On October 1st, we entered the “winter arc”. The term winter arc is slang and is not formally accepted by Merriam-Webster. This slang refers to that time of year when the temperature gets cooler, the days shorter, and is a time of the year to review your personal goals and develop a plan to build on healthy habits. Think of it as a preparation for those New Years Eve resolutions all too soon to come. For myself, I view this as a time to look back over the year personally and professionally; what have I accomplished in 2024 thus far and what do I want to accomplish going forward? This perfectly aligns with our own organizational performance review time, right? I would encourage our Within REACH readers to take a minute, breathe, congratulate yourself for your accomplishments. Take some time to think about your year, personally and professionally. You may even consider adding submitting to Within REACH as a personal or professional goal in the coming year :)
In this, the Fall/Winter issue of Within REACH, we want to remind you that Within REACH submissions are accepted on a rolling basis and that we accept stories and articles related to article critiques, human interest stories, literature reviews, evidence analysis, research, quality improvement, and proposed state or national legislation. Essentially, any story that aligns with our REACH professional model of practice is appropriate for peer review and publication. We would especially like to hear from those of you who have a potential Magnet story for our next certification! We want to keep the energy going and share in all of the good work you do for your patients and fellow nurses. By publishing in Within REACH, we have a recorded source of studies with outcomes and contact information and there is the potential to collect other stories for our next Magnet survey!
Editorial Chris Fish-Huson, PhD, RN, CNE Editor-in-Chief
7 Article: Comparison of the Verathon Bladder Scan PrimePlus and the BD BBS Revolution Bladders Scanner. Amy Lucas, Hunter D. Sharp, & Kathleen Manchin
13 Article: Executive Order Number Thirty Three- Establishing Cell Phone Free
3 Shine Awards
RECOGNITION/EVENTS
4 ANCC Magnet® Nurse of the Year Award Program
5 WOW Wall Curiosity, Compassion 6 WOW Wall Collaboration, Commitment
Citations & Recognitions
12 Awards/Offices held & Request for Magnet Conference Stories 16 Basic Research Classes 2024-2025 17 Where our Nurses have Presented
Virtual Journal Club
CarilionNursingResearchEditorialBoard:
Chris Fish-Huson, PhD, RN, CNE - Editor-in-Chief
Nancy Altice, DNP, RN, CCNS, ACNSBC
Desiree Beasley, MSN, RN, CCNS, CCRN
Sarah Browning, DNP, RN-BC
Charles Bullins, DNP, RN, AGACNPBC
Sarah Dooley, MPH, BSN, RN
Troy Evans, MSN, RN, CCRN, NHDPBC, NEA-BC
Cindy W. Hodges, MSN, RN-BC, FCN
James Ingrassia, MSN, RN
Lauren Miley, BSN, RN, PCCN
Laura Reiter, DNP, RN, CCRN, CNRN
Cindy Ward, DNP, APRN-CNS, RN-BC, CMSRN, ACNS-BC
Karyn Reese, CRMH—Nursing Director, 9 MTN PCU & Alicia Bales, CTCH—Senior Director of Nursing
A complete list of Shine Awards can be found here
Commitment!
The 4 South PACU enjoyed yet another Spirit Week! During the week of September 29th through October 4th PACU had our ThankFall Spirit week. Staff had treats throughout the week and a different theme each day. On that Friday we enjoyed an ORS Hotdog Tailgate! In PACU we get excited about our spirit weeks.
By: Amy Lucas, MSN, RN, CCNS, CCRN; Hunter D. Sharp, M.S.; Kathleen Manchin MPH, BSN, RN
Comparison of the Verathon Bladder Scan PrimePlus and the BD BBS Revolution Bladder Scanner
Background and Purpose
Bladder scanners measure bladder volume in order to identify and treat urinary retention (Saint et al 2016 & Yates 2016). Carilion has two types: Verathon and BD. Verathon has been used at Carilion for years and each nursing unit has at least one. The BD scanner is newer and two were purchased for pandemic units in 2020.
The use of these devices varies slightly. For the Verathon device, conductive gel is applied three inches above the pubic bone, live ultrasound identifies the bladder, and a scan determines volume. The device alerts the user to interfering conditions to prompt a rescan when indicated. The scanner is expected to report a volume that is within 7.5% of the actual volume in the bladder (Verathon 2016). For the BD device only the scanner head needs to be taken into the room, which can prevent cross contamination. For this device, the user applies conductive gel a few inches below the naval, applies pressure, and presses and releases the scan button. This scanner is reported to be accurate to within 12.5% + 12.5ml of the bladder volume (dBMEDx 2018).
The BD scanner is less expensive and offers reduced infection risk but there has been negative nursing feedback. This study aims to determine staff preference and if there is a clinically significant difference in the accuracy of the bladder scanners in a real-world setting. This will help with future purchasing decisions. Carilion Clinic Institutional Review Board determined that the study did not meet the definition of human-subjects research.
Method
Nursing staff on the two study units received education about each scanner and a QR code link to instructions was attached to the machines. During the comparison period each unit used one type of scanner exclusively for approximately 2 weeks and then used the other scanner exclusively for a few weeks.
There were no changes in patient care or documentation. A QR code with a link to a RedCap survey was attached to each scanner. Study team members entered patient scan and intermittent catheter volumes into a RedCap form. Volumes were included if the catheterization was completed within one hour of the scan. At the end of the study period, scanner accuracy and nurse surveys were reviewed.
The primary outcome of interest was staff preference and the difference in accuracy between scanners was secondary. Outcomes and overall statistical findings were descriptive and exploratory in nature, not warranting a power analysis for recommended group sample sizes. Numeric data was described as measures of central tendency and variation, while categorical data was described as frequencies and percentages.
Findings
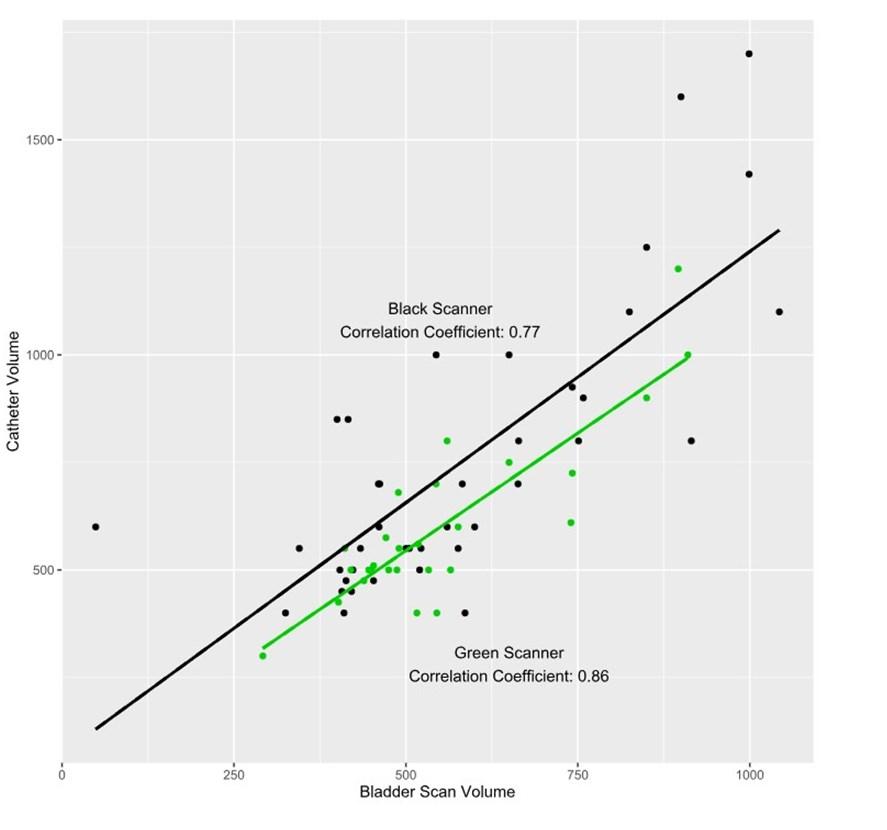
Thirteen people responded to the preference survey and 100% chose the Verathon scanner as the preferred scanner. 90% of those reviewing the BD and 67% of those reviewing the Verathon scanner reported receiving education. The most common concern related to BD scanner accuracy. Both scanners tended to underestimate the bladder volume, but the Verathon volumes had a better correlation. On average the Verathon scanner underestimated bladder volume by 49.63mL (range -304 to +145mL) and the BD scanner by 169.44mL (range -701 to +186mL).
The study team recommends continuing to use the Verathon bladder scanner. However, further nursing education is warranted. The staff on these two units received intensive education prior to the start of this study and even though delayed catheterizations likely affected results, the scan volumes were off by an average of 49.63mL, more than claimed by the company and volume differences ranged from 304mL less to 145mL more than the actual bladder volume. This difference is likely larger in units where staff have not received intense education. Underestimations could result in missed catheterizations and harm from bladder stretch injury, while excess catheterizations are time wasters and subject patients to unnecessary interventions. Staff knowledge and use of this device should be evaluated, and education done at regular intervals, including when onboarding.
Thanks to the bladder scanner comparison workgroup: Russell Beggarly, Brittany Spencer, Melissa Goad, Amber Janney, Bre Keck
Reference List
Ballstaedt L, Woodbury B. Bladder Post Void Residual Volume. [Updated 2023 Apr 23]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK539839/
dBMEDx BBS Revolution Operations and Maintenance Manual. (2018). https://static.bd.com/assets/product/Documents/ Urology%20and%20Critical%20Care%20(UCC)/PF10764_ud-revolution-ops-manual.pdf
Saint, S., Greene, T., Krein, S.L., Rogers, M.A.M., Ratz, D. Fowler, K.E., Edson, B.S., Watson, S.R., Meyer-Lucas, B., Masuga, M., Faulkner, K., Gould, C.V., Battles, J., and Fakih, M.G. (2016). A program to prevent catheter-associated urinary tract infection in acute care. TheNewEnglandJournalofMedicine , 374(22), 2111-2119. DOI: 10.1056/ NEJMoa1504906.
Verathon Bladderscan Prime Plus Operations and Maintenance Manual. (2017). https://www.verathon.com/sites/default/ files/2021-12/0900-4510-xx-60.pdf
Yates, A. (2016). Using ultrasound to detect post-void residual urine. NursingTimes,112 (32/33/34), 16-19.
Scatter Plot of Scan Results vs Catheter Volume
*green scanner= Verathon *black scanner= BD
Characteristic
Staff Survey Results
Scanner (Black), N = 101
Please rate the bladder scanner with 5 being the best and 1 being the worst.
What circumstances seemed to affect the accuracy of the bladder scanner?
If other, please specify.
scanner doesn't show bladder size like green one
to find correct spot.
Was there a circumstance when it was not appropriate to use the bladder scanner?
Scanner (Green), N = 31
Anything that you want us to know about the bladder scanner? Bladder scan was off by over 200 mL each scan.
not seem to be as accurate as the green scanner
I don't think it's accurate.
Did you receive education about the scanner?
Which scanner do you prefer
1 n (%)
2 0 2 4
N U R S I N G R E S E A R C H
C O N F E R E N C E
Date: November 21, 2024
Time: 8:30A 4:00P
Location: CRMH, 6th Floor
Auditorium
Register in Cornerstone
Sparking Innovation & Engagement in Nursing Research and EBP
Conference Objectives:
• Identify one or more resources available to support efforts in conducting Nursing Research and EBP.
• Identify a practice problem or challenge that nursing research or EBP might impact outcomes.
• Report an increased confidence in participating in nursing research or EBP study.
Conference Keynote:
Kimberly Ferren Carter, PhD., R.N.
May 2024 - September 2024 (& past presentations not noted prior to this edition)
Bath, J. (2024, May 18). When medicine and law collide. [Oral presentation]. Franklin County EMS Education Weekend. Rocky Mount, VA.
Bath, J. (2024, May 18). Just breathe...chest trauma and the pulmonary system. [Oral presentation]. Franklin County EMS Education Weekend. Rocky Mount, VA.
Bath, J., Weppner, J., Martinez, M., Collier, B., Harvey, E., & Mishra, V. (2024, June 14). Factor impacting mortality and withdrawal of life sustaining care in severe TBI. [Oral presentation]. The Carolinas-Virginias Chapter of the Society of Critical Care Medicine’s 2024 Annual Symposium. Myrtle Beach, SC. *won second place for research snapshots!
Bath, J., Downey, W., Farris, B., Pennington, D., & Harvey, E. (2024, June 14). Trauma boot camp to improve knowledge, skills, confidence and frequency of unplanned intensive care admissions. [Oral presentation]. The CarolinasVirginias Chapter of the Society of Critical Care Medicine’s 2024 Annual Symposium. Myrtle Beach, SC.
Lewis, O. (2024, August 8-9). Life saving rural trauma tips. [Oral presentation]. Drive Smart Distracted Driving Summit. Richmond, VA.
Bath, J. (2024, August 9-10). Diaphragmatic Pacing. [Oral presentation]. Respiratory Nursing Society and International Collaboratives 31st Annual Educational Conference. Roanoke, VA.
Bond, D. (2024, August 9). Is Buprenorphine one of the answers to the opioid crisis? [Oral presentation]. Respiratory Nursing Society and International Collaboratives 31st Annual Educational Conference. Roanoke, VA.
Ramsey, K. (2024, September 19). Protecting neonatal skin and thermoregulation. [Oral Presentation]. NICU Neurodevelopmental Care Conference. Roanoke, VA.
Harvey, E. (2024, September 30). Priorities of care for SCI in the ICU. Invited speaker. [Conference session]. American Association of Neuroscience Nurses Amplify: A Virtual Conference. Virtual.
McCallister, A. (2024, April 8-11). The impact of structured nurse leader development post-COVID. [Poster presentation]. American Organization of Nurse Leaders 2024 Inspiring Leaders Conference. New Orleans, LA.
Ashwell, B. (2024, April 9). Readiness to practice: S.O.A.Ring to the next level. [Poster presentation]. Carilion Clinic Research Day. Roanoke, VA.
Andrews, S. (2024, April 19). Implementing bedside handoff and improved patient experience. [Poster presentation]. Pathways to Knowledge Nursing Education Conference. Richmond, VA.
Ashwell, B. (2024, April 19). Readiness to practice: S.O.A.Ring to the next level. [Poster presentation]. Pathways to Knowledge Nursing Education Conference. Richmond, VA
Ryan, E. (2024, April 19) Improving patient falls in the ambulatory care setting. [Poster presentation]. Pathways to Knowledge Nursing Education Conference. Richmond, VA.
Lewis, O. (2024, April 28-29). The impact of school -based injury prevention curriculum on older adolescent related MVC mortality. [Poster presentation]. 10th Annual Injury and Violence Prevention Professionals Symposium. Nashville, TN.
May 2024 - September 2024
Harvey, Ellen M., Neuroscience CNS & Bath, Jen, Trauma CNS have completed the International Global Neuro Certificate Course – Fundamentals of Neurotrauma Care for Nurses, inaugural class September 2024.
Contact Chris FishHuson with your ideas so that we can find funders to support you!
Executive Order Number Thirty Three- Establishing Cell- Phone Free Education to Promote the Health and Safety of Virginia’s K-12 Students.
By: Jennifer E. Law, BSN, R.N.
On July 9th, 2024 Virginia Governor Glenn Youngkin issued an executive order charging stakeholders in health and education to define and implement “cell-phone free education” in Virginia public schools. These stakeholders included the Virginia Department of Education, the Virginia Department of Health and Human Resources, and the State Health Commissioner. In effect, this order bans K-12 students from accessing their phones during the school day, or “bell to bell”. Youngkin’s order specifically requires that these entities create a definition of cell-phone free education that includes the “elimination or severe restriction” of cell phones by students during class time. The order also states that these entities are to create model plans whereby Virginia school districts could implement said elimination or restriction. These plans are then to be implemented in all Virginia school districts at the latest by January 1st, 2025. Finally, Youngkin’s order requires the Department of Health to deliver information to the Virginia public highlighting the effects of excessive cell phone usage on children’s mental and physical health.
This executive order follows on several independent initiatives by Virginia school boards to prohibit cell phone usage in schools. For example, Senate Bill 28, introduced by Virginia state senator William M. Stanley Jr., was brought to the Virginia State Senate in December 2023 and referred to the Committee on Education and Health. SB 28 would “permit[s] each school board to develop and implement a policy to prohibit the possession or use of cell phones and other handheld communication devices during regular school hours.” The bill died in committee however, and was not brought to a vote.
Youngkin’s order comes at a time when the deleterious effects of cell phone usage on children are slowly gathering societal recognition. Several examples of these effects are highlighted in the document. Citing data from the American Psychological Association (APA), the order notes that social media usage among children averages
4.8 hours per day. This is a significant statistic. Research shows that adolescents that use social media for greater than three hours per day have a doubled risk of poor mental health (U.S. Department of Health and Human Services, 2023). In tangible terms, the decline of adolescent mental health in the past ten years, of which social media is a proven contributor,, has resulted in sky-rocketing suicide rates. Over the past decade, suicide rates have increased 167% for females and 91% for males (Exec. Order No. 33, 2024). Suicide is now the second leading cause of death in America for children and adolescents between the ages of 10 and 19 (McBride, 2020).
The evidence demonstrating the declining mental health of children in America is manifest. A 2020 study published in Pediatricsfound that over the preceding decade, emergency department visits for children between 5 and 17 years of age seeking mental health care increased by 60%; visits for anxiety disorders by 117%; visits specifically for self-harm by 325% (Lo et al., 2020). This massive increase in patients seeking mental health services has in many cases overwhelmed health care resources. For example, a 2018 study found that less than half of children that received a psychiatric diagnosis in an emergency department had a follow-up visit with a provider within a week, despite evidence showing that the risk of suicide is highest following a discharge (McBride, 2020). In many cases there are simply not enough resources to meet demands. According to an article published in PsychiatricServicesin 2009, over 77% of counties in America have a “severe shortage of mental health providers” - and this in 2009, a decade before the surge in mental health needs occurred (Thomas, et al., 2009).
Governor Youngkin’s executive order is a concrete attempt to address these appalling statistics. It is an immediate and substantial way of reducing the amount of time children spend on their phones. Cell phones have been demonstrably proven to have deleterious effects on health; allowing children constant unrestricted access to them is unconscionable. It is to be hoped that this measure will improve some of the mental health issues faced by Virginia children and in turn alleviate some of the burden on the healthcare system. However, the executive order only addresses personal cell
Phone use in public schools. It does not address the time children spend on school approved screens during instructional time. It might be wise for the stakeholders involved, such as the Virginia Department of Education, to examine the unbridled use of screens in public school instruction in order for students to experience the greater benefits offered by time spent entirely away from screens.
Executive Order No. 33. (2024).
https://www.governor.virginia.gov/media/governorvirginiagov/governor-of-virginia/pdf/eo /EO-33 -Cell-Phones-7.9.24.pdf
Lo, C.B., Bridge, J.A., Shi, J., Ludwig, L., & Stanley, R.M. (2020). Children’s Mental Health Emergency Department Visits: 2007 2016. Pediatrics145 (6).
https://doi.org/10.1542/peds.2019-1536
McBride, Deborah L., (2020). Emergency Department Preparedness for Children Seeking Mental Health Care. JournalofPediatricNursing,September October; 54: 106 108. https://doi: 10.1016/j.pedn.2020.07.007
Senate Bill No. 28. (2023). https://lis.virginia.gov/cgi-bin/legp604.exe?241+sum+SB28
Thomas, K.C., Ellis, A.R., Konrad, T.R., Holzer, C.E., & Morrissey, J.P. (2009). Cou-Level Estimates of Mental Health Professional Shortage in the United States. Psychiatric Services, Volume 60, Number10. https://doi.org/10.1176/ps.2009.60.10.1323
U.S. Department of Health and Human Services. (2023, May 23). SurgeonGeneralIssuesNew AdvisoryAboutEffectsSocialMediaUseHasonYouthMentalHealth .
https://www.hhs.gov/about/news/2023/05/23/surgeon-general-issues-new-advisoryabout-effects-social-media-use-has-youth-mental-health.html
Basic Research for the Healthcare Professional NR-CE333L
Thursday, December 19, 2024, 8A—12P
Thursday, February 20, 2025, 12P 4P (in-person)
Thursday, April 24, 2025, 4P 8P
Dissemination of Research and QI Studies NR-CE374L
Tuesday, February 18, 2025, 12P 3P
Developing Professional Posters NR-CE238L Tuesday, March 18, 2025, 12P – 2P
Developing a Competitive Abstract NR-CE335L
Thursday, March 20, 2025, 12P—3P
Nursing Research for Leadership NR-CE165L
Thursday, April 17, 2025, 2P – 4P (in-person)
Appraising & Synthesizing the Literature NR–CE372L
Thursday, May 22, 2025, 1P 4P
In Cornerstone, you may view each class description and the class objectives, and enroll by completing the class registration.
*All classes are held virtually unless otherwise noted as in-person.
“The World is a book, and those who do not travel read only a page.” – Saint Augustine
Practical Applications of Nursing Inquiry
Palm
United Kingdom
Lake Buena Vista
Williamsburg
Natl. Harbor, MD
Greenville
Nottingham
Anaheim
Aurora
VA 202 HOUSE BILL 971 “Nurse practitioners; patient care team provider, autonomous practice.”
By: Emily M. Ayles, R.N., ASN
Bill Summary from Bill List - Virginia Nurses Association:
“Nurse practitioners; patient care team provider; autonomous practice. Allows certain nurse practitioners to oversee patient care teams by changing "patient care team physician" to "patient care team provider." The bill defines "patient care team provider" as a patient care team physician, as defined in relevant law, or a nurse practitioner who meets certain requirements. The bill also lowers from five years to two years the amount of fulltime clinical experience required before an advanced practice registered nurse may practice without a practice agreement.”
Bill 971 is written to allow for the independent practice of advanced nurses once meeting required practices. This bill once passed allows for independent practice of an advanced nurse, i.e., Nurse Practitioner, without an overseer of a medical doctor. Before this legislative request, Nurse Practitioners needed a medical doctor to oversee all medical recommendations, practices, and prescriptions meaning a medical doctor was to sign off, or approve, all the practitioners work. With this bill being passed it now frees up the medical doctor who was overseeing the care to not have to double his work so he can focus on his patient’s and his own practices. This also will allow for more medical practices to open thus allowing access to healthcare to increase. With the allowance of advanced care nurses practicing on their own, once meeting the requirements, it can help relieve some of the stress of health care crisis and cut down on waitlists in offices.

The Research Council has a virtual journal club to provide an opportunity to read and discuss issues of concern or interest in healthcare. ! Using the Teams platform will allow participants to post their comments and opinions when it is convenient for them.
We hope to have a new discussion beginning every one to two months. There is a channel for each new topic with the article posted in the Files section. Discussion questions for the article will be located in the Notes. A separate tab will give access to the evaluation form. Please complete the evaluation to let us know your opinion about the journal club and what future topics you’d like to discuss.
CheckoutthelatestarticlebygoingtoTeamsandsearchingfor HealthcareHotTopicsJournalclub,selectSeptember2024Discussion, thenfilefromthetoptoreadthearticle,andbacktopostfordiscussion.
Participation in a journal club can be used to fulfill the Research criteria for RN 2. Leading a journal club discussion can be used to fulfill the Research criteria for RN 3.
Questions? Contact:
Chris Fish-Huson– Senior Director email: cdhuson@carilionclinic.org phone: 540-981-7536
Virtual Healthcare Hot Topics Journal Club!
Chris Fish-Huson, Ph.D., R.N., CNE, NASM-CPT
RN 2
Emily Ayles, RN, ASN, RMH 6S OP Surgery
Sheena Booth, RN, BSN, RMH 6W
Heather Brogan, RN, BSN, RMH 7S PCU
Martha Gibbs, RN, ASN, PCCN, RMH 7S PCU
Alexandria Gilmore, RN, ASN, Giles OR
Susan Hornsby, RN, BSN, Presurgical Testing
Emory Jones, RN, BSN, Infusion Center
Jennifer Law, RN, BSN, Giles ED
Scotti Lawson, RN, ASN, NRV Resource Pool
Alicia Lee, RN, ASN, NRV O-P Prep
Missy Mcguire, RN, ASN, Giles Med-Surg
Sarah Minnick, RN, ASN, RMH 7S PCU
Mckenzie Najjar, RN, BSN, PCCN, RMH 7S PCU
April Overfelt, RN, ASN, RMH, 7S PCU
Kristen Price, RN, BSN, Radiation Oncology
Joshua Roark, RN, ASN, Giles OR
Megan Rosenbloom, RN, BSN, RMH 7S ICU
Tracy Scruggs, RN, ASN, Presurgical Testing
James Sensabaugh, RN, ASN, Rockbridge ED
Jessica Shrewsbury, RN BSN, RMH PACU
Colleen Spencer, RN, BSN, Rockbridge ED
Sara Trent, RN, ASN, Giles ED
Kristy Waldron, RN, BSN, Presurgical Testing
Brittany Williams, RN, ASN, NRV Medical
RN 3
Stephanie Defilippis, RN, BSN, OCN, Infusion Center
Chastity Fontaine, RN, BSN, CEN, Giles ED
Sara Grimsley, RN, BSN, PCCN, RMH 7S PCU
Jamie Jamison, RN, BSN, CCRN, Franklin ICU
Ann Jimenez, RN, BSN, CEN, CCRN, Giles ED
Christy Rodgers, RN, BSN, CMSRN, NRV Medical
Katelin Walls, RN, MSN, CCRN-CSC, CNL, RMH
6S ICU
RN 4
Rebecca Dampeer, RN, BSN, CCRN, RMH 7S ICU
Sandra Hubbard, RN, BSN, TCRN, RMH 9S ICU