Better Breathing
UNDERSTANDING
celebrating Women in respiratory science

dysfunctional
and be in to win 1 of 5 $50 Prezzy Cards
Air quality in New Zealand
We speak to expert Dr Guy Coulson to find out more about New Zealand’s air quality and how we can improve the air in our homes.

Autumn 2023
SURVEY:
LEARN
breathing ASTHMA IN NZ
HELP US
MORE
Zoe Manderson explains how dysfunctional breathing affects breathlessness SPIROMETRY
MEET THE WINNERS FROM THE NEW ZEALAND RESPIRATORY ACHIEVERS' AWARDS
Meet two of the inspirational winners from the Respiratory Achievers' Awards.
Pg 6. Meet some of the Kiwi women leading the way in respiratory health .
Our Team In this issue...
Chief Executive
Letitia Harding
Research and Education Manager
Joanna Turner
Office and Donor Appeal Administrator
Dunia Cullingford
Grants and Fundraising Manager
Pam Francombe
PR and Communications Advisor
Charlotte Lee-Smith
Marketing & Communications Advisor
Sam Treseder
Māori Community Liason
Sharon Pihema
Corporate Sponsorship and Engagement Advisor

Amy-Rose Todd
Medical Director
Dr James Fingleton, BM, PhD, FRACP
Chief Cultural Advisor – Māori Sir John Clarke, KNZM, CNZM
Ground Floor, 85 The Terrace, Wellington 6011 PO Box 1459, Wellington 6140
04 499 4592
asthmafoundation.org.nz asthmaandrespiratoryfoundation asthmafndation
asthmaandrespiratoryfoundation
4. Community News

We find out more about the Wellington Sing Your Lungs Out choir, a community singing group for those with respiratory conditions, where enthusiasm matters more than talent, and we share an opportunity to help with child asthma research.
5. Air quality in New Zealand
We speak to expert Dr Guy Coulson to find out more about New Zealand’s air quality and how we can improve the air in our homes.


6. Women in Respiratory Science
To mark International Women in Science Day, we put the spotlight on four Kiwi women working in respiratory health and technology.
8. My breathing story
We meet two of the winners from our Respiratory Achievers’ Awards: Kayla White, the winner of the Cody Forbes Award for Courage, and Ed Lee who won the ‘Other Conditions’ category.


9. Respiratory Achievers’ Awards
Check out the photos from the Foundation’s recent Respiratory Achievers’ Awards held in Wellington.
You can also read this magazine online Just head to issuu.com /betterbreathing
10. Respiratory News
Find out the latest in respiratory news from New Zealand and around the world and learn some helpful tips for dealing with mould after flood events.
12. Dysfunctional Breathing
Respiratory physiotherapist Zoe Manderson explains how dysfunctional breathing affects breathlessness.
13. Understanding spirometry
We answer your questions about spirometry; a breathing test used to diagnose some respiratory conditions including COPD.
14. Asthma Societies
Find out more about Breathe Hawke's Bay and get the details of your local asthma society or support group.
... Leave a legacy for future generations

A gift in your will to the Foundation goes towards educating Kiwis and producing resources to reduce the number of unnecessary hospitalisations.

Thank you to Pub Charity Ltd. for their continued support of the Foundation, allowing us to provide Better Breathing magazine free of charge to the respiratory and healthcare communities.

Pg5.FindoutaboutairqualityinNew Zealand:isitasgoodaswethink?
ISSN 2703-4127 Thank you to our Friends of the Foundation for supporting our ongoing initiatives. Please recycle this material after use. This material has been printed with vegetable oil-based/mineral-free inks. The paper used comes from sustainable forests.
Contact us for more information: 04 499 4592
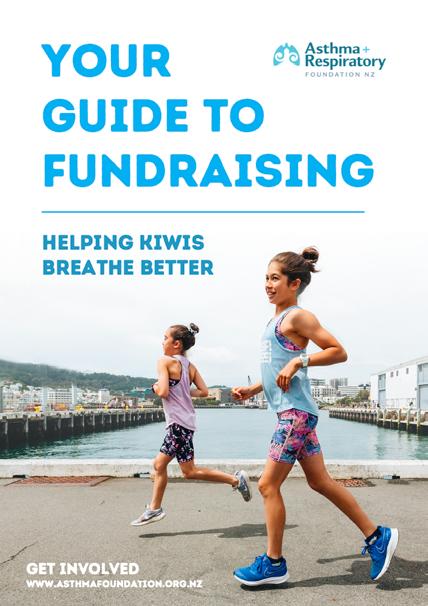
Cover photo: Ed Lee receives his Respiratory Achiever Award from Foundation Chief Cultural Advisor Sir John Clarke.
Letitia’s Message
of vaping products; extending safety requirements for disposable vaping products and restricting where specialist vape stores can be located, we think the rules need to go much further to protect the lung health of our young people.
 Kia ora koutou,
Kia ora koutou,
It has been a challenging start to 2023 for many of our respiratory community in the North Island due to the devastating effects of Cyclones Gabrielle and Hale. Dealing with a respiratory condition in emergency situations is especially stressful and can certainly be made worse when managing the clean-up phase. Our hearts go out to all those affected by these events.
When living through challenging times, it is easy to forget to take care of yourself. Please remember to look after respiratory health. Keep taking your regular medications, and if you can access your asthma action plans, please follow these. Take extra precautions during the clean-up phase when dealing with mould and contaminated silt. We have some useful tips on removing mould on page 11.
A bright spot over the last two months, was the Foundation’s Respiratory Achievers’ Awards held in late February. The awards are always a highlight for our team as we get to celebrate the achievements of outstanding individuals who have had to work harder than most to achieve their goals. We will be sharing our winners’ stories in the next few issues of this magazine, you can read the first of these on page 8.
We were incredibly lucky to receive support from our Friends of the Foundation Platinum Sponsor G.J. Gardner Homes which allowed us to host the 2023 Awards. I would encourage you to check out photos from this event on page 9.

I was also pleased at the start of this year to see new proposals from the Government aiming to tighten up vaping rules. This is something that the Foundation has been strongly advocating for and we welcomed the opportunity to provide feedback.
While we support the Government’s suggestions: restricting flavour names
Youth vaping continues at incredibly high levels, particularly among rangatahi. The last Action on Smoking and Health (ASH) Year 10 Survey found that 40% of Māori girls are vaping regularly. In our submission to Government, we have asked for further restrictions including; banning disposal vape products, reducing the maximum nicotine levels in all vapes to 20 mg/ml, and significantly reducing the current numbers of specialist vape retailers.
The team was pleased to welcome an intern, Katie Lowles, to the Foundation’s office for the first three months of this year. Katie is a PhD student at the University of Manchester working in immunology. She is helping us to update some of our asthma and COPD resources as part of her work experience, and we look forward to sharing some of her work later in the year.

Finally, with the colder seasons approaching it is time to think about taking action to protect your respiratory health. A useful concept we all learnt from COVID-19, is the idea of ‘flattening the curve’, or taking preventative measures to stop overwhelming our busy health system. It’s all commonsense stuff: staying at home when you are unwell, wearing masks on public transport or in crowded public spaces and being vigilant about handwashing. It is also important to keep up to date with your immunisations against the flu and COVID-19. People with respiratory conditions are prioritised for the flu vaccine, and those eligible can receive the vaccine for free. Flu vaccines will be available from 1 April 2023.
I hope you enjoy this issue of Better Breathing. We welcome your feedback on the magazine, or on any other aspect of our work, please feel to get in touch (our details are on the facing page),
Noho ora mai
Letitia Harding Chief Executive

3 Better Breathing
The Foundation is continuing to push for greater regulation of vaping in New Zealand.
Intern Katie Lowles has been writing new resources for The Foundation.
Letitia and Amy-Rose Todd with Olly Sundstrum of G.J. Gardner Homes, supporter of the Respiratory Achievers' Awards 2023.
Community News


SING YOUR LUNGS OUT WELLINGTON
You don’t need to be a singer to join the Wellington Sing Your Lungs Out choir. In fact, organiser Robyn Lange says most members would claim they can’t sing. “But it doesn’t matter at all, as together we make a good sound, and we have a fun time doing it.”
The choir was set up eight years ago, following a research project into the benefits of community singing for people with lung conditions, like COPD. The findings showed that group singing boosted the participants’ quality of life and improved their confidence, as well as helping with lung clearance and breathing control.
“For many people, that diagnosis of COPD can be life-shattering. They feel like they can’t do anything anymore and they are embarrassed by symptoms like coughing or breathlessness,” explains Robyn. “But at Sing Your Lungs Out, everyone understands those symptoms. You can cough away without judgement. It’s really an amazing group of people who are so welcoming and supportive of each other.”
The group meets weekly on Tuesday mornings at All Saints Church in Hataitai. The choir practice is preceded by an optional exercise group run by Robyn, who is a respiratory
physiotherapist, followed by a shared morning tea and then warm-up breathing exercises. The singing practice is led by a highly experienced singing teacher, who helps adapt the music to suit the needs of the participants. The song choices are varied, from old favourites to more modern tunes, and everyone gets to have a say.
Currently there are 23 members, with some having been there since the choir was first established. “There is a real mix of people and backgrounds – including some who never imagined they’d join a choir, yet they really love it,” says Robyn. The organisers are conscious of providing a safe environment, and the practice room is a large, well-ventilated space that is warm in winter.
The choir performs several short concerts throughout the year, with one of the highlights being an annual Christmas Carol performance at Wellington Hospital. Membership is free, and open to anyone with respiratory conditions.
Anyone who is interested in trying it out can drop into a practice session at 10.30, Tuesday at All Saints Church in Hataitai. For those based in Porirua, the Porirua Sing Your Lungs Out choir is held every Thursday at 11.30, at Mungavin Hall. Contact details are on the Foundation’s website: https://www.asthmafoundation. org.nz/about-us/supportgroups
Asthma in New Zealand Survey 2023
HELP NEEDED FOR CHILD ASTHMA RESEARCH
Can you help New Zealand researchers find out which inhalers are better at preventing asthma attacks in children?
Researchers from the Medical Research Institute of New Zealand (MRINZ) are looking for children to help with two important studies comparing the effectiveness of different asthma medications. For the first study, the researchers are looking for children between five to 15 years old who are currently only using a reliever inhaler/puffer (eg. Ventolin, Respigen or Bricanyl) to manage their asthma. In the second study, the researchers are seeking children aged five to 11 years old who are using a preventer inhaler (eg. Flixotide, Seretide or Pulmicort) and a reliever inhaler (eg. Respigen, Ventolin or Bricanyl). For more information or to enrol your child in the study go to: https://www.asthmafoundation.org.nz/getinvolved/help-with-research
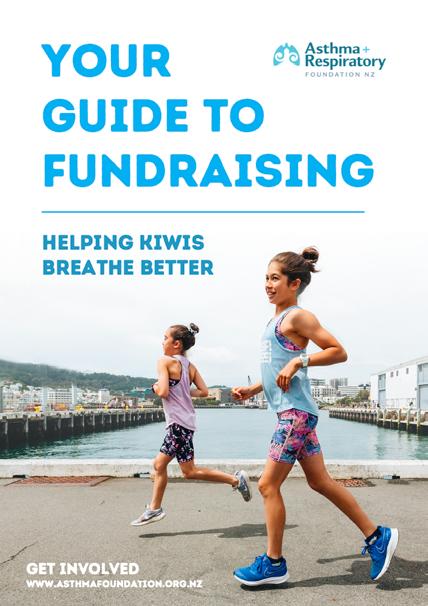
FUNDRAISING FOR THE FOUNDATION
Did you know that the Foundation receives no Government funding?
All our funding is provided by sponsors, community grant organisations and generous supporters like you. We have created a fundraising toolkit for our amazing family of supporters, with ideas and advice on how to run a fundraising event. Our team is always happy to support your efforts. You can find the new toolkit here: https://www.asthmafoundation.org.nz/get-involved
Ahead of World Asthma Day, the Foundation wants to find out more about Kiwis' experiences with asthma. We've created a short survey that you can fill out either for yourself or on behalf of a child with asthma. As a thank you for your time, survey respondents can choose to go into the draw to win one of five $50 Prezzy cards. You can access survey by scanning the QR code above.

4 Better Breathing
Be in to win 1 of 5 $50 Prezzy Cards! SCAN BELOW TO ACCESS THE SURVEY
Air quality in New Zealand –should we be worried?
Air Pollution in NZ
The HAPINZ 3.0 (Health and Air Pollution in NZ) study estimated that human-made air pollution was responsible for 13,229 cases of childhood asthma and 845 hospitalisations of children with asthma. It also estimated that air pollution causes 1.75 million restricted activity days for Kiwis, when people were prevented from regular activities due to air quality.
The main causes of air pollution are nitrogen dioxide from motor vehicles and fine particulate matter (PM2.5), tiny particles of pollution that come from domestic wood and coal fires, cars and windblown dust. The study showed that the areas worst affected were Auckland and Christchurch, followed by Dunedin, Tauranga and Hamilton.

Poorair quality has long been known to have a significant impact on people living with respiratory conditions. Gases and particles in the air from polluting sources like cars, coal and wood fires can get into the lungs and worsen existing conditions like asthma and COPD.
A recent New Zealand study found that many Kiwis are being exposed to air pollution, and that is causing serious health impacts especially for children with asthma. We spoke to Guy Coulson, an air quality scientist at the National Institute of Water and Air (NIWA) to find out more about air quality in New Zealand and the work of the Indoor Air Quality Research Centre NZ.
Do New Zealanders need to be worried about air quality?
By international standards the air quality in New Zealand is pretty good. But there are pockets of poor air quality, so if you live or work or travel around those pockets you are more likely to be affected. Those pockets include areas with a lot of wood-burning fires in winter and city centres where there is a lot of pollution, usually from traffic. In big cities, you can find pollution canyons, where pollutants gather in corridors between multi-storey buildings.
Should we be concerned about indoor air quality also?
There’s been a belief that indoor air was cleaner than outdoor air, but that’s not always true. Outdoor pollutants can come inside –things like traffic fumes, smoke etc – but there are also indoor pollutants. Mould is by far the biggest threat to indoor air quality, but there are also pollutants that come from some cleaning products and some materials or furnishings. But the problem is we don’t really know how much of a problem indoor air pollution is, because there is very little research on it.
Is that why the Indoor Air Quality Research Centre NZ was set up?
Yes, the Centre is a collection of half a dozen or more groups from around the country that all have an interest in air quality from a health or building perspective. There is growing interest in research on this topic, particularly as a result of COVID-19, and we want to coordinate our work.
What does the Centre do?
We advised the Ministry of Education after the last lockdown on how to best ventilate classrooms to minimise the spread of COVID in schools. We have recently received funding to look at how to best ventilate other environments with vulnerable populations like aged care facilities to reduce the spread of disease.
What is the best way to improve indoor air quality?
Opening windows is remarkably effective, unless you live in an area with a lot of wood-burning fires in the middle of winter. In that case, you might want to consider using a ventilation system or an air cleaner with a HEPA filter. Even during winter, opening all the windows and doors for a 10-minute blast to flush out all of the dust mites and stale air will make a big difference to air quality. Also, you can improve your source of heating by changing from woodburning to electric heating. It’s important to note that heat pumps do not ventilate rooms, but heat or cool existing air within a room.
How do we improve outdoor air quality?
It would be great if New Zealand could set a target for zero air pollution to go along with a zero carbon emissions target. It makes sense to tie those two goals together, as the sources responsible for carbon emissions are also responsible for a lot of our air pollution.
5 Better Breathing
Dr Amy Chan Senior Research Fellow, School of Pharmacy, University of Auckland

Imagine a future where you wake in the morning and your smart phone beeps with your daily asthma forecast. Senior research fellow Dr Amy Chan is working towards making that a reality.
Amy, who is based at the School of Pharmacy at the University of Auckland, is currently leading a study to develop an asthma attack prediction tool. For the first phase of her study, she will recruit 300 New Zealanders with asthma and then gather a range of data using a suite of technologies including FitBits, Smart Inhalers and Bluetooth peak flow meters. This data will be analysed to understand the most important factors in predicting an asthma attack and then developed into an accessible tool.
Cheryl Davies Senior Research, University of Otago

After more than two decades of involvement with research, Cheryl Davies still sees herself as an ‘emerging’ researcher. “I’m still on a learning journey and as a researcher that journey never really ends,” she says. Cheryl is
Amy’s interest in better predicting and managing asthma is driven by her own experiences. “I was the kid that couldn’t play with my cousins, because I had to be on a nebuliser. I was always on the sidelines on athletics day,” she remembers. “From a young age I wanted to cure the world of asthma.”
Inspired by the hospital pharmacists she saw during trips to pick up specialist medication, Amy trained to be a clinical pharmacist. Her desire to understand more about asthma, then led into research and a PhD involving digital technology and asthma: two interests that have shaped her research career. “People sometimes question the value of technology in managing asthma. But my re sponse is that technology allows us to detect changes in our bodies that may be too small for a human to notice but could be important indicators of an oncoming asthma attack,” Amy explains. “If we can detect these changes more quickly, we have a better chance of
managing asthma.” Technology has also been shown to greatly improve how people use their medications, with smart inhalers that send out reminders particularly effective in encouraging regular use.
Amy remains motivated by her childhood dream to cure asthma, but now she sees this as a joint effort. “It's exciting to use my skills to find another piece in the puzzle, and to hopefully make discoveries others can build on."
with the University of Otago. Her journey in respiratory research began many years ago. “I was asthmatic myself and two of my children had asthma. I was part of a community education group that really wanted to better understand and manage our asthma,” she explains.

Her group was involved in research for the Māori Asthma Review carried out in the early 1990s. A key finding from the review was that more Māori asthma services were needed providing services by Māori for Māori. “Our journey at Tu Kotahi began thanks to that review,” she says.
COPD, as well as wider issues affecting respiratory health like the impact of housing on health. The greatest rewards of her research career have been seeing the practical outcomes of her work. The findings of the Pukapuka Hauora Asthma guided how Māori health workers worked with whānau and tamariki with asthma. Early research on the benefits of insulation and heating contributed to the establishment of the Warmer Kiwi Homes programme, and subsidised programmes for heat pumps in homes.
Another career high has been seeing external researchers embrace mātauranga Māori and the growth of organisations, like Tu Kotahi, in undertaking their own research. “We realised quite early on that we needed a whānau ora approach that takes a broad view of whānau needs. We are not just working with individuals, but with the whole whānau.”
Since then, Cheryl has been involved in research projects covering a range of respiratory conditions: asthma, bronchiolitis and
Cheryl hopes to establish a kaupapa Māori research unit at the trust’s base at Kokiri Marae in Lower Hutt and continue to build the Māori health and research workforce.
6 Better Breathing
now
enrol
learn.asthmafoundation.org.nz
“I saw that we needed to have evidence of what was happening in our communities for change to happen and that piqued my interest in research.”
To celebrate international
Lucy Telfar-Barnard Senior Research Fellow, Department of Public Health, University
If you’ve ever wondered how we know that one in seven New Zealanders has a respiratory disease, then researcher Lucy Telfar-Barnard can give you the answer.

Lucy is a senior research fellow at the University of Otago’s Department of Public Health. She has been the lead author on the Foundation’s Impact of Respiratory Disease report since 2014. This report presents an important picture of the state of respiratory diseases like asthma, COPD and bronchiectasis in New Zealand, and how this is changing over time.
Lucy’s background is in epidemiology, the study of the spread of disease across populations. In simple terms, Lucy explains she can predict how likely you are to get a respiratory illness, but not diagnose if you actually have one.
She is motivated in her research by both a desire to make a difference to people’s health and by scientific curiosity. “I like to be presented with a puzzle and find an answer,” she explains. The last impact report, delivered in
2020, provided some potential answers to the longstanding question of how to reduce the rates of respiratory disease. “For many years, the trends in the report hadn’t changed much. But in that last report, the impact of COVID-19 protection measures drove a marked decrease in the rates of respiratory disease. It’s important that we learn from that experience and think about what practical, sustainable things we can continue to do to keep the rates of respiratory disease down,” she says.
Another lesson to take from COVID-19 is the concept of flattening the curve. “We need to apply this thinking to seasonal respiratory illnesses by taking early preventative measures to avoid overwhelming hospitals and GPs in winter,” she explains.
Lucy is currently investigating how New Zealand measures up to World Health Organisation guidelines on healthy homes. She is also preparing for the next update of Impact of Respiratory Disease in New Zealand report which is due out later this year.
Dervla Braem combines her love of science and engineering with practical creativity in her role as a Design and Development Engineer at technology company Dyson.

Dervla, who studied Mechatronics (electronics and mechanical engineering) at Canterbury University, now designs the next generation of vacuum cleaners, air purifiers and other home appliances for Dyson in the UK.
“I wanted to work on engineering products that people interact with. I love the maths and science side of engineering but wanted to combine it with a more creative and collaborative job,” she explains.
A typical day for Dervla involves designing and drawing new ideas and then heading to the lab where she works with motors, batteries and airflow technologies to bring her ideas to life.
Transferring ideas from drawings to the finished product is an exhaustive process, “The hardest part of the job is that it takes so many tweaks and different iterations of a product before it is right and something you have been working hard on may never become a finished product,” Dervla says. Despite this, being unafraid of failure is important in her role: “We are encouraged to think outside the box and design something unique to see what happens when we test it. Even if it’s not quite right, you end up learn ing something and pushing the project along.”
Dervla is passionate about creating equal opportunities for women in engineering: “We need to create a culture where women are confident to share ideas, and everyone has a voice – even the quietest people.
A women’s perspective is essential to engineering; if we want women to enjoy using our products, we need to have their insights into what is important in a product.”
Finally, Dervla shares some advice for overcoming imposter syndrome in male-dominated workplaces: “Finding a mentor who understands how you feel and has had similar experiences at work can be really beneficial for improving confidence. You need to remember that you are there for a reason and are capable of making a positive impact.”
7 Better Breathing
of Otago
Dervla Braem Design & Development Engineer, Dyson
Women In Science Day was Proudly supported by our Friend of the Foundation 7 Better Breathing
Women in Science Day, the Foundation spoke with four inspiring Kiwi women who are leading their fields in respiratory science.
Meet the winners: Kayla White and Ed Lee
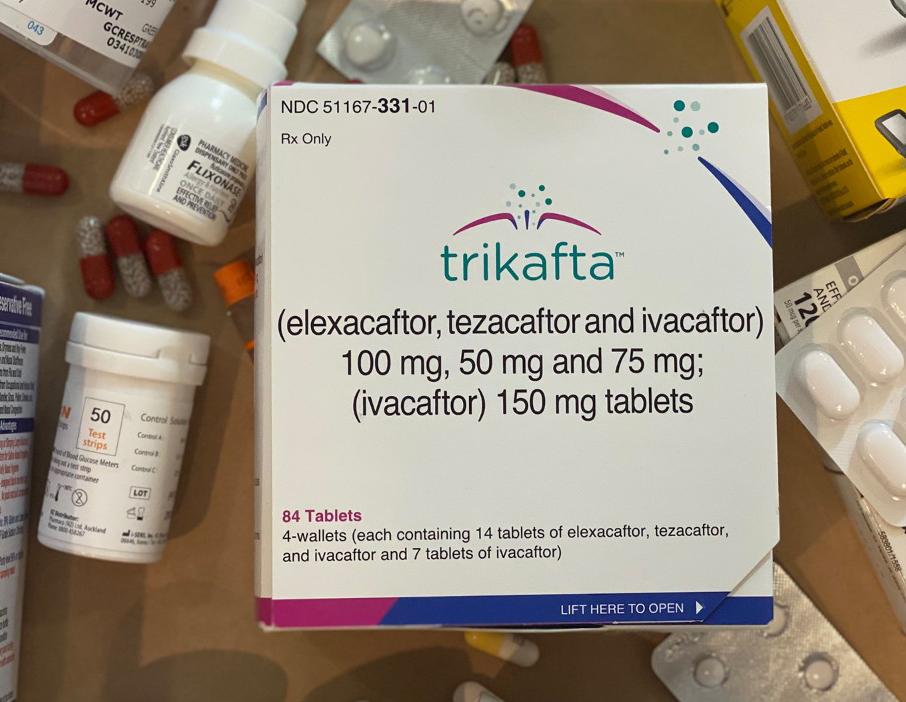
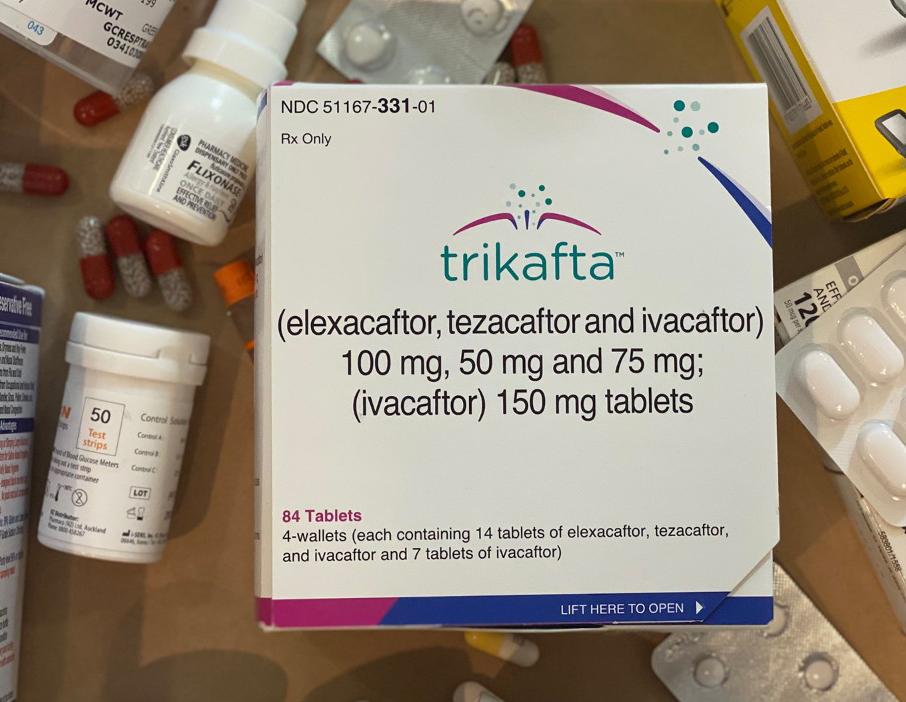
Wellingtonian Ed Lee received the 2023 Respiratory Achiever Award for ‘other conditions’ for his tireless advocacy on behalf of people living with Cystic Fibrosis (CF).


At 40 years old, Ed is one of the oldest people in New Zealand with CF. This condition causes thick and sticky mucus to build up in the lungs, making it hard to breathe and increasing the likelihood of infections. Each lung infection causes further lung damage, resulting in poor lung function. Edward’s lung function was 28% at its lowest.
CF took a huge toll on Edward’s quality of life, he spent a lot of time in hospital and was constantly on antibiotics, which damaged his liver and renal function.
The predominant treatment for CF in New Zealand is inhaling saltwater twice a day to remove mucus from the lungs. However, after hearing about Trikafta, which is a breakthrough treatment available in most E.U. countries, the UK and the US, Edward knew it was what he needed to get healthy and live a normal life. “Trikafta wasn't funded in New Zealand then, but I was in a fortunate and privileged position to be able to go to the US and pay for a Trikafta prescription,” Edward explains.
“It really is a miracle drug. I returned to the hospital after a couple of months of taking Trikafta and the radiologist thought something was wrong with the x-ray because she couldn’t believe the improvement in my lungs!”
Once Ed had experienced how transformative Trikafta had been for himself, he knew he wanted everyone with CF in New Zealand to access this medication. He had built connections with the wider CF community using social media and with the support of this community, Ed began lobbying for Trikafta to be funded in New Zealand. It was a long slog; talking to health authorities, politicians and the media to build their case. But this hard work paid off, when Pharmac announced this month that Trikafta was approved for use in New Zealand from April 2023.
Trikafta will be available for those aged six and above: “My hope is that these young children with CF will be able to take Trikafta before any permanent lung damage occurs and they can live most of their lives without feeling like they have a serious illness”.
Life has thrown some tough challenges at Kayla White, but the 13-year old’s determination and spirit have seen her fight to live the life she wants. Her bravery was awarded, when she received the Cody Forbes Award for Courage at the national Respiratory Achievers’ Awards, held by the Asthma and Respiratory Foundation.
The award ceremony held in Wellington, fell on Kayla 13th birthday; a milestone that doctor’s thought she was unlikely to reach. “She’s always been a fighter. From the very earliest days after she was born, she had such a strong will to live,” her mum Angela recalls.
Kayla was born with hydrops fetalis, a serious condition with a low survival rate and the cause of permanent damage to her lungs. She has 70% lung function and a range of respiratory conditions that make breathing very difficult. She was told by doctors at a young age that she wouldn’t be able to do anything physical.
“When Kayla is told she can’t do something, she will go out of her way to prove them wrong. She has absolutely defied those predictions,” Angela says. Kayla is involved in a semi-competitive cheerleading team, a marching team, Girl Guides, her school’s Kapa Haka team and choir. She runs in the cross country every year, takes part in competitive swimming and was in her school’s competitive Maths team. With her marching team she competed at a national competition.
“She will always give it a go, even if she is slower than everyone else or needs to run the cross country with her inhaler in her hand. She gets breathless but her pure determination gets her through,” says Angela.
Both Kayla and Angela admit there have been some very hard times. “She has been in hospital too many times to count and up to Starship numerous times. It’s hard on her. She had to miss a lot of school during COVID-19, because it was just too risky to go,” explains Angela.
Kayla is humble about her attitude and achievements. “It’s just normal to me. I want to do those things, so I keep going,” she explains. Angela is immensely proud of Kayla’s courage and willingness to give things a go. “She wasn’t meant to live, but she loves life and while others are sitting on the sidelines, she’s out there doing it.”
8 Better Breathing
Winners and finalists from the Respiratory Achievers' Awards: from left to right: Kayla White, Liam Dulver, Maryana Garcia, Mohammed Umair Khan, Ann Wheat, Charleigh Skelton-Morris, Ed Lee, Gary Syme, Oliver Ayton, Claire Richards, Taumata O Te Ra Lowe, Letitia Harding, Lady Kathy Clarke,


Oh, what a night! The Foundation celebrated the winners and finalists of our Respiratory Achievers’ Awards at a very special ceremony in Wellington, in late February. The winners were: Liam Dulver (Asthma 5 – 12 years), Mohammed Umair Khan (Asthma 13 – 18 years), Taumata O Te Rā Lowe (Adult Asthma), Gary Syme (COPD), Edward Lee (Other Conditions), Kayla White (Cody Forbes Award for Courage), Maryana Garcia (Media Awareness), Claire Richards (Respiratory Educator), Ann Wheat (Lifetime Service).



9 Better Breathing
Sir John Clarke.
Teen Asthma Award winner Mohammed Umair Khan with his father Muhammed Tabrez Khan. Ultra-marathon runner Nick Ashill with his daughter Abi.
Child Asthma Award winner Liam Dulver accepts his award from Sir John Clarke. Foundation Research & Education Manager Joanna Turner is in the background.
Adult Asthma Award winner Taumata O Te Ra Lowe (left) with partner Keena Richmond, and Other Conditions Award winner Ed Lee with his partner Kalyn Ponti.
Prepare for flu season

More Kiwis will be eligible for free flu vaccines in the lead up to winter 2023. The Government is making vaccines free for children aged six months to 12 years and Māori and Pacific people aged 55 to 64 years from 1 April 2023. People with long-term respiratory conditions like asthma, and those over the age of 65 years will continue to be eligible for free vaccines. “With another difficult winter season expected, and our health system still dealing with impact of COVID-19, we would encourage everyone with a respiratory condition to get the annual flu vaccine. It is an important way to look after your respiratory health over winter,” says Foundation Chief Executive Letitia Harding.
COVID vaccine for pre-schoolers
Pre-schoolers with complex health conditions, including chronic lung conditions such as bronchiectasis and poorlycontrolled asthma, can now access a new version of the children’s COVID-19 vaccine. This vaccine contains a lower dose of mRNA, formulated for this age group. It is a threedose course, with the second dose delivered three weeks after the first, and the final dose at least eight weeks after the second. Parents of eligible children can book the vaccine by calling Healthline on 0800 28 29 26.
New smoking laws and proposed vaping rules
The Foundation welcomed the passing of the Smokefree Environments and Regulated Products (Smoked Tobacco) Amendment Bill last year. This law introduces three major changes to protect Kiwis from the harms of tobacco. It bans the sale of tobacco to anyone born on or after 1 January 2009, significantly reduces the number of retailers selling tobacco
and over time will significantly reduce the nicotine content in tobacco products.
In January, the Government asked for feedback on how the new smokefree laws will be implemented and on new proposals to restrict vaping. The vaping proposals included new safety rules for disposable vapes, rules on how vapes are marketed to young people and where specialist vape retailers can be located.

The Foundation sees these proposals as a good start, but in our submission to Government we have asked them to do more. We want to see the Government reduce the nicotine content in vapes to a maximum level of 20 mg/ml (down from 50 mg/ ml), dramatically reduce the number of vaping retailers in New Zealand and ban disposable vapes. You can read our submission here: https:// www.asthmafoundation.org. nz/stories/have-your-say-onvaping
ASTHMA EMERGENCY KITS TO THOSE IN NEED

The Foundation has supplied two hundred asthma emergency kits to communities in need since the start of the year. One hundred kits, along with N95 safety masks and additional schools resources were sent to Gisborne to be distributed as needed to community organisations and schools following the devastation of Cyclone Gabrielle.
A further 100 kits were sent to decile one schools across New Zealand to provide vital health resources to coincide with the peak risk period for child asthma, weeks three and four of term one. These donations were made possible with funding from the N.H. Taylor Charitable Trust, the Lottery Grants Board and Te Taura Whiri i te Reo Māori.
10 Better Breathing
Respiratory News
TIPS FOR DEALING WITH MOULD
Recent devastating flooding events in the North Island means that mould is likely to be an even bigger problem for Kiwi homes in the coming colder months.
Mould is a common asthma trigger and recent local research has found that it can cause asthma to develop in children. Mould grows in damp, humid conditions and often thrives following flooding. In the clean-up phase after flooding, it is important to remove mould as quickly and safely as possible after drying out your home.
The Foundation recommends that people with respiratory conditions, who are sensitive to mould, avoid removing mould themselves, or being present when mould is being removed. If this isn’t possible, then we advise wearing a respirator or a properly fitted face mask and rubber gloves when removing mould. Fabric face masks will not protect against mould spores.
Be cautious about using bleach and other strong chemicals to remove mould, as the fumes can also trigger asthma. Either use diluted bleach, milder household detergents or a mix of vinegar and water (at a 80/20 ratio) to clean up mould. Avoid using dry brushes to remove mould as they can release more mould spores into the air.
To prevent mould from returning, be sure to keep your home well-ventilated either by using extractor fans, air conditioners or by regularly opening windows. Keep your furniture slightly pulled out from the wall so that air can circulate, preventing mould growth. Remember to wipe condensation from your windows and use a dehumidifier if you have one.
Life-extending CF drug funded
In March, Cystic Fibrosis advocates were thrilled by Pharmac’s announcement that it would fund the life-extending medication Trikafta. This decision follows years of advocacy from Cystic Fibrosis New Zealand and people living with CF. Trikafta has been shown to give people with CF, another 27 years of full health. Trikafta will be available from 1 April 2023 to people with CF, aged six and older, who meet certain criteria.
Epipens funded
Kiwis with serious allergies got some great news before Christmas when Pharmac announced it would fund Epipens from 1 February 2023. Epipens will be available to anyone who has experienced severe anaphylaxis or who is at ‘significant risk’. You can apply for funded Epipens through your GP. It is expected that 12,000 Kiwis with allergies will be eligible in the first year of funding, increasing to 17,000 after five years.
GAS STOVES AND ASTHMA
How bad are gas stoves for people with asthma? This issue has been debated recently in international media after American research claimed that one in eight children develop asthma from pollution produced by gas hobs. Similar research from Asthma Australia estimates gas stoves are responsible for 12% of childhood asthma.
When gas burns it can produce air pollutants like nitrogen dioxide, carbon monoxide, formaldehyde and fine particulate matter. These pollutants worsen air quality and can trigger asthma flare-ups, as well as contributing to the development of asthma.
New Zealand does not have statistics on how much gas stoves contribute to asthma, but there is no doubt using unflued gas stoves or heaters impacts Kiwis’ respiratory health, says Otago University senior researcher Lucy Telfar-Barnard. The risk is particularly high when unflued gas appliances are used in small spaces with no ventilation as air pollutants can build up to high levels.

“If your child has asthma, and you have an unflued gas appliance, I would definitely recommend exchanging them for flued or electric alternatives and I would certainly encourage people to use extractor fans,” Lucy advises.
American research: https://www.mdpi.com/1660-4601/20/1/75
Asthma Australia: https://asthma.org.au/about-us/media/new-report-goes-inside-australian-homes/
11 Better Breathing
Better Breathing 11
DYSFUNCTIONAL BREATHING
INFORMATION FROM RESPIRATORY PHYSIOTHERAPIST ZOE MANDERSON

People with lung conditions like COPD (chronic obstructive pulmonary disease) or asthma often experience breathlessness. This is because of the changes in their airways. But sometimes the way that you breathe can also contribute to breathlessness.

The diaphragm
Your diaphragm is your big breathing muscle. It is dome-shaped and sits below your ribs. As you breathe in, your diaphragm contracts and flattens down and air is drawn into your lungs. As you breathe out, your diaphragm relaxes up into a dome shape again. When it contracts down for your breath in, it squashes onto your tummy and makes your tummy push out; that is why diaphragm breathing is sometimes called tummy breathing. When you are breathing using your diaphragm, there is very little movement in your chest. You will mainly just see your tummy rise and fall with each breath in and out.
Accessory breathing muscles
In addition to the diaphragm, we also have little breathing muscles around our upper chest, known as the accessory
breathing muscles. They lift and open your upper chest. These muscles are there for when we need more air than our diaphragm can pull in, for example when you are exercising.
Dysfunctional breathing
Sometimes people get into a habit of using their accessory muscles to breathe most of the time, even when at rest. This is known as dysfunctional breathing. If you are breathing like this, you will see your chest rise and fall with each breath in and out (rather than your tummy). Dysfunctional breathing can make you feel breathless because your accessory muscles are much smaller and less efficient than your diaphragm.
People with lung conditions often need to use their accessory muscles to breathe when they are symptomatic (eg. if they are unwell or their asthma has been triggered) and this is a normal reaction. But it is important to return to relaxed tummy breathing if possible, once the episode has passed.
Certain lung conditions (for example emphysema) make it more difficult to use the diaphragm to breathe because the lungs’ resting size is more inflated

About the author
than normal. This pushes the diaphragm flat so it hasn’t got as much room to contract. So, people with emphysema have to rely on their accessory muscles to breathe all the time.
Check your breathing
You can check your own breathing pattern by resting one hand on your tummy and one had on your chest. Which hand is moving? If it is the hand on your tummy, you are using your diaphragm to breathe. If it is the hand on your chest, you are using your accessory muscles.
If you would like to learn more about you your own breathing pattern and how to optimise this, you should ask to see a respiratory physiotherapist.
12 Better Breathing
Zoe Manderson is a respiratory physiotherapist in Taranaki for Te Whatu Ora and a member of the Asthma and Respiratory Foundation’s Scientific Advisory Board.
Image supplied by BasicPhysiology.com 12 Better Breathing
Understanding spirometry
What is spirometry?
Spirometry is a simple breathing test that measures the flow and volume of air entering and leaving the lungs to find out how well your lungs are working. This is tested using a device called a spirometer.
Why would I need a spirometry test?
Spirometry can be used to diagnose asthma, chronic obstructive pulmonary disease (COPD) and other respiratory conditions. You may be referred for a spirometry test if you have signs or symptoms of a lung condition, before surgery or for other screening reasons. It is recommended as the ‘gold standard‘ test to confirm a diagnosis of COPD and to assess its severity.

What happens during a spirometry test?
The test involves taking a full breath in and blowing out as hard and as fast as you can into a tube attached to the spirometer device. The test will be done at least three times and can take from 10 to 20 minutes to complete. A clip may be placed on your nose to make sure that no air escapes from it during the test.
The spirometry test may be repeated to assess if your lung function improves after taking a reliever inhaler such as Salbutamol (Respigen, Ventolin, Salair).
How do I prepare for a spirometry test?
Your health professional should inform you on how to best prepare for the test. This may include information on which inhalers to withhold and for how long before the spirometry test. It is always a good idea to bring any inhalers you are using to the appointment. You may be asked to avoid certain activities before the test that could affect the results, such as drinking alcohol, caffeinated drinks, eating a large meal, smoking or doing strenuous exercise. Wear comfortable clothes, and it is best to go to the toilet before your test.
Is spirometry the same as peak flow?
No, these are different tests. A peak flow meter measures the peak speed at which you can blow the air out of the lungs, whereas spirometry is a tool used to measure a range of factors to diagnose and monitor lung conditions. Peak flow meters are useful for people with asthma to manage their condition.
Are there
any risks in having a spirometry test?
Spirometry is generally a safe test, however blowing out hard can put pressure on your chest, stomach, eyes and ears. You may feel dizzy at the end of the test. You might be advised against having this test if you have had a recent heart attack, stroke or experienced a collapsed lung, or if you have recently had eye, head or abdominal surgery, or a burst ear drum. Let the health professional doing the test know if you have recently coughed up blood and are unsure of the cause.
What do the results show?
Spirometry will produce a range of lung measurements which your health professional will interpret for you. Your health practitioner will need to look at your health history and your current symptoms and may recommend further testing like a CT scan.
A ‘normal’ spirometry result does not necessarily rule out a lung condition, and your health practitioner will look at other factors when considering a diagnosis.
How do I get a spirometry test?
Ask your healthcare practitioner about where you can get a spirometry test. Some primary care practices and asthma societies offer this service, or you may need to be referred to your local hospital for the test by your primary care practice.
13 Better Breathing
Asthma NZ - Auckland
Monday-Friday, 9am-5pm
09 623 0236
0800 227 328 anz@asthma.org.nz
581 Mt Eden Road, Auckland www.asthma.org.nz
Asthma Waikato
Monday-Friday, 9am-4pm 07 838 0851 info@asthmawaikato.org.nz
18 Claudelands Road, Hamilton East, Hamilton www.asthmawaikato.org.nz
Asthma and Respiratory Management BOP Inc
Monday-Friday, 9am-4pm 07 577 6738
0800 ARM BOP or 0800 276 267 reception@asthmabop.org.nz
254 Chadwick Rd, Gate Pa, Tauranga 3112 www.asthmabop.org.nz
Asthma NZ - Rotorua
Monday-Friday, 9am-5pm 07 347 1012
rotorua@asthma.org.nz
1290 Eruera Street, Rotorua 3010 www.asthma.org.nz
Eastern BOP Asthma and COPD support group

07 307 1447 or 0800 227 363 copd@drct.co.nz
C/O Karen Couchman, Disabilities Resource Centre Trust, 141 King Street, Whakatane 3120

Gisborne and East Coast Asthma Society (Inc) 06 868 9970 lynlolohea@hotmail.com
14 Kennedy Street, Gisborne 4010
Breathe Hawke’s Bay
Monday-Friday, 8.30am-3pm 06 835 0018 admin@breathehb.co.nz
199 Dickens Street, Napier www.breathehb.co.nz
Manawatu Breathe Easy 027 242 0669 sjorgi64@gmail.com
Horowhenua Breathe Easy Support Group 06 368 8069
Tu Kotahi Maori Asthma Trust
Lower Hutt
Monday-Friday, 8.30am-5pm 04 939 4629 / 0800 939 462 anne@kokiri-hauora.org.nz
7-9 Barnes St, Seaview, Lower Hutt 5010
Asthma NZ - Wellington
Monday-Friday, 9am-5pm 04 237 4520 wellington@asthma.org.nz
Level 2, 120 Featherston Street, Wellington 6011 www.asthma.org.nz
Marlborough Asthma Society
Any messages will be responded to during office hours Monday to Friday. 03 579 1609 0272057244 asthma.marlborough@xtra. co.nz
Nelson Asthma Society
Monday, Tuesday, Wednesday and Friday, 9am-2pm 03 544 1562 asthma.nelson@xtra.co.nz
9 Cambridge Street, Richmond, Nelson 7020 nelsonasthma.co.nz
CanBreathe Canterbury
Monday-Friday, 9am-4pm 03 386 0278
office@canbreathe.org.nz
196 Hills Road, Edgeware, Christchurch 8013 www.canbreathe.org.nz
Otago Asthma Society
Monday-Friday, 9am-12pm 03 471 6167, 027 471 6162 otagoasthma@xtra.co.nz
Dunedin Community House, 1st Floor, Cnr Moray and Great King Street, Dunedin 9016
Porirua SYLO Choir
Thursdays 11.30 - 12.30pm 027 405 6458 Supper Room, Mungavin Hall, Mungavin Avenue, Ranui, Porirua
Wellington SYLO Choir
Tuesdays 10.30am 027 817 1136
All Saints Church, 90 Hamiltons Road, Haitaitai
Breathe Hawke's Bay: Open for Business
Breathe Hawke’s Bay is open following Cyclone Gabrielle and the small team of asthma nurses is busier than ever serving the local respiratory community. The team look after people in central Hawke’s Bay, and as far north as Mahia and as far south as Waipukarau.
The team of three asthma nurses; Sue, Fiona, Jo assisted by administrator Raylene provide a wide range of support and education services to children and adults including in-depth one on one appointments, spirometry testing, a monthly COPD support group and outreach to local schools, Early Childhood Centres, sports groups and workplaces. They also offer training to local businesses and health providers.
Breathe Hawke’s Bay offers hour-long appointments to its clients to ensure that
there is plenty of time to fully discuss their condition and treatments, as well as covering any questions they might have. The team also provides home visits to those unable to come to their clinics. They welcome self-referrals from anyone living with asthma or COPD.
The team has been proactively working with teenagers in local high schools, running drop-in clinics to provide respiratory support. Manager Sue Parkes says this is a group that needs more support. “Often, they have had no education before on how to manage their asthma. There are issues with sharing inhalers, not using spacers and many issues with their housing.” The team is looking to technology to increase their capacity to reach young people and busy families.
Learn more at: www.breathehb.co.nz
14 Better Breathing
14 Better Breathing
GIVE YOUR FAMILY A HEALTHIER HOME WITH HRV
HRV home ventilation helps by delivering drier air from your roof space into your living areas, driving out damp, stale air. It filters the air too, reducing common allergens with a filter that uses the world’s finest air filtration medium, FilterLayr™.
HRV AirSense™, our premium system, is scientifically proven to reduce moisture* and helps prevent mould to give your family a warmer, drier healthier home.

While damp, stale air isn’t the only cause of asthma, the Asthma and Respiratory Foundation NZ sees it as a major contributor. That’s why HRV we’re proud to support its work as a Friend of the Foundation.

Here at HRV, our purpose is to make all Kiwi homes healthier. In New Zealand, asthma affects 1 in 8 kiwis – making a healthy home all the more important. hrv.co.nz 0800
*Based on a scientific study of 15 New Zealand homes conducted by Unitec Institute of Technology (Auckland) on behalf of HRV during winter and spring 2021. Results may vary depending on design and geographic location of a home.
15 Better Breathing
478 123















 Kia ora koutou,
Kia ora koutou,