Alzheimer’s and Dementia





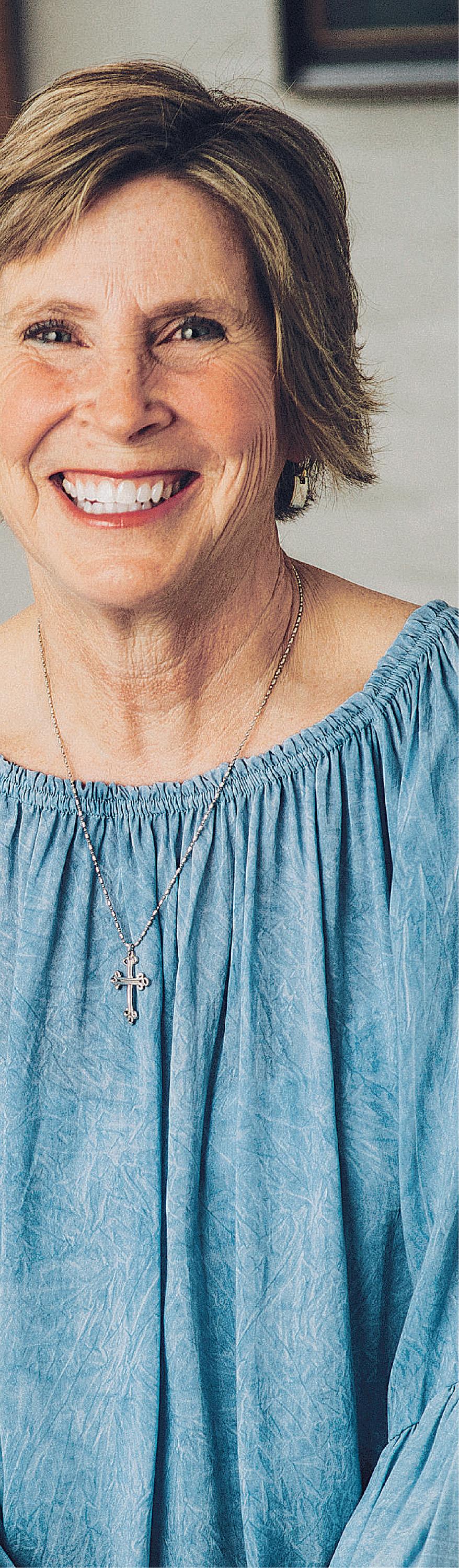
Leslie Cardé is an awardwinning New Orleans-based journalist who covers topics ranging from medicine to entertainment while working as a special projects medical producer for CBS. Leslie began her career in Los Angeles as a therapist treating traumatic brain injuries before transitioning to journalism as a medical reporter and editor for NPR. Moving to New Orleans, she became an anchor and medical editor at WDSU in New Orleans before landing at CNBC as one of its original anchors. She has covered the Middle East for CNN, was an executive producer and narrator at E! Entertainment, and has written, produced and directed the award-winning documentary, “America Betrayed.”

In this series of guides by The Times-Picayune and The Advocate, we’ll shine a light on issues surrounding the unique health concerns in our state. The Your Best Life publications will focus on how all of us can strive to live our best life through the tumult of health problems that face our state, on topics such as addiction, dementia and mental health. Your Best Life will be a comprehensive resource that will educate and inform readers on topics that are often difficult to talk about.
Reporting by Leslie Cardé and Amanda McElfresh Layout and design by Emily Sucherman • Edited by Annette SiscoJust before Christmas, our family realized something was very wrong with Dad.
Our father, a 79-year-old business owner living in Florida, had been picked up by the police.
He had left work as usual but had gotten lost and ended up 50 miles from home, traveling the wrong way on the highway, confused and in danger.
When I was a girl, Dad was the rock of our family. Strong and smart, understanding and supportive, he was so kind that he’d earned the family nickname “Saint.”
That night, the police got Dad to safety, and in the morning, they put him in an Uber and sent him home. But the incident threw the recent past into a new light.
The lost wallets and keys. The missing cell phones. The sudden, constant forgetfulness. We went to Florida and found our dad more disoriented than we could have ever imagined. We consulted with his doctors: The diagnosis was Alzheimer’s disease and vascular dementia. He was no longer safe living alone. We made a snap decision. Dad would be coming home with
us, to live in New Orleans.
My husband and I moved into the guest room. We put Dad in our room, on the first floor. And then, I froze.
I suddenly faced the magnitude of my new responsibility: fulltime caretaker. I had no idea where to start. I had to find new doctors for him, keep up with medications, meals and appointments, “senior-proof” our home. I had to have him supervised at all times. I worried that despite all my precautions, he would wander off.
There were so many decisions to make. I had no idea what my path would look like.
I turned to my friends and coworkers. And what I learned was eye-opening.
So many people are caring for parents with dementia. And they had so much to teach me.
How to keep Dad’s mind as active as possible? A friend suggested having him count change, no matter how long it took.
How to allow him to dress himself, despite arthritis and Alzheimer’s? Easy snaps and pull-on shoes.
When work-from-home ended,
Visit us online! nola.com/bestlife/
I learned about a local senior activity center, where Dad enjoys games and friendly lunches.
But while my friends were incredibly helpful, it was frustrating that I didn’t have one resource to go to — one place where I could see all my options. That was when we decided to create the guide you are reading now.
“Your Best Life” is packed with helpful information for those of us who are trying to negotiate this passage in the lives of aging loved ones.
In these pages, you’ll learn about symptoms, services and how to find help. Doctors weigh in, and there are helpful lists for caretakers.
And importantly, we report here on promising research into these conditions. There are many things you and I can do, right now, to reduce our own chances of developing dementia in the future.
My dad is doing much better now. I’ve learned that routine is key in our life. Nutritious meals, restful sleep and the proper medications are working their magic.
At night when I put my dad to
bed, I ask him if he had a good day. Thanks in part to what I’ve learned, and what we hope to share here, most days really are good ones.
I don’t know how much time I have left with my dad. But while he’s still with us, I want him to have his best life.
Every single day.
Alisha Owens is vice president of sales for Georges Media.

Think of your brain as the centralized computer station for your entire body. When it’s working properly, its marvelous underpinnings aren’t even noticeable.
Begin to speak, and the words just roll off your tongue. Think about making a movement, and before you know it, your arm has been flung into the air. Having a conversation with someone else is virtually effortless.
But in many people, who are living longer lives thanks to modern medicine, short-circuits in the brain’s wiring are causing forgetfulness, disorientation and even total obliviousness to the very world that surrounds them. Generations ago, we referred to these people with these sorts of problems as being senile. It was an all-encompassing umbrella term for those who had somehow lost their way in the world along with their ability to cope with life’s simple daily routines.
In the last century, doctors have known that it is in fact a disease called dementia which is responsible for the brain’s misfirings. Within the large category of dementia, Alzheimer’s disease accounts for 60-80% of all of the cases, and among Alzheimer’s patients, two thirds of Americans with the affliction are women. Does this mean it’s hormonal, biological, that women are getting less sleep? Currently, it’s all being studied. But, there are still far more questions than answers.
How and why these mental changes begin is still a major mystery to scientists who spend their lives studying dementia. In the meantime, it is important to
make the distinction between normal aging and the cognitive decline that often comes with it, and a diagnosis of some form of dementia, like Alzheimer’s.
Warning signs? Maybe not
“Almost every one of us will experience some form of agerelated cognitive decline, as we get up into our senior years,” said Dr. Demetrius Maraganore, chairman of the Department of Neurology at Tulane University’s School of Medicine.
“These changes are the sorts of things people notice in their 50s. It may take longer to retrieve certain stored information, or learning a new task may take longer than it did in one’s 20s. But, it should be noted that this sort of mild cognitive impairment is certainly not necessarily any sort of precursor to getting any form of dementia. Understanding the difference is critical.”
So, when should we become concerned about ourselves and those close to us?
If we’re mid-sentence and suddenly cannot retrieve the word we’re looking for to describe something, it’s probably nothing much to worry about. It’s just that slower retrieval process.
But, if you cannot find your way home from your daughter’s house, which you’ve been driving to and from for years, it’s time to see a neurologist for some testing.
And, of course, the frequency of some of the less consequential manifestations of cognitive impairment need to be taken into consideration, as well. If having a conversation is becoming increasingly difficult because you’re constantly unable to
retrieve thoughts or memories, it’s time for a diagnosis. Alzheimer’s diagnosis
“We don’t have a stick that we can put in your mouth and if it turns red, voila, you have Alzheimer’s,” said Dr. Ronald Fiore, a neurologist at Culicchia Neurological, LCMC Health. People don’t generally decide to get a brain scan, and even if they did, there’s very little doctors would learn from looking at the inner workings of their brains, Fiore said. “Most positive diagnoses of Alzheimer’s are made post-mortem, when a patient’s brain is dissected upon autopsy and the amyloid plaques and tangles are very evident.
“This doesn’t mean, however, that cognitive tests and a patient’s behavior won’t give you all of the clues you would need to make a rational diagnosis.”
So, how does one begin to find a cure for a disease when no one at this point is sure what starts the cognitive decline in motion?
We do know that 15-20 percent of cases are apparently hereditary, so if you have first or second generation relatives who had some form of dementia, it’s time to do some evaluating, whether that means becoming intimately

familiar with your own medical test scores, or taking some simple cognitive tests.
And it’s important to remember that there are specific measures we can all take, at risk or not, to either eliminate or forestall the onset of some of the dementias.
Blood flow an issue
“Although it’s rarer, some dementias are causes by vascular components.... those that have to do with blood flow,” said Dr. Gregory Bix, director of the Clinical Neuroscience Research Center at the Tulane University School of Medicine. “The rule of thumb is that if it’s good for your heart, it’s good for your brain.
“Your diet, your physical activity, your cholesterol levels, your blood pressure reading, your cardiovascular health generally, and staying sharp mentally all play into how well your brain will do long-term.
“We may not be able to stop dementia in its tracks, but we certainly know the contributing factors, and it’s time we all started paying more attention to what most of the physicians and scientists who work in this field know, which is that it is the No. 1 public health crisis of the future.”
Neurologists are increasingly optimistic that major improvements in prevention and treatment of dementia are on the horizon.
“It is inspiring to see the amount of effort going into tackling this disease,” said Dr. Sheryl Martin-Schild of LCMC Health, who specializes in neurology at Touro and New Orleans East Hospital. “There is still a lot of work to be done to identify the right patients, timing, and dosages for treatments and determine the magnitude of benefit. However, we saw with COVID that when efforts are focused and researchers empowered, massive changes can be made in a short amount of time. I think that is what we are seeing now in the world of dementia.”
Dr. Martin-Schild said researchers have identified modifiable risk factors that make a person more susceptible to Alzheimer’s, the leading cause of dementia. These include high blood pressure, physical inactivity, obesity, depression, diabetes, smoking, hearing loss, and binge drinking.
“Persons over 45 years of age who have cognitive decline are more likely to have at least four of those modifiable risk factors compared to persons without cognitive decline,” Dr. Martin-Schild said. “If we can
intervene earlier and address risk, disease is less likely to develop.”
However, Dr. Martin-Schild said that in many cases, a person doesn’t arrive for a cognitive assessment until their disease is already moderate to severe, when treatment is less effective. Individuals may attribute memory loss to normal aging. But patients who are ultimately diagnosed with dementia often display other cognitive issues, such as being easily distracted, trouble doing familiar activities or planning, leaving on appliances or faucets, or struggling to manage finances or medications.
Dr. Martin-Schild said it’s important to involve a patient’s loved ones from the beginning. During an assessment, she’ll often ask them to confirm a patient’s responses. Once a diagnosis is made, caregivers must know that their loved one’s needs will change, sometimes by the hour, as with “sundowning” when agitation occurs in the evening.
“We teach family members about the art of distraction. It’s important to recognize when a trigger occurs and transition to something the person is familiar with,” she said. “It may be
By Amanda McElfresh amcelfresh@theadvocate.coma photo album or a favorite song. We also tell caregivers to try not to get upset or defensive because this is a big struggle for their loved one.”
While the research continues, Dr. Martin-Schild said that recognizing and addressing risk factors is crucial for people of all ages. This includes eating a healthy diet, controlling blood pressure, and being physically active for at least 30 minutes five days a week.
“It doesn’t matter what form of exercise you choose,” she said. “What matters is that you put in the effort on a regular basis to keep your brain healthy and minimize the chemical stressors that ultimately lead to brain cell injury.”
For more information or to find a provider, visit LCMChealth.org.
At least 30 minutes of physical activity five days a week can reduce the risk of developing Alzheimer’s. “It doesn’t matter what form of exercise you choose,” said Dr. Sheryl Martin-Schild. drink it all in


Adiagnosis of Alzheimer’s can be devastating for both patients and their families. Sadly, many patients are not diagnosed early because their failing brain health is often written off to normal signs of aging. But, this isn’t an affliction that affects every senior citizen.
There are many people whose brains are healthy well into their 90s and beyond. But, the statistics are staggering and somber. Over 10% of people over the age of 65 have Alzheimer’s. So, how are they diagnosed?
“Most of the patients that I see are referred to me by primary treating physicians, are usually 70 to 80 years old, and are brought in by their adult child,” explained Dr. John Sawyer, an Ochsner lifespan neuropsychologist.
“It’s important to remember that 40-50% of people over the age of 65 already have plaques and tangles in their brains, so we want to make sure that the rest of the body is healthy, because plaques alone don’t necessarily translate to dementia.
“It can be something as simple as lack of sleep and anxiety which are contributing to poor brain function.”
When diagnosing patients, Sawyer says it’s important to rule out other factors before coming up with a diagnosis of Alzheimer’s.
A full 25% of dementia cases can be attributed to some sort of
vascular abnormality — that is, impaired blood flow. Whether it’s clogged arteries, diabetes, high blood pressure, high cholesterol, or smoking that is causing a lack of oxygenated blood to the brain, it’s important to rule out these contributing factors, which are often treatable, before making a formal diagnosis.
Diagnoses are not made by brain scans, because much of what causes Alzheimer’s and the various dementias doesn’t show up on an MRI. So, it is cognitive testing that measures everything from your ability to concentrate, your verbal memory, and your ability to tell where objects are in space (called visual-spacial processing). These are just a handful of the many elements which go into testing one’s many cognitive abilities.
At the Institute for Dementia Research and Prevention within the Pennington Biomedical Research Center in Baton Rouge (under the umbrella of LSU), the Louisiana Aging Brain Research Study is now in its 13th year, and has acquired a very large
database. It contains information that follows people annually, beginning in their 50s, to find out when cognitive decline first appears.
Most researchers believe that changes in the brain are occurring 10-15 years ahead of symptoms, and if subtle changes are recognized, we can introduce cognitive brain therapy and lifestyle changes to mitigate or delay the onset of Alzheimer’s. It’s a sophisticated set of tests that study participants are walked through (quite literally, in this case).
“It’s known in medical parlance as outwalking the grim reaper,” said Jeffrey Keller, PhD, founder and director of the Institute for Dementia Research and Prevention.
“How fast you can walk under a variety of circumstances is highly predictive of the development of dementia,” he said.
Doctors place patients in their study group on a moving mat that has thousands of sensors on it, detecting their stride, speed, and
cadence. Then, they add cognitive challenges while they are walking — things like spelling words backwards, recalling items, or learning a list.
Keller says that how well these tasks are carried out in tandem, over time, can predict the beginnings of what will later become mild cognitive impairment.
For most people, getting a comprehensive diagnosis is much less physical, and involves a consultation with a qualified professional who will first do a background analysis of signs or symptoms already present, and then administer one of two tests most often used to determine cognitive function.

The MOCA, or Montreal Cognitive Assessment, a rapid screening instrument for mild cognitive dysfunction, screening such areas as conceptual thinking, language, and calculations. The other test often administered is the MMSE, or Mini-Mental State Exam, a shorter cognitive screening test which rates the patient on a 30-point scale.
It’s important to be self-aware, and if you detect any of the warning signs, see a professional. Although Alzheimer’s, as yet, has no cure, researchers now have proven that implementing remedial measures can slow down the process, or eliminate fullblown Alzheimer’s disease.
say that we all forget words, occasion
But, if the problem is increasing in frequency, and you are unable to ever retrieve that word, it’s time to get a diagnosis.





Alzheimer’s disease, the most common form of dementia, is a degenerative process that begins with very mild, almost unrecognizable symptoms, and in almost all cases slides into an end-stage brain failure, leaving patients totally dependent upon others.
“Very early on, we just cannot detect dementia,” said Kevin Hargrave, MD, a neurologist who is the medical director of the Neuroscience Center at Ochsner General Hospital in Lafayette.
“As a neurologist experienced in dementia, with a certification in neuroimaging, I can sometimes


detect clues.
“However, if general radiologists read a brain scan, they’ll tell you about tumors, but they’re not looking for subtle clues that may indicate, for instance, frontotemporal dementia (an uncommon type, which causes problems with behavior and language), or indications of Alzheimer’s.”
And, within the world of medicine, doctors don’t go looking for ailments for which there is no viable treatment. So, doing a diagnostic brain scan would be rare, at best.
For the loved one of an elderly
“Fewer than 1 in 5 Americans are familiar with mild cognitive impairment (MCI), which can be an early stage of Alzheimer's.”

“The number of Americans living with Alzheimer’s is growing — and growing fast. More than 6 million Americans of all ages have Alzheimer’s.” www.alz.org
person who is exhibiting the beginning signs of Alzheimer’s, it’s important to be aware of the stages of this disease. There are seven recognized stages, which experts say require different sorts of care. These simplified stages are taken from the Clinical Dementia Scale, a guidepost which has a specific numbered scale for doctors.
STAGE 1: This stage won’t be noticed by others. A person may be worried about occasional lapses, but isn’t a reliable source that anything is actually wrong. For example: a resident at Lambeth House in New Orleans, who was living in the independent

living section of this facility, drove herself to a neurologist because she was concerned about losing her memory. Her concern? She was a new resident and couldn’t remember the names of all 100 people she had recently met. The neurologist pointed out that by the end of the day, he might not remember her name. He assured her that her fears were unfounded. It illustrates that everyone’s frame of reference is different.
“Although ordinarily, when the patient is concerned, there’s usually not a problem, you must still complete a further inspection, in the event the patient’s concerns
Our mi ssi on is to en ri ch li ve stouche db yd emen ti at hrou gh re sp ec tf ul com pa ssi on atec are. Ou rfocu si stow ards th e re si de nt ’s qu al it yo fl ife. Th es ta ff ares pec if ic al ly tr ai ne d and prov id ei nter ac ti ve ca re .L us hg arde ns an ds ecu re outdoo rp ati os en han ce our st im ul ati ng en vi ro nme nt.
• 24 -h our Li cen se dN ur se
• Pr ivates tu di oa nd ex pan ded st udi oa par tm en ts
• Th re ec hefp re pared mea ls da il y
• As se ss me nt and deve lo pm en t of perso na lized carep la ns
• Ad ap ti ve exerci se cla ss es
• Mu si ca lp er fo rm ance sa nd en te rt ain me nt
• 24 -h our eme rg en cy ca ll se rv ic e
• Ba th in ga nd dres si ng ass is ta nc e
• Li nen and la undr ys
have some basis,” Hargrave said.
STAGE 2: The second stage begins with holes in the memory. The patient may repeatedly go into rooms and not remember why they are there. Maybe they cannot find the right word, or are continually misplacing objects.




STAGE 3: Now, the differences in behavior are noticeable to others. The patient is in a state of mild cognitive impairment, forgetting what he’s just read, and losing short-term memory, for the most part.
STAGE 4: “At stage four, you’re in mild cognitive decline,” said Dr. Susan Nelson, an Ochsner internist with a specialization in geriatrics. “At Thanksgiving dinner, that person may put the turkey in the pantry rather than the oven. At stages three and four, this is when a lot of diagnoses are made.”
STAGE 5: This means forgetting personal information, like a phone number or address. In mild to severe cognitive decline at this

point, forgetting how to bathe or choose clothing are common symptoms.
STAGE 6: Now in severe cognitive decline, most patients in stage six are incontinent, with bowel and bladder problems. Many cannot remember the names of their loved ones.
STAGE 7: Total dependence on others. Walking and eating are extremely difficult without assistance. At this stage of Alzheimer’s, which represents very severe cognitive decline, patients struggle with words. Patients at this stage need skilled nursing care, or home healthcare, often round-the-clock.
“The decline can be swift, or can take a decade or longer, which is why it’s important for patients to make decisions when minor symptoms are first noticed. In this way, good decisions can be documented about what their care will be, as dictated by them, moving forward,” said Nelson.
As Alzheimer’s progresses, and other organs of the body apart from the brain are beginning to lose function, it may be necessary to consider palliative care, an extra layer of support for patients with serious illnesses. This sort of care is offered by many skilled nursing facilities where the patient is already residing. For those residing with relatives, and who are receiving home health care, oftentimes when the patient can no longer bathe himself or is losing weight because the brain is no longer able to receive signals that would indicate hunger, palliative care is probably indicated.
“Palliative care can be as helpful for



the caretaker as it is for the patient,” said Tiffany Liu, MD, a neurologist with LSU Lafayette. “Within the palliative care component are social workers who will actually come into the home and figure out how to specifically help.”


Liu added that there is a difference between palliative care and hospice. Hospice is definitively reserved for people who have six months or less to live. Unlike certain cancers which have already metastasized, spreading to other organs, no one can predict just how long an Alzheimer’s patient has to live. Some patients live 10 years or more after diagnosis.

Researchers at Pennington Biomedical Research Center are dedicated to finding answers about healthy aging.
At any point in time, this worldrenowned research center hosts multiple clinical trials related to Alzheimer’s and dementia. Topics can include whether or not physical activity can improve brain function, how an individual’s cognitive ability, quality of life, mood and mobility changes over time, and if certain pharmaceutical drugs can be used as a possible prevention for Alzheimer’s and dementia.

Certain divisions of Pennington Biomedical are specifically dedicated to this work, including the Institute for Dementia Research and Prevention (IDRP), which conducts longitudinal studies on key factors related to the development of dementia. The IDRP also runs clinical trials in conjunction with the National Institutes of Health and pharmaceutical companies to assess medications to treat and prevent dementia.

“While everyone would love to find disease-modifying medications or treatments, we are very proud that we have brought to Louisiana the first and only research institute of its kind between Houston and Birmingham,” Dr. Keller said. “We provide people across Louisiana with access to trials

and free evaluations.”

Dr. Owen Carmichael, Director of the Biomedical Imaging Center at Pennington Biomedical, said researchers are also using precision medicine to better identify dementia and Alzheimer’s risk factors. Carmichael said previous studies have shown that people who eat a healthy diet, exercise regularly, take proper medications and stay active tend to have a lower risk of dementia and Alzheimer’s.
However, there are still cases where people who follow all of those measures are diagnosed with dementia or Alzheimer’s.
“With some cancers, we know that a person with a certain genotype is at a higher risk. That’s what we don’t yet have in Alzheimer’s and what we need to move towards,” Carmichael said. “There is a whole host of unknowns related specifically to genetics.”
As the research continues, Keller and Carmichael said Pennington Biomedical is working to engage more participants in their work.
Historically, study participants tend to be affluent white individuals with the extra time to be involved in research. To ensure better representation, Carmichael and fellow researcher Rob Newton have been spending more time in AfricanAmerican and rural communities to
By Amanda McElfreshget to know residents, build trust and increase access to clinical trials.
“In African-American communities, there have been generations of mistreatment that have led to huge trust issues,” Carmichael said. “For people in rural areas, transportation has been a barrier, especially with recent gas prices. We’re working to build those relationships and also raise funds for mobile units to bring our work to them in a more tangible way.”
Dr. Keller said that by engaging more people in dementia and Alzheimer’s research, the impact of such studies could be even greater.
“We are not looking to do research just to publish papers and increase our knowledge,” he said. “We want to have an impact and I believe that the work we do here can make a difference in people’s lives.
Considering that $300 billion a year is currently spent on healthcare for those with dementia, a number which will explode to $1.5 trillion by the year 2060, it would seem only appropriate that research monies to study causes and cures would be pouring in.
Certainly, you would expect funding from a government whose entire healthcare system could easily be bankrupted by these scientific predictions.
But it hasn’t always been the case.
It certainly doesn’t mean, however, that individual academic institutions who’ve obtained large medical grants, and are even working with benefactors from the private sector are not hard at work trying to solve one of the biggest medical mysteries of our time.
The Alzheimer’s Association itself has granted over $70 million over the last year to 253 different scientific organizations. There’s ongoing research everywhere — in labs, at the Veterans Administration and even among Catholic nuns, just to scratch the surface.
Currently, a New IDEAS study is being conducted by the Alzheimer’s Association. The study involves amyloid scanning of the brain, not with an MRI, but with a PET (positron emission tomography) scanner which looks at so-called hot spots within the brain.
The study also involves the examination of biomarkers, changes that a disease like dementia might cause in the body that would show up on specific blood tests.
Longitudinal studies which can last decades can often give us a glimpse into the connection between early behaviors and an eventual diagnosis of Alzheimer’s.
‘Idea density’ vs. dementia?
In one striking study, beginning in 1986, University of Kentucky scientist David Snowdon studied 678 Catholic religious sisters –part of the School Sisters of Notre Dame.
By painstakingly researching the sisters’ personal and medical histories, testing them for cognitive function over the years and even dissecting their brains after death, he showed a connection between lucid expression early on in life and the ways that women of similar lifestyles, socioeconomic status, access to health care and social support performed in later life. None of these women had ever been married or had children, which gave them each similar risks for certain cancers and other diseases. Snowdon had access to autobiographies each of the women had written in their 20s, which allowed him to compare cognitive abilities early in life to the women’s present state.
Snowdon and his team had a wealth of information to conduct their study, with each
autobiography being given an “idea density score” that attributed a numeric value for the number of distinct ideas written per 10 words in a sentence.
Surprisingly, researchers found a strong positive association between idea density in early life and a lack of dementia later in life. Research suggests that nuns who had lower idea density scores had an increased risk of developing dementia and a lower life expectancy, while nuns with higher scores tended to live a long, dementia-free life. The association was so direct that Snowdon could predict which nuns might have dementia simply by reading their letters.
The ‘gold standard’
While it is true that genes and physical attributes of the brain are large factors in disease risk and presence, one impressive piece of the study was the life and death of Sister Mary. She is referred to as the “gold standard” of healthy aging because of the vibrant and full life she lived for over 100 years. Upon her death, analysis of her brain revealed
lesions and other signs of AD that should have caused her to have poor cognition and other health problems. She did not.
Sister Mary enjoyed reading, knitting and socializing up until her death. It is thought that her lifelong career as a teacher along with a well-balanced diet and proclivity for reading helped her defy physical and genetic predisposition to dementia. She is an example of how lifestyle choices may have much to do with who ends up with dementia and who rises above it.
Scientists are nearly unanimous in agreeing that with the brain, “use it or lose it.” The latest V.A. studies have even shown changes in the thickness of the gray matter in the brains of those still working versus those who had retired.
“This supports all of the evidence to date about building up cognitive reserves that may counteract what would otherwise naturally occur in your brain and cause cognitive issues,” said Dr. Demetrius Maraganore, chief of the Department of Neurology at the Tulane University School of Medicine.
On Sept. 27, Biogen and Eisau, two biotech companies, announced their development of an intravenous drug to treat Alzheimer's disease. Their phase III trial for lecanemab showed a 27% lessening of cognitive decline in the 1,800 people participating in the blind study who were given this drug vs. a placebo.
The drug targets the amyloid plaques that form in the brains of Alzheimer's patients, although most researchers aren't sure whether those plaques are a response to another cause, or the cause itself.
Cognitive scores were raised slightly less than half a point on an 18-point scale, and the drug did produce brain swelling and some bleeding in 21% of trial participants. The announcement has
most researchers waiting to see more data, which will be released in November, ahead of asking for FDA approval.
"If we actually see clinical improvements, should the FDA decide to approve this drug, then 27%, while it may sound like a low number, would be extremely beneficial for those who get this disease in their 50s, and otherwise would have a long life ahead of them if we could stop progression," said Dr. Demetri Maraganore, who is the director of the Tulane Healthy Brain Institute, and a life-long researcher into Alzheimer's.
Drug companies Roche and Eli Lilly are expected to make announcements within the next few months on drugs they have been testing.


The most important thing to remember about treating Alzheimer’s disease is that the many drugs which have been approved by the FDA over the years have had only minimal results at stopping its progression.
And even then, only when the disease is caught in its very early stages, when it can still be classified as a mild cognitive impairment.
These drugs are not cures. At best, they are aimed at slowing down brain deterioration in two categories: cognitive, which affects memory and orientation, and functional, which is responsible for one’s ability for example, to handle personal finances, or something as simple as doing household chores.
“One of the main pharmaceuticals we’ve seen used on early Alzheimer’s patients is a drug named Aricept,” said Dr. Heidi Sinclair, an internist with Ochsner 65+ in Baton Rouge.
“It is supposed to improve memory, but we’ve seen only mild to modest benefits. Just as important in slowing down any decline is making sure to get a good night’s rest (and always treat sleep apnea), participating in activities with others, and looking at any other medications you may already be taking to ensure that some of the side effects are not causing brain fog.”
Eat right Healthy eating is critical,
Sinclair said. Anything that is good for your heart and your kidneys is good for your brain. And, she stressed, stay away from processed food with lots of chemicals.
Eating real food, without labels, is the healthiest for the brain. In fact, some chemicals found in processed food can turn into toxins in the gut, and scientists already know there’s a connection between what’s in the gut and what may end up in the brain.
“We’ve known for quite some time now that chronic inflammation and toxins can travel to the brain,” said Anneliese Boettcher, PhD, an Ochsner neuropsychologist in New Orleans. “Once a diagnosis of mild cognitive impairment is made, our treatment goal is to slow everything down, and stabilize where you are, without further degeneration.”
Boettcher says that thus far nothing has reversed this disease, but some folks have managed to stay in a mild cognitive impairment phase for the rest of their lives by concentrating on
their health.
Research-based brain scans have shown an increase in brain density when the brain is fed the proper nutrients. It’s all about getting rich, oxygenated blood to those vital neurons in the brain, she said.
Science has already identified that those with higher educations, and those who continue to learn long after school is over are less inclined to be affected by Alzheimer’s. This is because these people are doing more cognitively demanding jobs over long periods of time, and are building up their cognitive reserves, which can protect the brain from the onslaught of Alzheimer’s.
Take your brain to the gym?
It’s all about expanding the brain, and keeping it engaged, and that means sometimes engaging in tasks that are difficult to do, whether it’s learning a new language, or writing with your non-dominant hand.
“I tell my patients to treat their brains like a muscle, and take it to the gym,” says Ochsner PhD and neuropsychologist Emily
When attempting to treat a diagnosis of mild cognitive impairment, preceding Alzheimer’s or dementia, it’s important to rule out other factors which may be causing anything from brain fog to memory loss. Poorly controlled blood pressure, cholesterol and diabetes can mimic symptoms which are initially apparent in those with cognitive issues.
Blood pressure: “If your blood pressure’s systolic number (the top number) is above 150, and your diastolic pressure (the bottom number) is above 90, and your LDL cholesterol is also high, you are damaging your small blood vessels,” said neurologist Tiffany Liu of LSU in Lafayette. “Those vessels supply blood to the white matter of the brain. Without sufficient amounts, the brain shrinks.”
Hearing loss: Years of science have revealed that there’s a correlation between hearing loss and the onset of dementia. Apart from interfering with social interactions and causing isolation, researchers now believe that there’s a physiological component involved. When the portion of the brain that interprets sound is no longer stimulated,
Brickell. “Do something that stimulates your brain. Volunteer at a dog shelter, learn a new recipe: anything that keeps the brain cells firing.”
Nicholas Bazan, M.D., who heads the Neuroscience Center of Excellence at LSU’s School of Medicine, has longed believed that music stimulates the brain and can even bring back memories. His book, “Una Vida: A Fable of Music and the Mind," was turned into a dramatic film in 2014, titled “Of Mind and Music.”
“We do not know yet precisely how circuits in the brain that are tied to memory are activated by music, but we do know that there’s a relationship between the two,” said Bazan.
Echoing these sentiments is Carol Bailey, RN, a dementia caretaker's trainer and consultant, who believes it's important to use music to engage the right side of the brain, working around damaged cognitive portions of the left side.
Engage the right side, which hasn’t been affected by the cognitive issues, she said, and it opens up a new portal, where just 10 minutes of music can lead to 2-3 hours of less agitation and less challenging behaviors for patients affected by any of the dementias, including Alzheimer’s.
the brain ages. It’s important for everyone over the age of 65 to get his or her hearing checked, so there’s a baseline against which any deterioration can be measured.
Vision: Get your eyes checked. Age-related macular degeneration, in which blurred vision or partial loss of vision occurs, is caused by abnormal blood vessels that leak fluid or blood into the part of the retina in the back of your eye which is responsible for central vision. When the brain doesn’t receive sufficient or correct visual information, this contributes to cognitive and memory problems, and can result in dementia.
“An eye exam can detect evidence of retinal vessel damage,” said LSU’s Bazan. “The retina is the window to the brain, and in an examination of that part of the eye, we can get clues and make predictions as to whether this individual will get Alzheimer’s.”
Without an existing cure for Alzheimer’s, treatment and prevention of this disease means keeping a close tab on organ functions throughout the body, which ultimately affect the brain.













Perhaps the worst thing about being the caregiver of parents is watching them regress.
They took care of you, and now you’re taking care of them. It’s counterintuitive and poses many psychological issues, particularly for parents who aren't used to being told what to do by their children.
And, it’s frustrating for caretakers to be confronted with a oncecompetent parent who now is out of touch with reality.
But, it’s important to remember that arguing with a dementia patient, whose brain is not functioning properly, is pointless.
“If your parent is living with you, and suddenly blurts out that they want to go home, even though that house was sold years earlier, it’s important to remember not to disturb their reality,” said Carol Bailey, R.N., who specializes in training caregivers about dementia.
“You need to redirect them to a place where they have feelings about home," Bailey said. "So, you open up the photo album and talk about the good old days. Their brains may have a vague feeling that something is wrong about their situation, but they don’t know what because their impaired brain fills in the holes with unreliable information.”
Cortisol vs. dopamine
It's important to remember that calling an Alzheimer’s patient out on their delusions is fruitless, because it doesn’t work, and causes them to be more agitated, says Bailey.
Furthermore, it raises their cortisol levels — which simply induces more stress. It may be viewed as making up stories, but their brains are giving them these false images. Going to their reality is important, without reinforcing
falsehoods.
So, when they suddenly ask to pick their kids up from school, your gentle response might be “How many children do you have?”
It’s all about re-direction.
For the well-being of the patient, it’s important to find ways to get them large doses of dopamine, the feel-good hormone, for their sense of well-being.
The process can be simple. If patients are organizers, give them tasks that instill a sense of accomplishment. Organizing coins from a jar, alphabetizing your bookcase or sorting magazines by topic: These are tactile endeavors that cause the brain’s neurons to fire, creating a synapse which produces better blood chemistry.
And it's important that the patient isn’t just taking in stimuli, but providing it, too. So, rather than brush a loved one’s hair, use their own hand on the brush, while you guide it.
Isolation fuels Alzheimer’s and dementia, so involve your parent or loved one in communal activities, where they are functioning and feeling needed. If they can help you cook, for instance, it gives them a sense of autonomy.
Being a caregiver can be frustrating, and can lead to feelings of helplessness and hopelessness, and therefore it’s important that the caregiver gets adequate support, not just physically, but emotionally as well.

“When a patient comes in to my office with their caregiver, it’s almost certain that the person stressed out is the one who’s taken on all of the responsibility of the person who is ill,” says Anneliese Boettcher, PhD, a neuropsychologist at Ochsner in New Orleans. “It’s important that caregivers focus on their own
mental health and wellness.”
Boettcher says that caregivers should rotate with other family members when it comes to outings or special time.
Senior centers in your community can take the burden off of at-home caregivers while the caregiver goes to work. It’s important for caregivers to check out podcasts on Alzheimer’s care, and get relevant books to read. Every community has local support groups where caregivers can commiserate with each other, and learn better ways to handle things at home, from others who have found themselves in the same situation. There are even Facebook groups to join.
There is a lot of guilt associated with moving loved ones to assisted living facilities or nursing homes, when the time comes. But, experts believe it’s important for caregivers to allow themselves to be the child or the spouse again, and leave the role of 24/7 care to professionals.
How does one move a parent into the home?
When is the right time to consider assisted living? How does a caregiver suddenly cope with an added financial burden?
There’s a lot of expert advice out there.
“The 36-Hour Day” by Nancy Mace and Peter Rabins: This book was recommended by many experts and is available at most libraries.
“How To Care For Aging Parents” by Virginia Morris: A one-stop shop for caregivers.

Alzheimer’s Association website: alz.org/care
AARP website: aarp.org. Search for family caregiving.
Google: Teepa Snow on You Tube. Snow is a dementia care consultant/educator and occupational therapist. Her videos, beginning with “Caring For Someone With Dementia," cover everything from getting your loved one up from the dining table, to tips on how to dress them in the easiest manner possible.







 By Leslie Cardé | Contributing Writer
By Leslie Cardé | Contributing Writer
As Alzheimer’s disease or dementia progresses, there’s inevitably a discussion concerning just how much assistance the person will need, and how well a home living situation will meet those needs.
“Our guideposts concern such things as whether their condition has now affected their job, whether or not their driving is in a safe realm, are they still able to pay bills on a timely basis, and overall, take into account just how much their condition has affected their day-to-day living,” said Anneliese Boettcher, PhD, Ochsner neuropsychologist.
For those considering taking in a loved one with a dementia diagnosis, there are all sorts of things to think about.
Will there always be someone at the house to look after this person? If they are being left alone, can that be done safely? Or, will it be necessary to hire a caretaker, which can be costly?
Can you install double deadbolt locks on the doors, so the person cannot amble out of the house, never to return? And, should you consider additional failsafes like cameras and alert buttons?
There are many types of assisted living residences, some that include an independent living wing, another area for those who need assistance, and another for those who need skilled nursing care. These combination facilities with tiered care
are called CCRCs, which stands for Continuing Care Retirement Community, or a Life Plan Community

“Our CCRC, Lambeth House in New Orleans, requires an in-depth assessment before moving in, to give us a good idea of placing the resident in the appropriate level of care,” said Jeré Hales, chief operating officer. Medicare generally does not pay for assisted living, and Social Security checks usually fall short of the cost. Therefore, residents of assisted living usually must rely on “private pay,” their personal resources, to pay for rent, meals, medication aides, activities and staff in assisted living communities.
There are facilities that allow residents on Medicaid within the nursing home component of the combined-resident facilities. But, to qualify, an individual must have less than $2,000 in countable resources.
New Orleans’ Woldenberg Village, owned by Touro Infirmary, LCMC Health, is a tiered facility, but it accepts qualified Medicaid patients in its nursing home. It’s important to check on a variety of facilities, as they all provide different services.
• If you decide that having your loved one at home is not practical and begin to research assisted living facilities, make sure to have a list of what you want to know before going to visit the facility.
• Always take your loved one to a primary care physician before considering assisted living. This is to rule out any underlying medical conditions that may mimic a loss of cognition.
• Compare prices of facilities. They vary wildly. Be sure to ask what sort of professionals are in residence, and who will be taking care of your loved ones.
• How many residents are in the facility, and what are the opportunities for social interaction?
• Talk to your loved one, take them to the facility and let them get familiar ahead of checking them in.




When a family member is diagnosed with Alzheimer’s or another dementia, it can be overwhelming. It means the family must pull together through fear and frustration in order to make the best decisions about care.
The two biggest bones of contention involve living arrangements, specifically who the primary caretaker will be initially, and how finances will be handled — even end-of-life decision-making.
When it’s just a spouse making these decisions in conjunction with the diagnosed patient, it’s much clearer who’s in charge. But, if the spouse is gone and there are multiple children, it can become much more complicated and can cause family conflicts.
“As both a social worker who counsels families, and an attorney who understands Louisiana law, I advise family members to get together with the patient when they are first diagnosed and are
still lucid, or in the best possible scenario beforehand when this person is still healthy, and find out what they want,” said Carrie Pailet, LCSW, JD, Gesund Pailet, LLC.
“Naturally, most people would prefer to stay in their own homes for the rest of their lives, but that’s not always possible for financial reasons, and caregiving issues, as well.”
Dividing caregiving evenly is probably not a reality, with siblings often living in different cities, but sitting down and making a list of what each family member will be responsible for is a good idea to unite everyone behind the best care for the patient.
If impasses about particulars arise, it might be time to get a mediator.
Pailet says that caregivers and family members can consult with a social worker, a psychologist, the patient’s doctor, or a member of
Isolation can exacerbate the symptoms of Alzheimer’s disease.
So, before you consider leaving a loved one at home during the day, while you’re at work, think about this.
No matter how many locks you have on doors and windows, no matter how many precautions you’ve taken, like turning off the stove, this person is still alone with his thoughts, with no form of external stimulation.
Having the TV on is not considered stimulation, as it’s one-way communication, and doesn’t give patients the sort of stimulation they need to fire up the brain.
Family members, particularly caregivers, often feel guilty about any number of things, most of which derive from feelings of inadequacy about knowing
the clergy to act as an impartial observer who can often see things more clearly, without personal family grievances getting in the way.
It’s important to create a list of what the disputes are specifically about before sitting down with any third party.
The goal should be to walk away with solutions, which may sometimes involve compromises and options you hadn’t previously thought of.
Pailet says that setting up an important document like a Power of Attorney is very important to handle early on, so that before anyone has been diagnosed, it’s clear who will be in charge and who is making the decisions for the loved one down the road.
These documents can also include a division of financial resources, so it becomes clear whether your relative might want a house sold to pay for care expenses or how much cash there is available for care, and even what the Social Security check brings in.
“Giving someone power-ofattorney simply means you’re putting someone in your shoes,” said Pailet. “It doesn’t mean you’re giving up your authority, but sharing it with someone you trust. DNR’s (do not resuscitate orders) can also be put into this
document, as it can include medical matters.”
This only comes into play if the person executing the powerof-attorney is no longer able to participate in the decision-making process. Ordinarily, that means a medical professional deems them incompetent.
When talking with family members about a loved one’s care, it’s important to keep the conversations civil. As any good therapist will tell you, that means not blaming someone else for any lapses in communication, and using what are called “I” statements. For example, you might say:
“I’m feeling frustrated and tired trying to keep up with my work schedule, while running dad around to his medical appointments,” rather than “You have no idea what it’s like to try and take care of someone who behaves like a 5-year old.” Being accusatory alienates the other party.
When moving a loved one from a family living environment into either assisted living or a nursing home, be sure to do your homework, and consult with the medical team members who have been involved with the testing and treatment measures for them.

just what to do, and concluding that whatever they are doing, it isn’t enough.
Two good websites cover different areas of concern.
The Governor’s Office of Elderly Affairs: www.goea. louisiana.gov gives information about aging and disability resources, aging well, and an ElderCare locator.
In the event there is no spouse or children, guardians can be found to oversee medical care at Louisiana Guardianship Services, Inc. : www.laguardianship.org.
This is for adults who are incapacitated to the extent that they are unable to make their own decisions, but do not have loved ones who can take on this responsibility.
Thanks to expanded home health services that meet multiple needs, more dementia and Alzheimer’s patients are remaining at home in a familiar environment surrounded by loved ones.

Lane Home Health offers several services, including skilled nursing, physical, occupational and speech therapy, medication management, medical nutrition therapy, and assistance with personal care. Lane Home Health has been in operation since 1984 and serves families within a 50-mile radius of Zachary, including the Baton Rouge area.

“When our health care professionals initiate care in a patient’s home, they perform a complete assessment of the patient and home environment,” said Lori Shaw, Lane Home Health’s clinical manager. “Additionally, they provide patients and caregivers with education on disease processes and communicate with healthcare professionals regarding the patient’s care.”
There is an emphasis on making the home environment as safe as possible. Physical and occupational therapists
focus heavily on preventing patient falls. This might include placing cues on the walls to remind patients to use their walker and shower chair, as well as installing grab bars, clearing clutter, and removing rugs and other tripping hazards.
“We like our patients to stay active but in a safe way,” Shaw said.
“Our occupational therapists teach patients how to do small tasks and household chores to keep them engaged and help maintain strength.”
Lane Home Health’s social workers assist caregivers and patients with legal matters such as living wills and power of attorney documents. They also provide information on finding an appropriate facility if the patient can no longer remain at home.
“Even after a diagnosis of dementia or Alzheimer’s, patients can continue to have meaningful lives,” Shaw said. “We encourage
By Amanda McElfresh amcelfresh@theadvocate.comthem to look at old photos, listen to music, stay involved in hobbies, and spend time with their loved ones.”
“Family members always want to understand what’s going to come next,” she said. “Some patients may develop behavioral issues or ask the same question several times, which makes for a challenging situation. Thankfully, we are able to provide resources in the community and from our staff so caregivers can also receive the support they need, as well.”
The financial consequences of a diagnosis of Alzheimer’s disease or any one of the rarer dementias can easily fall to the family of the patient. In any diagnosis that includes declining mental health, it’s important to get one’s financial house in order.

According to the National Institute on Aging, that may include putting legal documents together that include a will, a living trust, and an advance healthcare directive. Although these documents exist online, you may want to enlist an attorney, as some requirements for these documents change state by state. A living will records a person’s wishes, whereas a durable power of attorney designates a specific person as a proxy to carry out those wishes. A living trust addresses money management, while the diagnosed individual is still alive.
Louisiana is the only state which adheres to civil law, rather than common law, so assumptions about who is in charge in the absence of advance documents can be substantially different. Majority rules
“There is a statute in Louisiana which says that all of the children have equal rights to make decisions about their incapacitated parent,” said
Carrie Pailet, a social worker and attorney with Gesund Pailet, LLC. “Many folks are under the impression that it’s the oldest child who’s in charge, but in Louisiana, the majority rules.
“Of course, if you have an even number of children, there may be no actual majority, and that’s where problems come into play.”
Heading off problems before they begin is critical. If you notice that your loved one is having memory problems, it may be time to have a conversation with them and initiate some provisions for bill-paying, whether someone else takes charge or auto-payments are put into place.
Problems managing money are one of the first signs of dementia. It may be helpful to put limits on credit cards, as well, to manage spending that might become out of control.
Seventy percent of people over the age of 65 will need some
sort of long-term care. It may be temporary, but it can be expensive. According to AARP, the cost of a private room in a nursing home in 2020 was $115,000 a year, and it’s important to remember that is not a reimbursable expense under Medicare, unless the stay is under 100 days.
A year in an assisted living facility during that same period ran $55,000 a year, on average, nationwide. And, if you think the option to have in-home care is less expensive, hiring an hourly home health aide (based on a 44-hour workweek) was running $60,000 a year. Add to these amounts inflation over the last two years, and the cost is staggering.
There is the option of long-term care insurance, but it must be bought when you are still fairly young to make the premiums affordable. And, denials are frequent for those with pre-
existing conditions, whether it’s diabetes, heart disease or even obesity.
The big variable in the price of premiums depends upon how much you want the policy to cover, and for how long. The average price for premiums if you’re 55 years old is about $2,200 a year for $200 in benefits a day (although a private room in a nursing home costs around $300 a day.) Women, traditionally, are more expensive to insure, as they live longer.
But, wait until you’re 70 to get long-term care insurance, and a man’s premiums are roughly $5,000 a year, while a woman’s is over $7,000.
According to the RAND corporation, the truth is in the statistics.
Only a small percentage of Americans (5-10%) will require the extended type of nursing care (4 years or more) which longterm healthcare insurance was designed for. Another downside to buying this type of insurance is that prices aren’t fixed, and premiums can go up at any time, pricing you right out of the marketplace.
Decisions about any type of insurance should be made when a person is middle-aged, before the premium costs are prohibitive.
There are alternatives to buying long-term care insurance, but that means investing retirement money early enough to cover the rising cost of being a resident in an out-ofhome facility.
In Louisiana, state-run Medicaid programs will cover nursing care only after you’ve depleted any savings down to $2,000. That would mean depleting all of your retirement savings before becoming eligible. Before you think you can just begin giving money away after a diagnosis, the state has protected itself against this.
“There’s something called the look-back period,” explained Carrie Pailet, a social worker and attorney with Gesund Pailet, LLC.
“In Louisiana, that period of time is 60 months (five years). So, you cannot suddenly drain someone’s bank account. The state can determine if monies were given away at less than fair market value, and will deny your Medicaid claim.”
Statisticians have run algorithms which indicate that at the current rate of inflation, and with continually rising healthcare costs, by 2050, a private room at a nursing facility for a year will cost well over $300,000.
Any way you slice that number, it’s clearly a figure that will break most people’s banks, and many healthcare analysts say will break the system.











Although there is currently no cure for Alzheimer’s disease, it is certainly not for lack of research. But recent discoveries that have proven themselves in mice models may be the hope for the future of understanding and treating this mysterious disease that is taking the lives of so many elderly people.
The one fact that everyone in the various fields of neuroscience seems to agree upon is that inflammation in the body is causing inflammation in the brain, and the neurons in our brains do not do well under duress.
“We have good and bad lipids in our bodies, and the good ones are very protective of our brains,” said Nicholas Bazan, MD, PhD, and Director of the Neuroscience Center for Excellence at LSU.
“In 2017, elovanoids (the good lipids) were discovered, and we copied how the brain made them and reinserted these lipids into a Petri dish with human neurons, to prove our theories.”
To further prove how these lipids are protective, mice were given the bad Alzheimer’s gene, known as APOE-e4. As Bazan put it, within four to five months, their memories were down the drain.
“But, when we put the new lipid mediators through the noses of these mice, before giving them the bad gene, they did not lose memory and we protected the pathology of the brain,” Bazan said.
Could a simple nasal spray protect our brains from Alzheimer’s? Studies would still need to be done in primates, before clinical trials in humans, but the study is a step in the right direction.
At Ochsner, researchers are building databases to try to predict in younger people who will get Alzheimer’s.
“We leverage the databases as we explore younger people who may be having very minor symptoms,” said Emily Brickell, Ph.D, Ochsner neuropsychologist. “We are looking for subtle patterns using artificial intelligence. The sooner we figure out who’s at risk, the sooner we can do interventions.”
And, at LSU, research may be proving that just 30 mg a day of fiber in your diet will keep your bad gut bacteria in check, by absorbing toxins that can travel to the brain.
Dr. Walter Lukiw, professor of neuroscience at LSU, believes upping your soluble dietary fiber could be a game changer in protecting the brain. Most Americans do not get even half of the average 30 mg requirement.
At Tulane, Dr. Demetri Maraganore, chair of the Department of Neurology and director of the Healthy Brain Aging Initiative, believes that the population should be tested, because knowledge is power. Knowing your genetic profile can clue you in to your risks. For instance, if neither of your parents had Alzheimer’s, your risk
is only 10%. One parent with the disease ups your risk to 25%, and with two parents with Alzheimer’s, you inherit two copies of that gene, putting you at a 50% likelihood of risk.
Because Dr. Maraganore is a firm believer that gut health is imperative to a healthy brain, he has adhered to the Mediterranean diet for decades, for its fiber-rich, nutrient dense components.
Now, a process that’s been used in the past for those with chronic diarrhea may be the future of treating poor gut health leading to Alzheimer’s.
“We are talking about fecal transplants, being used successfully already in gastrointestinal disorders, that could be used to treat dementia and stop its proliferation. There’s an NIH grant to harvest healthy fecal gut matter.”
The hope is that if it works in primates, there may eventually be a pill that individuals could take to keep their microbiome in order.
‘We will solve the riddle’
Until the research pans out, doctors warn against quick fixes.
“You cannot turn on the television without someone talking about over-thecounter remedies for failing cognition,” said Dr. Ronald Fiore, neurologist at the Culicchia Neurological Clinic, part of LCMC Health at West Jefferson Medical Center.
“These pills won’t kill anyone, but they have no science behind them, and they are expensive. When your options for treatment are nominal, people become desperate.”
But the search continues to find both a treatment and a cure.
“We’ve split an atom,” said Carol Bailey, RN, dementia educator. “I have no doubt that eventually
we will solve the riddle of Alzheimer’s. In the meantime, we need to proceed with getting help to those who need it, and doing everything we can to prevent it.”
Studies are ongoing at the Institute for Dementia Research and Prevention at the Pennington Biomedical Reseach Center in Baton Rouge. If you’d like to part of the clinical trials, or even receive free cognitive tests via email, contact the director, Jeffrey Keller at: jeffrey.keller@ pbrc.edu.
Genetic testing. If you are interested in genetic testing, DNA registries like 23 and Me can do the testing with a saliva sample, says Dr. Demetri Maraganore of Tulane.
There is currently a blood test called Precivity which can detect markers that are the hallmarks of Alzheimer’s disease. However, it is not yet covered by insurance, says Dr. Tiffany Liu, a neurologist with LSU in Lafayette.
On the horizon, Dr. Kevin Hargrave, Medical Director of the Neuroscience Center of Ochsner General in Lafayette, believes that technology will define this disease.
“We will eventually be able to eliminate bad genes, just like we do with the sickle cell gene.”
Get vaccinated. Covid-19 has produced lingering after-effects in many patients, says Gregory Bix, MD, Director of the Clinical Neuroscience Research Center at Tulane University’s School of Medicine.
“Getting Covid increases inflammation, and in some it’s having a lasting effect. There are now millions of people at risk for post-cognitive decline.”
Up your fiber. For those wanting to increase their fiber (24 grams for women, and 38 for men) as a hedge against Alzheimer’s, these 10 are highest in fiber:
Chia seeds (34.4 grams per serving)
Popcorn (14.4)
Almonds (13.3)
Dark chocolate (10.9)
Oats (10.1)
Split peas (8.3)
Lentils (7.3)
Chickpeas (7)
Kidney beans (6.8)
Avocados (6.7)
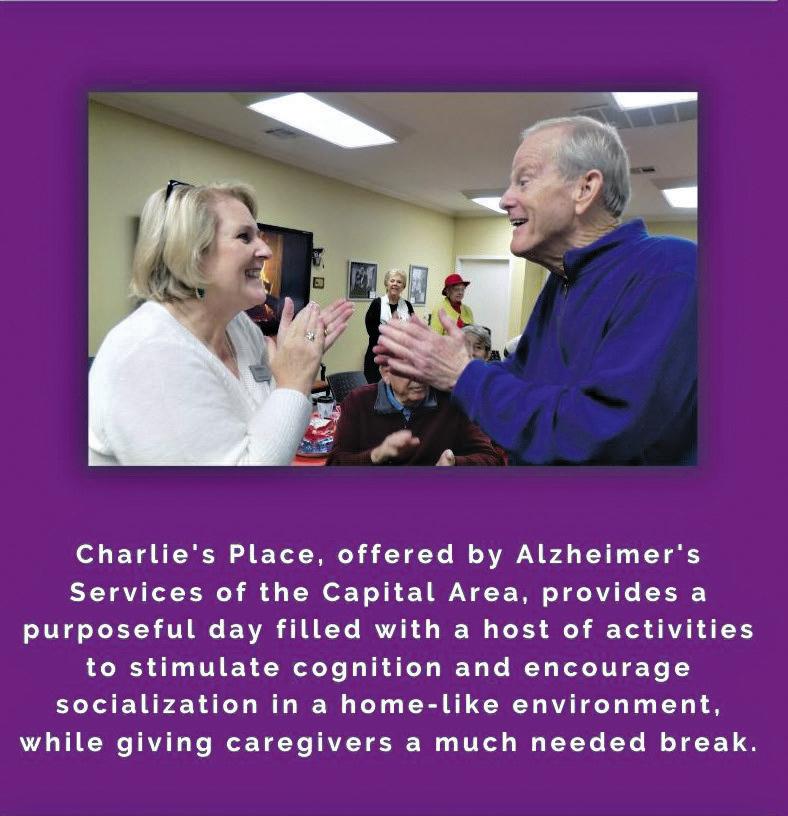
At Charlie’s Place, there’s no such thing as forgetfulness or memory loss; only new faces, a variety of activities and a place that feels just like home. Charlie’s Place Respite Centers, with locations in Baton Rouge and Gonzales, provide a safe environment for socializing for those suffering from Alzheimer’s disease.
“We provide a purposeful day,” said Barbara Auten, executive director of Alzheimer’s Services. “We have pet therapy, music therapy, exercise, and we have a garden where we roll out the putting green. We have an artist in residence who leads art projects with them. There is an array of activities that will stimulate and create that social environment.”
The clients interact daily with the iN2l, (It’s Never Too Late), a computer simulator program which provides interactive programs and activities such as a virtual bike ride.
“We had a client, a former pilot, who used the flight simulator and we set up the chairs like an airplane and our care attendants put stewardess caps on and served Cokes and peanuts while the client took them on a virtual flight,” Auten said. Charlie’s Place was named the
Adult Day Service Center in 2008 by the National Adult Day Services Association (NADSA) and is the only one of its kind in the state. This month, Charlie’s Place celebrates its 15th anniversary in Baton Rouge and 5th anniversary in Gonzales.
Besides special programs, Charlie’s Place provides a muchneeded break for caregivers.

Clients attend at least once a week and have set days in advance in an effort to accommodate caregivers’ schedules. Costs are based on daily rates.
The day services center is a program of Alzheimer’s Services of the Capital Area. The non-profit organization provides support and education to those affected by Alzheimer’s or memoryrelated dementia in 10 parishes: Ascension, Assumption, East and West Baton Rouge, East and West Feliciana, Iberville, Livingston, Pointe Coupee and St. Helena.

According to national statistics, approximately 21,000 individuals are affected with Alzheimer’s in the ten-parish area served, with the majority 65 years old and older. About 4% of that number includes younger onset or under the age of 65. And those numbers will continue to increase.
“People are living longer and
By Amanda McElfresh amcelfresh@theadvocate.comthey’re living long enough to develop Alzheimer’s,” said Auten, who suggests taking the MiniMental Status Exam (MMSE) at age 65 to establish a cognitive baseline.
November is Alzheimer’s Awareness Month and free memory screenings will be held every Thursday and Friday for three weeks from 9 a.m. - 12 p.m. Those dates are Nov. 3, 4, 10, 11, 17 and 18. Visit alzbr.org for locations. Other events for the month include a Fall Festival Nov. 9 from 1 p.m.- 3 p.m. at Alzheimer’s Services in Baton Rouge for those diagnosed with Alzheimer’s or a related dementia and their caregivers. The event will feature games, dancing, live music and cake cutting ceremony to celebrate the anniversaries of
Charlie’s Place. Visit alzbr.org to register for the event and to learn more about workshops and support groups for caregivers.

Charlie’s Place
Call: 225-334-7494
Online: http://alzbr.org/charlies-placeactivity-and-respite-centers/
ThisAt LCMC Health, we help people get the most out of life. That means keeping you well. And not just you, but your friends and neighbors, too. It’s what we do, from births to surgeries to checkups to emergencies, through more than two million patient visits each year. And we’re not slowing down. With 13,000 healthcare professionals across six hospitals, dozens of urgent care clinics and physician practices, comprising a $1 billion investment and counting, LCMC Health is making extraordinary care an expectation. We’re dedicated to keeping you, and every member of the communities we serve, well.
