
14 minute read
IDN OPPORTUNITIES
from Rep April 21
Building a Resilient Supply Chain
This year’s Contracting Professional of the Year helped to develop and implement unique solutions to supply chain challenges brought on by the pandemic.
Amanda Chawla, Chief Supply Chain Officer, VP at Stanford Health Care, Stanford Children’s Health & Stanford-Valley Care
In 2020, collaboration was top of mind for Amanda Chawla, chief supply chain officer/ vice president, Stanford
Health Care, Stanford Children’s Health and Stanford Health Care – ValleyCare. For instance, at the time of Federation of American Hospitals Conference last February, as Chawla watched the coronavirus developments overseas, she tried to plan for what was coming, not only for Stanford Medicine, but for the local community and industry in general. “I probably didn’t imagine the pandemic to the degree that it is today,” she said. “I was thinking about what was happening abroad at the time of Federation, the potential impact, and what were ways I could collaborate with my colleagues should COVID become prevalent in the United States? How could we work together to secure the Supply Chain?”
Chawla, this year’s The Jounral of Health Contracting’s Professional of the Year, answered those initial questions with ideas that helped Stanford Medicine navigate the COVID-19 pandemic, and benefited neighboring health systems as well.
Stanford Medicine tenets
Stanford Medicine is an academic medical center (AMC) focused on education, research and clinical care. The primary organizations are comprised of: ʯ Stanford University School of Medicine ʯ Stanford Health Care ʯ Stanford Health Care – ValleyCare ʯ Stanford Children’s Health
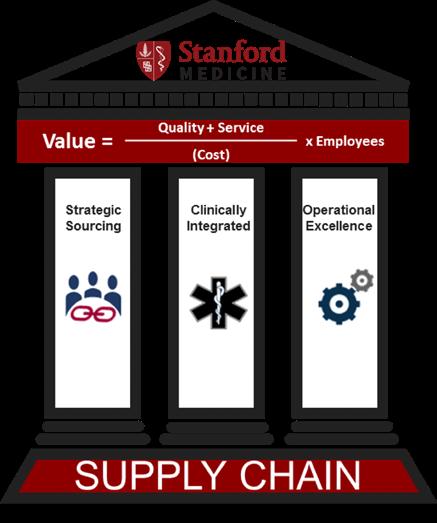
All told, Stanford Medicine’s clinical facilities includes approximately 146 operating/procedure rooms and over 1,200 beds. Stanford Medicine has about 3 million outpatient encounters a year with a non-labor spend of $1.5 billion. Supply chain is a shared corporate service across Stanford Health Care, Stanford Children’s Health and Stanford Health Care – ValleyCare. “Supply Chain is a strategic, operational, and executive function that impacts every single non-labor resource and every function in any organization. Healthcare Supply Chain requires a patient-centric approach and a dyadic clinical partnership that incorporates value (value = cost, quality, efficiency & outcomes) in every aspect of the business. Supply Chain is about executing board functions from planning, procurement to operations of logistics by keeping the patient at the heart of the equation – we provide the right item at the right time to healing hands that provide care to our patients. Supply Chain is really the supportive arm and sits across the entities.”
There are three tenants that bring those entities together, Chawla said. “One is our drive to be digitally driven,” she said. “The second is to be value focused, and value as defined by quality, safety cost, experience, whether it involves patients or stakeholders. The third is to be uniquely Stanford, which is the cutting-edge medicine component of changing the way we do things through innovations, education, and research. Having the privilege to lead in an AMC, I have the opportunity to collaborate with professionals across the health system and university and access to resources that assist with the advancement of our profession.”
– Amanda Chawla
Innovations and Innovation Task Force
Internally, Stanford Medicine leveraged resources, knowledge and the skillsets of its professionals to help propel the health system’s COVID19 response and solve problems that couldn’t have been solved through strategic procurement. The organization created an Innovation Task Force. Because the global supply chain was being stretched to the limit, Stanford Medicine leaders asked themselves, ‘What solutions could the organization come up with internally?’
As it turned out, plenty. For example, Stanford Medicine was short on media for the labs needed for COVID-19 testing. “Our lab and procurement team partnered with the School to pull raw materials used in research to make our own media for testing in house,” Chawla said. Stanford Medicine has been making its own media for COVID-19 testing ever since.
Another product shortage involved testing swabs. Supply was limited and, across the industry, supply chain departments were up against the same barriers. Stanford Medicine partnered with several companies in the Bay Area, such as 3D printing organizations and engineers, to try to solve its own supply chain problems.
Through these partnerships, Stanford Medicine was able to produce 3D-printed swabs. Another example of innovation was with PPE and disposables being short on the market, Stanford utilized 3D printing to solve the market limitations with standard face-shields, equipment parts, and CAPR/PAPR shields.
“We were able to solve some supply chain problems not only through direct international strategic sourcing, but leveraging collaborations and through the activations of an Innovations Task Force,” Chawla said.
In early March, as the pandemic worsened and shortages of critical
supplies surfaced, Chawla approached the CEO of an AI technology organization about creating a supply exchange for local healthcare providers. “When you’re in an urgent situation where traditional sourcing channels are limited, the idea is to be able to reach out to your colleagues across our industry and trade product. We know that not all purchasing is equal,” she said. “We have to come together as a healthcare provider industry supporting not only our systems and our community but support one another as healthcare supply providers. While this solution is intended for emergent needs, we still need to evolve and develop data sharing and intelligence that leads to a resilient Supply Chain. We are data-rich but intelligence poor – we must solve and address the gaps that will allow for visibility in the ‘Supply Chain’ linking raw materials to utilization to demand forecasting. We must address the simple dayto-day operations such as removing the ‘hunting and gathering’ of par management in logistics. Building an intelligent supply chain that allows us to have a push system, automated information, leading to reliability, performance, transparency, and value, is a must. Can we create a cultural change in our industry that forces transparency and collaboration? When we face the next global pandemic together, we’ve got to be able to collaborate, have solutions in place that protect not only our institutions and communities, but each other across the industry.”
The exchange would prove to be of immediate value for Stanford Medicine and other hospitals as supply shortages varied. Stanford Medicine did a number of exchanges where it had surplus of certain PPE size or item with another system who may have had another PPE size or item. Stanford Medicine traded products such as N95s, cleaning and disinfectant wipes and masks with other systems through the pandemic.
Keeping people at the center
When the pandemic hit, Stanford Medicine had to move towards a distributed workforce model almost overnight. Its category management, master data management, and purchasing teams all went off site. They’ve been working from home ever since,
Stanford Medicine

amid conditions that require tight coordination, communication, connection and collaboration.
The infrastructure component was critical. Stanford hospital leaders discussed how they could have their command center set up within supply chain so coordination could be maintained from leadership to frontline staff. To do this, they invested heavily in how communications occurred in addition to the structure itself. “We’ve always had monthly newsletters,” Chawla said. “We revamped those for use in our daily huddle structure and enhanced communications and connects through a myriad of different tools from daily cascading of huddles to podcasts to bi-monthly newsletters and increasing frequency of all hands leadership meetings.”
The podcasts have been a hit as they shine light on the frontline team members and present an opportunity for leaders to provide a personal touch to the messaging and organizational communications broken down in a meaningful way. 2020 has been an unprecedent year of disruption, angst and of change. Stanford Medicine navigated through the first supply disruption of the Cardinal packs and gowns to the pandemic to social justice to California fires to the election unrest. With the amount of disruption the nation has faced it has brought forward economic hardships, loss of homes, illness, job loss, unreliable childcare and much more.
“It’s not just one thing,” Chawla said. “Recognizing the impact of the disruptions, we have focused on well-being, health, the team and support. As a leadership team we have ensured that we’re keeping people at the center of what we do. Part of that for me, is empathy, respect, recognition and the communication, collaboration, and transparency – reaching out. Because at the end of the day, we’re all people, and we’re all in a human business.”
Resiliency
Taking a moment to step back and reflect on the past year, Chawla said it is important that we recognize the Supply Chain responded and performed in the way that it was designed to, with lean principles. Pre-COVID-19, the key tenants of supplier/provider relationships were efficiency and cost.
The silver lining that the pandemic has brought forward is an opportunity to change or double down on a perspective and approach. “I do not see cost or price of products and services being removed from the conversation – that is still going to
be part of the compensation for economic viability,” Chawla said. “But I would propose the conversation will shift in a more accelerated manner towards total value and reliability.”
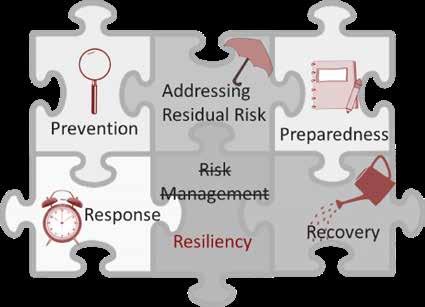
Stanford Medicine made two major decisions in the midst of the pandemic to focus on risk, resiliency, transparency and diversification. The resiliency part of the conversation was probably one of the most important elements that is being embedded within contracts with transparency and data as part of contractual language.
“Outside of contracting, it is important that in part of that evolving relationship with suppliers there are more in-depth conversations to build trust and understanding principles. The conversations may go something like, ‘I can’t do X for you; however, an area where we may be able to collaborate or provide support towards the problem or solution is on Z.’ It’s that trust and that knowledge of whether the supplier is a company you can rely on. Do they have safety stock? How do I ensure that my organization is going to be protected and that we are not going to impact patient care? How do we know what the supply is in terms of availability and demand? Importantly, how do we come together?”
Moving forward, there will be a greater demand for further insight into quality and control on inventory. Providers will want the right and intelligent information and visibility upstream Supply Chain, all the way to raw materials that leads to reliability and resiliency.
Indeed, conversations on visibility are happening all around the industry, Chawla said. There are questions to work through, such as what platform to use, data systems integrity and standards around the data. “There’s a lot that goes into it. And right now, as I see what we’re doing at Stanford, and what my colleagues are doing, a lot of it is the focus on resiliency. We’ve invested very heavily in a resiliency program and model.”
Data integrity and transparency are integral. Not just understanding what’s in the pipeline, but what the raw materials are, where they come in during the manufacturing process, how the product is transported, and what is the location of the distribution centers where the inventory is stored before it actually reaches hospitals and health systems. Understanding the current inventory on hand at any given moment to the consumption’s trends and demand fluctuations.
“I believe more organizations will take pause and re-assess their just-intime inventory model differently,” Chawla said. “Because if you think about it, most hospitals designed their Supply Chain to be a lean Supply Chain, to be Just-in-Time and to only keep a certain amount of inventory on hand. When the pandemic hit, our Supply Chain responded in the way that it was designed. It was not designed around resiliency. It was not designed around pandemics.”
Stanford Medicine did a risk stratification analysis of all the different types of disruptions that can occur from daily manufacturer back orders to a recall to situations that are specific to the Northern California region, like earthquakes or wildfires. The Supply Chain team then broke the stratification out into four quadrants, and discussed what was most likely to occur, the potential impact, and the hospital’s preparedness and response capabilities.
Based on that grid, the Supply Chain team came up with a number of different factors to examine and resolve as they built their resiliency program. This included data access, data management, analytics, processes across the intra-Supply Chain, and standard work. Another element was the investment of a resiliency program that supports business continuity and manages towards a resilient Supply Chain including risk mitigation scenarios and planning. Facilities also factored in. “We have invested capital into a resiliency warehouse in which we’re keeping certain amounts of supplies and operationalizing a hybrid model between just-in-time with our distributor, direct order management, and the resiliency warehouse.”
Supplier diversification was an important consideration. “Another important element our item management and assessment is using the 80/20 rule. How do we accelerate clinical equivalence substitutes, so when we have a product disruption with product X, we know what’s clinically acceptable as an alternative?”
The road ahead
Chawla said COVID-19 has accelerated the need to further invest in the Supply Chain on things that we should be doing and have needed to do. “It has brought the awareness to our organization as a lifeline – without the medical supplies to our care providers we are handcuffed on the core mission of providing patient care and that is the case for all healthcare institutions.”
Obtaining funding, support, clinical partnership, and investment for Supply Chain has been important. Stanford Medicine’s Supply Chain is clinically integrated and supported. “So we’re fortunate in that sense,” Chawla said. “But it’s brought that to a heightened awareness. We have forged stronger relationships with our clinical providers, leadership across the organizations and systems, improved some of our business processes that has provided greater visibility in our inventory, and are improving relationships with our strategic suppliers and collaborators.”
Chawla said that the next six to 12 months will be about adjusting to the next normal. “It’s going to involve recognition of what’s gone on in 2020, and how that changed our lives,” she said. “I think we’ve been in the stage of adapting to the new normal, but now it’s about living in that new normal. And it’s about transforming our leadership, business practices for enhancement and optimization for in the next normal of our future.”
Supply Chain and the U.S. healthcare system as a whole must utilize 2020 as a catalyst to lead and change. “Is COVID going away? Probably not. But how we respond, engage and operate can be different. We should utilize 2020 as a silver lining to design the next future.”
Doing the right thing
Chawla was born in India, but grew up in the suburbs of Seattle, Washington. Her family relocated to the United States primarily because of an aunt, who was a nurse. Chawla’s aunt passed away due to a medical error. While Chawla was very young when it happened, her aunt’s death was a pivotal event. “It had an impact on my family and in my personal life. As a result, I think about processes, structure, assuming good intent and as a leader my responsibility to provide support and care to people at the heart and center of leadership,” she said. “How do we create processes and infrastructures that eliminate the potential human errors in our processes? People intend to do the right thing and are good in their desire, but we are human, we do make mistakes. So how do we create an infrastructure that’s around processes and systems and leverage that in the work?”
Chawla got an early start to a career in healthcare as a medical assistant. While in high school and through college, she worked at a psychiatric hospital performing a myriad of functions from intake, admission, to providing direct patient care across pediatrics to adults. She also worked for a private practice, a group of physicians who wanted to start clinical trials. Chawla would end up opening their clinical trial site operations, establishing the operating procedures to marketing and recruitment. “Some of the things that the physician owners and leaders taught me was really how we lead and connect with people, whether it was on the frontline taking care of a patient, or whether it was running the office to speaking engagements. I learned early on that it was really about people. You can learn the technical aspects of the job, but you have to have the behavioral components and the leadership attributes to bring and lead people.”








