Intravascular QUARTERLY

Global Disclaimer: The views and opinions expressed in the Intervascular Quarterly Newsletter are those of the authors and do not necessarily reflect the official policies or positions of the Association for Vascular Access (AVA) or any of its leaders, volunteers, employees, committees, networks or other groups associated with AVA. For information on this publication, please email


THE E-NEWS PUBLICATION OF THE ASSOCIATION FOR VASCULAR ACCESS IQ CONTENT LETTER FROM THE PRESIDENT ........................................................ 04 AVA BOARD & STAFF ............................................................................... 06 AVA 2023 SESSION HIGHLIGHTS ........................................................ 10 NETWORK NEWS ....................................................................................... 19 OPTIMIZING PATIENT OUTCOMES AND SAVINGS ...................... 26 THE UN-BOXING ....................................................................................... 30 LIFE ON THE FRONTLINE ....................................................................... 32
IQ PRESIDENT’S MESSAGE BY
TONYA HEIM

IQ President’s Message
I am sure you are aware by now of the passing of our Founder, Suzanne Herbst. It was a joy each year, having her at the AVA Scientific Meeting presenting the Herbst Award recipient. She was in her element on that stage, honoring a colleague and inspiring all of us to improve the practice of Vascular Access. She will be so deeply missed at our Scientific Meeting in October in Portland. We will be doing a tribute to Suzanne as we open the conference this year.
Speaking of the AVA Scientific Meeting (AVASM), it is not too late to register. We have a great keynote speaker, and the general and breakout sessions will be inspiring as well. If you have never been to the Pacific Northwest, this is your opportunity to see a beautiful region of our great country. Check out the AVASM link at www.avainfo.org and click on the link About AVASM23, then click on Welcome to Portland for more information about things to do and places to eat while you are there. I hope to see you there.
I wanted to update you on the progress our Network Task Force has made. As a reminder, when we did the TOWS (SWOT backwards) survey at the end of 2022, we got a significant amount of feedback about the need to address issues regarding our Networks. As a result, we appointed a Network Task Force, chaired by our 2024 President-Elect, Karen LaForet. That Task Force has been meeting, has done an additional survey to help prioritize issues and put out a call for some Network Leaders to join the Task Force. We got a great response to that call and had more volunteers than slots available. I am happy to share that the following Network Leaders have been selected to serve on the Task Force; Jan Elliott from AVACNY, Lodena Moreau from WesTexVAN, Tara Fain from PeachVAN, Betsy Harmon from POLARVAN, Mark Rowe from ARVAN and Treasurer of AVA, and Tonja Stevens from DMVVAN and Presidential Advisor of AVA.
Relationships with other related Associations was another issue that came up in the data we got last winter. We have started to develop a priority list of Associations that make sense to partner with and have started to develop examples of partnership options to present when we reach out, such as education and advocacy. Some early conversations have occurred with a couple of Associations, but we have more work to do on this issue before we make further announcements. This is an exciting initiative that I think will reap a lot of benefits for AVA members.
4 THE E-NEWS PUBLICATION OF THE ASSOCIATION FOR VASCULAR ACCESS
Our Education Staff have continued to work hard to provide great content about Vascular Access and the engagement numbers demonstrate the success they are having. In June 2023, we had 2009 attendees at our educational offerings compared to 1364 in 2022. We issued 861 CE Certificates in June 2023 vs 604 in June 2022.
Our new offering, IV League Learning, has had good attendance at every session. If you haven’t joined a session yet, I would encourage you to do so. The sessions are every other week and are short presentations with an opportunity to have a discussion with the speaker. They are designed to be appropriate for Vascular Access Specialists but also for healthcare students and other clinicians who do not work full time in the Vascular Access space. Be sure and spread the word to students and colleagues you work with. It’s easy to register on the AVAinfo.org website. Thank you to Judy and Blake for your great work.
I am happy to report that our membership has continued to grow. We passed the 4000 mark in June with a total of 4133 members. As I shared at the AVASM last fall, I think that AVA has a huge opportunity to grow our membership. There are over 5,000 hospitals in the country in addition to the long-term care, dialysis, outpatient and other various places that Vascular Access is practiced. AVA has so much to offer and it is through spreading the Vascular Access excellence gospel to a broader audience that we will continue to raise the bar on patient outcomes. I encourage each of you to motivate at least one person to join AVA. Together we grow.
I started my message looking into the past with my note about Suzanne Herbst. I would like to end with a look to the future and how Suzanne’s vision lives on. Congratulations on the new 2024 slate of officers, I am excited to work with each of them next year.
5 SEPTEMBER 2023 | VOLUME X | ISSUE 3
AVA BOARD & STAFF
BOARD OF DIRECTORS
2023 PRESIDENT
Tonya Heim, MHA, MSN, RN, NEA-BC
2023 PRESIDENT-ELECT
Michelle DeVries, MPH, CIC, VA-BC™
2023 PRESIDENTIAL ADVISOR
Tonja Stevens, AGACNP, RN, BSN, VA-BC™
2023 TREASURER
Mark Rowe, MNSc, RNP, VA-BC™
2023 SECRETARY
Staci Harrison, DNP, RN
2023-24 DIRECTOR-AT-LARGE
Nael Mhaissen, MD
2023-24 DIRECTOR-AT-LARGE
Warren McGlauflin, RN, BS, VA-BC™
2023-24 DIRECTOR-AT-LARGE
Lynn Deutsch, MSN, RN, CRNI, VA-BC™
2022-23 DIRECTOR-AT-LARGE
Karen Laforet, RN, MCISc-AHCP, CCHN, CVAA, VA-BC™
2022-23 DIRECTOR-AT-LARGE
Nieltje Gedney, BA
2022-23 DIRECTOR-AT-LARGE
Chaitenya Razdan, MBA
STAFF
EXECUTIVE DIRECTOR
Brent Schwartz bschwartz@talley.com
CHIEF OPERATIONS OFFICER
Tonya Hutchison, CAE, thutchison@avainfo.org
DIRECTOR OF CLINICAL EDUCATION
Judy Thompson, MSNED, RN, VA-BC™ jthompson@avainfo.org
CLINICAL EDUCATION SPECIALIST
Blake Hotchkiss, BSN, RN, CCRN, CRNI, VA-BC™ bhotchkiss@avainfo.org
PROGRAM MANAGER
Lisa Colangelo lcolangelo@avainfo.org
JAVA EDITOR-IN-CHIEF
Michelle L. Hawes, DNP, CRNI, VA-BC™, ACRP-CP javaeditor@avainfo.org
ADVERTISING AND INTEGRATED PROGRAMS
Melissa Murphy advertising@avainfo.org
6 THE E-NEWS PUBLICATION OF THE ASSOCIATION FOR VASCULAR ACCESS
INCOMING 2024 AVA BOARD MEMBERS
It is with great pleasure and honor that we inform you the slate of candidates for the 2024 AVA Board of Directors, recommended by the AVA Board Development Commission (BDC), has been accepted by the membership. Thank you to everyone who participated and cast their vote!
The individuals who will join the AVA Board of Directors on January 1st, 2024, are Paul Blackburn, Lori Kaczmarek, Kristin Jacobs, Emily Levy, and Christine Vandenhouten. Michelle DeVries will step into her role as President and Karen Laforet will step into the President-Elect role. Nael Mhaissen, Lynn Duetsch and Warren McGlauflin will continue their terms as Directors-at-Large.
2024 PRESIDENT ELECT
KAREN LAFORET, RN, MCISC, VA-BC TM, CCHN©, CVAA©

AVA has the opportunity to be the global leader for vascular access, spearheading a partnership, collaboration with like-minded, associations or organizations aligned to improve vessel health preservation outcomes (e.g. NIHA, INS, Oley, CVAA, WoCoVa, ERCI, NCIVS, etc.). AVA will be the strategic resource and leader in providing access to education on a number of levels vis a vie the clinical practice guidelines and the collaboration with other organizations will help to standardize clinical practice. AVA’s established history of managing the tension in partnering with industry is unique and this expertise will support alignment with the partnerships to move towards global guidelines and standards and provide frameworks for healthcare policy and funding. The partnerships and leadership role will increase multi-disciplinary/interdisciplinary membership. The collaboration will showcase AVA’s history, values and mission to increase awareness of vascular access risks and benefits, increase advocacy efforts locally through to governmental arenas and increase public/clinician education in this area.
2024 TREASURER
PAUL BLACKBURN, RN, MNA, VA-BC TM
My vision for AVA is to become the driving force behind vascular access standards as well as providing a way to encourage innovation in healthcare--all while taking the cost out of care. I believe strongly in community service and have tried to serve my community in different ways. I have served previously with AVA and the AVA Foundation, as well as serving as a volunteer for the Boy Scouts of America for many years. I believe there is a great deal of work that can be done to alleviate suffering and improve the patient experience. I am dedicated to being involved in that work. I believe AVA is as well.

7 SEPTEMBER 2023 | VOLUME X | ISSUE 3
2024 SECRETARY
LORI KACZMAREK, MSN, RN, VA-BC TM


I desire to continue to lead AVA toward its continued membership growth. The pandemic tested the organization’s resolve to think outside the box to reach our members. I’ve been impressed with the expanded education offerings, outreach, and industry partnerships, which have increased AVAs visibility outside the US. I support additional progress in this area, reaching out to multiple disciplines. One day I envision AVA as a valued resource for physicians and advanced practice providers seeking knowledge about vascular access. While vascular access awareness is improving, I would like to see AVA partner more with advocacy groups. The expected changes regarding hospital-bacteremia and fungemia create an opportunity for AVA to be a leader in patient advocacy about the risk of vascular access and build a stronger case for the need for vascular access specialists.
2024-25 DIRECTOR-AT-LARGE
KRISTIN JACOBS, DNP, MBA, RN, VA-BC TM, NEA-BC
I feel the vision of AVA to have a world with safe vascular access aligns with my personal vision. This vision will not be achieved without innovation, providing strong education and resources, and growing AVA membership. I would like to find ways to improve membership with other disciplines such as physicians, renal groups, and interventional radiology groups. This makes take some “outside the box” thinking and leveraging relationships with current AVA members in those fields. I also feel we need to engage with members of the c-suite if we want to be most impactful. Although AVA has done an exceptional job of connecting with clinicians at the bedside level, I would support communication with c-suite teams and advanced practitioners such as nurse practitioners and PA-Cs. This would allow AVA to meaningfully contribute to hospital operations, outcomes, quality and safety initiatives, management, and potentially information technology enhancements. I envision strengthening our relationship with the Infusion Nurses Society and Oncology Nurses Society membership and leadership as well.
8 THE E-NEWS PUBLICATION OF THE ASSOCIATION FOR VASCULAR ACCESS
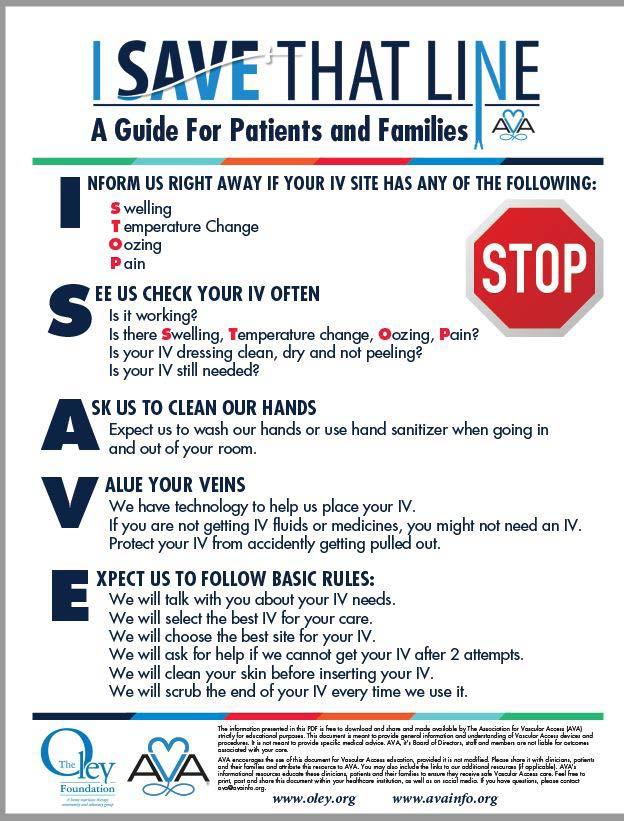
2024-2025 DIRECTOR-AT-LARGE EMILY LEVY, BS

My vision for the organization is to prioritize the inclusion of patient stakeholders at every level, including the Network level. This will ensure that patients have a voice in policies, procedures, and innovations, which is critical for the organization’s overall success and initiatives, such as I Save That Line. Patients increasingly take ownership of their devices and want to be included in leadership roles because they are the ones undergoing the procedure and living with these devices increasingly at home. We can further improve patient outcomes and satisfaction by bringing them to the forefront of the decision-making process. Moreover, I see a significant business opportunity for AVA to expand its Round Tables to include the patient community. Industry partners need help accessing patients’ input for R&D, marketing, and other areas, and AVA can play a vital role in bridging the gap between the two worlds. By creating opportunities for all stakeholders within the industry participation, we can increase the involvement and engagement of patients and industry partners alike.
I am excited to work towards this vision and believe it will be a significant step forward for the organization and the industry.
2024-2025 DIRECTOR-AT-LARGE
CHRISTINE VANDENHOUTEN, PHD, RN

As a new member of the Board of Directors, I would listen and become acquainted with the current challenges and initiatives. The current strategic plan identifies goals in the areas of membership, education, and awareness and advocacy. Unfortunately, many organizations are suffering the loss of members since today’s young professionals are less likely to join an organization. That said, they are passionate about causes. It will be important to attract them to causes that they can advocate for. AVA has done an outstanding job promoting webinars designed to address current practice challenges.
Second, I have been very involved in the education aspects of AVA. I worked closely on the PIV 101 and 201 curricula. I would like to promote the Curriculum broadly to nursing programs and health systems in which I am affiliated. Finally, I have done a great deal of political advocacy for issues affecting nursing. I am a member of the Institute for Healthcare Improvement (IHI) as well as the American Hospital Association (AHA). These affiliations provide me with opportunities to raise awareness of vascular access issues and the work that AVA is promoting.
9 SEPTEMBER 2023 | VOLUME X | ISSUE 3


REGISTRATION NOW OPEN AT: www.avainfo.org/annual Association for Vascular Access Annual Scientific Meeting October 14-17 Portland, Oregon
SESSION HIGHLIGHTS
SATURDAY, OCTOBER 14
1:45-2:45 PM
HEALTHCARE INNOVATION: ROLE & IMPACT OF CLINICIANS IN THE GLOBAL ECOSYSTEM
• Presenter: Kamna Giare-Patel, MS, RN, Chief Executive Officer, Cerespectus, Philadelphia, PA

Since childhood, I grew up in a home with a mother suffering from chronic illnesses, defying death countless times, and fully embracing life despite physical restrictions. Witnessing her fortitude and the life-enhancing impact of medical products and interventions formed my purpose in life. My personal journey continues to fuel my passion for designing new medical products and championing healthcare innovation, allowing for life-changing effects on patients and their families.
Healthcare systems are evolving and are impacted by rising consumerism, digital acceleration, advanced technologies, cost constraints, and the globalization of clinical needs. As clinicians, we play critical roles in driving innovation and transforming healthcare systems to address unmet needs.
This session will provide an overview on healthcare innovation and how it influences both the medical device industry and clinical settings based on shifting market trends and technological advancements. The role of clinicians is crucial in the global innovation ecosystem to generate successful patient-centric outcomes in dynamic environments. It is increasingly important to understand and create effective partnerships with other stakeholders such as the medical device industry, government, academia, regulatory agencies, and healthcare systems.
11 SEPTEMBER 2023 | VOLUME X | ISSUE 3
SESSION HIGHLIGHTS
SUNDAY, OCTOBER 15
8:45-10:00 AM
GENERAL SESSION: VASCULAR ACCESS DEVICE ASSESSMENT LIABILITY-NAVITAGING A MINEFILED POST-COVID
• Presenter: Russ Nassof, Esq., Executive Vice-President, RiskNomics, LLC

I am an attorney who currently sits on the Board Development Commission (BDC) and have been a past AVA Board of Directors member as well as the Treasurer and Secretary of the organization.
My General Session will address the increasing liability for vascular clinicians post-COVID specifically related to vascular access device assessment and care. Most clinicians are completely unaware of the legal quagmire they are potentially walking into everyday they enter the workplace and begin to provide IV therapy particularly when they are understaffed and with less competent colleagues.
Think Radonda Vaught could not be you? Think again…this presentation will identify potential collision points between the clinical standards of vascular access device assessment and care, the legal standards and actual day to day practice and what you need to consider to reduce exposure and liability risk. Every clinician is at risk.
12 THE E-NEWS PUBLICATION OF THE ASSOCIATION FOR VASCULAR ACCESS
SESSION HIGHLIGHTS
SUNDAY, OCTOBER 15
2:45-3:35 PM
ULTRASOUND GUIDED PERIPHERAL IV: ORIENTATION MADE EASY
• Presenter: Bethany L. Fitzgerald, MSN-RN, CNOR, University of Kansas


• Co-Presenter: Moriah Fields, BSN-RN, VA-BC, University of Kansas Health System

• Co-Presenter: Sarah Freund, BSN-RN, VA-BC (she/her/hers) - University of Kansas Health System and Children’s Mercy Hospital and Clinics
The vascular access professional is recognized as an expert in their field, trusted to perform procedures, and individualize patient care promoting optimal outcomes. Although the vascular access team member does not change from novice to expert upon receiving their new badge, some mature their skills at a noticeable pace compared to their peers. How do you tell if the team member is genuinely skilled or just lucky?
In this session, you will learn how three nurses in one Midwest health care system transformed their vascular access team orientation to distinguish luck from skill using a competency-based orientation model. Once the competency-based model was built, the team found the transition from novice to expert was not determined by the number of successful IV attempts but demonstrated through mastery of both hard and soft skills in the workplace.
This session will explore the power of a structured orientation and discuss the ten critical elements of successful IV insertion, while providing preceptors with the proper tools to articulate developmental needs of the learner. In this session, we will discuss how the length of vascular access orientation was trimmed in half while maintaining quality outcomes and improving team engagement. It’s not hard to make orientation easy!
13 SEPTEMBER 2023 | VOLUME X | ISSUE 3
Bethany Fitzgerald
Moriah Fields
Sarah Freund
SESSION HIGHLIGHTS
SUNDAY, OCTOBER 15
3:30-4:00 PM
PIV PRACTICE IN EMERGENCY DEPARTMENT: BEST PRACTICES VS. REALITY
• Presenter: Hui (Grace) Xu, Y (she/her/hers), Queensland University of Technology, Royal Brisbane and Women’s Hospital
Despite the evidence-based practice is developed to guide clinical practice, we know sometimes it is hard to follow guidelines and Standards in real practice.
Interested to hear what factors impact clinicians’ PIV insertion practices in complex, dynamic clinical settings like emergency departments? Please join the session ‘PIV practice in emergency department: best evidence vs. reality’, spoken by Dr Grace Xu.
Dr Grace Xu is a clinician-researcher, implementation science research fellow and emergency nurse practitioner from Australia. Her research interest includes emergency care, implementation science and vascular access.

14 THE E-NEWS PUBLICATION OF THE ASSOCIATION FOR VASCULAR ACCESS
SESSION HIGHLIGHTS
MONDAY, OCTOBER 16
4:00 PM
CHALLENGES & DILEMMAS IN VASCULAR ACCESS DEVICE SELECTION
• Presenter: Nadine G. Nakazawa, BCN, RN, VA-BC (she/her/hers), Vascular Access Clinician, Stanford Health Care

As patients with serious and chronic conditions are able to live longer and concurrently, more complex treatments are available; the vascular access clinician is faced with an increasingly complex assessment of the optimal vascular access device with the appropriate number of lumens to employ. Join me in exploring conflicting and complex conditions you may encounter when evaluating the most appropriate device to place.
This session is intended to stimulate your brain cells and allow you to share perspectives with one another! I look forward to seeing you in Portland!
TUESDAY, OCTOBER 17
8:30 AM
PEDINEOSIG COFFEE TALK!
• Do you have an interest in connecting with the Executive Leadership Council (ELC) for PediNeoSIG?
• Are you eager to network with fellow clinicians and discuss best practices in neonatal and pediatric vascular access?
• Or have you encountered a challenging clinical scenario and want to evaluate it with colleagues?
• The PediNeoSIG is excited to bring Coffee Talk back to conference this year. We look forward to this opportunity to network with fellow neonatal and pediatric specialists. Join us for your morning coffee and an hour of engaging discussion about current trends in vascular access impacting our patients, big and small.
Please let us know topics of interest or submit questions you would discussed. Submit here.
15 SEPTEMBER 2023 | VOLUME X | ISSUE 3
SESSION HIGHLIGHTS
TUESDAY, OCTOBER 17
1:45-3:00 PM
GENERAL SESSION: EXTREME VASCULAR ACCESS: EXPANDING VASCULAR ACCESS PRACTICE SKILLS AND STRATEGIES
• Presenter: Gail M. Egan, MS, ANP-C, FSIR, Nurse Practioner, Stanford Health Care, Granite Bay, CA
• Co-Presenter: Nancy Spencer, MS, FNP, FSIR, Nurse Practioner, Community Care Physicians, Schenectady, NY


Don’t leave early! The best is yet to come on Tuesday afternoon when two experienced nurse practitioners in Interventional Radiology will talk about expanding practice in extreme clinical situations in vascular access!
Learn about alternate access sites, use of devices in novel ways, and innovative clinical decision making! We will discuss off label use of devices, as well as scope of practice issues.
If you are new to vascular access, come hear about advanced techniques that you may want to consider in the future. And if you are an experienced clinician, there is something for you too…. learn about techniques you may not have considered, and how and when to deploy advanced technical maneuvers!
See you then!
16 THE E-NEWS PUBLICATION OF THE ASSOCIATION FOR VASCULAR ACCESS
Gail M. Egan Nancy Spencer
JOIN US IN OREGON AT AVA SCIENTIFIC MEETING 2023 PRECONFERENCE AS WE TRAILBLAZE THROUGH PEDIATRIC AND NEONATAL PICC INSERTION.
YOU TALKED...WE LISTENED!
Based on AVASM22 attendee feedback, we restructured the workshop to include a beginner and an advanced session. Stations were streamlined for hands-on learning utilizing pediatric and neonatal-sized needles, sheaths, and simulation pads. Session capacity was increased, a question-and-answer time was added to the end of each session, and each participant will be verified upon completing the program objectives.
The beginner session will be held in the morning and is designed for participants new to PICC insertion. The stations will include ultrasound guidance, direct puncture (sheath over needle), dressing and securement devices, Surgical ANTT (aseptic non-touch technique), PICC measurement, and patient bundling for procedural success. The session will conclude with a demonstration of a full PICC insertion.
The advanced session will be in the afternoon and designed for participants with approximately 3 years (~1000hrs/yr) of vascular access practice. The session will focus on the neonatal population and more challenging pediatric cases. The stations will include ultrasound guidance and the nuisances for neonates, neonatal Modified Seldinger Technique (MST), troubleshooting and challenging pediatric/neonatal cases, and ECG tip location technology. The session will conclude with a demonstration of a Mid-thigh Femoral PICC insertion.
Both sessions will also include a Child Life Specialist (CLS) presentation on how to best support and help the child cope during a PICC insertion through procedural medical play, preparation, education, and self-expression.
After a long day on the Oregon PICC Trail, please join us as we all put up our feet, eat, drink, and network around the campfire at the Pediatric Neonatal Reception. We look forward to seeing everyone in October for the AVA Scientific Meeting 2023.

17 SEPTEMBER 2023 | VOLUME X | ISSUE 3
The Association for Vascular Access (AVA), in collaboration with The Clinician Exchange (TCX), launched a new, best-in-class learning management system tailored to aspiring and established vascular access clinicians.
Providing cutting edge training, critically-acclaimed presentations from scientific meetings, journal review courses and much more, AVA Academy is a groundbreaking initiative that advances the heart of AVA’s mission – Protect the Patient | Educate the Clinician | Save the Line. Academy curriculum is now available to the public, and to active AVA members at a discount.
It's our mission to create greater public awareness of vascular access and to empower our members with significantly more educational resources, networking opportunities, and advocacy tools in support of and dedication to the patients that we are entrusted to serve.

AVA Academy is always open! View Course Catalog Launch My Courses Looking to further your education but struggling to find the time amidst a busy work schedule? AVA Academy is always open! AVA Academy is now open to all curious minds Choose and enroll in your classes today!
• Review course content, outlines and objectives
• Purchase courses
• Add courses to your personal Course List
• Available to Members, Non-members and all site visitors with a Guest Account
• If you're not an AVA member, consider Joining AVA or you may create a Guest Account at no charge
• Sign in to your personal AVA Academy Account



• Launch your courses
• Take quizzes
• Available to Members and Non-members with a Guest Account
• You will need to sign in to the AVA website prior to clicking Launch My Courses above
18 THE E-NEWS PUBLICATION OF THE ASSOCIATION FOR VASCULAR ACCESS
ADEMY Learn more at www.avainfo.org/AcademyLaunch
NETWORK NEWS
FLAVAN sprung into Spring 2023 hosting our 12th annual educational summit in the sand at Cocoa Beach, Florida where we welcomed 60 attendees and 11 vendor partners. Our day was filled with education, networking and learning about industry products.





Educational topics included Compassionate Care for Patients with a History of Substance Abuse presented by Chris Cavanaugh and sponsored by RyMed Technologies, Clinical Audit Cycle/Importance of Audits and Feedback presented by Amy Gregory and sponsored by 3M, Near Infrared Technology for Improving Peripheral Intravenous Catheter Placement: A Clinical Technology Implementation presented by Elizabeth Weathers and sponsored by AccuVein, Patient and Nursing Value of Long-Term PIVs presented by Connie Girgenti and sponsored by Tacy Medical, and Vessel Preservation presented by Malachi LeVeille sponsored by Teleflex. Attendees had opportunities to win several door prizes including FLAVAN memberships, GulfVAN educational day admission and an AVA membership.
Established in 2007, FLAVAN celebrates16 years as an AVA Network. We took time during our summit to recognize our past and present board members along with our sister networks in Florida.

19 SEPTEMBER 2023 | VOLUME X | ISSUE 3
FLAVAN WOULD LIKE TO CONGRATULATE OUR 2023 AVA SCIENTIFIC MEETING SCHOLARSHIP WINNERS.

Debbie Cooke and Tina Fahey both will receive a full 2023 AVA scientific meeting registration along with $200 towards travel expenses. Once they return, both ladies will present what they learned to our members.


FLAVAN’s board of directors attended and assisted our sister network, GulfVAN at their educational event held in Tampa, Florida.

For more FLAVAN news and upcoming events please visit our website by clicking the link FLAVAN and don’t forget to like and follow us on Facebook!
President Meagan Capen, APRN, CPNP-AC, MSN, VA-BC™
President Elect David Markle, RN, VA-BC™
Treasurer Amanda Pierce BSN, RN, VA-BC™
Secretary Austin Green BSN, RN, VA-BC™
20 THE E-NEWS PUBLICATION OF THE ASSOCIATION FOR VASCULAR ACCESS
NETWORK NEWS
GULFVAN IS PROUD TO ANNOUNCE OUR NETWORK’S 2023 SCHOLARSHIP RECIPIENTS!
GULFVAN OFFERS A MINIMUM OF TWO SCHOLARSHIPS TO OUR NETWORK MEMBERS EVERY YEAR: THE NINA MARIE MARINO-WILLIAMS SCHOLARSHIP AND THE JILL NOLTE OZARKVAN SCHOLARSHIP.


Sheila has been a GulfVAN member since 2019 and rarely misses a meeting. She currently works at John’s Hopkins All Children’s Hospital as the RN Clinical Supervisor of the Vascular Access Team where she supervises a team of nine nurses. She has been a nurse for almost 30 years and has always worked in Pediatrics. Sheila has been VA-BC certified since 2019. We are thrilled that Sheila finally gets to attend an inperson national meeting so she can take information back to her team and help Tampa Bay’s smallest patients.

OUR JILL NOLTE OZARKVAN SCHOLARSHIP HAS BEEN AWARDED TO SANDRA MEHNER.

Sandra has been a GulfVAN member since 2008 and is the current Secretary/Treasurer. She works at Moffitt Cancer Center for 9 years and previously managed the Vascular Access Team at Tampa General Hospital. Sandra has been VA-BC certified for 10 years and was a previous member of AVA’s Board Development Commission. We are thrilled that she can learn the latest vascular access information that will support Tampa Bay’s oncology patients.
Congratulations Sheila and Sandra! We are honored to have you represent GulfVAN in Portland, Oregon.

21 SEPTEMBER 2023 | VOLUME X | ISSUE 3
OUR NINA MARIE MARINO-WILLIAMS SCHOLARSHIP IS AWARDED TO SHEILA CASTLE.
NETWORK NEWS
AVACNY has planned an exciting and busy schedule for 2023, with three educational sessions already completed and more to come. Our recent events have been a great success.
At Delmonico’s Steakhouse in Utica, NY, we hosted a packed house for a presentation sponsored by PDI, with Speaker Jenny Bender MPH, BSN, RN, CIC, on Vascular Access Considerations in the Elderly and the Older Adult Living with Dementia: the Need to be Prepared for the Aging. The audience was engaged and we look forward to inviting Jenny back for another session.
On June 21st, Eddie Korycka, MSN-Ed, RN, with Access Vascular, spoke about the Pathway to Patency: Exploring the Challenges to Catheter Patency and the Technology That Reduces Them at the popular Lemon Grass Restaurant in Syracuse, NY.

On July 26th, ICU Medical speaker Anya Wunej, BSN, RN, spoke about Decreasing Hemolysis and False Positive Blood Culture Contamination with Optimal Process at another well-attended event in Syracuse.
Our 14th Annual Teaching Day Symposium is scheduled for Friday, November 10th, 2023, at the Craftsman Inn and Conference Center in Syracuse, NY. As always, We expect an excellent turnout among our usual sponsors. Nurses from all over New York State typically attend this fantastic educational opportunity.
Vendor registration is now open, with attendee registration available on September 1. Stay tuned for announcements about our speakers.
Our goals for the future are to continue offering educational opportunities, expand our network of healthcare providers, encourage certification through the Vascular Access Certification Corporation (VACC), and promote membership in the National Association for Vascular Access (AVA).

We have many new opportunities to host meetings and network with clinicians and industry professionals on the latest trends in vascular access and infusion therapy technologies in 2023 and 2024. Join us!
AVACNY: http://avacny.com
AVA National: http://www.avainfo.org
VACC: http://www.vacert.org
22 THE E-NEWS PUBLICATION OF THE ASSOCIATION FOR VASCULAR ACCESS
Learn More! Learn More!
AVA was founded on the premise that everyone should come together to address the complexities of VADs and their insertion, use, care, and maintenance The first meeting of AVA (as a committee in 1985) was attended by those of diverse backgrounds from hospitals, home care, industry, pharmacy, etc.
Today, AVA continues as a multidisciplinary organization of healthcare professionals that care about best outcomes for patients This is why AVA partners with device manufacturers who provide access to the best technology, resources, and education in the specialty of vascular access.



AVA has made it easy for YOU to have access to Devices, Products, and Solutions year-round! Check out this new resource and connect to AVA Industry Partners that want to help you provide the best outcomes for your patients.

LEARN MORE



23 SEPTEMBER 2023 | VOLUME X | ISSUE 3






24 THE E-NEWS PUBLICATION OF THE ASSOCIATION FOR VASCULAR ACCESS AVA CURRENTLY HAS 43 ACTIVE NETWORKS www.avainfo.org/networks info@vacert.org 414-231-8222 vacert.org December 2023 recertification by CE open now through 12/1/23. December 2023 exam applications open 9/1 through 10/15/23. Safer care. Knowledgeable clinicians. Improved outcomes. Vascular Access Board Certification VACC-0423-398 SHOP NOW!
Call for news, product evaluations, quality improvement initiatives, and patient stories.

IQ is a quarterly AVA Newsletter that serves our membership in a way that a peer-reviewed publication can’t. In this publication, our members can tell us how a product performs in the real world, let patients tell us about their side of the line, and share what our AVA Networks are up to.
IQ is a way for new authors to get started with publishing less formally. Submissions will require disclosures for product evaluations, patient permission to tell their stories, and references to support your statements. All IQ manuscripts are subject to scrutiny by the JAVA editor, and mentoring will be offered to help you be successful.
If you have questions or don’t know where to start, contact the JAVA editor @ javaeditor@avainfo.org.
SUBMISSION DATES ARE:
• November 24, 2023 for submissions for the Winter IQ
25 SEPTEMBER 2023 | VOLUME X | ISSUE 3 @associationforvascularaccess www.facebook.com/associationforvascularaccess/ @ISaveThatLine twitter.com/ISaveThatLine @i-save-that-line www.instagram.com/i-save-that-line/ Association For Vascular Access www.linkedin.com/company/association-for-vascular-access/ Association For Vascular Access www.youtube.com/AssociationForVascularAccess
SUBMIT TO AVA@AVAINFO.ORG
FOR COMMENTS OR SUGGESTIONS, PLEASE
OPTIMIZING PATIENT OUTCOMES AND SAVINGS: THE PROMISE OF STERILE BARRIER DRESSINGS IN UGPIV INSERTIONS
The following is a branded article. The information presented in this article is the opinion of the author(s) and patient(s) and not necessarily the view of the Association for Vascular Access. AVA expects the reader to investigate any manufacturer’s claims regardless of the forum. AVA appreciates the partnership with manufacturers to improve the lives of patients. Intravascular Quarterly invites other manufacturers to present their stories in this way.
PAM PRESSNALL, RN, VA-BC, VERO BEACH FL
NANCY MOUREAU, RN, PHD, CRNI, CPI, VA-BC, CEO, PICC EXCELLENCE, HARTWELL, GA
As hospitals navigate the changing demographics of their patient populations, many are seeing an increase in the use of ultrasound-guided peripheral intravenous (UGPIV) procedures. At the same time, hospitals also face significant financial strain due to inflation. Recent data show that hospitals have experienced higher costs for labor, supplies, and pharmaceuticals, while reimbursement rates have not kept pace with these increases.1 In response, hospitals are taking a closer look at their cost structures and exploring new approaches to remain financially viable without impacting patient care.
These combined trends – a challenging financial environment and a hospital-wide increase in UGPIV procedures – inspired our own quality improvement initiative for UGPIV insertions in our 245-bed hospital in Florida.2 During an observational study, a great deal of supply variation and waste among departments was identified, which led to concern about inefficiencies with both the number of supplies used and the time spent on these procedures. This raised important questions: with the increasing need for UGPIV insertions, could standardization of UGPIV supplies and procedures optimize protection and reduce costs, while maintaining – or even improving – the safety and comfort of this increasingly common procedure?
Current Practice – Wasteful and Inefficient Central Line Dressing Kits
We began our quality improvement project by evaluating current procedural practices and supplies used for UGPIV insertions, which revealed significant and consistent supply variation and waste.2 At the time, our inserters were trained on UGPIV procedures using a Central Line Dressing Kit, which contained: an antimicrobial sponge, sterile gloves, sterile probe covers, sterile gel, drape, gauze, skin antiseptic, and a securement device. Despite standardized training, we noted that some inserters were wasting many of the more expensive components of the kit. In addition, there was significant variation between departments regarding which products were used and which steps of the aseptic procedure were followed. This included practice inconsistencies in the use of sterile vs. non-sterile gloves, non-sterile gel, needles inserted through non-sterile gel, and frequent procedural contamination.
Most importantly, patient dissatisfaction was noted on several occasions, with many patients requesting that “the certified nurses” do the insertions, particularly after multiple unsuccessful attempts.2
26 THE E-NEWS PUBLICATION OF THE ASSOCIATION FOR VASCULAR ACCESS
1-2-3-
METHOD FOR STERILE BARRIER DRESSING
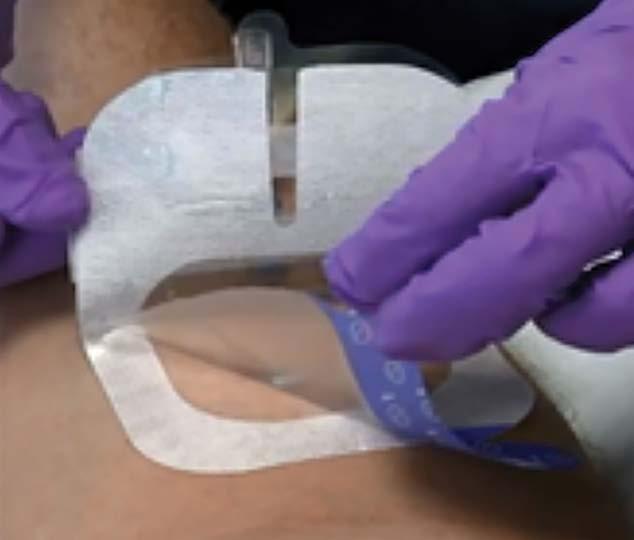
The Solution: IV Start Kit with Sterile Transparent Barrier Dressing
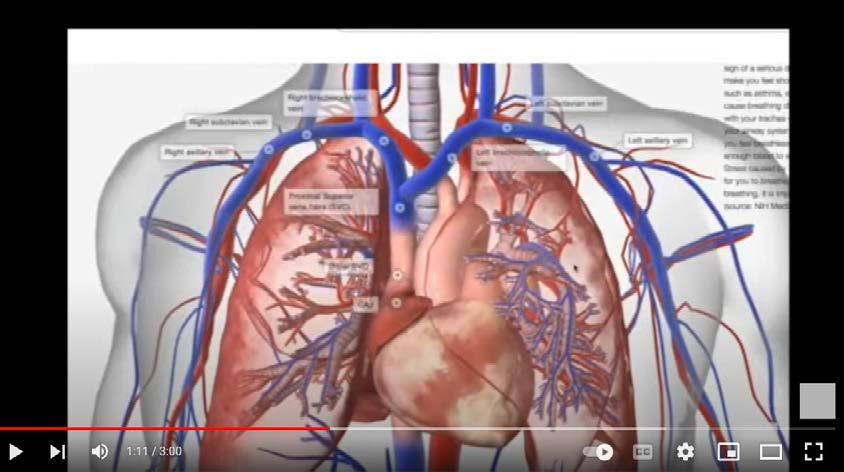
In 2021, our service standardized the UGPIV insertion process by replacing the Central Line Dressing Kits.2 Instead, inserters performed the procedure using only exam gloves, multiuse gel, and an IV Start Kit containing a transparent sterile barrier dressing (in lieu of a sterile probe cover). Designed specifically for vascular access procedures using ultrasoundguided technology, the barrier dressing provides sterile probe protection and prevents the ultrasound gel from coming into contact with the sterile insertion site. In addition, this form of probe protection also serves as a transparent dressing cover.
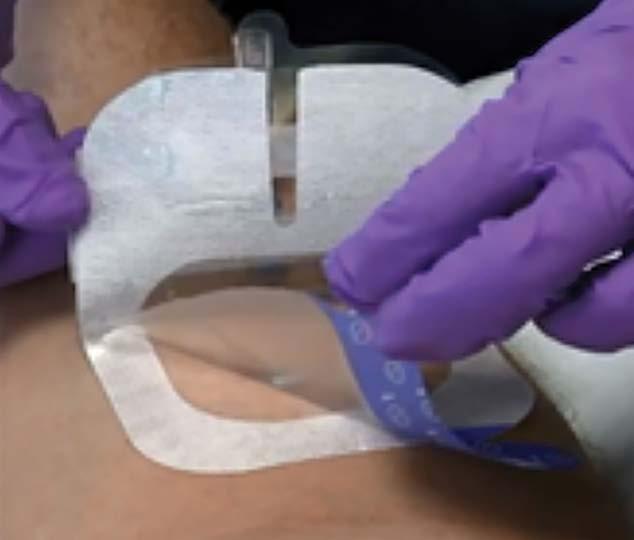


With the sterile barrier dressing, the ultrasound gel is not used at the insertion site, it is applied to a removable film layer on the backside of the dressing. The transparent nature of the dressing ensures visibility for target vessel identification. At the same time, this method of probe protection keeps the puncture area dry and free from the ultrasound gel. The dressing has an innovative design that allows ultrasound transmission while preventing the gel from touching the IV site. It provides a barrier between the non-sterile ultrasound probe and the gelfree sterile puncture site. After use, the top layer of the dressing, where the gel is applied, is lifted off and discarded. Nursing time is lessened by eliminating the post-insertion cleanup and preventing potential securement failure that can be caused by inadequate gel removal. A 2018 clinical product evaluation of the sterile barrier dressing with 14 patient applications, undergoing various vascular access procedures, concluded that the use of the dressing represented a significant improvement in gel separation and dressing adherence over other sterile barriers.3 The study also concluded that this newer method had the potential to improve the aseptic technique for ultrasound guided peripheral catheter insertions.

In a survey of 398 respondents for ultrasound guided peripheral catheter insertion practices, there was much variation over types of supplies used and answers that included not used, sometimes used, and always used for gloves and probe protection.4 Despite inconsistent supply usage, 92% stated that aseptic technique was very important, and 58% said probe protection was very important, while 42% said protection was somewhat or not important. The same type of variations existed with gel, stating non-sterile gel, single use gel, and sterile gel were not used, sometimes used, and only 48% said always for sterile gel. Sterile probe covers were indicated as always used in 25% and other barrier dressings were sometimes and always used in 29% of the clinician answers.

27 SEPTEMBER 2023 | VOLUME X | ISSUE 3
A qualitative observational review demonstrated that clinicians found the sterile barrier dressing improved patient care services and was easy to use.5 According to the results of this 2023 in-vivo qualitative report, 97% of respondents strongly agreed that the dressing provided gel and probe separation from the skin, and 98% preferred using the sterile barrier dressing over the sterile transducer cover.5 In addition, 97% agreed it was easy to apply, and 87% supported using the sterile barrier dressing to improve patient care by facilitating the aseptic insertion technique.
Standardizing Procedures and Improved Aseptic Technique Reduces Procedure Time and Cost
Our own quality improvement initiative evaluated the impact of changing to the new kit for efficiency and procedure standardization while incorporating aseptic non touch technique (ANTT) for UGPIV insertions.2 We compared the cost of supplies and length of procedures using current supplies (including sterile probe cover) versus the IV Start Kit and transparent barrier dressing were compared with procedure time and cost of supplies.
Reduced supply costs by 73%
Materials management records showed that prior to the change, the cost of supplies, including the Central Line Dressing Kit, was $25.32 per insertion.2 With the IV Start Kit and sterile barrier dressing, the cost dropped to $6.88 per insertion, resulting in a mean savings of $18.44 per UGPIV insertion. This represented a 73% reduction in supply costs associated with the IV Start Kit. With more than 90 catheters placed per month, this represents a potential annual cost savings of approximately $20,000.
Reduced nursing time by 50%
The change also resulted in a 50% reduction in nursing time when changing to an IV Start Kit.2 On average, nurses spent 6.51-12.14 minutes per insertion when using a full probe cover and Central Line Dressing Kit, but just 3.2-4.25 minutes when using the IV Start Kit and sterile barrier dressing. This resulted in a nursing efficiency gain of 8.4 hours per month. Freed up nursing time translates into more patients receiving skilled and successful insertions as well as happier patients and nurses.
Better aseptic technique
The sterile barrier dressing improves aseptic technique both during and after UGPIV insertions. It provides effective probe protection and reduces the risk of contamination by preventing gel from coming into contact with the sterile insertion site. It also eliminates potential complications that can result from inadequate gel removal, including securement and dressing adherence issues.
Continuing the Benefits of UGPIV Standardization
In the current environment, it is important for hospitals to give consideration to new methods to reduce costs, save nursing time, and improve patient outcomes. Our findings show that the standardization of supplies and procedures for UGPIV with a sterile transparent barrier dressing results in less waste with added value of time and overall cost savings. This benefits hospitals, clinicians and patients alike by simultaneously providing efficiency, safeguarding patients with standardized aseptic practices, saving clinicians’ time, and saving the hospital money.
Moving forward, we will need to perform intermittent checks and continued education for all current and new inserters to ensure that standardization of the UGPIV procedure can be maintained across all departments so that patients, clinicians and hospitals can continue to experience the benefits of this quality improvement initiative.
References
1. Sudimack A, Polsky D. Inflation Is Squeezing Hospital Margins—What Happens Next? Health Affairs Forefront. Published October 25, 2022. Available at: https://www.healthaffairs.org/content/forefront/inflationsqueezing-hospital-margins-happens-next. Accessed August 4, 2023.
28 THE E-NEWS PUBLICATION OF THE ASSOCIATION FOR VASCULAR ACCESS
2. Pressnall P, Moureau N. Simple & Efficient: Standardizing Ultrasound-Guided Peripheral Insertions with Barrier Dressing Cuts Waste, Saves Time, Costs Less, Improves Patient Safety. Poster presentation at Canadian Vascular Access Association & World Congress on Vascular Access Special Event, Toronto, Ontario, April 26-28, 2023.
3. Moureau N and Ostroff M. Observational Research of Ultrasound Guided Peripheral Catheter Barrier and Securement Dressing. Association for Vascular Access Abstract 491678, 2018.

4. Drafz M, Goeller K, Dizon B, Moureau N. Efforts Toward Standardization of UGPIV Insertion through Quantitative Clinical Product Evaluation. Presented at the 6th World Congress on Vascular Access, April 29–30, 2021 | Virtual. Available at https://www.parkerlabs.com/wp-content/uploads/2022/03/Clinical-ProductEvaluation-of-UltraDrape-4849_ParkerPosterHandout_PRODUCT_WoCoVA2021_2_FINAL.pdf. Accessed Aug. 4, 2023.
4. Moureau N, Gilbert GE. Survey of Ultrasound-Guided Peripheral Intravenous Practices: A Report of Supply Usage and Variability Between Clinical Roles and Departments. Journal of the Association for Vascular Access. 2020;25(3):28-38. Available at https://meridian.allenpress.com/ java/article/25/3/28/442553/Survey-of-Ultrasound-Guided-Peripheral-Intravenous. Accessed Aug. 4, 2023.
5. Drafz M, Goeller K, Dizon B, Cobbs A, Moureau N. Multi-center Qualitative Observational Evaluation of Ultrasound Probe Protection using a Sterile Transparent Barrier and Securement Dressing to Standardize UGPIV Catheter Insertions. Int J Nurs Health Care Res 2023;6:1418. https://doi.org/10.29011/2688-9501.101418
We invite you to submit original manuscripts that may improve patient outcomes and our understanding of the vascular access specialists’ role in the healthcare system. Manuscripts could include:
• Clinical Practice
• Patient Education
• Clinician Education
• Promoting & Sustaining Change
• Vascular Access Research
• Legal perspectives
• Financial Considerations
• Anything to move AVA’s mission forward.
For complete instructions, go to Information for Authors at www. avajournal.com
If you would like some mentoring help, email AVAFoundation@ avainfo.org. The AVA Foundation board can match you with free mentoring for AVA members on research and publication.
If you have general questions or don’t know where to start, contact the JAVA editor at: javaeditor@avainfo.org.
29 SEPTEMBER 2023 | VOLUME X | ISSUE 3
THE UN-BOXING
 MICHAEL VOLKOV, RN, VA-BC, CNPI, VALLEY CHILDREN’S HEALTHCARE, MADERA, CA
MICHAEL VOLKOV, RN, VA-BC, CNPI, VALLEY CHILDREN’S HEALTHCARE, MADERA, CA
I read many articles where the subjects are praised for “thinking outside of the box.” I also read articles where subjects perform procedures that either haven’t been done before, using “novel” techniques. While the latter may be accurate, the former is incongruent with science.
Our world is round. Boxes are flat-sided. Perhaps Flat-Earth society members can “think outside the box,” but we as Vascular Access Specialists (and also medicine in general) live in a circular world; both literally and occupationally.
There are over 8 billion people living on the Earth now. This infers directly that there are over 8 billion variations of vasculature and possible treatment options. Certainly the vast majority of humanity is similar and subsequently can be somewhat presumed to have similar issues. However, vessel health and preservation is inherently un-boxable; specifically because of all the options. We cannot use a “rule” for everyone. Each person/patient gets their very own unique, individualized care.
Perhaps we might be confusing treatments with algorithms, which by nature of printing documents creates boxes. Guidelines are straight-lined borders that guide best decisions. But even long, straight lines ultimately diverge. Veins bifurcate. Long stretches of highways have off-ramps, plumb-lines of buildings have to yield to windows/layers/structural supports. The boxes of those occasionally thinking outside of them are by very nature limiting and incongruent with the real world.
In our Vascular Access world, there should not be boxes outside of which to think. There are no boxes. Everything is worthy of consideration if there is obligatory co-thought to safety and efficacy. Over 8 billion options to treat a complex patient’s needs. There are no boxes; merely solutions that haven’t been realized yet. As Vascular Access Specialists, we should be at the forefront of providing solutions to the complex patients we encounter. What may work for the vast majority of patients may not work for that one unique patient we haven’t met yet.
Some in our own field have been condemned for providing solutions that truly worked, but were “outside” certain people’s boxes. After some time, these solutions were found to be not only really good and safe solutions, but became mainstream. Certainly patients’ lives have been vastly improved because there was no box being used for decision-making – there was a problem requiring a solution and that solution was realized.
I propose we put to death the phrase “thinking outside the box.” Thinking outside the box infers that you must return to the box after your epiphany and subsequently necessarily limits your options. Our ultrasound screens display round holes to poke with our round needles, and our round world has too many options to keep boxed up. Let’s just think about solutions, not borders, boxes, or other straight-lined limitations. Become unlimited. Un-box your mind!
30 THE E-NEWS PUBLICATION OF THE ASSOCIATION FOR VASCULAR ACCESS
AVAILABLE NOW
RESOURCE GUIDE FOR VASCULAR ACCESS
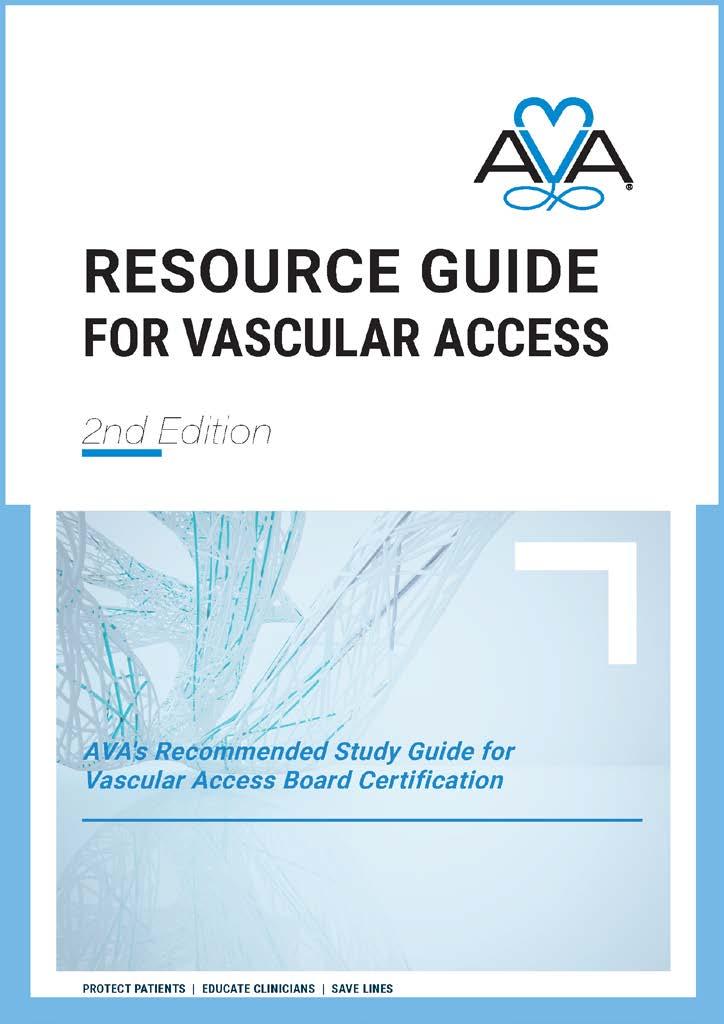
The 2021 AVA Resource Guide for Vascular Access: AVA's Recommended Study Guide for Vascular Access Board Certi cation provides an overview of basic vascular access knowledge and covers essential elements that clinicians implement on a daily basis. Throughout the Resource Guide, readers have access to high de nition images, videos, illustrations and engaging animations that give them a greater understanding of the concepts. The guide may be used to prepare for the vascular access board certi cation examination (VA-BC™), as well as serve as a resource throughout professional practice.
AVA MEMBER PRICE:
$99 digital only
$129 print only
$159 bundle (print and digital)
NON AVA MEMBER PRICE: $129 digital only

$169 print only $199 bundle (print and digital)
Digital Access:
Check
• Not a downloadable le. It is not printable and is for view on your device only. The digital access is not shareable with another account. You will receive a redemption key and an access link after purchase.
• Corrections and incremental updates to version one will automatically populate your digital copy (no additional charge)
31 SEPTEMBER 2023 | VOLUME X | ISSUE 3
PURCHASE IT ONLINE TODAY!
out the Resource Guide sneak peak videos on our YouTube channel!
LIFE ON THE FRONTLINE:
A LETTER FROM THE PARENTS OF AN AMAZING YOUNG WOMEN TO ALL HEALTHCARE PROFESSIONALS.
Becky, who is 16 years of age now, has asked us as her parents to write this letter not only to support her but also in hopes that no other patient will have to endure what she has gone through the past couple of years following complications of her CVL [Tunneled-Cuffed Central Venous Access Device]* placement. Becky has a rare form of intestinal failure called neuropathic chronic intestinal pseudo-obstruction, diagnosed at approximately four months of age. She requires TPN [total parenteral nutrition] to maintain nutrition and thus her life. Her first central line was placed in her right internal jugular on 9/7/07 while she was a patient in the NICU. The external stay suture was removed while still in the NICU at that hospital. This line lasted until April 2009 when it fractured over the clavicle due to her growth.
On 4/8/09 a physician placed a new CVL in the left subclavian. Again, the external stay suture was appropriately removed within the first two months after placement at a clinic visit. Amazingly, despite several repairs, Becky kept this line until 2/23/14 when it fractured near the exit site. It was removed and placed again in the left subclavian. The right subclavian was attempted but could not be used at that time. Again, the external stay suture was removed during a subsequent clinic visit, within the first few weeks to months following placement. Becky was able to keep this line for approximately 5 years which we are told is “unheard of” and is a testament to the excellent home care she has received.
Maintaining central line access is critical to her survival. She has only had one line infection which was successfully treated while preserving her central line. This line began leaking internally in August of 2019 and required replacement on her 12th birthday. A physician placed a new line in the right subclavian. Becky was pre-pubescent, having no breast tissue, at the time of this surgery. It certainly could have been anticipated that she would continue to grow as she previously had and that she keeps a line an average of 3-5 years, and we know based on her history that she will likely need a line the rest of her life. To our recollection no follow up appointment was made following this line placement. For some reason the external stay suture was left in.
As Becky continued to grow the exit site began growing granulation tissue, having redness, soreness and mild pain beginning around June of 2020 which she dealt with on her own as she was told this was “normal” and there wasn’t anything that could be done [see Figure 1]. The suture could have easily been removed at this time. On 10/14/21 the pain, discharge, and redness became so bad that we went to the ER [emergency room] with concern of a tunnel infection after speaking with the GI [gastrointestinal] team.
Blood cultures were drawn, and we were told there was nothing that could be done other than taking ibuprofen or Tylenol. She is unable to take ibuprofen due to GI bleeding and we try to avoid Tylenol because she has some TPN associated liver issues. Becky was told that she should not be experiencing any pain because sutures, central lines, and granulation tissue “do not cause pain.”
We were scheduled with the surgery clinic on 10/19/21 where we asked that the suture be removed because it seemed to us to be the main cause of the granulation tissue and were told suture could

32 THE E-NEWS PUBLICATION OF THE ASSOCIATION FOR VASCULAR ACCESS
Figure 1
not be removed because it “was holding the line in”. We had never been told this before and assumed that something had changed or was different with this line than every other previous line she had. In other words, we trusted and believed what we were told. Again, we were told there was nothing that could be done and that she should not be in pain from her line, the sutures, or the granulation tissue. The suture could have been removed at this time.
As Becky continued to grow in height and began to develop breast tissue, her skin and the granulation tissue grew over these sutures and her discomfort, pain, oozing, redness, etc. continued to worsen. Every time we would do a dressing change it would cause her immense pain to move or even touch the line. It was difficult to keep a dressing on for more than a couple days. This is a child who has dealt with intestinal and abdominal pain her entire life. Every time she rode her horse, she would complain that her right shoulder hurt. This got worse and worse until January of 2023 when we decided that we could no longer continue to “just deal with it” [see Figure 2].
We saw another physician on Jan 5th, 2023, and her comment NOW was that the suture “wasn’t doing anything but causing the granulation tissue to grow”. What???? At this point the suture was now underneath skin and granulation tissue and is not accessible without treating it with silver nitrate which was done that day in clinic. This was very painful and Becky was in tears, extreme pain and highly anxious. We continued to painfully treat the granulation tissue at home every 7 days from Jan 11, to Feb 19. Each treatment was painful and her chest, arm, shoulder were uncomfortable and painful to the point where she missed school because she could not comfortably “move her arm”. It was torture. After treating it with silver nitrate the granulation tissue would grow back within hours to days.

On Feb 22, 2023, a physician attempted to remove the suture in the clinic. Becky was in so much pain and crying that there was absolutely no way the removal could be done. On March 7, 2023, we were forced to visit the ED again because Becky woke in so much pain that she could not move her arm. Again, she missed school and both of us missed work. Once again, we were told there was nothing that could be done to help her. So, we sought a second opinion from another physician. After a long consultation and the doctor saying “I do not want to hurt you” a decision was made to put Becky under general anesthesia to remove this suture in an attempt to save the line. This procedure was done on April 13th. This was the first opening in the OR. She was very sore and uncomfortable for about a week following and some of the pain had subsided, but it was not completely resolved. However, within 10 days we saw another piece of blue suture poking through the newly grown granulation tissue. After this we spoke with the same surgeon and decided to attempt to remove the remaining suture by placing her under anesthesia again on June 15, 2023. Again, we had to wait for an opening in the OR. The surgeon’s comment in the post op consultation room was something like “I don’t know who put that line in, but I would have never used that much suture or left it in like that.” She commented that it was on so tight that it was “strangling the line” [see Figure 3]. We can still see an indentation in it. The very next day Becky could tell that she was better.

33 SEPTEMBER 2023 | VOLUME X | ISSUE 3
Figure 2
3
Figure
The surgeon was so concerned that her pain would be much more intense following the second procedure because she had to dig so much further up the line into her skin to retrieve the suture that she gave her oxycodone and had to put several dissolvable sutures to hold the dug-out skin together. However, Becky did not require any pain medication whatsoever. She was up and moving around and moving her arm more freely than she had in two years. It is painfully obvious that the suture was causing the issue all along just as we suspected. For two years this child has been gaslit by being told that granulation tissue does not hurt, and sutures do not hurt. We have the sutures in a specimen jar, and they are hard as a rock and stiff like barbed wire. There is no doubt in anyone’s mind that was causing the problem. She has had a central line her entire life that was never painful until this one.
We were able to attend the Oley Foundation conference in St Louis in June 27 – 30 in St Louis. This is a conference for patients, caregivers, clinicians, and suppliers of patients on enteral and parenteral nutrition. Dr. David Mercer spoke at this meeting on central line access and complications. Dr. Mercer is a multi-visceral transplant surgeon at Nebraska Medical Center and has done more intestinal transplants than anyone in the world. However, one of his main goals is to keep patients like Becky from needing an intestinal transplant by maintaining CVL access and limiting complications from TPN (liver failure and sepsis). I asked him during the Q&A as to how long the external “stay” suture should remain in following CVL placement. His response was that once the cuff has grown in, it takes approximately 3-6 weeks to be safe but one week would probably be ok [none of these recommendations follow the instructions for use for sutures]. The internal cuff is what “holds the line in”, not the external suture. There is a point at which the external “stay” suture is simply a foreign object causing more issues than it was ever meant to accommodate. If you would like to view the video, and hear his answers to my question it is available here. Day 1 Welcome - Bing video at approximately 2:13:30. This can be found on You Tube: The Oley Foundation Channel search Day One Welcome. Consider watching the entire video as you will learn so much from the patient’s perspective and from Dr. Mercer’s experience and expertise.
It is our plea and hope that in the future when you are caring for a patient who require long term vascular access through a central line that you will change your post op protocol such that they have a post op appointment within 6 weeks where the suture can be removed beyond its labeled use and/or the child grows skin and breast tissue over it or before it becomes so aggravating to the skin that granulation tissue takes over. This has caused Becky to miss school, miss social events, miss horse shows and practice, and a significant amount of pain and added anxiety to her already extremely difficult health situation. She has had to be placed under anesthesia twice, which is terrible for her GI motility, and has cost our insurance thousands of dollars. As her parents we have missed numerous days of productivity at our jobs, costing us financially, but more so countless sleepless nights and parental guilt that we did not advocate for her as much as we should have or could have. [We hope those who read this letter consider life from the patient’s point of view, advocate for them, and advance the science of vascular access for everyone.]
Most Sincerely,
Tonya and Markum [Becky’s Awesome Parents]
34 THE E-NEWS PUBLICATION OF THE ASSOCIATION FOR VASCULAR ACCESS





35 SEPTEMBER 2023 | VOLUME X | ISSUE 3 Educational Offerings from AVA Learn more at www.avainfo.org I Save That Podcast • Streaming on Spotif y, SoundCloud, iTunes, Stitcher, Google Play Music, iHeart Radio, Pandora, Amazon Music Intravascular Quarterly (IQ) • Published quarterly • E-newsletter sent to AVA members AVA Resource Guide for Vascular Access • Prepare for the VA-BC™ exam, as well as ser ve as a resource throughout professional practice AVA Academy • Continuing Education courses ALL available on demand • Procedural courses, webinars, scientific meeting sessions, etc. Journal of the Association for Vascular Access • Published quarterly • Approximately 3,000 subscribers Available anywhere you get your podcasts ACADEMY
36 THE E-NEWS PUBLICATION OF THE ASSOCIATION FOR VASCULAR ACCESS
DESIGNER SCRUBS FOR HEALTHCARE PROFESSIONALS AND SPECIALIZED GARMENTS DESIGNED FOR PATIENTS WITH SPECIFIC MAINTENANCE NEEDS FOR THEIR VASCULAR ACCESS.


The code entitles you to a 10% discount on designer scrubs as well as all Care+Wear products including PICC Line Covers, port access tops, and outfits for premature infants who are being cared for in the NICU.
Remember to use AVA10 to receive your discount.
1,50000

37 SEPTEMBER 2023 | VOLUME X | ISSUE 3
AVA10
Special discount just for AVA
Learn more here.
has partnered with Care+Wear to launch a joint discount program
AVA
Copyright 2023 Association for Vascular Access. All rights reserved.
Disclaimer: AVA (Association for Vascular Access) is a professional organization of vascular access professionals dedicated to improving vascular access practice and patient outcomes through education and other means. AVA publishes this periodic electronic newsletter for our membership and other interested parties for information purposes only. AVA distributes this electronic newsletter with the understanding that AVA is not engaged in rendering medical or professional service through the distribution of the IQ publication. AVA is not giving advice and does not subscribe to guarantee the accuracy or efficacy of the information provided. Privacy Policy and Unsubscribe Information -AVA maintains strict rules of confidence with regards to your email address and all other personal contact information. We will not, under any circumstances, sell, transfer, or provide your email address to any third party for any reason. Email lists are compiled on an opt-in basis by AVA for the sole purpose of distributing the IQ newsletter. AVA does not condone or participate in the distribution of unsolicited email. If you feel that you have received an email transmission from AVA in error, please contact AVA at and ask to be removed from the list. All removal requests are addressed promptly.

38 THE E-NEWS PUBLICATION OF THE ASSOCIATION FOR VASCULAR ACCESS































































 MICHAEL VOLKOV, RN, VA-BC, CNPI, VALLEY CHILDREN’S HEALTHCARE, MADERA, CA
MICHAEL VOLKOV, RN, VA-BC, CNPI, VALLEY CHILDREN’S HEALTHCARE, MADERA, CA