Research creates breakthroughs. And breakthroughs make more cancer survivors.

That simple equation hides sophisticated science, of course. But it’s the end result we care so much about. That’s why, in our new five year strategy, we are sharpening
our focus to concentrate on the most deadly cancers for even greater impact for people with cancer.

Seven cancers make up nearly 50% of all cancer deaths
Fifty years ago, less than half of breast and prostate cancer
patients could look forward to more than five years of survival. Today, thanks to investments in cancer research – like yours – the five-year survival rates are 85% and 95% respectively. That’s tremendous progress!
page 7
Autumn 2022 www.breakthroughcancerresearch.ie BREAKTHROUGH HOW YOU’RE CHANGING THE FACE OF CANCER RESEARCH INSIDE THIS ISSUE OUR VISION: 100% SURVIVAL FOR 100% OF CANCERS
Continued on
5 New projects Patients helping Patients Ring of Kerry Cycle
Dr. Elizabeth Burrows, Dr. Nora Lieggi, Orla Dolan and Dr. Frances Drummond
UNLOCKED: 5 NEW BREAKTHROUGH PROJECTS
Every one of them is possible thanks to your help
We’re pleased to share five exciting new projects with you. These projects – in partnership with the Irish Research Councilfocus on a range of cancers and their impact on patients’ lives.
Your compassion means we can work ever
harder to discover new treatments and care for people with cancer. With your every gift, we come closer to making more survivors!
Please read on to learn about the latest projects you helped to fund and the scientists behind them.
1A new, non-toxic way to deliver chemotherapy?

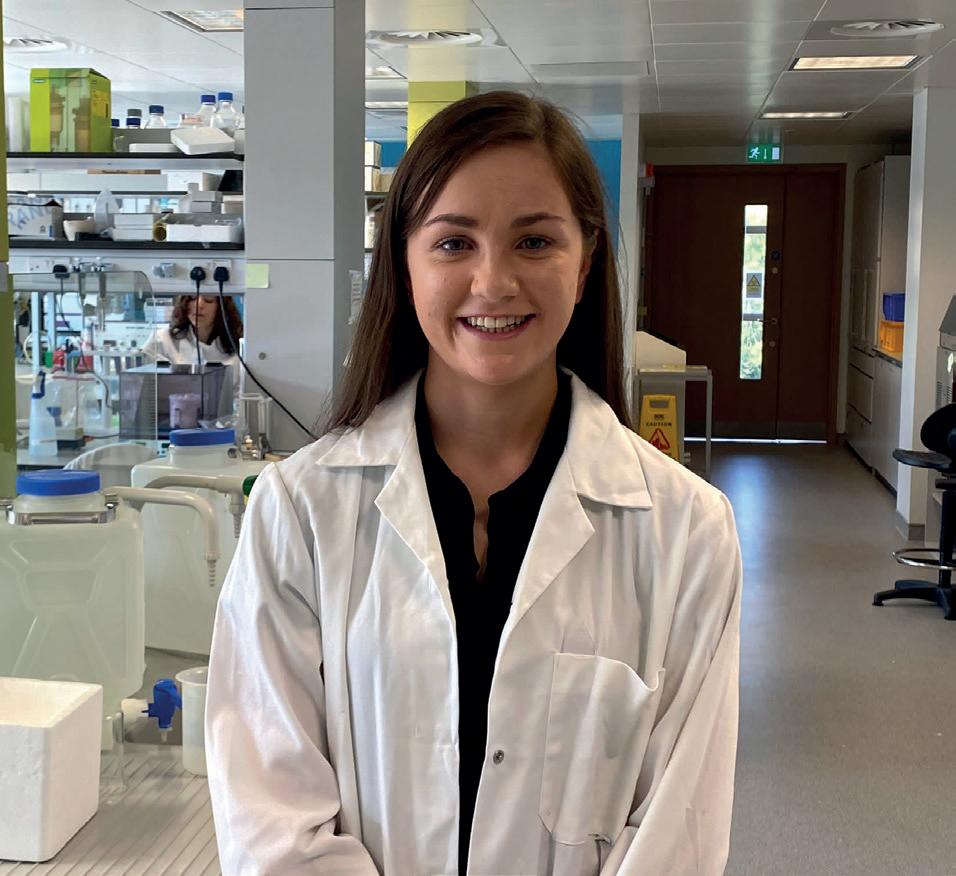
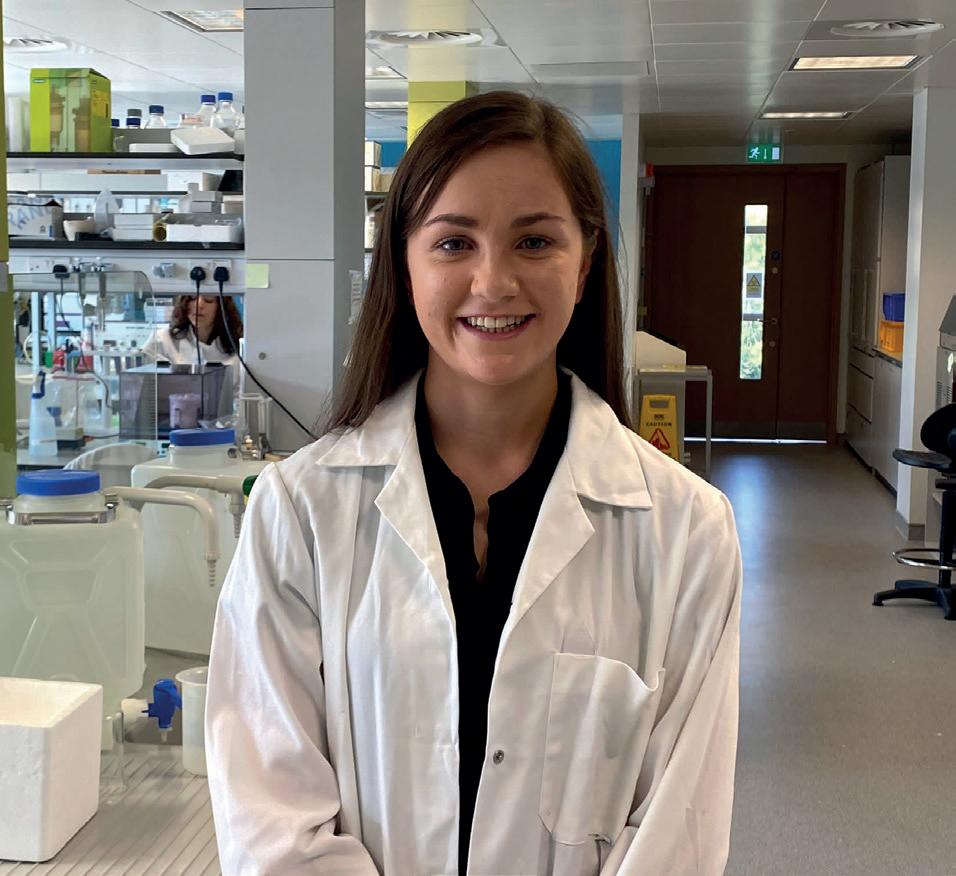
Jada Abdel Monem

Gamal will work in the lab of Professor Silvia Giordani in DCU. They will investigate the possibility of carbon-based nanoparticles (CNOs) as nontoxic drug carriers. These tiny particles could bring therapeutic agents – like chemotherapy – directly to the cancer.
We have seen revolutionary advances in cancer treatment during last 20 years. But there are too many patients with
hard to treat cancers, such as metastatic breast, pancreatic and prostate cancers. Right now we don’t have enough effective treatments for these patients.
Many drugs in development show potent anti-cancer effects. But they don’t work at all when given orally or intravenously. Delivering them right to the cancer could be the answer. CNOs are small enough to be safely sent through the circulatory system in the blood.
2How a survivor of leukaemia is working for better lives for others
At age 5, Avril Deegan was diagnosed with acute lymphoblastic leukaemia.
“As a childhood Leukaemia survivor, I feel I have a lot to offer to the research.”
Avril is researching resilience, social support, and quality of life amongst childhood leukaemia survivors and their parents.

Public and patient involvement (PPI) in research is crucial. Researchers like Avril are more likely to ask appropriate questions, grounded in their experience. They’re also more likely to ensure the research has a practical focus, understand the relevant healthcare context, and call on a network of other “expertsby-experience.”
Avril says, “With over 80% of


Jada’s work will focus on cancers that are currently incurable. CNOs offer the possibility of using extremely powerful drugs at low doses, decreasing side effects, and improving the quality of life for patients.
children surviving leukaemia nowadays, more research is needed into survivorship care.”


Avril will be working with Dr. Simon Dunne in Dublin City University.

2
Jada Abdel Monem Gamal
Avril Deegan
3





Better outcomes for patients with oesophageal cancer


Twelve years after Maria’s grandfather was treated for oesophageal cancer, she began her pharmacist training at the same hospital he was treated at. She saw the vulnerability of patients fighting this cancer. And she wanted them to have a better outcome.
Maria wants to find more effective treatments. To do that, she’s studying the cancer cell biology that underpins this disease.
She’s now starting a PhD in UCC with supervisor Dr. Sharon McKenna.
Ireland has nearly 450 new cases of oesophageal cancer
annually, one of the highest rates in Europe. The five-year survival rate is approximately 20%.


Maria is investigating genetic changes in our cells that can lead to abnormal cell growth, causing cancer. Current treatments usually kill these abnormal cells. But oesophageal cancer cells find ways to escape and become resistant to cell death.
At Cancer Research@UCC, they’ve found that one group of genes is more present in cancer cells that resist treatment. Early research shows the expression of these genes can be changed. This
4Exploring cancer-related cognitive impairment

Cancer-related cognitive impairment – trouble remembering, learning, concentrating, or making decisions – affects almost 30% of patients worldwide. But it’s not clear whether that impairment is because of the cancer itself, the treatment, or psychological factors.
Aideen Scriney will work with Dr. Lorraine Boran in DCU to explore cognitive impairment in cancer patients before they receive treatment. They hope to improve patients’ cognitive function after treatment.

Because of support like yours, more people are surviving





cancer. But now we need to address cognitive impairment and its effect on patients, especially before and during their treatment. There’s also a need to look at a patient’s subjective perception of their cognitive impairment as that will most affect their lives.
Aideen’s research will focus on preparing patients for the stress before treatment or surgery. With Dr. Boran, she’ll also look at the impact of exercise rehabilitation on cognitive impairment caused by cancer– an underresearched area.
could have an impact on drug resistance. Maria’s research aims to understand how these genes function and how this affects the response of cancer cells to chemotherapy. Her research may help us understand how to change the way these genes work, leading to less drug resistance and more effective treatments.
3
Maria Carey
Aideen Scriney
5Diagnosing and treating metastatic uveal melanoma

Uveal melanoma is a cancer that begins in the eye and frequently spreads to the liver. Once it moves to the liver, the prognosis is currently poor. Only 8% of patients will survive beyond two years.

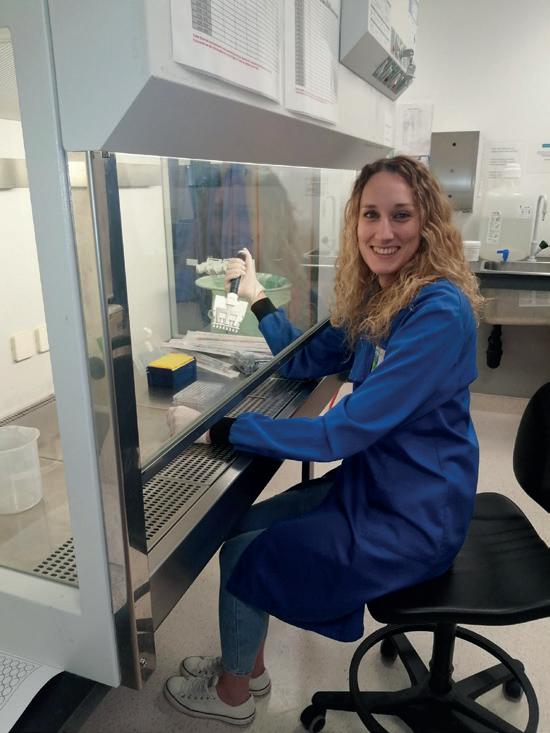
Dr. Valentina Tonelotto is a post-doctoral researcher. She will work in the lab of Professor Breandan Kennedy in UCD. Their research will explore the therapeutic potential of a protein (CysLT) in uveal melanoma development. Prof. Kennedy’s group has found reduced patient survival when increased levels of this protein are found. Targeting this
protein seems to have an effect on cancer cell growth.

Valentina will investigate whether drugs specific to CysLT block the growth of uveal melanoma in the liver. She will also study patients’
blood to identify factors associated with better or worse survival rates and look for new therapeutic targets.

Together, these new studies will evaluate the effectiveness of drugs targeting CysLT and identify the patients most likely to benefit from this treatment.
FUNDED WITH YOUR SUPPORT: NEW RESEARCH INTO LUNG CANCER
Daniella Anthea Agreie Gomes was awarded the Breakthrough PhD Scholarship 2022. Daniella will research how blood vessel growth in non-small cell lung cancer affects cell resistance to chemotherapy, and how to target it therapeutically. She will work with Professor Adriele Prina Mello in Trinity College Dublin.

Daniella’s research focuses on why new blood vessels form in lung cancer. These blood vessels carry oxygen and nutrients to the body’s tissues. It’s a vital function, necessary for growth and development as well as for wound healing.
But it also plays a role in the formation of cancer because tumours also need a blood supply to thrive.
Lung cancer is the number one cause of cancer deaths in Ireland for both men and women. Improving our understanding of the role these blood vessels play in lung cancer progression and response to therapies could greatly impact the lives of people with lung cancer. Daniella’s work will increase the chances of clinical success for new treatments or drugs.
4
Daniella Anthea Agreie Gomes
Continued from page 3
Dr. Valentina Tonelotto
You can join other people concerned about cancer!
In September, for the first time ever Breakthrough Cancer Research held a national collection day. The day was focused around World Cancer Research day. We had collectors in every county in Ireland and hope to grow the number of volunteers for next year.

“I SEE MYSELF AS THE VOICE OF THE PATIENT”
Dr. Chrys Ngwa is participating in the Public and Patient Involvement Panel (PPI) for Breakthrough Cancer Research. Three years ago, he was diagnosed with prostate cancer. The cancer was already stage 4. His prognosis wasn’t good.


With both a bachelor’s degree and a PhD in Microelectronics, Chrys has experience applying for grants, as well as experience as a cancer patient. He likens his function on the PPI panel as a bit like insider trading – but for the good.
“I know how it all works!” he says. “I’m part of a group that can actually influence the direction of research that will potentially improve patient outcomes in the future… that’s an incredible gift that
someone’s given to me. Absolutely, it is brilliant.” Research with, not to, patients
The aim of PPI is that cancer research is done ‘with’ people
with cancer, not ‘to’ them. Participants are involved in all aspects of our research department, depending on what is right for them. We see their confidence grow as they realise how important their
FIRST BREAKTHROUGH NATIONAL COLLECTION FOR WORLD CANCER RESEARCH DAY If you would like to get involved please contact Mary at 021 4226655 or mary@breakcancer.ie 5 Continued on page 6
Dr.
Chrys Ngwa
lived experience and opinions are to the research processes.
What Chrys wants you to know
Chrys knows his cancer is now untreatable. It will come back –whether that’s next year or five years from now.
In the meantime, Chrys is making the most of every moment with his family. And he’s helping everyone he can through his PPI involvement.
If you would like to get
involved in Breakthrough’s Public and Patient Involvement Panel and help improve cancer research, treatments, and care, please complete the online form on https://bit.ly/PPIForm or contact Dr. Frances Drummond on 021-4226655 or frances@breakcancer.ie Or hold your phone’s camera on the image below. And keep in mind that you don’t need to have had cancer to get involved!

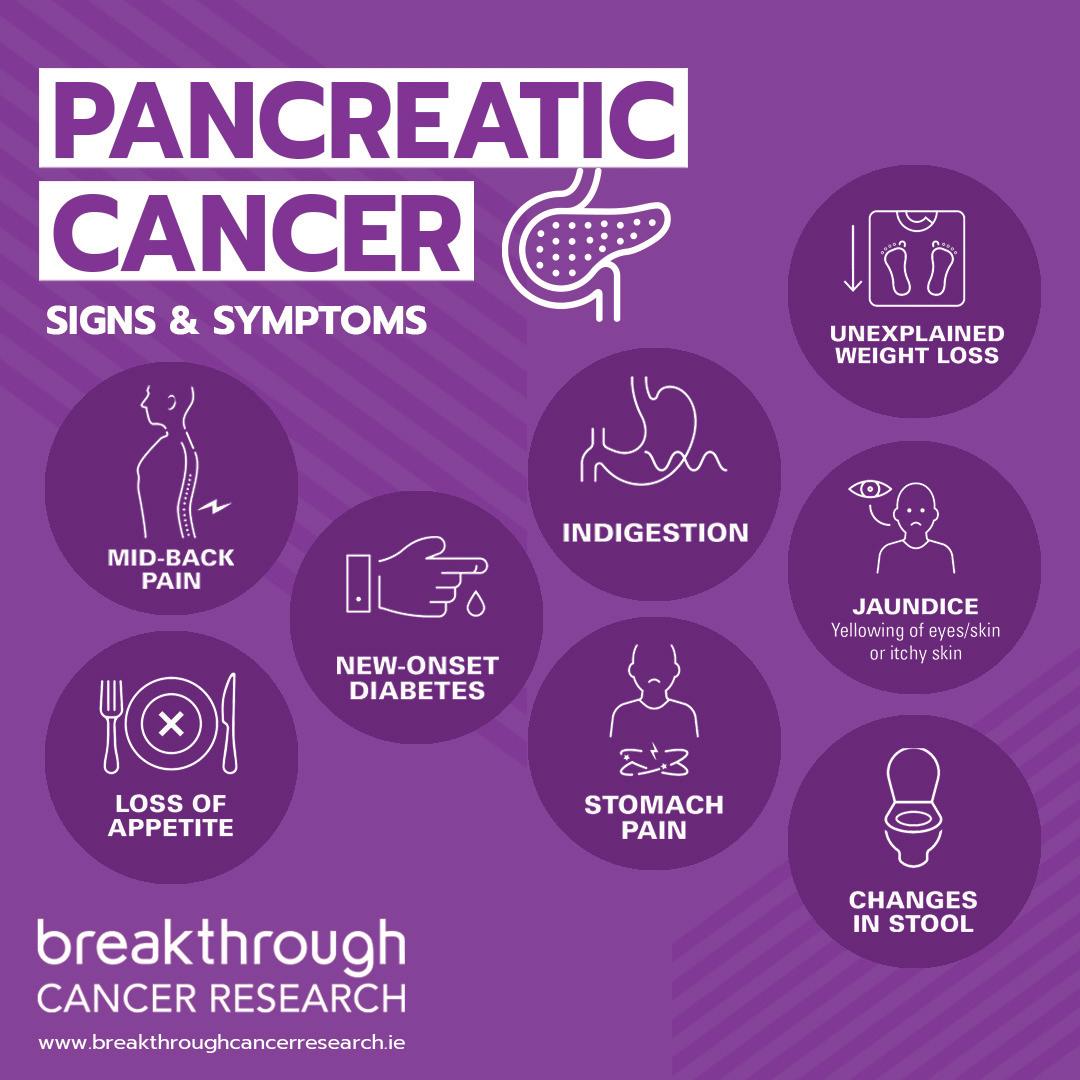
NEW PANCREATIC CANCER RESEARCH FUNDED, THANKS TO YOU
This year the successful Musgrave PhD Scholar is David Hackett.
radiotherapy. Patients can expect only a slightly longer life with these conventional therapies. And that benefit comes with significant side effects and a negative impact on their quality of life.
choices. This project will investigate a promising new RNA-based therapeutic strategy to improve the effectiveness of conventional chemotherapy and radiotherapy, improving survival rates.
David’s work focuses on pancreatic cancer. People diagnosed with pancreatic adenocarcinoma (PDAC) have an extremely poor prognosis. And 90% of all pancreatic cancers are PDAC. Currently, most patients will die within one year of diagnosis.
PDAC usually responds poorly to chemotherapy and
David will work with supervisor Dr. Stephen Maher in Trinity College Dublin. We need to learn why this cancer resists chemotherapy and radiotherapy. Then we need to identify biomarkers that can guide therapeutic

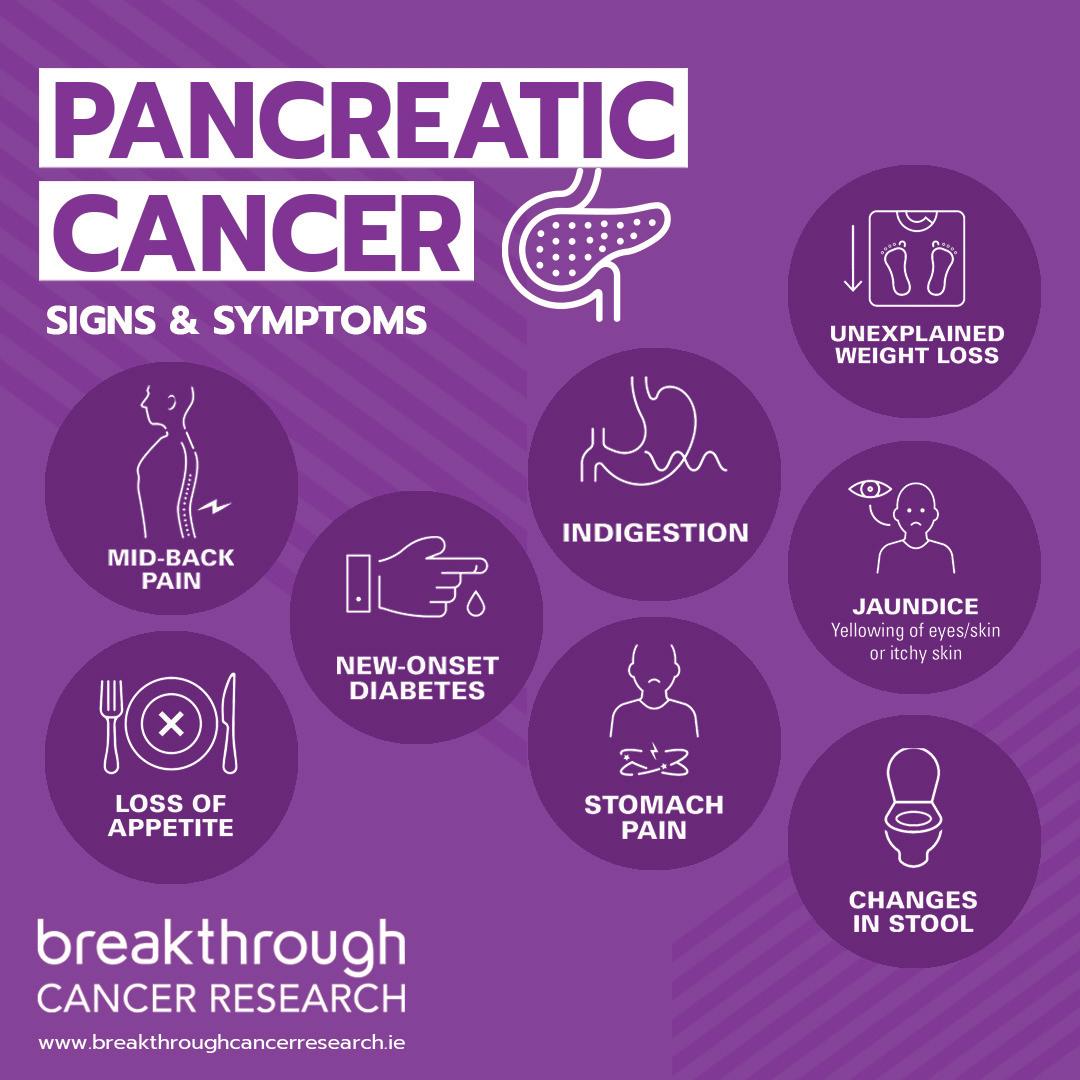
Signs and Symptoms of Pancreatic Cancer
6
HOLD YOUR PHONE’S CAMERA HERE:
Continued on from page 6
https://bit.ly/PPIForm
YOU’RE HELPING TO SAVE PEOPLE FROM THE MOST DANGEROUS CANCERS
Seven cancers account for almost half of all cancer deaths each year in Ireland.
Cancer survival isn’t equal. Seven cancers account for almost half of all cancer deaths each year in Ireland. Pancreatic, oesophageal, stomach, liver, lung, brain, and ovarian cancers cause so much heartbreak and fear! Overall, cancer survival has increased. But the incidence of these seven cancers is growing. That’s why, in our new five year research strategy, we are focusing on those seven hardest-to-treat cancers: we want even more impact. More lives lengthened or saved. Fewer broken-hearted loved ones.
WE MUST DIRECT OUR BEST RESEARCHERS AT THEM IF WE’RE TO SAVE MORE LIVES!


What poor prognosis cancers have in common






These cancers often have vague symptoms, leading to late diagnoses and few effective treatment options.
Sharing information about symptoms and
encouraging people to get checked is important. But there’s still too much we don’t know. And research funding for these cancers has been lower than for others. That’s why we’re stepping forward to focus even more on them.
We aim to double the Irish survival rates for people with poor prognosis cancers

We are fiercely determined. And so we’ve added big data to our priorities. Why? Because cancer is a complex disease. And innovative research generates huge amounts of data. Managing that data is key to increased understanding and advances in predictive, preventative, and personalised medicine.
With access to world-class computing capabilities, we can combine data with information about each person’s unique cancer. Then clinical teams can analyse and interpret the information… and take action for patients.
Your continuing support will be critical as we move forward. Our work only happens with your support. You are our partner, and we’re so grateful for your commitment!

7
Continued from page 1
THANK YOU FOR SUPPORTING THE RING OF KERRY CHARITY CYCLE!







Whether you rode, helped out on the day, or supported a cyclist, we’re so grateful for your help!
This July, the Ring of Kerry Charity Cycle took place for the first time in person since 2020, after stopping due to Covid. We were thrilled to have over 1300 cyclists cycling the 170Km of ‘The Ring’ for Team Breakthrough. Those cyclists included our fantastic ambassadors Paschal Sheehy and David Gillick.




Researchers funded by Breakthrough joined our team and volunteers and helped at registration, food stations, and the finish line.

The funds are still coming in. But we hope to have raised over 200K from this event for our Microbes and Cancer project. The project is part of

a national Precision Oncology Ireland programme.



Precision (or ‘personalised’) medicine uses data about a person’s genes, immune system, and microbiome, along with additional information on their cancer, to understand the unique pathways of a disease or treatment response in that person. Then it uses the information to target the patient’s treatment.



Precision Oncology Ireland will use cuttingedge technologies to generate unique genetic and molecular profiles for each patient’s cancer. The key advantage of the programme lies in the innovative computational methods applied. This helps make sense of cancer profiles. And it helps us
understand what drives each individual cancer. The results will be better cancer diagnostics, personalised cancer treatment, and faster drug development.
With every exciting breakthrough, you’re there beside us. Every gift takes us closer to new, better, kinder, and smarter treatments and makes more survivors. We’re so grateful to you!
Breakthrough Cancer Research, Glenlee, Western Road, Cork, T12 F9XD, Ireland. W www.breakthroughcancerresearch.ie E info@breakthroughcancerresearch.ie T 021 422 6655 LoCall 1890 998 998 Company Registration No: 496464 Registered Charity No. 20077945
Your support raised urgently needed funds for our Precision Oncology Research project
Researchers Patricia Flynn and Fiona O’Connell with Paschal Sheehy (left) and David Gillick (right)
Volunteers at Kenmare Food Station