Excellence in Sales

 Mike Malec CME Corp.
John Ballarin Abbott
Mike Malec CME Corp.
John Ballarin Abbott

 Henri P. Lori
Henri P. Lori



 Mike Malec CME Corp.
John Ballarin Abbott
Mike Malec CME Corp.
John Ballarin Abbott

 Henri P. Lori
Henri P. Lori

In this issue, we asked two of the top salespeople, Mike Malec, a CME Corp. account manager, and John Ballarin V, Central Region account executive for Abbott Rapid Diagnostics, for their insights and approach. Malec and Ballarin were honored this spring as the winners’ of this year’s Excellence in Sales Award. While their stories are unique, I read them to see what common threads reps can take away and use in their day-to-day interactions with customers and supplier partners.
The following are three of those threads: Communicate. “There was a time when our customers could cut a purchase order five or six weeks before they wanted their project delivered,” Malec said. “We would likely have everything delivered to our warehouse, and assembled and ready for delivery and placement, in plenty of time.” That’s no longer the case, he points out. “Today, we are lucky to receive half of the required items in that time frame. So, it’s critical to communicate closely with our customers about current lead times, as well as with the manufacturers about any changes in delivery times.
Collaborate. Ballarin said he promises a few things to his distribution partners: “‘I will be the quickest of any manufacturer rep to respond. I will give you and your customers the truth. If you bring me to a deal, it’s yours. If I do not know the answer, I will find it. You will have my support after the sale. I will make it easy for you, and I will always deliver on what I say I am going to do.’ These might sound very basic, but I have found that by doing these things, we manufacturer reps can earn their trust – which is the golden word, and what I always strive to earn.”
Connect. “If our manufacturer partners are confident in my ability to handle projects and see them through to completion, they can trust they are in good hands looking ahead at new opportunities,” Malec says. “Once manufacturer reps achieve this comfort level with their distributor reps, I believe they are more likely to want to continue the relationship.”
Dedicated to the Industry, R. Scott Adams
editorial staff editor
Mark Thill
mthill@sharemovingmedia.com
managing editor
Graham Garrison ggarrison@sharemovingmedia.com
editor-in-chief, Dail-eNews
Pete Mercer pmercer@sharemovingmedia.com
art director
Brent Cashman bcashman@sharemovingmedia.com
circulation
Laura Gantert lgantert@sharemovingmedia.com
sales executive
Amy Cochran acochran@sharemovingmedia.com
(800) 536.5312 x5279
publisher
Scott Adams sadams@sharemovingmedia.com

(800) 536.5312 x5256
founder Brian Taylor btaylor@sharemovingmedia.com
Subscriptions www.repertoiremag.com/subscribe or (800) 536-5312 x5259
Repertoire is published monthly by Share Moving Media 350 Town Center Ave, Ste 201 Suwanee, GA 30024-6914
Phone: (800) 536-5312, FAX: (770) 709-5432; e-mail: info@sharemovingmedia.com; www.sharemovingmedia.com

Now is the time to review, assess, and take action with your clients and their lab business.

In most of the country, the warm weather and longer days are signs that spring is about to transition into summer. What, you ask, does this have to do with physician office lab and distribution sales in general? Fair question. The short answer is that if you have not done so already, now is the time to shake off the “work from home” doldrums of the COVID pandemic and get back to running your territory full blast, with in-person customer meetings scheduled and a commitment to holding meaningful dialogue with your current and prospective customers.
It sounds easy, but the changes wrought by COVID have impacted us and our customers in profound ways. Getting back to a normal routine of personal calls, interspersed with virtual calls as needed, may take a commitment to use the best of the new tools we learned during the COVID pandemic and weaving them into our former customer call routine.
By Jim Poggi
In this column, I intend to take a page out of my grandmother’s book and discuss “spring cleaning”: getting ourselves mentally ready to drive the business as well as possible and improve customer satisfaction and revenue results at the same time. Follow along with me as I propose some time honored (and some new) ways to get back in the swing of things and feel fully in control and prepared for whatever comes our way!
First, no one is prepared without a thorough review of their customer
data. Have you analyzed the spend patterns of your top customers? Do you know their spend gaps by product category? Are you seeing trends in lab spend (either positive or negative) that you need to understand more fully? Are there any red flags concerning spend, satisfaction or supply chain issues that you need to acknowledge and address? Are you ready to present a quarterly business review discussing their situation and needs as well as their current spend patterns with you and your company?
For lab customers in particular, there are a number of issues you

always need to stay in front of. For instance, do any of your top customers have leases expiring soon? In my world, “soon” is within the next 12 months. Be sure to discuss lease renewal or acquisition of upgraded equipment early so it can be budgeted for and any technical questions get a fair and complete hearing. Is preventive maintenance of key equipment up to date? Be sure to check on maintenance intervals with your key lab suppliers. In addition, be sure to hold discussions on QC and proficiency testing results with your large lab instrument customers. It’s a best practice to schedule specific meetings with the involved supplier partners, the lab staff and lab manager to review the data and discuss any actions needed. At the same time, I strongly recommend reviewing training needs with the lab manager and your key lab suppliers, particularly if there has been staff turnover.
With the whirlwind of new lab tests, have you kept your key customers informed? If you have not, the danger is that someone else has! Be sure to check the lab benches and refrigerator to make sure you know which important tests your customer is using and who they are getting them from. The first key to achieve business growth is to avoid lost business. A sharp eye and appropriate questions with the lab staff and lab manager will prevent surprises. Be sure to also review your customers’ rapid order guides and standing orders to make sure they are up to date and that you are retaining the business you have worked so hard to get.
If discussions of new tests has fallen behind for any reason, be sure to
fully assess your customer’s testing needs, any questions they may have about new tests and schedule time with the appropriate lab suppliers to discuss and even demonstrate the latest technology.

Product demonstrations provide an exciting opportunity to create engagement with the staff and management of the physician office lab. These can be a great way to add a little excitement to your routine visits and cause the customer to think of their lab business in new ways with your guidance and that of your key lab manufacturers.
I would particularly focus on new products and technologies that fit well in their practice and patient population. Molecular tests and systems are constantly changing and represent a clear opportunity to discuss testing needs, especially before the onset of seasonal respiratory season. Your ongoing customer business reviews should take on these issues and set the stage for future success for your customer. Their satisfaction is your assurance of future business.
One key to renewing your customer relationships as we return to
a more normal pattern of personal visits is to treat each of your current customers as if they were new again. If you approach your customers with this mindset, you will be surprised at the new information you gain and you will also be able to perceive a very positive response from your customer based on how much care and thought you put into approaching them as if they were new once again. Spring is a time of renewal, and the certainly applies to our customer relationships.
Finally, good preparation allows you to be prepared for the unexpected
as well as major market changes you need to respond to. As an example, there are likely to be changes coming with EUA products in the near future. EUA clearance for EUA devices including lab tests is not parallel to the duration of Public Health Emergency that ended in mid-May, and the U.S. FDA has issued guidelines for transition of IVD tests from EUA to clearance under prevailing non-EUA standards. The defining FDA document was published on March 27, 2023 under the title: “Transition Plan for Medical Devices That Fall Within Enforcement Policies Issued During the Coronavirus Disease 2019 (COVID19) Public Health Emergency Guidance for Industry.”
Your key manufacturers are in the best position to inform you about their specific plans to transition their test kits under this guidance document. It is my expectation that the FDA’s guidance is intended to assure continued availability of needed respiratory tests as the EUA policies transition to the more typical oversight processes and procedures of the FDA for lab tests. Their guidance document makes it clear that they are sensitive to the needs of the public, as well as lab manufacturers, distributors and laboratories using these products.
Now is the time to get your basic business planning in place so you have time to deal with these changes and the emergence of this year’s respiratory season. “Luck is what happens when preparation meets opportunity” as the Roman philosopher Seneca observed. Lab has changed since Seneca’s days, but the need for thoughtful preparation has only become more important. An effective commitment to spring cleaning will reap rewards all year long. Are you ready?
Product demonstrations provide an exciting opportunity to create engagement with the staff and management of the physician office lab. These can be a great way to add a little excitement to your routine visits and cause the customer to think of their lab business in new ways with your guidance and that of your key lab manufacturers.





* In the USA, this product has not been FDA cleared or approved but has been authorized by the FDA under an Emergency Use Authorization for use by authorized laboratories; use by laboratories certified under the CLIA, 42 U.S.C. §263a, that meet requirements to perform moderate, high, or waived complexity tests. The product is authorized for use at the Point of Care (POC), i.e., in patient care settings operating under a CLIA Certificate of Waiver, Certificate of Compliance, or Certificate of Accreditation.
This product has been authorized only for the detection of proteins from SARS-CoV-2, influenza A and influenza B, not for any other viruses or pathogens; and, in the USA, the emergency use of this product is only authorized for the duration of the declaration that circumstances exist justifying the authorization of emergency use of in vitro diagnostics for detection and/or diagnosis of COVID 19 under Section 564(b)(1) of the Federal Food, Drug and Cosmetic Act, 21 U.S.C. §360bbb-3(b)(1), unless the declaration is terminated or authorization is revoked sooner.


 By Pete Mercer
By Pete Mercer
In an era of widespread resignations and “quiet quitting,” what is the most valuable thing that business leaders can take away from all the shifts in the workplace dynamic? If nothing else, it seems that everyone has decided that sanity is a necessity. Creating sane working environments is critical to the welfare of your workforce and the productivity of your organization.
Repertoire Magazine recently sat down with sales expert, keynote speaker and author Tim Richardson to discuss the importance of maintaining a sane and productive workplace. Richardson has worked for IBM and a Five Diamond resort property, and he’s worked as a professional speaker for almost 35 years.
For Richardson, the reasons why the office is so stressful for so
many people revolve around four primary expectations:
ʯ Individual performance expectations
ʯ Organizational performance expectations
ʯ End-user/customer expectations
ʯ Workforce expectations
“I think work expectations and anticipated outcomes are at an alltime high. Also, customer expectations are higher than ever and it’s critically important to get them right. If we fall short of our customer expectations, everyone has a megaphone in their pocket and can communicate mistakes with hundreds, even thousands, of people in an instant.”
Expectations are now more complex. For instance, on the one hand you have the always high organizational performance expectations of the shareholders and stockholders of the organization, while you also must contend with the dynamic expectations of a diverse workforce. “If you just break the diverse workforce down by generational preferences, that is complex enough,” Richardson said. “Just think about being in a leadership position and having to cater to people with very different work styles and needs.”
Since 2020, working in an office has become more complex. COVID-19 created so much chaos and disruption for the workplace, sending many “nonessential workers” to be furloughed or work from home. While working from home has become widely accepted, it took some significant adjusting for a lot of people to settle into what was, for many, a new way of working.
“Workplace comradery was severely lacking for quite a long period of time creating loneliness,
Why sane working environments are critical to the welfare of a workforce and the productivity of an organization.Tim Richardson
Diagnosing and managing hypertension starts with accurate BP measurements — so your customers need technology they can trust. The Welch Allyn Spot Vital Signs 4400 device offers:

• Ease of use
• Built-in BP Averaging
• Accurate BP Measurement with SureBP
• EMR connectivity

anxiety, and family challenges as parents had to rearrange their work lives while their kids were at home,” Richardson said. “Not only did you have to manage your own feelings around mental health, but you were responsible for gauging the mental health of people around you.”
In fact, COVID is the reason that Richardson spends so much time speaking about mental health and creating a sane workplace. “I had a long pause where I didn’t do any of the things that not only provide an income for me, but also provide me with a sense of purpose. Ultimately, my speaking focus came as a result of what I call the pandemic pause.”
breaks, then workers aren’t going to be on their A-game and they certainly aren’t going to have time for new thinking and innovation,” Richardson said.
When employees feel that they need to be available 24/7, they sacrifice personal time with their families, or they can’t completely log off when they are “on vacation,” which creates a culture where they don’t feel that they can draw the line between their work life and personal life.
Richardson said, “We need time to recoup, we need time to rest, we need time to renew and restore. We need very clearly defined expectations. I think if a leader is intentional
We need to honor that people need renewal time and give people down time to refuel.”
When the work-life balance is achieved, it gives people the time to recharge and come back to the office prepared to meet the goals the organization has set and bring new ideas to the table. It’s even more effective when business leaders are modeling that behavior for their teams, giving them a picture of what that balance looks like in practice.
In order to be truly effective in this arena, leadership needs to be intentional with how people look at their workload. For Richardson, many business leaders will need a sort of “altar call” to let them know that they’ve been taking the wrong approach.
For business leaders looking to take the reins and bring sanity back into their workspace, it’s important to set reasonable expectations for the office. Expectations are, of course, a part of the system, but there’s a significant difference between reasonable expectations and the kind of expectations that can kill morale.
“An overworked person is more likely to suffer from negative mental health concerns that are more common now than ever. If workloads are so high that there is no time for
and has well established priorities, they’re going to create those clear expectations for people that include time to pause.”
The first step to establishing sanity is allowing people to truly clock out at the end of the day and take time for themselves. Workaholics have a hard time with a work-life balance, but it’s critical to the mental and physical health of your employees, as well as their productivity when they are on the clock. “Many professionals wear busy like it’s a badge of honor, when it should be more rewarding to be totally in control.
When he worked for IBM, the last day of each month had everyone on the sales teams trying to earn their commission by pushing their prospects to make the final purchase. At the time, Richardson processed orders for PCs and mainframe computers that were being sold. His manager would come by and check on his team’s workflow.
If they were overloaded with orders, he would redistribute work. Because of his manager’s intentionality and intervention, it created sanity in a moment of chaos. Richardson said, “Leaders need to be visible, they need to be observing, they need to be understanding, and they need to have respect for employees and their personal lives. As simple and as basic as it sounds, all these things would improve workplace conditions, employee morale, employee retention, and even profitability.”
“We need time to recoup, we need time to rest, we need time to renew and restore. We need very clearly defined expectations. I think if a leader is intentional and has well established priorities, they’re going to create those clear expectations for people that include time to pause.”
Save time and decrease infection risk by reducing potential skin contact with Dukal’s easy-to-open technology. Dukal Stat Strip® Adhesive Bandages’ specially designed wrapper makes hygienic application as easy as grip, pull and apply - even with gloves.

Scan with your phone’s camera to request your free Stat Strip® sample.

Grip Pull
Apply
Apply
As a leader in the development and manufacturing of medical products, we partner with healthcare professionals to launch innovative solutions to unmet clinical needs.
> To learn more visit dukal.com
Pull to open and expose one side of the adhesive bandage. Grip both ends of the wrapper firmly. exposed side of bandage to skin, and pull to apply the other end. By Brian Sullivan
By Brian Sullivan
Recently on my podcast (Golf Underground with Co-Host Hall of Famer George Brett), we interviewed Hollywood actor Peter Dante. If you don’t know who Dante is, simply turn on TBS or TNT any weekend and no doubt you will see him as the quarterback in the movie “Waterboy,” or catch him in many other Adam Sandler movies such as “Grown Ups 2,” “Big Daddy,” “Little Nicky” and more. OK, let’s admit it, these movies are not exactly “cerebral cinema” designed to stretch your mind, but they sure are fun.
I asked Pete what his goal was when he left his East Coast life and moved to California on a whim, and was surprised by his response. He said he wasn’t quite sure what he wanted when he moved; he just knew he had to take a chance.
After landing a job on the Larry Sanders show as a production assistant, he began meeting several actors, one of them being Adam Sandler. That led to several other relationships that created a network of highpowered folks in the entertainment
industry. It also got him introduced to his wife Cindy, who is Brad Pitt’s manager. When I asked, “What’s the formula to creating such a powerful network?” his answer was amazingly simple. He said, “I like to have fun. I smile and laugh a lot and because of
that, I think people like being around me. That alone has opened up more doors than I could have ever imagined. I also don’t expect anything in return. I like a lot of people and a lot of people seem to like me back. Some call it networking, but I’m not sure what I call it. “
What a concept! Here are some other “Grown Up” tips we can learn from Dante that will help make you the star of your company and sales territory:
1. Give, Give and Give…and don’t do it with the intention of getting rich off others. Do it because it’s fun.
2. Ask questions and learn about others before telling them about you, your company or products.
3. Plan your Grown Up Networking by thinking about people you always wanted to meet. Make a list, then put yourself in a position to meet them. Commit to reaching out to one new person each day and be personal with the message. Firing off mass emails hoping to grow deep relationships is NOT very Dante like. Make this a habit and one year later you will know a ton of new people.
4. Go where you haven’t gone. If you aren’t meeting enough new people, it’s because you keep hanging in the same circles. You can keep your existing ones, but to expand your influence, you need new circles. Consider going outside your industry to learn fresh ideas and
perspectives. Join associations, local business groups or charitable organizations. Those places are loaded with the type of people you need to surround yourself with.
5. Ask for permission, then ask for help. Don’t be afraid to ask for introductions. One of the biggest problems with below average business/salespeople is they “sit on” the relationships they have. If you sell, ask your current customer “friends” to introduce you to others in that account. Trust me, those people are making decisions that affect your paycheck.
9. Dismiss nobody. What’s worse than somebody who thinks they are above others? Many accounts have been lost because a salesperson treated that “lower level” decisionmaker like a second-class citizen.
10. Expect to be in the room. The most successful people in business (or in Hollywood) at some point found themselves in a room full of high-powered people and wondered how the heck they got there. Act like you belong … because you do! Lastly, if you want to meet more people and build a ton of relationships, be the energy source in every
6. Share your network. The most successful businesspeople in any industry are those offering to introduce their friends to others. This leads to introductions that will expand your circle.
7. Follow up. If you make a new relationship, don’t leave it hanging. Give them a call or send an email telling your new buddy you are here to help them anytime. Or better yet, drop a quick hand-written note.
8. Don’t be a complainer. Enough said.
room. And the by-product of your great attitude and above average enthusiasm is … you will meet a ton of people who want you around. And their wanting will often lead to a few extra bucks in your pocket and perhaps a starring role in your company or industry. That’s when you will have become a Grown Up Business Star.
To learn how to become the Star of your industry, visit us at preciseselling.com. And if you love to laugh (whether you like golf or not), head over to your favorite podcast site and check out Golf Underground with Wardo, Sully and George Brett.
As Founder of PRECISE Selling, Brian Sullivan, CSP creates top performers in sales, customer service, negotiations, leadership, and presentation skills through seminars and Internet training programs. He is also the author of the book, 20 Days to the Top-How the PRECISE Selling Formula Will Make You Your Company’s Top Sales Performer in 20 Days or Less. To learn more, go to www.preciseselling.com.
If you aren’t meeting enough new people, it’s because you keep hanging in the same circles. You can keep your existing ones, but to expand your influence, you need new circles.
June is post-traumatic stress disorder (PTSD) Awareness Month. How can PTSD symptoms be recognized and treated?
Post-traumatic stress disorder (PTSD) awareness month is recognized each year in June. PTSD is a mental health condition that develops at any age in individuals who have witnessed a life-threatening event such as combat, natural disasters, car accidents, sexual assault, etc. About 6 out of every 100 people (or 6% of the U.S. population) will have PTSD at some point in their lives, according to the U.S. Department of Veterans Affairs’ National Center for PTSD.

Witnessing a life-threatening event can cause the onset of PTSD immediatly after, but symptoms may also appear months or years later. Symptoms of post-traumatic stress disorder include reliving a traumatic event (flashbacks), avoiding things that remind an individual of a traumatic event, having more negative thoughts and feelings than before the event, and feeling on edge. Symptoms can be triggered by external stimuli, such as hearing news reports, witnessing accidents, or seeing fireworks that cause an individual to relive the event or experience flashbacks. PTSD can also include avoidance of places, events, or objects that are reminders of a traumatic event.
After experiencing a life-threatening scenario, many individuals may experience the symptoms of PTSD, but some go on to develop chronic PTSD. Symptoms that last more than a month, are very upsetting, or that interfere with daily life are considered chronic PTSD, according to the U.S. Department of Veterans Affairs.
Treatments for PTSD include medication, psychotherapy, or a combination of both. Medications, such as selective serotonin reuptake inhibitors (SSRIs) and serotoninnorepinephrine reuptake inhibitors (SNRIs) help control sadness, worry, fear, and other psychological symptoms associated with the disorder.
Trauma-focused psychotherapy counseling aims to treat patients by focusing on the specific traumatic event witnessed. Psychotherapies include Cognitive Processing Therapy (CPT), where patients learn the skills to understand how trauma has
changed their thoughts and feelings and help with working toward emotional responses related to the event. Prolonged Exposure (PE) is a therapy that includes discussing a trauma repeatedly until the memories are no longer upsetting to regain control. Eye Movement Desensitization and Reprocessing (EMDR) involves focusing on sounds or hand movements while talking about the trauma so that the brain is able to process traumatic memories.
Treatments for PTSD can lead to a better quality of life for those that live with the condition. In the month of June and throughout the year, the U.S. Department of Veterans Affairs aims to spread the word to everyone afflicted with PTSD that effective treatments are available to help manage symptoms.
According to the National Institute of Mental Health, factors that may promote recovery after a traumatic event include seeking out support from friends and family, finding a support group, and developing a positive coping strategy.

With the same great protec tion you get from a Wolf barrier, this model features the ability to position the clear lead at any level between 45.25” and 74” for the ultimate in patient and operational visibility I t ’s great for dozens of applications.
Best of all, the internal counter balance mechanism makes it easy to lif t or lower…it requires minimal

• O verall width: 30.5”
• Opaque por tion of the shield has .8mm lead equivalent protec tion
• Clear panel provides .5mm lead equivalent protec tion


• 25” legs with casters provide strength, durability and easy transpor t within the clinic

• The per fec t right size solution for any environment: OR, ER, C T, X-ray, Urology, Pain Management, and Surgical Centers
• When lowered allows rapid transpor t to any location in hospital or clinic and easy-to -store

How wellness affects our professional lives.
By Pete MercerEveryone hits a point in their career where they feel stagnant. This can be the result of a number of factors, but the solution is often the same: personal wellness. Our wellness is a significant contributing factor to how we perceive and inhabit our daily lives. In most of the modern professional settings, we can find ways to either improve our outlook or surroundings. All it takes is a fresh perspective on the obstacles you are facing and a game plan to overcome them.

Repertoire Magazine recently sat down with Eileen O’Grady to discuss her idea of intentional change. O’Grady is a nurse practitioner and life coach, who helps people disrupt their own self-defeating behavior. In both the clinical and professional setting, she uses the idea of “intentional change” to help people find healthy growth paths to improve their lives.
O’Grady’s concept of intentional change is just about as straightforward as it sounds. It’s the idea that we can identify something that needs to change in our lives and take the active steps required to intentionally make that change. This concept is accessible to anyone who is willing to look inward and find ways they can improve themselves.
“People will come to me and say, ‘I’m overweight.’ And I’ll ask why. They’ll just say, ‘Well, I eat too much.’ And that’s often not the situation. It’s one or two very specific behaviors,” O’Grady explained. “Intentional change is this idea that each human being could have their own growth edge. Every problem has a solution, even if it means accepting the problem. That’s an intentional change.”
That intentionality is perhaps the most challenging part – it requires action that might be uncomfortable, especially if we are surrounded by things that will cause us to chase certain behaviors or habits. O’Grady said, “In order to be healthy and well in this society, we have to be super intentional. Just going out in the world, there are so many toxins that we get exposed to.”
O’Grady argues that we are heavily influenced by what we surround ourselves with, which can
make any intentional change much harder. Essentially, the very thing that might be holding us back from our greatest potential is our surrounding environment.
Because of the highly suggestive nature of people, it’s easy to get swept up in old habits. This is why O’Grady and her team work on coaching people and their environment at the same time.

She said, “When we’re coaching people, we often will coach the environment. Anyone that is trying to stop drinking or smoking, they often have to change their friends because there’s so much contagion with those behaviors. We all have that one friend that we get into trouble with when we go out. I don’t think we appreciate the contagion effect of these social behaviors.”
The process of changing our environment can be as in-depth and as difficult as we make it. We have to highlight the things around us that trigger certain behaviors and habits and remove them. For example, if someone wants to stop drinking,

they might need to avoid bars or restaurants that serve alcohol.
“It’s as simple as having some sort of sanctuary effect in your home. You don’t want to walk into your home and feel a cortisol hit because there’s clutter everywhere. Cleaning up our environment has a huge effect on our behavior,” O’Grady said.
The same is true for our workspaces. We spend most of our time in our workspace during the week, whether it’s a home office or an office building. When we let things like clutter and chaos creep into our working environments, it can create obstacles for productivity and unnecessary levels of stress that will interfere with our workflows.
Peace in the workplace is crucial to productivity. O’Grady said, “I think it’s really helpful to have regular meetings to talk about team norms and things like clutter in the break room. What can we do to have more peace in our workplace? We need open, candid conversations that address the tough issues to ensure that we have psychological safety in the workplace.”

The reason that our personal wellness impacts how we perform in the workplace is that all of our systems are interconnected. If we aren’t getting enough sleep or are otherwise ignoring some sort of crucial function, it can throw everything else off balance.
O’Grady argued that a lack of something as important as sleep often leaves us with short fuses, causes bad interactions with our coworkers, and significantly affects productivity. She said, “We have some pretty clear evidence that even
if you spend a few minutes a day in meditation or prayer, we can change our brain and become less reactive to our environment. Who doesn’t want to sign up for that?”
For business leaders, it’s especially important to lead a life that includes habits that improve our mental and physical health. Without a model for healthy habits and behavior for your organization, it’s hard to expect that there’s any recipe for success for your employees. O’Grady said, “We really can’t lead other people unless we’re becoming the CEO of our own lives.”
The idea of “becoming the CEO of your own life” means that we need to take back control from our surroundings and our bad habits, whether
we are struggling with mental or physical wellness.
When we become the CEO of our lives, we can better regulate ourselves and our emotional lives. We need to come into work rested, fed, and watered: basic, bedrock behaviors that will help us to thrive in what can be a stressful setting.
This is especially true for people who work in high stress jobs like healthcare. It’s no secret that healthcare professionals have been put through one of the most challenging periods in recent history with the COVID-19 pandemic. There are
countless (and continuous) stories of healthcare professionals who have hit a wall after experiencing high levels of stress and burnout. O’Grady said, “I really believe that having a high degree of well-being in ourselves and cultivating and promoting is a core leadership tenant. What we see, at least in the healthcare sector where I’m working, is that people can’t do this really hard job unless they’re really well resourced.”
That’s a universal truth for anyone working in a stressful industry or a toxic organization. Even if you aren’t in a leadership position to make changes within your organization, you can still make yourself the CEO of your own life. All it requires is making the right decisions for what you want and what you need to be productive in personal and professional settings.
“Intentional change is this idea that each human being could have their own growth edge. Every problem has a solution, even if it means accepting the problem. That’s an intentional change.”
Whether surgeons perform simple medical examinations or complex surgical procedures, they require a well-lit environment. A healthcare provider must see clearly to perform the surgery successfully. An operating room’s instruments and devices are rendered useless without appropriate lighting.
Choosing surgical lighting for a facility is not a responsibility that should be taken lightly. Key criteria for selecting the right light for a facility include efficiency, intensity, color rendition index, color temperature, and shadow control. By understanding these criteria, customers can choose high-quality, dependable lighting with a name they trust, Bovie®.
Symmetry Surgical®, now part of Aspen Surgical®, offers a broad portfolio of Bovie LED lights for exams, procedures, and surgical applications. Each application has similar requirements for color rendering, color temperature, and shadow control. The Bovie MI Series lights provide the best of all these criteria.

Today’s efficient LED lights use about half the electricity of their older halogen counterparts and generate little radiated heat, which can dehydrate tissue during a procedure. Halogen bulbs may only last 1,000 hours, while the LED bulbs used in Bovie’s MI Series lights are rated to last 50,000 hours.
Intensity relates to brightness and is measured in Lux. The higher the Lux, the brighter the light. With procedure and surgical lights, Lux is typically measured with the light source positioned an industry standard one meter (39”) from the subject site.
Color Rendition Index (CRI) measures a light's ability to accurately show an object’s colors when compared to natural light. It is measured on a scale of 0 to 100, with 100 being the best. All Bovie MI Series lights are rated with a CRI of 95 or higher.
Color temperature measures the color emitted by a light source and is measured in degrees Kelvin (°K) with daylight ranging from 4800 to 5100°K. Lower color temperatures (<4000°K) appear yellow, while higher color temperatures (>5400°K)
appear blue. For example, a dermatological condition can be difficult to diagnose in lighting that is too yellow or blue. The optimal color temperature for healthcare facilities is between 4000 and 4500°K. All Bovie LED lights emit a color temperature of 4300°K.
Shadow control reduces shadows in the surgical field due to instruments, hands, and heads beneath the light source. Larger lighting sources illuminate all sides of the surgical field. Bovie MI Series lights include many bulbs that articulate smoothly through an eleven-foot diameter to provide maneuverability and range to reduce shadows. Dual lighting heads are also available to mitigate shadows from the surgical site.
The ability to control the brightness, position, and direction of MI Series lights from within the sterile field allows the medical staff to operate more efficiently without breaking the sterile field or assigning an additional assistant to operate the lights.
Bovie’s MI Series LED lights include a wide range of options. MI 150 and MI 300 gooseneck examination lights are space-saving designs offering brilliant, color-accurate illumination. The MI 150 includes a single power setting and a fixed base, and the MI 300 features a sturdy rolling base and two power settings.
The MI 550 examination light is a compact but powerful design that emits 55,000 Lux of pure white illumination in single ceiling mount, dual ceiling mount, wall mount, and portable options.
The MI 750 light produces 75,000 Lux, plenty of light intensity for examinations and procedures. With two rings of LED bulbs providing excellent illumination for the reduction of shadows, and a sterilizable handle that includes the On/Off and three-stage dimming switches to allow the user to maintain the sterile field, this versatile model is available in single ceiling mount, dual ceiling mount, wall mount, and portable options.
The MI 1000 light provides flexibility and longevity to the surgical
suite. Its three rings of LED bulbs create a large array that provides exceptional shadow control. Available in single ceiling mount, dual ceiling mount, wall mount, and portable options, this workhorse includes five-stage dimming and On/Off switches on the sterilizable handle, plus an ambient light mode for minimally invasive procedures.

Do you need more light intensity for your surgery center, specialty practice, or outpatient care facility?
Bovie’s System Two surgical lights include the illumination characteristics of the MI Series LED lights, provide five-stage dimming (with ambient light mode) and On/Off switches on a sterilizable handle, and provide 130,000 Lux intensity in ceiling-mounted single, dual, and triple arm options capable of holding 32” video monitors and in-light mounted HD cameras.
Bovie medical lighting includes the full range of lighting criteria you need and the Bovie name you trust. Bovie medical lighting — an illuminating idea!


The dust has settled. The peaks and valleys of supply and demand of surface disinfection have gotten back to normal. Now is the perfect time to make a quick assessment of what surface disinfection products your customers have been using, and what might be needed moving forward. There have been so many improvements to the products in the market, a simple review will provide your accounts with the guidance needed.
First, look at the product label. This can be done with a physical inspection, or by reviewing the manufacturers’ product sell sheet, or website. Surface disinfectants are registered with the EPA, and EPA registration numbers are found on the product label.
Does the product used have the right kill claims for today’s complex environment? Certain pathogens are harder to kill than others. Sometimes it’s not about how many pathogens are listed on a label. The question is, are they the right ones for your account? If the facility has isolation areas, or high-risk patients (example: patients with C. difficile ) the recommendation is a product with sporicidal efficacy. Spores like C. difficile are hard to kill, so bleach or certain hydrogen peroxides are recommended.
 By Paul Girouard
By Paul Girouard
For general procedure areas, or clinical areas with sensitive equipment, a non-bleach would be recommended due to the corrosive nature of bleach. The most commonly used formulations used here are quaternary ammonium/alcohol disinfectants.
There are specific microorganisms to check for that are important because they are representative of a broader range of pathogens (TB is an example).
Clear steps you can take to determine if your accounts have the right surface disinfection products on hand.
An area of product improvement over the past few years has been kill times. Productivity has improved greatly as kill times have come down from 10 minutes to 1 minute on the newest products in the market. A kill time is defined as how quickly the product kills the listed pathogens. If there are several different times listed for different pathogens, you must take the longest time listed as the kill time for that disinfectant overall.
Wet times are also an important characteristic for review. The surface being disinfected needs to remain wet for the longest kill time on its label to be effective. Disinfectants are formulated so they do not evaporate too quickly. If they do, they will
not be effective and the surface disinfectant will need to be re-applied. There are other attributes of disinfectants that are important but a little more subjective. Is the odor pleasing? Does it leave a film on the surface, or is it compatible? Is it ready to use or does the staff need to mix and prepare?
It has been an interesting time in the surface disinfection
category. There have been significant leaps forward in product development. There are more options, new formulations, better performance of several known brands in the market. Change creates opportunities for you as a salesperson. Take this opportunity to provide guidance to your accounts and grow your infection prevention business.

Does the product used have the right kill claims for today’s complex environment? Certain pathogens are harder to kill than others. Sometimes it’s not about how many pathogens are listed on a label.
Trust Metrex’s portfolio of surface disinfection wipes to bring value to your customers and help you clean up.
Supply chain has played an important part in the building of UC Health’s new emergency department. It will play an even bigger role when the facility opens this year.
By Graham GarrisonEmergency services are a big part of UC Health’s legacy. The UC Department of Emergency Medicine is home to the first residency training program in the U.S., and the program celebrated its 50th anniversary in 2020. The department attracts top medical students from across the country to train in Cincinnati, and its faculty are national leaders in clinical teaching and research.
When UC Health got the greenlight to build a new facility for its emergency department from the ground up, leadership wanted the physical building to match their top tier ranking from a clinical perspective. To do that, they needed supply chain to play a key role.

The project was announced in October 2019. Ground was broken on the structures in late summer 2021, and completion is expected in late summer 2023, according to the IDN. The project includes:
ʯ Expand the UC Medical Center Emergency Department (ED) onto a previously vacant lot
adjacent to the hospital. The 41,000-square-foot addition will significantly improve capacity and patient flow, including reconfigured access for patient arrivals via ambulance and private vehicles.
ʯ Renovate the existing 35,000-square-foot ED to provide additional emergency response ability and “surge” capacity for emergency and crisis situations.
ʯ New construction of three additional floors above the new emergency department to accommodate an observation unit, a flexible ICU and a new 28-bed unit.
ʯ New construction of a four-story surgical building that will expand surgical capacity at the hospital, adding eight new operating rooms as well as new waiting areas and pre-operative clinics.
During the design phase, UC Health leadership that included supply chain and clinicians took a few trips across the country to look at best-in-class emergency department set ups, including Mayo Clinic, to determine how they wanted to set up their facility.

From a supply chain perspective, it was beneficial to be included early in the process, said Harold Dillow, assistant vice president of supply chain for UC Health. He has spent a lot of time with the emergency management service line people that represent College of Medicine, emergency management physicians, and then with UC Health’s own nursing administration that runs the ED to better understand what their expectations are for a best-in-class ED, and how the supply chain would service them. There are monthly meetings between supply chain, ED leadership that includes nursing and College of Medicine representatives,
and a consultancy agency quarterbacking the process to talk about the progress of the project.
From theoretical to actual UC Health’s current service model involves stocking a supply room in a couple of areas in the ED. Clinicians, nurses or technicians retrieve the supplies on their own. In the new ED, clinicians would like supply chain to provide everything they need at the point-of-use of where the care is being delivered, so the clinical person never has to leave patient care area or the “bedside”. It takes resources, more staff members and a new supply stocking strategy that UC Health’s team has been developing to be ready to roll out when the new ED is scheduled to open in July 2023. “It is fundamentally different than how we do
what the clinicians think would be the most used products at appropriate par levels. To stock the carts for the entire ED, supply chain will be allocated a large supply room in the middle of the space. The new ED is roughly the same number of rooms, but double the footprint.
“We have a lot of input on the design of the supply room because we want it to be big enough to not only have our inventory system hanging on the wall, but also space in the middle for the exchange carts to be restocked,” Dillow said. “We can take a full exchange cart, go to a room and grab one that’s been used and put the full one in. Theoretically there’s always plenty of supplies in every single room.”
Some parts of the process are already in place. For instance, last April, UC Health implemented a new point-of-use inventory management system that tracks supplies better and reorders with RFID technology. It’s a much more efficient way of reordering supplies, Dillow said. “So, setting up a best-in-class process and then layering on some technology we think is going to be a really awesome combination.”
it now,” Dillow said. “Now they retrieve supplies as opposed to us putting it at their fingertips.”
UC Health is developing an exchange cart process for the new ED. The concept is to always have supplies as close to full for the clinical team. Every single ED bay will have a cart stocked according to
Supply chain is working on a myriad of small details for the new ED, such as the routes they would use to stock rooms, and when they would do it, so they’re more offstage from the public. They’ve worked on where the carts are going to be staged in the rooms, and will eventually focus on the individual items the clinicians want in the carts.
“We’ve even gotten it down to what color handles should be on the carts, and the visual cue to let everyone know that a cart’s been used,” Dillow said. “Those are the granular types of decisions we’re figuring out so it can flow as smoothly as possible.”
Dillow said he’s excited to see the efficiencies gained from the new model. The estimated increased bedtime for clinicians alone was high enough to get a healthy FTE approval to build up the supply chain team in the ED for 24/7 across three shifts. “The goal is to have everybody practicing at the top of their license,” he said. “The nurses and physicians can be honed in on what they’re doing to help the patient as opposed to worrying about grabbing supplies. There’s going to be huge intangible cost savings, but more importantly real savings for the patient care time.”
The supply chain team has been quite busy over the last 12 months, and not just on the new ED rollout. Recent accomplishments include:
ʯ Managed through the highest surge of pandemic and ongoing global supply disruptions while supporting clinical operations. “Many in the industry experienced this the past few years, but it is worth recognizing our supply chain team’s extraordinary effort to deliver quality products in a timely manner with the odds stacked against them,” Dillow said. “While many items were procured via alternate sources or had to be converted, which resulted in clinicians having to use non-preferred product, we had great partnerships with the clinical team.”
ʯ Reduced capital investment for instrument purchases to support the new surgical building. Supply chain and UC Health’s Perioperative

Leadership Team partnered to calculate current instrument utilization and compare that to expanded case volumes to ensure only needed items were purchased. ʯ Simultaneously implemented two technology systems. UC Health chose to perform an ERP conversion and MMIS/WMS conversion at the same time.
“I will say it was very difficult to implement two systems concurrently, but the team put forth an exhaustive effort to accomplish this goal,” Dillow said. “These new platforms enable us to gain efficiencies from automating processes that have traditionally been manual work. We intentionally refined and documented our manual processes so that we could layer on technology that would
More than 70% of admitted patients need peripheral IV catheters.1 Catheter securement is essential to help prevent motion-related IV complications.

B. Braun Medical’s Clik-FIX catheter securement devices are designed with patient care in mind. Made with a cushioning foam base, Clik-FIX is designed to maximize patient comfort and help reduce the risk of pressure injuries from the catheter hub.
To learn more about B. Braun Medical’s full line of Catheter Securement Devices, visit bbraunusa.com/clikfix.
take us forward and not just be an expensive program built on inefficient, legacy processes.”
ʯ Completed a GPO RFP. This was a large initiative that required strategic alignment across several departments (Finance, Supply Chain, Pharmacy) and included clinical partners.
“The result was UC Health selecting a GPO partner that most closely understood our needs as a health system that includes an AMC and community-based acute care hospitals and large ambulatory footprint. This will deliver the highest quality contracts and products, and largest savings opportunities for UC Health.”


Another major achievement was managing through an extreme staffing crisis in Sterile Processing Department (SPD) where a large portion of the staff was recruited away for agency staffing companies. This directly impacted SPD’s ability to meet instrument tray demand for OR cases, Dillow said.
As a result, the SPD tray backlog, which is an indicator of SPD’s throughput and ability to provide ontime service, soared from a historical average of 50 trays to approximately 500 trays. Supply chain and PLT met multiple times per week for several months to jointly address the issue. A shared staffing model was implemented as an interim countermeasure as well as OR capacity management to ensure all scheduled cases were cared for. These interventions, combined with a coordinated recruiting effort with HR, resulted in the tray backlog returning to under 50.
“Over the last five to six years, supply chain has aligned and clinically integrated with our physician partners across all service lines,” said Dillow.
He said the springboard for this elevated engagement and alignment occurred because of their participation and involvement with the value analysis program and department specific product / implant standardization and savings initiatives related to:
ʯ Ortho Trauma implants.
ʯ Cardiology – CRM / DES.
ʯ Ortho Total Joints.
ʯ ENT – Cochlear implants.
ʯ Cardiovascular – Heart valves.
ʯ Radiology – Peripheral vascular products.
ʯ Ortho / Neuro spine implants.


Building trust through transparency and partnership with aligning clinical quality needs and outcomes with cost efficiencies has been one key to success. No silo product decisions or changes without alignment of providers has been another key. Supply chain has also partnered with the chief medical officer to appoint a medical director for supply chain. “This has really helped navigate conversations with physicians and gain buy-in for service line product strategy.”
Halfway into 2023, supply disruptions and staffing availability remain challenges to address. “The pandemic largely focused on PPE items,” Dillow said. “Once those were secured, it was really about operationalizing the stocking strategy needed to support COVID care.”
But since then, global supply disruptions are affecting a much broader portfolio of products. “There’s almost
no category that isn’t affected. Who would’ve thought crutches, of all things, would ever be an issue? That’s just one example of many.”
Because of this, UC Health’s sourcing and procurement teams have experienced a 900% increase in backorders. “The constant management of alternate sourcing and related logistics is very time consuming, and quite frankly, frustrating for the team.”
Once you get the product, there is the additional worry of appropriate staffing levels needed to manage the inventory. In the case of SPD, its staffing needed to build case carts to support the OR.
It’s hard to reflect on the last few years and not think about battle scars, Dillow said. However, the challenges presented during the pandemic and staffing crisis have silver linings. “We had to quickly adapt during those times to survive, and the key to surviving resulted in doing things differently.”
Although UC Health continually stress tests its processes to find
UC Health’s sterile processing department (which reports to supply chain) has consistently averaged less than one patient safety issue per month reported in its clinical quality database. “This is an enormous achievement considering the average was 160 issues/month in 2017. This continues to be the most important initiative we focus on and measure.”
Since 2016, UC Health’s supply chain has delivered an ROI of 8:1 when comparing achieved savings versus team investment. “In a world of financial uncertainty, supply chain is uniquely positioned to be one of very few departments that can deliver that type of value to the organization,” Dillow said. “There is a tremendous amount of work and cross-team collaboration within supply chain and with
improvement, those test scenarios simply didn’t include a once-in-a-century pandemic or having such a staffing deficit. So they adopted innovative ideas from their teams to create better processes and standardized those efforts where they made sense to carry on. “As a result, we have a better understanding of our end-to-end operations with process maps created because of the need to increase the speed of communication amongst supply chain teams, suppliers, and clinicians.”
UC Health also consolidated many reports and data sources that different supply chain leaders were using to manage the business. Now there is one source of truth that pulls together inventory levels, sourcing notes, and procurement information to make educated decisions based on a complete picture. “Lastly, we now have increased automation and data visibility that helps us be more proactive decision makers instead of always reacting and firefighting,” Dillow said.
clinical partners to develop strategy and execute projects that deliver these savings. I am extremely proud we continue to deliver year-over-year results to UC Health.”
One of the UC Health system-wide strategic pillars is “Community Commitment.” Embedded within that pillar is a goal to improve the economic vitality of local businesses, Dillow said. To achieve this goal, UC Health has an objective to increase women- and minority-owned enterprise spend to 6% by 2025, which is a 1% increase over the current goal. “To meet this goal, we have a well-developed Diversity program within supply chain that leads to engagement with community partners. Not only do we routinely host a forum open to the public that connects diverse vendors with UC Health leaders, but we also invest time in diverse supplier development.”
Novant Health and YMCA of Northwest North Carolina launch strategic partnership.
Novant Health and YMCA of Northwest North Carolina recently announced they have partnered to create integrated healthcare access for the Northwest North Carolina region.
Novant Health is a system of physician practices, hospitals and outpatient centers that focus on community wellness and convenience of healthcare access. The Northwest North Carolina YMCA encompasses 17 branch locations across Alexander, Davie, Forsyth, Iredell, Stokes, Wilkes, and Yadkin counties in North Carolina. Together, the organizations will expand wellness programming, support youth sports, and establish physical and telehealth clinic locations with the goal of creating integrated healthcare access throughout the region.
The primary focus of the partnership is to reach underserved and rural communities. Novant Health aims to increase health access points by introducing healthcare services in frequented, community-based centers such as the YMCA.
The partnership will “expand combined services, create new and innovative programming, and bring additional healthcare opportunities to East Winston, one of our most vulnerable areas, with a new, in-branch clinic,” said Darryl Head, president and CEO of the YMCA of Northwest North Carolina.
Novant Health is in the process of opening an innovative community care facility inside of the Winston Lake Family YMCA in Winston-Salem, North Carolina. The clinic, planned for opening in 2024, will offer primary care, women and children’s services, rehabilitation, and nutrition support.
While in the process of building the permanent clinic, Novant Health has already started providing patient
care through their Mobile Community Care Cruiser. The Novant Health Community Care Cruiser provides nontraditional healthcare access to further remove barriers to care. The mobile cruiser-based clinic improves community access to routine screenings, vaccines, nutrition education and counseling free of cost.
Wellness programming is imperative to maintain and improve overall population health, especially for communities that lack access to critical care.
“From diabetes prevention to cancer survivorship, Novant Health and the YMCA have always offered complementary services for our communities,” said Chad Setliff, senior vice president and president of Novant Health’s Winston-Salem market. “Moving forward, we’ll offer a more integrated wellness experience that leverages the best of both organizations to improve health outcomes for patients and members, strengthen wellness offerings, and reduce barriers to care through a combination of digital tools and co-located clinics.”
Other ways that Novant Health is increasing community healthcare access is through telehealth portals. Planned for the YMCA’s rural locations, each virtual-health portal will be equipped with a telehealth platform to offer patients on-demand and remote medical exams. Patients can connect to the platform through the “Tytocare” mobile phone application which virtually connects a patient at a portal to a clinician. Through the app, a clinician can examine the patient’s heart, lungs, skin, ears, throat, and abdomen without the need for costly travel costs associated with a visit to the emergency room or doctor’s office.
Planned for the YMCA’s rural locations, each virtual-health portal will be equipped with a telehealth platform to offer patients on-demand and remote medical exams.
What is excellence in sales? Numbers help, for sure. But every Repertoire reader knows it’s more than that. It’s that drive to get better, to help people, to have an impact on something meaningful. More often than not, it’s also fun. Since 2000, Repertoire recognizes two people – one from the distributor side, one from the manufacturer side –who embody that excellence. See if you can’t find something of yourself in their stories.

2023 Mike Malec, CME Corp.
2020 Stacy Comb, Claflin Company
2019 Jarrel Watkins, McKesson
2018 Mike McGoldrick, Henry Schein
2017 Victor Bakkar, McKesson Medical-Surgical
2016 Mike Ludwig, Henry Schein
2015 Todd Matthews, McKesson Medical-Surgical
2014 Chuck Ryan, McKesson Medical-Surgical
2012 Paul Lilly, McKesson Medical-Surgical
2011 KC Meleski, CME Corp.
2010 Steve Marshall, Cardinal Health
2009 Rich Bilz, Henry Schein
2008 Tom Jacob, McKesson Medical-Surgical
2007 Dick Daley, Affiliated Healthcare Systems
2006 Mike Leva, CME Corp.
2005 Marty McCurdy, PSS
2004 Denise Hassler, Caligor
2003 James Barnes, Cardinal Health
2002 Jim Wheeler, Seneca Medical
2001 Linda Phillip, McKesson Extended Care
2000 Brad Jacob, McKessonHBOC

John Ballarin V, Abbott Rapid Diagnostics
Claire Bishop, Quidel
Stephen Raggio, Welch Allyn
Dianna Hundl, Quidel
Patrick Thombs, Clorox Healthcare
Chris Huppert, Midmark
Nick Riordan, Welch Allyn
Nate Williams, Midmark
Louis Cupo, Cardiac Science
Mimi Hobson, Terumo
Mike Paige, Med Care Associates
Tommy Whitehead, Midmark
Denny Monnin, Midmark
Bob Chaldu, TIDI Products
Jack Moran, Med Care Associates
Steve Bakalar, Welch Allyn
Jeff Daner, Midmark
Close contact is essential for success in equipment sales.
After 34 years in medical sales, CME Corp. account manager Mike Malec still maintains there is nothing like a face-to-face meeting when it comes to connecting with your customers or suppliers. By the same token, it took but a few in-person meetings with CME’s Chris Godfrey and K.C. Meleski to cement his interest in joining the company, which has proved to be a great fit since he came on board in 2017. Malec is the recipient of the 2023 Excellence in Sales Award for a Distributor.
small ad in the Chicago Tribune for a medical sales rep position at The Burrows Company, a med/surg distributor in Wheeling, Illinois.” He was hired for the position and given a territory primarily on the South Side of Chicago.
Malec enjoyed his experience in non-disposable sales at The Burrows Company before moving to DeKroyftMetz in Central Illinois, where he began focusing on equipment. As much as he enjoyed working at DeKroyftMetz, he realized that working for a company without access to private label disposables could present a challenge when competing against large, national distributors. “That’s when I considered moving into equipment sales and service,” he says. “I had a great experience selling equipment with The Burrows Company and had retained some good contacts with the medical equipment manufacturers. I still had a high level of comfort talking about – and selling – equipment.”
His start in the industry following his college graduation might well be attributed to serendipity. “After graduating from Marquette University in 1989, I knew I wanted to pursue a career in sales – I just wasn’t certain what industry to join,” Malec recalls. A bit of research on his part suggested the medical profession could offer the growth and stability he was looking for. “I really didn’t know anything about medical sales at the time but decided to answer a
Malec decided to explore a position with CME. “After meeting with Chris Godfrey and K.C. Meleski, I was especially intrigued with the idea of joining the company,” he says. “For one, Chris and I had a lot in common, from our work experiences to many of our personal interests. The more I learned about CME, the more impressed I became with its business model, its all-encompassing medical equipment solution and the people who work there. It was – and continues to be – a great fit.”
As relationships in the industry have shifted, and delivery lead times and product availability have become more challenging, communication with customers and providers has become more important than ever, says Malec.


“There was a time when our customers could cut a purchase order five or six weeks before they wanted their project delivered. We would likely have everything delivered to our warehouse, and assembled and ready for delivery and placement, in plenty of time.” That’s no longer the case, he points out. “Today, we are lucky to receive half of the required items in that time frame. So, it’s critical to communicate closely with our customers about current lead times, as well as with the manufacturers about any changes in delivery times.
“Setting expectations with our customers is key,” he continues. “It’s essential to get involved with them early
Dawn Sheldon, director of client relations, MAC Medical Inc.
“Mike exemplifies professionalism and customer satisfaction. He listens to the true needs of the client and works as a partner with his suppliers in providing a true solution to meet their need. Mike will provide consistent followthrough from conception to closure of the project, ensuring customer satisfaction.”
Nate Williams, national accounts executive, Midmark
“Mike has an outstanding level of service, professionalism and followthrough and successfully masters the relationship building between manufacturer, dealer and customer, which is critical in our solution selling model. He’s a hard-working, top-performing professional who’s a pleasure to be around.”
Terry Mulheron, region director East, Champion
“Mike is a total professional who understands how to conduct business. He is a valued and dedicated partner of ours who has our full trust and confidence due to
in the process to give them a clear idea of what – and when – they need to order. The last thing we want is for a project to be delayed because equipment is not delivered. Our goal at CME is to be highly educated in the industry so that we can help our customers achieve their goal of opening on time, within their budget.”
It’s equally important to maintain close communication with his supplier partners as well, notes Malec. “Our VP of vendor relations, Mike Abbott, states it best: It all comes down to communication and collaboration. Working together, sharing contacts, ideas and opportunities is what truly ties the distributor rep to their manufacturer
his commitment, professionalism and kindness.”
Gregory Kwiatkowski, key account executive, Essendant
“Mike is the consummate professional, bringing relationship management expertise, as well as a profound understanding of the solutions and benefits to his ferociously loyal clients. He exemplifies what an authentic, trusted advisor should be to his clients and his colleagues.”
Frank Rowe, VP, sales & marketing, R&B wire Products, Inc.
“Mike provides outstanding support to his supplier partners in providing their products to meet his customer’s needs. He is willing to spend the time to get it right in all situations that he is involved in. I wish him all the best and good luck!”
Thomas Kosmowski, national sales manager, Novum Medical Products
“Mike is a true professional and great at relationship building between manufacturer, dealer and customer, which is critical in sales
and account management today. He is consistently engaged with our company and one of the top dealer reps we work with year in, year out.”
Rob Napkori,
“Mike is dedicated to his customers and ensures they have exactly what they need to meet their shortand long-term requirements. Mike couples his knowledge and experience in healthcare to strengthen relationships and be his customers’ source of information pertinent to their jobs. He is the consummate professional.”
“Over the past seven years, it has been a pleasure working with Mike. In each instance, Mike has been there, whether he’s accessing the lead or bringing me in with the quote and product information –up to and through the close. In a business climate where a cryptic text or an abbreviated email are all too common, Mike maintains a personal touch, which is what makes the difference between acceptable and excellent.”
partners. I’m a firm believer in forming relationships. Especially as electronic communications have become so prevalent, removing much of the human element necessary to building strong relationships, I find myself picking up the phone whenever possible. Better yet, a face-to-face meeting is still the best way to make a connection.
“If our manufacturer partners are confident in my ability to handle projects and see them through to completion, they can trust they are in good hands looking ahead at new opportunities,” he says. “Once manufacturer reps achieve this comfort level with their distributor reps, I believe they are more likely to want to continue the relationship.”
This especially holds true as he finds himself working with new contacts in different roles. “When I first began focusing on equipment sales, I primarily dealt with materials/purchasing people and project managers at the hospital or IDN whenever equipment was part of a project. Now, more often than not, I work with equipment planners who work on behalf of the provider. This has added another customer base to our business. In fact, some of my best customers today are equipment planners. We all strive to accomplish the same goal, so it truly is a team effort with all parties involved.”
The best way to stay relevant in the workplace is to go to work every day and give it your all, notes Malec. The same goes for his personal life. “Just as I work hard to ensure my customers see me as a reliable, valuable individual who gets the job done for them, I make it a point to always be available for my family.” Whether at work or at home, it’s so important that others can rely on you, he adds. “It’s one of the most important responsibilities we have.”

‘It’s critical to communicate closely with our customers about current lead times, as well as with the manufacturers about any changes in delivery times.’
Fifth-generation John Ballarin aims to win, just like the four before him.
For generations, the Ballarins of Michigan have been hard workers, competitors, winners. Could John Ballarin V –Central Region account executive for Abbott Rapid Diagnostics – have turned out any other way? Probably not. He is the recipient of the 2023 Excellence in Sales Award for a Manufacturer.

Born and raised in Westland, Michigan, about 16 miles from downtown Detroit, Ballarin received early training in automotive sales from his father, John Ballarin IV, for whom he worked two summers out of high school. “It was my first job, as he wanted me to ‘learn to put on a suit and go to work’ at a young age. I remember changing from my dress clothes to baseball clothes in the dealership bathroom so that I could head to baseball practice after working all day.”
A 41-year veteran of the automotive industry, Ballarin’s father was Top-Selling National Sales Consultant with Lincoln/Mercury for three consecutive years in the 1990s. He helped his dealership – Bill Brown Ford –bring the title of World’s No. 1 Ford Dealership home to Detroit for the first time in decades.
“He worked extremely hard, and advocated for all of his customers,” says his son. “His customers meant the world to him, and it was evident at his retirement based on how many customers were in that room and had been long-time family friends. I learned how important trust and relationships are – the foundation of everything.”
His grandfather – John Ballarin III – was a tough Korean War veteran who worked for the Michigan Consolidated Gas Company, or Michcon. “He hated to lose, no matter what,” says his grandson. “He came to all my games growing up and always wore the team hat. My father is the same way. Hates to lose, even if it’s a backyard game. I think that’s why he won’t golf with me unless it’s a scramble.”
His father built his business on referrals, he says. “This is how he managed to scale and sell 30+ cars a month on a consecutive basis. He treated everyone fairly and was honest with them. I witnessed him telling people, ‘Now might not be the right time for you to move forward with this deal.’ It was just so confusing to me, but now it all makes sense.
“Word spreads quickly when people are happy with the buying process. I also learned the sale is just the beginning of a relationship. That relationship is built on



service after the sale, [which] makes the next one that much easier.”
The senior Ballarin continues to play ice hockey four days a week. “Ask how the game went, you get the score, and how many goals he scored,” says his son. “Competitive edge is always there.”
At Madonna University in Livonia, Michigan, Ballarin was a starting pitcher and an integral part of the 2010 champions of the Wolverine-Hoosier Athletic Conference and an NAIA tournament contender. The Crusaders went 48-11 that year. Ballarin’s stats: 6 wins 2 losses, 3.30 ERA.
“We had a great team and a lot of fun,” he recalls. “It was a good group of guys who knew how to work
hard and play hard.” He turned down an opportunity to play professionally in the Peach State League. “I was a somewhat tall, left-handed pitcher who threw mid-80s and had an above-average curveball. (I never could figure out the changeup.) I knew that if I went off to play ball, it would delay everything else, and my chances of ‘making it’ were probably not that good. Most would think it was a tough decision, but for me it was pretty easy. I knew what I wanted in life.”
He never doubted the choice. “Healthcare had my interest at a very young age,” he says. “My mom was a nurse, and I always felt that working in healthcare gives you a sense of purpose. Having the privilege to be involved with products that ultimately reach the patient and make communities a better place is exciting to me.” Early on, he thought about pursuing the clinical side of medicine, “but those rotations didn’t work with college baseball,” he says. Instead he decided to pursue allied health administration.
His first exposure to the healthcare supply chain came during a four-month internship at Detroit Medical Center in 2009. He was part of the med/surg distribution RFP team and accompanied them on site visits to the distribution centers of potential partners.
In 2010, after graduating from Madonna, he joined Detroit Medical Center as a dispatcher/parts sourcing specialist, clinical engineering. One year later he joined Henry Ford Health System as a strategic sourcing analyst in capital equipment. In 2013 he took a short detour from healthcare to become North America 3PL performance relationship manager for chemical company BASF. In 2016 he rejoined healthcare, first as national account manager for Henry Schein with responsibility for Trinity Health, and later as senior manager national accounts for the Eastern U.S. In 2019 he joined HealthTrust Purchasing Group as an account director, and one year later, came to Abbott.

‘Having the privilege to be involved with products that ultimately reach the patient and make communities a better place is exciting to me.’

“Every move has had a purpose, and I am thankful for all of them,” he says. “They have allowed me to see every side of the healthcare sales/supply chain and even gain a small amount of experience in another industry’s supply chain.

“A lot of this has happened by chance or phone calls from friends telling me about an opportunity. This is a large industry, but it is small. It is important that you develop your own brand because people do business with people they trust. However, it’s not just about ‘being friends.’ When I say relationships, I mean being a trusted advisor, always bringing value and keeping communication open.
“I keep in touch with many people from every company that I have worked at. My network means the world to me, and I will never take it for granted. We always are sharing industry news, helping each other with contacts, bouncing ideas off each other, or simply having fun. Fun is important too, and I will try to never lose that.”
Even as a college intern at Detroit Medical Center, Ballarin displayed an interest in analytics, developing hospital-specific budgets for service contracts, repairs and maintenance. When he joined DMC full-time, he developed an organizational service log for service calls and assisted in developing a parts inventory management system. As strategic sourcing analyst at Henry Ford, he reduced the number of days needed for monthly reporting from four to one by identifying areas for improvement and implementing effective formulas.
At BASF, he played a key role in establishing and monitoring key performance indicators for third-party logistics providers and managed more than 150 third-party workers’ access rights in a database system. While at Henry Schein, he received Lean Six Sigma Greenbelt training, and at HealthTrust, he partnered with his client – Trinity Health – to reboot quarterly business reviews involving all key stakeholders, including food, energy management and med/surg. At Abbott, in addition to achieving steady growth in sales, he was selected to expose new hires to best practices in working with distribution.
“I work hard to keep myself out of the weeds, but I do have a very process-oriented mindset. I decided to go into project management, because really, everything is essentially ‘managing a project,’ especially when working with large customers or deals.
“In large accounts, I think an analytical approach fits very well,” he says. “They expect structure, and I think if you can bring them that skillset and help them plan their next capital budget, improve service line management or be part of their strategic growth plan, you are viewed as far more than a ‘sales rep’ and you might even be called their ‘trusted partner.’ That’s always my goal when working with a client.”
Using analytics, account executives can help customers with standardization, SKU consolidation, waste elimination, staffing and even workflow enhancements, he adds. “It’s about taking a good relationship and making it great. Helping them run a better business.”
As valuable as it is, analytics will never totally replace traditional sales skills, such as pre-call planning, relying on gut feelings, relationship-building and simply working harder than the next guy, says Ballarin. “I will never be the smartest individual on any team or in any room, but I will be willing to outwork anyone,” he says. “It’s something that was instilled in me at a young age. I always want to be the best at everything I do, and I put in my work.
“The people who win are those who understand their customers and realize there is no one-size-fits-all solution,” he continues. “You need to get to know your customers and bring value they might not even be thinking about. You work so hard that you know more about them than they know about themselves.
“When done best, it shouldn’t even feel like ‘selling.’ It should be putting in place a mutually beneficial solution to help them run a better business and take care of their patients. And as people’s workloads are expanding, the easier you can make someone’s job or the more value you can bring them, the better your chance of winning.”
“I promise a few things to my distribution partners: ‘I will be the quickest of any manufacturer rep to respond. I will give you and your customers the truth. If you bring me to a deal, it’s yours. If I do not know the answer, I will find it. You will have my support after the sale. I will make it easy for you, and I will always deliver on what I say I am going to do.’ These might sound very basic, but I have found that by doing these things, we manufacturer reps can earn their trust – which is the golden word, and what I always strive to earn.
“You know it’s working when a distribution rep calls you and says, ‘Can you go to account ABC and do a demo?’ There’s nothing more fulfilling than walking out of that account, knowing it’s a great fit for the customer and their patients, and calling the distribution rep to say ‘We got it done.’”
Ballarin applies the same approach to his work with distributors. “Coming from distribution myself, I understand that distribution ‘holds the keys to the kingdom,’” he says. “They are in accounts every day, holding the responsibility of being trusted consultants on everything from gauze to medical equipment.
Abbott Rapid Diagnostics account executive John Ballarin V will always remain grateful for his years spent playing high school- and college-level baseball.
“Baseball is so applicable to life and work in many ways,” he says. “If I had to pick a few things, one would be to ‘focus on the next pitch.’ As a starting pitcher, I would throw about 100 pitches a game. If I got in my head about one bad pitch, I knew that wouldn’t make for a good game, as there were 99 more to go.”
For their part, distributors should take advantage of ride days with their manufacturer partners, he says. “They work, and heck, we always seem to have a lot of fun doing them. Open communication is always key. Let me know if something isn’t working at an account or what I can do better.
“Distribution has thousands of products to sell. My goal is to make their life easier when selling my product. I am forever grateful for my distribution reps and will always show up for them when they need me. They are the lifeline of this business.”
Another lesson? Learning to fail. “Baseball is amazing. You can fail at the plate seven out of 10 times, but if you do that your entire career, you will be in the Hall of Fame. So, it’s learning to deal with failure and keeping the momentum going forward. “The other thing I learned was the importance of preparation. Playing baseball in Michigan, you are at a disadvantage with people who play outside year-round. It’s about figuring out where and how to train,
and staying sharp in the off-season. A lot of this relates to life. You might be dealt a little different situation than someone next to you, but how are you going to play that hand and WIN?”
Ballarin remains involved with the game today. He and his wife, Katie, have three boys – 6-year-old John VI and 4-year-old twins, Jake and Luke. “My boys are starting to get into sports now, and it is so fun to watch and be a part of.”
‘I work hard to keep myself out of the weeds, but I do have a very process-oriented mindset.’

Government procurement is a large and growing segment of the healthcare distribution market. That’s why HIDA recently published our Federal Procurement Market Report, to quantify the contribution of federal spending to the medical supply chain in unprecedented detail. With a total spend of $8.2 billion in contracts to healthcare distributors and manufacturers in 2021, the federal government is a major purchaser of medical supplies.

in purchases in FY 2020 to approximately $842 million in FY 2021. This accounts for approximately $3.7 billion of the approximately $4.9 billion federal government purchasing difference between FY 2020 and FY 2021.
Small businesses accounted for a significant proportion of the federal government’s medical supply purchases. Federal incentives for small business provide opportunities for the many small and independent distributors and manufacturers in the medical supply chain. Such support for all businesses – from national to local – diversifies the source of medical supplies, building resilience and capacity in the event of future surges in demand.
ByPurchases dropped 38% from FY 2020, but remained well above pre-pandemic numbers. In FY 2021, civilian departments/agencies accounted for $4.7 billion and defense departments/agencies $3.4 billion in medical supply purchases. About 98% of the federal government’s medical supply purchases were made by four departments. It makes sense for the overwhelming majority of federal purchases in the medical supply chain to be made by agencies tasked with preparedness (Department of Homeland Security), agencies with significant patient needs (Department of Defense, Veterans Affairs), or both (Health and Human Services).
Federal purchases related to the COVID-19 pandemic have followed a cyclical pattern tied to public health priorities. The Administration for Strategic Preparedness and Response (ASPR) – which manages the Strategic National Stockpile – went from approximately $4.5 billion
In FY 2021, there were $1.35 billion in purchases of medical supplies from diverse small businesses. This reflects a significant federal strategic commitment to provide equitable access to purchasing and contracting opportunities for diverse businesses. Supplier diversity is an important goal for both the public and the private sectors. It promotes innovation, identifies new sources of talent and rewards experience.
The COVID-19 pandemic proved that the public and private sectors have complementary roles to play in supply chain operations. The private sector has expertise in the manufacture and distribution of medical products across the entire continuum of care. The public sector has greater resources and access to information to respond effectively to a pandemic. Private companies and government agencies must work together to ensure the seamless functioning of the medical supply chain.



Editor’s note: COVID-19 might not be ending, but the Public Health Emergency is. And the impact on your physician office customers may be farreaching. Last month, Repertoire looked at potential implications on telehealth/digital health and the distribution and provision of COVID19 vaccines. This month we look at the implications of potential Medicaid cuts and changes in enforcement of the physician-self-referral Stark Law..
The federal Public Health Emergency (PHE) for COVID-19 expired this spring. “We are in a better place in our response than we were three years ago, and we can transition away from the emergency phase,” declared the Department of Health and Human Services in February. Among the changes expected to affect physician practices are:
ʯ Medicaid eligibility: The Medicaid Continuous Enrollment Provision will cease, which could lead to loss of Medicaid and Children’s Health Insurance Program (CHIP) benefits for many. In addition, Emergency Allotments for the Supplemental Nutrition Assistance Program (SNAP) will stop.
ʯ Stark Law: When the PHE ends, blanket waivers of certain provisions of the physician self-referral Stark Law will end.

Providers fear the end of the Public Health Emergency (PHE) will mean the loss of Medicaid coverage for millions of people. Through its “continuous enrollment provision,” the federal government during the PHE required state Medicaid agencies to provide coverage even if an individual’s eligibility changed. (Before the PHE, individuals could be cut from the program for failure to report a change in family status or income.) Consequently, enrollment for Medicaid and the Children’s Health Insurance Program (CHIP) increased by 20.2 million people from enrollment in February 2020, the Kaiser Family Foundation found.
Expiration of the continuous enrollment provision means that 17.4% of Medicaid and CHIP enrollees – approximately 15 million individuals – will probably lose Medicaid coverage, according to the Assistant Secretary for Planning and Evaluation of the U.S. Department
of Health and Human Services. Children and young adults will be impacted disproportionately, with 5.3 million children and 4.7 million adults ages 18-34 predicted to lose Medicaid/CHIP coverage. Nearly one-third of those predicted to lose coverage are Latino (4.6 million) and 15% (2.2 million) are Black.
Certain states may be hit particularly hard. Nevada’s enrollment in Medicaid and CHIP rose 47% during the pandemic, according to Kaiser Health News. Many signed up toward the start of the pandemic, when the state’s unemployment rate spiked to nearly 30%.
Approximately 25% of Illinois citizens are enrolled in Medicaid under Illinois’ current rules, says Rodney S. Alford, M.D., presidentelect of the Illinois State Medical Society. “The continuous coverage provision has provided muchneeded stability to patients who rely on the program to get healthcare services and has helped ensure that physicians who accept Medicaid patients can trust that their enrollment status is current. Illinois State Medical Society members are wary of the unavoidable disruption that will be caused when the redetermination process is resumed after more than three years of continuous eligibility.”
The American College of Physicians supports additional options to prevent coverage gaps, including creating the option for Exchanges to adjust special enrollment periods for people who have Medicaid and Children’s Health Insurance Plan coverage,
says Shari Erickson, chief advocacy officer and senior vice president of governmental affairs and public policy. “We also have been urging CMS to encourage state Medicaid agencies to engage with Medicaidparticipating physicians, particularly practices with an above-average share of Medicaid-enrolled patients, to help spread awareness of the post-Public Health Emergency coverage transition.” ACP also supports enabling states to extend postpartum Medicaid coverage for a full year.
People enrolled in the Supplemental Nutrition Assistance Program (SNAP) are already feeling the impact of the end of the PHE. The program provides nutrition benefits to supplement the food budgets of needy families. During the PHE, the federal government issued “Emergency Allotments” of $95/month or more to households getting SNAP benefits. But effective March 1, regular SNAP rules were reinstated. This could ultimately affect more than 41 million Americans, according to Axios.
“The American College of Physicians has called for SNAP benefit levels to be increased and the benefit calculation formula regularly adjusted to better reflect the rising costs of nutrient-dense food and other competing expenses,” says Erickson. Many studies have found that SNAP significantly reduced food insecurity for participants, improved health outcomes, reduced healthcare expenditures, lowered nursing home and hospital admission rates, and lowered cost-related medication nonadherence compared with nonbeneficiaries, she says.
The physician self-referral law, also known as the “Stark Law,” does two
things: 1) It generally prohibits a physician from making referrals for certain designated health services payable by Medicare to an entity with which he or she (or an immediate family member) has a financial relationship; and 2) it prohibits the entity from filing claims with Medicare for any improperly referred designated health services. On March 30, 2020, CMS issued blanket waivers of certain provisions of
the law so long as they were related to the COVID-19 emergency.
When the COVID-19 PHE ends, those waivers will terminate, and physicians and entities must immediately comply with all provisions of the Stark Law. That will entail some recordkeeping on their part.
“Clinicians who took advantage of the blanket waivers must make available to CMS, upon request, records relating to the use of the
waivers,” says Shari Erickson. “This means that clinicians should be maintaining separate documentation for their arrangements that justifies the purpose and scope of the arrangement. From a clinician standpoint, it can be burdensome to review all arrangements entered under the Stark Law waiver. It is also unsettling that there is uncertainty as to whether CMS will audit and ask for proof of compliant documentation under the waiver. This will distract physicians’ focus from caring for what is most important – the patient.”

As the government returns to a stricter approach to enforcing Stark, medical practices may experience some backlash from their patients. By law, providers are required to attempt to collect Medicare deductibles and co-insurance amounts from their patients, says Kelly Ladd, CEO, Piedmont Internal Medicine, Atlanta. Failure to do so could amount to enticement, a violation of Stark. During the pandemic, practices slowed down their collection efforts with little or no interference

When the COVID-19 PHE ends, physicians and entities must immediately comply with all provisions of the Stark Law.Claire Ernst Kelly Ladd
from CMS. But last July, CMS in a memo required physician practices to resume vigorous collection efforts. Piedmont complied, “but patients have been complaining because they had not received a bill before this past summer,” says Ladd.
Physician practices have a few other issues to address as the PHE ends, according to those with whom Repertoire spoke. They include:
ʯ Notification of shortages of critical devices.
ʯ Issues surrounding physician prescribing of controlled substances.

ʯ Staffing issues.
When the PHE ends, the U.S. Food and Drug Administration’s ability to detect early shortages of critical devices related to COVID-19 could be limited, says HHS. During the PHE, manufacturers of certain devices related to the diagnosis and treatment of COVID-19 were required to notify the FDA of manufacturing discontinuances or interruptions. That requirement could end, though the FDA at press time was seeking congressional authorization to extend it.
Throughout the PHE, the government waived provisions of the 2009 Ryan Haight Act, which requires a practitioner to have conducted at least one in-person medical evaluation of a patient before issuing a prescription for a controlled substance.
“The American Academy of Family Physicians has long urged Congress and the administration to remove barriers for physicians prescribing medication for opioid use disorder, and applauded SAMHSA
[the Substance Abuse and Mental Health Services Administration of HHS] and DEA [Drug Enforcement Agency] for temporarily waiving certain restrictions during the PHE,” says AAFP President Tochi Iroku-Malize, M.D.. At press time, AAFP was preparing comments on proposed rules regarding permanent telehealth flexibilities after the PHE ends. Those rules would create new limited options for telemedicine prescribing of controlled substances without a prior in-person exam.
“There is a lot of concern among MGMA members who started treating patients during the pandemic,” says Claire Ernst, director of government affairs, Medical Group Management Association. “Now they are back to in-person visits. The proposed rules didn’t go as far as we wanted. There are still a lot of roadblocks for people who need those medications and for prescribers.”
Physician offices and healthcare in general throughout the country are still
facing staffing shortages among physicians, mid-level providers RNs, medical assistants and front office and billing personnel says Ladd. “It has been very difficult to recruit, hire, and retain employees post-COVID shutdown.” Those issues are expected to continue after the PHE ends.
One question about staffing involves the supervision of residents. “Family physicians have emphasized that COVID flexibilities impacting the supervision of resident physicians have improved beneficiary access and medical training, particularly the expansion of the primary care exception,” says Dr. Iroku-Malize. During the PHE, CMS expanded the codes that were billable under the primary care exception, meaning that residents could provide more services without the presence of a supervising physician during the visit if the supervising physician was overseeing the care and discussing it before and after visits. AAFP is advocating for the permanent expansion of the Medicare primary care exception, she says.
Nursing shortages, already an issue pre-COVID, were exacerbated by the COVID-19 pandemic. Throughout the healthcare industry, hospitals, outpatient centers, and clinics have tirelessly sought qualified candidates to fill open nursing positions.
The U.S. Department of Labor predicts that more than 275,000 nurses are needed from 2020 to 2030, and that employment opportunities for nurses will grow at 9%, faster than all other occupations from 2016 through 2026.
The pandemic heightened staffing shortages throughout the healthcare industry. Already low on staff, healthcare industry employees worked long hours in stressful, unprecedented conditions.

Nurses, already in a fast-paced and high-demand career field, have faced a variety of new stressors because of the pandemic. Nationally, nurses are navigating increased patient volume, longer hours, critically ill patients with COVID-19, and emotional trauma and distress. Other factors contributing to the shortage include an aging population, an increase in early retirement, high turnover, burnout, exhaustion, and a lack of resources in nursing schools, according to the American Nurses Foundation.
In a study on the shortage from the American Nurses Foundation, 57% of those surveyed nurses said they felt “exhausted” in the past two weeks, and 43% said they felt “burnt out.” Only 23% said they felt “motivated and supported” in the workplace.
Many experienced nurses decided to leave the field during the height of the pandemic due to stress and burnout. Many more are leaving employers for healthcare agency positions, or different careers entirely, with the hope of finding higher pay and less stressful work environments.
National shortages have led to delays in patient treatment, overcrowding of emergency rooms, and
decreased patient well-being. Fewer nurses mean fewer staff must care for more patients. “Nursing shortages lead to errors, higher morbidity, and mortality rates. In hospitals with high patient-to-nurse ratios, patients experienced higher mortality and failure-to-rescue rates than facilities with lower patient-to-nurse ratios,” according to The National Library of Medicine.
Nurses are increasingly seeking support and resources within the workplace to cope with the demands of the profession. According to the American Medical Association, thoughtful, deliberate attention is needed “to ensure there are enough nurses available to provide the expert care patients need.”
So, what has been done nationally and state-wide to retain nurses in the healthcare industry?
The national and state response to the nursing shortage focuses primarily on workplace support, legislation, and improving nursing education programs.
Nurses are advocating for better working conditions, including higher staff-to-patient ratios, mental health resources and workplace support. According to the National Academy of Medicine’s recommendations for federal government action, “nursing organizations should initiate the implementation of structures, systems, and evidence-based interventions to promote nurses’ health and well-being.”
Healthcare organizations have implemented strategies such as recruiting travel nurses, increasing wages and bonuses, offering mental health and well-being support, and adapting staff models to address nurse burnout.
According to an American Nurses Foundation survey, 44% of respondents said their organization recruited travel nurses while 20% said they experienced increased access to mental health and well-being support services through their workplace.
Some states have considered changing healthcare practitioners’ scope of practice to address the shortage of providers. According to a Penn Live report, two Pennsylvania state senators in late January introduced a bill that would give full independence to nurse practitioners. In Pennsylvania, nurses work under the supervision of physicians. Yet many other states give much more independence to nurse practitioners, enabling them to fill roles such as owning and operating their own practice and making house calls, the report said.
Also, according to the American Academy of Physician’s Associates, a bill proposed in Colorado to the Colorado Senate Health and Human Services Committee was passed in early March that would remove the requirement for PAs to be supervised by a physician, the report said. The expansion of authority in Pennsylvania and Colorado would serve as a solution to healthcare industry staffing issues by allowing already employed professionals to issue care.
Nationally, Congress introduced the “Stop Nurse Shortages Act, H.R. 9200” that would authorize grant funding in support of nursing schools.
The funding would be allocated for nursing education programs to “create and expand accelerated nursing degree programs, hire and retain faculty, and offer financial assistance to students,” according to the American Organization for Nursing Leadership. Funding allocated for educational programs would provide support to nursing schools, allow nursing students to fast-track their education and begin their careers earlier, and encourage more students to pursue education by easing the burden of tuition.
Nursing education schools have worked to address the nursing shortage by partnering with local hospitals. The goal of these partnerships is to increase accessibility of education and participation in nursing programs.
Oklahoma City University and SSM Health St. Anthony’s in Oklahoma have developed a hospital-university partnership that provides students scholarship opportunities. The financial assistance aims to encourage qualified graduates to enter positions in the healthcare industry.
Cleveland Clinic introduced a similar hospital education program, the ASPIRE Nurse Scholars Program, which reaches out to high school juniors and seniors who are interested in a career in nursing.
Education programs such as these, and many more across the nation, foster an early interest in nursing and encourage recent graduates to enter and remain in the field.
The national and state response to the nursing shortage focuses primarily on workplace support, legislation, and improving nursing education programs.
Self-rooming versus traditional escorted rooming has become commonplace after the pandemic in health systems across the nation.
When visiting a physician’s office for an appointment, patients typically arrive, check in at the front desk, and then wait until a clinician or nurse calls them back from the waiting room to be seen by the doctor.

The traditional rooming system is what most patients experience when visiting a clinician’s office. However, during the COVID-19 pandemic, many clinical offices began to implement self-rooming into their practice model.
Self-rooming is when a patient checks in and then proceeds directly
to an exam room, bypassing the traditional waiting room experience of being led to an exam room by a staff member.
In October through December of 2020, a survey conducted by the Annals of Family Medicine on selfrooming preferences found that 86% of patients preferred self-rooming
to traditional rooming. Over onehalf of the staff surveyed also preferred self-rooming, according to the Annals of Family Medicine survey.
“Few patients felt less welcomed (10.6%), less cared about (6.8%), more isolated (15.6%), more lost/ confused (7.6%), or more frustrated (3.2%) with self-rooming compared
to escorted rooming.” Patients, especially those ages 65 and older and those in family medicine clinics preferred self-rooming, according to the Annals of Family Medicine.
Self-rooming decreases wait times for patients, increases patient satisfaction, and increases staff efficiency. Without the need for a staff member to call out a patient’s name and escort them to their room each time they come in for healthcare, more time can be spent by staff on other tasks to increase the overall efficiency of a doctor’s office.

“Our customers who use the self-rooming model typically have high patient satisfaction scores,” says Jeanne Kraimer, a product marketing manager for Midmark RTLS Solutions, Inc. The company’s Patient Flow Optimization solution uses realtime locating system (RTLS) technology to help facilitate clinic workflow. “Especially when paired with a collaborative care model, where various services such as phlebotomy are provided in the exam room, the efficiency gains not only mean shorter visits for the patient, it may also allow the clinic to see more patients or add providers to their schedule.”
During the COVID-19 pandemic, traditional waiting rooms became unsafe due to the potential for virus transmission. Health systems responded to the threat of COVID19 spread in waiting rooms by implementing self-rooming inside buildings with traditional clinical layouts. Self-rooming during the height of the pandemic promoted increased social distancing and aimed to avoid virus transmission in waiting rooms.
“While recent events certainly increased interest in this model, we’ve been helping clinics with selfrooming since 2010,” says Kraimer. “Our customers who use this model had a head start in keeping their patients safer during the pandemic.”
Ideally, the layout of a health center would be redesigned to accommodate for self-rooming. Features such as hallways with fewer intersections and dual-access rooms could be implemented in the structure of a clinicians’ office to increase system effectiveness.
Many health systems overcame self-rooming technology concerns during the pandemic and rapidly
redesigned the rooming process with little need for technology. The result was an increased use of the self-rooming system. Self-rooming has continued to be implemented as a post-pandemic feature across health systems.
“Although it isn’t necessary to implement self-rooming, having visibility into your entire clinic from a computer screen with RTLS technology can make the process easier,” Kraimer explains. “Being able to see which exam rooms are clean and available for patients, where each patient is located, which caregivers have seen them and who hasn’t seen them yet can make the daily management of self-rooming workflows quite seamless.”
Many health systems overcame self-rooming technology concerns during the pandemic and rapidly redesigned the rooming process with little need for technology.
















Medical sales reps are always looking for an edge. Even the smallest detail could mean the difference between a successful client encounter or a missed opportunity. What one feature or benefit of a well-established product could you provide that would convince a physician office of its value? What new CPT code out there could make a difference for reimbursement? What new products from medical device manufacturers are coming out that promise to change the game in the med/surg market?
Research suggests that online learning has been shown to increase retention of information, and take less time, meaning the changes coronavirus have caused might be here to stay

The following are 3 reasons that reps should consider investing their time and energy in online training.
A fine-tuned, industry tailored training site can give you the information you need in a digestible format. Training modules can provide all the necessary features and benefits of the product, why it is used, who to target, CPT codes and reimbursement, promotions, and links directly to the manufacturer.
Distributor sales reps are incredibly busy – visiting clients, taking calls, working with internal team members and vendor reps. Online training allows the rep to schedule to learn about products when it fits their schedule, and even go back to items when they need to.
According to recent research, in 2022, 83% of 515 surveyed learning leaders said the shift to a hybrid environment forced companies to
rethink how they handle corporate learning. Now instead of teaching in a room full of people, online learning has become a necessity. And that’s why 59% of the surveyed learning leaders believe traditional in-person learning will end.
Indeed, online training can get you up to speed, and even ahead of the pack, if you’re willing to invest the time to make each client encounter great. In a recent survey, 87% of distribution reps said they will not bring up a product if they haven’t trained on it. In the same survey distribution reps said they give on average 12-15 sales presentations following online training.
Fortunately, you don’t have to spend the time looking for those keys to success. SMM delivers training in multiple ways:
ʯ 2-Minute Drills, which are short videos that teach the rep how to start a conversation around a product.
ʯ EOL training modules, which are more in depth 8-12 minute trainings on a product or service.
Rather than having to jump in and out of a myriad of websites, trying to remember which username and password goes to what platform, an effective training platform allows reps access to many different products they talk with clients about on a daily basis, across countless product categories that are used in physician offices, long-term care facilities, ambulatory surgery centers, hospitals, health systems and IDNs.
ʯ Live videos with manufacturers going over their products and services.
ʯ Podcasts on topics manufacturers want distribution reps to know as they call on their accounts.
Share Moving Media is a market leader in designing programs to help train distribution, manufacturers, or end-users on market trends or products. For more information, visit sharemovingmedia.com/training.
Alzheimer’s is a prevalent disease affecting brain health and cognitive processing.
Purple is the official color of the Alzheimer’s awareness movement, and June marks the month to wear purple in support of brain health awareness related to the disease. Alzheimer’s Awareness Month sheds light on the symptoms and treatment options for individuals that are afflicted.
Alzheimer’s is the most common form of dementia, accounting for 60% to 80% of cases, according to the Alzheimer’s Association. Alzheimer’s causes memory and cognitive ability loss and is experienced primarily by individuals aged 65 and older.
Symptoms of Alzheimer’s disease often worsen over time. Alzheimer’s is a progressive form of dementia and can begin asymptomatic and advance into mild cognitive impairment, mild dementia, moderate dementia, to severe dementia. At each stage, an individual experiences less independence in carrying out daily life.
The most recognized early symptom of Alzheimer’s is difficulty remembering new information, as the disease impacts the part of the brain that controls the ability to learn. Severe symptoms include disorientation, mood and behavior changes, confusion, difficulty speaking, swallowing, and walking.
Worldwide effort has been made for research into therapies and medications aimed at treating individuals with Alzheimer’s disease.
There is currently no cure for Alzheimer’s, but two treatments are available that reduce functional and cognitive decline for patients. The
medications Lecanemab and Aducanumab are approved by the U.S. Food and Drug Administration (FDA), and address the underlying biological causes of Alzheimer’s, according to the Alzheimer’s Association.

New research conducted by the Mayo Clinic and 13 other institutions around the country are also searching for possible treatments and therapies through a scientific study of Alzheimer’s from a multiethnic perspective.
“We know that Alzheimer’s disease afflicts patients from African American backgrounds at a rate twice as high as that in white populations. For Latino Americans, the risk is one-and-a-half times greater than that in white populations,” said Dr. Nilüfer Ertekin-Taner, professor of neuroscience and neurology and physicians-assistant at Mayo Clinic. “These populations have traditionally
been understudied for Alzheimer’s disease, leading to a major knowledge gap. When we try to understand the molecular underpinnings, the disease fingerprints, we need to understand it for all of us to be able to identify biomarkers and therapies.”
The Mayo Clinic Alzheimer’s research aims to analyze blood and donated brain tissue samples from patients with varying ethnic backgrounds. The data collected will allow researchers to learn more about the molecular side of the disease and to begin developing treatments and therapies.
On June 21, thousands come together to “fight the darkness of Alzheimer’s,” according to the Alzheimer’s Association. The day June 21 is the summer solstice and longest day of the year and is symbolic for coming out of the darkness associated with the disease.
The worldwide gesture of symbolism is also a day of action that allows communities to show their support by signing up for an activity and turning it into a fundraiser. The Alzheimer’s Association encourages individuals to show support in the month of June by sharing their stories and experiences with Alzheimer’s, volunteering with the association, becoming an advocate for national policy changes, posting disease information to social media, and donating in support of research efforts.
Health insurers acknowledge the need for providing more mental health resources.
By Jenna HughesStress, depression, anxiety, and other mental illnesses all negatively impact an individual’s overall health. Indeed, mental illness is one of the most common health conditions in the United States. According to the Centers for Disease Control and Prevention (CDC), more than 50% of people will be diagnosed with a mental illness or disorder at some point during their lifetime. These conditions also lead to an increased risk of physical health issues such as diabetes, heart disease, and stroke.
Mental health conditions can make it difficult for an individual to maintain balance in everyday life. Several factors can contribute to a mental illness diagnosis including trauma, abuse, or chronic conditions. Mental health can change over time depending on factors such as
increased stress, biological characteristics, and lifestyle.
Looking after one’s mental health encompasses managing active life stressors and taking action to maintain future well-being. Several healthcare insurance companies recently announced more steps they are taking

to integrate behavioral health coverage into their services.
Stressors due to the COVID-19 pandemic have led more young adults, healthcare workers, and Americans in general to seek mental health resources. “The vast majority of Americans are struggling with their mental health. With the irreversibly accelerating need for mental health care comes a decrease in the stigma associated with getting care,” said Dr. Doug Nemecek, Chief Behavioral Health Officer of Evernorth
Health Services, the pharmacy, care, and benefits solution division of The Cigna Group.
Mental health services are costly for the patient and for the nation. Untreated behavioral health conditions increase the utilization and cost of care for physical conditions, costing billions of dollars annually. Depression alone is also responsible for $44 billion lost in productivity, according to Dr. Nemecek and the National Alliance on Mental Illness. There are significant implications to the economy if individuals do not get the behavioral health services they need.
Many insurers have expanded mental health resources with the goal of providing affordable and adequate mental health treatment options.
“UnitedHealthcare recognizes the intrinsic link between behavioral health and physical health and is dedicated to integrating behavioral health into medical care,” said Dr. Rhonda Randall, Chief Medical Officer, UnitedHealthcare. “With 1 in 5 Americans experiencing a mental illness within a given year, it’s important for us to offer a range of support programs for those who may need it, with the goal of helping to address access and affordability challenges.”
In 2023, UnitedHealthcare has continued to expand mental health resources to include online self-help tools, in-person and virtual clinician visits, a virtual behavioral coaching program, and 1:1 video conferencing or messaging with trained coaches. Employers can now purchase these resources to include in employee’s healthcare coverage packages.
Evernorth Health Services
(The Cigna Group) has also incorporated various initiatives to increase
mental health resources for patients. Through Cigna insurance, patients have access to webinars and seminars discussing behavioral awareness for the individual and for families. They also offer information on mental health for patients through blogs, incentive programs, health coaching, and a behavioral health and employee assistance program that connects employees to healthcare providers.
To help meet the growing demand for care, Evernorth Health Services has doubled the size of its provider network over the past five years. They have more than 315,000 behavioral health providers, and continue to grow their network aggressively. “We’ve also very intentionally grown our network for providers specializing in treatment of adolescents by 34% and those who specialize in ethnic issues by 20%,” said Dr. Nemecek.
According to Dr. Don Tavakoli, National Medical Director for Behavioral Health, UnitedHealthcare, “Primary care physicians (PCPs) are often the first responders when it comes to supporting all aspects of a person’s health. PCPs are the quarterback of the personal healthcare team, so it is important for people to keep up to date with their annual visits and reach out to them whenever they have mental health care questions or concerns.”
Health insurers who spoke with Repertoire recognize there are dynamic needs for mental health access in an ever-changing society.
UnitedHealthcare’s behavioral health programs aim to “Bring together technology, clinical expertise, and strategic collaborations to help ensure
Often, patients are referred to mental health services by their primary care physician. A visit to the physician’s office typically includes a questionnaire about recent changes in mental health. If a patient indicates a change in their mental health and well-being during an appointment, a primary care physician can treat disorders such as depression, anxiety, and emotional distress related to grief. They are also able to refer patients to further services if needed. Insurance can help cover the cost of these services for patients.
more people have access to quality, supportive behavioral healthcare services,” according to Dr. Tavakoli.
“Looking ahead, we need to focus on the coordination of care across medical, pharmacy, and behavioral health benefits in support of a whole-person health approach. This approach includes measuring patients before, during, and after their mental health care journey as well as matching individuals with providers who deliver the right level of care for their needs,” according to Dr. Nemecek.
If a patient indicates a change in their mental health and well-being during an appointment, a primary care physician can treat disorders such as depression, anxiety, and emotional distress related to grief.
Jake Pehrson knows what it takes to run a business.

As VP of operations at Premier Medical Distribution, Jake Pehrson often finds himself focused on strategic planning around the company’s finances, sales, regulatory compliance and more. He has also been known to pull orders in the warehouse and answer customers’ service calls. “As a small company, each of us must pitch in to help wherever necessary,” he says. In fact, this hands-on approach has helped him and his team navigate the challenges of the COVID pandemic, as well as ongoing challenges inherent in the continuously changing landscape of healthcare manufacturing and distribution, as they continue to build a robust and resilient business.
Indeed, Pehrson knows a thing or two about what it takes to run a business. His entrepreneurial roots can be traced back to a Commodore 128 that his parents gifted his family the Christmas of 1986. “Growing up in the 1980s, I was lucky enough to experience the early days of personal computing,” he recalls. “As a child, I had the opportunity to take part in the rapid growth of this exciting technological era.” He was also influenced by his father, whose keen entrepreneurial instincts led him to invest in the right technological tools to successfully navigate his businesses. “All of this afforded me a head start in computer and business literacy over many of my peers.”
After receiving a modem for his birthday the following year, Pehrson began assisting friends and neighbors with computer programming, maintenance and repair. “By the time I reached high school, I was able to leverage my skills to earn additional income by building computers and working at Egghead Software,” he says. “One could say that I had officially become a computer nerd! Then, during my senior year, I met another student, Marc, a likeminded individual with a passion for technology. Together, we founded a company that eventually grew into Design Technologies.”
Small but mighty, Design Technologies proved to be successful. The company comprised two distinct divisions: computer parts distribution and computer and network consulting, Pehrson explains. “As a small company catering to the local Salt Lake City market, we recognized the scarcity of companies offering computer and network parts and solutions at the time, and we sought
to address this gap. Given the size of the company, I assumed multiple responsibilities, with a primary focus on parts acquisition, accounting and consulting.”
While there are perks to selfemployment, it also comes with a number of challenges, notes Pehrson, one of the biggest being obtaining affordable health insurance. “I found it difficult to find health insurance that was both comprehensive
and affordable,” he says. “This issue became more important when I got engaged to my wife, Pepper. We looked forward to starting a family one day, and we knew health insurance was essential.” He happened to be consulting for Omnicare at the time and the company was ready to hire a full-time IT manager. “Omnicare provided an extensive benefits package, including healthcare, which ultimately led me to accept a position with the company.”
After about a decade working with Omnicare’s local medical supply division, the company decided to outsource his department, leaving Pehrson to choose between assuming a position in another department (which involved more travel time than he would have liked) or looking for a new job elsewhere. He had opted to look elsewhere when, as luck would have it, a managerial position at Omnicare became available. “I decided to remain with Omnicare in the managerial role,” he says. “Years later, in 2011, a small group of employees purchased Omnicare’s medical supply business and established Premier Medical Distribution. I was appointed the general manager at Premier.”
As general manager, Pehrson oversaw the day-to-day operations, ensuring they were carried out with efficiency, effectiveness and adherence to all applicable regulations and standards. “While wearing multiple hats as GM of a rapidly expanding company, I primarily dedicated my time to supporting our staff in delivering exceptional experiences for our customers,” he says.
In 2015, he was promoted to his current role, vice president of operations, and the company hired a new general manager to manage day-today operations. “This allowed me to
focus on working closely with the owners’ group to develop a comprehensive long-term strategic plan for the company. Together, we addressed a wide range of critical areas, including finance, sales and marketing, customer service, regulatory compliance and identifying new business opportunities. By taking a collaborative approach to strategic planning, we developed a clear roadmap for the future of the company while positioning ourselves for sustained growth and success.”
Working for a healthcare supplier, Pehrson and his team have grown to appreciate the industry’s continuously changing landscape. “Over the years, technology has played a critical role in providing solutions to our customers, helping them overcome challenges and streamlining the process of ordering supplies and equipment,” he says. “A decade ago, receiving orders via fax or phone was common; today, the majority of orders are transmitted
Pehrson quickly learned to navigate not only the opportunities, but a number of industry challenges as well.
“The pandemic had a profound impact on everyone,” he recalls. “However, as a small business, we found ourselves in a unique position to adapt quickly and provide essential PPE, vaccine testing and other medical supplies to a broad range of companies. We worked tirelessly to procure and manufacture products as quickly as possible, which required us to establish new business relationships and seek financial backing to support our growth.
“We had to make critical decisions in a matter of hours or days, rather than weeks or months, in order to respond to the rapidly changing situation,” he continues. “Although the rapid growth was difficult, it was also highly rewarding. While we continue to deal with the ongoing effects of the pandemic and how it has affected the global supply chain, we are gradually returning to normal business operations.”
through various technological channels, such as EDI, websites, APIs and others. Our customers expect us to integrate seamlessly with their systems to provide real-time inventory, track information and ensure instant access to invoices, past orders and other relevant data. As a result, we have invested significantly in technology – more so over the past three years than any other period in our company’s history – and the implementation has taken up a significant portion of my time.
“Although we may not deal directly with the same regulatory and reimbursement issues as our customers, we are significantly impacted by these issues due to our close relationship with them,” he points out. “If they face reimbursement issues, it may affect their ability to settle their bills; if they require better outcomes, we must provide products that meet their needs. Our primary focus is on caring for those who care.”
‘We had to make critical decisions in a matter of hours or days, rather than weeks or months.’
Jake Pehrson looks seaward and forward
For as long as he can remember, Jake Pehrson, vice president of operations at Premier Medical Distribution, has been drawn to the water. “Growing up, I often brought home snakes, frogs and fish from the nearby canal,” he recalls. “I was always on the hunt for something new.” And, though his home state, Utah, had little to offer in the way of ocean life, one of his favorite childhood vacation memories was finding a starfish on a family trip to Oregon. His disappointment over being told he couldn’t bring his discovery home didn’t temper his enthusiasm. “Several years later, I stumbled on an ad in the back of Boys Life Magazine for seahorses, starfish, hermit crabs and pipefish, and I knew I had to have them!” He saved money working odd jobs around the house and in his neighborhood, and eventually sent away for the sea creatures. “Weeks later, on a cold winter day, the exotic animals arrived on my doorstep!”
That was just the beginning, he recalls. “Over the years, my love of marine life only intensified. I became a certified scuba diver and explored the depths of the ocean, marveling at the incredible beauty of the underwater world. My passion for marine life has become an integral part of who I am, and I remain grateful for the experiences that have shaped my life’s journey.”
After marrying his wife, Pepper, he set up a saltwater aquarium in their first condo. “I was driven by my passion to learn more about sea life and coral, but at that time, the information available in books and on the internet was limited and resources were scarce,” he says. “Looking to enhance my knowledge on


the subject, I decided to join the local saltwater club.” As he became more aware that the world’s coral reefs were in peril, he sought an opportunity to focus on the commercial propagation and growth of corals through a new venture he started, Coral Planet. “In partnership with scientists and fellow hobbyists, we were able to develop techniques to reduce or eliminate the need to import corals for the aquarium trade. Our efforts saw the sale of these corals to public and private aquariums, pet stores and even medical research facilities for cancer treatments. Coral Planet remains a consulting business, committed to reef sustainability.”
During this time, Pehrson was approached by another club member, Professor Adam Blundell, to serve as the club’s vice president. “During our tenure, Professor Blundell and I implemented significant reforms to promote education on coral propagation, as well as coral and fish nutrition. We shared our discoveries through meetings and nationwide outreach via the internet and tradeshows. Although my involvement with the club is now limited to an advisory capacity, I continue to host their website and provide counsel when needed.”
When he’s not looking seaward, Pehrson enjoys spending time on his ranch – the Utah Bee Ranch, that is, which he started in 2014. “Beekeeping is a passion that holds a special place in my heart,” he says. “When I was 8 years old, I accompanied my grandfather on some errands one Saturday, and we stumbled upon a beekeeping store. The moment I went inside, I was captivated by the idea of keeping bees. After many years, I finally decided to fulfill my childhood dream and become a beekeeper.
“Today, I am known as Jake the Bee Guy. You might find me on a spring Saturday morning gathering wayward
swarms in the act of saving the bees. Although Utah Bee Ranch is more of a hobby than a business, taking care of these incredible creatures brings me great joy.”



Pehrson’s success, professionally and hobby wise, is grounded in his ability to communicate and work with others – skills he largely attributes to his longtime involvement in the Boy Scouts of America. “I actively participated in Cub and Boy Scouts during my childhood, which provided me with numerous valuable life experiences,” he says. “The BSA programs offered me opportunities to fulfill merit badge requirements, camp in the great outdoors, engage in exciting activities such as rappelling and river rafting, and acquire new skills. These experiences enriched me as a person, giving me a unique perspective on life that many never have the chance to experience.
“Although I had never intended to become a leader in the Boy Scouts, as I grew into adulthood, I felt a sense of duty to give back and provide young scouts with the same joyful experiences I had. My long-term involvement in the organization has significantly contributed to my personal and professional growth. As a leader in the Boy Scouts, I have honed my skills in leadership, communication and mentoring. I have acquired valuable life skills, such as problem-solving, critical thinking and adaptability, which have enabled me to work effectively with teams and navigate complex situations in the workplace. The sense of responsibility and commitment instilled in me through scouting has also translated to my personal life, where I apply the same principles in my relationships and other areas.”
Cardinal Health Canada announced plans to open a new distribution center in the Greater Toronto Area, expanding its distribution footprint to nine strategic locations to better meet the medical and surgical product demands of the Canadian healthcare system.
The 163,000 square-foot facility will integrate state-of-the-art robotic technologies to deliver operational efficiencies as well as enhanced employee, customer and supplier experiences. Working with autonomous mobile robots means that each employee stays within a specific zone in the facility and becomes an expert on the products located in that area, reducing physical labor while improving productivity. For customers, the
AMR implementation will increase picking and packing accuracy.
The new distribution center is estimated to be fully operational in late 2023 to early 2024. This will bolster Cardinal Health Canada’s distribution footprint in Ontario to 541,000 square feet and raise its national footprint to 1,120,000 square feet.
This is the third new distribution center for Cardinal Health’s Medical Segment to be announced within North America since April 2023.
Henry Schein announced the acquisition of Regional Health Care Group, a medical products distribution company serving public- and
Zealand.
Since 1998, Henry Schein has served the Australian and New Zealand dental market, providing a wide range of dental products, equipment, and services to dental professionals. The addition of RHCG expands Henry Schein’s offering to medical practitioners in the region.
Henry Schein acquired RHCG, which had sales for the 12 months ended June 30, 2022, of $42 million, from Maurie and Bernard Stang, who wholly owned the company and retain a minority interest in Henry Schein’s ANZ dental business. Henry Schein expects the transaction to be neutral to 2023 diluted earnings per share when excluding amortization expenses and accretive thereafter. Financial terms were not disclosed.
G. Gilmer Minor III, Chairman Emeritus and former CEO of Owens & Minor, has died at the age of 82. He led Owens & Minor from 1981 to 2005, growing the business from a less than $300 million medical supply firm to a $4.82 billion organization.
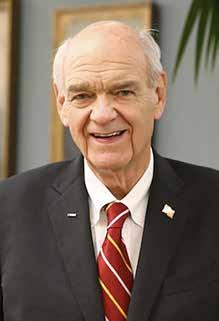
After his tenure as CEO, he worked as the non-executive chairman of the board until 2013. He worked at Owns & Minor for the entirety of his professional life, joining in 1963. Before becoming president in 1981 and CEO in 1984, he worked in sales, operations and management capacities
In a media release, Owens & Minor said, “Gil’s own words spoke volumes about who he was, and how much he cared about the success of the company his family founded, as well as his fellow teammates: ‘As proud as I am of our success, I am probably prouder of the way we have handled adversity and the strong fiber of the company that has held us together. And, most of all, I am proud to be part of a team that cares so much about each other, our customers and our suppliers, and always strives to do better.’”
As the number of outpatient clinics increase, instrument processing becomes a greater challenge for our customers. They may already understand the need for effective sterilization to reduce risk—but instrument processing is more than sterilization and it begins before they ever touch an instrument. Midmark instrument processing solutions were designed around CDC-recommended1 best practices to help make regulatory compliance to clinical standards as easy (and as automated) as possible.
Contact your Midmark Representative to start the conversation.
1 https://www.cdc.gov/infectioncontrol/guidelines/disinfection/sterilization/sterilizing-practices.html







© 2023 Midmark Corporation, Versailles, Ohio USA


revolutionized personal hand protection forever with the invention of the world’s first nitrile exam glove. Since that time, the integrated manufacturer has accomplished a “Legacy of Firsts” for health care providers:
SUPPLY CHAIN ASSURANCE. CHAIN OF CUSTODY. BORN AND BRED IN THE .
2022
Stood up two more high speed monorail lines now with 800M glove capacity annually
1990
Invented of the world’s first nitrile exam glove
First 510(k) for the world’s first nitrile exam glove
Patent for nitrile exam held for over a decade
Research, development, and production of nitrile exam gloves in the USA since 1990
1990
1995
2000
Inventor of the world’s first nitrile accelerator-free exam glove (low dermatitis potential)
2012
Invented ECO BEST TECHNOLOGY ®
Launched the world’s first biodegradable nitrile exam glove
2010
Additional 40,000 square foot expansion in 2022
2021
Stood up two high speed monorail lines adding 400M glove capacity annually
29 Chemotherapy Claims and Fentanyl Tested
2020
510(k) for the Fayette, AL production facility
2020
2004
Inventor of the world’s black nitrile elocstratic discharge glove
2018
Expanded Eco Best Technology ® in all exam gloves
2019
40,000 square foot expansion in Fayette, AL
BE THE FIRST TO BRING YOUR CUSTOMER A USA MADE EXAM GLOVE FROM A TRUSTED MANUFACTURER SINCE 1970.