Home Blood Pressure Monitoring
How blood pressure readings taken at home can reduce a patient’s anxiety and lead to better health outcomes.






How blood pressure readings taken at home can reduce a patient’s anxiety and lead to better health outcomes.





Relationship – the way in which two or more concepts, objects, or people are connected, or the state of being connected.
Stop for a minute and think about the relationships in your life. Better yet, think about the relationships over the course of your life. Some changed the trajectory of your life, some just made your life better, some taught you hard lessons, and some helped you with the career you have today.
We live in a time where we work remotely and make dozens of Zoom calls a week. But the value of relationships hasn’t gone away. In fact, they may be more important than ever. I think about meeting Steve Martin during an industry event 20 years ago. We were hitting range balls one evening and started talking. That chance encounter not only provided me with a lifelong friend, it changed my career and the entire direction of the company I was working for at the time. Due to the relationship I formed with Steve, over the next two years we started growing our branded business with PSS 15% to 20% a year. Then one day Steve called and said: “Scott, our private label business is yours to win.” That single chunk of business doubled our sales in the U.S. None of this would have happened if it weren’t for the relationship.
As important as relationships are with current and potential customers like Steve, they are every bit as important with the people we work with every day. In a similar story, 20 years ago during a HIDA Executive Conference I met Brian Taylor (shockingly working on his putting), on a practice green. I know this sounds like all I do is golf. Brian and I formed a relationship that week and he later became one of my mentors, which led to me taking over Repertoire for him 15 years ago. What a career change for me in one chance encounter.
I realize I write about this topic about once a year, and maybe I do it for myself as a reminder to be thankful for the value of my relationships. Hopefully it’s a good reminder for you as well. Building relationships is one of the keys to a fulfilled life. “Life is relationships; the rest is just details,” wrote Gary Smalley. That couldn’t be truer. Step back and reflect on your relationships and the ones yet to come. They change our lives.
Dedicated to the Industry,
R. Scott Adams Publishereditorial staff
editor
Mark Thill mthill@sharemovingmedia.com
managing editor
Graham Garrison ggarrison@sharemovingmedia.com
editor-in-chief, Dail-eNews
Pete Mercer pmercer@sharemovingmedia.com
art director
Brent Cashman bcashman@sharemovingmedia.com
circulation
Laura Gantert lgantert@sharemovingmedia.com
sales executive
Amy Cochran acochran@sharemovingmedia.com
(800) 536.5312 x5279
publisher Scott Adams sadams@sharemovingmedia.com

(800) 536.5312 x5256
founder Brian Taylor btaylor@sharemovingmedia.com
Subscriptions
www.repertoiremag.com/subscribe or (800) 536-5312 x5259
Repertoire is published monthly by Share Moving Media 350 Town Center Ave, Ste 201 Suwanee, GA 30024-6914
Phone: (800) 536-5312, FAX: (770) 709-5432; e-mail: info@sharemovingmedia.com; www.sharemovingmedia.com


Why baseline tests are the foundation of health and wellness for today’s patient base.
No single lab result has much meaning, other than in an acute care setting. For instance, in the emergency room critical lab data is used immediately for heart attack, stroke, diabetic coma, overdose and a number of other life-threatening conditions.
Stated in other terms, diagnosis, treatment and management of nearly any clinical condition requires the establishment of a patient baseline of test results. Once that baseline is established, clinicians typically follow results to determine whether a chronic health condition is more likely to occur later in life. So, these
lab tests are used to initiate or modify a patient treatment program.

Yes, I’ve put that news out before, but let me put another consideration in play: there are several very good reasons a quiet group of Americans – the “unworried, unaware unwell” – need to be uncovered for their own good.
By Jim PoggiBefore I explore this argument further, who exactly are the “unworried, unaware unwell”? This group could be defined several different ways, but my practical definition is those younger adults who do not display obvious symptoms of the early onset of a chronic disease, who also believe their life and health habits will preclude development of a chronic disease. These folks are most likely to exercise routinely, follow their fitness statistics using a wearable device, don’t smoke, drink moderately if at all and engage in healthy eating habits for the most part.
So, many of these folks have made the decision not to have routine physicals, clinician visits and probably have no clue of their baseline lab
results. Theoretically, they should be a shining example for all of us. If we all took such good care of ourselves, everyone would lead longer, healthier lives, right?
If that were only true, but it’s not. So, what’s the problem? Well, there are 23 pairs of problems: their chromosomes. While we cannot change our eye color, hair color or most other physical characteristics, we also cannot control the underlying metabolic traits conferred by our genes. Some folks get the lucky genes and live long, relatively healthy lives regardless of their lifestyle. There are plenty of rock stars who are living proof of this. Others are living proof that sometimes bad things happen to good people. They develop a chronic disease or debilitating
condition years before their peers, despite healthy life habits.
In this column, I intend to further explore the merits of physician visits and lab testing for the diseases that comprise the 10 leading causes of death in early adulthood, with routine monitoring of these conditions and why establishment of a baseline of lab results is so important.
The incidence of a couple of potentially very dangerous chronic conditions will serve to remind us that chronic diseases become more severe with age, but often display their first abnormal lab results much earlier. So, if you are a member of the “unworried, unaware unwell” or think you might know one, keep reading. What you read may help you or folks you know to get ahead of a chronic disease before it creates complications that may detract from your quality of life.
For years, hypertension has been considered the “silent killer.” It has no overt symptoms, but undiagnosed, can lead to heart attack, stroke, kidney disease, blindness and death. It occupies a lofty place on the ten leading causes of death, involved in heart (No. 1), stroke (No. 5) and kidney disease (No. 10). It can easily be diagnosed at any age by a simple blood pressure test as part of a routine physical, with lab studies for lipids and metabolic panels as well as routine blood pressure measurements.
No biggie, right? Wrong. According to the CDC, nearly 116 million Americans have high blood pressure. That’s over one in three Americans. Worse yet, only 24% of adults with high blood pressure have it under control. Yeah, but hypertension is an old folks’ disease. Nope, not so. Twenty-two percent of adults

between the ages of 18 and 38 have high blood pressure. In the 40-59 age group, it rises to 54.5%. So, you can jog, eat healthily, and check your stats on your wearable device, but you cannot outrun the statistics.
Even the “unworried, unaware unwell” need routine health care visits with blood pressure checks and routine lab results. Surely, their commitment to a healthy lifestyle brings them into physician offices frequently. Not so much. From the age of 10 all the way up to 54, the average American visits a primary care physician once or fewer annually. The earlier age group data is skewed by school physicals, and data for older groups includes preemployment screening. So, in the real world, this group continues to feel as if they have no need for routine healthcare visits.
Let’s assume your “unworried, unaware unwell” friend has dodged the hypertension bullet. Unlikely considering the statistics, but let’s make that assumption. Are they in the clear? Not really.
Diabetes, especially type 2, is on the rise and is often a comorbidity with hypertension. The CDC estimates 96 million prediabetic Americans are walking alongside of 37 million already diagnosed. That’s a total of 134 million Americans, more than the number of hypertensives mentioned earlier. Diabetes ranks No. 8 on the list of leading causes of morbidity and mortality and is associated with nearly 50% of all deaths and disability in America. While that may be true, it’s just for folks with poor health habits and older folks, right? Not so fast. Eating habits and lack of exercise are factors for sure, but genetic predisposition plays a
Of 1.5 million Americans diagnosed with diabetes in 2017, one-third were adults under the age of 44. Youth is not an absolute protection against diabetes.
First, it’s very clear that routine health care visits, with quality vital signs measurements and routine lab results including baselines at an early

age are sentinels that can make every American aware of their baseline readings for critical health indicators. Hopefully, it is now also clear that while age and taking responsibility for a healthy lifestyle can make a difference, they are no guarantee against development of a chronic condition, even early in life.
Awareness of the need to have an annual healthcare visit is an important
The ID NOW ™ is an easy-to-use, molecular platform that rapidly detects infectious respiratory diseases so you can make informed treatment decisions quickly.
ID NOW™ INFLUENZA A & B 2 5–13 minutes
Detects up to 20% more true positives than rapid antigen tests1,2
ID NOW™ STREP A 2 2–6 minutes
Requires no culture confirmation for negative results3
ID NOW™ RSV <13 minutes
Detects up to 25% more true positives than rapid antigen tests4

ID NOW™ COVID-19 2.0 6–12 minutes EUA authorized for near-patient testing environments

element to improving individual health outcomes and those of the American public at large, but they are only part of the solution. Some Americans are hampered by either financial concerns or live in areas where access to healthcare is limited compared to more affluent urban and suburban communities. Solutions to these challenges are well beyond the capabilities of the average American, but those of us with a choice need to opt for routine healthcare visits and establishment of a baseline of our healthcare data. As I have learned from personal experience, reviewing your wearable device statistics on your phone is no substitute for healthcare visits.
As mentioned above, there is a certain level of denial among the younger, more fit population that contributes to reluctance to engage in routine healthcare visits and lab results. What about these folks? It is my opinion that the expanding range of healthcare options including community clinics, urgent care centers and retail convenience clinics can and should play a role here. In the recent past, a national retail clinic chain developed a program to offer hemoglobin A1c testing on a walk-in basis. Unfortunately, it received a lukewarm reception from the public. Based on a deeper understanding of the statistics available to us, I wonder whether it is time to re-address this option. There is no question that earlier diagnosis can lead to earlier intervention. In addition, diabetes is increasing rapidly, and the U.S. life expectancy statistics have tumbled since COVID and have responded more slowly than in other developed countries. It would be interesting to see whether a combination of education and awareness at readily available clinical settings along with fast, inexpensive blood pressure
and hemoglobin A1c testing could provide an improvement in earlier detection of serious chronic diseases, improving duration and quality of life.
Setting aside the dream state of a large-scale program to screen Americans to diagnose chronic conditions early, as appealing as it may be, what options are currently available?
ʯ HPV/PAP tests for cervical cancer
ʯ Chlamydia/Gonorrhea testing (at-risk individuals)
ʯ HIV, syphilis, and HCV screening (at-risk individuals)
ʯ Tuberculosis screening (at-risk individuals)
ʯ Colorectal cancer screening (age-related and risk-related)
ʯ Drug screening (at-risk individuals)
Bottom line: in our role as consultants, we are often asked to recommend which lab tests our customers
Medicare pays for:
ʯ An annual wellness visit with an assessment of physical and cognitive health that MAY include lab tests.
ʯ MOST lab tests are covered by Medicare based on physician prescription.
ʯ Medicare offers a diabetes prevention program which includes weekly group meetings, hemoglobin A1c testing and body mass assessment.
ʯ HIV and Hepatitis C testing are also covered for eligible Medicare recipients.
ʯ Eligible patients should discuss options with their healthcare provider to learn more.
ʯ Many of these screening tests are for specific risk groups
ʯ Blood pressure screening
ʯ Prediabetes screening
ʯ Urinary tract infection testing during pregnancy
should offer. But, do we take the proactive step to recommend who and when to test? We may feel this is out of our responsibility level and that some of our customers may consider we are overstepping our bounds. Engaging in these sorts of conversations can lead to some interesting discussions that can cause at least some of our customers to take more active steps to screen their patients. I think it’s worth it for us and our customers. We establish or reinforce our value as forwardthinking consultants. Our caregiver customers receive information that can and likely will make a difference in the health of their patients. That first step to have baseline tests performed is a small investment. It takes less time than a sit-down dinner, concert or even our daily fitness walk but can pay significant dividends down the road. It’s worth thinking about how we can impact the lives and health of the “unworried, unaware unwell.”
Even the “unworried, unaware unwell” need routine health care visits with blood pressure checks and routine lab results.
*In the USA, the BD Veritor™ System for Rapid Detection of SARS-CoV-2 has not been FDA cleared or approved but has been authorized by the FDA under an Emergency Use Authorization for use by authorized laboratories; use by laboratories certified under the CLIA, 42 U.S.C. §263a, that meet requirements to perform moderate, high, or waived complexity tests. The product is authorized for use at the Point of Care (POC), i.e., in patient care settings operating under a CLIA Certificate of Waiver, Certificate of Compliance, or Certificate of Accreditation.
This product has been authorized only for the detection of proteins from SARS-CoV-2, not for any other viruses or pathogens; and, in the USA, the emergency use of this product is only authorized for the duration of the declaration that circumstances exist justifying the authorization of emergency use of in vitro diagnostics for detection and/or diagnosis of COVID_19 under Section 564(b)(1) of the Federal Food, Drug and Cosmetic Act, 21 U.S.C. §360bbb-3(b)(1), unless the declaration is terminated or authorization is revoked sooner.

One system with multiple assays delivering reliable results for SARS-CoV-2,* Flu A, Flu B, RSV, and Group A Strep within 15 minutes at the point-of-care.
McKesson Medical-Surgical held its national sales conference in sunny Las Vegas in late May, with more than 1,600 McKesson sales team members and 600 supplier representatives.

In the spirit of the Bold Moves meeting theme, sales team members were encouraged to hunt growth opportunities and learned how McKesson’s strategy and investments are supporting customers’ success and the sales team’s growth both in the current fiscal year, and far into the future. The McKesson sales teams and suppliers connected on the extensive tradeshow floor and in supplier sessions through the week, previewing the latest products and talking about the newest advancements.
Attendees also participated in a community activity that supported the Foundation for Hospital Art. They helped complete a hand-painted mural that will be placed in a healthcare facility in the Las Vegas area. The foundation was established in 1984 and is dedicated to softening the hospital environment with colorful paintings, wall murals and ceiling tiles.
Thank you to all suppliers and McKesson team members who made this year’s sales conference a very special event.











Empowering women to lead and succeed in the healthcare industry, Professional Women in Healthcare® (PWH®) recently held its fifth annual PWH® Leadership Summit in San Antonio, Texas, May 1–3, 2023. The Summit was an invaluable opportunity for industry leaders to gain knowledge and insight

into maximizing their career growth and development.
This year’s Summit featured dynamic sessions designed to empower, inspire and propel career development. Over 250 attendees were provided with opportunities to build their personal brand, develop meaningful relationships
within the industry and gain critical skills for leading into the future. Attendees enjoyed networking events, mentoring opportunities, and workshop activities and heard from keynote speakers and prominent industry leaders to apply their learnings in their careers and personal life.
Allison Therwhanger, PWH® Chair and Vice President of Corporate Accounts for Innovia Medical, stated, “I continue to be inspired by our members for their commitment to our industry and their empowerment journey. Together, we are fostering an environment that encourages growth and drives a more diverse and inclusive healthcare industry equally led by women.” Allison added, “On behalf of the PWH® Board, I would like to express our gratitude to our attendees, our Summit Sponsors, PWH Corporate Partners, dynamic speakers and dedicated member volunteers for making this year’s event so impactful. I’d especially like to thank the PWH® Summit Committee, led by April Shomper, who also serves as Vizient’s Event Director.”
During the Summit, two prestigious annual awards were presented. The first was the Jana Quinn Inspiration Award, given to Natasha Jackson, Director of Education & Training at Enclara, for leadership and inspiration within her company and the industry. Natasha is a role model to her family and a mentor to many, a true servant leader. The Anne Eiting Klamar Leadership Award of Distinction was presented to Julee Prefer, President of Healthcare Solutions. Julee serves as a mentor to many in the PWH organization. She is one of the original PWH founding members, past chair and led the charge for the first Leadership Summit. She continues to be a leader within the organization as an advisor
to the board and through her advisory position to the Leadership Summit committee.
Vizient sponsored the opening keynote speaker, Judi Holler, a podcaster, best-selling author and entrepreneur, who energized the audience with an interactive session, “Think Like a CEO and Take More Confident Action,” featuring improvisation techniques, allowing participants to think on their feet and make confident decisions. Judi taught us to shut down self-doubt, step out of our comfort zones, and acknowledge and celebrate fear by changing the rules to celebrate our courage to live more balanced and successful lives.
The Leadership Insights series continued this year with keynotes from various industry leaders. Sponsored by Midmark, attendees were energized by thought-provoking presentations, gaining valuable leadership and professional development insights. A few takeaways from the session include:
ʯ Sanchia Patrick, Vice President of Strategic Marketing, Henry Schein, The Link Between Personal Brand & Purpose, “The power of brand is connected to purpose. Identify your purpose. Refine it. Draw close to it.”

ʯ Rob Saron, President and Director/SVP Global Distribution, Bovie Medical, Leading Through Change, “Take care of yourself. Focus on what matters. Do, schedule, delegate, eliminate.”
ʯ Laura Reline, Vice President, Supplier Management, NDC, Inc., Powerful Partnerships, “Take time to nurture relationships; make authentic connections.” Also, “If you don’t have passion for what you do, find something new.”
ʯ Stephen Downey, Chief Supply Chain Patient Support Services Officer, Cleveland Clinic, Workplace Joy & Motivation, “You control your conference room table. Control your joy and your strength.”
ʯ Monica Davy, SVP, Chief Culture, Diversity & Impact Officer, Vizient, The Power of Authenticity, “Culture is how you feel on Sunday night going into Monday morning.” During a fun “snowball” activity, attendees identified something they hide at work – lack of confidence, anxiety, challenging relationships and health, to name a few. Attendees learned the power of showing up to work as their authentic selves.
Education is an essential part of learning and development at the Summit. It helps keep knowledge current, ensures that professionals remain competitive in their field and allows for acquiring new skills. Several leadership workshops were held, including one hosted by Joe Machicote, Chief Diversity Officer for Premier, who gave a powerful presentation on creating an environment to sustain Diversity, Equity, Inclusion and Belonging (DEI&B), educating the audience on understanding personal bias, leading by example, having respect and trust and influencing others. Sue Hulsmeyer, Vice President of Human Resources and Corporate Communications for Midmark and Natalie Martin, Director Creative Services for NDC, Inc., hosted a workshop on personal brand and professional presence, providing education on self-awareness exercises and defining/refining your personal impact.
Other valuable sessions by industry leaders included profit and loss management, staying connected in a digital world, speed mentoring, conflict management strategies and the value of coaching. These breakouts allowed attendees to engage


and interact with facilitators and other attendees to gain knowledge they can implement when they return to work.
Tuesday’s sessions ended with a Fireside Chat, “The Curious Will Climb to the Top,” sponsored by

GOJO Industries and moderated by Patty Olsen, Chief People Officer for Vizient. During the conversation, Stephanie Hertzog, CEO North America Energy and Resource for Sodexo, and Billy Abrams, President of Distributed Products for Medline, shared contrasting insights from inside and outside the industry, speaking about embracing what you don’t know and anchoring yourself
in flexibility, rather than the status quo. They shared insights on creating career paths, mentors, investing in the workforce and the importance of being a good listener.

Tuesday evening provided attendees an opportunity to enjoy networking under the stars on the Sky Terrace at The St. Anthony Hotel, sponsored by NDC, Inc. The rooftop energy was electric as leaders connected and
discussed professional and personal insights they had gained.
On the final day, Scott Adams, Publisher of Repertoire Magazine, moderated a great, interactive discussion sponsored by B. Braun, featuring a healthcare leadership panel to discuss leading through everchanging times. The panel included Janis Dezso, Vice President, US Non-Acute Sales for Aspen Surgical; Anne Eiting Klamar, M.D., Chair of the Board for Midmark; Joan Eliasek, President, McKesson Canada and Cindy Juhas, Chief Strategy Officer for CME. These industry icons – and recently inducted members of the Medical Distribution Hall of Fame – brought humility, friendship and humor as they discussed bringing their organizations forward and motivating employees despite future uncertainties. The audience appreciated their wisdom, authentic advice, encouragement and sharing of valuable lessons learned.
The Summit concluded with a closing keynote by Sara Canaday, who used a dynamic combination of insights, examples and research based on her book, Leadership Unchained to challenge attendees to look at things differently and stressed the importance of being accountable for your goals.
“We are already looking forward to next year’s Summit to include even more networking, hands-on education and inspiration in Louisville, Kentucky,” said April Shomper, Chair of the PWH® Summit Committee. “We are grateful for the support of the attendees and look forward to hosting another Summit that has proven to be so valuable to the growth of our industry leaders.”
Save the Dates: April 29 – May 1, 2024, Louisville Marriott Downtown. Registration opens this fall.

Serving US healthcare providers for over 30 years, Dukal offers solutions to protect and manage a comprehensive scope of wound care needs.

> Antiseptics & cleansing
> Applicators & swabs
> Bandages
> Burn care
> Casting
> Impregnated dressings
> Medical tapes & adhesives
> Small procedure kits
> Wound closure
> Wound dressings
Dukal is working with healthcare professionals around the world in manufacturing and supply chain solutions, to mitigate disruptions that impact business and patient health. Helping you manage everything from product to patient. Because when people have access to better health, they have access to a better future.

> Visit dukal.com to learn more
 Scan with your phone’s camera to view our wound care solutions.
Scan with your phone’s camera to view our wound care solutions.
Developing sales leaders is a critical component in the job of a sales manager. Sales managers need to be equipped with the skills and knowledge to develop and train upcoming leaders in the organization, but the role of sales management has changed over the years.
Repertoire Magazine recently spoke to Patrick Malone, a leadership mentor and independent business advisor with over 40 years of experience, about the current state of business and sales management. Malone started in customer service with American Greetings in Cleveland, Ohio, where he worked his way up to the role of vice president for the Southeast region. In the last 20 years, he’s worked with a company called The PAR Group, focusing on sales leadership development.
Most recently, he’s hosted several live talk radio shows in a two-hour block every weekday morning.
Sales tactics and the products that reps sell have improved over the years, but Malone argues that the process of managing a sales team hasn’t changed. “It’s basic nuts and bolts. Managing and coaching a group of salespeople hasn’t really changed over the years.” While the



people and the way that a sales manager connects with them might have changed, the skills required to manage a sales team haven’t.
On the other hand, the responsibilities of a sales manager have changed quite a bit from Malone’s perspective, especially when it comes to forecasting. He said, “I think the one thing I’ve seen that’s different is sales managers today are carrying forecast responsibility in addition to their management roles. Sales managers get promoted because they were good salespeople, and when they move into that role, all their emphasis is on their portion of the forecast. The sales management piece of the equation becomes secondary.”
According to Malone, too many leaders think that sales is still a numbers game. Nowadays, sales is much more of a skills game. It takes repetition to really nail down the details of a successful sales call.
What are those skills? Malone said, “The ability to ask questions in a way that the customer recognizes that you really do care. Once you’ve asked the question, you need to acknowledge the answer that you get, without saying ‘I heard you.’ These are subtle skills. I know a lot of people can ask questions, but it becomes more of an interrogation than a demonstration of real interest.”
One component in the sales setting that has changed drastically over the years is the customer. The customer experience is at the forefront of every transaction, which can mean the difference between whether you close a deal or not. The internet has raised the expectations of customers before they’ve even made contact with the sales rep.
Malone said that sales reps need to approach customers with a personalized touch to be most effective. He explained, “Sales reps need to understand the customer’s business before the meeting. Customers will be like, ‘Don’t expect me to educate you. You better be interested in my business – not based on what your company told you was of value but tell me why I should do business with you.’ You don’t have to change your product; you just have to find out what is important to that customer and how your product meets that need. Leave the other stuff alone.”
What does it take to make a good sales manager? To be truly effective, salespeople need to be able to trust their managers. Here are the best qualities for a sales manager:
ʯ Sets clear and concise goals –The best sales managers keep communications very clear and simple. With well-defined goals, your sales team is capable of accomplishing so much more than you might think possible. “There’s a thing out there that I call toxic ambiguity. Too many salespeople get the idea that a
The best thing that a new sales rep can do is to go visiting around in their territory without even trying to sell anything. This approach can help to establish a relationship between the sales rep and the customer without the pressure of a deal on either side. Starting these relationships on the right foot is crucial to the success of the sales rep. Malone said, “Gather the knowledge, ask the right questions, understand the nuances between one customer and the next. Don’t try to be interesting, be interested.”
People typically respond better to those situations if you show an interest in what their business does and how they solve the problems of their own customers. Take notes and use this time to strategize, but don’t forget to leave a good first impression on your prospects.
manager wants more sales. What does that mean? It’s so vague that it’s hard to quantify.” Clear, concise and attainable goals are the best way to drive efficiency and productivity.
ʯ Makes good assessments –Sales managers need to make good assessments of what their sales reps need. Malone said that there are three areas where sales reps have needs: education, skills, and coaching. Keep this approach simple for the best results.
ʯ Continues to raise the bar –Sales managers need to constantly raise their expectations for the sales team. “They need to keep raising the bar and presenting bigger challenges, because that’s how the salesperson is going to grow.”
“Gather the knowledge, ask the right questions, understand the nuances between one customer and the next. Don’t try to be interesting, be interested.”

 By Brian Sullivan
By Brian Sullivan
Unless you have been living under a rock, you’ve probably heard about Artificial Intelligence and more specifically, ChatGPT. While debates about it someday destroying the world linger (Elon is a bit nervous), let’s harness this techpowerhouse to rise above the competition in medical sales. Personally, ChatGPT has become an amazing asset in my own company’s sales toolkit.
For those still curious about what it is, ChatGPT is an AI-driven chatbot capable of understanding and responding in human language. In sales, particularly medical sales, it’s a game-changer in finding new customers, boosting sales, and refining the overall customer experience.
Here are 7 ways ChatGPT can immediately help you better serve your customers – and your commission check.




I am amazed at how many companies I work with who can’t tell me exactly what they do and why they are better than the competition. Use ChatGPT to shape your ideal sales pitch. For example, while writing this article I asked ChatGPT to write me a 30-second elevator pitch for one of my clients. I can promise you that this version is way better than the 43 different versions I heard roll off the tongues of my students in a recent seminar.
At my company (PRECISE Selling), we identify prospects and then view their social media, blogs, and PR posts. We then present these findings to ChatGPT in the form of context. For example, “A medical device manufacturer has just released a new product, but their blog posts indicate they’re struggling with demonstrating its unique benefits to healthcare professionals. How could I craft an introductory email offering our sales training services?” BAM! ChatGPT will then generate a response based on the information and context you’ve provided.
Ask ChatGPT questions like “What are the latest tech trends benefiting healthcare providers?” or “What are current trends in healthcare?” to brainstorm content ideas. (Although keep in mind that ChatGPT only includes data up until September 2021) Share this content on LinkedIn or with your clients to establish yourself as a valuable resource in the field.
ChatGPT can review your profile, suggest keywords to enhance visibility, help create an attractive headline, and draft an engaging summary that articulates your passion and proficiency in medical sales. An ‘extreme makeover’ could just be the ticket to make your profile stand out!
ChatGPT can aid in drafting personalized follow-up emails or messages. Ask it to generate templates based on customer interactions and preferences, ensuring you’re in regular contact and top-of-mind for your clients.
Let’s face it, staffing shortages and changing regulations aren’t going away any time soon, which means it’s the adaptable salesperson who thrives. In such times, knowing your customer and their needs, staying on top of industry trends, and offering personalized service can make all the difference, and that’s precisely where ChatGPT shines.
If you are a salesperson who believes there aren’t enough hours in the day and have the burning desire to dominate in sales, technology like ChatGPT is a life changer. It takes tasks that used to consume hours and completes them in seconds. In fact,
Use ChatGPT to analyze past conversations and transactions to offer personalized experiences to your clients. By recognizing their needs and preferences, you can recommend products and services that are highly relevant to them, enhancing customer satisfaction and loyalty.
Utilize ChatGPT as a personal coach or training tool. Ask it questions about sales strategies, negotiation tactics, and new medical products in the market. It can even help you practice pitches or scenarios, allowing you to learn and improve constantly.
I am beginning to wonder how on earth I lived without it (in business).
But don’t forget, technology should never replace the human touch. It’s the combination of advanced technology and authentic human connection that makes a truly unstoppable salesperson. So, use these ChatGPT tips to crush your sales goals and provide a better overall customer experience.
And if you are one of the salespeople who may be saying, “Oh no! I haven’t even figured out how to login to ‘the Twitter’ yet, fear not. Just go to openai.com/blog/chatgpt and ask it any question you want. And don’t be surprised if you become awfully chatty with your new best friend.
Let’s face it, staffing shortages and changing regulations aren’t going away any time soon, which means it’s the adaptable salesperson who thrives.

The instrument cleaning, sterilization, and disinfection product segment is such an important part of the overall infection prevention category. This is an area that if not done correctly, could shut down a facility. This silver lining here? Where there are challenges for your account, there are opportunities for you to lean in and be a resource.
Sales opportunities for instrument sterilization can be found in acute care, surgery centers, and primary care where there are in-office procedures being performed. Primary care is where your guidance is needed the most due to limited resources in comparison to acute care.

The sterilization process can get complex, and unfortunately is a tedious process that gets delegated. This often means that the tough tasks get assigned to the least experienced, lowest paid in the facility. You can be of help by providing educational tools, product recommendations, and formularies to help staff get up to speed and direction.
There are a few areas that need additional focus when thinking about the category:
Like most areas of infection prevention, there is a process of cleaning and disinfection/sterilization. Emphasis needs to be placed on the AND. Cleaning is done by using enzymatic cleaning solutions which breakdown and remove the bioburden on the surface of the instrument
before sterilization. This is a crucial step in the process and helps with the overall performance and lifespan of the instruments. After the instrument is cleaned, it can move along in the process of disinfecting (scopes) or sterilization (instruments).
As a category, sterilization is diverse in all the products that roll up into it. There are pre-cleaners, sterilants, disinfectants, pouches, wraps, testing strips, and indicators in all types, shapes, and sizes. It’s best to look at the entire process and create checklists for all the products needed. Are you not getting all the business? This is a category where some major branded suppliers sell directly to the facility. Distribution
should never lose business to these suppliers. All the benefits of inventory management, product access, order minimums and freight are in your favor. Everyone needs help and direction. This is an opportunity to provide service, make recommendations, and bundle the entire category.
It’s best to review consumption of product. You will find occasions where customers are not complying with CDC guidelines. An example of this is testing strips. Does the account test the glutaraldehyde or OPA with the appropriate testing strip before each use? Periodic or even daily testing is not enough. Biological indicators are also probably
being underused. Sterilization needs to be tested with each load. There are often good intentions but bad habits in the market. Use education to help drive compliance to guidelines.
It’s a good idea to have the Guideline for Disinfection and Sterilization in Healthcare Facilities (2008) on hand. The user-friendly guideline hasn’t changed through the years and is available here: cdc.gov/infectioncontrol/ guidelines/disinfection.
There are several excellent distribution-friendly suppliers that make up the sterilization category. Take advantage of the educational resources and support that are widely available for both you and your customers.
A United Front
EmPower dual enzymatic detergent and MetriCide OPA Plus high-level disinfectant are the ideal combination for cleaning and high level disinfection of medical instruments.

For more information on products, visit metrex.com
Metrex is dedicated to distribution. We are here to support all your Instrument Reprocessing needs. If you want to preserve business, talk to your customers about switching to Metrex.

Here are three reasons why it’s important to talk to your customers about Strep A diagnostics during this year’s back-to-school season. First, although group A strep infections can occur any time of year, they are more common in the United States in winter and spring. Second, while it’s true anyone can contract a GAS infection, children between the ages of 5 and 15 years are most susceptible. And third, based on preliminary 2022–2023 data from the Centers for Disease Control and Prevention, less severe group A strep infections in children have returned to levels similar to or higher than those seen in pre-pandemic years.

The Centers for Disease Control and Prevention is looking into an increase in invasive group A strep (iGAS) infections among children in the United States. These infections are caused by the bacteria getting into parts of the body where it is not normally found, such as the lungs or bloodstream. Not to be confused with routine strep throat, iGAS infections include necrotizing fasciitis (a serious bacterial infection that destroys tissue under the skin), streptococcal toxic shock syndrome (a rare but serious bacterial infection which can develop quickly into low blood pressure, multiple organ failure and
Group A streptococcus (GAS), also referred to as strep A, is a common bacterium. Many of us carry it in our throats and on our skin and it doesn’t always result in illness, according to the UK Health Security Agency. However, GAS does cause several infections, some mild and some more serious. Milder infections include scarlet fever, impetigo (red sores around the nose and mouth), cellulitis and pharyngitis (sore throat). These can be easily treated with antibiotics. The more serious –but rarer – infections linked to GAS come from invasive group A strep, known as iGAS. These infections are caused by the bacteria getting into parts of the body where it is not normally found, such as the lungs or bloodstream. In rare cases an iGAS infection can be fatal.
GAS is spread by close contact with an infected person and can be passed on through coughs and sneezes or from a wound. Some people can have the bacteria present
death), cellulitis with blood infection, and pneumonia.
CDC estimates that in the most recent five years, approximately 14,000 to 25,000 cases of invasive group A strep disease have occurred each year in the United States. Between 1,500 and 2,300 people die annually due to invasive group A strep disease.
While iGAS infections are still uncommon, the number of cases rose in 2022, particularly among children under 10, reports the UK Health Security Agency. It isn’t possible to say for certain what is causing higher case numbers, but it is likely a combination of factors, including increased

social mixing compared to the previous years as well as increases in other respiratory viruses.
Per the U. S. Centers for Disease Control and Prevention, preliminary 2023 data indicate iGAS infections have remained high in children in some areas of the country even after respiratory viruses decreased in those areas. This is occurring during the time when group A strep infections are normally highest (December through April). Additionally, some areas of the country have also seen an increase in iGAS infections in adults, particularly those aged 65 years or older.
in their body without feeling unwell or showing any symptoms of infections, and while they can pass it on, the risk of spread is much greater when a person is unwell.
The CDC doesn’t track noninvasive group A strep, but estimates
that pharyngitis causes an estimated 5.2 million outpatient visits and 2.8 million antibiotic prescriptions annually among U.S. persons aged 0–64 years. Globally, the burden from GAS infections is even greater. The World Health Organization estimates 111 million children in the developing world have impetigo and 470,000 new cases of acute rheumatic fever (a potential outgrowth of GAS) occur each year.
Currently, GAS is not resistant to penicillin and amoxicillin, firstline antibiotics for strep throat, sa7s CDC.
“Many viral syndromes can present similar to strep, however, clinicians and pediatricians look for specific signs (e.g., sore throat without cough, palatial petechiae, sandpaper
‘Rapid results can help provide timely information so patients can isolate appropriately.’Aparna Ahuja
rash), which help determine which diagnosis scores higher on differentials,” says Aparna Ahuja, M.D., divisional vice president of medical, clinical and scientific affairs for Abbott’s rapid diagnostics business. “There is some overlap of symptoms, including fever, sore throat, nausea and vomiting, but absence of cough is one of the key distinguishers for strep compared to viral infections like COVID and flu. In the eventuality of a misdiagnosis and not prescribing the right treatment for strep pharyngitis cases, further spread of infection along with worsening of symptoms/progression is a possibility.”
syndrome (TSS) or necrotizing fasciitis, which are not diagnosed with a rapid test or managed on an outpatient basis. “Most physicians prefer rapid tests, as results are known quickly and decision on further course of treatment can be made
Rapid molecular tests help to provide high-quality actionable results at the point of care, she says. During one visit, the cause of illness can be identified and targeted therapy initiated, which leads to a better patient outcome. “Additionally, having rapid results can help provide timely information so patients can isolate appropriately, which helps avoid spreading strep A infections to family members and the larger community. It leads to fewer missed days of school or work for individuals and their families, and helps reduce antibiotic use in subjects who explicitly ask for a prescription.”
The usage of rapid point-ofcare (POC) tests is increasing, says Dr. Ahuja, adding that she is speaking about strep A pharyngitis and scarlet fever but not severe strep infections such as streptococcal toxic shock
immediately, while the patient is still available to the doctor. For patients –in this case, often children – there’s a desire to understand the cause of the illness and get appropriate treatment to enable quick recovery.”
Because of molecular technology and performance, tests such as Abbott’s CLIA-waived ID NOW™ Strep A 2 test do not require any follow-up culture to confirm negative results, enabling clinicians to treat confidently at the point of care with early positive detection and often during a patient visit, says Dr. Ahuja. “This efficiency supports antimicrobial stewardship. Inappropriate prescription of antibiotics results in ineffective treatment, and may contribute to antimicrobial resistance, which is an increasing public health concern.”
The following starter questions may be useful for medical products salespeople discussing strep A testing with their physician customers, says Abbott.
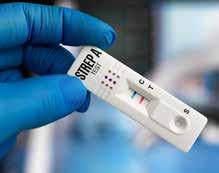
ʯ “Doctor, if you do not get results back on strep A quickly enough, what impact does that have on patient care?”
ʯ “Are you currently able to confirm strep A results needed to determine treatment during a patient visit?”
ʯ “If you had this ability, how would it impact your workflow and staffing today?”
ʯ “If you currently lack the ability to confirm strep A results during a patient visit, does this lead to any concern about overtreatment
or undertreatment? Delay in obtaining test results may mean that patients receive unnecessary antibiotics or that patients with GAS do not receive the antibiotics they need.”
‘Most physicians prefer rapid tests, as results are known quickly and decision on further course of treatment can be made immediately.’
Comprehensive toxicology menu now with 14 CLIA 1 categorized moderate complexity assays.
270 BENCHTOP ANALYZER

Toxicology screening solutions for physician offices, pain management, treatment centers and laboratories testing 200+ patient samples/mo.
MODERATE COMPLEXITY ASSAYS – FDA 510(K) CLEARED
6-acetylmorphine (6-AM Heroin metabolite)
Amphetamine
Barbiturates
Benzodiazepines
Benzoylecgonine (Cocaine metabolite)
Buprenorphine
Cannabinoids (THC)
EDDP (Methadone metabolite)

Fentanyl*
Methamphetamine
Opiates
Oxycodone
Phencyclidine (PCP)
Tramadol
Scan this QR code to view the ImmTox™ 270 product video



Editor’s note: Home blood pressure (BP) monitoring is a cost-effective solution for better BP management, early detection of potential problems, and patient convenience. Repertoire asked Julie Roth Jakubowski, MD, FACP, Head of Medical Affairs, Front Line Care, Baxter to explain the rationale behind home blood-pressure monitoring and some messages sales reps might share with their clinical customers about it.
Repertoire: Why is home blood pressure (BP) monitoring essential? What’s wrong with just having BP measured during your annual checkup at the primary care doc’s office?
Dr. Julie Jakubowski: Home BP monitoring is essential because blood pressure can fluctuate and may differ appreciably when measured in the office or at home. Higher out-of-office blood pressure is associated with increased cardiovascular risk resulting from underdiagnosis, misdiagnosis, undertreatment, overtreatment and misuse of antihypertensive medications.1 This fluctuation can occur when measured during an annual checkup at the primary care doctor’s office. Some of the common reasons for blood pressure measurement fluctuation found in office based measurement are: masked hypertension (i.e., office readings suggestive of normal BP but above normal BP outside of office settings) and white coat hypertension, which is characterized by elevated office readings but normal readings when measured outside the office. 2 - 5
Home BP monitoring allows patients to actively participate in the management of their BP and has been shown to improve adherence to antihypertensive medications.6
Therefore, home BP monitoring and recording of blood pressure readings can provide your healthcare professional with valuable information to determine if you truly have high blood pressure and, if you do, what your treatment options are and whether your treatment plan is working. 7
monitoring for all people with high blood pressure to help the doctor determine whether treatments are working or adjustments should be made to medication or treatments 1 It’s important to note that home monitoring, or self-measured blood pressure, is not a substitute for regular visits to your physician. The best way to determine if a patient is a good candidate and will comply with home blood pressure monitoring is to include strategies shown that will result in higher levels of compliance with home blood pressure monitoring.
Repertoire: Among the doctor’s patient base, who are the most likely candidates for home BP monitoring and why?
Dr. Jakubowski: The American Heart Association recommends home
It has been found that engaging the patient and, if possible, the family, in a team-based care approach results in greater compliance. This involves engaging with patients on the importance of home blood pressure monitoring as it relates to their overall heath and the benefits of controlling hypertension. Additionally, providing education and training to patients and their families on how to take a proper blood pressure measurement and recording the results to share with their doctor, including when to contact the office, helps establish a shared sense of control and compliance in their overall health. 8

Repertoire: What are the barriers to making home BP monitoring effective or practical? How can the patient and doctor address those challenges?
Dr. Jakubowski: The main barriers are:
ʯ Concerns over the validity of test results, reliability and quality of home blood pressure devices.
ʯ Patient motivation and adherence to regularly check their blood pressure at home.
ʯ Concerns over forgetting to check their blood pressure and that skipped readings could testing results.
ʯ Technique concerns, which may be worsened by experiencing inconsistent blood pressure measurement techniques at the doctor’s office.
ʯ Cost for a home BP monitor.9
These barriers can be addressed by:
ʯ Providing guidance on selecting a monitor that has been validated with appropriately sized upper arm cuffs. (See: www.validatebp.org
www.ama-assn.org/system/files/ 2020-11/smbp-cuff-selection.pdf 10 )
ʯ Providing education on the importance and adherence of home blood pressure monitoring.
ʯ Providing education on proper preparation, positioning, instructions on how often to test and how to record results.
ʯ Training on how and when to communicate results back to the doctor’s office.
ʯ Verification of patients’ understanding of resources available.
For patients who are concerned about the cost of owning a validated blood pressure monitor for home use, the medical team can explain how the monitor can decrease overall costs associated with better management
of hypertension and reduce potential adverse health outcomes.
Repertoire: Anything to add about how healthcare professionals can most effectively integrate home BP monitoring into their workflow?
Dr. Jakubowski: A way to help integrate home BP monitoring into an office workflow is to identify a support staff member who can teach patients how to use monitors, validate devices, and review action plans and blood pressure logs. In addition, developing a protocol to address frequency of office visits, handle inquiries from patients about home monitor concerns, etc., will help integrate this important benefit to both the office and the patient for long-term health benefits.12
References:
1 Shimbo, D, et al. Self-Measured Blood Pressure Monitoring at Home: A Joint Policy Statement From the American Heart Association and American Medical Association, AHA Journal, 22 June 2020;142:e42–e63
2 Whelton PK, Carey RM, Aronow WS, et al. 2017
ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCA Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol 2018; 71: e127-248. DOI: 10.1016/j.jacc.2017.11.006
3 Verdecchia P, Angeli F, Reboldi G. Masked and white-coat hypertension. Moving to African-Americans. J Am College Cardiol 2015; 66(20): 2170-2172. DOI: 10.1016/i.jacc.2015.09.008
4 Tientcheu D, Ayers C, Das SR, et al. Target organ complications and cardiovascular events associated with masked hypertension and white-coat hypertension. J Am College Cardiol 2015; 66(20): 2159-2169. DOI: 10.1016/i.jacc.2015.09.007
5 Gorostidi M, Vinyoles E, Banegas JR, de la Sierra A. Prevalence of white-coat and masked hypertension in national and international registries. Hypertens Res 2015; 38: 1-7. DOI: 10.1038/hr.2014.149
6 Centers for Disease Control and Prevention. Self-Measured Blood Pressure Monitoring: Actions Steps for Clinicians. Atlanta, GA: Centers for Disease Control and Prevention, US Dept of Health and Human Services; 2014.
7 https://www.heart.org/en/health-topics/high-blood-pressure/the-facts-about-high-blood-pressure/common-high-blood-pressure-myths.
8 Trefond, J et al. Home blood pressure monitoring and adherence in patients with hypertension on primary prevention treatment: a survey of 1026 patients in general medicine in the Auvergne region, BMC Prim Care, 2022; 23: 131.
9 Carter, E. et al, Patient Barriers and Facilitators to Ambulatory and Home Blood Pressure Monitoring: A Qualitative Study, Am J Hypertens. 2018 Jul; 31(8): 919–927.
10 https://www.ama-assn.org/delivering-care/hypertension/bp-monitoring-you-can-count-list-validated-devices-grows
11 https://www.mayoclinic.org/diseases-conditions/high-blood-pressure/in-depth/high-blood-pressure/art-20047889
12 https://www.nyc.gov/assets/doh/downloads/pdf/csi/hyperkit-hcp-bpselfmon-guide.pdf
It’s important to note that home monitoring, or self-measured blood pressure, is not a substitute for regular visits to your physician.
Repertoire: Why is home blood pressure monitoring essential? What’s wrong with just having your BP measured during your annual checkup at the primary care doc’s office?
Neal Weingart, President and CFO, American Diagnostic Corp.: There are three measurements you can count on at any physician office visit: weight, temperature, and blood pressure. Blood pressure is ubiquitous because it’s such an important metric in our overall health profile. But it’s tricky, too, because small variations in technique can cause large variances in measurements, even on the same patient. So the readings you get in the office are really just one data point that doesn’t tell us very much overall.
Steve Kelly, Vice President of Sales, American Diagnostic Corp.: And it’s not just technique that’s at play. White Coat Hypertension – the phenomenon where patients tend to have higher blood pressure in the presence of health care workers, particularly physicians – is very real. With all these factors, it can be a challenge to make treatment decisions based exclusively on the in-office numbers.
In these cases, doctors will usually recommend at-home monitoring.
Repertoire: How does monitoring at home complement measurement in a clinical setting?
Kelly: There’s a big difference between monitoring your blood pressure at
home and having a reading taken in a busy physician’s office. Research confirms that readings are more accurate if you take five to ten minutes to relax before starting a measurement, for instance, but that’s just not practical in a clinical setting.
Weingart: And that’s just one variable. We know that measurements should be taken on a bare arm, that feet should be flat on the floor, that the back should be supported, and that the measurement arm should be positioned at heart level on a cushion or a table. Each of these alone can affect a reading by 5-40 mmHg (millimeters of mercury), so imagine the cumulative impact. It’s so much easier to manage the overall environment at home.
Kelly: It’s also easier to take daily readings at home, which allows you to see trends instead of isolated readings. And trends are essential
to successful management of blood pressure conditions like hypertension.
Repertoire: Have cases of high blood pressure worsened among the U.S. health population in recent years?
Weingart: High blood pressure, or hypertension, is defined as a systolic blood pressure greater than 130 mmHg or a diastolic blood pressure greater than 80 mmHg. And the numbers are staggering.
ʯ According to the CDC, nearly half of adults in the U.S. – about 116 million people – have hypertension or are taking medication for hypertension.

ʯ Every year, Americans make more than 56 million physician office visits where essential hypertension is the primary diagnosis.
ʯ Around one million emergency department visits are attributed to essential hypertension.
On top of that a large observational study published in the Circulation, the Journal of the American Heart Association , found a small, but consequential, rise in average blood pressure during the early peak of the COVID -19 pandemic in 2020. Average systolic blood pressure – the top number in the blood pressure reading – increased by about 2 millimeters of mercury (mmHg), while average diastolic pressure – the bottom number –also rose slightly.
Kelly: It’s an unfortunate trend overall, but it’s also a tremendous opportunity for patient education and engagement. Helping patients get
set up to monitor blood pressure at home is relatively fast and easy and allows them to actively participate in the treatment process.



Repertoire: What questions can distributor reps ask their clients to ensure they have the most up to date equipment?
Kelly: Reps can start the conversation by asking, “How important is it to you that patients monitor their blood pressure at home?” Depending on the response, you can make sure doctors understand how valuable these devices are to managing conditions like hypertension. Then provide expert recommendations for the models that will be best
suited for both the practice and their patients.
The connectivity piece is essential to the conversation, too, so follow-up questions should touch on how they want patients to share the data they collect at home. Solutions could be as easy as setting up a dedicated email address where readings should be sent electronically between visits or having patients bring their phones to appointments to show reading data or trend graphs.
Weingart: In the end, doctors will be getting more and better information on the status of patients, which will lead to more effective treatment plans.

Human-centered care is a focus of many healthcare systems and corporations as the medical industry navigates ongoing pandemic-related workplace challenges.
In the past few decades, healthcare has undergone a shift from private physician-owned practices to medical offices being integrated into large health systems.
Health networks have many benefits such as streamlined care, increased patient access, and collaboration between doctors. However, despite the benefits of health networks, as systems have expanded, clinicians’ intentionality toward patient care has decreased. Individualized and human-centered patient care has been at times neglected due to the advent of large healthcare systems.
Healthcare industry professionals are also facing many challenges that impact their ability to provide the best possible care to patients. Clinicians continue to experience the impacts of the pandemic, citing burnout, emotional distress, and fatigue that interfere in the workplace with caregiving ability.
The Arnold P. Gold Foundation and Henry Schein recently hosted a virtual webinar addressing humanism in healthcare, titled “Post-Pandemic Future – Why Humanism in Healthcare Matters,” featuring the following panelists:
ʯ Richard Levin, M.D., President and Chief Executive Officer of The Arnold P. Gold Foundation.


ʯ Allison Neale, MPP, Member Chair of the Gold Corporate Council; Vice President of Public Policy at Henry Schein; and Managing Director of the Henry Schein Cares Foundation.
ʯ Olapeju Simoyan, M.D., BDS, MPH, Gold Humanism Honor Society member; Medical Director of New Directions Treatment Services; and Professor in the Department of Psychiatry at Drexel University College of Medicine, and board-certified in family medicine and addiction medicine.





 ʯ Reed V. Tuckson, M.D., FACP, Former Trustee of the Gold Foundation; Managing Director of Tuckson Health Connections, LLC; Founder of the Black Coalition Against COVID-19; Co-Founder of the Coalition for Trust in Health & Science; and member of Henry Schein’s Board of Directors.
ʯ Reed V. Tuckson, M.D., FACP, Former Trustee of the Gold Foundation; Managing Director of Tuckson Health Connections, LLC; Founder of the Black Coalition Against COVID-19; Co-Founder of the Coalition for Trust in Health & Science; and member of Henry Schein’s Board of Directors.
The Arnold P. Gold Foundation was founded in 1988 to sustain and elevate the human connection in healthcare. The nonprofit organization began its work as a change agent in the medical education space, and then extended into nursing education and healthcare in practice. In 2017, the Gold Foundation brought together corporate healthcare leaders, including Henry Schein, to create the Gold Corporate Council (GCC). The independent companies on the council support the Gold Foundation’s mission of humanism in healthcare through both collaborative efforts and their own policies and initiatives. Henry Schein was one of the founding members and has helped expand the Gold Foundation’s mission into the corporate sector.
According to the Gold Foundation, humanistic care emphasizes the elements of compassion, collaboration, and scientific excellence in healthcare when working with and treating a patient, as well as working with colleagues. A clinician who considers humanistic care in their practice understands that the entire healthcare journey is unique to each individual. Reintroducing the human aspect of care within the medical industry reminds medical staff to focus on the interpersonal aspect of healthcare and to focus on taking care of people and their well-being
first. According to the Gold Foundation, humanism emphasizes human interests, values, and dignity at the center of all healthcare operations.
Clinicians have long experienced barriers to providing care, and the pandemic heightened the already present challenges. The healthcare worker shortage, administrative tasks, technology challenges, and disease transmission from COVID-19 have made humanistic care increasingly more difficult to implement day to day within medical practices.
connection in healthcare, which is essential to patients and clinicians.”
Dr. Simoyan discussed how we must recognize the importance of humanism in healthcare, in this national crisis in healthcare and always.
“It is important for us to have self-compassion. It is beyond the individual level and is going to require changes on a system level, as well, to say we’re humans, not robots.” She quoted fellow dentist-physician Jill Rigert, DMD, MD: “We need systems that are made for humans, not robots. Nothing in a career is more important than your life.”
“On average, doctors work twice as long on administrative tasks like the electronic health record as they do with patients. Thirty years ago, most doctors owned their own practices and set their time and priorities as patient circumstances demanded. Now, most doctors are employees of huge health systems,” said Dr. Levin.
It is necessary within the healthcare industry to address healthcare workers’ concerns so employees can provide exceptional patient care. The Gold Humanism Honor Society (GHHS) was started in 2002 with that goal in mind and has grown over the years to more than 45,000 members and 180 chapters, recognizing the health organizations that value humanism within their practices. According to GHHS, the peer-nominated honor society “reinforces and supports the importance of human
In the healthcare industry, clinicians must first take care of their physical and mental well-being before assisting others. Metaphorically speaking, in the event of an emergency, flight attendants advise passengers to place their own oxygen masks on before helping others. If physicians don’t first prioritize their own needs, they are unable to provide others with care.
Seeking medical care or receiving news of a medical diagnosis is often an emotional and vulnerable experience. Humanistic practices encourage doctors to recognize this aspect of an individual’s healthcare journey and consider it throughout the treatment process.
Through a series of essays submitted by students at Geisinger Commonwealth School of Medicine in Scranton, Dr. Simoyan captured
“At every single step, when that individual enters the healthcare ecosystem, there’s an opportunity for a relationship that drives people to start and maintain positive health changes.”
– Allison Neale, MPP
the emotional response of aspiring healthcare workers to the current national crisis in healthcare. She quoted one medical student’s essay in the literary journal Black Diamonds, of which Dr. Simoyan was the Founding Editor/Editor in Chief: “A disease is more than a diagnosis, it’s an event. It is often a realization of one’s own vulnerability. Remembering this can help us understand and connect a truly empathize with our patients.”
Healthcare equity for all individuals is a focus within humanistic healthcare. Minority and socio-economically challenged populations often face significant barriers to accessing high-quality healthcare. Even when accessible, there are disparities in the quality of care delivered, resulting in suboptimal health outcomes. Equity within healthcare requires prioritized attention to the distribution of resources and opportunities that considers individual circumstances and needs. However, many challenges stand in the way of health equity in the nation, including continuing challenges post-pandemic, uneven regional distribution of medical providers, pre-existing social determinants of diseases, distrust of the health system, and lack of access to affordable care options such as Medicaid.
“We have unfortunately learned from a major report several years ago from the prestigious National Academy of Medicine that African Americans and Hispanics do receive a lower quality of health care across a range of diseases such as cancer, cardiovascular diseases, HIV, AIDS, diabetes, and mental health. Unfortunately, these inequities express themselves in premature, unnecessary,
and preventable misery and suffering,” said Dr. Tuckson.
As noted above, health outcomes are often the consequence of social determinants such as housing, access to healthy foods, transportation, violence, and technology access.
As such, many causes of health disparities, according to Dr. Tuckson, can be found “at the crosssection of the social forces of our society. We’ve learned how important housing, food access, the ability to find healthy fruits and vegetables, fairness in care delivery, and access to technology-enabled care, are for optimal health outcomes.”
Additionally, trust in the healthcare system is paramount to bridging the care access gap. Health insults such as the Tuskegee Syphilis Study, an unethical medical research study on Black men with syphilis conducted from 1932 to 1972, continue to contribute to an extensive distrust of the health and science community by many African Americans. The decades-long study denied participants the medication that would have treated their disease. There continues to be widespread mistrust in the healthcare system, and therefore Dr. Tuckson emphasized that compassion and trust must be reestablished through a shared community vision of health goals and a consistent respect for the dignity of each individual.
“What we’re talking about is whether or not the healthcare system is responding to its ethical responsibility to respectfully address all the people who share our time and space and whether they will live or prematurely die,” said Dr. Tuckson.
Healthcare leaders can contribute to facilitating humanistic care across
health systems. Healthcare industry leaders have a responsibility to nurture workplaces and medical offices as spaces that support humanism first and foremost.
“Human engagement is the cornerstone of effective healthcare but also extremely important to running a successful enterprise,” said Neale.
When a patient visits a medical office, their experience is impacted by everyone they interact with. They form a relationship directly with the clinician who is treating them, but also with everyone whom they engage with. Patients are impacted in the same way by the person who draws their blood, the person who makes their appointment or processes their bill, and all staff within a medical facility. This presents an opportunity for the entire staff of a health organization to create meaningful, individualized connections with patients.
“At every single step, when that individual enters the healthcare ecosystem, there’s an opportunity for a relationship that drives people to start and maintain positive health changes,” said Neale.
Humanism in healthcare emphasizes a respectful and compassionate relationship not only between doctors and patients, but also throughout a healthcare team, including other clinicians, members of the healthcare team, and family members. Implementing humanistic practices in medicine strives to improve healthcare outcomes and ensure overall patient and clinician well-being.
According to Dr. Levin, “The human connection in healthcare leads to more meaning. That is why doctors and nurses got into this field in the first place. Humanism helps create better outcomes, better patient experience, and a better bottom line.”
Futuro Health’s education to career programs address industry’s allied health workforce shortages.
 By Jenna Hughes
By Jenna Hughes
The healthcare worker shortage continues to cause employment gaps across the medical industry. Eighty-five percent of healthcare facilities are facing allied staff shortages, according to a recent report published by AMN Healthcare. Many positions in healthcare remain vacant, leaving health systems searching to fill innumerable entry-level to advanced medical roles. Now more than ever, there are abundant opportunities available for individuals interested in beginning a career in the healthcare industry. According to Futuro Health, a California-based non-profit organization focused on improving the health and wealth of communities, 2.3 million additional healthcare workers will be needed to fill vacant positions in the United States by 2025.
Yet, for adults managing jobs and daily family responsibilities, the thought of returning to school to earn a credential can be daunting. The rising cost of tuition is also a barrier for many individuals who wish to pursue additional education to enter the healthcare field.
Since Futuro Health’s inception in 2020, thanks to initial community benefits funding from Kaiser Permanente, over 5,000 diverse adults will have completed their education journey with no debt and gained the interpersonal and technical training valued by healthcare providers. With 90% ethnic diversity and over 50% linguistic diversity, Futuro Health Scholars bring cultural competence and lived experiences, which are crucial for improving health outcomes and promoting equity. Furthermore, graduates come with demonstrated ability to thrive in a digital/hybrid environment, which are important skillsets as the deployment of digital health and virtual care become increasingly common.
Futuro Health delivers education programs that prepare individuals for careers in allied health positions. The mission of the nonprofit organization is to bridge the national healthcare workforce gap by continuing to grow a network of educated and qualified health professionals. The organization makes the path into allied health careers more accessible by creating adaptable and affordable healthcare education opportunities. Futuro Health’s workforce solutions are designed to scale efficiency, a unique combination of data and technology platform, enrollment portal, healthcare curriculum expertise, education provider ecosystem, dedicated success coaches, and “Human Touch Healthcare” coursework, to begin
addressing the provider’s talent acquisition and retention challenges.
Van Ton-Quinlivan, chief executive officer of Futuro Health, formerly the executive vice chancellor of California Community Colleges, now oversees the process of connecting diverse adults to education programs leading to healthcare careers. Ton-Quinlivan was named a White House Champion of Change under the Obama Administration in recognition of her career in education and is an appointee to the State of California Governor Newsom’s Health Workforce and Education Training Council.
an “ecosystem” approach. “We call it ecosystem engineering,” she explains. “No one education provider can provide the needed variety in occupational training. But, because we’ve engineered an ecosystem of providers, we’ve created a robust solution for employers built to scale,” said Ton-Quinlivan.
All Futuro Health education journeys prepare individuals with the skills and qualifications they need to perform in healthcare-related jobs. Learners are empowered with interpersonal and technical skills for careers in allied health positions during their education journeys as a Futuro Health Scholar. Additionally,
“Workforce development is a team, not an individual, sport. Employers do not need to tackle workforce challenges on their own,” said TonQuinlivan. “Day to day, I am inspired by the ability to connect individuals from diverse communities to good opportunities in allied health careers and the importance of decent educational pathways made available as a way for students in the healthcare field to have economic mobility.”
Any solution built for scale to healthcare worker shortages will require more than incremental steps; a combination of best practice tactics and stakeholders is necessary. According to Ton-Quinlivan, addressing the healthcare worker shortage requires
they receive technical education from a curated selection of programs approved by Futuro Health’s team of experts in curriculum development.
Futuro Health’s technical training offerings range from patientfacing clinical roles to behavioral health and health informatics (IT) programs of study. Individuals can access careers such as medical assistants, phlebotomists, patient care representatives, pharmacy techs, surgical techs, sterile processing technicians, healthcare data analysts, peer support specialists, community health workers with behavioral health emphasis, and many more. Futuro Health now has over 20 approved training offerings across 65 education partner campuses.
As a best practice, Ton-Quinlivan encourages employers to pool their
Learners are empowered with interpersonal and technical skills for careers in allied health positions during their education journeys as a Futuro Health Scholar.
openings. “The reason why employers need to form a consortium and aggregate their jobs is to match their hiring processes with the volume in which education produces students,” according to Ton-Quinlivan.
Futuro Health’s health education programs focus heavily on current medical practices to ensure the development of a thoroughly prepared and stable workforce. The organization consults employers on open employment opportunities and tailors each educational program based on industry needs.
Generous tuition scholarships provided through Futuro Health encourage students from diverse backgrounds to pursue a degree. Many participants are able to attend programs tuitionfree, which removes the burden of education-related debt in making the decision to pursue a degree.
In California, Kaiser Permanente, Dignity Health, Sutter Health, Lucile Packard Children’s Hospital at Stanford, and others underwrite scholarships and provide financial support so that learners from diverse backgrounds can receive an education and begin a career in healthcare through Futuro Health
To further educational opportunities and continue to address workforce shortages, Futuro Health partners with public higher education institutions and health systems including the University of California, Berkeley, California State Universities, community colleges, and employers. Futuro Health is also a partner in a federal grant called the California Consortium for Public Health Informatics and Technology (CCPHIT). CCPHIT “aims to increase representation of underrepresented communities and
will educate 700 adults for careers within the public health IT workforce by 2024.”
“The rule of thumb in workforce development is that you collaborate to create a talent pool and then you complete at the point of hiring. To successfully grow the talent pool, the three entities of employers, educators, and community organizations must come together doing what they do best,” according to Ton-Quinlivan.
The programs have the potential to jumpstart individuals into new health careers, introduce them to a career in the healthcare industry, and increase earning potential, among many more impacts.
For Alicia, Futuro Health Medical Assistant Scholar Graduate, going back to school seemed daunting, as she was paying off student loans, pregnant with her first child, and working full time. She had always
Futuro Health pre-arranges programs and enrolls learners in all elements of a healthcare education journey so that adults can focus on their career first and foremost.
“It is not an easy task for adults to go back to school. So, part of what we do is build students’ confidence so that they can get back into their studies, whether it be in-person or a hybrid-online format, and just show them that they can manage their family and have time to study,” according to Ton-Quinlivan. “There’s a lot of work done to build their confidence to go back to school.”
The Futuro Health programs offer flexibility within a participants’ coursework to allow individuals the opportunity at any point in their career to advance and grow in healthcare. Numerous students who have been through the program have been able to return to school while raising a family, while managing student debt from previous degrees and education, and while employed.
wanted to pursue a career in the medical field. Upon becoming a Futuro Health Scholar, she went back to school and found employment at Kaiser Permanente. According to Alicia, “Futuro Health helped me to secure my dream and my passion when I happened to go into debt.”
Another student, Damien, Futuro Health Scholar Graduate, learned about all the different types of career trajectories within IT in the medical field. Damien, through the Health IT Specialist Program, discovered a newfound passion for healthcare informatics and successfully transitioned away from his prior industry, where he was laid off during the pandemic.
“We’re inviting other states and employers to contact us so that we are able to bring education and healthcare workforce staffing solutions to other regions in the U.S. We are actively seeking employer partners if they have a volume of externships or open jobs, then they are part of the solution,” said Ton-Quinlivan.
Generous tuition scholarships provided through Futuro Health encourage students from diverse backgrounds to pursue a degree.
An easy to use, efficient solution that you can share information, documents and more in just a few clicks.

The month of August marks the nationwide initiative to stay up to date on vaccinations to prevent disease and keep the population healthy.
By Jenna HughesWhen fall flu season inevitably comes around, doctors reiterate that patients should receive a vaccination to protect themselves and others. Vaccines provide disease immunity to the individual and also the community at whole by preventing transmissible infectious diseases.
August is National Immunization Awareness Month (NIAM), held to observe the importance of population-wide vaccination.
According to the National Foundation for Infectious Diseases and Voices for Vaccines, among U.S. children vaccinated in the last 20 years, vaccines will prevent 21 million hospitalizations and more than 700,000 deaths.
“For people living across the nation, it is important to know that vaccines are the best way to prevent serious illness, hospitalization, and even death from infectious diseases.
Vaccination is essential to creating communities of immunity and protecting vulnerable people who can’t
get vaccinated,” said American Academy of Family Physicians (AAFP) President Dr. Tochi Iroku-Malize.

The AAFP and the Advisory Committee on Immunization Practices (ACIP) develop recommendations for vaccinations and provide age group specific immunization schedules to the population each year.

Many children missed routine checkups and childhood vaccinations because of the COVID-19 pandemic, according to the Office of Disease
Prevention and Health Promotion (OASH) and the Centers for Disease Control and Prevention (CDC). The pandemic affected schools across the nation from enforcing state and national vaccination requirements.
According to the CDC, vaccination coverage nationally decreased to 94%, one percentage point lower than the previous year, for all required vaccines for children during the 2020-21 school year.
To get children back on track to begin school and to protect themselves and others, it is important for them to receive all of the required vaccines. If parents delay early childhood vaccinations, children are more susceptible to highly contagious diseases such as measles, whooping cough, and chickenpox. These transmissible diseases are serious, and even deadly, for young children that are unvaccinated.
“Different vaccines are given at different ages as young children’s immune systems develop. It’s important that they stay up to date with vaccinations to keep them healthy or boost immunity that can fade over time. If they get behind on vaccinations, it can open the door for the child to get sick and potentially spread that disease to other people as well,” said Dr. Iroku-Malize.
The best way to protect children from preventable diseases is through routine vaccination. One-time vaccinations throughout childhood are essential to provide immunity against certain life-threatening diseases before children are exposed. According to the CDC, vaccines use small amounts of antigens to help a child’s immune system recognize and fight serious diseases if they are to be exposed in the environment.
Vaccines are tested to ensure that they are safe for children to receive at
the recommended ages, and they can be administered at routine well-being doctor’s visits that young children are likely already attending.
“Before vaccines are made available to the public, multiple stages of research, testing, and clinical trials are conducted to make sure they are safe and effective,” said Dr. Iroku-Malize. “If you have questions or are unsure about a certain vaccine or immunization in general, talk with your family physician. They will help you make the decision that’s best for you and your family’s health.”
During the pandemic, misinformation widely circulated regarding the COVID-19 vaccines and vaccines in general. False information spread publicly about vaccines is confusing and makes it more difficult to find trustworthy and scientifically-based vaccine information, said Dr. Iroku-Malize. Primary care physicians thoroughly understand the risk and benefits of vaccines, and can provide through and detailed information to assist families in the process of making the decision to vaccinate themselves and their children.
“Family physicians are well-prepared to address vaccine hesitancy and answer any questions patients may have. Primary care physicians and doctors are trusted sources of information and develop relationships with our patients. This provides the opportunity to have honest and open conversations with our patients about their concerns. When a patient expresses concern, I reassure them about the vaccine safety process,” said Dr. Iroku-Malize.
The benefits of vaccination to the population at large are that they
protect the health and well-being of the people around you, including family, friends, coworkers, classmates, and even strangers.
“When you get vaccinated, you protect yourself and those around you. Your vaccination status impacts those who are unable to get vaccinated, such as infants under six months old and people who are immunocompromised,” said Dr. Iroku-Malize.
According to the CDC, vaccines have reduced the prevalence of diseases that once caused serious illness and death. The immunity that vaccines provide have the potential to prevent the incidence of illnesses such as the flu, COVID-19, Hepatitis B, HPV, and many more.
“Vaccines have eradicated many diseases that at one time were disabling or deadly. Without vaccines, diseases like polio could come back and threaten public health on a large scale,” said Dr. Iroku-Malize.
AAFP encourages “creating a community of immunity” through vaccination. AAFP provides the public with detailed vaccine schedules, guides patients through disease “practice planning” that encourages healthy behaviors in patients and publishes extensive patient vaccine education information. These resources inform the public on vaccine efficacy and increase trust in vaccine safety so that more of the population is encouraged to receive immunizations.
“The AAFP shares resources and tools with our physician members, and we also advocate for equitable access to vaccines year-round. During National Immunization Awareness Month in August, and year-round, we continue to promote the importance of vaccination to both family physicians and the public,” said Dr. Iroku-Malize.
The total cost of patient care is a winding path delicately traversed.

In past generations of Value Analysis, the focus was more on savings with contract renewals, the development of a capitated price model and matrices and price at the pump downward shifts, said Shaneka Demps, Manager, Value Analysis, BayCare Health System. “Compared to three years ago, Value Analysis today has shifted to finding value in utilization practice changes, eliminating unnecessary waste and establishing clinically appropriate criteria for use in some cases,” Demps said.
“Even more so, we are all traveling quickly down the road of total cost of patient care inclusive of reimbursement differences, length of stay reduction and the impact of hospital-acquired conditions. This road has become a winding path that must be delicately traveled with each Value Analysis project.”
In a conversation with Repertoire, Demps discussed how Value Analysis professionals can effectively interact with and educate suppliers, as well as a glimpse into what the future of the profession may hold.
How do you interact with and screen suppliers during the Value Analysis process? What are the parameters you set for suppliers?
Shaneka Demps: We interact with new or interested vendors via our supply chain interest portal. Vendors are able to reach out by a direct email to our Value Analysis Department or Contracting Team. Depending upon the category, vendors are set up with the appropriate Clinical Value Analysis RN or Contract Manager to have a brief conversation exploring a potential partnership.

Our goal is to connect that new vendor with our service line leader for a brief 10-minute introduction to our system and to describe how they may provide a solution to enhance our current product and services portfolio, improve quality and save costs.
How are Value Analysis appointments scheduled with suppliers? Do you prefer them to contact an internal champion first (e.g. –physicians, service line administrator, nurse leader) who then notifies you of a request? Demps: We want them to contact us initially so we’re aware of the product or category they plan to promote. That way we can head off any issue with existing contracts and compliance. Once the initial review is cleared, then they would work with clinicians to identify a potential champion within the BayCare Health System. That champion would then be the best spokesperson when reviewing with the committee and would be willing to fill in the necessary clinical pieces, which is super helpful.
The challenge here is not to overstep, which may be quite easy to do. For example, leaving samples
or doing a “small trial” would be against our policy. Every item has to be fully vetted and approved for trial by our Value Analysis Committee prior to use on a patient. That means that even if your clinical champion is excited about your technology and ready to give your product a try, they must follow our internal process and present you and your product to the committee before any trials may begin. This can be a bit of a sticky widget. One last caution of approach with the “clinical champion” is not to overwhelm them. Being too assertive or not setting appointments with the clinicians could leave them feeling uneasy with your future attempts to communicate.
How do you educate suppliers? What are some best practices for suppliers to undertake in order to start the Value Analysis process?
Demps: Generally, our Supplier Information page on the BayCare Health System website provides specific information on our processes to help our vendor partners understand what to expect as well as what we expect from them. Our clinicians are also very savvy and fully aware of how the Value Analysis process works. They are excellent at steering the vendors in the right direction.
If there is a question, we are happy to connect with the vendor and speak about our process and learn more about how they envision a long-lasting partnership with our hospital system.
What one thing would you change to help improve the value analysis process in the future?
Demps: Today, we value true partnership with our vendor partners driven by clinical engagement with our service lines and physician champions. I believe that the Value Analysis process will always be an evolution. It must be nimble yet firm.
The one thing that I would change, with hopes to improve the process in the future, would be greater crowd sourcing and data sharing with similar IDNs. Sharing innovative ideas with each other and the blueprint that it took to achieve success could help every Value Analysis Team across the region and beyond. Every healthcare system has its own identity and DNA, but at the true center of each one, we are patient centric, we wish to be sustainable and to provide extraordinary care to our community.
Being too assertive or not setting appointments with the clinicians could leave them feeling uneasy with your future attempts to communicate.

Healthcare industry employees have continued to face increased workplace challenges since the pandemic, as clinicians balance staff shortages, stress and burnout, and disease transmission with their daily responsibilities. To allow staff to perform confidently in the workplace, it is essential for medical industry leaders to foster a supportive workplace culture and make a commitment to employee well-being.
A positive business culture prioritizes the welfare of its employees foremost. In the constantly changing healthcare marketplace, the companies that stand out are the ones that support their employees throughout all levels of the organization and that foster trust, open communication, and support within the workplace.
Ochsner Health’s health system was recognized in 2023 for its exceptional workplace culture. Ochsner Health was awarded the Gallup Exceptional Workplace Award (GEWA) in early 2023, which recognizes the most engaged workplace cultures in the world. The award elevates organizations that are committed to developing human potential. It celebrates businesses that “put the engagement of their people at the center of their business strategy and weave that commitment into their organizational culture,” according to GEWA.
Ochsner Health delivers health services to patients throughout Louisiana, Mississippi, and the Gulf South. The not-for-profit healthcare system’s mission is to inspire healthier and stronger communities through leadership in cancer care, cardiology, neurosciences, liver and kidney transplants, pediatrics, and more.
“The medical industry has greatly changed because of the pandemic. Medical staff and providers were challenged in ways we had not seen before, including being stretched thin, resulting in staffing shortages in New Orleans and around the country. We invest not only in our employees but also in our communities,” said Tracy Schiro, executive vice president and chief human resources officer of Ochsner Health.
Nationally, only 32% of employees in the U.S. workforce are considered engaged with their business’ vision and values. In 2022, Ochsner’s employee engagement reached an all-time high and was ranked in the 86th percentile across healthcare organizations throughout the country, according to a March 2023 press release from Ochsner Health.
Organizations that are nominated for the award prioritize investing in
their employees by always listening, measuring, and making decisions that ensure employee satisfaction and a unique company culture.
Ochsner Health invests in its culture by providing benefits, resources, and programs to engage employees in the workplace. This engagement fuels commitment and passion for everyday work among all staff from physicians, providers, clinicians to non-clinical staff.
Ochsner Health maintains engagement throughout an individual’s career by fostering a company culture that values compassion and a patient-first environment. Employees are empowered in growth and professional development at all levels of their career through access to in-person and online education programs that encourage individualized growth.
“Our culture is one of pride, connection to purpose, collaboration and innovation resulting in the relentless pursuit of making Ochsner the leading destination for the region’s top talent and for high-quality healthcare. We value the growth, health, and well-being of each member of our Ochsner team,” said Schiro.
Businesses inevitably run into challenges when carrying out everyday operations. In the face of workplace challenges, considering employee’s well-being first and foremost contributes to a resilient and successful operation.
“One of the biggest challenges the medical field has faced is staffing. Ochsner has an innovative approach to supporting the pipeline of healthcare workers into the organization. Ochsner increasingly
invests in internal and external workforce development opportunities. As we face a shortage of caregivers, Ochsner is being intentional about how we grow our workforce. We are focused on people first and on training providers who will build careers in our communities,” said Schiro.
The pandemic has seen unpredictability within the workplace because of healthcare staffing shortages and continued disease challenges. Due to these circumstances, national healthcare systems are struggling to retain employees. Ochsner Health has experienced its return on investment in culture firsthand and has exemplified that investing in its people leads to great rewards.
Students participate in facility tours, continuing education opportunities, and hiring events to expose them to the medical field while in school. The Workforce Development team assists high school and college aged students with growth into healthcare careers through nursing pre-apprenticeships and pipeline programs.
“Ochsner is an award-winning workplace because we intentionally invest in culture and employee experience. This is done through a comprehensive listening strategy, as well as shaping positive experiences throughout an employee’s entire journey with Ochsner, including prehire,” said Schiro. “Each employee, clinical and non-clinical, truly cares
Ochsner has adapted to pandemic and workplace-related challenges by ensuring that employees are committed to their work and provide high-quality healthcare. The strong company culture and commitment to exceptional healthcare has assisted in the face of national workplace challenges.
The development of an awardwinning workplace begins pre-hire, according to Schiro. Ochsner supports the pipeline of healthcare workers through its Career Outreach and Workforce Development team. The Career Outreach team mentors’ students early on in their healthcare education experience and assists them on the path to nursing, healthcare, and corporate fields.
about our patients and the community. It is evident in everything they do and even when you simply walk into an Ochsner facility.”
Ochsner recognizes that success for an award-winning workplace relies on taking care of all members of a team from healthcare staff to executive leadership. The culture strives to create a positive experience throughout the entire career journey for all healthcare employees. Culture at the company reflects pride, connection to purpose, collaboration, and innovation, according to Schiro.
“Ochsner is proud to have a bold vision to inspire healthier lives and stronger communities,” said Schiro. “We are fueled by the talent, passion, and diversity of our employees who continue to push the limits to advance medicine to change and save lives. We won’t slow down.”
The culture strives to create a positive experience throughout the entire career journey for all healthcare employees.
Presbyterian Health contributes to improved health of communities in New Mexico through the expansion of its Northern Roots food as medicine program.
Presbyterian Health in New Mexico is committed to improving nutrition and food access to ensure patient health. While proper nutrition is key to overall well-being, many communities lack access to healthy food options. Presbyterian Health aims to close the nutrition gap through its food as medicine programs.
“In 2021, we began universal screening of all Presbyterian patients for social determinants of health (SDOH) that include questions on whether they are experiencing food insecurity, transportation, housing, violence, substance use and other social needs,” said Carrie Thielen, director of regional community health, Presbyterian Healthcare Services. “So far, we have completed 2 million screenings and found that food insecurity is one of the most common needs.”
Food is medicine
Without proper nutrition, the body cannot function properly, and health suffers. Often, communities lack access to nutritious food for various reasons including distance, availability, and economic barriers. However, eating a healthy and wellbalanced diet is critical to a patient’s overall health.

“Food is medicine and people cannot be healthy without access to healthy food. We recognize that healthy food is critical to preventing and treating chronic illness, such as diabetes and heart disease, as well as helping children be able to come to school ready to learn and be successful,” according to Thielen.
Food prescription programs provide communities with readily available and affordable fresh produce. Presbyterian Health’s Northern Roots program supplements clinical care through nutrition by removing financial barriers to purchasing fresh produce and increasing fruit and vegetable consumption. By providing access to healthy foods, patients’ experience lower blood pressure and risk of heart disease.
Participants in the program have benefitted greatly, with 90% of participants saying Northern Roots increased their ability to provide healthy food for their family, and 66% saying their fruit and vegetable consumption increased “a lot,” according to a March 2023 press release from Presbyterian Health.
The New Mexico Department of Health and the Brindle Foundation provided Presbyterian Health with over $200,000 in 2022 to assist with the expansion of food prescription programs.
The funding will allow Presbyterian to expand nutritious food offerings and connect the community to nutrition education. The program also “provides wraparound support for participants, such as connecting them to WIC programs, providing healthy recipes and cooking demonstrations, and additional support through a community health worker,” according to Thielen.
Additional funding to food prescription programs will allow Presbyterian Health to expand produce prescriptions to other communities as well such as Socorro and the South Valley in New Mexico.
“We are excited to expand food prescriptions programs to reach more families with children, thanks to additional funding from the state, private grants and extensive support from our own health plan, Presbyterian Health Plan,” according to Thielen. This expanded programming will include more families in Northern New Mexico, as well as rural communities in other parts of the state.”
Nearly 100 distributors, along with some of their key manufacturer partners, recently came to Washington D.C. to ask Congressional leaders to support legislation to strengthen the healthcare supply chain.
Attendees heard from Representative Richard Hudson (R-NC), a senior member of the House Energy and Commerce Committee. Rep. Hudson is leading bipartisan efforts to reauthorize the Pandemic and All-Hazards Preparedness Act (PAHPA). HIDA also honored Senator Patty Murray (D-WA) with the Preparedness Policy Excellence Award for her work as the lead sponsor of the Prepare for and Respond to Existing Viruses, Emerging New Threats (PREVENT) and Pandemics Act.
Then fly-in participants met with the offices of over 80 Senators and Representatives. Many of these meetings were with members on committees with jurisdiction over the medical supply chain, including the Senate Health, Education, Labor and Pensions (HELP) Committee, House Energy and Commerce Committee, House Transportation and Infrastructure Committee, and Senate Commerce, Science and Transportation Committee. In Hill meetings, HIDA members stressed several key issues essential to strengthening the medical supply chain:
PAHPA Reauthorization: HIDA urges Congress to reauthorize the Pandemic and All-Hazards Preparedness Act (PAHPA) prior to its September 30, 2023 expiration. PAHPA’s all-hazards approach provides an opportunity to ensure consistency across all disaster response efforts.
Support For Domestic Manufacturing: HIDA recommends that PAHPA reauthorization include a package of incentives to sustain the industrial base of critical products – such as government support
to reduce capital expenditures through tax incentives, committed long-term contracts of at least 5 years, and targeted policies such as innovative technology assistance to companies investing in domestic and warm base capacity.
Public/Private Partnerships: HIDA supports the creation of a permanent Medical Product Distributor Supply Chain Advisory Group of industry and federal partners from the Assistant Secretary for Preparedness and Response (ASPR) and the Strategic National Stockpile (SNS) to engage in regular communication and monitoring of the supply chain, flag potential disruptions, and collaborate on solutions.
In 2021 and 2022, transportation delays became a healthcare issue. HIDA research estimates that approximately 31,000-46,000 containers of critical medical supplies were delayed an average of 29 days throughout the transportation system. HIDA supports the creation of a “fast
pass” process to expedite medical supplies throughout the nation’s transportation system.
Provisions Enacted By PREVENT Pandemics Act: HIDA supports the retention and expansion of key provisions in the Prepare for and Respond to Existing Viruses, Emerging New Threats and Pandemics Act, including supply chain assessment, vendor-managed inventory, limiting sales of SNS product only to other federal agencies, and stronger FDA authority to increase penalties for selling counterfeit devices.
Years of work from our members and staff advancing our priorities in Washington is starting to achieve results. Building on these successes is a priority. HIDA has facilitated unprecedented collaboration between our industry and federal agencies – from ASPR, the Strategic National Stockpile to the White House. We are leveraging HIDA conferences to solidify the partnership between federal partners and the medical supply chain.

Healthcare Industry Resilience Collaborative awards first-ever transparency badges to 8 healthcare suppliers.
Courtesy of the Healthcare Industry Resilience Collaborative
The Healthcare Industry Resilience Collaborative (HIRC), a non-profit consortium of healthcare supply chain leaders focused on increasing transparency and resiliency, this month recognized the first awardees of the new HIRC Transparency Partner Badge. This distinction is designed to validate the companies’ continuous efforts and commitment to supply chain transparency and resiliency.
The inaugural badge awardees are:
ʯ B. Braun
ʯ Cardinal Health
ʯ Cook Medical
ʯ Innovative Health
ʯ Medtronic
ʯ Philips
ʯ Sandoz
ʯ Stryker
The awardees gave two primary reasons for pursuing the badge: to increase trust with providers, and to increase supply chain reliability to improve patient outcomes.
“HIRC Transparency Badging is an outstanding step forward for the healthcare industry to define what good looks like in supply chain transparency and resiliency,” said Tom Harvieux, chair of HIRC, and chief supply chain officer at BJC HealthCare. “We invite all suppliers to join HIRC and pursue the transparency badge,” Harvieux said.
HIRC is an organization of hospitals and suppliers – lead by AdventHealth, BJC HealthCare, Corewell Health, Cleveland Clinic, Mayo Clinic, Stanford Health Care, and others – that has come together to
promote resilience and transparency in the healthcare supply chain.
“The healthcare supply chain has lacked definitive information telling buyers when they can trust a supplier to be transparent – until now,” said Bill Selles, SVP Supply Chain at Corewell Health.
tangibly identify who they are, and we need more providers to use the evidence-based badges to support purchasing decisions,” says Katie Dean, Business Operations and Transformation Leader at Stanford Health Care.
According to HIRC, the transparency badge is an important step toward greater transparency in healthcare, and transparency is a critical foundation to healthcare supply chain resiliency. This reality was reinforced by a recent survey of HIRC’s provider and supplier members. According to the findings:
To qualify for the transparency badge, awardees must grant full visibility to all provider members regarding the following transparency measures:
ʯ Mapping insights of final assembly and beyond for all locations that provide critical and essential products sold into the U.S. market
ʯ A Business Continuity Maturity (BCM) assessment
ʯ
“Providers can only reward transparent and resilient suppliers if we can
ʯ 99% of providers and suppliers agree that in order to create a more resilient healthcare supply chain, we must increase transparency.
ʯ 100% of providers and 92% of suppliers agree that transparency, including visibility to geography and business continuity planning, is important to supply chain resiliency.
ʯ 77% of providers are more likely to do business with a supplier who has the Transparency Badge, all else being equal.
ʯ 88% of suppliers agree that having the Transparency Badge will have a positive and meaningful impact on their customer’s perception of them.
When asked to select the 3 most important components to transparency, communications candor, risk awareness, criticality alignment, bi-directional data sharing, and upstream visibility rose to the top:
ʯ Candor on potential supply chain disruptions (73%)
ʯ Awareness to external risks to the upstream supply chain (50%)
ʯ Alignment on what are the critical products needing protection (49%)
ʯ Bi-directional sharing to make demand v. capacity more accessible (49%)
ʯ Visibility into my upstream supply chain (48%)
ʯ Sharing of risk assessments to characterize preparedness (29%)
According to HIRC, the transparency badge process is simple to follow, standardized, and designed to empower trusted relationships. HIRC notes that the badge itself is only a step – but one that it believes is an important milestone in enabling a collaborative approach to solving for supply chain resiliency.
Commentary from the Healthcare Community Regarding the HIRC Transparency Partner Badge Awards
“ This is an outstanding step forward in coming together as an industry to define what good looks like in supply chain transparency and resiliency.”
– Tom Harvieux, Chair of HIRC, and Chief Supply Chain Officer | BJC HealthCare.
“Congratulations to this inaugural cohort of HIRC Transparency Partner Badge recipients!”
– Molly Zmuda, VP of Spend Management Services & Delivery | Vizient, Inc.
“ This is a monumental step towards reinforcing the partnership between the supplier and provider community in support of patient care.”
– Sree Duggineni, Executive Director of Supply Chain | City of Hope.
“Such a major milestone in our industry! It’s important to see suppliers actively demonstrate their commitment to resiliency.”
– Regine Villain, SVP of Supply Chain & Chief Supply Chain Officer | Ochsner Health.
“Such an important development in building out the foundation of resiliency in healthcare. Suppliers who take on this responsibility are creating the trust needed for a safer supply environment.”
– Tom Lubotsky, VP of Supply Chain | Allina Health
Commentary from Supplier Awardees of the HIRC Transparency Partner Badge
B. Braun
“ B. Braun has chosen to meet the HIRC Transparency Badge requirements as part of our supply chain transparency journey. HIRC and the SRS tool are an important component of our facility, warehouse and vendor transparency initiative which will allow our company and our customers to quickly assess and understand any potential impacts from disruptions across the globe. At B. Braun, providers are our purpose, and a secure supply chain ensures that they have the products they need to focus on what matters most – the patients they serve.”
– Jeremy H. How, Corporate Vice President Sales Operations | B. Braun
Cardinal Health
“ Transparency is core to our manufacturer and customer engagement models. Cardinal Health chooses to meet the HIRC Transparency Badge requirements because it aligns to the collaborative relationships we have with providers in order to anticipate supply chain challenges and proactively provide solutions before there is an issue.”
– Robert Rajalingam, President, U.S. Medical Products and Distribution | Cardinal Health
Cardinal Health
“Cardinal Health has a core team that focuses on resiliency and transparency within our operating model and is committed to maturing based on customer and industry needs. We leverage data, collaborative discussions, and industry position to enhance our capabilities and exceed expectations.”
– Pete Bennett, SVP, Global Logistics | Cardinal HealthCook Medical
“ The Transparency Badge is a great way to show our commitment to being a strong business partner. I’m pleased to say that Cook is recognized as a leader in this space, and this badge is another way to reinforce our obligation to the customers and patients we serve.
One thing we lack in our industry are standards. Health systems, suppliers, and distributors often follow their own rules with little consistency. HIRC has a real opportunity to create some of these standards with their growing membership. We need someone to take ownership and bring all stakeholders to the table to shape the future, and I believe that HIRC can do this and do it well.”
– Ross Harvey, Vice President, Global Supply Chain | Cook MedicalInnovative Health
“At Innovative Health, we believe it is our obligation to give providers as much transparency into our supply capabilities as possible, in order to ensure that they never run out of supplies to treat their patients. We believe that supplier transparency and resilience will become absolutely critical in providers’ vendor selection in the coming months, and as a technology leader, we need to promote and support this.”
– Rick Ferreira, CEO | Innovative HealthMedtronic
“ We are honored to be an inaugural recipient of the HIRC Transparency Partner Badge. This recognition is a direct reflection of the Medtronic Mission to alleviate pain, restore health, and extend life. Congratulations to all suppliers that have stepped forward to meet the HIRC challenge. We are creating a more resilient healthcare supply chain, together.”
– Joe Robinson, Vice President, Enterprise Risk & Continuity | MedtronicPhilips
“ The pandemic put the healthcare supply chain front and center for everyone and reminded us of the importance of transparency if we are to help health systems achieve their patient care goals in these challenging situations. The HIRC Transparency Badge is proof of our commitment to working with like-minded organizations like HIRC to develop standards and a secure collaboration platform that help us to deliver on our goal of improving lives.”
– Jeff DiLullo, Market Leader North America | PhilipsSandoz
“Sandoz is proud to endorse and comply with HIRC’s Transparency Badging program as we believe providing transparency and visibility into our supply chain is a core fundamental to establishing trust with our patients and providers. By complying with HIRC’s transparency program, we believe the strength of our supply chain will be measured against a strong baseline that is understood by our customers and aligns with our mission to provide access to patients and be the most trusted supply chain in the industry.”
– Kevin Cook, VP Supply Chain North America | Sandoz“Stryker has made significant investments and improvements to our supply chain planning and resiliency initiatives. We are passionate about being a constant for our customers and their patients. The HIRC Transparency Badge allows us to highlight the work we have done and the investments we have made while also improving communication and trust with our hospitals. I believe the spirit of transparency will open the dialogue between Stryker and our customers to better understand their needs and how we can best show up beside them.”
– Kevin Steed, Vice-President/General Manager, Enterprise Account Management | Stryker“Stryker continues to make investments and shift our approach with the goal of being an industry leader for product quality and availability. Our commitment is to focus on continued improvement while always keeping the patient in mind.”
– Dale C. Pease, Vice-President, Division Operations, Medical, Global Quality and Operations | StrykerIf you’ve shopped at the grocery store and decided to commit to buying the brand-named product such as Colgate, Nestle, or Betty Crocker, then you’ve experienced brand awareness.
Brand awareness is the extent that consumers associate with and recognize a specific brand. Brand awareness embeds itself into consumers’ lifestyles. When a brand is well-advertised, a consumer makes purchasing decisions automatically without having to weigh the decision against another similar brand.
It is important for companies in the medical distribution industry to set themselves apart when marketing their business or products, so consumers choose your company over other options.
So, why is establishing brand awareness important? And how can your brand implement it?
With so many companies to choose from in today’s marketplace, healthcare industry consumers especially want to make purchases from brands that they know well and trust.
Consumers can do extensive research on a brand online and read about other consumer’s opinions of the company before ever making a purchasing decision of their own. Companies can leverage technology as an advantage and do extensive online marketing to reach more customers. When consumers are familiar with a brand and have experienced it
many times in advertisements, they are more likely to trust the company and continue to make purchases.
Strategically placed advertisements aimed toward a company’s target audiences attract a consumer’s attention and create an awareness of the brand. Health systems can advertise through social media, event sponsorship, magazines, newspapers, and online, etc., which all creates visual imagery of a brand and fosters increased awareness among consumers. Through online, social media, and event advertising, consumers view and interact with content, thus learning about the brand and creating customer recognition. Targeted ads on platforms such as Facebook, Instagram, and LinkedIn allow consumers to interact with posts, comment, and provide feedback, all of which spread the word about a brand.
Brand equity is the value of a brand. Equity is determined by positive consumer experiences and brand perception. Effective brand awareness tactics create repetitive positive experiences with a brand for a customer.
When a customer is aware of a brand, they recognize it, make purchasing decisions, and start to prefer it over other similar brands. This preference over other brands for consumers indicates high brand awareness and will help to build a brand’s long-term equity.
Brands within the medical distribution industry can greatly benefit from increasing their brand awareness. Share Moving Media, with over 30 years of experience working within the medical supply chain industry, can help your brand create the content that is needed to foster consumer’s trust and increase brand awareness and equity.
When a customer is aware of a brand, they recognize it, make purchasing decisions, and start to prefer it over other similar brands. This preference over other brands for consumers indicates high brand awareness and will help to build a brand’s long-term equity.
Today’s marketplace is saturated with numerous forms of advertising. For companies in the medical distribution industry, finding a niche within the busy marketing space has become challenging. How can your company stand out among other medical suppliers?
Niche marketing is the promotion of a product or service to a specialized segment of the market. With niche marketing, businesses target specific audiences to promote their brand. Niche marketing allows a business, such as a healthcare supply company, to understand the specific needs of the consumer and tailor their marketing strategy to meet those needs.
A brand can determine subsections of the market to target by considering demographic information, attitudes, values, geographic location, and more, of specific market groups. In the healthcare space, that could be hospitals, health systems, IDNs and GPOs.
Read on for examples of successful niche marketing campaigns from other sectors of the economy:
Whole Foods grocery stores target a niche market of affluent, conscious consumers who focus on health and well-being. Many Whole Foods products are organic and environmentally conscious, which targets a very specific audience that desires a high-quality and luxury grocery store experience.
The online mattress brand Casper targets specific market segments through creative online media content that encourages customers to
interact with the brand’s site. Content including blogs, social media posts, and an extensive website engage consumers with the goal of them making purchasing decisions.
3 Square Square is a payment system for small businesses, non-profit organizations, and independent companies that can be used by plugging the system into phones or tablets to process credit card transactions. The niche market of
small business owners may not have the resources to pay high credit card fees and Square targets this small market segment with their unique technological solution.
Share Moving Media can assist you with determining the marketing tactics that will set your brand apart. With over 30 years of experience in the healthcare and medical distribution industry, we can help you develop the content your brand needs to stand out.
Free community-based mental health screenings through Project Health allow underrepresented communities to gain access to behavioral healthcare.
Mental Health services have seen increased demand throughout the United States as a result of the COVID-19 pandemic. According to the American Psychological Association in a November 2022 press release, the demand for treatment for trauma and stressor related disorders and substance use disorders has grown since the pandemic began. Seventynine percent of psychologists said they had seen an increase in the number of patients with anxiety disorders since the beginning of the pandemic, and 66% saw an increase in demand for treatment of depression. Despite more patients needing behavioral care, many are unable to receive the screenings, tests, and treatment they need due to healthcare access barriers.

In an effort to address the behavioral healthcare gap nationally, CVS Health announced it will enhance its free community-based behavioral health program through Project Health, the organization’s mental health screening service.
Project Health offers free, no insurance necessary health assessment screenings, such as tests for blood pressure, Body Mass Index (BMI), glucose and total cholesterol screenings, and mental health screenings. These tests can help detect the risk for chronic conditions like diabetes, hypertension, and heart disease. Early detection can identify chronic illnesses before they become life-threatening and also reduce national healthcare dollars spent on these diseases.
Since 2006, Project Health has hosted free community events to keep communities healthy. Patients that attend have access to in-pharmacy assessments, mobile care units, and the Project Health mobile health application.
Project Health events are hosted at CVS Pharmacy locations and at community organizations. CVS Health plans to host nearly 2,000 Project Health screening events across the U.S. in 2023 and add nearly 100 organizations as mobile unit hosts going forward. Health screening sites will now also offer Patient Health Questionnaire (PHQ-2) assessments to identify individuals who require additional evaluation for depression. Following the health screenings, participants can meet with a nurse practitioner who can provide referrals for treatment and advice for follow-up care.
“We continue to see a need for accessible mental health care across
the country,” said Sheryl Burke, SVP of Corporate Social Responsibility and Chief Sustainability Officer. “Our events now serve more communities than ever, tapping into our CVS Pharmacy footprint and a vast network of local organizations to host our mobile units and help ensure transportation is not a barrier to receiving health services.”

Many communities face barriers to quality healthcare or lack access altogether due to factors including lack of insurance, transportation barriers, healthcare staffing shortages, etc. Project Health helps to bridge healthcare access gaps through accessible treatment locations, which
allow individuals who would otherwise go without healthcare to get the services and treatment they need.
Project Health focuses on introducing accessible treatment locations in areas of significant need and to populations that have been historically under-resourced. In 2022, 82% of people who received care at a Project Health event identified as a race other than White/Caucasian, and 68% reported a household income below $50,000.
Last year, CVS provided $5.5 million dollars in free medical services, and hosted nearly 1,700 events. Project Health’s aims to increase the amount of people who are able to access mental and behavioral health services within communities that otherwise would not have access.
Health screening sites will now also offer Patient Health Questionnaire (PHQ-2) assessments to identify individuals who require additional evaluation for depression.
Nephron Nitrile announces new CEO Nephron Nitrile announced William “Billy” Emerson Harris has been named Chief Executive Officer. In this position, Harris will use his 30 years of experience to bolster the recent onshore manufacturing and distribution investment Nephron Nitrile is making in West Columbia, S.C. The facility is estimated to produce nearly three billion nitrile gloves per year.

“Having Billy join our team is a win-win – for Nephron Nitrile and South Carolina manufacturing,” said Nephron Nitrile Owner Lou Kennedy. “Throughout his career, Billy has successfully navigated the challenges of a growing and changing industry. His experience and goaldriven approach to business and leadership will ensure our talented team continues to achieve the ambitious objectives we set at the beginning of this journey: to offer customers the next level in Made-in-America glove manufacturing and distribution right here in our state, strengthening the domestic supply chain and creating new jobs.”
“It is all about having U.S.-produced exam and general-purpose disposable nitrile gloves,” said Harris. “I could not turn down the opportunity to join an organization with such a strong commitment to best-inclass automated manufacturing and quality that exceeds industry standards.”
Prior to joining the Nephron Nitrile team, Harris served as Chief Commerce Officer of SHOWA Group, a fully integrated manufacturer of both medical and industrial PPE hand protection. He has more than three decades of manufacturing industry experience, including serving as Birtcher Medical Systems Director of International Sales, Vice President of Sales at Adams Scientific, CEO of Sempermed USA and CEO of Sri Trang USA, Inc.
BD announced that it has signed a definitive agreement to sell its surgical instrumentation platform to STERIS for $540 million. The sale includes V. Mueller™, Snowden-Pencer™ and Genesis™ branded products and three manufacturing
facilities located in St. Louis, Mo., Cleveland, Ohio and Tuttlingen, Germany. Approximately 360 employees who support this platform will transfer to STERIS upon the completion of the transaction. The sale is expected to close within BD’s fiscal year 2023, on September 30.
STERIS is a leading global provider of products and services that support patient care with an emphasis on infection prevention. With global sales of $5 billion, STERIS has more than 17,000 dedicated associates around the world working together to supply a broad array of infection prevention and other procedural products and services, focused primarily on health care, pharmaceutical, medical device and dental customers. BD’s surgical instrumentation platform is complementary to STERIS’s Healthcare segment and will allow them to better meet hospitals’ and surgery centers’ product and service needs.
“The Surgical Instrumentation platform has a 120-year legacy of providing reliable and trusted highquality products, and STERIS is well positioned to maximize the value of this extensive portfolio and is fortunate to be adding such a dedicated and talented team to its organization,” said Rick Byrd, president of the Interventional segment at BD. “This transaction further advances the BD Interventional segment’s focus on high-growth end markets. We look forward to continuing to address unmet needs in health care through a highly differentiated and innovative set of solutions and products.”
Cardinal Health announced its plans to build a new distribution center in the Greenville, South Carolina, area, to support its at-Home Solutions business, a market-leading home healthcare medical supplies provider serving people with chronic and serious health conditions in the United States.
At approximately 350,000 square feet, the new building will provide at-Home Solutions with the space and automation it needs to serve its existing customers and patients while allowing for business expansion. The new facility is at-Home Solutions 11th distribution center nationwide, estimated to bring up to 200 job opportunities to the Greenville region over the next two years.
While the distribution center has the capability to support all 50 states, its primary focus will be customers located in the Carolinas, Virginia, Georgia, Alabama,
Tennessee, Missouri and Louisiana. Once operational, it will ship approximately 8,000 packages per day directly to patient homes. The business currently ships approximately 55,000 packages per day from its 10 sites.
Advanced automation technology and robotics within the facility, including outbound conveyor automation and state-of-the-art warehouse management systems, will further increase inventory capacity and improve service levels for the business so the right products can be at the right place at the right time.
This will be the second Cardinal Health distribution center to feature AutoStore empowered by Swisslog, the fastest order fulfillment system per square foot in the market.
Henry Schein donates healthcare products to support Special Olympics Healthy Athletes screenings at the 2023 Special Olympics World Games
Henry Schein supported the Special Olympics Healthy Athletes® screenings at the Special Olympics World Games, that took place from 17 to 25 June 2023 in Berlin, Germany, by donating a range of oral health and medical products essential to overall health and wellness. The Healthy Athletes program offers health screenings and education to participating Special Olympics athletes with the goal of promoting healthy lifestyle choices and identifying problems that may need additional follow-up care.
Henry Schein has supported Special Olympics since 2018 donating essential health care products to support programs in the United States, Canada, Germany, Israel, Jamaica, and the United Kingdom. Through this partnership, the Company has been named a Special Olympics health provider partner.
According to Special Olympics, an organization recognized by the International Olympic Committee, people with intellectual disabilities are frequently among the most medically vulnerable populations in any country, despite severe need and higher health risks.
Henry Schein’s donations will be used during the Special Olympic World Games for screenings in five of the Healthy Athletes disciplines, including Special Smiles, which provides athletes with comprehensive oral health care information, free dental screenings, instructions on proper brushing and flossing techniques, and if needed, a referral to a dental care provider at home trained to treat people with intellectual disabilities. Henry Schein’s donations also support Fit Feet (podiatry), FUNFitness (physical therapy), Health Promotion (prevention and nutrition), and Strong Minds (emotional health).
Since its inception in 1997, Healthy Athletes has delivered over two million free health screenings and trained over 300,000 health care professionals, clinical volunteers, and students in using adapted screening protocols and in communicating effectively with people with intellectual disabilities.
Medline announced that after more than 26 years of leadership, Charlie Mills (CEO), Andy Mills (President) and Jim Abrams (COO) will retire from their current roles. They will continue to serve the company on its Board of Directors, with Charlie Mills leading as Chairman of the Board and Andy Mills and Jim Abrams as Vice Chairmen. To culminate a five-year succession planning process, Medline has elevated company executives Jim Boyle to serve as the next Chief Executive Officer, and Jim Pigott as the next President & Chief Operating Officer. The leadership transition will be effective October 1, 2023.
“Jim Boyle and Jim Pigott have been instrumental in Medline’s growth and success during their nearly 60 years combined within the organization, and we are excited for them to lead us into the future,” said Charlie Mills, current chief executive officer of Medline. “In blending Medline’s high-performance culture and customer-centric approach with their extensive understanding of healthcare, they are perfectly suited to propel Medline forward while continuing to build upon our rich legacy.”
Boyle joined Medline in 1996 and has served as Executive Vice President since 2018, managing its customer base of over 5,000 healthcare providers across the continuum of care and overseeing more than $21 billion of annual sales. Boyle was responsible for the strategic direction and execution of the commercial functions across all healthcare segments, as well as the Marketing, Operations and Logistics departments. In addition, he oversaw Medline’s distributed products business and led the customer support infrastructure, meeting the unique challenges of Medline’s customer base and its patient communities.
Pigott joined Medline in 1992 and most recently served as Executive Vice President. In this role, he oversaw the strategy and execution of Medline’s 27 product divisions, comprised of more than 20 manufacturing sites and 14,000 employees. In addition, Pigott led Medline’s global sourcing and inventory management organizations. Over the years, he was involved in the company’s expansion into several product segments, including surgical, laboratory, diagnostics and cardiology, as well as the growth of its domestic manufacturing footprint.
Watch
Heart disease is the leading cause of death in the US. 1 That’s why early detection is not only important—it can save lives. The Midmark Digital ECG brings the patient, provider and EMR together at the front line of care.

EMR Connectivity
Works seamlessly with today’s top EMR systems
Workflow
See data, test and store reports in one place

Signal Strength
Capture high-quality cardiac waveforms


