

Times Have Changed
There are some well-worn phrases you just don’t hear much of anymore when it comes to the physician office lab.


Times Have Changed
Owens & Minor Foundation, HOPE partner to support U.S. service members and military families.
Build the future of our profession by nominating a medical supply chain emerging leader.
Pediatricians
of
online media on children’s health. 50 Facing Healthcare Challenges
Supply chain leaders share how they are tackling industry issues with forward-thinking solutions. 52 Get the Picture
Diagnostic medical sonography plays a key role in better clinical outcomes for patients across a wide array of health conditions.
Henry Schein Medical helps healthcare professionals prepare young patients for back-to-school season with a wide range of medical product offerings.
Using Mentalism Techniques as a Sales Tactic
Basic principles from a high concept performance art that sales reps can tap into.
for supply chain?

By Way of Introduction
For 19 years I’ve had the privilege of getting to do the “behind-thescenes” work on Repertoire Magazine . When our longtime editor Mark Thill called to say he was closing out his last issue with the publication, it was a bittersweet moment for me. Mark has been an incredible example and mentor. Each issue I’ve gotten a chance to see how one of the best business editors around goes about his work: the way he interviews, the stories he thinks are important, and the dedication to his craft.
It’s hard to believe my first issue working on Repertoire was almost two decades, three kids and three 529s ago. My hair now is a little grayer and my steps a little more mindful due to a few weekend warrior mishaps, but my curiosity in all things med/surg has only increased after watching Mark cover the industry.
Now it’s my turn. I’m a little nervous for obvious reasons. Following Mark is a tall task. But I’m also excited, because it means reaching out to more Repertoire readers and industry veterans and asking for them to help us make sense of the changing landscape of med/surg distribution.
And boy is it changing. Like you, I’ve witnessed the chaotic nature of the pandemic, recessions, healthcare legislation and shifting consumer attitudes toward healthcare. I’ve been both incredibly frustrated at times with the challenges our industry continues to face, and incredibly grateful to the work our frontline caregivers have provided – as well as your focus and dedication to providing products and services to those caregivers.
Never was this more apparent than during the pandemic. The work that distributors and manufacturers put in amid chaotic conditions was nothing short of inspiring. I mean that. It was an honor to go to work (albeit behind the home office desk for a time) and tell the stories that we hoped would encourage, educate and embolden you.
That task holds true today. Although the bylines may be changing, our mission of providing you timely content won’t.
Here’s to a bright future for all of us.
Graham Garrison Editor
editorial staff
editor Graham Garrison ggarrison@sharemovingmedia.com
editor-in-chief, Dail-eNews Jenna Hughes jhughes@sharemovingmedia.com
content creator Pete Mercer pmercer@sharemovingmedia.com
art director Brent Cashman bcashman@sharemovingmedia.com
circulation Laura Gantert lgantert@sharemovingmedia.com
senior sales executive Amy Cochran acochran@sharemovingmedia.com (800) 536.5312 x5279
publisher Scott Adams sadams@sharemovingmedia.com (800) 536.5312 x5256
founder Brian Taylor btaylor@sharemovingmedia.com
Subscriptions
www.repertoiremag.com/subscribe or (800) 536-5312 x5259
Repertoire is published monthly by Share Moving Media 350 Town Center Ave, Ste 201 Suwanee, GA 30024-6914 Phone: (800) 536-5312, FAX: (770) 709-5432; e-mail: info@sharemovingmedia.com; www.sharemovingmedia.com
More breathing room this respirator y season
It’s back-to-school season, which means flu and strep are back in season, too. Be prepared for all your patient testing needs with advanced diagnostic solutions from QuidelOrtho.

Compact and versatile testing with proven lateral-flow technology and advanced fluorescence chemistry. Accurate and objective flu and strep results automatically reported in as few as three minutes.
Benchtop molecular diagnostics platform with capacity to run one to 12 tests at a time. Uses proprietary helicase-dependent amplification with fluorescence detection to make diagnosing flu and strep faster and easier.
Scan to learn more, or to order contact, your QuidelOrtho representative
American Medical Supplies & Equipment: An Independent, Family Business
By Pete Mercer
 Independent distributors are a critical piece in the overall puzzle of healthcare, streamlining the healthcare supply chain by linking manufacturers directly to providers. Equal parts flexible and scrappy, these organizations provide a much-needed service to ensure that healthcare organizations are equipped to care for their patients.
Repertoire Magazine recently spoke to Victor Amat, the president of American Medical Supplies & Equipment, about being an independent distributor, overcoming challenges, and the shifting market.
Where it started
Based in Miami, American Medical was founded in 1983 by Amat’s father and uncle. After working in the industry since 1965, they moved from Pennsylvania to Florida and decided to open their own company. They were working for Dade Medical at the time – after Dade closed its doors, they started American Medical. While his father and his uncle have since passed away, Amat (who joined the company in 1985) has loyally served as the president of American Medical since 2000.
American Medical serves primary care – physicians, clinics, Medicare Advantage HMO clinics, ancillary clinics. Amat said, “We serve the single-doc practitioner all the way up to a multifacility Medicare Advantage Clinic and everywhere in between.”

Amat is proud of American Medical’s mission to put the customer first. With every customer interaction, his team is constantly looking to solve the problems of the customer. He said, “We do all our own installations – I do not just sell equipment and drop it off at a facility. Right now, we’re working on a project with about 30 exam rooms, so we are doing all the installation and integrated systems. Everything is a white glove service when we deliver equipment and supplies.”
Building relationships with customers is only part of the equation: American Medical also works with a variety of manufacturers to ensure that only the best products are being sourced for their customers.
Amat and his team believe in loyalty. He said, “We try to be loyal to those manufacturers that are willing to work with us, and we try to stay loyal to IMCO manufacturers. We have been a member of IMCO since 1992, which has kept us competitive with the national players and the breadth of products and manufacturers that any member would have access to.”
Preparing for disasters
Like everyone else in the industry, American Medical had to find a way to come out the other side of the pandemic. In many ways, they are still working through the fallout of the pandemic with their customers.



• Volume measurement accuracy: ±7%
• No annual calibration required
• Automatic patient selection
• Pubic bone interference indicator

• Customizable profiles for adults, pediatrics, & neonate
• WiFi & HL7 included for EMR integration & data transfer
• Comprehensive array of parameters with ECG, SPO2 & NIBP with options for CO2 & 5AG


• Clinical training available from our staff sonographer
• Lightweight, portable, & handheld design with long battery life
• Quick interchangeable transducers including endocavity option
• Connects to iOS & Apple, with no subscription fees or additional cost to unlock reports & extra features
• Sedation monitor with Masimo or Nellcor SPO2
• Bed to Bed Remote patient view for up to 12 monitors
• Compact & ergonomic design with a 10-inch touchscreen
Training Included Free In-Person Demos From Your MTMC Rep Delivered Patient-Ready With All Standard Accessories Exceptional Service & Support For The Lifetime Of The Machine


Patient Monitor
Handheld Ultrasound
Patient Monitor
Bladder Scanner
Bladder Scanner
“I think the uncertainty of everything is keeping them up at night,” Amat said. “During the pandemic, we talked to a few of our customers about stockpiling, which some of them had the warehousing space to have some type of safety stock, the threeto-six-month supply of some of their PPE equipment in case this happens again.”
As for American Medical, current events are enough to keep Amat up at night. When he joined the company, 90% of the products that they sourced were American made. Now, that arrangement has flipped to where 80% of their products are now made overseas.
For a smaller and independent distributor, Amat said that their biggest pain point is “expenses that are beyond our control.”
With the rising cost of liability insurance, vehicle and truck insurance, and healthcare insurance, it’s sometimes overwhelming to try and stay afloat in today’s market. Regulatory enforcement has put his team in a spot where they are investing in technology and software to be compliant.
If all of that were not enough, American Medical is also based in Miami, which means that they must plan for hurricane season every year. “Our building has been hit by a hurricane twice. Hurricane Irma kind of took the roof off the building in 2005. For our disaster plan, we tarp the inside of our building so that if the roof is compromised, everything inside remains dry.”
American Medical’s servers have moved to the cloud, instead of hosting everything on site. This will allow them to resume operations much more quickly if their building is hit by another hurricane.


The advantages of being an independent distributor
For Amat and American Medical, operating in the independent distributor space gives them an opportunity to serve their customers on their own terms. The freedom to be able to make your own decisions in this industry is rare, and it allows Amat and his team to come up with creative solutions to complex problems.
“We can change company policy by sticking my head out of my office and letting people know what we’re doing now. There isn’t a lot of red tape or bureaucracy – the buck stops here. We can change what or how we do things on a dime,” Amat said.
That idea of independence is not about making reckless decisions but meeting the needs of the customers without that red tape that larger organizations usually have to navigate. “We are flexible to each customer’s needs.
Things that we do for one customer, we can change how we do them for another customer. There are customers that have certain requirements when you deliver products, and we have been flexible enough to have different delivery requirements for each customer. It’s what differentiates us from the nationals.”
Amat said ultimately it is the people of American Medical who have allowed the independent distributor to successfully navigate everything from hurricanes to pandemics, and market disruptions in between.
“I have people that have worked for me for close to 30 years and have people that are as young as we hired them four months ago, and everywhere in between,” he said. “If we treat people right and you lead them, they’ll stick around. I think everyone needs leadership at one point or another – it’s not always about dollars, it’s about how you treat people.”
STAND OUT


Healthcare is in crisis. Prices are soaring. Resources are being stretched and quality patient care cannot be compromised.
Partnering with Mölnlycke is a step toward better outcomes for you, your customers, and their bottom line.









Making Things Better in Healthcare
For First Quality’s Matt Meyer, teamwork is the key to creating value for distribution partners.
 Matt Meyer realized what his dream job was in college, after he landed a part-time job at a distribution center for a medical supply company. During his time working in the distribution center’s warehouse, he’d interact with the medical sales reps that were coming in for meetings. As a college student, he was always struck by the sales reps’ kindness and career guidance.
Finding medical device sales to be both interesting and rewarding, Meyer decided to pursue the career post-grad. Soon after he graduated from college, he got the opportunity to take a role as an account manager at a medical equipment manufacturer in the Detroit area.
“I decided to apply for an account manager position for a medical manufacturing company, and was fortunate enough to be hired. Looking back, I had no idea at the time how big of an impact that decision would have on the rest of my life,” said Matt Meyer, now the U.S. Distribution Lead for First Quality®
From there, Meyer worked his way up throughout his career at various healthcare-focused organizations, finally landing at his current company in 2022. In Meyer’s current position, he manages First Quality’s relationships with medical distributors, providing products that go to skilled nursing facilities, home medical equipment providers, and other healthcare partners.
“I am in a unique role at First Quality, because through

my relationships with distributors I’m connected in some way to every account they sell to, but I don’t directly manage any of them,” said Meyer. “This role requires me to be highly collaborative both internally with our extensive sales team and externally to ensure that the company and client are reaching our goals together.”
Creating winning partnerships
Early in his career, Meyer worked with a manager that used a concise, three-step formula for
building high-performing teams. It included hiring talented people, creating a culture of winning, and fostering a drive to deliver results. The approach stuck with him, and it’s exactly what he appreciates about being part of First Quality.
“I’m fortunate to work with extremely talented colleagues on our sales team who are passionate about making things better for the people who use our products,” said Meyer. “First Quality has a strong culture that empowers us to make decisions and take strategic risks while celebrating our successes and learning from our failures, which results in a natural drive to deliver results.”
In 1989, First Quality recognized that there was an unmet need for high-quality, disposable incontinence products tailored for seniors in healthcare settings. First Quality’s teams visited skilled nursing facilities and it became clear that the staff needed access to the right products for residents, said Meyer. The company also acknowledged that nursing facility and hospital staff needed access to education
Matt Meyer
and support services to create more effective incontinence management programs.
“Today, our Prevail® adult incontinence products remain a leading choice among skilled nursing facilities,” said Meyer. “We help residents who are managing incontinence have a more dignified experience, while also supporting their family and professional caregivers. We’re grateful to be able to do that in partnership with our distribution partners, who are equally committed to the facilities and people they serve.”
Strength in the face of challenge
The healthcare industry continues to face staffing shortages within hospitals and nursing facilities, posing ongoing challenges for healthcare professionals and distributors.
“In the skilled nursing facility world, obstacles associated with staffing levels continue to be on the minds of owners, operators and clinicians everywhere. For many, a lack of staff is preventing empty beds from being filled,” said Meyer.
To mitigate staffing challenges, First Quality has created incontinence management programs that aim to reduce workloads for nursing staff and improve medical facility efficiency. The company’s personalized approach to incontinence management can reduce manual labor for skilled nursing facilities by fitting each patient with incontinence products that are the right size and absorbency for their individual needs, which is “part of the value that we bring to customers alongside our distributor partners,” said Meyer.
Post-COVID, sales reps have also recognized that certain aspects of care that used to take place within the hospital or assisted living facility are now moving to a home care setting. Family members without any medical training are increasingly becoming instant caregivers.
“First Quality understands that caring for a loved one with incontinence can be overwhelming, so the company has invested heavily in our Prevail eNurseTM programs to support those caregivers,” said Meyer. “This gives caregivers access to our clinical team who can answer questions about product selection, sizing, skin health and other incontinence-related topics. We continue to invest in our suite of
at the same time supporting its customers’ emission reduction goals. For example, all of First Quality’s manufacturing sites in Pennsylvania are now powered by carbon-free electricity.
“Our sustainability team is also focused on incorporating more recycled content into our packaging, which is something we know is important to our customers,” said Meyer. “Most of our product packaging includes a minimum of 20% post-consumer recycled (PCR) content and our packaging experts are exploring how to incorporate even more in the future.”
First Quality’s mission for the future goes beyond sustainability into improving healthcare industry outcomes overall.
Post-COVID, sales reps have also recognized that certain aspects of care that used to take place within the hospital or assisted living facility are now moving to a home care setting. Family members without any medical training are increasingly becoming instant caregivers.
digital tools and clinical resources for caregivers who are helping patients manage incontinence at home, and for professional caregivers at facilities.”
Sustaining the future
First Quality’s motto is “Make Things Better,” which includes sustainability efforts and leaving the healthcare industry better for future generations. The company actively aims to reduce greenhouse gas emissions from its manufacturing facilities, while
“The size and scale of First Quality allows the organization to be nimble and make impactful decisions quickly, which allows us to get all the volume-based advantages of a big company without the organizational clutter to weigh us down,” said Meyer.
“I’m grateful that we have an experienced leadership team that is unconcerned where ideas are generated,” said Meyer. “It ultimately empowers us to make decisions and benefit the industry and our customer foremost.”

Cross-Industry Selling Strategies
What medical sales can learn from other sectors.
By Brian Sullivan
 While I “grew up” in the medical industry as a manufacturer rep working with distributors, clinics, surgery centers and hospitals of all sizes, for the last 20 years as founder of PRECISE Selling, I have had the opportunity to learn from other industries. And guess what? There are a lot of things we can learn from ‘em!
In the vibrant festival of sales strategies, where every pitch and close is as different as the attractions offered, medical sales reps might sometimes feel like they’re in charge of the first aid tent –indispensable, but not exactly the main attraction. Meanwhile, over in tech and consumer goods, salespeople are throwing neon-lit parties with every transaction. So, what can the medical distribution and manufacturer reps learn from their flashier cousins in other sectors? Quite a bit, as it turns out.
1 The tech sector’s love affair with data
Tech sales teams don’t just use data; they practically worship it. Every decision, from lead priori-
tization to the optimal time for a follow-up call, is backed by a heap of data and analytics. What’s the takeaway for medical sales? Start loving your data hard. Track outcomes religiously and learn from the numbers. If the tech guys can predict a client’s sneeze from three software updates away, you can certainly forecast a hospital’s inventory needs before they run out of gauze.
This means, as a salesperson, you need to know (the data) on how many prospecting calls you need to make with either existing clients or new ones, to generate one demo/detailed meeting. It also means you need to bring clinical data to your presentations to prove that your solution’s

return far outweighs the invest. Clinical data, white papers/studies, and ROI calculators are a lot more powerful than a rep saying, “I’m telling you, I have a ton of clinics who love this thing.”
2 Consumer goods’ flair for engaging presentations
Let’s face it: selling consumer goods often revolves around creating a buzz. It’s all about shiny packages and eye-catching displays. Now, no one’s suggesting you bedazzle your medical devices or perfume your pharmaceuticals (please don’t), but there’s a lesson here in presentation. Make your pitches as engaging as a Super Bowl commercial. Remember, doctors and hospital admins


are humans too – they’re just as interested in a well-told story or a visually appealing chart as the next person.
And don’t forget, you too are part of the overall solution. Brand yourself, be different, be creative. If you look, sound, act and smell like every other rep in your category, you will get no attention, never mind a demo or sale.

3 Automotive industry’s follow-up game
Ever bought a car? Remember how the salesperson practically became your new best friend, checking in regularly until you either gave in and bought the car or filed a restraining order? There’s a middle ground in our industry. Regular follow-ups show that you care about more than just quotas; you’re there to solve problems. So, channel your inner car salesman – just don’t overdo it. You want to be remembered for your persistence, not your pestering.
4 Fashion’s use of influencers
The fashion industry has long known the power of influencers. And no, we’re not suggesting you get an Instagram star to pose with
a stethoscope. However, every hospital and clinic has its influencers – key opinion leaders who sway decision-making. Identify these individuals, and tailor your pitch to meet their specific needs and preferences. They might not share their outfit of the day, but their endorsement could be your ticket to a successful sale.
5 Hospitality’s customer service
If the hospitality industry were a person, it’d be that super attentive friend who remembers your coffee order and asks about your cat’s health. Medical sales could use some of that attentiveness. It’s not just about making the sale; it’s about enhancing the customer experience. From smooth onboarding processes to handling complaints with a smile, the level of service you provide can set you apart from competitors.

6 Real estate’s local knowledge
Real estate moguls are all about location, location, location. They know every detail about the areas they cover. Similarly, medical sales reps should become local experts in their market segments. Know your territory inside and out – from regional health concerns to local administrative quirks. Being a local guru can make your advice much more personalized and impactful.





7 Entertainment’s ability to captivate
Lastly, take a cue from the entertainment industry. No, you don’t need to sing or dance (unless you’re really good at it). But think about how films and TV shows captivate audiences. They tell compelling stories that evoke emotions and keep people coming back for more. Craft narratives around your products that highlight their impact on patient care and hospital efficiency. Make your clients the heroes of a success story featuring your products.
In conclusion, while the medical sales field might seem worlds apart from tech gadgets, fast cars, or fashion, the fundamental principles of selling apply universally. By borrowing a little sparkle from these sectors, you can inject some excitement and effectiveness into your strategies. Remember, it’s not just what you sell; it’s how you sell it. Now, go out there and make those sales sparkle, and maybe, just maybe, consider that bedazzled defibrillator cover. Just kidding. Or am I?
Brian Sullivan, CSP, is the founder of PRECISE Selling and a leading voice in the field of sales training and development. He believes in the potential of every salesperson to achieve their best and continually challenges sales professionals to reach new heights. To have Brian Sullivan or one of his stable of trainers and coaches help your team get to the top, visit them at www.preciseselling.com.





















































































Endotracheal Tube Holders
Hold-n-Place® Foley Catheter Holders
IV-ARMOR® ACE Connectors® Abdominal Binders
Post-Surgical Bras
Tracheostomy Tube Holders
NasoGastric Tube Holders
Bendable ArmBoards
Transducer Holder
Rude or Invested in Success?
How to ask the right questions in the right way to better understand your customers’ needs.
By Patrick T. Malone

 We succeed when we help others succeed, and that is the role of sales and customer service professionals. The opportunities are many, such as helping a clinic improve compliance programs or increasing patient involvement.
That goal of helping others succeed, then begs the questions “How can we help others succeed if we don’t know where they want to go?” Or “Where are they now?” Or “What is standing in the way?” Or any number
of additional questions that will provide us with information that is necessary if we really want to help others succeed.
I was surprised to read of a research project from the School of Business at George Mason
University. It concluded that many business school students were reluctant to ask what they defined as “sensitive” business questions because of the fear of being rude. Those fears are not limited to MBAs. I have seen


the same reluctance in other professionals across a wide variety of industries.
While no one wants to be rude, nosey, overbearing, or insensitive, I believe the fear of asking some questions is often overblown. After all, the best decisions, business or personal, are based on the best information available at that time. So, consider these suggestions to reduce the risk of appearing rude when asking questions that are necessary but also could be considered sensitive.
confirmation. So never ask a question that can be answered with a “yes or no” while you are in the investigative portion of the conversation. Save those for the conclusion of the conversation when you are confirming your understanding of the information uncovered.
Desensitize the questions by triangulating to focus on the problem as opposed to the people. Replace the words you and yours with it, that, and this. Personal pronouns evoke emotions, one of which is sensitivity. Impersonal pronouns keep the focus
There is a dramatic difference between hearing a response and understanding it. Prove you truly do understand by briefly summarizing the response or by asking a relevant question about the response.

Succinct yet sensitive
Business questions should be brief, concise, and open-ended. Prefacing your question with a preamble to soften the question is never a clever idea. Your mission is to gather information, not to become enamored with the sound of your own voice. Openended questions get information, close-ended questions only get
on logic and fact. Some emotion will always be present in any conversation, so the challenge is to minimize the impact of negative emotion while boosting the effects of positive emotion.
A simple question like “how important is teamwork in the practice?” reveals our own bias. It shows that we believe teamwork is important and are only interested in understanding the degree of importance in this practice. Check your biases at the door by creating neutral questions. “What does the practice’s culture look like?” or “Help me understand your practice’s culture.”
Asking the right questions, the right way, is a good start. The way you acknowledge the responses you receive to those questions is of equal importance. Questions
without acknowledgement of the responses received are rude and sound very much like interrogation. Be present. Unfortunately, many of us plan our next question while our client is still responding to the initial question. Their responses deserve our 100% attention. A brief pause often signals how well we are processing the information just received.
There is a dramatic difference between hearing a response and understanding it. Prove you truly do understand by briefly summarizing the response or by asking a relevant question about the response.
Remember that your questions are asking for another’s point of view and do not be surprised if that conflicts with your own point of view. This is where the word RESPECT goes a long way facilitating an informative conversation. Also remember that the word “respect” is not synonymous with the word “agree.” You are not saying the other person is right rather, simply respecting their right to a different point of view at this moment in the conversation.
America may run on Dunkin or Krispy Kreme or Tim Horton, but business runs on the best information available. You are in the business of helping your clients succeed and to do that you must obtain the information that drives successful decisions. Appropriate business questions will help both you and your client get where you both wish to go.
PS: Have a business question that you are reluctant to ask? Send it to me with the appropriate context and I will offer some suggestions.


• RSV
• Flu + SARS Antigen*
• SARS Antigen* SARS Antigen+** Influenza A+B Strep A+

• RSV + hMPV
• Influenza A+B
• Strep Complete (Strep A+C/G) SARS-CoV-2*

• RSV
• Influenza A+B
• Strep A
QuickVue In-Line® Strep A
QuickVue+® Strep A

Sofia 2 and Solana platforms come equipped with the power of the Virena® System
Observe, track, report and respond rapidly to
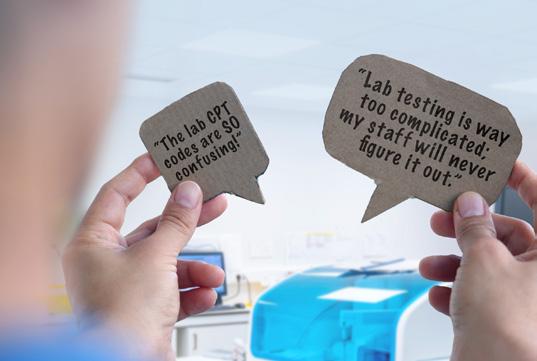
Times Have Changed
There are some well-worn phrases you just don’t hear much of anymore when it comes to the physician office lab.
By Jim Poggi
“Lab is too hard to sell; I’m sticking to med/surg.”
This used to be a daily comment we all heard a few years ago from even seasoned distributor account managers. Back then, when lab was a new adventure for many of us, we all assumed we needed to be technical lab experts. Lab seemed to have its own foreign language, and even the association between lab products and CLIA regulations felt daunting. We were comfortable “going it alone” for med/surg products we had sold for years, but lab was a different animal altogether.
How wrong we were in our assumptions and sales approach! We eventually learned that the key to selling lab was to know enough to “sell the meeting” and that team selling with our key manufacturers and colleagues who had more experience with lab would make all the difference in our success. With that change in our thought process, and the implementation of specialty lab sales forces with many distributors, we have grown the business and learned how to optimize our own personal lab business and revenue.


For many of us, lab is now as comfortable as our daily med/ surg products were a few years ago. The effort shows, and we have built stronger customer relationships and a durable source of revenue for us and clinical value for our customers. Our willingness to step out and learn a new skill and provide new ways to improve the customer experience proves that we can grow as consultants and become an even stronger advocate for our physician office customers.
The following is a whimsical look at lab objections and challenges from both the customer and sales account manager perspective. Hopefully, it will rekindle a few memories and elicit a laugh or two as folks realize the number of stumbling blocks we placed in front of ourselves, but conquered anyway.
“Open a lab; you can make a ton of money!”
If this does not sound familiar, you are either a rookie in the lab business, have amnesia or selective memory. Not only do I remember hearing it, I may even remember saying it. The story varied some, but a key advantage of a physician office lab in the pre-CLIA days and up to the introduction of PAMA was the argument that creating a lab was a way for a physician practice to add a revenue stream to their practice. We sometimes discussed the clinical advantages of having a lab on site, but we more often pointed to the ability to capture revenue by bringing in-house several of the most frequently requested send out tests.
While true, this was a pretty narrow value proposition and
often did not address the core reason to perform lab tests on site: “to initiate or modify a patient treatment program”. It also led to the possibility that the physician office lab may not live up to the perceived high profitability the customer imagined, creating the possibility of customer dissatisfaction.
finally enforced in 1992. Nearly every sales rep in distribution and lab manufacturing heard it, and we also had the same sorts of questions on our minds that we heard from our customers. In the early going, concerns about CLIA and compliance with the new regulations drove many manufacturers and distributors
Have a formal plan, get it in front of the customer, your lab manufacturers and any other parties helping with the implementation including consultants to get the job done right. Overplanning beats underplanning every time.
PAMA and the increasing sophistication of our customers has helped us and our lab manufacturers to develop a far broader view of the value of lab and far more impactful customer value propositions. Lab is fundamental to the best standards of patient care and our story includes facts to back up this promise readily. Today we can track trends in patient lab values, screen for chronic diseases early enough to improve patient outcomes and even to uncover predispositions to diseases even before they become apparent. We have come a long way, and we continue to improve in this area. As consultants, our value and story has improved significantly over time. While there are challenges associated with PAMA, we can also thank PAMA for helping us to improve.
“CLIA is too confusing; no lab for me.”
I have heard this statement frequently since CLIA ’88 was
to limit their focus on lab tests. Gradually, as knowledge increased and the interpretation of the regulations became more well known, this trend began to reverse itself.
At the same time, many local lab consultants arrived on the scene to help. National consultants followed and today many distributors have internal resources available to help customers understand and cope with CLIA. Even more recently, cloud-based expert software and lab management solutions have entered the market and can help start up a new lab or assist an existing lab to know, understand and comply with the myriad CLIA regulations on technology, result quality and personnel standards. Check with your colleagues and trusted lab manufacturers to understand the wide range of CLIA help available today. Assistance is far more available than it was in the early going.
ID NOW™ PLATFORM
ONE SWAB THREE RESULTS
THE ID NOW™ PLATFORM GIVES CLINICIANS THE FLEXIBILITY TO TEST FOR COVID-19 AND EASILY ADD ON FLU A & B BASED ON CLINICAL NECESSITYWITHOUT THE NEED FOR COLLECTING AN ADDITIONAL SWAB.*
With the ID NOW™ Platform, the clinicians have the power to decide which tests to run based on patient presentation, circulating prevalence and seasonality. By reducing unnecessary testing, clinicians can save time and resources, allowing for rapid diagnosis and improved patient workflow.

“The
lab CPT codes are SO confusing!”
That statement was mostly made by the sales and marketing teams of lab manufacturers and distributors, but reflected the state of the payor market before PAMA when nearly every CPT code had a carrier specific payment amount.
Remember before PAMA, the Protecting Access to Medicare Act? Before 2018, when PAMA went into effect, most lab CPT codes were locally determined by each Medicare payor. At that time, there were 57 separate payors and consequently up to 57 different reimbursements for each assay. While many of the more common ones had similar or identical reimbursement across payors, many of them did not. And while some codes were attractive in some markets, other codes for the same test were not. Immunoassay tests and tumor markers stand out as tests whose reimbursement varied significantly from payor to payor and market to market.
“Pee in the cup and leave it next to the sink.”
Once upon a time, pretty much every annual physical or patient visit with concerns about diabetes or urinary tract infection involved a urinalysis test. Now, not so much. When was the last time you were asked to “pee in the cup” on a routine annual physical? Last time you saw urine cups stacked up in the doctor office rest room? These have ceased to be common sights.
But, as you sell lab and more importantly patient care, urinalysis stands out as the quickest, most comprehensive and non-invasive way to screen for diabetes, urinary tract infection and other organ diseases. Test frequently, diagnose early and save time, money and help patients recover more quickly are all reasons to support increased use of urinalysis.
Fact to share: UTI is one of the more common reasons for the development of sepsis, so urinalysis also supports diagnosis of a
As a sales consultant, we need to be mindful that many practices now have a broader variety of influencers, and as a result, we need to take the time to understand the dynamics of decision making in the practice.
One of the benefits of PAMA was that most legacy local reimbursements for lab tests were abolished in favor of national reimbursement limits. Today there are 1991 lab CPT codes, and only 51 local codes. As a result, it is far easier for you, your trusted lab manufacturers and our customers to understand the reimbursement level for most lab tests.
potentially life-threatening illness as well as many longerterm chronic diseases. The CPT code for routine urinalysis is 81003. It is national and reimburses $2.25. Urinalysis including a microscopic test is CPT code 81001 and reimburses $3.17 nationally. Remember that toxicology screening is also done on urinalysis as is microalbumin/creatinine testing
to assess kidney function. These assays have their own CPT codes and reimbursement. Need more information? Consult your trusted urinalysis lab manufacturer.
“I can diagnose flu; I don’t need to test.”
In the early days of flu testing between the late ’90s and early 2000s, this was a pretty common customer objection. We often heard it with a raised customer eyebrow and the implied suggestion that we were challenging the clinical knowledge of the physician we were talking to. Awkward. But, in studies published by the Centers for Disease Control and Prevention (CDC), the data shows that many respiratory illnesses mimic influenza symptoms and we can focus on the clinical story, not how good the physician is at respiratory pathogen diagnosis. In any given year, the number of influenza tests that correlate with the disease is under 40% and with the advent of COVID-19, the numbers continue to drop. For the past season, only 16% of all influenza tests reported to CDC were positive. The end result: to be sure, your customers need to test. There is a wide variety of respiratory pathogens and many have similar symptoms.
“Every long-term care facility vaccinates patients; no need to test the patients.”
I personally fell for this one a few years ago. When you first hear it, it seems to make sense. Then once you do a little thinking, it no longer does. The latest data suggests that only 27% of elder Americans have a sufficient response to the flu vaccine to be protected. So, just because every

patient in a long-term care facility gets a flu shot does not mean that flu will not take hold and circulate throughout the facility.
The most effective way to avoid spreading the flu throughout the facility is to test patients with symptoms, and then isolate those who are positive for flu. This also applies to COVID-19 and RSV. Elder patients typically have more severe symptoms from any of these respiratory pathogens and run the risk of contracting pneumonia as a complication of the underlying disease. This progression can be serious and even life threatening.
“We can’t find the patient record in the files.”
Setting the issue aside of how much a customer likes their EMR, paper files and their issues (misfiles, lost files, “borrowed files” that never return) are in the past. Your efforts along with government subsidies and the development of a robust suite of EMR products have finally brought us into the 21st century. EMR in addition to other technologies I will discuss later in this column have made data more timely, accurate and accessible. At-home testing seems to be the last hold out, but there is technology in development to integrate at-home testing into EMR. Still clunky, but effort is there to plug this gap.
“The patient called looking for their lab results.”
For the most part, the neverending round of phone calls from the physician office to the patient and back again has been made a thing of the past due to EMR and patient portals. At one point, I calculated that before EMR and

patient portals it took an average of seven calls back and forth for the physician office to get lab test results to working adults. EMR and patient portals have made a patient’s confidential data easy to access safely and shows result history clearly and in a way that is easy to understand. Portals I am familiar with also show test result trends over time, which results are abnormal, permit asking questions and making appointments online and significantly streamline the back office process both for caregivers and patients alike.
“We can figure this out without too much training.”
This is the surest way I know of to fail when switching from a waived lab solution to a moderate complexity solution. Limited training for a new chemistry or hematology system can lead to several adverse outcomes from inaccurate results to no results at all. Building a strong implementation program with your lab manufacturer and sticking to the program is the surest way to make this transition successful. Have a
formal plan, get it in front of the customer, your lab manufacturers and any other parties helping with the implementation including consultants to get the job done right. Overplanning beats underplanning every time. If you don’t believe me, try both and let me know how it goes.
“Medicare is the lowest cost payor; we do not accept Medicare.” I have seen versions of the “we do not accept Medicare” sign at any number of physician offices in my career. At one point, probably more than 20 years ago, Medicare and Medicaid paid less than commercial insurance for lab tests. But the whole premise behind PAMA was to align Medicare with the lower costs being paid by private insurance for lab tests. And that premise was confirmed by the Office of the Inspector General’s reporting. PAMA has taken some halting steps to align with private insurance and after some legislative delays, 2025 will see what the next round of proposed cuts will look

like. Medicare has the authority to lower reimbursement for tests that have higher reimbursement than private insurance by up to 15% in 2025. The data is being collected and analyzed this year and the next Clinical Lab Fee Schedule, due in December of 2024, will show what the current gap looks like. Don’t be surprised to see some further cuts for the coming year.
“The doctor will see you now.”
A time long ago, before the clinical staff included Nurse Practitioners and Physician Assistants, this usually meant you were going to see your primary care physician, and they would be looking at you, not a laptop screen. For many practices, this situation now means you will see a member of the physician’s staff, and your vitals will be taken by a medical assistant. This is not necessarily a bad thing, but it does reflect changes to both staffing and the cost of managing a clinical practice that are increasing.
As a sales consultant, we need to be mindful that many
practices now have a broader variety of influencers, and as a result, we need to take the time to understand the dynamics of decision making in the practice. Whether the practice has an existing lab or you are working with them to have them consider implementing a lab, you need to know each decision maker, their role and their attitude toward lab and its impact on patient care. The savvy consultant knows and understands each influencer in the practice and actively works with them on current and future practice opportunities.
“Lab testing is way too complicated; my staff will never figure it out.”
Once upon a time, before most lab chemistry reagents were liquid ready to use, lab instrument systems had built-in help and we even had the first CLIA waived hematology or molecular systems, this statement was truer than not. With lab technology becoming ever easier and the trickle down of highly sophisticated technology (PCR and other
molecular tests in particular), those days are over.
The well-equipped physician office lab today can perform chemistry, immunoassay, hematology and molecular tests that even large-scale hospital labs found challenging to implement just a few years ago. The progress of technology, along with more sophisticated training methods and help via the internet has leveled the playing field to a large extent where lab testing is concerned. Systems are smaller, smarter, faster, easier to use and have more fail-safe mechanisms to prevent errors than ever before. Add in your consulting efforts along with your lab equipment manufacturers and your commitment to customer satisfaction, and lab testing has never been easier or more accessible from a technical viewpoint.
I see the future as bright for easier to use microbiology systems to enter the market in the next few years. They will probably be powered by molecular systems similar to those in use today, and the range of available assays will also grow.
I wonder when and if the most exciting developments in cancer diagnosis and monitoring will make it to the physician office lab. Liquid biopsy and other cellular detection methods are becoming more frequently used in tertiary care centers and I believe it is only a matter of time before they make it to the physician office lab. In combination with large scale data sets and expert system analytical tools, there is a revolution happening that is sure to come our way. I wonder what the next version of “things you don’t hear much anymore” will include. Watch this space and we will learn together.
All Cards On the Table
Why transparency in a post-pandemic healthcare setting is foundational to a strong supply chain.

 As a global medical products distributor, Cardinal Health approaches the topic of preparedness for any disruption with a focus on transparency, said Mary Byrne, vice president of Global Regional Planning for Cardinal Health’s Global Medical Products and Distribution business.
“We take an open, all-cards-on-the-table approach specific to the needs of the customer and their portfolio of products.”
Byrne has led strategic initiatives and transformation in several industries, including healthcare, technology and defense.
“We understand that every healthcare provider has products that are critical to care and their ability to maintain operations,
and those products can differ widely based on the type of care and location of that particular provider. We prefer to work collaboratively with each customer and advise on an approach to preparedness that meets their unique needs.”
Transparency is an area of great focus at Cardinal Health. In 2023, the distributor received the HIRC Transparency Badge (and renewed it again in 2024), which acknowledges transparency as a foundational element of a strong supply chain, Bryne said. The
badge is awarded by the Healthcare Industry Resilience Collaborative (HIRC), a nonprofit healthcare supply chain trade association focused on tackling resiliency issues for continuity of patient care. The renewal of the HIRC Resiliency Badge demonstrates Cardinal Health’s continued dedication to the highest standards of transparency and resiliency in healthcare supply chain management, Byrne said. “We’re very proud of our team members who work every day to drive excellence within our supply chain for our customers and their patients.”
Additionally, earlier this year, Cardinal Health achieved the HIRC Resiliency Badge at the Diamond level, the highest award possible, indicating “outperforming” scores for Cardinal Health’s medical product distribution business in key areas critical to a resilient supply chain. “We are the first distributor to be recognized by HIRC for both supply chain resiliency and transparency,” Byrne said. “Through its comprehensive, multi-layered approach, the HIRC Resiliency Badge program enables distributors like Cardinal Health to better compete on the merits of supply chain resiliency and helps healthcare providers more readily select suppliers with demonstrated resiliency.”
The Diamond level is attained through a rigorous external assessment from either PwC or Accenture against HIRC’s standard – a 400-point maturity rubric that assesses resiliency and operational maturity, said HIRC Executive Director Jesse Schafer. It’s a two-month process, with one month of supplier readiness, where suppliers must
upload artifacts that include key performance indicators, policy, procedure, self-assessment, and ultimately an interview. Then in month two, PwC or Accenture will crosswalk those artifacts versus the public facing rubric on HIRC’s website and make a maturity assessment. All those results are weighted.
Industry-wide standards
The number of healthcare providers using HIRC standards in sourcing continues to trend upward. Today, HIRC stands at almost 50 health systems using its standards, from Advent Health to Yale New Haven Health. The number of suppliers participating continues to grow.
providers desperately want to select for resiliency in their sourcing process,” said Schafer.
“At Stanford Health Care, resiliency is non-negotiable,” said Katie Dean, vice president of Supply Chain, Stanford Health Care. “We helped build the Resiliency Badge program to better identify resiliency and to select for this capability in strategic relationships at an industry level.”
Tom Lubotsky, vice president of Supply Chain, Allina Health, said his organization is fully committed to resiliency as key selection and performance criteria for purchasing products. “The evidence of a reliable environment to deliver products has clearly risen in its
“We helped build the Resiliency Badge program to better identify resiliency and to select for this capability in strategic relationships at an industry level.”
“We need resiliency for continuity of patient care,” said Schafer. “There is a belief that a community approach through a nonprofit consortium with a collaborative culture is the right way to achieve it.”
The Resiliency Badge is a new incentive that’s creating the response HIRC organizers were hoping to see among industry stakeholders, said Schafer. The standards are intended to make resiliency a commercial differentiator and a win for sourcing and selection. “When providers say, ‘Do this, and you’ll more often receive juicy contracts from me,’ the industry reacts, and the reason we’re doing this is because our
importance as we evaluate, select and monitor the performance of our suppliers.”
HIRC standards are also being used by other industry evaluators in their assessments. This past May, Gartner announced it was adding a quantitative risk management component to the Healthcare Supply Chain Top 25 for 2024 at a 5% weighting. This component of the ranking credits health systems for taking a leading role in their approach to risk management through increasing engagement with HIRC.
Gartner said it has been watching this space intently as an informal and formal industry
collaborator since the founding of HIRC. “HIRC has made great strides as a consortium for patient-centric healthcare supply chain resiliency standards and best practices,” Gartner said in a release. “The group is a non-competitive, non-exclusive and member-driven organization where leaders in this space are convening to improve supply chain resiliency for the industry.”
badged suppliers. This represents 30% of the available score for this component.
` Resiliency Leader tracks health systems implementing resiliency standards with suppliers. For 2024, this is simply including HIRC resiliency standard term questions in competitive bids with suppliers. This represents 40% of the available score for this component.
“By integrating our AI-powered platform with HIRC’s industry expertise and best practices, we’re creating a comprehensive solution that goes well beyond traditional supply chain management.”
For 2024, the allocation of this 5% weighting will be granted with increasing levels of engagement with HIRC standards. HIRC will provide Gartner data in categories, per their own internal guidelines communicated to their members:
` Resiliency Engaged is focused on being an engaged member of HIRC attending more than 50% of their meetings. This represents 30% of the available score for this component.
` Resiliency Accountable tracks health systems having dedicated resources for risk management activities. Gartner research shows that 56% of U.S. systems have such resources today. Along with this resource allocation, points will be awarded for having a formal supply chain business continuity plan and being able to report spend with HIRC transparency and resiliency
“Like our journey on the quantitative capabilities around ESG partnering with the groups Healthcare Anchor Network and Practice Greenhealth, we view measuring health systems for risk management on a continuum,” Gartner said. “Over time, our hope is to modify these measures to be more comparative of how individual health systems are to each other. But, for now, membership, engagement and leadership are important enough to get started.”
HIRC also recently announced a long-term strategic partnership to co-develop transformative technology and data standards with Clarium, Inc., an AI-powered platform for healthcare supply chain, leveraging data sharing, crowd-sourcing, and intelligent automation to help hospitals and health systems achieve resiliency, best practices, and operational excellence.
The partnership’s first initiative is the development of Resiliency Monitor, a tool designed to provide real-time visibility into healthcare supply chain performance. Resiliency Monitor will offer providers and suppliers evidence-based requirements to more efficiently achieve badge award status and will offer the following features:
` Dynamic metrics at distributor, manufacturer, product category, and item levels
` Automated data sharing aligned with HIRC’s Transparency and Resiliency Badge
` At-a-glance performance assessments for providers and suppliers
Resiliency Monitor will be available to all HIRC members, with a premium tier subscription available that will provide additional insights and features.
“Our collaboration with HIRC represents a pivotal advancement in healthcare supply chain and in ensuring the continuity of patient care,” Clarium said in a release.
“By integrating our AI-powered platform with HIRC’s industry expertise and best practices, we’re creating a comprehensive solution that goes well beyond traditional supply chain management. Our shared vision is to empower healthcare providers and suppliers with real-time insights, enabling them to proactively address challenges and optimize operations. This partnership isn’t just about building software together – it’s about transforming how the healthcare industry approaches supply chain resiliency and efficiency.”
Proactive planning
Even with new tools, technology and standards, planning still must
Trich Or Treat?


Trixie
happen at the relationship level between provider and supplier. As such, Cardinal Health proactively discusses supply chain resiliency with customers on a regular basis. “It’s baked into the DNA of our medical products distribution organization,” Byrne said. “The industry – especially providers – are interested in what we’re doing to drive an efficient and resilient supply chain so they can continuously count on us to deliver the products they need when they need them.”
There are several factors that Cardinal Health believes providers should be aware of when considering preparedness. First, healthcare providers need to know where their supply chains are most exposed or at-risk. It is important that providers acknowledge these exposures and then take a proactive approach to addressing them.
“You don’t want to have a conversation about risk when you’re in the middle of a crisis –you want to be prepared ahead of any major disruption,” said Byrne. “This brings us back to the importance of transparency. It helps tremendously when we can speak openly about factors that create better resiliency. Twenty years ago, resiliency was not a department or even a list of projects across most companies. Now, it’s simply the right way to do business. Cardinal Health has a dynamic, ongoing process to continually evaluate our operations and develop new and innovative ways of operating with consistent resiliency.”
Many provider organizations are already taking the right steps toward resiliency, engaging in conversations about implementing
a full suite of preparedness tools, including multi-sourced supplies, multi-modal transportation, critical-to-care products, advanced planning approaches, near-shoring of products and more. It’s also important for providers to consider their local regulations, Byrne said. In California, for example, employers in hospital settings are required to have specific inventory levels of personal protective equipment (PPE) at all times.
meaningful change that is making a difference in preparedness and resiliency. Byrne cited recent examples like the advocacy for transportation “fast-passes” for medical products during emergencies, more transparency in data-sharing, and resiliency assessments for suppliers.
Cardinal Health continues to work with providers on developing a collaborative planning approach. This includes integrating
Cardinal Health continues to work with providers on developing a collaborative planning approach. This includes integrating the customer’s insights and data on the volume of products they need from the distributor to drive patient care.
Ideally, providers should consider collaborating with suppliers in an advanced model referred to as Collaborative Forecasting, Planning, and Replenishment (CPFR), Byrne said. CPFR is a recent addition to the healthcare industry, developed initially by VICS and further developed by Gartner. “We find that sharing this model and driving collaboration across the supply chain drives some of the best outcomes.”
Bryne said Cardinal Health also encourages healthcare providers to take advantage of industry partnerships such as HIRC and the Healthcare Industry Distributors Association (HIDA). These organizations are engaging across the healthcare industry and government agencies to implement
the customer’s insights and data on the volume of products they need from the distributor to drive patient care. Cardinal Health also works closely with customers to segment their portfolios and identify their criticalto-care products.
“Our goal is to have a strong understanding of the customer’s needs, which requires an open dialogue and sharing of information. This helps us proactively identify potential substitute products to drive contingency plans in case of disruption,” said Byrne. “Customers tell us they appreciate this deeper level of collaboration and transparency, and we see the mutually beneficial results. Working hand-in-hand with our customers helps both sides be more strategic and prepared.”
See what’s possible

Distributors and self-distributing health systems now have complete transparency of their Dukal products’ from purchase order to delivery.
Product Assigned at the Factory Level
Product Tracking at the Item Level
Worldwide Tracking Compatible Excel Reporting
Automated Communication

Scan here to learn more or visit dukal.info/insight
Dukal is working with healthcare professionals around the world in manufacturing and supply chain solutions, to mitigate disruptions that impact business and patient health. Helping you manage everything from product to patient.
> Learn more at dukal.info/insight
Better Together
The Abbott Pandemic Defense Coalition was created to stop disease outbreaks before they stop us.
 Viruses never sleep. They move fast and change fast, “which is why we must move faster,” said Abbott.
Indeed, ongoing collaboration across the public and private sectors is critical to identify and rapidly respond to global disease outbreaks. No organization, network or country is enough to effectively fight against viral pathogens.
The Abbott Pandemic Defense Coalition was created to “stop disease outbreaks before they stop us,” according to the company. The Coalition is a network of over 20 scientific and public health organizations across five different continents focused on identifying, tracking, and responding to known and emerging disease threats to help prevent the next pandemic, while helping to end existing endemics.
“Think of the coalition like a sophisticated weather tracking system: Infectious experts with eyes on the ground using tests and technology to know how disease threats are changing – or even if new ones pop up – to stay one step ahead. We can sound the alarm and proactively address potential threats too – just like we would for a hurricane, so the necessary resources are available before an event occurs.”
Abbott said innovation happened very quickly during the COVID-19 pandemic across the U.S. healthcare system. The company is taking those learnings to apply them to address a potential next pandemic. “Our account managers work closely with customers and distribution representatives to provide testing solutions

that can flex to meet their needs based on what viruses are circulating, aligning to industry diagnostic stewardship initiatives (right test, right patient, right time).” Faster test results for infectious diseases improves operational efficiency, reduces risk, and most importantly improves speed time to treatment for patients.
Customers continue to be alert to viruses and their potential to turn into an outbreak.
“The recent human cases of H5N1 prompted discussions with both our customers and distribution representatives.
Through our work by the Abbott Pandemic Defense Coalition, as well as ongoing cross reactivity testing by our R&D teams, we were able to provide timely guidance.
“In this instance, we could share that today we continue to primarily see the H5N1 virus circulate among animals and that the good news is not only are we monitoring this, but countermeasures do exist. One countermeasure is influenza tests that detect H5N1, which quickly tell a person if they have the flu so treatment can be given.”

The 2025 PWH® Leadership Summit is headed to Frisco, Texas!
Frisco is a hub of modern innovation and growth, offers a vibrant and cutting-edge environment, making it the ideal location to inspire and empower industry leaders at this year’s leadership conference.
All leaders are welcome! Open to women & men from all career levels – Aspiring Leaders to C-Suite Executives. Gain actionable takeaways through our PWH Leadership Insights (TED-style talks), empowering keynote speakers, engaging panel discussions, workshops & breakout sessions that cover a host of topics around pressing leadership issues

The Empathetic Leader: Leading Yourself & Others
Erin Diehl, Keynote Speaker, Business Improv Edutainer, Failfluencer, and Professional Zoombie
Leadership is defined by actions, not titles, and YOU are the key to keeping people engaged, retained, and attracting top talent. Studies show that positive energy leads to higher engagement, lower turnover, and improved employee well-being. A leader’s energy, whether good or bad, has a ripple effect throughout the organization.
Erin Diehl uses her research, enthusiasm, and improv training to foster self-love, empathy, and inner peace. Discover how to harness these traits to create positive energy and empathetic leadership.
This interactive keynote combines play, improv, and experiential learning to promote a culture of positivity and abundance.

Erin Diehl is also the host of The improve it! Podcast, a Top 1% Global Podcast, and the author of the Amazon Best Seller, “I See You! A Leader’s Guide to Energizing Your Team Through Radical Empathy”. And let’s not forget her impressive track record of convincing over 39,000 professionals to embrace their inner chicken dancer!

Registration now open at mypwh.org Register today to attend the industry’s only conference completely dedicated to inclusive leadership development.
Collaborative Care and Mental Health
How integrating behavioral health services into primary care could yield better clinical outcomes.
 The head and the body are one connected system and should be treated as such, said Diane Powers, MA, MBA. “We know from many research studies that behavioral health conditions worsen medical conditions and vice versa,” she said. “It makes sense to treat them together.”

That is one of the chief goals of the AIMS Center, of which Powers is Co-Director. The AIMS Center was created 20 years ago to help healthcare organizations, clinicians, payers, and policymakers implement the Collaborative Care Model (CoCM) – a method of integrating behavioral health services into primary care and other medical settings using the principles of the chronic care model. Specifically, it is a patient-centered and population health approach that uses measurement-based treatment to target and evidence-based interventions to achieve significantly better patient outcomes as compared with usual care.
CoCM adds a behavioral health care manager and a psychiatric consultant to the primary care or medical team. They use a population health registry to support their work. CoCM has been proven in over 90 research studies worldwide to get more patients better faster than other approaches, even when usual care includes a co-located therapist in the primary care clinic.
“The AIMS Center has worked with hundreds of healthcare organizations and trained more than a thousand clinicians over the past 20 years and through that process we have learned quite a bit about what it takes to implement a healthcare innovation like CoCM, both what to do and what not to do,” Powers said. “We provide many resources on our website and we also provide implementation coaching, clinical training, a population health registry, and evaluation support. The AIMS Center continues to conduct research on CoCM and recent investigations include using CoCM for co-occurring opioid use
disorder and mental health conditions and using text messaging as an adjunct to treatment.”
New project to scale collaborate care model
This spring, AIMS and Concert Health, a Collaborative Care Platform, announced a three year, multi-state project to facilitate mental health care for 2,700 patients with complex psychiatric disorders in primary care settings. Specifically, the project will leverage and scale a Telepsychiatry Collaborative Care Model (CoCM) to help identify and treat patients with bipolar disorder and/or post-traumatic stress disorder (PTSD).
The initiative is funded through a $2.5 million award from the Patient-Centered Outcomes Research Institute (PCORI). PCORI awarded this funding to the AIMS Center research team to implement findings from the PCORI-funded SPIRIT study, which demonstrated that telepsychiatry collaborative care significantly and substantially improved clinical outcomes for patients with bipolar disorder and PTSD living in medically underserved areas, according to a release.
“The collaboration between the AIMS Center and Concert Health stems from a research trial completed a few years ago that compared telehealth CoCM to telehealth care delivered by both a psychiatrist and psychologist for patients experiencing bipolar disorder and/or post-traumatic stress disorder (PTSD),” said Powers. That study did a direct comparison of those two treatment approaches and found that CoCM was as effective while being significantly more
cost-effective and more practical considering the workforce shortages for psychiatrists and psychologists. The current project will scale CoCM for patients with bipolar disorder and/or PTSD who are being treated by Concert Health, a CoCM vendor. As a vendor, Concert Health partners with healthcare organizations to provide the behavioral health care manager, psychiatric consultant, and registry that make it possible for them to offer CoCM. The AIMS Center will train Concert Health trainers in a form of behavioral activation that was developed at the University of Washington and is designed to treat patients with bipolar disorder and PTSD.
Telepsychiatry Collaborative Care is an evidence-based model in which an integrated primary care team, including a care manager and telepsychiatrist consultant, collaboratively identify and treat patients with behavioral health conditions in primary care settings. The study also found that this model efficiently leveraged behavioral health specialist time when compared to a traditional referral approach. Published in JAMA, the findings are significant considering only one-third of patients with complex psychiatric disorders engage in specialty mental health care, and only onetenth receive adequate treatment in primary care.
Over the next three years, Concert Health and the AIMS Center will scale the findings from this research, partnering with more than 150 primary care clinics located in medically underserved areas or caring for medically underserved populations across several states. The
AIMS Center will train Concert Health’s lead psychiatric trainers and lead care manager trainers in Collaborative Care management for bipolar disorder and/ or PTSD. They will then train Concert Health’s expert care team, who will then partner with primary care providers to screen patients identified with a behavioral health need for bipolar disorder and/or PTSD, provide treatment to their patients with a patient-centered “treat to target approach,” and provide psychiatric consultation, making specific treatment recommendations focusing on symptom reductions. Concert Health’s care experts, who have treated nearly 100,000 patients, become an integrated part of preexisting care teams through sustained clinical partnerships.
Concert Health leverages the telepsychiatry CoCM paired with their expert behavioral health care team and technology platform. This is designed to create an extra layer of connection between each patient and their primary care team. The organization has spearheaded nine peer-reviewed studies that provide rigor around the measurement and reporting of CoCM outcomes, according to a release. Today Concert Health partners with leading health systems – including Advent Health, Mass General Brigham, Mercy, and CommonSpirit Health –independent health systems, independent medical groups, Federally Qualified Health Centers, and Rural Health Clinics. Concert Health reports it has driven strong clinical outcomes with half of its patients seeing at least a 50% decrease in anxiety or depression symptoms (PHQ9
or GAD7) in less than 90 days. Patients also express strong satisfaction with their experience – Concert Health’s care team upholds a 72 net promoter score (72) among patients.
“The goal of this project is to move the CoCM intervention for bipolar disorder and PTSD from research to practice as a first step to a more widespread dissemination through the AIMS Center,” Powers said.
health in the same setting is stigma, Powers said. “While there have been significant gains in the past several decades in breaking down stigma, it remains a barrier to the effective integration of behavioral health services into medical settings.”
Another barrier is payment models. Until the advent of the Collaborative Care CPT codes, it was difficult to receive reimbursement for this team-based care. In many healthcare organizations,
Concert Health leverages the telepsychiatry CoCM paired with their expert behavioral health care team and technology platform. This is designed to create an extra layer of connection between each patient and their primary care team.
All of the clinics that participated in the research trial demonstrating the effectiveness of telehealth CoCM for bipolar disorder and PTSD were federally qualified health centers that serve low-income and otherwise underserved patient populations. Some of the participating clinics were also located in rural areas. “There are other studies that have examined CoCM for common mental health conditions like depression and anxiety delivered in medically underserved areas, including one study that demonstrated that CoCM delivered via telehealth was superior, but this is the first study we are aware of that examines CoCM for bipolar disorder and PTSD, which is why it is so noteworthy,” Powers said.
Eliminating the stigma
One reason it has been difficult for U.S. healthcare providers to provide care for both physical and mental
they have separate service lines for medical and behavioral healthcare, meaning they have separate budgets and sometimes separate medical records. Additionally, some health plans carve out behavioral healthcare to organizations outside the medical clinic, entrenching silos. The CoCM approach shows promise for several reasons. Patients often prefer to receive treatment in a setting where they already have a relationship with their provider. There is also less stigma associated with receiving care at a medial clinic than at a mental health clinic, something that is particularly true in rural areas where stigma is more prevalent and where your neighbors will see where your car is parked. “In addition, CoCM has been shown in several studies to be more cost-effective than usual care, something that is important to payers and policymakers.”
Save on tests this season!
Save on tests this season!
Buy 4 kits and get one at no additional cost! †
Take advantage of these limited time offers!
Take advantage of
Mix & Match: Promotional offerings available in any combination.
BD item number Mix & Match: Promotional offerings available in any combination.
advantage of these limited time offers! BD item number Mix & Match: Promotional offerings available in any combination.
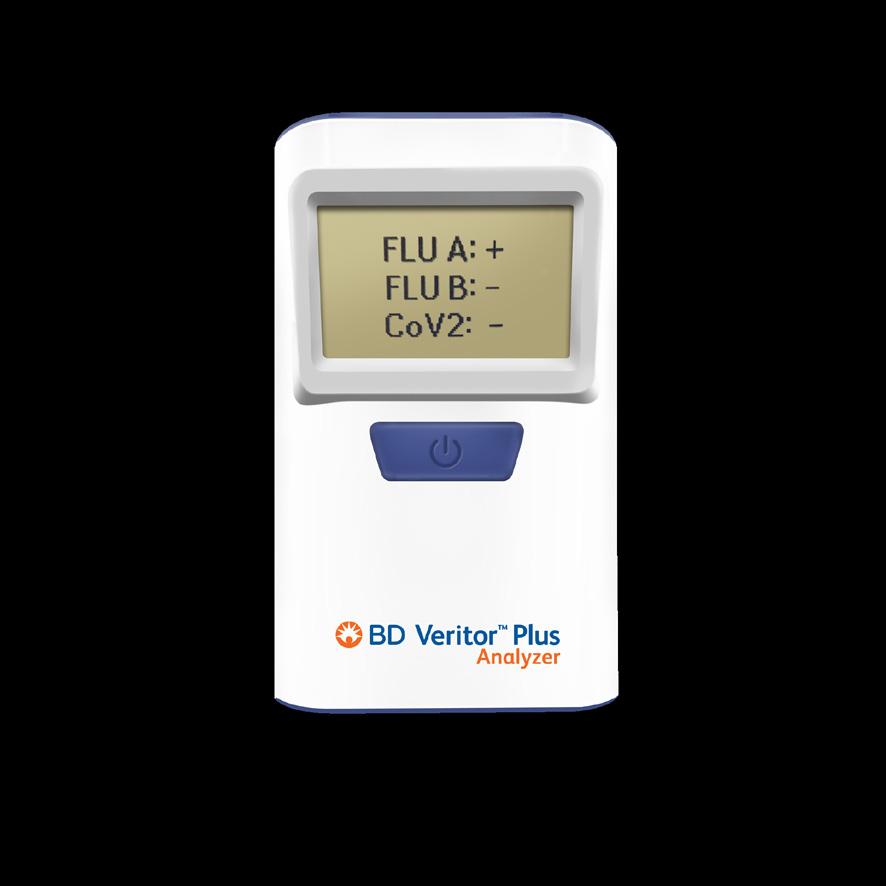
BD Veritor™ System for Rapid Detection of SARS-CoV-2 & Flu A+B* kits and get a kit at no additional cost
256088 Buy 4 BD Veritor™ System for Rapid Detection of SARS-CoV-2 & Flu A+B* kits and get a kit at no additional cost
BD Veritor™ System for Rapid Detection of SARS-CoV-2** kits and get a kit at no additional cost
256088 Buy 4 BD Veritor™ System for Rapid Detection of SARS-CoV-2 & Flu A+B* kits and get a kit at no additional cost
256082 Buy 4 BD Veritor™ System for Rapid Detection of SARS-CoV-2** kits and get a kit at no additional cost
256082 Buy 4 BD Veritor™ System for Rapid Detection of SARS-CoV-2** kits and get a kit at no additional cost
BD Veritor™ System for Rapid Detection of Respiratory Syncytial Virus CLIA-waived kits and get a kit at no additional cost
256038 Buy 4 BD Veritor™ System for Rapid Detection of Respiratory Syncytial Virus CLIA-waived kits and get a kit at no additional cost
BD Veritor™ System for Rapid Detection of Flu A+B laboratory kits and get a kit at no additional cost
256038 Buy 4 BD Veritor™ System for Rapid Detection of Respiratory Syncytial Virus CLIA-waived kits and get a kit at no additional cost
256041 Buy 4 BD Veritor™ System for Rapid Detection of Flu A+B laboratory kits and get a kit at no additional cost
256041 Buy 4
BD Veritor™ System for Rapid Detection of Flu A+B CLIA-waived kits and get a kit at no additional cost
Veritor™ System for Rapid Detection of Flu A+B laboratory kits and get a kit at no additional cost



256045 Buy 4 BD Veritor™ System for Rapid Detection of Flu A+B CLIA-waived kits and get a kit at no additional cost

Learn more about the BD respiratory season stocking event at: go.bd.com/veritoroffer
256045 Buy 4 BD Veritor™ System for Rapid Detection of Flu A+B CLIA-waived kits and get a kit at no additional cost Learn
Learn more about the BD respiratory season stocking event at: go.bd.com/veritoroffer
† Valid through December 31, 2024. Promotion may not offer additional discounts for BD Veritor™ Plus System users under existing pricing contract/ agreement. Offer is applicable to new and current BD Veritor™ Plus System users. The value of any rebates, discounts, or incentives provided may constitute a “discount or other reduction in price” under Section 1128B(b)(3)(A) of the Social Security Act (42 U.S.C. Sec.1320a-7b(b)(3)(A)). Customer shall satisfy any and all requirements imposed on buyers relating to discounts or reductions in price, including, when required by law, to disclose all discounts or other reductions in price received from BD and to accurately report under any state of federal healthcare program the net cost actually paid by customer.
† Valid through December 31, 2024. Promotion may not offer additional discounts for BD Veritor™ Plus System users under existing pricing contract/ agreement. Offer is applicable to new and current BD Veritor™ Plus System users. The value of any rebates, discounts, or incentives provided may constitute a “discount or other reduction in price” under Section 1128B(b)(3)(A) of the Social Security Act (42 U.S.C. Sec.1320a-7b(b)(3)(A)). Customer shall satisfy any and all requirements imposed on buyers relating to discounts or reductions in price, including, when required by law, to disclose all discounts or other reductions in price received from BD and to accurately report under any state of federal healthcare program the net cost actually paid by customer.
† Valid through December 31, 2024. Promotion may not offer additional discounts for BD Veritor™ Plus System users under existing pricing contract/ agreement. Offer is applicable to new and current BD Veritor™ Plus System users. The value of any rebates, discounts, or incentives provided may constitute a “discount or other reduction in price” under Section 1128B(b)(3)(A) of the Social Security Act (42 U.S.C. Sec.1320a-7b(b)(3)(A)). Customer shall satisfy any and all requirements imposed on buyers relating to discounts or reductions in price, including, when required by law, to disclose all discounts or other reductions in price received from BD and to accurately report under any state of federal healthcare program the net cost actually paid by customer.
* In the USA, the BD Veritor™ System for Rapid Detection of SARS-CoV-2 & Flu A+B has not been FDA cleared or approved but has been authorized by the FDA under an Emergency Use Authorization for use by authorized laboratories; use by laboratories certified under the CLIA, 42 U.S.C. §263a, that meet requirements to perform moderate, high, or waived complexity tests. The product is authorized for use at the Point of Care (POC), i.e., in patient care settings operating under a CLIA Certificate of Waiver, Certificate of Compliance, or Certificate of Accreditation. This product has been authorized only for the detection of proteins from SARS-CoV-2, influenza A and influenza B, not for any other viruses or pathogens; and, in the USA, the emergency use of this product is only authorized for the duration of the declaration that circumstances exist justifying the authorization of emergency use of in vitro diagnostics for detection and/or diagnosis of COVID 19 under Section 564(b)(1) of the Federal Food, Drug and Cosmetic Act, 21 U.S.C. §360bbb-3(b)(1), unless the declaration is terminated or authorization is revoked sooner.
* In the USA, the BD Veritor™ System for Rapid Detection of SARS-CoV-2 & Flu A+B has not been FDA cleared or approved but has been authorized by the FDA under an Emergency Use Authorization for use by authorized laboratories; use by laboratories certified under the CLIA, 42 U.S.C. §263a, that meet requirements to perform moderate, high, or waived complexity tests. The product is authorized for use at the Point of Care (POC), i.e., in patient care settings operating under a CLIA Certificate of Waiver, Certificate of Compliance, or Certificate of Accreditation. This product has been authorized only for the detection of proteins from SARS-CoV-2, influenza A and influenza B, not for any other viruses or pathogens; and, in the USA, the emergency use of this product is only authorized for the duration of the declaration that circumstances exist justifying the authorization of emergency use of in vitro diagnostics for detection and/or diagnosis of COVID 19 under Section 564(b)(1) of the Federal Food, Drug and Cosmetic Act, 21 U.S.C. §360bbb-3(b)(1), unless the declaration is terminated or authorization is revoked sooner.
** In the USA, the BD Veritor™ System for Rapid Detection of SARS-CoV-2 has not been FDA cleared or approved but has been authorized by the FDA under an Emergency Use Authorization for use by authorized laboratories; use by laboratories certified under the CLIA, 42 U.S.C. §263a, that meet requirements to perform moderate, high, or waived complexity tests. The product is authorized for use at the Point of Care (POC), i.e., in patient care settings operating under a CLIA Certificate of Waiver, Certificate of Compliance, or Certificate of Accreditation.
* In the USA, the BD Veritor™ System for Rapid Detection of SARS-CoV-2 & Flu A+B has not been FDA cleared or approved but has been authorized by the FDA under an Emergency Use Authorization for use by authorized laboratories; use by laboratories certified under the CLIA, 42 U.S.C. §263a, that meet requirements to perform moderate, high, or waived complexity tests. The product is authorized for use at the Point of Care (POC), i.e., in patient care settings operating under a CLIA Certificate of Waiver, Certificate of Compliance, or Certificate of Accreditation. This product has been authorized only for the detection of proteins from SARS-CoV-2, influenza A and influenza B, not for any other viruses or pathogens; and, in the USA, the emergency use of this product is only authorized for the duration of the declaration that circumstances exist justifying the authorization of emergency use of in vitro diagnostics for detection and/or diagnosis of COVID 19 under Section 564(b)(1) of the Federal Food, Drug and Cosmetic Act, 21 U.S.C. §360bbb-3(b)(1), unless the declaration is terminated or authorization is revoked sooner.
** In the USA, the BD Veritor™ System for Rapid Detection of SARS-CoV-2 has not been FDA cleared or approved but has been authorized by the FDA under an Emergency Use Authorization for use by authorized laboratories; use by laboratories certified under the CLIA, 42 U.S.C. §263a, that meet requirements to perform moderate, high, or waived complexity tests. The product is authorized for use at the Point of Care (POC), i.e., in patient care settings operating under a CLIA Certificate of Waiver, Certificate of Compliance, or Certificate of Accreditation.
This product has been authorized only for the detection of proteins from SARS-CoV-2, not for any other viruses or pathogens; and, in the USA, the emergency use of this product is only authorized for the duration of the declaration that circumstances exist justifying the authorization of emergency use of in vitro diagnostics for detection and/or diagnosis of COVID 19 under Section 564(b)(1) of the Federal Food, Drug and Cosmetic Act, 21 U.S.C. §360bbb-3(b)(1), unless the declaration is terminated or authorization is revoked sooner.
This product has been authorized only for the detection of proteins from SARS-CoV-2, not for any other viruses or pathogens; and, in the USA, the emergency use of this product is only authorized for the duration of the declaration that circumstances exist justifying the authorization of emergency use of in vitro diagnostics for detection and/or diagnosis of COVID 19 under Section 564(b)(1) of the Federal Food, Drug and Cosmetic Act, 21 U.S.C. §360bbb-3(b)(1), unless the declaration is terminated or authorization is revoked sooner.
** In the USA, the BD Veritor™ System for Rapid Detection of SARS-CoV-2 has not been FDA cleared or approved but has been authorized by the FDA under an Emergency Use Authorization for use by authorized laboratories; use by laboratories certified under the CLIA, 42 U.S.C. §263a, that meet requirements to perform moderate, high, or waived complexity tests. The product is authorized for use at the Point of Care (POC), i.e., in patient care settings operating under a CLIA Certificate of Waiver, Certificate of Compliance, or Certificate of Accreditation. This product has been authorized only for the detection of proteins from SARS-CoV-2, not for any other viruses or pathogens; and, in the USA, the emergency use of this product is only authorized for the duration of the declaration that circumstances exist justifying the authorization of emergency use of in vitro diagnostics for detection and/or diagnosis of COVID 19 under Section 564(b)(1) of the Federal Food, Drug and Cosmetic Act, 21 U.S.C. §360bbb-3(b)(1), unless the declaration is terminated or authorization is revoked sooner.
BDVeritor.com

Mental Wellbeing for All
The National Council for Mental Wellbeing advocates for equity in mental health and substance abuse treatment.
By Jenna Hughes
 Ongoing post-pandemic social challenges have resulted in increased mental health and substance abuse issues across the U.S. Mental illnesses are among one the most common health conditions in the country. According to the Centers for Disease Control (CDC), more than 1 in 5 adults are currently living with one or more mental illnesses. Mental health and wellbeing impact how a person thinks, feels, and acts, and encompasses an individual’s emotional, psychological, and social wellbeing needs.

The accessibility of mental health and substance abuse treatment is therefore exceptionally important to leading a healthy life. Nearly 30 million people across the U.S., however, don’t have access to affordable, comprehensive mental health and substance abuse treatment, according to the National Council for Mental Wellbeing.
To address this gap, The National Council for Mental Wellbeing works to ensure that mental wellbeing is a reality for everyone. The 501 (c) (3) nonprofit
association is the unifying voice of nonprofits and organizations delivering mental health and substance use recovery services throughout the U.S.
By driving policy and social change, The National Council for Mental Wellbeing advocates for equitable access to mental health services on behalf of more than 3,400 mental health and substance use treatment organizations. It serves more than 10 million children, adults, and families in total.
The National Council for Mental Wellbeing aims to build a greater overall national capacity for care delivery. Through the support of mental health organizations and investing in the workforce, The National Council promotes mental wellness as a
workforce development, improving public health, the equity of mental health access, and integrated healthcare initiatives.
The organization employs industry-specific expertise to transform the behavioral health field, empowering mental wellness organizations to succeed through its tailored consulting and training services. Through programs on critical topics including Crisis Response, high-performance leadership academies, National Mental Health Workforce Acceleration, Harm Reduction and Public Safety, an Overdose Prevention and Harm Reduction Resource Hub, and more, the National Council guides mental health organizations on the most updated industry practices.
By driving policy and social change, The National Council for Mental Wellbeing advocates for equitable access to mental health services on behalf of more than 3,400 mental health and substance use treatment organizations.
core component of health care.
To achieve this, the organization advocates for policy change and support to strengthen the substance use and mental health safety-net system, invest in provider capacity, and increase health industry-wide mental health literacy.
The National Council’s industry initiatives
The National Council of Mental Wellbeing’s focus areas for supporting the mental health industry include public policy and advocacy,
Integrated health care training provided through the National Council also offers healthcare organizations with the building blocks needed to address mental health and substance abuse so that patients’ whole health needs are covered.
Mental wellness training for healthcare organizations includes everything from guidance through team-based care and shared decision-making to bridging the gap of physical and behavioral healthcare delivery silos. Screening, Brief Intervention, and
Referral to Treatment (SBIRT) consulting additionally equips organizations with the skills and processes needed to successfully implement SBRIT models.
Navigating industry challenges
The ongoing effects of the COVID-19 pandemic have continued to cause workforce shortages to be a crisis within the mental health field. According to the Bureau of Health Workforce, more than half (169 million) of the U.S. population lives in a Mental Health Professional Shortage Area, as of December of 2023. The National Council for Mental Wellbeing addresses these disparities by leading the delivery of capacity-building research, resources, and tools to advance workforce development nationally and advocate for supportive policies at the federal and local levels.
diagnosis or insurance status. The National Council’s consultants help mental health and substance abuse organizations meet the CCBHC requirements defined by SAMHSA and the state through finance, service delivery, and partner collaboration assistance.

The National Council raises awareness about health care inequities and provides members with comprehensive support to tackle health equity issues.
The organization’s workforce development goals also include the education and training of current and future members of the mental health treatment workforce. The National Council assists Certified Community Behavioral Health Clinics (CCBHCs), which are currently revolutionizing behavioral healthcare and strengthening health services. CCBHCs are specially designated clinics with the funding and framework to offer mental health services regardless of someone’s
Mental wellness priorities
Ongoing efforts to support the mental health and wellness industry include The National Council’s Mental Health First Aid (MHFA) program, which teaches individuals and organizations how to assist and support patients that may be experiencing a mental health or substance abuse challenges.
Through enrollment in an early-intervention course administered virtually or in-person by the National Council, participants
learn the skills needed to recognize and respond to the signs and symptoms of mental health challenges. The course covers common signs and symptoms of mental health and substance abuse challenges, how to interact with a person in crisis, and how to connect a person with help, as well as expanded content on trauma, substance use, and self-care. The training also provides resources on how all people can provide an individual with initial mental wellbeing support, until the individual can find appropriate professional help.
The organization additionally provides dynamic programming to build public health’s capacity to address persistent health disparities in the industry. As an organization, The National Council raises awareness about health care inequities and provides members with comprehensive support to tackle health equity issues.
Webinars, tools, and other resources on health equity are aimed at supporting mental wellness organizations in addressing racial inequities and associated stigmas leading to mental health and substance abuse treatment disparities. The goal of this training is to advance health equity in integrated care settings and expand access to comprehensive, coordinated mental health care.
The National Council’s proposed actions related to health equity include advancing policies that bolster substance use disorder prevention, care, and recovery, protecting and growing funding for mental health awareness training programs, expanding access to telehealth, and more; all with the goal of working toward ensuring mental wellbeing as a reality for everyone.



On the Move
How providers aim to improve healthcare accessibility with mobile clinics.
By Pete Mercer
 As the healthcare industry continues to evolve, providers need to be prepared to evolve with it. One of the most recent evolutions in the delivery of care is the mobile health clinic, a sort of ‘clinic-in-a-car’ approach to providing patients with the care they need. Motor vehicles, ranging from large vans to buses, are outfitted and resourced with all the tools necessary to act as a care delivery system on wheels.
This innovative turn is a solution for several hot button issues facing the industry. Increasing accessibility is a significant pain point for the entire healthcare industry – many patients are
stranded in healthcare deserts without a consistent or reliable mode of transportation to get to their doctor’s appointments. Another significant pain point is the financial aspect of receiving
care – exorbitant inflation rates are making spending money on preventive care less likely, while others are struggling to make payments to manage their chronic illnesses. This wide spectrum of
healthcare challenges is where the mobile clinic can thrive.
Mobile clinics provide a simplified healthcare solution that allows patients to receive convenient, affordable, and timesaving patient-centered care. These clinics offer services like health screenings, immunizations, minor injury treatment, and sick visits to community members that might not otherwise have access to the quality healthcare services they deserve. Organizations like HealthWorks, The Mayo Clinic, and many others are branching out to create a more accessible and affordable system for their communities.
What are mobile clinics?
Mobile health clinics are customized vehicles that travel to communities to provide a wide range of health services. These clinics are typically staffed by physicians, nurses, community health workers, or other health professionals. These units are designed to help provide care to underserved communities, helping these patients overcome many barriers in the way to accessing the care they need. There are so many patients in the United States who lack access to basic healthcare because of barriers like time, geography, and trust, making innovative healthcare
trends like mobile clinics such a unique opportunity for underserved communities.
NPR reported in 2023 that the number of mobile clinics on the road has grown since 2019. “Many were used for COVID19 testing and vaccinations. And health and community centers started using mobile units to bring primary care, behavioral health, and reproductive services to outof-the-way patients.”
At the beginning of 2024, the MOBILE Healthcare Act went into effect, allowing health centers to use federal funds to establish mobile healthcare for their communities, which would increase
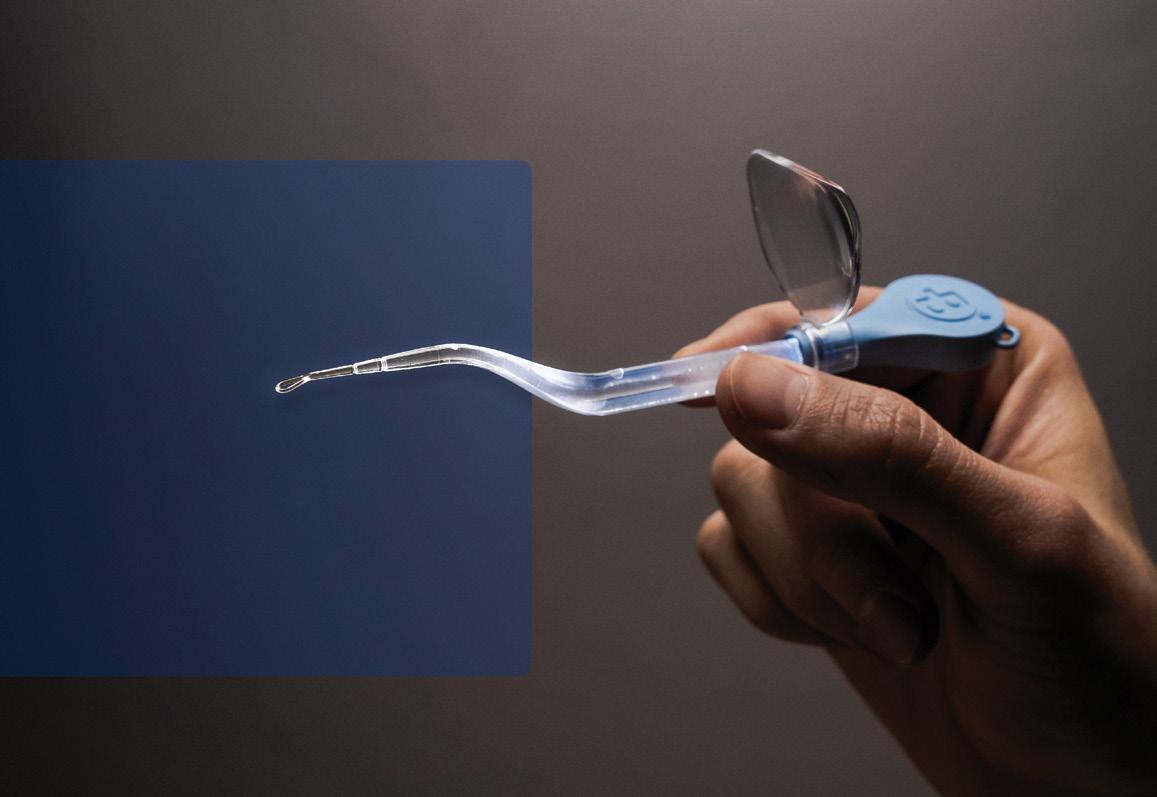
Unlock Profit Potential

access to medical services for any underserved areas.
Congressman Richard Hudson, one of the architects of the original bill, said in a media release, “The MOBILE Health Care Act is critical to improve health care quality and access across our country, especially in rural and underserved areas. I have heard directly from community health centers in North Carolina and across the country about the positive impact this bill and the flexibilities it provides would have on communities and patients.”
Reducing healthcare costs
In addition to breaking down any barriers that patients might face in receiving patient care, mobile health clinics often provide care at a lower cost than traditional healthcare delivery modes. According to Mobile Health Map, a network of mobile clinics that work together to advance health equity, for every
$1 spent on mobile health, $12 are saved, resulting in a return on investment of 12:1.
Patients who use mobile clinics can receive cost-effective preventative care, which can reduce the amount of care those individuals will need over their lifetime, while also reducing expensive emergency room visits in the event of an emergency.
Because the goal of mobile clinics is to increase accessibility, healthcare organizations can use these clinics to specifically target uninsured patients, low-income patients, rural patients, and even patients who are homeless. Additionally, they can be used to increase primary care and wellness checks for public schools and local businesses, which would allow students, teachers, and employees of the businesses to receive a wellness check without taking the time to travel and wait at a primary care facility.
HealthWorks, a Wyomingbased healthcare provider, has a
Mayo’s Mobile Health Clinic
Mayo Clinic Health System’s Mobile Health Clinic includes two exam rooms, an on-site laboratory and telehealth equipment connecting patients to Mayo Clinic providers for care.
It provides preventive health screenings, chronic disease management and community partnerships.
Services include:
` Acute illness/infection
` Anticoagulation/INR checks
` Chronic disease checks
` Immunizations
` Pacemaker checks (virtual)*
` Pediatrics*
` Preventive services
` Specialty consults (virtual)*
` Sprains and fractures — If casting or imaging (X-ray/ CT/MRI) is required, you may be referred to a brick and mortar facility*
` Wellness visits
pilot mobile clinic program that brings services like sick visits, minor injury treatment, and well-child exams to public school in the Cheyenne area. Monica Woodward told The Cheyenne Post that students in this district will be seen by the mobile clinic, regardless of their ability to pay.
She said, “We know that lack of insurance prevents parents from seeking care that is needed. HealthWorks serves all patients regardless of ability to pay. We want all kids to achieve optimal health and will serve as a resource for them.”
The HealthWorks mobile clinic does not replace required school health services for Free Appropriate Public Education (FAPE), but instead provides support, according to the company. It also does not replace parents/ guardians, school nurses, school counselors, pediatricians, or other existing services. Services are determined at the local level and in accordance with state and local policies and/or law.
Getting out in the community
The opportunity that mobile clinics present for demographics like school-aged children is huge. The Cheyenne Post covered a partnership between HealthWorks and the Laramie County School District 1 to provide physical and behavioral health services to students, faculty and staff. “We are excited to have this one-of-akind mobile service available for our students, faculty and staff,” Superintendent of Schools Dr. Margaret Crespo said to The Cheyenne Post. “The main goal is to focus our work on bringing partnership and opportunities for our students and families as
outlined in our strategic plan through community engagement and healthy environment.”
With visits lasting 30 minutes or less, HealthWorks is working to provide a better option for students and teachers with time constraints, while relieving the parents the burden of taking time off from work.
Improving accessibility
A huge component of improving accessibility is meeting the needs of those who use the largest amount of healthcare services in the United States: adults 65 and older. As patients get older, they will invariably need access to
healthcare more often, but those in rural areas have fewer options for transportation.
Chronic disease is particularly prevalent in older patients, necessitating frequent healthcare visits to monitor health and mitigate further issues. Diabetes, heart disease, hypertension, and cancer are all chronic illnesses that require constant medical surveillance. For the elderly, this becomes even more complicated as their own physical mobility suffers – past a certain age, many are not even driving themselves to their own doctor’s appointments.
The Mayo Clinic Health System Mobile Health Clinic saw a
Experience the Blickman Difference
significant need in their elderly patients. “I’ve always been focused on opportunities to create access to care, especially in these small communities. Essentially, we’re traveling to people’s doorsteps and providing high-quality, patient-centered care,” Emily Majerus, a Family Medicine PA at Mayo Clinic in Austin, Minn., said. “Patient compliance increases when you make care so convenient. I can see them on Tuesday and follow up with them on Thursday. The mobile clinic functions just like my brick-and-mortar clinic in Austin. It just has more wheels and windows.”

ADAPTABLE WORK AND PREP SURFACES
Our specialty back table is designed to provide additional room for extensive surgeries which require a wide array of equipment and instruments. Height adjustment from 46-49” is achievable with either pneumatic assist or manually. The top tier ‘hide-away’ shelf is angled for easier instrument viewing and access and holds multiple trays. Tables have sanitary closed tops to prevent bacterial build up and sealed reinforcing channels which provide rigidity and durability. Sealed casters eliminate corrosion and each supports up to 400 lbs.
For more information on what we can do for you or to request a quote, contact us today! info@blickman.com • (800) 247-5070







Our extensive line of tables includes adjustable, instrument and stationary models with several available in MR Conditional. www.blickman.com


The Dangers of Screen Time
Pediatricians are raising the alarm on the negative effects of screens and online media on children’s health.
 With the rise of social media and sophisticated and targeted online advertising, screen time has become increasingly engaging and pervasive, said Natalie D. Muth, MD, MPH, RDN, FAAP, FACSM. Screentime has greater risk to negatively impact the knowledge, attitudes, and beliefs of children and adolescents as well as their behaviors.
Screen time and media use can be harmful in a few ways, said Dr. Muth. These include:
` Sedentary time spent on screen and media can displace time that could otherwise be spent engaging in physical activities
like outdoor play or sports, for example.
` Screen time is often when mindless eating and snacking occurs, contributing to worsened nutrition.
` Advertisements and other screen time exposures have been shown
to negatively impact nutrition and food choices.
` Growing research shows the potential negative effects of social media and screen time exposure on a child and adolescent’s mental health and well-being.
“Not all screen time is harmful, but it is important to consider potential risks and benefits and monitor screen time activity and usage carefully,” said Dr. Muth, who is a spokesperson for the American Academy of Pediatrics, primary care pediatrician and obesity medicine specialist in the WELL Clinic at Children’s Primary Care Medical Group in San Diego.
Currently, families and social media may harbor myths or misinterpret definitions of “healthy.” Pediatricians and other primary pediatric health care providers have a crucial role in helping to promote lifestyle factors beneficial for the health of children of all weights, shapes, and sizes.
Environmental triggers
Screen time is one of several pitfalls to healthier lifestyles for children growing up in today’s society. Alarmingly, few children and adolescents meet federal nutrition or physical activity recommendations, according to “The Role of the Pediatrician in the Promotion of Healthy, Active Living”, a clinical report published this year by the AAP. The report updates recommendations last made in 2015 and overviews ways to lower risks of illnesses such as obesity or disordered eating.
The AAP states that practical strategies to promote healthy, active living are urgently needed. “Few children and adolescents meet federal recommendations for nutrition or physical activity, and rates of poor or inadequate sleep, negative health effects from screen use and social media, and mental health concerns in children and adolescents have increased,” researchers said in
the report. Childhood obesity and disordered eating, including binge eating disorder and atypical anorexia nervosa, remain complex biopsychosocial illnesses with many genetic, environmental, and social drivers; healthy lifestyle remains an important component of both prevention and treatment, the APP said.
“ We are most likely to make healthy ‘recommended’ choices when the healthy choice is the easy choice. The environment in which we live makes it challenging to eat a diet rich in whole grains, fruits and vegetables and low in ultra-processed, sugary/ salty foods. At the same time, for many kids the built environment makes it challenging to reach the recommended 60 minutes of physical activity per day.”

“We are most likely to make healthy ‘recommended’ choices when the healthy choice is the easy choice,” said Dr. Muth, lead author of the clinical report. “The environment in which we live makes it challenging to eat a diet rich in whole grains, fruits and
vegetables and low in ultra-processed, sugary/salty foods. At the same time, for many kids the built environment makes it challenging to reach the recommended 60 minutes of physical activity per day. If we are serious about supporting kids and families in achieving good health and meeting nutrition and activity guidelines, we need to make the healthy choice the easy choice.”
Difficult discussions
According to the Centers for Disease Control and Prevention, approximately 1 in 5 U.S. children and adolescents have obesity. During childhood, obesity can put children at risk for physical conditions such as type 2 diabetes, high blood pressure, and liver disease, and psychological conditions such as bullying, low self-esteem, and anxiety. Young children who are overweight in kindergarten are four times more likely to have obesity by 8th grade than those who are not overweight in kindergarten. If current trends continue, the CDC forecasts that by 2050, the majority of today’s children and adolescents (57.3%) are projected to have
obesity by age 35. “Action is needed so our children grow up healthy and strong,” said Dr. Mitch.
Obesity has an impact on medical costs. Compared to children with healthy weight, the CDC estimates that total medical expenditures for children with severe obesity are $909 higher each year. Despite all these warning signs, obesity is difficult to discuss with younger patients and their families for several reasons, Dr. Muth said. One is a long-standing
Key factors
stigmatization and weight bias. This includes a “blame” mentality. There is also risk of negatively impacting a child’s self-esteem and body image or having the discussion in a way that prompts a child or adolescent to engage in dieting or other harmful behaviors.
“People come in all shapes and sizes and one is not necessarily better than another, and there is a strong genetic or inherited component of body size,” Dr. Muth said.
In an article for healthychildren.org, Dr. Muth listed the following things that affect a child’s health and weight:
Nutrition. Setting regular meal and snack times can support healthy weight. Another key: having healthful foods such as fruits, vegetables and whole grains on hand while minimizing highly processed foods and sugary drinks.
Physical activity. Kids need physical activity built into every day –whether that’s playing sports, playing outdoors, helping with family chores, walking or biking to school, engaging in physical education, taking a family walk or any other physical activity they enjoy.
Sleep. When kids (and adults) don’t get enough sleep, their bodies release stress hormones to help them get through the day. These biological patterns affect appetite and the way our bodies burn (or store) excess calories.
Healthy tech use. This issue is closely related to sleep, since screen time before bed disrupts sleep cycles. But it’s also a factor in making time for healthy activities that get us moving.
Emotional and social issues. Feeling loved, seen and appreciated are just as central to your child’s health as nutrition and exercise. The brain and the body are one system – so when kids feel safe and secure, their bodies function well.
Scan the QR code to read the full article.
Health is the primary focus. While health risks can be associated with obesity, they do not necessarily go hand in hand. “Also, many environmental factors that are outside of a child’s control can impact behaviors,” Dr. Muth said. “This is complicated and complex, making discussion on an individual level more challenging, as the many social determinants of health play a powerful role.”
The pediatrician’s role
Dr. Muth believes pediatricians are a trusted source of information and guidance. They see children frequently over a long period of time and are best positioned to monitor growth trends, identify challenges, and sensitively and credibly speak with a child and family in exploring strategies to help optimize a child or adolescent’s health and well-being. They also provide recommendations based on science which is particularly important in this day of misinformation and rampant sharing of bad and potentially harmful advice.
Practitioners must communicate in a way that is sensitive and supportive with a focus on health. This includes listening to understand where a child and family currently are, what their goals or desires are, and working together to develop a plan that supports healthy, active living across domains of nutrition, activity, sleep, screen and media use, and social emotional wellness. It also includes advocating for community and environmental changes that help support the healthy choice as an easy choice.
“This takes into account social determinants of health and where a child or adolescent lives, learns, and plays,” Dr. Muth said.
ZOLL AED 3 ®

Real CPR Help®
Proven Real CPR Help guides rescuers in delivering high-quality CPR consistent with current guidelines. Real-time feedback on depth and rate of compressions is displayed on the enhanced colored bar gauge.

SMART. READY. TRUSTED.

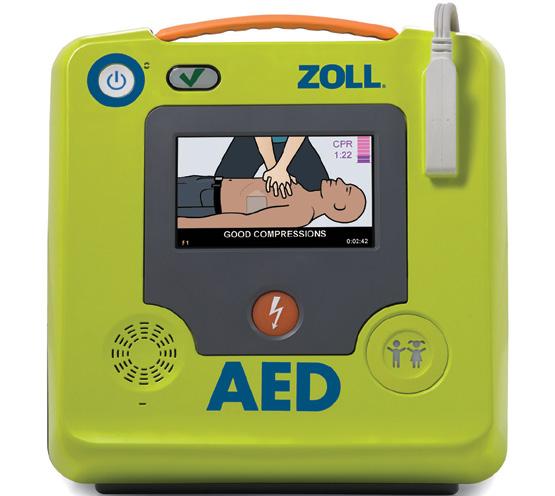
Long-life Consumables
Five-year battery and pad life means fewer replacements and the benefit of the lowest total cost of ownership.
Integrated Pediatric Rescue
The universal design of the CPR Uni-padz™ electrodes gives rescuers a single, versatile solution for both adult and pediatric victims of SCA.
“QUICK! GRAB THE ZOLL!”
Mission Focused
Our AED technology innovations provide rescuers with the tools to act quickly and confidently to help save lives.
Legacy of Excellence
A pioneer in resuscitation technology, ZOLL has been empowering first responders and unexpected heroes around the world for more than 25 years.

Facing Healthcare Challenges Headfirst
Supply chain leaders share how they are tackling industry issues with forward-thinking solutions.
By Pete Mercer
 The challenges the healthcare industry faces daily are nothing new – anyone who works in healthcare can tell you it comes with the territory. No challenge is insurmountable though – it’s all about finding creative ways to face those challenges headfirst.
At the Association of National Account Executives Annual Conference, Brent Petty moderated a conversation between Dameka Miller, VP, Strategic Sourcing for Trinity Health, and John Dockins, Executive Director, Strategic Sourcing for Cleveland Clinic, discussing the major challenges and issues facing the various stakeholders in today’s healthcare market.
The ANAE Annual Conference provides an opportunity for ANAE members and prospective
members to network with their peers and customers, while hearing from leading supply chain executives and GPOs on working successfully with IDNS.
Looming
cybersecurity threats
Cybersecurity attacks are becoming more and more commonplace in healthcare, revealing a frightening vulnerability in the care continuum. How are healthcare providers supposed to prepare for a cybersecurity threat?

Dockins said, “Cybersecurity threats are real – I think they are going to continue, and they are definitely on the rise. I think we must solve this one together, between us all in this room, suppliers, GPOs, and providers. Let’s get CISO’s talking, let’s get those information security people talking with each other. We need to open the dialogue about how we harden and secure the network across the spectrum.”
Creating that dialogue about securing healthcare networks could be a critical step towards avoiding cybersecurity disruptions. While some disruptions might only affect the financial services and payroll departments of healthcare providers, the most significant concern is a doomsday scenario that Dockins described later.
“I imagine this big red button that our CISO has access to when we are notified of a breach, and he pushes the red button and everything is cut off. Great. What if tomorrow that call comes in and says that patient monitoring is being affected? Can’t disconnect it. In the moment, you don’t know what the breach is. Is it a data
breach? Would it impact the actual software of the equipment? Would it start to manipulate monitoring results? How would we deal with that? I don’t know if there’s an answer to that. I still get chills to myself because what keeps me up at night is how to keep our patients safe during something like that.”
That scenario is something that has been top of mind for Trinity Health’s CEO, Miller said. They recently launched a cross-functional team that is challenging everyone to imagine a scenario like that and how they can best respond to it. “We already have a separate IT system set up, so if there’s ever something that attacks our system, it’s going completely offline.”
Implementing artificial intelligence
Artificial intelligence is one of the hot-button issues across the board, but the potential of implementation in the healthcare space is an interesting exercise in simplifying processes throughout the care continuum. Miller discussed how her team is using artificial intelligence to improve their outcomes by taking over those routine tasks.
“We have a version of AIinformed bots that are doing the work in our procurement and accounts payable teams,” Miller said. “We’ve been able to program routine tasks so that two bots are able to do the work for about 10-plus FTEs now. We are also excited about the implementation of a contract life cycle management system with AI built into it, which will give us a better idea of how reimbursement and what we’re paying to the supply chain side are matching up. Finally, my team is using ChatGPT for third-party research.”
Dockins is looking to artificial intelligence for real-use cases in large language models. “It’s just taking massive amounts of data from multiple systems and putting it in one giant pot to predictably tell you what is happening or going to happen for things like different reimbursements by geography, demand planning, planning for backorders and allocation, and real-time inventory tracking.”
positive or negative, the wound council is going to look at it and figure out if that’s the best thing for us to do because sometimes the low-cost solution is not always the best solution.”
The pandemic made the supply chain famous, bringing people like Miller and Dockins out of the basement and into critical conversations with the C-suite. That brings plenty of opportunities to
Value analysis is a set of techniques, knowledge, and skills used to improve the value of a product by eliminating unnecessary costs or improving its functions without compromising its quality, reliability, and performance.
The role of value analysis
With a value analysis team, providers are equipped with the knowledge and resources they need to make better decisions on the supplies and products that the hospital purchases. Value analysis is a set of techniques, knowledge, and skills used to improve the value of a product by eliminating unnecessary costs or improving its functions without compromising its quality, reliability, and performance.
“At Trinity, we have what we call a clinical framework,” Miller said. “We have a clinical framework team that has oversight of, for example, wound care, and we have representation from across the country to weigh in on woundtype decisions. Our value analysis team is plugged into that, and they are tasked when something is new and emerging in the market. What’s the clinical evidence? What’s the reimbursement? What’s the potential cost impact? And
improve efficiency and identify challenges in front of the major decision makers in the hospital, but it also creates an environment with more oversight on all the decisions that need to be made.
Dockins said, “If we look at the inpatient floors, I think we’d all agree that nurses are consistently stretched thin. They’re asked to do more, there’s fewer of them. We could probably spend the rest of the day talking about that challenge. However, traditionally, account executives have resources within your organization that you could apply and potentially come and put them on the floor for a temporary time basis and help us figure out if there is a better way, right? That’s where I think value analysis could go. That’s where we’re trying to push it. Yes, we’ll look at clinical evidence, yes, we’ll look at reimbursements – but how do we look at outcome data?”

Get the Picture
Diagnostic medical sonography plays a key role in better clinical outcomes for patients across a wide array of health conditions.
By Jenna Hughes
 Ultrasound (sonogram) is the most utilized form of diagnostic imaging available after X-ray, according to the Society of Diagnostic Medical Sonography (SDMS). Doctors order ultrasounds for women, men, and children to gain insight into the inner workings of the body.
As such, sonographers play an indispensable role in modern healthcare by utilizing ultrasound technology to create images of the body’s internal structures, said Mitzi Roberts, president of the Society of Diagnostic Medical Sonography and SDMS Foundation
Board. “Their expertise in capturing detailed images allows physicians to diagnose and monitor a wide range of conditions.”
Using ultrasound, physicians can monitor women’s health conditions, gynecological problems, and heart conditions, while limiting
invasive procedures. In men, ultrasound can diagnose everything from heart disease to abnormalities in the prostate gland or testicles. In children, doctors can use ultrasound to detect illnesses and disorders such as appendicitis or spina bifida.

Ultrasound does not use ionizing radiation, making it a safe option for imaging. “The skill and dedication of sonographers ensure that healthcare providers can offer the highest standard of care to their patients,” said Roberts.
Ultrasound is a science built around sound waves. Ultrasounds, or sonograms, should be performed only for diagnostic purposes. During a sonograph test, a sonographer places a small device known as a transducer against the patient’s skin on the area of the body being scanned. The transducer then sends high frequency sound waves into the body, which bounce off its internal structures. From there, a computer analyzes the sound waves and creates visual images of the patient’s
body, providing physicians with valuable medical information.
Heart disease, stroke, abnormalities in the abdomen or reproductive system, gallstones, liver damage, and kidney function all exhibit telltale signs that ultrasound helps detect, according to the SDMS.
Industry challenges and advocacy
In recent years, sonographers have faced workforce shortages, continuous learning and adaptation with technological advancements, increased workloads and patient volume, resource constraints, patient safety, emotional and physiological stress, and more.
“As the demand for their expertise grows, sonographers face a variety of issues that impact their ability to deliver optimal care,” said Roberts.
The organization represents the sonography profession’s interests through advocacy initiatives at both the federal and state level. This includes sonographer credentialing, state licensure, coding and reimbursement, and more.
“Advocacy is at the heart of the SDMS’ mission,” said Roberts. “On the legislative front, the SDMS engages with policymakers to ensure legislation reflects sonographers’ vital role in healthcare, to protect their scope of practice, and to ensure that sonographers meet rigorous education and competency standards to safeguard patient safety.”
“The SDMS also engages in professional advocacy by educating the healthcare community on the critical role sonographers play in patient care,” said Roberts. By setting industry standards and advocating for continuous professional development,
Sonographer certification is considered the standard of care. Currently, New Hampshire, New Mexico, North Dakota, and Oregon are the only states with approved requirement of licensure for sonographers. Policies for sonography can be complex and may vary from state to state.
In 2024, the SDMS launched a new initiative to address sonographer workload and well-being. The goal of the SDMS project is to extract the lessons learned from plans that have been implemented to address sonographer workload and well-being, as well as create a toolkit for sonographers to utilize when creating similar plans in their own facilities.
the SDMS helps sonographers stay at the forefront of technological advancements and best industry practices.
Sonographer education and credentialing
Healthcare employers are increasingly seeking demonstration of professional competence through sonographer certification. In the
field of sonography, an individual takes one or more certification exams to become certified for a specific area (abdomen, vascular, etc.), and the certification organization then awards a credential to the individuals that pass the examination.
Sonographer certification is considered the standard of care. Currently, New Hampshire, New Mexico, North Dakota, and Oregon are the only states with approved requirement of licensure for sonographers. Policies for sonography can be complex and may vary from state to state.
The SDMS, as a result, has developed the “SDMS Legislative Monitor App,” which tracks state and federal legislative bills related to sonography.
“One of the core initiatives of the SDMS and Medical Ultrasound Awareness Month (MUAM) is the safety and noninvasive nature of ultrasound, because it is a reliable, safe imaging modality that does not involve radiation, making it suitable for a wide range of patients,” said Roberts. “The SDMS actively advocates for licensure for sonographers to enhance the credibility of the profession.”
The SDMS also provides opportunities for individuals to earn continuing medical education (CME) while also providing educational resources for the sonography community. The SDMS allows members to earn CME credits, outlines sonographer CME requirements, and provides members with access to the SDMS CME tracker. SDMS also offers Clinical Reviews and career resources to professional sonographers, which are a collection of online resources designed
to enhance the knowledge, skills, and competency of those in the field.
Sonography awareness
Medical Ultrasound Awareness Month (MUAM) is held annually in October to increase awareness of diagnostic medical sonography, and the role sonographers play in healthcare. The key tenets of MUAM include promoting public awareness of sonography, highlighting the role of sonographers in healthcare, and emphasizing the safety and efficacy of sonography.
for sonographers, emphasizing patient care, safety, and the evolving role of sonographers in healthcare,” said Roberts.
The SDMS is also currently updating the Code of Ethics for the Profession of Diagnostic Medical Sonography, which aims to promote excellence in patient care by fostering responsibility and accountability among diagnostic medical sonographers. According to Roberts, The Code of Ethics serves as a guide and framework for addressing ethical issues in clinical settings, business practices, education, and research.
Using ultrasound, physicians can monitor women’s health conditions, gynecological problems, and heart conditions, while limiting invasive procedures. In men, ultrasound can diagnose everything from heart disease to abnormalities in the prostate gland or testicles. In children, doctors can use ultrasound to detect illnesses and disorders such as appendicitis or spina bifida.
Many organizations join the Society of Diagnostic Medical Sonography in promoting MUAM, including the American Institute of Ultrasound in Medicine, the American Registry for Diagnostic Medical Sonography, the American Society of Echocardiography, Cardiovascular Credentialing International, and the Society for Vascular Ultrasound.
Recently, SDMS worked on revising the sonography clinical document titled “Scope of Practice and Clinical Standards for the Diagnostic Medical Sonographer,” which “sets forth the most current standards and expectations
“MUAM seeks to inform the public about the critical role of ultrasound in diagnosing and treating medical conditions. By increasing awareness, the campaign helps people understand how ultrasound works, its safety, and its applications in various medical fields,” said Roberts. “MUAM is dedicated to recognizing and celebrating the contributions of sonographers. It emphasizes the expertise and skills of these medical professionals, showcasing their importance in the healthcare system and their impact on patient care.”
Workout your sales in the New Year!
PRECISE Selling Bootcamp
WHAT YOU WILL LEARN AT THIS BOOTCAMP:
Proven Sales Techniques:
Learn and apply the PRECISE Selling methodology, a resultsdriven approach to sales that has been proven to increase performance and close rates.
Targeted Prospecting:
Master the art of identifying and reaching out to high-potential leads in the medical industry.
Effective Communication:
Develop skills to communicate complex product information clearly and persuasively.
Please join Repertoire Magazine’s PRECISE Selling Bootcamp on December 11-12, 2024 in Fort Worth, Texas! This meeting is designed specifically for professionals in the medical manufacturing industry.
This intensive day and a half training program will equip your team with the skills and strategies needed to excel in today’s competitive market.
Overcoming Objections:
Gain strategies for handling objections and turning them into opportunities.
Building Relationships:
Learn how to establish and maintain strong, long-term relationships with healthcare professionals and decision-makers.

Scan QR Code to Register
Care Outside the Hospital Walls
A new hope, or slippery slope, for supply chain?
By R. Dana Barlow

Editor’s note: This article originally appeared in The Journal of Healthcare Contracting, a sister publication of Repertoire Magazine.
 Before the turn of the millennium many either feared or desired the term “alternate site” in the healthcare market.
Those who feared it generally worked in acute care settings, nervous that these non-acute care facilities would siphon all the revenue-generating patients away, which would leave the hospitals with only
the sickest patients consuming resources that would place financial operations and jobs in jeopardy.
Those who desired the term generally saw those facilities as a way to gain a competitive advantage and
to control clinical pathways within the emerging integrated delivery networks (IDNs) that defined a reforming industry. Not surprisingly, the feared became economic prey for the desired.
For supply chain executives and professionals, the term represented an expansion of responsibilities, mindsets, duties and accountability – and a raft of inherent and ongoing challenges in terms of strategic sourcing with value analysis, contracting and distribution of products and services, regardless of their affiliation with or ownership by hospitals, hospital systems or IDNs.
For context, non-acute or remote care comprises ASCs, clinics, physician offices, diagnostic imaging centers, freestanding laboratories, urgent care facilities, retail clinics, home health programs and hospital-at-home programs.
Sidestepping the sin-bin
Not surprisingly, hospitals attach a greater importance to supply chain operations due to the volume and value of products and services brought in and recorded on the expense side of the balance sheet. But it needs to be standardized and unified for optimal budgetary and economic advantage, sources recommend.
“In the acute care environment, understanding and optimizing supply expense is a focus for most IDNs,” Paul Oppat, executive director, Supply Chain Services, at Phoenix-based Banner Health, said “The preponderance of their supply expense occurs in their hospitals. However, outside of hospitals and ASCs, supply expense is often not a high priority. Optimizing the supply chain is a team sport and we are working to energize additional focus in this area.
“Outside the hospitals, logistics and administrative costs impact a higher percentage of the supply spend due to
the nature of smaller and often frequent ‘last-mile’ deliveries,” Oppat continued. “With this in-mind, our challenge is to create supply chain replenishment models that are easy for people who are not supply chain experts, and balance service needs with transaction cost.”
Staffing/support model and ordering/item master management represent two key hurdles in the non-acute space, according to Atanas Ilchev, system director, Supply Chain Operations, UChicago Medicine.
“In our early stages of nonacute facilities expansion we had to figure out a staffing model that is flexible enough to support low-volume facilities,” he indicated. “This was a real challenge given the fact that neither hospital supply chain nor our partners/distributors were ready to assist with our staffing needs for non-acute facilities. The second challenge is related to ordering controls as the non-acute facilities are not on the main ordering platform/ERP (enterprise resource planning) system. This could lead to multiple nonapproved products penetrating facilities causing supply expenses to continuously increase and potential compliance issues.”
Ian O’Malley, executive director, Strategic Sourcing, UChicago Medicine, points to non-acute care sourcing and transactions knotting the value analysis process as well as relationships with clinicians outside of hospital settings.
“In our VA process we incorporate revenue cycle and finance data into our total cost of care analysis before a device or technology is approved,” he said. “The different reimbursement models
and acquisition cost models for the same technology across these sites of care has challenged us to refresh and update multiple models for each device/technology. While a technology may be approved for one site of care, it may not make financial sense in other sites of care, so we may have to work with our clinicians to identify alternative approaches to treatment that provide clinically equivalent outcomes. Our group does push back strongly where costs are different by site-of-care as companies need to adjust their pricing strategy to take into account the growth of this market segment, so organizations don’t have to maintain multiple price points that create item master and invoicing issues downstream.”
Cost and accounting pressures may ease a bit now that UChicago Medicine has converted all its non-acute care sites to the IDN’s unified ERP and inventory management system, according to Eric Tritch, senior vice president and Chief Supply Chain Officer. But geography inserts an additional wrinkle.
“Another factor that complicates the analysis is when you operate in multiple states, there are typically different rates from government insurance plans like Medicaid, so what might be financially viable in one region may lose money in another,” Tritch said. “Service providers are often also geographically located and cannot always service all sites, or many aren’t set up to support non-acute locations and certainly non-hospital at home, so as [Ilchev] mentions, our staffing models and partners have needed to evolve.”
Neil Allen, senior director, Spend Management and Administration, The University of Kansas Health System, Kansas City, Kansas, highlights the complexity behind supply chain operational planning when dealing with changing players, processes and procedures.
“It is challenging to establish the right long-term strategy in an ever-evolving landscape,” he acknowledged. “A strategy that is not scalable and does not evolve will inevitably introduce rising supply costs and inefficient operations. Standardization across all areas of care can also pose a challenge, particularly as the nonacute space continues to grow at a rapid pace. Without a structured approach, supply standardization and ease of operations become increasingly difficult. The impact of classes of trade can also be a struggle due to the added cost and the potential to create a more complex distribution network. As the non-acute space continues to grow, multifaceted operations and the rise of additional costs will greatly affect outcomes.”
Pursuing hat tricks
As roiling budget and labor/staffing issues mount, supply chain operations must bob and weave around hurdles and speed bumps to fulfill their expansive duties, sources concur.
For The University of Kansas’ Allen, supply chain needs to make it about the patients first and supported by technology second.
“Establishing clinically integrated teams that align with both the clinical and patient aspects is critical,” he noted. “These multi-disciplinary teams can help ensure strategies and decisions

“ Outside the hospitals, logistics and administrative costs impact a higher percentage of the supply spend due to the nature of smaller and often frequent ‘last-mile’ deliveries. With this in-mind, our challenge is to create supply chain replenishment models that are easy for people who are not supply chain experts, and balance service needs with transaction cost.”
– Paul Oppat, Banner Health
remain clinically focused. Another important aspect is establishing key metrics that can be used to improve operations, reduce supply costs and ensure off-formulary and off-contract supplies are visible and managed. Furthermore, ensuring value analysis and contractual opportunities are not confined to all discussions and negotiations across all areas of care is essential.
“Providing technology to support supply management allows clinicians to remain focused on patient care and less on supply chain activities,” Allen continued. “Automation and simplifying supply ordering, backorder management, sub-processing and other workflows is essential in reducing labor costs.”
Banner’s Oppat encourages supply chain to demonstrate as well as promote its importance.
“We need to educate stakeholders about the positive impact an optimized supply chain will have on their patients and their business,” he insisted.
“To quote Doug Bowen, Banner’s Chief Supply Chain Officer, the ‘the supply chain is everyone’s business’.”
Eric Helliker, Supply Chain Area Director at Banner, recognizes the variation that non-acute facilities bring to operations.
“We need to be flexible with our customers and understand that different parts of the continuum require different service levels. There is not a ‘one size fits all’ in the non-acute space,” he indicated.
“We need to develop close relationships with business partners
who can bring economies of scale to last-mile delivery where we may not be as efficient,” Oppat added.
UChicago Medicine’s Ilchev concentrates on the big picture of labor and the recruitment of service providers to assist when necessary.
“One creative method to address staffing needs at non-acute facilities that we have deployed successfully is partnering with a third-party vendor who is willing to adopt your standards and act as an extension of the supply chain department from the main acute facility,” he noted. “Also, we have partnered with our distributor to meet staffing needs as well. Both of these solutions come at a cost as flexible and highly trained
personnel are needed at non-acute facilities. In addition to that, for a well-organized non-acute support program to work, one needs to address the overall departmental structure to maintain standards, service levels and meet the needs of clinicians.”
Structured process granularity likely will make the most difference, Ilchev insists.
“The best method to introduce control over supply ordering is by implementing formularies and regular review of supply spend for each of the non-acute facilities to ensure compliance to formulary and control over supply spend,” he added.
Still, UChicago Medicine’s O’Malley urges supply chain leaders


to stand firm on departmental and organizational objectives, using technology as an enabler.
“Contractually we push our suppliers for one price point for our system regardless of site of care,” he said. “In rare situations where we can identify the need for disparate pricing our group can accommodate but this adds
costs to the contracting and item master maintenance work long term, so a strong justification is needed. We have also partnered with IT to begin enabling more remote support capabilities from our suppliers –think ‘telesupport.’ These technologies allow the rep to virtually enter the room and provide

support/guidance as needed, thus reducing the costs to support multiple sites of care and allowing them to patch into multiple procedures across the system –the same as if they would be on site at our large acute location.”
Such a philosophy drives the suppliers and vendors with whom UChicago Medicine chooses to work, according to Tritch.
“We are also cultivating partners that can be flexible for smaller facilities,” he said. “One resource needs to wear many hats, and the closer to the home, the more hats they need to wear. We are developing processes and technology that keep these flexible providers or caregivers from having to be experts in things outside their domain and focus on making things easy and automated to provide the supplies and services needed for care.”
Lighting the lamp
From dedicated teams to product formularies to standardization, IDN supply chain leaders have implemented processes to smooth out the kinks and rough edges that defined the boundaries between acute and non-acute facilities in the past.
“We have invested in a small team of talented supply chain professionals who focus on the non-acute supply chain full-time,” said Banner Health’s Oppat. “They ensure a positive customer experience while partnering with key stakeholders to improve supply chain performance.”
From people to products, supply chain sets and implements standards, according to Hollie Gallagher, Banner Health’s Supply Chain Services senior program director.
IDN News
Intermountain Health expands partnership with Story Health
Intermountain Health, one of the nation’s premier not-for-profit health systems, announced an expanded relationship with Story Health, a digital health company transforming specialty care delivery, that will increase patient access to Intermountain’s nationally-recognized cardiology care across the health system.
The expansion follows a highly successful pilot program launched by Intermountain and Story Health in January 2023 for patients with a new heart failure diagnosis. Heart failure is increasingly prevalent and costly and is expected to grow by more than 25% by 2030, with a price tag that is expected to eclipse the $30 billion mark.
While there are enormous challenges, clear evidence demonstrates that the management of medical therapies for this population can significantly reduce morbidity, reduce hospitalizations, and improve quality of life. Specifically, getting patients on optimized medication, known as guideline directed medical therapy (GDMT), has been shown to increase life expectancy of heart failure patients up to five years and can reduce hospitalizations by more than 70%.
Using Story Health’s program, which utilizes a virtual and asynchronous care model, Intermountain Health patients enrolled in the pilot program experienced a significant clinical improvement, including an increase in achieving medication optimization (GDMT) – with 80% of those medication changes handled without a clinic visit.
AllSpire Health Partners selects Premier, Inc. as its National GPO Premier, Inc. announced that it has been selected by AllSpire Health GPO, LLC (AllSpire), a regional group purchasing organization (GPO), as its primary national GPO and to support AllSpire’s more than $3.5 billion in annual GPO purchasing volume. Premier will leverage its scale and actionable data to evaluate products and services – and support the continued development of a best-in-class contract portfolio to drive efficiencies, economic success and high-quality patient care for AllSpire Health GPO members, their patients and the communities they serve.
Under terms of the agreement, AllSpire Health GPO members that comprise 54 acute care hospitals with more than 12,200 licensed acute beds will be Premier GPO members and
fully utilize Premier’s national contract portfolio. Premier will further support the development of AllSpire’s regional contract portfolio for categories where local market dynamics drive optimal value and service.
Mayo Clinic to expand Hospital Rehabilitation Care
Brooks Rehabilitation, a leader in treating patients after life-altering brain injuries, spinal cord injuries, strokes and other complex conditions, will open an inpatient rehabilitation hospital on Mayo Clinic’s Phoenix campus. Brooks Rehabilitation has been ranked by U.S. News & World Report as the No. 1 rehabilitation hospital in Florida and top 20 in the nation, and the new hospital will join Brooks’ network of three existing inpatient rehabilitation hospitals in Florida.
The rehabilitation hospital will reside on eight acres adjacent to Mayo Clinic’s Phoenix hospital, near the Arizona State University Health Futures Center. The estimated $70 million project will begin construction in December 2024 with a projected opening in summer 2026. Plans include a three-story, 80,000-square-foot hospital with 60 private patient rooms and the ability to expand as demand for services increases. The new hospital is expected to add more than 200 jobs to the market at full maturity.



A Worthwhile Cause
Owens & Minor Foundation, HOPE partner to support U.S. service members and military families.
By Pete Mercer
 The Owens & Minor Foundation and Hope for the Warriors (HOPE) announced a collaboration that would support HOPE’s clientele – active U.S. servicemembers, veterans, and military families. Through this partnership, Owens & Minor has an opportunity to come alongside HOPE and serve those who have served our country.
“A core part of The Foundation’s work is empowering our teammates by supporting causes that align with our mission and represent their unique perspectives,”
Owens & Minor Foundation president Faith Cristol said in a media
release. “We are excited to partner with an organization like HOPE, whose tireless efforts to help improve the lives of servicemembers and their families are a perfect reflection of The Foundation’s goal of building healthier communities.”
How the partnership will work
The Owens & Minor Foundation collaborates closely with the Owens & Minor Teammate Resource Groups (TRGs) to align with causes that are important to the members of the Owens


& Minor team. At Owens & Minor, each TRG provides space, resources, and support for underrepresented identity groups to develop goals that will help propel the Teammate and the organization forward. Through ongoing events and outreach, each TRG provides unique opportunities to connect and foster community across the company. All are welcome to join any TRG as a member or an ally.
Addressing critical needs
Owens & Minor has been proudly supporting active members of the military, veterans, and military families since the day it was founded.
In a statement, the Owens & Minor Foundation said, “Supporting our veterans and military families is core to who we are, and this initiative is a natural extension of that commitment. We were drawn to HOPE because the programs directly address critical
The MVP Support team works with veterans throughout their post-military journey and connects them with new opportunities through HOPE’s programs and alongside HOPE’s strategic partners.
The Foundation will help to support over a thousand HOPE clients through two pathway programs: Hope’s Critical Needs Program and HOPE’s Military Veteran Peer (MVP) Support Program. The Critical Needs Program aids financially vulnerable veterans, families, and caregivers who were impacted by the 9/11 attacks, and the MVP Support Program provides crucial peer support and community building for veterans and their families.
Recently, the Veterans TRG supported a HOPE initiative called the Memorial Day 30X30 Challenge, encouraging Owens & Minor staff across the company to stay active for at least 30 minutes a day for 30 days. The initiative started in May and tracked 70,697 minutes of actives, generating almost $5,000 in contributions for HOPE.
needs of veterans and their families, from financial assistance to mental health support. It’s an initiative that is deeply personal for many of our teammates.”
While the financial aspect of this is a significant part of the partnership, the Owens & Minor Veterans TRG is actively providing opportunities for Owens & Minor staff to build community by sharing their time and talents to support HOPE’s mission.
HOPE’s MVP Support Program will put HOPE’s Military Relations Program Managers, who are trained in mental health first aid and peer support, in contact with a veteran or active service member in need. The MVP Support team works with veterans throughout their post-military journey and connects them with new opportunities through HOPE’s programs and alongside HOPE’s strategic partners.
MVPs also provide personal engagement and customized peer support and create a place of acceptance and community for veterans and their families whether virtual or in-person.
The Owens & Minor Veterans TRG
According to The Foundation, the Veterans TRG was a critical part of establishing this partnership. This group plays an important role in attracting, supporting, and developing those who have served in the armed forces.
The Veterans TRG is an essential resource for veterans and active members of the military who work at Owens & Minor, providing a welcoming and inclusive environment for veterans to transition into civilian careers and leverage their skills in leadership, collaboration and problem-solving.
Additionally, the Veterans TRG advocates for veterans and veterans’ causes on behalf of Owens & Minor team members and in local communities, as well as serving as a forum for active and former military service members to support each other. The TRG recently hosted a post-traumatic stress disorder awareness program for all Owens & Minor teammates, providing education about PTSD and promoting awareness of support programs and resources for those affected.
A representative from Owens & Minor said in a statement, “Ultimately, this initiative reflects the Foundation’s view that it is not enough to say, ‘thank you for your service.’ Through this collaboration, and the efforts of the Veterans TRG, we are backing up those words with action.”
Emerging Leaders
Build the future of our profession by nominating a medical supply chain emerging leader.
 Healthcare distribution is a dynamic and rewarding profession. Professionals in the healthcare supply chain are essential in optimizing the flow of goods, reducing costs, and improving the efficiency of healthcare delivery. The industry is rapidly evolving with advancements in technology and increasing focus on sustainability, offering continuous learning and growth prospects.
But it’s also much bigger than that, and much more personal.
Many of the people that I meet and work with in healthcare distribution are deeply committed to ensuring that when medical care is needed, the necessities of medical care are there. It is a purposedriven profession. For young people who want meaningful careers that impact their communities, healthcare distribution is a strong industry to consider.
We need more talented, passionate people working in the medical supply chain. And HIDA is working to find them.
Over the past three years, HIDA has been building out resources on workforce development in the medical supply chain. We have developed online resources at our webpage – jobs.hida.org where people can find jobs and internships at our member companies. And HIDA’s Job Board serves as an online application hub for our Medical Supply Chain Emerging Leaders program.
The Emerging Leaders program recognizes college students pursuing degrees in supply chain management and public health who have a demonstrated interest in working in healthcare distribution. This past February, HIDA selected our first-ever cohort of Emerging Leaders – recognizing 11 students from 5 different colleges and universities. These Emerging Leaders came from diverse backgrounds. They included first-generation college students, students who studied abroad, and those balancing their education with part-time employment. All of them had work experience in healthcare, transportation, or logistics. Many had experience in all three.
These Emerging Leaders were offered a complementary registration to attend HIDA’s MedSupplyChain conference in Florida. While at the conference, these students attended panel discussions about healthcare distribution, engaged in networking opportunities, and met with industry leaders. They learned about opportunities and challenges in the medical supply chain and brought a unique perspective to conversations.
This year, HIDA plans to expand our Emerging Leaders program by increasing the number of applicants and the number of colleges that are represented. We’d like you to help us do that. If you know of a
promising college student with a passion to help others and an interest in healthcare distribution, please send them to jobs.hida. org to learn how they can apply. You can contact either myself (ruthven@hida.org) or Chandler Mobley (mobley@hida.org) for more information.


Wyeth Ruthven, Director of Congressional and Public Relations, HIDA
The Emerging Leaders program recognizes college students.
Health News
Antibiotic resistance awareness
Antibiotic resistance is an evolving issue within the healthcare industry, with The Centers for Disease Control (CDC) estimating that more than 2.8 million antimicrobial-resistant infections arise in the U.S. each year. Antimicrobial resistance occurs when certain types of bacteria mutate, so that antibiotic medicines are not able to stop their growth. Antibiotic resistance results in bacterial infections being extremely difficult to treat, leading to serious health issues for hospitals’ patient populations and the community.
In July 2024, the CDC published “Antimicrobial Resistance Threats in the United States (2021-2022)”, highlighting new data showing that six bacterial antimicrobial-resistant hospitalonset infections increased by a combined 20% during the COVID-19 pandemic compared to the pre-infection period. Antimicrobial resistance peaked in 2021 and remained above prepandemic levels through 2022. The CDC has called for increased healthcare professional and community awareness of Antibiotic Resistance. The (CDC’s) Be Antibiotics Aware partner toolkit includes messages, social media content, and other resources related to antibiotic safety for healthcare professionals. Additionally, the CDC’s MyHealthfinder resources also guide individuals on using medicines safely and preventing infections when getting medical care
Proper antibiotic use protocol for healthcare professionals, according to the CDC, includes implementing systems to alert hospitals when patients have drug-resistant infections, reviewing and perfecting infection control practices, and ensuring that hospital staff have access to prompt and accurate lab testing for antibiotic-resistant bacteria.
Average hip, knee replacement patient may be getting younger
We often think of the typical joint replacement patient being a senior (aged 65 and older). However, knee and hip replacement is becoming increasingly common among younger adults with chronic joint pain, according to U.S. News & World Report.
Today, the average age of joint replacement surgery patients is 57 years old, according to the U.S. News & World Report and Dr. Richard Berger, Rush University Medical Center orthopedic surgeon. Younger age groups are typically less apprehensive with these types of procedures because they are looking to avoid life-long, debilitating knee and hip pain.
Nearly 28% of hip replacement procedures are now being performed on men and women younger than 55, according to research from the American Academy of Orthopedics’ annual meeting in 2023 and U.S. News and World Report. By 2030, people younger than 65 are expected to account for 52% of hip replacements and as many as 62% of total knee replacements.


Smart watch tracking and healthcare data
Many people track fitness and health metrics using a wearable smartwatch device. These types of devices have recently become an integral part of people’s health and fitness routines. Some wearable devices on the market can now detect health changes such as irregular heart rhythms, oxygen levels, blood glucose, sleep tracking, and more.
More than a quarter of the U.S. population wore a smartwatch (or other type of wearable, connected device) for health and fitness tracking in 2023, according to Insider Intelligence/eMarketer and CNN. By 2026, it is projected that more than 100 million Americans will be using a smartwatch or wearable device for fitness and health tracking.
CNN interviewed Dr. Leana Wen, an emergency physician and clinical associate professor
at George Washington University to understand more about the efficacy of smartwatches in tracking health data. According to Dr. Wen, smartwatches track fitness data such as steps per day, and they can encourage people to increase exercise time and walk more. According to CNN and Dr. Wen, a study published in March 2024 found that for individuals taking 9,000-10,000 steps per day, the risk of cardiovascular disease was lowered by 21%, and the chance of premature death decreased by 39%. So, wearables do promote healthier routines for many individuals.
However, Dr. Wen cautioned that smartwatches are not approved to diagnose heart attacks or other life-threatening conditions. If an individual has chest pain or any other symptoms of a heart attack or other heart condition, she advises that it is best to seek immediate medical
care, instead of relying on wearable devices. Smartwatches can help encourage healthy behavior, according to Dr. Wen, but it is important that this new technology does not replace medicalgrade monitoring equipment for necessary health tracking.
Sugar substitute erythritol may raise cardiovascular risk
New Cleveland Clinic research shows that consuming foods with erythritol, a popular artificial sweetener, increases risk of cardiovascular events such as heart attack and stroke. The findings, from a new intervention study in healthy volunteers, show erythritol made platelets (a type of blood cell) more active, which can raise the risk of blood clots. Sugar (glucose) did not have this effect.
Published in Arteriosclerosis, Thrombosis and Vascular Biology, the research adds to increasing evidence that erythritol may not be as safe as currently classified by food regulatory agencies and should be reevaluated as an ingredient. The study was conducted by a team of Cleveland Clinic researchers as part of a series of investigations on the physiological effects of common sugar substitutes.
The current research builds on the team’s previous study, published last year in Nature Medicine, which revealed that cardiac patients with high erythritol levels were twice as likely to experience a major cardiac event in the following three years compared to those with low levels. The study also discovered that adding erythritol to patients’ blood or platelets increased clot formation. These findings were confirmed by preclinical studies.
Preparing for Back-to-School Season
Henry Schein Medical helps healthcare professionals prepare young patients for back-to-school season with a wide range of medical product offerings.
 To help healthcare professionals get patients ready for the upcoming school year, Henry Schein Medical is offering a range of pediatric supplies for vaccinations and health screenings. The company aims to keep students healthy during the start of the 2024 school year.
Henry Schein Medical’s Back-To-School Product Guide features vaccines, medical supplies, and equipment specifically to treat infants, children, and adolescents. Practitioners can find cold storage equipment, hypodermics, pharmaceuticals, capital equipment, medical and surgical supplies, point of care diagnostics, and more from renowned suppliers including American Diagnostic Corporation, Baxter, Midmark, BD, Dukal, Abbott, QuidelOrtho, Sekisui, and many more.
“Henry Schein Medical’s strong relationships with suppliers are the cornerstone of our ability to ensure practices receive what is needed to effectively provide backto-school care,” said Stephanie Shen, chief product officer for Henry Schein’s North America Distribution Group. “Through these collaborative partnerships, we can continue to deliver reliable, high-quality solutions that assist providers in delivering exceptional patient health care.”
Henry Schein Medical’s Fully Integrated Service Team (FIST) provides customers with strategic resources and integrated solutions
that enable quality patient care by providing a comprehensive selection of products. Medical product offerings now include a wide range of options for healthcare professionals prepping physicians’

offices for the busy back-to-school season, including products such as Dukal LLC’s adhesive kid-friendly bandages, Abbott’s ID Now Influenza A&B Test Kits, BD Needle Syringes, and more. The company’s five distribution center model (plus a specialty distribution center) across the U.S. allows for greater control and stocking efficiencies, ensuring a 96% fill rate and with more than 93% of customers serviced with the products they need the next day.
In addition to Henry Schein Medical’s product portfolio, Team Schein Members also help students start the school year confidently through the company’s “Back to School” program. The program started in 1998 to provide underserved students with backpacks, gift cards, and school supplies to help ensure their success. Team Schein members come together in support of this program each year to pack backpacks filled with school supplies and essentials for the upcoming school year. According to Henry Schein Cares, the “Back to School” has helped more than 65,000 children around the world.
Industry News
Midmark Corporation hosts Professional Women in Healthcare regional event and annual board meeting Midmark Corp., recently hosted a Professional Women in Healthcare (PWH) regional event at Hotel Versailles in Versailles, Ohio. This event coincided with the PWH executive board meeting, also held at Hotel Versailles and Midmark during the same week, marking the 20th anniversary of PWH.
The regional event, attended by 80 guests, included PWH board members and leadership, Midmark Teammates, partner organizations, regional customers and guests. Rob Sackett, chief operations officer for Midmark, welcomed guests to the event and expressed his enthusiasm for the significant gathering of healthcare leaders while congratulating PWH on reaching an incredible milestone. Sackett stated, “The impact of PWH is profound and resonates throughout our industry. We are proud to support PWH as a corporate partner.”
The event included a panel discussion featuring esteemed panelists who are distinguished recipients of leadership awards boasting extensive expertise in communications, human resources, finance and corporate culture. The evening concluded with a live Q+A session, allowing attendees to interact directly with the panelists and gain actionable insights for advancing their careers. The panel discussion

was moderated by Vicky Lyle, vice president of industry relations for Owens and Minor. Panelists included Allison Therwhanger, vice president of corporate sales for Innovia Medical and chair of PWH; Sue Hulsmeyer, chief people and administrative officer for Midmark and Jenny Collopy, vice president, chief marketing and communications officer, The Christ Hospital Health Network. The panelists shared insights on leadership excellence and mentorship within the healthcare supply chain and other healthcare sectors.
Allison Therwhanger commented, “PWH is thrilled to celebrate 20 years of empowering women in our healthcare industry. The events at Midmark this week exemplify our commitment to creating a platform for leadership development, mentoring and networking for those women wanting to lead and succeed in their careers.”


Dr. Anne Eiting Klamar, chair of the board for Midmark and co-founder of PWH stated, “As we celebrate the 20th anniversary of PWH, we are reminded of the lasting impact women leaders have had on our industry. Midmark is honored to support PWH and its continued vision to foster leadership excellence by providing professional growth resources and a supportive community for women in various healthcare sectors.”
The PWH executive board and leadership team also enjoyed a tour of the Midmark Experience Center at Midmark’s headquarters in Versailles, where they learned more about Midmark’s commitment to innovation and healthcare excellence. The recent expansion of Midmark’s Experience Center and Technology Center underscores its dedication to redefining healthcare delivery and enhancing patient and caregiver experiences.
PWH board; (top) Q&A panel; Rob Sackett, Midmark
Using Mentalism Techniques as a Sales Tactic
Basic principles from a high concept performance art that sales reps can tap into.
By Pete Mercer
 Can you read the minds of your customers? You might wish you could, but most of us don’t have that gift. Until we can figure out a way to literally tap into the minds of our customer base, we will have to settle for more creative tactics. Mentalism, the performance art where the performer demonstrates the appearance of highly developed intuition, is as close as it gets – but how can sales reps tap into such a high concept performance art?

On a recent episode of The Cure ... With Scotty and Sully, hosts Scott Adams and Brian Sullivan spoke to Josh Fletcher about how mentalism techniques can transform your sales approach, covering everything from building rapport and reading people to overcoming objections and handling stress.
The art of persuasion
Essentially, mentalism is all about persuading people to make a choice, much like sales. Fletcher gets up on stage and through a series of cleverly worded prompts and questions can convincingly nudge his audience towards a specific outcome. Fletcher said, “I like to say in the performance aspect, it’s kind of like what you’d expect from a magician, but I’m not making things appear or disappear. I’m messing with people’s minds and trying to figure out what they’re thinking.”
He’s looking at body language to better understand how his audience will react in real-time, then adjusts his approach based on those reactions. For him, the most important thing in his shows is to get people on his side. He said, “Sometimes even if something is in someone’s
SUBSCRIBE to The Cure on YouTube by scanning the code below
best interest, there are so many roadblocks that are popping up in their way and sometimes will actually get in their own way for making the best decision and being able to subtly help people, guide them to where they’re ultimately going to be happy, but do it in a way that makes them own that decision and feel good about it.”
Using mentalism in sales
While mentalism might be a specialized performance technique that would take years to master, sales reps can use the basic principles in their meetings with customers. Body language reveals a lot of information about how your customers are engaging with your sales approach. According to Fletcher, it starts with a very simple tactic: using your natural skills to help you better understand your audience.
“When you start trying to tell people what decision they should make, our natural inclination is just to dig our heels in. But when you listen and then you are prescribing to them from a professional educated standpoint, you’re solving their problem versus telling them what they should do,” Fletcher said.



The Next Generation of Midmark® Steam Sterilizers
Midmark Steam Sterilizers are designed inside and out to make instrument processing as easy and as automated as possible.
01 Navigate cycle setup and other processes with a clear, fingerprint-resistant 5-inch touchscreen you can utilize while wearing gloves.
02 Determine cycle status—cycle in progress, cycle complete and cycle error—from a distance with a progressing color-coded LED light bar, large cycle countdown clock and audible cues.
03 Stay audit-ready with device reminders, user authentication, unlimited storage of routine care events for the life of the sterilizer, and automated cycle recordkeeping.
See what makes them different at: midmark.com/automateIP













Hillrom
