
4 minute read
The “C” Word
The Cannabis and Cancer-Care Conundrum
By Dianne Armitage
Advertisement
As a three time breast cancer survivor, I was excited to write about the progress being made when it comes to using cannabis to combat the side effects of, and perhaps even create a cure for, cancer. It didn’t take much research to turn my hopes into a mixture of frustration and anger.
I’ve lived within the been there, done that cancer bubble since 1996, hoping if the cancer returns, my treatment options would be vastly improved. Unfortunately, I’ve been appalled by the snail’s pace at which progress is made in terms of treatment modalities, outside of the box thinking, and compassionate consideration when it comes to letting people fighting for their lives try treatments that haven’t been scientifically proven, but show promise.
A study published by the National Institute of Health’s (NIH) National Cancer Institute (NCI) in June of this year determined that no ongoing studies of cannabis as a treatment for cancer in people had been found in the CAM (Complementary and Alternative Medicine). They did note that small studies have been done, but either the results have not been reported or suggested a larger study was needed.
These included data on: • Cannabidiol (CBD) taken by mouth to treat solid tumors that have recurred (come back). • An oral spray combining two cannabinoids (delta-9-THC and CBD) given with temozolomide to treat recurrent glioblastoma multiforme (an aggressive brain cancer). • CBD taken by mouth to treat acute graft-versus-host disease in patients who have undergone a stem cell transplant.
What about cannabis-based therapies to combat nausea, vomiting, and pain relief for individuals undergoing chemotherapy?
Dr. Marisa Weiss, founder and president of www.breastcancer.org, an oncologist, internationally recognized breast cancer specialist, and breast cancer survivor, recently conducted the first ever study to evaluate the underlying reasons that women with breast cancer use cannabis as part of their treatment regimen. Weiss, who is based in Philadelphia, decided to incorporate cannabis into her pain management program in 2018 when Pennsylvania first opened its medical marijuana program, because even more than the nausea associated with their treatments, women with breast cancer experience pain.
Her study discovered that 73 percent of women with early stage and 89 percent of women with metastatic disease sought medical cannabis for pain relief. Additionally, the study showed that 45 percent of the early stage and 89 percent of the women with cancer that had spread to other parts of the body were using medical cannabis to help overcome anxiety. Insomnia was another stumbling block for many patients, with 50 percent of the early stage, and 33 percent of the metastatic group turning to medical marijuana for relief. Surprisingly, only 4 percent of the early stage, and 33 percent of the women with metastatic disease used cannabis for nausea. It is interesting to note that most patients suffered an average of three symptoms. Pain was rarely experienced alone; insomnia and anxiety were frequently combined.
Dr. Weiss is working on a randomized controlled trial for Ananda Hemp gelcaps to treat chemotherapy-induced peripheral neuropathy for patients with breast, ovarian, or colon cancer. She is also a co-investigator on a study out of Columbia University which is testing cannabinoids for peripheral neuropathy caused by chemotherapy in breast cancer.
A 2018 study of clinical oncologists attitudes about cannabis for therapeutic use found that, while 80 percent were discussing cannabis with their patients, only about 30 percent said they knew anything significant about it. Which raises the question, how do you find a doctor who is knowledgeable if you are interested in exploring a cannabis assist?
Based in Santa Barbara, Dr. Morton Sacks has long offered personalized, comprehensive medical cannabis evaluations. When I posed this question to him, he responded, “The patients I have seen in the past 13 years found me by word-of-mouth or were referred by oncologists or other medical professionals. That is how the average layperson can find a qualified practitioner.”
When asked whether he has personally seen instances where cannabis made a positive difference, he shares: “I had a patient (a physician) who was being treated for lymphoma with chemotherapy, and had severe anorexia and nausea which did not respond to Zofran or Marinol, a synthetic THC. He stated that he felt he was dying. He had never inhaled marijuana. I advised him to get a joint and light up. With a few inhalations he started eating, and recovered. That was 10 years ago. He never used cannabis again.”
How do we move this conversation forward in meaningful ways? By letting our healthcare professionals and elected officials know it’s way past time! Don’t be shy about starting a conversation with your primary care doctor or oncologist. And a phone call or letter to elected representatives at the local, state, and federal level is one more way to make your voice heard.
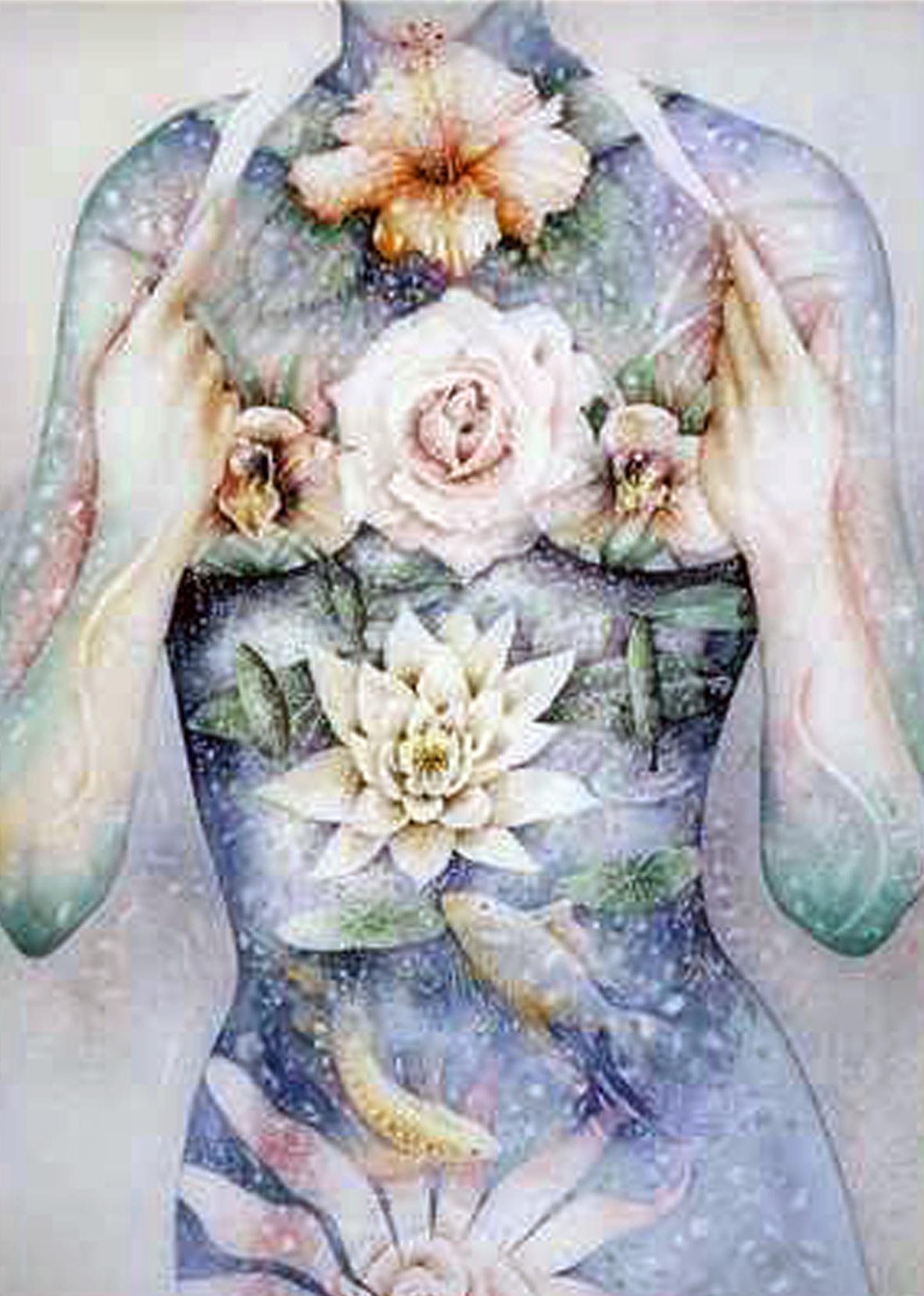
"Body of Flowers" by Meganne Forbes, Visionary Artist
Dianne Armitage is a freelance writer and the owner of WriteOn!, based in Carpinteria, Calif. She wrote a monthly humor column for Amoena’s breast cancer website for several years (yes, it was a humor column). Dianne is proudly owned by two French bulldogs, who prefer to remain nameless.










