





We understand that the nature of the care industry can be unpredictable. We want to make sure you’re covered when it matters most. Our industry experience means we know what types of risks you face, so speak to us today to discover how we can keep your business protected. At Phoenix we work with you to tailor a sustainable solution to your insurance to deliver improved risk management and savings.







Welcome from Care England
Professor Martin Green OBE, Chief Executive at Care England, welcomes you to the first anniversary issue of Savings, Solutions, and Sustainability (SSS)
Money saving updates
Discover quarterly solutions to some of the most pressing challenges you may be facing in your care setting, alongside key news stories from the sector.
Under the spotlight with Oliver Soriano
Oliver Soriano, Chief Nurse Officer at Lancashire & South Cumbria NHS Foundation Trust, recounts past and present experiences of internationally recruited health and care workers.
Protect your people: Social care providers must prioritise financial inclusion
Alex Ramamurthy, Head of Health & Social Care at Wagestream, examines factors impacting care workers’ finances and grapples with the issue of financial exclusion.
Orchard Care Homes: Reframing dementia care
Read how Hannah Miller, Head of Dementia at Orchard Care Homes, has developed and delivered Orchard’s Dementia Promise and Reconnect communities.
Break the cycle: Prepare for challenging talks about fee uplifts
Liam Fitzgerald, Senior Associate at Anthony Collins Solicitors, shares candid guidance to help you prepare for annual fee rate negotiations.






How to… Reduce your water and wastewater costs
Graham Mann, Director and Co-Founder of SwitchWaterSupplier.com, explains how you can become water wise and save money on your care setting's water bills.
Invest in growth: Why care about tendering in 2025?
Chris Martin, Managing Director at Tenders-UK, explains recent changes to procurement rules, and how you should get ready to make the most of new opportunities in 2025.
Legal matters
Philippa Doyle, Head of Social Care at Hempsons, highlights updates from the regulator issued in response to recommendations from Dr Penny Dash’s final report.

Act now: Take cyber security seriously or face the consequences
Kurtis Toy, Chief Executive at the Cyber Centre of Excellence (CCoE), outlines the essential steps to protect your care business from a cyber attack.
Members' voice: Your questions answered In this issue, Care England members' questions on physical activity, single-handed care, insurance, and more, are responded to with the latest advice and guidance.







Professor Martin Green OBE Chief Executive, Care England @Care England
Richard Ayres Social Care Advisor, Care England @Care England
Oliver Soriano Chief Nurse Officer, Lancashire & South Cumbria NHS Foundation Trust @WeAreLSCFT
Alex Ramamurthy Head of Health & Social Care, Wagestream
Search ‘Wagestream’ and ‘Alex Ramamurthy’
Hannah Miller Head of Dementia, Orchard Care Homes
Search ‘Orchard Care Homes’
Liam Fitzgerald Senior Associate, Anthony Collins Solicitors
Search ‘Liam Fitzgerald, Anthony Collins’
Graham Mann Director and Co-Founder, SwitchWaterSupplier.com
Search ‘Graham Mann, H2O Building Services’

This issue is CPD accredited. Scan the QR code to claim your CPD certificate and collect your points.



Chris Martin Managing Director, Tenders-UK Search ‘Tenders UK’
Philippa Doyle Head of Social Care, Hempsons @PhilippaDoyle1
Kurtis Toy Chief Executive, Cyber Centre of Excellence (CCoE) @CCOE_UK
editor@caremanagementmatters.co.uk
Lead Editor: Henry Thornton Content Editor: Aislinn Thompson
Designer: Rebecca Mendil Director: Lisa Werthmann
Studio Manager: Jamie Harvey
Advertising Manager: Aaron Barber aaron.barber@caremanagementmatters.co.uk
Care England is pleased to announce two brand new Facebook groups, one for Care England members only and the other is open to non-members and, specifically, carers. Please share these groups within your organisations and encourage engagement.

Care England Carer Community: www.facebook.com/share/g/15oAx8U5Ty
Care England Member Community: www.facebook.com/share/g/19V8CNMC5k
Professor
Martin Green OBE,
Chief Executive at Care

It is hard to believe we are celebrating the first anniversary of SSS. This publication has become a lifeline for providers across England, bringing together ideas, solutions, and practical advice to help navigate one of the most challenging periods in our sector’s history.
This issue comes at a time of deep uncertainty and pressure. The Autumn Budget, while offering a token grant, has left providers grappling with soaring costs and an ever-widening funding gap. It is no exaggeration to say that many providers are facing a financial cliff edge, with staff, services, and the people who depend on them caught in the balance.
England, welcomes you to the first anniversary issue of Savings, Solutions, and Sustainability (SSS). commitment. From practical cost-saving tips to workforce strategies and insights into how others are overcoming similar challenges, SSS is here to support you. It is not about quick fixes or empty promises – it is about sharing real, actionable ideas that can help you make a difference, no matter the size or structure of your organisation.
The Budget has made it clear that we cannot rely solely on Government to solve the problems facing adult social care. While Care England will continue to push for fair funding and reform, we also know the value of coming together to share knowledge, innovate, and build resilience.
undoubtedly be some of the toughest we have faced, with 2025/26 shaping up to be a particularly challenging time. But as difficult as things are, I am constantly reminded of the strength, resilience, and compassion that define our sector. These qualities are what keep us moving forward, even in the face of adversity.
I want to take a moment to thank every single person working in social care. Whether you are a provider, care worker, or someone behind the scenes, your work is invaluable. You are not just supporting individuals – you are supporting families, communities, and the very fabric of our society. Your commitment and care are what make this sector extraordinary, and they are deeply appreciated.
I would also like to thank the contributors to this publication who have shared their time, knowledge, and insights to make SSS the resource it is today. Your expertise and generosity have helped countless others, and I am so proud of what we have built together over the past year.
The challenges we face are immense, but so too is the determination of our sector. Every day, providers and their teams are delivering vital support to people who rely on us – working tirelessly, innovating, and finding ways to make things work even in the toughest of circumstances. It is this spirit that inspires SSS, and it is what this publication is all about, finding and sharing solutions to keep care services running and sustainable.
This issue reflects that
This publication is a testament to the power of collaboration. Over the past year, SSS has brought together contributors to share their expertise and their insights have already helped countless providers navigate complex challenges. Whether it is improving energy efficiency, addressing recruitment and retention, or planning for the future, the goal of SSS remains the same, to help you find solutions that work for your service and the people you support.
The next few years will
As we mark this first anniversary, I hope you find this edition of SSS useful, inspiring, and practical. If you have ideas, questions, or feedback for future editions, please do not hesitate to share them. This is your publication, and we are here to help you navigate the road ahead.
Thank you for being part of this journey with us. Together, we can face the challenges ahead and work towards a future where adult social care gets the recognition, funding, and support it truly deserves.
Professor Martin Green OBE is Chief Executive at Care England. Email: info@careengland.org.uk : @CareEngland


The adult social care sector is brimming with innovation to address some of the most critical challenges you may be facing. As well as presenting some of the solutions, the following money saving updates share key news stories from the sector. In this issue, topics covered include changes to food waste regulations, Environmental, Social, and Governance (ESG), and pressure ulcer prevention.
The TSA is launching a new initiative to help commercial laundries become more sustainable. The Global Laundry and Rental Emissions (GLARE) platform will allow laundries to easily measure their carbon footprint and aims to highlight how they can reduce their emissions.
Increasingly, health and social care providers are scrutinising their suppliers’ sustainability credentials – GLARE will give you transparent and comparable data about laundries’ emissions.
The TSA’s Sustainability Steering Group worked with consultant Grain Sustainability to make provisions within the industry’s sustainability roadmap to measure and reduce carbon emissions, using well-established platforms such as Compare Your Footprint.
This platform became the foundation for GLARE – however, the long-term vision is to specifically tailor it for the laundry industry. For example, it holds the potential to include emissions factors relating to oxygenated bleaches, as used by commercial laundries, and recycled rental textile products.
The TSA is the trade association for the textile care services industry. Visit www.tsa-uk.org for more information.
Cofresco Foodservice – brand owners of Wrapmaster® – has partnered with SUEZ recycling and recovery UK, to launch a new recycling scheme to support sustainability and recyclability – Return to Recycle by Wrapmaster®.
Wrapmaster® is offering you the chance to claim a brand-new Wrapmaster® for free, when you recycle any end-of-life food wrap dispenser, regardless of brand. Return to Recycle by Wrapmaster® provides a solution for responsible and reliable recycling at the end of a dispenser’s life, as it can be returned and reprocessed to create new products – such as white goods.
You will be supplied with a pre-paid return label to send back your dispenser. Once received, you will be emailed a voucher for a free Wrapmaster® dispenser, which can be redeemed with a participating distributor of your choice.
In a UK facility, the returned dispensers themselves will be shredded, washed, and separated into polymers and metals, which are reprocessed and made ready for recycling. Once polymers and metals have been reprocessed, they are sent to UK and EU manufacturers to be used as a substitute to virgin material in the creation of new products.
To participate, visit www.wrapmaster.global/return-to-recycle and fill out the online form.
Care providers across the UK are being encouraged by ReFood, one of the UK’s leading food waste recyclers, to act fast and get prepared before stringent new food waste legislation comes into effect in early 2025.
Applicable to all businesses that generate food waste on site, the new rules state that all commercial food waste (be that preparation waste, offcuts, spoiled produce, or plate scrapings) should be separated at source, stored, and collected for recycling by a reputable service provider. Any business that fails to adhere will be liable to significant penalties.
Non-household municipal premises will be required to make arrangements for separate food waste collections and present the waste in accordance with legislation by 31st March 2025. Micro-firms will have extra time to implement new requirements for dry recyclable waste streams (excluding film) and food waste – they must comply by 31st March 2027.
While you may be concerned about the cost and disruption of the new legislation, ReFood has highlighted that working with a proven supplier can simplify the process. Alongside this, it can significantly improve your sustainability credentials.
For more information, read issue 4 of Savings, Solutions, and Sustainability
A White Paper commissioned by Care England has suggested that an innovative mattress-turning system has the potential to prevent pressure ulcers occurring for people receiving adult social care, improving their comfort and promoting healing – all while delivering significant cost and resource savings to care providers and the NHS.
The paper, called Preventing Pressure Ulcers: The Role of Automatic Lateral Turning Systems for Innovative Approaches to Pressure Ulcer Prevention in Care Homes, examines and summarises a 12-week trial of the Levabo Turn All automatic lateral turning system (ALTS), developed in partnership with Algeos Ltd (UK).
According to the White Paper, pressure ulcers are one of the most painful and preventable conditions faced by some of the most vulnerable individuals in adult social care. The report has stated pressure ulcers affect 700,000 people annually in the UK at a cost to the NHS of £1.4-£2.1bn a year.
The trial focused on residents with dementia with multiple and complex comorbidities, and those receiving palliative end-of-life care who are particularly vulnerable to pressure ulcers due to immobility and frailty. The primary aims were to assess the effectiveness of the system in reducing pressure ulcer incidence, its impact on caregiver workload, resident comfort, and overall cost-effectiveness.
One of the homes taking part in the trial, the Taylor and Taylor Group, said that each caregiver would save two hours a day through not having to manually turn an individual during a 24-hour period. For 11 people needing this facility, this would save 22 hours weekly. Based on an average salary, this equates to approximately £1,600 per week - the approximate cost of one system.
To read the White Paper, visit www.careengland.org.uk (search ‘Preventing pressure ulcers’).
AKW, a leading provider of accessible bathrooms and kitchens for people with reduced mobility, dementia, visual impairments, and other health conditions, has demonstrated a commitment to Environmental, Social, and Governance (ESG) by exceeding its associated targets this year.
AKW ESG milestones include over £32,000 in cash and £400,000 worth of AKW products donated to charities and causes in local communities over the past 18 months; over 135 employee volunteering days undertaken – funded by AKW – in a range of charity initiatives; and 4.76 tonnes of single-use plastic saved, thanks to AKW changing the way its products are packaged. Also, the organisation has reported that its carbon emissions have been reduced by 13.76% through investment in renewable electricity and solar panels over the past three years.
To find out more about AKW’s latest ESG activities, visit www.akw-ltd.co.uk/esg







Care England speaks to Oliver Soriano, Chief Nurse Officer at Lancashire & South Cumbria NHS Foundation Trust, about how the experiences of internationally recruited health and care workers have improved during his career, and what still needs to be done to raise standards.
Care England: What motivated you to seek job opportunities abroad and why did you choose to work in the UK?
Oliver Soriano: Growing up, I did not think that there was an opportunity to work abroad. After passing the nurse licensure exam and receiving my nurse registration, I volunteered at the Philippine Red Cross as an instructor in safety as well as basic life support. It was fulfilling, but equally, I noticed a lot of my nurse colleagues and friends started moving abroad to places like the Middle East or America to work as a nurse and be near to family and relatives. At that period, my sister was already in the UK, but I was not sure if there would be a job for me there.
It was not until a few years later that I received an offer to work in the UK, and I finally moved here in 1998. I was not really thinking about career progression or money when I decided to come to the UK, it was purely to be near to my family.
CE: What types of support did you find most helpful when you arrived in the UK?
OS: I think the NHS and social care sectors were still working out how to best support internationally
educated people at the time. I think the most helpful element was the practical support with settling in, including the offer of accommodation and a workplace training induction, but looking back, it was not enough and what we received was very basic compared to what our internationally educated nurses receive now.
CE: In your view, what works well with current international recruitment pathways?
OS: What works well now is down to a memorandum of understanding between governments to enforce fair and ethical standards on employers recruiting from abroad. That has helped massively because we have heard about disproportionate levels of support being offered and even cases where individuals have paid rogue agencies large sums of money for non-existent roles.
Within these standards, the Government has ensured that organisations have funding to ensure pastoral support is provided to people joining the workforce from abroad. That has helped to create a ‘Gold standard’, whereby for example, people are met and greeted from the moment they touch down in the UK. NHS
and social care agencies should also provide a pre-departure engagement to alleviate any potential anxieties.
International embassies also operate a strict process to ensure high standards of safeguarding and wellbeing are met and will be prepared to withdraw recruitment pathways if these are not being adhered to. I was lucky enough to be part of a steering group in 2020 that reviewed these standards and made improvements for future internationally educated health and care workers.
CE: What tangible actions can employers take to ensure these standards are at the forefront of their international recruitment strategies?
OS: Given all the work that NHS Trusts and social care providers are already delivering according to the International Workforce Recruitment Toolkit, I think it is about employers and the communities they operate in having cultural appreciation, knowing what the culture is like in the countries individuals are coming from. This could be the way they dress, talk, or any religious or spiritual views.
In the UK it can be the case of people being expected to adjust
to a new way of life immediately. We have heard cases of people coming from some South East Asian countries where it is disrespectful to make eye contact with an authority figure, being mistaken for being rude.
But it works both ways. When I came to the UK, I needed to understand more about this country’s love of football and drinking tea. I think shared inquisitiveness is crucial and I believe we are moving towards that point. A great example of this is where a care setting adds food from an individual’s home country to its scheduled menu. If we want to make our internationally recruited global workforce feel like it belongs, employers must embrace cultural appreciation in its totality.
CE: What are some of the key professional challenges you have faced and how have you overcome them?
OS: In the Philippines, I was a registered nurse specialising in mental health, which allowed me to work in any field or specialist area of nursing. This was different when I came to the UK, as I was required to do a conversion course to achieve a registration in mental health nursing. In addition, my qualifications were not sufficient for me to work in a mental health setting in the UK, so I had to do an 18-month programme to become a registered mental health nurse.
I reminded myself that embracing training and development opportunities was one way of ensuring progression in my career. That is the type of person I am, I wanted to learn a lot and be inquisitive. I have also learned from colleagues and supervisors and I was lucky enough to have a mentor who was willing to share their
knowledge about how to develop professionally.
CE: In that sense, do you believe that enough is being done to unlock the potential of the sector’s international workforce?
OS: I think nowadays there are more programmes, mentorship schemes, and resources to support the international workforce, but are employers doing enough to engage people in them? As leaders, we must ask ourselves whether we are doing everything we can to spot talent and motivate our employees to seize development opportunities.
The other side of this is that people coming to work from abroad may be happy to reach a certain level and remain there for the rest of their careers, and in a sense, maintaining their sense of belongingness, happiness, value, and respect, is the greatest way of retaining them. ‘Thriving’ for me now is not necessarily about seeing people progressing up the ranks ‘traditionally’, it is more about people achieving their personal goals.
CE: When it comes to barriers that may be preventing development in the workplace, personal or professional, what advice can you give international recruited workers to overcome these?
OS: I always ask people that I am supporting what their goals are. I did not think about it that way when I came to the UK, I just focused on keeping my head down and doing my job well. I did not think about what I was going to do next. Being in my current professional position, I can see now how useful it would have been to have someone asking me about my future back then.
The second thing I ask is do they have someone in their personal or professional lives
that can help them to set and work towards their goals. This could even be through a diaspora network, of which I am aware of about 30-35 currently operating. Thirdly, it is about identifying the tools to help people to achieve their goals, such as training or resources to develop their desired skillsets, such as more effective communication or negotiating.
CE: Finally, in your role as President of the Philippine Nurses Association, what are you hearing about current experiences of the Philippine workforce?
OS: The main issue is racial discrimination or bullying, or not receiving adequate support to fulfil the duties being placed upon them. We have been hearing about people arriving in the UK and being put in charge of a 20- or 30-bedded ward within two days. Racism has been widely reported as being targeted towards Asian or South Asian nationals, alongside the black community.
I have also heard people’s concerns about their prior professional experience being unrecognised. In my experience, most nurses have between two- and 10-years’ experience before coming to the UK, and yet they are not being paid fairly based on this when they arrive here. This is a form of systemic discrimination, and it must change.
But it is not just about money; some people have wide-ranging research and academic skills too that are not being acknowledged and utilised effectively when they arrive in the UK. It is my commitment within the Association to continue advocating for not just the Filipino health and care workforce but going beyond to support our BAME colleagues to reach their potential and thrive in their fields.
Oliver Soriano is Chief Nurse Officer at Lancashire & South Cumbria NHS Foundation Trust.
Email: oliver.soriano@lscft.nhs.uk : @WeAreLSCFT




Alex Ramamurthy, Head of Health & Social Care at Wagestream, delves into the findings of a recent report examining factors impacting care workers’ finances and provides recommendations for employers grappling with the issue of financial exclusion.
The UK’s social care sector stands on fragile ground. The well-documented workforce shortages, currently numbering 131,000 vacancies according to Skills for Care, are only part of the story. Behind these vacancies is another, more overlooked crisis – the financial exclusion of social care workers.
Financial inclusion is defined as access to useful and affordable products and services. It is an essential part of participating equally in society, enabling people to find ways to better manage their transactions and expenses, and reduce the risk of debt. However, due to various societal, cultural, and economic constructs, lowto moderate-income employees may experience the opposite – financial exclusion.
Certain demographic groups are more vulnerable to financial exclusion, with lower pay and variable incomes being primary factors. Women and people from ethnic minority backgrounds are disproportionately affected, and these are two of the groups powering the social care workforce in the UK.
When workers are financially stressed, it affects their productivity, engagement, and overall wellbeing. Paying attention to financial inclusion is not just a moral obligation – it is a business necessity. You must prioritise financial inclusion as part of your workforce strategy. Doing so will not only benefit your employees but will also yield tangible cost savings, reduce staff turnover, and help you to deliver more consistent, high-quality care.
The recently published report by Care England and Wagestream, Inclusion at the Crossroads, offers a critical look at the financial health of social care workers and presents actionable recommendations for employers. Its findings should serve as a wake-up call for the entire sector.
Inclusion at the Crossroads is based on a survey of 1,718 social care employees, who are representative of the demographic makeup of social care workers in the UK. The majority (80.2%) identified as women, 18.9% as men, and the remaining ~1% either selfidentified in another way or chose not to say. Most come from a white ethnic background (73.1%), over a quarter (25.8%) from an ethnic minority background, and the remainder chose not to say. This is representative of the UK social care sector but is not reflective of the overall UK population1 .
Data from the most recent census (2021) shows that in the UK, 81.7% of individuals identify as white and 18.3% come from an ethnic minority background2. The social care sector has almost 10% fewer workers from a white background and almost 10% more workers from an ethnic minority background than is reflected in the general population.
Through exploring the intersectional experience of gender and ethnicity, Inclusion at the Crossroads reveals five key findings which shed light on the financial struggles that so many workers in the sector face, and the simple, affordable actions you can take to help.
Continued →
“Nourish was a game changer for our company. Nourish has enabled us to really improve our patient care and evidence the great work the team does”
Sarah Beaumont, Associated Wellbeing



Why Choose Nourish?
Nourish is the most trusted digital care planning provider in the UK, used daily to provide outstanding, co-produced care to support 400,000 people across residential and home care settings. Save time, improve outcomes and keep everyone in your circles of care engaged and informed with Nourish.
To book a free personalised demo, please contact us on 023 8000 2288 or email hello@nourishcare.com

One of the report’s most critical findings is that inconsistent working hours are a major driver of financial instability among social care workers. A striking 31.3% of all respondents reported that their working hours ‘change a lot’ from week to week, leaving them unable to predict their income. For workers from ethnic minority backgrounds, this figure rises to 36.9%, compared to 29.2% for their white colleagues. The lack of predictable hours leads directly to erratic pay, making it challenging for employees to manage their budgets or save for unexpected costs.
Poor commissioning practice can have a devastating effect on the ability to create stable and secure work practices.
Research by the Aspen Institute in the US shows that income volatility leads to late bill payments, increased risk of debt, and housing instability3. This is exacerbated by the commissioning practices in home care services, where work is often allocated minute by minute. Such practices create volatile shift patterns, preventing workers from receiving stable, contracted hours.
As Professor Martin Green OBE, Chief Executive at Care England, argues in the report, ‘Poor commissioning practice can have a devastating effect on the ability to create stable and secure work practices.’ This problem requires urgent attention from care providers and commissioning bodies if the sector is to become more stable and sustainable.
The findings also reveal that financial exclusion hits women from ethnic minority backgrounds the hardest. According to the report, fewer than half (49.3%) of ethnic minority women working in social care can regularly pay their household bills. In contrast, 62.1% of white women and 65.6% of white men report being able to meet their financial obligations.
These statistics are more than just numbers – they represent real-world struggles that many social care workers face every day. When employees cannot meet basic needs like food, rent, and utility bills, their stress levels can skyrocket. Financial stress is a key driver of absenteeism, poor mental health, and reduced productivity.
The report includes direct testimonials from workers facing these challenges. One respondent noted, ‘It's very difficult to manage bills when hours are chopped and changed every week.’ Another expressed frustration over not being able to work more hours to meet financial demands due to poor health, ‘I can’t work more hours; otherwise, I’m hospitalised.’ This is not just a problem for employees; it directly affects you. Financially stressed workers are less engaged and more likely to leave their jobs for better opportunities, further exacerbating the staffing crisis in the sector.
One of the report’s most surprising findings is the significant gap in access to state benefits for ethnic minority workers. The data shows that employees from an ethnic minority background working in social care are three times less likely to receive state support compared to their white peers, even when their income levels are similar. Only 6.9% of ethnic minority women reported receiving any form of state benefit, compared to 16.6% of white women. This disparity is often due to a lack of awareness, complex application processes, or barriers such as language and immigration status.
Given that many social care workers are on lower or variable incomes, access to benefits like Universal Credit, Carer’s Allowance, or the Warm Home Discount can significantly improve their financial stability. The fact that so many ethnic minority workers are not receiving these supports represents a missed opportunity to reduce financial stress.
Savings are a crucial buffer against financial shocks, yet the report reveals that nearly 93% of all social care workers surveyed fall short of the UK Government’s recommended savings levels. For women-led and ethnic minority households, the situation is even more dire. Over half (52.6%) of women-led households have less than £50 in savings, including 40% who have no savings at all. Ethnic minority households fare similarly, with 38.5% having less than £50 set aside.
Without savings, even minor financial disruptions –such as an unexpected medical bill, a car repair, or an increase in energy costs – can push workers into crisis. This leaves many reliant on high-cost credit options which only deepen their financial difficulties. Research by StepChange found that households with as little as £1,000 in savings are half as likely to fall into problem debt. Yet only 20.2% of social care workers in the survey had more than £1,000 in savings4
The financial exclusion of ethnic minority workers is compounded by their disproportionate reliance on
subprime financial products. Inclusion at the Crossroads highlights that ethnic minority workers are far more likely to use high-cost credit options, such as payday loans, rent-to-own services, or informal borrowing from family and friends. Nearly 40% of ethnic minority workers reported borrowing from friends or family, compared to 35.6% of white workers.
High-cost credit options can trap workers in cycles of debt, exacerbating their financial instability. Once a worker becomes reliant on payday loans or rent-to-own services, the interest and fees can quickly accumulate, making it even harder to get back on track financially. In contrast, workers with access to more affordable credit options or employer-sponsored savings programmes are better able to manage their expenses without resorting to predatory financial products.
Throughout this research, it is clear that particular groups of workers are experiencing multiple intersecting challenges. It is also clear that you have a role to play, and have the potential to alleviate or even eliminate some of these challenges. Several major employers who contributed case studies to the report, such as Barchester Healthcare, Bupa Care Services, Lifeways Group, HC-One, and Home Instead, demonstrate that employers in social care recognise this role and are investing heavily to make a positive change in the financial lives of their employees.
The commitment shown so far lays a strong foundation for even greater positive change. The report offers four simple recommendations that, if implemented, can significantly improve the financial inclusion of your workforce:
• Aim to meet the standard for living hours, as provided by the Living Wage Foundation. Currently, over 31% of social care workers experience volatile hours, yet providing stable, predictable hours is one of the most powerful ways you can reduce financial instability. By committing to the Living Hours standard, which guarantees a minimum number of contracted hours per week, you can give your workers the financial predictability they need. This will not only improve employees' financial security but also reduce your recruitment and training costs.
References
• Provide support for your workforce to discover and apply for state assistance they are entitled to receive. Many workers in the social care sector are missing out on state benefits that could make a significant difference in their financial wellbeing. You can help by offering workshops or one-on-one support to guide employees through the benefits application process. This relatively simple intervention can significantly improve the financial stability of employees, particularly workers from ethnic minority backgrounds who are currently missing out on this support.
• Implement a payroll savings programme and structure it on an opt-out basis so that employees build up savings by default. Encouraging workers to save through workplace savings schemes can help them build an emergency fund. These schemes are particularly effective when structured on an opt-out basis, ensuring that all employees automatically start building savings, which are a crucial pillar of financial wellbeing.
• Review your workplace policies and benefits through the lens of diversity, equity, and inclusion (DE&I). Inclusion is not just about representation; it is about creating an environment where all employees can thrive. Reviewing DE&I policies through the lens of financial inclusion ensures that financial wellbeing becomes a core part of your company’s strategy. Prioritising fair wages, secure working hours, and access to affordable financial services will help you build a more resilient and engaged workforce.
The evidence is clear
The financial wellbeing of social care workers is an urgent issue that can no longer be ignored. For too long, financial exclusion has been sidelined in discussions about workforce challenges, but the evidence is clear – addressing financial inclusion is essential for the sustainability of the sector. Care providers are at a crossroads. By prioritising financial inclusion, you can ensure your staff are more resilient, engaged, and equipped to provide the highest standard of care. This is not just an ethical imperative, it is a business strategy that will pay dividends in the long run. The time for action is now. You can download a copy of Inclusion at the Crossroads at www.careengland.org.uk/inclusion
1Workforce Intelligence, Skills for Care (2024). The state of the adult social care sector and workforce in England. www.skillsforcare.org.uk/stateof. Accessed 2nd October 2024. 2ONS (2021). Census results. https://census.gov. uk/census-2021-results. Accessed 2nd October 2024. 3Aspen Institute (2017). Income Volatility, Why it Destabilizes Working Families and How Philanthropy Can Make a Difference. www.aspeninstitute.org/publications/incomevolatility-destabilizes-families-philanthropy-can-make-difference. Accessed 2nd October 2024. 4StepChange (2020). Tackling the coronavirus personal debt crisis. www.stepchange.org/policy-and-research/debt-research/ covid-debt-2020. Accessed 2nd October 2024.
Alex Ramamurthy is Head of Health & Social Care at Wagestream. Email: alex.ramamurthy@wagestream.com : Search ‘Wagestream’ and ‘Alex Ramamurthy’









Unleash the power of Swift Management Services Ltdyour go-to Health and Social Care Consultancy! Our expert team of consultants specialises in the Care Home Sector, ready to deliver immediate solutions for short-term challenges or forge lasting partnerships through our retained consultancy service. When it comes to care home excellence, we don't just assist - we elevate. Get ready to experience unmatched support, tailored to your needs, every step of the way!

Assistance with new Registrations Planning and development of new builds/extensions
Strategic Reviews Crisis Management
Assistance with Regulatory issues


Orchard Care Homes operates 23 care homes across the Midlands and North of England. Orchard is driving change in dementia care and aiming to reframe how people living with dementia in care homes are seen and supported.
In each issue, Care England hears from its members about solutions that have worked for them. Whether it is a new technology, a workforce management tool, or partnerships to strengthen operations, this feature showcases solutions and encourages you to think differently and try new practices. In this issue, Hannah Miller, Head of Dementia at Orchard Care Homes, explains the pivotal role she has played in developing and delivering Orchard’s Dementia Promise and Reconnect communities.
Orchard currently has nine Reconnect communities across six homes with plans to create more in the future. Reconnect communities are designed to provide support for people living with dementia whose primary care need relates to distress they experience and behaviours that can result from this.
Many of these people have spent time in hospital, sectioned under the Mental Health Act or have been rejected from previous care homes due to what is commonly labelled as ‘challenging behaviour’. As such, they can very easily be seen as too much of a risk to care providers, becoming caught in a revolving door situation being repeatedly rejected by care homes or returning to hospital.
Additionally, these people are frequently subjected to one-to-one care, the highly restrictive process of having a care worker constantly at their side. Not only is this questionable in terms of how it is facilitated, impacting on people’s human right to liberty and free movement, it is also an extremely expensive practice, does not address the causes of the person’s distress, and arguably adds to their frustration.
Reconnect and Orchard’s Dementia Promise aim to enable people living with dementia to live their lives to the full, ending traditional, formulaic, and task-driven care home experiences. There are many elements needed to achieve these changes in longstanding culture and practices. Orchard has invested in its colleagues and estate to ensure this aim becomes reality.
There are three significant components underpinning successful Reconnect communities –selecting the right team, providing that team with the knowledge and skills to effectively support people, and creating environments which enable and promote truly positive outcomes for people.
Building the right team is vital in ensuring people achieve the best outcomes possible. The most important attributes of team members are their attitude and ability to connect with people. Whilst experience and qualifications are important, they alone do not ensure a genuine passion for the role.
Orchard selects people who have a genuine drive for change in dementia care, who do not focus solely on a diagnosis of dementia and define people through that diagnosis, and who are enthusiastic about finding ways for people to get the most out of life.
As Head of Dementia, I have developed Orchard’s Dementia Promise training which equips colleagues with the right skills and knowledge, removes stigma surrounding dementia, and encourages positive care approaches, with the overarching goal of achieving true equity for people living with dementia.
The bespoke, detailed, evidence-based training lasts five days and covers the following modules:
• Dementia awareness and sensory changes.
• Communication.
• Law, guidance, and regulation.
• Engagement and meaningful occupation.
• Distress and de-escalation.
• Home environment.
• Physical health.
• Family support.
Reconnect and the Dementia Promise training focus on people, not dementia. It is vital we begin our understanding by recognising that we are supporting people, first and foremost. The training is backed by in-home coaching and mentoring from our dementia team. We are challenging and changing decades of negative ‘care home’ language, which drives thinking and therefore behaviour towards people.
For example, the terms ‘challenging behaviour’, ‘aggressive’, and ‘non-compliant’ immediately label people in ways that create dehumanising, problematic perceptions and do not encourage viewing them as valued members of society, nor do they support understanding the reasons for people’s behaviour or what we can do to help them feel more at ease.
Colleagues are trained to understand causes of distress using the PINCH ME tool and Newcastle Model. Causes can be broad ranging and are unique to each individual. The use of anticholinergic medications, a range of medicines which can have an additional negative cognitive impact, is explored.
We are determined to reduce the use of antipsychotics and benzodiazepines, medication used frequently when someone is distressed. While there is a place for these at times, they mask people’s ability to express themselves and can be extremely harmful over time.
Pain management is a key focus, with studies suggesting over 50% of people living with dementia are living with undiagnosed and therefore untreated pain. This is an area the sector must attend to, not only from a clinical perspective, but from an equality perspective too.
We incorporate short videos of best practice from renowned dementia specialists and people living with dementia – bringing to life the challenges they face and showing how people can live a meaningful, enjoyable life with dementia. These firsthand accounts bring true meaning to the training.
Engagement and meaningful occupation are fundamental cornerstones of Reconnect and the Dementia Promise training covers this extensively. It begins by considering ourselves, how we spend our time, and what we do in everyday life to Continued →
feel purposeful and bring meaning to our lives. The traditional care home approach of timetables and often generic activities has been replaced. People are encouraged to occupy themselves as they would have done throughout their lives in ways that are relatable to them.
The training delivery is far from formulaic. Every session is different, with colleagues encouraged to share their experiences as part of the discussion. This results in rich experiential sessions, drawing on human emotion, empathy, and bringing teams together as true partners.
Reconnect environments have numerous features aimed at supporting people to maintain life skills, have purpose, and reduce difficulties people living with dementia can have with orientation particularly in unfamiliar environments.
The biggest change Orchard has made is to push the boundaries of possible and embrace a positive risk approach. Reconnect communities have several functional spaces such as laundries, craft and creative rooms, garden rooms leading to outside spaces, gaming rooms with pool tables, and functioning DIY workshops.
This all encourages people to maintain life skills and have a sense of achievement and ownership of their lives. Each community has a series of small lounge diners with kitchenettes equipped with facilities you would expect to find in a functioning kitchen. These are for people living in the community to use when they wish, with any support needed.
The Reconnect model of care has resulted in life-changing outcomes for people living there.
People are no longer subjected to one-to-one care, they are engaging in life, and we have seen significant reductions in the use of psychotropic medication.
From being either under Section or served notice from previous care homes, life has changed for
people. People are supported to get out into the local community, wash cars, go shopping and to the pub, travel on buses, visit the coast, exercise, do DIY projects, household tasks, and much more.
1. M’s previous care home served notice as they were unable to accommodate his needs. During his Reconnect assessment, M chatted about his days living in the local area and how he was a domino champion for a local pub. Since living in Reconnect, M has not required one-to-one care and explores the community, engages with staff, and enjoys talking to his peers who grew up in the same area. His community psychiatric nurse could not believe how quickly he settled in, none of his previous behaviours have occurred and he engages in various activities.
2. R was in hospital under Section; he had multiple admissions over the past few years. R was known for having paranoid thoughts in previous placements due to low stimulation, which caused him to disengage. The hospital found Reconnect to be a great environment for R as it offered lots of stimulation which reduced his paranoid thoughts. Once at Reconnect, he became engaged with life and those around him. He loves cleaning and going around with the housekeepers helping to mop, sweep, and clean the windows within the home. He also enjoys going into the workshop completing DIY and painting. The hospital is happy with how well R has settled as he had so many failed placements in the past.
Orchard is continuing to evolve the Reconnect model in line with emerging best practice and learnings from the experiences of people in our homes. We believe our approach is truly changing dementia care for the lives of people delivering and receiving support.
‘This is how all dementia care should be. Grandma moved from another home, the difference in her is remarkable, she is so happy. I love that people are encouraged to do things themselves, their own laundry room and woodwork room, a world away from other care homes.’
‘My client needed one-to-one support in hospital due to her cognition and behaviours. She was declined placements at other homes. Speaking to family, they are delighted. She is engaging in meaningful activity and enjoying her life again.’
‘I'm here to support and advocate for people living here. The best part of my role? The time I spend with people. We have a blast together! Creating special moments reminds you why you love your job.’
Hannah Miller is Head of Dementia at Orchard Care Homes. Email: info@orchardcarehomes.com : Search ‘Orchard Care Homes’


A winning combination of high-performance hygiene, reduced carbon footprint, and cost savings.
Use less and achieve more with typical operational cost savings of 20%.
We help care homes to realise significant savings by making strategic swaps to products and systems that will simply do the job better; saving them time, effort, energy consumption and waste.
Our offering goes a lot further than just supplying products and services. Focused on value, we make it possible for care homes to
✓ Use fewer, but more effective consumable products
✓ Get better cleaning results – first time
✓ Improve performance
✓ Maximise infection control
✓ Create less waste
✓ Save valuable time
✓ Reduce environmental impact
✓ Cut operating spend
✓ Focus on providing excellent levels of care.
We’re here to make a difference to lives, making work-life easier and more rewarding for people working in a care home, to make care home life better for those who live there.
Contact us to request a complimentary audit of your consumables.


Our optimised laundry system, in partnership with P&G Professional, drives cost savings, delivering up to 20% reduction of your laundry operational costs.
in partnership with

Prepare for challenging talks about fee uplifts

It is never easy to negotiate an uplift in fees, and at a time of funding constraints, care home managers and other providers of adult care services could be forgiven for putting off the inevitable. However, being prepared to discuss fees proactively with the relevant contracting authority in a professional manner could improve your chances of securing a ‘fair, reasonable, and sustainable’ outcome.
Looking ahead to next April, when most contracting authorities start a new funding cycle, you need to start preparing for fee negotiations with your local authority or the Integrated Care Board (ICB) as early as possible. Local authority budgets are facing severe pressure due to rising costs and a systemic lack of funding over many years, with more local authorities on the brink of being forced to serve Section 114 notices due to financial difficulties.
With local government facing so many challenges, you may be reluctant to rock the boat by demanding an uplift in fees
to cover the increased costs associated with meeting the needs of individuals in receipt of your services. You may be worried that demanding more fees from the contracting authority could cause them to move placements elsewhere. However, you should be honest with yourself and ask whether continuing to deliver services without a necessary fee uplift is sustainable. You should also bear in mind the adage that ‘if you do not ask, you will not get’.
In his review of spending on NHS services1 published in September, Lord Darzi said it is impossible to decide whether society’s healthcare needs are being met, without also considering social care services. His report concluded that NHS finances are ‘not being spent where they should be’, with most funding targeted at hospitals, and too little ending up in the community.
Recognising the role that social care services can play in alleviating pressure on hospitals
Continued →

Together, we will design a vision of care and inspire change in the sector.
Guiding you on a journey of digital transformation
Giving you more time to deliver outstanding care and drive your success

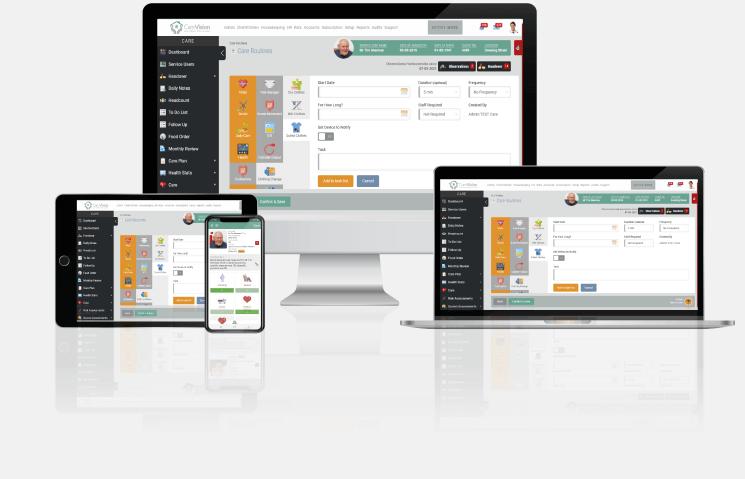
CareVision was the guide that helped me through the challenges I faced. Their responsive way of working and understanding of the care sector enabled us to get real, positive support from people that had a plan to get us where we needed to get to. Since making the decision to go with CareVision, we are working as a real team across departments. We are now rated outstanding and are ready for anything that comes our way.
and the healthcare system in general, Lord Darzi described them as ‘vital in their own right, helping people with disabilities, and all of us as we age, to lead full and independent lives for as long as possible’.
Whilst Lord Darzi’s findings underline the importance of social care, the £22bn ‘black hole’ in the country’s public finances means that further funding for local government is unlikely. For care homes and other care providers, this means that more below inflation or even 0% fee uplifts are to be expected.
On a positive note, the Government has scrapped the planned cap on care costs in England, which was due to be introduced in October 2025, so there may be some scope for you to increase charges where necessary to offset your underfunding. However, the reality is that many care providers have been underfunded for many years, and as such, you have likely come to rely on regular top-up fees from the families of those receiving care. Where this is the case, you may be reluctant or unable to ask for more.
With costs rising and an ageing population, which means more people living longer with chronic health conditions, meeting the cost of social care services is a major social problem. However, Lord Darzi’s review does at least point to a time when things might improve for health and social care services and the Government’s proposed 10-year plan is eagerly awaited.
With the common occurrence of providers not receiving an uplift which is ‘fair, reasonable, and sustainable’ for 2024/25, and the expectation that this will not improve for 2025/26, many care providers will feel compelled to challenge it, and there are steps you can take to optimise your chances of achieving a favourable outcome.
Being prepared to open negotiations early with the relevant contracting authority is important and you may feel that the time has come to take a front-footed approach. For those taking this approach for the first time, it may be reassuring to know that local authorities are usually willing to discuss a potential uplift in fees if there is a well-evidenced business case to support your demands.
The reticence of some care providers to ask for more funding in the past has in some ways played into the hands of the contracting authorities, which have become accustomed to setting fees without any fear of being challenged. This cycle should be broken to make way for open and honest negotiations.
Most local authorities will confirm fee uplifts with effect from 1st April, but decision-making processes typically start several months earlier. You should aim to prepare a well-considered business case well ahead of time. The starting point should of course be a consideration of how much funding is needed to deliver services for everyone in your care.
To do this, you will need to analyse your own costs, including for example, your total property, energy, food, utilities, and labour costs, taking into account how much they have increased in the past, and forecasting how much they might increase in the year ahead. Gathering accurate cost data and using this to model how costs could change in future, will help to reinforce your business case for a fee uplift.
When negotiations get underway, it may help for you to know what to expect and to be prepared for all outcomes. Despite the huge budgetary constraints that local authorities are facing, it is always hoped that they will recognise the importance of working with care providers, viewing you as a partner to support them in meeting their
statutory obligations. If a local authority receives a letter challenging the uplift offered it may write back to you explaining that it wants to work with you to find a satisfactory resolution. Whilst these letters are helpful and demonstrate the contracting authority’s willingness to talk about the matter, they should not be taken as indication that more funding is available.
Being prepared to meet face to face is another positive sign of a willingness to negotiate, and such opportunities should be welcomed by both parties. For care providers, in-person meetings are an opportunity to assert your business case for a ‘fair, reasonable, and sustainable’ fee uplift based on clear cost data and other evidence. When setting up these meetings, it is important to ensure the right people are in the room – this is usually done by establishing a clear line of communication with the key decision makers at the outset.
When preparing your business case for a fee uplift, you should start by asking the question: ‘What do we need to maintain a sustainable placement?’ This approach will ensure that the individuals who receive care, and their families, are at the centre of your thinking throughout the negotiations. It may also help to carry out a benchmarking exercise to establish what care providers in the area are charging for comparable services, and what fees they receive from the relevant contracting authority. Reaching out to sector bodies and support organisations, such as Care England, could be helpful in providing access to third-party sector data. Another factor when gathering evidence and building a compelling case for a fee uplift is to adhere to the contracting authority’s specified timelines and procedures. These can differ from one local authority to the next, so it is important to find out what they are in each case.
With the best will in the world, you know that fee negotiations do not always go according to plan. In these situations, you will need to decide whether to challenge the fee uplift being offered or not. Being prepared for this outcome is important as there can be a lack of transparency around decisionmaking processes and there could be a tendency for things to take longer than necessary.
Some contracting authorities may be tempted to put off delivering ‘bad news’ about fee uplifts until the last minute to mitigate the risk of a challenge being mounted. If you feel that information about decision-making processes is being withheld, you could consider making a Freedom of Information (FoI) request for copies of minutes where fee uplifts have been discussed. Being ready to react to the official fee uplift letter when it eventually lands also makes sense.
Whilst being prepared for all eventualities is important, the best, and most amicable, way to resolve any dispute over funding will always be to sit down and talk about it. In the current climate, however, expectations on both sides may be miles apart. For example, a care provider which has been historically underfunded for years may be seeking an uplift of 25% or more, whereas the contracting authority may only be offering 2% or less. In this scenario, if both parties are prepared to negotiate and make concessions, even slightly, this could help the parties to bring about a mutually agreeable resolution.
References
If there is a lack of any willingness to negotiate however, you may feel that the time has come to escalate matters. It may be appropriate to remind the relevant contracting authority of its statutory obligations, such as the Care Act 2014. Whilst it is not a decision to be taken lightly, it could become necessary to terminate placements if a ‘fair, reasonable, and sustainable’ fee uplift cannot be reached. If you have a good track record and consistently deliver services of a high standard, then the contracting authority is unlikely to want that relationship to end, which could encourage it to reconsider the fee uplift offered.
Using legal specialists to support you by providing bespoke advice and preparing appropriate letters and other communications can help to demonstrate that you are serious about challenging the fee uplift offered and are prepared to take further action if necessary. Whilst every situation is different, these letters could explain that you are prepared to take the matter to the Local Government and Social Care Ombudsman if a sustainable resolution cannot be found. They could also explain that a judicial review is another option receiving consideration. Guidance from support bodies, such as Care England, can be helpful here too.
As a care provider, it might seem unacceptable to talk about ‘terminating placements’, but this could be the only option left if you are struggling to remain viable or already operating at a loss.
If it becomes necessary to take this action, you should explain to the contracting authority that it needs to inform families as soon as possible to ensure they are aware of the situation and allow them to be involved. Throughout your negotiations and in all communications with the contracting authority, you should make it clear that each care package you are responsible for is a person with needs that must be met.
When challenging a fee uplift offered, you should look for any evidence that might support your case. This should include a careful examination of any contracts, even if they have expired. Some contracts could provide a ‘formula’ for calculating fee uplifts in response to inflationary cost increases, which must be adhered to. In other cases, the contract might state that uplifts are at the council’s discretion. In either scenario, the council is required to comply with its obligations under the Care Act 2014, which requires fees to be fair, reasonable, and sustainable. When seeking a fee uplift, you must be thorough in your approach. Being clear about how much funding is required to meet the needs of people in your care is essential, as is meeting deadlines and procedural requirements set out by the contracting authority. With the right approach and support, you can achieve the fee uplifts needed to continue to deliver much-valued services to the communities you serve.
1Department of Health and Social Care (2024). Independent investigation of the NHS in England. www.gov.uk/ government/publications/independent-investigation-of-the-nhs-in-england. Accessed 7th October 2024.
Liam Fitzgerald is a Senior Associate at Anthony Collins Solicitors. Email: liam.fitzgerald@anthonycollins.com : Search ‘Liam Fitzgerald, Anthony Collins’
Sarah transformed her care home with QCSempowering her team, staying compliant, and driving success. Now she focuses on what truly matters... exceptional care.
FIND OUT HOW QCS CAN HELP YOUR CARE HOME THRIVE



Graham Mann, Director and Co-Founder of
SwitchWaterSupplier.com, explains how you can become water wise and save money on your care setting's water bills.
Never a week goes by without energy prices making media headlines. There are many businesses in the care sector grappling with the ever-increasing but seldom decreasing energy prices; however, water is the forgotten utility. Why? It all comes down to cost and price volatility.
I talk to many businesses inside and outside of the care sector that have never reviewed their water and wastewater bills. It is strange, but often true. In the general order of things, water is rarely discussed until there are pressure problems, or the taps run dry due to water leaks and leak repairs, or water pipe renewals take place in the road and cause the usual interruptions to supply. In short, we take water for granted and we do not see the value of it – that is, until the taps run dry. Water is life; try running a care facility without water for longer than an hour.
Water and wastewater services are cheap,
right? Yes, in years gone by, pre-water market deregulation water was cheap. Then along came water market deregulation on 1st April 2017 in the English water market; in Scotland, deregulation occurred in April 2008, serving 1.3 million businesses, charities, and public sector organisations. This was followed by above-inflation water and wastewater price rises. In 2024, for instance, we had significant increases in water charges.
For example, Southern Water made an 18% increase in water charges and a 13% increase in wastewater charges, not to mention a 13% increase in fixed charges for drainage. The north east also took a hit, with Northumbrian Water increasing water charges by 12.7% and wastewater charges by 11.3%. When you factor in the usual water retail fees of around 10% on top, these are significant increases. In fact, I am predicting that, due to increases including those in 2023, 2024, and those predicted to come in three years’ time, charges will have increased on average by 75%.
Why such significant year-on-year increases?
Increases in all regional water and wastewater supplies are being driven by the usual suspects: energy costs, wages, tax increases, and the desperate need to repair and renew water and wastewater infrastructure, such as water pipes, sewer pipes, drains, and sewage treatment works. All of this is in need of huge investment.
So, who pays? As you will be all too aware, it is customers like you. So, how can you reduce your water and wastewater costs and mitigate those annual increases in charges? Now that the water market has deregulated, you can switch water supplier and get a better deal.
I know from previous experience of talking to care home providers that many have now switched water supplier and are paying default charges, which are higher than if the business contracted with a new supplier. Some switched a few years ago and a lot has changed since then – there are great deals available in the water retail market, if only you know where to look.
Switching water supplier is a gateway to future savings, as well as refunds due to historical billing errors. For example, Harbour Healthcare switched water supplier and commissioned a water audit across its estate, resulting in six-figure savings. Another care provider went out to market, resulting in savings of £120,000 by switching alone. In my experience, without exception, by switching water supplier and commissioning water bill validation and water audits, significant savings and refunds can be achieved by most, if not all, care home providers.
So how do you find the best possible deal by switching water supplier? The good news for care providers is that Care England has recently signed a landmark partnership deal with SwitchWaterSupplier.com, the UK’s only business water comparison site, which tenders water supply contracts on a live tender platform to all the water retail companies in the water market. This is to ensure you get the very best-value deal and service from the
leading water industry experts.
With this service, your water billing data is uploaded to the platform, and the suppliers bid for your contract over a 60-minute duration. The best offers appear at the top of the list in descending order. At the end of the 60-minute process, the tender results are sent to you, and you select the best-value deal.
When your new supplier has been selected, a Customer Service Director at SwitchwaterSupplier.com manages the switch from your existing water supplier to your new supplier. Readings are taken from the water meters at your sites to enable the account to be closed and then re-opened with your new supplier using actual readings. This ensures you have accurate continuity of billing going forwards.
I am often asked how it is possible to make any other savings if you have switched water supplier already. If you have already switched water supplier, then it is best to commission a water audit of your water and wastewater bills. Water audits are the best way to identify savings and refunds due to historical overcharges. Many care home businesses have successfully claimed thousands of pounds in rebates due to incorrectly levied charges. Adding to this, the charges going forwards would also be reduced.
Historical overcharging is rife within the water market and there are many different areas of overcharging. For example, in the Midlands Severn Trent area, hundreds of care home providers are being overcharged due to the incorrect tariff applied, particularly care homes supporting people living with dementia. Other areas of savings and refunds are due to historically incorrect meter readings and surface water charges for the treatment and disposal of rainwater based on site area charges. Many sites within this sector will be overcharged and water audits will uncover incorrect charges.
So, how will you know your water bills are correct going forward in the future? Most
water suppliers will, at some point in time, send out incorrect bills due to glitches in their billing systems and incorrect wholesale water market data. The water market is not that different to the energy market where, from time to time, gas and electric bills are incorrect. The same happens in the water market. The trick is knowing how to spot the errors, which can be costly if not spotted and rectified.
If your business has multiple sites, we recommend that a water bill validation project is undertaken to ensure bills are checked and validated prior to payment by water industry experts. Water bill validation is a cost-effective way of ensuring bills are correct. This is your insurance against incorrect charging and overpayment. Future bills are diverted to the appointed water consultants and the bills are checked and validated. The data from the bills – for example, meter readings, water consumption, and standing charges – is all recorded in a water database. In fact, all elements of the bills are recorded and there are many.
Only when the bills are deemed correct
will they be sent to your accounts payable for settlement, so you can be secure in the knowledge that the bills are accurate, improving benchmarking and water efficiency. The water database created and updated through the water bill validation process is of utmost importance to drive down water consumption and costs. Recording the water consumption per site is vital to determine whether the site is an efficient water user or poor water user. Sites will be benchmarked in accordance with how many beds are operating within the care environment.
The water consultants at SwitchWaterSupplier.com have consumption and water-billing data for thousands of sites within the care sector and will set the water consumption per bed at a realistic target that your care business is able to achieve, working in partnership with water industry experts. Driving down your water consumption through a focused and proven water management strategy will not only control and maintain savings, but it will also ensure your business will hit sustainability and environmental targets.
All businesses, charities, and public sector organisations in England and Scotland that are eligible are now able to choose who provides their water and wastewater retail services. There has been much said about the benefit to businesses in switching water suppliers, but what are they? Depending on the size of your organisation, the benefits vary and are not always limited to the outcome of a switch between water retailers and the potential savings it might bring about.
For the first time, deregulation in England brought about UK-wide opportunities, including:
• Lower bills and charges as a result of competition between water retailers and the opportunity to switch between suppliers.
• Improved value for money as water retailers look to provide unique selling points that include water efficiency services.
• Improved standards of customer service based on the more competitive market in which retailers must operate.
• Services to improve your own operational efficiencies, such as consolidated billing for multiple sites.
• More access to help to become a more water-efficient business, further reducing costs.
Whilst the markets in England and Scotland are broadly similar, offering many of the same benefits, they are independently run and operated.
Graham Mann is the Director and Co-Founder of SwitchWaterSupplier.com Email: graham.mann@switchwatersupplier.com : Search ‘Graham Mann, H2O Building Services’












Chris Martin, Managing Director at Tenders-UK, explains what you need to know about recent changes to procurement rules, and how you should get ready to make the most of new opportunities in 2025.

2024 has been a time of change. The new Government's commitment to revitalising the health and social care sector has presented a unique opportunity for you to work with the public sector and make a real difference to lives across the country. However, the landscape is becoming increasingly competitive, with budgets tightening alongside the rule changes. Your existing contracts could well be at risk, but there is also considerable growth out there for those companies willing to pursue it.
The UK care sector is undergoing significant changes, and tendering is at the heart of this transformation. With billions of pounds being procured annually by local authorities, NHS bodies, and central Government, the care space is ripe with opportunities for organisations looking to maintain and grow their business sustainably. Transparent buying processes, long-term contracts, and stable demand all make the public sector an excellent market for any care company.
The tendering process aims to provide fairness and a level playing field for bidders. This means that all care providers, regardless of size or history, have an equal opportunity to bid for contracts based on the quality of their services and their ability to meet the needs of the public sector. Bidding is not enough though – to win you will need to meet requirements on things like Care Quality Commission (CQC) scores and previous experience, as well as having a clear vision for the future of the contract.
Most public sector contracts run from three to five years. While it is true that public sector pay rates can be lower than private sector rates, the ability to guarantee volumes of hours over the long term can provide a solid foundation for business growth. With that certainty, you can invest in your people and infrastructure knowing they will be busy for years to come.
Continued →














Regardless of what happens with social care funding reforms under this new administration, this public sector demand will remain consistent if not increase with an ageing UK population. This means a diverse range of opportunities to provide different complementary services.
By partnering with the public sector, you can deliver truly impactful services which benefit communities. For example, one client combined an Extra Care facility contract with contracts for community-led groups' activities, such as dementia cafés and befriending groups. The client operated those services from the communal spaces in the facility which helped connect residents with the wider area.
The UK has a long history of comprehensive procurement rules focused on fairness. Over the past decade, several key regulations have shaped the procurement landscape. Since 2015, the Public Contracts Regulations have governed how the UK public sector buys goods and services. But this year has seen two major rules changes which will impact any future public contracts you bid for.
In January 2024, the NHS and health buyers changed how they purchase services and started applying the Provider Selection Regime. This is a new system for arranging healthcare services in England, introduced in the Health and Care Act 2022. It replaces the competitive tendering process with a more flexible arrangement.
Under this regime, NHS bodies and local authorities can determine the most suitable provider for a service, sometimes without necessarily conducting a competitive procurement. They can consider factors such as quality, integration, and social value, not just price. They must still adhere to principles of transparency, proportionality, and non-discrimination but this does increase the risk that contracts could be lost behind closed doors.
Secondly, although passed in 2023, the implementation of the UK Procurement Act has been pushed back to February 2025 to give the new Government time to produce a policy statement. The Act is a new law that aims to simplify and streamline the process of awarding public contracts.
It introduces new principles emphasising value for money, public benefit, transparency, and integrity. It also provides streamlined procedures for lowervalue contracts and more flexibility for authorities to consider social, environmental, and economic factors. In addition, the Act places an increased emphasis on supporting small businesses and local economies and introduces a new digital platform for supplier
registration and bidding.
These changes present opportunities and risks for organisations working with the UK public sector. By staying informed and adapting to the new rules, you can position yourself for success in this evolving market.
The amount of time it can take to produce a winning tender can vary wildly, with submission ranging from a few pages of text to hundreds of pages of complex responses and calculations. All that time and effort should only be spent on bids which you can credibly win, and which can deliver lasting benefits to your organisation.
To be successful, you need to understand your local care commissioners and what they need so you can be ready to help them buy in the right way. Established local providers can shape best practice and specifications based on their knowledge. For example, helping buyers consider local community needs or recruitment challenges in the area.
Under the new rules, commissioners are required to publish pipelines of upcoming tenders. By targeting specific counties or regions, you can plan for the next few years and start proactively preparing to bid successfully in those areas. We know that most tenders (more than 80%) are published late but having a plan of what you intend to bid for can help you invest your time and energy in the contracts which matter most.
Reaching out to commissioners to understand timelines, requirements, and provide market insights is crucial. With NHS staff rotating more rapidly than council staff, keeping track of the people who are responsible for your contracts is often the first step to preparing to keep those contracts. Do not just focus on the people running the service day to day, build relationships with the people sponsoring those contracts as they will be setting the strategic direction for any future tenders.
The new rules also enable innovation partnerships and negotiated settlements. Those working at the leading edge (for example working with Virtual NHS wards) should be talking to buyers about trials you can run ahead of a procurement to test out new ideas.
If you are an incumbent provider, also make sure you are totally clear on any contract extensions available and what they could mean for the contract reset. For example, understanding what Transfer of Undertakings (Protection of Employment) or TUPE means for your existing staff, or thinking about how contract change could affect capital investment.
Tendering may seem like a task reserved for head office or senior management, but that is a common misconception. Alongside the other changes I have described, commissioners are increasingly changing the way they score tenders by adopting ‘confidence-based’ scoring systems. This is a catch-all term for any way of scoring bids which relies on a reviewer’s subjective opinions on things like ‘concerns’ or ‘strengths’.
That means that your score is driven by how the reader feels reading your written responses. Essentially, if the bid makes them feel confident in you, you get a high score. If something about your bid worries them, your score drops and can drop far. Without delving into the psychology, it is clear that real-world evidence and human stories are critical in building confidence. A detailed, vivid response is far more convincing and trustworthy, making it more likely to score highly. This means that tenders cannot just be the responsibility of commercial staff in a central office. They need to be driven by the connection and insight of frontline staff to ensure bids are relevant, credible, and impactful. If you find yourself asked to contribute these ideas and stories to a tender, here are three tips from one of our social care experts who interviews registered managers and care staff every week:
1. Take nothing for granted: Though buyers have a responsibility to have a 'technically competent evaluator', that does not mean they know the sector like you do. Be explicit about what you did, why you did it, and the choices you made to get there.
2. Acknowledge the real impact of your work: We spend our days talking to people who change lives for the better every day, and one of the things they have in common is that they take excellence for granted because ‘it is the day job’. Do not do that. See the value in what you do from the perspective of an outsider, maybe a loved one of the person you are supporting.
3. Be specific: Detail matters. The more specific you can be, the more likely it is that the reader will know that what you are saying is true. Obviously protect the names and details of your staff and residents/service users, but when it comes to dates, hours, and systems make sure you are being as detailed as possible.
All that helps whoever is writing the bid to demonstrate the impact you can have on the lives and wellbeing of the people you support.
The deadline is closer than you think
If you need to write a bid, the first step is being ready for it. You will typically only have four to eight weeks from when the tender is first published until the deadline for submission. That needs to be enough time for you to work out what the buyer needs, whether you can meet that need, and then write and price a response which shows them exactly why you are the best people for the job.
Every bid you submit will feel like an unfinished masterpiece, because there is always more you can do to make it stronger. How you use the time you are given can have a huge impact on the outcome of the tender. Make the most of the time by making informed decisions early, drafting and sharing content, and creating time for critical reviews.
Some smaller framework call-off contracts can give you much less time (typically one or two weeks), but they will also be asking you to submit less information as they will be asking you to bid for specific packages or sites. For these contracts, it is incredibly important that you spend time understanding exactly what each package requires, and that you offer a plan which shows you can meet the needs of those individuals.
The last thing to remember about a tender is that it is an ongoing conversation that does not finish until you reach that deadline. ‘Clarifications’ are how bidders communicate with the buyer – asking questions about the tender documents or the service being procured. Great buyers see clarifications as an opportunity to close out any ambiguities or issues with their tender, and so can often publish detailed replies or updated documents. Keeping track of those clarifications can sometimes be neglected – which can lead to unfortunate surprises later in the process.
The evolving procurement landscape in the UK care sector offers significant opportunities for care providers willing to adapt and engage proactively with public sector buyers. By understanding the tendering process, staying informed about evolving regulations, and leveraging local expertise and knowledge, you can position yourself for growth and success in 2025. To learn more about tender opportunities in your area and the help available to prepare for them, visit www.careengland.org.uk/tender-opportunities
Chris Martin is Managing Director at Tenders-UK. Email: chris.martin@tenders-uk.com : Search ‘Tenders UK'

The sector faces three core challenges: workforce shortages, inadequate funding, and regulatory pressures. Vivup, MINT, and SMART are three innovative tools to help you overcome them.
Recruitment and retention challenges remain a critical concern in the care sector, driven by high stress, low wages, and limited support for care workers. This impacts both providers and the people relying on high-quality care. Vivup offers a comprehensive wellbeing package tailored to address these challenges:
• Easing financial strain: Discounts on everyday expenses worth up to £1,500 annually per employee.
• Providing mental health support: Access to 24/7 counselling, online cognitive behavioural therapy (CBT), and self-help tools to reduce stress and burnout.
• Enhancing physical health: Online GP consultations and menopause support to address health concerns promptly.
• Delivering specialist assistance: Resources for managing debt, domestic abuse, and family issues.
At a cost of £5 per employee annually, Vivup allows you to holistically support your staff, improving job satisfaction, boosting morale, and reducing turnover. Essex County Council’s adoption of Vivup has already demonstrated its potential, aiding recruitment efforts and setting an
example for other local authorities (visit www.careengland.org.uk, search ‘Essex County Council’).
Underfunding is another significant challenge, with providers often struggling to cover the true costs of delivering services. Care England’s Market Intelligence Tool (MINT) equips you with the insights needed to secure fair funding and strengthen financial sustainability. Key features of MINT include:
• Transparency: Benchmark local authority fee rates against actual care costs, building a strong case for fair funding.
• Informed advocacy: Evidence-based data supports you to engage effectively with commissioners.
• Strategic planning: Navigate financial pressures confidently and plan for the long term.
By leveraging MINT, you can address funding gaps and advocate for fee rates that truly reflect the cost of care, creating a more stable and sustainable future for your service.
Regulatory compliance is one of


the most demanding aspects of operating in social care. The Care Quality Commission’s (CQC's) shift to its single assessment framework in 2023 has made streamlined processes even more essential. SMART Quality, developed by Care England, simplifies compliance while ensuring you are always prepared for inspections. Key benefits of SMART Quality include:
• Centralised evidence management: SMART Quality aligns with the CQC’s framework, enabling providers to store, report, and record evidence against quality statements in one place.
• Built-in CQC standards: Each quality statement and key question from the CQC’s framework is embedded within SMART Quality, with links to relevant regulations.
• Customisation and alerts: Customise review elements, flag areas needing further action, and set notifications to ensure nothing is missed.
• Historic reports: Access CQC reports that display ratings under each quality statement since 2016.
As the CQC adopts continual assessment, SMART Quality ensures you are always inspection-ready, reducing administrative burdens and allowing you to focus on delivering exceptional care. For more information, visit www.careengland.org.uk (search ‘Vivup’, ‘MINT’, and ‘SMART’).

Philippa Doyle, Head of Social Care at Hempsons, highlights updates from the regulator issued in response to recommendations from Dr Penny Dash’s final report.
for removal. QSs may also move domains, but until we are told otherwise, the current QSs are the ones you will be judged against.
It is important to present the right information in response to specific questions. To do so, you need to work through each QS. Understand what the CQC is looking for, reflect on your own compliance with the regulations, and consider what evidence you have or need to secure a score that truly represents what you deliver.
Hempsons welcomes the CQC’s recognition that it must work on regulatory effectiveness and SAF implementation. Taking scoring from evidence category level to quality statement (QS) level will allow you to concentrate on demonstrating how well your service operates in response to a particular question, rather than being judged on individual evidence.
Having a CQC handbook that describes what ‘Good’ looks like will always be beneficial, but a good service is one that is regulatory compliant, so working through the regulations and the QSs side by side ought to earn you at least a ‘Good’ rating. The 303 key lines of enquiry (KLOE) have been replaced with 34 QSs, but the regulations underpinning them and the care you are required to deliver have not changed. The CQC tells us the 34 QSs may change, and it is investigating any duplication
Points mean prizes with the SAF. Securing the best possible score in response to each QS will inform the rating of your service. Think carefully about what information and evidence you have within your service and tailor what you share so that it truly fulfils the QS’s requirements. Responding to a QS is like answering an exam question at school – do not just write everything you know about a subject – or give the CQC every piece of information you have – make sure you are answering the question, with the best-quality evidence.
You are delivering high-quality care in often pressurised circumstances and the strength in your service is often your staff’s caring nature. Evidencing the excellent work being delivered is often not captured as comprehensively as it could be. Therefore, it is important to identify where some enhanced record keeping could turn a ‘Requires improvement’ into a ‘Good’ or ‘Outstanding’ rating.

Your service should be working through an action plan of learning, development, and improvements – focus on one or two QSs each month. Show the CQC that you not only care but that you understand your regulatory responsibilities and have the evidence to demonstrate compliance. For example, the first QS focuses on learning culture. ‘We have a proactive and positive culture of safety based on openness and honesty, in which concerns about safety are listened to, safety events are investigated and reported thoroughly, and lessons learned to continually identify and embed good practices.’
The CQC will look for evidence in feedback
The CQC wants to see information being fed back to staff and the people you support and that there is organisational learning and development.
from commissioners and in your processes, including duty of candour records, evidence of learning and improvement, and incident records. It will be looking for proof that safety is a priority in your service – that staff are encouraged to speak up and incidents are investigated, risks are not overlooked or ignored, and lessons are learned from incidents or complaints. The CQC wants to see information being fed back to staff and the people you support and that there is organisational learning and development.
Key regulations to consider include ‘Duty of candour (Reg. 20)’, ‘Good governance (Reg. 17)’, ‘Safe care and treatment (Reg. 12)’, ‘Safeguarding (Reg. 13)’, and ‘Complaints (Reg. 16)’.
With Care England’s support, Hempsons has developed a toolkit to help social care providers navigate the SAF. With accompanying training, the toolkit brings the regulations and quality statements to life. It provides guidance and support to help you showcase your service in the best possible light and secure an optimum CQC score. For more information, visit www.hempsons.co.uk/services (select ‘Navigating the CQC quality statements’).
Philippa Doyle is Head of Social Care at Hempsons. Email: p.doyle@hempsons.co.uk : @PhilippaDoyle1

Senior leaders may be liable for data breaches and incur consequences such as fines and legal claims in the event of a cyber attack. Following the publication of a recent White Paper on the topic, Kurtis Toy, Chief Executive at the Cyber Centre of Excellence (CCoE), outlines the essential steps to protect your business.
Care providers, cyber security risk, and how to mitigate it are the main topics discussed in a recent in-depth White Paper, Protecting care providers from cyber attack, published by Care England in association with the CCoE.
Traditionally, you, like many other businesses, have relied on setting and forgetting standard anti-virus solutions and firewalls as your main source of cyber protection. While these products still have their place, care providers are being warned that this is no longer adequate against the rising cyber threat.
The landscape has become more complex, with cyber criminals finding ways around standard anti-virus solutions with zero-day attacks – those never seen before and therefore unable to be recognised and stopped – along with other methods of infiltration, such as through third-party supply chains and sophisticated phishing methods.
While you may not be the intended or original target, having cyber protections that are not up to date or adequate in today’s environment increases the likelihood of being exposed to potentially devastating consequences – financial, legal, and reputational. A recent search
of the dark web of just 20 domain names revealed 16,000 email addresses and passwords from care providers.
There have been multiple instances in the UK care sector in recent years where organisations believed they had adequate cyber security protection but were later found to be vulnerable. In January 2023, Cambian Group, a large provider of children’s care services, suffered an unauthorised breach which impacted its operations.
There has also been a string of significant NHS attacks this year. In June 2024, ransomware hackers infiltrated the computer systems of a company used by two NHS Trusts leading to major disruption with hundreds of patient appointments cancelled. Other attacks, such as the WannaCry attack in 2017 on the NHS, the Hackney Council cyber attack in 2020, the Blackbaud Data Breach in 2020, and the COVID-19 Vaccine Rollout Phishing and Ransomware incident in 2021, are detailed in the White Paper, highlighting the incident, what the vulnerability was, its impact, and the key lessons you can take from it.
Continued →

While these examples feature large organisations, it is likely that as bigger businesses become more attuned to the risks and strengthen their defenses, smaller companies will be targeted because of their supply chain links to organisations such as the NHS and local authorities. To help mitigate this increasing risk, cyber security protection which provides defence-in-depth, or layered solutions, is needed.
In the White Paper’s introductory statement, Professor Martin Green OBE, Chief Executive at Care England, said, ‘In the last year we have seen a huge increase in cyber attacks on health and social care organisations. As a sector we have, so far, avoided any major attacks, but we have seen other organisations in health and social care, including the NHS, badly hit. Whilst care providers are becoming more aware of the risk, there is still some way to go in raising awareness and implementing effective cyber security measures.’
Professor Green added that relegating the importance of cyber security due to its unseeable nature was a ‘dangerous’ move. ‘The adult care sector continues to face a great deal of pressure. Regulation, staff shortages, high staff turnover, and underfunding are major daily issues. Cyber security is a less visible threat and therefore often takes lesser priority, but this is a dangerous situation. A successful cyber attack could leave care sector businesses open to financial repercussions, reputational damage and, worst of all, potential harm to service users through loss or corruption of data,’ he added.
He also warned that the position of care providers in the supply chain would increasingly make them an attractive target for cyber attack. ‘Our members’ position in the supply chain with links to local authorities and other care organisations, such as the NHS, makes them an attractive target. While this has not yet been exploited on a significant scale, it is only a matter of time,’ he added, ‘As a sector we cannot ignore cyber threat. It is time to start thinking seriously about the risk of cyber attack, because unfortunately it is not a case of “if”, it is a case of “when”.’
Based on previously seen attacks on the health and social care sector, the White Paper highlights some key takeaways for the UK care sector:
• Social care organisations, particularly smaller ones, often underinvest in cyber security, mistakenly believing that basic firewalls and antivirus software are sufficient.
• Legacy IT systems in the care sector are often not updated regularly, making them vulnerable to known exploits like WannaCry.
• Many organisations depend on third-party vendors for data management and other services, but do not sufficiently assess these vendors’ cyber security practices.
• Personal data from social care systems, once breached, often ends up on the dark web, exposing vulnerable populations to fraud and identity theft.
• Cyber security threats evolve, and the care sector must continuously update its defences and train its staff in identifying phishing attempts and other cyber threats.
The White Paper marked the culmination of a year-long research project undertaken by Care England and the CCoE. Six organisations took part in a pilot – two large national providers, one learning disability provider, two small providers, and Care England. Each were given access to a range of practical support and solutions and then asked to feed back their experiences. The first stage of the project aimed to understand the cyber threats facing the care sector, while the second stage road tested different elements of cyber protection with participants.
The key cyber concerns identified through the pilot study were budgets, clicking a link that affects the company, data breach, phishing emails, ransomware, insider threat, malware, management support, security strategy, and state-sponsored attacks. The average rating participants gave as to whether cyber security was a concern for their organisation was four and a half out of a possible five, highlighting that cyber is a key worry for care providers.
I was impressed with the willingness of the pilot’s participants to engage with the trial. What I understood from the pilot study is that we need to remove as many barriers as possible to cyber security because this is a sector that is already under resourced and time poor.
During the pilot study, I explained that the CCoE’s research activities and projects across many sectors to date had consistently found worrying gaps in cyber security which the businesses and organisations were unaware of. Frequently seen vulnerabilities we found included badly configured services and out of date software, forgotten servers, and neglected websites affected by mergers or organisational changes. Often configuration changes can be made which accidentally make information available online without an organisation’s knowledge. These are effectively open back doors which could be exploited by those with malicious intent.
While the remedy to these vulnerabilities can be fairly simple, such as updating software or hardware to a version which is not vulnerable, these risks need to be highlighted and addressed before they are exploited.
I also acknowledged the difficulty businesses have in assessing vendors’ claims in a crowded marketplace, especially when they lack in-house expertise. This was echoed by one of the providers who took part in the research project who said the most valuable part of the pilot was the reassurance the CCoE gave them around who to trust. ‘We get offered a lot of cyber
security solutions, but it is hard to know how much of what is recommended is good and whether it will enhance the security of the organisation, or whether it is being offered to meet sales targets,’ said Manlio Mannisi, Head of IT at SeeAbility.
There are many types of cyber attack your organisation could fall victim to. These include malware, phishing, ransomware, zero-day attacks, Advanced Persistent Threats (APTs), supply chain attacks, and extortionware.
The most recent data from Verizon’s 2024 Data Breach Investigations Report1 highlighted that 68% of breaches involved a human element. This means understanding the risk posed by staff and deploying staff training to help them understand cyber security is essential.
The risks of staff accidently facilitating a cyber attack could be higher in the care sector than some other sectors. Staff using their own devices is common in the care sector, which can cause potential problems when linking to company databases through insecure networks. Time-poor employees may also be more likely to click a nefarious link.
Hackers having access to artificial intelligence (AI) has also been highlighted as a threat by the National Cyber Security Centre’s Annual Review 20232. AI will increase the speed at which cyber attacks can be developed and deployed by lower-skilled hackers, making it increasingly likely that you will be targeted directly or caught up in a supply chain attack.
Organisations storing personal data have legal obligations to ensure this data is stored safely and protected from being stolen or intercepted through a breach, including a cyber attack. Under UK law, health data is treated as ‘special category data’ due to its sensitive nature, which requires greater efforts to protect it.
With the social care sector digitising its care records and data at pace, and with many providers already facing funding issues and at risk of closing services, becoming the victim of a cyber attack would bring additional financial burden, both in
terms of recovery costs and possible fines from the Information Commissioner’s Office (ICO). A serious attack could also leave you exposed to reputational damage and potentially have devastating consequences for service users.
The cyber security industry is one in which many experts claim to have the one overriding solution, but no single solution exists which can meet your organisation’s cyber needs and risks. What is needed for optimal protection is a layered approach to security.
Following the success of the pilot programme carried out by Care England and the CCoE, Care Protect was designed as a complete package of support and protection. Care Protect is designed to be suitable for organisations of any size and can be tailored and adapted if required.
The five elements of the package necessary to protect your organisation are:
• Access to a half-day National Cyber Security Centre-assured board course.
• Passive scan of vulnerabilities – a report is generated on any vulnerabilities found and advice given on how to resolve them.
• Online staff cyber security training.
• Access to a virtual Chief Information Security Officer (vCISO) support session, including an individual vCISO session where tailored advice is given on improving cyber security. This could include advice on how to manage risk from the use of personal devices, such as mobile phones.
• AppGuard licences - licences for the zero-trust cyber security solution AppGuard, which can be installed on individual devices.
To speak to someone to discuss your cyber security or about procuring Care Protect for your organisation, contact Care England at info@careengland.org.uk or the CCoE at enquiries@ccoe.org.uk. To read the Protecting care providers from cyber attack White Paper, visit www.careengland.org.uk/cyber-centreof-excellence
References 1Verizon (2024). 2024 Data Breach Investigations Report. www.verizon.com/business/en-gb/resources/reports/dbir. Accessed 21st October 2024. 2National Cyber Security Centre (2023). National Cyber Security Centre Annual Review 2023. www.ncsc.gov.uk/files/Annual_Review_2023.pdf. Accessed on 21st October 2024.
Kurtis Toy is Chief Executive at the Cyber Centre of Excellence (CCoE). Email: enquiries@ccoe.org.uk : @CCOE_UK

We invite you to explore the incredible events listed below! These gatherings offer insightful and enjoyable experiences, providing a perfect opportunity to learn, connect, and collaborate with fellow providers. Don't miss out!
1 2
NAPA Conference & National Activity Awards | 24th January 2025
The NAPA Conference is the only UK event dedicated exclusively to activity and engagement. The day will feature hands-on workshops, expert-led discussions, and practical insights, all designed to enrich and inspire those in activity provision.
Social Care Summit North 2025 | 13th February 2025
This summit attracts a range of attendees, including care homes, home care providers, adult specialist care providers, retirement housing providers, technology developers, local government and more.
Care England 2025 Conference & Exhibition | 13th March 2025
3 4
Explore latest trends, technologies, and best practices shaping the care industry. Expert speakers and panelists have been lined up to share their views on how the sector will develop.
Care Show London | 30th April - 1st May 2025
Care Show London is a two-day conference and exhibition event offering the most invaluable knowledge-sharing, face-to-face networking, and innovationinspiring opportunities for those working in the adult social care sector.
To register for these events and see more, please visit www.careengland.org/events
Care England is always eager to hear from its members and strives to answer any questions and queries its members may have. In this issue, Care England answers questions on physical activity, single-handed care, insurance, and more.
Q: What steps can I take to protect my care service from cyber attacks?
A: Protecting your care service from cyber attacks starts with understanding the potential risks and vulnerabilities within your organisation. Care providers are increasingly reliant on digital systems for everything from care planning to payroll, making them prime targets for cyber criminals. The key is to focus on foundational security measures that are practical and effective.
First, ensure your systems and software are always updated with the latest patches and security updates. Cyber attacks often exploit weaknesses in outdated systems, so this simple step can significantly reduce your vulnerability. Alongside this, strong password policies and multi-factor authentication add an essential layer of protection by making it harder for attackers to access sensitive data.
Another critical area is staff training. Many cyber attacks begin with phishing emails or similar tactics that rely on human error. Training your team to recognise suspicious activity, avoid clicking on unknown links, and report potential threats is one of the most effective ways to prevent breaches. Backing up your data regularly is also essential. Ensure backups are encrypted and stored securely, so even if a ransomware attack occurs, your critical information can be recovered without paying a ransom. Finally, develop an incident response plan. Knowing how to identify, contain, and recover from an attack can make all the difference in minimising disruption and ensuring a swift return to normal operations.
These measures do not require a complete overhaul of your systems but can provide robust protection against many common cyber threats, keeping your service secure and compliant. For more information, read the feature beginning on page 40 or visit www.careengland.org.uk/cyber-centre-of-excellence
Q: How do I make sure my care home has the right coverage and is not overpaying for unnecessary insurance policies?
A: Navigating insurance in the care sector can be daunting, but it is crucial to have comprehensive coverage tailored to your specific risks. Care England’s Demystifying Insurance guide highlights key areas to focus on to streamline this process.
Start by reviewing your current policies to ensure they cover essential areas, such as public liability, employer’s liability, property insurance, and professional indemnity. One common pitfall is underinsurance – where policies do not provide adequate coverage for potential claims. This can leave you vulnerable in the event of an incident.
Work with a broker or specialist provider who understands the unique needs of adult social care. They can help you compare policies and negotiate competitive rates. It is also worth checking if your policy includes added-value services like risk management support, which can help reduce premiums over time.
Do not forget to review your insurance annually, especially if your service has Continued →
undergone changes such as expanding your workforce, upgrading equipment, or introducing new services. Regular reviews ensure your coverage stays relevant and cost effective.
Finally, clear communication with your insurer about your care setting’s needs and risks can result in more tailored and affordable policies. For more information, visit www.careengland.org.uk/demystifying-insurance
Q: Is single-handed care safe for residents, and what are the key steps to implementing it?
A: Single-handed care is a transformative approach that uses specialised equipment and techniques to enable one care worker to support a resident in tasks that might typically require two. It can improve efficiency, reduce costs, and foster a stronger sense of independence for the people you support and maintain their dignity.
To ensure safety, the first step is a comprehensive needs assessment for each resident to identify where single-handed care could be applied without compromising care quality. This is followed by training your care team to use the equipment effectively, such as slide sheets, transfer boards, or hoists.
A recent report, Are two people always required for moving and handling? recommends involving occupational therapists to guide implementation, ensuring the right balance between efficiency and dignity.
It is also important to trial the approach gradually and gather feedback from staff and residents. While it will not be suitable for everyone, many services have found it to be an effective way to optimise resources and maintain high-quality care.
If you are considering this, seeking guidance from specialists or peer services that have implemented single-handed care successfully is a great way to start. For more information, visit www.careengland.org.uk/single-handed-care.
Q: How can regular physical activity benefit older people in care settings, and what is the best way to encourage participation?
A: Regular physical activity is vital for older people, not just for physical health but for overall wellbeing. Exercise helps maintain mobility, balance, and strength, which are essential for reducing the risk of falls and maintaining independence.
For those living in care settings, even light activities can improve cardiovascular health, enhance mood, and support better sleep. The mental health benefits are equally significant – group fitness sessions or gentle activities like chair exercises can reduce feelings of isolation, foster social connections, and boost confidence.
To encourage participation, it is important to offer activities that are enjoyable, accessible, and tailored to individual abilities. Start with simple options like
seated yoga, light resistance exercises, or guided walks around the facility. Creating a routine and celebrating small achievements can help residents feel motivated and valued.
The Be Great Fitness guide highlights that success often lies in making fitness fun and integrating it into daily life. This could mean incorporating music, introducing games, or organising themed sessions that bring residents together in a positive and relaxed environment.
Remember, it is not about pushing limits – it is about improving quality of life through consistent, gentle movement that feels good. For more information, visit www.careengland.org.uk/be-great-fitness.
Q: Is there support to help my organisation meet the new requirements of the CQC’s single assessment framework (SAF)?
A: The introduction of the CQC’s SAF represents a significant shift in how care providers are assessed, focusing on consistent quality across all services. To support you in navigating these changes, Care England and Hempsons have developed a comprehensive SAF toolkit.
This toolkit is designed to help you align your practices with the CQC's new framework. It breaks down the SAF into clear, manageable components and includes practical templates, guidance, and examples tailored to the specific needs of care services. The goal is to make the process less daunting and ensure you are well prepared for inspections.
By using the toolkit, you can confidently assess your service against the CQC’s five key questions – safe, effective, caring, responsive, and well-led –and address any gaps proactively. It also helps you document evidence in a way that aligns with the framework’s expectations, ensuring transparency and demonstrating your commitment to high standards.
The SAF toolkit is a valuable resource for care providers of all sizes, offering a structured approach to compliance while supporting continuous improvement. Investing time in understanding and implementing the toolkit now can save significant stress during inspections and help your service thrive under the new framework. For more information, visit www.careengland.org.uk (search ‘Toolkit’).


Over 200 nutritious meals made with sustainably-sourced ingredients
Easy to order, store, cook and serve


Guaranteed nutrition and safety: our meals are tested in our onsite laboratory
Caters to every taste, dietary and cultural preference including dysphagia, dementia and malnutrition
No need for a chef

To book a FREE tasting call 0808 239 2399 or visit carehomes.apetito.co.uk

