ONE STEP CLOSER Reforming the Mental Health Act Integrated care Bright ideas Painting the picture A perspective from County Durham Rethinking housing with care leaseholds A National Care Service OCTOBER 2022 www.caremanagementmatters.co.uk





Are your care staff being weighed down by the burden of maintaining paper-based care records? Using a Digital Care Planning System doesn’t have to be daunting! A simple way for staff to create care plans and log care as it happens Used by over 3,500 care providers 40% Staff retention increase Number 1 choice for care staff More time to care Reduces stress teamworkFacilitates Book a demo with us today Scan me to find out more 01483 357 657 www.personcentredsoftware.comhello@personcentredsoftware.com
Social Care Insights

Deborah Rozansky from the Social Care Institute of Excellence (SCIE) shares a proposal for a Palliative and End of Life Care Evidence Centre.
Inside CQC
Debbie Ivanova, Director for People with a Learning Disability and Autistic People at the CQC, explains the importance of co-production and highlights how the regulator will continue to support people with learning disabilities and autistic people.
CMM News
Into Perspective
Can providers impact on ageist attitudes? Our experts share their views.
Celebrating Excellence
Alive Activities won the Technology Award and the Dementia Care Award at the Markel 3rd Sector Care Awards 2022. Find out how this small charity is making big changes.
Event Preview
A look at what’s to come at the CMM Insight Berkshire, Buckinghamshire and Oxfordshire Care Association Conference 2022.
What’s On?
Straight Talk
Mark Adams, Chief Executive of Community Integrated Care, reflects on the Boris Johnson leadership and what progress was made for social care.
In this issue REGULARS
Painting33

the picture of a National Care Service
The Labour Party is calling for a National Care Service offering free care at the point of need. So how would this work in reality? And is it something the care sector should be getting behind? John Kennedy shares his views.
One step closer to reforming the Mental Health Act
The draft Bill for Mental Health Act reforms has been published. Andrew Parsons from Weightmans offers insights into the key changes and what the social care sector can expect to see in terms of the impact of the amendments.

The Care Innovation Challenge: CMM meets the finalists CMM interviews the last group of finalists in NCF’s Care Innovation Challenge to discover their ideas to improve the sector.
FEATURES
Bright ideas: Rethinking tenure in housing with care Associated Retirement Community Operators (ARCO) is campaigning for a change in how leasehold works for the care sector, to better protect consumers and providers and encourage developments. Sally Ireland, Director of Legal and Compliance at ARCO, explores the background and the proposed reforms.
Working together: Integrated care boards
Integrated care systems are here to stay – so what works and what doesn’t? What impact will place-based arrangements have and how can providers get involved? We hear from County Durham Care Partnership on the changes coming into play.

CMM October 2022 3
0905073046484950
2043 4338332520 25 38
Commissioning
Designer:PRODUCTION
Rebecca
01223sales@caremanagementmatters.co.uk207770

Assistant aaron.barber@carechoices.co.uk
Director of David david.werthmann@carechoices.co.ukWerthmann












4 CMM October 2022 Michael Laing Director PartnershipDurhamServices,CommunityIntegratedofCountyCare Isobel Jones Chief Executive, Alive Activities Mark Adams, Chief IntegratedCommunityExecutive,Care @CQCProf @durhamcouncil @aliveactivities @ComIntCare EDITORIAL editor@caremanagementmatters.co.uk Editor: Olivia Hubbard
Editor: Angharad Burnham Content Editors: Aislinn Thompson, Henry Thornton
Mendil Director of Creative Operations: Lisa Werthmann Studio Manager: Jamie Harvey ADVERTISING
Advertising Manager: Aaron Barber
Sales:
SUBSCRIPTIONS Non-care and support providers may be required to pay £50 per Carewww.caremanagementmatters.co.uk01223info@caremanagementmatters.co.ukyear.207770ManagementMattersispublished by Care Choices Ltd who cannot be held responsible for views expressed by contributors. Care Management Matters © Care Choices Ltd 2022 CCL REF NO: CMM 19.7 CMM magazine is officially part of the membership entitlement of: CONTRIBUTORS Andrew Parsons WeightmansPartner, John Kennedy CommentatorConsultantIndependentand Jess Kuehne Senior forAgeism,ManagerProgrammeforCentreAgeingBetter Tom Owen Director, My Home EnglandLife Sarah Burns Joint Head of CareCountyCommissioning,StrategicIntegratedDurhamPartnership RozanskyDeborah@SCIE_socialcare ExcellenceInstituteSocialDirector,Careof(SCIE) Sally Ireland Director of Legal and OperatorsCommunityRetirementAssociatedCompliance,(ARCO) @durhamcouncil @CQCProf @JohnnyCosmos @Weightmans @ARCOtweets@MyHomeLifeUK@jesskue Debbie Ivanova Director for People with a CommissionCareAutisticDisabilityLearningandPeople,Quality(CQC)
SOCIAL CARE INSIGHTS
From Deborah Rozansky
The Director of Policy, Research and Information at the Social Care Institute for Excellence on a centre for Palliative and End of Life Care.


A few years ago, we stated on our website that it’s important that social care and health professionals who work with people at the end of life – and their families – have access to high-quality resources and information so they can give the best care possible.
The COVID-19 pandemic has provided a stark reminder of the importance of palliative and end of life care services (PEoLC). Parliament recognised this by establishing a new legal foundation for PEoLC as part of the Health and Care Act 2022. The recently formed Integrated Care Boards (ICBs) are now required by the Act to commission these services for their local populations.
Recent Government guidance (July 2022) and the revised Ambitions for Palliative and End
of Life Care: A national framework for local action 2021-2026 (May 2021) provide a framework and roadmap for taking the statutory duties forward. What remains clear, however, is that addressing the gaps in both research and practice for end of life care will be needed to meet the policy aspirations for improvements in clinical practice, service models and care debates,Alongsideexperiences.theparliamentarywewerecommissioned by
Marie Curie last year to carry out a short study into the feasibility of creating an Evidence Centre for PEoLC. We undertook a review of potential models, such as ‘What Works Centres’ and collaborative research centres, how they are governed, how they develop their strategic priorities and how they
influence both policy and practice. We also stakeholdersinterviewedinvolvedin PEoLC research and evidence translation to gauge support for the idea and get views about what the centre could achieve and how it might operate. We found that, ‘The opportunities are many, but the resources are few’ and ‘The current system emerged out of good ideas, rather than evidence.’
An initial prospectus for an evidence centre was drafted and, as we sought further feedback, we discovered a similar proposal from King’s College London. Bringing the two proposals together and partnering with Marie Curie and King’s College London, we further tested the evidence centre idea at a round table event with a wider
range of Roundtablestakeholders.discussions tested the case for the new centre, its potential purpose and helped to determine its role. Delegates have been supportive of the overall concept and said that the centre could play a crucial role in translating evidence into relevant and actionable guidance about how PEoLC services could be improved, and in helping decisionmakers and commissioners to put these improvements in place. Most importantly, we got a strong steer about involving people who have experience of PEoLC in the centre’s governance and activities.
Co-production is integral to our work, and we aim to work in partnership with people who draw on social care, their carers, families and citizens.
One roundtable participant reminded everyone of the huge power of those who deliver and lead the care experience; the need to share that power to harness everyone’s voice as part of the centre. Clearly, one of the next steps will be to ensure that coproduction becomes a central plank in the evidence centre’s formation.
In early September, we published the proceedings of the roundtable along with the initial prospectus. We encourage you to engage with our proposal and to provide us with your feedback. Achieving the ambitions of the centre will require cross-sector leadership and a consensus about the initial priorities for improving palliative and end of life care.
Deborah
CMM October 2022 5
Rozansky is the Director of Policy, Research and Information at the Social Care Institute for Excellence (SCIE). Email: deborah.rozansky@scie.org.uk Twitter: @SCIE_socialcare
Replace petty with





cash
individual cards Talk to us at The Care Show 12-13th Oct, Stand E93 Trusted by Soldo cards empower care home employees to make urgent purchases safely, without the paperwork. soldo.com/care
The best care is designed in partnership with the people who use it. People who use services should have the power and opportunity to shape their care. From designing the model of care to how care is delivered, this involvement should be genuine co-production and a partnership of equals.
Supporting your team to have the confidence and skills to work collaboratively is important. I am always impressed by teams that feel able to stand up and advocate for working in this way.
People often tell us how they feel valued by staff who show a genuine interest in their wellbeing and with whom they have a connection. It’s about asking people: What are your aspirations? Who would you like to live with? Respectful, friendly and meaningful conversations make people feel valued, so please keep taking the time to connect on a personal level with people in your care.
Inside CQC
DEBBIE IVANOVA
Debbie Ivanova, Director for People with a Learning Disability and Autistic People at the CQC, explains the importance of co-production, updates on the Because We All Care campaign and highlights how the regulator will continue to support people with learning disabilities and autistic people.

Being open to feedback, shaping training and services around people’s needs and making day-to-day interactions meaningful, are all aspects of open, positive cultures that we see in outstanding services.
These beliefs are also central to CQC’s engagement and co-production with people with lived experience, their families, providers and stakeholders. When we produce reports or consider a new way of working, we listen to many voices. It remains important to do everything we can to ensure people have care developed in partnership with them.
BECAUSE WE ALL CARE CAMPAIGN
From 31st August, CQC’s public behaviour change campaign moved into a new phase: encouraging people who have chronic and long-term conditions, as well as their friends and family, to share feedback on care.
Because We All Care is run in partnership
with Healthwatch England and aims to show how positive and negative feedback is valuable in understanding people’s experiences to inform the delivery of quality care.
We hope providers join the campaign to use free resources in the stakeholder toolkit, which includes an animation, imagery and graphics. We will publish research findings on our website, with insights from 1,000 people with a chronic illness and their carers, helping to shed a light on people’s experience of receiving support. The campaign also explores attitudes to providing feedback and the impact people believe this will have on care.
COMMITMENT TO PEOPLE
We have reviewed and updated CQC registration guidance to strengthen our regulation of services for people with a learning disability and autistic people. If providers haven't been assessed against Right Support, Right Care, Right Culture,
they will not be able to provide specialist care for people with a learning disability and/or autistic people.
Upholding people’s dignity and showing respect to people using services whomever they are, whatever their needs, is the cornerstone of quality care. We are working on a report called Who I Am Matters, which I will keep you updated on in more detail. It centres on the experiences of people with learning disabilities and autism in acute hospitals. Sadly, people with learning disabilities die earlier than neurotypical people and often have poor experiences of accessing and using health services. I encourage you to watch out for this report and join us to raise awareness of the issues we uncover.
I am aware that many providers may be facing challenges around energy costs and staffing. We are committed to raising these issues and working with others to support the sector. If you are experiencing difficulties, speak to your trade association, local authority or us.
Debbie Ivanova is Director for People with a Learning Disability and Autistic People at the Care Quality Commission. Twitter: @CQCProf
"It remains important to do everything we can to ensure people have care developed in partnership with them"
CMM October 2022 7
Do you have a question for the CQC on its campaigns and work to support people with learning disabilities? Visit www.caremanagementmatters.co.uk and share your feedback on the article.
Dignity. Privacy. Independence.
Meet Vayyar Care, a unique, touchless, virtual caregiver that provides instant fall detection and resident activity data.

� No intrusive cameras
� No embarrassing wearables
� No hard-to-reach buttons
Join the Greyt Revolution www.vayyar.com/care/b2b stuart.barclay@vayyar.com

MYSAFEFEELINGISRIGHT!
Care sector pays tribute to HM Queen Elizabeth II
Britain's longest-reigning monarch died peacefully, surrounded by her family, at Balmoral in Scotland on Thursday 8th September.
As MPs gathered to pay tributes to the Queen, Prime Minister Liz Truss described her as ‘one of the greatest leaders the world has everProfessorknown’.
Vic Rayner OBE, Chief Executive Officer of the National Care Forum (NCF), said, ‘We mourn with the nation in our loss of Her Majesty Queen Elizabeth II who has been a model of dedicated service for over 70 years. As the patron of many of our member organisations she has demonstrated unreserved commitment to care, charity and community through her ongoing patronage and her previous patronage of members.’
Care England, on behalf of its Chief Executive Officer, Professor
Martin Green OBE, said, ‘Care England is saddened by the death of Her Majesty the Queen. We will always be grateful for her support to so many charities and care services over her long and distinguished reign. We send our condolences to HM the King and all the Royal Family.’
Dr Jane Townson, Chief Executive Officer of the Homecare Association, said, ‘Rest in peace, Your Majesty. Thank you for your incredible service over so many years. Nobody could have been more dedicated and hardworking. Your warmth, humanity and sense of humour lifted our spirits.’
Richard Murray, Chief Executive of The King’s Fund, said, ‘It is with great sadness that we learnt of the death of Her Majesty the Queen. The Queen had been Patron of The King’s Fund since the start of
her reign. In that time, the UK has seen great gains in life expectancy, medical innovations have saved the lives of millions, and most recently the Queen was a source of hope and stability as COVID-19 spread across the UK and the wider world.
‘Our thoughts are with His Majesty King Charles III and the rest of the Royal Family. We are thankful for the extraordinary life and work of the Queen.’
The news of the passing of HM Queen Elizabeth II is a cause of great sadness to all of us at CMM. Our thoughts and deepest condolences are with the Royal Family and everyone around the world united at this difficult time. Thank you for your dedicated service and commitment to care, charity and community, Your Majesty. You were a beacon of hope to so many, you will be truly missed.
PM sets out energy support package
The Prime Minister, Rt Hon Liz Truss MP, has announced plans to cap average household energy bills at £2,500 a year from October. At time of writing, there has not yet been any detail about specific support for the social care sector.
The Government has announced that there will be a new six-month scheme for businesses, which will provide equivalent support to that being offered to consumers. After that six-month period, ministers plan to offer ‘focused support’ to vulnerable industries. Truss says the Government will also support all business charities, offering an equivalent guarantee for six months.
Surging energy prices are already having an impact on the healthcare sector, following reports of care
homes shutting down due to rising energy costs. According to Care England, based on the October 2022 market rates, and with 454,933 CQC registered beds, the approximated impact of the rising energy prices on the sector over the last year has been over £2bn per annum.
The Homecare Association is calling on the Government to provide immediate emergency grant funding of £107m (per annum) to help cover increased fuel costs incurred by care workers in delivering homecare.
Care England is calling for the introduction of a per-bed energy price cap equivalent to the proposed domestic energy price cap or the reimbursement of providers for the increased energy costs incurred by other means, the extension of the
£400 energy rebate to vulnerable people in care and supported housing, introducing parity in the way they are treated compared with those living in their own homes and the removal of VAT and the Green Levy on energy bills.
The National Care Forum (NCF) said care settings need to be included in the domestic price cap and we need an emergency ring-fenced energy fund that could flow from central Government to local care providers. In relation to the energy crisis, The Independent Care Group (ICG) wants the new Prime Minister to include care and nursing homes in the price cap for energy prices, grant people living in care settings utility bill rebates and help domiciliary providers tackle huge fuel costs.
AMBIENT SUPPORT
Ambient Support appoints Will Thornton as its new Regional Manager for Lincolnshire and the Midlands. Will has held a number of senior roles across East and North London, including as a commissioner, plus he has worked for several Midlands-based charities including Residential Care, Community Services and more recently for Blind Veterans UK.
BELONG
Dementia care specialist Belong has appointed Ali Gopaul to its operations team, with oversight of the organisation's Greater Manchester care villages, as well as the group's health and fitness provision across all locations. In his new role as Operations Manager, Ali will work closely with teams in Atherton, Wigan and Didsbury.
CORNERSTONE
Cornerstone Healthcare Group has appointed Niki Richards to the role of General Manager of its 99-bed service, South Africa Lodge in Waterlooville, Hampshire. Niki, a registered nurse, has previously worked in senior leadership roles within the NHS, the National Care Standards Commission, Healthcare Commission, CQC and large care providers.
HEALTHCARE HOMES
Healthcare Homes welcomes Ian Hadingham as Operations Managing Director to Manorcourt Homecare. Ian previously held the role of Group Director of live In care with City and County Healthcare Group. He also worked as Operations Director with MiHomecare and Care Delivery Director with Allied Healthcare.
CMM October 2022 9 NEWS
APPOINTMENTS
Call for PM to deliver on social care
HOLMES CARE GROUP
Holmes Care Group has announced two new appointments, with the recruitment of a Head of Operations and Head of Dementia and Lifestyle Enhancement, to its senior leadership team. Holmes Care welcomes Sheilah Harvey as its Head of Operations, who joins the company with over 30 years of experience across the UK and Australia and a strong knowledge of the health and community care sector. Yvonne Manson also joins Holmes Care as the Head of Dementia and Lifestyle Enhancement, following 26 years of experience working in the care sector.
ORBIS EDUCATION AND CARE
Orbis Education and Care has appointed Kris Davies in a new role for the organisation, as its Head of Academy Living.
Kris’s new role will see the organisation build on its existing work to create personal development pathways for young people and adults to identify and progress in vocational and employment opportunities. Kris will draw on his background in Occupational Therapy and as a Behaviour Specialist to identify further opportunities for learning and personal development for individuals with autism and a learning disability.
CMMtheAreAPPOINTMENTSyougettingbenefitofthewebsite?
Sign up today to start getting more from CMM.
It’s FREE for care providers.
www.caremanagementmatters.co.uk
Social care organisations are calling on Liz Truss, the new Prime Minister, to commit and take urgent action to deliver on adult social care. The National Care Forum (NCF) has said that the current £5.4bn earmarked for social care is simply not enough to address the challenges facing theCaresector.England is calling on the Prime Minister and her Cabinet to ensure that the Conservative manifesto promise to ‘fix social care’ happens under her leadership and immediate support is madeAsideavailable.fromthe energy price cap, Care England is calling on the Government to direct a greater share of the money generated through the Health and Social Care Levy towards the adult social care sector, implement the recommendations of the Levelling Up, Housing and Communities Committee report and commit to
addressing existing inequalities through increased funding to the adult social care sector.
There have also been calls for the Government to commit to a long-term workforce strategy for adult social care, which aligns pay and benefits with the NHS and local authority-run services and to remove with immediate effect the charges made by the Home Office and for the full reimbursement of recruitment costs by providers for overseas recruitment.
Nick Sanderson, Chief Executive of Audley Group, urges the new Housing Secretary to look beyond empty promises to build more houses ‘when the solution is to build smart.’ He said, ‘I urge Mr Clarke to look beyond the empty promises to build more houses and consider how to better use the homes that already exist. More housing has never been the problem. The Government’s focus
must shift to specialist housing, and fast. It’s never going to be greener to build more when the solution is to build smart.’
Kari Gerstheimer, CEO and Founder of Access Social Care, said, ‘Liz Truss recently announced her plan to divert £13bn from NHS funding to finance local authority spending on social care. The sector can now only hope that she acts on these bold commitments without causing harm to an NHS already on the cusp of crisis. Access Social Care welcomes the recognition that, without a properly funded and adequately supported social care system, the capacity issues in hospitals and the health service will become yet more intolerable. However, the suggestion that we should divert vital financing from one service to pay for another seems deeply problematic.’
NHS invites people for autumn booster
Care home residents and staff were some of the first people in the world to receive the new, varianttackling jabs, as the NHS COVID-19 booster vaccination programme moves to the next phase.
The new bivalent jab targets both the original strain of the virus and its Omicron variant. The manufacturers Pfizer and Moderna have had vaccines approved by the medicines regulator and the NHS will use
Aroundboth.four million people who are at highest risk, including the over 75s and those with weakened
immune systems, are now eligible to book a vaccine through the National Booking Service. The NHS will visit hundreds of care homes with thousands more planned throughout September and October. A record 3,100 sites are expected to be part of the rollout.
NHS Chief Executive Amanda Pritchard said, ‘The precision and speed of the NHS COVID-19 vaccination programme allowed us to get back to a pre-pandemic way of life and doing the things that we love. While we know that this winter will be challenging with a
likely resurgence in both COVID-19 and flu for the first time since before the pandemic, the best way to protect yourselves and your loved ones from serious illness is to get the newly approved, next generation COVID vaccine when invited to do so, as well as your annual flu jab, to ensure you have maximum protection.’
More than 126 million COVID-19 vaccines have been administered since the first COVID-19 jab was delivered outside of clinical trials to Maggie Keenan in Coventry in December 2020.
Report reviews care market in South East
Care England has joined the South East Social Care Alliance (SESCA) to express significant concern at the findings of a report on the stability of the adult social care market.
Between 11th May and 11th July 2022 SESCA collected data via an online survey sent to 3,227 adult social care provider contacts across eight counties in the South East covering the whole region except
for the Isle of Wight. Overall, there were 198 responses (6%).
• Staff are leaving the sector faster than providers can replace them with 83% of providers finding it more difficult to replace staff than in the past.
• 38% of those leaving their role are exiting the adult social care sector. Competition from other sectors/NHS and low morale are
the driving forces.
• The workforce crisis is leading to a reduction in the amount of care available.
• Funding increases for costhaveauthority/NHS-fundedlocalclientsnotkeptpacewithactualincreases.
• 45% of providers in the South East have considered exiting the market.
10 CMM October 2022 NEWS


CMM October 2022 11 software that helps care homes thrive Learn how Sage can help: • Increase revenues by 25% without adding additional headcount. • Save over 400 person-hours annually. • Streamline your operations and automate your financials. Download product brochure
Asymptomatic testing paused in care homes
Regular asymptomatic testing for COVID-19 in all remaining settings in England paused from 31st August, as COVID-19 cases continue to fall.
Free testing for the public ended on 1st April as part of the Government’s ‘Living with COVID-19 plan’, but asymptomatic testing continued to be used in some settings during periods of high case rates.

The vaccination programme means COVID-19 cases have now fallen to 40,027 and the risk of transmission has reduced. Deaths have fallen to 744 and hospitalisations to 6,005 between 17th-24th August, meaning wider asymptomatic testing can soon end as planned in most instances. Symptomatic testing in high-risk settings will continue.
Testing will remain in place for admissions into care homes and hospices from both hospitals and the community, and for transfers for immunocompromised patients into and within hospitals to protect those who are most vulnerable. Testing will also be available for outbreaks in certain high-risk settings such as care homes.
The Department of Health and Social Care (DHSC) has said yearround symptomatic testing will continue to be provided in some settings, including:
• NHS patients who require testing as part of established clinical pathways or those eligible for COVID-19 treatments.
• NHS staff and staff in NHS-funded independent healthcare provision.
• Staff in adult social care services and hospices and residents of care homes, extra care and supported living settings and hospices.
• Staff and detainees in prisons.
• Staff and service users of certain domestic abuse refuges and homelessness services.
DHSC explores international recruitment campaign
New plans are being considered by the Department of Health and Social Care (DHSC) on international recruitment to ‘boost’ staffing numbers.
A DHSC spokesperson said, ‘Our new international recruitment taskforce is considering innovative ways to boost staffing numbers within health and adult social care. As part of this, we will work with the sector and recruitment experts to examine how to recruit staff from overseas more effectively into adult social care.’
Professor Vic Rayner OBE, Chief Executive of the National Care Forum (NCF), responded to the news on international recruitment and said, ‘There is no doubt that there is a need to take action in relation to the social care workforce. An international workforce has always been a fundamental and valued element of the delivery of front-line care, with colleagues welcomed from across Europe and a wide range of other countries, and efforts to support and streamline current approaches to international recruitment would be welcome.’
Julia O’Connor, Managing Director of Patterson Healthcare, a recruitment specialist for the health and care sector, said, ‘Whilst on the face of it this may seem like very welcome news given the current staff and candidates shortages within the NHS and the wider health and social care sector, however, if we look at care and support worker roles, these are some of the lowest paid roles in the country and this begs the question as to where international workers will live and stay when they arrive in the UK.’
The recruitment specialist urges providers to spend time on advertising, make the first three lines of your recruitment advert really sing and think about what benefits you are able to offer to employees.
12 CMM October 2022 NEWS
All-in-one PASS with Roster Scan me Digital care management for today and tomorrow Scheduling • Payroll • Invoicing • Reporting
Sector calls for COVID-19 workforce sick pay
Providers have called for urgent sick pay provisions for care workers.

Regulations in England mandate twice weekly lateral flow tests for carers, with those testing positive forced to stay at home. However, the Infection Control Fund that previously met the costs of sick pay ended in the spring, therefore care providers have been meeting the unfunded costs of sick pay directly through debt or utilising their increasingly exhausted reserves.
The current statutory sick pay for care workers is £99.35 per week if they call in sick and sector leaders say many care workers simply do not have the savings to live on statutory sick pay of less than £100 a week. Due to the financial pressures, care workers who test positive for COVID-19 will not declare these positive tests to ensure that they can remain at work or will choose to leave a sector that
is already in a workforce crisis.
Community Integrated Care, a charity that employs more than 5,000 social care workers across the UK, has asked the Government to reinstate funding for this enforced sick leave. The charity has seen almost 50% of its workforce –around 2,500 staff – forced to take time off with COVID-19 in the past six months. Following the cessation of funding, most of the cost of sick pay has been met from the charity’s reserves at a cost of almost £1m.
Liz Jones, Policy Director for the National Care Forum (NCF), said, ‘The Government needs to invest in the sector, so that it can give people the same terms that are reasonably expected within the NHS and so many other industries.'
Visit the Department of Health and Social Care (DHSC) website to read the latest updated guidance for care homes.
Report on sector quality improvement

The King’s Fund has published a new discussion paper, exploring how local authorities in England improve the quality of care.
The King’s Fund found examples of local authorities doing excellent work in very difficult circumstances. In particular, they found that there were good examples of local authorities creating a supportive environment for effective improvement through building capacity, for example, by borrowing staff with specific expertise from neighbouring areas; building capability, for example, by inviting staff to regular senior management discussions to expose them to quality issues; demonstrating leadership, for example, setting a clear strategic vision for quality improvement; creating a culture for improvement to thrive, for example, by creating
a safe environment where staff feel comfortable raising
Whileconcerns.thereis good work going on across the five local authorities that The King’s Fund selected, The King’s Fund said many of the markers of a quality improvement approach were missing – for example, being able to define and agree what quality includes, a clear theory of change, measurement of impact or continual efforts to continue and sustain improvement.
This paper is intended to prompt fresh thinking about how to support people to improve adult social care – a highly skilled and challenging task. The King’s Fund said quality improvement is not a magic bullet; it needs resources, expertise and a willingness to work differently.
Total CQC Compliance Solutions CQC Experts work with you to achieve and maintain CQC Compliance for your business, allowing your staff to focus on caring. Call us on 01462 222600 to find out how we can support you. www.cqcexperts.com • hello@cqcexperts.com Visit us at The Care Show - Stand G65 and chat to an ‘Outstanding’ care provider. Policy packs from £74.95 per month RegistrationCQCSupport ComplianceOngoingCQC PoliciesProcedureandPacks discount10%usingCMM10% NEWS CMM October 2022 13
We peoplehelpwho care
Are you recruiting overseas candidates for the care industry?

To work in the UK, candidates need proof of B1 level in English. They can get it with Skills for English
Skills for English is a Secure English Language Test (SELT), approved by the UK Home Office for Visa and Immigration purposes, that can be taken outside of the UK.
Work with us
Approved for UKVI
Skills for English is one of only 4 SELT tests that can be taken outside of the UK
125+ countries
Easily find an available session in a global network of Home Officeapproved test centres
Fast results
The test results are usually available within 3-5 days
Find out more
Get in touch to discuss how you can add Skills for English test to your services: hello@skillsforenglish.com
English language testing for UK Health and Care Workerskillsforenglish.comVisa
New study on music therapy and dementia
The research, by Casio Music UK, in partnership with Music For Dementia and charitable care provider Methodist Homes (MHA), placed keyboards in homes for residents to use as part of its ‘Light Up My Life’ research initiative.
The project took place in some of MHA’s specialist dementia care homes nationwide over a six-month period. Casio provided key lighting keyboards to care homes to use in music therapy and music activity sessions that engaged over 100 residents living with dementia, to improve music participation and, ultimately, enhance their quality of life. The sessions that took place were a mix of one-to-one sessions and group sessions, dependent on the structure of the care home. The key lighting technology meant that participants were able to simply follow the lights on the keyboard, which would guide them to the correct notes without any prior musical knowledge or previous piano playing experience. A range of well-known pieces of music were preloaded into the keyboards for residents to enjoy. This unique key lighting technology was
fundamental to the overall core element of the ‘Light Up My Life’Somecampaign.ofthe key findings
included:•79%of music therapists and 64% of care home staff said residents showed improved signs of memory recall after playing the keyboard and producing a recognisable song.
• 95% of music therapists and 71% of care home staff were in agreement that playing the keyboard increased or enhanced opportunities for social interaction for the residents with staff and relatives.
• 70% of music therapists saw a reduction in anxiety and depression amongst the residents, further supporting the evidence base that music therapy reduces the need for medication.
• 95% of the residents who participated said that they were elated or felt happy after completing a song on the keyboard and 86% of music therapists agreed. The sessions enhanced the residents’ wellbeing.
Organisations unite to oppose Bill
The Relatives and Residents’ Association (R&RA) has joined 120+ organisations calling for the Government to abandon plans that R&RA believe will ‘weaken’ human rights protections.
The Bill of Rights Bill, introduced to Parliament in June under the leadership of Boris Johnson and Dominic Raab, would repeal and replace the Human Rights Act.
Helen Wildbore, Director of the R&RA said, ‘This is a hugely concerning Bill which would strip away crucial rights
IN FOCUS
protections and place older people needing care in an even more vulnerable situation. We are pleased to hear the new Government have shelved these plans, but they must be dropped entirely. With social care in crisis, and the costof-living devastating families and care services, these must be the urgent priorities for the Government, rather than wasting precious time and energy on an unworkable, unnecessary new law to weaken fundamental rights.’
New analysis on unmet need
WHAT’S THE STORY?
New analysis by Age UK for the Care and Support Alliance (CSA) has found that a massive 2.6 million people aged 50 and above are living with some form of unmet need for care in England. This is the best estimate so far produced for the numbers of people in mid-life, as well as of above State Pension Age, who require assistance with one or more activities of daily living, like washing and eating. The 2.5 million over-50s in this position are equivalent to 12% – or one in eight – of the entire same-age population in this country.
Furthermore, recent evidence suggests almost three quarters (73%) of social services directors are reporting more breakdowns of unpaid carer arrangements (ADASS Spring Survey 2022).
WHAT WERE THE FINDINGS?
The latest data by Age UK and the Care and Support Alliance show that:
• 70% (1.8 million) of those with an unmet need for care have difficulty dressing.
• 18% (450,000) of those with an unmet need for care have difficulty walking across a room.
• 47% (1.2 million) of those with an unmet need for care have difficulty bathing or showering.
• 12% (320,000) of those with an unmet need for care have difficulty eating.
• 36% (930,000) of those with an unmet need for care have difficulty getting in and out of bed.
• 23% (600,000) of those with an unmet need for care have difficulty using the toilet.
• 7% of people in their 50s have an unmet need for care; 12% in their 60s; 15% in their 70s; 21% in their 80s and older.
• 21% (540,000) of people with an unmet need for care are often lonely, compared to 6% of people who have no need for care and 12% of people who have a need for care which is met.
(Age UK analysis of data from wave 9 of the English Longitudinal Study of Ageing, scaled up to the population of England using data from the 2021 Census.)
WHAT DID THE EXPERTS SAY?
Caroline Abrahams, Charity Director of Age UK and Co-Chair of the Care and Support Alliance, said, ‘At the moment, all the data points to social care becoming weaker as time goes on, not stronger, particularly when you look at the state of the workforce, where vacancies are increasing month by month. This is scarcely surprising when you consider how uncompetitive the terms and conditions in social care now are: the incoming administration must understand that they will not begin to turn the curve on quality and access in social care until they ensure care staff are properly recompensed for the incredible work they do.’
Visit the Age UK website for further information on this story.
CMM October 2022 15 NEWS
NEWS / IN FOCUS
Minister supports care innovation challenge
The Minister for Social Care and Mental Health, Gillian Keegan, has offered her support to the Care Innovation Challenge finalists and said innovative ideas are so important to transform the careThesystem.fivefinalist teams selected from the Care Innovation Challenge creative weekend spent the morning of 10th August presenting their ideas for innovation in social care to Alice Ainsworth, Deputy Director of the Adult Social Care Technology Policy Team and NHS Transformation Director at the Department of Health and Social Care’s Victoria Street office.
Gillian Keegan said, ‘We are investing £5.4bn to reform social care and end unpredictable care costs so people can access affordable care when they need it
When technology is embedded seamlessly into care and support services, it can be transformative, enhancing the quality of care and helping people to live more independent, fulfilled lives. That is why the innovative ideas generated by the contestants in the Care Innovation Challenge are vital in demonstrating the power of technology to transform the careNHSsystem.’Transformation Director Alice Ainsworth thanked the teams for all their efforts so far, saying, 'All the ideas are viable solutions for reform. We are looking forward to working with you to see how your innovations can improve the outputs for people needing social care.’
The five finalist teams will be showcasing their ideas at The Care Show, the largest care event in the UK, on 12th-13th October.

Call for clarity over National Care Service Bill
Scotland Excel, the centre of procurement for the local government sector, is seeking clarity over the future of national and local social care commissioning in its response to the call for views on the National Care Service Bill.
The Bill was published on 21st June 2022 to allow Scottish Ministers to transfer social care responsibility from local authorities to a new, national service. As Scotland Excel oversees national social care commissioning and procurement on behalf of councils, it is keen to see clarity over future roles and responsibilities for national and local commissioning.
In its response to the Bill, Scotland Excel is seeking further information on:
• Whether Scotland Excel will continue to deliver national care arrangements.
• Which parts of commissioning will be delivered nationally and locally.
• Clarity over roles and responsibilities at a local and national level.

• What the future governance models will be and how they will link to the robust governance already in place.
• How this will link with current and planned legislation.
Julie Welsh, Scotland Excel’s Chief Executive, said, ‘For more than 10 years, we have delivered national social care arrangements in collaboration with the wider sector, and national care commissioning on behalf of councils and HSCPs and this is a key strategic function for us, covering both adult social care and children’s services.’
Visit the Scotland Excel website for more information.
16 CMM October 2022 NEWS
Applications for the Care Sector integrated into Microsoft Teams CareComplianceEnquiryPropertyTimeRosteringHR&AttendanceMaintenanceManagementManagement. www.CarePoint365.co.uk Tel: 020 4558 1503 email: getintouch@carepoint365.co.uk
Deafblind UK to host virtual conference





The virtual Deafblind Convention, hosted by Deafblind UK, is back for its second year on 6th October. The event will comprise many well-known international and UKbased speakers who will focus on the topic of ‘Embracing Change’.
This event will feature speakers who have a professional or personal interest in sight and hearing loss. Chief Executive Steve Conway said, ‘It’s a real
pleasure to bring you this event once again. Being deafblind means living with constant change; it’s an ever-evolving cycle that has no end point. From experiencing first symptoms to adapting to a global pandemic, sight and hearing loss changes lives. This event will explore how deafblindness forces change and how a changing world impacts deafblindness.’
Care England Agency Fee Survey
Care England’s Agency Fee Survey unveiled the extent to which the COVID-19 pandemic has exacerbated the reliance on agency staff, reaching a point of unsustainability for the sector. The survey found that:
• 78% of respondents said they are using more/significantly more agency staff compared to April 2021, with 88% saying it was more/significantly more
challenging to book them.
• 86% of respondents said the costs of agency staff have increased since April 2021, 74% said they had to contact multiple agencies to source agency staff and 77% said it became more difficult to book them. There was a theme of poor-quality, less-experienced and inappropriately trained staff, with 73% of respondents
Deafblind UK hosted the UK’s very first Deafblind Convention last year and over 700 delegates attended. This year is set to be no different, bringing people together to share thoughts, opinions, research and experiences of living better with sight and hearing loss. Delegates will be able to personalise their day by choosing from a wide range of insightful talks, giving
a truly unique experience to all whoThisattend.year’s event will include Deafblind UK’s ‘Stepping Forwards’ commendations: official recognition and thanks to certain people and organisations who have gone over and above the call of duty to support Deafblind UK, and therefore the wider deafblind community, this year.
reporting that agency staff were less reliable.

• Agency rates were significantly greater than carer (£19.57 vs £9.90) and nurse (£27.56 vs £19.49) employee hourly rates.

Professor Martin Green OBE, Chief Executive of Care England, said, ‘The use of agency staff has been a bandage over more deeprouted recruitment and retention
issues, which now, expectedly, are unravelling. The results of our recent survey demonstrate the severity of these issues, with the usage and cost of agency staff increasing dramatically over the last year. This is not only affecting the quality and continuity of care but compounding pressures on the NHS. Without central intervention, these issues will only worsen over the coming months.’
CMM October 2022 17 NEWS
When industry knowledge and wisdom are needed, when a discreet sale is desired, our clients choose DC Care to sell their healthcare business. SALES | ACQUISITIONS | APPRAISALS | CONSULTANCY 01937 849 268 www.dccare.co.uk sales@dccare.co.uk specialist healthcare business agents Independent expertise Nationwide knowledge A selection of care businesses recently successfully sold by DC Care... SOLD We have a wealth of experience and industry knowledge and we are very proud that DC Care is established as one of the largest independent Care specific agencies in the UK. If you are considering a sale of your care facility, please call us on 01937 849 268 or send an email to sales@dccare.co.uk for a free, no-obligation Market Appraisal. specialist healthcare business agents ANNIVERSARY20TH
NEWS FROM ACROSS THE GLOBE
Japanese care home recruits infants
Ichoan nursing home in Kitakyushu, a city of 940,000 in Fukuoka, has launched a new baby worker programme to help people connect across generations.AsJapan’s population has aged, the use of nursing homes has grown rapidly. The
number of people in such homes more than doubled to 1.8 million between 2005 and 2020, according to the Japanese Government. The concept of letting nursing home residents interact with children is not new. The New York Times reported that in Seattle in the
US, residents of Providence Mount St Vincent have shared their facility with a childcare programme for newborns to five year olds since 1991.
Among Ichoan’s 120 residents, the oldest is 101 and the youngest baby worker is two months old. Kimie Gondo, the nursing home’s
Genetic sequencing to predict COVID-19 severity
Researchers at Drexel University in Pennsylvania have created a computer model that could help them be better prepared for predicting COVID-19 variant surges. The model uses machine learning algorithms, trained to identify correlations between changes in the genetic sequence of the COVID-19 virus and upticks in transmission, hospitalisations andThedeaths.Drexel model, which was recently published in the
journal Computers in Biology and Medicine, is driven by a targeted analysis of the genetic sequence of the virus’s spike protein — the part of the virus that allows it to evade the immune system and infect healthy cells; it is also the part known to have mutated most frequently throughout the pandemic — combined with a mixed effects machine learning analysis of factors such as age, sex and geographic location of COVID-19 patients.
The research team used a newly developed machine learning algorithm called GPBoost, based on methods commonly used by large companies to analyse sales data. Via a textual analysis, the programme can quickly home in on the areas of the genetic sequence that are most likely to be linked to changes in the severity of the variant. It layers these patterns with those that it gleans from a separate perusal of patient metadata (age and
Planning for improved care in Somaliland
The World Health Organization (WHO) and King’s Global Health Partnerships (KGHP) were invited by the health authorities in the Awdal and Marodijeex regions to support efforts to improve quality of care through development of a quality-ofcare strategy, recognising the significant impacts caused by care that is not effective,
safe and people centred. The support used the recent WHO technical package on Quality of Care in Fragile, Conflict-affected and Vulnerable Settings and drew heavily on 20+ years of collaboration between KGHP (a health systems strengthening initiative within King’s College London) and local authorities. It is part of a wider project that
also includes capacity-building on quality improvement and use of WHO tools to identify priority gaps in patient safety andThequality.workshop and mission were roundly welcomed as successful and important steps in advancing quality of care in the Awdal and Marodijeex regions. At the meeting, it was
Director, said she was inspired to start the programme when she took her newborn granddaughter with her to work and saw how the residents smiled and played with her. The programme began with just one baby in 2021 and has now grown to 32 infant ‘employees’, mostly from families in the area.
sex) and medical outcomes (mild cases, hospitalisations, deaths). The algorithm also accounts for, and attempts to remove, biases due to how different countries collect data. This training process not only allows the programme to validate the predictions it has already made about existing variants, but it also prepares the model to make projections when it comes across new mutations in the spike protein. It shows these projections as a range of severity.
decided to produce a quality strategy and establish a quality technical working group to oversee its development and implementation. The situational analysis findings were discussed and validated and will now be incorporated into a final report that will be used to guide development of the policy and strategy.
Half of global healthcare facilities lack basic hygiene services
Half of healthcare facilities worldwide lack basic hygiene services with water and soap or alcohol-based hand rub where patients receive care, and at toilets in these facilities, according to the latest Joint
Monitoring Programme report by the World Health Organization (WHO) and UNICEF.
Around 3.85 billion people use these facilities, putting them at greater risk of infection, including 688 million people who
receive care at facilities with no hygiene services at all. The latest report, Progress on WASH in Health Care Facilities 2000–2021: Special focus on WASH and infection prevention and control, has for the first time established
this global baseline on hygiene services – which assessed access at points of care as well as toilets – as more countries than ever report on critical elements of WASH services in their hospitals and other health centres.
18 CMM October 2022 NEWS NEWS
NEWS




































LOVE LAUNDRY We understand how important laundry equipment is to your care or nursing home. Our goal? To make it simple. Made for you Bespoke laundry and finance options to suit you. Safe and sound Helping you create an infection-free environment. Count on us Professional, approachable and at your service. 08000 546 546 WASHCO.CO.UK

20 CMM October 2022
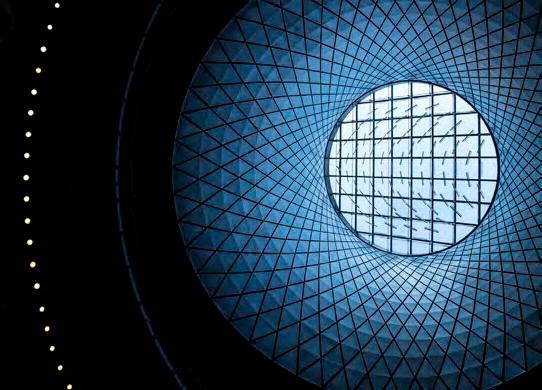
Painting the picture of a National Care Service

There is much discussion at the moment about the proposals for a National Care Service (NCS). The plan is for it to be envisioned on very similar lines to theTheNHS.former
Labour leader, Jeremy Corbyn, promised a National Care Service in the 2019 manifesto but his successor, Kier Starmer, has said he will be writing the manifesto from scratch. The independent left-leaning think tank, The Fabian Society, announced in July that it’s developing a roadmap towards a National Care Service for England. A study will make recommendations to the Labour party policy review and to shadow Health and Social Care Secretary, Wes Streeting MP. The research is funded by Unison and is led by The Fabian Society’s General Secretary, Andrew Harrop.
Wes Streeting has been vocal in his support for the new care service and said, ‘I would love to see a National Care Service delivered exactly on the same terms as the NHS, publicly owned, publicly funded, free at the point of use.’Publicly owned, publicly funded and free at the point of use. All sounds very attractive – or does it? Won’t we just be in danger of swapping one top-down failed system – local authority commissioning – with another equally unresponsive state bureaucracy?
MODELS OF CARE
The NHS model works for health; it’s not perfect but nothing ever is. Free at the point of delivery is efficient and the model has stood the test of time. It is largely cherished as a national treasure. Granted it may be underfunded but the fundamental architecture fits and is popular; it feels fair.
Is social care the same as health? Or does it need a different architecture? Or indeed does it need any architecture at all? The NHS
Research is underway to review what a National Care Service would look like in practice. John Kennedy, a Consultant in adult social care, reviews the proposal and asks, should we be careful about what we wish for?
>
CMM October 2022 21
is fundamentally a science-led, evidence-based medical model of treating illness and disease. It’s like the nation’s mechanic. I take my car to the garage to be fixed and serviced – just like I take my body to the doctor if something is misfiring. The medics diagnose and tell me what they think the best fix will be, based on science and experience.
Generally speaking, if my ignition coil is shot, then I need a new ignition coil. If my arm is broken, I need it resetting and splinting. There may be a narrow set of treatment options but, fundamentally, there is not much scope for exercising my consumer choice and, arguably, neither should there be. It wouldn’t make much sense to be offered an amputation or to hear a medical professional say, ‘let’s see if it gets better on its own’!
That’s not how social care works. The same want or need can require very different solutions depending on a person’s individual situation, attitude to risk, relationships, life experience and neighbourhood. The social care sector should be as diverse in its offerings as the people it serves. We’ve endured too long with a well-meaning but fundamentally unresponsive architecture. Commissioner sovereignty has leant towards meeting the needs of commissioners and not the people drawing on social care – protecting budgets, narrowing choices and limiting progress. The models of care, design of services and customer choices have changed substantially little since my first shift as a care assistant in 1984.
Before we rush into a ‘silver bullet’ of an NCS, shouldn’t we first decide what we want social care to look, feel and taste like? Can we envision a future as proposed by Social Care Future: ‘Don’t we all want to live in the place we call home with the people and things that we love, in communities where we look out for one another, doing the things that matter to us?’
The crucial part of this is the ‘we’. What is good, what is wanted and what is demanded is defined by us, the people drawing on social care. What is decided by the person; us not them. This is the difference and this is the concern of an NCS – that it will decide, will limit choice and will continue to embed sclerosis. How will the aspiration of a ‘publicly owned, publicly funded, free at the point of use’ drive change?
Publicly owned. Why? There is not much evidence that publicly run necessarily has the intended effect on quality or efficiency. There have been just as many scandals and failures in the health service and publicly run social care. Isn’t it the attitude and ethos of those running services which can be lacking or wanting in public and private sector organisations? Shouldn’t we be ensuring that the fundamental engineering of the sector is fit for purpose, thereby maximising the chances of getting it right? What does publicly owned add to the quality, diversity and effectiveness of social care?
Publicly funded, free at the point of delivery: if it is free at the point of delivery, does that mean that my consumer sovereignty is stymied? Does this mean I need permission? Publicly funded, if realised in the same way as local authority commissioning, risks further disempowering of the consumer and inevitably leads to rationing and limited choices.
Surely what we want to encourage is a varied and diverse social care offering, where those who draw on social care are the key agents in the design and delivery of the services they draw on.
A single national health and social care workforce. Recruited and inducted, trained and developed, together, across the NHS and social care. A single pay spine. Shared values, the same competencies and skills. This would elevate the status and esteem of social care and improve the mutual understanding and ability to work together across
health and social care. It would also provide the public with confidence.
Of course, we are just about to create another addition to team quango in health and social care with the creation of the new Integrated Care Systems (ICS). Allegedly given the money and the power to bring the systems together in a coherent and effective way. Metaphorically to ‘knock heads together’. Where would a National Care Service fit into this already crowded superannuated room?
Instead of trying to ‘commission’ or ‘direct’ the system, why not instead put in place the engineering that allows this vision? Build into the system some key framework and levers – engineering, which allows the consumer to buy with confidence from organisations with the right values and a workforce that is skilled, competent and valued. Simplify the architecture and beef up the engineering.
MARKET REGULATION
For decades, we have quibbled over the true cost of care, with a multitude of reports from charities and consultants. If we standardise the workforce costs with a national workforce pay scale, then it’s not rocket science. It would be fairly easy to establish a minimum fee for care homes and a fair rate for homecare workers: to establish a ‘true rate for care’.
In many sectors, there is a market regulator – OfGem, OfWat, etc –which balances the Value for Money (VFM) for the consumer against the needs of organisations to achieve viability and invest in the future. Why not for the care sector? To ensure that, in return for a ‘fair price’, there is investment in quality and that excess profit is not taken. This could take the form of a market regulator, who is able to scrutinise providers and call out those sending ‘rent and consultancy fees’ to the Cayman Islands. We need market oversight that regulates fees and ensures charges and profits for care are within reasonable and defensible grounds. OfCare, anyone?
CONSUMER POWER
Sovereignty in the market needs to shift significantly into the hands of those who draw on services. Providers will then deal directly with customers and innovation and significant market segmentation will follow. All markets change if people demand more of one thing or indeed stop buying another. This mechanism for change is missing. The consumer, as in many markets, needs support in navigating but this needs to be a fundamental change from ‘assessment’ to ‘facilitation’ –it’s a power shift.
How we pay for it and who pays is a whole different question. But surely before we decide the how – publicly owned, publicly funded and free at the point of delivery – we should first decide what we want it to be? Then, we should look at the policy that will help to achieve that. We seem to be putting the cart before the horse.
We need a new system with solid engineering and little architecture. We need to look at the engineering of social care – what needs to be in place to widen choice, drive innovation and, crucially, empower and protect consumers. Let’s embrace a much more flexible, vibrant and fleet-of-foot social care sector. Yes, embed the fundamental engineering, workforce and market oversight but let the consumer drive the market, not the system. Otherwise, in the famous words of Henry Ford, ‘You can have any colour you want, as long as it’s black.’ CMM
What do you think about the proposed policy of a National Care Service? Should social care remain a separate entity to the NHS and should the manifesto be ditched? Visit www.caremanagementmatters.co.uk and share your feedback on the article.
John Kennedy is an Independent Consultant and Commentator in adult social care. John is the author, with Des Kelly OBE, of Power to People: Proposals to reboot social care in Northern Ireland (2017) and John Kennedy’s Care Home Enquiry (2014). Email: jpkennedy366@gmail.com Twitter: @JohnnyCosmos
22 CMM October 2022
PAINTING THE PICTURE OF A NATIONAL CARE SERVICE >











































• Available in 11 sizes, from 18mm-40mm (Ø) • Longer length – 130mm • Large buffer/comfort zone to prevent backflow and sheaths blowing off • Latex-FREE • Customise/remove excess length (scissors provided) • Perfect fit/size for all A bag for all seasons and occasions Short and strong. No more embarrassing leaks? • Specifically designed for wheelchair users • 700ml and 1300ml sizes • Shaped to the contours of the bended knee • Available in 9 sizes, from 18mm-35mm (Ø) • Shorter length – 75mm • Stronger adhesive • Buffer/comfort zone to prevent backflow and sheaths blowing off • Latex-FREE Bendi Bags • Traditionally shaped leg bag • 600ml and 1000ml sizes • 7cm shorter in length than many 750ml bags – no unsightly taps dangling Comfort Bags • Ideal for sun, sports and even some short clothing • 500ml capacity • Dress as YOU want, not to cover the leg bag Discreet Bags 11 sizes 9 sizes Urology products that make a difference Unique features and benefits often designed by end users. Available prescriptionon FREE HOME DELIVERY SERVICE Providing a personal service from a professional team. For your FREE information pack contact 0800 999 5596 or email prescriptions@manfredsauercare.co.uk For more information, please contact the helpline on: 01604 595 helpline@manfred-sauer.co.uk696 Or visit: www.manfred-sauer.co.uk




24 CMM October 2022 Call, email or click online to book your training needs today! T: 01622 766078 E: info@edify-consultancy.co.uk W: TrustedCAREEXPERTSwww.edify-consultancy.co.ukINTRAININGproviderstosomeof the largest care organisations in the UK… ... and the very smallest. Over 160 course options with face to face, virtual and online delivery options. Now is the time to go digital uk.autumn.care info@autumn.care 0800 009 2121 10 key reasons care providers are choosing to go digital, what will yours be? 10 KEY REASONSBOOK A DEMO Book a demo to find out how AutumnCare can help
ONE STEP CLOSER
TO REFORMING THE MENTAL HEALTH ACT
The Government has published a draft Mental Health Bill for pre-legislative scrutiny, to modernise the Mental Health Act for the 21st century. Andrew Parsons, a Mental Health Lawyer and Partner at Weightmans, shares the updates and explains how it could impact on people who draw on care.

The Mental Health Act 1983 (MHA) covers the assessment, treatment and rights of people with a mental health disorder. The Act provides the legal basis for authorising an individual’s detention and/or compulsory treatment when there is a risk they may harm themselves or others.
The Act provides a framework for people needing care for mental illness, either in the community or in hospital. It also contains separate guidance for those who are involved in criminal proceedings or are under sentence. The MHA ensures that individuals who are subject to the criminal justice system and have mental health needs can be treated, where necessary, in a hospital setting.
THE STORY SO FAR
Former Prime Minister Theresa May commissioned an independent review of the MHA, owing in part to reported growing social and cultural issues with the Act. At the time, the number of detentions under the MHA had increased by 40% between 2007 and 2016. This increase was affecting a disproportionate number of people from black and ethnic minority groups, with black people four times more likely than white people to be detained. It was also felt that some procedural aspects of the MHA were outdated and needed a fresh approach.
HEADLINE CHANGES
The draft Bill runs to some 77 pages. It retains the existing Act but inserts amendments in the same way as the last reforms, made in 2007. Accordingly, the broad structure of care under the MHA remains the same. However, there are some headline changes that practitioners must be aware of:
1. Changes to Community Treatment Orders
The Bill will tighten the use of Community Treatment Orders (CTO), including the requirement for an appointed community clinician. CTOs were a key part of the 2007 amendments to the MHA, but there is a view that they have been used too much.
Clause 19 of the Bill seeks to regulate its use through an amendment to s.17A of the MHA. Now, the community clinician responsible for overseeing the individual’s care will be involved in decisions regarding the use and operation of a CTO. It is hoped this will strengthen the link between the community and the responsible clinician, ensuring the patient continues to make positive progress. It is also hoped that it will better enable more informed decisions about the need to continue the restrictions in a CTO.
The driver behind these changes is the principle of using the least restrictive option and it has also prompted two further changes to the use of CTOs, detailed in Clause 20. Now, conditions of a CTO may only be imposed where they are ‘necessary’ – where previously they were required to be both ‘necessary and proportionate’. Further, the Bill grants the Tribunal a new power to ask a responsible clinician to consider whether a certain CTO condition is truly necessary, in cases where the patient has not yet been discharged from their CTO.
2. Autism and learning difficulties
The Independent Review published its report in December 2018 and made 154 recommendations for reform. The Government’s response to the review was published on 13th January 2021 and accepted the majority of those recommendations.
Following manifesto promises in 2017 and 2019, it was announced in the Queen’s Speech on 10th May 2022 that draft legislation would be introduced to reform the Mental Health Act 1983.
The stated purpose of the new draft Bill is to ensure that people living with mental health conditions have greater control over their treatment, and that they receive the dignity and respect they deserve. It will also work to improve the position of those with learning disabilities and autism and the handling of their discharge after being hospitalised.
PEOPLE FIRST
A core element of the Bill is finding ways to give people more control by putting them at the centre of decisions about their own care. As part of this, the Bill adopts four key principles, which are:
• Choice and autonomy, ensuring that people’s views and choices are respected.
• Advocating the least restrictive option, so that MHA powers are introduced gradually and only when necessary.
• Therapeutic benefit, ensuring people are supported to recover so that they can be discharged from the MHA.
• Ensuring that people drawing on mental health services are viewed and treated as individuals.
Under the current MHA, people with a learning disability can be detained for assessment and treatment under s2, and for treatment under s3, where this is associated with abnormally aggressive or seriously irresponsible conduct. This has led to some patients being subjected to lengthy detentions with apparently little therapeutic benefit.
The draft Bill therefore aims to make it clearer that, for the purposes of detention under the MHA, learning disabilities alone will not be sufficient. People with these conditions will only be able to be detained for treatment under the MHA, if it can be shown that they are suffering from a co-occurring mental disorder that is not a learning disability – often referred to as having a ‘dual diagnosis’. This also supports the principle of the least restrictive option.
A new section – 125A – has also been added into the draft Bill to cover the arrangement of care, education and treatment review meetings for children and adults with an Education, Health and Care Plan under the Children and Families Act 2014, who have been detained under the MHA. This is because NHS England has >
"An Integrated Care Board must try to ensure that the needs of people with a learning disability can be met without detaining them under the MHA"
"The stated purpose of the new draft Bill is to ensure that people living with mental health conditions have greater control over their treatment, and that they receive the dignity and respect they deserve"
26 CMM October 2022 ONE STEP CLOSER TO REFORMING THE MENTAL HEALTH ACT
>
Intelligently designed to comply with Doc M Building Regulations, our Sanitaryware range ensures users have inclusive access to, and can efficiently and safely use toileting facilities with as much dignity and ease as possible, a sentiment which reinforces our key values. Ten pack options are available, allowing you to make the right choice for the space available and the needs of the building’s Sanitarywareusers.Solutions

Call 01905 823274, email marketing@akw-ltd.co.uk or visit www.akw-ltd.co.uk/contact-us















Powerful insights & analytics tools to inform better decision making & improve outcomes Customisable & easy to use interface 24/7 Personalisedsupport care plans and timelines Used by over 2,500 care services across a wide variety of care types Your digital care management platform Supporting care services to go digital Find out more about how Nourish can benefit your care service by booking a free personalised demo: 023 8000 2288 | caring@nourishcare.co.uk | www.nourishcare.co.uk "Nourish was a game changer for our company. Nourish has enabled us to really improve our patient care and evidence the great work the team does." Sarah Beaumont, Associated Wellbeing Integrates with eMAR, pain management apps & GP Connect Meet us at the Care Show on Stand H82 at the NEC, Birmingham on 12th & 13th October
CMM October 2022 27
> previously issued guidance on holding reviews in these areas to help reduce unnecessarily long stays in hospital. There was a particular focus on assessing whether a person with learning disabilities is safe and receiving the right care and treatment in hospital. However, it was found that recommendations from the reviews were not always enacted and there was often no follow-up process.
Finally, a new part – Section 125E – sets out that Integrated Care Boards (ICB) and local authorities will also need to consider risk registers and the needs of the local ‘at risk’ population when carrying out commissioning duties. The clause aims to ensure that the right community provisions are in place for people with a learning disability, so that they are not admitted into in-patient units unnecessarily.
An ICB must try to ensure that the needs of people with a learning disability can be met without detaining them under the MHA. The ICB must also ensure that an individual’s unique needs are at the heart of any decision making.
3. Detention criteria
The long-standing criteria for detention under sections 2, 3 and 5 of the MHA (and for renewal of detention) are amended to add two new tests. Firstly, that ‘serious harm may be caused to the health and safety of the patient or of another person’. Secondly, those assessing whether the individual meets those criteria must consider the nature, degree and likelihood of the harm and how soon it would occur. The same changes to the criteria apply to CTOs and discharge by the tribunal.
4. Nearest relative
Concern has been raised for some time regarding the MHA approach of selecting a patient’s representative by reference to an established
list of suitable individuals within the legislation. The Bill proposes to change this and instead allow patients to select their own representative, to be known as the Nominated Person, to replace the nearest relative. If the individual lacks the mental capacity to do this at the point of detention and has not previously nominated an individual, then an Approved Mental Health Professional (AMHP) may appoint someone instead.
5. Care Plans and the definition of ‘medical treatment’
Where appropriate, the draft Bill requires clinicians to prepare personalised care and treatment plans for certain people detained under the MHA. These plans must be kept under regular review. The Bill also includes provisions as to how these plans will be monitored, imposing requirements on the managers of a hospital to do this.
The Bill also amends the definition of ‘appropriate medical treatment’ to require that, when considering whether treatment under the MHA is appropriate for a patient, there is a reasonable prospect that this would have a therapeutic benefit for that patient.
WATCH THIS SPACE
This is by no means an exhaustive summary of all the new provisions in the Bill. There are clearly many other areas of change on the horizon, with those outlined above being some of the most significant. This will require health and social care providers to introduce new processes, update policies and deliver staff training to ensure success and compliance with the amended mental health legislation. Further, the thrust of the changes would suggest that the use of the MHA will be reduced, which may impact on social care providers when they need to refer residents to psychiatric services for alternative provision.
CMM
 Do you think the proposed changes to the Bill go far enough? And what are your current concerns surrounding the Mental Health Act? Visit www.caremanagementmatters.co.uk and share your feedback on the article.
Andrew Parsons is Partner at Weightmans. Email: andrew.parsons@weightmans.com
Twitter: @Weightmans
Do you think the proposed changes to the Bill go far enough? And what are your current concerns surrounding the Mental Health Act? Visit www.caremanagementmatters.co.uk and share your feedback on the article.
Andrew Parsons is Partner at Weightmans. Email: andrew.parsons@weightmans.com
Twitter: @Weightmans
28 CMM October 2022 ONE STEP CLOSER TO REFORMING THE MENTAL HEALTH ACT

The free online CQC confidence course from It only takes one hour to complete Register for the free online course Join over 100 learners
INTO PERSPECTIVE
AGE OF AGEISM
Recent research conducted by McCarthy Stone, based on a poll of 5,000 adults and interviews with later life experts and older people, revealed that 43% of people under 65 fear they’ll be regarded as frail and somehow less important in older age, yet more than half (51%) of over 65s say they actually feel more confident and resilient in later life. This indicates a significant misrepresentation amongst the public of what later life will really be like. Such attitudes towards ageing will only perpetuate existing negative stereotypes associated with older people and the wider adult social care sector. While ageism is typically discussed in relation to the experiences of older people, younger people report more perceived age discrimination than other age groups, and the main contributing factors towards ageism against younger people include health status and care dependence, according to the World Health Organisation’s (WHO) global report on ageism.
A PROVIDER’S ROLE
In a Department of Health and Social Care blog post, Dr Mervyn Eastman argues that social care providers may fall into the trap of using language and adopting behaviours that cater to the successful operation of the organization, at the expense of positive individual outcomes for older people receiving care. This could include conducting assessments and/or managing resources based on stereotyped assumptions of what it means to be an older adult. Guidance published by the Social Care Institute for Excellence argues that strong leadership at all levels of adult social care provision is
required to overcome ageism. For example, providers should engage people using services and their families to shape future support. Those in leadership roles should also set the standard for the rest of the organisation. This could be achieved through a number of channels, including training, expectations and supervision to recognise and tackle ageism and creating a culture that supports equality and challenges discrimination, the guidance summarises.
RELATIONSHIPSBUILDING
Neil Gandecha, Estate Manager at Foxholes Care Home, understands that providers who facilitate intergenerational interactions between younger and older people can create mutually beneficial relationships that address age segregation. At Foxholes, they organise activities such as pen pal projects, creating the opportunity for connections to be made and negative stereotypes to be quashed.
A recent report launched by the Agile Ageing Alliance, with support from Clarion Housing Group, is urging the housing sector to create more inventive and inclusive spaces or Smart NeighbourhoodsMultigenerational(SMNs)for ageinclusive relationships to blossom. The report states that SMN’s should include public spaces, with plenty of rest stops, to facilitate engagement across all generations and that this familiarity will also serve to combat ageism.
On a smaller scale, providers such as intergenerationallocalsuccessfullyWestgateHertfordshire-basedHealthcarehaveconnectedwithschoolstoencouragerelationships and break down ageist assumptions.
HOW CAN SOCIAL CARE PROVIDERS HELP TO TACKLE AGEISM? attitudes towards adults, both younger and older, will continue to damage public perception of adult social care unless those who serve the sector play their part in tackling the issue. Ageism threatens the sector’s core objective to empower people to live the lives they choose to lead, free from prejudice. While providers are working tirelessly to achieve successful outcomes for people in their care, they must forge a path for others to follow in the effort to eradicate ageism in the sector.
30 CMM October 2022
Ageist
Changing the narrative
Jess Kuehne, Senior Programme Manager for Ageism, Centre for Ageing Better @jesskue


Much of the general public assumes that older age is inevitably linked to vulnerability, dependency and decline. This is despite the fact that many older people continue to be active and participate in and contribute to workplaces, communities and society in many different ways.
So where does this portrayal come from? Research from the Centre for Ageing Better found that despite different language used by different sectors –covering national Government, news, social media, charities and more – many of their narratives draw on similar stereotypes.
When we looked at language used by health and social care organisations, we found much of the language focuses on death and physical decline. Ageing is talked about as a process of increasingly bad health, and older people are commonly portrayed as frail, vulnerable and dependent.
This means that health and social care organisations, along with other sectors, are contributing to a narrative from which the general public naturally adopts language and frames when talking about ageing.
You may ask why this kind
of language matters. It matters because language influences attitudes and behaviours. Stereotypes and ageist language can result in a lack of respect for older people and can lower the quality of care they receive. It can also result in individuals internalising these stereotypes and subsequently behaving in a manner in which they have been told a stereotypical older person behaves.TheCentre for Ageing Better has produced a guide to help give people the confidence to challenge ageism and champion positive and realistic representations of ageing and later life. The guide is designed as a practical tool to support organisations in communicating about ageing and older age. We have also just released a new collection of photos for our age-positive image library highlighting older carers and we hope that social care providers will join us in promoting thisIftool.weall make these small changes, we can make a big impact on how we view ageing, and the way older people are valued across society.
It’s time to tell a new story.
Passive, unheard and unseen
Tom Owen, Director, My Home Life England @MyHomeLifeUK

Ageism is so embedded in our culture it is often invisible to us. It affects young as well as older people. It is engrained within our policies, our behaviours and ourOlderattitudes.people typically have poorer access to treatments for common health conditions; care assessments/plans are less likely to focus on what older people wish to achieve in their lives compared to youngerAgeismpeople.functions to block out the reality of what is to come for us all as the clock ticks forward. It therefore makes us more likely to use words that treat older people as objects – the elderly – and in care settings (‘feeders’, ‘toileting’ or ‘doubles’). We may adopt ‘elderspeak’ rather than communicating adult to adult. We may disregard the views of older people about how they are coping at home and what they need in favour of the perspective of a son or daughter or other professional.Wegenerally want to wrap older people in cotton wool, so that they are passive and out of mind. We are therefore disapproving of any dangerous activity that they might wish to do. It’s ironic that, as a society, we more readily allow teenagers to take high risks, despite
the fact they have so many more years to lose compared to a person in their last few years of life.
At My Home Life England, we witness and support so many great leaders working in care homes, domiciliary care and other care settings who support their teams to reflect on practice and to consider how it might feel to be you, but just older and in need of care and support. Some use ‘language posters’ to record the words that should (and shouldn’t) be adopted within the care home. Many have accessed a variety of tools from My Home Life and other places to enable the views of those living in care homes to be heard. Sometimes the act of simply giving space for older people to communicate about how they feel can be both empowering for the older person and transformational in terms of reducing an institutionally ageist culture.
Ageism will creep up on all of us. It will chip away at our confidence and sense of competence until we begin to start acting as society wants us to: passive, unheard and unseen. We celebrate all of those social care practitioners who honour the voices of older people, amplifying their voices and working tirelessly to challenge ageism that surrounds us all.
31
• Governance documents • Audit Tools • Dependency Tool • Clinical Policies & Procedures • FREE Downloads • Risk Assessment Templates • PRN Protocols E-Document Shop Now OPEN!







32 CMM October 2022 Utilising AI and smart automation to transform pain management in your care home. Over 1 million globallyassessmentspaincompletedusingPainChek®! PainChek ® accurately and safely assesses pain for people living with dementia, or other cognitive impairment, who cannot reliably self-report their pain. PainChek ® combines smart automation and AI to provide care teams with fast, accurate and reliable pain assessments- ensuring no pain goes undetected and untreated. For more information, visit www.painchek.com/uk/ or call 0333 577 3397 Care Management System Providing the intelligent software solution for care home and domiciliary care. Included in the suite: Care and Support, our care planning platform. Policies and Procedures. Quality Assurance, our audit and inspection records app. Supervision and appraisal records. Mandatory Training (with Matrix) and Care Certi cate. Providing Expert Health & Social Care Consultancy Services Further Information www.carequalitysolutions.co.uk Email: support@carequalitysolutions.co.uk We Can Help With: • Undertaking Mock CQC inspections reporting and development of action plans • Satisfaction surveys or ‘mystery shopper’ reviews • Review of Care Quality & Governance systems • Supporting preparation for regulatory inspections and monitoring visits • Undertaking a wide range of audits • New business startups and preparing to register for the first time • Changes to your registration • Providing management support and oversight
THE CARE INNOVATION CHALLENGE


CMM MEETS THE FINALISTS
The National Care Forum (NCF) Care Innovation Challenge, a hackathonstyle creative weekend, returned on 2nd-3rd July 2022. CMM’s Olivia Hubbard caught up with the finalists to find out more about their innovations. To conclude our interviews, we were delighted to speak to Team Fall Free, Team Star and Team Care Tech Guide.
Creative thinkers, entrepreneurs and experts from the sector, including people with lived experience, came together at Coventry University’s Technopark for two days of idea generation and prototype trialling. Five finalist teams were selected to present their ideas at The Care Show, the largest care event in the UK, on 12th-13th October at the NEC in Birmingham. Good luck to the finalists: Team Care Tech Guide, Team Chip, Team Fall Free, Team Myghty and Team Star. The winning team will receive £1,000 in prize money, media coverage and mentoring to develop their idea.
INTRODUCING TEAM FALL FREE
Team members Ethan Booth and Mutong Li are both studying an M.Sc in Applied Infectious Diseases
Epidemiology at University College London (UCL) and are mid-way through their dissertations. I applaud Mutong’s commitment to join the call – he apologies for the slight signal break up, whilst
Left to right: Mutong Li, Ethan Booth, Kourosh Simpkins
>
CMM October 2022 33
he navigates his way around a train station in Hong Kong. Kourosh Simpkins is studying a B.Sc in creative computing. I can see why the judges said they loved the team’s charisma! They can’t stop smiling and despite being thousands of miles apart at that very moment, they were very much in sync with one another.
CMM: So, what brought you to the Care Innovation challenge?
Team Fall Free (Ethan): It’s a funny story because we came to the forum with a different idea – which was a software to assist researchers with literary review. We then discovered that the care forum wasn’t related to what we were trying to pitch, so we had to come up with a different idea on the spot!
We thought about our skills and strong statistical backgrounds and how certain health concerns/diseases can be predicted. Our mentors, Meiling Huang of RWK Goodman and Atholl Craigmyle of Hilton Nursing Partners suggested that we explore fractures.
CMM: What is your idea in a
Teamnutshell?Fall
Free (Kourosh): We are trying to develop software that uses your medical information, such as your age, gender and BMI, to predict your risk of fractures in the next three months. The technology would also aim to assess your risk of having a fracture and would make thatrecommendationspersonaltoreducerisk.
CMM: Who is your target Teamaudience?Fall
Free (Ethan): We would target two groups of clients; families and individual people and health and care organisations who work directly with people, such as care homes. We are building an app, which is connected to the database, for family members


to use. There will be one centralised database. Social care organisations will have access to a web interface – just like an excel spreadsheet.
CMM: What market research did you Teamdo?Fall
Free (Ethan): I spoke to my dad – he’s 75 years old – to get his thoughts. We also considered how it might work for carers, such as an unpaid carer caring for an older relative. There is potential to look at a chat function, where you can be put in touch with a GP. We could also reach out to some of the companies who are doing this and try to form a partnership.
CMM: Have you explored your competitors in the space?
Team Fall Free (Ethan): We are familiar with Xantura – I believe they collect data from individuals to estimate a risk of hospital admissions for all causes. Our unique selling point would be our specialism for estimating fracture risk, and providing personalised recommendations, essentially an orthopaedist in a pocket, if you will.
CMM: Have you considered the finances of the app?
Team Fall Free (Kourosh): We are thinking of charging £8.33 per month as a subscription. It would be cheaper for care homes due to the higher volume of clients. The main hurdle is that it’s an app, so we need to pay for technology monthly. The days of free apps are long gone. As more people sign up, we may be able to lower the price.
CMM: How would you describe the Care Innovation weekend?
Team Fall Free (Mutong): The judges said they really liked our charisma! The mentors really liked how we worked together as a team. It was a new experience for us, it was fantastic. It was worth it!
INTRODUCING TEAM STAR
Tracey Wakeling is Registered Manager of two Green Square Accord extra care schemes in Coventry. One is for people with dementia and the other is for people with mental health and learning disabilities. Claire Dineen is the Deputy Manager at Green Square Accord’s Arden Grove and has been working in care for 26 years. They both started in the care sector as care workers. Tracey and Claire united with Lizzi Jordan – an engagement and inclusion officer at Surrey Choices – at the Care Innovation weekend.
CMM: What’s your innovation Teamidea?
Star (Tracey): We are offering the idea of local reablement and assessments with housing for people living with dementia. Not enough people with dementia get accepted into reablement. People think that reablement is something we have all over the country, but we aren’t actually meeting people’s needs. Although we are focusing on people with dementia initially, this is something that can be rolled out to other areas, such as learning disabilities; it could have many different models under it.
CMM: What’s your plan to progress the project?
Team Star (Tracey): We are looking at doing a six-week pilot programme, where people
can come and work with the staff at Arden Grove, to see if we can work with these people to get them to a stage where they can remain in extra care and avoid going into residential care. The staff will be upskilled via a programme which isn’t currently used in extra care called RESTORE 2; staff will be trained to take oxygen levels, blood pressure, to do sugar testing and urine testing. This will help staff to identify early signs of deterioration.
CMM: What’s the evidence for the Teamneed?Star
(Tracey): According to Coventry City Council, over the last six months, 36.9% of people have moved into residential care unnecessarily. Our programme is not going to be the solution for everyone, but it will give people the opportunity to meet the needs of people needing care.
CMM: Who would benefit from the service in particular?
Team Star (Tracey): The dementia and mental health managers are saying that there are so many more people coming through now with Korsakoff’s syndrome, also known as independentlydownindependent.towithalcoholcommonlytypesyndrome’,‘Wernicke-Korsakoffanon-progressiveofdementiawhichismostcausedbychronicabuse.However,peopleKorsakoffcancomebackthestageofbeingquiteWithsomework,theline,peoplecanliveagain.Thereis
 Left to right: Claire Dineen, Tracey Wakeling, Lizzi Jordan
Left to right: Claire Dineen, Tracey Wakeling, Lizzi Jordan
34 CMM October 2022 THE CARE INNOVATION CHALLENGE: CMM MEETS THE FINALISTS
>
>



no risk of bed blocking, they already have their place, then they move on.
CMM: Who has supported you with the project?
Team Star (Tracey): There is obviously interest; the managers of mental health and dementia said they have been crying out for something like this for ages to come into the system. The reablement brokerage team are saying that it makes them so happy because this is something that we don’t have. Professor Vic Rayner OBE and Professor Martin Green OBE were both very supportive and we have had meetings with them. I spoke to Coventry City Council and it's something that they are excited about. I also spoke to the manager of Dementia and Mental Health in Coventry, and he said this is something that’s really needed.
CMM: Lizzi, what prompted you to join forces with Claire and
TeamTracey?Star
(Lizzi): I think Tracey and Claire’s approach is to have people’s best interests at heart, which was really refreshing. Tracey and Claire have so much experience in the sector and lived experience and they have noticed that gap in the market. Sometimes the best ideas come from people with the best experience.
CMM: Have you been surprised about how quickly the project is
Teamdeveloping?Star(Tracey):
We started off with an idea, but we have learned so much along the way – through people we have met, meetings we have had. Things have really surprised us. It’s going to be of benefit to staff because they are going to have extra skills, so hopefully it will have a good impact on the workforce. It’s a winner all round really.
INTRODUCING TEAM CARE TECH GUIDE
Liam Palmer runs five care homes in Gloucestershire and has been working on his innovation project for a few years. He tells me he was a bit reluctant to attend at first because he didn’t want people to think Care Tech Guide were pretenders! After a conversation with Professor Vic Rayner OBE, any anxieties quickly subsided.

CMM: Liam, tell us about your background to working in care.
Team Care Tech Guide (Liam): In 2018, I did my Level Five diploma in social care. I was running an 80-bed care service at the time. It was all paper based and one of the residents lost half a stone over a two-week period and it got missed because of the crossover of staff. I worked in logistics before care and I thought, surely there could be a system that could give you an alert?
I did my final project for my Level Five on researching planning systems for care. I found that there were some very specific gaps in the market for social care. I thought if I was going to do something here then we need to determine what’s good technology. So, we started with defining standards for tech. I partnered with a research care company and my co-founder, Louie Werth, who is doing his
PHD at Cambridge in Research, because I needed someone to cover the information data part.
He then said in a moment of clarity that we should do something like Money Supermarket for care technology. We should make it simple and accessible. We put our efforts into developing something that was a hybrid between a Which? guide, Money Supermarket and Google. We know those ideas work. The significant thing was to take ‘Tech for Care’ and put a boundary around it to show that it warrants attention. The potential is huge –social care is enormous.
CMM: How does the software Carework?Tech
Guide (Liam): We are helping people to draw up a shortlist of technology they might want to use. We will share articles to offer users some inspiration or, if a user has a clear idea of what they want, we will signpost accordingly. It’s going to be about education – we aren’t going to do a ‘which is best’.
CMM: What would be your overall vision and goal for the Carefuture?Tech
Guide (Liam): We would like to get embedded into the various ecosystems within social care. Whether we are a finalist or a winner, NCF can say that this came through us.

We are part of this movement and doing this with all the key players. Hopefully, it will be a benefit for many parties.
CMM: How would you describe your overall experience of the Care Innovation weekend?
Care Tech Guide (Liam):
It was exhausting! It was really intense. It was a very well-structured process and there were mentors all over the place, dropping in. I had never done anything like that before. It was a really uplifting environment. I think the mentors helped with collaboration and we were all working to bring concepts to life – it wasn’t competitive. We are honoured to get into these finals, we support all the other finalists and it’s about the good of the sector. I’ve heard the final is going to be a bit Britain’s Got Talent with Chief Executives of care providers judging! I’m going to demo/present a well-developed solution and we will rest on that – not personality or charm – youth is obviously not on my side! Let the best group win!
CMM: Have you considered how the project will work Carecommercially?TechGuide (Liam):
Suppliers will pay for it as a form of marketing and there will be add-ons. My first research was with 70 suppliers, and I have contacted every single one. In terms of route to market, we are thinking of putting everyone up there and doing it for free initially. You have to register as a care provider to access it.
People could try and copy this idea and do a basic listing service but there is so much thought that’s been put into this. We work with key organisations; we are hoping that our standing in the social care community protects us.
CMM
Visit www.caremanagementmatters.co.uk to read an extended version of the interviews. For more information about the Care Innovation weekend, visit https://careinnovationhub.org.uk/ To contact Team Fall Free, email fallfree.cih@gmail.com To contact Team Star, email tracey.wakeling@greensquaredaccord.co.uk To contact Care Tech Guide, email liam@carehomeleadership.org
Left to right: Liam Palmer, Professor Vic Rayner OBE
36 CMM October 2022 THE CARE INNOVATION CHALLENGE: CMM MEETS THE FINALISTS
>









CMM October 2022 37 > THE CARE HOME BROKERAGE PROFESSIONALS If you are looking to sell your trading or closed care home, contact our Managing Director, Nick Greaves on 07943 107 887 or nick@ngacare.co.uk The Leys Northamptonshire Brookside Court Leicester Woodlands Derbyshire LD Portfolio Midlands The Chestnuts Kent Groby Lodge Central The Lodge Leicestershire ViewKingsthorpe PurposeCare46Nottinghambedroomshomewithnursingbuilt Hazelford Nottinghamshire

BRIGHT IDEAS: Rethinking tenure in housing with care BRIGHT IDEAS:
The need for new ideas in social care leasing arrangements has become evident in recent years. The pandemic has focused attention on housing with care, where older people can enjoy self-contained accommodation with communal facilities but also access the support and care that they need. Meanwhile, ongoing leasehold reform is impacting on the way property is held in England and Wales. At ARCO, we are proposing a set of reforms to better protect consumers and to allow the sector to grow, which we call Leasehold Plus. We’re also aware of developments in rental and new ideas for care homes which could give better security to residents.
CURRENT ARRANGEMENTS
The current arrangements in England and Wales (Scotland has a different system of property law) are broadly as follows. Housing with care properties, or Integrated Retirement Communities (IRCs), are either for sale as leasehold property, for rent, or for shared ownership.
The for-sale market is dominated by mid-market and luxury providers. Property is sold on a long lease (125 – 999 years) for the payment of a premium (purchase price) in the same way as an ordinary flat in the general property market. In a traditional leasehold set-up, the customer pays the purchase price, and then pays a variable service charge which is subject to landlord and tenant legislation and covers the landlord’s costs of services, repairs, maintenance, improvements, insurance and management. When the resident moves out, they sell on the lease as it stands to a new purchaser, who pays them the purchase price and then takes over the obligations of the lease, including the payment of service charges and any ground rent to the landlord.
THE CASE FOR REFORM
IRCs combine age-appropriate housing with communal facilities (restaurant, leisure facilities, grounds, etc), an active social programme, and care and support for those who need it. Care, if needed, is paid for under a separate contract. IRC operators are long-term service providers to their residents. Their business model is very different from that of an ordinary residential property developer whose priority is to build and sell new properties and then move on to the next scheme.
The current leasehold model – what we might call ‘legacy leasehold’ – is not ideally suited to Integrated Retirement Communities. Leasehold is an ancient form of holding property which featured strongly in the feudal system and where some legislation dates back to 1709!
We recently surveyed 4,000 older consumers across the UK and asked them about downsizing/moving to specialist housing and what factors would influence their choice. The responses confirmed our view that older customers are worried about high or unpredictable service charges or other regular costs. 90% said that they would be concerned that ongoing monthly charges would keep getting more expensive, and 63% were worried about expensive unexpected bills.
Many IRCs have adapted their leaseholds, where possible, to offer customers the choices that they want. They insulate their customers from the risks of rises in costs or the need for major works by capping, indexing or fixing service and management charges. This ‘fixed service charge’ model is popular with consumers and allows them to plan effectively for their retirement. The IRC model is also not dependent on ground rent, with many operators instead using event fees which are charged on the sale or assignment of the lease. ARCO
How people own and occupy property in care homes and housing with care has seemed relatively straightforward up until now, but new developments at home and abroad have created an impetus for reform. Sally Ireland, Director of Legal and Compliance at Associated Retirement Community Operators (ARCO), explores possible reforms.
BRIGHT IDEAS: RETHINKING TENURE IN HOUSING WITH CARE
CMM October 2022 39
>
As experienced Care Home practitioners we provide training to teams in sustainable innovation and leadership, to embed companionship, partnership working and wellbeing designed to build enriched quality of life into care homes.
Developing a culture of care with wellbeing, positive relationships and inclusion at its heart, in a 6 x 1hr per week online training programme.


Develop how to address loneliness, helplessness and boredom with companionship, partnerships and meaningful quality of life. and join the care evolution



UK
An inspiring care model enhancing retention & wellbeing Contact us today
Call today on 01626 868192 • 07483 359471 or visit www.eden-alternative.co.uk IntegrationsReporting and Analytics Daily Customer CareCare Work Management Are you looking for a Digital Rostering and Scheduling System? Real-Time Care™ brings more time for the actual care work Fastroi Ltd | www.fastroi.com | sales@fastroi.com Real-Time Care™ (RTC™) is a comprehensive software package for reablement and home care services which helps provide the best quality care and meets the high requirements of care services. RTC™ delivers efficient processes, notable cost savings and reliable capacity checking by digitising processes and daily routines.
supported the Leasehold Reform (Ground Rent) Act 2022 which prohibits the charging of ground rent in new residential long leases.
Jamie Bunce, Chief Executive at Inspired Villages, said, ‘We recognise that our customers want cost certainty to give them peace of mind in their retirement, so we’ve got a range of measures in place to support that. The service charge at all our new schemes will be linked to the Consumer Price Index and the Earnings Index, which removes the likelihood of shock increases due to things such as an increase in village centre utility costs, and we are in the process of introducing this to our first six villages. Our event fee similarly protects residents from unexpected long-term maintenance costs for the village and means we can improve the resale value of their property. As a business, we had also already taken the decision to remove ground rent from leases for all our new villages before the Leasehold Reform (Ground Rent) Act 2022 came
However,in.’
there are some changes which are not possible within the current leasehold framework. Placing the burden of resale on the consumer (or their family if they have passed away) causes stress to families at a difficult time and also means that new incoming residents are not fully protected by UK consumer law, because the transaction is not trader to consumer. The risks of mis-selling increase. While operators could buy back the property from the consumer, this is rare outside of the charity sector because of the impact of Stamp Duty (SDLT). In addition, the model that many IRCs use (fixed service charges plus event fees) does not have any specific regulation in UK law. ARCO fills the gap through its Standards programme for operators who are our members, but more legal certainty would increase consumer confidence and help the sector to grow to fulfil its potential.
A NEW MODEL FOR IRCS
With this in mind, we are proposing a modified form of leasehold – Leasehold Plus – specific to the IRC sector. This would allow operators to buy back the property and re-sell it to a new buyer – with Stamp Duty payable by the new buyer but not by the operator. The operator could choose to buy back before a new buyer is found – perhaps to refurbish the property – but would only be required to do so once a new buyer had been found and a three-way transaction could take place. In each case, a new lease would be granted, so the problems
of selling on inflexible long leases would fall away, since terms could be modified each time to suit the incoming purchaser.
The new buyer would be fully protected by UK consumer law and the operator would retain control over the marketing of the property and could ensure that the new customer had all relevant information before purchasing. The new system of Leasehold Plus would be accompanied by regulation of event fees and fixed service charges, with sectorspecific regulation in a statutory Code of Practice to protect consumers and provide the legal certainty which would allow the sector to grow.ARCO Strategic Partner, Trowers & Hamlins, has researched the proposition and the legal changes required. Partner Kyle Holling said, ‘We at Trowers have said for some time now that the key to better regulation of the IRC sector is striking the right balance between protecting the customer and encouraging investment in and the growth of quality operators. The Leasehold Plus model has the potential to achieve this, acting as an initial step towards sector-specific regulation in a way that can be progressed quickly for the benefit of all.’
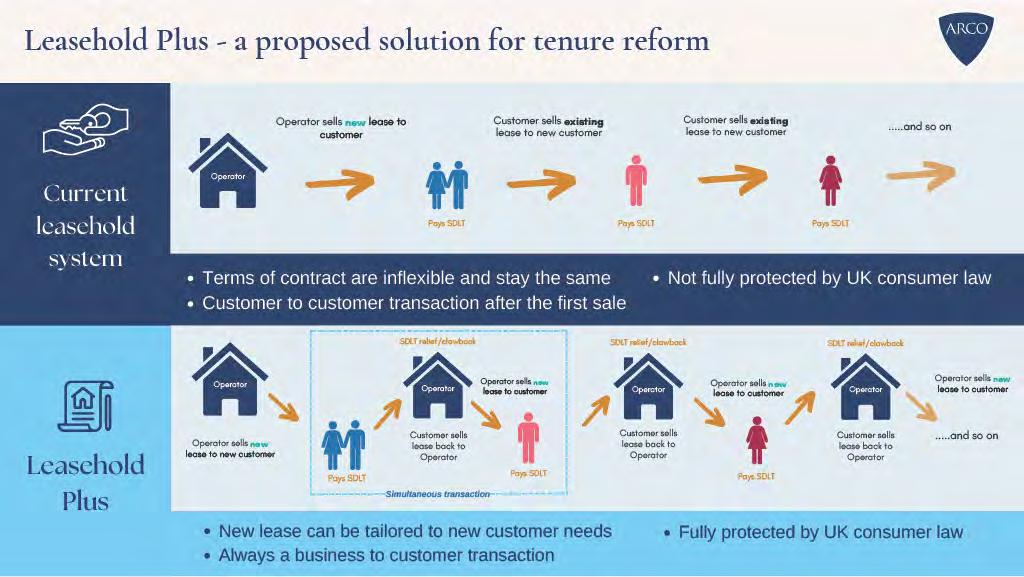
WIDER SECTOR
This system – based on property ownership – would work well for IRCs. However, what of care homes or assisted living apartments (typically rented apartments where older people with higher care needs can receive care)? Some IRC operators offer the more
‘independent living’ IRC apartments, assisted living rental apartments, and a care home or care home with nursing on a single site. The assisted living option is very popular with older people with a higher level of care needs who may want an alternative to a care home. These apartments are well suited to rental, but some IRC operators are currently considering options for customers who want to invest the proceeds of a property sale as a capital deposit rather than paying a monthly or annual rent; so further legal changes may be required.Somecare home operators are also looking to diversify either into the IRC model or assisted living. One issue here is that to provide security of tenure, the resident must be free to choose their own care provider if, for example, they are unhappy with the service provided by the in-house care company, or it cannot meet their needs.
LOOKING TO THE FUTURE
Both the pandemic and scandals elsewhere in the leasehold property sector have rightly focused attention on the rights of residents in specialist housing and care provision. We hope that through legal reform – including through the Older People’s Housing Task Force – we can offer more choice and better protection to older people so that they can enjoy later life while accessing the care and support that theyARCO’sneed. vision is for 250,000 older people to be able to live in an IRC by 2030. Leasehold Plus would help to make this a reality. CMM
CMM October 2022 41 BRIGHT IDEAS: RETHINKING TENURE IN HOUSING WITH CARE
What do you think of ARCO’s proposals for Leasehold Plus? How could this impact on the wider sector? Share your thoughts and feedback on the CMM website, www.caremanagementmatters.co.uk Sally Ireland is Director of Legal and Compliance at ARCO. Email: info@arcouk.org Twitter: @ARCOtweets >

































































































42 CMM October 2022 JOIN THE CONVERSATION USING OUR HASHTAG #CARESHOW FIND US ON: " @CARESHOW ! @CARESHOWS ' /CARE-SHOW Building a better future for care 13-14 October 2021 NEC Birmingham leading care suppliers expert care speakers CPD accredited conference sessions theatres200+150+110+6 ORGANISED BYCERTIFIED BY GET YOUR FREE CELEBRATINGREGISTER12-13WWW.CARESHOW.CO.UK/TICKETSTICKETNECBIRMINGHAMOCTOBER2022FORTHECARESHOWCARE...
Working together: Integrated care boards
This year has seen a significant shift in the way the sector works in collaboration with wider health organisations and the community. Under the Health and Care Act 2022, 42 integrated care boards (ICBs) were established on 1st July 2022, replacing clinical commissioning groups (CCGs). Each ICB has a constitution setting out the Board membership and governance arrangements for the organisation. As required by the Act, clinical commissioning groups (CCGs) worked with designated ICB leaders, to engage with key local stakeholders to develop their Previously,constitutions.theclinicalcommissioning group (CCG) in County Durham matched the local authority boundaries which certainly helped with integration. Following the change on 1st July 2022, the Integrated Care Board for the North East and North Cumbria (NENC) assumed commissioning responsibilities. The NENC area covers 13 local authorities from the border with Scotland to Staithes – a distance of 133 miles. It includes rural areas, cities and some areas with stubborn health inequalities. This was a major shift in commissioning and presented all partners with the dilemma of how to keep a local, place-based focus and work at scale. However, by working together in County Durham, we are moving towards a solution that is based on our strong track record.
COUNTY DURHAM CARE PARTNERSHIP






Here in Durham, we have been working at integration for a good 10 years. Most colleagues know each other really well and solve problems together every day. Our integrated model is the County Durham Care Partnership, which brings together NHS and social care organisations such as County Durham and Darlington Foundation Trust, our Integrated Care Board Durham County Council and other health and care providers in a true collaboration. This united approach has helped to drive our ambition to further develop system-wide integrated models of care.

Michael Laing, Director of Integrated Community Services, and Sarah Burns, Joint Head of Integrated Strategic Commissioning, share a perspective from the County Durham Care Partnership about integrated working.
CMM October 2022 43
>
Our vision is about putting people at the centre of everything we do, moving away from a hospital-based model of care to a new way of working, based on collaboration and partnership. We want to provide more care in people's homes and their community and, at the same time, break down barriers between services. This means joining up the work of general practices, community services and hospitals to meet the needs of people requiring care and finding new, more efficient ways of supporting people. This could be population-based prevention initiatives or developing provision for very complex health or care services.
Of course, this is never as simple as it sounds. Different financial regimes, workforce terms and conditions, national targets and policies make operational integration a real challenge. One simple but important example is paying for care. NHS services are free at the point of use and based on clinical need. Social care is charged for depending on savings, income and eligibility criteria.
In County Durham we have formed Teams Around the Patient (TAPs) which are made up of social workers, GPs and their teams and NHS Community Services Teams. There are three different sets of pay scales, pension arrangements and holiday entitlements, some of them set Whatnationally.wehave done in County Durham is recognise these differences but focus on improving customer experience through streamlining pathways together. We have concentrated on what we can change rather than what we can’t, including shared IT systems with GPs, co-location, joint senior managerial posts and shared points of access.
REGIONAL OPPORTUNITY
Although the NENC Integrated Care Board is huge, it realised the importance of working at place. The Board has committed senior staff resources to work at a place-based level and takes an active role in place-based partnerships. The Board has committed to co-producing a Joint Committee for Health and Care in County Durham and we are working on this together.
The Integrated Care Board has been in place for less than 100 days. It is in a period of transition but is moving at pace to work out what should be done at scale and what should be done at place. We already arrange many services at scale. Highly specialist cancer care, cardiology, mental health and children’s care are some examples.
We also know that working across this large geography means that one size doesn’t fit all. Ideas can be developed at scale, but they need to be tailored for local implementation. In a place as large as County Durham, we often have to tailor services within our county to work for our local communities as it is so diverse. The partners in The County Durham Care Partnership recognise that, too. Many of them work across larger geographies and have learnt how to gain efficiencies of working at scale, but also how to be part of very local teams.
The change to the Integrated Care Board means we can work at scale. We must not forget that most care is delivered in people’s homes and communities. It is a huge privilege to work in the newly developing Integrated Care Board and to see recognition of the importance of placebased care, but most importantly, to work for both health and social care.
SUCCESSFUL WORKING
In health and care, we are surrounded by colleagues who want to do their
best for people, push boundaries and make a change. Turning good ideas into a reality can, however, be a challenge due to either the different processes and procedures in place at different organisations or the availability of funding.
There has been a logical way to address this in Durham; we created roles that span organisations. For example, I am employed by Durham County Council and the North East and North Cumbria Integrated Care Board and I work in a commissioning role. In my role as the Joint Head of Integrated Strategic Commissioning, I feel equally accountable for the success of all of the members of the County Durham Care Partnership. This makes a huge difference to how I view things and how we work as a partnership. Mine is just one example of how these cross-organisational roles work. We have found from doing this that staff are more focused on our population and less focused on individual organisations.
For tangible proof of the reality of what happens when strategy is converted into action, we need only look to Barnard Castle – an attractive market town set in beautiful Teesdale. In the Richardson Hospital we have co-located community services, social care, therapies, mental health, out-patients, a community hospital and GPs all working together to serve the same population. When we were there in hot weather everyone was sharing ice creams – a sure sign that integration is working.
In 2021, it took just five working days for the Council and the NHS Trust to set up a vaccination centre in the Civic Suite of County Hall. We vaccinated over 11,000 people and supported each other with a shared determination to protect the nation from COVID-19. It was great to see council staff, librarians, leisure assistants and facilities managers working alongside clinical colleagues. The task now is to translate that level of shared determination into ‘making strategies’.
ON THE HORIZON
Our NHS Trusts, social care and GPs already have integrated working arrangements in place, but we are entering a new phase, opening a new chapter in our story.
Our ambition is to deliver outstanding care for our residents. Bearing in mind the challenges we face – demand, complexity, workforce, estates, finance – the only way we can do this is through closer working. In County Durham, this means working together with our Integrated Care Board in a Joint Committee arrangement. We are realistic about our different governance arrangements, quality and inspection frameworks, HR rules and planning timetables but we don’t let them stop us. Therefore, by December 2022, our councillors and senior leaders expect to be working in a shadow Joint Committee sharing resources to deliver outstanding care.
Sometimes it is good to have a fresh view of the area in which you work. Sam Allen, Chief Executive of our Integrated Care Board, has visited the County Durham Care Partnership. She gave us great encouragement and inspired us to intensify our collaborative working. We are often so busy managing day-to-day operations, waiting times, outstanding reviews, and staff rotas that we forget about the progress we have made. Sam heard about some groundbreaking clinical innovation we are doing with Durham University and heard some uplifting patient stories. She was kind enough to give us some feedback and said, ‘I was blown away by the digital innovation, integration and partnership working. Truly impressive and so much to be proud of!’ CMM
WORKING TOGETHER: INTEGRATED CARE BOARDS 44 CMM October 2022
In what ways is your team approaching integration? What best practice examples can you share? Visit www.caremanagementmatters.co.uk and share your insights and feedback on the article. Michael Laing is the Director of Integrated Community Services at the County Durham Care Partnership. Email: Michael.laing2@nhs.net Twitter: @CDCarepartners Sarah Burns is the Joint Head of Integrated Strategic Commissioning at the County Durham Care Partnership. Email: Sarahburns3@nhs.net Twitter: @CDCarepartners >





www.caremanagementmatters.co.uk*Discountscannotbeusedinconjunctionwitheachother.@CMM_Magazine #CMMInsight Organised bySupported by Berkshire, Buckinghamshire and Oxfordshire Care Association Conference 20th October 2022 The Doubletree by Hilton, St Anne’s Manor, Wokingham, Berkshire Corporate Sponsor In association with Lancashire Care Conference 30th November 2022 Mercure Blackburn Dunkenhalgh Hotel, Lancashire DIARYFORDATESYOUR DISCOUNTS AVAILABLE* for associationandCMMmembers
CELEBRATING EXCELLENCE
Winning two awards at the Markel 3rd Sector Care Awards was a dream come true for us. Alive is a small charity based in Bristol and to have our work recognised by others was so incredible. Despite our size, we have always responded to the challenges faced by older people with innovation, compassion and commitment. We’ve always tried to do things differently, while really keeping the needs of older people right at the heart of what we do.

A FORCED CHANGE

We’ve delivered face-to-face activities for older people in care homes for 13 years – everything from gardening, music, exercise, reminiscence, technology and community engagement. We’ve trained care staff to ensure activity is person-centred and meaningful. We’ve campaigned to ensure older people’s mental, spiritual and


emotional wellbeing are prioritised alongside their physical wellbeing.
However, in March 2020, COVID-19 hit and we were no longer able to deliver our activities in care homes as before and our earned income had stopped. We were left with two choices: either respond and adapt, or, well, that second choice didn’t bear thinking about.
As ever, it was important that our response matched what older people and their carers really wanted, not what we thought they wanted. So, when we found that the nature of our live Zoom sessions was proving challenging for carers, we asked what we could do. Carers asked us to make our high-quality activities, inspiration and ideas available when they needed it, when they could access it easily. They wanted something that could be delivered to individuals in rooms and in groups, so the idea of interactive downloadable activities, or Alive on Demand, was born.
Alive Activities won two Awards at the Markel 3rd Sector Care Awards 2022. Chief Executive, Isobel Jones, shares the projects that won them the awards and how they came about.
46 CMM October 2022
AwardsCareSector3rdMarkel
DEVELOPING A NEW MODEL
We searched for funding, which we won. We looked for a suitable technology platform to use, which we found. We put together a team of creative and inspirational people to begin to mould Alive on Demand into a usable platform. It was incredible how quickly it came together. How ideas can be put into practice when you have the right people in place working brilliantly together with boundlessEvidently,energy.itwas challenging to get it off the ground. The biggest obstacles were technical; dealing with Apple and having apps approved. This delayed the project, but they are now up and running thanks to the tenacity of our Alive staff.
We now have a platform of over 250 inspiring, educational and engaging videos that are suitable for all older people, but especially for those living with dementia. They can be found on an easy-to-use platform through an app or browser. Care workers or family members can filter the videos on subject, presenter, video length, or level of dementia. There are even extra resources associated with each video so care staff can run a great activity session based around the video – from simple quizzes to picture resources, to musical scores. There is a huge range and variety of content, from City Tours and reminiscence sessions to poetry, art classes, gardening and music. Some of the videos are calming, such as a boat trip, or a walk through the woods, or a gentle day at the beach, all designed to support people living with dementia and provide a different sensory experience. Very often there are fewer resources for people with more advanced dementia and so Alive on Demand is working towards increasing the support here.
Users can sign up easily, either for an individual subscription or a care home subscription just by joining online. The process is simple and easy to use.
We’re incredibly proud of what we’ve achieved in a short period of time. We are seeing care homes using it brilliantly in their group and one-to-one sessions. It’s really broadening and supporting their activity provision and helping care staff to get back to delivering group sessions which has been a struggle. True to our values, though, it’s being used as a vehicle for discussion, for older people to connect to their memories and to share their stories with others and not just to watch. Our vision is for this to grow, for many care homes to sign up, for us to be able to support people in their homes with engaging and informative videos that they help us to shape.
OUR OASIS OF PEACE
The second award we received was for dementia care – this time for the development of a Dementia Friendly Allotment in Bristol. Like the development of Alive on Demand, this came into being during lockdown. We were given the keys to the allotment plot in March 2020 and were slightly concerned as to how we would make it happen given the circumstances.
As ever, the resilience of my staff and volunteers shone through and, in a COVID-safe way, they somehow transformed a barren, hard patch of land into a ‘heaven and oasis of peace’ for people living with dementia and their carers to come and garden and spend time with others.
When you look at the before and after photos it’s astonishing to see what the team managed to achieve. With challenges from COVID-19, a shortage of funding, a lack of available resources, and a steep learning curve, it’s not far off a small miracle!
The first major challenge was crowdfunding for a compost toilet, but we achieved that and, with some incredible support from local businesses, we were able to make the plot completely wheelchair friendly with paths and raised beds. We worked hard to keep the other allotment holders involved in our vision, as it did resemble a building plot at times, but they stuck with us and now they can see the real benefits of the allotment and what a difference it is making to people every week.
We are now running gardening groups three to four times a week for people living with dementia and their care partners. Memory Cafés and community groups are bringing their members up for cream teas and social gardening over the warmer months. We have a regular team of volunteers who support the participants and help us with maintenance. The allotment really is delivering what we had hoped – a social space for both individuals and their carers to relax, enjoy, connect with nature and find joy. One carer said, ‘I’ve got my old John back here,’ while another said, ‘We look forward to this every week.’ We’ve seen improvements in mobility and speech from participants; carers have found time, space and a sense of peace, with one commenting, ‘It doesn’t matter what I or Andrew look like or what has gone on in the day or week, we are comfortable and relaxed here.’
We want to share the allotment with others (you may well have seen us on Gardeners’ World in September). We want more participants to come and benefit, but we also want to share our experience and knowledge with others, and we are helping and supporting other groups to set up similar projects. If others can benefit as much as our participants, it will be a joy to see.
DESERVED RECOGNITION
The teams on both projects have worked tirelessly to bring these projects to fruition in incredibly difficult circumstances, and for them to be recognised at the Awards was so important for them. It just shows what can be achieved with hard work, determination and passion. CMM
Isobel Jones is Chief Executive at Alive Email:Activities.info@aliveactivities.org Twitter: @aliveactivities
Sign up to Alive on Demand at aliveondemand.co.uk or get in touch at aod@aliveactivities.org. For further information on the Community Gardening project, email aliveactivities.orgcommunitygardening@ or follow @alivegardening on
HeadlineTwitter.Sponsor
The Dementia Care Award was kindly sponsored by

The Markel 3rd Sector Care Awards is run specifically for the voluntary care and support sector. Visit www.3rdsectorcareawards.co.uk to view the 2022 event winners and find out more about next year’s event. Sponsorship opportunities are available.
With thanks to our sponsors: National Care Forum, Learning Disability England, The Care Provider Alliance, Association of Mental Health Providers and VODG.
CMM October 2022 47
Care Management Matters (CMM) is thrilled to be returning to face-to-face CMM Insight events as we look forward to the upcoming Berkshire, Buckinghamshire & Oxfordshire Care Association Conference. The conference, in association with Berkshire Care Association, Milton Keynes and Buckinghamshire (MKB) Care Association and the Oxfordshire Association of Care Providers (OACP), will take place at The Doubletree by Hilton St Anne’s Manor, Wokingham, on 20th October 2022. The conference aims to bring the quality of a national conference to a local stage, focusing on the issues that matter to providers in Berkshire, Buckinghamshire andTheOxfordshire.daywillinclude presentations from high-level sector representatives, offering expert insight into the local picture, along with an exhibition of carefully selected services and products and a choice of interactive workshops to delve into a subject further. There will also be networking opportunities with like-minded providers and senior decision-makers from the independent care and support sector to learn more about delivering best practice in a changing market.
A HUB OF INFORMATION
A packed agenda awaits delegates attending the Berkshire, Buckinghamshire & Oxfordshire Care Association Conference. The day’s keynote speech will be delivered by Matilda Moss, Head of Integrated Commissioning at Buckinghamshire County Council. Matilda
will be presenting the view from the council, which will provide an overview of the changes providers can expect as a result of the latest Government reforms and how the local authority in Buckinghamshire aims to work alongside and support services. Next up will be Dan Hayes, Chief Executive Officer at The Orders of St John Care Trust. Dan will be sharing a provider’s view of how increased access to technology is helping to support people in a person-centred way against the backdrop of the latest Government reforms and white papers.
In amongst exhibition viewing and an unmissable panel discussion featuring the conference’s speakers, Neil Eastwood, Founder and Chief Executive at Care Friends, will be dissecting the timely subject of care worker recruitment. Neil will share the latest thinking, research and innovation, drawing on his connections with employers of care staff from around the world. Every one of Neil’s recommendations can be easily implemented and most cost nothing but have been repeatedly proven to make a big Complementingdifference. the conference’s agenda, a selection of interactive workshops will cover legal updates relating to the Care Quality Commission (CQC), how technology can help improve CQC inspections and the use of Artificial Intelligence (AI) in social care. Neil Grant, Partner at Gordons Partnership, will explain how services can best prepare for the changes to minimise the risk of regulatory intervention and downgrading of ratings. Peter
Ellis, Director at Intelligent Care Software, will discuss some of the reasons why social care providers should consider using digital care management software. Lastly, Vayyar Imaging Ltd will explore how simple pieces of equipment that use AI can benefit the sector in a non-intrusive way.
The conference’s afternoon offering will pick up where the morning left off, discussing the sector’s hot topics and their application to the adult social care landscape in the area. Delegates will be joined by Amanda Lyons, Engagement Lead at Buckinghamshire, Oxfordshire and Berkshire West Integrated Care Board, who will be discussing changes to Integrated Care Boards and Systems, including an overview of how the local system will work, its aims and priorities. In addition, Richard Ayres, Social Care Adviser at Care England, will be examining the fair cost of care and The Prince’s Trust will explain how it works with and supports young people to access employment and start their careers in the health and social care sector.
BOOK NOW
Book your tickets today and view the conference’s full agenda by visiting the CMM website. Join the conversation on Twitter by tagging @CMM_Magazine and using the hashtag #CMMInsight. Sponsorship and exhibiting opportunities are still available. Visit the CMM website to secure your place at the Berkshire, Buckinghamshire & Oxfordshire Care Association Conference. CMM
EVENT PREVIEW
20th October 2022, Wokingham CMM INSIGHT BERKSHIRE, BUCKINGHAMSHIRE & OXFORDSHIRE CARE ASSOCIATION CONFERENCE 2022 Look out for announcements about CMM Insight events happening in 2022 @CMM_Magazine #CMMInsight www.caremanagementmatters.co.uk 48 CMM October 2022


CMM October 2022 49 CMM EVENTS Please mention CMM when booking your place. Sign up online to receive discounts to CMM events. Contact:Date/Location:Event:Contact:Date/Location:Event:Contact:Date/Location:Event: Berkshire, Buckinghamshire and Oxfordshire Care Conference 20th October, Berkshire Web: co.uk/event/markel-3rd-sector-care-awards-2023/Web:3rdMarkelevent/lancashire-care-conference-2022/Web:30thLancashirecare-association-conference-2022/event/berkshire-buckinghamshire-oxfordshire-www.caremanagementmatters.co.uk/CareConferenceNovember,Lancashirewww.caremanagementmatters.co.uk/3rdSectorCareAwardsMarch2023,Birminghamhttps://www.caremanagementmatters. WHAT’S ON? Contact:Date/Location:Event:Contact:Date/Location:Event:Contact:Date/Location:Event:Contact:Date/Location:Event:Contact:Date/Location:Event:Contact:Date/Location:Event:Contact:Date/Location:Event: Adult Social Care Workforce Data Set 4th October, virtual Web: events/Web:28th-29thThekings-fund-annual-conference-2022Web:1st-2ndThethe-first-time-2022-23-2/using-the-data-security-and-protection-toolkit-for-Web:25ththeUsingmental-health-2022/Web:18thMentalWeb:12-13thTheWeb:11-12thCommunityWN_UkDzdhxwSCWpKJh4f0iZHAhttps://us06web.zoom.us/webinar/register/CareLiveOctober,Londonhttps://www.communitycarelive.co.uk/CareShowOctober,NECBirminghamhttps://www.careshow.co.uk/Health2022October,Londonhttps://govconnectevents.co.uk/events/theDataSecurityandProtectionToolkitforfirsttimeOctober,virtualhttps://www.digitalsocialcare.co.uk/events/King’sFundAnnualConferenceNovember,Londonhttps://www.kingsfund.org.uk/events/the-NCFCEOConferenceNovember,Londonhttps://www.nationalcareforum.org.uk/
MARK ADAMS • CHIEF EXECUTIVE • COMMUNITY INTEGRATED CARE

considered the rather crucial question of whether there would be anyone left to deliver that
So,care.my first piece of advice to our new Health and Social Care Minister, Therese Coffey is to reorder her ABC (ambulances, backlogs, care) mission and place care at the front of that list because, without this particular cog in the machine turning as it should, the problems besetting the other areas will continue.
With the new Prime Minister now in post, Mark Adams, Chief Executive of Community Integrated Care, reflects on the Boris Johnson leadership and what progress was made for social care.
As my old adversary Boris steered his space-hopper into the sunset following his final stand-up routine outside Number 10, virtually none of the British press spotted the comedy nugget nestled among the metaphor muesli that was his farewell address. It was even omitted entirely from the BBC Fact Check of his largely fictitious farewell speech.
But I’m sure everyone in the social care sector emitted a collective howl of outrage as he delivered the final punchline to his three years as our Prime Minister: ‘We’ve reformed socialWell,care.’inthe true spirit of the pantomime that was Boris Johnson’s term in office: Oh no, youThisdidn’t.sector remains in the
grip of an existential crisis which has consistently eluded the understanding of a Government that demonstrated every day it had no idea what the social care sector actually did, never mind what was ailing it. Who else would name a tax which delivers sixth sevenths of its income directly to the NHS a ‘social care’
No,levy?Boris Johnson has not reformed social care. In fact, what is actually happening feels more like dissolution. In July, Skills for Care announced that vacancies in the sector had risen by 52% to 165,000 between July 2021 and July 2022. That means more than 50,000 support workers have left the sector entirely. Many will have finally taken the golden hello from an Amazon distribution
hub or been tempted onto a till by a newly-opened Aldi. Some will even have gone to the NHS where, according to our own research Unfair to Care which we commissioned last year, they could earn around 39% or £7k a year more for doing exactly the same job. Sadly, they could even earn 20% more if they decided to join the NHS as a hospital porter.
And this exodus of exhausted and disillusioned support workers will continue unless there is an immediate and significant financial intervention. The so-called social care levy, by the time it trickles down to the care sector, is unlikely to even fund the cap on individual lifetime care costs which, I suspect, Boris believed was the burning issue. He doesn’t seem to have
Secondly, whilst social care continues to be funded by cash-starved local authorities, our workforce will never earn a wage commensurate with the skilled and increasingly complex support it provides. And without a workforce strategy that delivers parity with the NHS, recruitment and retention will continue to be both the source and the cause of policy failure.
So, as well as getting the ABCs right, Ms Coffey should issue an immediate SOS – sort outInstaffing.mytime with Community Integrated Care, I have genuinely witnessed the very best of humanity. The courage, incredible compassion, professionalism and selflessness that characterises not just the headline events we witnessed during the pandemic, but every time one of our colleagues goes on shift, is extraordinary. But the financial distress that people working in front-line social care roles are experiencing is heart-breaking.So,myfinal piece of advice is simply to genuinely understand and know the value of the real contribution made to society by socialThecare.Government that manages that will be the first to go some way to reforming it.
Mark Adams is the Chief Executive of Community Integrated Care. Email: mark.adams@c-i-c.co.uk the new Prime Minister and the Health and Social Care Secretary?
50 CMM October 2022
Twitter: @MarkAdamsCEO Do you agree with Mark’s comments and what’s your message to
Visit www.caremanagementmatters.co.uk and share your feedback on the article.


















IMAGINE IF YOU COULD QUICKLY DIFFERENTIATE BETWEEN THE SYMPTOMS OF YOUR RESIDENTS’ RESPIRATORY INFECTIONS 1-3 ID NOW ™ RAPID MOLECULAR RESPIRATORY TESTING PLATFORM ID NOW™ IS AN EASY-TO-USE CONNECTABLE INSTRUMENT WHICH PROVIDES POSITIVE RESULTS FOR: • SARS-CoV-2 in 13 minutes or less 5 • Influenza A & B in as little as 5 minutes , with 95% detected within 7 minutes 4 and negative results in 13 minutes 5 • RSV in 13 minutes or less 5 • Strep A in as little as 2 minutes , with 99% detected within 3 minutes 6 and negative results in 6 minutes 5 SCAN TO LEARN MORE ABOUT ID NOW ID NOW ™ PLATFORM ID NOW™ - Helping you to put your residents’ needs first by treating them quickly, and isolating where needed. 1. NHS England and NHS Improvement. Primary Care Bulletin. Updated June 29, 2021. Accessed November 2021. Virusesand2021.coronavirus/primary-care/other-resources/primarycarebulleting/june-https://www.england.nhs.uk/2.ZhouH,TsouJH,ChinthalapallyM,LiuH,JiangF.DetectionDifferentiationofSARS-CoV-2,Influenza,andRespiratorySyncytialbyCRISPR. Diagnostics. 2021;11(5):823. 3. MedTech Europe. The Value of Diagnostic Information in Acute Respiratory Infections — Observations From the COVID-19 Pandemic. Accessed November depictedowners.trademarks©ProductVirologyofcase-on-respiratory-disease_case-study.pdf.https://www.medtecheurope.org/wp-content/uploads/2021/04/vodi-2021.4.MooreN,etal.EvaluationtheAlere™iInfluenzaA&B2Assay.Posterpresentedat:ASMClinicalSymposium;2018;WestPalmBeach,Florida.5.Abbott.IDNOW™Inserts.6.Abbott.DataonFile.IDNOW™StrepA2ClinicalTrial.2022Abbott.Allrightsreserved.AlltrademarksreferencedareofeithertheAbbottgroupofcompaniesortheirrespectiveAnyphotosdisplayedareforillustrativepurposesonly.Anypersoninsuchphotosisamodel.COL-1564208/22
OVER 3.8 million issued in grants SINCE 2020 to care workers in need!
Knowing someone is there to help can be just the Lifeline needed. This is why we never stop.
The future of social care is everyone's responsibility.
Please support The Care Workers' Charity.
For over a decade, the charity has supported thousands of individuals working in social care with hardship grants to help them cope with emergencies such as loss of income, illness, homelessness and bereavement. We have now expanded our ambitions and support to protect both the financial and emotional wellbeing of those employed in social care, providing access to free counselling.
Find us on:





www.thecareworkerscharity.org.uk