The kind dedicated to serving the underserved.
The kind who hasn’t missed any of her children’s soccer games.
CCHCS offers a competitive compensation package:
• 40-hour workweek (affords you true work-life balance)
• Generous paid time off and holiday schedule
• State of California retirement that vests in 5 years (visit CalPERS.ca.gov for retirement formulas)
• Robust 401(k) and 457(b) savings plans (tax defer up to $46k – $61k per year)
• Paid CME, with paid time off to attend
• Paid Insurance, license, and DEA renewal
• And much more




The kind who wants off the HMO treadmill.
By now, doctors know California Correctional Health Care Services (CCHCS) offers more than just great pay and State of California benefits. Whatever your professional interest, CCHCS can help you continue to hone your skills in public health, disease management and education, addiction medicine, and so much more. All without the burdens of battling insurance companies or unrealistic RVUs.
$311,496 – $336,900 (Time-Limited Board Certified)
$295,884 – $320,028 (Lifetime Board Certified)
$280,344 – $303,216 (Pre-Board Certified)
*
$358,224 – $387,432 (Time-Limited Board Certified)
$340,272 – $368,028 (Lifetime Board Certified)
$322,392 – $348,696 (Pre-Board Certified)
*Doctors at select institutions receive additional 15% pay.


816 21st Street, Sacramento, California 95811 www.familydocs.org (415) 345-8667 cafp@familydocs.org
President
Alex McDonald, MD, CAQSM, FAAFP
Immediate Past President
Raul Ayala, MD, MHCM
President-elect
Anthony Chong, MD, FAAFP
Speaker
Kim Yu, MD, FAAFP
Vice-Speaker
Brent Sugimoto, MD, FAAFP
Secretary/Treasurer
Jorge Galdamez, MD
Chief Executive Officer
Lisa Folberg, MPP
Foundation President
Ron Labuguen, MD, FAAFP
AAFP Delegates
Lee Ralph, MD
Lisa Ward, MD, MPH, FAAFP
AAFP Alternates
Shannon Connolly, MD, FAAFP
Alex McDonald, MD, FAAFP
CMA Delegates
Kimberly Buss, MD
Felix Nunez, MD
Sumana Reddy, MD, FAAFP
CMA Alternate Delegates
Robin Linscheid Janzen, MD, FAAFP
Noemi Doohan, MD, PhD
Adia Scrubb, MD, MPP
David Tran, MD
Scott Nass, MD, MPA, FAAFP, AAHIVS, Editor
Josh Lunsford, Managing Editor
Lisa Folberg, MPP Chief Executive Officer lfolberg@familydocs.org
Karen Alvarado Advocacy Assistant kalvarado@familydocs.org
Anita Charles Manager, Educational Programs acharles@familydocs.org
Morgan Cleveland Manager, Operations & Governance mcleveland@familydocs.org
Jerri Davis, CHCP Vice President, Professional Development, CME/CPD jdavis@familydocs.org
Laurie Isenberg, MILS, CHCP Director, Education and Professional Development lisenberg@familydocs.org
Christine Lauryn Manager, Member Communications clauryn@familydocs.org
Josh Lunsford Vice President, Membership & Communications jlunsford@familydocs.org
Pamela Mann, MPH Executive Director, CAFP Foundation pmann@familydocs.org
Marissa Montano, PhD Vice President, Advocacy & Policy mmontano@familydocs.org
Jonathan Rudolph Manager, Finance jrudolph@familydocs.org
Tiyesha Watts Legislative & Policy Advocate trwatts@familydocs.org

The California Family Physician is published quarterly by the California Academy of Family Physicians. Opinions are those of the authors and not necessarily those of the members and staff of the CAFP. Non-member subscriptions are $35 per year. Call 415-345-8667 to subscribe.
pcipublishing.com




Alex McDonald, MD, CAQSM, FAAFP CAFP President
The "Amazon generation," representing individuals who have grown up in the era of digital convenience and on-demand services, has and will continue to have a profound impact on health care in several ways. This generation often values and promotes the principles of consumerism, customer service, choice, value, and quality. Yet do these principles neatly apply to a complicated, nuanced, and sometimes emotionally charged industry such as health care?
Health care, often considered a service industry, faces a myriad of challenges and barriers that distinguish it from conventional markets that are currently creating shifts and tension with the “Amazon Generation.” Unlike typical service sectors where market pressures and consumerism play a pivotal role, health care grapples with unique complexities that stem from the nature of its services, ethical considerations, and the critical importance of patient wellbeing.
One of the primary challenges in health care lies in the asymmetry of information between physicians and patients. Unlike other service industries where consumers can make informed choices based on readily available information, health care often involves intricate medical knowledge that is beyond the understanding of the average person or requires extensive experiences and understanding of how medical knowledge applies to a specific individual or situation. This lack of common knowledge and experience hinders the ability of individuals to shop around for services and make truly informed decisions about their health.
Furthermore, the urgency and unpredictability of health care needs, particularly in emergency settings, limit the application of market pressures. In emergencies, individuals do not have the luxury of time to shop for the best deals or consider alternative options. The critical nature of health care services, where timely intervention can be a matter of life and death, diverges from the traditional market dynamics that rely on competitive choices.
Insurance networks further complicate the application of market principles in health care. Many individuals find themselves restricted to narrow networks, limiting their choice of health care providers. This lack of flexibility can lead to challenges in accessing specialized care or receiving services from preferred providers, thus undermining the consumer-centric model seen in other service industries.
The cost structure of health care, often shrouded in opacity, poses another barrier. Unlike markets where pricing is

transparent, health care costs can be hidden, convoluted, and impossible to discern. Patients may face unexpected bills, and the lack of price competition can contribute to the perpetuation of high health care expenses. This lack of cost transparency undermines the principles of market-driven consumerism, where individuals are empowered to make choices based on price and quality.
Moreover, the ethical dimensions inherent in health care introduce a layer of complexity not encountered in typical service industries. The primary focus of health care providers is on patient welfare and adherence to ethical standards, which may at times conflict with market-driven incentives. The obligation to prioritize the best interests of the patient may diverge from profit-oriented motives that dominate many service sectors.
Many younger individuals now prioritize personalized, patientcentered, user-friendly, streamlined, tech-enabled, convenient care––sometimes with a specific diagnosis and treatment in mind before they interact with the health care system. Many of the complexities of the traditional delivery of health care, articulated above, are at odds with many of the on-demand services expected by the Amazon Generation.
This generation and rise of consumerism are pushing the health care industry to adopt new ways of delivering care. Some of these changes show promise to improve the patchwork and dysfunctional health care system in the United States. The demand of information accessibility and health portability is forcing data exchange services and health care systems to communicate and coordinate in new ways. Price transparency is getting the attention of many in the health policy world with ongoing work to try to better help avoid surprising billing and help patients understand costs before they go to the doctor. Wearable technology and Artificial Intelligence will continue to allow doctors to make better data-driven decisions and avoid human error, but should be noted, AI will not be able to ever provide the empathetic and personal care that many have come to expect. Patient empowerment and experience may help engage patients in their health care decisions and improve medication adherence or lifestyle choices to reduce or avoid health problems. Consumerism has contributed to a shift towards value-based care, where the emphasis is on delivering high-quality care and positive outcomes. Patients may be more likely to seek doctors who offer value in terms of both
continued on page 8

Pre-exposure prophylaxis (PrEP) is 99% effective at preventing HIV from sex when taken as prescribed, making it a game changer for ending the HIV epidemic. Yet, not enough people who could benefit from PrEP are prescribed it. You can help increase PrEP coverage by talking to all your sexually active patients about the benefits of PrEP.
CDC’s updated PrEP Toolkit contains resources for you and your patients, including:
• The latest CDC guidance on prescribing PrEP to prevent HIV.
• Posters about PrEP, available in both English and Spanish, to display in your practice.
• Strategies for starting conversations with your patients about PrEP.
• Information for patients about how PrEP works, its side effects, and how to pay for it.


continued from page 6






effectiveness and patient experience. Doctors and health care systems are compelled to enhance the quality of their services, adopt best practices, and differentiate themselves to attract and retain patients in a more competitive environment.
There are several aspects of consumerism of the Amazon Generation that may create new challenges or problems. Limited understanding of medical information may lead to misinterpretation of treatment options, potential non-compliance, suboptimal health outcomes, or wasted
centric approach, with multiple different points of contact with various care delivery models, may contribute to fragmented care coordination and increase risk. Perhaps most concerning, increased patient demand, expectations, and emphasis on consumer satisfaction can contribute to stress and burnout among health care professionals resulting in fewer doctors. Doctors may face challenges in managing patient expectations while maintaining clinical excellence, potentially affecting their well-being, job satisfaction, and bottom line.

unauthorized access, compromising confidentiality. Consumerism may contribute to the overutilization of health care services, driven by patient demand for unnecessary tests, treatments, or interventions. Without proper medical expertise, this can result in misinterpretation of symptoms, delays in seeking appropriate care, and potential health risks. A consumer-
Unlike typical service sectors where market pressures and consumerism grapples with unique complexities that stem from the nature of its services, ethical considerations, and the critical importance of patient and physician well-being. While the Amazon Generation brings positive aspects by empowering patients and fostering competition, it also raises challenges such as potential disparities in access to information, services, and low-value care. Striking a balance between consumer empowerment and maintaining the integrity of health care delivery remains a key consideration for the evolving health care landscape. Addressing these challenges requires a nuanced approach that considers the distinctive characteristics of health care while striving to balance transparency, quality, access, costs, and patient engagement all within a patientcentered, evidence-based decisionmaking process.










Tiyesha Watts
CAFP, Legislative and Policy Advocate
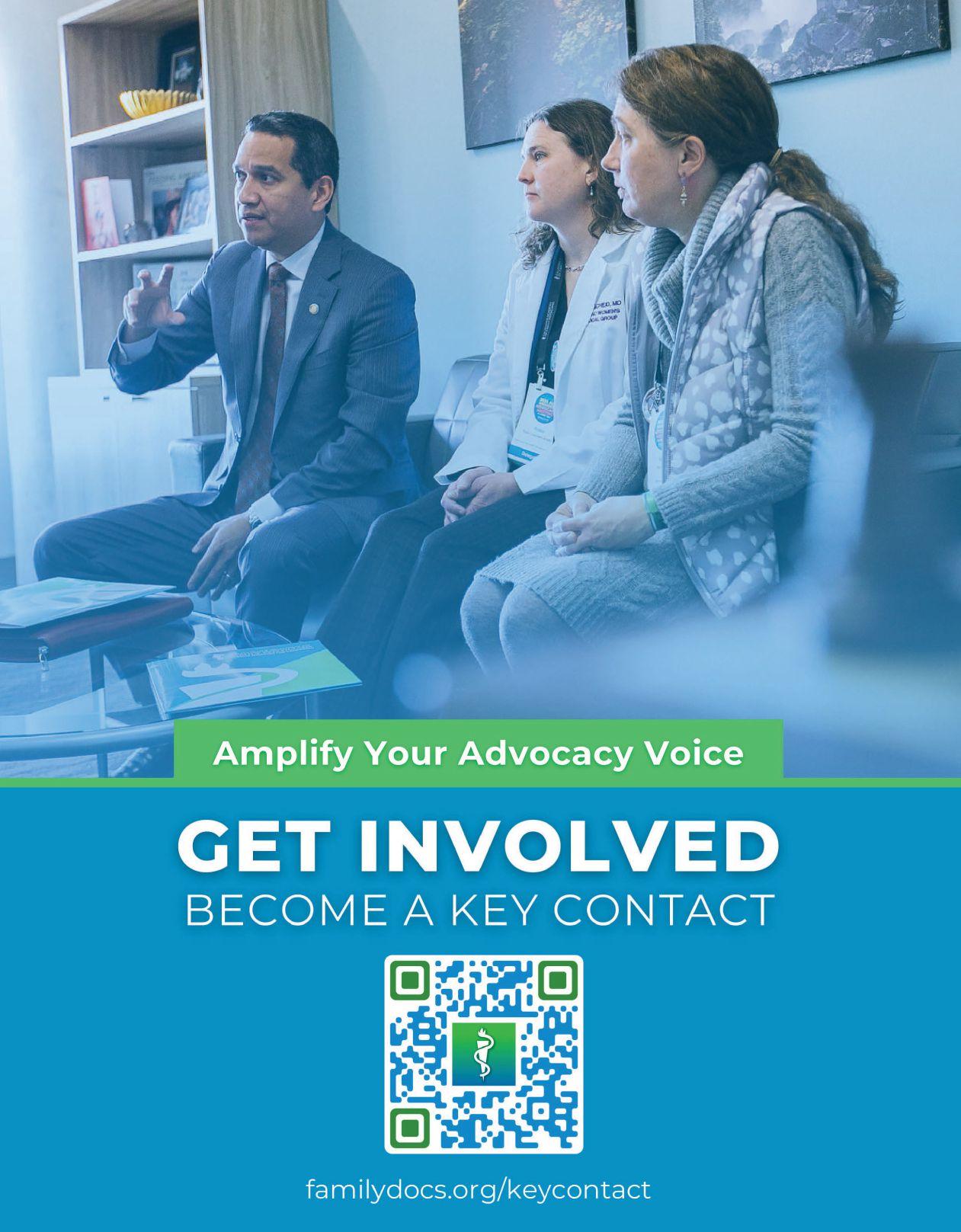
California’s family physicians are a force to be reckoned with. Our physicians are buzzing with the motivation to advance access and innovation in primary care. It is no secret that our current health care system is a system of sick care. It is also no secret that family physicians are leaders in proactive, person-centered, empathetic, and effective healthcare. Physician-led advocacy is an impactful way to translate the excellent patient care and clinical expertise of family physicians to public policy that can and should support gold-standard care for healthier, happier communities.
Throughout CAFP’s history, our physicians have always been passionate about patient care and in creating change to make healthcare more accessible and equitable. Not only has the passion grown over the years, but so has the volume of family physicians that recognize and use the power of their voices at the federal, state, and local levels. The most salient way that our members participate in internal and external CAFP advocacy is through the annual All Member Advocacy Meeting (AMAM)— which has been an evolving and growing part of CAFP over the years. The expanding engagement in advocacy is mirrored in the transition from the traditional Congress of Delegates (COD) between 2012 and 2016 to a more advocacy-oriented AMAM.
Historically, the COD provided a platform for delegates to discuss and vote on matters vital to family medicine. The transition to the AMAM added broader learning and engagement opportunities for members. AMAM represents more than just a format change; it embodies a commitment to inclusivity, and member engagement. The AMAM uplifts the passion and commitment to advocating for family medicine that is at the heart of the organization Through interactive sessions, workshops, and presentations, AMAM equips family physicians with the tools and knowledge to
advocate effectively for their specialty and patients, fostering networking, collaboration, and grassroots advocacy. Since its inception nearly ten years ago, AMAM has grown bigger and better with feedback from members.
This year, over 200 CAFP members gathered for AMAM on April 13-14 and Lobby Day on April 15. The weekend was filled with informative sessions, interactive workshops, and engaging discussions— many around the record number of CAFP resolutions submitted this year. Attendees heard from the Director of the Department of Health Care Access and Information, Elizabeth Landsberg on the state investments in primary care and how family physicians, like you, can (and do!) engage with the state department. The event also featured a keynote presentation by Dr. Margot Savoy that complemented the major advocacy efforts of CAFP around addressing the social determinants of health. AMAM attendees were also able to participate in training tracks about campaigns and elections and talking to legislators.
The weekend culminated in Lobby Day on April 15, marking the beginning of Family Physician Week, April 14-20, and the

opportunity to put the weekend advocacy lessons to the test. CAFP members spent the day engaging with legislators to discuss CAFP priorities and raise awareness of the importance of family medicine. At the peak of lobby day, the Family Physician Week resolution, ACR 165, was heard on the Assembly floor, receiving significant support from legislators. In a special moment, CAFP members in Assembly chambers were acknowledged for the excellent, frontline work of family physicians.
As we reflect on the success of the recent AMAM, CAFP looks forward to continuing the momentum in advocating for family medicine. Whether you were part of the magic this year, or missed out, save the date for next year's AMAM and Lobby Day, and make a difference in shaping healthcare policy that impacts you and your patients. Your voice and advocacy are indispensable in our collective efforts to strengthen family physician advocacy and promote optimal healthcare for all Californians. See you there!
Until Next Time: Mark your calendar to save the date for the next AMAM on March 15-16, 2025, and Lobby Day March 17!


Shannon Connolly, MD
Melissa Campos, MD

Three years ago, the CAFP Board of Directors met to develop a strategic plan. It was a weekend that built upon months of planning and preparation. The Board engaged in deep conversations about why we practice family medicine, what the CAFP’s role could be in healing society’s suffering, and how we might lead healthcare transformation. We listened to each other and challenged one another to set an aspirational agenda for our professional organization. We considered complex issues such as why we don’t have an adequate family medicine workforce and why the house of medicine struggles so much to achieve health equity. The strategic plan that came out of this created a clear directive to engage in justice, equity, diversity, and inclusion (JEDI) work. This was the beginning of the CAFP’s first JEDI task force.
Over the next year, the newly formed task force provided recommendations on how to enshrine these priorities into the very structure of our organization, so this work is enduring and


prioritized. However, it soon became clear that a temporary task force would not suffice. If the CAFP was to change the culture of our specialty such that future generations will consider health equity work as vital as anything else we do in medicine, we needed an enduring body to advance this work. Last year the Board approved the new, permanent JEDI Committee, and the following is a report on some of the work we have been doing.
One of the first projects of the JEDI Committee was to understand and gather baseline information on CAFP leadership and propose strategies for advancing diversity at the CAFP. In 2023, a 14-question survey was electronically sent to the CAFP’s Board of Directors and Alternates, members of the CAFPs committees, chapter presidents, NCCL Delegation members, the Student and Resident Council, and staff. The survey included questions about self-identified race, ethnicity, gender, age, sexual orientation, practice setting, disability status, and languages spoken. Of the 165 surveys that were sent out, 154 were completed, resulting in a 93 percent completion rate.
"Race is a social construct that is used to group people based on physical characteristics, behavioral patterns, and geographic location. Racial categories are broad, poorly defined, vary by country and change over time. People who are assigned to the same racial category do not necessarily share the same genetic ancestry; therefore, there are no underlying genetic or biological factors that unite people within the same racial category. By using race as a biological marker for disease states or as a variable in medical diagnosis and treatment, the true health status of a patient may not be accurately assessed, which can lead to racial health disparities.
The American Academy of Family Physicians (AAFP) opposes the use of race as a proxy for biology or genetics in clinical evaluation and management and in research. The AAFP encourages clinicians and researchers to investigate alternative indicators to race to stratify medical risk factors for disease states." (AAFP July 2020 BOD) (AAFP 2020 Congress of Delegates)
With full transparency, we recognize that there are fundamental methodological limitations in the collection of data regarding identities such as race, ethnicity, gender, and sexual orientation. Many datasets that are widely used and accepted rely on groupings of identities that do not adequately reflect the experiences or self-identifications of those people. We recognize that race is a social construct and people within the same racial category may have vastly different cultures, life experiences, languages, and geographic origins. We recognize that even the language we use to describe different identities is dynamic and subject to variable interpretation. With that context, we felt the data was still worth evaluating as a first attempt to understand who comprised our CAFP leadership.
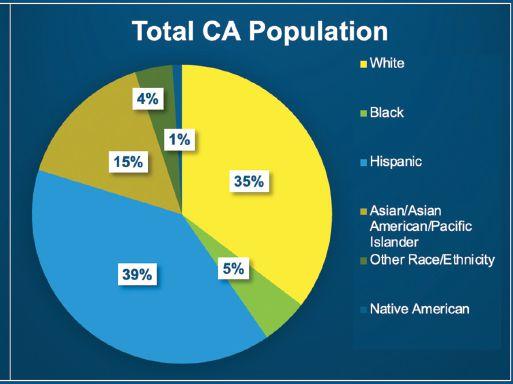
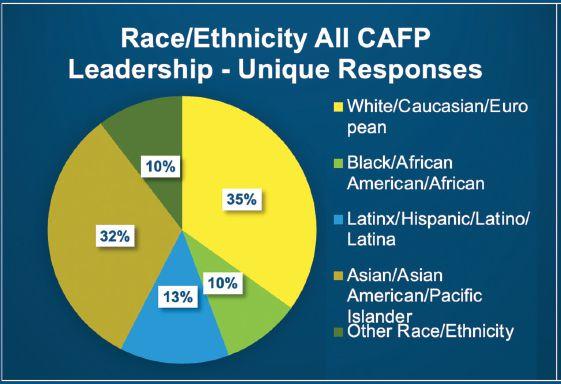
To provide context for the data that the CAFP collected in our survey, we attempted to use comparison populations when relevant. Data on comparison populations comes from a variety of sources and is limited by what is publicly available and the specific methodologies of those studies.
Some results of the survey are shown here:
Thirty-five percent of CAFP leadership identified as White/Caucasian/ European, 32% Asian/Asian American/ Pacific Islander, 13% Latinx/Hispanic/ Latino/Latina, 10% Black/African/ African American, and 10% other race/ ethnicity. Latinx/Hispanic/Latino/Latina individuals were underrepresented in CAFP leadership when compared to the population of the state of California. Sixtyseven percent of CAFP leadership identify as female, 30% male, and 3% Nonbinary/ Other.
As a committee, we recommended to the Board that the CAFP endeavor to have its leadership mirror the population of California, with an emphasis on adequate representation, and even permissive overrepresentation of historically underrepresented demographics. The Committee advocates for the inclusion of individuals belonging to many different identities in CAFP leadership. However, we proposed that the initial focus be on achieving proportional and diverse racial and ethnic representation, with the
understanding that this is just one of many steps towards addressing health equity. From our survey data, it is clear that there is a significant underrepresentation of Latinx individuals in CAFP leadership, and this presents a clear opportunity for action. The committee recommended that the CAFP strive to achieve significantly improved leadership representation by 2030.
To help achieve this representation goal, the Committee also provided the Board with specific strategies for recruitment, retention, and advancement of a more diverse leadership as well as ways to provide education and representation at CAFP events. The JEDI Committee has only just begun building out a framework for centering diversity, equity, continued on page 14
continued from page 13
and inclusion work for the CAFP. As we look to the future, we recognize that to be effective, we must continue to collect data, and benchmark and measure the effects of the work we do. We look forward to continuing to develop recommendations for the
Board and ensuring transparency in the work that we do by regularly updating our page on our website with information for our members on our work. Please check out familydocs.org/jedi for our latest.


California Physician Leaders
Represent CAFP at the 2024 NCCL
CAFP extends a huge thank you to all our delegates and physician leaders who took time out of their busy schedules to represent us at the AAFP's National Conference of Constituency Leaders (NCCL) in Kansas City last week. In addition to honing their advocacy skills and knowledge, drafting resolutions, and offering testimony on proposed new national policy, and serving in key volunteer roles, our California delegation came away with six Californians elected to leadership positions!
Congratulations to the newly elected leaders! Let’s all celebrate:
• New constituency co-conveners: Toussaint Mears-Clarke, MD, FAAFP, Rob Assibey, MD, FAAFP, Peony Khoo, MD, FAAFP, and Shruti Javali, MD;
• Cynthia Chen-Joea, DO, FAAFP was elected as the New Physician Director to the AAFP Board; and,
• Anna Askari, MD, MS was elected American Medical Association Young Physicians Section (AMA-YPS)
In addition to their respective roles helping to plan the 2025 NCCL, all six will be headed to the AAFP Congress of Delegates (COD) in Phoenix this coming September. At COD, the new constituency co-conveners will serve as Alternate Delegates to the Congress, and subsequently serve as Delegates at the 2025 Congress in Anaheim.
Find out more about NCCL at www.aafp. org/nccl. If you are interested in serving as a representative of CAFP at NCCL, let us know! Email us at cafp@familydocs. org for more information on applying for 2025.







































































































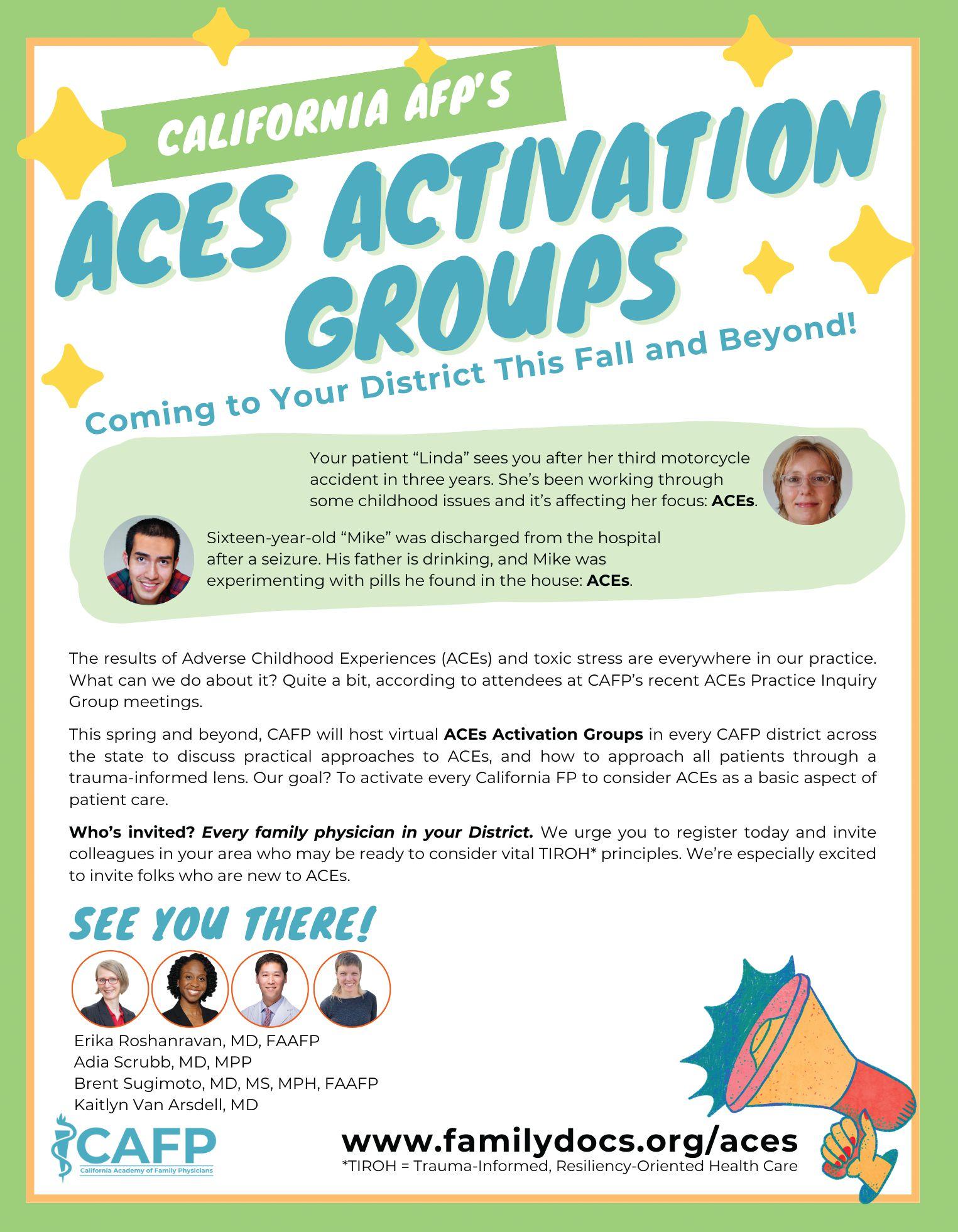
Moazzum Bajwa, MD, MPH, MSc
Over the last five years, California has led the national momentum for enacting policy on screening for adverse childhood experiences (ACEs). While there is tremendous evidence of the impact of ACEs on health and life opportunities across generations, there are challenges with implementing intervention for ACEs in busy primary care settings. Family physicians are ideal champions for bridging the gaps between education and action to improve the well-being of their patients. At UC Riverside School of Medicine, Dr. Adwoa Osei (Associate Professor of Pediatrics) led an interdisciplinary group in creating an innovative workshop to address ACEs as determinants of health equity. Our team included perspectives from primary care physicians, resident physicians, medical students, and clinical social workers. Our work began in the fall of 2020 in the wake of the national reckoning in social justice, health equity, and antiracism. This coincided with the ACEs Aware campaign through the California Department of Healthcare Services and later with the University of California ACEs Aware Family Resilience Network (UCAAN).
As practicing physicians, we recognized the need for in-clinic interventions that were practical and would not demand considerable time and resources; our support staff are already tasked with completing a dizzying array of screening tools with each patient visit. A major objective of our workshop is to empower physicians with a variety of resiliency-fostering tools and interventions for use with patients in any clinical setting. Our ultimate goal is to shift the community perspective on ACEs from asking patients “What’s wrong with you?” to focusing on “What’s strong with you?” Through this trauma-informed approach, we partner with our patients to disrupt the cycle of structural violence that impacts health disparities in our communities.
Prior to the workshop session, the learners completed an e-learning module that highlighted health impacts of ACEs, introduced mnemonics for screening for both symptoms of toxic stress response and buffering or protective factors on health, and demonstrated the use of the brief in-clinic interventions to foster resiliency. We then organized small-group virtual discussions centered on clinical cases involving ACEs and toxic stress response.

The results of our survey assessments after the workshop demonstrated a significant increase in learner’s knowledge and skills (from 17% to 89%) in identifying buffering factors for patients exposed to ACEs. Most importantly, three months after the educational workshop, over 40% of the learners were performing one of the brief in-clinic interventions on promoting resiliency during their longitudinal primary care clerkship. Although our initial workshop involved medical students as part of their required curriculum at UC Riverside School of Medicine, it can be implemented with any clinical audience. The openaccess toolkit includes educational slides on ACEs and toxic stress, facilitator guides, learner handouts, and follow-up surveys. Through presentations at conferences and seminars, we continue to improve upon the toolkit based on feedback from other physicians and experts. We encourage family physicians to lead trauma-informed workshops on ACEs and health determinants in their own communities, in collaboration with their patients and colleagues, as one small way of bending the arc towards health justice.

Osei A, Paz CG, Stuparich M, Racataian-Gavan R, Nelms L, Suliman Y, Smith A, Bajwa M. Screening for Toxic Stress Response and Buffering Factors: A Case-Based, TraumaInformed Approach to Health Equity. MedEdPORTAL. 2022 Mar 4;18:11224. doi: 10.15766/mep_23748265.11224. PMID: 35321319; PMCID: PMC8894523.
https://www.mededportal.org/doi/full/10.15766/mep_23748265.11224
Moazzum Bajwa, MD MPH MSc, is associate professor of family medicine at the University of California Riverside and director of Community Health & Social Medicine at Riverside University Health System (RUHS/UCR) Family Medicine Residency program.


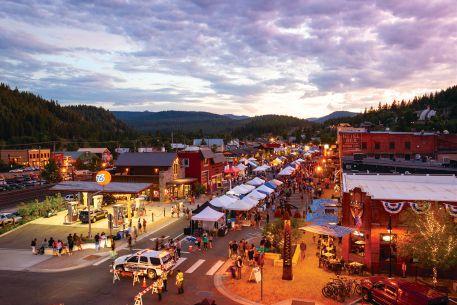
Learn more about a primary care career at Adventist Health
At Adventist Health, we are dedicated to transforming the health experience of the more than 100 communities we serve. Our focus is the whole person — mind, body and spirit. As a faith-based health system founded on Seventh-day Adventist heritage and values, we know you want more purpose in your work. We will ensure you find it.
Adventist Health is 28 hospitals, 440 clinics and 4,500 providers throughout the West Coast and Hawaii.
Why Choose Adventist Health
• Opportunities in locations to suit any lifestyle
• Starting bonus up to $60,000
• Residency/Fellowship stipend
• Additional bonus and incentive structures Qualified Public Service Loan Forgiveness (PSLF) Employer
• Leadership and academic opportunities available
• Large network of primary care and specialty providers
Scan the QR code to learn more about opportunities at Adventist Health or visit PhysicianCareers.ah.org To speak to a recruiter directly, please email us at phyjobs@ah.org
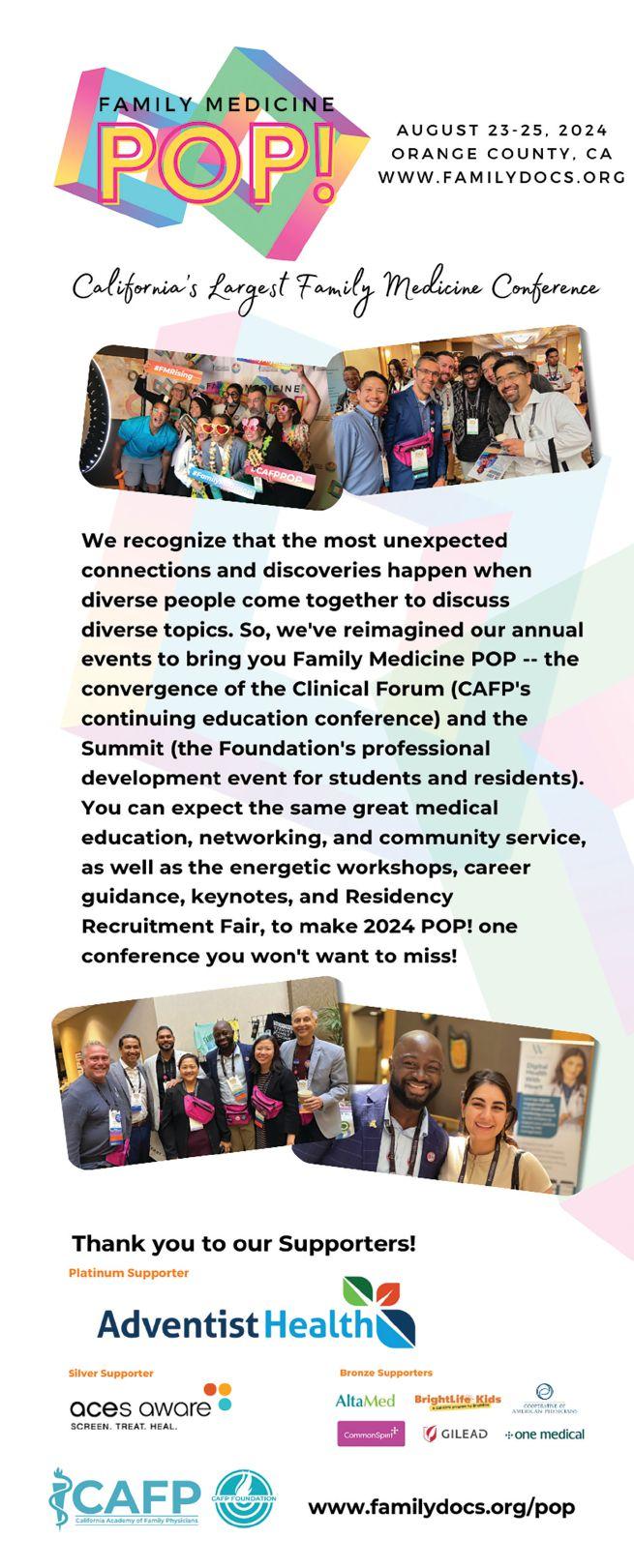
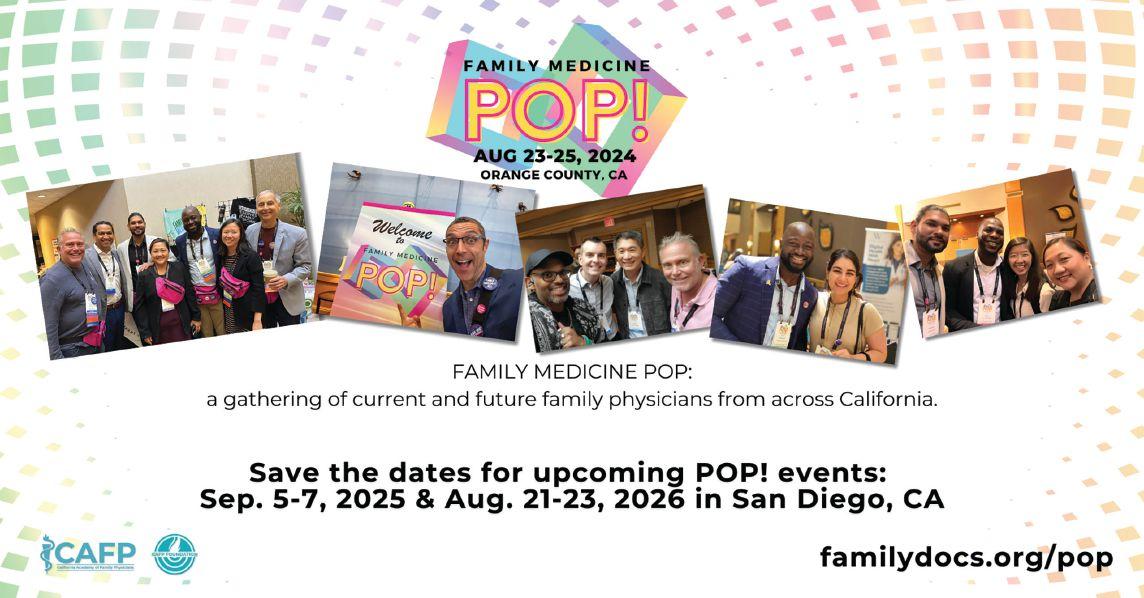
Friday, August 23, 2024
TIME TITLE
8:00 am - 1:00 pm CAFP Foundation Board of Trustees Meeting
8:00 am - 12:00 pm Pre-Conference Workshop: Advanced Gynecologic Procedures (registration required)
8:00 am - 12:00 pm Pre-Conference KSA: Care of Women (registration required)
9:00 am - 12:00 pm Committee Meetings
12:00 PM Exhibits Open
1:00 pm - 1:15 pm Grand Opening Carol Havens, MD, FAAFP, FASAM Ron Labuguen, MD, FAAFP Laura Murphy, DO, CAQSM Alex McDonald, MD, FAAFP
1:15 - 2:00 pm
Keynote Address: Weathering the (Mis)information Storm: How Physicians Play a Key Role as Trusted Messengers Katelyn Jetelina, MPH, PhD
2:00 - 2:45 pm The Fourth Wave: Emerging Drugs, Fentanyl and Today's Overdose Crisis Mario San Bartolome, MD, MBA, MRO, FASAM
2:45 - 3:00 pm Refreshments with Exhibitors
3:00 - 3:30 pm Physician Voices: Reclaiming Our Identity in Healthcare Lalita Abhyankar, MD & Maryal Concepcion, MD, FAAFP
3:30 - 4:15 pm Beyond Numbers: Fostering Successful Primary Care Obesity Management through the Lens of Cultural Humility "Ecler Jaqua, MD, MBA, DipABOM, FAAFP, FACLM & Erin Calicchio"
4:15 - 5:00 pm The What-Why-Hows of ACEs Screening in Adulthood in a Busy Residency Teaching Clinic Monica Hau Le, MD, MPH & Andreé Franco-Safaie, MD, MPH
5:00 - 5:30 pm Don't Forget: Screening for Cognitive Impairment in Primary Care Heather Schickedanz, MD & Bekah McLean
5:30 - 7:00 pm Welcome Reception and Exhibits
Saturday, August 24, 2024
*Schedule subject to change.
TIME TITLE FACULTY & SPEAKERS
7:00 - 8:00 am Breakfast and Exhibits
8:00 am - 6:00 pm Professional Headshots (sign-ups available)
8:00 - 8:15 am Day 2 Welcoming Remarks Ron Labuguen, MD, FAAFP
8:15 - 8:45 am Psychedelics, Imagination and the Health Connection Cassandra (Cassi) Vieten, PhD
8:45 - 9:35 am Resident Poster Competition Presentations Rob Assibey, MD
9:35 - 10:15 am Confronting Medical Bias: Acknowledging History, Challenging Inequities Monica Hahn, MD, MPH, MS, AAHIVS
10:00 am - 1:00 pm CAFP Residency Network (CRN) Meeting (Closed Meeting)
10:15 am - 10:30 pm Refreshments with Exhibitors
10:15 - 11:00 am Putting ACES into Practice as a Student or Resident Adia Scrubb, MD, MPP & Kaitlyn Van Arsdell, MD
10:15 - 11:00 am I'm Finishing Residency, Now What? Matt Varallo, DO & Anna Askari, MD
10:30 - 11:15 am Burnout in Female Physicians: Root Causes and Through Paths Karen Muchowski, MD, FAAFP
10:30 - 11:15 am A Game Changer in Sports: Addressing Mental Health in Young Athletes Marcia I. Faustin, MD, FAAFP
11:00 am - 12:00 pm Survival Tips for Getting Into Residency Francesca Adriano, MD, FAAFP
11:00 am - 12:00 pm The Power of Grassroots Advocacy: Strategies for Cultivating Change in Your Community (a mini-workshop) Moazzum Bajwa, MD, MPH
11:15 am - 12:00 pm Research in the Real World: Why & How to Engage Shruti Javali, MD, M. Shoaib Khan, MD, FAAFP, AAHIV & Tessa Stecker, MD
11:15 am - 12:00 pm Patient-Centered Approaches to Reproductive Health Care Shannon Connolly, MD, FAAFP
12:00 - 1:00 pm Luncheon
1:00 - 1:15 pm Exhibitor Break
1:15 - 2:00 pm Direct Primary Care: Reimagining Family Medicine Maryal Concepcion, MD, FAAFP
1:15 - 2:00 pm Improving Cancer Screening in LGBTQ+ Communities: Educating Patients and Primary Care Providers Julio Hernandez Rodriguez, MD
1:15 - 2:00 pm Putting ACES into Practice as Student or Resident Adia Scrubb, MD, MPP & Kaitlyn Van Arsdell, MD
1:15 - 2:00 pm I'm Finishing Residency, Now What? Matt Varallo, DO & Anna Askari, MD
2:00 - 2:30 pm Updates for ABFM Diplomats Gerardo Moreno, MD, MSHS
2:00 - 2:30 pm Alphabet Soup: Acronyms and Action for Respiratory Viruses Lauren Simon, MD, MPH, FAAFP
2:00 - 3:00 pm Physician Employment: How To Navigate Negotiations & Legal Issues Scott Kessenick, Esq.
2:00 - 3:00 pm The Power of Grassroots Advocacy: Strategies for Cultivating Change in Your Community (a mini-workshop) Moazzum Bajwa, MD, MPH
2:30 - 3:00 pm Reproductive Health and the Risks of Health Information Exchanges Panna Lossy, MD
2:30 - 3:00 pm Primary Care of HIV: An Update George Kent, MD
3:00 - 5:00 pm Refreshments with Exhibitors
3:15 - 5:15 pm Free Workshop: Striking a Balance: Understanding Pain Management and Opioids Carol Havens, MD, FAAFP, FASAM, Karen Muchowski, MD, FAAFP & Lee Ralph, MD
3:30 - 6:30 pm Residency Recruitment Fair
4:00 - 6:30 pm Orange County, Riverside/San Bernardino County, Los Angeles County Chapter Mixer
Sunday, August 25, 2024
*Schedule subject to change.
TIME TITLE FACULTY & SPEAKERS
8:00 am - 12:00 pm Student and Resident Procedures Workshops
8:15 - 9:30 am Breakfast and Table Talks
9:30 - 9:45 am Day 3 Welcoming Remarks
9:45 - 10:15 am AI, Ethics, and the Family Physician Brent Sugimoto, MD, MS, MPH, FAAFP
10:15 -11:15 am Family Medicine Update Hobart "Hoby" Lee, MD, FAAFP
11:15 - 11:30 am Break
11:30 am - 12:30 pm Family Medicine Jeopardy!
12:30 - 12:45 pm Closing Remarks
1:00 - 5:00 pm Post-Conference Workshop: Vasectomy (registration required) Alex McDonald, MD, FAAFP & Uziel Sauceda, MD
1:00 - 5:00 pm Post-Conference KSA: Hypertension (registration required) Van Nguyen, DO, FAAFP
Laurie Isenberg, MILS, CHCP Director of Education and Professional Development

When I spoke with Katelyn Jetelina, MPH PhD this morning, she hadn’t been home in two weeks. Most recently she had flown straight from Texas, where she and her family viewed the eclipse (“I’m not a religious person, but…”) to New York State to receive Albany University’s Axelrod Prize in Public Health.
Dr. Jetelina is always on the move and is no stranger to recognition for her work in epidemiology. She earned a medal of honor from the U.S. Department of Health and Human Services, and this year Time Magazine included her in 2024’s Time 100: Most Influential People in Health. [embargoed until May 1 – look for link then]
You may remember Dr. Karen Muchowski’s Show & Tell article, An Email Newsletter Worth Receiving [https://www. familydocs.org/show-and-tell-an-emailnewsletter-blog-worth-receiving/]. She was referring to Dr. Jetelina’s amazing blog, Your Local Epidemiologist [https:// yourlocalepidemiologist.substack.com]. Known among fans as YLE, the blog is a public health newsletter that translates ever-evolving science to the public, with well over 300 million views. YLE has been a continuing source of sanity to Dr. Muchowski and many other family physicians seeking unbiased analysis of vaccine safety and efficacy as well as vaccine hesitancy.
Jetelina writes about vaccines and firearms, mental health, long COVID, reproductive health… you name it, she’s explained it – in approachable language and with charts and graphs to make any data lover smile. Her main goal is to equip people to make evidence-based decisions about health.
Why POP? Dr. Jetelina is a strong advocate for family physicians and primary care. She understands that family physicians are trusted messengers, central to public health and part of the solution to misinformation: “We have a saying that when public health works, it's invisible,” Jetelina said. “But we have to get out of this mindset. We have to start communicating — and not just with each other, scientist-to-scientist. We need to

be better at talking to the communities we serve.” https://ysph.yale.edu/news-article/ popular-epidemiologist-lays-out-future-pathof-public-health-communication/12/19/23 And this is doubly true for family physicians. More and more evidence shows a top-down approach (health officials, government, media) to health information diffusion to the public will not suffice in the 21st century. A well-organized bottom-up approach of trusted messengers needs to be built and aligned to improve trust and combat misinformation for the public. Physicians are the most trusted source of health information to the public and, thus, are a key part of the solution. Public health needs to work handin-hand with healthcare and innovators so clinicians feel equipped on the front line, including increasing capacity, availability of plain language resources, and fostering an online presence that is responsive and anticipatory to patient information needs on the ground.
Her work in YLE as well as with the Health Trust Initiative https://healthtrust.org/, as Senior Scientific Advisor to the White House, Centers for Disease Control and Prevention, and Resolve to Save Lives https://resolvetosavelives.org/ all pushes the message out: communicate!
We look forward to hearing Dr. Katelyn Jetelina do just that on stage at CAFP’s 2024 Family Medicine POP! We hope to see you there, Friday afternoon, August 23 in Orange County. https://familydocs.org/pop
Jeff Luther, MD, FAAFP Chair, Legislative Affairs Committee
In parallel to the Legislative process, the state budget process is governed by constitutional deadlines throughout the year. The first budget deadline is January 10th. By this date, each year, the Governor must produce a proposed budget for that fiscal year. In May, updated economic forecasts and more accurate revenue protections (from taxes) culminated in the ‘May Revision’ of the budget. This year, the May Revision was released on May 10, 2024 for the Fiscal Year (FY) 2024-2025 budget.
California is facing a substantial, growing budget deficit, or shortfall. Earlier this year, Governor Newsom announced a $37.9 billion budget shortfall—to which the Legislature and Governor came together to release an early action plan to swiftly begin to address the budget problems. The early action plan addressed $17.3 billion of the shortfall. The May Revision, however, projects an additional $7 billion to the total budget deficit—leaving the net shortfall for this fiscal year at $27.6 billion. To make the fiscal situation worse, the state projects budget shortcoming not only FY 2024-2025, but also in FY 2025-2026. The result is a budget proposal leveraging a multi-year strategy to balance the budget. Despite the administration’s efforts to preserve key programs and investments, the May Revision includes several alarming budget solutions that impact vital state funding imperative to growing primary care in California.
The Song-Brown program, the solely primary care focused GME funding program administered by the Office of Health Care Access and Innovation (HCAI) is included in a multiyear funding eliminations for health care workforce initiatives. The May Revision proposes eliminating $330.9 million in FY 2023-24, $302.7 million in FY 2024-2025, $216 million in 2025-2026, and $19 million in FY 2027-2028.
In addition, the FY 2023-2024 budget promised an additional $70 billion for GME as part of the Managed Care

Organization (MCO) tax allocations. The May Revision alludes to eliminating or deferring this funding.
The May Revision also proposes to leverage MCO tax funding in the Governor’s budget solutions--re-allocating the funding and dialing back $6.7 billion over multiple years. This funding is crucial for family physicians and includes the necessary Medi-Cal provider rate increases planned for January 2025.
Decreased Investments for Behavioral Health
The May Revision also proposes several cuts to behavioral health initiatives important to family physicians. These adjustments include reductions in the Children and Youth Behavioral Health Initiative funding ($72.3 million one-time in FY 2023-2024, $348.6 million in FY 2024-2025, and $5 million in FY 2025-2026), and eliminating $280 million one-time over multiple years for grants to Medi-Cal providers as part of the Equity and Practice Transformation Payments.
The Legislature has only a few weeks after the May Revision is released to negotiate the final budget. This will be in print as the ‘Budget Bill’ by June 12th and passed by the Legislature by June 15th. The Governor has 15 days to sign the Budget Bill into law by July 1, 2024, the start of the new fiscal year.
Although the Legislature sends the main budget bill to the Governor for their signature by June 15, the Legislature can use policy area specific bills, known as “trailer bills” to provide additional details on expenditures listed in the budget bill. Trailer bills do not have the same deadlines as the budget bill – but rather can be passed any time before the end of the Legislature session. Another mechanism the Legislature has to adjust the budget after the deadline is to make revisions to the budget bill using what is called ‘budget bill junior’. This bill also follows the regular Legislative session deadlines.
Gianna O’Hara, DO

An 80-year-old woman rolled into the ICU with her frail frame and withering smile. Suddenly, in the middle of the hall, her smile disappeared and an all too familiar scene requiring immediate CPR occurred. As her family watched in horror, ribs breaking and blood spewing out of their grandma’s chest, we declared her deceased moments later.
This would be one of many instances in which I, then a resident and now a Geriatrician, wished prior conversations about a patient’s end-of-life decision-making and goals of care had occurred - before the worst happened. As primary care physicians, geriatricians, internists, and advanced practice providers, we are in a unique position to help patients and their families understand their individual end-oflife decisions by having goals of care (GOC) discussions with them. These conversations should be viewed as informed consent instead of being treated like a menu option at a restaurant.
Ideally, this discussion would happen in the primary care setting, where the stakes and stress are low, but the future planning yield is high. In one study, 52 percent of patients reported having GOC discussions at clinic visits while the physicians reported a 66 percent rate.
These conversations would help to decrease family strife that surrounds what is often a fraught situation. After a year and a half of managing my grandfather’s chronic diseases, he was finally diagnosed with active myelodysplastic syndrome. Despite medical management, his anemia was uncontrolled. Multiple hospitalizations later, he attended his oncology appointment.
“We could top you up and get you back to Mexico.” These words stabbed through me like a knife. How could Grandpa’s oncologist be saying this when the medications were not working, after receiving over a dozen blood transfusions, and my grandfather was refusing further hospitalizations? Speaking to my grandmother the next day, I had to break the news to her that Grandpa was not doing well and likely would require hospice soon.
I didn't know how quickly that day would come, as within seven days we placed him on hospice, and he passed. Had my grandfather’s physicians expressed the gravity of his disease, my family would have been more prepared, and I would have been able to act as a family member instead of as his doctor.
While it takes time to have these conversations in a true informed consent fashion, we save a lot in the process. We decrease patient and family stress (both future and current), save time and money for the system, and you can always still get paid. Using CPT 99497, you too can be compensated for advanced care planning by spending 16 minutes or more.
I challenge more primary care physicians to practice informed consent GOC discussions so patients and their families, even ones with geriatricians as granddaughters, do not have to go at it alone.

Join the Banner Health Team, in an outdoor paradise where the beautiful Sierra Nevada and Cascade mountains meet the desert of the Great Basin in Susanville, California — where you’ll have the time to connect with your patients, your practice, your family and the great outdoors! We offer dedication to work/life balance unmatched in our industry. Meaning you get to spend more time doing what you love. That’s HEALTH CARE made easier, LIFE made better!
• Unbeatable Housing Affordability in CA
• $100K Sign-On Bonus
• $270K Salary Guarantee
• $100K Educational Loan Repayment
• Focus on Physician Well-being and Development
• Robust Benefits and Retirement Packages
• Retention Bonus Available
• Eligible for $50K from California Health Planning
• Eligible for HRSA Educational Loan Repayment
• Location qualifies for federal loan forgiveness (PSLF)
Join our Provider Network! Register using our job portal: PracticeWithUs.BannerHealth.com Or, email CV: primarycaredocs@bannerhealth.com For information call Martha Gonzales 602.747.4328


Scott Nass, MD, MPA, FAAFP, AAHIVS Editor
With this first editorial column, I am honored to take the reins of California Family Physician from the venerable Brent Sugimoto. I was privileged to serve as his associate editor for the past two issues, and I learned a great deal from him and the amazing Josh Lunsford, our managing editor.
For me, stepping into the editor role is really a dream come true. I found my way to family medicine (and medicine generally) after working in the not-for-profit sector following graduate school, but my first career ambition in college was publishing; I wanted to shape books, magazines, anything really - to help tell stories through words and pictures.
And what incredible stories we have to tell: those of our patients and communities, of leadership and vision, of innovation in industry, of advocacy and creating positive change. We have so much to celebrate as family physicians. When we gather together and combine our energy and expertise, we are particularly adept at weaving new tales.
In April at the All-Member Advocacy Meeting, we flexed our advocacy muscles, hearing testimony on a record number of resolutions brought forward from our county chapters and individual CAFP members, and then traveling to the capitol to speak with our legislators about AB 2250 and the critical role social determinants of
health play in the lives of our patients. We will continue our journey together this August, when we close out summer with Family Medicine POP! - learning from our peers about the latest in family medicine while networking with other family docs, residents, and medical students from around the state.
I would also like to use this space to highlight the Project RAINBOW report released earlier this year by a coalition of organizations seeking to identify and disseminate best practices to protect the rights of LGBTQ+ patients - especially transgender, gender-diverse, and intersex youth, who are particularly at risk of discrimination in healthcare. Because family physicians provide necessary care to so many LGBTQ+ patient throughout California, CAFP was a natural participant in the project, and I gladly joined with other healthcare professionals to inform the final report, available online at https:// www.familydocs.org/news-newly-released-project-rainbow-report. Take a look to learn how you can help make healthcare more inclusive.
When we combine our experience with our passion, we can accomplish anything. I cannot wait to hear your stories, and I look forward to sharing many of them in the pages of this magazine.
Until next time
Scott


Primary Care Physicians - Supervisory and Staff Opportunities
Open location now: Northern California, Nevada, and Pacific Islands
The Department of Veterans Affairs (VA) needs primary care professionals who possess the energy, compassion, and commitment to serve those who served our country. Eligible applicants must be able to provide comprehensive general primary care and comprehensive women’s health care.
Whether you are a new graduate or an experienced professional, physicians are always needed at the VA.
These locations have a lot to offer to those seeking good weather and an abundance of outdoor activities such as hiking, snow skiing, boating, hunting and fishing. Enjoy the area’s beautiful rural settings with access to many national parks, rivers, and lakes at your fingertips. Whether you’re interested in work/life balance, research or academics you will find that working for the VA offers many benefits not to mention the great honor we have in serving our nation’s heroes. Located near San Francisco, one of America’s favorite cities, Sacramento, is not far from the world class ski attractions at Lake Tahoe and the beautiful Napa Valley. Don’t forget Nevada’s amazing landscapes are often overshadowed by the glitter and glitz of its biggest city, Las Vegas.
Available benefits:
• 26 days paid vacation; 13 days paid sick time; 11 paid federal holidays; 15 days military.
• Annual performance bonus up to an additional $15K per year
• Guaranteed salary increases.
• Licensure: 1 full & unrestricted active U.S. license
• CME: $1,000/year and 5 days of paid absences for CME courses
• Federal Retirement Plan and Separate 401K with partial agency match
• Health Insurance (Dental & Vision supplemental insurance available) and Life Insurance
• Education Debt Reduction Program (EDRP), student loan payment reimbursement program up to $200,000
Candidate Eligibility: 1) US Citizen, Green Card or Visa 2) BE/BC Family Medicine, Geriatrics or Internal Medicine 3) Active medical license in any State 4) Confirmed vaccination for seasonal influenza only. Supervisory candidates should: have demonstrated leadership experience or demonstrate informal leadership training, experience and skills.










The 2024 Hero of Family Medicine award was presented to Adia Scrubb, MD, MPP, for her demonstrated exemplary dedication, leadership, and advocacy in advancing the field of family medicine. The Hero of Family Medicine goes to a CAFP member who is a passionate advocate for patients, colleagues, and the family medicine specialty.
Dr. Adia Scrubb is an Oakland native and is currently practicing full scope family medicine at Kaiser Vacaville, California. Dr. Scrubb received her medical degree from the David Geffen School of Medicine at UCLA and the Charles R. Drew University of Medicine and Science in Los Angeles. Dr. Scrubb does not shy away from ensuring that issues important to family physicians and our patients are prioritized in discussion, including being a champion for traumainformed care and equity in care. She has served as a key advocate for ACEs, serving on the California Surgeon General’s ACEs Aware Clinical Implementation subcommittee. Scrubbs is also a part of the CAFP Family Medicine Initiative in Trauma Informed Care (FIT) as well as the CAFP JEDI committee.

Dr. Scrubb can also always be counted on to share her expertise with policy makers, exemplified when she served as a key witness for Assembly Bill 85 in 2023, a bill that made it all the way to the Governor’s desk. Recently, Dr. Scrubb testified in the Assembly Health Committee hearing for Assembly Bill 2250, which then advanced out of the Assembly Health Committee. To hone her advocacy skills, Dr. Scrubb also holds a Masters of Public Policy at the UCLA Luskin School of Public Affairs as part of the PRIME program.
The 2024 Champion of Family Medicine award was presented to State Assemblymember Pilar Schiavo. During the Lobby Day visits, CAFP members had the opportunity to meet with Assemblymember Pilar Schiavo, D-40. During this meeting, Assemblymember Schiavo was presented with the Champion of Family Medicine award, recognizing her unwavering commitment to expanding health care access and affordability. Assemblymember Schiavo has been an advocate for family medicine, championing legislation including the 2024 Family Physician Week resolution (ACR 165), among others, that directly address issues crucial to family medicine and the well-being of their patients.

$239,000 - $273,000 with a 5% increase on 11/1/24
Contra Costa Health is seeking full-time and part-time BC/BE Family Medicine, Pediatric or Internal Medicine Primary Care Physicians. Our health centers across Contra Costa County are integrated with specialty care services and the public hospital.
We are looking for providers from diverse backgrounds and lived experiences who share our vision of providing equitable and quality health care to all members of our Contra Costa community. Desired applicants would work with a motivated practitioner group to provide innovative community medicine that empowers patients by fostering an environment of belonging and well-being.
To learn more, please contact: Recruit@cchealth.org

We offer:
• Flexible full- and part-time scheduling; no required weekends and no call!
• Modern facilities serving the needs of ethnically and culturally diverse populations
• Opportunity to be involved in resident teaching with our nationally recognized Family Medicine Residency Program
• Comprehensive compensation package
• 4 hours of paid administrative time a week, with opportunity for more paid time
• Favorable HPSA score for national and state loan repayment programs
• EPIC medical record system
Family medical practice for sale near downtown San Mateo, Ca. Solo family doctor retiring. Step in and take over a fully stocked and staffed medical clinic.
Located in a small medical office building rental, with several nearby other offices as part of call group.
Local medical group will help with contracting on very favorable terms. Be as busy as you want to be, with new patients calling daily. Minimal buy in expense.
Contact at


Monday, November 4, 2024, 8:00 am - Wednesday, December 4, 2024, 11:59 pm. Earn 20.00 hours, AOA Category 1-A credits.
The goal of the 2024 Virtual Primary Care Update is to provide primary care providers with the latest in practice guidelines over a wide variety of frequently encountered topics and disease processes. Program participants will then apply the knowledge gained back to their existing rural, suburban or urban practice allowing them to bridge the gap between previous therapies and the current best practices.
Specialty Credits: Over 20 specialty credits available including internal medicine, preventative medicine, OMM/NMM, and more!
Visit okla.st/cme-credits to see Enduring Credits and Package options.
Join a team that’s been helping to redefine what it means to be a community clinic for more than 50 years.

Consider joining our team of dedicated, motivated and enthusiastic team players who make a difference in the community. Vista Community Clinic is a federally qualified, not-for-profit healthcare clinic with state-of-the-art clinics throughout the Southern California regions of North San Diego, Orange, Riverside and Los Angeles Counties.
Our compensation and benefit program includes: Competitive compensation, sign-on bonus, relocation allowance, health, dental, vision, company-paid life, long-term disability, flexible spending accounts, retirement plan, malpractice coverage, CME allowance and no on-call hours. We are a NHSC loan repayment eligible organization.
Family Medicine Physician
Full Time and Part Time Opportunities in the cities of Vista, Oceanside and La Habra Compensation range is $280,000 - $300,000+
Pediatric Medicine Physician
Full Time Opportunity in the city of Torrance Compensation range is $245,000 - $280,000+
For more information visit www.vcc.org or email hr@vcc.org
EEO/AA/M/F/Vet/Disabled

50 years1972-2022

Help Your Patients Make Better Informed Decisions About Their Care
The California Prostate Cancer Coalition, founded in 1997 as a 501(c)(3) not-for-profit organization, is dedicated to saving men’s lives!!!
www.prostatecalif.org
https://naspcc.org/docs/informed-decision-making-laminate2023.pdf www.naspcc.org