CarilionClinic.org/community-health-assessments
Executive Summary
Carilion Clinic is committed to joining with our partners to pursue the essential work of improving and maintaining the health of Tazewell County in accordance with our mission. Periodically assessing the health concerns of each community is a key component of addressing needs. Every three years, the Tazewell County Community Health Assessment (TCCHA) aims to uncover issues, indicate where improvement is needed and track and promote progress in key areas so that there is demonstrated, ongoing change. The CHA process and the public availability of its findings enable and empower our community to effectively improve and maintain health.
Carilion and the Cumberland Plateau Health District (CPHD) partnered to conduct the 2024 TCCHA alongside additional community partners, the Community Health Assessment Team (CHAT). After review and discussion of the data collected, the 2024 TCCHA led the CHAT to identify seven priority health issues in the community
Community Health Improvement Process
Carilion believes in continuous quality improvement. The triennial CHA serves as a formal way of identifying community needs and developing plans to address them. It shapes the ways we support our mission in the community and encourages collaboration and alignment with clinical teams Not only does this process identify current needs and disparities, but also helps to ensure we are regularly evaluating and shifting to meet emerging needs

Priority Health Needs
In collaboration with the CHAT, we identify key health needs to align resources and other efforts for the following three years. The CHAT reviews extensive data, asks questions and participates in a consensus-building prioritization process The 2024 TCCHA resulted in the following health priorities:



Drivers of Priority Health Needs
The CHA process focused on prioritization of health conditions and outcomes, rather than a broader focus on their root causes. We recognize that access to healthcare and other services and the social determinants of health (SDOH) are key facilitators of good health and well-being. As such, we focused on those and other health factors as a strategic component of action planning The key drivers of each priority health condition, as identified by the CHAT, are discussed in the corresponding sections of this report.
Board Adoption
This document was approved by the CTCH Board of Directors on July 24, 2024, and formally adopted as the 2024 Tazewell County Community Health Assessment.
Disclaimers
This document has been produced to benefit the community. Carilion encourages the use of this report for planning purposes and is interested in learning of its utilization. Comments and questions are welcome and can be submitted to Carilion Clinic at communityoutreach@carilionclinic.org
Members of the leadership team reviewed all documents prior to publication. Every effort has been made to ensure the accuracy of the information presented in this report; however, accuracy cannot be guaranteed. Members of the Tazewell County CHAT cannot accept responsibility for any consequences that result from the use of any information presented in this report.
Carilion began conducting CHAs prior to the IRS adoption of the 501(r)(3) standard which requires not-for-profit hospitals to conduct a Community Health Needs Assessment (CHNA) every three years. While meeting the CHNA requirement, Carilion maintains the longstanding formal name Community Health Assessment for our process and reports. A crosswalk of this document based on the 501(r)(3) standards can be found in Appendix A.
Our Partners
Community Health Assessment Leadership Team
The CHA Leadership Team collaborates to guide major functions of the CHA, including CHAT recruitment, data collection/analysis and shaping meeting structure. In addition to Carilion staff, membership includes leadership from the local health district. Carilion organizes and facilitates leadership team meetings.
• Carilion Clinic:
o Shirley Holland, VP, Community Health and Development
o Molly Roberts, Manager, Community Benefit
o Ashley Hash, Community Health Improvement Program Manager
o Holly Ostby, Community Health Improvement Program Manager
o Nicholas (Nick) Bilbro, Community Benefit Analyst
• Cumberland Plateau Health District:
o Reisa Sloce, Health Director
o Daniel (Dan) Hunsucker, Population Health Coordinator
o Victoria Bartfai, Health Educator, Maternal & Child Health
Community Health Assessment Team
The CHAT is a dynamic group of health and human service agency leaders, individuals/organizations serving/representing the interests of priority populations and local representatives from various community sectors. The following community partner organizations participated in the 2024 TCCHA:
Organization
Appalachian Agency for Senior Citizens
Carilion Planning and Community Development
Carilion Tazewell Community Hospital
Clinch Valley Community Action
Cumberland Plateau Health District
Cumberland Plateau Planning District
Department of Social Services
Organization Type
Older Adults
Population Health
Healthcare
Safety-Net Services
Population Health
Planning/Development
Safety Net Services
Four County Transit Transportation
Industrial Development Authority (IDA)
Project13Three
Tactical Retreat Unplugged
Tazewell Chamber of Commerce
Transportation/Economic Development
Recidivism Reduction
Alternative Care – Mental/Behavioral Health
Chamber of Commerce
Tazewell County Public Library Library
Tazewell County Public Schools
Tazewell County Sheriff's Office
Town of Tazewell Sheriff's Office
VA Cooperative Extension
Vibrant Health & Wellness Coaching
Public School Representative
Public Safety
Public Safety
Cooperative Extension
Private Health Coaching Service
To see a list of specific 2024 CHAT participants, please see Appendix B.
Data Team
Additional data support was provided by the Virginia Department of Health Division of Population Health Data
• Khristina Morgan, Community Health Epidemiology Regional Coordinator
• LeeAnn Gardner, Community Health Epidemiologist, Central Shenandoah Health District
• Taiwo Ilechie, Community Health Epidemiologist, Roanoke City and Alleghany Health Districts
Our Process
The first step in the ongoing community health improvement process is to conduct a CHA. Every three years, Carilion follows the formal process described below to identify community needs and develop plans to address them. The 2024 TCCHA officially began on October 12, 2023 and concluded with the final CHAT meeting on June 13, 2024.
STEP 1: Define Community Served
Carilion Tazewell Community Hospital (CTCH) is located in Southwest Virginia in Tazewell County. CTCH is a not-for-profit, 56-bed hospital dedicated to quality care and patient comfort. Offering both inpatient and outpatient services, CTCH also impacts the health of the community through its Swing Bed program—extended recovery for patients with skilled care needs before transitioning home.
The service areas for Carilion’s CHAs are determined by unique patient origin of the hospital in each respective market. Focus is placed on areas that are considered Medically Underserved Areas (MUAs) and Health Professional Shortage Areas (HPSAs).
In fiscal year 2023, CTCH served 7,351 unique patients. Patient origin data revealed that during this year, 94% of those patients lived in Tazewell County

Additional Community Demographics
In addition to Carilion, key safety net providers in the region include the Tazewell Community Health Center (a federally qualified health center), Cumberland Mountain Community Services, local offices of the Virginia Department of Health (VDH) and other service organizations. Despite these entities’ presence, many low-income, uninsured and underinsured residents do not have sufficient access to affordable healthcare services.
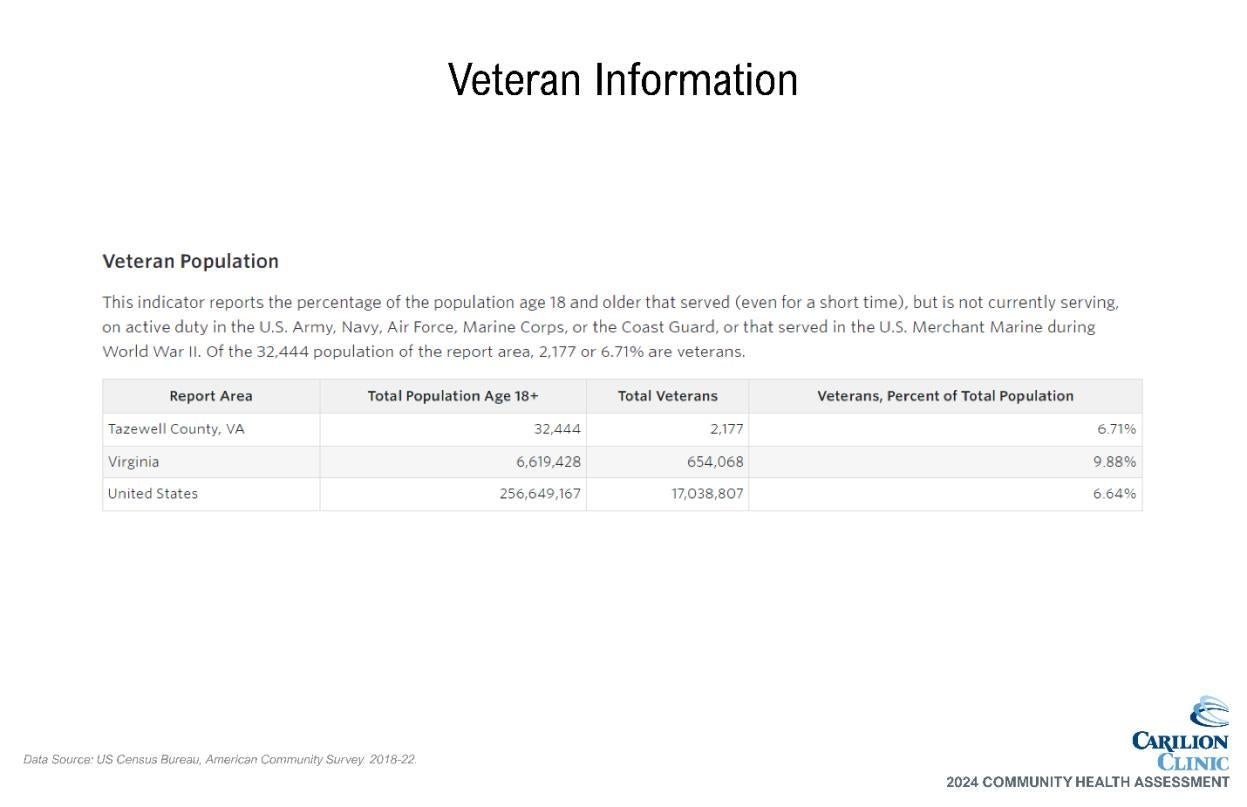
The county is less densely populated, has a higher median age, a lower median household income and is less racially and ethnically diverse than the state average. The Weldon Cooper Center for Public Service predicts a negative 3.3% population change for the county by 2040 1
Table 1. Select Demographics of the TCCHA Service Area
Source: US Census Bureau, ACS, 2018-2022
Table 2. Income Data for the TCCHA Service Area
Source: US Census Bureau, ACS, 2018-2022
Compared to state and national averages, a larger percentage of Tazewell residents receive health insurance coverage through public insurance options emphasizing the value continued support of these programs brings to the community. Specific to CTCH inpatients and outpatients in fiscal year 2023, 33.23% received Medicaid while 3.60% were self-pay, a proxy for uninsured.
Table 3. Insurance Status of TCCHA Service Area
Source: US Census Bureau, ACS, 2018-2022
Table 4. Racial/Ethnicity Demographics, TCCHA Service Area
Source: US Census Bureau, ACS, 2018-2022
1 University of Virginia Weldon Cooper Center for Public Service. (2023). Virginia Population Estimates. Retrieved from https://coopercenter.org/virginia-population-estimates
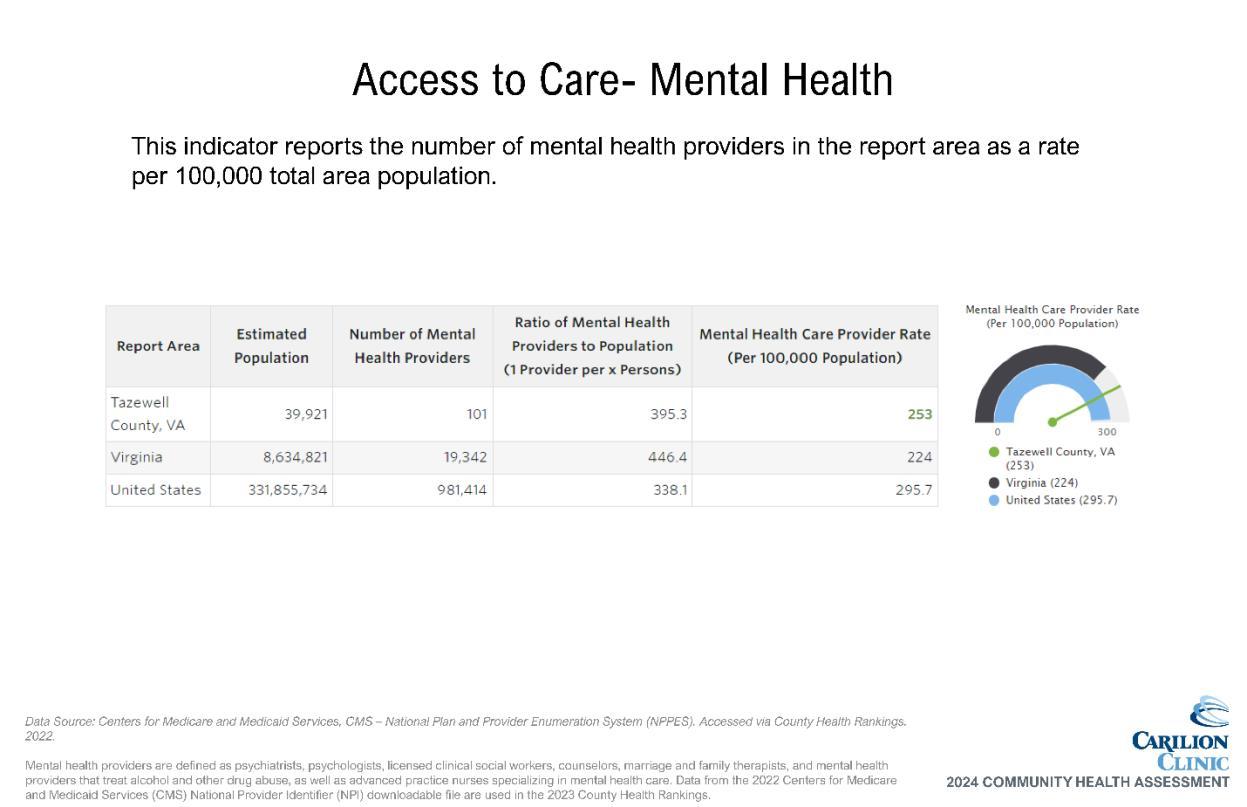
The county is in the less densely populated far southwest section of the state, with fewer resources in comparison to the rest of the state. Tazewell County carries designations of lowincome population HPSA for Primary Care and Dental Care, a geographic HPSA for Mental Health and is currently identified as a MUA 2,3
Target Population
The target population for Carilion’s CHA projects consists of underserved/vulnerable populations disproportionately impacted by SDOH, including poverty, race/ethnicity, age, education, access and/or lack of insurance. Data are reviewed where available by different life stages, including parents of children and adolescents, women of child-bearing age, adults and the elderly. Other considerations include race, ethnicity and income levels. All patients are included in this assessment regardless of insurance payments or financial assistance eligibility. Distinct efforts are taken to ensure the CHA reflects those residing in MUAs and HPSAs.
STEP 2: Convene Community Health Assessment Team
A 30-member CHAT participated in the assessment activities. Hearing voices from across our service area is crucial to a CHA’s success. Broad-interest community reach is a main qualification when inviting individuals to join the CHAT. Direct invitations were sent to the CPHD, local governments, the local school system, social service organizations, other community organizers and nonprofit leaders.
The CHAT met four times throughout the process, with each meeting serving a distinct purpose.
• Meeting 1: Introduction and Overview of the Process; Launch of Community Health and Well-Being Survey
• Meeting 2: Data Presentation and Data Walk
• Meeting 3: Prioritization of Needs and Discussion
• Meeting 4: Action Planning: Key Drivers and Impact/Feasibility Activity
Each meeting built on the one prior and fostered dialogue amongst CHAT members. Meetings were held in person and virtually with interactive opportunities to participate and engage with data and facilitated discussions with other CHAT members
The CPHD team was engaged from the beginning of the planning process (spring of 2023) throughout the assessment period and all CHAT meetings CPHD’s involvement helped shape all aspects of this assessment. The team identified community partners to serve on the CHAT, provided discussion points and suggestions on structure of CHAT meetings and offered feedback on the prioritized needs. Additionally, CPHD representatives were active on the CHAT and participated in all activities including the Stakeholder Listening Session and the prioritization activity.
In addition to CPHD, the CHAT included other individuals or organizations serving or representing the community’s medically underserved, low-income and minority populations. Examples include:
• Safety Net Services (e.g., Clinch Valley Community Action, Tazewell DSS)
• Public school systems (e.g., Tazewell County Public Schools)
• Incarcerated/Returning Citizen Support Services (e.g., Project13Three)
2 https://data.hrsa.gov/tools/shortage-area/hpsa-find
3 https://data.hrsa.gov/tools/shortage-area/mua-find
These organizations and individuals helped gather community input by distributing the Community Health Survey. CHAT member input was solicited through the Stakeholder Survey and Listening Session. Combined, these efforts led to the identification and prioritization of community health needs.
STEP 3: Collect and Review Relevant Health Data
Various data were collected and shared regularly with the CHAT, including primary and secondary data on health outcomes, health status, socioeconomic factors and quality of life. Secondary data served as a key driver of the process, with primary data adding community context and perspectives to understand the needs of subpopulations within the community.
Community Health and Well-Being Survey
A Community Health and Well-Being Survey was conducted as part of the TCCHA. This survey was used to evaluate the community’s health and identify potential geographic areas to target improvements. Input and oversight of survey development was provided by the CHAT and the CHA Leadership Team.
A 27-question survey instrument was utilized. It asked questions about access to care and other services, health status, community strengths, quality of life, subjective well-being and demographics (Appendix C: Community Health and Well-Being Survey). The survey instrument included commonly used questions and metrics from the following established community surveys:
• Cantril’s Ladder
• Community Themes and Strengths Assessments, National Association of County and City Health Officials, Mobilizing for Action through Planning and Partnerships
• Community Healthy Living Index, YMCA
• Behavioral Risk Factor Surveillance System, Centers for Disease Control and Prevention (CDC)
• National Health Interview Survey, CDC
• Youth Risk Behavior Surveillance System, CDC
• Martin County Community Health Assessment, Martin County, North Carolina
• Previous Tazewell County Community Health Surveys
The population of interest for the survey was Tazewell County residents 18 years of age and older. Surveys were distributed from October 2023 through December 2023. A drawing for a $50 grocery store gift card was offered as an incentive for those completing the survey.
The following subpopulations were especially targeted for sampling:
• Underserved/vulnerable populations disproportionately impacted by SDOH, including:
o Poverty
o Race/ethnicity
o Education
o Lack of insurance
A non-probability sample method was used, where respondents were not randomly selected. Although the survey was available to all residents living in Tazewell County, oversampling of the targeted subpopulations occurred through specific outreach efforts through community partners.
Oversampling ensured that needs and assets specific to this subpopulation of interest were captured.
The survey instrument was available in both English and Spanish via the following methods:
• Qualtrics link and QR code
• Phone line (888-964-6620)
• Paper surveys (collected by volunteers and/or staff of partner agencies)
Outreach strategies for survey distribution included:
• Social media
• Flyers and posters distributed throughout the community with survey QR code, URL and phone line information
• Survey URL posted on partner agency websites
• Recruitment of participants on site at CHAT member organizations
In total, 196 surveys were collected and validated. Full survey results and validation methodology can be found in Appendix D
All responses were entered into Qualtrics by survey respondents or, in the case of surveys completed on paper, by Carilion staff. Surveys were analyzed and reported using Qualtrics and Microsoft Excel.
Stakeholder Listening Sessions and Survey
CHAT members were invited to provide an additional perspective on the needs and barriers to health facing our community. Carilion staff from across the organization facilitated small group discussions. To quantify focus group data, CHAT members were asked to complete the Stakeholder Survey. A summary of the data can be found in Appendix E.
Community stakeholders, leaders and providers were encouraged to complete the Stakeholder Survey after participating in a listening session. The survey was also shared with leaders who may not have attended a listening session. The online survey was shared at the CHAT meetings and via email. Surveys were analyzed and reported using Qualtrics and Microsoft Excel.
Secondary Data
Secondary data came from two primary sources: SparkMap and the VDH Division of Population Health Data. SparkMap is a product from the University of Missouri that quickly and accurately aggregates data across geographies for 80+ indicators from publicly available sources such as the American Community Survey, County Health Rankings and the CDC. Secondary data analysis was provided through SparkMap’s tables, maps and visual diagrams depicting indicators that are better or worse than the state average, trends over time and comparisons across different population segments such as race and life cycle.
A team of VDH epidemiology staff provided and analyzed data from specific VDH departments a critical component of the data walk. Data provided included mortality due to specific chronic diseases, incidence rates of sexually transmitted infections, sociodemographic data, cancer rates and others. VDH was also able to provide data broken down by gender and race/ethnicity for many health topics.
Table 5. Data Sharing Summary
Community Demographic Data Secondary - CHAT 1 Presentation
Health Factors Data
- CHAT 1 Presentation - CHAT 2 Overview in Presentation - Data Packet Email prior to CHAT 3
Health Outcomes Data Secondary - CHAT 1 Overview in Presentation - CHAT 2 Data Walk - Data Packet Email prior to CHAT 3
Community Health & Well-Being Survey
Community Listening Sessions (CLS)
Stakeholder CLS
STEP 4: Prioritize Community Health Needs
- Data Packet Email prior to CHAT 3
- Data Packet Email prior to CHAT 3
- Data Packet Email prior to CHAT 3
Using their community knowledge, data collectively reviewed and additional data requested and shared, CHAT members were asked to complete an electronic survey to prioritize community health needs. Prioritization topics included specific health conditions or outcomes reflecting those conditions which contribute to morbidity and mortality in the service area. The prioritization survey matched the structure utilized during the data walk at CHAT Meeting 3. This resulted in the identification of 13 community health needs.
During CHAT Meeting 4, members completed a dot voting activity to further refine the priority list. A discussion ensued to determine the final prioritized needs based on scope of issue, burden on community and feasibility to address at the community level based on CHAT member perspectives and perceptions Appendix F summarizes the prioritization activity, including the results of each exercise component.
The 2021 TCCHA and the subsequent Implementation Strategy were posted publicly though multiple electronic channels and shared widely by community partners. An email address was provided for submission of written comments, but none were received for consideration in the identification and prioritization of health needs.
STEP 5: Strategic Planning to Address Priority Health Needs
The final CHAT meeting served as a springboard into both hospital and community action planning. The prioritized needs were again reviewed, and a two-part activity ensued. CHAT members identified key drivers of the prioritized health outcomes/conditions using the Robert Wood Johnson County Health Rankings framework as reference. Following the identification of drivers, an impact and feasibility analysis was completed in small groups to help identify leading strategies for community change.
Our Impact: Evaluation of Actions Taken in Response to 2021 TCCHA
The top prioritized needs established in the 2021 TCCHA were grouped into four overarching categories: mental health, socioeconomic factors, culture and health behaviors. Key strategies included health education, grant funding to address SDOH and support for the efforts of community partners in addressing the needs, both directly and indirectly. Below is a snapshot of outcomes from these efforts through June 30, 2024


Our Priority: Health Equity
Carilion is part of a growing movement of health system stewards committed to unlocking our community’s potential to thrive. We, along with key partners, strive to identify and address health and socioeconomic factors that impact our communities’ health and well-being. We know that where you live is an important contributing factor of health status and outcomes. We are committed to advancing a culture of health where policies, systems, education, research and resources align for optimal health status.
Our mission calls for us to meaningfully address health inequities and disparities. Equity is a key lens for the CHA process, guiding our actions as we seek to understand community health needs. As we move forward into developing community heath improvement strategies, we will remain focused on identifying and serving those who need it most, seeking to broaden the potential for everyone across our communities to thrive.
The Area Deprivation Index (ADI), a tool developed by the University of Wisconsin-Madison, sheds light on what are considered disadvantaged areas of the community based on census block groups (neighborhoods).4 This granular data helps emphasize the importance of conditions that shape our daily lives. The image below shows ADI scores on the higher end of the range (6-10) for all block groups in Tazewell County. Some variation can be seen, with lower scores located closer to town centers Tazewell and Bluefield. Data used in creating the index includes factors for income, education, employment and housing quality some of the key social determinant factors that influence health outcomes.


4 https://www.neighborhoodatlas.medicine.wisc.edu/
As we work to improve health equity across our region, our guiding principles include improving access to care and addressing SDOH. This assessment focuses on those principles in the context of specific prioritized health outcomes. To expect a shift in health outcomes, we must focus on improving the underlying factors that lead to them seen in the figure below in a coordinated manner. We will be addressing specific SDOH needs as aligned with the CHA focus areas.
Figure 1. Social Determinants of Health

Source: Institute for Clinical Systems Improvement; Going Beyond Clinical Walls: Solving complex Problems, 2014. Analysis and adaptation from the University of Wisconsin Population Health Institute’s County Health Rankings model, 2010. Graphic designed by ProMedica and shared by the American Hospital Association.

Our Priority: Addressing Chronic Disease
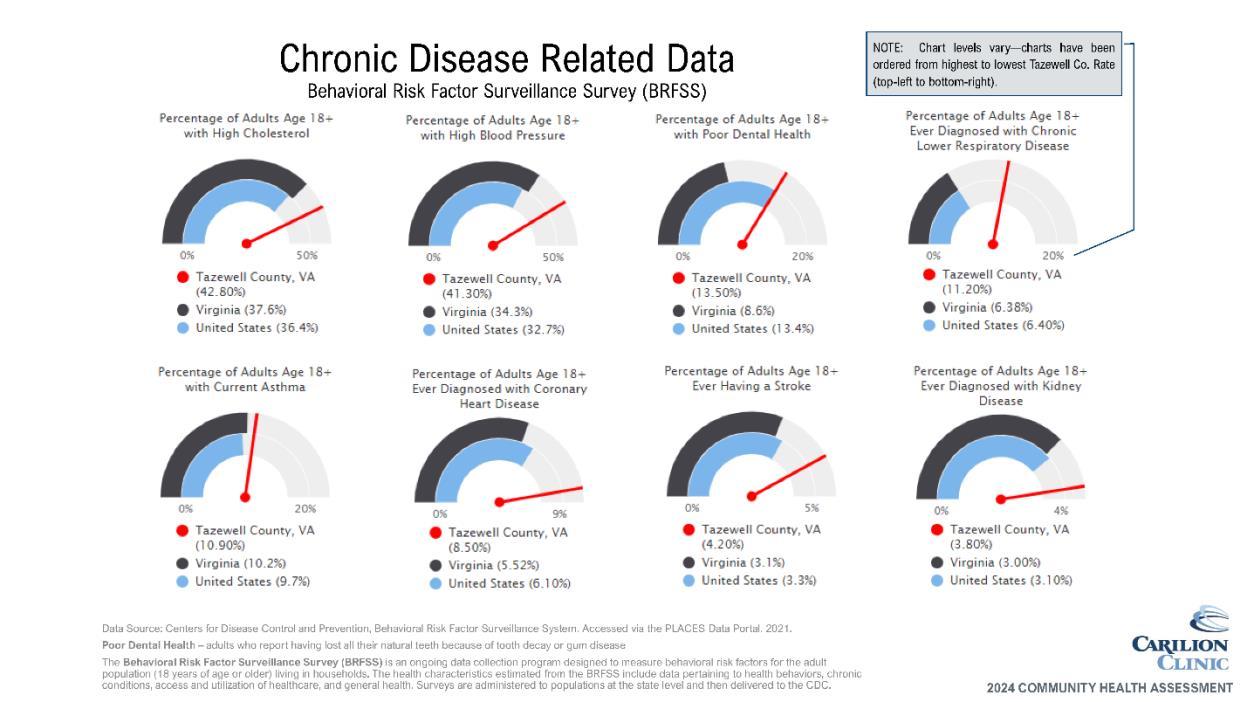
Our prioritization process resulted in the elevation of three specific chronic diseases for focus: overweight/obesity, diabetes and hypertension The following data indicates potential areas for opportunities
Data shows need
• Residents of Tazewell County have a higher-than-average occurrence of:
o Physically unhealthy days
o Obesity
o Diabetes
o Heart disease
o High blood pressure
Community indicates need
• Community survey respondents indicated:
o Overweight/obesity and high blood pressure as top health conditions impacting their/their family’s health
o Lack of exercise and poor eating habits as top factors affecting their/their family’s health and wellbeing
o Access to parks and recreation and clean air two top responses to our community’s greatest strengths
• CHAT participants noted the interwoven relationship between chronic disease, mental health other discussed priorities
Why This Matters
According to the Institute for Health Metrics and Evaluation (IHME), high body-mass index (BMI), high blood pressure and dietary risks are within the top 10 risks driving death and disability. In other words, these are some of the key impacts on overall health, well-being and life expectancy.5 Additionally, chronic diseases are a leading driver of healthcare costs 6
Chart 1 shows the average number of self-reported physically unhealthy days from the CDC’s Behavioral Risk Factor Surveillance System (BRFSS), which is higher for Tazewell than Virginia’s state average. This metric helps illustrate the impact chronic disease may have on residents’ perceptions of their physical health and quality of life.
The remaining data (Charts 2-4) shows that Tazewell County exceeds Virginia state averages in self-reported adult obesity rates, adult diabetes rates and coronary heart disease rates.
Tazewell County’s rates of high blood pressure also exceed the state average 7 When reviewing by census tract in Map 2, some variation is seen. This may be connected to the proximity/ease of access to town centers Tazewell and Bluefield, specifically and the increased availability of resources. Because blood pressure is known to increase with age for most people,8 it’s important to note that the data available at this census tract level is not age-adjusted.
5 United States | Institute for Health Metrics and Evaluation (healthdata.org)
6 https://www.cdc.gov/chronic-disease/about/index.html
7 Centers for Disease Control and Prevention, Behavioral Risk Factor Surveillance System. Accessed via the PLACES Data Portal. 2021.
8 Franklin, Stanley S., et al. "Hemodynamic patterns of age-related changes in blood pressure: the Framingham Heart Study." Circulation 96.1 (1997): 308-315.
Chart 1. Physically Unhealthy Days



Chart 4. Adults With Heart Disease



Source: Centers for Disease Control and Prevention, Behavioral Risk Factor Surveillance System: 2021 Accessed via SparkMap.
Key Drivers
Community partners identified many key drivers of these chronic diseases, including access to healthy foods, time required to prepare food, access to care, education of prevention and disease management, culture/readiness to change and the impact of stress and trauma.
According to the CDC, many preventable chronic diseases are caused by the same behaviors, which include smoking, poor nutrition, lack of physical activity and excessive alcohol use. This was evident in the CHAT participants’ discussion of the interwoven relationship of many of these priority areas. By adopting strategies to influence these behaviors, we can ultimately impact multiple diseases (and perhaps priority areas) with coordinated strategies.
Resources Available
A detailed list of community partners is available in Appendix G. Key resources to address chronic diseases in the Tazewell County area include:
• Carilion health education programming
• Diagnostic, management and treatment services through healthcare systems
• Prevention and self-management education services
• Healthy behavior support services

Our Priority: Addressing Mental Health and Substance Use
Our prioritization process resulted in the elevation of mental health challenges, substance use and depression as focus areas. The following data indicates potential areas for opportunities.
Data shows need
• Residents of Tazwell County have a higher-than-average occurrence of:
o Mentally unhealthy days
o Cigarette smoking
o Depressive disorder
o Overdose deaths
Why This Matters
Community indicates need
• Community survey respondents indicated:
o Stress is a top health condition impacting their/their family’s health
o Mental health/substance use services would improve quality of life in our community
o High concern for access to inpatient substance use services
According to IHME research, drug use disorders are the number two cause of death and disability in the United States. Depressive disorders and anxiety disorders, both mental health challenges, are ranged at fifth and eighth, respectively.9 All of these health conditions have been worsening in recent years, especially in relation to the impacts of the COVID-19 pandemic
Chart 5 shows the average number of self-reported mentally unhealthy days from the CDC’s Behavioral Risk Factor Surveillance System (BRFSS), which is higher for Tazewell than Virginia’s state average. This metric helps illustrate the impact mental health has on residents’ quality of life. On average, county residents report experiencing a higher number of mentally unhealthy days (6.16) than physically unhealthy days (4.55).
The remaining data (Charts 6-8) shows that Tazewell County exceeds Virginia state averages in self-reported adult depressive disorder, cigarette smoking and overdose death rates.
Most overdose deaths were opioid-related and 5-year aggregate (2018-2022) Tazewell County rates for both all overdoses and opioid-related overdoses are nearly twice the rate of the state average for the same period This illustrates the continued disparate impact of the opioid epidemic on the county
9 United States | Institute for Health Metrics and Evaluation (healthdata.org)
Chart 5. Mentally Unhealthy Days



Chart 8. Deaths From Overdose

Key Drivers
Community partners identified many key drivers of substance use, including access to mental healthcare, mental healthcare challenges, access to medicated assisted therapy, poverty, trauma, mental health challenges and cultural norms. Identified drivers of mental health challenges included trauma, stigma, access to services, cultural norms and lack of social connections. Mental health and substance use are intertwined. Both areas can benefit from some of the same strategies, especially related to prevention. However, there are key differences in effective strategies with individuals who are actively experiencing challenges in those topic areas, which allows for all community partners to have a role in the work to address them.
Resources Available
A detailed list of community partners is available in Appendix G Key resources to address mental health and substance use in the Tazewell County area include:
• Counseling, treatment and prevention services
• Harm reduction and other recovery services
• Area prevention coalition (SATIRA)

Our Priority: Addressing Interpersonal Violence
Our prioritization process resulted in the elevation of interpersonal violence as a focus area. The following data indicates potential areas for opportunities
Data shows need
• Tazewell County is lacking data on assault deaths (homicides) due to low reported numbers
• Residents of Tazewell County have a higher-than-average occurrence of:
o Deaths from firearms
o Deaths from accidents
Why This Matters
Community indicates need
• CHAT participants indicate concern for intimate partner violence/child abuse and the resulting generational impact
• CHAT participants noted difficulties in measuring the need:
o Underreporting
o Data suppression
o Stigma/safety concerns
• Survey respondents indicate following top strengths of our community:
o Good place to raise children
The American Public Health Association issued a policy brief in 2018 recommended that violence be deemed a public health crisis.10 Since that time, data shows that violence in our communities has increased. Violence as defined by the policy brief refers to “the intentional use of physical force or power, threatened or actual, against oneself, another person, or against a group or a community, which either results in or has a high likelihood of resulting in injury, death, psychological harm, maldevelopment, or deprivation”. This encompasses a wide range of challenges including child maltreatment, elder maltreatment, intimate partner violence, bullying and broader community violence.
The impact of violence is far-reaching and includes not only the directly affected individual, but also those who are exposed indirectly and the community at-large. Gun violence, for example, continues to be an issue of national concern and negatively impacts entire groups of people in addition to direct victims. While CHAT partners did not raise firearms as a priority concern for Tazewell County, deaths from firearms are higher than the state average
Adolescents are especially at risk for experiencing violence and research has shown that children who experience violence are at risk for long-term physical, behavioral and mental health problems.11 Violence prevention strategies that protect children, therefore, can create lasting, even generational, improvements to their health and well-being.
10 https://apha.org/policies-and-advocacy/public-health-policy-statements/policy-database/2019/01/28/violence-is-a-public-healthissue
11 https://health.gov/healthypeople/objectives-and-data/browse-objectives/violence-prevention


Key Drivers
Community partners identified many key drivers of interpersonal violence, including lack of community support, lack of relationship/emotional regulation skills, mental health and substance use challenges, lack of family/social support, lack of community connection, trauma, unhealthy relationships and lack of support services Interpersonal violence can be very closely related to both SDOH and mental health and substance use challenges, further emphasizing the importance of cross-cutting strategies to address multiple health priorities.
Resources Available
A detailed list of community partners is available in Appendix G. Key resources to address interpersonal violence in the Tazewell County area include:
• Emergency shelter/transitional housing
• Law enforcement
• Crisis intervention team
Next Steps
Carilion Tazewell Community Hospital Health Improvement Strategy
As we continue to work with community partners, we will develop a Community Health Improvement Plan for Tazewell County, with expected completion before the end of calendar year 2024. Key focus areas will include not only the priority health outcomes, but also crosscutting ways to address those outcomes by improving access to care and addressing SDOH.
Carilion will also participate in planning processes with other community stakeholders to address health needs in conjunction with a hospital-specific plan.
Appendices
Account for patents without regard to insurance payments or FAP eligibility. 9
Assess the health needs of the community.
Identify significant health needs 9-12
Prioritize those needs. 12
Health needs include requisites for improvement of maintenance of health status in the community at large. Appendix F
Health Needs Include requisites for improvement of maintenance of health status in particular parts of the community. Appendix F
Identify resources potentially available to address them. Appendix G
Solicit and take into account input from persons representing the broad interests of the community, including those with special knowledge of public health.
Include all of the following sources to Identify and prioritize significant health needs and identify potentially available resources: Public health department official. 5, 9
Members of medically underserved, low-income, and minorities in community served, or individuals/organizations serving or representing them. 9-12
Written comments received on the hospital facilities most recent conducted CHNA and implementation strategy. 12
Document the CHNA in a written report that is adopted for the hospital facility by an authorized body.
Definition of community served and how this was determined. 7-9
Description of process and methods used to conduct the CHNA. 7-12
Description of how broad-interested community input was solicited and taken into account. 7-12
Description of the process and criteria used to identify needs as significant. 12, Appendix F
Prioritize the significant needs. Appendix F
Description of resources potentially available to address identified significant health needs. 18, 21, 24, Appendix G
Evaluation of impact of actions taken to address previous CHNAidentified significant health needs. 13
Describe the data and other information used in the assessment. 16-24, Appendix H
Describe the method of collecting and analyzing this data and information. 7-12
501R Requirement Page
Identify any CHNA- related collaborative or contracted parties n/a
Describe how Carilion takes into account input received from persons representing broad interests of the community:
Input provided. 7-12
How and over what time period input provided. 7-12
Name, nature, and extent of organizations providing input. 5, Appendix B
Describe medically underserved, low-income, or minority populations being represented by those providing input. 5, 9-10 Appendix B
Adopted by Board 3
Appendix B: CHAT List
Name
Organization Name
Brian Beck Appalachian Agency for Senior Citizens/Four County Transit
Holly Otsby Carilion Community Benefit
Nick Bilbro Carilion Community Benefit
Ashley Hash Carilion Community Benefit
Molly Roberts Carilion Community Benefit
Penny Shelton Carilion Community Health and Outreach
Karen Mulkey Carilion Community Health and Outreach
Alicia Bales Carilion Tazewell Community Hospital
Kim Brown Carilion Tazewell Community Hospital
Jennifer Bourne Clinch Valley Community Action
Jordan Dillon Cumberland Plateau Planning District
Anne Coates Department of Social Services
Curtis Breeding Industrial Development Authority (IDA)
Ema Johnson Project13Three
Matthew Brandt Tactical Retreat Unplugged
Keisha Cole Tazewell Chamber of Commerce
Erica Galloway Tazewell County Public Library
James C. Wilkes Tazewell County Public Library
Chris Stacy Tazewell County Public Schools
Teresa Stiltner Tazewell County Sheriff's Office
Randy Ann Davis Town of Tazewell Sheriff's Office- E911
Kathy Dalton VA Cooperative Extension
Kristen Gibson VA Cooperative Extension
Tammy Sparks VA Cooperative Extension
Cecil Peck Cumberland Plateau Health District
Paige Lucas Cumberland Plateau Health District
Victoria Bartfai Cumberland Plateau Health District
Daniel (Dan)
Hunsucker Cumberland Plateau Health District
Reisa L. Sloce Cumberland Plateau Health District
Susan Jewell Vibrant H&W Coaching
Organization Type
Transportation/Older Adults
Community Health ImprovementCarilion Clinic
Community Data Analysis - Carilion Clinic
Community Health ImprovementCarilion Clinic
Community Benefit - Carilion Clinic
Peer/CHW - Carilion Clinic
Health Education - Carilion Clinic
Healthcare - Carilion Clinic
Emergency Medicine - Carilion Clinic
Safety-Net Services
Planning/Development
Safety-Net Services
Transportation/Economic Development
Recidivism Reduction
Alternative Care - Mental/Behavioral Health
Local Business Representative
Community Spaces - Library
Community Spaces - Library
Public School K-12
Public Safety
Public Safety
Child Development - 4H
Family Consumer Science
Child Development - 4H
Public Health
Public Health (Data)
Public Health (Maternal and Child Health)
Public Health (Pop Health Coordinator)
Public Health
Private Health Coaching Service
Appendix C: Community Health and Well-Being Survey





Appendix D: Survey Results and Validation Methodology
Due to the nature of the Community Health and Well-Being Survey and its public availability through online methods, data validation was necessary. To validate survey responses, data was filtered by zip codes within Carilion’s entire service area. These responses were used for further data analysis
























Appendix E: Qualitative Data Results













Appendix F: Prioritization Table
Prioritization Survey Dot Voting Activity
Using their community knowledge, data collectively reviewed, and additional data shared, CHAT members were asked to complete an electronic survey to prioritize community health topics:
• The survey matched the structure utilized during the data walk at CHAT Meeting 2
• First prioritized broad categories, then specific topics within those categories
• CHAT facilitators ranked the following to develop results:
o Broad categories (resulting top 3 indicated by bold type below)
o Topics within each of the 3 top broad categories
o Remaining topics
• Results include:
o Top 3 topics of each of the top 3 broad categories
Method
o Top 5 topics of the remaining categories
Mental Health/Substance Use
• Substance use
• Poor mental health
• Depression Chronic Disease
• Overweight/obesity
• Diabetes
• High blood pressure Maternal/Child Health
• Teen pregnancy
• Infant mortality
• Low birthweight Injury/Violence & Infectious/Communicable Disease
• Domestic violence/Intimate partner violence
• Firearm injuries/deaths
• Motor vehicle crashes
• STIs
• Hepatitis C
Using the results of the Prioritization Survey, the group was asked to individually choose 5 topics to prioritize:
• The CHAT facilitators hung pages around the meeting room, each with one of the topics from the Prioritization Survey results.
• Each CHAT meeting attendee was given 5 dot stickers and instructed to place one sticker on each of the 5 topics they felt were most important to address in the next three years.
• After voting was completed, the CHAT facilitators quickly tallied and ranked the results.
• The CHAT was presented with the top 5-7 topics, unranked. The number of results presented depended on any ties and how closely votes were distributed. If topics were additional (i.e. not in the true top 5), CHAT facilitators noted this to the group and separated them visually on the screen.
Top 6 (ties present):
• Substance use
• Mental health
• Depression
• Overweight/obesity
• Diabetes
• Domestic violence/Intimate partner violence
Group Discussion
The group was asked to reflect on the results of the dot voting exercise. The following points were made during that discussion:
• Mental Health vs. Substance Use vs. Overdose
o Yes, mental health, substance use, and overdose are all intertwined, but so are many of the other identified areas (for example, STIs & Hep C w/Sub use)
• Violence in more general, not just domestic violence/Intimate partner violence
• Consider how certain communities/groups are impacted more than others:
o Food insecure
o Unstably housed
Top 5:
• Substance use
• Mental health (including depression)
• Overweight/obesity
• Diabetes
• Violence
*Results are not presented in any ranked order.
Appendix G: Resources to Address Prioritized Needs
Organization Organization Type Contact Information Programs/Services
CHRONIC DISEASE
A Child Shall Lead Them Food Pantry (276) 979-9541
Carilion Community Health and Outreach
Community HealthCarilion (540) 512-5200
Food Access
Chronic Disease Prevention Education
Stress Management Education Carilion Tazewell
Community Hospital Hospital - Carilion (276) 988-8700
Tazewell Community Health Federally Qualified Health Center (276) 979-9899
Tazewell Health Department Local Health Department (276) 988-5585
Virginia Cooperative Extension Cooperative Extension (276) 988-0405
Emergency Care
Diagnostic and Treatment Services
Primary Health Care (w/Medicare, insured, & sliding scale)
Community Health Education
Chronic Disease Prevention and Control Education
Nutrition Education
Food Safety Education
MENTAL HEALTH AND SUBSTANCE USE
Tazewell Community Health Center Federally Qualified Health Center (276) 979-9899
Tazewell Health Department Local Health Department (276) 988-5585
Clinch Valley Community Action Community Action (276) 988-5583
Cumberland Mountain Community Services Board Community Services Board (276) 988-7961
Project13Three Recidivism Reduction
https://www.project13th ree.com/
Virginia Cooperative Extension Cooperative Extension (276) 988-0405
INTERPERSONAL VIOLENCE
Tazewell Victim/Witness Victim/Witness Support (276) 385-1250
Clinch Valley Community Action Community Action (276) 988-5583
Tazewell County Department of Social Services Domestic Violence Services (276) 988-8500
New Day Recovery Center
Behavioral Health Care (w/Medicare, insured, & sliding scale)
Blood-borne pathogen and STI testing Community Education
24-hr Crisis Hotline: (276) 979-8959
Behavioral Health Care (w/Medicare, insured, & sliding scale)
Behavioral Health Care (w/Medicare, insured, & sliding scale)
Substance Abuse Services (Project Link & The Laurels)
Pastoral Care Recovery
Precovery (social support for youth)
Stress Management Education
Child Development/Parenting Education
Family Financial Education
Victim/Witness Advocacy & Support Violence/Crime Awareness
24-hr Crisis Hotline: (276) 979-8959
Family Crisis Services (domestic violence and sexual assault services)
Education and Community Outreach
Volunteer Advocate Program
Virginia Domestic Violence and Sexual Assault Hotline: 1-800-838-8238
Domestic Violence Prevention Program
Protective Services (Child, Adult)
Appendix H: Data Packets
The following pages include secondary data shared with the CHAT as well as chronic disease hospitalization data access through the Virginia Hospital and Healthcare Association (VHHA) Analytics data portal.
Key Takeaways- Secondary Data shared with the CHAT for Data Walk
Leading causes of death (2018-2021)
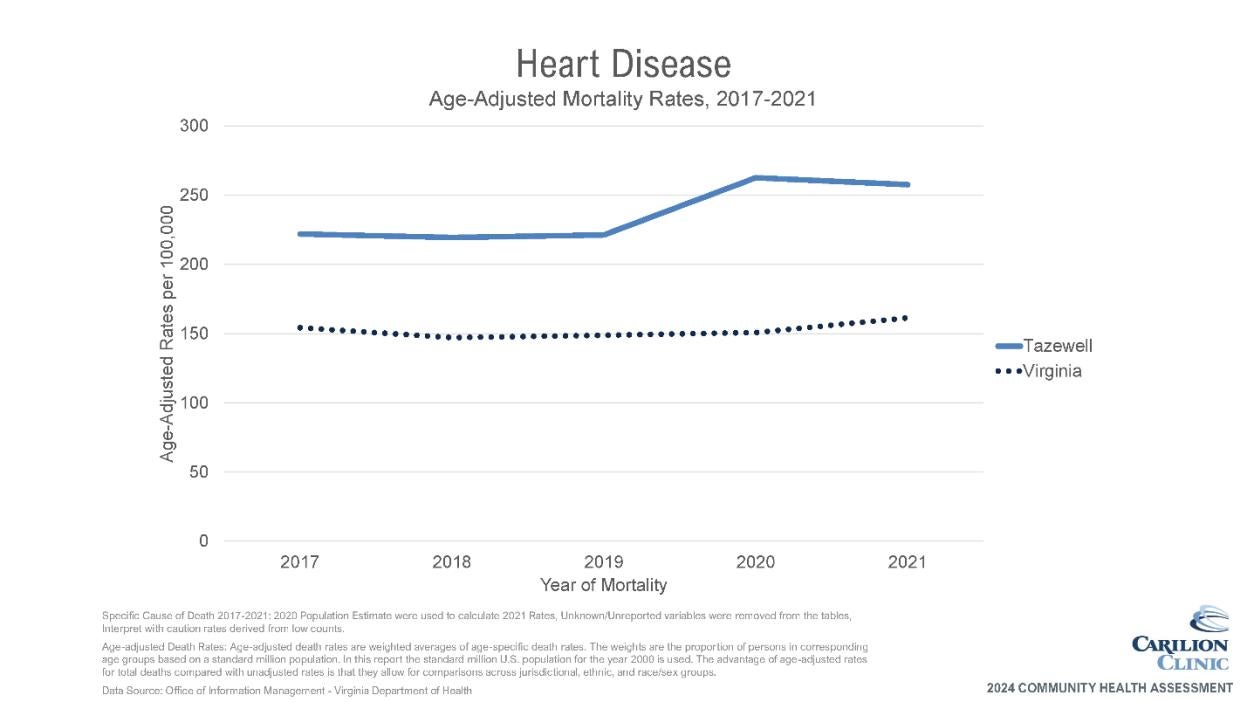
1. Diseases of the heart
2. Malignant neoplasms
3. Chronic Lower Respiratory Disease
4. Accidents (unintentional injuries)
5. COVID-19
Mental Health/Substance Use
• Overdose deaths have been climbing since 2019 and are much higher than state average
• Deaths due to drugs, alcohol, suicide are all about twice the state average
Maternal/Child Health
• Teen pregnancies are higher than Virginia but appear to be on the decline
• Potential disparity for low birthweight in the Black Non-Hispanic population
• High percentage of smoking during pregnancy
Injury/Violence
• Unintentional injury deaths are higher than Virginia across both sex and age groups
Infectious/Communicable Disease
• STIs (chlamydia, gonorrhea) are much lower Virginia average
• Rate of new diagnosis of hepatitis C infection also higher but may be steady or decreasing
Chronic Disease
• Cancer death rates appear to be higher than state average for both genders to varying degrees based on cancer type
• Chronic disease hospitalizations for hypertension and diabetes are higher than state average, as are chronic disease death rates (diabetes, COPD, heart disease)