

NUH Together


Winner William: City hosts
British Transplant Games

Bow-wowing out: Pooches
Ruby’s last tour

Charity Challenge: Raising cash for Children’s Hospital
DISCOUNT FOR NHS STAFF

Langridge Homes Limited
17-21 Clumber Avenue, Sherwood Rise
Nottingham NG5 1AG
Tel: 0115 962 6626
Deborah Lofthouse: +44 7522 579759
Email: sales@langridgehomes.com

We are pleased to offer a selection of three to five bed homes currently available on the Church Farm development in the small town of Ripley. The town is based on the outskirts of Derbyshire and has a great range of shops as well as easy access to Derby City centre.
Our development is located off Deanery Way, Church Farm, Ripley DE5 3TR

One of our latest developments is nestled in the heart of Giltbrook village. The selection of four and five bed homes are all within a short drive to a range of popular towns, cities and transport links and have a range of local amenities nearby, including the ever popular Giltbrook Retail Park.
Our development is located on Acorn Avenue, Giltbrook, Nottingham, NG16 2UF.




We are pleased to offer a selection of homes on our Stable View development in Calverton. The site is within easy walking distance of the village centre. The village hosts a range of shops and amenities, including a Sainsbury’s Local, Post Office, leisure centre and library. Nottingham City Centre is also easily accessible by a range of methods, including a bus route directly from the village.

Westhouse Farm View offers a range of new one to five bed homes in Bestwood Village. Situated adjacent to open countryside, our latest development provides a village feel, is in close proximity of Bestwood Country Park and is approximately a 12 minute drive to the M1.
Our development is located Off Moor Road, Bestwood Village, Nottingham, NG6 8ZQ.



One year on from the publication of People First, I want to reflect on progress made and thank colleagues for their continued hard work and commitment. Managing industrial action, ambulance handovers, and four-hour wait performance through winter was challenging. Although we are seeing improvements in our urgent and emergency care pathways, I accept that too many people have waited too long this winter. I’d like to thank those colleagues who continue to work hard to improve our services, often under difficult circumstances. I would also like to thank our many partners for their enduring support.
In the face of sustained pressure, we have:
• Protected beds for planned procedures, to ensure patients could have their operations.
• Treated more patients thanks to an increase in capacity from the respiratory and frailty Virtual Ward programme, our Same Day Emergency Care Unit and the Transfer of Care Unit.
• Opened Leengate at the QMC and Jubilee Unit at City to support flow through our hospitals.
Patient flow, recruitment and retention, and culture and leadership remain some of our biggest challenges. Looking ahead to the second year of People First, an enhanced focus on quality and financial sustainability is vital as we are experiencing significant cost pressures, like much of the NHS. We are working on our Financial Sustainability Plan, and over the next two years we aim to reduce our deficit and get back to break-even.
We are investing in the future of our hospitals through several capital build programmes. Work is progressing to create the first NHS purpose-built National Rehabilitation Centre, as part of the Government’s New Hospital Programme. The 70-bed facility will transform rehabilitation care, research, and training in the UK and will open in 2025.
Construction work has started on our new Neonatal Intensive Care Unit at the QMC, which we hope will be completed by the end of 2024. This will increase the number of intensive, highdependency and special-care cots from 17 to 38.
NUH has been chosen to run a new city-centre, state-of-theart Community Diagnostic Centre, which will support GPs by providing an additional 100,000 diagnostic appointments a year; it is set to open in 2025. n
Quality publications, that cover a specific demographic to help your business reach new customers
Advertising opportunities available in our staff magazines, care directories, and independent living guides






CARE DIRECTORIES
County, City and Borough Council care directories are comprehensive guides to nursing care, residential care and independent living support. Created for individuals and their families exploring the possibility of moving to nursing/ residential care or seeking advice and support to continue living independently at home.




Hospital at Home: supporting patients in their own homes
NHS STAFF MAGAZINES

NHS publications are circulated throughout hospitals to staff, patients and visitors on a regular basis. Advertising within the publications enables companies to promote their services to NHS employees and are an excellent way to Increase their customer base within this very targeted audience.


OPTIONS CARE AND INDEPENDENT LIVING GUIDES
Options provides older people with important information from health organisations such as CQC, ICB and the NHS. Circulated through various healthcare professionals including Council social work teams, NHS hospital discharge, community nurses, and various age related charities.

Nancy’s op uses iMRI
An innovative ‘in-op’ MRI scanner has allowed neurosurgeons to remove 100% of a toddler’s brain tumour in one go.
Nancy Dakin, then 14 months, became the 50th person to benefit from the Intraoperative Magnetic Resonance Imaging (iMRI) scanner – which allows neurosurgeons to ‘live scan’ during an operation.
Surgeons had originally thought they might only be able to remove 50% of Nancy’s tumour.
Mum Gemma said: “It was terrifying, we were on edge the whole time, just pacing up and down in the hospital. After eight hours, she came out and we couldn’t believe it. She was awake straight away and playing with a fidget toy and smiling at the doctors!”
Gemma and Dad Sam had taken Nancy to the GP after a few weeks of worrying
symptoms. She had surgery within six days of being referred to the QMC.
Donald Macarthur, Paediatric Neurosurgeon at Nottingham Children’s Hospital, said: “Many people worked hard and raised a lot of money to help fund our iMRI scanner.
“The iMRI scanner is amazing! It’s been a real roller-coaster of emotions. The staff here have been brilliant.”
“It’s helping us achieve the best possible results in brain tumour operations for our little patients like Nancy, and we are able to show parents immediately afterwards how successful the surgery has been.
“Many of our young patients are now able to have their MRI scans without needing to have general anaesthetics, which is great for them and is helping with waiting lists too.”
There are only a handful of iMRIs in the UK. The project was a joint funding partnership between NUH, Nottingham Hospitals Charity, the University of Nottingham, and Children with Cancer charity.
Nigel Gregory, Deputy Chief Executive at Nottingham Hospitals Charity, said: “A huge thank you to our supporters from across Nottingham, who donated towards this fantastic project.”
Gemma said: “The iMRI scanner is amazing! It’s been a real roller-coaster of emotions. The staff here have been brilliant. If we were millionaires, we’d end up having nothing because we’d give it all to them.” n
£25m health centre for city
A £25m state-of-the-art ‘one-stop shop’ in Nottingham will help speed up the diagnoses of illnesses such as cancer – meaning people can get life-saving treatment more quickly.
The new Community Diagnostic Centre (CDC) – one of 13 national CDCs funded by the Department for Health and Social Care – will open in Spring 2025 as part of the Broad Marsh regeneration project. It will be run and staffed by NUH.
CDCs will offer direct access to diagnostics services such as MRI, CT, x-ray, ultrasound, echocardiography, ECG, and lung-function testing –speeding up diagnoses and people’s access to life-saving treatments.
The CDC will initially provide an extra 100,000 diagnostic appointments each year. Once at full capacity it will offer more than 140,000 appointments annually, which will be available to patients through hospital consultants initially, and eventually via GPs. Until then, community diagnostics tests are available behind NEMS Platform One near Nottingham Railway Station.
Paul Matthew, our Chief Financial Officer, said: “We are delighted that our excellent, highly skilled and dedicated NUH staff will be running the future CDC, which will help to change the lives of so many of our patients for the better.
“This centre will be vital in reducing the number of people in Nottingham and Nottinghamshire waiting too long for diagnostic tests so that they can then either have peace of mind they deserve, or can begin any treatment required sooner. It will also enable patients to access these tests without needing to travel to a hospital.”
The CDC will create 75 jobs, including consultant radiologists, radiographers,

Brought to life: An artist’s impression of the new CDC
“The CDC is exactly the kind of facility everyone wants to see at Broadmarsh. It will provide a boost for businesses and jobs in the area by increasing footfall.”
imaging assistants, physiologists and administrators. When the unit is at full capacity it will employ 135 people.
NUH will be leasing the building from Nottingham City Council.
The Lister Gate facility will be the second CDC in the county; a centre in Mansfield will be run by Sherwood Forest Hospitals NHS Foundation Trust.
Nottingham City Council Leader Coun David Mellen said: “The Community Diagnostic Centre is exactly the kind of facility everyone wants to see at Broadmarsh. It will provide a boost for businesses and jobs in the area by increasing footfall.
“It will also help address some of the significant health issues and inequalities Nottingham faces as a city. People will be able to access vital health services right in the centre of the city.”
Amanda Sullivan, Chief Executive at NHS Nottingham and Nottinghamshire Integrated Care Board, said: “The CDC will provide an easier and altogether better patient experience by having a host of diagnostic services in one place.
“Earlier diagnosis is better for everyone. Not only will the increased testing help to improve the health of the local population and meet the growing demand for diagnostic services, it will also help free up capacity at our local hospitals and save money for the health and care system.” n
• CDCs are part of the NHS Long Term Plan to offer diagnostic care in convenient locations, to save people having to attend hospital.
• CDCs aim to improve population health outcomes and efficiency, reduce cancer waiting times and health inequalities, and help to address the elective backlog recovery exacerbated by the COVID-19 pandemic.
• The national programme is backed by £2.3bn government funding. It has so far delivered an extra 6m tests, checks and scans.



Elmbank offers first class accommodation and nursing care in a luxurious setting, combining a whole host of equipment and modern facilities designed specifically to meet the needs of elderly adults.
Facilities and services:
• Laundry • Dry cleaning (at an additional cost)
• Newspapers and magazines (charged monthly to your account)
• Toiletries, personal items and stationery can be purchased within the home
• Entertainment provided on a regular basis
• Activity co-ordinators organise activities including exercise classes, quizzes, birthday buffets and outings to surrounding parks, city shops, markets, restaurants and pubs.

Bodycams rolled out Staff and patient safety our priority
A sharp rise in aggression towards our staff has seen hundreds more bodycams rolled out across our hospitals, after a successful threemonth trial in A&E.
One nurse has told how she has had death threats, and has seen colleagues punched, kicked, and spat at during her six years in our Emergency Department.
“I’ve seen staff assaulted, punched, kicked and spat at,” said Deputy Charge Nurse Hannah Freer. “It’s just not acceptable and needs to stop.”
The bodycams will be worn in clear view of the public and will be switched on only when an individual is being violent or abusive, and after they have been told they will be recorded and footage used in any future prosecution.
Hannah says aggression gets worse when A&E is under pressure, and people face long waits.
“Some patients may be more aggressive due to their condition - we accept this. However, we know that in many cases the aggression and violence cannot be excused.
“We are here to help and deserve to be treated with respect and kindness.”
Medical Director Keith Girling said: “The safety and wellbeing of our staff and patients is our ultimate priority. Violent and aggressive behaviour - against our staff, other patients or visitors - has absolutely no place in our hospitals and will not be tolerated.
“We encourage our staff to always report these incidents and we will support prosecutions against anyone found guilty of abusing our staff in any way.”
Nottinghamshire Police say the bodycams are a deterrent and a way or providing records of incidents.

Superintendent Heather Maelor said: “We stand alongside our NHS colleagues in condemning any incident of violence or aggression towards hospital staff, or any other emergency worker, and will continue to work closely with our partners to find further ways to prevent these offences.” n

A Nottingham nurse is one of 53 thanked as part of an epic UK-wide charity Tour of Appreciation.
Andrew Gould is cycling 3,500km to raise £50,000 for the WellChild charity – and stopping along the way to personally thank WellChild nurses for everything they do.
Rachel Gregory, a WellChild nurse at Nottingham University Hospitals NHS Trust, had tea and biscuits ready as she welcomed Andrew to the Queen’s Medical Centre.
The WellChild charity supports children with long-term, complex health conditions, and offers three-year funded WellChild nursing posts to NHS Trusts, with Trusts taking over the funding after that.
“I helped write the bid for the role and thought, actually, this is perfect with my community background and experience in intensive care,” said Rachel, who has been a long-term ventilation (LTV) WellChild nurse for 10 years. The Trust recognised the impact Rachel was having and boosted the team with two more nurses.
Now a 17-strong multi-disciplinary LTV service, it covers Nottinghamshire, Lincolnshire and Derbyshire. It has around 120 children – and that caseload is growing.
“We offer complex community support and do as much as we can in a child’s home and community - the WellChild nurse post makes this possible,” said Rachel. “WellChild’s ethos is about keeping children at home; my role is to support them to stay well at home and allow them to live life to the fullest.
“Our families can struggle to get to the hospital, because the children’s needs are so complex,” said fellow NUH LTV nurse Sarah Walker. “They’ve got to park, they might have wheelchairs, lots of equipment… it can be a real trek - going out to them takes that pressure off them.”
Rachel and her team cover patients until they are 18 years old. “We go on that journey with them, we see them from being a baby right through – we are really lucky,” said Sarah.

Thanks Rachel!
UK tour to thank nurses
But how to transition their complex caseload to adult service is a challenge.
“Due to medical advances, children who wouldn’t have survived years ago are reaching adulthood,” said Rachel.
Rachel took Andrew to the WellChild Better at Home suite, one of only 10 in the UK thanks to a collaboration with the University of Nottingham. Here, parents and carers learn life-saving interventions they may need to make for their child, allowing a child to go home sooner.
“We do a staged discharge,” said Rachel. “Once the child is clinically stable, we walk around the grounds, then out to the park, slowly building the family’s confidence to go home.”
Andrew said: “The stories of the WellChild nurses and the families that they work with are an absolute inspiration - the skill, care and passion of these nurses is the beating heart of the WellChild charity.”
The team also offers training to schools. Rachel said: “Sometimes
WellChild relies heavily on fundraising
mainstream schools can be concerned initially. A year later, they’re talking about the child’s achievements rather than focusing on their health needs.”
Rachel has supported Sophie Cooper and her family for many years. Sophie has a complex range of conditions including Cerebral Palsy, Dystonia, Epilepsy, Scoliosis, Chronic Lung Disease and Gut Motility Disorder. She has a tracheostomy and is ventilated.
Sophie’s mum Leanne said: “One of the many brilliant things about having a WellChild nurse is they understand the importance of having families together at home and they understand the complexities of caring for a child with significant health care needs and they empathise with the impact that has on parents and siblings. They get it.”
Rachel added: “Our children are out there, with real complex health needs but we offer that specialist support – and they are living their lives.” n
• Last year, WellChild nurses supported over 2,300 children, young people and families. Its Helping Hands volunteers created 37 safe sensory spaces for children at home.
• With less than 2% of income coming from statutory sources, WellChild relies heavily on fundraising.

Gently does it... NUH designs bespoke incubator
Our medical engineers have designed and developed a bespoke incubator to transport critically ill babies around our hospital.
The Neonatal Critical Care Movement System (N-CCMS-1) incorporates all essential life-support equipment to ensure continuity of care while moving babies to theatre, for tests, or to the Children’s Hospital. It was designed in collaboration with our clinical team, and mirrors equipment used in our neonatal units.
With no similar system on the market, Aiden O’Brien, Clinical Engineer, and Dave Clay, Workshop Manager, were tasked to design and develop a solution ahead of the Neonatal Unit’s temporary move to Nottingham Children’s Hospital in September 2023.
“The doctors loved it and it changed the whole moving day, as families were reassured their babies were comfortable and safe.”
The move was a milestone in the Maternity and Neonatal Redesign (MNR), and the N-CCMS-1 was used to move 12 babies and their families.
“It was revolutionary,” said Critical Care Sister Amy Morley. “Moving babies from one ventilator model to another can require additional time for a baby’s breathing to stabilise, and this system removes that issue. Our main concern was how the babies would cope during the move, but it was flawless.
“The N-CCMS-1 also reflects the improvements in care standards,
equipment capabilities and regulatory requirements that have developed since previous systems were produced.”
Jenny Machell, MNR Lead Nurse, said: “This took extensive work and testing between medical, nursing and the clinical engineering team, before the N-CCMS-1 was used. It was great collaborative work - we are going to ask for three more transport incubators.
“The doctors loved it and it changed the whole moving day, as families were reassured their babies were comfortable and safe.” n




I was alive - now I’m living says cancer survivor Cindy
Cancer survivors are getting their lives back – thanks to a trail-blazing initiative at a post-cancer service at Nottingham City Hospital.
Nottingham Macmillan Late Effects helps people manage the physical, the psychological, and the psychosexual consequences of cancer treatment –and is the only place in the UK using photobiomodulation (PBM) therapy to treat the long-term effects of radiotherapy.
Cindy Martin, 64, who was left with disfiguring scars after surgery for stage 4 cancer of the saliva gland, says PBM therapy has given her back her life.
“The radiotherapy was so intense, my skin became necrotic. By the time I found Late Effects, I was convinced I would always have open wounds on my face.”
Radiation-induced fibrosis is completely unavoidable and can develop years after radiotherapy has stopped. Patients can
be cured of their cancer, but left with disabling and debilitating consequences.
“My face was awful,” said Cindy. “Skin would come off in clumps, and I lost my earlobe. It also affected my mobility - it was like I had a steel rod in my neck. All my identity had been taken away.”
The PBM machine has a large ‘shower head’ with LED lights, and takes around 15 minutes. Patients are trained to administer the treatment themselves; it is quick, simple, non-invasive, drug-free, and doesn’t cause any pain.
Emma Hallam is a Consultant Therapeutic Radiographer at NUH – and the person who thought of using PBM on radiationinduced fibrosis; it is usually used to treat lymphoedema – a long-term (chronic) condition that causes swelling.
Emma says: “We have people who have survivor’s guilt – they say that they feel lucky to be alive but sometimes wish that they hadn’t
How the Late Effects service is growing across the UK
• Emma has devised a patient questionnaire as a 10-year monitoring tool.
survived due to the long-term –sometimes disabling – side effects.
“Head and neck patients get much more radiation-induced fibrosis – they can’t eat, they can’t drink, can’t sleep – due to dry mouths and thick secretions.
“At Late Effects, we use a holistic approach to help improve quality of life and address all needs.”
PBM is just a small part of the Late Effects Service. The service uses a multidisciplinary collaborative approach, with a dedicated rehabilitation and followup clinic, therapeutic radiographers, dieticians, and speech and language therapists, and a specific head and neck programme. Patients can be also be referred to clinical psychologists.
“I was alive but I wasn’t living,” says Cindy. “Emma and her team have made such a difference to my life, I just can’t thank them enough – I wouldn’t be here today if it wasn’t for them.” n
• Global peer-to-peer sharing, and working with patients and charities has helped promote the need for the service. Nottingham has been pivotal in helping establish around 20 services across the UK.
Ruby bow-wows out
Doggy diva Ruby has retired as a therapy dog after bringing smiles to thousands of people over the years.
Ruby and fellow therapy dog Bertie leave a lasting impression on everyone they meet. In QMC foyer, Rebecca Guest recalled, emotionally, how Ruby had visited her in the highdependency unit during the pandemic. And a young woman thanked them for helping during her antenatal appointments – and invited them to meet her newborn.
Ruby and Bertie are Pooches – Pets
Offering Ongoing Care Help & Extra Support – set up by healthcare assistant and owner Dale Buckland in 2012.
For Dudley, on B49, Ruby brought back memories of his own dog, Lucy. “A dog is a friend at night when you’re on your own,” he said.
Healthcare Assistant Georgia Wing said: “Ruby brings such joy to the ward – it makes our patients smile and that makes me happy.”
Nottingham Hospitals Charity, which funds Pooches, said: “Ruby has had a wonderful career, making a difference to people’s everyday lives and helping to ease patients’


anxiety, and she brings joy to staff as well.”
Dale said: “Ruby loves being adored. After we’ve done our rounds, we always stop and get a sausage from the chip shop. Ruby might not be on the
wards any more but I reckon she will still get a sausage.”
Then Dale led Ruby – for the last time –down the corridor to visit that newborn and the young mum she’d made such an impression on. n


Snooker champ’s thanks Dave shows off medal to our team
Gifted snooker player Dave Bolton feared he’d never play again after a near-death experience. Now – after scooping a medal at an international tournament – he’s thanked our staff for making it possible.
Dave, 48, was rushed into hospital with a clot blocking the blood supply to his bowel. Wife Michelle was warned he might not make it. Emergency surgery to remove most of his bowel left him facing potentially a lifetime of intravenous feeds.
Dave needed an intravenous feed for 12 hours a day, every day. Our Intestinal Failure team built him up and organised a homecare package.
And when Dave was heading to Thailand for the World Disability Billiards and Snooker World AbilitySport Games, creating a strict feeding schedule around a strict playing schedule – with an eight-hour time difference – was no mean feat for our clinicians. But Dave made it worthwhile, scooping a bronze medal.
Dave has been an avid snooker fan since he was eight, inspired by legend Jimmy ‘the Whirlwind’ White, who lived near him in Tooting, London.
“He used to wash my grandad’s car to raise money to play in the local snooker hall.”
Dave moved to Notts at 13. As a top-flight amateur, with a highest break of 142, he played in pro-ams. At the end of last year, he hit 140 for the first time since his surgery in 2022.

He won the 2023 The Cube UK Disability Snooker Championship in September; the WDBS German Open in October; the World AbilitySport Games in Thailand in December; and the British Open in January.
“I’d been told I’d never play again – but I never give up. There’s a saying – ‘it’s not the size of the dog, it’s the fight in the dog’ – and this is what I live by day to day.” n
Farewell to iconic city landmark
An iconic landmark will disappear from Nottingham’s skyline as part of our Trust’s move towards green energy.
The 164ft chimney at City Hospital – between Gates 4 and 5 on Edwards Lane – will be removed in sections over several months. It is expected to be completed by June.
The chimney was part of a coal-fired boiler plant used to heat City Hospital for many years. Thanks to £25m grant from the Public Sector Decarbonisation Scheme, a
new energy centre has been built, using more efficient energy and environmentally friendly technologies.
NUH’s Director of Estates and Facilities, Andrew Chatten, said: “This chimney is one of a pair of structures that have dominated the City Hospital skyline. We’ve already removed one.
“This represents the significant work that we’re undertaking across our sites as we move towards our net-zero ambition,
which aims to help save money, provide a better quality of life for patients and staff, and play our part towards sustainability in Nottingham and Nottinghamshire.”
Our net-zero agenda supports the commitment by the NHS to be the first health service in the world to reach netzero carbon. By 2040, we hope to have achieved a net-zero carbon operation for all our emissions from heating and energy use, and 80% reduction of our carbon footprint indirect emissions. n
Giving patients a choice
A new virtual unit is giving our end-oflife patients the option to spend their final days at home with their families.
The pilot palliative ward is staffed by specialty teams based at Hayward House at Nottingham City Hospital and can cater for up to six people. The patients are reviewed each day by consultants and visited by community nursing staff.
The virtual ward offers patients the best of both worlds, said Heather Young, who heads up the virtual ward programme at our Trust. It gives patients a choice about their end-of-life care at a stage in their lives when they may feel they don’t have any; and it gives them specialist support in the comfort of their own home.
The virtual ward also helps relieve the still “significant” post-pandemic pressures on our hospitals.
Palliative medicine consultant Dr Cathrine Vincent said: “It’s really important that we talk to people about where they want to be at the end of their lives - and most patients want to be in their own home. Get people in their own environment if that’s where they want to be - that comfort can help people get better.”
Dr Vincent mentioned a recent patient who wasn’t sleeping in hospital and chose to go on the virtual ward.
“It means symptoms are better controlled. Pain, anxiety, breathlessness… all those things improve when people feel better in themselves - and being in their own environment can often help with that.
“Sometimes people think palliative care is about dying, it’s not. It’s about living every last day, month, year, as well as they can.” n

How a Virtual Ward benefits patients
• Virtual wards use technology to deliver NHS care in people’s homes.
• Virtual wards are supporting thousands of people across Nottinghamshire who would otherwise be in hospital. They
are being cared for, supported, and monitored in the place they call home, which helps early discharges from hospital and can avoid unnecessary readmissions.
Catering team scoops national award
Our catering team has won a prestigious national award for its infant feeding menu at our children’s hospital.
The Catering Production and Food Service team scooped the Hospital Catering Award at the Public Sector Catering Awards after developing the new menu.
“We were up against some fantastic nominees,” said Food Production
Manager Sue Austin. “It was an honour to represent the Trust to accept the award. I am very proud of our team.”
Catering, dietetics and nursing staff worked together to create a baby pouch infant feeding menu, explore the creation of meals onsite, and to produce a blended food menu for patients being fed via a tube. An
electronic ordering system monitors take-up of the meals to help avoid unnecessary waste.
Catering Facilities Manager Marie Gurling said: “I’m so proud to be part of the catering team at NUH. It is a great achievement to be recognised for all our hard work and new initiatives which have been introduced to improve our patients’ experience.” n
New family room
A new family room has been opened to provide respite for the parents and carers of critically ill children at Nottingham Children’s Hospital.
The room on the Paediatric Intensive Care Unit (PICU) gives families a chance to step away from the ward environment into a homely and welcoming space, with comfortable seating, relaxing artwork and a well-equipped kitchen area.
It also provides a space where clinicians can have conversations with parents and carers, away from their child’s bedside, where families can meet and benefit from the support of others who are going through a similar experience.
The refurbished room was funded by the True Colours Trust’s Breathing Spaces programme and Nottingham Hospitals Charity.
Sophie Wilne, Clinical Director of Nottingham Children’s Hospital, said: “This family room will make such a difference to families whose children are being cared for in PICU.
“This can be an incredibly stressful time for parents and carers, and this room

offers them some respite from the busy hospital environment. They can come and make a hot drink, sit on a comfortable sofa, and have some sense of normality for a short while before returning to their child’s bedside, hopefully feeling a little more rested and refreshed.
“Thank you to the True Colours Trust and Nottingham Hospitals Charity for making this possible.”
Nottingham Hospitals Charity’s Big Appeal aims to raise £1.5m to fund further improvements to Nottingham Children’s Hospital. n
Why not become a charity Friend?
From just £5 a month you can support the area of the hospitals that is closest to your heart, and know that your regular gift is making a difference to patients and staff every day.
A monthly donation allows you to spread the cost of your support throughout the year and provides Nottingham Hospitals Charity a reliable, regular income to enable us to plan ahead and make long-term improvements for our patients, their families, and our staff.
Your monthly donation can help us:
• buy specialist equipment for more than 110 wards
• build and renovate facilities for patients and their families
• fund vital medical research
• support NHS staff with training and wellbeing support
Nigel Gregory, Chief Executive at Nottingham Hospitals Charity, said:

“Becoming a Friend of Nottingham Hospitals Charity, by setting up a regular monthly gift, is such a wonderful way to show your support for our hospitals. Your donation will go towards whatever area of our hospitals means the most to you – whether that’s the Children’s Hospital, cancer wards, medical research, or any other area.
“I’d like to thank all those who continue to give a monthly gift to the Charity, and encourage anyone considering becoming a Friend to get in touch with us and find out more.” n
William Reckless – who lost both his legs and nine of his fingers at the age of three due to sepsis –has walked and cycled four miles to raise money for Nottingham Children’s Hospital.
William was rushed to QMC in January 2020. When he arrived, he had a cardiac arrest and was resuscitated.
“We were told to prepare for the worst,” said mum Gemma. “He was not expected to survive. Thankfully, William pulled through. But it was a long and tough journey.
“I’d left home with William in January, leaving my husband Mike with our one-year-old daughter Georgia, expecting to be home in a few hours with some antibiotics. I didn’t return until over two months later when William was discharged.”
In March, William walked two miles and cycled two miles to mark the four years since his amputations – and to raise money for the Big Appeal.
The Big Appeal was launched by Nottingham Hospitals Charity to raise £1.5m to fund improvements such as play areas and family rooms.
Gemma said the family would be forever grateful for the care they received at NUH: “Although we were living every parent’s worst nightmare, everyone at the hospital was incredible. They not only looked after William but supported our entire family.
“While William was in the Paediatric Intensive Care Unit (PICU) we were given a room nearby, which was funded by Nottingham Hospitals Charity, so that we could grab a few hours’ sleep and a shower, but know we could be back at his bedside within minutes if the situation were to change.
“This meant everything to us, I couldn’t bear to be apart from him at that time.”
To sponsor William’s fundraising, please visit www.justgiving.com/ page/williamsbig n
William, 7, in charity challenge

“Although we were living every parent’s worst nightmare, everyone at the hospital was incredible. They not only looked after William but supported our entire family.”
Charity’s rally call
Creating a sanctuary for parents
Baby loss charity Forever Stars has launched a £50,000 appeal to help support Nottingham families who have suffered miscarriages – and it needs your help.
Forever Stars has named its appeal Supporting 1 in 4 for 2024, as around one in four pregnancies ends with a miscarriage.
Its appeal will revamp Ward A23 at QMC, part of our Emergency Gynaecology and Early Pregnancy Assessment Unit, which gives specialist care and support to around 10 families experiencing baby loss every day. The charity also aims to transform an outside space into a sanctuary and remembrance garden for families.
“We are an area that sees a lot of sadness and we want to do what we can to make our ward a more positive place for our patients,” says A23 matron Lucy Groves. “There is no bereavement area or “serenity” suite - these women deliver in a very clinical environment. Forever Stars has already funded the fixtures and fittings to change two delivery rooms into bereavement suites.”
“The garden is a sanctuary where families can retreat to try to deal with the weight of their loss,” says Forever Stars co-founder Richard Daniels. “It’s also a valuable waiting area for fathers, and somewhere siblings can get fresh air and be kept occupied and distracted playing with toys while the rest of the family receives treatment. But it needs a lot of attention.”
Lucy said: “The campaign will fund a garden with a remembrance area, where families can plant a flower in memory of their baby, and it will also be a place for reflection.”
Forever Stars was set up by Richard and his wife Michelle after the stillbirth of their daughter Emily on 19 December 2013.
“A23 has a fantastic team that supports families dealing with baby loss,” says Richard. “We really want to create a better environment for families at what is a very difficult and scary time.”

Fundraisers:
“As well as raising funds, we need people to donate their skills, time, materials, and talents.”
“We desperately need help – donations and resources from as many people and businesses as possible. As well as raising funds, we need people to donate their skills, time, materials, and talents.”
The charity is appealing to local artists to paint murals, and have a ‘want’ list:
• seating, heating and lighting
• audio systems
• artificial grass
• bedding plants
• children’s outdoor toys
“This is one of our biggest ever challenges, and something we know we can’t do alone. We need as many people as possible to help us to create a truly special environment for the families that need to use the ward. Support – big or small - can make a genuine difference to families who rely on A23 during their miscarriage journey,” says Richard.
To donate your time, expertise or materials, please email: enquiries@foreverstars.org. n


City to host 2024 British Transplant Games
More than 1,000 transplanted athletes will be taking part in this year’s British Transplant Games in Nottingham – and celebrating the gift of life.
Transplanted athletes aged three to 8o-plus, from more than 60 hospital teams across the UK, and surrounded by family, friends and volunteers, will take part in the Games, which run from Thursday 1 to Sunday 4 August.
Nottingham Hospitals Charity has helped fund the Games, which aim to raise awareness of organ donations. Chief Executive Nigel Gregory said: “We’re delighted to have helped bring the 2024 British Transplant Games to Nottingham, by providing funding for the Games to take place in our city. It’s an important event for transplant recipients across Nottingham and the whole country, as well as donor families, and a wonderful chance to come together with people who have been through similar experiences.”
Tim Reddish CBE DL, Chair of the 2024 Games, said it was an absolute honour to have been selected to chair the Games. “My career in sport will, I’m sure, assist me in making this a fantastic Games and I look forward to sharing my experience and knowledge of competitive sporting events.
“This is also a wonderful chance to express our gratitude towards the donor families and live donors who selflessly contribute to improving the quality of life for people all over the UK. I strongly encourage everyone in the vicinity of the Games to attend and witness first-hand the inspiring stories of the athletes and families involved this summer!”
Dr Paul Harden, Chair of Transplant Sport, said: “I have no doubt this year’s Games will be the best yet through our ongoing support network from the stakeholder board, talented athletes and volunteers making it their mission to leave a legacy behind in Nottingham.”
For more information on the British Transplant Games and how you can get involved, visit: www.britishtransplantgames.co.uk/ n


William was just surviving – now he’s thriving
One boy taking part in this year’s Games is six-year-old William, who received a kidney from his mum at QMC.
William was born at 33 weeks and tests revealed he had abnormal kidney function. He had both kidneys removed when he was two, and had been on dialysis for over a year before the transplant took place in November 2021.
Mum Alice said: “It was amazing to see William taking part in last year’s games –he was meant to do the obstacle course but he had a broken arm. We were all really proud when he won gold in the beanbag bullseye.”
“Thankfully I was able to give him a kidney and now he has the world at his feet. He’ll be on medication for life, and supplements – but he won’t be on dialysis any more.”
William celebrated his 5th birthday on last year’s World Kidney Day, and went on to scoop a gold medal in the beanbag bullseye event at the 2023 British Transplant Games.
“William is a completely different child since the transplant,” said Alice. “He has more energy, his personality is amazingbefore he was too tired or unwell to show who he really was - he is thriving and not just surviving.”
Consultant paediatric surgeon Mr Alun Williams carried out William’s transplant.
He said: “William and his family are tremendous examples of the transformation that transplantation brings about, and it’s a delight to see the whole family thriving. Life with kidney disease is tough for the whole family and to be able to help makes such a difference.
“Living donation is especially important, and innovations like the national kidney sharing scheme are making the most of opportunities for transplants - not everyone can donate directly to their intended recipient

“I’m so grateful that there are people with the knowledge that have dedicated their life to helping people who wouldn’t survive without them.”
and this is a way to allow donors to donate and see ‘their’ recipients have their transplants. We are seeing more and more altruistic non-directed living donors too, which is excellent.”
Alice said: “I’m so grateful that there are people that have dedicated their lives to helping people who wouldn’t survive without them.” n


How did we do?
Have you or your loved ones received great care at one of our hospitals? Did you know you could nominate an employee or a team for one of our People First Recognition Awards?
With more than 19,000 employees, we are passionate about recognising and rewarding their achievements – and you can help.
Our Public Award for is for a person or team who has demonstrated high-quality
clinical care and/or compassion or kindness to you or a loved one. You can also nominate non-clinical or administrative staff if you feel they have provided great care or support.
Our awards are open for nominations all year round and collated for judging at the end of the summer. An internal panel shortlists the nominations and then highly commended and winning nominees are chosen by an external judging
panel and announced at our annual awards ceremony in the autumn.
Nominating a person or team can go a long way. It doesn’t take long to submit a nomination and you could really make a big impact on the person or team by doing so.
To find out more and to make a nomination visit www.nuh.nhs.uk/awards or scan the QR code. n

Staff clock up 1,000 years’ service
More than 1,000 years’ NHS service has been honoured with a celebratory afternoon tea.
Chief Executive Anthony May and former Chief Nurse Michelle Rhodes handed out awards to colleagues with 25, 35 and 40 years’ service.
“I’ve always loved coming to work and feeling that I can make a difference,” said Lianne Finnerty, the only person to celebrate 40 years.
“I’ve been part of many improvements over the years and have worked with lots of wonderful and knowledgeable people who care about improving services for our patients.”
Lianne – Head of Quality, Risk & Safety for Cancer and Associate Specialities and Designated Individual for the Trust Human Tissue Authority Post Mortem Licence – said: “It was lovely to be acknowledged – it makes me feel very proud to work at NUH.”
Senior Interpreting and Translation Services Innovation Lead Renata Towlson – who celebrated 25 years – said: “It was a touching tribute and made me reflect on the NHS and the professional achievements in my life so far.”
Former Chief Nurse Michelle Rhodes said: “It was a privilege to honour 1,000 years’ service, commitment, and skills at my last long service celebration before retirement. The fact so many have stayed here and devoted their lives to the patients we care for is one of the many things that makes NUH so special.” n

NUH is very inclusive
– I’m a very different Owen now
A 20-year-old man with learning disabilities has praised our Trust for being so inclusive.
Owen Hayes was a recruit on Project Search, a Nottingham College programme that works with local employers to secure internships for young people with learning disabilities or difficulties.
The programme brings together work experience and training in employability and independent. Each student has a support network including a tutor, job coaches and business mentors to help the transition from college to work.
Placements are varied and include logistics, catering, domestic services, and more, and students have three in the 12-month course. The aim is to place students in full-time, paid employment at the end of the year, with a commitment to ongoing support from the employer.
Owen had tried several college courses without much success, and was struggling to find something he enjoyed. This started
to affect his self-esteem and his mental health took a downturn.
He enrolled on Project Search and had several logistics roles, immediately developing good relationships with his colleagues – and was offered an apprenticeship with our Estates and Facilities team.
Owen is deaf and has a learning disability. He said: “In the real world it is very hard or someone like me to find a job so somewhere like this where everyone is included, race, religion, disability or anything doesn’t matter in this hospital –it’s very inclusive.”
“One of the benefits of an apprenticeship is gaining experience and confidence,” said Owen,“ and it really shows how much you have grown as a person.
“From a year ago to now, it is a very different Owen from what people normally see me as.”
Hear Owen talk about his experiences: youtu.be/yln0aBoDQT4?feature=shared n

UK first for Nottingham NUH hosts rare liver disease study
When a life-sciences company sought the ideal venue to conduct research with inpatients into a potential new treatment, the NIHR Nottingham Clinical Research Facility (CRF) based at the QMC was the obvious choice.
During February, our CRF was one of just two centres worldwide and the only facility in the UK to conduct part of a clinical study into a new treatment for Primary Biliary Cholangitis (PBC) – a rare liver disease with severe symptoms of fatigue and cognitive impairment.
Anders Karlsson, CEO of the company sponsoring the clinical trial, said: “The study team at NIHR Nottingham CRF has been extraordinary professional in both managing the challenge of recruiting patients from all over UK, which includes co-ordination with the patient support organisation the
PBC Foundation, the patients and their local hospital, scheduling patients’ travel and all related study arrangements.
“In addition to managing the practicalities of performing a very complex clinical study, the research team at NIHR Nottingham CRF has also exceeded all expectations in keeping timelines and a day-to-day contact with the clinical study sponsor and their assigned clinical research organisation.”
Nottingham hosted five patients on a purpose-built inpatient ward, to confirm the correct dose of the trial drug. During their seven-day stay, our team of research nurses and physicians monitored and cared for the patients around the clock.
Nottingham CRF has 18 adult and five paediatric inpatient beds dedicated to research, alongside dedicated outpatient and specialist clinics n
New arrival in NUH Research
Mums-to-be in Nottingham are invited to join an important national research initiative, which aims to find out what influences the health and wellbeing of families.
NUH has become the latest research site to join the ‘BaBi’ (Born and Bred in) Network, which has recruited more than 31,000 participants. More information is available on our website: www.nuh. nhs.uk/babi-nottingham n
Nottingham CRF has 18 adult and five paediatric inpatient beds dedicated to research, alongside dedicated outpatient and specialist clinics.
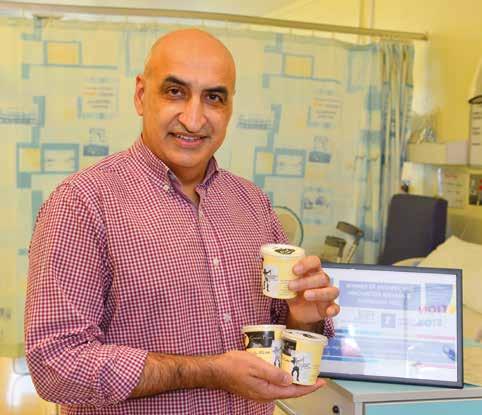
N-ICEly does it.... again!
Researchers at NUH are celebrating two more prestigious national awards for their protein-enhanced Nottingham Ice Cream - N-ICE Cream™.
N-ICE Cream™ won both the Innovative Food Product and Best Health and Nutrition Product categories at the Business Awards UK Food Industry Awards, the fastest growing awards platform in the UK.
This takes the number of awards won by N-ICE Cream™ to five in just 18 months, and celebrates the formal collaboration between Nottingham University Hospitals NHS Trust and Matlock Meadows Dairy Farm, which has seen three new flavours added to the N-ICE Cream™ range.
Professor Opinder Sahota, Consultant in Ortho-Geriatric medicine at NUH and Honorary Professor at the University of Nottingham, leads on the research into N-ICE Cream™.
He said: “It is fantastic to be celebrating news of two more wins for N-ICE Cream™, our nutritious muscle-targeted high- protein ice cream.
“The Food Industry Awards are judged by a panel of industry experts so this is yet more credible external recognition for our innovative product.”
“What is most important is that we create opportunities for more patients to benefit from N-ICE Cream™, which has been developed to address the serious problem of malnutrition and muscle weakness among older people.”
Kate Byrne, Managing Director at Business Awards UK, said: “Winning both the Innovative Food Product and Best Health and Nutrition Product categories is a testament to the commitment of NUH in addressing critical health issues through ground-breaking solutions.
“Their dedication to combating malnutrition among the elderly with their innovative product is not just a win for their team, but a significant step forward in the food industry. We’re proud to
showcase such transformative work that not only meets a crucial need but also sets a new standard for nutritional care.”
Previous awards for NUH’s N-ICE Cream™ were:
• Best Dairy Protein Product, World Dairy Innovation Awards 2023
• Winner of the Health Innovation category, World Food Innovation Awards 2023
• National award for NHS Innovation, Medipex Ltd, 2022. n
Want to take part in a hearing study?
Do you use hearing aids but still struggle to hear, even when you are in quiet places?
If so, you may be able to take part in a ground-breaking national research study that involves our Audiology service team.
NUH is one of nine NHS Trusts taking part in the COACH trial (COmpAring Cochlear implants with Hearing aids in adults in
severe hearing loss) – the first research study of its kind worldwide.
Currently, we do not know whether a cochlear implant is more effective than hearing aids in adults whose hearing test results and speech understanding scores are just outside the range that would make them eligible to receive a cochlear implant on the NHS.
This is the ‘grey area’ that we are hoping this trial will provide an answer to; it could also influence NHS policy.
The research is being managed by the National Institute for Health and Care Research (NIHR), Nottingham Biomedical Research Centre and the University of Nottingham. To find out more, visit: www.coachtrial.ac.uk. n
Bringing down the barriers
Imagine falling ill abroad and being unable to articulate how you’re feeling to a doctor.
Polish-born Renata Towlson knows that not understanding what’s being said in a medical situation can add extra stress to an already stressful situation.
Renata has a passion for making sure every patient has access to our Interpreting and Translation Services – with help available in more than 55 languages, thanks to the wider Nottingham community
“NUH and Nottingham City are so multicultural and multi-lingual,” said Renata, a qualified interpreter. “And that offers such an enormous, invisible human resource.”
Renata worked with the International School of Linguists to create a training programme for anyone with a passion for languages who wants to help fellow nationals.
“I am passionate about giving people the chance to use their skills to help shape their lives in their adopted country - it is a
tough ride! Linguistic skills allow people to offer meaningful help and offer them the opportunity to build a career.”
In-house and community volunteer interpreters and 85 freelance interpreters support around 25,000 bookings a year. NUH volunteers are given basic training and can also be supported to become a qualified interpreter.
John Cipko grew up speaking English and Polish. He became a volunteer after taking early retirement from his 32-year NHS career – and gained such a glowing reputation that he quickly moved on to paid, freelance employment at NUH.
He said: “The satisfying thing is feeling like I’ve helped people, and getting thanked by the client, the doctors and consultants. They often tell me that without my help they would have struggled to help the patient.”
To find out more about interpreting and translation opportunities at NUH, contact renata.towlson@nuh.nhs.uk n

35ft-fall man thanks rehab staff

A Nottingham roofer who fell 35ft onto concrete has thanked the NUH teams who nursed him back to health and taught him to walk again.
Simon Bell, 58, had a brain injury, internal bleeding and damage to his internal organs. He had also fractured his shoulder and broken all of his ribs on the righthand side.
He has no memory of the accident in May 2023 or his first six weeks in hospital.
Simon said: “I was in intensive care and my body was in shutdown. I wasn’t good – they had to remove my spleen; my liver and kidneys were damaged; and they kept pumping blood out of my lungs. I was in quite a mess.”
After five weeks in Intensive Care and six weeks on the Major Trauma Ward, Simon was transferred to Linden Lodge at City Hospital to begin his rehabilitation with a
specialist team of nurses, physiotherapists, occupational therapists, and psychologists.
He said: “I had very little movement in my righthand side – I could only move my fingers. I couldn’t shower, or walk, and was in a wheelchair.
“I wanted to be better – I’d previously been fit and active. If anyone dropped out of a physio session or if the team had spare time, I was in the gym. I always felt better after exercise and was motivated to push myself to do a bit more. The harder you work at it, the harder the staff work with you.”
The dedication of our staff and Simon’s determination and positive mindset meant Simon was out of his wheelchair within five weeks – and headed home in September.
Simon still has a long road to full recovery, but said: “It was a big step but I am pleased to be home.” n
Earlier cancer diagnosis onsite
More targeted treatments on way
New technology will allow for earlier diagnosis of cancer and more targeted treatments with fewer side effects.
Two new Genexus machines – installed at the Genomics laboratory at NUH, part of NHS East Genomic Laboratory Hub – allow doctors to bring detailed testing with limited samples on-site, simplifying, shortening and streamlining the diagnosis process.
Each machine can process up to 16 samples at once, testing multiple genes in parallel and in detail. Previously, the lab could process only one test sample on a single gene at a time.
Amanda Corkill, Genomic and Molecular Medicine Service Manager, said: “We are now able to deliver some of the more advanced genomic tests for lung cancer, colorectal cancer and melanoma for patients across Nottinghamshire and will soon be expanding to cover further tumour types.”
Anthony May, NUH Chief Executive and Chair of the NHS East Genomics Executive Group, said: “It is fantastic news for our patients and staff that more urgent cancer testing can now take place onsite at our Nottingham laboratory. This new technology helps us to move closer to our ultimate aim; working with our partners to provide more testing across our region.


“It is fantastic news for our patients and staff that more urgent cancer testing can now take place onsite at our Nottingham laboratory.”
“Ultimately we want to ensure that anyone who could benefit from genomic testing has access to it, regardless of who they are, where they live or what hospital they are treated at.”
Further developments in molecular testing are planned in whole genomic
methylation profiling of brain tumours, whole genomic sequencing of paediatric tumours, brain tumours and sarcomas, and in the delivery of genomic testing in haematological malignancy.
Find out more at: www.eastgenomics.nhs.uk n
Anthony May is new Chair for NHS East Genomics Executive
Our Chief Executive, Anthony May, has taken over as Chair of the NHS East Genomics Executive Advisory Board.
NHS East Genomics oversee and deliver genomic testing in our region through the East Genomic Laboratory Hub (comprising laboratories at Cambridge University Hospitals, Nottingham University Hospitals, and University Hospitals of Leicester). Sitting alongside the East GLH is the East Genomic Service Alliance (GMSA), which is responsible for mainstreaming genomics in the local NHS.
Working with partners, the Board will support the systematic embedding and mainstreaming of genomic medicine services in our region, as well as overseeing the delivery of Genomic Networks of Excellence, the Newborn Screening programme, and transformation projects, to name a few key areas. It will also be responsible for the delivery, quality and performance of the genomics laboratory services through East GLH. n
Surgeons train medics in war-torn country
Two NUH surgeons have been training Ukrainian medics to perform keyhole surgery - after senior doctors fled the country at the start of the conflict.
Charles Maxwell-Armstrong and Katie Walter – colorectal surgeons – were part of a six-strong cohort delivering training in a hospital in Lutsk in the north-west of the country.
“The hospital was surrounded by armed soldiers on the day we left as it prepared to take a convoy of wounded soldiers arriving by special evacuation trains from the frontline,” said Katie.
“The doctors told us how, at the start of the conflict, many senior doctors fled the country; they had received donations of kit and medical equipment from around the world but this was not always kit they knew how to use or needed; and they are still short of many supplies.
“Many of those left in charge were three or four years out of medical school, working very long hours covering understaffed units. Those working near the frontline were clearly scarred from the atrocity and trauma they had witnessed.”
Basic laparoscopic training for 150 junior surgeons, with hands-on simulations, was followed by advanced training via live video links to operating theatres.
Charles said: “Operating in a foreign theatre in the middle of a war zone, in front of 150 Ukrainian surgeons, on patients you’ve never really met, with equipment you’ve had to scrape together, and with a team you’ve never worked with – where very few people spoke English – it was a challenge.”
Lutsk is in the north-west of Ukraine, miles from the fighting, but the war was ever present, with rockets flying overhead and sirens going off. With large gatherings banned, registration onto the training was all done by word-of-mouth.
“Hospitals do get bombed in Ukraine,” said Charles. “We had to be really careful - you put 150 colorectal surgeons in one

“We were asked ‘What are people saying in Europe? Have they forgotten about us?’”
place and one strike could wipe out a generation of surgeons.”
The visit was organised by SMART Medical Aid, a Dutch-Ukrainian charity set up in 2014, and aimed to establish a formal teaching programme for Project IOLE (Improving Outcome in Laparoscopic Surgery by Education), which has been approved by the Association of Coloproctology of Great Britain and Ireland (ACGBI) and the Royal College of Surgeons of England.
The group met with the Ukrainian Minister of Health, Viktor Liashko, to press home the need for a national, funded training programme; Charles is one of those returning in May.
“The Ukraine people went out of their way to look after us,” said Katie. “Parents told us how they wake their children in the night to head to shelters, or spend nights on the bathroom floor comforting their children sleeping in the bath (deemed the safest place in the house to offer protection in a blast).
“We were asked ‘What are people saying in Europe? Have they forgotten about us?’”
“It is clear that the inevitable stress that comes with living in a country at war adds a chronic, inescapable pressure to their lives.
“Large gatherings are banned, there is a 10pm curfew, roads are littered with antitank “hedgehogs”, windows are taped to limit shatter-damage, bomb sirens are going off and mobile phone bomb apps ring alerts throughout the day.”
Both Charles and Katie paid tribute to the resilience of the Ukrainian people. “I’ve come back with immense respect and admiration for the strong and resilient people and a desire to do something more to show them my support,” said Katie.
“I’ve never known anything like it before,” said Charles. “What sticks with me about the visit is the sheer resilience of the people.” n
Homebirths now available around the clock
More choice for mums-to-be
A round-the-clock homebirth service is now available for mumsto-be in Nottingham.
The enhanced homebirth service meets a commitment made to our communities in 2023 to offer a sustainable 24-hour service.
It was agreed to suspend the service in January to allow for a review of staffing and support arrangements, taking into consideration the changing patterns in birthing choices locally and nationally to develop a service that is sustainable and offers clarity to both patients and staff.
Now the homebirth service is fully up-and-running – and is offered around-the-clock to those who meet the criteria.
“We have always been committed to a full homebirth service as we know it is the right thing to do for our mums-tobe,” said Sharon Wallis, NUH Director of Midwifery. “However, we also have a responsibility to ensure any service can be safely staffed and sustainable.
“I want to thank local birthing people and their families for their patience while we have put plans in place, and am really pleased that we have been able to now offer a 24-hour service for those individuals that meet the criteria for a homebirth.
“Our homebirth team lead joined the Trust in January and we continue to recruit to a full team, and in the interim I am grateful to colleagues from our community and hospitals teams who have committed to additional shifts to enable us to offer the service now.”
Anyone who wants any further information is encouraged to speak to their midwife or consultant obstetrician. n

Pupils raise £1,250 for books for young patients
A city primary school has donated £1,250-worth of books to children in our hospital – after pupils did a twoweek sponsored read-a-thon.
Pupils at Glade Hill Primary School in Bestwood Park raised £3,000 in total, funding new books for their school as well for our children’s hospital.
“We organised the read-a-thon to promote a love of reading,” said teacher Alice Whiles. “We also wanted our children to put themselves in someone else’s shoes, so we expanded it so that youngsters in hospital could share that enthusiasm, and escape from reality for a while. To raise that amount in just two weeks is pretty amazing.”
Eight pupils delivered the books – each containing a personal inscription – to the QMC school, which is a Hospital and Home Education Learning Centre (HHELC) - a Nottingham City school and part of the Nottingham School's Trust.
“If the child is feeling unwell, having a story read to them is a brilliant way for
us to get to know them and for them to begin to trust us,” said HHELC teacher Jess Bowering.
“This is brilliant – our young patients can still read, or enjoy being read to,” said teaching assistant Kathy Harwood. “It gives them a sense of normality.”
“I think it is important that they have books while they are in hospital, and I hope it helps them feel better,” said eight-year-old Aliyah.





