















VOL. 104 ISSUE: 05
CONTACT THE DN
Newsroom: 765-285-8245
Editor: 765-285-8249, editor@bsudailynews.com
EDITORIAL BOARD
Kate Farr, Editor-in-chief
Trinity Rea, Print Managing
Editor
Olivia Ground, Digital Managing
Editor
Katherine Hill, News Editor
Meghan Braddy, Associate News
Editor
Zach Carter, Sports Editor
David Moore, Associate Sports
Editor
Derran Cobb, Associate Sports
Editor
Ella Howell, Lifestyles Editor, Copy Editor
Maria Nevins, Video Editor, Podcast Editor
Layla Durocher, Social Media
Editor
Andrew Berger,Photo Editor
Isabella Kemper, Associate Photo Editor
Jessica Bergfors, Visual Editor
Brenden Rowan, Visual Editor
Corey Ohlenkamp, Adviser
The Ball State Daily News (USPS-144-360), the Ball State student newspaper, is published Thursdays during the academic year except for during semester and summer breaks. The Daily News is supported in part by an allocation from the General Fund of the university and is available free to students at various campus locations.
TO ADVERTISE
• (765) 285-8256 or dailynewsads@bsu.edu
• Hours: 8 a.m.-5 p.m. Mon-Fri.
• ballstatedaily.com/advertise
TO SUBSCRIBE Call 765-285-8134 between 9 a.m. and 3 p.m. Mon. -Fri.
Subscription rates: $45 for one year. POSTMASTER: Send address changes to Daily News, AJ278, Ball State University, Muncie, IN 47306
JOIN THE DAILY NEWS
Stop by room 278 in the Art and Journalism Building. All undergraduate majors accepted and no prior experience is necessary.
In the Sept. 5 issue of the Ball State Daily News, Jessica Velez’s name was incorrect on pg. 9. Her last name is Velez, not Valez. Kyle Smedley’s name is incorrect on pg. 8. His last name is Smedley, not Smedly.
To submit a correction, email editor@bsudailynews.com.


Last year, the Ball State Daily News published its first special edition based around the topic of mental health. Our staff recognized the growing concern surrounding mental wellness and wanted to produce a paper that could share information and resources, as well as remind our peers and our own staff that no one is alone in their mental health struggles.
In our newsroom, we strive to expand our coverage off campus and into the Muncie community. We aim to pop the metaphorical Ball State bubble and connect campus, Muncie and beyond.
Because of our greater community and statewide coverage, last year’s mental health paper started a discussion beyond the walls of our newsroom and the footpaths of our campus. It was the wake-up call we hoped it would be. We intend to keep the discussion ongoing.
It just takes the proper dialogue and action to overcome the stigma around mental health. Talking about the situation as it is — being honest and bringing awareness — is what leads to change. As journalists, it’s our job to promote that dialogue.
Every single one of us is affected by mental health to some degree. But we are in this together — we are not alone.
Thank you for reading,



Conversations about vaping addictions often leave out the mental health effects.
Indiana Democrats are urging caution over the potential sale of U.S. Steel, citing concerns that President Biden may block the deal. They warn the sale could impact jobs and the local economy, particularly in Northwest Indiana where U.S. Steel’s major plant operates.
Marion County Supreme Court Judge Timothy Oakes dismissed a case Sept. 10 that sought to overturn a state agency’s decision to exempt terminated pregnancy reports from public record. Oakes ruled in favor of the Indiana Department of Health, which stopped sharing the reports following the state’s adoption of a near-total abortion ban.
Just before noon Sept. 9, an individual was seen near Ball State University with a visible firearm, a university communications official said via email. The university police made contact with the individual and ascertained there was no threat to campus, nor a lawful violation. The individual never entered university buildings or campus property.

Conversations about vaping addictions often leave out the mental health effects.
Olivia Ground
Digital Managing Editor
Take in a deep breath, hold it for five seconds, then blow it out. Count to five again.
In the time it took you to do that, the metaphorical vape in your hand has reached your brain, creating a buzz of adrenaline and energy, according to smokefree.gov.
Former smoker and community member Heather Ashton said the buzz of nicotine is exciting at first, which is what often draws kids to the modern-day smoking epidemic of vaping.
Ashton grew up around smoking and can even recall the different times in her childhood when her mother would send her out for cigarettes with money and a note. Cigarettes were easily accessible to her.
She recalls she started smoking as young as twelve.
“I don’t even know that I necessarily liked the taste, but it gave me a buzz,” Ashton said.
Ashton can recall cigarette advertisements were frequent, showing off models and celebrities smoking. It was a cool thing at the time.
Cigarette smoking rates are down for high school-aged youth and college students, Jordan Moss, program director with Tobacco Free Coalition of Delaware County said. Regardless of this, it doesn’t mean nicotine addictions have gone anywhere. If anything, they’re just as strong, he said.
The new vice for this buzz is electronic cigarettes (e-cigarettes) and vapes—something uniquely
targeted to the generation of current high school and college-aged students.
“We do always let students know that they are referred to as the guinea pig generation because we don’t know the long-term effects of vaping …” Moss said, “It’s big tobacco using their exact same kind of plan to get a whole nother generation latched.”
Moss said most teens report that they started smoking because they felt anxious, depressed and stressed.
“I would say anytime that you wake up in the morning and you’re thinking, ‘This is what I have to do right now,’ it’s not good for your health at all,” Ashton said, recalling the way her nicotine addiction affected her mental health.
I’d tell [young vape users] to consider if they want to be a slave to that vape for the rest of their life.”
- HEATHER ASHTON, Former smoker
But beyond the negative side effects of smoking, like tar lungs and shortness of breath, many students don’t know the wide range of negative side effects a nicotine addiction can cause.
Reports have shown that vaping and using e-cigarettes can expose users to toxic amounts of cancer-causing chemicals that aren’t currently regulated by the FDA. Additionally, these chemicals create negative impacts on the brain of the user. So much so, that many popular vapes used in the United States are banned in the U.K., Moss said.
“Why would anyone want to be a consumer that is making someone else money but killing themselves at the same time?” Ashton questioned.
“… As a teenager and a young person, your brain is still developing. I’m sure that it had some residual effects that I may never know.”
Moss added this constant exposure to nicotine on the undeveloped under-25-year-old brain creates its own sets of learning impacts.
“Nicotine exposure affects learning, memory and attention span,” Moss said.
He also added that the mental distress, which causes many teens to start smoking, only gets worse as they develop a nicotine dependency.
According to studies referenced by the National Institute on Drug Abuse, teenagers who use e-cigarettes are more likely to continue using nicotine as adults. They also may be at greater risk
of smoking conventional cigarettes later in life.
“What happens is when you use nicotine, it actually changes the way synapses are formed in your brain, which is the learning pathway or how to get back to memories and things like that,” Moss said. “That’s why nicotine is so harmful, especially to those under 25.”
A nicotine addiction is a specifically difficult addiction to overcome, creating additional mental health issues on top of ones already formed by smoking.
According to the National Institute on Drug Abuse, a nicotine addiction operates and hinges on the dopamine rush you get from the buzz when you hit your vape. The initial buzz creates a dopamine hit that feels similar to a reward system in the brain.
“We have a reward system in our body [and] in our brain that starts out by doing the important things, like eating, sleeping, all those important things. And we get dopamine released, it’s our happy rewards thing. It’s a neurotransmitter,” said Lynn Witty, the Medical Director at the Ball State Healthy Lifestyle Center and Director of Community Organization with the Addictions Coalition of Delaware County.
“So if you put a drug in, that can also attach to those little happy receptors and release more dopamine. You get used to it, and so you actually have to use more and more of the drug to get the same amount, or not even the same amount of that quick, happy feeling. And so over a period of time, as you’re increasing your drug use, you can easily become addicted,” Witty said.
However, both Witty and Moss credit this addiction and tolerance to nicotine as the reason why many smokers who become addicted find themselves more depressed or anxious than when they started smoking.
“That’s why people try to use nicotine replacement therapy like gum or patches. They do struggle because it’s not hitting their body as quickly as that first hit,” Moss said.
According to the Centers for Disease Control, withdrawal shows up in emotional changes, irritability, inability to sleep, lack of concentration and more. These are all things that can affect the mental health of someone who uses nicotine products.
“I say all the time, if people knew how good you felt after not smoking for one year, they would never smoke,” Ashton said. “I think it’s probably the same with vaping … They don’t realize how bad it actually makes them feel until you’re out of it.”
Moss also stressed that nicotine addiction, especially in those under the age of 25, increases irritability, anxiety and mood swings. It can also lead to an impairment of self-control, cognition and performance.
“We’re trying to tell parents [to] start as early as [they] can. If you see someone vaping in public, you know, let them know … We want to make sure we stay away from those. Those hurt our bodies,” Moss said.
Witty adds that intervention by family and loved ones can be helpful because often addiction can become a difficult thing to overcome.
“You also have to think, if it’s someone who’s not trying to quit, they’re looking to see how they can get a vape to use or find a place to use it,” Witty said. “And that’s always in the back of your mind … The most important thing is getting that fix.” Ashton smoked for multiple decades of her life, quitting after having her child and realizing how much of his life she would be missing out on while smoking. For her, it’s important students of all ages know the impact smoking will have on their life.
“I’d tell [young vape users] to consider if they want to be a slave to that vape for the rest of their life,” Ashton said. “If you want to be a slave to that, figure it out because when you’re in college, you don’t have much money. I remember times where I didn’t have much money in college. I would smoke butts … You’re still finding a way to do it. But is it worth it?”
Moss encourages anyone who vapes to try and go 10 days without smoking. He says that most can’t make it, but it opens their eyes to the problem. For students who are ready to quit, there are resources available.
Beyond call hotlines, textlines and virtual resources like apps, Witty highlights resources like the counseling center and the Healthy Lifestyle Center on campus for students to talk it out with someone. She encourages finding support in peers, people you can trust and loved ones.
“Search out one of those people, someone you trust just even direct you in the you know, right direction for getting help. It’s hard to do by yourself,” Witty said.
Contact Olivia Ground via email at olivia. ground@bsu.edu or on X @liv_ground_25.
1 in 10 Indiana high school students reported current (past 30 day) use
1 in 30 Indiana middle school students reported current (past 30 day) use of any tobacco product.
21% of adults in Delaware County smoke.
60%
13.2% of teens think only flavoring is in their vape. of teens know there is nicoteen in their vape.
13.7% of teens “don’t know.”

20 44



75
90 = = = = CIGARETTES CIGARETTES
As the winter months approach, there are ways for Ball State students to tackle seasonal depression.
Meghan Braddy Associate News Editor
As the days grow colder during the fall semester, many college students experience more than just a change in the weather.
Seasonal depression, also known as Seasonal Affective Disorder (SAD), affects a significant number of students, particularly in cities like Indianapolis, where “the percentage of time that the sky is overcast or mostly cloudy remain[s] about 57 percent throughout the season,” according to Weather Spark.
SAD is a mental health condition triggered by seasonal changes, typically starting in late fall and lasting through winter.
According to the Mayo Clinic, reduced sunlight during these months is thought to lower serotonin levels, which affects mood and disrupts the body’s circadian rhythm, impacting sleep and energy.
Nationwide, SAD is a mood-related condition
that affects almost 5 percent of the U.S. population annually, and the symptoms can be present for nearly half of the year, according to McGovern Medical School.
For students at Ball State University, addressing this condition has become essential in ensuring mental health and academic performance do not suffer during the colder months.
Aubrey Driscoll, the associate director for prevention and wellness at Ball State’s counseling center, has recognized the challenges posed by Indiana’s harsher winters and taken significant steps to address seasonal depression among the student population.
“Seasonal affective disorder often begins in young adulthood. It can present very similarly to depression, with common symptoms including persistent sadness, feelings of hopelessness or helplessness, loss of interest in hobbies, decreased energy, difficulty concentrating, and changes in sleep or appetite,” Driscoll said via email.
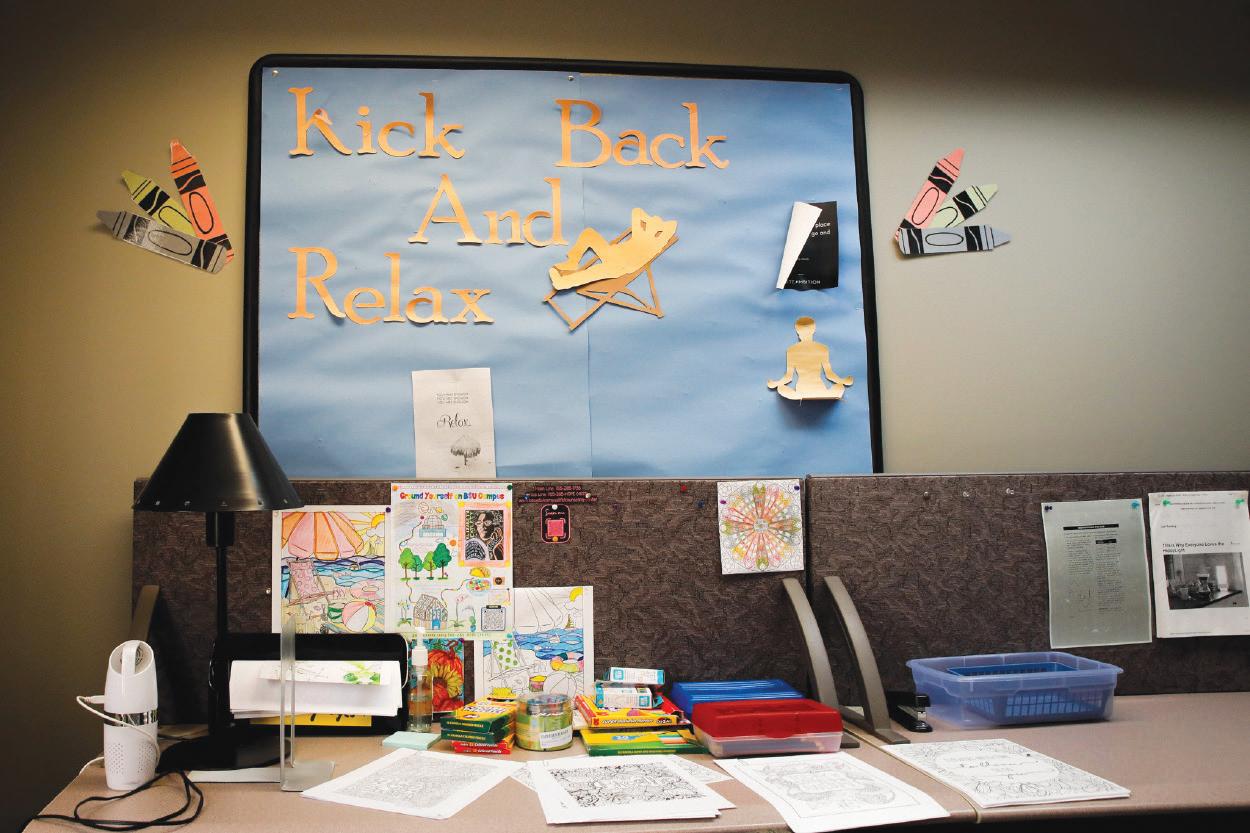
The counseling center offers various services and resources to help students manage their symptoms and maintain their well-being during the drearier months. One of the most prominent resources the counseling center provides is light therapy.
“Light therapy boxes deliver a therapeutic dose of bright light that mimics outdoor light,” Driscoll said. “Research has shown that this type of light may lift one’s mood and ease some of the symptoms of seasonal affective disorder, such as tiredness or fatigue.”

According to the National Library of Medicine, nearly 42 percent of Americans are vitamin D deficient, which can exacerbate symptoms of seasonal depression. For some students, simply increasing sunlight exposure or taking vitamin D supplements can significantly improve their mood and energy levels.
The counseling center provides light therapy boxes on campus to help with this deficiency, offering a convenient and accessible way for students to combat the effects of seasonal depression.
According to the Mayo Clinic, light therapy is considered one of the most effective treatments for SAD, with many individuals experiencing significant improvements in their symptoms after regular use.
Regardless of the therapy’s success, Driscoll emphasized the importance of proper usage.
“Before using any type of light therapy box, it is important to consult with a healthcare provider first to determine whether the use of light therapy is advisable and, if so, how it should be used,” she said.
Driscoll added that each light therapy box contains information about light therapy and instructions students should read and understand before using it. The resource and relaxation room
at the counseling center in Lucina Hall 310-A has two light therapy boxes for student use.
In addition to light therapy, Ball State’s counseling center offers individual counseling services. These one-on-one sessions allow students to discuss their experiences with seasonal depression and develop personalized coping strategies.
The counseling center’s staff therapists are trained to address the unique challenges of SAD, helping students navigate the emotional and psychological impact of the disorder while balancing their academic responsibilities.
“The Ball State counseling center provides a wide variety of self-help/on-demand and professional resources to Ball State students. All counseling center services are free,” Driscoll said. “There are no session limits for individual therapy as we strive to work with each individual student to best meet their needs.”
She also highlighted that if students are concerned about their mental health during the colder months, they could explore this concern with a therapist at the office by scheduling a first appointment. At this appointment, students work with a therapist to create a plan that connects them with the resources that best fit their needs.
Second-year theater creation major Dylan Piazzoni has struggled with mental health challenges during the winter months.
“I think [therapy is] helpful in general, not even just for seasonal depression. But I think the bigger stipulation for it is you need to … acknowledge that you have a problem at first,” he said.
While Ball State University offers on-campus resources for seasonal depression, students can also benefit from the support available offcampus in Muncie.
Open Door Health Services provides various mental health services, including counseling sessions and screenings. According to its website, its behavioral health team is “committed to helping individuals and families regain control of their mental well-being by providing individualized care.”
Open Door also emphasizes its sliding fee scale, making mental health services more accessible for students with limited financial resources.
IU Health Ball Memorial Outpatient Behavioral Health offers extensive mental health services, including individual therapy, group therapy and psychiatric evaluations.
According to its website, its team “works together to provide comprehensive care for a wide range of mental health conditions.” This facility provides specialized care for students experiencing severe symptoms of seasonal affective disorder or those who may require medication for their depression.
Still Waters Professional Counseling provides faith-based counseling services, offering a holistic approach to mental health care for seasonal depression.
According to its website, “Still Waters offers a judgment-free zone where clients can address their mental health concerns and develop coping strategies with the help of professional therapists.” Their services focus on addressing a variety of mental health issues, including types of depression, anxiety and stress, while incorporating spiritual elements into their counseling approach.
When asked about the resources Still Waters provides for seasonally depressed students, owner
Your experience is uniquely individual to you, and you’re not alone in how you feel.”
- DYLAN PIAZZONI, Second-year theatre creation major
Meredith Boatright said via email, “Still Waters provides individual … therapy, as well as traumasensitive yoga classes led by a licensed therapist starting [at] the end of this month.”
While off-campus facilities provide mental health support, students can also adopt everyday strategies to manage seasonal depression on their own.
The National Institute of Mental Health (NIMH) and Mayo Clinic suggest several approaches. For example, maximizing exposure to natural light by spending time outdoors, even on cloudy days, can boost mood and energy levels. Maintaining a regular sleep schedule also helps regulate mood and improves overall well-being, and physical activity reduces symptoms of depression and increases energy.
BLUES,
22
Spending time outdoors during daylight hours can help boost mood and energy levels, even on cloudy days.
Consistent sleep patterns can help regulate mood and improve overall well-being.
Exercise has been shown to reduce symptoms of depression and increase energy levels.
Counseling services, whether oncampus or off-campus, can help manage SAD. Speaking with a mental health professional can help develop personalized coping strategies.
Using a light therapy box for about 20-30 minutes each morning can effectively alleviate SAD symptoms.
Try sitting near bright windows at home or work to maximize your Vitamin D intake. Open the blinds, trim any tree branches that block sunlight to your windows or consider adding skylights.
Source: National Institute of Mental Health (NIMH) and Mayo Clinic.

JESSICA BERGFORS, DN DESIGN

Delaware County officially begins construction of a mental health and rehabilitation center.

Katherine Hill News Editor
Construction is underway for Delaware County’s new regional mental health and rehabilitation center. Delaware County Commissioners hosted a “groundbreaking ceremony” to commemorate the solidification of the center’s blueprints and the beginning of construction.
The ceremony, held Aug. 21, was attended by state representatives from the surrounding area who were given a hard hat and shovel. The purpose was for them to be hands-on and actively involved in the groundbreaking.
Though the somewhat labor-intensive digging may have induced a few calluses, Democratic representative Sue Errington of District 34 enforced the necessity of the work.
“There is a very real need for services to address [mental health-related] issues in Delaware County, and this facility is much needed in East Central Indiana,” Errington said via email.
Discussions related to a possible regional rehabilitation center began as early as April 2024 when state officials approved nearly $104 million in renovation projects throughout the area. The $7.6 million facility is funded by the federal COVID-19-era American Rescue Plan (ARP) and
a $2.5 million grant from the state, Errington said in an official statement on Facebook.
According to Mental Health America, Indiana is continually ranked among the ten states with the largest adults with mental illness population.
In 2023, the state ranked 41st among the 50 states. However, it’s an improvement from the state’s 43rd ranking in 2022.
“a significant [nationwide] increase in underage major depressive episodes … Indiana showed the greatest increase.”
The state saw a near six percent increase while the national and regional average was four percent. Countywide, Delaware County ranked highest in the state among populations of adults who reported mental distress.
There is a very real need for services to address [mental health-related] issues in Delaware County, and this facility is much needed in East Central Indiana.”
- SUE ERRINGTON, Democratic representative of District 34
Mental health is important to monitor among all age groups, according to the Centers for Disease Control.
Poor mental health can also bring about poor coping mechanisms, strengthening the likelihood of addiction no matter a person’s age.
A report published in April 2022 by the Indiana Family and Social Services Administration found that between 2008 and 2016, there was
“Substance abuse and mental health go hand in hand; to solve one issue, we must also address the other,” Errington said.
According to Next Level Recovery Indiana, nearly 4.2 million people nationwide “felt they needed treatment [but] did not seek it because they feared negative attitudes from their community.”
At the local level, Indiana University reported in 2024 that almost 1 in 12 Hoosiers “meet the criteria
for having a substance use disorder.”
To combat these issues at the state level, local initiatives matter and often act as a pivotal step toward change on a mass scale. City officials know this.
“This is kind of a bittersweet day,” County Commissioner Shannon Henry said during the ceremony’s press conference. “A rehabilitation center is not something we want to build. It’s something this region needs. We’ve got to have it for the people.”
The facility is the first of its kind in Delaware County and the surrounding Muncie community.
“I’m honored to have had even a small role in establishing these services in our community and providing additional support for those who need it,” Errington said.
The facility is an in-patient care center, working in conjunction with — but ultimately different from — the Muncie Crisis Center, which will handle emergency mental health issues. A February 2023 city press release confirmed the crisis center is also under construction using ARP funds and is expected to be built by December 2026. Contact Katherine Hill via email at katherine. hill@bsu.edu.















Services in Muncie are opening up the conversation surrounding pregnant people’s mental health.



Benny Buddies is a new initiative intended to build a connection between American and international students. They’re hosting a “speed friending” event Sept. 17 from 3:30 p.m. to 5 p.m. in room 107 of the Multicultural Center. The deadline to sign up for Benny Buddies is Sept. 18 at 5 p.m., and partner pairings will be announced the following day.
The annual Muncie event will take place Sept. 21 from 1 p.m. to 10 p.m. in downtown Muncie. The event includes tethered hot air balloon rides, live music and entertainment, food vendors with spicy food and BBQ, and games and contests. The street festival event schedule is located on downtown Muncie’s website, as well as location and parking details.
The Boy Scouts of America Troop 22 is hosting their 31st annual hog roast Sept. 14 starting at 11 a.m. at the Delaware County Fairgrounds. Tickets are $10 in advance, $12 at the door, $5 for kids 5 to 10 years old, and free for kids 4 and under. The meal includes a BBQ pork sandwich, scout-made applesauce, baked beans, baked potatoes, a drink and dessert. You can eat there or carry-out is available.
In comparison to the rest of the country and the Midwest, Indiana has the highest population percentage for reported mental illnesses.
Kate Farr, Trinity Rea Editor-in-chief, Print Managing Editor
A 2024 study conducted by Forbes found Indiana to be the seventh worst state in the country for mental health care. The study based its findings on a few key percentages from each state, based on data from Mental Health America (MHA).
Regardless of the quality of care provided by the state, it is extremely important to seek help with mental illness.
In 2022, MHA found that 56.7 percent of adults in the state with a mental illness do not receive adequate treatment. That’s higher than the national average of 56 percent.
On top of this, a 2022-2023 report from The Healthy Minds Network found that 41 percent of students have experienced depression, with 20 percent reporting symptoms of severe depression. That’s nearly half of students.
Advocating for easier access to mental health care is important but so is showcasing and taking advantage of resources readily available.
In Delaware County, there are a handful of mental health facilities, including clinics and treatment centers that specialize in youth mental health. Advancements are being made within the county to expand upon the available care centers as well.
However, if you need help today, the Indiana affiliates of NAMI (National Alliance on Mental Illness) offer education and emotional support for families, friends and individuals with severe mental illnesses.
The NAMI Indiana crisis line is staffed with volunteers who can help identify symptoms and find the right treatment options for everyone. Staff is available Monday through Friday from 9 a.m. to 5 p.m.
If you are experiencing a mental health crisis or suicidal thoughts, call the Suicide & Crisis Hotline at 988. The hotline operates on a 24/7 basis.
Contact Trinity Rea via email at trinity.rea@bsu. edu and Kate Farr via email at kate.farr@bsu.edu.
DELAWARE COUNTY BY THE NUMBERS (2024)
17.9%
22.0% of adults experience frequent mental distress. per 100,000 people die from deaths of despair, such as suicide. of Medicare users have depression.
88.1%
Source: U.S. News & World Report
Anxiety disorders, depressive episodes, suicide rates and drug abuse in Indiana declined in 2021 and 2022. There was a resurgence in 2023.
1 in 9 Indiana sixth-grade students attempted suicide one or more times.
1 in 5 Indiana tenth-grade students attempted suicide one or more times.

Age-adjusted Suicide Rate per 100,000 people (2013-2022)
Indiana has a state average of 21.59 percent of any mental illness. Delaware County falls between 22.5 and 22.9 percent — a whole percentage point higher than the entirety of Indiana. The Midwest had the highest percentage of serious mental illness at 4.32 percent, slightly higher than the national average of 4.13 percent.
Source: Indiana Family and Social Services Administration

If you or someone you know is experiencing a mental health crisis or thinking about suicide, call


With postpartum healthcare entering the conversation, there are options for pregnancy mental health support.
From the moment someone finds out they’re going to have a baby, they have immediately signed on to what can feel like countless
When things go smoothly, pregnant people can expect ultrasounds, bloodwork, fetal monitoring, genetic testing, vaccinations and more at their
With the amount of appointments, the mental health of those who are pregnant can sometimes be overlooked. The cries of a child can often drown out the silent pleading for help that often comes
Associate Lecturer of Health Science at Ball State University Jean Marie Place, who is also a maternal and child health researcher, said that simply put, the mental health of pregnant people matters because everyone’s mental health matters.
symptoms of depression or anxiety,” Hess said via email.
Open Door has a behavioral healthcare program included in their maternity care, and they screen patients throughout pregnancy and postpartum for perinatal mental health disorders (PMHD). They also have both individual and group counseling and provide education about mental health throughout pregnancy.
Hess explained that depression and anxiety can impact new parents, including those who don’t carry the child. She said 1 in 10 fathers experience postpartum depression, and adoptive parents can also experience postpartum depression and other mental health concerns.
“Becoming a parent is such a significant life change and has a profound impact on a person’s sense of self and their ability to cope with dayto-day stress,” Hess said via email. “Sleep is also a major factor to consider, and oftentimes, sleep deprivation can exacerbate mental health issues as well.”
I’ve had to initiate some of those conversations, but it’s so worth it to feel like I’m not alone, and people want to help.”
- LEA WATSON, Mother
“Regardless of whether they’re pregnant or not, individuals from a human rights framework deserve to be mentally healthy,” Place said. “When you put pregnancy into the picture, it’s important as well because being mentally healthy during pregnancy is going to have some pretty long-term implications on children.”
According to Frontiers in Psychiatry, when it comes to perinatal depression — depression during and/or after pregnancy — the growth of the fetus is at risk, resulting in low birth weights as well as earlier delivery. Additionally, it can lead to the development of insecure attachment and problems in social-emotional, neurocognitive, language and motor development.
Dr. Corie Hess is a behavioral health provider at Open Door Health Services and is the founder of the Muncie Maternal Mental Health Coalition, which helps new parents find specialized mental health care through community partnerships. She encouraged those whose mental health causes significant distress or gets in the way of their ability to care for themselves to seek help.
“Emotional well-being is just as important as physical health. Just as someone might share physical symptoms with their provider during an OB[-GYN] visit, it is also important to share
Place echoed Hess, saying that part of the mental strain of being a new parent comes from it simply being an “incredible adjustment.” But on top of that, she said it’s a combination of hormones. About 7 to 20 percent of pregnant people are affected by depression, but they’re more likely to develop depression and anxiety during their first year after childbirth, according to Mental Health America. The organization found that 70 to 80 percent of pregnant people experience negative feelings or mood swings a few days after giving birth, generally due to hormones.
Lea Watson moved to Muncie to start The Navigators ministry at Ball State with her husband Logan in 2019. Watson is currently a mother of two and is expecting her third, but this is her fourth time being pregnant.
Watson and her husband experienced a miscarriage after their first conception, which has caused a lot of anxiety throughout her other pregnancies, especially in her first trimesters when pregnancy is “more fragile.”
According to Frontiers in Global Women’s Health, those who experience a miscarriage are more at risk of developing depression, anxiety and PTSD for subsequent pregnancies.








Ball State head coaches share their own experiences with mental health and how they are helping their student-athletes deal with their struggles.


The Mid-American Conference (MAC) announced that junior forward Delaney Caldwell has been named the MAC Offensive Player of the Week. This honor comes after Caldwell accumulated seven overall points on the week, including goals in each of the Cardinal’s three matches. This is Caldwell’s first MAC Player of the Week honor and Ball State soccer’s first of the season.
Ball State football is set to travel to Florida Sept. 14 to face the No. 10 ranked Miami Hurricanes. This game will mark the ninth time in program history that the Cardinals have taken on an Associated Press Top 10 team. Ball State enters the game after a 42-34 victory at home over Missouri State. The game also marks the beginning of a three-game road trip for the Cardinals.
Ball State Athletics Hall of Fame member and former Ball State men’s volleyball player Greg Romano will officially be inducted into the Midwestern Intercollegiate Volleyball Association (MIVA) Hall of Fame. Romano will be inducted Nov. 2 at the MIVA Hall of Fame in Columbus, Ohio. After his time as a Cardinal, Romano finished top five in Ball State history for career kills.











































































































































sept. 25 10 - 1:30





With an increasing number of athletes speaking up about their mental health struggles, Ball State coaches share their own experiences and how they help their players.
Derran Cobb Associate Sports Editor
It’s 6:30 a.m., and as Ball State football players begin to make their way into Scheumann Stadium, one man stands there greeting each athlete.
Before any football begins, head coach Mike Neu finds it important to welcome in his players and have conversations with his team — ones unrelated to the sport.
Not every conversation between him and the athletes centers around practice or approaching games. Out of all the discussions he has with his players about their struggles off the field, his main point of emphasis centers around one thing. You are not alone.
According to The American College of Sports Medicine, approximately 30 percent of women and 25 percent of men who are student-athletes report having anxiety. Only 10 percent of all college athletes with known mental health conditions seek care from a mental health professional.
Neu has made a point to get to know everything about his athletes, to show them they are more than just football players.
Every night for the two-and-a-half weeks of training camp, he had each player and staff member share their story, asking them questions like: Where are you from? What have you been through in your life? [Who is] a hero in your life? [What is] a hardship you’ve faced in your life?
“Every time I go through that exercise, it just fascinates me what some young people have already experienced at this point in their life, some of the deaths, some of the tragedy, some of the violence, some of the things that they’ve been exposed to already at such an unbelievable young age,” Neu said.
He said having every player share the things they have gone through in life lets others who are struggling know that there is another person on their team who has dealt with the same thing.
“That just brings people together, and all of a sudden, they form an instant bond because they had something similar take place in their life. To me, that’s when you know I am not alone,” Neu said. “… To me, that’s powerful, and that’s one of the best things that we do.”
Head men’s volleyball coach Donan Cruz shares the same belief that when athletes find a common connection, it creates a healthier atmosphere.
“Probably the most significant barrier that we face is you’re always trying to figure out a one-size-fitsall type of mentality, and it’s unrealistic,” he said. “What is a struggle to me might not be the same for someone else … I think then [connecting about mental health] creates a more positive group. You have a more positive environment and then our goal is [that] we’re trying to thrive and be successful.”

30% 25% 10% of all college athletes with known mental health conditions seek care from a mental health professional.
Source: American College of Sports Medicine 10% 30% 25%
- MICHAEL LEWIS, Head Men’s Basketball Coach of female student-athletes report having anxiety. of male student-athletes report having anxiety.
He also knows how important it is for his athletes to know that their coaches are on their side. Similarly to Neu, Cruz and his staff are readily available for their players, having conversations with them that are not strictly volleyball-centric.
“I think just that small gesture, ‘Hey, you need someone to talk to, hit me up,’ goes a long way, and sometimes as a coach, you forget to just simply say that. So we try to make an emphasis on how accessible we are,” Cruz said. “[We] encourage guys to come up to our office and just come say hi. I think those things end up leading into a more open space for good dialogue.”
With more and more professional and collegiate athletes speaking up about their struggles, others find that they’re able to share their own experiences.
Cruz explains that when he was growing up — and even well into his 20s — telling someone you’re unhappy was seen as weak.
“The idea that athletes can find some safe space in saying, ‘Hey, I could talk about the fact that I’m dealing with some pressure,’ [is] not a sign of weakness. Being able to share that now, I almost feel it’s, in some respect, a sign of strength,” Cruz said.
Head men’s basketball coach Michael Lewis echoes this.
knows these individuals are more than just studentathletes. Behind the sport, they are human, and sports are not forever.
“We try to develop the whole person. We’re not just renting them as basketball players. We want [them] to become good students. We want to get them involved in the community where they’re productive people when they leave here,” Neu said. “ I want them to be great husbands and fathers down the line. I want them to provide a great life for their family.”
While student-athletes of course have a lot on their plates, so do their coaches. They also deal with long nights, extended road trips, pressure to succeed, and having to spend time away from their family and friends. Lewis even said he spends more time around his players than he does his own children sometimes. How do they deal with it?
Balance.
I think it’s something that, for a long time, was kind of put on the back burner, especially on the male side, because you don’t want to feel like you’re admitting weakness or different things like that, and that’s not the case.”
“I think it’s something that, for a long time, was kind of put on the back burner, especially on the male side, because you don’t want to feel like you’re admitting weakness or different things like that. And that’s not the case,” Lewis said.
Student-athletes have a lot of things to deal with — from showing up to practices and workouts at the crack of dawn to preparing for exams to worrying about their in-game performances and the possibility of injury. On top of that, they have their own everyday issues to deal with whether it be socially, financially or something personal.
Because of this, mental health often falls to the back of their list of priorities.
Lewis finds it especially important because he
“I try to keep a balance. When I can be with my family, I try to be present. I try to leave work at work. But obviously there [are] some times [where] if I’m going to be around my family, I’ve got to take work home,” Lewis said. “I don’t get the quantity that maybe others get, but [I] make sure the time that I do have is quality time with them, and just letting my family, especially my two daughters, understand that they always come first.”
Neu relies on his wife and his faith.
“Every week as coaches, we have Bible study on Thursdays and that helps — just talking about something besides football and to know that you always have that as part of your life, front and center,” Neu said. “I think [it] is really important for me because I’ve always left every Bible study that we’ve had together on Thursday feeling great.” With more athletes and coaches speaking up and finding support for their struggles, perhaps the stigma can fade.
Contact Derran Cobb via email at derran. cobb@bsu.edu or on X @Derran_cobb.

‘It’s







High school sports are said to help with studentathlete’s mental health struggles.
Zach Carter, David Moore Sports Editor, Associate Sports Editor
Mental health has become an increasingly talked about topic in the sports world. Many professional sports organizations often promote the importance of mental health. The Indianapolis Colts are a prime example of this. In 2020, the Irsay family kickstarted the “Kicking the Stigma” campaign to help raise awareness and support athletes struggling with mental health.
While such campaigns get as much recognition as they do, some of the lower-level and younger athletes can often be forgotten. Specifically concerning high school athletics, mental health problems begin in this time of adolescence.
“We as coaches — and the athletes themselves — put so much pressure on [ourselves] to perform well,” Wapahani volleyball head coach Valorie Wells said. “They want to do well for the school and community, so they put a lot of pressure on themselves, which kids aren’t really used to.”
Since many new aspects of life come to high school students at a rapid pace, students can struggle to handle the stress, Wells said. Then, there’s the added pressure of reaching peak performance in a sport one’s been playing since childhood.
“All kids want to be the star player,” said Matt Luce, Wapahani athletic director and boy’s basketball head coach. “But the best leaders bring their kids and teammates together to help them learn a role and just enjoy being a teammate of a high school team.”
It’s not always a rosy path. Everybody wants to win and be the best player, but it’s about going through the struggles of a long season, being unselfish and playing your role.”
- MATT LUCE, Wapahani athletic director
I’m glad now it’s an open mindset where kids can go talk and be vulnerable and share their feelings.”
- CHRIS OVERHOLT, Delta head football coach
Yet, some programs are taking this challenge head-on in the way athletes are trained and how they are coached. Delta athletic director Tilmon Clark has that idea on his checklist when hiring a new head coach.
“When I hire a coach, I have to be able to know that coach is going to have a connection with student-athletes and have them ready to compete and want to have fun at the sport,” Clark said.
While Delta head football coach Chris Overholt was hired in 2016, the former Eagles football player wanted to incorporate ways to check on his athletes. Whether that was meals with the team or one-on-one meetings with the staff, the blue and gold are trying to find ways to make sure everyone is in a good place before stepping on the gridiron.
“We even have after-practice meetings with players where they get into position groups,” Overholt said. “We like to do a check-in with the kids and most of the players have their coaches and my personal phone number. We pride ourselves on relationships in our program.”

One of the biggest obstacles many students face is getting out of the mindset that there is something wrong with them if they admit to struggling mentally, Wells said. She encourages her players to seek help from a counselor if they feel it’s needed, as she has sought out professional help herself.
“I tell them from the beginning, ‘You come first,’” Wells said. “I make sure to tell them it’s OK to see a counselor, and I share with them that I have my issues too and that I see a counselor. It’s really about making them feel like they aren’t alone.”
A large part of the emphasis in Wapahani’s program begins with connecting with the studentathletes off the field. Building relationships and continuing to foster those is a crucial aspect of ensuring that students feel seen for who they are as a person, not just as a player.
“The best coaches are the ones that see the kids off the court — the ones that see them in the classroom, or in the hallway saying hi to them, or seeing them in the study hall and checking on their studies,” Luce said. “The coaches that are able to find time off the court and off the field to get to know them as a student-athlete have the most success because they’re the ones who see them every day in the hallway.”
One of the hardest things is balancing the fine line
between how much energy to put toward school and how much to put toward sports, Luce said. Finding that balance can be a challenge at times.
“Sports is a great way to learn about life because it’s not always easy,” Luce said. “It’s not always a rosy path. Everybody wants to win and be the best player, but it’s about going through the struggles of a long season, being unselfish and playing your role. That’s a large part of why I decided years ago to be a teacher and coach.”
It’s the same thing Wes-Del athletic director and head football coach Matt Nuckols has noticed in his time with the Warriors.
“I think that’s a big piece when we start talking about how mental health is affecting some of our athletes,” Nuckols said. “We try to teach them in our games and our practices that things won’t always go right — how to handle things when they do go well but also how to fight through and deal with those issues.”
With Wes-Del being one of the smaller schools in Delaware County enrollment-wise, Nuckols believes that aspect plays a big part in the process.
“Our teachers in the building pretty much have every kid that comes through here for the most
They want to do well for the school and community, so they put a lot of pressure on themselves, which kids aren’t really used to.”
- VALORIE WELLS, Wapahani volleyball head coach
part,” he said. “So those players make connections with coaches and teachers that are there for them.
That’s just a perk to being in a close-knit, strong community and small school like ours.”
The close-knit community at a smaller school is said to be helpful due to student-athletes being able to see each other often. With that aspect, it may help some students be able to talk openly with others when they need someone to help with more than their athletic skills.
Whether mental health becomes something that high school athletic departments embrace more in the future, the change that has occurred over the last 20 years is something current coaches and directors are happy to see.
“I’m definitely happy it is the way it is now,” Overholt said. “I think there’s always the stigma, especially with boys, ‘Don’t cry [and] don’t share your feelings. Just be tough.’ I’m glad now it’s an open mindset where kids can go talk and be vulnerable and share their feelings.
“It’s important, and it’s something I buy into. I know I have people that I talk to — that I can share with — and it’s definitely nice having those avenues in my life.”
Contact Zach Carter via email at zachary. carter@bsu.edu or on X at @ZachCarter85 and David Moore via email at david.moore@bsu.edu or on X @gingninj63.






The Mississinewa River has brought me comfort throughout my life.
‘I don’t know what the rest of my days look like, but fishing will never go away.’

Zach Carter
Sports Editor, “Carter’s Comments”
Zach Carter is a third-year journalism major and writes “Carter’s Comments” for the Daily News. His views do not necessarily reflect those of the newspaper.
“You know a dream is like a river Ever changin’ as it flows And the dreamer’s just a vessel That must follow where it goes Trying to learn from what’s behind you And never knowing what’s in store Makes each day a constant battle Just to stay between the shores.”
That’s the opening verse of Garth Brooks’ song “The River.” As a child, I didn’t understand what Brooks was trying to say.
However, Jan. 14, 2022, was one of those days where it was hard to stay between the shores.
Around 10 p.m. that evening, I received one of the worst phone calls of my life. My mom called to tell me that my grandma Marsha passed away in the hospital after dealing with a brief illness. Being 20 minutes away at the time, I grabbed my keys and raced home.
Two minutes into the drive, I knew I was going too fast. I was in shock and a breakdown was looming. That’s when I turned down a little side road that led to a spot I was all too familiar with. When my tires hit the gravel lot, I put my 2006 Chevy Silverado in park. My head hit the steering wheel and tears began to fall on my lap.
The spot I mourned for my grandma was my second home: the Mississinewa River.
For some, a safe space could be anything. It could be a restaurant, a loved one’s house or even their bedroom.
But for me, it’s always been the river.
My grandpa Edward still lives in the only house my grandparents have ever owned. The neighborhood sits on the Mississinewa River, which became the place where I’d spend hours.
I understand that for some people, fishing is boring. I can’t argue that there aren’t times when nothing happens. But when a fish takes the bait, everything quickly goes from 0 to 60. It’s thrilling, sometimes scary and fun all at the same time.
My grandpa and I aren’t the type of fishermen that target certain fish. One day it’s bass, and the next day it could be carp or catfish. To us, it doesn’t matter. What mattered was the enjoyment.
When I was growing up, there were many life lessons I learned while sitting next to him on the bank. Telling me to attend college, to stay out of trouble. And the stories he told me about his life all remain in my mind and heart.
Nowadays, I don’t get to fish with him as often due to my busy schedule. However, I soon hope that changes.
While I would say those moments are my favorite part of fishing, other things stick out. As a guy who has spent time walking, kayaking and camping along the water, I have started to pick up on some things.
One of my favorite things about a river is its characteristics. Some rivers are slow-moving and shallow. Others have fast rapids, and you have to hit the holes throughout the stretch. To me, it’s always been fascinating to think about what a stretch looked like 50 years ago. Due to flooding and farming, land can change and rivers flow differently.
But it’s not just the river itself that draws me in. Seeing wildlife and the wonders of the natural world reminds me that the wilderness remains even after human contamination.
For some reason, that realization always made me happy in a way. It proves our species hasn’t ruined everything on this once-wild planet. It shows that nature prevails.
Since my grandma passed, all of those thoughts have resonated more deeply.

I was tested once more last semester as my mental health was put to the test again. For the first time in my young journalism career, I hit writer’s block. At the same time, my great-uncle Carl was battling cancer.
Throughout that time, two things kept me from losing it: a few friends and fishing along the river. I’d sit on the bank for hours as I tried to put together a simple lede for my next writing venture. I was constantly questioning whether or not my ability to write freely and easily would return.
Eventually, my uncle lost his battle and was gone. The river was there once again as a place where I could cry and be away from the world.
I write all this and think about the rest of my life.
While my mental health has been solid for most of my 20 years, the moments where it was hard to go on were fixed when a rod was in my hand and there was water in front of me. I don’t know what the rest of my days look like, but fishing will never go away.
According to a study by the National Library of Medicine, researchers found that anglers experienced an improvement in their mental health during the COVID-19 pandemic. That idea goes along with my experiences, as the memories will never fade and the feeling of a trip’s first catch will never get old.
However, when my life ends, I know two things. One, I hope my friends and family remember the good times. I hope they go fishing for themselves and enjoy the place where I was at my happiest. Second, I hope it ends like how another country artist, Kameren Marlow, describes the moment in his song “On My Way Out.”
“On my way out, when it’s my time to go I hope the road to get there goes by my old fishing hole I hope the one that broke my line is still swimming around ’Cause I’d like to try him one more time.”
Contact Zach Carter via email at zachary.carter@bsu. edu or on X @ZachCarter85.










Ella Howell is a fourth-year journalism major and writes “The Down-Low” for the Daily News. Her views do not necessarily reflect those of the newspaper.
ntil my last year of middle school, I remained in a blissful state of ignorance.
I often questioned the origins of mental illness but could never understand the fact that some people woke up daily plagued with an indescribable sadness.
There’s a very specific feeling of lightness that comes with that state of ignorance. But it really isn’t possible to grasp until it’s no longer there.
Before being diagnosed with depression and anxiety, which began a daily regime of taking a specially curated cocktail of antidepressants, I started to become very self-aware of my presence and appearance at all times.
To a certain extent, that was a normal aspect of my age at the time, but there was an accelerator adding fuel to that hormonal fire.
By my second year of high school, I was very confused about my identity and was extremely self-conscious.
The diminishing state of my mental health, in an already challenging time in adolescence, kept me from realizing the main issue: my mom’s mental health.
I’ve always been compared to my mom and viewed as being just like her. I’ve been told countless times that I look like her, sound like her and act like her. As the state of her mental health plummeted, it was no shock to me that mine followed right behind.
Children with a parent who has a serious mental illness (SMI) are 50 percent more likely to develop a mental health problem and 32 percent more likely to have a SMI themselves, according to the National Library of Medicine.
My own mother was responsible for some of the worst things that have ever been said or done to me. Other adults I was supposed to trust developed a tainted perspective of me because they saw me through the lens of someone with a severe mental illness. I felt very alone and began to isolate myself.
I began to pull away from all of my friend groups, became more introverted and started engaging in selfdestructive behavior. By my third year of high school, I had one close friend, and I had never connected with another person the way I connected with her. I think I recognized a similar internal struggle in her that I was experiencing within myself.
When my mom threw soda at me in our kitchen, she was the person I called as it dripped out of my hair and into a sticky puddle by my feet. When my father told me he thought it was best if I didn’t come home for the night after talking to my mom, I cried in her car as she called her parents to tell them I was sleeping at their house.
Without her, I truly believe I wouldn’t have made it through that time in my life.
But both of our mental states grew to become mutually destructive.
During a time when I was at my worst, I turned to what I thought was my only safe space. Looking back, I realize while acting as a haven for one another, we were also causing harm.
My friend’s parents decided that our relationship was not good for each other, and they were right. After being cut off from one of my few sources of support, I was devastated.
As my mom’s mental health worsened and I got older, I tried to have conversations with her that something wasn’t right and that she should seek professional help. Those conversations never went over well. After multiple unsuccessful conversations, combined with the fact that I was leaving for college in less than a year, I gave up trying.
Just two months after my mom’s diagnosis, I was tucked under a blanket in the dark, watching back-toback episodes of Gilmore Girls — a normal ritual for me with an endless queue of shows — when I heard my doorbell ring. A few minutes later, there was a knock at my bedroom door.
I told who I assumed was my mom to come in without even sitting up, hoping to avoid another confrontation about what I did all day, but I heard my friend’s voice for the first time in six months as she walked through my door.
I sat up, again with the false expectation that this would be the magical solution to my poor mental state. She explained to me that she told her parents she was leaving, packed a bag and made the over five-mile trek to my house on foot.
After talking with my parents, she moved in with us and stayed in my room with me. The first few weeks were fine; I had my best friend back in my life. But it slowly shifted as I saw a lot of similarities in her. Not with myself this time, but with my mom.
I recognized the harm she was doing not only to my mental state but to my already emotionally vulnerable family. After two months of her living at my house, there were a few too many instances that left me and my family worried about her.
Her dad came to pick her up and take her back home. Shortly after, she received the same diagnosis my mom had just months before. This time, the emptiness of her presence in my life left me with more of a realization than a sense of desolation.
After being surrounded by turmoil and instability for a few years, I truly believe that mental illness can be contagious. It is part of our responsibility to those around us to find a way to prevent our poor mental health from feeding each other and spreading to our loved ones. Whether you need medication, to speak with a therapist or a simple change in routine, not only do you owe it to others, you owe it to yourself to escape from that shared anguish.
It is easy to fall into a cycle of mutual destruction with the people you’re supposed to love, and admitting you need help is one of the first steps to breaking that cycle.
Contact Ella Howell via email at ella.howell@bsu.edu.
Anosognosia is a condition that keeps someone from recognizing the state of their health. It is very common among people with certain mental conditions. According to the Cleveland Clinic, 40 percent of people with bipolar disorder experience this.
When I wasn’t out with my friend, I was at home in my bed, avoiding my mom to preserve what little energy I had. I sobbed almost daily for hours for absurd reasons. Getting showered and dressed for the day was a win.
In March of 2021, three months after I graduated high school, my mom was diagnosed with bipolar disorder after an episode of psychosis. Due to a lack of treatment for her mental health, her mind just crashed out.
I thought her getting better would be a magical fix to all of my problems, but it wasn’t. I felt guilty for the years of damage to my relationship with my mom. I felt I could’ve done more to protect the connection we had when I was younger.
Continued from Page 12
In Watson’s experience, the conversation surrounding pregnancy and mental health has been more focused on postpartum mental health. She has discussed the topic, but mainly with her close friends.
“We all have gotten pregnant together around the same [time]; we definitely have shared the highs and lows of pregnancies together,” Watson said. “I would say there’s a pretty negative view around birth in general … I haven’t heard a positive birth story in a really long time.”
In addition to hormones and adapting to life changes, Hess also emphasized that pregnancy is not necessarily always the root of mental health struggles. Pregnancy can also exacerbate symptoms of mental illness that were already present before the influx of hormones. Watson has struggled with anxiety since college, where she sought out counseling. Following the loss of her first pregnancy, childbearing became a specific source of stress for her.
She wants others who may find themselves in a similar position in their pregnancy to know that they are not alone. She said great parents have had some “really scary thoughts” during those unprecedented times.
“I’ve had to initiate some of those conversations, but it’s so worth it to feel like I’m not alone, and people want to help … If you’re feeling depressed first, that’s normal, and you’re not alone,” Watson said. “If it’s impacting your daily life, definitely don’t be ashamed to reach out to your doctor.”
Watson highlighted that the best way to care for the baby is to manage the health of the person carrying them, especially their mental health.
Some resources in Muncie include the Muncie Maternal Mental Health Coalition; Ball State also has a Counseling Practicum Clinic where Place said there are student clinicians trained to deal with PMHD. The Muncie YMCA also has a support group led by “doctoral-level students from the Ball State Counseling Center” in partnership with Hess’s coalition.
Hess encourages those struggling to also seek online support groups. She wants people to know they’re not alone, it’s not their fault and support is available.
“Postpartum Support International is a great organization that has free virtual support groups that anyone can attend,” Hess said via email. “There is also the National Maternal Mental Health Hotline [1-833-TLC-MAMA]. This is a free, confidential hotline that new parents can call or text 24/7 to get support.”
Place said that there are a variety of options and strategies to help you or your loved ones get through difficult times.
“There’s a lot of stigma around maternal mental health, unfortunately, and so I think one of the most important things someone could do is listen,” Place said. “Try to offer that ordinary magic of empathy.” Contact Ella Howell via email at ella.howell@ bsu.edu.

first pregnancy, childbearing became a source of stress for
Continued from Page 07
In addition, seeking professional support, whether through on-campus counseling services or off-campus resources, can provide students with personalized coping strategies and ongoing emotional support throughout the season.

For Piazzoni, something that worked for him was finding a support system.
“One [strategy] is to find a group of friends that you trust,” he said.
Piazzoni also believes that “college is more about embracing what we want to do and what our interests are,” emphasizing the value of engaging in activities and joining clubs that align with personal interests.
By taking advantage of these resources and personal coping strategies, students can better manage the effects of seasonal depression and maintain their academic performance and overall quality of life throughout the winter months.
“You’re not alone,” Piazzoni said. “Your experience is uniquely individual to you, and you’re not alone in how you feel.”
Contact Meghan Braddy via email at meghan. braddy@bsu.edu or on X @meghan_braddy.
Peppery salad slice
Poem division
Muse for poets
Part of one’s inheritance?
“Sound Mind, Sound Body” athletic brand
“Dune” and “Dune: Part Two” director Villeneuve
DOI head Haaland
Raised trains
“__ Christmas!”
Apple tablets
Confidentiality contract, for short
Less stuffy
Had a feeling
Primps
Went for a run?
Novelist Calvino 48 “Behold!”
49 Christine of the Paramount+ series “Evil”
Coach
Rae of “Barbie”
Sound of shame
Spanish “Of course”
__ shorts: garment with lots of pockets
Hoppy brew, for short
Cartoon frame
Pillbox, for one























With over 12 options for birth control, let’s find one that works for you.


