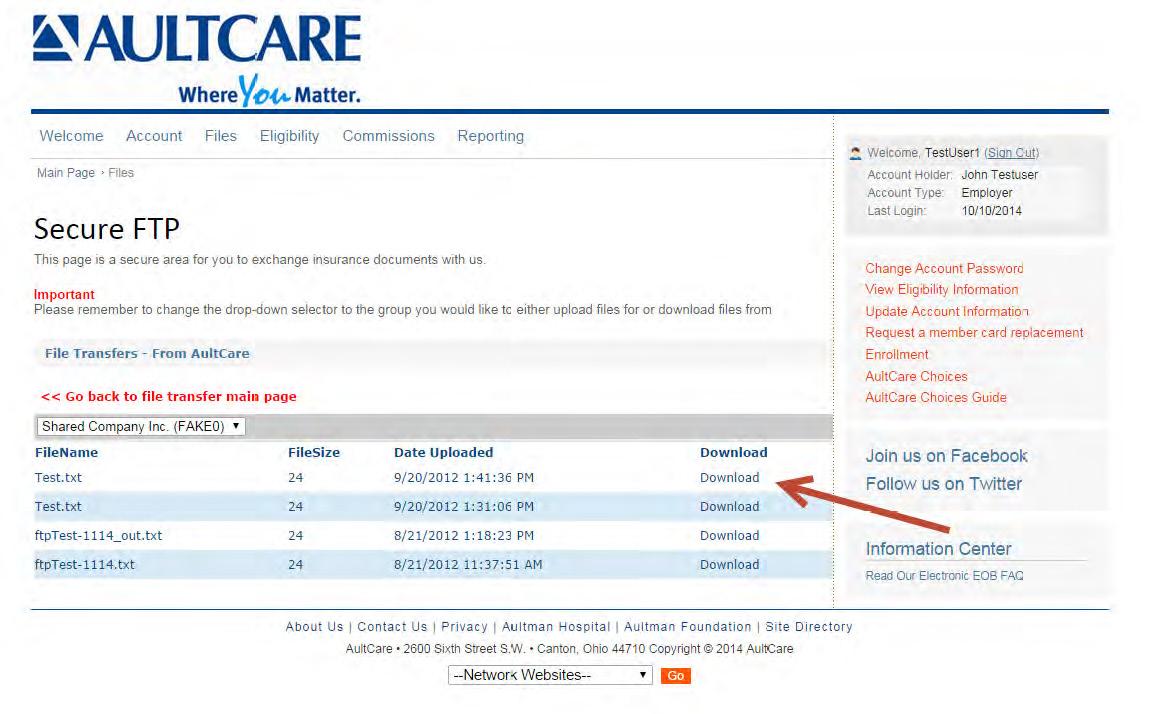
Downloading a File
Step #1
Click on the text labeled Download files that have been posted for you
Step #2
When you click the link, a dropdown list will appear. From the list, select the group name to view files. (Based on your authorization, only those particular group names will be displayed.)

Step #3
For employers who have more than one Aultra account, select the appropriate account from the drop down box.

4

Step #4
Once you see a list of files, click on the Download link to view/download it on your computer.
5
Uploading a File
1. Click the link labeled Click here to upload files.

An example of the upload center is shown to the right.


2. Select the group number associated with your file upload.
3. Select the specific file type.
4. Browse for the file you want to upload on your computer.
5. Select Upload.
Previously Uploaded Files
You can also see files previously uploaded.
If you have questions, contact your group coordinator, or for technical assistance, email the Aultra Web Team at AultConnect@AultCare.com.
6

Step #1
Log in to your employer secured account and select Eligibility.

Step #2
Click Search to view a list of active members. Member ID Cards on the Employer Portal

7
Step #3
Select a name to view the member’s ID card.


Step #4
To view a copy of the member ID card, select this link: Member Card click here.




www.aultcare.com PCP Co-Pay $ Specialist Co-Pay $ Member Employer: Group #: Member: Member ID: Effective: Rx Claims: Rx Bin: Rx PCN: Rx Group: Issuer: For Pharmacy Help Desk 888-219-3164 In-Network Ded Ind/Family $ Out-of-Network Ded Ind/Family $ In-Network OOP Ind/Family $ Out-of-Network OOP Ind/Family $ Pharmacy Plan Medical Plan da : Mail: AultCare P.O. Box 6910 Canton, OH 44706 Claims Submission Customer Service/Eligibility This card is not a guarantee of coverage. For verification and coverage details call 330-363-6360 or 1-800-344-8858 weekdays, 7:30 AM to 5:00 PM. Hearing Impaired: Call 711 PRECERTIFICATION is required for all elective admissions and within two working days following an emergency admission. For preadmission certification, call Utilization Management at 330-363-6397 or 1-800-344-8858 weekdays, 8:30 AM to 5:00 PM. Benefits may be reduced if this does not occur. 7525/22 8 www.aultragroup.com Aultra
ENROLLMENT INFORMATION
The following information is provided to explain the process of enrolling and terminating employees and/or dependents. In order to ensure timely enrollment of new eligible employee, please complete and return the membership report and group employee application.
Attachment #1: Step-By-Step Guide
This guide was created to assist with the completion of enrollment application/change form. The text denoted in red provides additional information to help understand what information is being requested.
Attachment #2: Enrollment Application
All new employees and those employees requesting a change in their coverage, must complete this entire form, unless otherwise instructed, to prevent delays.
Any questions you have as you complete this form may be directed to Customer Service.
Once completed, these forms may be mailed to: AultCare
Eligibility Department PO Box 6910 Canton, OH 44706
It may also be faxed directly to our eligibility Department at 330-363-7746. All changes must be received by the 10th of the month to be reflected on your next bill.
Attachment #3: Cancellation and Continuation Form
Please indicate all cancellations on this report. Do not make changes on the monthly premium statement. Utilize transaction codes for each change. Include enrollment form where indicated and provide within 31 days of event. (Signed enrollment forms must include spouse's signature when applicable.
Attachment #4: HIPAA Disclosure Form Notice of Privacy Practice Member Guide Letter
The attached enclosures must be given to any potential AultCare enrollee in addition to the Group Employee Application so that the person understands portability and creditable coverage.
Attachment #5: Getting the Most from your Healthcare plan
Guide for Completing the Enrollment Application/Change Form
Please complete this form in its entirety.
EMPLOYER USE ONLY
This section is to be completed by the employer representative.
Employer Group Numbers
List all Aultra group numbers that apply. (Medical, Dental, Vision)
Employee Location/Job Classification
Use this section to designate an employee classification, if needed. These designations should be set-up as rate codes during the implementation of your plan.
(Example: hourly vs. salary; executive or management; physical plant location.)
Leased Network
Designate if the employee is accessing an out-of-area network. (Cigna, First Health Network, etc.)
Aultra Effective Date
Provide the date the coverage is set to begin.
EMPLOYEE COVERAGE ELECTION
This section is to be completed by the employee.
A) NEW POLICY APPLICATION
New Group New Hire Open Enrollment
Waiving Coverage
Designate the reason for applying for coverage or if coverage is being waived. If waiving coverage, a signature is required on the back of this form.
Qualifying Event — Explain:
If applying for coverage for a qualifying event, please provide a detailed explanation. (For example: spouse lost coverage, marriage, birth, adoption.)
Hire Date
If the original hire date is not available, please provide the month and year.
Coverage Type(s) Requested:
Check All that Apply Medical Dental Rx
Vision STD Life Flex HSA HRA
Be sure to check all benefit options being elected.
Plan Requested: Plan Name
Use this section to designate the employee’s plan election. (Example: PPO, HDHP or OPT 1, OPT 2, etc.)
ADDITIONAL COVERAGE FOR DEPENDENTS
This section is to be completed by the employee.
A(dd), C(hange), D(elete)
Please provide the reason code for enrolling or disenrolling dependents.
Social Security Number SSN are required for all dependents with coverage.
Benefits Selected (M,D,V,R)
List all that apply.
Other Insurance Coverage? (Y/N)
If yes, please complete the other coverage information on the back of this form.
OTHER COVERAGE INFORMATION
This section is to be completed by the employee if any covered persons have other health insurance coverage.
MEDICARE INFORMATION
This section is to be completed by the employee if any covered persons are enrolled in Medicare.
OTHER INFORMATION
This section is to be completed by the employee to designate any specified needs.
All Employees
Signature______________ Date __________
Employee must sign and date when electing coverage.
Employees Waiving Coverage
Reason for waiver of coverage: ______________
Employee and spouse must provide reason for waiving coverage.
Signature______________ Date __________
Employee and spouse must sign if either are waiving coverage.
Please submit this form to Aultra by one of the following methods:
Email: aultcareeligibility@aultcare.com |
Fax: 330-363-7746 | Mail: Aultra Member Services
PO Box 6910 Canton, OH 44706
Employer to send completed form to Aultra by one of the following methods.
7032/20
Enrollment Application/Change Form without
Employer Employer Name Group Numbers Employee Location/ Leased Network Aultra Job Classification Yes No Effective Date AULTRA USE ONLY Date Completed Completed By Card Sent EMPLOYER USE ONLY M - Medical D - Dental V - Vision R - Prescription ADDITIONAL COVERAGE FOR DEPENDENTS A(dd), C(hange), D(elete) Relationship to Enrollee First Name M.I. Last Name (If different from employee) Social Security Number Benefits Selected (M,D,V,R) Gender (M or F) Date of Birth Other Insurance Coverage? (Y/N) Date of Qualifying Event (Qualified enrollment must be made within 31 days of event) A) NEW POLICY APPLICATION New Group New Hire Open Enrollment Waiving Coverage You Only You & Your Spouse You & Your Child(ren) You, Your Spouse & Your Child(ren) Qualifying Event — Explain: B) EMPLOYEE INFORMATION Last Name First Name Middle Initial Suffix Gender Male Female Date of Birth Social Security Number Home Address Zip (Number & Street) County City State Code Preferred Email Primary Care Physician Name Phone Number Address (HMO Only) Marital Status Married — Date of Marriage Single Widowed Divorced Separated Employment Currently on Hire Hours Worked Are you currently actively at work? Status Full Time Part-Time Retired COBRA Date Per Week Yes No If not, why? Coverage Type(s) Requested: Plan Requested: Check All that Apply Medical Dental Rx Vision STD Life Flex HSA HRA Plan Name EMPLOYEE COVERAGE ELECTION 8128/24
Medical Questions
IMPORTANT INFORMATION
Upon your effective date with this plan, will you or any of your family members have other health insurance? YES NO
If yes, what is the name of the other insurance company?
If yes, what type(s) of other health insurance will you have? Check all that apply Medical Dental Rx Vision
Do you or your spouse or any enrolled dependents have Medicare coverage? YES NO If yes, please provide information below.
Do you have Medicare Part D coverage? YES NO If yes, what is the effective date of your coverage?
Do you, or any of your dependents, have any cultural or linguistic needs? YES NO
If yes, what are they?
Ethnicity: Non-Hispanic/Latino Race: White Black American Indian/Alaska Native Language: English Spanish Hispanic/Latino Choose not to answer Asian Native Hawaiian/Pacific Islander Other _________________________ Choose not to answer
RELEASE OF INFORMATION/PLEASE READ CAREFULLY
I am applying for group health coverage through Aultra Administrative Group and its related entities (“Aultra”). I acknowledge the coverage for which I am applying is subject to eligibility requirements and the terms of the policy. I acknowledge that I have read and understood all of the information contained within this document. Additionally, I acknowledge that all information that I have entered in this application, to the best of my knowledge, is complete, true, and accurate. I understand that any attempt to mislead or defraud Aultra is considered insurance fraud.
INSURANCE FRAUD WARNING:
Any person who, with intent to defraud or knowing that he or she is facilitating a fraud against an insurer, submits an application or files a claim containing a false or deceptive statement is guilty of insurance fraud.
I acknowledge that Aultra may use and disclose my protected health information, as well as, the protected health information of my family for payment, treatment, and operations. This information may be disclosed to other insurance companies, third party administrators, state and federal agencies, health care providers and other organizations and persons that perform professional, business, or insurance functions for Aultra, as permitted by state and federal law.
The information may be used for, but not limited to, processing enrollment applications, risk classifications, detecting or preventing fraud, internal and external audits, claims administration, case management, quality improvement programs, public health reporting, law enforcement investigations, coordination of benefits, medical management programs, and subrogation.
Medicare
Medical Effective Date Enrollee
ID
(Part A) (Part B)
Medicare
Hospital Effective Date
Name
Number
INFORMATION
MEDICARE
OTHER COVERAGE INFORMATION
OTHER INFORMATION
All Employees
I have read all of the statements contained in this application and declare that by signing this application the information I have provided is true and complete to the best of my knowledge. Electronic Signature Disclaimer: Please be advised that Aultra will not deny the enforceability or effect of an electronic signature solely because it is in an electronic format. Any valid signature provided in this section shall have the same legal effect and enforceability as a manually executed signature. I authorize deduction from my wages, as necessary, for any required premium for the coverage for which I have applied.
Signature Date
Employees Waiving Coverage
I have read all of the statements contained in this application and declare by signing that the information I have provided is true and complete to the best of my knowledge. I understand that I am eligible to apply for coverage through my employer. And I acknowledge that, subject to the terms and conditions of the policy, by waiving coverage at this time, I may not be able to enroll myself or my family again until the next annual enrollment period or a special enrollment period. I hereby decline coverage for (check all that apply): Myself Spouse Child(ren)
Reason for waiver of coverage:
Signature Spouse Signature Date
Per the 2015 FTC TCPA, Aultra or a vendor of Aultra, may contact you for demographic, satisfaction, and/or medical care management information in accordance with its obligation under Federal Law.
Please submit this form to Aultra by one of the following methods:
Email: aultcareeligibility@aultcare.com | Fax: 330-363-7746 | Mail: Aultra Member Services PO Box 6910 Canton, OH 44706
Cancellation/Continuation Notification
Please indicate all cancellations on this report. Do not make changes on the monthly premium statement. Utilize transaction codes for each change. Include enrollment form where indicated and provide within 31 days of event. *Signed enrollment forms must include spouse’s signature when applicable.
TRANSACTION CODES
Cancellation of Coverage:
A. Cancellation – Left Employment/Termination (Include in Comments section Termination Date & if Voluntary, Involuntary or due to Gross Misconduct)
B. Cancellation – Deceased (Specify Date of Death in Comments section)
C. Cancellation – Layoff (Include in Comments section the Date of Layoff & if Voluntary or Involuntary)
D. Cancellation - Waiving (Specify in Comments if waiving coverage, include Enrollment Form with waiver section signed*.)
E. Cancellation – Reduction in hours: no longer meets minimum eligibility requirements
Continuation of Coverage:
F. COBRA Coverage Elected (Include Expiration Date, Copy of signed election form & proof of first payment) (This is not necessary if Aultra administers the COBRA)
G. State Continuation of Coverage (For employers under 20 – please indicate expiration date of State Continuation of Coverage in the Comments section. Please include a signed Continuation of Coverage Election Form.)
Other:
H. Other (Include detailed explanation)
I understand Aultra is relying on my answers to the above questions to ensure overall compliance for my group health plan. I certify the answers are true to the best of my knowledge and belief. I also understand I am responsible for promptly notifying Aultra if any information changes.
Please submit this form to Aultra by one of the following methods:
Email: aultcareeligibility@aultcare.com | Fax: 330-363-7746 | Mail: Aultra Member Services PO Box 6910 Canton, OH 44706
Please contact Customer Service with any questions: 330-363-2050
ID NUMBER TRANS. CODE COVERAGE TYPE M-Medical, D-Dental, V-Vision COMMENTS Today’s Date: Employer: Group Numbers: Completed By:
EFFECTIVE DATE OF TRANSACTION EMPLOYEE NAME LAST,FIRST,M.
7033/20

Notice of HIPAA Special Enrollment Rights
We would like to take this opportunity to advise you of an important provision in your health care plan. To participate, you must complete an enrollment form. Dependent upon which specific plan you wish to enroll in, you may have to pay part of the premium through payroll deduction.
Additionally, HIPAA requires that we notify you of the “Special Enrollment Provision”.
Special Enrollment Provision
Loss of Other Coverage. If you decline enrollment for yourself or for another eligible dependent (including your spouse) while other health insurance or group health plan coverage is in effect, you may be able to enroll yourself and your dependents in this plan if you or your dependents lose eligibility for that other coverage (or if the employer stops contributing toward your or your dependents’ other coverage). However, you must request enrollment within 30 days after your or your dependents’ other coverage ends (or after the employer stops contributing toward the other coverage).
New Dependent by Marriage, Birth, Adoption, or Placement for Adoption. In addition, if you have a new dependent as a result of marriage, birth, adoption, or placement for adoption, you may be able to enroll yourself and your new dependents. However, you must request enrollment within 30 days after the marriage, birth, adoption, or placement for adoption.
To request special enrollment or to obtain more information about the plan’s special enrollment provisions, contact your AultCare Service Center at 330-363-6360 or 1-800-344-8858
Procedures for Requesting Certificate of Creditable Coverage/Certificate of Health Plan Coverage
HIPAA requires that plan sponsors and/or insurers provide a Certificate of Creditable Coverage/Certificate of Health Plan Coverage (HIPAA Certificate) to each individual who requests one, so long as it is requested while the individual is covered under the AultCare Health Plan or within 24 months of the individual’s coverage under the AultCare Health Plan ending. The request also can be made by someone else’s behalf for an individual. For example, an individual who previously was covered under the AultCare Health Plan may authorize a new plan in which the individual enrolls to request a certificate of the individual’s Creditable Coverage/Health Plan Coverage from the AultCare Health Plan. An individual is entitled to receive a Certificate upon request even if the AultCare Health Plan has previously issued a Certificate to that individual.
Requests for Certificates should be directed to AultCare Corporation, Attn: Member Services, P.O. Box 6910, Canton, Ohio 44706-0910 or by calling your AultCare Service Center at 330-363-6360 or 1-800-3448858.
Telephone requests are accepted only if the Certificate is to be mailed to the address the plan has on file for the individual to who the request relates. Other requests must be made in writing.
All requests must include:
The name of the individual for whom the Certificate is requested;
AultCare Group Number and Identification Number
P.O. Box 6910 | Canton, OH 44706
PHONE: 330-363-6360 | TOLL FREE: 1-800-344-8858
TTY LINE: 711
WEBSITE: www.aultcare.com

The last date that the individual was covered under the plan;
The name of the participant that enrolled the individual in the plan; and
A telephone number to reach the individual for whom the Certificate is requested.
Required written request must also include:
The name of the person making the request and evidence of the person’s authority to request and receive the Certificate on behalf of the individual
The address to which the Certificate should be mailed.
The requester’s signature
After receiving a request that meets these requirements, the plan will act in a reasonable and prompt fashion to provide the Certificate.
(Note: A preexisting condition exclusion does not apply to enrollees of AultCare plans that have renewed effective January 1, 2014 and after.)
The Certificate of Creditable Coverage/Health Plan Coverage can be used as proof of loss of coverage.
P.O. Box 6910 | Canton, OH 44706
PHONE: 330-363-6360 | TOLL FREE: 1-800-344-8858
TTY LINE: 711
WEBSITE: www.aultcare.com

HIPAA/Omnibus Rule and Self-Funded Group Health Plans
In regards to the Health Insurance Portability and Accountability Act of 1996 and the Omnibus Rule of 2013, employers who provide medical benefits to their employees using self-funded health plans need to be aware of their compliance responsibilities. This notification is intended to provide an overview for the employer sponsors of self-funded health plans.
All employer health plans are regulated by the Health Insurance Portability and Accountability Act of 1996 (HIPAA). The Omnibus Rule of 2013 strengthened the privacy and security rules of HIPAA.
HIPAA-covered entities, including self-funded group health plans, and their “business associates,” should review their responsibilities under HIPAA and the Omnibus Rule.
When an employer purchases insurance through a group policy, exposures and risks from different Protected Health Information (PHI) may occur. It is usually limited to enrollment and summary information used to shop for insurance.
However, when an employer funds the benefits, instead of purchasing the insurance, the employer can directly, or through its agent (Aultra), access its employees’ medical information and is responsible for complying with privacy and security rules.
These rules include:
Requirements regarding uses and disclosures of health information
Notification of breaches
Preparation and distribution of notices of privacy practices and procedures
Updating business associate agreements
Training personnel who have access to PHI
For more comprehensive information on the HIPAA and the Omnibus Rules, please contact your own company’s Benefits Counsel.
P.O. Box 6910 / Canton, OH 44706-0910
PHONE: 330-363-2050 / 1-855-270-8497 / FAX: 330-363-7717
WEBSITE: www.aultragroup.com
AultCare/Aultra Insurance Plans—Notice of Privacy Practices
Your Information. Your Rights. Our Responsibilities.
This Notice of Privacy Practices (NPP) describes how medical and claims information about you may be used and disclosed, how you can get access to your information, and your rights under HIPAA. Please review this NPP carefully. Feel free to share it with your family or personal representative.
Introduction
AultCare Insurance Company (dba AultCare HMO), which is part of an Organized Health Care Arrangement with AultCare Corporation, AultCare Health Insuring Corporation dba PrimeTime Health Plan, and Aultra Administrative Group (AultCare or We) is a Group Health Plan Covered Entity under HIPAA.
We’re committed to safeguarding the Privacy and Security of Protected Health Information of its enrollees and their eligible dependents (you) in paper (PHI) or electronic form (ePHI).
This NPP describes our HIPAA-compliant policies and procedures for the Use and Disclosure of your PHI/ePHI, including the use of PHI/ePHI for eligibility, enrollment, underwriting, claims processing, coordination of benefits, and payment of treatment under your group health plan in compliance with HIPAA’s Privacy and Security Rules (updated by the Omnibus Rule of 2013), the HITECH Act, and the Genetic Information Nondiscrimination Act (GINA).
You may access this NPP on our website www.aultcare.com. If you do not have a computer or internet access, or if you want a paper copy of this NPP, please call our Service Center at 330-363-6361 or 1-800-344-8858.
Not every use or disclosure of PHI, with or without a signed Authorization, is listed in this NPP. Uses or disclosures not specified in this NPP often require an Authorization. Please contact our Privacy Officer if you have a question, concern, or need further guidance.
Terms
Accounting. An Accounting is a list of disclosures of your PHI/ePHI we have made.
Authorization. An Authorization is a document signed and dated by the individual who authorizes the use or disclosure of PHI/ePHI for purposes other than treatment, payment, or healthcare operations.
Business Associates. We contract with outside business associates that may access, use, or disclose PHI/ePHI to perform covered services for us. Examples include auditing, accounting, accreditation, actuarial services, and legal services. Business associates must protect the privacy and security of your PHI/ePHI to the same extent we do. If a business associate delegates services to a subcontractor or agent, that subcontractor or agent also is a business associate that must comply with HIPAA.
Covered Entities Covered entities include health care providers (e.g. hospitals, doctors, nurses, nursing homes, home health agencies, durable medical equipment suppliers, other health care professionals and suppliers), and group health plans. AultCare is a group health plan covered entity.
Designated Record Set. A designated record set is a group of records containing PHI in paper or electronic form that we created and store. A designated record set include medical, healthcare and service records, billing, claims and payment information, eligibility and enrollment information, and other information we use to make decisions regarding the coverage and payment of medical care under your plan. Records created by others are not part of a designated record set.
1
Disclose. Disclose means our releasing, transferring, providing access to, or divulging PHI/ePHI to a third party, including covered entities and their business associates: (1) for treatment, payment, and health care operations; or (2) when you permit us by your signed authorization; or (3) as required by law.
Genetic Information. Genetic information includes genetic testing of the individual or family members.
Health Plan. Health plan means an individual or group health plan that provides, or pays the cost of, medical care and includes a health insurance issuer, HMO, Part A or B of Medicare, Medicaid, voluntary prescription drug benefit program, issuer of Medicare supplemental policy, issuer or a long-term care policy, employee welfare benefit plan, plan for uniformed services, veterans health care program, CHAMPUS, Indian health service program, federal employee health benefit program, Medicare Advantage plan, approved state child health plan, high risk pool, and any other individual or group health plans or combination that provides or pays for the cost of medical care. AultCare is a group health plan.
Health Care Operations Health care operations include quality assurance, performance improvement, utilization review, accreditation, licensing, legal compliance, provider/supplier credentialing, peer review, business management, auditing, enrollment, underwriting, stop-loss/reinsurance, and other functions related to your health plan, as well as offering and providing preventive, wellness, case management, and related services.
Individual. Individual means the enrollee or eligible dependent (including minors) to whom PHI belongs It also applies to your family member or personal representative acting on your behalf.
Minimum Necessary. We will limit the use or disclosure of your PHI/ePHI to the minimum needed to accomplish the intended purpose of the use, disclosure, or request.
Payment. Payment means the activities by a group health plan to obtain premiums or to determine or fulfill its responsibility for coverage and the provisions of benefits under your plan and includes eligibility or coverage determination, coordination of benefits, adjudication and subrogation of health benefit claims, billing, claims management, EOBs, health care data processing, reinsurance (including stop-loss and excess), determination of medical necessity, utilization review (including pre-certification and retrospective review), and related activities.
Personal Representative. Personal Representative means a person acting on behalf of the individual, including family, spouse, guardian, attorney-in-fact under a durable or general power of attorney, or friend assisting the individual with healthcare and payment decisions.
Protected Health Information (PHI/ePHI). PHI/ePHI means individually identifiable medical and health information regarding your medical condition, treatment of your medical condition, and payment of your medical condition, and includes oral, written, and electronically generated and stored information. PHI/ePHI excludes de-identified information or health information regarding a person who has been deceased for more than 50 years.
Treatment. Treatment means the provision, coordination, and management of health care and services by one or more health care providers, including referrals and consultations between providers or suppliers.
Use. Use means our accessing, sharing, employing, applying, utilizing, examining, or analyzing your PHI/ePHI within the AultCare organization for payment and health care operation purposes. Your PHI/ePHI is accessible only to members of AultCare’s workforce who have been trained in HIPAA Privacy and have signed a confidentiality agreement that limits their access and use of PHI/ePHI, according to the minimum necessary standard, to perform the authorized purpose.
2
Wellness Program. Wellness Program means a program that an employer has adopted to promote health and disease prevention, which is offered to employees as part of an employer-sponsored group health plan or separately as a benefit of employment.
Your Rights
When it comes to your health information, you have certain rights. This section explains some of your rights and our responsibilities.
You may get a copy or summary of your health and claims records:
You may ask to see or get a copy of your health and claims records and PHI kept in a designated record set Please call the Service Center to ask how to do this. There are some restrictions.
We will get you a paper copy or electronic version of your health and claims records, or give you a summary, usually within 30 days of your request. We may charge reasonable, cost-based fees.
You may ask us to correct your health and claims records:
You may ask us in writing to correct your health and claims records in a designated records set if you believe they are incorrect, inaccurate, or incomplete. Please call the Service Center or visit our website to get an amendment request form.
We may say “no” to your request, but we’ll tell you why in writing within 60 days.
You will have an opportunity to appeal.
You may request confidential communications of communications by alternative means:
You may ask us to contact you about claims, premiums, EOBs, or other matters about your health plan and coverage in a specific way, such as home phone, office phone, or cell phone, or by alternate means, such as an address different from your home or usual email address.
Let us know if you do not want us to leave any voice mail message.
Contact the Service Center to request. We will consider all reasonable requests.
You may ask us to limit (restrict) what we use or disclose:
You may ask us in writing not to use or disclose certain health information for treatment, payment, or operations. We may honor your request if you pay for treatment in full out-of-pocket.
Please call the Service Center for a restriction request form or visit our website.
While we will consider reasonable requests, we are not required to agree to your request. We may say “no” if restricting information could affect your care or if disclosure is required by law.
You may request a list (“Accounting”) of those to whom we’ve disclosed PHI/ePHI:
You may ask in writing for a list of disclosures of your PHI/ePHI (Accounting) for the six years prior to your request.
We will include all disclosures except for those about treatment, payment, and health care operations, and disclosures made to you or you authorized us to make. We’ll provide one accounting a year for free but will charge a reasonable, cost-based fee if you ask for another one within 12 months.
3
You may get a copy of this NPP:
You may ask for a paper copy of this NPP at any time, even if you have agreed to receive this NPP electronically. We will provide you with a paper copy promptly.
You may access electronic copy of this NPP on our website at any time.
You may choose someone to act for you:
You may choose a family member or personal representative to receive PHI/ePHI from us, exercise your rights, and make choices for you.
We will use reasonable efforts to confirm that the person is authorized to act on your behalf before we take any action.
You may file a complaint if you believe your rights have been violated:
If you believe your privacy or your HIPAA rights have been violated, we urge you to contact our privacy officer, either by calling the Service Center or filing a written complaint at AultCare, P.O. Box 6029, Canton, OH 44706.
We take all complaints very seriously. We will investigate and take appropriate action if needed.
You also may file a complaint with the U.S. Department of Health and Human Services Office for Civil Rights by sending a letter to 200 Independence Avenue, S.W., Washington, D.C. 20201, calling 1-877-6966775, or visiting www.hhs.gov/ocr/privacy/hipaa/complaints/.
We will never retaliate against you for filing a complaint, asking a question, or expressing a concern.
Communicating with You
This section describes how we may communicate with you, family members, or your personal representative.
Communicating with You:
We may communicate with you about claims, premiums, or other things regarding your health plan.
Communicating with Family or Others Involved In Your Care:
We may disclose your PHI/ePHI to designated family, friends, guardians, persons named in a durable or general power of attorney, personal representatives, or others assisting in your care or payment of claims.
Minors and Emancipated Minors:
We may disclose a minor’s PHI/ePHI to the minor’s parent(s) or guardian, unless there are legal or policy reasons not to.
We will not disclose PHI/ePHI to the parent(s) or guardian of an emancipated minor. A minor is emancipated if he/she: (1) does not live with his/her parent(s); (2) is not covered by parental health insurance; (3) is financially independent of parent(s); (4) is married; (5) has children; or (6) is in the military.
4
Deceased Enrollees:
If you die, we may disclose your PHI to the executor or administrator of your estate.
We may disclose PHI/ePHI to your spouse, family, personal representative, or others who were involved in your care or management of your affairs, unless doing so would be inconsistent with your wishes made known to us.
Uses and Disclosures
This section describes how we typically use or disclose your PHI/ePHI with and without an Authorization.
No Authorization Needed:
We will create, receive, or access your PHI/ePHI, which we may use or disclose to other covered entities for treatment, payment, and health care operations, without the need for you to sign an Authorization.
We will disclose PHI/ePHI needed to treat or authorize treatment. For example, a doctor or health facility involved in your care may request your PHI/ePHI to make treatment decisions covered by the plan.
We will use or disclose your PHI needed for payment. For example, we will use information about your medical procedures and treatment to process and pay claims, to determine whether services are medically necessary, and to pre-authorize or certify services covered by your health plan.
We may disclose PHI/ePHI to governmental or commercial health plans that may be obligated under coordination of benefit rules to process and pay your claims.
We will use and disclose your PHI/ePHI as necessary or required by law to administer your plan and for our health care operations. For example, we may use or disclose PHI/ePHI for underwriting purposes. We will not use or disclose genetic information for underwriting purposes.
We may disclose PHI/ePHI to business associates to perform covered services. It is not necessary for you to sign an Authorization for us to share PHI/ePHI with our business associates for covered services.
Authorization Needed:
We will not use or disclose your PHI/ePHI for any purpose other than treatment, payment, or healthcare operations without your signed HIPAA-compliant Authorization, unless required by law.
We will not disclose psychotherapy notes without a signed Authorization unless required by law.
We will not disclose your PHI/ePHI to your employer without your signed Authorization. We may disclose PHI/ePHI to the plan sponsor of your health benefit plan on condition that the plan sponsor certifies that it will maintain the confidentiality of PHI/ePHI and will not use PHI to make employment-related decisions or employee benefit determinations.
We will not release medical records if subpoenaed, unless you sign an Authorization, or the lawyers sign a qualified protective order, or if we receive a valid court or administrative order.
You may choose to receive information about health-related products or services or fundraising:
We may use your PHI/ePHI if we believe you may be interested in, or benefit from, treatment alternatives, wellness, preventive, disease management, or health-related programs, products or services that may be available to you as an enrollee or eligible beneficiary under your health plan. For example, we may use your PHI/ePHI to identify whether you have a particular illness, and contact you to let you know about a disease management program is available to help manage your illness.
5
Let us know if you do not want to be contacted or receive information about these services and programs. Opting out will not affect coverage or services.
We will not sell or disclose your PHI/ePHI to third-parties for marketing without your Authorization, which will indicate whether we are paid for selling PHI.
We may contact you about charitable fundraising. If you do not want to be contacted or receive fundraising materials, let our Service Center know. Opting out will not affect coverage or services.
Wellness Programs:
If you voluntarily choose to participate in a Wellness Program, you may be asked to answer questions on a health risk assessment (HRA) and/or undergo biometric screenings for risk factors,
Wellness Programs may also provide educational health-related information or services that may include nutrition classes, weight loss and smoking cessation programs, onsite exercise facilities, and/or health coaching to help employees meet their health goals.
If your employer has entered or may enter into a contract with us to perform services, as well as receive, collect, use, disclose, and store data in connection with a Wellness Program. We will protect the privacy of your PHI.
Use and Disclosure of Health Information Permitted or Required by Law
We may use or disclose PHI/ePHI, without your Authorization, as required by law, including, but not limited to:
Workers’ Compensation
Public health agencies
FDA and OSHA
Ohio Department of Insurance and other regulatory and licensing agencies
Armed Forces to assist in notifying family members of your location, general condition, or death
Law Enforcement
Homeland security
Emergency and disaster
Prevent threat of serious harm
Proof of immunization
Breach Notification
You have the right to notification if a breach of your PHI/ePHI occurs. We will promptly notify you by firstclass mail, at your last known address, or by email (if you prefer) if we discover a breach of unsecured PHI/ePHI, which includes the unauthorized acquisition, access, use, or disclosure of your PHI/ePHI, unless we determine through a risk analysis that a low probability exists that the compromise of your PHI would cause you financial, reputational, or other harm.
We will include in the breach notification a brief description of what happened, a description of the types of unsecured PHI involved, steps you should take to protect yourself from potential harm, a brief description of what we are doing to investigate the breach and mitigate any potential harm, as well as contact information for you to ask questions and learn additional information.
6
Changes to this NPP
This section describes how and when we may changes NPP and how we will inform you of any material changes.
We reserve the right to change this NPP at any time, which we may make effective for PHI/ePHI we already used or disclosed, and for any PHI/ePHI we may create, receive, use, or disclose in the future.
We will make material amendments based on changes in the HIPAA laws.
The revised NPP will be posted on our website www.aultcare.com. Copies of revised NPPs will be mailed to all enrollees covered by the plan, and copies may be obtained by mailing a request to: Privacy Coordinator, P.O. Box 6029, Canton, Ohio 44706.
If you have questions or need further assistance regarding this NPP, you may contact the Service Center at 330-363-6360 or 1-800-344-8858. If you are hearing impaired and have access to a TTY phone, you may reach us at our TTY line at 330-363-2393 or 1-866-633-4752. Our Service Center hours are from 7:30 a.m. to 5:00 p.m., Monday-Friday.
CT2:739688_v1
AultCare/Aultra General Tag Lines for the State of Ohio
English
If you, or someone you are helping, have questions about AultCare/Aultra you have the right to get help and information in your language at no cost. To speak with an interpreter, call Local: 330.363.6360 Outside Stark County: 1.800.344.8858 TTY Local: 330.363.2393 Outside Stark County: 1.866.633.4752
Spanish Español
Si usted, o alguien a quien usted está ayudando, tiene preguntas acerca AultCare/Aultra tiene derecho a obtener ayuda e información en su idioma sin costo alguno. Para hablar con un intérprete, llame al Local : 330.363.6360 Fuera del condado de Stark : 1.800.344.8858 TTY Local : 330.363.2393 Fuera del condado de Stark : 1.866.633.4752
Chinese 中文
如果您,或是您正在協助的對象,有關於AultCare/Aultra保险公司 方面的問題,您有權利免費以您的母語得到幫助和訊息。洽詢一位翻譯員,請撥電話本地:330.363.6360 斯塔克縣外: 1.800.344.8858 TTY線本地:330.363.2393斯塔克縣外:1.866.633.4752。
German
Deutsche
Falls Sie oder jemand, dem Sie helfen, Fragen zum AultCare/Aultra haben, haben Sie das Recht, kostenlose Hilfe und Informationen in Ihrer Sprache zu erhalten. Um mit einem Dolmetscher zu sprechen, rufen Sie bitte die Nummer Local: 330.363.6360 Außerhalb von Stark County : 1.800.344.8858 TTY –Linie Local: 330.363.2393
Außerhalb von Stark County : 1.866.633.4752 an.
Arabic
7
ةيبرعلا ةيبرعلا لكتةيانود نم كتغلبةيرورضلا تامولعملاو ةدعاسملا ىلعلوصحلا يف قحلا كيدل ، ب لصتا مجرتم عم ثدحتلل .ةف صوصخبةلئسأهدعاستصخش ىدل وأكيدلناكنإ نيمأتلاةكرش AultCare/Aultra كراتس ةعطاقمجراخ . 1.866.633.4752:يلحملا طخلا330.363.2393 TTY : كراتس ةعطاقمجراخ 1.800.344.8858
Pennsylvania Dutch Deitsch
Wann du hoscht en Froog, odder ebber, wu du helfscht, hot en Froog baut
AultCare/Aultra hoscht du es Recht fer Hilf un Information in deinre eegne Schprooch griege, un die Hilf koschtet nix. Wann du mit me Interpreter schwetze witt, kannscht du Local: 330.363.6360 Außerhalb von Stark County: 1.800.344.8858 TTY –Linie
Local: 330.363.2393 Außerhalb von Stark County : 1.866.633.4752 uffrufe.
Russian
русский
Если у вас или лица, которому вы помогаете, имеются вопросы по поводу Страховая компания
AultCare/Aultra, то вы имеете право на бесплатное получение помощи и информации на вашем языке. Для разговора с переводчиком позвоните по телефону Местный: 330.363.6360 Вне Старка County : 1.800.344.8858 TTY линия Местный: 330.363.2393 Вне Старка County : 1.866.633.4752.
French Français
Si vous, ou quelqu'un que vous êtes en train d’aider, a des questions à propos de Compagnie d'Assurance
AultCare/Aultra, vous avez le droit d'obtenir de l'aide et l'information dans votre langue à aucun coût. Pour parler à un interprète, Appelez Locale 330.363.6360 En dehors du comté de Stark : 1.800.344.8858 ligne ATS Local : 330.363.2393 En dehors du comté de Stark : 1.866.633.4752
Vietnamese
Việt Nam
Nếu quý vị, hay người mà quý vị đang giúp đỡ, có câu hỏi về Công ty Bảo hiểm AultCare/Aultra quý vị sẽ có quyền được giúp và có thêm thông tin bằng ngôn ngữ của mình miễn phí. Để nói chuyện với một thông dịch viên, xin gọi Địa phương: 330.363.6360 Bên ngoài của Stark County : 1.800.344.8858 TTY đường dây Địa phương: 330.363.2393 Bên ngoài của Stark County : 1.866.633.4752.
Cushite-Oromo
Isin yookan namni biraa isin deeggartan AultCare/Aultra, irratti gaaffii yo qabaattan, kaffaltii irraa bilisa haala ta’een afaan keessaniin odeeffannoo argachuu fi deeggarsa argachuuf mirga ni qabdu. Nama isiniif ibsu argachuuf, lakkoofsa bilbilaa Local: 330.363.6360 Outside of Stark County: 1.800.344.8858 TTY Line Local: 330.363.2393 Outside of Stark County: 1.866.633.4752 tiin bilbilaa.
Korean 한국어
만약 귀하 또는 귀하가 돕고 있는 어떤 사람이AultCare/Aultra 보험 회사 에 관해서 질문이 있다면 귀하는
그러한 도움과 정보를 귀하의 언어로 비용 부담없이 얻을 수 있는 권리가 있습니다. 그렇게 통역사와 얘기하기 위해서는 지역 : 330.363.6360 스타크 카운티 의 외부 : 1.800.344.8858 TTY 라인 지역 : 330.363.2393 스타크 카운티 의 외부 : 1.866.633.4752 로 전화하십시오.
Italian
Italiano
Se tu o qualcuno che stai aiutando avete domande su AultCare/Aultra, hai il diritto di ottenere aiuto e informazioni nella tua lingua gratuitamente. Per parlare con un interprete, puoi chiamare Locale: 330.363.6360 Al di fuori di Stark County : 1.800.344.8858 TTY linea Locale: 330.363.2393 Al di fuori di Stark County : 1.866.633.4752.
8
Japanese 日本語
ご本人様、またはお客様の身の回りの方でもAultCare/Aultra保険会社についてご質問がございましたら、 ご希望の言語でサポートを受けたり、情報を入手したりすることができます。料金はかかりません。通 訳とお話される場合、 ローカル:330.363.6360 スターク郡の外:1.800.344.8858 TTYラインローカル:330.363.2393 スターク郡の外: 1.866.633.4752までお電話ください。
Dutch Nederlands
Als u, of iemand die u helpt, vragen heeft over AultCare/Aultra, heeft u het recht om hulp en informatie te krijgen in uw taal zonder kosten. Om te praten met een tolk, bel Local : 330.363.6360 Buiten Stark County : 1.800.344.8858 TTY Line Local : 330.363.2393 Buiten Stark County : 1.866.633.4752.
Ukrainian український Якщо у Вас чи у когось, хто отримує Вашу допомогу, виникають питання про Страхова компанія
AultCare/Aultra, у Вас є право отримати безкоштовну допомогу та інформацію на Вашій рідній мові. Щоб зв’язатись з перекладачем, задзвоніть на Місцевий : 330.363.6360 Поза Старка County : 1.800.344.8858 TTY лінія Місцевий : 330.363.2393 Поза Старка County : 1.866.633.4752.
Romanian Română
Dacă dumneavoastră sau persoana pe care o asistați aveți întrebări privind Compania de Asigurari
AultCare/Aultra, aveți dreptul de a obține gratuit ajutor și informații în limba dumneavoastră. Pentru a vorbi cu un interpret, sunați la Locale : 330.363.6360 In afara Stark Judet : 1.800.344.8858 TTY linie Locale : 330.363.2393 In afara Stark Judet : 1.866.633.4752.
Non-Discrimination Notice:
AultCare/Aultra complies with applicable Federal civil rights laws and does not discriminate on the basis of race, color, national origin, age, disability, or sex. AultCare/Aultra does not exclude people or treat them differently because of race, color, national origin, age, disability, or sex. AultCare/Aultra provides free aids and services to people with disabilities to communicate effectively with us, such as: Qualified sign language interpreters and written information in other formats (large print, audio, accessible electronic formats, other formats). AultCare/Aultra provides free language services to people whose primary language is not English, such as: Qualified interpreters and information written in other languages.
If you need these services, or if you believe that AultCare/Aultra has failed to provide these services or discriminated in another way on the basis of race, color, national origin, age, disability, or sex, you can contact or file a grievance with the: AultCare/Aultra Civil Rights Coordinator, 2600 6th St. S.W. Canton, OH 44710, 330-3637456, CivilRightsCoordinator@aultcare.com. You can file a grievance in person or by mail, fax, or email. If you need help filing a grievance, our Civil Rights staff is available to help you.
You can also file a civil rights complaint with the U.S. Department of Health and Human Services, Office for Civil Rights electronically through the Office for Civil Rights Complaint Portal, available at https://ocrportal.hhs.gov/ocr/portal/lobby.jsf, or by mail or phone at: U.S. Department of Health and Human Services 200 Independence Avenue, SW Room 509F, HHH Building Washington, D.C. 20201 1-800-368-1019, 800-537-7697 (TDD). Complaint forms are available at http://www.hhs.gov/ocr/office/file/index.html.
9

Dear Member,
Aultra recognizes the importance of understanding your benefits as well as our operating procedures prior to your enrollment. This information would include, but is not limited to, the following:
Covered benefits
Non-covered benefits
Access to doctors, healthcare providers, and facilities (provider network)
Key medical management (Utilization Management) procedures
Potential network, service, or benefit restrictions
Pharmaceutical management procedures
Policies and practices regarding collection, use, and disclosure of Protected Health Information (PHI), including:
o Routine notification of privacy practices
o Use of authorizations
o Access to medical records
o Protection of oral, written, and electronic information across the organization
o Information for employers
To ensure this information is easily accessible to our potential members, we provide the information in our Member Guide, which is located on our website www.aultcare.com. The Member Guide can be found on the Members page under the Member Information section.
To request a printed copy of the Member Guide, please contact Customer Service at 330-363-2050 or 1800-270-8497. Representatives are available Monday-Friday from 7:30 am – 5:00 pm. (For hearingimpaired assistance, please call 711).
Sincerely,
Aultra Sales and Retention Departments
P.O. Box 6910 | Canton, OH 44706
PHONE: 330-363-2050
| TOLL FREE: 1-855-270-8497
| TTY: 711
FAX: 330-363-7717
WEBSITE: www.aultragroup.com
EMPLOYEE COUNT ANALYSIS
Various state and federal laws have requirements based on employee counts. When counting employees, it’s important to conduct a related employer analysis.
The information detailed below does not constitute legal advice and is intended only for informational purposes. Please reach out to your benefits counsel to discuss your individual circumstances.
1. RELATED EMPLOYER ANALYSIS requires counting all employees of all members of the employers in a controlled group of companies or affiliated service group to determine employee count. Below is a summary of those groups.Bank Name
A controlled group may exist when two or more companies have any of the following:
• A Parent-Subsidiary Relationship: Exists when one or more chains of organizations are connected through ownership of a common parent company and 80% or more of the voting power or total value of each member of the group is owned by another member of the group, except for the common parent.
• A Brother-Sister Relationship: Exists when at least 50% of the voting power or total value of two or more organizations is owned by the same 5 or fewer persons taking into account only the ownership of each such organization that is identical for each other organization.
• A Combination Relationship: Exists when two or more organizations are members of a group that has common ownership which includes both parent-subsidiary relationships and brother-sister relationships, in which case all such organizations are considered the same controlled group of business.
An affiliated service group may exist when two or more organizations have a service relationship and/or ownership relationship with one another as satisfied by 1 of 3 tests (A-Org Test; B-Org Test; or Management Group Test).
More information about Controlled and Affiliated Service Groups can be found in the following IRS publication: https://www.irs.gov/pub/irs-tege/epchd704.pdf
2. GROUP SIZE FOR A FULLY INSURED PLAN OFFERING UNDER OHIO LAWnk Name
Under Ohio law, a small, Ohio-based employer, for purposes of a group health plan and with respect to a calendar year and a plan year, is an employer who employed an average of at least two but no more than fifty eligible employees on business days during the preceding calendar year and who employs at least two employees on the first day of the plan year. With “Eligible Employee” being defined as an employee who works a normal work week of thirty or more hours. Eligible employee does not include a temporary or substitute employee, or a seasonal employee who works only part of the calendar year on the basis of natural or suitable times or circumstances. Ohio Rev. Code § 3924.01
3. CONSOLIDATED OMNIBUS BUDGET RECONCILIATION ACT (COBRA) ANALYSIS
COBRA generally applies to all private sector group health plans as well as plans sponsored by state and local governments. To be subject to COBRA, employers need to have at least 20 employees on more than 50% of their typical business days in the previous calendar year. When counting employees for COBRA purposes, both full- and part-time employees are counted, taking into consideration the above Related Employer Analysis. Each part-time employee counts as a fraction of a full-time employee. The fraction should be equal to the number of hours worked divided by the number of hours required to be considered full-time. (For example, a company requires a full-time employee work 40 hours a week. A part-time employee who works 20 hours a week is considered ½ of a full-time employee.) If you have fewer than 20 employees, you may be subject to state continuation of coverage requirements under ORC 3923.38 depending on whether your group health plan is subject to state regulation. These plans typically include Insured, MEWA plans, and self-funded public employers.
For more information, visit https://www.dol.gov/sites/dolgov/files/EBSA/about-ebsa/our-activities/resource-center publications/anemployers-guide-to-group-health-continuation-coverage-under-cobra.pdf
7774/22
MEDICARE SECONDARY PAYER (MSP) ANALYSIS
MSP is a federal law that requires Medicare pay secondary to group health plans unless certain circumstances apply. These exceptions are based on group size and the scenarios are listed below. This is not intended to be a comprehensive guide to the MSP law. As an employer group sponsoring a group health plan, you are required to maintain documentation regarding your total employee counts during the year. Please use the above Related Employer Analysis to report your employee count.
If Medicare requests a review of MSP status, AultCare will reach out to obtain information regarding your group size during the period in question. Medicare can inquire about claims that are several years old, so it’s imperative to maintain accurate records.
MSP SUMMARY RULES
Medicare Beneficiary
Age 65 or older (employee or spouse) and group health plan due to current employment of the Medicare beneficiary or the beneficiary’s spouse
Age 65 or older (employee or spouse) and group health plan not due to current employment (e.g. through a retiree health plan or COBRA) of the Medicare beneficiary or the beneficiary’s spouse
Disabled under age 65 (employee, spouse, or dependent) and group health plan due to current employment of the Medicare beneficiary or the beneficiary’s spouse or parent
Employer Characteristics
Employer with fewer than 20 employees
Employer with at least 20 employees full or part-time in at least 20 weeks of the preceding or current year (the 20 weeks do not have to be consecutive)
Primary Payer Secondary Payer
Medicare Group Health Plan
Group Health Plan
Medicare
All employers regardless of the number of employees Medicare Group Health Plan
Disabled under age 65 (employee, spouse, or dependent) and group health plan not due to current employment (e.g. through a retiree health plan or COBRA) of the Medicare beneficiary of the beneficiary’s spouse or parent
ESRD patient (employee, spouse, or dependent) during the first 30 months of Medicare ESRD coverage
During at least half the year of the employer’s regular business days in the previous calendar year, the employer had:
Employer with fewer than 100 employees
Employer with at least 100 employees during at least half the year of the employer’s regular business days in the previous calendar year
All employers regardless of the number of employees
Medicare Group Health Plan
Group Health Plan
Medicare
ESRD patient (employee, spouse, or dependent) regardless of age beginning with the 31st month of Medicare ESRD coverage
All employers regardless of the number of employees
If, when ESRD coverage begins, the employer plan is already primary payer according to MSP provisions
If, when ESRD coverage begins, the employer plan is correctly secondary payer because it is not subject to the applicable MSP provisions for working aged or for disability
All employers regardless of the number of employees
Medicare
Group Health Plan
Group Health Plan (Active and COBRA coverage)
Medicare
Medicare
Medicare, regardless of coverage for age 65 or disability, for the duration of ESRD coverage
Group Health Plan (Active and COBRA coverage)
Group Health Plan (Active and COBRA coverage)
More information about Medicare Secondary Payer rules can be found in the following publication: https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/Downloads/MSP_Fact_Sheet.pdf
4.
ANNUAL DETERMINATION OF GROUP SIZE DEMOGRAPHICS
1. RELATED EMPLOYER ANALYSIS
Does the attached Related Employer Analysis define your company as part of a controlled group or affiliated service group?
Yes No
a. If yes, list the other Related Employer name(s):_________________________________________________________
b. If yes, consider that fact when answering all of the questions below.
2. GROUP SIZE FOR A FULLY INSURED PLAN OFFERING UNDER OHIO LAW*
For Ohio-based employer plans, provide the number of employees in the preceding calendar year that worked at least 30 hours during a normal work week? (Note: If your answer is between 2 to 50 employees, you will be offered a Small Group or MEWA plan option.)
*Self-funded plans or employers outside Ohio may skip this question.
3. CONSOLIDATED OMNIBUS BUDGET RECONCILIATION ACT (COBRA) ANALYSIS
To determine the appropriate continuation of coverage (COBRA vs State Continuation) provide the following counts for 50% of the typical business days in the previous calendar year:
Full-time ________ Part-time (Each is counted as a fraction of a full-time employee.) ________
Total number of employees ________
4. MEDICARE SECONDARY PAYER (MSP) ANALYSIS
a. Did you (including all Related Employers) have 100 or more full-time, part-time, seasonal employees or partners on 50 percent or more of your business days during:
The current calendar year? Yes No
The preceding calendar year? Yes No
b. Did you (including all Related Employers) have 20 or more full-time, part-time, seasonal employees, or partners for each working day in each of 20 or more calendar weeks (weeks do not have to be consecutive) during:
The current calendar year? Yes No
The preceding calendar year? Yes No
If you checked “Yes” for the current calendar year, and the 20-employee threshold was met during the current year, provide the date:_________________.
I understand AultCare is relying on my answers to the above questions to ensure overall compliance for my group health plan. I also understand the information submitted will be used to determine: whether Medicare will be the primary payer of claims for my Medicare-eligible insured(s), employer size for continuation of coverage, and employer size status under State and Federal regulations. I certify the answers are true to the best of my knowledge and belief. I also understand I am responsible for promptly notifying AultCare (as indicated above) if my answers to any of these questions change because our organization has increased or decreased the number of employees. I understand that CMS penalties may apply. Signature of Company Officer or Authorized Representative Print Name Title
7775/22
_____________
Daily Contact Email Address Date Executive Email Address Return to: AultCare Insurance Company Attn: Retention Department | P.O. Box 6910, Canton, OH 44706 | retention@aultcare.com
/ Legal
of Company Group Number Employer Identification Number (EIN/TIN)
Employer Name
Name
Specific Participant Notices and Disclosures Under Health Care Reform
The following provides a checklist of the specific notices and disclosures under health care reform. For each topic, we provide a citation to the statutory provision, a description of the notice or disclosure, effective date/timing of distribution, and who is required to comply.
Citation to Statutory Provision Description of Notice or Disclosure
Exchange Notice [FLSA§ 18B]
Patient protections [PHSA § 2719A]
Rescissions Prohibition [PHSA § 2712]
Information Reporting of Minimum Essential Coverage
MEC (Insurers and Employers That Self- Insure) [Code § 6055]
Information Reporting of Employer-Sponsored Coverage (Applicable Large Employers ALE) [Code § 6056]
Summary of Benefits and Coverage (SBC) & Glossary of Terms & Notice of Material
Modifications to SBC {SMM} [PHSA § 2715]
Information on Exchanges and the consequences if employee purchases a QHP through Exchange in lieu of employersponsored coverage
Choice of primary care provider/ pediatrician (if plan requires or allows for this) and OB/GYN care without referral (if applicable, include in SPD or any description of benefits)
(Notice of the right to designate any participating PCP; designate a pediatrician as PCP for any child and obtain OB/GYN care without PA or referral)
30 day advance notice of retroactive cancellation or discontinuance of coverage (permitted only in limited circumstances such as fraud or misrepresentation of a material fact upon event or on request)
Forms 1094-B directly to IRS and 1095-B to covered employee
Written statement of health coverage provided
Forms 1094-C directly to IRS and 1095-C to the covered employee
Written statement of health coverage provided
SBC must meet certain appearance, language, and content requirements & 60-day advance notice required for material modifications not reflected in most recent summary
Date/Timing Required to Comply
To new employees hired after October 1, 2013, within 14 days of their start date
Employers subject to FLSA
9/23/10
After 9/23/10
Generally, annually on or before 1/31 after calendar year in which coverage was provided
Generally, annually on or before 1/31 after calendar year in which coverage was provided
Distribution starting with first open enrollment
beginning on or after 9/23/12; Exchange/FFM notice must occur within 14 days after start date
Group health plans and insurers (n/a to grandfathered plans or coverage)
Group health plans and insurers
For Insurers, sponsors of self-insured plans, and other entities providing “minimum essential coverage”
Applicable large employers
Group health plans and insurers
Group Health Plans: Federal Mandates Other
Than COBRA
& HIPAA
Mental Health Parity
• Under the MHPA/MHPAEA, cost-exemption notices notifying participants and beneficiaries of the plan’s reliance on the increased cost exemption, including among other things, a statement regarding the availability upon request of a summary of the information on which the exemption was based (required only if plan claims exemption) Triggered only if plan claims the exemption from MHPAEA Provide upon event (must provide a 30 days advance notice to participants, beneficiaries and DOL) or on request
• Opt-out notices notifying enrollees of opt-out by selffunded non-federal governmental plan, annually and upon enrollment
• Employer Health Plans must provide a comparative analysis of the application of Non-Quantitative Treatment Limits (NQTLs) to Mental Health/Substance Use benefits in comparison to Medical/Surgical benefits to ensure parity exists.
Women’s Health and Cancer Rights Act (WHCRA)
• Enrollment notices notifying participants of WHCRA rights included upon initial enrollment, if not included in an SPD that is distributed upon initial enrollment
• Annual notices notifying participants of WHCRA rights, if not included in an SPD that is distributed annually
• Opt-out notices notifying enrollees of opt-out by selffunded non-federal governmental plan, annually and upon enrollment Plans
Newborns’ and Mothers’ Health Protection Act (NMHPA)
• Include in the SPD – Must describe, with respect to childbirth hospital stay for mother and newborn the applicable State or Federal requirements and the plan’s coverage – use DOL model language
• Opt-out notices notifying enrollees of opt-out by selffunded non-federal governmental plan, annually and upon enrollment
Patient Protections Under Health Care Reform
• Written notice of the right to designate a primary care provider or pediatrician and to obtain obstetrical or gynecological care without preauthorization or referral must be provided not later than the first day of the first plan year beginning on or after September 23, 2010, and with SPD
Surprise Billing
• Employer Health Plans must provide to participants, in plain language, information regarding balance billing protections in both emergency and certain nonemergency situations. The information must be listed on the plan’s website and on all EOBs.
Cost Transparency Rules
• Employer Health Plans must make available to members price comparison information. The information must be accessible in an internet-based self-service tool (or paper upon request). By January 1, 2023, plans must have price comparison information for 500 items and services as described in regulation. By January 1, 2024, all other items and services must be accessible through the internet tool.
Group Health Plans: Federal Mandates Other
Member ID Cards
• Must list the plan’s deductible and out-of-pocket information, as well as, the plan’s contact information.
Continuity of Care
• Employer Health Plans must continue to cover certain benefits on an in-network basis when a provider or facility ceases to be in-network. Will require COBRAlike provisions, with plan notifying enrollee of right to obtain this benefit and enrollee electing the benefit. Generally applicable for serious and complex (or terminal) medical conditions.
Provider Directory and Coverage Information Requests
• Employer Health Plans must create a database on a public website that includes a list of providers and facilities that are in-network. Information must be verified and updated every 90 days (to remove providers who have left network.) If information that plans provide about in-network status is incorrect, the plan enrollee may be protected from higher cost-sharing amounts.
Americans with Disabilities Act (ADA)
• EEOC notice of rights to be posted on employer’s premises
• No specific notice requirements with respect to employersponsored group health plans, except for certain wellness programs - ADA Wellness Program Notice to be provided at initial enrollment and at annual enrollment (If wellness program includes an activity only or outcome based reward, SPD must include contact information and statement that an alternative standard is available and that recommendations of attending physician will be accommodated) EEOC has model notice
Than COBRA &
HIPAA
Genetic Information Nondiscrimination Act (GINA)
• Employers should include language in any lawful request for medical information specifically directing the individual or health care provider not to provide genetic information (EEOC model language is available)
Medicare Secondary Payer (MSP) Requirements
• Exemption notice: Multiemployer or multiple employer plans seeking small employer exception from age-based MSP rules must send letters to affected employees notifying them and their spouses that employer is exempted from the MSP rules
• Mandatory reporting rules: Although the mandatory reporting rule requirements require reporting to the government in certain situations, they do not appear to require any additional notices or reporting to plan participants (although required reporting entities (RREs) may need to use model language documents to collect information from plan participants in order to qualify for a reporting safe harbor)
Medicare Part D: Creditable Coverage Disclosure and Coordination of Benefits Requirements
• Disclosure notices (creditable coverage and noncreditable coverage disclosure notices) to be sent to Part D eligible individuals
• Provided at initial enrollment; annually by Oct. 15; upon certain events and on request
• For Group health plans with prescription drug coverage
CMS has model notices
HIPAA and COBRA
HIPAA COBRA
• Include nondiscrimination disclosure in SPD ACA §1557 now requires the posting of a notice of nondiscrimination with translated taglines in other languages offering assistance. 1557 also prohibits discrimination based upon race, color, national origin, sex, age or disability in health program or activities receiving funding from HHS (includes Medicare, Medicaid, QHP/FFM, etc.)
• Special enrollment notices to employees describing special enrollment rules and rights given at initial enrollment, on event or upon request. Can include in annual enrollment materials, too. Describe special enrollment rights in the SPD
• CHIP notice at annual enrollment (consider special enrollment notice at annual as well) Annual notice describing possible premium assistance available in State in which employees reside Model notice found on DOL
• Notice of privacy practices to individuals given at initial enrollment, on event (60 days after a material revision of the notice) or upon request. NPP has specific requirements as to its contents – use HHS model notice; Notice of availability of NPP given at least once every 3 years (can be given at annual enrollment each year)
• Notice to employees regarding potential opportunities for State premium assistance subsidy (beginning in 2010)
• Other HIPAA notices such as Breach notices, responses to individual rights to access own PHI, etc. apply as well, but are beyond the scope of this checklist
• Recommendation to send standalone notice to employee and spouse within initial notice time period
• Initial notices to covered employee and covered spouse explaining COBRA rights and obligations generally in SPD – must include a general description of COBRA coverage and description of qualified beneficiary/covered employee’s obligations; Provide within 90 days after individual’s coverage commences
• Description of COBRA rights and obligations found in SPD –statement of rights and obligations relating to continuation of coverage
• Election notices to qualified beneficiaries who experience a qualifying event providing information about rights and obligations relating to a specific qualifying event or upon request; DOL has model notice; Provide within 14 days after receipt of qualifying event notice from employer or qualified beneficiary/covered employee. Or within 44 days after qualifying event for which the employer is responsible (term of employment, death) recommend send first class mail with documentation; Furnish to each qualifying beneficiary (single notice can go to employee and spouse at same address and serves as notice to dependent children)
• Notice of unavailability of COBRA coverage to individuals who may expect to receive coverage on event or upon request
• Notice of termination of COBRA coverage to affected qualified beneficiaries on event or upon request
• Notice of conversion to affected qualified beneficiaries where plan provides conversion option
• Notice of insignificant shortfall on event or upon request
• Model notices for COBRA premium reduction subsidy
• Other COBRA notices may apply as well, but are beyond the scope of this checklist
Required Participant Disclosures Other than in SPDs and SBCs
Qualified Medical Child Support Orders (QMCSOs)
• QMCSO receipt letters notifying participant and each alternate recipient of the receipt of a QMCSO and of the plan’s procedures for determining whether a medical support order is a QMCSO
• QMCSO determination letters notifying participant and each alternate recipient as to whether an order has been determined to be a QMCSO
• QMCSO procedures can be given, if requested by a participant or beneficiary and if not included in the plan’s SPD (procedures typically included in SPD)
• National Medical Support Notices (NMSNs). In addition to observing QMCSO requirements above, and completing the Employer/Plan Administrator Responses to Parts A and B in accordance with the NMSN instructions, the employee, child, and custodial parent must be notified that coverage will become available. If the NMSN is determined not to be appropriately completed, the employee, custodial parent, and alternate recipient must be notified.
ERISA ERISA
• Summary Plan Description (SPD) – Includes eligibility, benefits and plan design
Required Coverage for Dependent Children (Michelle’s Law)
• If coverage for a dependent child is conditioned upon the dependent’s status as a student, any request for certification of student status must include a notice as to the provisions of Michelle’s Law
• Opt-out notices notifying enrollees of opt-out by self- funded non-federal governmental plan, annually and upon enrollment
• Statement of ERISA Rights (model language in DOL regs) SPD is provided within 90 days for new participants (120 for new plans) and at least every 5 years if any material changes (10 years if no changes) Provide to all covered participants (generally not beneficiaries) – also provide to surviving spouse, QMCSO recipient and COBRA qualified beneficiary. Provide by first class mail or hand deliver at the work place. Electronic delivery is permitted under certain rules. Document delivery method.
• Summary of Material Modifications (SMM) – updates the SPD - upon event or at request SMM is provided when there is any material change or change to any required SPD content – provide within 60 days after material reduction in covered services or benefits or within 210 days after end of plan year in which the change is adopted
• Summary of Benefits and Coverage (SBC) – written plan summary with prescribed format and content SBC provided with enrollment materials (60 day advance notice for midyear material modifications affecting SBC content) Can be paper or electronic (for online enrollment) Must go participants and beneficiaries
• Summary Annual Report (SAR) (required if plan is (1) funded; or (2) insured with 100 or more participants at beginning of plan year)
– Annually 9 months after PY ends or 2 months after Form 5500 extension; Is a summary of Form 5500 – for the participants – model language found on DOL. If plan does not file 5500, then no SAR is required
• Responses to written participant requests for documents
•
•
•
–
in the
or in separate document distributed and referenced in the SPD
Claims procedure notices
typically found
SPD
Offer of assistance in non-English language (taglines)
Other ERISA notices may apply as
but are beyond the scope of this checklist
well,











Remember to present your ID card at each provider visit. Understanding Your Member ID Card from Aultra Member Medical Plan www.aultragroup.com Pharmacy Plan Effective: Employer: Group #: Member: Member ID: Rx Claims Processor: Rx Bin: Rx Group: Issuer: Member Medical Plan www.aultragroup.com Effective: Employer: Group #: Member: 1034-XX 0653 123----M()D()V() 1034-XX 0653 123----M()D()V() 20180724T32 Sh: 0 Bin 2 J04A Env [1] CSets 1 of 1 20180724T32 Sh: 0 Bin 2 J04A Env [1] CSets 1 of 1 The information shown is for general informational purposes. Please call Aultra at 330-363-2050 or 1-855-270-8497 with questions. Employer Information: Use this information to contact Aultra & register for your online account. Health Plan Information: Coverage effective date & information for provider or specialist if applicable. Member Information: Use this information when you contact Aultra & register for your online account. Pharmacy Information: Pharmacy coverage. Front of Card Please note: This is a sample card. Your personalized, Aultra ID card will contain your specific plan information. Health Plan Claim Contact Information: The mailing address for medical claims. Eligibility Disclaimers & Information: The contact information for eligibility. Dental Claim Contact Information: If you have dental coverage, this is the mailing address. Pre-Certification Requirement Information: Contact Utilization Management (UM) with questions regarding elective procedures. Dental Information: Dental coverage if applicable. Back of Card Need a replacement ID card? Log into your online account at www.aultragroup.com to print a copy and/or request a new one. 1060/18 Customer Service/Eligibility This card is not a guarantee of coverage. For verification and coverage details, contact Aultra at 330-363-2050 or 1-855-270-8497 weekdays, 7:30 a.m. to 5:00 p.m. Utilization Pre-Certification is required for all elective admissions and within two working days following an emergency admission. Certify by calling Utilization Management at 330-363-2050 or 1-855-270-8497. Mail Claims: Mail Aultra Administrative Group P.O. Box 6910 Canton, OH 44706 Claims Submission Customer Service/Eligibility This card is not a guarantee of coverage. For verification and coverage details, contact Aultra at 330-363-2050 or 1-855-270-8497 weekdays, 7:30 a.m. to 5:00 p.m. Utilization Pre-Certification is required for all elective admissions and within two working days Mail Claims: Mail Aultra Administrative Group P.O. Box 6910 Canton, OH 44706 Claims Submission 1034-XX 01D6 123----M()D()V() 1034-XX 01D6 123----M()D()V() 20180724T32 Sh: 0 Bin 2 J04A Env [1] CSets 1 of 1 20180724T32 Sh: J04A Env [1] CSets
GETTING THE MOST FROM YOUR HEALTHCARE PLAN
Aultra is dedicated to providing you and and your family with convenient access to healthcare. In order to provide access to quality care, it is important to keep Aultra updated with any major life events. In addition, Aultra may reach out to you if more information is required regarding you and your family to accurately manage your health plan.
MAJOR LIFE EVENTS
Notifying Aultra of any major life events ensures continued healthcare coverage. If any of the below life events have recently occurred, please notify your Human Resources Coordinator as soon as possible.
» Marriage
» Divorce or legal separation
» Spouse now working
» Spouse loss of health coverage
» New baby
» Adoption
» Child between ages 19 – 25 requires coverage
ADDITIONAL INFORMATION



If Aultra requires additional information, you may receive a form in the mail.
Please complete the form and return it to Aultra as soon as possible. Examples of additional information:
» Other Coverage – If your spouse and/or child(ren) have other health coverage, Aultra will ask you to complete an Other Coverage form each year to confirm.
» Divorce/Not Married – Aultra may request a copy of your divorce decree or court order if you are divorced or a single parent covering children on your plan. The required court document provides information on which parent’s healthcare plan has been ordered to pay first. If you do not have a court document, you will be asked to complete an Affidavit for Financial Support annually.
» Injury – Aultra will need to know if an injury is related to an accident that may be connected to a Workers’ Compensation claim, automobile or other accident. You will receive an Accident Questionnaire to confirm how the injury occurred.
CONTACT US 330-363-2050 | 1-855-270-8497
www.aultragroup.com
6170/20
you youmatter
EXPLANATION OF BENEFITS/APPEALS
Explanation of Benefits:
AultCare is now posting Explanation of Benefits (EOB) forms electronically. You can access, view or print an electronic EOB from the AultCare website anytime you want. Please refer to the following instructions.
Encourage your employees to obtain access to their claim information on the website or to call the service center to answer specific questions about their claims.
Appeals:
The attached documents outline AultCare’s appeal procedures and timelines.
Internal Appeal Request Form
If you disagree with a determination decision about a specific benefit, you have the right to file an internal appeal with AultCare using this form. You may also submit your appeal in writing and include any comments, documentation, or records relevant to your appeal.
AultCare Treating Physician Certification for Experimental/Investigational ABD
You may have your provider complete this form if your request for benefit determination has been denied as Experimental or Investigational. (We do not require completion of this form, but provide it for your convenience. Your provider must certify to us in writing that your request is of an expedited nature before we will proceed with it as an expedited appeal.)
AultCare Treating Physician Certification for Internal Appeal and/or External Review
You may have your provider complete this form if your request for benefit determination has been denied and you are requesting an expedited appeal or review. (We do not require completion of this form, but provide it for your convenience. Your provider must certify to us in writing that your request is of an expedited nature before we will proceed with it as an expedited appeal.)
External Review Procedures Summary
An explanation of the External Review procedure for all Insured and Public Employer Plans effective 02/2012.
External Review Request Form
If you disagree with our appeal decision and have exhausted your internal appeal rights, you can request an External Review using this form. (For Insured and Public Employer Plans Only)
AultCare Request for Review by the Ohio Department of Insurance
If we have denied your request for an External Review and you disagree with our decision, please use this form.
Online EOB (Explanation of Benefit) for Claim Guide
AULTCAREANDAULTRAEOBGUIDE
Background
Welcome to our AultCare family. Whether you are a new member, or have been with us for many years, we are proud to help you and your employees with one of your most precious commodities, your health.
Our websites give you the ability to view your EOB (Explanation of Benefit) claims online. EOBs contain detailed information relating to claims, including diagnosis and costs involved. The remainder of this document contains information on availability of EOBs and how to find them.
Before you can use the AultCare website as a logged in member, you must register for a secure online account. This document is designed to walk you through each step to create your online members account. There are additional “How to Guides” to help members, employers, providers, vendors and brokers located in the AultSupport area of our website.
If you have questions, you can email the AultCare Web Team at AultConnect@AultCare.com.
Sincerely,
Your AultCare Team
Access your EOBs on www.aultcare.com
AULTCAREANDAULTRAEOBGUIDE 2
How do I know if an EOB is available for a claim?
Availability of EOBs per claim depends on the date of the claim.
An online EOB will be available no earlier than 1 week after we receive a claim.
o An EOB will also not be available if it incurred prior to August, 2011.
If your claim is through an Aultra group, an online EOB for that claim will be available no earlier than 1 week after we receive claim.
o The EOB is also not available if it incurred prior to 2008.
Step 1) Log into our website at www.aultcare.com

Step 2) Log in with your username and password
AULTCAREANDAULTRAEOBGUIDE 3
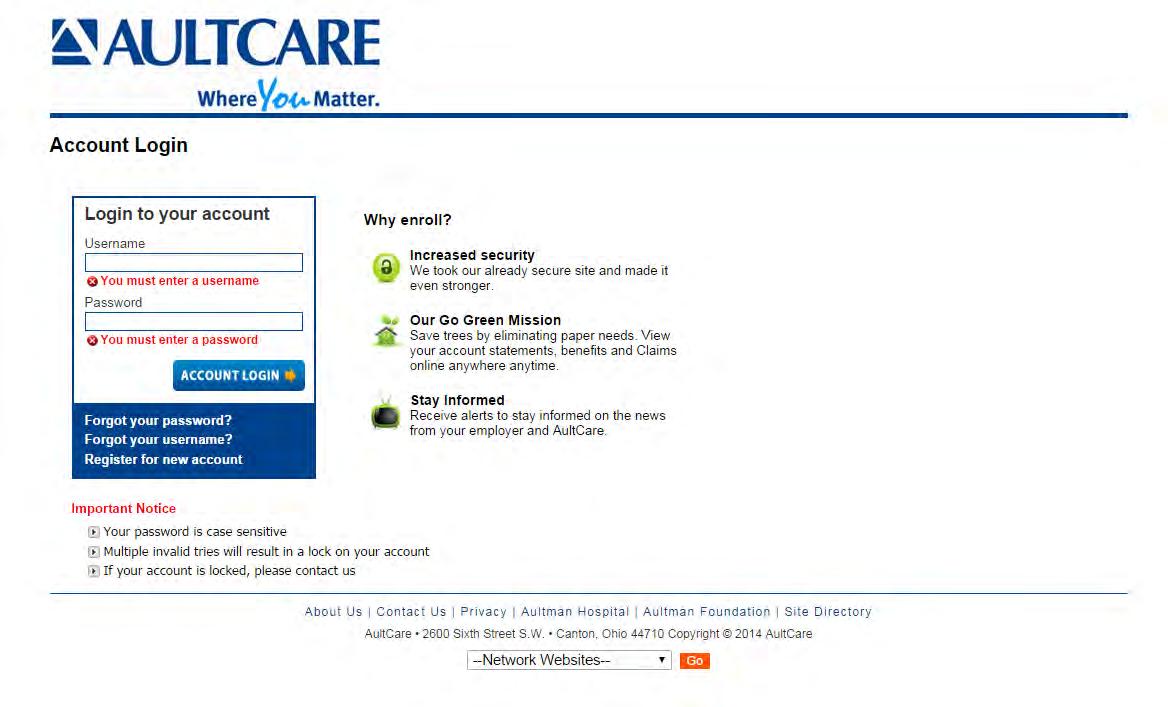
AULTCAREANDAULTRAEOBGUIDE 4
Step 3) Click on the “Claims and EOBs” link near the top of the page

AULTCAREANDAULTRAEOBGUIDE 5
Step 4) Enter your search criteria and click the “Search” button

AULTCAREANDAULTRAEOBGUIDE 6
Step 5) Locate a claim and look for the “EOB” link:

If you have questions, you can contact your group coordinator, or for technical assistance, email the AultCare Web Team at AultConnect@AultCare.com
AULTCAREANDAULTRAEOBGUIDE 7



UNDERSTANDING YOUR EXPLANATION OF BENEFITS (EOB)
WHAT IS AN EOB?
An EOB is a statement from your health insurance plan detailing the costs towards a medical procedure or service you received. An EOB is not a bill.
The purpose of an EOB is to clearly state the cost of care received, costs covered by the insurance plan, and member cost share.
HOW DO I RECEIVE MY EOBS?
Members are automatically enrolled to receive their EOBs via their secured, online member account.
To access your EOBs:
• Visit www.aultragroup.com and log into your account.
• Select My Claims
• Use the filters to find a specific claim or scroll to the bottom of the page to view your claims. Select a claim number to review the EOB.
If you would like to receive paper EOBs via mail, please contact Aultra Customer Service.
ITEMS OF INTEREST

When reviewing your EOB, these areas are clearly denoted. On the reverse side of this flyer, there is an example of an EOB.
• Claim payment details
» Provider name
» Claim number
• Date of service and name of procedure/service
• Cost of procedure/service
• Any applicable discounts and provider adjustments
• Payment amount paid by Aultra based on your plan’s deductible, copayment and insurance
• Amount the member is responsible to pay
6313/20
CONTACT US 330-363-2050 | 1-855-270-8497 www.aultragroup.com

If you have questions regarding this correspondence, please call 330-363-2050 or 855-270-8497. M - F 7:30 AM to 5:00 PM EST, or visit our website at www.aultragroup.com
*If this plan is the secondary payer, the patient responsibility field may not reflect accurately. Please confirm the amount due with your provider of service. **For current accumulator information, please view your account on our website. *** The affiliation fee is a contracted amount between the provider and the leased network. The patient is not responsible for this amount.
Group: Group #: Explanation of Benefits Enrollee Copy Date: This is not a bill
Member ID: Employee: Patient Name: Patient #: Provider Name: Claim#: Dates of Service -- CPT/Mod Procedure Billed Amount Ineligible Amount Inel Code Contractual Adjustment Coin-Copay/ Deductible Payment Amount Adj Code 165.00 25.00 37.88 102.12 OG 0.00 Patient Responsibility 25.00 102.12 25.00 TOTALS 165.00 102.12 Total Net Payment: Amount Payment To: Check No 102.12 Reason Code Description OG OHC/PREFERRED HEALTH CHOICE NETWORK DISCOUNT, PATIENT NOT LIABLE. Additional
D DD DD DD DF FF FA AA AT TT TT TT TD DD DD DD DT TT TA AA AA AA AD DD DA AA AD DD DF FF FT TT TF FF FD DD DF FF FF FF FF FF FF FF FT TT TF FF FD DD DD DD DA AA AD DD DA AA AA AA AD DD DD DD DD DD DD DD DD DD DF FF FA AA AD DD DD DD DF FF FT TT TT TT TF FF FD DD DD DD DT TT TD DD DT TT TA AA AA AA AF FF FF FF FA AA AD DD DT TT TD DD DD DD DA AA AD DD DD DD DA AA AF FF FF FF FA AA AF FF F Electronic Service Requested Canton, OH 44706-0910 P.O. Box 6910 AULTRA ADMINISTRATIVE GROUP P279702801E P279702801E 202003202020 DATE OF SERVICE -- CPT/MOD PROCEDURE Member address information Group information Claim payment detail EXAMPLE: EXPLANATION OF BENEFITS (EOB) Date of service and name of procedure/service Cost of procedure/service Amount based on adjustments and coinsurance/copay/deductible Amount Aultra will pay Member responsibility amount O3 O3 FEE ADJUSTMENT/PROVIDER DISCOUNT, PATIENT NOT REQUIRED TO PAY.
Messages
GRIEVANCES AND APPEALS
GRIEVANCE PROCESS
If you are unsatisfied with Aultra or your network providers, you are advised to contact Aultra as soon as possible to begin the grievance process. You can contact Aultra about your concern and you will be forwarded to someone who can assist you in the necessary steps to help reach a resolution. You may also mail your grievance to: Grievance and Appeal Coordinator, PO Box 6029, Canton, OH 44706.
APPEALS PROCESS
If you disagree with a determination about a specific benefit, you have the right to appeal Aultra’s decision and request a review of the determination through the appeals process. The appeal process can be initiated by you and/or your provider or your authorized representative. Your appeal must be submitted within 180 calendar days of the adverse determination and should contain a statement describing the reasons why you feel your claim/services should not have been denied, written comments, documents, records or other information relating to the claim/service.
A full and fair review will be conducted, taking into consideration all of the information received with the appeal. Clinical appeals, or appeals relating to decisions based on medical necessity, are conducted by health professionals. Appeals can be mailed to: Grievance and Appeal Coordinator, PO Box 6029, Canton, OH 44706.
Aultra will send you a notification in writing regarding the determination of your appeal based upon the type of appeal. Time frames are as follows:
» Pre-service appeals will be answered within 15 calendar days of receipt.
» Post-service appeals will be answered within 30 days of receipt.
» Urgent/concurrent care appeals will be answered as soon as possible, but not greater than 72 hours of receipt.
You may contact Aultra or refer to your plan documents for more information on how to file an appeal. You can also contact Aultra if you would like a copy of the appeal process specific to your group plan. Please refer to your plan documents and/or letter of denial for additional levels of appeal available to you.
US
| 1-855-270-8497
CONTACT
330-363-2050
www.aultragroup.com
you youmatter 6229/20

INTERNAL APPEAL REQUEST FORM Page 1 of 3 AAG Internal Appeal Request Form Rev. 2/2012, 2/2020 Name of person filing appeal: Relationship to covered person: Covered Person/Applicant Authorized Representative (please complete the Appointment of Authorized Representative section) How would you like us to contact you? Phone Fax Email Mail Contact information of authorized representative (if applicable) Mailing Address: Daytime Phone: Evening Phone: Email Address: Fax: Covered Person/Applicant Information Name: ID Number: Mailing Address: Daytime Phone: Evening Phone: Email Address: Fax: Treating Physician/Health Care Provider Information Name: Mailing Address: Phone Number: Email Address: Fax Number: Contact Person: Phone Number: Internal Appeal Specifications 1. Are you requesting an expedited appeal because your health, life or ability to regain maximum function may be in serious jeopardy while you wait up to 30 days for a decision on your appeal? YES NO 2. Are you requesting an expedited appeal because your physician certifies that your pain can not be controlled while you wait up to 30 days for a decision on your appeal? YES* NO 3. Are you requesting a Concurrent Expedited Internal Appeal and Expedited External Review and your physician certifies that it is necessary?(Note: Request for External Review form is not required.) YES* NO

INTERNAL APPEAL REQUEST FORM
*If you answer YES to question 2 or 3 above, your physician must certify that your condition could, in the absence of immediate medical treatment, result in any of the following:
-Seriously jeopardize your life or health or your ability to regain maximum function, or
-Subject you to severe pain that cannot be adequately managed without the care or treatment that is the subject of the claim. You may also have your physician certify if you answer YES to question 1.
Briefly describe why you disagree with this decision (you may attach additional information, such as a physician’s letter, bills, medical records, or other documents to support your claim):
Appointment of Authorized Representative (complete when someone else is representing you in this appeal)
You may represent yourself, or you may ask another person, including your treating health care provider, to act as your authorized representative. You may revoke this authorization at any time.
I hereby authorize to pursue my appeal on my behalf.
Signature of Covered Person (or legal representative**)
Signature and Release of Medical Records
Date
To appeal the denial of coverage, you must sign and date this Appeal Request Form and consent to the release of medical records.
I hereby request an appeal. I attest that the information provided on this form is true and accurate to the best of my knowledge. I authorize my treating physician, health care provider, and/or health plan issuer to release all relevant medical or treatment records to an independent review organization, the Ohio Department of Insurance, and/or my health plan issuer. I understand that the independent review organization, the Ohio Department of Insurance, and/or my health plan issuer will use this information to make a determination on my appeal and that the information will be kept confidential and not be released to anyone else. This release is valid for one year. I understand that I or my authorized representative is entitled to receive a copy of this authorization.
Signature of Covered Person (or legal representative**)
**Parent, Guardian, Conservator or Other - please specify
Date
Page 2 of 3
Internal Appeal Request Form Rev. 2/2012, 2/2020
AAG

Be certain to keep copies of this form, your Notice of Adverse Benefit Determination and all documents and correspondence related to this claim.
Page 3 of 3
Internal Appeal
Form Rev. 2/2012, 2/2020
INTERNAL APPEAL REQUEST FORM
AAG
Request
SEND THIS FORM AND A COPY OF YOUR NOTICE OF ADVERSE BENEFIT DETERMINATION TO ONE OF THE FOLLOWING ADDRESSES: Fax Number: 330-363-3066 Email Address: Aappeals@aultcare.com Mailing Address: Attention: Grievance and Appeal Coordinator P.O. Box 6029 Canton, Ohio 44706

TREATING PHYSICIAN CERTIFICATION FOR EXPERIMENTAL/INVESTIGATIONAL ADVERSE BENEFIT DETERMINATIONS
Note to the Treating Physician
Covered Persons may request an external review when a health plan issuer has denied a health care service or course of treatment that is considered experimental or investigational and is NOT explicitly listed as an excluded benefit under the covered person’s health benefit plan. This form is for the purpose of providing the certification necessary to obtain a review. Please complete the entire form including the certification and return the executed form to the address shown below.
Fax Number: 330-363-3066
Email Address: Aappeals@aultcare.com
I hereby certify that I am a treating physician for (hereafter referred to as “the covered person”); and that I have requested the authorization for a drug, device, procedure or therapy denied for coverage due to the health plan issuer’s determination that the proposed therapy is experimental and/or investigational. I understand that in order for the covered person to obtain the right to an external review of this denial, as treating physician I must certify that the covered person’s medical condition meets certainrequirements:
Page 1 of 2 AAG Treating Physician Certification Form for Experimental/Investigational Adverse Benefit Determinations Rev. 2/2012, 2/2020
MAILING ADDRESS: Attention:
P.O.
General Information Name of Covered Person/Patient: Covered Person’s Health Plan ID Number: Name of Treating Physician: Licensure and Area of Clinical Specialty: Mailing Address: Phone Number: Email Address: Fax Number: Contact Person: Phone Number:
Grievance and Appeal Coordinator
Box 6029 Canton, Ohio 44706

TREATING PHYSICIAN CERTIFICATION FOR EXPERIMENTAL/INVESTIGATIONAL ADVERSE BENEFIT DETERMINATIONS
In my medical opinion as the covered person’s treating physician, I hereby certify to the following: (Please check all that apply)
Standard health care services have not been effective in improving the condition of the covered person
Standard health care services are not medically appropriate for the covered person
There is no available standard health care service covered by the health plan issuer that is more beneficial thanthe requested health care service
Please provide a description of the recommended or requested health care service or treatment that is the subject of the adverse benefit determination. Please include any documentation that will be beneficial to the review process. Please attach additional sheets as necessary.
Treating Physician Printed Name: Signature Date
Page 2 of 2 AAG Treating Physician Certification Form for Experimental/Investigational Adverse Benefit Determinations Rev. 2/2012, 2/2020

TREATING PHYSICIAN CERTIFICATION FOR INTERNAL APPEAL AND/OR EXTERNAL REVIEW
Note to the Treating Physician
Covered Persons may request an internal appeal and/or external review when a health plan issuer has denied a health care service or course of treatment. The standard internal appeal and external review processes can take up to 30 days from the request date to the date a decision is rendered. Expedited appeals or reviews are only available under the circumstances shown below. This form is for the purpose of providing the certification necessary to obtain an expedited appeal or review. Please complete the General Information section along with the appropriate certification and return the executed form to the addresses shown below:
Fax Number: 330-363-3066
Email Address: Aappeals@aultcare.com
I hereby certify that I am a treating physician for (hereafter referred to as “the covered person”); that adherence to the time frame for conducting a standard internal appeal would, in my professional judgment, subject the covered person to severe pain that cannot be adequately managed without the requested care or treatment; and that, for this reason, the covered person’s appeal should be processed on an expedited basis.
Page 1 of 2 AAG Treating Physician Certification Form for Internal Appeal and/or External Review Rev. 2/2012, 2/2020
MAILING ADDRESS: Attention:
P.O. Box
General Information Name of Covered Person/Patient: Covered Person’s Health Plan ID Number: Name of Treating Physician: Licensure and Area of Clinical Specialty: Mailing Address: Phone Number: Email Address: Fax Number: Contact Person: Phone Number: Expedited Internal Appeal Certification
Grievance and Appeal Coordinator
6029 Canton, Ohio 44706
Printed Name:
Treating Physician

TREATING PHYSICIAN CERTIFICATION FOR INTERNAL APPEAL AND/OR EXTERNAL REVIEW
Signature Date
Concurrent Expedited Internal Appeal and Expedited External Review Certification
I hereby certify that I am a treating physician for (hereafter referred to as “the coveredperson”); and (select all thatapply):
that adherence to the time frame for conducting an expedited internal appeal would, in my professional judgment, seriously jeopardize the life or health of the covered person or would jeopardize the covered person’s ability to regain maximum function; and that, for this reason, the covered person’s expedited internal appeal should be conducted simultaneously with an expedited external review.
that the recommended experimental or investigational treatment would, in my professional judgment, be significantly less effective if not promptly initiated; and that, for this reason, the covered person’s expedited internal appeal should be conducted simultaneously with an expedited external review. I have attached the completed Treating Physician Certification Form for Experimental/ InvestigationalAdverse BenefitDeterminations.
Treating Physician Printed Name:
Signature Date
I hereby certify that I am a treating physician for (hereafter referred to as “the covered person”); that adherence to the time frame for conducting a standard external review would, in my professional judgment, seriously jeopardize the life or health of the covered person or would jeopardize the covered person’s ability to regain maximum function; and that, for this reason, the covered person’s external review should be processed on an expedited basis.
Treating Physician Printed Name:
Signature Date
Page 2 of 2
Treating Physician Certification Form for Internal Appeal and/or External Review Rev. 2/2012, 2/2020
AAG
Expedited External Review Certification

Understanding the External Review Process
Under Ohio law, Aultra Administrative Group is required to provide a process that allows a person covered under a health benefit plan or a person applying for health benefit plan coverage to request an independent external review of an adverse benefit determination. An adverse benefit determination is a decision by Aultra Administrative Group not to provide benefits because we believe services are not medically necessary, or not covered, excluded, or limited under the plan, or we believe the covered person is not eligible to receive the benefit. An adverse benefit determination can also be a decision to deny health benefit plan coverage or to rescind coverage.
Opportunity for External Review
An external review may be conducted by an Independent Review Organization (IRO) or by the Ohio Department of Insurance.
A covered person is entitled to an external review by an IRO in the following instances:
• The adverse benefit determination involves a medical judgment or is based onany medical information
The adverse benefit determination indicates the requested service is experimentalor investigational, and the treating physician certifies at least one of the following:
o Standard health care services have not been effective in improving the condition of the covered person
o Standard health care services are not medically appropriate for thecovered person
o No available standard health care service covered by Aultra Administrative Group is more beneficial than the requested health care service
There are two types of IRO reviews, standard and expedited. A standard review is normally completed within 30 days. An expedited review for urgent medical situations is normally completed within 72 hours and can be requested if any of the following applies:
The covered person’s treating physician certifies that the adverse benefitdetermination involves a medical condition that could seriously jeopardize the life or health of the covered person or would jeopardize the covered person’s ability to regain maximum function if treatment is delayed until after the time frame of an expedited internal appeal or a standard external review
Page 1 of 4
External Review Procedures Summary Rev. 2/2012, 2/2020
EXTERNAL REVIEW PROCEDURES SUMMARY
AAG

EXTERNAL REVIEW PROCEDURES SUMMARY
The adverse benefit determination concerns an admission, availability of care, continued stay, or health care service for which the covered person received emergency services, but has not yet been discharged from a facility
An expedited internal appeal is in process for an adverse benefit determination of experimental or investigational treatment and the covered person’s treating physician certifies in writing that the recommended health care service or treatment would be significantly less effective if not promptly initiated
A covered person is entitled to an external review by the Ohio Department of Insurance in either of the following instances:
The adverse benefit determination is based on a contractual issue that does notinvolve a medical judgment or any medical information
The adverse benefit determination indicates that emergency medical services did not meet the definition of emergency AND the health plan issuer’s decision has already been upheld through an external review by an IRO
Request for External Review
The covered person must request an external review within 180 days of the date ofthe notice of final adverse benefit determination issued by Aultra Administrative Group.
All requests must be in writing, except for a request for an expedited external review.
Expedited external reviews may be requested electronically or orally; however written confirmation of the request must be submitted to Aultra Administrative Group no later than five (5) days after the initial request.
If the request is complete Aultra Administrative Group will initiate the external review and notify the covered person in writing that the request is complete and eligible for external review.
o The notice will include the name and contact information for the assigned IRO or the Ohio Department of Insurance (as applicable) for the purpose of submitting additional information
o The notice will inform the covered person that, within 10 business days after receipt of the notice, they may submit additional information in writing to the IRO or the Ohio Department of Insurance (as applicable) for consideration in the review
2
4
External Review Procedures
2/2012,
Page
of
AAG
Summary Rev.
2/2020

EXTERNAL REVIEW PROCEDURES SUMMARY
Aultra Administrative Group will also forward all documents and information used to make the adverse benefit determination to the assigned IRO or the Ohio Department ofInsurance (as applicable).
If the request is not complete Aultra Administrative Group will inform the covered personin writing and specify what information is needed to make the request complete.
If Aultra Administrative Group determines that the adverse benefit determination is not eligible for external review, we must notify the covered person in writing and provide the covered person with the reason for the denial and inform the covered person that the denial may be appealed to the Ohio Department of Insurance.
The Ohio Department of Insurance may determine the request is eligible for external review regardless of the decision by Aultra Administrative Group and require that the request be referred for external review. The Department’s decision will be made in accordance with the terms of the health benefit plan and all applicable provisions of the law.
IRO Assignment
The Ohio Department of Insurance maintains a secure web based system that is usedto manage and monitor the external review process.
When Aultra Administrative Group initiates an external review by an IRO in this system, the Ohio Department of Insurance system randomly assigns the review to an Ohio accredited IRO that is qualified to conduct the review based on the type of health careservice.
Aultra Administrative Group and the IRO are automatically notified of the assignment.
IRO Review and Decision
The IRO must forward, upon receipt, any additional information it receives from the covered person to Aultra Administrative Group. At any time Aultra Administrative Group may reconsider its adverse benefit determination and provide coverage for the health care service. Reconsideration will not delay or terminate the external review. If Aultra Administrative Group reverses the adverse benefit determination, they must notify the covered person, the assigned IRO and the Ohio Department of Insurance within one day of the decision. Upon receipt of the notice of reversal by Aultra Administrative Group, the IRO will terminate the review.
In addition to all documents and information considered by Aultra Administrative Group in making the adverse benefit determination, the IRO must consider things such as; the covered person’s medical records, the attending health care professional’s recommendation, consulting reports from appropriate health care professionals, the terms of coverage under the health benefit plan and the most appropriate practice guidelines.
The IRO will provide a written notice of its decision within 30 days of receipt by Aultra Administrative Group of a request for a standard review or within 72 hours of receipt by
3 of 4
External Review Procedures Summary Rev. 2/2012, 2/2020
Page
AAG

EXTERNAL REVIEW PROCEDURES SUMMARY
Aultra Administrative Group of a request for an expedited review. This notice will be sent to the covered person, Aultra Administrative Group and the Ohio Department of Insurance and must include the following information.
o A general description of the reason for the request for external review
o The date the independent review organization was assigned by the Ohio Department of Insurance to conduct the external review
o The dates over which the external review was conducted
o The date on which the independent review organization's decision was made
o The rationale for its decision
o References to the evidence or documentation, including any evidence-based standards, that was used or considered in reaching its decision
Binding Nature of External Review Decision
An external review decision is binding on Aultra Administrative Group except to the extent that we have other remedies available under state law. The decision is also binding on the covered person except to the extent the covered person has other remedies available under applicable state or federal law
A covered person may not file a subsequent request for an external review involving the same adverse benefit determination that was previously reviewed unless new medical or scientific evidence is submitted to Aultra Administrative Group
If You Have Questions About Your Rights or Need Assistance
You may contact:
Ohio Department of Insurance
ATTN: Consumer Affairs
50 West Town Street, Suite 300, Columbus, OH 43215
800-686-1526 / 614-644-2658
614-644-3744 (fax)
614-644-3745 (TDD)
Contact ODI Consumer Affairs:
Gateway.insurance.ohio.gov/UI/ODI.CS.Public.UI/Comment.mvc/Display
CommentSubmission
File a Consumer Complaint:
Gateway.insurance.ohio.gov/UI/ODI.CS.Public.UI/Complaint.mvc/Displa
yConsumerComplaintForm
4
Review
2/2012,
Page 4 of
AAG External
Procedures Summary Rev.
2/2020

*If you answer yes, your physician must certify that your condition could, in the absence of immediate medical treatment, result in the following:
-Seriously jeopardize your life or health or your ability to regain maximum function, or
FORM Page 1 of 3 AAG External Review Request Form Rev. 2/2012, 2/2020 Name of
Relationship to covered person: Covered Person/Applicant Authorized Representative (please complete the
of Authorized Representative section) How would you
Phone Fax Email Mail Contact information of
representative (if
Mailing Address: Daytime Phone: Evening Phone: Email Address: Fax: Covered Person/Applicant Information Name: ID Number: Mailing Address: Daytime Phone: Evening Phone: Email Address: Fax: Treating Physician/Health Care Provider Information Name: Mailing Address: Phone Number: Email Address: Fax Number: Contact Person: Phone Number: External Review Specifications 1. If your situation is urgent, are you requesting an expedited review?* YES NO 2. Is your requested health care service considered an experimental or investigational treatment?** YES NO
EXTERNAL REVIEW REQUEST
person filing request for external review:
Appointment
like us to contact you?
authorized
applicable)

EXTERNAL REVIEW REQUEST FORM
-Subject you to severe pain that cannot be adequately managed without the care or treatment that is the subject of the claim
**If you answer yes, your physician must certify that he or she is requesting authorization for a drug, device, procedure or therapy denied for coverage due to the determination that the treatment is experimental and/or investigational and the your medical condition meets certain requirements:
-Standard health care services have not been effective in improving your condition
-Standard health care services are not medically appropriate for you
-There is no available standard health care service covered by the health plan issuer that is more beneficial than the requested health care service
Briefly describe why you disagree with this decision (you may attach additional information, such as a physician’s letter, bills, medical records, or other documents to support your claim):
Appointment of Authorized Representative (complete when someone else is representing you in this appeal)
You may represent yourself, or you may ask another person, including your treating health care provider, to act as your authorized representative. You may revoke this authorization at any time.
I hereby authorize to pursue my external review on my behalf.
Signature of Covered Person (or legal representative**)
Signature and Release of Medical Records
Date
To appeal the denial of coverage, you must sign and date this Appeal Request Form and consent to the release of medical records.
I hereby request an external review. I attest that the information provided on this form is true and accurate to the best of my knowledge. I authorize my treating physician, health care provider and/or health plan issuer to release all relevant medical or treatment records to the independent review organization and/or the Ohio Department of Insurance. I understand that the independent review organization and the Ohio Department of Insurance will use this information to make a determination on my external review and that the information will be kept confidential and not be released to anyone else. This release is valid for one year. I understand that I or my authorized representative is entitled to receive a copy of this authorization.
Page 2 of 3 AAG External Review Request Form Rev. 2/2012, 2/2020

Signature of Covered Person (or legal representative**) Date *Parent, Guardian, Conservator or Other - please specify
SEND THIS FORM AND A COPY OF YOUR NOTICE OF FINAL ADVERSE BENEFIT DETERMINATION TO ONE OF THE FOLLOWING ADDRESSES: Fax Number: 330-363-3066 Email Address: Aappeals@aultcare.com Mailing Address: Attention: Grievance and Appeal Coordinator P.O. Box 6029 Canton, Ohio 44706
Be certain to keep copies of this form, your Notice of Final Adverse Benefit Determination and all documents and correspondence related to this claim.
Page 3 of 3
External Review
2/2012, 2/2020
EXTERNAL REVIEW REQUEST FORM
AAG
Request Form Rev.

REQUEST FOR REVIEW BY THE OHIO DEPARTMENT OF INSURANCE
Briefly describe why you disagree with the decision to deny your request for external review (you may attach additional information, such as a physician’s letter, bills, medical records, or other documents to support your claim):
Page 1 of 2 AAG Request for Review by the Ohio Department of Insurance Rev. 2/2012, 2/2020 Name of person filing request for review by the Ohio Department of Insurance: Relationship to covered person: Covered Person/Applicant Authorized Representative (please complete the Appointment of Authorized Representative section) How would you like us to contact you? Phone Fax Email Mail Contact information of authorized representative (if applicable) Mailing Address: Daytime Phone: Evening Phone: Email Address: Fax: Covered Person/Applicant Information Name: ID Number: Mailing Address: Daytime Phone: Evening Phone: Email Address: Fax: Treating Physician/Health Care Provider Information Name: Mailing Address: Phone Number: Email Address: Fax Number: Contact Person: Phone Number: Review Specifications

REQUEST FOR REVIEW BY THE OHIO DEPARTMENT OF INSURANCE
Appointment of Authorized Representative (complete when someone else is representing you in this appeal) You may represent yourself, or you may ask another person, including your treating health care provider, to act as your authorized representative. You may revoke this authorization at any time.
I hereby authorize to pursue my review by the Ohio Department of Insurance on my behalf.
Signature of Covered Person (or legal representative*)
Signature and Release of Medical Records
Date
To appeal the external review denial, you must sign and date this Request for Review by the Ohio Department of Insurance Form and consent to the release of medical records.
I, , hereby request a review of the external review denial. I attest that the information provided on this form is true and accurate to the best of my knowledge. I authorize my treating physician, health care provider and/or health plan issuer to release all relevant medical or treatment records to the Ohio Department of Insurance. I understand that the Ohio Department of Insurance will use this information to make a determination on my request for review of the denial and that the information will be kept confidential and not be released to anyone else. This release is valid for one year. I understand that I or my authorized representative is entitled to receive a copy of this authorization.
*Parent, Guardian, Conservator or Other - please specify
Be certain to keep copies of this form, your Notice of Denial of External Review Request for Administrative Reasons and all documents and correspondence related to this review.
2 of 2
for
the
2/2012, 2/2020
Page
AAG Request
Review by
Ohio Department of Insurance Rev.
Signature of Covered Person (or legal representative*) Date
Fax
ATTN:
50
SEND THIS FORM AND A COPY OF YOUR NOTICE OF DENIAL OF EXTERNAL REVIEW REQUEST FOR ADMINISTRATIVE REASONS TO ONE OF THE FOLLOWING: Phone Number: 1-800-686-1526 / 614-644-2658
Number: 614-644-3744 TDD: 614-644-3745 Mailing Address: Ohio Department of Insurance
Consumer Affairs
West Town Street, Suite 300, Columbus, OH 43215
MONTHLY INVOICES
An example of the monthly invoice that each company receives is provided on the following page. The invoice you receive may differ in column headings and amounts.
Examples of column headings include: Medical, Dental, Vision, various PPO Access Fees, COBRA and HIPAA. Self-funded companies may also see Dental Fees, Conversion Fees, Prescription Clinical fees, Specific Reinsurance and Aggregate Reinsurance. The last column provides the total fees for each employee.
The top portion of the invoice indicates the Run Date of the invoice and the Due Date of the payment. AultCare strives to have all bills run by the 15th and mailed by the 25th of each month. Payment is then due by the date indicated. If you have signed up to receive your bill electronically, you will be notified by e-mail that the invoices are available and you will access your invoice throughout our website at www.aultcare.com.
Any adjustments made to membership, such as termination, will be indicated in a section before the Grand Total. Eligibility changes that were received by the 10th of the month will be reflected on that month’s bill. General policy is to credit up to three months for terminations, so it is important to be up-to-date with eligibility changes. It is your responsibility to review this monthly billing for accuracy. Please note when mailing in your payment that no adjustments are to be written on the invoices and the amount sent should equal the Grand Total.
Please remit premium payment to: AultCare Insurance Premium Enclosed PO Box 6910 Canton, OH 44706
Account Summary Statement Glossary of Terms
• Account Summary Statement – The new billing statement will be referred to as an Account Summary Statement. You may have more than one account summary since our claims management system billing module organizes account statements by product, which could include different plan or benefit types.
• Companion Spreadsheet – To provide improved analytic capabilities, we have created a companion spreadsheet, which conveniently combines multiple Account Summary Statements. The spreadsheet contains multiple worksheets with different breakouts of your billing statement including Detail, Summary of Coverage Type, Summary by Rate Code, and Summary by Invoice Number. (Click on the Sample Excel Invoice link under the Miscellaneous category to open the document.) The companion spreadsheet can be accessed through our secure AultCare Employer Web Portal. If you do not have an online account, please refer to section two of the Administrative Guide)
• Additional Columns – On the 3rd page of the sample billing statement, you will find additional columns. Our new billing statement is a universal bill, and many of our clients have multiple products, which are reflected in the columns.
• Statement Date – Typically, AultCare runs your bill 15 days prior to the due date. Payments submitted for a prior month that do not arrive by the statement date may not appear on your next month’s bill.
• Rate Code - The rate code reflects how we categorize your employee population. Rate codes can reflect coverage type, plan type, and other internal classifications required to accurately administer your plan.
• Payment Methods – You may send 1 check, even though you may have received multiple Account Summary Statements. It is important to note that you must return all remittance vouchers at the bottom of each Account Summary Statement to ensure proper posting. The total due can be found on the detail page under the “Grand Total” heading. Complete the Funding Form with your desired payment method.
o Payment By EFT – Paying by EFT is the easiest and quickest way to pay your bill.
o Payment by Check – You may pay by check, but please remember to return all remittance vouchers to ensure proper posting.





Rate Code Member Coverage Type COBRA Leased Netwo rk Medical Admin Network Fees Dental Vision HRA/HSA /FLEX Stop Loss Ancillary Broker Comp Total ACTIVE A15S BROWN, JIM 1 $236.55 $0.00 $0.00 $0.00 $0.00 $0.00 $0.00 $0.00 $236.55 ACTIVE A15S DELAMIELLEURE, JOE 1 $236.55 $0.00 $0.00 $0.00 $0.00 $0.00 $0.00 $0.00 $236.55 ACTIVE A15S GRAHAM, OTTO 1 $236.55 $0.00 $0.00 $0.00 $0.00 $0.00 $0.00 $0.00 $236.55 ACTIVE A15S Total Employee Count: 3 $709.65 $0.00 $0.00 $0.00 $0.00 $0.00 $0.00 $0.00 $709.65 ACTIVE S2C BROWN, PAUL 1 $427.70 $0.00 $0.00 $0.00 $0.00 $0.00 $0.00 $0.00 $427.70 ACTIVE S2C HICKERSON, GENE 1 $427.70 $0.00 $0.00 $0.00 $0.00 $0.00 $0.00 $0.00 $427.70 ACTIVE S2C LAVELLI, DANTE 2 RN35 $898.15 $10.00 $0.00 $0.00 $0.00 $0.00 $0.00 $0.00 $908.15 ACTIVE S2C MOTLEY, MARION 1 $427.70 $0.00 $0.00 $0.00 $0.00 $0.00 $0.00 $0.00 $427.70 ACTIVE S2C Total Employee Count: 4 $2,181.25 $10.00 $0.00 $0.00 $0.00 $0.00 $0.00 $0.00 $2,191.25 Current Month Total $2,890.90 $10.00 $0.00 $0.00 $0.00 $0.00 $0.00 $0.00 $2,900.90 ACTIVE A15S KOSAR, BERNIE 1 ($236.55) $0.00 $0.00 $0.00 $0.00 $0.00 $0.00 $0.00 ($236.55) Adjustment - June 2018 Total Employee Count: 1 ($236.55) $0.00 $0.00 $0.00 $0.00 $0.00 $0.00 $0.00 ($236.55) ACTIVE A15S KOSAR, BERNIE 1 ($236.55) $0.00 $0.00 $0.00 $0.00 $0.00 $0.00 $0.00 ($236.55) Adjustment - July 2018 Total Employee Count: 1 ($236.55) $0.00 $0.00 $0.00 $0.00 $0.00 $0.00 $0.00 ($236.55) COBRA PACKETS 0 $0.00 $0.00 $0.00 $0.00 $0.00 $0.00 $100.00 $0.00 $100.00 Manual Adjustment Total $0.00 $0.00 $0.00 $0.00 $0.00 $0.00 $100.00 $0.00 $100.00 AR Balance Amount 0 $0.00 $0.00 $0.00 $0.00 $0.00 $0.00 $9,547.90 $0.00 $9,547.90 AR Balance Amount Total $0.00 $0.00 $0.00 $0.00 $0.00 $0.00 $9,547.90 $0.00 $9,547.90 Adjustment Total ($473.10) $0.00 $0.00 $0.00 $0.00 $0.00 $9,647.90 $0.00 $9,174.80 Grand Total $12,075.70 Aultra
Group Invoice Date: 8/1/2018

Self Funded - Funding Arrangements
CLAIM PAYMENTS and ADMINISTRATIVE FEES
CLAIM CHECK & EFT RUN - Select the preferred day of the week for the claim check run.
NOTIFICATION - The day following the check run, AultCare will provide a claim report and invoice for the total dollar amount due for claims processed. Select the preferred notification method.
E-Mail: Yes No If yes, provide e-mail address and person to receive this information.
Web: Yes No If yes, AultCare will post claim information to the employer portal, www.aultcare.com
FUNDING ARRANGEMENT - Benefit checks are released upon receipt of appropriate funding. Select and complete one payment option
AultCare Draft from your account: Yes No If yes, provide the following: Bank Name:
{
MONTHLY ADMINISTRATIVE FEE INVOICE
(Pay as billed, enrollment adjustments will be made to subsequent invoices)
FUNDING ARRANGEMENT - Select and complete one option
ACH Transfer to AultCare: Yes No
AultCare Corporation Account Number: 01039702501
Routing Code: 044000024
AultCare Draft from your account: Yes No If yes, provide the following:
COMPANY NAME:_______ ________________________________ Group # ___________________
MONDAY TUESDAY WEDNESDAY THURSDAY FRIDAY
Bank
Account
Routing
Contact & Phone Number:
Number:
Code: ________________________________________
{ } Withdraw funds the day after closing is received
}
Withdraw funds upon notification from company to benefitinvoice@aultcare.com
ACH
Huntington
AultCare
{ } Withdraw funds after ____ business days from closing (no greater than 4 days)
Transfer to AultCare: Yes No
Bank
Corporation Account Number: 01038342153 Routing Code for ACH payments: 044115090 Routing Code for Wire transfers: 044000024
Bank Name: Bank
&
Number: Name on Account: Tax Identification Number: _______________________________________ Account Number: Routing Code: ________________________________________ Note: Automatic withdrawal on the 1st of every month Completed by (printed name): ___________________________________________________ Signature: Date: Forward to Technical Support & Billing Revised 2/1/19
Contact
Phone
Group Reporting USER GUIDE

INTRODUCTION
Data Availability
The reports are built using medical and pharmacy claims data as well as membership, enrollment and provider information. Throughout the reports, you will find both paid amounts and utilization metrics. The paid amount is the amount paid to the provider by the health plan on a claim.
Reporting Dates
Most monthly reports are based on paid dates and show year to date values. Some reports show the previous months values along with the year to date. Reinsurance reports will be based on your reinsurance contract incurred and/or paid dates.
Medical Claims Category
This report utilizes AultCare methodologies to stratify claims into high level categories. This methodology classifies healthcare claims data into groupings of similar types of services and calculates utilization measures. The Medical Claims Category Report allows you to compare current month and year to date on a total and a paid per unique enrollee basis by service category.
Diagnosis and Medical Procedure Summary
The Diagnosis and Medical Procedure Summary report contains two separate reports. Each worksheet displays a summary of the medical claims grouped by the primary diagnosis or primary procedure code. The report contains number of enrollees, the total paid, the total volume, the paid per unit, and the paid per unique enrollee.
Eligibility Breakdown Summary Report
One important component to understanding your healthcare information is to understand your population. In the Eligibility Breakdown Report you will find your total population as well as the distribution of your population by relationship and reporting division.
Cost Per Employee by Benefit
This report summarizes the total paid amount by benefit by month displaying the cost per enrollee and the cost per employee on a monthly basis and a year to date basis. This is a good tool to use to see how your healthcare costs are changing throughout the year.
Specific Reinsurance Individual Summary
Specific Reinsurance is the form of excess risk coverage that provides protection against a high claim cost on any one individual. This is protection against abnormal severity of a single claimant rather than abnormal frequency of claims in total. Specific stop-loss is also known as individual stop-loss. The Specific Reinsurance Individual Summary reports on any member who has a paid amount greater than 50% of the contract’s specific deductible reported on the terms of the stop loss contract. The report indicates the amount above the specific retention, amounts that have been reimbursed by the stop loss carrier and any outstanding or open amount.
Lag Report by Benefit
The Lag Report is usually requested for a client’s accounting and audit purposes. This report shows two full years plus the current year of paid dates and analyzes historical claims information to determine the length of time lag between the date of service and the date a claim is paid.
Pharmacy Summary Report
The Pharmacy Summary Report shows your top 25 drugs and a summary of your pharmacy costs by Therapeutic class. The report contains the paid amount, number of prescriptions, and the cost per prescription.
IRSElig Report
This report provides an accounting of each member covered by month. The report is a useful tool which provides the information necessary for the annual ACA 1094/1095 reporting.
ENROLLEE QUESTIONNAIRES
This section provides an explanation of various questionnaires that enrollees may receive if there is a question regarding how to pay a claim. Encourage employees to respond to any forms received in order to have their claims paid quickly and correctly.
Attachment #1: Other Coverage Information Form (2-page form)
Unless otherwise instructed by a self-funded company, AultCare will send out a yearly Other Coverage Information Form to be updated with the next claims received for any member of the family following one year on the plan. Upon receipt of the completed form, the system is noted with the updated information and any pended claims are processed.
Attachment #2: Accident Questionnaire
The Accident Questionnaire is mailed in the cases of accidents mainly to determine if a third party might be responsible for an accident. Claims are pended until we receive a signed response to the questionnaire. Cases involving a third party are referred to our Subrogation Department to pursue reimbursement for the Plan.
Attachment #3: Designation of Authorized Representative Form
The Designation of Authorized Representative Form is used to confirm permission to discuss with or disclose to a person’s protected health information (PHI).
Have you, your spouse, or any dependents covered under this Aultra plan had any other Medical, Dental, Vision, RX, or Medicare coverage in the past 24 months?
No: The rest of the form does not need to be completed. Please sign and date the second page and return to Aultra.
Yes: Please complete entire form, sign, date, and return to Aultra.
Do you have health insurance in which you are the enrollee/policyholder for other than this Aultra plan?
If additional space is needed, please use page 3.
For any children age 18 or older who have insurance coverage other than through a natural/step parent, please complete part 4A.
FORM PART 3 CHILDREN INFORMATION Children’s First and Last Names Relationship Natural child of enrollee & spouse Natural child of enrolleePart 4 Natural child of spousePart 4 Other______________Part 4 Natural child of enrollee & spouse Natural child of enrolleePart 4 Natural child of spousePart 4 Other______________Part 4 Natural child of enrollee & spouse Natural child of enrolleePart 4 Natural child of spousePart 4 Other______________Part 4 Natural child of enrollee & spouse Natural child of enrolleePart 4 Natural child of spousePart 4 Other______________Part 4 Group # Enrollee Name Member ID # Actively Working Retired Date of Retirement _________________ Disabled-Working Disabled-Not Working
OTHER COVERAGE INFORMATION
No: Previous Carrier Termination Date Yes: Complete below OTHER Coverage: Active plan Retiree plan COBRA Individual plan Medicare Insurance Name Group # Effective Date Current Employer Name Who is covered under OTHER plan? Check coverage(s): Medical Dental Vision Prescription Supplemental/Medicaid PART 1 ENROLLEE INFORMATION Spouse’s Name Date of Birth Date of Marriage Is spouse
No
of Employer
No Part-time Benefits not offered Unemployed Self-employed Cost Waiting period Eligible for coverage date _____________ Date prior coverage terminated ______________ Yes OTHER coverage: Active plan Retiree plan COBRA Individual plan Medicare Policyholder’s Name ID # Group # Insurance Name Effective Date Who is covered under spouse’s plan? Check coverage(s): Medical Dental Vision Prescription Supplemental/Medicaid PART 2 SPOUSE INFORMATION (complete
employed?
Yes If Yes, Name
Does spouse have other coverage?
if married)
Please complete all information in this section for each child covered under your plan who have a different biological parent other than the enrollee and spouse listed on the first page. If not previously provided, court documentation and/or divorce decrees must be submitted to Aultra in order to accurately update your records.
Any person who, with intent to defraud or knowing that he or she is facilitating a fraud against an insurer, submits an application or files a claim containing a false or deceptive statement is guilty of insurance fraud. I acknowledge that AultCare may use and disclose my protected health information, as well as, the protected health information of my family for payment, treatment, and operations. This information may be disclosed to other insurance companies, third party administrators, state and federal agencies, health care providers and other organizations and persons that perform professional, business, or insurance functions for AultCare, as permitted by state and federal law. The information may be used for, but not limited to, processing enrollment applications, risk classifications, detecting or preventing fraud, internal and external audits, claims administration, case management, quality improvement programs, public health reporting, law enforcement investigations, coordination of benefits, medical management programs, and subrogation.
Reviewed: 01/2022 Group # Enrollee Name Member ID #
Child’s Name Is their address the same as the enrollee? Yes No
no,
Address
17 or older,
provide
of
school Name of Other Biological/Adoptive Parent Parent’s Date of Birth Other Parent’s Address Does child(ren) have insurance coverage other than this Aultra plan? Yes No Same as spouse’s coverage? Yes No If no,
complete the information below. Policyholder’s Name Relationship to Child Insurance Name Effective Date Term Date Check coverage(s): Medical Dental Vision Prescription Supplemental/Medicaid PART 4 DIVORCED, LEGALLY SEPARATED, SINGLE PARENT, OR OTHER Child’s Name Is insurance coverage available through adult child’s employer? Yes No Policyholder’s Name Relationship to Child Insurance Name Effective Date Term Date Check coverage(s): Medical Dental Vision Prescription Supplemental/Medicaid PART 4 A CHILDREN WITH INSURANCE COVERAGE OTHER THAN A PARENT’S PLAN Name___________________________________ Part A Effective Date _______________ Part B Effective Date _______________ Part D Effective Date _______________ Reason for Medicare coverage: Age 65 or older Disabled End Stage Renal Disease (ESRD) Date dialysis treatment began _______________ Dialysis started at Facility Self/home dialysis Date of kidney transplant _______________ PART 5 MEDICARE INFORMATION ( Please complete for all Medicare recipients) Enrollee’s Signature _____________________________________________ Date __________________ Enrollee’s Phone Number _________________________ Email ____________________________________ Name___________________________________ Part A Effective Date _______________ Part B Effective Date _______________ Part D Effective Date _______________ Reason for Medicare coverage: Age 65 or older Disabled End Stage Renal Disease (ESRD) Date dialysis treatment began _______________ Dialysis started at Facility Self/home dialysis Date of kidney transplant _______________
6910
If
provide
If
please
date
graduation from high
please
Please mail or fax this form to: Aultra Attn: COB, PO Box
Canton, OH 44706 or 330-363-7746 Attn: COB
7504/22
Note: If any changes occur during the year, please notify Aultra at 330-363-2050 | 1-855-270-8497 | TTY: 711.
INSURANCE FRAUD WARNING:

ACCIDENT QUESTIONNAIRE
ALL CLAIMS RELATED TO THIS INJURY WILL BE PENDED WHILE AWAITING THE RETURN OF THIS FULLY COMPLETED QUESTIONNAIRE. IF YOU HAVE ANY QUESTIONS WHILE COMPLETING THIS QUESTIONNAIRE, DO NOT HESITATE TO CONTACT OUR OFFICE AT (330)363-6360.
1.What was the date of your accident/injury?__________________
2.How did your accident/injury occur?__________
3.Where did the accident/injury occur? (Please check appropriate box)
Auto/Motorized Vehicle
Home
Work – if yes, was a workers comp claim filed ___yes ___no
No accident, sudden onset (please contact the Service Center)
Other, please specify____________________________________________________
4.Automobile Accident Information
a) If an automobile accident, were you a driver, a passenger, or a pedestrian
b) If an auto accident, were all covered family members involved wearing seatbelts at the time of the accident?_______________________________________________________
c) If accident involved a motorcycle or recreational vehicle, was a helmet being worn at the time of accident?__________________________________________________________
d) If motor vehicle accident, were you or a covered family member under the influence of drugs or alcohol. (Includes all motorized recreational vehicles, boats, etc.)?
e) Is there a police report? ( ) Yes ( ) No If yes, where can we obtain a copy?
f) Were any parties in the accident charged? Who? What offense? ___________________
5.What is the name, address and telephone number of other insurance carriers that a claim has been filed with? Claim number and adjuster name?____________________________________
6.Were you responsible for the accident? ( ) Yes ( ) No
7.Was another party responsible for your accident? ( ) Yes – please proceed to page 2 ( ) No – please sign and return form; do not complete page 2
5 Fulton Dr. NW / P.O. Box 35276 / Canton, OH 44735-5276
(330)493-7278 / www.aultragroup.com
484
Phone:

8.a)What is the name, address and telephone number of the party responsible for your accident?
b)What are the name, address, and telephone number of the other party’s insurance carrier? Claim number and adjuster name. ____________________________________________________________________________
9.) Have any payments been made on expenses incurred as a result of this accident? ( ) Yes ( ) No If yes, please explain. ____________________________________________ _____________________________________________________________________________
10.) Have you retained an attorney? ( ) Yes ( ) No If yes, what is the name, address, and telephone number of your attorney? _____________________________________________________________________________
I hereby authorize that the plan administrator is entitled to recover claim payments made on my behalf, from any future settlement in my favor, from the third party of other insurance carriers responsible for my accident and corresponding claim(s) outline above. Recovery can also be made from me if I receive the settlement directly from the third party or other insurance carrier.
I hereby authorize the plan administrator to forward copies of claims to the insuring company and attorney.
I hereby authorize release of any information necessary to verify or investigate items pertaining to this accident.
5 Fulton Dr. NW / P.O. Box 35276 / Canton,
(330)493-7278 / www.aultragroup.com
484
OH 44735-5276 Phone:
Claimant’s
Group Number: ______________ Enrollee’s Name:________________ ID#:_________________________ This information should be mailed to Aultra Administrative Group, PO Box 35276, Canton, OH 44735-5276, or faxed to the attention of the Subrogation Dept. (330) 363-5897.
_______________________________ __________________________
Signature Date
You have the right to appoint a representative, including an attorney to act on your behalf. This form is used to confirm permission to discuss with or disclose to a person’s protected health information (“PHI”) held by the affiliated entities AultCare Corporation, Aultra Administrative Group (AAG), and AultCare Insurance Company (AIC) which also does business as PrimeTime Health Plan and AultCare HMO to a particular individual who acts as the person’s personal representative. We are not always required to grant such access, but each request will be carefully reviewed and approved if warranted. Use of this information is strictly limited to that purpose.
Name:
Date of Birth:
ID Number: Group Number:
I hereby authorize the following person to act as my personal representative as indicated below. I understand that this authorization is voluntary and that I may revoke this authorization at any time except to the extent that action has been taken in reliance on this authorization.
Name of Representative:
Relationship:
Password personal representative must provide to access “PHI” about me:
Password:
I understand that I have the right to limit the information that is released under this authorization. For example, I may limit my personal representative’s access to information about a particular issue. Any such limitations must be described below in writing. I understand that by leaving this section blank, I am imposing no limitations on disclosure. However, if my authorization is for use/disclosure of substance abuse information, I understand that the recipient may be prohibited from disclosing substance abuse information under the Federal Substance Abuse Confidentiality Requirements. Note: State Law mandates that Authorizations are limited to 12 months. This form will expire upon 12 months from the date of signature unless an earlier date is noted here.
I understand that I may revoke this authorization at anytime by providing written notice of such revocation to the Health Plan.
I have had full opportunity to read and consider the content of this form. I understand that this authorization is consistent with my request. I understand that, by signing this form, I am confirming my authorization that the Health Plan may use and/or disclose my PHI to the person named as personal representative for the purpose as described above.
Your Signature: Date: Form must be signed by member. If form is signed by Power of Attorney or Legal Representative, a copy of documentation of position held must be attached to form.
Please return the completed form to: ATTN: Privacy Coordinator, PO Box 6029, Canton, OH 44706.
Designation of Authorized Representative Form
(S)ummary of (B)enefits and (C)overage GUIDELINES
Attachment #1: Employer Guide to SBC’s
Attachment #2: Sample SBC
Attachment #3: Glossary of Health Coverage and Medical Terms

EMPLOYER GUIDE
SUMMARY OF BENEFITS AND COVERAGE
GLOSSARY OF HEALTH COVERAGE AND MEDICAL TERMS

Summary of Benefits and Coverage
On Feb. 14, 2012, the Departments of Treasury, Internal Revenue Service, Labor, Health and Human Services, and Employee Benefits Security Administration released a final rule that implemented disclosure requirements under section 2715 of the Public Health Service Act.
This health insurance market reform under the Patient Protection and Affordable Care Act requires group health plans and health insurance issuers in the group market to provide a summary of benefits and coverage and uniform glossary to members of their health plans.
Final Regulations were again issued in June 2015. A revised SBC template and uniform glossary was finalized for Plan Year 2021.
Table of Contents
• What’s an SBC and a Uniform Glossary?
• What is Culturally and Linguistically Appropriate Manner?
• How do I meet the Electronic Disclosure requirements to distribute the SBC to my employees?
• What happens if I fail to comply?
• Who will provide me with the materials I need for distribution to my employees?
• When will I receive my SBC?
• Who should receive the SBC?
• When do I need to distribute the materials?
• FAQs

What’s an SBC and a Uniform Glossary?
The Summary of Benefits and Coverage or “SBC” and Glossary of Health Coverage and Medical Terms or “Uniform Glossary” are designed to help consumers better understand their health coverage and allow for easy comparison of other coverage options when shopping, applying, enrolling and re-enrolling into a health plan. The SBC is a resource for your employees that will summarize your health plan options including:
• Deductible
• Out-of-pocket and annual limits
• In- and out-of-network provider coverage
• Coverage of common medical events
• Excluded services
• Common covered services
• Rights to continue coverage
• Member grievance and appeal rights
• Coverage examples for having a baby and managing type 2 diabetes
The “Uniform Glossary” lists commonly used terms in insurance coverage. You can access the glossary by logging on to www.aultragroup.com.
1 of 8 Insurance Company 1: Plan Option 1 Coverage Period: 01/01/2013 – 12/31/2013 Summary of Benefits and Coverage: What this Plan Covers & What it Costs Coverage for: Individual + Spouse | Plan Type: PPO Questions: Call 1-800-[insert] or visit us at www.[insert] If you aren’t clear about any of the underlined terms used in this form, see the Glossary. You can view the Glossary at www.[insert] or call 1-800-[insert] to request a copy. This is only a summary If you want more detail about your coverage and costs, you can get the complete terms in the policy or plan document at www.[insert] or by calling 1-800-[insert] Important Questions Answers Why this Matters: What is the overall deductible? $500 person / $1,000 family Doesn’t apply to preventive care You must pay all the costs up to the deductible amount before this plan begins to pay for covered services you use. Check your policy or plan document to see when the deductible starts over (usually, but not always, January 1st). See the chart starting on page 2 for how much you pay for covered services after you meet the deductible Are there other deductibles for specific services? Yes $300 for prescription drug coverage. There are no other specific deductibles You must pay all of the costs for these services up to the specific deductible amount before this plan begins to pay for these services. Is there an out–of–pocket limit on my expenses? Yes. For participating providers $2,500 person / $5,000 family For non-participating providers $4,000 person / $8,000 family The out-of-pocket limit is the most you could pay during a coverage period (usually one year) for your share of the cost of covered services. This limit helps you plan for health care expenses. What is not included in the out–of–pocket limit? Premiums, balance-billed charges, and health care this plan doesn’t cover. Even though you pay these expenses, they don’t count toward the out-of-pocket limit Is there an overall annual limit on what the plan pays? No. The chart starting on page 2 describes any limits on what the plan will pay for specific covered services, such as office visits. Does this plan use a network of providers? Yes. See www.[insert].com or call 1-800-[insert] for a list of participating providers If you use an in-network doctor or other health care provider, this plan will pay some or all of the costs of covered services Be aware, your in-network doctor or hospital may use an out-of-network provider for some services. Plans use the term in-network, preferred, or participating for providers in their network See the chart starting on page 2 for how this plan pays different kinds of providers Do I need a referral to see a specialist? No. You don’t need a referral to see a specialist You can see the specialist you choose without permission from this plan Are there services this plan doesn’t cover? Yes. Some of the services this plan doesn’t cover are listed on page 4 See your policy or plan document for additional information about excluded services OMB Control Numbers 1545-2229 1210-0147, and 0938-1146 Corrected on May 11, 2012
What is Culturally and Linguistically Appropriate Manner?
This requirement provides employees and dependents the option to request their SBC in a non-English language if they reside in a county that meets or exceeds a 10 percent threshold of non-English speaking residents. The SBC that we provide will contain directions for non-English speaking individuals to receive further information in their non-English language.
How do I meet the Electronic Disclosure requirements to distribute the SBC to my employees?
Under the Department of Labor Electronic Disclosure requirement, if your employees are able to effectively access documents provided in electronic format at their worksite (i.e. e-mail) and this access is a part of their duties as an employee, you can send the SBC to them electronically. You can also allow the employees to elect to receive their SBC electronically.
Eligible employees (not currently enrolled) can receive the SBC electronically as long as a paper version option is available upon request. You can accomplish this by email, e-card, posting on your intranet or sending a postcard.
What happens if I fail to comply?
POTENTIAL FINES AND PENALTIES
• Up to $1,000 per day (adjusted for inflation) for each instance of willing non-compliance
• A fine of $100 per day per affected individual until compliant
Who will provide me with the materials I need for distribution to my employees?
As your health issuer or third-party administrator, we are committed to providing you with the tools that you need to meet this regulatory requirement.
• We will provide you with an SBC master copy for distribution (electronically or paper copy) for your employees, dependents and eligible employees for health insurance coverage. This will include an SBC for each benefit package you offer and a new SBC when coverage changes.
• Continuously monitor changes to regulation that may impact you.
When will I receive my SBC?
We will deliver your SBC to you at the following times:
• Upon my application for coverage or within 7 days
• Within 7 days upon my request
• If terms of my plan are not yet final, upon the first day of coverage
• Upon changes to my plan
• If automatically re-enrolled, a new SBC will be provided at that re-enrollment
Who should receive the SBC?
If you have an employee and all of the dependents reside at one address, only one SBC is required to be distributed.
However, if an employee has dependents who have an alternate address, you are required to distribute an SBC to those alternate addresses.
You are also required to distribute an SBC to all of your employees who are eligible for health insurance coverage, even if they are not currently enrolled in your health plan
When do I need to distribute the materials?
OPEN ENROLLMENT
You need to provide the SBC with open enrollment materials. If you do not hold an open enrollment period, provide the SBC no later than the first date your employees are eligible to enroll for coverage.
ONLINE ENROLLMENT
If you offer online enrollment, you are permitted to provide the SBC at the time of online enrollment or online renewal of coverage electronically but must provide the option to receive a paper copy.
AUTOMATIC RENEWAL
If you have an automatic renewal, the SBC must be provided 30 days prior to the first day of the new plan year. This SBC will reflect the plan that the employee and dependents are currently enrolled.
UPON REQUEST
If you have an employee or dependent who requests an SBC or Uniform Glossary, you must fulfill the request within seven business days. If the request is online, then you can deliver it electronically but you must provide the option to receive a paper copy.
SBC CHANGES
If the SBC changes from what was distributed at enrollment, you must provide an updated SBC prior to the first day of coverage.
SPECIAL ENROLLMENT
For Special Enrollment, you must provide an SBC within 90 days after they enrolled in your plan.
MIDYEAR BENEFIT CHANGES
If you make a midyear change to your plan that changes the content of your SBC, you must provide a 60-day advance notice to employees. This can be complete via a new SBC or a separate notice (summary of material modification).
Frequently Asked Questions
1. Does this regulation impact small and large groups?
Yes. Whether you are a small or large employer group, the SBC requirements apply to your health plan.
2. Does this apply to both fully insured and self-insured plans?
Yes, this impacts both fully insured and selfinsured plans.
3. Am I exempt because I am in a “grandfathered” plan?
No, the SBC requirement applies to both “grandfathered” and “non-grandfathered” plans.
4. Do I need an SBC for stand-alone dental or vision benefits?
No, the SBC regulations do not apply to standalone excepted benefits. Excepted benefits are generally benefits that require the individual to pay an additional premium.
5. Can I combine the SBC and Uniform Glossary with other documents?
Yes, as long as the SBC is displayed at the beginning.
6. Do COBRA enrollees receive SBCs?
Yes, COBRA enrollees have the same rights as other enrollees to receive SBCs.
7. Do I have to provide the SBC and Uniform Glossary in color?
No, you are permitted to provide in color or grayscale.
7589/22 2600 Sixth Street SW • Canton, Ohio 44710 • 330-363-2050 • 1-855-270-8497 • TTY: 711 • www.aultragroup.com


The Summary of Benefits and Coverage (SBC) document will help you choose a health plan. The SBC shows you how you and the plan would share the cost for covered health care services. NOTE: Information about the cost of this plan (called the premium) will be provided separately. This is only a summary. For more information about your coverage, or to get a copy of the complete terms of coverage, contact Aultra at 330-363-2050 or go to www.aultragroup.com. For general definitions of common terms, such as allowed amount, balance billing, coinsurance, copayment, deductible, provider, or other underlined terms, see the Glossary. You can view the Glossary at www.aultcas.com/aultragroup/login.aspx or call 330-3632050 or 1-855-270-8497 to request a copy.
Important Questions Answers
For network providers
What is the overall deductible?
Are there services covered before you meet your deductible?
Are there other deductibles for specific services?
$2,000 Individual / $4,000 Family
For out-of-network providers
$4,000 Individual / $8,000 Family
Yes. Network preventive care and services that apply a copayment are covered before you meet your deductible.
Why This Matters:
Generally, you must pay all of the costs from providers up to the calendar year deductible amount before this plan begins to pay. If you have other family members on the plan, each family member must meet their own individual deductible until the total amount of deductible expenses paid by all family members meets the overall family deductible.
This plan covers some items and services even if you haven’t yet met the deductible amount. But a copayment or coinsurance may apply. For example, this plan covers certain preventive services without cost sharing and before you meet your deductible. See a list of covered preventive services at https://www.healthcare.gov/coverage/preventive-care-benefits/.
What is the out-of-pocket limit for this plan?
No.
What is not included in the out-of-pocket limit?
For network providers
$2,000 Individual / $4,000 Family
For out-of-network providers
$8,000 Individual/ $16,000 Family
You don’t have to meet deductibles for specific services.
The out-of-pocket limit is the most you could pay in a calendar year for covered services. If you have other family members in this plan, they have to meet their own out-of-pocket limits until the overall family out-of-pocket limit has been met.
Copayments for medical services, copayments or coinsurance for prescription drugs, premiums, balance-billing charges, and health care this plan doesn’t cover.
Even though you pay these expenses, they don’t count toward the out-of-pocket limit.
(DT - OMB control number: 1545-0047/Expiration Date: 12/31/2019) Transitional Relief, Not HSA Comp, Embedded Deductible & OOP, No MOOP Page 1 of 7 (DOL - OMB control number: 1210-0147/Expiration date: 5/31/2022) (HHS - OMB control number: 0938-1146/Expiration date: 10/31/2022)
of Benefits and Coverage: What this Plan Covers & What You Pay for Covered Services Coverage Period: Beginning on or after 01/01/2022 : AULTERNATIVE 2000 100 B Coverage for: Individual/Family Plan Type: PPO
Summary
Important Questions Answers
Why This Matters:
Will you pay less if you use a network provider?
Do you need a referral to see a specialist?
Yes. See www.aultragroup.com or call 330-363-2050 or 1-855-270-8497 for a list of network providers.
No.
This plan uses a provider network. You will pay less if you use a provider in the plan’s network. You will pay the most if you use an out-of-network provider, and you might receive a bill from a provider for the difference between the provider’s charge and what your plan pays (balance billing). Be aware, your network provider might use an out-of-network provider for some services (such as lab work). Check with your provider before you get services.
You can see the specialist you choose without a referral.
[* For more information about limitations and exceptions, see the plan or policy document at www.aultragroup.com.] Page 2 of 7

All coinsurance costs shown in this chart are after your deductible has been met, if a deductible applies.
If you visit a health care provider’s office or clinic
If you have a test
visit
If you need drugs to treat your illness or condition
More information about prescription drug coverage is available at www.aultragroup.com
Preferred Generic drugs (Tier 1)
Preferred Brand / NonPreferred Generic drugs (Tier 2)
Non-Preferred Brand / NonPreferred Generic drugs (Tier 3)
Specialty Generic (Tier 4)
**Limited to a 30-day fill
Retail 1-34 day supply: $10 copayment or 20% coinsurance, whichever is greater;
Retail or Mail order 60-day supply: $27 copayment
Retail 1-34 day supply: $20 copayment or 30% coinsurance, whichever is greater;
Mail order 60-day supply: $55 copayment
Retail 1-34 day supply: $45 copayment or 50% coinsurance, whichever is greater;
Mail order 60-day supply: $110 copayment
Retail or Mail order: $125 copayment or 20% coinsurance, whichever is greater
Deductible does not apply to office visits with a Network Provider, or for visits to an Out-of-Network Provider for an injury.
You may have to pay for services that aren’t preventive. Ask your provider if the services needed are preventive. Then check what your plan will pay for.
Specialty Brand (Tier 5)
***Limited to a 30-day fill
Retail or Mail order: $125 copayment or 20% coinsurance, whichever is greater
[* For more information about limitations and exceptions, see the plan or policy document at www.aultragroup.com.]
Deductible does not apply. You may obtain up to a 60-day supply of Tier 1 drugs at the retail pharmacy. A 34-day supply is available at retail pharmacy for Tier 2 and Tier 3 drugs, and You may obtain up to a 60day supply through Mail Order. Tier 4 and Tier 5 Specialty/Limited Distribution Medications are limited to a 30-day supply.
Specialty Medications must be obtained from Aultra’s Preferred Specialty pharmacies. Certain preventive medications may be covered at 100%, with no cost to You. Also, certain classes of medications require a Prior Authorization or Step Therapy. For a complete list of these medications please visit the Aultra website at www.aultragroup.com.
Page 3 of 7
Limitations,
Important Information Network Provider (You will pay the least) Out-of-Network Provider (You will pay the most)
Common Medical Event Services You May Need What You Will Pay
Exceptions, & Other
Primary care
$25 copayment/visit Illness: 20%
Injury:
visit to treat an injury or illness
coinsurance;
$25 copayment
Specialist
Preventive care/screening/ immunization No cost share 50% coinsurance
Diagnostic test (x-ray, blood
0% coinsurance 20% coinsurance None Imaging (CT/PET scans, MRIs) 0% coinsurance 20% coinsurance None
work)
If you have outpatient surgery
you need immediate medical attention
If you have a hospital stay
If you need mental health, behavioral health, or substance abuse services Outpatient services
Benefits paid based on the corresponding medical benefit.
Benefits paid based on the corresponding medical benefit. Services for Mental Health, Behavioral Health, or Substance Abuse are payable on the same basis as any other illness.
If you are pregnant Office visits
Benefits paid based on the corresponding medical benefit.
Benefits paid based on the corresponding medical benefit.
[* For more information about limitations and exceptions, see the plan or policy document at www.aultragroup.com.]
Cost sharing does not apply to certain preventive services. Depending on the type of service, a copayment, deductible or coinsurance may apply.
Page 4 of 7 Common Medical Event Services You May Need What You Will Pay Limitations, Exceptions, & Other Important Information Network Provider (You will pay the least) Out-of-Network Provider (You will pay the most)
Facility fee (e.g., ambulatory surgery center) 0% coinsurance 20% coinsurance None Physician/surgeon fees 0% coinsurance 20% coinsurance None If
Emergency room care $50 copayment/visit $50 copayment/visit Deductible does not apply to this service. Emergency medical transportation 0% coinsurance 0% coinsurance Network deductible will apply. Urgent care $25 copayment/visit $25 copayment/visit Deductible does not apply to this service.
Facility fee (e.g., hospital room) 0% coinsurance 20% coinsurance Preauthorization is required. Physician/surgeon fees 0% coinsurance 20% coinsurance None
Inpatient services 0% coinsurance 20% coinsurance Preauthorization
is required.
Childbirth/delivery professional services 0% coinsurance 20% coinsurance None Childbirth/delivery facility services 0% coinsurance 20% coinsurance Preauthorization is
required.
If you need help recovering or have other special health needs
Children’s eye exam
If your child needs dental or eye care
Coverage is provided for vision screening for all children at least once between the ages of 3 and 5 years, to detect the presence of amblyopia or its risk factors.
Children’s glasses
Children’s dental check-up
Abortion (except in cases of rape, incest, or when the life of the mother is endangered)
Acupuncture
Bariatric Surgery
Cosmetic Surgery
Dental Care
Habilitation Services
Hearing Aids
Long Term Care
[* For more information about limitations and exceptions, see the plan or policy document at www.aultragroup.com.]
Non-Emergency care when traveling outside the U.S.
Routine Eye Care
Routine Foot Care
Weight Loss Programs
7 Common Medical Event Services You May Need What You Will Pay Limitations, Exceptions, & Other Important Information Network Provider (You will pay the least) Out-of-Network Provider (You will pay the most)
Page 5 of
Home health care 0% coinsurance 20% coinsurance Preauthorization is required.
limited to 60 visits
calendar
Rehabilitation services 0% coinsurance 20% coinsurance Must be injury/illness
therapy is limited to 35 treatments per calendar year. Habilitation services Not covered Not covered Skilled nursing care 0% coinsurance 20% coinsurance Preauthorization is required. Coverage is limited to 50 days per illness. Durable medical equipment 0% coinsurance 20% coinsurance Preauthorization is required for a single item with a purchase price over $2,500. Hospice services 0% coinsurance 20% coinsurance Preauthorization is required.
Coverage is
per
year.
related. Manipulation
No
50%
cost share
coinsurance
Not
Not
covered
covered
Not
Not
covered
covered Excluded Services & Other Covered Services:
Services Your Plan Generally Does NOT Cover (Check your policy or plan document for more information and a list of any other excluded services.)
Other Covered Services (Limitations may apply to these services. This isn’t a complete list. Please see your plan document.)
Chiropractic Care
Infertility Treatment
Private Duty Nursing
Your Rights to Continue Coverage: There are agencies that can help if you want to continue your coverage after it ends. The contact information for those agencies is: for group health coverage subject to ERISA, contact Department of Labor’s Employee Benefits Security Administration at 1-866-444-EBSA(3272) or www.dol.gov/ebsa/healthreform; for non-federal governmental group health plans, contact Department of Health and Human Services, Center for Consumer Information and Insurance Oversight, at 1-877-267-2323 x61565 or www.cciio.cms.gov. Church plans are not covered by the Federal COBRA continuation coverage rules. If the coverage is insured, individuals should contact their State insurance regulator regarding their possible rights to continuation coverage under State law. Other coverage options may be available to you too, including buying individual insurance coverage through the Health Insurance Marketplace. For more information about the Marketplace, visit www.HealthCare.gov or call 1-800-318-2596.
Your Grievance and Appeals Rights: There are agencies that can help if you have a complaint against your plan for a denial of a claim. This complaint is called a grievance or appeal. For more information about your rights, look at the explanation of benefits you will receive for that medical claim. Your plan documents also provide complete information to submit a claim, appeal, or a grievance for any reason to your plan. For more information about your rights, this notice, or assistance, contact: for group health coverage subject to ERISA, contact Department of Labor’s Employee Benefits Security Administration at 1-866-444-EBSA(3272) or www.dol.gov/ebsa/healthreform or call the Ohio Department of Insurance 1-800-686-1526; for non-federal governmental group health plans and church plans that are group health plans, contact Aultra at 1-855-270-8497 or call the Ohio Department of Insurance 1-800-686-1526.
Does this plan provide Minimum Essential Coverage? Yes
Minimum Essential Coverage generally includes plans, health insurance available through the Marketplace or other individual market policies, Medicare, Medicaid, CHIP, TRICARE, and certain other coverage. If you are eligible for certain types of Minimum Essential Coverage, you may not be eligible for the premium tax credit.
Does this plan meet the Minimum Value Standards? Yes
If your plan doesn’t meet the Minimum Value Standards, you may be eligible for a premium tax credit to help you pay for a plan through the Marketplace.
Language Access Services:
[Spanish (Español): Para obtener asistencia en Español, llame al 330-363-6360 / 1-800-344-8858.]
[Tagalog (Tagalog): Kung kailangan ninyo ang tulong sa Tagalog tumawag sa 330-363-6360 / 1-800-344-8858.]
[Chinese (中文): 如果需要中文的帮助, 请拨打这个号码 330-363-6360 / 1-800-344-8858.]
[Navajo (Dine): Dinek'ehgo shika at'ohwol ninisingo, kwiijigo holne' 330-363-6360 / 1-800-344-8858.]
To see examples of how this plan might cover costs for a sample medical situation, see the next section.
PRA Disclosure Statement: According to the Paperwork Reduction Act of 1995, no persons are required to respond to a collection of information unless it displays a valid OMB control number. The valid OMB control number for this information collection is 0938-1146 The time required to complete this information collection is estimated to average 0.08 hours per response, including the time to review instructions, search existing data resources, gather the data needed, and complete and review the information collection. If you have comments concerning the accuracy of the time estimate(s) or suggestions for improving this form, please write to: CMS, 7500 Security Boulevard, Attn: PRA Reports Clearance Officer, Mail Stop C4-26-05, Baltimore, Maryland 212441850.
[* For more information about limitations and exceptions, see the plan or policy document at www.aultragroup.com.]
Page 6 of 7
About these Coverage Examples:

This is not a cost estimator. Treatments shown are just examples of how this plan might cover medical care. Your actual costs will be different depending on the actual care you receive, the prices your providers charge, and many other factors. Focus on the cost-sharing amounts (deductibles, copayments and coinsurance) and excluded services under the plan. Use this information to compare the portion of costs you might pay under different health plans. Please note these coverage examples are based on self-only coverage.
Peg is Having a Baby (9 months of in-network pre-natal care and a hospital delivery)
Managing Joe’s Type 2 Diabetes (a year of routine in-network care of a wellcontrolled condition)
Mia’s Simple Fracture (in-network emergency room visit and follow up care)
This EXAMPLE event includes services like:
Specialist office visits (prenatal care)
Childbirth/Delivery Professional Services
Childbirth/Delivery Facility Services
Diagnostic tests (ultrasounds and blood work)
Specialist visit (anesthesia)
In this example, Peg would pay:
This EXAMPLE event includes services like:
Primary care physician office visits (including disease education)
Diagnostic tests (blood work)
Prescription drugs
Durable medical equipment (glucose meter) Total Example Cost
In this example, Joe would pay:
This EXAMPLE event includes services like:
Emergency room care (including medical supplies)
Diagnostic test (x-ray)
Durable medical equipment (crutches)
Rehabilitation services (physical therapy)
The plan would be responsible for the other costs of these EXAMPLE covered services.
Page 7 of 7
$2,000
The plan’s overall deductible
$25
Specialist copayment
Hospital
0%
Other
0%
(facility) coinsurance
coinsurance
$12,700
Total Example Cost
Cost Sharing Deductibles $2,000 Copayments $10 Coinsurance $0 What isn’t covered Limits or exclusions $60
total Peg would pay is $2,070
The
$2,000
The plan’s overall deductible
$25
Specialist copayment
coinsurance 0% Other coinsurance 0%
Hospital (facility)
$5,600
Cost Sharing Deductibles $1,140 Copayments $540 Coinsurance $0 What isn’t covered Limits or exclusions $20 The total Joe would pay is $1,700 The plan’s overall deductible $2,000 Specialist copayment $25
Hospital (facility) coinsurance 0%
Other coinsurance 0%
Total Example Cost $2,800 In this example, Mia would pay: Cost Sharing Deductibles $1,840 Copayments $110 Coinsurance $0 What isn’t covered Limits or exclusions $0
total Mia would pay is $1,950
The



MISCELLANEOUS
Attachment #1: Urgent Care and After-Hours Clinic Information
Attachment #2: AultLine
Attachment #3: Prescription Information Website
Attachment #4: A Guide to Our Services
BE PREPARED
Get the right care. Whether that’s finding the right doctor, specialist, therapist or something else altogether. Just use the Find a Provider button at www.aultragroup.com or contact Aultra at 330-363-2050 (toll-free: 1-855-270-8497, TTY: 711).
Find care near you whenever you need it. You get in-network coverage at hospitals, ambulatory care facilities and providers. With location options in more places, Aultra gives you more.
• And more! Who usually provides
• Symptoms feel life-threatening or disabling
• Chest pain or severe shortness of breath
• Major injury or broken bones
• Sudden or unexplained loss of consciousness
• Allergic reactions (minor)
• Bumps, cuts, scrapes, rashes
• Burning with urination
• Burns (minor)
• Cold, cough and sore throat
• Sinus pain and fever (minor)
• Eye or ear pain or irritation
• Shots
Same as retail health clinic plus ...
• Asthma (mild)
• Back pain
• Nausea or diarrhea
• Headache (minor)
Same as walk-in doctor’s office plus ...
• Animal bites
• Sprains and strains
• Stitches
• X-rays
• Cold & flu symptoms
• Allergies
• Sinus problems
• Respiratory infection
• Skin problems
Do you have health related questions or concerns? By calling 330-363-7621 or 1-877-336-9113, an operator will take your information and an experienced registered nurse will return your call.
Money-saving tip
Visit hospitals and doctors that are in your plan. If you don’t, you’ll often pay much more out-of-pocket for your care.
* Not all plans include the Teladoc® service. Please contact your AultCare representative to see if Teladoc® is included in your healthcare plan.
Emergency Room Retail Health Clinic Walk-in Doctor’s Office Urgent Care Center
Teladoc ® Doctors
in emergency medicine Physician assistants or nurse practitioners Family practice doctors Doctors
be
at right away Board-certified doctors For non-emergencies: 4 hours $1,145 30 minutes $92 30 minutes $102 30 minutes $133
minutes $55
*
trained
who treat conditions that should
looked
10
Average
When to
care
wait time and cost
go
6355/20 $ 12 11 10 9 8 7 6 5 4 3 2 1
SAVE TIME ANDMONEY
AULTLINE 24/7
Aultra provides telephonic health services 24 hours a day, 7 days a week. If you have health-related questions or concerns, contact AultLine at 330-363-7621 or 1-877-336-9113 to speak with a trained medical professional CONTACT US
YOUR TRUSTED SOURCE OF INFORMATION AND SUPPORT
AultLine is a trusted source of information and support for a wide range of health concerns and topics. You can find answers to questions regarding family health, medication, illness, injury first aid, and much more. Calls are confidential and free of charge.
If you have an emergency, call 911 or go to the emergency room.
AultLine is unable to assist with questions regarding benefits or claims. If you have questions, please contact Aultra during normal business hours for assistance.
HEALTH–RELATED QUESTIONS OR CONCERNS?
Do you have health–related questions or concerns? When you contact AultLine, an operator will take your information, and an experienced, registered nurse will return your call.
Contact AultLine if you have questions or concerns regarding:
» First aid instructions
» General health information
» Determination of what level of care is most appropriate for your condition
» Answers for your medication questions
» Suggestions for self-care



330-363-2050 | 1-855-270-8497 www.aultragroup.com
you youmatter
OPTUMRX® ONLINE RESOURCES
The OptumRx website and mobile app provide tools and information to help you take care of yourself and your pharmacy benefits. It’s easy to track an order, search for a lower-cost medication, sign up for home delivery, and more.
MANAGE YOUR PRESCRIPTION NEEDS ON YOUR MEMBER ACCOUNT
To access your OptumRx account:
1. Visit the Aultra website (www.aultragroup.com).
2. Log in to your Aultra online member account.
3. Once you are logged into your member account, click the My Resources tab.
4. Select OptumRx to be directed to your OptumRx account.
MANAGE YOUR PRESCRIPTION NEEDS ON THE AULTCARE APP
To access your account using your mobile device:
1. If you have not done so, download the AultCare app from the Apple App Store® or Google Play™.
2. Sign into the AultCare app using the same username and password as your online Aultra member account.
3. At the bottom of your screen, select More.
4. Click My Resources and a drop down menu will appear.
5. Select OptumRx to be directed to your OptumRx account.
CONTACT US 330-363-2050 | 1-855-270-8497 www.aultragroup.com
you youmatter
Save time and manage your health using these optumrx.com tools:
Place an order – Skip the pharmacy line and order medications you take regularly — you’ll get a 90-day supply delivered to your home and may pay less
Skip the pharmacy line and order medications you take regularly — you’ll get a 90-day supply delivered to your home and may pay less
Price a drug – Compare costs from different pharmacies or find lower-cost alternatives for possible savings
Price a drug – Compare costs from different pharmacies or find lower-cost alternatives for possible savings
Order status – Track your home delivery medication status
Order status – Track your home delivery medication status
Pharmacy locator – Find the closest network pharmacy
Pharmacy locator – Find the closest network pharmacy
Notifications and reminders – Set up text message pharmacy notifications and/or reminders to take your medication or refill a prescription
Notifications and reminders – Set up text message pharmacy notifications and/or reminders to take your medication or refill a prescription
Benefit View real-time benefit information and your plan’s
Benefit lookup – View real-time benefit information and your plan’s prescription drug list
My prescriptions – Manage home delivery medication renewals, delivery status and more
My prescriptions – Manage home delivery medication renewals, delivery status and more
Savings Advisor – See opportunities to save on your prescriptions
Savings Advisor – See opportunities to save on your prescriptions
And with the app, you can do all of the above, plus refill a prescription by scanning your medication’s barcode or sending a photo of the pill bottle.
And with the app, you can do all of the above, plus refill a prescription by scanning your medication’s barcode or sending a photo of the pill bottle.
All Optum trademarks and logos are owned by Optum, Inc. All other trademarks are the property of their respective owners.
If you, or someone you are helping, have questions about AultCare/Aultra you have the right to get help and information in your language at no cost. To speak with an interpreter, call Local: 330-363-6360 Outside Stark County: 1-800-344-8858 TTY Local: 711 Outside Stark County: 711.
Si usted, o alguien a quien usted está ayudando, tiene preguntas acerca AultCare/Aultra tiene derecho a obtener ayuda e información en su idioma sin costo alguno. Para hablar con un intérprete, llame al Local: 330-363-6360 Fuera del condado de Stark: 1-800-344-8858 TTY Local: 711 Fuera del condado de Stark: 711.
如果您,或是您正在協助的對象,有關於AultCare/Aultra保险公司 方面的問題,您有權利免費以您的母語得到幫助和訊息。洽詢一位翻譯 員,請撥電話 本地:330-363-6360 斯塔克縣外:
1-800-344-8858 TTY線本地:711 斯塔克縣外:711.
AultCare/Aultra complies with applicable Federal civil rights laws and does not discriminate on the basis of race, color, national origin, age, disability, or sex.
7124/21
7017/20
PROGRAMS AND SERVICES
Through our partnerships, coordination, products, network and customer service, Aultra offers members a wide variety of programs and services. These programs and services provide a diverse spectrum of value to members towards their health and wellness.
Care Coordination
Aultra’s Care Coordination program encompasses all of the clinical areas of Aultra including:
» Utilization Management
» Primary Care Connection
» Case Management
» Disease Management
» Pharmacy
» Wellness
As an Aultra member, you may receive the following services:
» Assistance with chronic illnesses
» Help with transitioning care
» Access to healthcare professionals
» Educational mailings
24-Hour Nurse Hotline
» Tele-monitoring programs for heart failure and diabetes
» Assistance with navigating the healthcare system
When it comes to your health, Aultra members can talk with an experienced, registered nurse and get advice or answers to their health-related questions day or night.
Please call 330-363-7620 or 1-866-422-9603 for additional assistance.
Online Health Library
If you are preparing for surgery, living with a chronic condition or want to take a more active role in your health, our online health library can empower you to take care of your health. The online health library can help you prepare for surgery and manage your health conditions.
The online health library delivers reliable information, created in collaboration with only board-certified physicians, making it easy to understand.
To view the online health library, visit www.aultragroup.com/health--care-coordination.
7860/23
Medical Cost Estimator
In an effort to empower members to take control of their healthcare dollars, members have access to a Medical Cost Estimator. This program was designed to provide an estimate as to what members can expect to pay for a wide variety of in-network services and procedures, while taking into consideration their deductible/out-of-pocket expenses.
Advantages of the Medical Cost Estimator
» Compares costs of most common procedures between physicians, hospitals and facility charges
» Provides members with a greater transparency
» By utilizing this tool, members have the opportunity to save money
Online Resources


Throughout Aultra website, you are able to manage your account information including: reviewing your claims and Summary of Benefits, ordering ID cards and accessing a wide variety of forms. Aultra’s website is also a great resource for many other health-related topics.
Health & Wellness
» Provider directory
» Health programs and services
» Health information and tips
AultCare Blue Button
» Organize and store medical information
» Download text file
» Share data with members of your care team
AultmanNow
Prescription Information
» Prescription history
» Money saving drug alternatives
» Detailed drug information
» National pharmacy search
Quick Forms
» Member card replacement
» Medical information
» Dental claim form
» Vision claim form
» Other coverage information
Online Resources
» Account statements
» Benefits
» Claims
Aultra partners with AultmanNow, a convenient telehealth service for medical consultation, diagnosis and prescriptions (when appropriate). Members of AultmanNow have 24/7/365 on-demand access to affordable medical care via phone and online video consultation.
Features of AultmanNow
» Access to a U.S. board-certified provider
» Assessment of non-urgent and non-acute conditions
» Beneficial to use on weekends and vacations
» Addition of convenience and value to healthcare
TELEHEAL TH
CONTACT US 330-363-2050 | 1-855-270-8497 | TTY 711 www.aultragroup.com you youmatter You have the right to
and
your
no
To speak with an interpreter, call 330-363-6360 (TTY 711). ATENCIÓN: si
a su
de asistencia lingüística. Llame al 330-363-6360 (TTY: 711). 注意: 如果您使用繁體中文,您可以免費獲得語言援助服務。請致電330-363-6360(TTY:711)。
the basis of race, color, national origin,
assistance
information in
language at
cost.
habla español, tiene
disposición servicios gratuitos
AultCare/Aultra complies with applicable federal civil rights laws and does not discriminate on
age, disability, or sex.
YOUR ONLINE ACCOUNT
Aultra’s online portal features an updated look and easy to access resources to enhance your experience and provide the tools you need to take an active role in your healthcare.
Follow these steps to login to your account:
Select Account Login on the homepage of www.aultragroup.com.
If you are an existing Aultra member, you will need to register for a new account regardless if you had an account on our old platform. You can use the same username when you register, but you may need to update your password.
All new Aultra members will need to register for an online account.




Through this feature, member ID cards can be downloaded, printed, or sent via postal mail.
Review an estimate of expenses for in-network services and procedures.
Use our online directory to find an A compilation of other resources are available on the platform but vary dependent on your plan.
Other Coverage Information
Explanation of Benefits FAQ
*If applicable
1 2 3
7024/20 CONTACT US 330-363-2050 | 1-855-270-8497 www.aultragroup.com youmatter

A guide to our services.
202 3 7861/23
Things to have ready when you call us:
> Your AultCare ID Card, which has your group information and member ID number
> Your Explanation Of Benefits (EOB) form if you are calling about a claim (You can access your EOBs by going to www.aultcare.com and logging into your account.)
AultCare Service Center Contact Information
> 330-363-6360 (local)
> 1-800-344-8858 (toll-free)
> TTY users should call: 711
> Monday - Friday 7:30 am - 5:00 pm EST
Special Communication Needs
AultCare offers numerous services to meet the cultural and linguistic needs of our members. These services include access to translators of various foreign languages and a TTY line for the hearing impaired.
24-Hour Nurse Hotline Contact Information
> 330-363-7620
> 1-866-422-9603 (toll-free)
www.aultcare.com AultCare Mailing Address: AultCare P.O. Box 6910 Canton, OH 44706
Health
AultCare
Plans
Helpful Tips

2 About AultCare 4 Your Physician is Your Partner in Health & Wellness 6 Care Coordination - Disease Management Program - Case Management Program - Primary Care Connection - Utilization Management Program - Pharmacy Program What’s Not Covered Filing a Claim Grievance & Appeals Enrollee Rights & Responsibilities Privacy Practices Frequently Asked Questions Glossary 11 13 15 17 19 21 23
About AultCare.
For 35 years, AultCare has provided quality healthcare plans at an affordable cost to the community it serves. Through the use of innovative plan designs, superior customer service, and a high-quality network, AultCare strives to satisfy enrollees and clients and remain committed to providing affordable healthcare plan options.
Not only do we help control healthcare costs, we are a health and wellness company full of valuable resources to prevent health concerns arising in the first place. Sometimes health issues are inevitable. We have programs and staff in place to help manage those issues, too.
Healthcare is complex and confusing, but it doesn’t need to be. Through use of our personalized customer service, our members can rely on AultCare for guidance navigating the healthcare system. AultCare is proud to support its members and serve as a trusted resource in the community.

Where You Matter
We believe your healthcare plan should be focused on your needs, in ways that matter to you. From the network you choose to how you receive communication from us, our plans and services are designed with you in mind so that you can take an active role in your health. When you are covered by AultCare, you are part of our local family!
When you call us, we pick up the phone. You won’t get stuck in an automated answering system. When you have questions, we are here to help you. We make it easy for you to get information day or night. Meet with us in-person, call us to speak with a knowledgeable customer service representative, or visit our website at www.aultcare.com anytime you need answers.
Advocate
We help our members live healthier lives by giving them the tools and support that will help them take control of their health. If you are diagnosed with a health condition, our experienced Care Coordination team can identify your healthcare needs and provide you with programs and services you need.
24-Hour Free Nurse Line
We offer our members a way to get credible health information and support 24 hours a day, 7 days a week. AultCare members can talk with an experienced registered nurse and get answers to their health-related questions and concerns by calling 330-363-7620 or toll-free 1-866-422-9603. Calls are confidential.
2

Accurate
Accuracy is at the heart of what we do. Our processes are tested and streamlined, so you can trust that what you receive from us is dependable and accurate. We value your trust and are committed to giving you consistent, excellent service.
Recognition
The National Committee for Quality Assurance (NCQA) has awarded our Commercial PPO, Commercial HMO, Medicare HMO, and Marketplace PPO products with NCQA Health Plan Accreditation.
Answers
Prefer to use the internet? The AultCare website, www.aultcare.com, is your health and wellness hub and where you can manage your account.
On the website, you can:
• Create an online account to manage your personal claim information, view your EOBs, download forms, and more
• Look for providers
• Find current health-related information
• Tell us what matters to you by taking satisfaction surveys





3 A Guide to Our Services
Your Physician is Your Partner in Health & Wellness
You should visit your primary care physician for regular checkups to maintain your best level of health and wellness.
Choosing a Doctor
When you join AultCare, you can see any doctor in the network. If you need specialty care, your Primary Care Physician (PCP) can identify network doctors who treat your condition. You can also go to our website to search for a doctor in our network.
Begin your search by visiting www.aultcare.com. You can identify and select network physicians according to the characteristics important to you, including:
• Office location
• Language spoken
• Gender
• Specialty
• Hospital affiliations
• Acceptance of new patients
• Board certifications
Customer service representatives are also available to help. They can help find a doctor who can meet your special or cultural needs.

Your physician may have more than one office. Alternate offices and locations of your physician may be considered outside the network. Please refer to the online Provider Directory at www.aultcare.com or contact the AultCare Service Center at 330-363-6360 or 1-800-344-8858 to confirm if an office is in-network.
Refer to your plan documents for your physical and wellness benefits and for specific information about access to providers.
If you need mental health and/or substance abuse services and do not have a mental health provider, please contact your primary physician. If your need is an emergency, go to the nearest emergency facility for evaluation. There are behavioral health providers available to you within your network.
4

In Case of Emergency
If you have a medical problem that must be treated right away and it is outside your physician’s normal office hours, call his/her office and the physician on call will assist you.
If you have an emergency, call 911 or go to the nearest emergency care facility. You do not have to contact AultCare to obtain emergency services.
If you are out-of-town and need emergency care, please go to the nearest emergency care facility. If you become ill and you are out-of-town, and it is not an urgent or emergency situation, try to call your physician first. If that is not possible, seek treatment at the nearest medical care facility or physician’s office. Notify the AultCare Service Center the next business day if you are admitted to an out-of-town hospital. Schedule an appointment with your physician for all follow-up care and services.
Some examples of emergency situations are:
• High fever
• Convulsions
• Difficulty breathing
• Uncontrolled vomiting and/or diarrhea
• Broken bones
• Possible miscarriage or pregnancy with vaginal bleeding
• Poisoning
• Severe bleeding
• Severe burns
• Severe pain in the stomach or chest
• Shock
• Unconsciousness
Remember, if you need emergency services:
1. Go to the nearest emergency care facility. Be sure to present your AultCare ID card.
2. If you are admitted to the hospital, please make sure AultCare is notified on the next business day.
3. Remember to contact your PCP as soon as possible after your visit.
4. Schedule an appointment with your PCP for all follow-up care and services.
A Guide to Our Services
5
Care Coordination
AultCare offers many health and wellness services to its members. These services are streamlined into a program known as Care Coordination. With Care Coordination, AultCare members have access to a team of local physicians, nurses, dietitians, pharmacists, and other clinical and non-clinical staff to help resolve any potential and ongoing health and wellness issues. This system allows AultCare to provide its members with a comprehensive approach to healthcare. Members may be affected by one or more programs provided by Care Coordination. The programs work collectively to cover all aspects of a member’s health and wellness.
Disease Management Program
Provides members with education on prevention, ensuring members with chronic health issues have all the tools and services necessary to improve their health.
The Disease Management program offers an integrated and comprehensive approach to manage conditions, reduce complications, improve quality of life, and decrease costs. Disease Management nurses reach out to members with diagnoses such as Diabetes, Congestive Heart Failure (CHF), and Chronic Obstructive Pulmonary Disease (COPD) through telemonitoring programs. Outreach is also provided to members with mental health concerns through the Disease Management program.
Members will receive targeted materials to introduce available opportunities and AultCare Care Coordination resources. Nurses will also contact members for preventive care reminders and available educational programs. Common reminders AultCare nurses provide are preventive screenings, adherence follow-up, medication follow-up, and information on how to improve overall outcomes.
24-Hour Nurse Hotline
AultCare offers a health and information line to assist members with health-related questions day or night. By calling 330-363-7620, or toll-free 1-866-422-9603, you will be directed to an experienced registered nurse who is available 24 hours a day to answer your health-related questions and provide confidential information. They will be able to:
• Provide first aid instructions and general health information
• Determine what level of care is most appropriate for your condition
• Answer your medication questions
• Offer suggestions for self-care

6

Case Management Program
Promotes quality, cost-effective outcomes through assessment, planning, coordination, education, and referral
The Case Management program is made up of nurses and social workers who help members receive the care, information and community services they need. The program promotes quality, cost-effective outcomes through assessment, planning, coordination, education, and referral. AultCare case managers may contact members if they have recently had a long hospital stay, have a new cancer diagnosis, have a complex medical issue, or require specialized care from an out-of-network provider.
Primary Care Connection (PCC)
Serves as the link between the member, the primary care physician, and the health plan to help the member navigate the healthcare system and receive integrated care
AultCare’s Primary Care Connection focuses on providing patient-centered, accessible, comprehensive, and coordinated care. PCC nurses connect with members over the phone or face-to-face for as long as needed. Education is offered to those dealing with chronic and acute conditions along with additional information and resources to ensure members’ needs are met. The PCC team of nurses is the link between members, providers, and the health plan.
Utilization Management (UM)
Helps control healthcare costs through management of the use of healthcare resources
Pre-Certification
Pre-Certification, also known as pre-authorization or pre-approval, is the process of notifying your health plan prior to an elective hospital stay or elective surgery procedure. This process helps to determine that all medical care possibilities have been explored and are within acceptable time limits. The pre-certification process has two parts:
1. Notification - AultCare receives a request for services from your provider
2. Determination of coverage/verification of eligibility - we review your plan document and clinical information as it relates to the request for services
Getting pre-certification for a procedure does not mean the service will be covered and paid at the highest level of benefit, or at all.
All claims are subject to review upon receipt of the actual claim or documentation and are subject to updates in eligibility upon receipt of the actual claim.
Refer to your plan documents, access our website at www.aultcare.com or contact the AultCare Service Center to determine if your particular plan has additional pre-certification requirements or to obtain a list of items requiring pre-certification.
Reference Based Pricing vs. Usual Customary Reasonable Allowances
All benefits are subject to Reference Based Pricing (RBP) or Usual Customary and Reasonable Allowances (UCR). Amounts exceeding RBP or UCR for services rendered by a network provider are not patient responsibility. Amounts exceeding the RBP or UCR for services rendered by a non-network provider or for services rendered under a traditional plan in the absence of a provider network, are the financial responsibility of the patient. If you have questions regarding this information, please contact the AultCare Service Center. Please refer to your Certificate or Plan Document and Summary Plan Description for details on your coverage.
7

Utilization Management Evaluation of New and Existing Technology
AultCare investigates all requests for coverage of new technology using a medical technology assessment company as a guideline. If additional information is needed, AultCare utilizes sources including, but not limited to Medicare and Medicaid policies and Food and Drug Administration releases of any current medical peer review literature. This information is reviewed and evaluated by AultCare’s medical director and other physician advisors in order to determine if a new technology is appropriate for coverage under your AultCare plan. Members may request that a certain new technology be investigated for coverage by contacting the UM department.
How to Submit a Request for Pre-Certification
Requests should be submitted by phone, fax or in writing to:
AultCare Care Coordination
P.O. Box 6910
Canton, Ohio 44706
Phone: 330-363-6360 or 1-800-344-8858
Fax: 330-454-9635

Denials are documented in the form of a letter to you and the requesting provider. The letter includes:
• The specific reason for denial
• Reference to the benefit provision, guideline, protocol or other similar criteria on which the denial decision is based
• Decision of additional information needed to analyze the request
• Notification that you can obtain a copy of the actual benefit provision, guideline, protocol or criteria on which the denial was based (this is upon request and at no extra cost)
• Description of your appeal rights and appeal process, including your right to have an authorized representative act on your behalf
• A description of the expedited appeal process if the denial is urgent pre-service or urgent concurrent review
If the denial is based on medical necessity, a reviewer is available to discuss the decision with the physician or provider.*
AultCare provides you with access to staff to discuss the UM process and any issue relating to the UM process. Professional staff members are available from 8 a.m. to 5 p.m. Monday - Friday by contacting the AultCare Service Center at 330-363-6360 or toll free at 1-800-344-8858.
TTY users should call: 711. If you call after business hours, please leave a message and we will respond to your call the next business day.
*Emergency care does not require pre-certification.
8

Pharmacy Program
This information only applies if AultCare is your pharmacy benefit administrator
AultCare’s pharmacy program provides you with a variety of safe, effective and affordable prescription choices to meet your medication needs. Find out what medications are covered under your plan by accessing your plan’s formulary at www.aultcare.com or by contacting AultCare Customer Service. The formulary is a list of medications your plan covers based on evaluations of efficacy, safety, and cost-effectiveness.
If your pharmacy benefits are covered under a co-pay structure, you will save money by asking your doctor if your prescription can be filled with a generic equivalent or by choosing drugs in the lowest-cost tiers of your plan design. Talk to your doctor about which prescriptions will work best for you. Generic medications, with the lowest co-payments, are affordable alternatives that have met multiple quality and safety standards set by the FDA.
For certain prescription drugs, AultCare has additional requirements for coverage.
These requirements ensure the drug prescribed is clinically appropriate for the plan member and also helps us manage drug plan costs. A team of physicians and pharmacists developed these requirements for our plan to help us provide quality coverage to our members. For a current listing of medications that require prior authorization, please visit the website at www.aultcare.com or call customer service at 330-363-6360 or 1-800-344-8858.

9

Mail Order
Some AultCare plans include the option to have your prescriptions filled by mail-order.
A mail-order option offers you an alternative to the retail pharmacy for long-term medications. With mail-order service, you have the convenience of home delivery and the ability to refill orders online, by phone, fax, or mail.
To have your prescription filled by mail-order, simply ask your physician for a new prescription. Check your plan documents to see how many days supply your plan will cover.
Mail your prescription to your mail-order vendor/ pharmacy, or have your physician fax it. Please refer to your individual schedule of benefits to determine your actual copayment. Most plans allow up to a 60 or 90-day supply by mail-order. To obtain information regarding the mail-order services, please call AultCare at 330-363-6360 or visit the Pharmacy Services page on our website at www.aultcare.com.
Prior Authorization/Step Therapy
Certain medications require prior authorization or step therapy, meaning your physician must consult with AultCare before prescribing a medication for you for the first time.
For a current listing of medications requiring prior authorization, visit the Pharmacy Services page at www.aultcare.com.

Medication Safety
The medications you take are an important part of your health. AultCare has compiled guidelines you can use to help your doctor and pharmacist provide you with quality healthcare. They are as follows:
• Keep an updated list of all the medications you take (including prescription, over-thecounter, herbal remedies and supplements).
• Make sure all of your doctors know all of the medications you are taking.
• Read prescription labels carefully and always follow the directions exactly. If you have questions about a prescription, such as side effects or interactions with other medications or food, ask your doctor or pharmacist. If a medication you’ve taken before looks different, notify your pharmacist immediately.
• When you get a new prescription ask your doctor if it replaces any of your current medications.
• Keep medications in their original container, unless you use a pill organizer.
• Discard all expired medications properly.
• Whenever possible, use only one pharmacy. This will ensure you do not take conflicting medications. If you use both retail and mail order pharmacies, make sure each pharmacy is aware of all your medications and allergies.
A Guide to Our Services
10
What’s Not Covered
Members should refer to their plan documents to determine which healthcare services are covered and to what extent.
The following is a partial list of services that are usually NOT covered. However your plan documents may contain exceptions to this list based on state mandates or the plan design purchased.

• All medical and hospital services not specifically covered in, or which are limited or excluded in your plan documents, including costs of services before coverage begins and after coverage ends
• Care, services or supplies which are not deemed medically necessary
• Treatment, services or procedures that are experimental, or investigative
• Non-rehabilitative chiropractic services
• Dental care, except as specifically stated in the benefit descriptions
• Eyeglasses, contact lenses, hearing aids and their fittings, and hearing tests except as specifically stated in the benefit descriptions
• Radial keratotomy, lasik, or related procedures
• Cosmetic surgery, except as specifically stated in the benefit descriptions
• Respite, custodial, and residential care except as specifically stated in the benefit descriptions

11

• Sterilization reversal and some infertility processes and related services
• Implantable drugs and certain injectable infertility drugs
• Physical, mental or substance abuse examinations done for or ordered by third parties
• Immunizations for travel or work
• Over-the-counter medications and supplies
• Marital counseling
• Services for the treatment of sexual dysfunction or inadequacies including therapy, supplies or counseling
Most plans exclude all forms of gastric restrictive procedures for the purpose of weight loss/control. Check your specific plan or contact the AultCare customer service to determine if these procedures are covered under your specific plan.
You must consult your specific plan document. Contact AultCare customer service if you have additional questions.
We Want Your Feedback
As a part of our AultCare family, your opinions are important to us. What our members tell us helps us to evaluate our services and processes, and make improvements when needed.
• New Enrollee Survey
• Member Satisfaction
Ways you can complete a survey:
The surveys can be taken two ways: online or printed and a paper copy returned by mail. To take the survey online, log into your AultCare online member account. Register for a new account if you do not have one. Once logged in, the survey link will appear at the bottom of your screen.
If you do not have internet access, but would still like to participate, contact the AultCare customer service to request a paper copy.
As always, your answers are confidential, anonymous, and in no way will affect your coverage.

A Guide to Our Services 12
Filing a Claim
Physician Claims
You do not need to send in claim forms when you use network providers. As long as you use network providers, your physician will submit claims to AultCare for you.
If your doctor is not a network provider, call AultCare Utilization Management at 330-363-6360 or 1-800-344-8858. In some cases, we may continue to pay for covered services at the network provider rate for a limited period of time to let you complete a course of treatment. We also will help you find an in-network provider or you may reference our provider directory at http://www.aultcare.com/findaprovider.
If you have an approved referral to a non-network provider, those services may be covered at the same level as network providers. Charges that exceed Usual, Customary and Reasonable (UCR) rates are not covered by your plan and are therefore your responsibility to pay. Refer to your plan’s schedule of benefits for details.
If your non-network provider does not send in your claim, you should:
1. Fill out the Application for Benefits form
2. Include a copy of the bill from your non-network provider
3. Mail the forms to AultCare at the address below:
AultCare P.O. Box 6910 Canton, Ohio 44706

13
Application for Benefits
You can get a copy of the Application for Benefits form on AultCare’s website at www.aultcare.com or by calling customer service at 330-363-6360 or 1-800-344-8858.
A separate Application for Benefits form is needed for each bill. Be sure to complete all sections of the form that apply to your situation and sign it.
Hospital Claims
When you receive services at a hospital, show your AultCare ID card. The hospital will send the claim information to AultCare.
Other Coverage
Every year, AultCare will request an update about other coverage that you and your dependents may have. The information about other coverage is necessary so we know whether to pay as primary or secondary on claims for your family members. You may not be able to collect benefits from both plans.

Application for Benefits
You will need to show your ID card when you go to a provider for services. Your provider will use the information on the card to verify coverage. If your coverage changes, you might receive a new ID card. Use the most current card as reflected by the effective date on the card.
Keep Your Records Up to Date
We need current information about you and your dependents to accurately pay claims. Outdated or incorrect information can cause mistakes, delays in payment or denial of coverage.
Updating Your Records
Tell your employer (groups) or AultCare (individuals) within 31 calendar days if there are changes in your:
• Name
• Address
• Phone number
• Marital status
• Family status, including information about your dependents, new dependents, changes in family status or who is to be covered by the health plan
Remember: Notify your employer of changes, additions, or to end coverage as soon as possible.
14
Grievances and Appeals
How to let AultCare know if you are dissatisfied or disagree with a decision about your benefit coverage.
Use this information to let AultCare know if you are dissatisfied or disagree with a decision about your benefit coverage. If you are dissatisfied with AultCare or your network providers, please contact us as soon as possible. Your concerns will be forwarded to the Grievance Department who will conduct a thorough investigation and provide a written response to you within 30 days. This is known as the Grievance Process. You may contact AultCare customer service to voice your concern or you may also put your grievance in writing to the attention of:
AultCare Grievance and Appeal Department
P.O. Box 6029
Canton, Ohio 44706
If you disagree with a determination about a specific benefit, you have the right to appeal AultCare’s decision. This is known as the Appeals Process. The appeal process can be initiated by you, your provider, or your authorized representative. Your appeal must be submitted within 180 calendar days of the adverse determination and should contain a statement describing the reasons why you feel your claim/services should not have been denied, in addition to written comments, documents, records, or other information relating to the claim/service. A full and fair review will be conducted, taking into consideration all of the information received with the appeal. Clinical appeals, or appeals relating to decisions based on medical necessity, are conducted by health professionals who are:
• The same or similar specialty as the servicing physician or requesting provider
• Board-certified, if applicable

15

Appeals will not be reviewed by the individual who made the original decision nor will they be a subordinate of that person. Appeal decisions are based only on appropriateness of care and the existence of coverage. AultCare does not specifically reward practitioners of care or other individuals for issuing denials of coverage or service care.
AultCare will provide a written notification detailing the outcome of your appeal. The timeframe for the appeal response is dependent on the type of appeal filed. Timeframes and descriptions of appeal types are as follows:
Pre-Service Appeal:
An appeal filed prior to receiving the requested service. Notification of a decision will be issued within 10 days of our receipt of your appeal.
Post-Service Appeal:
An appeal filed after services have been received. Notification of a decision will be issued within 30 days of our receipt of your appeal.
Urgent Appeal:
An appeal, if not answered expeditiously, could seriously jeopardize your health. You will be notified of our decision as soon as possible, but no later than 72 hours of our receipt of your appeal.
Appeals can be mailed to:
AultCare Grievance and Appeal Department
P.O. Box 6029
Canton, Ohio 44706
AultCare communicates your appeal rights in many ways to ensure each member understands their rights. Your plan documents, your Explanation of Benefits, and a benefit denial letter describe your appeal rights as an AultCare member. Every member is granted the same first level of appeal rights or internal review. If you initiate a first-level appeal and we uphold our original decision, your resolution letter will outline your additional appeal rights, which may include external review rights. Your rights vary depending on state and federal laws.
For more information on your appeal rights, you can review your plan document, Explanation of Benefits, benefit denial letter, appeal resolution letter or contact AultCare customer service for a copy of your appeal procedure at 330-363-6360 or toll-free 1-800-344-8858.

A Guide to Our Services 16
Enrollee Rights & Responsibilities
Quality healthcare benefits are responsibilities shared with your doctors and your plan. We want you to know your rights and responsibilities. Please read your plan documents for a full description. If you have a question, concern, or a recommendation for how AultCare could improve its policies for promoting enrollee responsibilities and rights, contact us through our website at www.aultcare.com or call customer service at 330-363-6360 or toll-free at 1-800-344-8858.
You have a responsibility to:
• Take your AultCare ID card when you go to the doctor, hospital, drug store, or healthcare provider. It contains important information. Having your card may help save time and prevent mistakes.
• Tell the doctor or nurse about your condition. Tell your doctor what medications you are taking. Answer any questions the doctor or nurse may ask you truthfully. This information may help your doctor form treatment goals and alternatives. Understand your health problems and participate in developing mutually agreed-upon goals.
• Ask questions if you do not understand something about your medical condition and the treatment alternatives (including medications) the doctor is recommending.
• Follow your doctor’s medical advice and instructions. Take medications as directed. Let the doctor know if you have a bad reaction. Let your doctor know if your symptoms do not get better, or if they get worse. Schedule recommended follow-up appointments.

17

• Live a healthy lifestyle.
• Check your Schedule of Benefits.
• Let your employer (groups) or AultCare (individuals) know if there are changes with you and your dependents.
• Obtain all required pre-approvals (pre-certifications) and second opinions.
• Ask your employer or call AultCare if you have questions about your coverage or responsibilities.
You have a right to:
• Receive information about the organization, its services, its practitioners and providers, and member rights and responsibilities.
• Receive information about your coverage and services (see your plan documents).
• A list of doctors, hospitals, and other AultCare network providers. Visit our website at www.aultcare.com or call AultCare customer service.
• Be treated with dignity and respect.
• A frank discussion with your doctor about your medical condition, including appropriate and medically necessary treatment options, regardless of cost or benefit coverage and to participate in making decisions about your healthcare. Your doctors are independent. They are not restricted or prohibited from discussing treatment options with you, including those not covered.

• Privacy of your healthcare and claims information. Your Protected Health Information will be used to pay claims, as permitted by HIPAA and as described in your Notice of Privacy Practices. Protected Health Information will not be disclosed to others without your authorization, except as permitted by HIPAA and state law.
• Ask questions, raise concerns, make complaints, and appeal denials, as explained in your certificate or benefits booklet.
• Make recommendations about AultCare’s Member Rights and Responsibilities Policy.
• Request accommodation if you have limited knowledge of the English language.
18
Privacy Practices
Notice of Privacy Practices
AultCare, on behalf of AultCare Insurance Company, maintains a Notice of Privacy Practices that provides information on the use and disclosure of Protected Health Information (PHI). This notice is available on our website www.aultcare.com. If you would like a copy of AultCare’s Notice of Privacy Practices, please contact customer service at 330-363-6360 or toll-free at 1-800-344-8858.
AultCare prides itself on ensuring our members’ PHI is maintained with appropriate privacy and confidentiality. All employees are held to internal standards of protecting written, oral, and electronic PHI. Use and Disclosure of PHI to plan sponsors is handled with security and certification the plan sponsor agrees to AultCare’s policies on PHI.
AultCare maintains a Notice of Privacy Practices that provides important information on the Use and Disclosure of PHI and your rights regarding your PHI. Highlights from the notice are outlined on the right.
Uses and Disclosures
Unless permitted by state or federal law, we will not use or disclose your protected health information for any purpose without your express written authorization. You have the right to revoke that authorization and we will take every effort to honor those requests.
We are permitted or required by law to make certain uses and disclosures of your protected health information without your authorization. For a detailed list of the uses and disclosures that do not require your authorization, please review the Notice of Privacy Practices. Examples of such uses and disclosures include:
• Treatment
• Payment
• Healthcare operations

19

Access to Your Protected Health Information
You have the right to copy and/or inspect much of the protected health information that we retain on your behalf. All requests for access must be made in writing and signed by you or your representative.
Restrictions on Use and Disclosure of Your Protected Health Information
You have the right to request restrictions on certain uses and disclosures of your protected health information for treatment, payment, or healthcare operations by notifying us of your request for a restriction in writing.
Amendments to Your Protected Health Information
You have the right to request in writing an amendment or correction to the protected health information we maintain about you. We are not obligated to make all requested amendments, but we will give each request careful consideration. All amendment requests should be in writing, signed by you or your representative, and must state the reasons for the amendment/correction request.
Accounting for Disclosures of Your Protected Health Information
You have the right to receive an accounting of certain disclosures made by us of your protected health information after April 14, 2003. Requests should be made in writing and signed by you or your representative.
Please review the Notice of Privacy Practices for more detailed information on our Use and Disclosure of Protected Health Information. The Notice of Privacy Practices and the necessary request forms are available on our website at www.aultcare.com/aultcare-privacy. If you would like a copy of the notice or the request forms, please contact customer service at 330-363-6360 or toll-free at 1-800-344-8858.

20
Frequently Asked Questions
Q. Q.
Q.
Do I need a Primary Care Physician (PCP)?
We recommend you have a PCP to help guide you in your healthcare needs.
How can I find a doctor? How do I find a doctor in my network?
You may search for network doctors in various ways:
• Visit the AultCare website at www.aultcare.com. Click on the ‘Find A Provider’ button at the top of the page. Select the ID card that matches the ID card you have to search the correct network directory.
• Call AultCare customer service.
When making an appointment with your doctor, be sure to confirm the doctor or provider is still a network provider.
What if my PCP cannot provide the care I need?
Your doctor may refer you to a specialist. If the recommended specialist is in your network, no additional actions are necessary.
Q. A.
What if my doctor refers me to an non-network doctor?
If the specialist is not in the network, your network doctor will need to provide detailed information to AultCare Utilization Management and request an approval before you seek treatment.
Q.
Q. A. A. A. A. A.
My PCP or network doctor has sent a request for my treatment with a non-network doctor. How will I know if my treatment was approved?
You will receive a letter from AultCare Utilization Management. The letter will tell you if your treatment has been approved at the network level of benefits, or if it has been denied (for PPO plans, services can be partially approved, which means the services have been approved at the non-network level of benefits).
If you receive care from a non-network provider, you may have to pay a different deductible and/or co-insurance. You will be responsible for paying any difference between what the provider charges for the service and what the plan allows.
The letter approving my care at the network level of benefits mentioned UCR. What does this mean?
This means that the non-network treatment requested by your network doctor has been approved at the network level of benefits, and payable based on Usual, Customary, and Reasonable (UCR) schedule of charges.
21
What does UCR mean?
UCR is a schedule of average fees most providers in the area charge for a given procedure. It affects insurance reimbursement and out-ofpocket charges you might have to pay. If your provider charges more than the UCR, you will be responsible for paying the difference between what the provider has charged and the UCR amount that will be used to pay your benefits.
Will I owe the amounts over UCR?
Yes. The amounts over UCR are not covered by your plan. You are responsible for those amounts. We suggest discussing payment options with your provider.
I received a letter that the recommended treatment was not approved. What does this mean?
Although the treatment may be recommended by your doctor, it may not be covered under your plan. If your referral is not approved, there is not reduced coverage for the treatment under your plan. Always refer to your plan document for specific limitations that apply. Refer to page 15 for your appeal rights.
What if I need help understanding my approval/denial letter content?
Contact Utilization Management at 330-363-6360 or 1-800-344-8858. Refer to your plan document for specific limitations that apply. Refer to page 15 for your appeal rights.
What if I need after-hours care in or out of the area?
If you need care after hours, contact your physician’s office. If you feel your needs are urgent or your situation is an emergency, proceed to the nearest emergency room, urgent care center, or call 911.
How do I view my medical benefits online?
Go to www.aultcare.com
- Log into your account
- Click on “Eligibility”
- Select “Member” from the drop-down box
- Select “Active” from the Status drop-down box
- Click “Search”
- Select plan to see benefits OR
Call customer service at 330-363-6360 or toll free at 1-800-344-8858
TTY users should call: 711.
Q. Q. A. A. Q. A. A. Q. Q. A. Q. A. 22
Glossary
This glossary defines many commonly used terms, but it is not a full list. These glossary terms and definitions are intended to be educational and may be different from the terms and definitions in your plan or health insurance policy. Some of these terms may not have the same meaning when used in your policy or plan, and in any case, the policy or plan governs. (See your Summary of Benefits and Coverage for information on how to get a copy of your policy or plan document.)
Allowed Amount- This is the maximum payment the plan will pay for a covered healthcare service. May also be called “eligible expense,” “payment allowance,” or “negotiated rate.”
Appeal- A request for your health insurer or plan to review a decision that denies a benefit or payment (either in whole or in part).
Balance Billing- When a provider bills you for the balance remaining on the bill your plan does not cover. This amount is the difference between the actual billed amount and the allowed amount. For example, if the provider’s charge is $200 and the allowed amount is $110, the provider may bill for the remaining $90. This happens most often when you see an out-of-network provider (non-preferred provider). A network provider (preferred provider) may not bill you for covered services.
Claim- A request for a benefit (including reimbursement of a healthcare expense) made by you or your healthcare provider to your health insurer or plan for items or services you think are covered.
Coinsurance- Your share of the costs of a covered healthcare service, calculated as a percentage (for example, 20%) of the allowed amount for the service. You generally pay coinsurance plus any deductibles you owe. (For example, if the health insurance or plan’s allowed amount for an office visit is $100 and you’ve met your deductible, your coinsurance payment of 20% would be $20. The health insurance or plan pays the rest of the allowed amount.)
Complications of Pregnancy-
Conditions due to pregnancy, labor, and delivery that require medical care to prevent serious harm to the health of the mother or the fetus. Morning sickness and a non-emergency cesarean section generally are not complications of pregnancy.
Copayment- A fixed amount
(for example, $15) you pay for a covered healthcare service, usually when you receive the service. The amount can vary by the type of covered healthcare service.
Cost-Sharing- Your share of costs for services a plan covers that you must pay out of your own pocket (sometimes called “out-of-pocket costs”).
23
Some examples of cost-sharing are copayments, deductibles, and coinsurance. Family cost-sharing is the share of cost for deductibles and out-of-pocket costs you and your spouse and/or child(ren) must pay out of your own pocket. Other costs, including your premiums, penalties you may have to pay, or the cost of care a plan does not cover usually are not considered cost-sharing.
Cost-Sharing Reductions- Discounts that reduce the amount you pay for certain services covered by an individual plan you buy through the Marketplace. You may get a discount if your income is below a certain level, and you choose a Silver level health plan or if you are a member of a federally-recognized tribe, which includes being a shareholder in an Alaska Native Claims Settlement Act corporation.
Deductible- An amount you could owe during a coverage period (usually one year) for covered healthcare services before your plan begins to pay. An overall deductible applies to all or almost all covered items and services. A plan with an overall deductible may also have separate deductibles that apply to specific services or groups of services. A plan may also have only separate deductibles. (For example, if your deductible is $1000, your plan won’t pay anything until you’ve met your $1000 deductible for covered healthcare services subject to the deductible.)
Diagnostic Test- Tests to figure out a health problem. For example, an x-ray can be a diagnostic test to see if you have a broken bone.
Durable Medical Equipment (DME)Equipment and supplies ordered by a healthcare provider for everyday or extended use. DME may include: oxygen equipment, wheelchairs, and crutches.
Emergency Medical ConditionAn illness, injury, symptom (including severe pain), or condition severe enough to risk serious danger to your health if you did not receive medical attention right away. If you did not receive immediate medical attention you could reasonably expect one of the following:
1) Your health would be put in serious danger;
2) You would have serious problems with your bodily functions; 3) You would have serious damage to any part or organ of your body.
Emergency Medical TransportationAmbulance services for an emergency medical condition. Types of emergency medical transportation may include transportation by air, land, or sea. Your plan may not cover all types of emergency medical transportation, or may pay less for certain types.
Emergency Room Care / Emergency Services- Services to check for an emergency medical condition and treat you to keep an emergency medical condition from getting worse. These services may be provided in a licensed hospital’s emergency room or other place that provides care for emergency medical conditions.
Excluded Services- Healthcare services that your plan does not pay for or cover.
Formulary- A list of drugs your plan covers. A formulary may include how much your share of the cost is for each drug. Your plan may put drugs in different cost-sharing levels or tiers.
24
For example, a formulary may include generic drug and brand name drug tiers and different cost-sharing amounts will apply to each tier.
Grievance- A complaint communicated to your health insurer or plan.
Habilitation ServicesHealthcare services that help a person keep, learn or improve skills and functioning for daily living. Examples include therapy for a child who is not walking or talking at the expected age. These services may include physical and occupational therapy, speech-language pathology, and other services for people with disabilities in a variety of inpatient and/or outpatient settings.
Health Insurance- A contract that requires a health insurer to pay some or all of your healthcare costs in exchange for a premium. A health insurance contract may also be called a “policy” or “plan.”
Home Healthcare- Healthcare services and supplies you receive in your home under your doctor’s orders. Services may be provided by nurses, therapists, social workers, or other licensed healthcare providers. Home healthcare usually does not include help with non-medical tasks, such as cooking, cleaning, or driving.
Hospice Services- Services to provide comfort and support for persons in the last stages of a terminal illness and their families.
Hospitalization- Care in a hospital that requires admission as an inpatient and usually requires an overnight stay. Some plans may consider an overnight stay for observation as outpatient care instead of inpatient care.
Hospital Outpatient Care- Care in a hospital that usually does not require an overnight stay.
Individual Responsibility
Requirement- Sometimes called the “individual mandate,” the duty you may have to be enrolled in health coverage that provides minimum essential coverage. If you do not have minimum essential coverage, you may have to pay a penalty when you file your federal income tax return unless you qualify for a health coverage exemption.
In-Network Coinsurance- Your share (for example, 20%) of the allowed amount for covered healthcare services. Your share is usually lower for in-network covered services.
In-Network Copayment- A fixed amount (for example, $15) you pay for covered healthcare services to providers who contract with your health insurance or plan. In-network copayments usually are less than out-of-network copayments.
Marketplace- A marketplace for health insurance where individuals, families and small businesses can learn about their plan options; compare plans based on costs, benefits and other important features; apply for and receive financial help with premiums and cost-sharing based on income; and choose a plan and enroll in coverage.
25
Also known as an “Exchange.” The Marketplace is run by the state in some states and by the federal government in others. In some states, the Marketplace also helps eligible consumers enroll in other programs, including Medicaid and the Children’s Health Insurance Program (CHIP). Available online, by phone, and in-person.
Maximum Out-of-Pocket LimitYearly amount the federal government sets as the most each individual or family can be required to pay in cost-sharing during the plan year for covered, in-network services. Applies to most types of health plans and insurance. This amount may be higher than the out-of-pocket limits stated for your plan.
Medically Necessary- Healthcare services or supplies needed to prevent, diagnose, or treat an illness, injury, condition, disease, or its symptoms, including habilitation, and that meet accepted standards of medicine.
Minimum Essential Coverage- Health coverage that will meet the individual responsibility requirement. Minimum essential coverage generally includes plans, health insurance available through the Marketplace or other individual market policies, Medicare, Medicaid, CHIP, TRICARE, and certain other coverage.
Minimum Value Standard-
A basic standard to measure the percent of permitted costs the plan covers. If you’re offered an employer plan that pays for at least 60% of the total allowed costs of benefits, the plan offers minimum value and you may not qualify for premium tax credits and cost-sharing reductions to buy a plan from the Marketplace.
Network- The facilities, providers and suppliers your health insurer or plan has contracted with to provide healthcare services.
Network Provider (Preferred Provider)A provider who has a contract with your health insurer or plan who has agreed to provide services to members of a plan. You will pay less if you see a provider in the network. Also called “preferred provider” or “participating provider.”
Orthotics and Prosthetics- Leg, arm, back and neck braces, artificial legs, arms, and eyes, and external breast prostheses after a mastectomy. These services include: adjustment, repairs, and replacements required because of breakage, wear, loss, or a change in the patient’s physical condition.
Out-of-Network Coinsurance- Your share (for example, 40%) of the allowed amount for covered healthcare services to providers who do not contract with your health insurance or plan. Out-of-network coinsurance usually costs you more than in-network coinsurance.
Out-of-Network Copayment- A fixed amount (for example, $30) you pay for covered healthcare services from providers who do not contract with your health insurance or plan. Out-of-network copayments usually are more than in-network copayments.
Out-of-Network Provider (Non-Preferred Provider)- A provider who does not have a contract with your plan to provide services. If your plan covers out-of-network services, you will usually pay more to see an out-of-network provider than a preferred provider. Your policy will explain what those costs may be. May also be called “non-preferred” or “non-participating” instead of “out-of-network provider.”
26
Out-of-Pocket Limit- The most you could pay during a coverage period (usually one year) for your share of the costs of covered services. After you meet this limit the plan will usually pay 100% of the allowed amount. This limit helps you plan for healthcare costs. This limit never includes your premium, balance-billed charges or healthcare your plan does not cover. Some plans do not count all of your copayments, deductibles, coinsurance payments, out-of-network payments, or other expenses toward this limit.
Physician Services- Healthcare services a licensed medical physician, including an M.D. (Medical Doctor) or D.O. (Doctor of Osteopathic Medicine), provides or coordinates.
Plan- Health coverage issued to you directly (individual plan) or through an employer, union or other group sponsor (employer group plan) that provides coverage for certain healthcare costs. Also called “health insurance plan,” “policy,” “health insurance policy” or “health insurance.”
Preauthorization- A decision by your health insurer or plan that a healthcare service, treatment plan, prescription drug or durable medical equipment (DME) is medically necessary. Sometimes called prior authorization, prior approval or precertification. Your health insurance or plan may require preauthorization for certain services before you receive them, except in an emergency. Preauthorization is not a promise your health insurance or plan will cover the cost.
Premium- The amount that must be paid for your health insurance or plan. You and/or your employer usually pay it monthly, quarterly, or yearly.
Premium Tax Credits- Financial help that lowers your taxes to help you and your family pay for private health insurance. You can get this help if you receive health insurance through the Marketplace and your income is below a certain level. Advance payments of the tax credit can be used right away to lower your monthly premium costs.
Prescription Drug Coverage- Coverage under a plan that helps pay for prescription drugs. If the plan’s formulary uses “tiers” (levels), prescription drugs are grouped together by type or cost. The amount you’ll pay in cost sharing will be different for each “tier” of covered prescription drugs.
Prescription Drugs- Drugs and medications that by law require a prescription.
Preventive Care (Preventive Service)-
Routine healthcare, including screenings, check-ups, and patient counseling, to prevent or discover illness, disease, or other health problems.
Primary Care Physician (PCP)- A physician, including an M.D. (Medical Doctor) or D.O. (Doctor of Osteopathic Medicine), who provides or coordinates a range of healthcare services for you.
27
Primary Care Provider- A physician, including an M.D. (Medical Doctor) or D.O. (Doctor of Osteopathic Medicine), nurse practitioner, clinical nurse specialist, or physician assistant, as allowed under state law and the terms of the plan, who provides, coordinates, or helps you access a range of healthcare services.
Provider- An individual or facility that provides healthcare services. Some examples of a provider include a doctor, nurse, chiropractor, physician assistant, hospital, surgical center, skilled nursing facility, and rehabilitation center. The plan may require the provider to be licensed, certified, or accredited as required by state law.
Reconstructive Surgery- Surgery and follow-up treatment needed to correct or improve a part of the body because of birth defects, accidents, injuries, or medical conditions.
Referral- A written order from your Primary Care Provider for you to see a specialist or receive certain healthcare services. In many Health Maintenance Organizations (HMOs), you need to obtain a referral before you can receive healthcare services from anyone except your Primary Care Provider. If you do not receive a referral first, the plan may not pay for the services.
Rehabilitation Services- Healthcare services that help a person keep, get back, or improve skills and functioning for daily living that have been lost or impaired because a person was sick, hurt, or disabled. These services may include physical and occupational therapy, speech-language pathology, and psychiatric rehabilitation services in a variety of inpatient and/or outpatient settings.
Screening- A type of preventive care that includes tests or exams to detect the presence of something, usually performed when you have no symptoms, signs, or prevailing medical history of a disease or condition.
Skilled Nursing Care- Services performed or supervised by licensed nurses in your home or in a nursing home. Skilled nursing care is not the same as “skilled care services,” which are services performed by therapists or technicians (rather than licensed nurses) in your home or in a nursing home.
Specialist- A provider focusing on a specific area of medicine or a group of patients to diagnose, manage, prevent, or treat certain types of symptoms and conditions.
Specialty Drug- A type of prescription drug that, in general, requires special handling or ongoing monitoring and assessment by a healthcare professional, or is relatively difficult to dispense. Generally, specialty drugs are the most expensive drugs on a formulary.
UCR (Usual, Customary and Reasonable)The amount paid for a medical service in a geographic area based on what providers in the area usually charge for the same or similar medical service. The UCR amount sometimes is used to determine the allowed amount.
Urgent Care- Care for an illness, injury, or condition serious enough that a reasonable person would seek care right away, but not so severe as to require emergency room care.
English
English
AultCare/Aultra Notice Tag Lines for the State of Ohio
AultCare/Aultra Notice Tag Lines for the State of Ohio
This Notice has Important Information. This notice has important information about your application or coverage through AultCare /Aultra. Look for key dates in this notice. You may need to take action by certain deadlines to keep your health coverage or help with costs. You have the right to get this information and help in your language at no cost. Call Local: 330.363.6360 Outside Stark County: 1.800.344.8858 TTY Local: 711 Outside Stark County: 711
This Notice has Important Information. This notice has important information about your application or coverage through AultCare /Aultra. Look for key dates in this notice. You may need to take action by certain deadlines to keep your health coverage or help with costs. You have the right to get this information and help in your language at no cost. Call Local: 330.363.6360 Outside Stark County: 1.800.344.8858 TTY Local: 711 Outside Stark County: 711
Spanish
Español
Spanish Español
Este Aviso contiene información importante. Este aviso contiene información importante acerca de su solicitud o cobertura a t ravés AultCare/Aultra. Preste atención a las fechas clave que contiene este aviso. Es posible que deba tomar alguna medida antes de determinadas fechas para mantener su cobertura médica o ayuda con los costos. Usted tiene derecho a recibir esta información y ayuda en su idioma sin costo alguno. Llame al Local : 330.363.6360 Fuera del condado de Stark : 1.800.344.8858 TTY Local : 711 Fuera del condado de Stark : 711
Este Aviso contiene información importante. Este aviso contiene información importante acerca de su solicitud o cobertura a t ravés AultCare/Aultra. Preste atención a las fechas clave que contiene este aviso. Es posible que deba tomar alguna medida antes de determinadas fechas para mantener su cobertura médica o ayuda con los costos. Usted tiene derecho a recibir esta información y ayuda en su idioma sin costo alguno. Llame al Local : 330.363.6360 Fuera del condado de Stark : 1.800.344.8858 TTY Local : 711 Fuera del condado de Stark : 711
Chinese
中文
Chinese 中文
本通知有重要的訊息。本通知有關於您透過 AultCare/Aultra 保险公司 提交的申請或保險的重要訊息。請留意本通知內的重要 日期。您可能需要在截止日期之前採取行動,以保留您的健康保險或者費用補貼。您有權利免費以您的母語得到本訊息和幫助 。請撥電話 本地: 330.363.6360 斯塔克縣外: 1.800.344.8858 TTY 線 本地:711 斯塔克縣外: 711。
本通知有重要的訊息。本通知有關於您透過 AultCare/Aultra 保险公司 提交的申請或保險的重要訊息。請留意本通知內的重要 日期。您可能需要在截止日期之前採取行動,以保留您的健康保險或者費用補貼。您有權利免費以您的母語得到本訊息和幫助 。請撥電話 本地: 330.363.6360 斯塔克縣外: 1.800.344.8858 TTY 線 本地:711 斯塔克縣外: 711。
German
Deutsche
German
Deutsche
Diese Benachrichtigung enthält wichtige Informationen. Diese Benachrichtigung enthält wichtige Informationen bezüglich Ihres Antrags auf Krankenversicherungsschutz durch AultCare/Aultra. Suchen Sie nach wichtigen Terminen in dieser Benachrichtigung. Sie könnten bis zu bestimmten Stichtagen handeln müssen, um Ihren Krankenversicherungsschutz oder Hilfe mit den Kosten zu behalten. Sie haben das Recht, kostenlose Hilfe und Informationen in Ihrer Sprache zu erhalten. Rufen Sie an unter Local: 330.363.6360 Außerhalb von Stark County : 1.800.344.885 8 TTY –Linie Local: 711 Außerhalb von Stark County : 711
Diese Benachrichtigung enthält wichtige Informationen. Diese Benachrichtigung enthält wichtige Informationen bezüglich Ihres Antrags auf Krankenversicherungsschutz durch AultCare/Aultra. Suchen Sie nach wichtigen Terminen in dieser Benachrichtigung. Sie könnten bis zu bestimmten Stichtagen handeln müssen, um Ihren Krankenversicherungsschutz oder Hilfe mit den Kosten zu behalten. Sie haben das Recht, kostenlose Hilfe und Informationen in Ihrer Sprache zu erhalten. Rufen Sie an unter Local: 330.363.6360 Außerhalb von Stark County : 1.800.344.885 8 TTY –Linie Local: 711 Außerhalb von Stark County : 711
Arabic
Arabic
Pennsylvania Dutch
Deitsch
Pennsylvania Dutch
Deitsch
Die Bekanntmaching gebt wichdichi Auskunft. Die Bekanntmaching gebt wichdichi Auskunft baut dei Application oder Covera ge mit AultCare/Aultra. Geb Acht fer wichdiche Daadem in die Bekanntmachung. Es iss meeglich, ass du ebbes duh muscht, an beschtimmde Deadlines, so ass du dei Health Coverage bhalde kannscht, odder bezaahle helfe kannscht. Du hoscht es Recht fer die Information un Hilf in deinre eegne Schprooch griege, un die Hilf koschtet nix Local: 330.363.6360 Außerhalb vo n Stark County : 1.800.344.8858 TTY –Linie Local: 711 Außerhalb von Stark County : 711
Die Bekanntmaching gebt wichdichi Auskunft. Die Bekanntmaching gebt wichdichi Auskunft baut dei Application oder Covera ge mit AultCare/Aultra. Geb Acht fer wichdiche Daadem in die Bekanntmachung. Es iss meeglich, ass du ebbes duh muscht, an beschtimmde Deadlines, so ass du dei Health Coverage bhalde kannscht, odder bezaahle helfe kannscht. Du hoscht es Recht fer die Information un Hilf in deinre eegne Schprooch griege, un die Hilf koschtet nix Local: 330.363.6360 Außerhalb vo n Stark County : 1.800.344.8858 TTY –Linie Local: 711 Außerhalb von Stark County : 711
Russian русский Настоящее уведомление содержит важную информацию. Это уведомление содержит важную информацию о вашем заявлении или страховом покрытии через Страховая компания AultCare/Aultra Посмотрите на ключевые даты в настоящем уведомлении. Вам, возможно, потребуется принять меры к определенным предельным срокам для сохранения страхового покрытия или помощи с расходами. Вы имеете право на бесплатное получение этой информации и помощь на вашем языке. Звоните по телефону Местный: 330.363.6360 Вне Старка County : 1.800.344.8858 TTY линия Местный: 711 Вне Старка County : 711.
French Français
Russian русский Настоящее уведомление содержит важную информацию. Это уведомление содержит важную информацию о вашем заявлении или страховом покрытии через Страховая компания AultCare/Aultra Посмотрите на ключевые даты в настоящем уведомлении. Вам, возможно, потребуется принять меры к определенным предельным срокам для сохранения страхового покрытия или помощи с расходами. Вы имеете право на бесплатное получение этой информации и помощь на вашем языке. Звоните по телефону Местный: 330.363.6360 Вне Старка County : 1.800.344.8858 TTY линия Местный: 711 Вне Старка County : 711.
French Français
Cet avis a d'importantes informations. Cet avis a d'importantes informations sur votre demande ou la couverture par l'intermédiaire de Compagnie d'Assurance AultCare/Aultra. Rechercher les dates clés dans le présent avis. Vous devrez peut -être prendre des mesures par certains délais pour maintenir votre couverture de santé ou d'aide avec les coûts. Vous avez le droit d'obtenir cette information et de l’aide dans votre langue à aucun coût. Appelez Locale: 330.363.6360 En dehors du comté de Stark : 1.800.344.8858 ligne ATS Local : 711 En dehors du comté de Stark : 711
Cet avis a d'importantes informations. Cet avis a d'importantes informations sur votre demande ou la couverture par l'intermédiaire de Compagnie d'Assurance AultCare/Aultra. Rechercher les dates clés dans le présent avis. Vous devrez peut -être prendre des mesures par certains délais pour maintenir votre couverture de santé ou d'aide avec les coûts. Vous avez le droit d'obtenir cette information et de l’aide dans votre langue à aucun coût. Appelez Locale: 330.363.6360 En dehors du comté de Stark : 1.800.344.8858 ligne ATS Local : 711 En dehors du comté de Stark : 711
Vietnamese
Việt Nam
Vietnamese
Việt Nam
Thông báo này cung cấp thông tin quan trọng. Thông báo này có thông tin quan tr ọng bàn về đơn nộp hoặc hợp đồng bảo hiểm qua chương trình Công ty Bảo hiểm AultCare/Aultra. Xin xem ngày then chốt trong thông báo này. Quý vị có thể phải thực hiện theo thông báo đúng trong thời hạn để duy trì bảo hiểm sức khỏe hoặc được trợ trúp thêm về chi phí. Quý vị có quyền được biết thông tin này và được trợ giúp bằng ngôn ngữ của mình miễn phí. Xin gọi số Địa phương: 330.363.6360 Bên ngoài của Stark County : 1.800.344.8858 TTY đường dây Địa phương: 711 Bên ng oài của Stark County : 711.
Thông báo này cung cấp thông tin quan trọng. Thông báo này có thông tin quan tr ọng bàn về đơn nộp hoặc hợp đồng bảo hiểm qua chương trình Công ty Bảo hiểm AultCare/Aultra. Xin xem ngày then chốt trong thông báo này. Quý vị có thể phải thực hiện theo thông báo đúng trong thời hạn để duy trì bảo hiểm sức khỏe hoặc được trợ trúp thêm về chi phí. Quý vị có quyền được biết thông tin này và được trợ giúp bằng ngôn ngữ của mình miễn phí. Xin gọi số Địa phương: 330.363.6360 Bên ngoài của Stark County : 1.800.344.8858 TTY đường dây Địa phương: 711 Bên ng oài của Stark County : 711.
AultCare/Aultra Notice Taglines Revised 6/2021 (TTY) 617/16
ةيبرعلا لاخ نم ةيطغتلا ىلع لوصحلل كبلط صوصخب ةمهم تامولعم راعشلاا اذه يوحي .ةماه تامولعم راعشلاا اذه يوحي نيمأتلا ةكرش AultCare/Aultra تلا عفد يف ةدعاسملل وا ةيحصلا كتيطغت ىلع ظافحلل ةنيعم خيراوت يف ءارجا ذاختلا جاتحت دق .راعشلاا اذه يف ةماهلا خيراوتلا نع ثحبا ىلع روصحلا يف قحلا كل .فيلاك ةدعاسملاو تامولعملا كتغلب ـب لصتا .ةفلكت يأ نود نم 330.363.6360 : كراتس ةعطاقم جراخ
طخل TTY:يلحملا 711 : كراتس ةعطاقم جراخ 711
1.800.344.8858
AultCare/Aultra Notice Taglines Revised 6/2021 (TTY) 617/16
ةيبرعلا لاخ نم ةيطغتلا ىلع لوصحلل كبلط صوصخب ةمهم تامولعم راعشلاا اذه يوحي .ةماه تامولعم راعشلاا اذه يوحي نيمأتلا ةكرش AultCare/Aultra تلا عفد يف ةدعاسملل وا ةيحصلا كتيطغت ىلع ظافحلل ةنيعم خيراوت يف ءارجا ذاختلا جاتحت دق .راعشلاا اذه يف ةماهلا خيراوتلا نع ثحبا ىلع روصحلا يف قحلا كل .فيلاك ةدعاسملاو تامولعملا كتغلب ـب لصتا .ةفلكت يأ نود نم 330 363 6360 : كراتس ةعطاقم جراخ 1.800 344 8858 طخل TTY:يلحملا 711 : كراتس ةعطاقم جراخ 711
Cushite-Oromo
English
AultCare/Aultra Notice Tag Lines for the State of Ohio
Beeksisni kun odeeffannoo barbaachisaa qaba . Beeksisti kun sagantaa yookan karaa AultCare/Aultra tiin tajaajila keessan ilaalchisee odeeffannoo barbaachisaa qaba. Guyyaawwan murteessaa ta’an beeksisa kana keessatti ilaalaa. Tarii kaffaltiidhaan deeggaramuuf yookan tajaajila fayyaa keessaniif guyyaa dhumaa irratti wanti raawwattan jiraachuu danda’a. Kaffaltii irraa bilisa haala ta’een afaan keessaniin odeeffannoo argachuu fi deeggarsa argachuuf mirga ni qabaattu. Lakkoofsa bilbilaa Local: 330.363.6360 Outside of Stark County: 1.800.344.8858 TTY Line Local: 711 Outside of Stark County: 711 tii bilbilaa.
This Notice has Important Information. This notice has important information about your application or coverage through AultCare /Aultra. Look for key dates in this notice. You may need to take action by certain deadlines to keep your health coverage or help with costs. You have the right to get this information and help in your language at no cost. Call Local: 330.363.6360 Outside Stark County: 1.800.344.8858 TTY Local: 711 Outside Stark County: 711
Spanish Español
Korean 한국어
Este Aviso contiene información importante. Este aviso contiene información importante acerca de su solicitud o cobertura a t ravés AultCare/Aultra. Preste atención a las fechas clave que contiene este aviso. Es posible que deba tomar alguna medida antes de determinadas fechas para mantener su cobertura médica o ayuda con los costos. Usted tiene derecho a recibir esta información y ayuda en su idioma sin costo alguno. Llame al Local : 330.363.6360 Fuera del condado de Stark : 1.800.344.8858 TTY Local : 711 Fuera del condado de Stark : 711
본 통지서에는 중요한 정보가 들어 있습니다. 즉 이 통지서는 귀하의 신청에 관하여 그리고 AultCare/Aultra 보 보험 회 회사계획 을 통한 커버리지 에 관한 정보를 포함하고 있습니다 본 통지서에서 핵심이 되는 날짜들을 찾으십시오 귀하는 귀하의 건강 커버리지를 계속 유지하거나 비용을 절감하기 위해서 일정한 마감일까지 조치를 취해야 할 필요가 있을 수 있습니다. 귀하는 이러한 정보와 도움을 귀하의 언어로 비용 부담없이 얻을 수 있는 권리가 있습니다 지 지역 : 330.363.6360 스 스타크 카 카운티 의 외 외부 : 1.800.344.8858 TTY 라 라인 지 지역 : 711 스 스타크 카 카운티 의 외 외부 : 711 로 전화하십시오.
Italian
Italiano
Chinese 中文
本通知有重要的訊息。本通知有關於您透過 AultCare/Aultra 保险公司 提交的申請或保險的重要訊息。請留意本通知內的重要 日期。您可能需要在截止日期之前採取行動,以保留您的健康保險或者費用補貼。您有權利免費以您的母語得到本訊息和幫助 。請撥電話 本地: 330.363.6360 斯塔克縣外: 1.800.344.8858 TTY 線 本地:711 斯塔克縣外: 711。
Questo avviso contiene informazioni importanti sulla tua domanda o copertura attraverso AultCare/Aultra. Cerca le date chiave in questo avviso. Potrebbe essere necessario un tuo intervento entro una scadenza determinata per consentirti di mantenere la tua coper tura o sovvenzione. Hai il diritto di ottenere queste informazioni e assistenza nella tua lingua g ratuitamente. Chiama Locale: 330.363.6360 Al di fuori di Stark County : 1.800.344.8858 TTY linea Locale: 711 Al di fuori di Stark County : 711.
German Deutsche
Japanese 日本語
Diese Benachrichtigung enthält wichtige Informationen. Diese Benachrichtigung enthält wichtige Informationen bezüglich Ihres Antrags auf Krankenversicherungsschutz durch AultCare/Aultra. Suchen Sie nach wichtigen Terminen in dieser Benachrichtigung. Sie könnten bis zu bestimmten Stichtagen handeln müssen, um Ihren Krankenversicherungsschutz oder Hilfe mit den Kosten zu behalten. Sie haben das Recht, kostenlose Hilfe und Informationen in Ihrer Sprache zu erhalten. Rufen Sie an unter Local: 330.363.6360 Außerhalb von Stark County : 1.800.344.885 8 TTY –Linie Local: 711 Außerhalb von Stark County : 711
この通知には重要な情報が含まれています。この通知には AultCare/Aultra 保険会社 の申請または補償範囲に関する重要な 情報が含まれています。この通知に記載されている重要な日付をご確認ください。健康保険や有料サポートを維持するには、 特定の期日までに行動を取らなければならない場合があります。ご希望の言語による情報とサポートが無料で提供されます。 330.363.6360 スターク郡の外: 1.800.344.8858 TTY ライン ローカル: 711 スターク郡の外: 711 までお電話ください。
Arabic
Dutch Nederlands
Deze mededeling heeft belangrijke informatie. Deze mededeling heeft belangrijke informatie over uw aanvraag of dekking via AultCare /Aultra. Kijk naar belangrijke datums in deze mededeling. Het kan nodig zijn om actie te ondernemen binnen bepaalde termijn en om uw zorgverzekering te behouden of hulp met kosten te krijgen. U heeft het recht op deze informatie en hulp in uw taal zonder k osten. Bel
Local : 330.363.6360 Buiten Stark County : 1.800.344.88 58 TTY Line Local : 711 Buiten Stark County : 711.
Pennsylvania Dutch Deitsch
Ukrainian український
Die Bekanntmaching gebt wichdichi Auskunft. Die Bekanntmaching gebt wichdichi Auskunft baut dei Application oder Covera ge mit AultCare/Aultra. Geb Acht fer wichdiche Daadem in die Bekanntmachung. Es iss meeglich, ass du ebbes duh muscht, an beschtimmde Deadlines, so ass du dei Health Coverage bhalde kannscht, odder bezaahle helfe kannscht. Du hoscht es Recht fer die Information un Hilf in deinre eegne Schprooch griege, un die Hilf koschtet nix Local: 330.363.6360 Außerhalb vo n Stark County : 1.800.344.8858 TTY –Linie Local: 711 Außerhalb von Stark County : 711
Це повідомлення містить важливу інформацію. Це повідомлення містить важливу інформацію про Ваше звернення щодо страхувального покриття через Страхова компанія AultCare/Aultra. Зверніть увагу на ключові дати, вказані у цьому повідомленні. Існує імовірність того, що Вам треба буде здійснити певні кроки у конкретні кінцеві строки для того, щоб зберегти Ваше медичне страхування або отримати фінансову допомогу. У Вас є право на отримання цієї інформації та допомоги безкоштовно на Вашій рідній мові. Дзвоніть за номером телефону Місцевий : 330.363.6360 Поза Старка County : 1.800.344.8858 TTY лінія Місцевий : 711 Поза Старка County : 711.
Romanian Română
Russian русский Настоящее уведомление содержит важную информацию. Это уведомление содержит важную информацию о вашем заявлении или страховом покрытии через Страховая компания AultCare/Aultra Посмотрите на ключевые даты в настоящем уведомлении. Вам, возможно, потребуется принять меры к определенным предельным срокам для сохранения страхового покрытия или помощи с расходами. Вы имеете право на бесплатное получение этой информации и помощь на вашем языке. Звоните по телефону Местный: 330.363.6360 Вне Старка County : 1.800.344.8858 TTY линия Местный: 711 Вне Старка County : 711.
Prezenta notificare conține informații importante. Această notificare conține informații importante privind cererea sau acope rirea asigurării dumneavoastre de sănătate prin Compania de Asigurari AultCare/Aultra. Căutați datele cheie din această notificare. Este posibil să fie nevoie să acționați până la anumite termene limită pentru a vă menține acoperirea asigurării de sănătate sau asistența privit oare la costuri. Aveți dreptul de a obține gratuit aceste informații și ajutor în limba dumneavoastră. Sunați la Locale : 330.363.6360 In afara Stark Judet : 1.800.344.8858 TTY linie Locale : 711 In afara Stark Judet : 711.
French Français
Non-Discrimination Notice:
Cet avis a d'importantes informations. Cet avis a d'importantes informations sur votre demande ou la couverture par l'intermédiaire de Compagnie d'Assurance AultCare/Aultra. Rechercher les dates clés dans le présent avis. Vous devrez peut -être prendre des mesures par certains délais pour maintenir votre couverture de santé ou d'aide avec les coûts. Vous avez le droit d'obtenir cette information et de l’aide dans votre langue à aucun coût. Appelez Locale: 330.363.6360 En dehors du comté de Stark : 1.800.344.8858 ligne ATS Local : 711 En dehors du comté de Stark : 711
AultCare/Aultra complies with applicable Federal civil rights laws and does not discriminate on the basis of race, color, national origin, age, disability, or sex. AultCare/Aultra does not exclude people or treat them differently because of race, color, national origin, age, disability, or sex. AultCare/Aultra provides free aids and services to people with disabilities to communicate effectively with us, such as: Qualified sign language interpreters and written information in other formats (large print, audio, accessible electronic formats, other formats). AultCare/Aultra provides free language services to people whose primary language is not English, such as: Qualified interpreters and information written in other languages.
Vietnamese Việt Nam
If you need these services, or if you believe that AultCare/Aultra has failed to provide these services or discriminated in another way on the basis of race, color, national origin, a ge, disability, or sex, you can contact or file a grievance with the: AultCare/Aultra Civil Rights Coordinator, 2600 6th St. S.W. Canton, OH 44710, 330-363-7456, CivilRightsCoordinator@aultcare.com. You can file a grievance in person or by mail, fax, or email. If you need help filing a grievance, our Civil Rights staff is available to help you.
Thông báo này cung cấp thông tin quan trọng. Thông báo này có thông tin quan tr ọng bàn về đơn nộp hoặc hợp đồng bảo hiểm qua chương trình Công ty Bảo hiểm AultCare/Aultra. Xin xem ngày then chốt trong thông báo này. Quý vị có thể phải thực hiện theo thông báo đúng trong thời hạn để duy trì bảo hiểm sức khỏe hoặc được trợ trúp thêm về chi phí. Quý vị có quyền được biết thông tin này và được trợ giúp bằng ngôn ngữ của mình miễn phí. Xin gọi số Địa phương: 330.363.6360 Bên ngoài của Stark County : 1.800.344.8858 TTY đường dây Địa phương: 711 Bên ng oài của Stark County : 711.
You can also file a civil rights complaint with the U.S. Department of Health and Human Services, Office for Civil Rights electronically through the Office for Civil Rights Complaint Portal, available at https://ocrportal.hhs.gov/ocr/portal/lobby.jsf, or by mail or phone at: U.S. Department of Health and Human Services 200 Independence Avenue, SW Room 509F, HHH Building Washington, D.C. 20201 1-800-368-1019, 800-537-7697 (TDD) Complaint forms are available at http://www.hhs.gov/ocr/office/file/index.html.
AultCare/Aultra Notice Taglines Revised 6/2021 (TTY) 617/16
ةيبرعلا لاخ نم ةيطغتلا ىلع لوصحلل كبلط صوصخب ةمهم تامولعم راعشلاا اذه يوحي .ةماه تامولعم راعشلاا اذه يوحي نيمأتلا ةكرش AultCare/Aultra تلا عفد يف ةدعاسملل وا ةيحصلا كتيطغت ىلع ظافحلل ةنيعم خيراوت يف ءارجا ذاختلا جاتحت دق .راعشلاا اذه يف ةماهلا خيراوتلا نع ثحبا ىلع روصحلا يف قحلا كل .فيلاك ةدعاسملاو تامولعملا كتغلب ـب لصتا .ةفلكت يأ نود نم 330 363 6360 : كراتس ةعطاقم جراخ 1.800 344 8858 طخل TTY:يلحملا 711 : كراتس ةعطاقم جراخ 711
AultCare/Aultra Notice Taglines Revised 6/2021 (TTY) 617/16

P.O. Box 6910 Canton, Ohio 44706