Annual Academic Report 2015-16





The year 2016 marked the 20th anniversary of Connecticut Children’s Medical Center. Since opening on April 2, 1996, the center has experienced tremendous growth and achieved national recognition for comprehensive, world class care of patients and their families.

Dear Colleagues and Friends,
It is with great pleasure that we present the seventh annual report from the Department of Pediatric Surgical Subspecialties of Connecticut Children’s Medical Center and the third combined report with the Department of Pediatrics. This report continues to reflect the solid alignment between surgery and pediatrics and the continued multi-disciplinary growth of combined surgical and pediatric programs at Connecticut Children’s Medical Center.
The year 2016 marks my first as the Surgeon-in-Chief, and I am inspired by the challenge. I am fortunate to be part of a fantastic Department of Surgery with numerous innovative, bright, and enthusiastic surgeons. Connecticut Children’s Medical Center is poised for exponential growth and opportunity over the next several years, and I am excited to be part of this journey.
Over the last two years, the surgical services have continued to experience growth, performing procedures on over 9,000 children annually with 1,718 cases performed in 2016 at our new ambulatory surgery center in Farmington, CT. We continue to aggressively pursue our vision to bring the very best surgical care to the children of the region while simultaneously pursuing our two other core missions: research and education.
Some specific highlights from the past two years:
We have seen expansion of our surgical services through the recruitment of some of the “best and brightest” in their respective fields. We have successfully recruited two pediatric urologists from top national programs – Dr. Carlos Medina from New York Methodist Hospital, Weill Cornell Medical College, and New York Presbyterian Hospital, and Dr. Anne Dudley from Vanderbilt University in Nashville, TN. Additionally, Dr. Sonia Chaudhry is completing a hand fellowship that will further broaden the expertise in the Division of Orthopedics.
Innovation through research is integral to the mission of the department. We continue to focus efforts on children with solid tumors, premature lung disease, esophageal
disease, otitis media, injury prevention, and sports-related injuries. Several federal grants and invention patents were submitted over the past two years focusing on diagnosis and treatment of these diseases. We also have established research collaborations with Biostage, working on a new way to engineer esophageal tissue, and with the Massachusetts Institute of Technology to improve our ability to diagnose otitis media. Finally, we have developed an Innovation Center to harness new ideas generated by the faculty.
Connecticut Children’s Medical Center remains the exclusive site for pediatric surgical subspecialty training for the University of Connecticut School of Medicine surgical residency programs. Annually, dozens of residents from the University of Connecticut and other institutions receive their required pediatric surgical experience at Connecticut Children’s. The Pediatric General Surgery, Pediatric Orthopedics, and Pediatric Urology programs continue to train the future leaders in surgical subspecialties and have graduated several successful fellows since the last report. Additionally, Pediatric Anesthesia has begun its fellowship training program, and we look forward to welcoming their first trainee.
As we continue to champion innovative programs and serve as educators for the next generation of pediatric surgeons, we remain focused on providing the highest quality, state-of-the-art care for children of the region.
Sincerely,
Christine Finck, MD, FACS
Donald Hight, MD, Endowed Chair of Pediatric Surgery
Surgeon-in-Chief
Executive
Vice President
Connecticut Children’s Medical Center
Associate Vice Chair of Surgery, University of Connecticut School of Medicine
The years 2015 and 2016 brought exciting clinical advances, expansion to new regions of Connecticut, recruitment of some of the best and brightest, and great strides in research and education.
Dear Colleagues and Friends,
It is my pleasure once again to share with you the highlights of two remarkable years of growth, innovation and progressive change for the faculty and staff of the Department of Pediatrics at the University of Connecticut School of Medicine and at Connecticut Children’s Medical Center. As you page through this report, my third as Chair of Pediatrics and Physician-in-Chief, you will see that 2015 and 2016 brought exciting clinical advances, expansion of our services to new regions in the state of Connecticut, recruitment of some of the best and brightest in pediatric specialties, and great advancements in research and education for the faculty and staff of the Department of Pediatrics. On these pages, I am also pleased to highlight the contributions of our colleagues in Surgical Specialties, Anesthesiology and Radiology. There have been several notable honors and achievements over the last two years. To name a few, in 2015, our highly successful Joint Commission Survey results confirmed that our commitment to providing care in an environment of safety and quality at Connecticut Children’s ranks among the nation’s best. Surveyors complimented us for having “the best results of any survey conducted in the 2015 calendar year.” In 2016, Connecticut Children’s Medical Center was identified as one of the most technologically advanced children’s hospitals in the world by TopMastersInHealthcare. com with a ranking of #21. Not to be overlooked, for the sixth year in a row, Connecticut Children’s was named to U.S. News & World Report 2015-2016 Best Children’s Hospitals rankings.
Connecticut Children’s welcomed more than 20 new physicians across many specialties. Among them, we’re proud to count four nationally recognized clinicians and researchers. Dr. James Moore, an acclaimed neonatologist and researcher, was recruited from the Children’s Medical Center of Dallas to serve as the head of the Division of Neonatology. Dr. Ching C. Lau, leading oncologist and cancer researcher, joined our staff in 2016. Dr. David A. Weinstein, pediatric endocrinologist, scientist, and the world’s top researcher on Glycogen Storage Disease (GSD) also joined Connecticut Children’s. Dr. Emily Germain-Lee, an internationally known
pediatric endocrinologist and scientist specializing in the clinical care and translational research of genetic and metabolic bone diseases, was welcomed in 2016 and is the new division head of the Endocrinology Division. We also honored four faculty members who retired over the past two years: Dr. Victor Herson, chief of the Division of Neonatology, Dr. Susan Ratzan, chief of the Division of Endocrinology, Dr. Gigi Burke, head of the Department of Research, and Dr. Michelle Cloutier, former chief of the Division of Pulmonary Medicine and director of the Asthma Center. We are indebted to them for their steadfast support of the Department of Pediatrics and our Children’s Hospital.
The largest clinical site of the division, the Primary Care Center at Connecticut Children’s, received National Committee for Quality Assurance (NCQA) Level 3 Medical Home recognition in 2015. In achieving that recognition, the center met rigorous standards set by the NCQA and was recognized for coordinating patient care, maintaining a high level of quality in service delivery, and ensuring that patients and families remain at the center of all care. In 2016, we began a partnership with Community Health Center (CHC), a federal qualified health center headquartered in Middletown, CT, to continue to provide the children and families of Hartford primary pediatric care, and we will further expand the scope of that care to include enhanced behavioral health and dental services. This partnership with CHC also will bring significant new funding from the federal government to support improved health care for the children of Hartford. Regionally, for the convenience of our patients and their families, and to better serve the children of Connecticut, we expanded our services to more areas of the state. In 2016, in collaboration with UConn Health Center, we opened Connecticut Children’s Primary Care clinics in East Hartford and West Hartford.
The tremendous work done by several of our divisions continues to receive national recognition for its uniqueness, innovation, and quality of care. In the Infectious Diseases and Immunology Division, our Ryan White program’s work for youth and adolescents at risk of and infected with HIV has been recognized internationally for its novel initiatives in identifying and caring for high-risk individuals. Under the
direction of the Endocrinology Division’s Dr. Cem Demirci, our Diabetes Education Program was reaccredited by the American Association of Diabetes Educators, one of only three programs certified in Connecticut in 2015, and the only one dedicated to the care of children and adolescents with diabetes. In the Pulmonology Division, under the leadership of Dr. Craig Schramm, our Central Connecticut Cystic Fibrosis Center continues to be one of the Top 10 CF centers in the country based on combined pulmonary and nutritional outcomes. Two physicians in our Cardiology Division, Drs. Shai Upadhyay and Felice Heller, were among the first group of cardiologists in the country to receive board certification in Adult Congenital Heart Disease, a newly recognized sub-specialty of the American Board of Internal Medicine. In December of 2015, the American Academy of Sleep Medicine congratulated Connecticut Children’s Sleep Center on meeting the high standards required for receiving accreditation as a sleep disorders center. In spring of 2016, we opened our Neurodiagnostic and Sleep Lab, offering state-of-the-art equipment and resources to provide the best quality diagnostics.
The Division of Digestive Diseases, Hepatology and Nutrition, under the pioneering leadership of Dr. Jeffrey Hyams, continues to be a national and international leader. The division’s Center for Pediatric Inflammatory Bowel Disease (IBD), the largest program in the region between Boston and New York, currently provides care to over 800 children with Crohn’s disease and ulcerative colitis. It remains the Clinical Coordinating Center for a $10.4 million grant from the National Institutes of Health to lead the PROTECT Study: Predicting Response to Standardized Pediatric Colitis Therapy. This five-year effort coordinates the resources of 29 leading pediatric IBD centers in North America to study newly diagnosed children with ulcerative colitis.
Led by Dr. Heather Schlott, our extracorporeal membrane oxygenation (ECMO) program, in partnership with Pediatric Surgery and Neonatology physician colleagues, as well as nursing, respiratory therapy, and perfusion team members, has grown and been extremely successful, with outcomes that exceed national benchmarks. Connecticut Children’s received a Silver Award (the highest award possible for our
size program) for its excellent outcomes from the national Extracorporeal Life Support Organization.
We also successfully introduced several new services to better serve our patients and families. In 2016, we launched a new sedation unit to help our patients manage the stress and challenges of medical procedures. The Cardiology and Hematology-Oncology divisions at Connecticut Children’s are collaborating to develop a cardio-oncology program (Cardiovascular Oncology Prevention Experience, COPE). This initiative, under the leadership of Drs. Olga Toro-Salazar and Andrea Orsey, aims to prevent and/or minimize heart damage caused by chemotherapy, and consequently reduce cardiac morbidity and mortality in childhood cancer survivors. A new biotech center also has been opened. It currently houses four investigative researchers, all working to find ways to treat and prevent childhood illnesses. Our Emergency Medicine Division instituted a direct bedding process, which has produced substantial improvements in time metrics, most notably at the front end of the process such as arrival-to-provider times. As a result, we have had stellar performance in our Left Without Being Seen (LWBS) rates.
In the area of international outreach, 2016 saw the creation of Connecticut Children’s Center for Global Health, led by Dr. Adam Silverman and Karen Callahan, BAS, BSN, MHS, RN, CPN. Focusing primarily on reducing morbidity and mortality in medically underserved populations, the center supports the activities of faculty and staff while working with partners to build in-country capacity to reduce major causes of child morbidity and mortality globally.
The National Science Foundation (NSF) awarded a $213,071 grant to Connecticut Children’s Dr. Christine Ohannessian for support of the project entitled “Collaborative Research: Bidirectional Effects Between Parental Work-Family Conflict and Adolescent Psychosocial Adjustment.” This is the first NSF grant received by Connecticut Children’s. Dr. Ohannessian was named director of the new Behavioral Research Center at Connecticut Children’s Medical Center.
As in years past, our educational efforts had tremendous
impact at the undergraduate, graduate and professional levels. Under the direction of Dr. Melissa Held, 3rd and 4th year medical students continued to have outstanding training and experience in their clinical rotations at Connecticut Children’s. Their rotations continue to be among the most highly rated at the School of Medicine and each year approximately 20% of the fourth year graduating class choose a career in Pediatrics or a Pediatrics-combined residency program. The residency program, led by Dr. Edward Zalneraitis, and Assistant Program Directors, Drs. Christine Skurkis, Sharon Smith, Patricia Joyce and Mark Greenstein, continued to attract talented participants who achieved highly, and went or will be going on to valued practices and highly desirable fellowships. The program is active in improving assessment, scholarship, resident and faculty well-being and procedural competence. Fellowship coordinators Jack Wakefield, Marianne Custer, Opeyemi Aina, Lindsay Haythorn and Amanda Ross supported 11 pediatric subspecialty fellowships which graduated 11 talented fellows and successfully filled 15 of 21 available fellowship positions. Pediatric Anesthesiology and Pediatric Infectious Diseases Fellowship Programs were newly accredited in 2015 and 2016.
The Office of Continuing Medical Education, supported by Deirdre Palmer, Diane Mouradjian, and Kenneth Spiegelman, MD, accredited a total of 756 hours of instruction to 2,079 individual participants for a total of 27,568 contact hours. In 2015, Grand Rounds were made available via live streaming online which resulted in a 23 percent greater reach of our weekly lectures across the state. In 2016, thanks to generous support from the Ahearn Family Foundation, Grand Rounds were made available via podcast.
In all of our endeavors, we are grateful for the support and assistance of the academic leadership at the UConn School of Medicine and UConn Storrs; our new CEO, Jim Shmerling; the Executive Management Team; and the board of directors at Connecticut Children’s. I also wish to thank the staff of the Division of Academic Administration, under the outstanding leadership of Annamarie Beaulieu, MPH, and the administrative team for the Department of Pediatrics to whom I owe an ongoing debt of gratitude, Esperanza Lesmes, Rachel Cunningham, Laurie Papacs, and There-
sa George, for everything they do to keep things running smoothly. Finally, my sincere thanks go to Gigi Burke, PhD, who retired in 2016 from her role as head of the Division of Research, and associate chairs Drs. Karen Rubin and Francis DiMario, who have provided a guiding light in the many endeavors required of my office. I am indebted to Lisa Benson, senior director of Research Operations and Sponsored Programs, who has done a tremendous job as the interim head of the Division of Research while a national search for a chief research officer is underway. I am also thankful to Justin Radolf, MD, professor of Medicine and Pediatrics, and senior scientific advisor at Connecticut Children’s, for his energy, steadfast support and mentorship of our faculty, and stewardship of our research enterprise.
Congratulations to you all for two outstanding years. I look forward to 2017 with great enthusiasm and in anticipation of the wonderful possibilities that await us.
Sincerely,
Juan C . Salazar, MD, MPH, FAAP
Professor and Chair, Department of Pediatrics
University of Connecticut School of Medicine
Executive Vice President of Academic Affairs
Physician-in-Chief
Connecticut Children’s Medical Center

On November 2, 2015, Connecticut Children’s welcomed its new President and Chief Executive Officer James E. Shmerling. His appointment marked the culmination of a national search that began with a list of 300 candidates. Shmerling replaced Marty Gavin, who retired after serving as President and CEO of Connecticut Children’s for nine years.
In 2015-16, Connecticut Children’s hired more than 20 new physicians across many specialties.
In 2015, Connecticut Children’s highly successful Joint Commission Survey results confirmed that the medical center’s commitment to providing care in an environment of safety and quality ranks among the nation’s best.
In 2016, Connecticut Children’s Medical Center was identified as one of the most technologically advanced children’s
hospitals in the world by TopMastersInHealthcare.com with a ranking of #21.
Connecticut Children’s was named to U.S. News & World Report 2015-2016 Best Children’s Hospitals rankings for the sixth year in a row with the report recognizing the Urology program.
In December of 2015, the American Academy of Sleep Medicine accredited Connecticut Children’s new Sleep Center.
The National Science Foundation (NSF) in December 2015 awarded a $213,071 grant to Dr. Christine Ohannessian for support of the project entitled “Collaborative Research: Bidirectional Effects Between Parental Work-Family Conflict and Adolescent Psychosocial Adjustment.” This is believed to be the first NSF grant received by Connecticut Children’s.
The largest clinical site of the division, the Primary Care Center at Connecticut Children’s, received National Committee for Quality Assurance (NCQA) Level 3 Medical Home recognition in 2015.

Under the pioneering leadership of Dr. Jeffrey Hyams, the Division of Digestive Diseases, Hepatology and Nutrition, continued its role as a national and international leader. The division’s Center for Pediatric Inflammatory Bowel Disease (IBD) provides care to over 800 children with Crohn’s disease and ulcerative colitis. It remains the Clinical Coordinating Center for a $10.4 million grant from the National Institutes of Health to lead the PROTECT Study: Predicting Response to Standardized Pediatric Colitis Therapy.
Dr. Jasmeet Mokha, a graduate of the Digestive Diseases, Hepatology and Nutrition fellowship program and now an attending physician, published novel work concerning the relationship of the intestinal microbiome and cholestasis in premature infants receiving parenteral nutrition. Dr. Mokha won the Nutrition Award at the World Congress of Pediatric Gastroenterology, Hepatology, and Nutrition in Montreal.
Led by Dr. Heather Schlott, Connecticut Children’s extracorporeal membrane oxygenation (ECMO) program, received a Silver Award (the highest award possible for Connecticut Children’s program) for its excellent outcomes from the national Extracorporeal Life Support Organization.
Under the direction of Dr. Cem Demirci, the Diabetes Education Program was reaccredited by the American Association of Diabetes Educators, one of only three programs certified in Connecticut in 2015, and the only one dedicated to the care of children and adolescents with diabetes.
Connecticut Children’s Central Connecticut Cystic Fibrosis Center continues to be one of the Top 10 CF centers in the country based on combined pulmonary and nutritional outcomes.
In the Division of Infectious Diseases, the Ryan White program’s work for youth and adolescents at risk of, and infected with, HIV has been recognized internationally for its novel initiatives in identifying and caring for high-risk individuals.
The Easy Breathing© for Schools program was one of 26 finalists for the 2016 Hospital Charitable Services Awards.
Three Connecticut Children’s nurses, Aimee Bareiss, MSN, RN, CPN, Kristina Kaminski, MSN, RN, and Julia Anne Morri-
son, MSN, RN, authored an article titled “The Huddle: Becoming a Team,” which is now featured on a prominent professional nursing website, Advance Healthcare Network for Nurses.
Connecticut Children’s Maintenance of Certification (MOC) Part 4 Portfolio was renewed in 2015 for another two years.
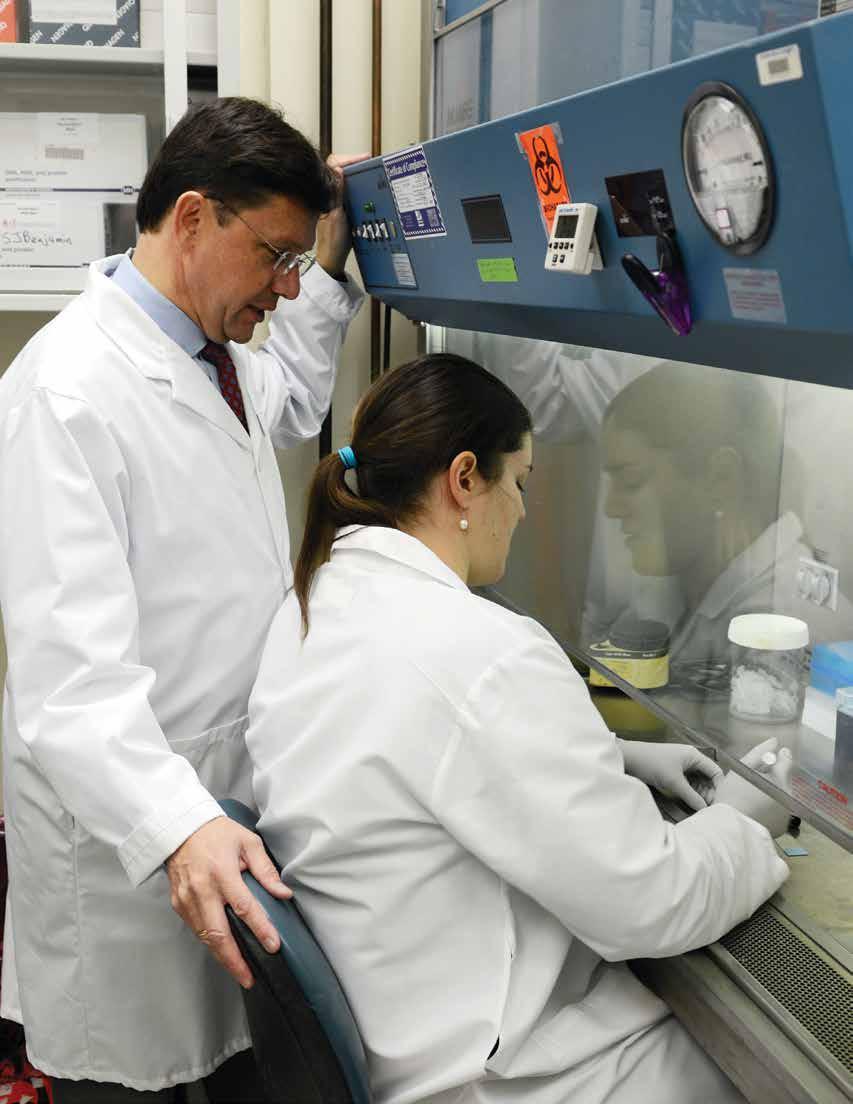
Connecticut Children’s created a new biotech center, which houses four investigative researchers, all working to find ways to treat and prevent childhood illnesses.
Pediatric cardiologist Dr. Fred Bernstein, in collaboration with pediatric cardiothoracic surgeon Dr. Mohsen Karimi, was instrumental in completing the first cardiac interventional/surgical hybrid procedure performed at Connecticut Children’s.
In what is likely a “first” for Connecticut, pediatric cardiologist Dr. Shailendra Upadhyay performed the first zero X-ray ablation for supraventricular tachycardia.
Drs. Upadhyay and Felice Heller were among the first group of cardiologists in the country to receive board certification in Adult Congenital Heart Disease, a newly recognized subspecialty of the American Board of Internal Medicine.
The Division of Pediatric General and Thoracic Surgery introduced vacuum bell elevation, an innovative new treatment option for patients with pectus excavatum.
Connecticut Children’s Otolaryngology Division created a comprehensive aerodigestive team to treat laryngotracheal, pulmonary and gastrointestinal disorders.
Dr. Valerie Côté of the ENT Division introduced sleep endoscopy evaluation in the operating room. This diagnostic step enables clinicians to identify multiple potential sites of obstruction to tailor treatment options and appropriately counsel families.
Otolaryngologists Scott Schoem, MD, and Christopher Grindle, MD, started performing totally implantable bone-anchored hearing devices. Families now have the option of choosing the standard system called the Baha Connect, or the newer, totally implantable system known as Baha Attract.
In the Division of Pediatric and Adolescent Gynecology, surgical services expanded in 2015 to include daVinci robotically assisted minimally invasive procedures for select patients. Division Head Dr. Frederick Rau performed a robotically-assisted laparoscopic excision of a congenital uterine anomaly with preservation of future fertility.
Regionally, for the convenience of patients and families, and to better serve the children of Connecticut, Connecticut Children’s expanded its services to more areas of the state. In 2016, in collaboration with the UConn Health Center, Primary Care clinics were opened in East Hartford and West Hartford.
In 2016, Connecticut Children’s began partnering with Community Health Center (CHC), a federal qualified health center headquartered in Middletown, CT, to continue to provide the children and families of Hartford primary pediatric care at an established New Britain Avenue office. The partnership promises significant new funding from the federal government to support improved health care for the children of Hartford.
In spring of 2016, Connecticut Children’s opened the Neurodiagnostic and Sleep Lab, which offers state-of-the-art equipment and resources to provide the best quality diagnostics.
Also in 2016, Connecticut Children’s launched a new sedation unit to help our patients manage the stress and challenges of medical procedures.
Connecticut Children’s Division of Emergency Medicine instituted a direct bedding process. The results include substantial improvements in time metrics and, consequently, stellar performance in Left Without Being Seen (LWBS) rates.
In the area of international outreach, 2016 saw the creation of Connecticut Children’s Center for Global Health, led by Dr. Adam Silverman and Karen Callahan, BAS, BSN, MHS, RN, CPN. Focusing primarily on reducing morbidity and mortality in medically underserved populations, the center supports the activities of faculty and staff while working with partners to build in-country capacity to reduce major causes of child morbidity and mortality globally.
Two new fellowships, Anesthesiology and Infectious Diseases, received approval by the Accreditation Council for Graduate Medical Education (ACGME).
In 2015, Grand Rounds were made available via live streaming online which resulted in a 23 percent greater reach of our weekly lectures across the state. In 2016, thanks to the generous support from the Ahearn Family Foundation, Grand Rounds were made available via podcast.

Dr. Ching Lau Awarded Inaugural Martin J. Gavin Endowed Chair
Ching C. Lau, MD, PhD, division head of the Division of Pediatric Hematology-Oncology in the Department of Pediatrics at the UConn School of Medicine, was awarded the inaugural Martin J. Gavin Endowed Chair in Hematology-Oncology. The announcement was made in late 2016 with an award ceremony in early 2017.
The Endowed Chair in Hematology/Oncology is named in honor of former Connecticut Children’s President and CEO Martin J. Gavin, who retired in October of 2015.
Dr. Lau, a distinguished pediatric oncologist and cancer researcher, joined Connecticut Children’s in October 2016. He holds joint positions as professor at the Jackson Laboratory (JAX) for Genomic Medicine, and as head of the Division of Pediatric Hematology-Oncology in the Department of Pediatrics at the UConn School of Medicine.
James E. Shmerling, DHA, FACHE, president and CEO of Connecticut Children’s, said he remembers when he started his career in hospitals 37 years ago, a pediatric cancer diagnosis seemed hopeless. “But now there is hope,” he said. “Children have hope, moms and dads have hope. Funding a chair allows us to accelerate the research and will leapfrog us to some of the discoveries that will cure children with cancer.”
Dr. Lau, who came to Connecticut Children’s from Texas Children’s Hospital in Houston, said, “One of the things I discovered when I started interviewing here at Connecticut Children’s is that this institution is very visionary. The leadership is committed to advancing the field and has the determination to make it happen. It’s not just the hospital that is willing to commit to that, but the community as well. I dream that one day when I look at a child diagnosed with cancer I can look him or her in the eye and say, ‘You will be cured without having to come to the hospital for therapy. You just have to go home and take this medicine.’”

Dr. Cem Demirci Awarded Chase Family Chair in Juvenile Diabetes
Connecticut Children’s Dr. Cem Demirci was awarded the UConn Health Center’s Chase Family Chair in Juvenile Diabetes. The prize, announced in 2016, was bestowed in recognition of Dr. Demirci’s selfless commitment and dedication to the care of diabetic children. As medical director of Connecticut Children’s Diabetes Program for the last six years, Dr. Demirci leads a first-rate team of
educators, clinicians and support staff whose goal is to improve the lives of young patients with Type 1 diabetes. The Chase Family Chair includes a generous monetary award that may be used for the care of patients and for innovative research involving Type 1 diabetes. The chair was first awarded to Connecticut Children’s Dr. Susan Ratzan in 1985 in recognition of her revolutionary work and multidisciplinary approach to caring for children with Type 1 diabetes.

As an academic teaching hospital, Connecticut Children’s strives to encourage, support, and recognize the academic activities and achievements of its faculty, and support the highest quality Medical Education and Pediatric Fellowship programs.
With faculty based at multiple institutions and throughout the community, administration of the Department of Pediatrics, staffed at the University of Connecticut Health Center by Laurie Papacs, Administrative Officer, and Theresa George, Administrative Fiscal Assistant, is comprised of centrally managed academic functions and decentralized business and research management functions.
The Office of Academic Administration, in cooperation with the Chair’s Office, staffed at Connecticut Children’s Medical Center, manages academic appointment, promotion, and development activities, merit tracking for both in-residence and affiliated faculty, academic faculty contracts, produces the combined Department of Pediatrics & Pediatric Surgical Subspecialties and the Faculty Resource Guide. New to the office of Academic Administration in 2015-2016 was the development and implementation of the Department of Pediatrics three-year (2016-2019) strategic plan, and support for the Departments of Pediatric Surgery in the development of their three-year (2017-2020) strategic plan.
The department is staffed by Esperanza Lesmes, Academic Operations Program Manager; with assistance from Deborah Hornblow, per diem editor; and Brian Lesmes, per diem intern, and includes the following offices:
In 2015, three faculty members from the Department of Pediatrics and two faculty members from the Department of Surgery were nominated and promoted to a senior rank. Also, one appointment was submitted and granted the appointment to senior rank. In 2016, 11 faculty members from the Department of Pediatrics and two faculty members from the Department of Surgery were nominated, as well as two appointments of newly hired faculty were submitted and are
currently under review by the Senior Appointment and Promotions Committee (SAPC).
The Office of Continuing Medical Education, supported by Deirdre Palmer, Diane Mouradjian, and Kenneth Spiegelman, MD, accredited a total of 756 hours of instruction to 2,079 individual participants for a total of 27,568 contact hours. Accredited CME offerings include Grand Rounds, Pediatric, and Mental Health Lecture series, regularly scheduled educational series, and half-, full-, and multi-day conferences.
Fellowship coordinators Jack Wakefield, Marianne Custer, Opeyemi Aina, Lindsay Haythorn (October 2016), and Amanda Ross (October 2016), supported 11 pediatric subspecialty fellowships and 19 fellows. In 2015 and 2016, the pediatric fellowship programs graduated 11 fellows and successfully filled 15 of 21 available fellowship positions. In preparation for the 2016 and 2017 academic years, coordinators effectively supported recruitment of 206 applicant interviews throughout the two years. Pediatric Anesthesiology and Pediatric Infectious Diseases Fellowship Programs were newly accredited in 2015 and 2016.
Eminet Abebe Gurganus, Program Development and Implementation Manager, along with Jessica Ryan, Program Associate, collaborated with faculty and community partners to develop 14 new MOC activities for a total of 26 (13 internal and 13 community-focused) that promote quality improvement efforts within the hospital and serve as a bridge to the community to disseminate the hospital’s excellent quality improvement work to community practitioners. We also welcomed Taylor Dauphin, Program Associate, in 2016. The generous support of United Healthcare continues to fund our PQI/MOC activities.
In 2016, Connecticut Children’s welcomed our new medical photographer, Erin Blinn, who officially begins her new role in January 2017. Erin will apply her artistic talents and passion for children to support patient care, research, legal documentation, continuing medical education and public relations efforts through quality photographic images that will enhance our website, publications, research articles and medical records.
Departmental highlights over the last two years include 2015:
Grand Rounds were made available via live streaming online which resulted in a 23 percent greater reach of our weekly lectures across the state
Pediatric Anesthesia was approved by the ACGME as a new UConn School of Medicine Fellowship program that will reside at Connecticut Children’s, led by Dr. Michael Archambault
Our office of Continuing Medical Education sponsored two new external conferences that provided AMA credits to a total of 28 physicians sponsored by the International Lactation Consultant Society
2016:
Pediatric Infectious Diseases was approved by the ACGME as a new UConn School of Medicine Fellowship program, to reside at Connecticut Children’s, led by Dr. Nick Bennett as Program Director
Our office of Continuing Medical Education sponsored two new external conferences (Motivational Interviewing Training, and Society for Pediatric Sedation) that provided AMA credits to a total of 145
Thanks to the generous support from the Ahearn Family Foundation, Grand Rounds were made available via podcast
Thanks to the generous support of the Dr. Paul A. “Tony” Andrulonis Memorial Fund for Child and Adolescent Mental Health, the Office for Continuing Medical Education sponsored a half-day mental health symposium titled “Office-Based Strategies to Help Anxious Kids” for community pediatricians and health care providers
Staff
Annamarie
Beaulieu, MPH, BBA Director, Academic Affairs
Laurie Papacs
Administrative Officer, Department of Pediatrics
University of Connecticut School of Medicine
Theresa George
Administrative Fiscal Assistant Department of Pediatrics
University of Connecticut School of Medicine
Esperanza Lesmes Academic Operations Manager
Connecticut Children’s Medical Center
Diane Mouradjian Continuing Medical Education Coordinator
Deirdre Palmer Continuing Medical Education Coordinator
Brian Lesmes Research Intern
Marianne Custer
Fellowship Coordinator
Jack Wakefield Fellowship Coordinator
Opeyemi Aina Fellowship Coordinator
Lindsay Haythorn Fellowship Coordinator
Amanda Ross Fellowship Coordinator
Eminet Gurganus Program Development and Implementation Manager, OCCH and PQI/MOC
Jessica Ryan
Program Specialist, OCCH and PQI/MOC
Taylor Dauphin Program Associate, OCCH and PQI/MOC
Erin Blinn Medical Photographer
The mission of the Division of Adolescent Medicine is to provide comprehensive health care to adolescents between the ages of 11 and 25, to educate health and mental health providers (particularly pediatric residents) regarding the needs of adolescents, to promote adolescent health in the community, and to advance adolescent health through clinical research.
During 2015-2016, the Division of Adolescent Medicine offered primary care, consultative clinical services and resident education at the Primary Care Center (PCC) of Connecticut Children’s Medical Center. With the transition of the PCC to Community Health Center at Connecticut Children’s (CHC@ CCMC) in July 2016, the division continues to offer these same services at the same site. The division welcomed a second adolescent medicine specialist, Dr. Alyssa Bennett, in July 2016. Beginning in 2017 the division will offer consultative services to community and subspecialist provider practices at a Connecticut Children’s site in Farmington.
The clinical services currently provided by the division include the following:
Adolescent Medicine primary care and consultative health services at CHC@CCMC
Medical Directorship at Trinity College Health Center
Clinical services rendered by our community clinical partners while mentoring Connecticut Children’s pediatric residents on their Adolescent Medicine electives are provided by the following preceptors at their respective sites:
Hartford Job Corps Center: providing primary care health services to adolescents and young adults, under the direction of Medical Director Paul Clarke, MD
Westminster School, Simsbury, CT: providing primary care health services to adolescents, under the direction of Medical Director Davis Smith, MD
Student Health Services at University of Connecticut (Storrs), Sports Injury Clinic: under the direction of Director of Medical Services Jeffrey Anderson, MD, FACSM
Women’s Ambulatory Health Services, Family Planning and Teen Clinic: under the direction of Amy Nelson, MD

The division offers an Adolescent Medicine Selective, a onemonth ambulatory experience required for all second-year pediatric residents. An advanced adolescent medicine elective is tailored to the needs of third-year pediatric residents by request.
Staff
Nancy H. Miller, MD Division Director
Alyssa Bennett, MD
Paul Clarke, MD
Davis Smith, MD
Amy Nelson, MD
Jeffrey Anderson, MD, FACSM
Grael O’Brien, MD
Sudeshna Basu, MD
The division received approval by the Accreditation Council for Graduate Medical Education (ACGME) for a pediatric anesthesiology fellowship training program. Dr. Thomas Manning will be our first fellow starting in July of 2017.
The Division of Pediatric Anesthesiology draws on the long history of anesthesia excellence in Hartford, CT, to provide superb clinical care, innovative teaching, academic achievement and a commitment to patient safety. The division’s successes depend on the exceptional teamwork of our physicians, nurse anesthetists, advanced practice nurses and staff.
The division consists of 15 anesthesiologists, over nine CRNAs, and two APRNs. The Connecticut Children’s Hartford campus is our principal clinical site but we provide care at numerous locations throughout the greater capital area. We coordinate care for over 9,000 patients each year that require elective and emergent surgery, endoscopy, imaging and cardiac catheterization at the Hartford campus. Additionally, we care for over 1,000 children at the Ambulatory Surgery Center in Farmington. For patients requiring MRA, nuclear medicine, interventional radiology or transplant services at Hartford Hospital, we provide the necessary expertise and a familiar face. Urgent procedures at Connecticut Children’s NICU in Farmington also are covered by our division. Our vision is to provide compassionate care with extraordinary expertise for children in Connecticut.
Dr. Eapen Mathew is the newest member of the division. He is board certified in both pediatric anesthesiology and pain management. The majority of his time will be spent in Anesthesiology adding depth to our acute pain service. Additionally, he will spend time with the division of Pain and Palliative Medicine rounding on inpatients and staffing a clinic. Dr. Michael Archambault, in addition to his work with simulation-based training of anesthesiology and otolaryngology residents, will take on the additional responsibility of fellowship director. Dr. Christina Biello and Dr. Jeff Hyams in Gastroenterology continue their work on Propofol dosing in endoscopy patients. Drs. Craig Bonanni and Mark Indelicato are working with Dr.
Brendan Campbell in Surgery on projects using National Surgical Quality Improvement Project (NSQIP) data to decrease blood transfusions in spine surgery and streamline care in appendicitis patients. Dr. Gregory Kernisan continues his work with Haitian medical services, and this year was appointed to the board of directors of the Haitian Health Foundation, overseeing health care and educational activities in Haiti. Jay McIsaac, MD, MS, Department of Anesthesiology, moderated a panel on Anesthetic Management During Mass Casualties and presented “Mass Shootings and OR Management” at the Annual Meeting of the American Society of Anesthesiologists in Chicago, IL, on October 24, 2016. Dr. McIsaac is a founding board member of the Trauma Anesthesiology Society, the Chair of Disaster Preparedness for the Connecticut State Medical Society, and a member of the ASA Committee on Trauma and Emergency Preparedness. He is an Associate Clinical Professor of Anesthesiology at both the UConn and Quinnipiac schools of medicine.
Publications
McCunn M, Dutton RP, Dagal A, Varon AJ, Kaslow O, Kucik CJ, Hagberg CA, McIsaac JH, Pittet JF, Dunbar PJ, Grissom T, Vavilala MS. Trauma, critical care, and emergency care anesthesiology: a new paradigm for the ‘acute care’ anesthesiologist? Anesth Analg. 2015 Dec; 121(6):1668–73.
Lehn RA, Gross JB, McIsaac JH, Gipson KE. Needleless connectors substantially reduce flow of crystalloid and red blood cells during rapid infusion. Anesth Analg. 2015 Apr; 120(4):801-4.
McIsaac JH, et al. Operating room mass casualty checklist. ASA Committee on Trauma and Emergency Preparedness and the Trauma Anesthesiology Society Committee on Mass Casualties. 2015 Dec 7.
Staff
Craig Bonanni, MD, FAAP
Division Head
Michael Archambault, MD
Christina Biello, DO
Amy Bouchard, DO, FAAP
Edward Cortland, MD, FAAP
Deanne Daggett, MD
John Garrison, MD
Mark Indelicato, MD, MSc, FAAP
Gregory Kernisan, MD
Carole Lin, MD
Anil Mathew, MD, FAAP
Eapen Mathew, MD
Joseph McIsaac, MD, MS
Joseph McRuiz, MD
Gerald Piserchia, MD
Robin Roman, MD
Valerie Rossetti, MD, MPH
Gregory Rutkowski, MD
Amir Tulchinsky, MD
Heather Allen, CRNA
Elizabeth Beatson, CRNA
Stephanie Cardino, CRNA
Kelly Gorski, CRNA
Allison Holtman, CRNA
Wendy Lord, CRNA
Dana McCarsky, CRNA
Barbara Richards, CRNA
Christine Rouleau, CRNA
Tracy Kunkel, APRN
Stephania Kushnir, APRN

The past two years have been busy for C3R’s Asthma Center. In mid-2015, the Asthma Center completed a collaboration with Hartford Public Schools to pilot the Building Bridges school-based asthma program. Funded by the GlaxoSmithKline Foundation and in collaboration with Denver Public Schools and Children’s Hospital of Colorado, the program aims to improve academic performance by decreasing school absences through improved asthma control in inner-city students.
Final data analyses demonstrate a 24.5 percent reduction in absentee rate, which translates into more than five fewer missed school days in the 2014-2015 school year. The program was streamlined, based on feedback from school nurses, clinicians, and families, into a sustainable school-centered program that school nurses could implement. In August 2015 and August 2016, Hartford Public School nurses were trained in Easy Breathing© for Schools, the adapted version of Building Bridges. To date, almost 30 school nurses have been trained in the program. Led by Christine Langton, MSW, MPH, and Jing Marrero, MSII, MPH candidate, the program has received increased visibility and demand statewide and outside of Connecticut. In August 2016, all New Haven Public School nurses were trained as well as Goodwin College nursing students. In May 2016, Jessica Hollenbach, PhD, was invited to present the adaptation of Building Bridges to Easy Breathing for Schools at the Nationwide Children’s Hospital 7th Annual Pediatric Asthma Conference. Lastly, we are thrilled to announce that the Easy Breathing for Schools program was one of 26 finalists for the 2016 Hospital Charitable Services Awards.
In 2015, the Easy Breathing program enrolled its 150,000th child, with more than 40,000 children diagnosed with asthma. In mid-2016, Rutgers Robert Wood Johnson Medical School was trained in the program and began implementing it within the primary care community. To date, the Rutgers Easy Breathing team has trained four primary care practices across the community. Currently, Easy Breathing is active in six states – Ohio, Kansas, Kentucky, Florida, New Jersey and Vermont. The Easy Breathing program also initiated a collaboration with a start-up incubator called CoHero. CoHero has developed a metered dose inhaler with a sensor that links to
a smartphone app. From July to September 2015, we conducted focus groups with CoHero to assess the need or desire in the primary care community for this type of technology and asked pediatricians how they could use this information to better serve their patients. We determined that PCPs were varied in their interest in obtaining real-time adherence data, with the ability to customize type and frequency of reports a top priority for them. Results from these focus groups were presented by Jessica Hollenbach at the 36th Annual Meeting of the Society for Behavioral Medicine and were published in the Journal of Asthma.
In August 2016, the Asthma Center received a planning grant from the NHLBI. The goal of this planning grant, titled the “Asthma Neighborhood: Collaborative for Asthma Equity (CASE) in Children,” was to engage multiple asthma sectors in Hartford to maximize programmatic synergies and to conduct a community needs assessment, the results of which were used to propose a clinical trial. To achieve this goal, we created the Hartford Collaborative for Asthma Equity (CASE) (the “Collaborative”), composed of researchers, families, students, schools, school-based health clinics, pharmacy, primary care clinicians, asthma specialists, local and state health departments, community organizations, payers of medical services and housing operators. From each member’s perspective, the collaborative created an asthma neighborhood that collectively supports families. Features of the asthma neighborhood include identifying children with asthma at high risk for poor outcomes; cross-sector, consistent asthma education; and creation of a communication/information sharing platform that includes the child’s asthma treatment plan and medical services utilization data. Informed by the results of the needs assessment, the collaborative proposed a clinical trial that integrates five evidence-based interventions (Easy Breathing; Easy Breathing for Schools; a community health worker-led home visitation program adapted to asthma; Healthy Homes; and the Severe Asthma Program) into a new model of care for children with asthma. We hypothesize that a cross-sector, integrated system of asthma care will decrease the frequency of oral corticosteroids prescribed for asthma exacerbations (primary outcome); will be sustained, reproducible, and reach large numbers of children with asthma (process outcomes);
and will be effective both in African-American and Hispanic/ Puerto Rican children, two groups with high asthma morbidity. The multi-million dollar proposal, titled “The Asthma Neighborhood: Eliminating Disparities, Empowering Families,” was submitted to the National Heart, Lung, and Blood Institute in November 2016.
In January 2017, leadership of the Asthma Center will be transferred to Drs. Jessica Hollenbach, PhD, and Tregony Simoneau, MD, as co-directors.
The Early Childhood Obesity (ECHO) Prevention Program study, submitted by the Hartford Childhood Wellness Alliance and funded by NICHD, was completed in January 2016, and the final analysis is underway. Early findings suggest a lower maternal/child dyad dropout rate in the intervention dyads, longer breastfeeding duration with suggestions of delayed introduction of solids, and less sugar-sweetened beverage consumption.

Publications
Hollenbach JP, Cloutier MM. Childhood asthma management and environmental triggers. Pediatr Clin North Am. 2015 Oct; 62(5):1199-214.
Brehm JM, Tse S-Z, Croteau-Chonka DC, Forno E, Litonjua AA, Benjamin A, Raby BA, Chen W, Yan Q, Boutaoui N, Acosta-Pérez E, Avila L, Weiss ST, Soto-Quiros M, Cloutier MM, Hu D, Pino-Yanes M, Wenzel SE, Spear M, Kolls JK, Burchard EG, Canino G, Celedón JC. A genome-wide association study of post-bronchodilator lung function in children with asthma. Am J Respir Crit Care Med. 2015: 192:634-7.
Bender BG, Krishnan JA, Chambers DA, Cloutier MM, Riekert KA, Rand CS, Schatz M, Thomson CC, Wilson SR, Apter A, Carson SS, George M, Gerald JK, Gerald L, Goss CH, Okelo SO, Mularski RA, Nguyen HQ, Patel MR, Szefler S, Weiss C, Wilson KC, Freemer MM. American Thoracic Society-National Heart, Lung and Blood Institute Implementation Research Workshop Report. Ann Am Thorac Soc. 2015: 12(12):S213-21.
Levy BD, Noel PJ, Freemer MM, Cloutier MM, Georas SN, Jarjour NN, Ober C, Woodruff PG, Barnes KC, Bender BG, Camargo CA Jr, Chupp GL, Denlinger LC, Fahy JV, Fitzpatrick AM, Fuhlbrigge A, Gaston BM, Hartert TV, Kolls JK, Lynch SV, Moore WC, Morgan WJ, Nadeau KC, Ownby DR, Solway J, Szefler SJ, Wenzel SE, Wright RJ, Smith RA, Erzurum SC. Future research directions in asthma. An NHLBI Working Group Report. Am J Respir Crit Care Med. 2015; 192(11):1366-72.
Cloutier MM, Wiley J, Wang Z, Grant A, Gorin AA. The Early Childhood Obesity Prevention Program (ECHO): an ecologically-based intervention delivered by home visitors for newborns and their mothers. BMC Public Health. doi:10.1186/s12889-015-1897-9.
Cloutier MM. Asthma management for primary care providers: increasing adherence to asthma guidelines. Curr Opin Allergy Clin Immunol. 2016; 16(2):142-7.
Rosas-Salazar C, Han Y-Y, Brehm J, Forno E, Acosta-Perez E, Cloutier MM, Alvarez M, Colon-Semidey A, Canino G, Celedon J. Gun violence, African ancestry, and asthma: a case-control study in Puerto Rican children. Chest. 2016 Jun; 149(6):1436-44.
Forno E, Weiner DJ, Mullen J, Sawicki G, Kurland G, Han YY, Cloutier MM, Canino G, Weiss ST, Litonjua AA, Celedón JC. Obesity and airway dysanapsis in children with and without asthma. Am J Respir Crit Care Med. 2016 Aug 23.
Smith GJ, Thrall RS, Cloutier MM, Manautou JE, Morris JB. Acetaminophen attenuates house dust mite-induced allergic airway disease in mice. J Pharmacol Exp Ther. 2016 Sep; 358(3):569-7.
Lemanske RF Jr, Kakumanu S, Shanovich K, Antos N, Cloutier MM, Mazyck D, Phipatanakul W, Schantz S, Szefler S, Vandlik R, Williams P. Creation and implementation of SAMPRO™: a school-based asthma management program. J Allergy Clin Immunol. 2016 Sep; 138(3):71123.
Weiss CH, Krishnan JA, Au DH, Bender BG, Carson SS, Cattamanchi A, Cloutier MM, Cooke CR, Erickson K, George M, Gerald JK, Gerald LB, Goss CH, Gould MK, Hyzy R, Kahn JM, Mittman BS, Mosesón EM, Mularski RA, Parthasarathy S, Patel SR, Rand CS, Redeker NS, Reiss TF, Riekert KA, Rubenfeld GD, Tate JA, Wilson KC, Thomson CC; ATS Ad Hoc Committee on Implementation Science. An official American Thoracic Society research statement: implementation science in pulmonary, critical care, and sleep medicine. Am J Respir Crit Care Med. 2016 Oct 15; 194(8).
Hollenbach JP, Cushing A, Melvin E, McGowan B, Cloutier MM, Manice M. Understanding clinicians’ attitudes toward a mobile health strategy to childhood asthma management: a qualitative study. J Asthma. 2016 Nov 23: 0. Epub ahead of print.
Michelle Cloutier, MD Director, Asthma Center
Jessica Hollenbach, PhD Co-Director, Asthma Center
Tregony Simoneau, MD Co-Director, Asthma Center
Christine Langton, MSW, MPH Senior Program Evaluator
Autherene Mitchell, BS Database Reporting Analyst
Hilary Norcia, MPH Easy Breathing© Program Coordinator
Carol Vinick, APRN Research Assistant
Brian Lesmes, BA Data Entry Intern
Nicole Gherlone, BS Research Assistant/Data Entry Intern
Michael Powell, BS Data Entry Intern
Amy Anderson Administrative Assistant
In 2015, the Children’s Center for Community Research transitioned into two new divisions: The Center for Behavioral Health and the Asthma Center (see p. 16).
The Center for Behavioral Health (CBH) focuses on developmental and clinical psychology research, especially as it relates to child and adolescent health and pediatric care. The research conducted by CBH is interdisciplinary, collaborative, and emphasizes the psychological and physical health of children, adolescents, and their families. Research conducted by CBH primarily takes place in settings such as Connecticut Children’s medical clinics, schools, homes, and community organizations.
In 2015, the Center for Behavioral Health welcomed Faculty/Investigator Jessica Guite, PhD, Research Assistant Ashley Pantaleao, MA, and Research Associate Anna Vannucci, MS.
In 2016, Administrative Assistant Amy Anderson, BS, Research Assistant Victoria Galica, BA, Research Assistant Courtney Lincoln, MA, and volunteer Sarosh Khan, BA, were welcomed to the team.
The past few years have been an exciting time of transition for the Center for Behavioral Health. Our work on the longitudinal Adolescent Adjustment Project (AAP) yielded 22 presentations at national conferences and 12 publications. In addition to our work on the AAP, we launched two new research projects. The National Science Foundation-funded BALANCE project is a partnership between Connecticut Children’s Medical Center, the University of Maryland, and Georgia State University. It began in December of 2015. The goal of the project is to examine the interplay between parental work and family conflict and the manner in which this interplay is related to adolescent psychological health and adjustment. Much of 2016 has been spent collecting data from adolescents and their parents. We now are finalizing data collection and have almost 100 families with complete data for the BALANCE project. In 2015, we also initiated the PANDA
(Predictors of Adolescent Depression and Anxiety) project, funded by the Alvord Foundation. The primary aim of the PANDA project is to uncover predictors of gender differences in depression and anxiety during early adolescence. We now are preparing for data collection, which will take place in five middle schools in Connecticut and Massachusetts during November and December of 2016. In 2015-2016, Dr. Ohannessian also collaborated as a co-investigator with Dr. Yifrah Kaminer from the Psychiatry Department at UConn Health on two separate NIH-funded projects focusing on treatments for adolescents with substance use disorders. In addition, in 2016, Dr. Ohannessian co-edited a special issue of the Journal of Youth and Adolescence (with Dr. De Los Reyes from the University of Maryland) focusing on discrepant perceptions of the family between adolescents and their parents.
The inclusion of Dr. Guite’s program of research focusing on chronic pediatric pain, illness and disability, and parent and family coping has expanded the Center for Behavioral Health’s scope to include intervention research. During 2015-2016, Dr. Guite served as the principal investigator at Connecticut Children’s for a NIH-funded U34 clinical trial planning grant for “Fibromyalgia Integrative Training Program for Teens (FIT Teens),” a new cognitivebehavioral group therapy enhanced with neuromuscular exercise training for the treatment of juvenile fibromyalgia. This fruitful external collaboration with Dr. Susmita Kashikar-Zuck at Cincinnati Children’s Hospital Medical Center and collaborators across seven sites has generated an application for a NIH Phase III multi-site clinical trial implementation cooperative agreement (U01) to further test the FIT Teens intervention. Also during this time, Dr. Guite and co-PI Dr. Beth Russell, from UConn, initiated the development of “Parents as Coping Coaches,” a brief parent-focused group intervention for parents of adolescents with chronic pain conditions supported by a cross-institutional seed grant through Connecticut Children’s and UConn/CHIP.
During 2015-2016, the Center for Behavioral Health continued to extend its external collaborations with partners including the University of Connecticut at Storrs, UConn Health, UConn School of Social Work, the University of Delaware, the University of Maryland, Pennsylvania State University, Georgia State University, the University of New Orleans, Drexel University, Cincinnati Children’s Hospital Medical Center/University of Cincinnati, Children’s Hospital of Philadelphia/University of Pennsylvania, Children’s Hospital of Wisconsin/Medical College of Wisconsin, Hartford Hospital/The Institute of Living, and the Alvord Foundation.
De Los Reyes A, Ohannessian CM, Laird R. Developmental changes in discrepancies between adolescents’ and their mothers’ views of family communication. J Child Fam St. 2016; 25:790-7.
Herres J, Ohannessian CM. Adolescent coping profiles differentiate reports of depression and anxiety symptoms. J Affect Disord. 2015; 186:312-9.
Ohannessian CM, Finan L, Schulz J, Hesselbrock V. A longterm longitudinal examination of the effect of early onset of alcohol and drug use on later alcohol abuse. Subst Abuse. 2015; 36(4):440-4.
Publications
Ohannessian CM, De Los Reyes A. [editors] Special issue: Discrepancies in adolescent-parent perceptions of the family and adolescent adjustment. J Youth Adolesc. 2016; 45(11).
Vannucci A, Flannery KM, Ohannessian CM. Social media and anxiety in emerging adults. J Affect Disord. 2016; 207:163-6.
De Los Reyes A, Ohannessian CM. Introduction to the special issue: discrepancies in adolescent-parent perceptions of the family and adolescent adjustment. J Youth Adolesc. 2016; 45:1957-72.
Ohannessian CM, Laird R, De Los Reyes A. Discrepancies in adolescents’ and mothers’ perceptions of the family and mothers’ psychological symptomatology. J Youth Adolesc. 2016; 45:2011-21.
Ohannessian CM, Flannery K, Simpson E, Russell B. Family functioning and adolescent alcohol use: a moderated mediation analysis. J Adolesc. 2016; 49:19-27.
Kaminer Y, Ohannessian CM, McKay J, Burke R. The Adolescent Substance Abuse Goal Commitment (ASAGC) questionnaire: an examination of clinical utility and psychometric properties. J Subst Abuse Treat. 2016; 61:42-6.
Finan L, Schulz J, Gordon M, Ohannessian CM. Parental problem drinking and adolescent externalizing behaviors: the mediating role of family functioning. J Adolesc. 2015; 43:100-10.
Ohannessian CM. A longitudinal examination of the relationship between technology use and substance use during adolescence. In: Blair SL, Claster PN, Claster SM, editors. Sociological studies of children and youth, technology and youth: growing up in a digital world. Emerald Publishing Group Ltd; 2015. Vol 19. p. 293-313.
Cloutier MM, Wiley J, Huedo-Medina T, Ohannessian CM, Grant A, Hernandez D, Gorin AA. Outcomes from a pediatric primary care weight management program: Steps to Growing Up Healthy. J Pediatr. 2015; 167:372-7.
Ohannessian CM. The interactive effect of paternal problem drinking and maternal problem drinking on adolescent internalizing problems. Addict Behav. 2015; 50:70-3.
Evans JR, Jastrowski M, Kristen E, Guite JW, Weisman SJ, Hainsworth KR. Psychometric properties of the Pain Stages of Change Questionnaire: new insights on the measurement of readiness to change in adolescents, mothers and fathers. J Pain. 2015; 16(7):645-56.
Ohannessian C, Milan S, Vannucci A. Gender differences in anxiety trajectories from middle to late adolescence. J Youth Adolesc. Epub ahead of print, 2016 Nov 26. doi: 10.1007/ s10964-016-0619-7.
Staff
Christine McCauley Ohannessian, PhD
Director, Center for Behavioral Health
Amy Anderson, BS
Kaitlin Flannery, MA
Victoria Galica, BA
Jessica Guite, PhD
Anne Heller, LMFT, MA
Sarosh Khan, BA
Courtney Lincoln, MA
Magdalena Owczarska, BA
Ashley Pantaleao, MA
Emily Simpson, MA
Anna Vannucci, MS

The mission of the Division of Pediatric Cardiology is to care for and improve the cardiovascular health of newborns, children and adolescents, and transition them into healthy adulthoods. We strive to embrace discovery, teamwork, integrity and excellence in all that we do.
We have opened up new satellite ambulatory offices in Farmington where we provide clinical consultations, EKGs and ECHO studies for both our pediatric and adult congenital heart disease patients. This is in addition to our other ambulatory pediatric clinics in Danbury, Glastonbury and Shelton. We also see fetal cardiac patients in conjunction with our colleagues at Danbury Hospital.
Dr. Fred Bernstein, in collaboration with our pediatric cardiothoracic surgeon, Dr. Mohsen Karimi, was instrumental in completing the first cardiac interventional/surgical hybrid procedure performed here at Connecticut Children’s.
Dr. Shailendra Upadhyay performed the first Zero X-ray catheter ablation for supraventricular tachycardia in the state of Connecticut. Connecticut Children’s is the only medical facility in the state to perform this procedure without X-ray use.
In 2016, Dr. Bernstein participated in a National Cardiovascular Data Registry initiative seeking to reduce radiation exposure to pediatric cardiac catheterization patients. This quality improvement initiative resulted in a clinical reduction of radiation exposure by more than 70 percent. This exposure level ranks among some of the lowest in the country.
Dr. Upadhyay, a four-year member of our division, is the only certified pediatric electrophysiologist in the state. Under his guidance, the arrhythmia services at Connecticut Children’s provide the full array of cardiac rhythm management to children with heart rhythm disorders. Connecticut Children’s provides one of only three pediatric pacemaker clinics run by a pediatric electrophysiologist in the New England area.
Our echo lab continues to expand and now includes six sonographers, and performs over 6,500 studies per year. In 2016, our application for ICAEL certification was completed. We also initiated a scheduled lecture series for cardiologists and sonographers to promote educational and technical advancements in pediatric sonography. We have designed and implemented echocardiography protocols and have worked to standardize disease-specific protocols. We have comprehensive quality initiatives to optimize care for our patients, and we review these quality assessments quarterly. Our echo lab has a special interest in 3-D imaging and in the assessment of myocardial mechanics, which supports our cardio-oncology program.
Our fetal cardiology program continues to grow, providing comprehensive diagnostic services and management of fetal cardiac disease. Over the past year, we performed over 200 fetal echocardiograms. Our dedicated fetal team includes cardiologists, nurses and specially trained sonographers. The coordination of care between pediatric cardiologists, obstetricians, maternal fetal medicine specialists, neonatologists, and pediatric cardiothoracic surgeons allows us to optimize the outcomes for a vulnerable patient population. Our heart center, which opened in 2015, includes space specifically designed for fetal evaluations and for family counseling. Our recent work in developing a fetal registry and promoting clinical care pathways allows us to continually track and optimize outcomes. We have recently extended our impact by providing educational services for colleagues at Danbury Hospital.
Cardiac magnetic resonance (CMR) imaging has become an important diagnostic tool in the care of all patients with congenital and acquired heart disease. This unique, non-invasive advanced imaging modality allows better assessment of not only the anatomy but also key physiologic parameters including the assessment of blood flow through cardiac structures and quantitative data to assess chamber size and cardiac function. In addition, the unique 3-D images produced by CMR
offer unprecedented graphic detail especially tailored for surgical pre-operative planning for pediatric and adult patients with congenital heart disease. The pediatric CMR Program has grown significantly in the past 11 years and has provided care to over 1,400 pediatric cardiac patients.
Non-Invasive Imaging: Innovations with the CardioOncology Program
The Cardiology and Hematology-Oncology divisions at Connecticut Children’s collaborate in developing a cardio-oncology program, COPE (Cardiovascular Oncology Prevention Experience). This program aims to prevent and/or minimize heart damage caused by chemotherapy exposure and consequently reduce cardiac morbidity and mortality in childhood cancer survivors. This program created a registry of pediatric cancer patients treated with cardio-toxic medications from 1985 up to the present. The registry provides retrospective data, retrospective and prospective cardiac imaging and serologic biomarkers from pediatric cancer patients treated at Connecticut Children’s. We have assembled an interdisciplinary team of cardiologists and oncologists to initiate primary, secondary and tertiary heart failure prevention strategies in our childhood cancer survivors exposed to cardio-toxic chemotherapy. The goal of this program is to reduce any variability in clinical practice and improve outcomes for our patients. The creation of this interdisciplinary team has facilitated prevention strategies and the development of clinical pathways to standardize clinical care for our patients.
A central mission for our division is to educate future providers in our community.
Dr. Felice Heller and Dr. Upadhyay provide training in congenital heart disease for adult cardiology fellows from Hartford Hospital and John Dempsey Hospital. Dr. Alicia Wang also provides training in fetal cardiology for the maternal fetal medicine fellows at the University of Connecticut.
Dr. Bernstein is currently developing the Connecticut Children’s-ER fellowship curriculum with a specific focus on advanced central vascular access in the pediatric population.
We provide sub-specialty training for pediatric residents in Pediatric Cardiology. We also contribute to the training of medical students at both the University of Connecticut and at the state’s newest medical school, Quinnipiac University.
The echo school for pediatric echo-sonographers is now in its sixth year. In November of 2015, our school was the second pediatric echo school in the nation to be recognized by the Joint Review Committee on Education in Cardiovascular Technology (JRC-CVT) and by the Commission of Accreditation of Allied Health Education Programs (CAAHEP).
In January of 2016, Brooke Davey, MD, was awarded the Connecticut Children’s McNeill Teaching Award.
In 2016, Dr. Fred Bernstein was elected a fellow of the American College of Cardiology (ACC).
Dr. Upadhyay and Dr. Heller were among the first group of cardiologists in the country to receive board certification in Adult Congenital Heart Disease, a newly recognized sub-specialty of the American Board of Internal Medicine.
Dr. Seth Lapuk was nominated to the board of directors of the Founders Board of the American Heart Association, the oldest and largest of the AHA’s seven regional boards.
New England Congenital Cardiology Research Foundation Award – T-Cell receptor excision circles: a novel approach to identify immunodeficiency in newborns with congenital heart disease. (08/15–07/16) PI: Dr. Brooke Davey. Co-Investigator: Dr. Olga Salazar.
University of Connecticut Institute for Systems Genomics (ARC) – Use of diversity outbred mice to study cardiotoxicity of chemotherapeutic agents. (2013-17) PI: Dr. Olga Salazar.
Hoffman Foundation – The role of aerobic exercise to modulate cardiotoxicity in long-term cancer survivors. (2014-15) PI: Dr. Olga Salazar.
Hartford Foundation for Public Giving – Establishing cardiac magnetic resonance imaging as the standard of care for childhood cancer patients exposed to anthracycline therapy. (12/2015) PI: Dr. Olga Salazar.
Publications
Heller F, Dabaj I, Mah J, Bergounioux J, Essid A, Bönnemann C, Rutkowski A, Bonne G, Quijano-Roy S, Wahbi K. Cardiac manifestations of congenital LMNA-related muscular dystrophy in children: three case reports and recommendations for care. Cardiol Young. Epub 2016 Dec 12.
Upadhyay S, Marie Valente A, Triedman JK, Walsh EP. Catheter ablation for atrioventricular nodal reentrant tachycardia in patients with congenital heart disease. Heart Rhythm. 2016; 13(6): 1228–37.
Arora B, Upadhyay S, Toro-Salazar O, Gluck J, Sadiq I, Radojevic J, Darsaklis K. Blessing in disguise: absent pulmonary valve in an adult without ventricular septal defect. Circulation. 2015; 132(Suppl 3). A15284 LP-A15284.
Davey B, Rychik J. The natural history of atrioventricular valve regurgitation throughout fetal life in patients with atrioventricular canal defects. Pediatr Cardiol. 2016 Jan; 37(1):50-4. Epub 2015 Aug 4.
Toro-Salazar O, Ferranti J, Lorenzoni R, Walling S, Mazur W, Raman S, Davey B, Gillan E, O’Loughlin M, Klas B, Hor K. Feasibility of echocardiographic techniques to detect subclinical cancer therapeutics–related cardiac dysfunction among high-dose patients when compared with cardiac magnetic resonance imaging. J Am Soc Echocardiogr. 2016 Feb; 29(2):119-31. Epub 2015 Dec 8.
Londono-Obregon C, Goldmuntz E, Davey BT, Zhang X, Slap GB, Kim YY. Adult CHD: the ongoing need for physician counseling about heredity and contraceptive options. Cardiol Young. 2016 Jul 7:1-6. Epub ahead of print.
Paris Y, Toro-Salazar OH, Gauthier NS, Rotondo KM, Arnold L, Hamershock R, Saudek DE, Fulton DR, Renaud A, Alexander ME, on behalf of the New England Pediatric Cardiology Association (NECCA). Regional implementation of a pediatric cardiology syncope algorithm using SCAMPS methodology. J Am Heart Assoc. 2016 Feb 19;5(2): e002931 doi:10.1161/ JAJA.115.002931.
Chhabra L, Crespo E, Toro-Salazar O, Upadhyay S
A usual arrhythmia in an unusual heart. J Am Coll Cardiol. 2016 April; 67(13_S):1116-1116. doi:10.1016/S07351097(16)31117-2.
Toro-Salazar OH, Gillan E, Ferranti J, Orsey A, Rubin K, Upadhyay S, Mazur W, Hor KN. Effect of myocardial dysfunction in cardiac morbidity and all cause mortality in childhood cancer subjects treated with anthracycline therapy. Cardio-Oncol. 2015 Nov; 1(1). doi:10.1186/s40959-0150005-8..
Faculty
Harris Leopold, MD
Division Head Emeritus
McDara Tynan, MD
Interim Division Head
Frederic Bernstein, DO, FACC
Brooke Davey, MD
Alex Golden, MD, MMM
Felice Heller, MD
Colleen Jo, MD
Seth Lapuk, MD, FAAP, FACC
Olga Toro-Salazar, MD
Shailendra Upadhyay, MD
Alicia Wang, MD
Amy Carlucci Wu, MD
Leon Chameides, MD
Professor Emeritus
The Pediatric Cardiothoracic Surgery service is an innovative merged practice supported equally by Connecticut Children’s Medical Center and Yale-New Haven Children’s Hospital. This joint program provides world-class surgical care and support to the children and adults of Connecticut born with congenital heart disease.
We submit operative data and outcomes to the Society of Thoracic Surgeons (STS) Congenital Cardiac Surgery Database. This represents the largest clinical database for our specialty in the world. The STS Database includes more than 94 percent of the Congenital Cardiac Surgery programs in North America. This serves as an excellent benchmark for our outcomes and for the quality of the care we provide. We continue to rank very well with these objective benchmarks. Our results are included and updated on the STS website (www.sts.org).
The section of Pediatric Cardiothoracic Surgery embraces discovery, teamwork, integrity and excellence in all that we do. Dr. Mohsen Karimi continues to champion our blood conservation program. This allows us to perform transfusion-free open-heart surgery for many of our patients.
Innovations
Minimally invasive surgery for selected congenital heart defects
Continued work on blood conservation, transfusionfree protocols
Combined Hybrid Cath Lab/OR approach for a Ventricular Septal Defect (VSD) closure during 2016
Education
Ongoing education of and support for Cardiac Nurses in PICU
Publications
Zahr RA, Kirshbom PM, Kopf GS, Sainathan S, Steele MM, Elder R, Karimi M. Half a century’s experience with classic Glenn shunt. Ann Thorac Surg. 2016; 101:177182.
Karimi M, Kirshbom PM. Anomalous origins of coronary arteries from the pulmonary artery: a comprehensive review of the literature and surgical options. World J Pediatr Congenit Heart Surg. 2015 Oct; 6(4):526-40.
Karimi M, Kirshbom PM, Kopf GS, Steele MM, Sullivan JM. Persistent pulmonary hypertension in a neonate with transposition of great arteries and intact ventricular septum: a case report and review of the literature. World J Pediatr Congenit Heart Surg. July 2015; 6(3):462-5.
Staff
Paul Kirschbom, MD Division Chief
Mohsen Karimi, MD
Jill Sullivan, PA-C
The Division of Child and Adolescent Psychiatry remains a highly vibrant resource within the Department of Pediatrics at the Connecticut Children’s Medical Center. In 2015, we expanded our division to include three new Connecticut Children’s-based FTE psychologists (to serve on the consultation-liaison, Hematology-Oncology, and Pain and Palliative services) and one additional child and adolescent psychiatrist to serve as consultant to the behavioral health emergency services within the Pediatric Emergency Department. In addition, our team at Connecticut Children’s has continued to partner with the inpatient Hospitalist Service (IMT) to develop clinical pathways for our most complicated patients in order to provide effective collaborative care models based on extensive research of evidence-based treatment and national consensus models.
At Connecticut Children’s, the division’s services include: a consultation/liaison service that provides inpatient and outpatient evaluation and treatment services of children and adolescents with co-morbid psychiatric and medical conditions; emergency psychiatric assessment, triage and disposition services within the Connecticut Children’s Emergency Department; and psychologists who provide assessment and psychotherapy to the Divisions of Gastroenterology, Endocrinology, Obesity and Weight Management, Hematology-Oncology, and Pain and Palliative Services.
At the Institute of Living (IOL), clinical services include: individual, group, and family therapies; pharmacotherapy; and diagnostic evaluations. These services are provided through: inpatient units for children and adolescents; the Child and Adolescent Rapid Emergency Services (C.A.R.E.S) unit, a very short-term setting interfacing directly with Connecticut Children’s Emergency Department that focuses on the assessment, stabilization, and disposition of children and adolescents in acute behavioral crisis; the Grace Webb School, a therapeutic educational setting for children and adolescents with co-existing psychiatric and learning difficulties; an outpatient child and adolescent clinic; an Extended Day Treatment Program for older school-aged children; and a partial hospital program for children and adolescents. The adolescent program has a specialized track for early onset psychotic disorders.
On the campus of the Institute of Living (IOL), 2015 brought the celebration of our first anniversary as one of the hubs for the new ACCESS-Mental Health CT program, a collaborative educational, consultation and assessment program between primary care providers and child and adolescent psychiatrists providing more than 1,000 phone consults to primary care physicians (PCPs) and 2,200 care coordination activities since the program started in June of 2014. Under the leadership of Dr. Kim Brownell as medical director, our team has consistently obtained excellent ratings on all hub activities from our PCPs.
On the campus of Connecticut Children’s, we continue to work closely with the Inpatient Management Team (IMT), developing collaborative care pathways, and completed a medically unexplained physical symptoms (MUPS) pathway, and we will be joining a multidisciplinary team to develop a new pathway to target and standardize an approach to acute encephalopathy/delirium. In addition, we have been working with the administration at Connecticut Children’s to promote the development of a pediatric psychology division, which will be directly under the management of Connecticut Children’s. Barbara Rzepski, PhD, the current director of pediatric psychology, has been instrumental in guiding this process.
Additionally, Connecticut Children’s and the Institute of Living (IOL) remain highly active teaching sites for many trainees: Child and Adolescent Psychiatry fellows; General Psychiatry residents; Psychology interns; Pediatric residents and medical students; as well as a post-doctoral fellow who joins our consultation-liaison service for 12 months. This past year, we had over 50 learners assigned to one of our clinical sites including pediatric residents who are now rotating through our adolescent service as part of their adolescent medicine training, in addition to doing electives in child and adolescent psychiatry on our outpatient and consult services.
In the research area, Dr. Lisa Namerow and her colleagues from the IOL, Dr. Gualberto Ruano and Michael Stevens, PhD, have completed their three-year project addressing the role of pharmacogenomics in the treatment of pediatric depression. In addition, Michael Stevens, PhD, remains active in the area of fMRI research in mental health conditions such as ADHD,
autism and mood disorders. In addition, our psychopharmacology pediatric research, under the leadership of Dr. Salma Malik within the Burlingame Center at the IOL, continues to have active and ongoing projects.
Our faculty remain active both in the community and nationally providing presentations on a variety of mental health issues to schools, primary care, and Grand Rounds, and we have been honored to present at national academic meetings on risk assessments and international child and adolescent psychiatry at the American Academy of Child and Adolescent Psychiatry in San Antonio, TX, in October 2015, and on obesity and pain at the International Academy on Pain in April 2015, and the American Academy of Psychology in September 2015.
Publications
Charvet LE, Kasschau M, Datta A, Knotkova H, Stevens MC, et al. Remotely supervised transcranial direct current stimulation (tDCS) for clinical trials: guidelines for technology and protocols. Front Syst Neurosci. 2015; 9:26. PubMed PMID:
25852494; PubMed Central PMCID: PMC4362220.
Book GA, Stevens MC, Assaf M, Glahn DC, Pearlson GD. Neuroimaging data sharing on the neuroinformatics database platform. Neuroimage. 2015 Apr 16. PMID: 25888923.
Witt ST, Stevens MC. Relationship between white matter microstructure abnormalities and ADHD symptomatology in adolescents. Psychiatry Res. 2015 May 30; 232(2):16874. PMID: 25795595; NIHMSID: NIHMS669687; PMCID: PMC4417010.
Stevens MC, Gaynor A, Bessette KL, Pearlson GD. A preliminary study of the effects of working memory training on brain function. Brain Imaging Behav. 2015. Epub ahead of print. PMID: 26138580.
Santos M, Baughcum A, Burton E, Cadieux A, Curran J, Gaffka B, Gray J, Shaffer L, Testa E, Ward W. Fellowship training in pediatric obesity: key components. Prof Psychol Res Pr. 2015 Dec; 46;400-8.

Santos M, Pont S, Estrada E. Childhood obesity related co-morbidities: identification and treatment. In: Hassink S, Hampl S, editors. Clinical management of childhood obesity. McGraw-Hill; 2015.
Astur RS, Palmisano A, Hudd EC, Carew AW, Deaton BE, Kuhney F, Niezrecki R, Santos M. Pavlovian conditioning to food reward as a function of eating disorder risk. Behav Brain Res. 2015; 291;277-82.
Puri MR, Sahl R, Ogden S, Malik S. Prader-Willi Syndrome, management of impulsivity and hyperphagia in an adolescent. J Child Adolesc Psychopharmacol. 2016 May;26(4):403-4.
Staff
Robert Sahl, MD
Division Head
J. Craig Allen, MD
Michal Assaf, PhD
Sudeshna Basu, MD
Kim Brownell, MD
Eric D. Cohen, MD
Suzanne Femino, APRN
Julie Goslee, MD
Brad Jerson, PhD
Malik S, Azeem MW. Psychopharmacogenomics in pediatric psychiatry with a focus on cytochrome P450 testing. Psychiatr Ann. 2016 Jan;46(1):52-7.
Namerow L, Rzepski B, Wakefield E, Kutner E, Sahl R. Pain amplification syndrome: a biospsychosocial approach. Sem Pediatr Neurol. 2016 Winter.
Saili Kalaskar, MD
Emily Kutner, PhD
Mirela Loftus, MD
Daane Logsdon, DO
Salma Malik, MD
Lynn Mangini, MD
Lisa Namerow, MD Director of Consultation Services to Connecticut Children’s Medical Center
Francisco Ripepi, MD
Kenneth Robson, MD
Rosemary Coratola, PsyD, LMFT
Jessica Guite, PhD
Mary Gratton, PhD, LCSW
Barbara Rzepski, PhD Director of Pediatric Psychology
Melissa Santos, PhD
Michael Stevens, PhD
Emily Wakefield, PsyD
The Division of Community Pediatrics is the largest division at Connecticut Children’s Medical Center. There are 21 active, 20 courtesy, and 90 refer-and-follow members.
The division is concerned with issues regarding the advocacy and delivery of health care to children in community-based settings and institutions such as office-based practice, well-baby nurseries, community health centers, schools, camps, foster-care adoptive services, etc. Our members provide primary pediatric care to most children from the Greater Hartford area. Members see to well care, sick care, and behavioral health needs of children. Member pediatricians diagnose most chronic diseases of children in our area. Our members work closely with specialists in other divisions to coordinate care for the sickest children in the community.
Pediatricians in the division consult with local school systems to address public health and sports medicine issues. Our members serve on a variety of hospital committees, and they provide neonatal care at John Dempsey Hospital in Farmington, Hartford Hospital in Hartford, Manchester Memorial Hospital in Manchester, and Saint Francis Hospital in Hartford. Members are interviewed by public media including radio, television and newspapers on a wide variety of pediatric and public health care issues of local and national interest, including childhood obesity, school safety and bullying, vaccine advocacy, and changes to guidelines for cold and cough care for young children.
Division members provide instruction and supervision for student and resident continuity practices as well as the pediatric ambulatory rotation for third year students. In addition to providing rich and varied clinical experiences, members educate students and residents about external issues that influence child health care, such as delivery care models, working with consultants and other professionals to address health care plans for children, coding and other business practicalities in community pediatrics, and time and personal health management. We seek to identify innovative practice styles in health care delivery and opportunities to improve patient education and health outcomes.
Members engage in many collaborative programs within broader department- and state-based initiatives to provide better care for children. These include the Easy Breathing© Program, which has led to improved health practices and better outcomes for children with asthma; the Medical Home initiative, to help coordinate care for children with special health care needs; and the creation of collaborative practice models/co-management guidelines, including migraine headaches, Lyme disease, voiding dysfunctions, premature adrenarche, and concussions.
One of the primary goals of our division is the improvement of care coordination and communication between specialists and generalists. With that purpose in mind, we invite consultants to our monthly meetings to discuss clinical topics of joint interest and address barriers to information sharing.
Members are actively involved in ongoing education through Grand Rounds and evening lecture series in pediatrics and child mental health, to promote topics of interest to the community physicians as well as nurse practitioners, physician assistants and school nurses who care for children in the community setting.
The division sponsors a lectureship in honor of Christopher O’Connor, MD, that addresses topics of concern to community-based pediatrics.
Drs. Larry Scherzer and Aruna Ramanan were honored to be named Outstanding Outpatient Clinical Preceptors by the University of Connecticut School of Medicine. Scherzer was awarded the honor in 2014-15, Ramanan in 2015-16.
In November of 2015, Dr. Karen Rubin presented CoManagement Experience (at Connecticut Children’s) at the Patient Centered Collaborative Conference: Investing in Primary Care: Patients, Professionals and Payments in Washington, D.C.
Publications
Feyissa E, Cornell E, Chandhok L, Wang D, Ionita C, Schwab J, Kostyun R, Wilion F, Rubin K. Impact of co-management at the primary-subspecialty care interface on follow-up and referral patterns for patients with concussion. Clin Pediatr. 2015. doi: 10.1177/0009922814566929.
Staff
Douglas MacGilpin, MD co-Division Head
Larry Scherzer, MD co-Division Head
Robert S. Adamenko, MD
Luis Alonso, MD
Supriya Atianard, MD
Brenda K. Balch, MD
Meredith W. Barrows, MD
Amy H. Baumer, MD
Lucia C. Benzoni, MD
Thomas B. Binder, MD
Nancy B. Brown, MD
David L. Brown, MD
William Brownstein, MD
Leon Chameides, MD Professor Emeritus
Carolyn Clark, MD
Paul Clarke, MD
Della M. Corcoran, MD
Allison S. Cowl, MD
J. Michael Curi, MD
Sachin Dhingra, MD
Louis DiMauro, MD
Leo J. DiStefano, MD
Allyson Duffy, MD
Nancy S. Dunbar, MD, MPH
Jeffrey M. Factor, MD
Parvin Fadakar, MD
John J. Fote, MD
Bruce Freeman, MD
Cecille Freilich, MD
Thomas Fromson, MD
Richard W. Geller, MD
Gregory S. Germain, MD
Susan Glasser, MD
Dyan Griffin, MD
Marshall P. Grodofsky, MD
Richard C. Harvey, Jr., MD
Hillary S. Hernandez-Trujillo, MD
Elizabeth Herz, MD
Delbert H. Hodder, MD
Peter J. Jannuzzi, MD
Brad Jubelirer, MD
Anjum Khera, MD
Kimberly Kim, MD
Margaret Kloby, MD
Natalie Komaiszko, MD
Lauren Kopyt, MD
Gubbanna S. Kumar, MD
Sydney Ladenheim, MD
Jerome Lahman, MD
Christine Lamoureux, MD
John H. Lavalette, MD
Carol Leicher, MD
Deepa Limaye, MD
Foong-Yi Lin, MD
Stephen J. Maddox, Jr., MD
Asha Manaktala, MD
Kathleen A. Marinelli, MD
Linda Mathew, MD
John Mathews, MD
Bruce McDonald, MD
Louis M. Mendelson, MD
Judith C. Meyers, PhD
Debora Mihaley-Sobelman, MD
Donald Mordavsky, MD
Sylvia Nash, MD
Margaret O’Neill, MD
James O’Connor, MD
Kathy Pae, MD
Hemant K. Panchal, MD
Elizabeth T. Pericat, MD
Ishrat Quadri, MD
Chitraleka Ramanan, MD
Tina Roman, MD
Cynthia C. Roque, MD
Viviann Rubin, MD
Kweku G. Sam, MD
Lynelle Schneeberg, PsyD
Jennifer Schwab, MD
Gavin Schwarz, MD
John F. Siraco, MD
Candra L.
Smith-Slatas, MD
Daniel L. Spada, MD
Kenneth N. Spiegelman, MD
Prasad Srinivasan, MD
Neil Stein, MD
Martha Sternberg, MD
Carrie S. Streim, MD
Charles Thompson, MD
Robert R. Toscano, MD
Kerline A. Vassell, MD
Christopher Veale, MD
Rachna Walia, MD
Ramindra Walia, MD
Matthew Warren, MD
Harry C. Weinerman, MD
Allison Whitaker, MD
Felicia M. Wilion, MD
Richard S.K. Young, MD
Robert W. Zavoski, MD
Sophia Zervas-Grant, MD
Barbara Ziogas, MD

The Division of Pediatric Critical Care is dedicated to the delivery of state-of-the-art child and family centered care for critically ill and injured children.
The division’s mission is accomplished by a collaborative group that champions a multidisciplinary approach to care, the incorporation of best available evidence into clinical practice, and acquisition of new knowledge through clinical research. Attention to patient safety, continuous performance improvement, and education of physicians, nurses, and other care team members is paramount.
Major awards and academic accomplishments among the division members include important contributions to several national societies and both internal and external collaborations:
Dr. Christopher Carroll continues many clinical and translational research activities, collaborating with investigators at Connecticut Children’s, Jackson Laboratories, and internationally. He lectures frequently at international conferences on asthma, respiratory disease, critical care, and new media. He continues in leadership roles in major medical organizations including:
Associate Editor of two journals: Chest and Journal of Asthma
Serves as chair of the New Media Workgroup, is a member of the Steering Committee of the Critical Care NetWork, is an ex-officio of the Scientific Presentation and Awards Committee, a member of the Council of Advisors, a member of the Board of Trustees for the CHEST Foundation, and is social media advisor for the American College of Chest Physicians
He has an appointment to the Program and the Planning Committee of the American Thoracic Society
He has an appointment to the Multidisciplinary Critical Care Knowledge Assessment Program Committee, and serves on the Social Media Workgroup
Dr. Adam Silverman continues his support of global health care activities as the director of the Center for Global Health, which organizes the annual Global Healthcare Fair and Global Health Film Festival. Over the last two years, he has lectured over 15 times regionally, nationally and internationally about
global health care topics. He co-organized a session where speakers from the U.S., Canada, and Uganda discussed “Pediatric Critical Care in Resource-Limited Settings” at the 2016 AAP NCE meeting. He co-authored an abstract presented at the 2015 PAS meeting in San Diego, CA, about the reduction in newborn mortality observed in Haiti since the initiation of collaborative capacity-building efforts. Locally, he continues to support the Global Healthcare Educational Pathway for pediatric residents, provides supervision for an elective for pediatric residents to Hospital Bernard Mevs in Port-au-Prince, Haiti, and organizes the activities of Connecticut Children’s Medical Center staff members who travel to developing countries to help improve the health care of children. He also continues to serve as the membership chairperson for the American Academy of Pediatrics Section on International Child Health. In 2016, he received the James P. Friedman Justice Award from the Congregation Beth Israel Social Justice Committee.
Dr. Heather Schlott continues as medical director of the hospital’s extracorporeal membrane oxygenation (ECMO) program, in partnership with Pediatric Surgery and Neonatology physician colleagues, as well as nursing, respiratory therapy, and perfusion team members. This technology provides stateof-the-art heart and lung support for our most critically ill and injured patients. The program has grown and been extremely successful, with outcomes that exceed national benchmarks. In fact, Connecticut Children’s received a Silver Award (the highest award possible for our size program) for its excellent outcomes from the national Extracorporeal Life Support Organization. Dr. Schlott also led the development and implementation of our continuous renal replacement therapy (CRRT) program, which has grown with excellent clinical results. These capabilities are key components of modern PICU care and specifically crucial to the expansion of our Cardiac Surgery program.
Starting in 2016, Dr. Schlott assumed multidisciplinary leadership responsibility for Connecticut Children’s Medical Center’s participation in the Children’s Hospital Association “Improving Pediatric Sepsis Outcomes” Collaborative, which has a goal of reducing sepsis deaths by 75 percent and hospital-onset severe sepsis by 75 percent by 2020.
In further regard to the Cardiac Surgery program, Dr. Kenneth Banasiak has taken a lead role in clinical, educational, and performance improvement aspects of the multidisciplinary process in collaboration with our Cardiology and Cardiac Surgery colleagues. They are implementing clinical pathways that will standardize and streamline the care of post-operative patients. He also is creating a new Critical Care Physiology course for pediatric residents.
Dr. Daniel Fisher continues his work with colleagues in the divisions of Otolaryngology and Pediatric Surgery to hone the activities of the Critical Airway Response Team, which responds to life-threatening emergencies in children with upper airway obstruction. In addition, he continues his leadership in the refinement of the hospital’s recently implemented comprehensive electronic medical record, which has a huge impact on the quality of daily patient care, safety improvement, and clinical research.
Dr. Leonard Comeau continues his activities to improve the comfort and quality of care for our patients, both in the PICU and hospital-wide. He is a leader of our developing comprehensive palliative care program. He participates in care delivered by the Sedation Service, and also serves as the leader of the quality and safety oversight activities of the Sedation and Analgesia Committee. He serves as the chair of the hospital Ethics Committee, which deals with issues related to the appropriateness and decision-making regarding health care for some of our most complicated patients.
Dr. Allison Cowl continues her clinical research collaborations with the Pediatric Acute Lung Injury and Sepsis Investigators (PALISI) international network, focusing on various aspects of the management of sedation and pain during the care of critically ill children. She is implementing clinical research protocols spurred by results of a national multicenter study of sedation practices in children with severe respiratory failure. She serves as the lead for educational efforts in the PICU including expansion of the Critical Care subtrack, with multiple new rotations for pediatric residents who are interested in pursuing careers in acute care pediatrics and specifically, Pediatric Critical Care Medicine. She has also completed a study of the deployment of PICU services in relation to a subset of surgical patients.
Dr. Rosanne Salonia continues her work as a member of the Emergency Response Committee, which oversees the use of the Pediatric Early Warning Score system (PEWS/MET) in focusing attention on patients at risk for clinical deterioration. She manages the associated database and coordinates the ongoing evaluation of the data. She also continues her clinical research collaboration with the Pediatric Neurocritical Care Research Group (PNCRG), which deals with various aspects of care of patients with severe brain injuries (such as management of sedation and delirium). She also is involved in collaboration with the national Children’s Hospitals’ Solutions for Patient Safety group, which works to eliminate serious safety events in children’s hospitals.
Dr. Zucker is the chairperson of the Peer Review Committee, which oversees the medical staff’s evaluations of individual physician’s clinical performance and patient outcomes in pursuit of the best and safest care for our patients. In conjunction with external facilitators in 2016, he was the physician champion for a professional development program designed to improve medical staff members’ resilience and engagement in the workplace.
Publications
Bhandari A, Carroll CL, Bhandari V. BPD following preterm birth: a model for chronic lung disease and a substrate for ARDS in childhood. Front Pediatr. 2016; 4:1-7.
Hymel KP, Herman BE, Narang SK, Graf JM, Frazier TN, Stoiko M, Christie LM, Harper NS, Carroll CL, Boos SC, Dias M, Pullin DA, Wang M. Theoretical re-analysis of two previously published datasets: reply. J Pediatr. 2016; 171:321-2.
Carroll CL, Bruno K, vonTschudi M. Free open access medical education and social media: the future of medical and nursing education? Am J Crit Care. 2016; 25(1):93-6.
Hymel KP, Herman BE, Narang SK, Graf JM, Frazier TN, Stoiko M, Christie LM, Harper NS, Carroll CL, Boos SC, Dias M, Pullin DA, Wang M, for the Pediatric Brain Injury Research Network (PediBIRN) Investigators. Potential impact of a validated screening tool for pediatric abusive head trauma. J Pediatr. 2015; 167(6):1375–81.
Canarie MF, Barry S, Carroll CL, Hassinger A, Kandil S, Li S, Pinto M, Valentine S, Faustino EVS. Risk factors for delayed enteral nutrition in critically ill children. Pediatr Crit Care. 2015; 16(8):e283-89.
Sala KA, Moore A, Desai S, Welch K, Bhandari S, Carroll CL. Factors associated with disease severity in children with bronchiolitis. J Asthma. 2015; 52(3):268-72.
Gupta P, Robertson MJ, Beam B, Gossett JM, Schmitz ML, Carroll CL, Edwards JD, Fortenberry JD, Butt W. Relationship of ECMO duration with outcomes after pediatric cardiac surgery: a multi-institutional analysis. Minerva Anestesiol. 2015; 81:619-27.
Essouri S, Carroll CL, for the Pediatric Acute Lung Injury Consensus Conference Group. Noninvasive support and ventilation for pediatric acute respiratory distress syndrome: proceedings from the pediatric acute lung injury consensus conference. Pediatr Crit Care. 2015; 16(5):S102-10.
The Pediatric Acute Lung Injury Consensus Conference Group. Pediatric acute respiratory distress syndrome: consensus recommendations from the Pediatric Acute Lung Injury Consensus Conference. Pediatr Crit Care. 2015; 16(5):428-9.
Choo EK, Ranney ML, Chan T, Trueger NS, Walsh AE, Tegtmeyer K, McNamara SO, Choi RY, Carroll CL. Twitter as a tool for communication and knowledge exchange in academic medicine: a guide for skeptics and novices. Med Teach. 2015; 37(5):411-6.
Weiss SL, Fitzgerald JC, Pappachan J, Wheeler D, JaramilloBustamante JC, Salloo A, Singhi SC, Erickson S, Roy JA, Bush JL, Nadkarni VM, Thomas NJ; Sepsis Prevalence, Outcomes, and Therapies (SPROUT) Study Investigators and Pediatric Acute Lung Injury and Sepsis Investigators (PALISI) Network. Global epidemiology of pediatric severe sepsis: the sepsis prevalence, outcomes, and therapies study. Am J Respir Crit Care Med. 2015; 191(10):1147-57.
Chapters
Carroll CL. Near fatal asthma in children. In: Turner D, editor. Current concepts in pediatric critical care. Des Planes, IL: Society of Critical Care Medicine; 2016.
Carroll CL. Mechanical ventilation in pediatric asthma. In: Rimensberger PC, editor. Neonatal and pediatric mechanical ventilation: from basics to clinical practice. Heidelberg, Germany: Springer; 2015. p. 1313-24.
Staff
Aaron Zucker, MD Division Head
Kenneth Banasiak, MD
Christopher Carroll, MD
Leonard Comeau, MD
Allison Cowl, MD
Daniel Fisher, MD
Rosanne Salonia, MD
Heather Schlott, MD
Adam Silverman, MD
Petronella Stoltz, APRN
The Division of Pediatric Dentistry provides a full range of primary and specialty dental services for children. Significant expertise is offered in the areas of treatment and prevention of dental diseases with special focus in areas of dentofacial development, craniofacial anomalies, oral pathology, behavior management modalities, dental care for children with special health needs, and dental public health issues affecting children.
Services available include restorative dentistry, surgical treatment of oral and perioral hard and soft tissue pathology, dental treatment with procedural sedation, oral rehabilitation under general anesthesia, and treatment of minor orthodontic problems. The division provides quality oral health care in a timely and caring manner. Emphasis is placed on assisting other specialty divisions within Connecticut Children’s Medical Center in managing their patients’ overall health care needs by preventing and treating oral disease. The division also is committed to supporting research activities consistent with the Connecticut Children’s and University of Connecticut School of Dental Medicine institutional missions.
The UConn School of Dental Medicine’s Division of Pediatric Dentistry, headed by Dr. Mina Mina, operates a full-service dental clinic at Connecticut Children’s. The dental clinic is the principal clinical site for the UConn School of Dental Medicine’s Advanced Education Residency Program in Pediatric Dentistry. Dr. Bina Katechia serves as the Residency Program Director, and Dr. Jorge Rabat is the Assistant Residency Program Director. Dr. Keri Discepolo serves as the Director of the Division of Pediatric Dentistry.
The division is currently comprised of 58 members of the dental staff, 33 active, 21 courtesy, and four consulting. There are 40 pediatric dentists, 15 oral surgeons, one orthodontist, one oral pathologist, and one prosthodontist. From January 2015 to December of 2016, the Division of Dentistry performed 1,239 oral rehabilitation surgical cases in the operating room. The Connecticut Children’s dental clinic provided 9,227 outpatient clinical and preventive visits. Over 11,637 dental procedures were completed in the clinic. The pediatric residency also utilizes the services of the Procedural Sedation Services to perform sedation for dental patients on a weekly
basis. A total of 275 patients received nitrous oxide sedation during the delivery of dental services in the clinic.
The Pediatric Residency program supported research presentations by dental residents at the annual meeting of the American Academy of Pediatric Dentistry in May 2016. The residency was pleased to have five residents complete the program in June 2016, and five of them challenged and successfully completed the Qualifying Examination of the American Board of Pediatric Dentistry (ABPD) that same month. The current combined first- and second-year resident classes have a total of 10 residents. This represents the culmination of our continued residency program expansion, facilitated by a 5-year $1.8 million HRSA Title VII Grant. The dental clinic also provides a site for the clinical education of UConn Dental Students, UConn Advanced Education in General Dentistry residents, Tunxis Community College Dental Hygiene students, Tunxis Community College Dental Assistant students, Prince Regional Vocational Technical School Dental Assistant students, and Porter and Chester Dental Assistant students.
In addition to Drs. Katechia, Mina, Rabat, and Discepolo, three full-time UConn Pediatric Dentistry faculty serve as attendings, including Dr. Deborah Redford-Badwal, the Dental Director of the Connecticut Children’s Craniofacial Disorders Team. The clinic is additionally supported by three part-time UConn attending faculty. Oral Surgery support for the clinic is provided by residents and attending faculty from the UConn Oral and Maxillofacial Surgery Residency Program, directed by Dr. David Shafer.
The following members of the division received a variety of honors and accolades over the past year:
Drs. Bina Katechia and Monica Cipes serve as consultants to the Examination Committee of the American Board of Pediatric Dentistry.
Dr. Ira Greene is president of the Connecticut Society of Pediatric Dentists.
Dr. Keri Discepolo is vice president of the Connecticut Society of Pediatric Dentists.
Publications
Rifaey HS, Villa M, Zhu Q, Wang YH, Safavi K, Chen IP. Comparison of the osteogenic potential of mineral trioxide aggregate and endosequence root repair material in a 3-dimensional culture system. J Endod. 2016 May; 42(5):760-5. doi: 10.1016/j. joen.2016.02.001.
Discepolo K, Sultan M. Investigation of adult stainless steel crown longevity as an interim restoration in pediatric patients. Int J Paediatr Dent. 2016 Jul 30.
Popple B, Wall C, Flink L, Powell K, Discepolo K, Keck D, Mademtzi M, Volkmar F, Shic F. Brief report: remotely delivered video modeling for improving oral hygiene in children with ASD: a pilot study. J Autism Dev Disord. 2016 Aug;46(8):2791-6.
Sagomonyants K, Kalajzic I, Maye P, Mina M. Enhanced dentinogenesis of pulp progenitors by early exposure to FGF2. J Dent Res. 2015 Aug;94(11):1582-90.
Sagomonyants K, Mina M. Stage-specific effects of fibroblast growth factor 2 on the differentiation of dental pulp cells. Cells, Tissues, Organs. 2015 Mar;199(5-6):311-28.
Staff
Keri Discepolo, DDS, MPH Division Head
Joanna Douglass, BDS, DDS
Ira Greene, DDS
Bina Katechia, DDS, MSc
Mina Mina, DMD, MSD, PhD
Jorge Rabat, DDS
Deborah Redford-Badwal, DDS, PhD
Moises Y. Salas, DDS, MPH
Gary Schulman, DDS
Yu-Hsiung Wang, DDS, PhD
Paulette Chung, RDH

The division’s mission is: 1) to provide comprehensive and compassionate diagnosis and management for children with neurodevelopmental and behavioral problems that range from normative deviations to rare disorders; 2) to teach health care professionals about these problems; 3) to add to existing knowledge by researching relevant questions in the field; and, 4) to offer advocacy, and to support public policy development.
The Division of Developmental and Behavioral Pediatrics (formerly known as Developmental and Rehabilitation Medicine) is composed of a diverse faculty of Developmental-Behavioral Pediatricians (DBPeds) who practice at a number of sites throughout the state.
The division added Dr. Robert D. Keder, a DevelopmentalBehavioral pediatrician in May 2016. His research interests include bullying. Beyond his extensive clinical interests, he brings expertise in building documentation elements for and specialty-specific use of the electronic health record (EHR).
Division clinical services occur in a number of settings – outpatient, inpatient, and community-based (e.g., schools, CT Birth-to-Three system, and other agencies). We provide direct consultation, ongoing clinical care, and school-based program consultation.
The division has focused extensive resources on developing the Autism Spectrum Assessment Program (ASAP). We have established a collaboration that includes DBPeds, SpeechLanguage Pathology, and Neurology (i.e. the “Neurogenetics ASAP program”). This provides a direct line from the autism diagnosis to standard-of-care clinical and laboratory evaluation. It also provides the option for all patients to participate in our research collaborations.
Seek funding for Connecticut Bioscience Innovation Fund (CBIF) genetics grant, the goal of which is to assess whether the “AllSeq” platform is a good mechanism for
bringing additional genetic insights into clinical practice for people with autism.
Collaborate with the sedation team to help children with autism and other developmental disabilities to prepare for medical procedures. This will have organization-wide impact and has the potential to alter standards of care for autism.
Develop a statewide school consultation program.
Adjust the optimal “divisional location” for Pediatric Physiatry, considering the organizational strategic commitment to a Neurosciences Center of Excellence.
The division’s research includes: Multidisciplinary “ARC” initiative between CT Children’s Medical Center, UConn Health Center and the Jackson Laboratory: Neuronal Synaptic and Circuit Dysfunction in the Autism Spectrum Disorders. Dr. Milanese is one of the principal investigators. 2013-2018. Funded by: Institute for Systems Genomics.
Connecticut Children’s Medical Center was awarded an 18-month grant (January 2016-June 2017) to study and promote culturally effective autism screening, referral and service provision in pediatric practices and Birth-to-Three programs. PI: Thyde Dumont-Mathieu, MD, MPH.
Future research projects include identifying ways to improve shared decision-making within the well-child care visit in order to better convey autism risk and the urgency of obtaining early intervention, as well as determining the feasibility of screening and evaluating children in nontraditional venues such as child care centers.
Dworkin PH. [editorial] Towards a critical reframing of early detection and intervention for developmental concerns. J Dev Behav Pediatr. 2015; 36:637–8. doi: 10.1097/ DBP.0000000000000216.
Garg A, Dworkin PH. Surveillance and screening for social determinants of health. The medical home and beyond. JAMA Pediatr. 2016; 170:189-190. doi:10.1001/jamapediatrics.2015.3269.
Hughes M, Joslyn A, Wojton MM, O’Reilly M, Dworkin PH
Connecting vulnerable children and families to communitybased programs strengthens parents’ perceptions of protective factors. Infants Young Child. 2016; 29(2):114–127. doi:0.1097/IYC.0000000000000059.
Dworkin PH, Sood B. A population health approach to system transformation for children’s healthy development. Child Adolesc Psychiatric Clin N Am. 2016; 25(2):307-17. doi: 10.1016/j.chc.2015.12.004.
Robins DL, Adamson LB, Barton M, Connell JE Jr, DumontMathieu T, Dworkin PH, Fein D, Greenstein MA, Hsu H-W, Kerns C, Newschaffer C, Plumb J, Shattuck P, Turchi R, Vivanti G. [letter to the editor] Universal autism screening for toddlers: recommendations at odds. J Autism Dev Disord. 2016; 46(5):1880-2.
Garg A, Boynton-Jarrett R, Dworkin PH. Viewpoint. Avoiding the unintended consequences of screening for social determinants of health. JAMA. 2016; 316(8):813-4. doi:101001/ jama.2016.9281.
Dworkin PH. Screening: general considerations. In: McInerny TK, Adam HM, Campbell DE, Kamat DM, Kelleher KJ, editors. American Academy of Pediatrics Textbook of Pediatric Care. 2nd ed. Elk Grove Village, IL: American Academy of Pediatrics; 2016. p. 191-5.
Staff
Ann Milanese, MD
Division Head
Thyde Dumont-Mathieu, MD
Paul H. Dworkin, MD
Mark A. Greenstein, MD
Robert D. Keder, MD
John Pelegano, MD
Sarah Schlegel, MD
Jennifer Ryiz-Semmel, BSN, RN, CPN, CLC

The Division of Digestive Diseases, Hepatology, and Nutrition is committed to cutting edge and innovative clinical care of infants, children and adolescents, pioneering clinical, translational, and basic research, and the education of the next generation of physicians.
In 2016, the division, small by the standards of other children’s hospitals, was a leader on both the national and international stages. Our Center for Pediatric Inflammatory Bowel Disease (IBD), the largest program in the region between Boston and New York, currently provides care to over 800 children with Crohn’s disease and ulcerative colitis. We are the Clinical Coordinating Center for a $10.4 million grant from the National Institutes of Health to lead the PROTECT Study: Predicting Response to Standardized Pediatric Colitis Therapy. This five-year effort coordinates the resources of 29 leading pediatric IBD centers in North America to study newly diagnosed children with ulcerative colitis. PROTECT, along with the Crohn’s and Colitis Foundation of America (CCFA) RISK stratification study of 1,200 newly diagnosed children with Crohn’s disease, has squarely placed Connecticut Children’s at the epicenter of pioneering research in pediatric inflammatory bowel disease. Dr. Jeffrey Hyams, Division Chief, heads the IBD program and continues to lead many international efforts to improve the health of children with these disorders. He was also the co-chairman of the Rome IV book on functional gastrointestinal disorders in children that serves as the basis for all research in this important area. The Rome IV book was published in 2016.
Dr. Wael Sayej of the division continues his productive work in the laboratory of Dr. Christine Finck from the Department of Surgery to improve our understanding of the role and function of esophageal epithelial cells in eosinophilic esophagitis (EoE) utilizing biomimetic systems. The team is also working on developing a patient-specific diagnostic test that will confirm the diagnosis of EoE and identify the triggers responsible in each patient. The team is also performing state-of-the-art research on esophageal tissue engineering. Dr. Sayej directs the EoE program, which includes Susan Goodine, RN, and Lori Alexander, RN. We continue to strive to formally establish a clinical center for gastrointestinal eosinophilic disorders. Over 250 patients are currently being cared for in the program.
Dr. Zev Davidovics directs our fecal transplant team for the treatment of refractory Clostridium difficile infection and collaborates with Dr. George Weinstock at Jackson Laboratories to study how specific bacteria help eradicate Clostridium difficile infection. Dr. Davidovics also is involved with ground-breaking research on the microbiome of breast milk. Dr. Jasmeet Mokha, a recent graduate of our fellowship program and now an attending physician, published novel work concerning the relationship of the intestinal microbiome and cholestasis in premature infants receiving parenteral nutrition. Dr. Mokha won the Nutrition Award at the World Congress of Pediatric Gastroenterology, Hepatology, and Nutrition in Montreal, Canada.
Our Multi-Disciplinary Intestinal Rehabilitation Team (IRT) is the only one of its kind in the state. Co-directed by Drs. Zev Davidovics and Karan Emerick, this group focuses on the care of children with intestinal failure of all causes. Phyllis Bebyn, RN, and Kate Samela, RD, are integral parts of this team that also facilitates transition from hospital to home.
Our Center for Pediatric Liver Care, directed by Dr. Karan Emerick, provides care to children with a wide range of hepatic disorders including chronic hepatitis B and C, metabolic liver disease, autoimmune disease, and acute and chronic liver failure. It provides pre- and post-transplant care to 40 children. Samantha Lee, APRN, joined the center in 2016 and has helped to develop a formal program to care for children with non-alcoholic fatty liver disease (NAFLD).
Dr. Bella Zeisler is a key member of the Aerodigestive Program at Connecticut Children’s Medical Center. This coordinated program of otolaryngologists, pulmonologists, gastroenterologists, and speech therapists care for children with complex airway, pulmonary and gastrointestinal disorders.
Dr. Fran Mohr has become the Division Quality and Safety Officer as part of the GI Service Line Development. She will be working closely with the hospital Quality and Safety Program. Dr. Peter Townsend joined the faculty in 2015, followed by Dr. Melissa Fernandes, who completed her fellowship at University of California, San Francisco, and Dr. Jasmeet Mokha who completed his fellowship at Connecticut Children’s.
Our fellowship program under Dr. Sayej’s leadership has benefited from the recruitment of highly qualified graduating pediatric residents who spend three years receiving their subspecialty training. The great depth in our pediatric surgical and radiology programs as well as the great variety of clinical disorders and the intimate involvement of our faculty in education makes our fellowship program particularly attractive.
Publications
Sun H, Papadopoulos EJ, Hyams JS, Griebel D, Lee JJ, Tomaino J, Mulberg AE. Well-defined and reliable clinical outcome assessments for pediatric Crohn disease: a critical need for drug development. J Pediatr Gastroenterol Nutr. 2015; 60:729-36.
Sharma S, Eckert D, Hyams JS, Mensing S, Thakkar RB, Robinson AM, Rosh JR, Ruemmele FM, Awni WM. Pharmacokinetics and exposure-efficacy relationship of adalimumab in pediatric patients with moderate to severe Crohn’s disease: results from a randomized, multicenter, phase-3 study. Inflamm Bowel Dis. 2015; 21:783-92.
Oliva-Hemker M, Hutfless S, Al Kazzi ES, Lerer T, Mack D, LeLeiko N, Griffiths A, Cabrera J, Otley A, Rick J, Bousvaros A, Rosh J, Grossman A, Saeed S, Kay M, Carvalho R, Keljo D, Pfefferkorn M, Faubion W Jr, Kappelman M, Sudel B, Schaefer ME, Markowitz J, Hyams JS. Clinical presentation and five-year therapeutic management of very early-onset inflammatory bowel disease in a large North American cohort. J Pediatr. 2015; 167:527-32.
Ning K, Gettler K, Zhang W, Ng SM, Bowen BM, Hyams J, Stephens MC, Kugathasan S, Denson LA, Schadt EE, Hoffman GE, Cho JH. Improved integrative framework combining association data with gene expression features to prioritize Crohn’s disease genes. Hum Mol Genet. 2015; 24:4147-57.
Grossi V, Lerer T, Griffiths A, LeLeiko N, Cabrera J, Otley A, Rick J, Mack D, Bousvaros A, Rosh J, Grossman A, Saeed S, Kay M, Boyle B, Oliva-Hemker M, Keljo D, Pfefferkorn M, Faubion W, Kappelman MD, Sudel B, Markowitz J, Hyams JS. Concomitant use of immunomodulators affects the du-
rability of infliximab therapy in children with Crohn’s disease. Clin Gastroenterol Hepatol. 2015;13:1748-56.
Cutler DJ, Zwick ME, Okou DT, Prahalad S, Walters T, Guthery SL, Dubinsky M, Baldassano R, Crandall WV, Rosh J, Markowitz J, Stephens M, Kellermayer R, Pfefferkorn M, Heyman MB, LeLeiko N, Mack D, Moulton D, Kappelman MD, Kumar A, Prince J, Bose P, Mondal K, Ramachandran D, Bohnsack JF, Griffiths AM, Haberman Y, Essers J, Thompson SD, Aronow B, Keljo DJ, Hyams JS, Denson LA; PRO-KIIDS Research Group, Kugathasan S. Dissecting allele architecture of early onset IBD using high-density genotyping. PLoS One. 2015 Jun 2; 10(6):e0128074.
Wang X, Yamamoto Y, Wilson LH, Zhang T, Howitt BE, Farrow MA, Kern F, Ning G, Hong Y, Khor CC, Chevalier B, Bertrand D, Wu L, Nagarajan N, Sylvester FA, Hyams JS, Devers T, Bronson R, Lacy DB, Ho KY, Crum CP, McKeon F, Xian W. Cloning and variation of ground state intestinal stem cells. Nature. 2015 Jun 11; 522(7555):173-8.
Choshen S, Finnamore H, Auth MK, Bdolah-Abram T, Shteyer E, Mack D, Hyams J, LeLeiko N, Griffiths A, Turner D. Corticosteroid dosing in pediatric acute severe ulcerative colitis: a propensity score analysis. J Pediatr Gastroenterol Nutr. 2016; 63:58-64.
Hyams JS, Di Lorenzo C, Saps M, Shulman RJ, Staiano A, van Tilburg M. Functional disorders: children and adolescents. Gastroenterology. 2016 Feb 15. pii: S0016-5085(16)00181-5.
Turner D, Levine A, Walters TD, Focht G, Otley A, López VN, Koletzko S, Baldassano R, Mack D, Hyams J, Griffiths AM. Which PCDAI version best reflects intestinal inflammation in pediatric Crohn’s disease? J Pediatr Gastroenterol Nutr. 2016.
Turner D, Koletzko S, Griffiths AM, Hyams J, Dubinsky M, de Ridder L, Escher J, Lionetti P, Cucchiara S, Lentze MJ, Koletzko B, van Rheenen P, Russell RK, Mack D, Veereman G, Vermeire S, Ruemmele F. Use of placebo in pediatric inflammatory bowel diseases: a position paper from ESPGHAN, ECCO, PIBDnet, and the Canadian Children IBD Network. J Pediatr Gastroenterol Nutr. 2016 Jan; 62(1):183-7.
Livshits A, Fisher D, Hadas I, Bdolah-Abram T, Mack D, Hyams J, Crandall W, Griffiths AM, Turner D. Abdominal X-ray in pediatric acute severe colitis and radiographic predictors of response to intravenous steroids. J Pediatr Gastroenterol Nutr. 2016; 62:259-63.
Singh N, Rabizadeh S, Jossen J, Pittman N, Check M, Hashemi G, Phan BL, Hyams JS, Dubinsky MC. Multi-center experience of vedolizumab effectiveness in pediatric inflammatory bowel disease. Inflamm Bowel Dis. 2016; 22:2121-6.
Grossi V, Hyams JS. The safety of treatment options for pediatric Crohn’s disease. Expert Opin Drug Saf. 2016; 15:138390.
Dubinsky MC, Rosh J, Faubion WA Jr, Kierkus J, Ruemmele F, Hyams JS, Eichner S, Li Y, Huang B, Mostafa NM, Lazar A, Thakkar RB. Efficacy and safety of escalation of adalimumab therapy to weekly dosing in pediatric patients with Crohn’s disease. Inflamm Bowel Dis. 2016; 22:886-93.
Jensen T, Blanchette A, Vadasz S, Dave A, Canfarotta M, Sayej WN, Finck C. Biomimetic and synthetic esophageal tissue engineering. Biomaterials. 2015 Jul; 57:133-41.
Sayej WN, Ménoret A, Maharjan AS, Fernandez M, Wang Z, Balarezo F, Hyams JS, Sylvester FA, Vella AT. Characterizing the inflammatory response in esophageal mucosal biopsies in children with eosinophilic esophagitis. Clin Transl Immunol. 2016 Jul 1; 5(7).
Grossi V, Bezler N, Sayej W. Ulcer of the duodenum caused by a pancreatic neuroendocrine tumor in an adolescent. Clin Gastroenterol Hepatol. 2016 Sep 6. pii: S15423565(16)30623-1.
Sayej WN, Knight Iii PR, Guo WA, Mullan B, Ohtake PJ, Davidson BA, Khan A, Baker RD, Baker SS. Advanced glycation end products induce obesity and hepatosteatosis in CD-1 wild-type mice. Biomed Res Int. 2016; 2016:7867852. doi: 10.1155/2016/7867852. Epub 2016 Jan 31.
Davidovics ZH, Vance K, Etienne N, Hyams JS. Fecal transplantation successfully treats recurrent D-lactic acidosis in a child with short bowel syndrome. J Parenter Enteral Nutr. 2015.
Samela K, Mokha J, Emerick K, Davidovics ZH. Transition to a tube feeding formula with real food ingredients in pediatric patients with intestinal failure. Nutr Clin Pract. 2016 Aug 4.
Mokha JS, Davidovics ZH. Improved delivery of fat from human breast milk via continuous tube feeding. JPEN J Parenter Enteral Nutr. 2016 Feb 5. pii: 0148607115626902.
Mokha JS, Davidovics ZH, Samela K, Emerick K. Effects of ethanol lock therapy on central line infections and mechanical problems in children with intestinal failure. JPEN J Parenter Enteral Nutr. 2016 Jan 29. pii: 0148607115625057.
Semancik E, Sayej WN. Oral immunotherapy for peanut allergy induces eosinophilic esophagitis: three pediatric case reports. Pediatr Allergy Immunol. 2016 Aug; 27(5):539-41.
Davidovics ZH, Carter BA, Luna RA, Hollister EB, Shulman RJ, Versalovic J. The fecal microbiome in pediatric patients with short bowel syndrome. JPEN J Parenter Enteral Nutr. 2015 Jun 9. pii: 0148607115591216.
Chapters
Davidovics Z. Neoplasms of the gastrointestinal tract. In: Wyllie R, Hyams JS, Kay M, editors. Pediatric gastrointestinal and liver disease. Elsevier Health Sciences; 2015.
Loomes K, Emerick K. Pediatric cholestatic liver disease. In: Wyllie R, Hyams JS, Kay M, editors. Pediatric gastrointestinal and liver disease. Elsevier Health Sciences; 2015.
Samela K, Vance K, Bush L, Chatfield B. Nutritional assessment. In: Pediatric gastrointestinal and liver disease. Wyllie R, Hyams JS, Kay M, editors. Elsevier Health Sciences; 2015.
Hyams J. Will Justin be different? In: Rotbart H, editor. Miracles we have seen. HCI Books; 2016.
Hyams J. Feeling his pain. In: Rotbart H, editor. Miracles we have seen. HCI Books; 2016.
Grossi V, Sayej WN. Colitis. In: The NASPGHAN fellows concise review of pediatric gastroenterology, hepatology and nutrition. 2nd ed. 2016.
Grossi V, Sayej WN. Radiation oncology. In: The NASPGHAN fellows concise review of pediatric gastroenterology, hepatology and nutrition. 2nd ed. 2016.
Mokha J, Sayej WN. Colic and gas. In: The NASPGHAN fellows concise review of pediatric gastroenterology, hepatology and nutrition. 2nd ed. 2016.
Mokha J, Sayej WN. Appendicitis. In: The NASPGHAN fellows concise review of pediatric gastroenterology, hepatology and nutrition. 2nd ed. 2016.
Pressley-Wallace A, Sayej WN. Chronic constipation and encopresis. In: The NASPGHAN fellows concise review of pediatric gastroenterology, hepatology and nutrition. 2nd ed. 2016.
Jenson T, Sayej WN, Finck C. Esophageal tissue engineering. In: Frontiers in stem cell and regenerative medicine. Vol 3. United Arab Emirates: Bentham Science; ebook; 2015 Nov 4. 11-04-2015-Ebk series/FSCRMR/EOI-59.
Staff
Jeffrey Hyams, MD
Division Head
Zev Davidovics, MD
Karan Emerick, MD
Melissa Fernandes, MD
Franziska Mohr, MD
Jasmeet Mokha, MD
Wael Sayej, MD
Peter Townsend, MD
Bella Zeisler, MD
Heidi Sweeney, APRN
Kristin Philipp, APRN
Samantha Lee, APRN
Books
Wyllie R, Hyams J, Kay M, editors. Pediatric gastrointestinal and liver disease. 5th ed. Philadelphia: Elsevier; 2015.
Fellows
Victoria Grossi, DO
Angela Pressley-Wallace, MD
Temara Hajjat, MD
The Division of Emergency Medicine is committed to a continuous quality improvement process, and we have improved our efficiency, the safety of our health care delivery system, and ultimately our patient satisfaction.
In 2015, the Emergency Department of Connecticut Children’s Medical Center treated 57,636 patients, and in 2016, we treated 61,360, our highest annual volume ever. The Division of Emergency Medicine is composed of 17 Pediatric Emergency Medicine board-certified/eligible, fellowship-trained attendings, four per diem Emergency Medicine-trained attendings, one Pediatrician, nine per diem Pediatricians, 10 Advanced Practitioners, and four per diem Advanced Practitioners.
Two of our faculty received academic promotion. Dr. Sharon Smith was promoted to Professor of Pediatrics, and Dr. Steven Rogers was promoted to Associate Professor of Pediatrics. Our faculty was joined in 2015 by Dr. Henry Chicaiza. He completed a fellowship in Pediatric Emergency Medicine here at Connecticut Children’s and then worked for a year as an attending physician at Stony Brook Children’s Hospital in Stony Brook, NY, before returning to join our division. He has an interest in Point of Care Ultrasound. In 2016, Mariann Nocera, MD, joined our faculty after completing a fellowship in Emergency Medicine at Hasbro Children’s Hospital in Providence, RI. Her interest is use of simulation in adult education. Three advanced practitioners also started in 2016: Lauren Appel, APRN, Nicole Chaves, PA-C, and Katelyn Claudomir, APRN.
Members of the Division of Emergency Medicine continue to be highly involved in leadership and committees at Connecticut Children’s with participation by the division in over 35 hospital committees. Regionally, Dr. Jim Parker is the vice chairperson for EMS-C for the State of Connecticut and the North Central Region Medical Advisory Council. Dr. Michael Soltis serves on the state’s Child Fatality panel and the Abusive Head Trauma working group. Dr. Steven Rogers continues to serve on the executive board of the Eastern Society for Pediatric Research and as the program chairperson for the Injury Free Coalition
for Kids. He also continues to be on the editorial board and serves as a reviewer for multiple journals.
Education and research remain a significant part of our mission. The faculty taught and mentored pediatric residents, Emergency Medicine residents, family practice residents, medical students, dental students and advanced practitioner students. Dr. Kristin Welch is the division’s faculty education coordinator and is leading the evolution of our resident orientation and evaluation process. This year, Dr. Welch is sharing the role of faculty education coordinator with Dr. Lana Friedman.
The Pediatric Emergency Medicine Fellowship is now in its 17th year. Dr. V. Matt Laurich assumed the role of program director in July 2015 after having served as associate program director under Dr. John Brancato. Dr. Brancato had served as program director for 14 years, building the fellowship from its infancy to the successful program it is today. The fellowship expanded to its new full complement of six fellows in July of 2016. Dr. Brancato continues in his role as associate medical director. An undergraduate research assistant program that was developed by Dr. Sharon Smith and taught by our faculty supports the research productivity of our division. Dr. Smith also serves as the division’s director of research and is the director of Pediatric Advanced Life Support (PALS) for the institution. Research projects covering topics such as violence prevention, simulation, ultrasound-guided IV placement, lethal means restriction, nutrition and asthma are ongoing. Dr. Smith also serves as chair of the membership committee for the Eastern Society for Pediatric Research. Dr. Carla Pruden has led the division and the institution’s efforts in simulation. In 2016, she assumed the role of medical director of Simulation. She hosts a bimonthly simulation session for the Emergency Medicine attendings, monthly session for the trauma team, and ad hoc sessions for the hospital using new high fidelity mannequins.
The main focus of our mission is to provide efficient high quality care to our patients. This has led to an examination of the throughput process and a continual quality im-
provement process. Our efforts to improve the treatment of sepsis have resulted in increased recognition of the clinical state and compliance with the pathway and better timeliness of treatment. It has become a model for how the institution is treating sepsis. By instituting a direct bedding process, we have seen substantial improvements in our time metrics, most notably at the front end of the process such as arrival to provider times. As a result, we have had stellar performance in our Left Without Being Seen (LWBS) rates.
The Institute of Trauma, after a successful re-verification by the American College of Surgeons for designation as a Level 1 Pediatric Trauma Center in 2014, is making the commitment to treat all Level 1 pediatric trauma patients at the Connecticut Children’s geographic site, decreasing the number of pediatric patients that are seen at Hartford Hospital. Dr. Parker is medical director of the Transport program, which is almost finished filling transport nursing positions, which will allow the transport program to transition to a nurse-led team. The process for building another medical transport vehicle is ongoing.
Among the awards garnered by our staff in 2015, Henry Chicaiza was named a faculty finalist for the Eastern Society for Pediatric Research Young Investigator Award. In 2016, Steven Rogers was awarded the 2016 Medical Staff Award: Outstanding Physician for Quality and Safety.
Publications
Nevin J, Wilkens P, Smith S, Sturm J, Chicaiza H. Physical exam and historical patient factors associated with diagnosis of pneumonia. J Pediatr Child Care. 2015 Jan.
Chicaiza H, Hellstrand K, Lerer T, Smith S, Sylvester F. [reply] Potassium hydroxide: an alternative reagent to perform the modified apt test. J Pediatr. 2015 Jan 9.
Hellstrand K, Hoppa E. Low back and leg pain with refusal to ambulate in a 6-year-old male. Clin Pediatr. 2015 Nov 4. Epub ahead of print.
Miano D, Silvis R, Culbertson MC, Campbell B, Smith SR. Abdominal CTs do not improve outcomes for children with suspected acute appendicitis. West J Emerg Med. 2015 Dec; 16(7): 974-82.
Masso PD Jr, Griffin LC, Stevens M, Mangini L, Smith SR CARES: improving the flow of psychiatric patients in the pediatric emergency department. PEC. 2015; 31(3):173-7. PMID: 25706924.
Kasmire KE, Rogers SC, Sturm JJ. Trampoline park and home trampoline injuries. Pediatrics. 2016 Sep; 138(3). doi: 10.1542/peds.2016-1236.
Lapidus G, Borrup K, DiVietro S, Campbell B, Beebe R, Grasso D, Rogers S, Joseph D, Banco L. Practical applications of injury surveillance: a brief 25-year history of the Connecticut Injury Prevention Center. Inj Prev. 2016; 22:i12-i16. doi:10.1136/injuryprev-2015-041818.
Campbell B, Borrup K, Derbyshire M, Rogers S, Lapidus G. Efficacy of driving simulator training for novice teen drivers. Conn Med. 2016; 80(5):291-6.
Corrigan C, DiVietro S, Campbell B, Rogers S, Beebe R, Clough M, Lapidus G. A retrospective analysis of fatal pediatric injury in America, the Northeast, and Connecticut. Conn Med. 2016; 80(9):517-24.
DiVietro S, Beebe R, Clough M, Klein E, Lapidus G, Joseph D. Screening at hair salons: the feasility of using community resources to screen for intimate partner violence. J Trauma. 2016; 80(2):223-8.
Morrisey D, Riese A, Violano P, Lapidus G, Baird J, Mello M. Child passenger safety training for pediatric interns: does it work? RI Med J. 2016 Mar; 29-32..
Chapters
Hoppa E, Perry HE. Stridor. In: Bachur RB, Shaw K, Chamberlain J, Lavelle J, Nagler J, Shook J, editors. Fleisher and Ludwig’s textbook of pediatric emergency medicine. 7th ed. Philadelphia: Lippincott, Williams and Wilkins; 2015. p. 48690.
Staff
Attendings:
John Peng, MD, FAAP, FACEP
Division Head and Medical Director
John Brancato, MD
Associate Director
Henry Chicaiza, MD
Lana Friedman, MD
Andrew Heggland, MD
Eric Hoppa, MD
V. Matt Laurich, MD
Mariann Nocera, MD
James Parker, MD
Carla Pruden, MD
Steven Rogers, MD
Adam Silverman, MD
Sharon Smith, MD
Michael Soltis, MD
Jesse Sturm, MD
Kristin Welch, MD
James Wiley, MD
Per Diem Attendings: Zoe Casey, MD
Sandra Johnson, MD
Seth Lotterman, MD
Avital Porat, MD
Pediatrician:
Christine Cornachio, MD
Per Diem Pediatricians: Brenda Balch, MD
Meredith Barrows, MD
Karl Hellstrand, DO
Kathryn Kasmire, MD
Molly Naples, MD
Richard Pierce, MD
Elizabeth Smith, MD
Charles Thompson, MD
Nancy Trout, MD
APRNs / PAs: Lauren Appel, APRN
Chelsea Byrd, PA-C
Nicole Chaves, PA-C
Lauren Christofori, PA-C
Katelyn Claudomir, APRN
Carol Erickson, Lead APRN
Ann Gorjanc, PA-C
Garry Lapidus, PA-C
Sarah Orlando, PA-C
Christopher Scheinberg, APRN
Lisa Tryon, PA-C
Per Diem APRNs / PAs: Mallory Breitmaier, APRN
Keri Curtis, PA-C
Kate Pesce, APRN
Jill Peterson, APRN
Margaret Seitz, PA-C
Pediatric Emergency Medicine Fellows:
Tasha Desai, PGY4
Karl Hellstrand, PGY6
Noah Jablow, PGY4
Kathryn Kasmire, PGY6
Laurie Malia, PGY5
Hannah Sneller, PGY5

Connecticut Children’s Medical Center has a longstanding commitment to patient safety, highest quality clinical care, and continual improvement. To formalize that commitment and to foster its continued development, in 2016 the medical center created the Division of Excellence in Patient Safety & Clinical Quality.
The division’s goal is to drive patient safety to the standard of zero-harm, to provide the highest quality care, to teach methods of improvement, and to use research to inform our programmatic efforts and innovations. We integrate patient safety and quality across our institution using a rigorous high reliability framework. Six key components guide our efforts:
We continually strive to foster a culture of safety
We have a culture of continual improvement
We ensure the engagement of all team members
We are data-driven and transparent
We focus on high reliability
We have a structure and process for prioritization
This framework supports our strategy to achieve the highest quality, evidence-based, safest, zero-harm, family centered and most efficient care possible.
Our faculty members are national leaders and serve on multiple peer-review groups and study sections as well as on several national steering committees and boards dedicated to patient safety and clinical quality. Dr. Andrea Benin has been integrally involved in the development of national pediatric quality measures, and in 2016 completed the nationally recognized Baldrige Executive Fellows Program, focused on her quality work. We have recently completed the research for several grant-sponsored projects, and Dr. Heather Tory has received a funding award for her work in developing quality measures in Pediatric Rheumatology. Also in 2016, three of our faculty members, Drs. Natalie Bezler, Brendan Campbell and Ilana Waynik, began national course work in leading quality improvement.
We have a robust program in infection prevention and point of care testing under the guidance of Dr. Thomas Murray, as well as rigorous antimicrobial stewardship activities, including
academic research in stewardship by Dr. Jennifer Girotto. We participate nationally in Solutions for Patient Safety bundles, and Dr. Campbell is leading work with the National Surgical Quality Improvement Program; our active participation in these types of benchmarking databases has allowed the organization to evolve the transparency of reporting, as well as to understand our performance in the context of like institutions and promote the highest standards. The division’s support of continual improvement efforts throughout the organization, with the appointment of Dr. Alex Golden as the associate medical director of Continual Improvement last year, has also had a significant impact on our ability to provide the highest quality and safest clinical care. Additionally, many of our faculty members are championing quality and safety efforts within the service line structure of our organization as Quality and Safety Officers: Drs. Bezler, Campbell, Golden, Jonathan Martin, Sherene Mason, and Franziska Mohr, and Petronella Stoltz, APRN.
The division also is committed to promoting education in quality and patient safety principles and methodology. In 2016, we sponsored our 5th annual Illuminations Patient Safety and Quality Conference, which featured abstract presentations by Connecticut Children’s faculty and staff and keynote speakers. Dr. Carla Pruden has taken on the role of medical director of Simulation, with the goal of developing a robust simulation program to promote high quality and safe care at Connecticut Children’s. We mentor fellows in medical informatics on key informatics research projects, and in 2016 a neonatology fellow completed the academic requirements for fellowship with a focus on quality improvement research under the guidance of Dr. Sink – the first fellow in that track at Connecticut Children’s.
In the next year, we look forward to expanding our use of scientific methodology to improve our innovations in driving zero-harm, patient safety and quality.
We have had several publications in the past few years and have several more in preparation. We also have had multiple poster presentations at national meetings in the past year.
Publications
Benin AL, Fodeh SJ, Lee K, Koss M, Miller P, Brandt C. Electronic approaches to making sense of the text in the adverse event reporting system. J Healthc Risk Manag. 2016; 36:10-20.
Fodeh SJ, Brandt C, Miller P, Koss M, Benin AL. Feature selection based LapSVM to classify medical event reports and enhance patient safety. AMIA Annu Symp Proc. 2015: 39.
Benin A, Fodeh SJ, Koss M, Lee K, Miller P, Brandt C. Using the adverse event reporting system: can analysis be streamlined by text processing? AMIA Annu Symp Proc. 2015:1414.
Suter L, Barber CE, Herrin J, Leong A, Losina E, Miller A, Newman E, Robbins M, Tory H, Yazdany J. American College of Rheumatology White Paper on Performance Outcome Measures in Rheumatology. Arthritis Care Res. 2016; 68(10):1390-401.
Tory HO, Solomon DH, Desai SP. Analysis of quality improvement efforts in preventing glucocorticoid induced osteoporosis. Semin Arthritis Rheum. 2015; 44(5):483-8.
Campbell BT, Austin DM, Kahn O, McCann MC, Lerer TJ, Lee K, Thaker S, Herbst KW, Rader CR. Current trends in the surgical treatment of pediatric ovarian torsion: we can do better. J Pediatr Surg. 2015; 50:1374-7.
Hagadorn JI, Brownell EA, Herbst KW, Trzaski JM, Neff S and Campbell BT. Trends in treatment and in-hospital mortality for neonates with congenital diaphragmatic hernia. J Perinatol. 2015:1-7.
Courter JD, Nichols K, Kazazian C, Girotto JE. Optimal levofloxacin dosing for pediatric community-acquired pneumonia. J Pediatric Infect Dis Soc. 2016 Feb 21. Pii:pow006 [Epub ahead of print].
Welsh C, Miah R, Girotto J. Survey evaluating the practice of children’s hospitals having pharmacist collaborative drug therapy management protocols. J Pediatr Pharmacol Ther. 2016 Nov-Dec; 21(6):494-501.
Dassner A, Nicolau D, Girotto J. Management of pneumonia in the pediatric critical care unit: an area for antimicrobial stewardship. Curr Pediatr Rev. 2016 Dec 4 [Epub ahead of print].
Magsarili H, Girotto JE, Bennett N, Nicolau DP. Making a case for pediatric antimicrobial stewardship programs. Pharmacotherapy. 2015; 35(11):1026-36.
Liang C, Girotto J. Influenza immunization update: 20162017. Pharm J New England. Summer 2016:24-26.
Goodlet KJ, Girotto JE. Optimal vaccine administration for patients undergoing chemotherapy. Conn Med. 2016 May; 80(5):305-11.
Dassner A, Girotto JE. Important Updates for Influenza Vaccination: 2015-2016. Pharm J New England. 2015; 12(4):19-20.
Staff
Andrea Benin, MD
Division Director
Heather Tory, MD, MPH
Alex Golden, MD, MMM
Brendan Campbell, MD, MPH
Natalie Bezler, MD
Franziska Mohr, MD, MRCPCH
Sherene Mason, MD, MBA
Jonathan Martin, MD
Carla Pruden, MD, MPH
Thomas Murray, MD, PhD
David Sink, MD
Ilana Waynik, MD
Jennifer Girotto, PharmD
Petronella Stoltz, APRN
The introduction of a number of subspecialized multidisciplinary clinics highlighted two years of innovation and expansion of our clinical offerings. Our Diabetes Education Program was reaccredited by the American Association of Diabetes Educators, one of only three programs certified in Connecticut in 2015, and the only one dedicated to the care of children and adolescents with diabetes. This attests to the high quality and standards that our staff of diabetes educators, including registered dietitians, nurses, social workers, nurse practitioners and physicians under the able leadership of Dr. Cem Demirci, provide to over 1,200 children with Type 1 and Type 2 diabetes and their families. With the addition of Carey Driscoll, PNP, we have a full service program to care for the endocrine needs of our community.
Emily Germain-Lee, MD, was recruited to become Chief of the Division of Pediatric Endocrinology at Connecticut Children’s Medical Center and a tenured Professor of Pediatrics at the University of Connecticut School of Medicine effective October 28, 2016. Prior to her move she was a tenured Professor of Pediatrics at the Johns Hopkins University School of Medicine and Professor/Research Scientist at the Kennedy Krieger Institute in Baltimore. Dr. Germain-Lee is internationally recognized for her clinical care and research in bone disorders, and she has brought her clinical and translational research program in rare bone disorders to Connecticut Children’s and UConn Health. For much of her career, she has focused her clinical and laboratory research efforts on Albright hereditary osteodystrophy (AHO) and has moved her Albright Center to Connecticut Children’s with her laboratory at UConn Health. Through the Albright Center, Dr. GermainLee follows the largest population of AHO patients in the world, and most of these patients will travel to Connecticut to continue to be followed by her. Moreover, upon joining Connecticut Children’s/UConn Health, she has started the Center for Rare Bone Disorders as well as the Osteogenesis Imperfecta (OI) Center, with OI being another major focus of Dr. Germain-Lee’s clinical and laboratory research efforts. Dr. Germain-Lee will continue her affiliation with Johns Hopkins/ Kennedy Krieger Institute as Adjunct Professor in order to maintain active collaborations. As vice president and member of the board of the Human Growth Foundation for over a de-
cade, she will continue to help children with growth disorders worldwide through advocacy, education, and research. She is a member of the Society for Pediatric Research and was invited to serve a second term as Editorial Board Member of the Journal of Clinical Endocrinology and Metabolism, one of the top research journals in Endocrinology.
The division has continued to grow and expand its services in the new Connecticut Children’s Medical/Surgical Center at 505 Farmington Avenue in Farmington, CT. Our patients and families continue to compliment us on the space, which offers easy access and parking as well as the welcoming environment created by a larger waiting area. While the primary home of the division is now in Farmington, the division continues to care for hospitalized patients on the Hartford campus of Connecticut Children’s Medical Center and at our office at 85 Seymour Street for children who are enrolled in our weight management program and who need bisphosphonate infusions and DXA scans in our multiple bone disease centers. The Hartford clinic is also of benefit to families with limited ability to travel to Farmington.
In 2016, we have continued with transition in leadership of the division. Dr. Susan Ratzan, a founding member of the division and former division head, and most recently interim division head, retired as of December 2015. She continues to see patients part-time. We appreciate all her years of service and commitment to Endocrinology. Clinical Director Dr. Paola Palma Sisto assumed the role of interim division chief as well. She provided very strong and dedicated leadership in the division, including the introduction of new models of patient care, such as a multidisciplinary diabetes clinic that includes all disciplines involved in the care of diabetes patients for a comprehensive approach to the patient, offering a “one-stop shopping” opportunity for families. Under her leadership, new and established clinics have been developed and expanded. We greatly appreciate Dr. Palma Sisto’s untiring work as interim division chief.
The Coordinated Care Clinic (CCC), directed by Dr. Cem Demirci, cares for our most challenging and complex diabetes patients in a multidisciplinary setting. It has expanded to the Farmington location. A number of new subspecialized clinics
are being led by members of our diverse faculty. They include a Metabolic Bone Clinic run by Dr. Nancy Dunbar, a multispecialty Neuro-oncology Clinic supported by Dr. Rebecca Riba-Wolman, the development of a formal Gender Identity clinic run by Dr. Priya Phulwani, and the previously mentioned centers established by Dr. Germain-Lee.
Dr. Nancy Dunbar continues to be involved in matters of global health. Starting in 2015, she increased her involvement with the ultra-rare metabolic bone disease, hypophosphatasia. Her work as a national and global advisor for Hypophosphatasia and Alexion pharmaceuticals allowed her to give six different presentations about hypophosphatasia around New England and the Northeast in 2015 to physician groups. She is a valued colleague in the Center for Rare Bone Disorders and OI Center that Dr. Germain-Lee has recently established. Dr. Dunbar’s achievements in 2015 also included continued work with Hôpital Sacré Coeur in northern Haiti and its pediatric diabetes program. In December 2015, she co-organized a two-week visit for the Haitian pediatrician who directs the Haitian diabetes program. He spent seven days at Connecticut Children’s in the hospital and at the endocrine outpatient office to learn how we evaluate and manage our children with Type 1 Diabetes. She organized a local fundraiser for the HSC Pediatric Diabetes Program that raised over $12,000 – 100% of funds going to the care of the 50 children with Type 1 in northern Haiti. The funds provided for medical and surgical care, insulin, and other diabetes supplies.
Dr. Priya Phulwani is the medical director of the Gender Identity Program and was the invited pediatric Grand Rounds speaker on “Gender Dysphoria” at Connecticut Children’s, Day Kimball, Waterbury and Danbury hospitals. She participates with members of the Urology and Psychology divisions in the multidisciplinary clinic for Disorders of Sexual Development. She is also the endocrinologist in the multidisciplinary Bariatric clinic and presented on the “Pharmacology of Obesity” at the 2015 adolescent Bariatric Symposium, and for the UConn MPH program on “Generation XXL: Pediatric Obesity, Type 2 Diabetes, and Bariatric Surgery.”
Dr. Karen Rubin continues in her role as Associate Clinical Chair of the Department of Pediatrics and head of Clinical
Care Innovation at Connecticut Children’s Medical Center. She has been approved for a grant from the Innovation Seed of Connecticut Children’s Office for Community Child Health to study “Referral Guidelines at the Interface Between Primary and Subspecialty Care: A Novel Approach to Development and Dissemination.” She presented at the PCPCC (Patient-Centered Primary Care Collaborative) Annual Fall Conference in Philadelphia, PA, on “Investing in Primary Care: Patients, Professionals & Payment,” and “Co-Managing and Integrating Care Across the Neighborhood.” She also attended the International Turner Syndrome Clinical Care Guidelines Consensus Meeting, Transition Between Pediatric and Adult Care, in Cincinnati, OH, in September of 2016, as speaker and section co-chair. At the Pediatric Endocrine Society Annual Meeting in Baltimore, MD, on May 2, 2016, she presented the PES Survey Findings of Care Delivery and Payment Models for United States Pediatric Diabetes Care Teams, and the PES SCAMPs Quality Network Update.
Our weight management program continues to innovate in the care of patients challenged with weight loss. Dr. Melissa Santos, the program director for the Obesity Center for Treatment, Research and Education at Connecticut Children’s Medical Center, continues to add new advances in care and to encourage engagement of patients in the program, as well as the multispecialty Pediatric Bariatric Program. The techniques include use of technology to engage patients and to inspire change. Dr. Santos presented at local meetings including organizing the Bariatric Symposium for local general and specialty practitioners involved in both pediatric and adult bariatric care. Her national presentations included abstracts or workshops at both the Symposium on Pediatric Pain, and the Society of Pediatric Psychology Annual Conference in 2015. Dr. Santos, in collaboration with other authors, presented a poster titled “The Impact of Support Group on Adolescents Undergoing Bariatric Surgery,” and a workshop titled “Integrated Treatment Approaches for the Young Child With Obesity” at the American Psychological Association Annual Convention in August 2016. She also presented in collaboration a workshop titled “Advancing the Care of the Young Child With Severe Obesity” at the annual Pediatric Endocrine Society meeting in May 2016 in Baltimore, MD.
Dr. Christine Trapp was appointed the Medical Director of the Obesity Center, with the task of overseeing the medical assessment and management of the program’s patients and assessing the impact of the weight management program on overall health. Dr. Trapp completed her Masters in Clinical and Translational Research at the University of Connecticut Health Center under the mentorship of Dr. Michele Cloutier and will use those skills to work on obesity prevention and her role as the Obesity Center Medical Director.
Our fellowship training program has successfully recruited well-qualified trainees each year, and all graduates have moved on to clinical academic positions. Dr. Palma Sisto assumed the directorship of the Pediatric Endocrine Fellowship along with Dr. Rebecca Riba-Wolman. Dr. Palma Sisto is also the Director of Fellowships for the Department of Pediatrics, overseeing six medical and three surgical fellowships to assure that all fellowships at Connecticut Children’s meet ACGME requirements.
Division members provide leadership in a number of clinical and research collaborations. The clinical collaborations include the following: Drs. Rubin and Palma Sisto co-direct the Thyroid Center, a multidisciplinary, coordinated program with Surgery, Radiology, Pathology, and Nuclear Medicine for the evaluation and treatment of children with thyroid nodules and thyroid cancer. Dr. Riba-Wolman directs the Endocrine Late Effects Clinical Program in the monthly STAR program in the Oncology division for long-term survivors of childhood cancer. Dr. Priya Phulwani is the Endocrine Director of the multidisciplinary (Genetics, Urology, Psychiatry) program for youth with disorders of sexual development.
The ongoing research in the Division of Endocrinology includes the following: Dr. Demirci has collaborated on a grant with researchers at Jackson Laboratories at the UConn Health campus to study “Immune correlates of non-coding genomic variants associated with Type I diabetes.” Dr. Santos continues to collaborate with Jackson Laboratories on a proposed study of the epigenetics of obesity. As part of Dr. Germain-Lee’s move to Connecticut Children’s/UConn Health, she has transferred several research grants, including an NIH R21 grant focused on Albright hereditary osteodys-
trophy for which she is principal investigator. She already has submitted an R01 grant application as PI to the FDA in October 2016 (also focused on AHO), as well as a group grant in December 2016 as PI to the Connecticut Regenerative Medicine Research Fund. This grant is focused on rare bone disorders, and Dr. Nancy Dunbar will be a co-investigator on this endeavor. This grant would join forces between Connecticut Children’s Medical Center, the UConn School of Medicine, the UConn School of Dental Medicine, and the UConn Storrs campus. Additionally, in December 2016, she submitted an NIH U01 grant application as co-investigator focused on signaling pathways involved in rare bone disorders, and in February, 2017, she will be submitting an NIH R01 grant application as co-investigator examining the metabolic and bone effects of specific circulating proteins in the context of aging; this R01 will be a collaborative effort between Jackson Laboratories and the UConn School of Medicine.
The division transitioned successfully into Care Navigator (EHR) for our ambulatory practice in the fall of 2015. The ability to communicate between areas and among the practice has significantly improved patient care and efficiency of delivering the care.
Publications
Golden D, Kolmakova A, Sura S, Vella AT, Manichaikul A, Wang X-Q, Bielinski SJ, Taylor KD, Ida Chen Y-D, Rich SS, Rodriguez A. Lymphocyte activation gene 3 and coronary artery disease. JCI Insight. 2016; 1(17):e88628.
Trapp CM, Burke G, Gorin AA, Wiley JF, Hernandez D, Crowell RE, Grant A, Beaulieu A, Cloutier MM. The relationship between dietary patterns, body mass index percentile, and household food security in young urban children. Child Obes. 2015 Apr; 11(2):148-55. doi: 10.1089/chi.2014.0105.
Epub 2015 Feb 26.
Oktay K, Bedoschi G, Berkowitz K, Bronson R, Kashani B, McGovern P, Pal L, Quinn G, Rubin K. Fertility preservation in women with Turner Syndrome: a comprehensive review and practical guidelines. J Pediatr Adolesc Gynecol. 2016 Oct; 29(5):409-16.
Cornell E, Chandhok L, Rubin KR. Implementation of referral guidelines at the interface between pediatric primary and subspecialty care. Healthc: J Deliv Sci Innov. 2015 Jun; 3(2):74-9.
Rosenfield RL, Dimeglio L, Mauras N, Ross N, Shaw N, Greeley D, Haymond M, Rubin KR, et al. [commentary] Launch of a quality improvement network for evidence-based management of uncommon pediatric endocrine disorders: Turner Syndrome as a prototype. J Clin Endocrinol Metabl. 2015 Apr; 100(4):1234-6.
Santos M, Cadieux A, Gray J, Ward W. Pediatric obesity in early childhood: a physician screening tool. Clin Pediatr. 2016; 55:356-362.
Cadieux A, Getzoff E, Baughcum A, Shaffer L, Santos M, Gaffka B, Gray J, Burton E, Ward W. Recommendations for psychologists in Stage III Pediatric Obesity Programs. Child Health Care. 2016; 45:126-45.
Santos M, Baughcum A, Burton E, Cadieux A, Curran J, Gaffka B, Gray J, Shaffer L, Testa E, Ward W. Fellowship training in pediatric obesity: key components. Prof Psychol Res Pr. 2015 Dec; 46:400-8.
Astur RS, Palmisano A, Hudd EC, Carew AW, Deaton BE, Kuhney F, Niezrecki R, Santos M. Pavlovian conditioning to food reward as a function of eating disorder risk. Behav Brain Res. 2015; 291:277-82.
Palma Sisto PA, Gafni RI, Alter CA, Bauer AJ, DeBoer M, Boyce AM, Huang SA, LaFranchi SH, Lekarev O, Miller BS, Silverman L, Stratakis CA, Thornton PS, Weinzimer SA. Pediatric ESAP 2015-2016: Pediatric Endocrine Self-Assessment Program. Washington, DC: Endocrine Society; 2015.
Chapters
Santos M, Pont S, Estrada E. Childhood obesity related co-morbidities: identification and treatment. In: Hassink S, Hampl S, editors. Clinical management of childhood obesity. McGraw-Hill: 2015.
Staff
Emily Germain-Lee, MD Division Head
Paola Palma Sisto, MD Clinical Director
Cem Demirci, MD
Nancy Dunbar, MD
Priya Phulwani, MD
Susan Ratzan, MD
Rebecca Riba-Wolman, MD
Karen Rubin, MD
Christine Trapp, MD
Sunitha Sura, MD
Melissa Santos, PhD
Karen Bucci, PNP
Carey Driscoll, PNP
Nancy Paulhus-Orkin, PNP
The mission of the Pediatric General and Thoracic Surgery Division is to provide the highest quality family centered surgical care. A new initiative implemented in our division is a continual improvement process. As part of this initiative, we are reviewing our division specific clinic wait times and offering same-day visits in an effort to improve patient access and experience.
The Division of Pediatric General and Thoracic Surgery performs a full range of clinical services for patients from newborns to young adults. This includes prenatal consults, the treatment of congenital anomalies, enteral access, pediatric gynecology, non-reconstructive urology and surgical oncology. Connecticut Children’s is an American College of Surgeons-verified Level I Pediatric Trauma Center. We currently have satellite offices in Farmington and Danbury, and we are performing surgeries at the Ambulatory Surgery Center in Farmington and at Danbury Hospital. We also have added a new satellite in Glastonbury.
The mission of the division is to continue to provide the highest quality of care for children in Connecticut. This includes easy patient access for subspecialty consultation as well as enhancing care of children through innovative surgical techniques and instrumentation. We have added a new, innovative treatment option for patients with pectus excavatum: vacuum bell elevation. Dr. Meghna Misra has recruited our first two patients for this treatment.
Exciting Initiatives: Quality Improvement and Multidisciplinary Programs
Connecticut Children’s continues to be involved in the American College of Surgeons’ Pediatric National Surgical Quality Improvement Program (NSQIP), the first multi-specialty program designed to measure and improve the quality of children’s surgical care. Dr. Brendan Campbell is the Surgeon Champion for the NSQIP Program, and has been successful in implementing standardized pathways for solid organ injury, pyloric stenosis, and non-accidental trauma.
The Division of Pediatric General and Thoracic Surgery continues to drive several multi-disciplinary services aimed at facilitating and improving patient care and experience. Through the
Multidisciplinary Thyroid Group, children with thyroid diseases are able to be evaluated simultaneously by a surgeon as well as an endocrinologist. Dr. Christine Rader is the Surgical Director of the Extracorporeal Membrane Oxygenation Program, a multi-disciplinary program aimed at caring for some of our sickest patients requiring life support. Dr. Weiss continues to co-direct the multidisciplinary prenatal evaluation program with Hartford Hospital Obstetrical Maternal Fetal Medicine.
Education
A central mission for our division is to educate the future leaders in our community. In pursuit of this goal, the Division of Pediatric General and Thoracic Surgery continues its ACGME-accredited pediatric surgery fellowship. Our current fellow, Yue Yung Hu, came to us from Beth Israel Deaconess Medical Center in Boston and will graduate in 2017. Dr. James Healy, our next fellow, starts in August 2017. In addition, Dr. Christine Rader is the site director for the Quinnipiac medical student pediatric core curriculum. In 2016, we had 60 Quinnipiac medical students rotate through our service.
Publications
Manworren RC, McElligott CD, Deraska PV, Santanelli J, Blair S, Ruscher KA, Weiss R, Rader C, Finck C, Bourque M, Campbell B. Efficacy of analgesic treatments to manage children’s postoperative pain after laparoscopic appendectomy: retrospective medical record review. AORN J. 2016 Mar; 103(3):317.
Campbell BT, Borrup K, Derbyshire M, Rogers S, Lapidus G. Efficacy of driving simulator training for novice teen drivers. Conn Med. 2016; 80:227-32.
Lapidus G, Borrup K, DiVietro S, Campbell BT, Beebe R, Grasso D, Rogers S, Joseph D, Banco L. Practical applications of injury surveillance: a brief 25-year history of the Connecticut Injury Prevention Center. Inj Prev. 2016; 22:i12-i16.
Briere CE, McGrath JM, Jensen T, Matson A, Finck C. Breast milk stem cells: current science and implications for preterm infants. Adv Neonatal Care. 2016 Oct 4. PMID: 27749687.
Leopold S, Al-Qaraghouli M, Hussain N, Finck C. Magnetic resonance imaging diagnosis of volvulus through mesenteric defect in neonate. AJP Rep. 2016 Apr: 6(2):e239-42. PMID: 27551577.
Finck C, Rader C, Rudzic A, Gadepelli S. Extracorporeal life support. NaT American Pediatric Surgical Association (APSA); 2016.
Chapters
Sekaran AK, Campbell BT. Ovarian torsion. In: Rauch DA, Gershel GC. Caring for the hospitalized child: a handbook of inpatient pediatrics. 2nd ed. Chicago: AAP Section on Hospital Medicine; 2016.
Campbell BT. Meckel’s diverticulum and other omphalomesenteric duct remnants. In: Wyllie R, Hyams JS, editors. Pediatric gastrointestinal and liver disease. 5th ed. Philadelphia: Elsevier Saunders; 2016. p. 618-21.
Rader CM. Inguinal hernias and hydroceles. In: Wyllie R, Hyams JS, Kay M, editors. Pediatric gastrointestinal and liver disease. 5th ed. Philadelphia: Elsevier; 2016. p. 614-17.
Jensen T, Sayej W, Finck C. Esophageal tissue engineering. In: Frontiers in stem cell and regenerative medicine. Bentham Science; 2016.
Hu Y, Jensen T, Finck C. Surgical conditions of small intestine in infants and children. In: Yoe CJ, DeMeester SR, McFadden DW, Matthews JB, Fleshman JW, editors. Shackelford’s surgery of the alimentary tract. 8th ed. W.B. Saunders. 2016.
Staff
Christine Finck, MD, FACS
Surgeon-in-Chief; Vice Chair Department of Surgery; Chief, Division of Pediatric General and Thoracic Surgery
Michael Bourque, MD, FACS
Brendan Campbell, MD, MPH, FACS Director of Trauma; Pediatric Surgical Quality and Safety Officer
Meghna Misra, MD, FACS Director, Pectus Program
Christine Rader, MD, FACS Director, Extracorporeal Membrane Oxygenation Program
Richard Weiss, MD, FACS Medical Director, Pediatric Surgery Division
Nicole Boone, PA
Jessica Cooper, APRN
Samantha Pelow, APRN
Jeanette Rybski, APRN
Elisabeth Campbell, PA

The Division of General Pediatrics is committed to fostering the health and well-being of children, families and communities.
To realize this mission, we provide exceptional clinical care in partnership with families, teach evidence-based clinical pediatrics to the next generation of pediatric health care providers, and pursue original research and vigorous advocacy around issues important to children, families and the public. All of our activities place special emphasis on caring for children with special health-care needs, including disadvantaged children, children growing up in low-income families, and children with complex and chronic medical conditions.
The Division of General Pediatrics continues to provide the majority of pediatric primary care to Hartford’s children through the ambulatory and primary care clinics at Connecticut Children’s Medical Center and the Burgdorf/ Bank of America Health Center. In 2016, the division welcomed two new clinical care and teaching sites: Connecticut Children’s Primary Care at East Hartford and at West Hartford, staffed by four experienced pediatricians (Drs. Larry Scherzer, Aruna Ramanan, Latesha Thomas and Paula Lucuara Revelo). Members of the division provide ambulatory care to infants, children and adolescents, and inpatient care in the newborn nurseries at Hartford Hospital and University of Connecticut Health Center for children with lead poisoning and for children with suspected abuse or neglect. Our ambulatory services include health supervision, behavioral health care, chronic disease management, and urgent care using a Medical Home model. Adolescent Medicine subspecialty primary care and consultative services also are provided within the Division of General Pediatrics. The division houses innovative, community-wide clinical programs such as the Hartford Regional Lead Poisoning Treatment Center and the Reach Out and Read literacy program. Under the direction of Nina Livingston, MD, the Suspected Child Abuse and Neglect (SCAN) program has continued to expand, and became a separate academic division in 2015. General Pediatrics division faculty have gained regional and national prominence for clinical research, education, and
program development in the fields of injury epidemiology and prevention, child abuse and neglect, child behavior and development, culturally effective health care, emergent literacy promotion, and the development of Medical Home-based systems of care for children and youth with special health-care needs.
The largest clinical site of the division, the Primary Care Center at Connecticut Children’s, received National Committee for Quality Assurance (NCQA) Level 2 recognition in 2015 and Level 3 recognition in 2016. In achieving that recognition, the practice met rigorous standards set by the NCQA and was recognized for coordinating patient care, maintaining a high level of quality in service delivery, and ensuring that patients and families remain the center of all care. Improvement projects included enhancing access to primary care services, resulting in a 13 percent increase in patient volume, tracking adherence to palivizumab prophylaxis guidelines for preterm infants, and enhancing immunization, developmental, behavioral health and preschool vision screening rates. In 2016, through a partnership with Community Health Center, Inc., the Primary Care Center transitioned to become a Federally Qualified Health Center, CHC@CCMC. This partnership brings enhanced access to behavioral and dental services to the children of Hartford.
Faculty members in the division play a central role in education in the University of Connecticut system by providing the majority of pediatric primary care and newborn nursery educational experiences for medical students and pediatric residents in the region. Other rotating learners from UConn and other institutions include family practice residents, dental residents, psychiatry residents, child psychiatry fellows, and students from nurse practitioner, physician assistant and medical assistant programs. Division members serve on a wide variety of hospital, university and state committees. Membership on national committees includes the National Center for Culture Competence Advisory Group (Alberto Cohen-Abbo, MD) and the Society for Pediatric Dermatology Education Committee (Keri Wallace, MD). Research interests in the division include health literacy, cultural competence,
immunization, obesity, and screening in primary care. Division members collaborate in a wide variety of projects, including the Asthma Center’s Easy Breathing© program, co-management protocols with Connecticut Children’s pediatric subspecialists, patient recruitment for Dr. Tregony Simoneau’s study “Determining the Immunologic Fingerprint of Allergic Asthma: What Can the Long Noncoding RNA Tell Us?” and the NIH-funded project “The Asthma Neighborhood: Collaborative for Asthma Equity in Children” (Dr. Michelle Cloutier, PI).
Patricia Joyce, MD, continues her work with the REACH (Resident Education in Advocacy and Community Health) pathway and community/advocacy education for all residents, working in collaboration with Connecticut Children’s Office for Community Child Health, and a wide range of community agencies. Division Head Dr. Catherine Wiley continues her advocacy work in the area of emergent literacy and serves as Medical Director of Reach Out and Read Connecticut. She also serves as co-chair of the Department of Public Health State Health Improvement Project (Healthy Connecticut 2020) Immunization Committee. In partnership with the Village for Families and Children, Dr. Wiley and Dr. Karen Rubin (Office of Innovation) received a grant from United Health Foundation, “Two Generation Pediatrics: Integrating Intergenerational Family Services into Primary Care,” that will support interdisciplinary primary care-behavioral health at the East and West Hartford sites. Dr. Grael O’Brien continues to serve as site director for the CORNET (Continuity Clinic Research Network) of the Academic Pediatric Association and has also been very active on the Curriculum Reform Committee of the School of Medicine. Melissa Held, MD, and Patricia Joyce, MD, continue to modify aspects of the Ambulatory Pediatrics Clerkship to further improve upon this highly regarded experience.
Dr. Hilda Slivka received a continuing grant from the Connecticut Department of Public Health for the Hartford Regional Lead Poisoning Treatment Center in 2015, and upon her retirement in 2016, Drs. Patricia Garcia and Jennifer Haile assumed responsibilities for the Lead program and received a continuing grant in 2016. Drs. Keri
Wallace and Ed Zalneraitis received an AAP Walter Tunnessen Jr. Visiting Professor grant in 2016, sponsored by the AAP Section on Dermatology. Dr. Anton Alerte received a grant from Kaiser Permanente entitled “On Demand Teaching Modules for Student Continuity Practice (SCP) Faculty Preceptors,” and presented a workshop, “Effective Speaking 101: How to Avoid the Deadly Powerpoint” at COMSEP. He continues to serve as director of UConn’s Clinical Medicine course. In 2015 he also became president of the Connecticut Chapter of the American Academy of Pediatrics, and he continues to serve as chair of the Chapter’s Committee on Foster, Kinship and Adoption Care. Darlene Abbate, APRN, served as secretary and president-elect of the Connecticut Chapter of the National Association of Pediatric Nurse Practitioners in 2015 and assumed the role of president of that organization in 2016.
Publications
Brownell EA, Smith KC, Cornell EL, Esposito, PA, Wiley C, et al. Five-year secular trends and predictors of nonconsent to receive donor milk in the neonatal intensive care unit. Breastfeed Med. 2016 May. Epub ahead of print.
Hooft AM, Asnes AG, Livingston N, Deutsch S, Cahill L, Wood, JN, et al. The accuracy of ICD-10 codes: identifying physical abuse in 4 children’s hospitals. Acad Pediatr. 2015;15(4):444-50.
Karamessinas L, Wiley C. Hematemesis in an infant. Consultant for Pediatricians. 2015;14(2):91-2.
Wiley C. Immunizations: vaccinations in general. Pediatr Rev. 2015;36(6): 249-59.
Staff
Catherine Wiley, MD
Division Chief
Anton Alerte, MD
Norrell Atkinson, MD (SCAN)
Alberto Cohen-Abbo, MD
Patricia Garcia, MD
Jennifer Haile, MD
Patricia Joyce, MD
Jaye Ladinsky, MD
Nina Stuart Livingston, MD (SCAN)
Paula Lucuara Revelo, MD
Margaret McLaren, MD, MBBChir
Lisa Menillo, MD
Rebecca Moles, MD (SCAN)
Jody Navitsky, MD
Joseph Newell, MD
Grael O’Brien, MD
Aruna Ramanan, MD
Laurie Scheiner, MD
Larry Scherzer, MD
Molly Senn-McNally, MD
Hilda Slivka, MD
Jody Terranova, DO
Latesha Dawson Thomas, MD, CLC
Nancy Trout, MD
Keri Wallace, MD
Jessica Zimmerman, MD
Darlene Abbate, APRN
Meredith Brown, PA-C
Julia Christofori, APRN
Keith Ellis, APRN
Margaret Grammatico, PA-C
Karen Hull, APRN
Monica Joyce-Montaudy, APRN
Eileen Keane, APRN
Kathleen Laurie Kelliher, PA-C
Priscilla Malloy, APRN
Dianne Powers, APRN
Abby Theriaque, APRN
The members of the Division of Gynecology at Connecticut Children’s Medical Center continue to provide state-of-theart pediatric and adolescent gynecology consultative services in our four Greater Hartford offices, the Connecticut Children’s operating rooms, and the Connecticut Children’s emergency room and in-patient settings.
The clinical services provided include specialty care in all areas of medical and surgical gynecologic care for children and adolescents. These include reproductive health issues, vulvar and vaginal infections in children and adolescents, management of abnormal uterine bleeding and pelvic pain, adolescent endometriosis, congenital abnormalities of the reproductive tract, ovarian cysts and masses, and adolescent hormonal and contraceptive issues. The Division of Gynecology is directed by Dr. Frederick Rau, a fellowship-trained pediatric and adolescent gynecologist. Our team of gynecologists from the Gynecology and Obstetrics Division of Women’s Health Connecticut provides 24/7 coverage of the Connecticut Children’s Medical Center’s Emergency Room, operating room, and in-patient floors.
Office evaluations of pediatric and adolescent patients are done at the Gynecology and Obstetrics Division of Physicians of Women’s Health by Dr. Frederick Rau, Division Director, and Drs. Emily Rosenbush, Kerrie Henry, Catherine Graziani, Kelly Sturrock, Erin Pickett, Ellen Robinson, Marlaine Miller, Elizabeth Purcell and Ellen Lamb at locations in Hartford, Farmington, Glastonbury and Rocky Hill. Our extensive range of pediatric and adolescent-friendly gynecologists has improved the ability of community physicians to refer families for age-appropriate gynecologic care.
Our physicians are members of the North American Society for Pediatric and Adolescent Gynecology, an international organization dedicated to the gynecologic care of children and teenagers.
Our physicians collaborate at Connecticut Children’s Medical Center with the University of Connecticut School of Medicine Obstetrics/Gynecology and Pediatrics residents and University of Connecticut School of Medicine and Dartmouth Medical School medical students for in-patient, emergency room and operating room patient care.
Our physicians emphasize a supportive and minimally intrusive strategy while seeing children, adolescents and families.
For 2016-2017, the division will maintain and improve our patients’ access to superior specialty care in pediatric and adolescent gynecology to promote reproductive health and wellness for our community’s children and teenagers.
Staff
Frederick J. Rau, MD Director, Division of Gynecology
Catherine Graziani, DO
Kerrie Henry, MD
Erin Pickett, MD
Elizabeth Purcell, MD
Ellen Robinson, MD
Emily Rosenbush, MD
Kelley Sturrock, MD
Marlaine Miller, MD
Ellen Lamb, MD
We improve the lives of children with cancer and blood disorders by delivering high quality family centered academic health care. We continuously improve what we do through discovery and partnerships. We have three broad areas of focus: Quality & Safety, Service & Access, and Research & Teaching.
In the past two years, the Division of Hematology/Oncology has continued to excel in our ability to provide the highest quality of care with our focus on the patient and family experience; we are supported by a talented group of advanced practitioners and nurses as a key component of our service model. Over the past two years we have continued to broaden our programs and develop our areas of expertise at the same time. Highlighting our expertise within the division includes our programs in Palliative care, Survivorship, and our newly established program in Supportive Care. In addition, disease expertise has continued to grow in the areas of Neuroblastoma, Neuro-Oncology, Sarcoma and other solid tumors, Adolescent and Young Adult cancers, and the newly established Hematologic Malignancies program. Our comprehensive Advanced Cancer Care Program is continuing to expand with increased regional and national referrals to our Clinical Trials Program and Center for Advanced Cancer Care Program for novel therapeutics.
We have continued the alignment of our advanced practitioner staff to provide continuous, streamlined, and patientcentered care in both inpatient and outpatient facilities. To that end, we have established a Care Team Model of comprehensive care, supporting each patient with a team of nurses, advanced practitioners, a social worker, and a physician to provide longitudinal care. In the upcoming year, our most significant initiative is to establish our service line model of care, linking our inpatient, outpatient, and infusion services into one streamlined model and broadening our outreach to communities we have not previously served.
We are humbled by our high commendations from patients and families, a testament to our continued striving for a family centered approach to care delivery. We are supported by our two active family advisory boards for sickle cell disease and cancer care. Utilizing their input, we have implemented processes to improve the patient and family experience so that
children and families dealing with serious disease can do so with as much comfort and support as possible.
Our research efforts continue to expand. Our participation in the Children’s Oncology Group is one of the highest in the country. We are members of two national consortia: the National Pediatric Cancer Foundation’s Sunshine Project and the Neuroblastoma Medulloblastoma Translational Research Consortium, bringing novel Phase 1 and Phase 2 treatments to children with relapsed and refractory cancers. We have also continued to expand our partnership with Jackson Laboratories to develop a personalized approach to cancer therapeutics. Under the leadership of Dr. Michael Isakoff, the Adolescent and Young Adult Program, supported by the Nascembini Family and the Reid R. Sacco Adolescent and Young Adult Cancer Alliance, has collaborated and continued our consultation services for young adults at Hartford Hospital, St. Francis Medical Center, and UConn Health Center. Additionally, Dr. Isakoff has received support from Lea’s Foundation for Leukemia Research to support the opening of clinical trials focused on the area of leukemia and lymphoma. Dr. Andrea Orsey is leading the way in advancing the supportive care for patients undergoing cancer therapy. She has continued to work on a pilot yoga intervention project to improve pediatric cancer patients’ quality of life. Dr. Donna Boruchov’s expertise and state grant funding for our sickle cell patients has guided regional standards for exceptional care. Dr. Boruchov also has received grant funding for participation in nationwide genotyping and repository of our hemophilia patients. Dr. Natalie Bezler, MD, has been awarded a St. Baldrick’s infrastructure grant to help develop our Hematologic Malignancies Program, with funding to begin in 2017. In addition to contributing to residency training for which we consistently receive outstanding feedback for our program, we have submitted an application to the Accreditation Council for Graduate Medical Education (ACGME) for a clinical fellowship program in pediatric hematology-oncology. This represents another milestone in our mission to provide the best educational opportunities to the next generation of leaders in pediatric hematologyoncology.
Dr. Nehal Parikh left our division in May 2016 to pursue a career in industry. We thank him for his service in the past and
wish him the best in his future endeavors. At the end of 2016, Dr. Ching Lau, MD, PhD, joined the division as the new division head. He is an internationally renowned expert in cancer genomics and will be leading the academic growth and development of our division. Dr. Lau will be leading the joint program in precision oncology for children, in collaboration with Jackson Laboratory for Genomic Medicine in Farmington, CT, where his research laboratory will be located. In addition, Dr. Lau brings a wealth of clinical knowledge and will help drive our division forward as we continue to expand.
Publications
Grossi V, Bezler N, Sayej W. Ulcer of the duodenum caused by a pancreatic neuroendocrine tumor in an adolescent. Clin Gastroenterol Hepatol. 2016 Sep 6. pii: S15423565(16)30623-1. doi: 10.1016/j.cgh.2016.08.042. Epub ahead of print.
Green AL, Yi J, Bezler N, Pikman Y, Tubman VN, Obeng EA, O’Neil T, Mersereau R, Morrissey L, Billett AL. A prospective cohort quality improvement study to reduce the time to antibiotics for new fever in neutropenic pediatric oncology inpatients. Pediatr Blood Cancer. 2016 Jan; 63(1):112-7. doi: 10.1002/pbc.25712.
Toro-Salazar OH, Ferranti J, Lorenzoni R, Walling S, Mazur W, Raman SV, Davey BT, Gillan E, O’Loughlin M, Klas B, Hor KN. Feasibility of echocardiographic techniques to detect subclinical cancer therapeutics-related cardiac dysfunction among high-dose patients when compared with cardiac magnetic resonance imaging. J Am Soc Echocardiogr. 2016 Feb; 29(2):119-31. doi: 10.1016/j.echo.2015.10.008
Marina NM, Smeland S, Bielack SS, Bernstein M, Jovic G, Krailo MD, Hook JM, Arndt C, van den Berg H, Brennan B, Brichard B, Brown KL, Butterfass-Bahloul T, Calaminus G, Daldrup-Link HE, Eriksson M, Gebhardt MC, Gelderblom H, Gerss J, Goldsby R, Goorin A, Gorlick R, Grier HE, Hale JP, Hall KS, Hardes J, Hawkins DS, Helmke K, Hogendoorn PC, Isakoff MS, Janeway KA, Jürgens H, Kager L, Kühne T, Lau CC, et al. Comparison of MAPIE versus MAP in patients with a poor response to preoperative chemotherapy for newly
diagnosed high-grade osteosarcoma (EURAMOS-1): an open-label, international, randomized controlled trial. Lancet Oncol. 2016 Oct;17(10):1396-1408. doi: 10.1016/S14702045(16)30214-5.
Levine SR, McNeer JL, Isakoff MS. Challenges faced in the treatment of acute lymphoblastic leukemia in adolescents and young adults. Clin Oncol Adolesc Young Adults. 2016 Feb; 2016(6):11-20. https://doi.org/10.2147/COAYA.S61424.
Reed DR, Mascarenhas L, Manning K, Hale GA, Goldberg J, Gill J, Sandler E, Isakoff MS, Smith T, Caracciolo J, Lush RM, Juan TH, Lee JK, Neuger AM, Sullivan DM. Pediatric Phase I trial of oral sorafenib and topotecan in refractory or recurrent pediatric solid malignancies. Cancer Med. 2016 Feb;5(2):294-303. doi: 10.1002/cam4.598.
Isakoff MS, Goldsby R, Villaluna D, Krailo MD, Gorlick R, Doski JJ, Womer RB, Janeway KA. Rapid protocol enrollment in osteosarcoma: a report from the Children’s Oncology Group. Pediatr Blood Cancer. 2016 Feb; 63(2):370-1. doi: 10.1002/pbc.25754.
Isakoff MS, Bielack SS, Meltzer P, Gorlick R. Osteosarcoma: current treatment and a collaborative pathway to success. J Clin Oncol. 2015 Sep 20; 33(27):3029-35. doi: 10.1200/ JCO.2014.59.4895. Review.
Wong T, Goldsby RE, Wustrack R, Cash T, Isakoff MS, DuBois SG. Clinical features and outcomes of infants with Ewing sarcoma under 12 months of age. Pediatr Blood Cancer. 2015 Nov; 62(11):1947-51. doi: 10.1002/pbc.25635.
Overholser LS, Moss KM, Kilbourn K, Risendal B, Jones AF, Greffe BS, Garrington T, Leonardi-Warren K, Yamashita TE, Kutner JS. Development of a primary care-based clinic to support adults with a history of childhood cancer: the Tactic Clinic. J Pediatr Nurs. 2015 Sep-Oct; 30(5):724-31. doi:10.1016/j. pedn.2015.05.023.
Cortezzo DE, Sanders MR, Brownell EA, Moss K. End-of-life care in the neonatal intensive care unit: experiences of staff and parents. Am J Perinatol. 2015 Jul; 32(8):713-24. doi: 10.1055/ s-0034-1395475.
Orsey AD, Wakefield DB. Does socioeconomic status impact physical activity and sleep among children with cancer? Pediatr Blood Cancer. 2016 Nov; 63(11):2004-10. doi: 10.1002/pbc.26143.
Canfarotta M, Riba-Wolman R, Orsey AD, Balarezo F, Finck C. DICER1 syndrome and thyroid disease. J Pediatr Surg Case Rep. 2016 May 14. http://www.sciencedirect.com/science/article/pii/S221357661630094X
Patel P, Robinson PD, Orsey AD, Freedman JL, Langevin AM, Woods D, Sung L, Dupuis LL. Chemotherapy-induced nausea and vomiting prophylaxis: practice within the Children’s Oncology Group. Pediatr Blood Cancer. 2016 May: 63(5):887-92.
Toro-Salazar OH, Gillan E, Ferranti, J, Orsey AD, Rubin K, Upadhyay S, Mazur W, Hor KN. Effect of myocardial dysfunction in cardiac morbidity and all-cause mortality in childhood cancer subjects treated with anthracycline therapy. Cardio-Oncology. 2015 Nov;1(1). http://cardiooncologyjournal.biomedcentral. com/articles/10.1186/s40959-015-0005-8.
Band ME, Sheldon C, Brancato J, Parikh NS, D’AlessandriSilva C. A 17-year-old with steroid-resistant nephrotic syndrome. Pediatrics. 2016 May; 137(5). pii: e20153205. doi: 10.1542/peds.2015-3205.
Malia LA, Wolkoff LI, Mnayer L, Tucker JW, Parikh NS. A case report: Jacobsen Syndrome complicated by ParisTrousseau Syndrome and Shone’s Complex. J Pediatr Hematol Oncol. 2015 Oct; 37(7):e429-32. doi: 10.1097/ MPH.0000000000000372.
Saulnier Sholler GL, Gerner EW, Bergendahl G, MacArthur RB, VanderWerff A, Ashikaga T, Bond JP, Ferguson W, Roberts W, Wada RK, Eslin D, Kraveka JM, Kaplan J, Mitchell D, Parikh NS, et al. A Phase I Trial of DFMO targeting polyamine addiction in patients with relapsed/refractory neuroblastoma. PLoS One. 2015 May 27; 10(5):e0127246. doi: 10.1371/journal.pone.0127246.
Parikh NS, Howard SC, Chantada G, Israels T, Khattab M, Alcasabas P, Lam CG, Faulkner L, Park JR, London WB, Matthay KK; International Society of Pediatric Oncology. SIOPPODC adapted risk stratification and treatment guidelines:
recommendations for neuroblastoma in low- and middle-income settings. Pediatr Blood Cancer. 2015 Aug; 62(8):130516. doi: 10.1002/pbc.25501. PMID: 25810263; PMCID: PMC5132052.
Banfield E, Brown AL, Peckham EC, Rednam SP, Murray J, Okcu MF, Mitchell LE, Chintagumpala MM, Lau CC, Scheurer ME, Lupo PJ. Exploratory analysis of ERCC2 DNA methylation in survival among pediatric medulloblastoma patients. Cancer Epidemiol. 2016 Oct; 44:161-6. doi: 10.1016/j.canep.2016.08.020. PMID: 27607585; PMCID: PMC5050141.
Johnson KJ, Hainfellner JA, Lau CC, Scheurer ME, Woehrer A, Wiemels J. Immune factors and viral interactions in brain cancer etiology and outcomes, The 2016 Brain Tumor Epidemiology Consortium Meeting report. Clin Neuropathol. 2016 Sep-Oct; 35(5):280-6. doi: 10.5414/NP300985. PMID: 27546018; PMCID: PMC5094287.
Li Y, Nakka M, Kelly AJ, Lau CC, Krailo M, Barkauskas DA, Hicks JM, Man TK. p27 is a candidate prognostic biomarker and metastatic promoter in osteosarcoma. Cancer Res. 2016 Jul 1; 76(13):4002-11. doi: 10.1158/0008-5472.CAN-153189. PMID: 27197201; PMCID: PMC4930684.
Davis CF, Ritter DI, Wheeler DA, Wang H, Ding Y, Dugan SP, Bainbridge MN, Muzny DM, Rao PH, Man TK, Plon SE, Gibbs RA, Lau CC. SV-STAT accurately detects structural variation via alignment to reference-based assemblies. Source Code Biol Med. 2016 Jun 18; 11:8. doi: 10.1186/s13029-0160051-0. PMID: 27330550; PMCID: PMC4913042.
Davis CF, Ritter DI, Wheeler DA, Wang H, Ding Y, Dugan SP, Bainbridge MN, Muzny DM, Rao PH, Man TK, Plon SE, Gibbs RA, Lau CC. SV-STAT accurately detects structural variation via alignment to reference-based assemblies. Source Code Biol Med. 2016 Jun 18; 11:8. doi: 10.1186/s13029-0160051-0. PMID: 27330550; PMCID: PMC4913042.
Amirian ES, Scheurer ME, Zhou R, Wrensch MR, Armstrong GN, Lachance D, Olson SH, Lau CC, et al. History of chickenpox in glioma risk: a report from the glioma international casecontrol study (GICC). Cancer Med. 2016 Jun; 5(6):13528. doi: 10.1002/cam4.682. Epub 2016 Mar 13. PMID: 26972449; PMCID: PMC4924393.
Hingorani P, Janeway K, Crompton BD, Kadoch C, Mackall CL, Khan J, Shern JF, Schiffman J, Mirabello L, Savage SA, Ladanyi M, Meltzer P, Bult CJ, Adamson PC, Lupo PJ, Mody R, DuBois SG, Parsons DW, Khanna C, Lau C, et al. Current state of pediatric sarcoma biology and opportunities for future discovery: a report from the Sarcoma Translational Research Workshop. Cancer Genet. 2016 May; 209(5):182-94. doi: 10.1016/j.cancergen.2016.03.004. Epub 2016 Apr 5.
Venkatramani R, Murray J, Helman L, Meyer W, Hicks MJ, Krance R, Lau C, Jo E, Chintagumpala M. Risk-based therapy for localized osteosarcoma. Pediatr Blood Cancer. 2016 Mar 26; 63(3):412-7. doi: 10.1002/pbc.25808. Epub 2015 Oct 26. PMID: 26501936.
Hu M, Guan H, Lau CC, Terashima K, Jin Z, Cui L, Wang Y, Li G, Yao Y, Guo Y, Li YM, Zhong D, Xiao J, Wan X, Lian X, Feng F, Ren H, Zhao Y, Cheng X, Gu F. An update on the clinical diagnostic value of β-hCG and αFP for intracranial germ cell tumors. Eur J Med Res. 2016 Mar; 12; 21:10. doi: 10.1186/ s40001-016-0204-2.
Lindsay H, Huang Y, Du Y, Braun FK, Teo WY, Kogiso M, Qi L, Zhang H, Zhao S, Mao H, Lin F, Baxter P, Su JM, Terashima K, Perlaky L, Chintagumpala M, Adesina A, Lau CC, Williams Parsons D, Li XN. Preservation of KIT genotype in a novel pair of patient-derived orthotopic xenograft mouse models of metastatic pediatric CNS germinoma. J Neurooncol. 2016 Mar 8; 128(1):47-56. doi: 10.1007/s11060-016-2098-9.
Ceccarelli M, Barthel FP, Malta TM, Sabedot TS, Salama SR, Murray BA, Morozova O, Newton Y, Radenbaugh A, Pagnotta SM, Anjum S, Wang J, Manyam G, Zoppoli P, Ling S, Rao AA, Grifford M, Cherniack AD, Zhang H, Poisson L, Carlotti CG Jr, Tirapelli DP, Rao A, Mikkelsen T, Lau CC, et al. Molecular profiling reveals biologically discrete subsets and pathways of progression in diffuse glioma. Cell. 2016 Jan 28; 164(3):55063. doi: 10.1016/j.cell.2015.12.028. PMID: 26824661; PMCID: PMC4754110.
Amirian ES, Armstrong GN, Zhou R, Lau CC, Claus EB, Barnholtz-Sloan JS, et al. The glioma international case-control study: a report from the Genetic Epidemiology of Glioma International Consortium. Am J Epidemiol. 2016 Jan 15; 183(2):85-91. Epub 2015 Dec 10.
Brown AL, Lupo PJ, Okcu MF, Lau CC, Rednam S, Scheurer ME. SOD2 genetic variant associated with treatment-related ototoxicity in cisplatin-treated pediatric medulloblastoma. Cancer Med. 2015 Nov; 4(11):1679-86. doi: 10.1002/ cam4.516. Epub 2015 Sep 24.
Ritter DI, Haines K, Cheung H, Davis CF, Lau CC, Berg JS, et al. Identifying gene disruptions in novel balanced de novo constitutional translocations in childhood cancer patients by wholegenome sequencing. Genet Med. 2015 Oct 8; 17(10):831-5. doi: 10.1038/gim.2014.189. Epub 2015 Dec 8.
Zhao S, Kurenbekova L, Gao Y, Roos A, Creighton CJ, Rao P, Hicks J, Man TK, Lau C, et al. NKD2, a negative regulator of Wnt signaling, suppresses tumor growth and metastasis in osteosarcoma. Oncogene. 2015 Sept 24; 34(39):5069-79. doi: 10.1038/onc.2014.429. Epub 2015 Jan 12.
Chintagumpala M, Eckel SP, Krailo M, Morris M, Adesina A, Packer R, Lau C, Gajjar A. A pilot study using carboplatin, vincristine, and temozolomide in children with progressive/ symptomatic low-grade glioma: a Children’s Oncology Group study. Neuro Oncol. 2015 Aug; 17(8):1132-8. doi: 10.1093/ neuonc/nov057. Epub 2015 Apr 7. PMID: 25854526; PMCID: PMC4490875.
Bielack SS, Smeland S, Whelan JS, Marina N Jovic G, Hook JM, Krailo MD, Gebhardt M, Pápai Z, Meyer J, Nadel H, Randall RL, Deffenbaugh C, Nagarajan R, Brennan B, Letson GD, Teot LA, Goorin A, Baumhoer D, Kager L, Werner M, Lau CC, et al; EURAMOS-1 investigators. Methotrexate, doxorubicin, and cisplatin (MAP) plus maintenance pegylated interferon alfa-2b versus MAP alone in patients with resectable high-grade osteosarcoma and good histologic response to preoperative MAP: first results of the EURAMOS-1 Good Response Randomized Controlled Trial. J Clin Oncol. 2015 Jul 10; 33(20):2279-87. doi: 10.1200/JCO.2014.60.0734. Epub 2015 Jun 1.
Burstein MD, Tsimelzon A, Poage GM, Covington KR, Contreras A, Fuqua SAW, Savage MI, Osborne CK, Hilsenbeck SG, Chang JC, Mills GB, Lau CC, Brown PH. Comprehensive genomic analysis identifies novel subtypes and targets of triple-negative breast cancer. Clin Cancer Res. 2015 Apr 1;
21(7):1688-98. doi: 10.1158/1078-0432.CCR-14-0432. Epub 2014 Sep 10. PMID: 25208879.
Zhu S, Denman CJ, Cobanoglu ZS, Kiany S, Lau CC, Gottschalk SM, Hughes DP, Kleinerman ES, Lee DA. The narrow-spectrum HDAC inhibitor entinostat enhances NKG2D expression without NK cell toxicity, leading to enhanced recognition of cancer cells. Pharm Res. 2015 Mar; 32(3):77992. doi: 10.1007/s11095-013-1231-0. Epub 2013 Nov 8.
Jalali A, Amirian ES, Bainbridge MN, Armstrong GN, Liu Y, Tsavachidis S, Jhangiani SN, Plon SE, Lau CC, et al. Targeted sequencing in chromosome 17q linkage region identifies familial glioma candidates in the Gliogene Consortium. Sci Rep. 2015 Feb 5; 5:8278. Epub 2015 Feb 5. doi: 10.1038/ srep08278. PMC4317686.
Whelan JS, Bielack SS, Marina N, Smeland S, Jovic G, Hook JM, Krailo M, Anninga J, Butterfass-Bahloul T, Böhling T, Calaminus G, Capra M, Deffenbaugh C, Dhooge C, Eriksson M, Flanagan AM, Gelderblom H, Goorin A, Gorlick R, Gosheger G, Grimer RJ, Hall KS, Helmke K, Hogendoorn PC, Jundt G, Kager L, Kuehne T, Lau CC, et al; EURAMOS collaborators. EURAMOS-1, an international randomised study for osteosarcoma: results from pre-randomisation treatment. Ann Oncol. 2015 Feb; 26(2):407-14. doi: 10.1093/annonc/ mdu526. Epub 2014 Nov 24.
Woehrer A, Lau CC, Prayer D, Bauchet L, Rosenfeld M, Capper D, et al. Brain tumor epidemiology – a hub within multidisciplinary neuro-oncology. Report on the 15th Brain Tumor Epidemiology Consortium (BTEC) Annual Meeting, Vienna, 2014. Clin Neuropathol. 2015 Jan-Feb; 34(1):40-6. PMID: 25518914.
Staff
Ching Lau, MD, PhD
Division Head
Michael Isakoff, MD
Clinical Director
Natalie Bezler, MD
Donna Boruchov, MD
Eileen Gillan, MD
Kerry Moss, MD
Andrea Orsey, MD
Nehal Parikh, MD
Keri Curtis, PA
Sabrina Colangelo, APRN
Meredith Davide, APRN
Christine, Eaccarino, APRN
Karina Engelke, APRN
Taryn Hamre, APRN
Emily Peluso, APRN
Kimberley Roche, APRN
Katherine Steven, APRN
Sarah Wentworth, APRN
Amanda Zuse, APRN
The Division of Hospital Medicine is committed to providing exceptional, value-based care to hospitalized children and their families. We emphasize educational excellence, strong collaboration, and academic contribution to our young and rapidly expanding field. In 2016, Hospital Medicine was recognized for the first time as an official specialty by the American Board of Medical Specialties.
Pediatric Hospital Medicine is the fastest growing specialty within Pediatrics and our division has paralleled that growth. We provide general inpatient pediatric care at Connecticut Children’s Medical Center in Hartford, as well as at our 12bed satellite unit at St. Mary’s Hospital in Waterbury, CT. Our patient volume has grown over 50 percent in the past five years (2012 to 2016). We continue to partner with primary care groups to assume the care of their inpatients – 98 percent of general pediatric inpatients are now cared for by our service. We oversee a highly capable group of APRNs and PAs who provide outstanding care and have helped to lead many of our improvement initiatives.
Clinical accomplishments during the past two years were numerous. As a division, we have taken a lead role in process improvement, with a focus on optimizing patient flow while ensuring high quality. Our APRN/PA group led a project in which we discharged Observation patients within the goal of 24 hours at a rate of 84 percent, compared to the prior 34 percent. The division spearheaded a movement to expand Family Centered Rounds from our own group to other specialties within the inpatient setting. We have continued our Comanagement Program in which we provide medical expertise in the care of complex surgical patients. This consult service has improved communication and family satisfaction, and has led to better care for children with complex needs. Through our Clinical Effectiveness arm, we have led in standardizing best practice via multiple new Clinical Pathways. There are now over 20 pathways in active use, and we have demonstrated reduced length of stay and costs with no increase in readmits, while improving patient outcomes (See Figure 1).
Effective pathways can demonstrate how hospitalists improve value, a concept that will be increasingly important as health care systems continue to evolve.
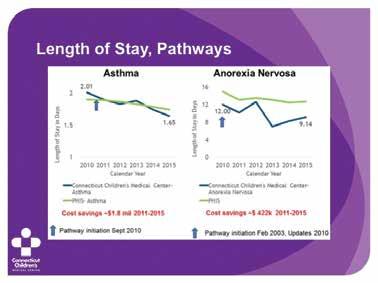
Education of the next generation of pediatric providers remains a crucial part of our mission. Our faculty members continue to excel in this area. Dr. Kathy Kalkbrenner earned the annual Faculty Award for Excellence in Teaching in both 2015 and 2016, as well as the Award for Teaching in Acute Care in 2016. Dr. Cathy Sullivan received the Volunteer Physician of the Year award from the medical students of the University of Connecticut School of Medicine in 2016, for her excellence in teaching over the years.
Members of the division continue to share their work on a national level. Division head Dr. Anand Sekaran and Dr. Ilana Waynik joined forces with Phoenix Children’s to lead a workshop at the Pediatric Hospital Medicine annual meeting to teach faculty from around the country how to create and implement Clinical Pathways. Dr. Sekaran contributed a chapter in the definitive handbook for Pediatric Hospital Medicine entitled Caring for the Hospitalized Child. Dr. Waynik presented at the national meeting of Child and Adolescent Psychiatry on Clinical Pathways geared towards mental health. Dr. Christine Skurkis presented nationally as well in the field of Medical Education. Our lead APRN, Basia Adams, spoke about her work at the annual Illuminations Conference on Quality, and her abstract on patient flow was one of three finalists for the overall Best Abstract award.
As hospitalists, we continue to evolve in how we provide value, educate trainees, and improve care. Our goal is not only to
measure our performance against national standards but to be at the top of those standards. Yet as we continue to grow, we strive to maintain our greatest core value of putting patients and families first in all we do.
Dr. Waynik and Dr. Nicholas Bennett of the Infectious Diseases Division were awarded a 2015 Adopt-a-Program Award in the amount of $35,000 in support of an expansion of the Connecticut Children’s Medical Center Antimicrobial Stewardship Program to assist pediatric stewardship initiatives throughout the state of Connecticut.
Chapter
A Sekaran, B Campbell. Ovarian torsion. In: Gershel JC, Rauch DA, editors. Caring for the hospitalized child: a handbook of inpatient pediatrics. 2nd ed. American Academy of Pediatrics. 2017.
Staff
Anand Sekaran, MD Division Head
Emilee Colella, MD
Richard Johnson, MD
Kathy Kalkbrenner, MD
Sumith Madhavarapu, DO
David Marcello, MD
Chris McDermott, MD
Marta Neubauer, MD
Christine Skurkis, MD
Catherine Sullivan, MD
MacDara Tynan, MD
Ilana Waynik, MD
Basia Adams, Lead APRN
Kara Denz-Fluck, PA-C
Jill Herring, APRN
Grace Hong, APRN
Samantha Lee, APRN
Abby Theriaque, APRN
The Division of Human Genetics resides jointly in the Department of Genetics and Genome Sciences as well as the Department of Pediatrics. The mission of the division is to provide high quality, timely and state-of-the-art genetic consultations, counseling, and treatment for patients from the prenatal period throughout childhood and into adulthood.
Care throughout the lifespan is provided across two campuses by a team of clinical geneticists, genetic counselors and a metabolic dietician. In 2016, our former division head, Dr. Sally Rosengren, retired after more than 20 years of dedicated service. Dr. Joseph Tucker has been named as interim division head.
Our team currently consists of 1.0 FTE clinical medical geneticist, 2.0 FTE prenatal genetic counselors, 1.8 FTE hereditary cancer genetic counselors, 1.0 FTE teratology counselor, and 0.4 FTE metabolic dietician. The clinical, administrative, and academic offices are currently housed at the UConn Health campus at 263 Farmington Ave., Farmington, CT, where children and adults are seen in a general genetics clinic, and where prenatal and hereditary cancer patients receive genetic counseling. MotherToBabyCT provides additional prenatal counseling services at 195 Farmington Ave., Farmington, CT. Additional pediatric services are provided at our Connecticut Children’s outpatient clinic at 11 South Road, Farmington, CT.
A full-service cytogenetics laboratory run by Dr. Peter Benn at John Dempsey Hospital in Farmington provides genetic testing services.
Patients with metabolic disease identified through the Department of Public Health Newborn screening program, as well as children diagnosed at a later age, are seen at the UConn Health campus in conjunction with our metabolic dietician.
Increased use of non-invasive prenatal genetic testing continues to increase the number of patients being seen by the prenatal service, and frequently updated test offerings for patients with hereditary cancers has increased the patient numbers being seen and evaluated by the hereditary cancer counseling program. MotherToBabyCT, our teratogen counseling program, is expanding its coverage throughout the state.
Collaborations with Connecticut Children’s Medical Center, Department of Public Health Newborn Screening Program, UConn’s Maternal–Fetal–Medicine program, and UConn’s Neag Cancer Center in Farmington are robust and active. A Department of Public Health annual contract helps to support the newborn screening/metabolic and MotherToBabyCT programs.
The division’s educational mission begins in the first year of medical school and goes through postgraduate fellowship. We have an active medical genetics and genomics residency training program and have successfully matched a candidate, Dr. Jaclyn Gordon from St. Joseph’s Regional Medical Center in Paterson, NJ, for July 2017. There are also student, resident, fellow, and genetic counseling learners who spend a month’s rotation in genetics.
The years 2015-2016 have been busy for Dr. Benn who delivered invited presentations to international audiences at conferences throughout the United States and internationally. Dr. Benn serves as a reviewer for many publications including the American Journal of Medical Genetics, the American Journal of Obstetrics and Gynecology, Genetics in Medicine, and Prenatal Diagnosis. He is a member of the board of the International Society for Prenatal Diagnosis.
The division’s teratogen counseling program, MotherToBabyCT, received a grant entitled “Reproductive and Environmental Health Network” through HRSA.
Robin Schwartz, MS, CGC, is co-chair of Education and Workforce Development for the Genetic Advisory Committee at the CT Department of Public Health.
Robin Schwartz, MS, CGC, and Jennifer Stroop, MS, CGC, are both collaborating investigators in the CICATS project, “Determining clinical significance of mismatch repair variants,” with PI Chris Heinen, PhD.
Joseph Tucker, MD, currently serves on the board of directors for New England Regional Genetics Group (NERGG).
He continues in his role as an active member of the GUPPE program, and along with the Urology, Psychiatry, Psychology, and Endocrinology divisions at Connecticut Children’s, they provide multidisciplinary care for children with disorders of sexual development.
Sharon Voyer Lavigne, MS, LGC, serves on the board of directors for the Organization of Teratology Information Services (OTIS). She also serves as vice president of the board of directors for Post Partum Support International, CT Chapter.
Publications
Benn P. Non-invasive prenatal testing using cell free DNA in maternal plasma: recent developments and future prospects. J Clin Med. 2015; 3:537-65.
Benn P, Curnow KJ, Chapman S, Michalopoulos SN, Hornberger J, Rabinowitz M. An economic analysis of cell-free DNA non-invasive prenatal testing in the U.S. general pregnancy population. PloS One. 2015 Jul9. http://dx.doi.org/10.1371/ journal.pone.0132313.
Dar P, Gross SJ, Benn P. Reply to PMID: 25111587. Am J Obstet Gynecol. 2015; 213:253-4.
Benn P. [commentary] Zhang H, Gao Y, Jiang F, Fu M, Yuan Y, Guo Y, Zhu Z, Lin M, Liu Q, Tian Z, Zhang H, Chen F, Lau TK, Zhao L, Yi X, Yin Y, Wang W. Non-invasive prenatal testing for trisomies 21, 18 and 13: clinical experience from 146,958 pregnancies. Ultrasound Obstet Gynecol. 2015; 45:512-3.
Benn P, Borrell A, Chiu RW, Cuckle H, Dugoff L, Faas B, Gross S, Huang T, Johnson J, Maymon R, Norton M, Odibo A, Schielen P, Spencer K, Wright D, Yaron Y. Position statement from the Chromosome Abnormality Screening Committee on behalf of the Board of the International Society for Prenatal Diagnosis. Prenat Diagn. 2015 Aug; 35(8):725-34.
Gross SJ, Ryan A, Benn P. Noninvasive prenatal testing for 22q11.2 deletion syndrome: deeper sequencing increases the positive predictive value. Am J Obstet Gynecol. 2015; 213:254-5.
Dar P, Gross SJ, Benn P. Positive predictive values and falsepositive results in noninvasive prenatal screening. Am J Obstet Gynecol. 2015; 213:595-6.
Gross SJ, Stosic M, McDonald-McGinn DM, Bassett AS, Norvez A, Dhamankar R, Kobara K, Kirkizlar E, Zimmermann B, Wayham N, Babiarz JE, Ryan A, Jinnett KN, Demko Z, Benn P. (2016). Clinical experience with single-nucleotide polymorphism-based non-invasive prenatal screening for 22q11.2 deletion syndrome. Ultrasound Obstet Gynecol. 2016 Feb 4; 47(2):177-83.
Rose NC, Benn P, Milunsky A. Current controversies in prenatal diagnosis 1: should NIPT routinely include microdeletions/microduplications? Prenatal Diagn. 2016 Jan; 36(1):10-4.
Benn KN, Benn P, Campbell WA, Amirhossein M, Shamshirsaz AA. Genetic sonogram: components and role in the era of prenatal screening. Fetal Matern Med Rev. Epub 2015 Sep; 1-18. doi: 10.1017/S096553951500008X.
Karam F, Sheehy O, Huneau M-C, Chambers C, Fraser WD, Johnson D, Kao K, Martin B, Riordan SH, Roth M, St-André M, Lavigne SV, Wolfe L, Bérard A. Impact of maternal prenatal and parental postnatal stress on 1-year-old child development: results from the OTIS antidepressants in pregnancy study. Arch Women Ment Health. 2016 Oct 8; 19(5):835-43. Epub 2016 Mar 8.
Malia LA, Wolkoff LI, Mnayer L, Tucker JW, Parikh NS. A case report: Jacobsen Syndrome complicated by Paris-Trousseau Syndrome and Shone’s Complex. J Pediatr Hematol Oncol. 2015 Oct; 37(7):e429-32.
Chapters
Benn P. Prenatal diagnosis of chromosome abnormalities through chorionic villus sampling and amniocentesis. In: Milunsky A, Milunsky J, editors. Genetic disorders and the fetus: diagnosis, prevention, and treatment. 7th edition. Chichester, UK: Wiley; 2016. p. 178-266.
Cuckle H, Pergament E, Benn P. Maternal serum screening for chromosome abnormalities and neural tube defects. In: Milunsky A, Milunsky J, editors. Genetic disorders and the fetus: diagnosis, prevention, and treatment. 7th edition. Chichester, UK: Wiley; 2016. p. 483-540.
Staff
Joseph Tucker, MD
Interim Division Head
Mark Greenstein, MD
Luisa Kalsner, MD
Peter Benn, PhD
Alicia Craffey, MS, CGC
Sharon Voyer Lavigne, MS, LGC
Ginger Nichols, MS, CGC
Robin Schwartz, MS, CGC
Brittany Gancarz, MS, CGC
Jennifer Stroop, MS, CGC
Sherry Gray, MS, MPH, CDN
Robert Greenstein, MD
Faculty Emeritus

The Division of Infectious Diseases and Immunology continues to care for patients with unusual and chronic infections, and those with immune deficiencies. The years 2015 and 2016 marked further growth clinically and academically for the division.
“Growth” was the theme of 2016 in the division, with the opening of two new satellite sites, at Danbury and Farmington, in addition to the move to our larger, custombuilt clinic suite on the Hartford campus. Dr. Tom Murray’s research collaborations with our pediatric pulmonary division have blossomed into a combined ID/Pulmonary clinic for children with cystic fibrosis and other chronic lung conditions. As our scope of practice has widened both clinically and geographically, we have been looking to increase our staffing, and in 2016 we hired an experienced nurse practitioner, Grace Hong, APRN. Grace brings considerable expertise in the development of the clinical pathways initiatives at Connecticut Children’s, including several that have involved the Antimicrobial Stewardship Program (ASP).
The ASP graduated their second PL2-pharmacy resident this year and successfully recruited a third. We also worked on an outreach effort to outlying hospitals in the state, supported by a $35,000 grant from the Friends of Connecticut Children’s. We hope to assist other hospitals to bootstrap their efforts in developing and maintaining pediatric antimicrobial stewardship efforts – something that will become increasingly important as the new CMS (Center for Medicaid Services) and Joint Commission requirements come into effect in 2017.
Our Ryan White program’s work for youth and adolescents at risk of, and infected with, HIV has been recognized internationally for its novel initiatives in identifying and caring for high-risk individuals. There continues to be a need to work with newly infected individuals and to reduce risk. As well as our Medical Case Managers’ work on the Popular Opinion Leader initiative, school outreach, and the Willow support meetings for mothers infected with HIV, our clinic offers a comprehensive Pre-Exposure Prophylaxis (PrEP) for at-risk youth. PrEP includes test-
ing, counseling, and preventative measures to reduce the risk of acquiring HIV and other sexually transmitted diseases.
Perhaps the most exciting development of 2016 was the successful application for a new fellowship program in Pediatric Infectious Diseases at Connecticut Children’s Medical Center, through the University of Connecticut. This three-year program has been designed to offer fellows key experiences in the areas of antimicrobial stewardship and the diagnosis and management of patients with primary immune deficiencies – building on our existing expertise with the Antimicrobial Stewardship Program and our board-certified immunologists in the division. Most of the fellow’s time will be spent in research, and we have identified opportunities at UConn’s Farmington and Storrs campuses in the areas of immunology, infectious diseases, and pharmacology, as well as in the renowned Center for Anti-Infective Research and Development at Hartford Hospital.
The division continues to publish cutting-edge research, funded by NIH R01 and R03 grants held by Dr. Juan Salazar, as well as clinical reports and reviews.
R56 AI097210 NIAID – Mechanisms of impaired mycobacteria sensing by TLR2 and TLR4 polymorphic variants. (Active: 7/17/2014-6/30/2016) PI: Dr. Juan Salazar.
R0-1 AI090166 NIAID – Phagosomal signals shape inflammatory responses to Borrelia burgdorferi. Direct amount per year $315,000. (Active: 07/15/20116/30/2016) PI: Dr. Juan Salazar.
R03 TW00972 – Mechanisms of immune evasion in human syphilis. (Active: 3/1/2013-11/30/2015) Co-PI: Dr. Juan Salazar.
AI-29735 NIH RpoS regulation of Borrelia burgdorferi genes in vivo. (Active 2/1/2013-1/31/2018) Co-Investigator: Dr. Caimano.
Publications
Fitzstevens JL, Smith KC, Hagadorn JI, Caimano MJ, Matson AP, Brownell EA. Systematic review of the human milk microbiota. Nutr Clin Pract. 2016 Sep 27.
Caimano MJ, Drecktrah D, Kung F, Samuels DS. Interaction of the Lyme disease spirochete with its tick vector. Cell Microbiol. 2016 Jul; 18(7):919-27.
Miller DP, Oliver LD Jr, Tegels BK, Reed LA, O’Bier NS, Kurniyati K, Faust LA, Lawson CK, Allard AM, Caimano MJ, Marconi RT. The Treponema denticola FhbB protein is a dominant early antigen that elicits FhbB variant-specific antibodies that block factor H binding and cleavage by dentilisin. Infect Immun. 2016 Jun 23; 84(7):2051-8.
Gulia-Nuss M, Nuss AB, Meyer JM, Sonenshine DE, Roe RM, Waterhouse RM, et al. (Caimano MJ, 31/93). Genomic insights into the Ixodes scapularis tick vector of Lyme disease. Nat Commun. 2016 Feb 9; 7:10507.
Bauer WJ, Luthra A, Zhu G, Radolf JD, Malkowski MG, Caimano MJ. Structural characterization and modeling of the Borrelia burgdorferi hybrid histidine kinase Hk1 periplasmic sensor: a system for sensing small molecules associated with tick feeding. J Struct Biol. 2015 Oct; 192(1):48-58.
Grassmann AA, McBride AJ, Nally JE, Caimano MJ. Generation of mammalian host-adapted leptospira interrogans by cultivation in peritoneal dialysis membrane chamber implantation in rats. Bio Protoc. 2015 Jul 20; 5(14). pii: e1536.
Caimano MJ, Dunham-Ems S, Allard AM, Cassera MB, Kenedy M, Radolf JD. Cyclic di-GMP modulates gene expression in Lyme disease spirochetes at the tick-mammal interface to promote spirochete survival during the blood meal and tick-to-mammal transmission. Infect Immun. 2015 Aug; 83(8):3043-60.
Luthra A, Anand A, Hawley KL, LeDoyt M, La Vake CJ, Caimano MJ, Cruz AR, Salazar JC, Radolf JD. A homology model reveals novel structural features and an immunodominant surface loop/opsonic target in the Treponema pallidum BamA Ortholog TP_0326. J Bacteriol. 2015 Jun; 197(11):1906-20.
Iyer R, Caimano MJ, Luthra A, Axline D Jr, Corona A, Iacobas DA, Radolf JD, Schwartz I. Stage-specific global alterations in the transcriptomes of Lyme disease spirochetes during tick feeding and following mammalian host adaptation. Mol Microbiol. 2015 Feb; 95(3):509-38.
Magsarili HK, Girotto JE, Bennett NJ, Nicolau DP. Making a case for pediatric antimicrobial stewardship programs. Pharmacotherapy. 2015 Nov; 35(11):1026-36.
Valdez TA, Marvin K, Bennett NJ, Lerer T, Nolder AR, Buchinsky FJ. Current trends in perioperative antibiotic use: a survey of otolaryngologists. Otolaryngol Head Neck Surg. 2015 Jan; 152(1):63-6.
Courter JD, Nichols KR, Kazazian C, Girotto JE. Pharmacodynamically guided levofloxacin dosing for pediatric community-acquired pneumonia. J Pediatric Infect Dis Soc. 2016 Feb 21.
Goodlet KJ, Girotto JE. Optimal vaccine administration for patients undergoing chemotherapy. Conn Med. 2016 May; 80(5):305-11.
Feder HM Jr, Plucinski M, Hoss DM. Dengue with a morbilliform rash and a positive tourniquet test. JAAD Case Rep. 2016 Nov 9; 2(5):422-3.
Vetter NM, Feder HM Jr, Ratzan RM. Rat bite fever caused by a kiss. Am J Emerg Med. 2016 Jun; 34(6):1190.e3-4.
Feder HM Jr, Rigos L, Teti K. Pott’s disease in a Connecticut toddler. Lancet. 2016 Jul 30; 388(10043):504.
Seña AC, Zhang XH, Li T, Zheng HP, Yang B, Yang LG, Salazar JC, Cohen MS, Moody MA, Radolf JD, Tucker JD. A systematic review of syphilis serological treatment outcomes in HIV-infected and HIV-uninfected persons: rethinking the significance of serological non-responsiveness and the serofast state after therapy. BMC Infect Dis. 2015 Oct 28; 15:479.
Rideout M, Held M, Holmes AV. The didactic makeover: keep it short, active, relevant. Pediatrics. 2016 Jul; 138(1).
Talwalkar JS, Murray TS. The approach to pseudomonas aeruginosa in cystic fibrosis. Clin Chest Med. 2016 Mar; 37(1):69-81.
Towle D, Callan DA, Lamprea C, Murray TS. Baby bottle steam sterilizers for disinfecting home nebulizers inoculated with non-tuberculous mycobacteria. J Hosp Infect. 2016 Mar; 92(3):222-5.
Murray TS, Peaper DR. The contribution of extended-spectrum β-lactamases to multidrug-resistant infections in children. Curr Opin Pediatr. 2015 Feb; 27(1):124-31.
Benin AL, Fodeh SJ, Lee K, Koss M, Miller P, Brandt C. Electronic approaches to making sense of the text in the adverse event reporting system. J Healthc Risk Manag. 2016 Aug; 36(2):10-20.
Hernandez-Trujillo H, Orange JS, Roy JA, Wang Y, Newcomb CN, Liu Q, Hennessy S, Lo Re V 3rd. Validity of primary immunodeficiency disease diagnoses in United States Medicaid data. J Clin Immunol. 2015 Aug; 35(6):566-72.
Hernandez-Trujillo VP, Scalchunes C, Hernandez-Trujillo HS, Boyle J, Williams P, Boyle M, Orange JS. Primary immunodeficiency diseases: an opportunity in pediatrics for improving patient outcomes. Clin Pediatr (Phila). 2015 Nov; 54(13):1265-75.
Girotto JE. Skin/soft tissue, bone, and joint infections. In: Todd T, Eiland L, editors. Advanced pediatric therapeutics. 2015.
Courter JD, Nichols K, Kazazian C, Girotto JE. Optimal levofloxacin dosing for pediatric community-acquired pneumonia. J Pediatric Infect Dis Soc. 2016 Feb 21. Pii:pow006. Epub ahead of print.
Staff
Juan C. Salazar, MD, MPH
Division Head
Nicholas Bennett, MBBChir, PhD
Clinical Director
Andrea Benin, MD
Alberto Cohen-Abbo, MD
Henry M. Feder, Jr., MD
Melissa Held, MD
Hillary Hernandez-Trujillo, MD
Thomas Murray, MD, PhD
Gavin Schwarz, MD
Melissa J. Caimano, PhD
Jennifer Girotto, PharmD
Grace Hong, APRN

The Division of Neonatal-Perinatal Medicine directs one of the largest and most diverse clinical services in New England and is the perinatal regional center for northern Connecticut. In 2015, we had a transition in leadership as Victor Herson, MD, stepped down from his leadership role, and we welcomed James Moore, MD, PhD, as the new Division Head of Neonatology.
The primary mission of the Division of Neonatal-Perinatal Medicine is to provide quality, state-of-the-art care to neonates in our region, in addition to advancing education, training, and cutting edge research. The division faculty provides care at multiple sites across the state including Connecticut Children’s Medical Center (Hartford), Connecticut Children’s Medical Center at the University of Connecticut Health Center (UCHC)/John Dempsey Hospital (JDH) in Farmington, St. Francis Hospital and Medical Center (SFHMC) in Hartford, and Eastern Connecticut Health Network (ECHN) in Manchester. Our faculty members not only work collaboratively across these sites, but are partners with Yale Neonatology, and the March of Dimes, in leading the Connecticut Perinatal Quality Collaborative, helping to improve maternal and newborn care at the state level.
The division’s global outreach initiatives continued to expand in both 2015 and 2016. Victor Herson, MD, and Sandra Motta, MD, continued to work with teams from Connecticut Children’s Center for Global Health traveling to and teaching Neonatal Resuscitation to health care providers in Haiti. In addition, Naveed Hussain, MD, and Leonard Eisenfeld, MD, headed a team from Connecticut Children’s Medical Center and the University of Connecticut to the NICE Institute for the Newborn in Hyderabad, India. The team led multiple training sessions with the staff and medical providers there to help set up the region’s first Infant Cooling Program for the treatment of Hypoxic Ischemic Encephalopathy (HIE). Our ongoing collaboration with the NICE Institute has resulted in 23 infants successfully managed for HIE in the first 12 months of the program’s operation.
The research mission of Neonatal-Perinatal Medicine continues to grow including basic, clinical and translational areas of investigation, including human milk, breastfeeding medicine,
fetal/neonatal allergy and immunology, necrotizing enterocolitis, and oxygen targeting and associated toxicity. Division members continue to present their work in publications and at national research conferences. James Moore MD, PhD, cochaired an international symposium, in addition to presenting his own research on the use of Near Infrared-Spectroscopy in Neonatology at the Pediatric Academic Societies meeting in 2016. David Sink, MD, and James Hagadorn, MD, presented their findings at the 2015 iNICQ quality summit at the Vermont Oxford Network (VON). This iNICQ quality collaborative focused on alarm safety and safe oxygen therapy for premature infants. Multidisciplinary teams from 118 NICUs participated. Drs. Sink and Hagadorn presented work from Connecticut Children’s on improving patient safety by reducing alarm fatigue in the NICU. In 2015 and 2016, the division had more than 35 publications, and 28 national presentations.
As an academic section of Neonatology, education through teaching and mentoring neonatology fellows, pediatric residents, medical, nurse practitioner, physician assistant and pharmacy students is a primary objective. Under the leadership of James Hagadorn, MD, our fellowship program continues to attract the highest caliber fellows. The faculty continue to lecture and organize Neonatology board review courses, publish textbooks in the field, and, in 2016, hosted the first annual “Symposium on Neonatal Advances: Update on Respiratory Practice” at the Connecticut Children’s Medical Center NICU in Farmington. This conference was co-chaired by Mariann Pappagallo, MD, and Janet Schwenn, and it featured five internationally recognized speakers.
Publications
Briere C-E, Lucas R, McGrath JM, Lussier M, Brownell E. Establishing breastfeeding with the late preterm infant in the NICU. J Obstet Gynecol Neonatal Nurs. 2015 Jan-Feb; 44(1):102-13. PMID:25573231.
Bundhoo A, Paveglio S, Rafti E, Dhongade A, Blumberg RS, Matson AP. Evidence that FcRn mediates the transplacental passage of maternal IgE in the form of IgG anti-IgE/IgE immune complexes. Clin Exp Allergy. 2015 Jun; 45(6):108598. PMID: 25652137.
Brownell EA, Hagadorn JI, Lussier MM, Goh G, ThevenetMorrison KN, Lerer TJ, Herson VC, Howard CR. Optimal periods of exclusive breastfeeding to predict any breastfeeding duration through one year. J Pediatr. Mar 2015; 166(3):56670.e1. PMID: 25950919.
Bracken SJ, Adami AJ, Szczepanek SM, Ehsan M, Natarajan P, Guernsey LA, Shahriari N, Rafti E, Matson AP, Schramm CM, Thrall RS. Long-term exposure to house dust mite leads to the suppression of allergic airway disease despite persistent lung inflammation. Int Arch Allergy Immunol. 2015; 166(4):243-58. PMID: 25924733.
Briere C-E, McGrath JM, Cong X, Brownell E, Cusson R.
Direct-breastfeeding premature infants in the neonatal intensive care unit. J Hum Lact. 2015 Aug; 31(3):386-92. PMID: 25900843.
Hagadorn JI, Brownell EA, Herbst KW, Trzaski JM, Neff S, Campbell BT. Trends in treatment and in-hospital mortality for neonates with congenital diaphragmatic hernia. J Perinatol. 2015 Sep; 35(9):748-54. PMID: 25950919.
Smith AL, Garbus H, Rosenkrantz TS, Fitch RH. Sex differences in behavioral outcomes following temperature modulation during induced neonatal hypoxic ischemic injury in rats. Brain Sci. 2015 May 22; 5(2):220-40. PMID: 26010486.
Lussier MM, Brownell EA, Proulx TA, Bielecki DM, Marinelli KA, Bellini SL, Hagadorn JI. Daily breastmilk volume in mothers of very low birth weight neonates: a repeatedmeasures randomized trial of hand expression versus electric breast pump expression. Breastfeed Med. 2015 Jul-Aug; 10(6):312-7. PMID: 26204125.
Cong X, Ludington-Hoe SM, Hussain N, Cusson RM, Walsh S, Vazquez V, Briere CE, Vittner D. Parental oxytocin responses during skin-to-skin contact in pre-term infants. Early Hum Dev. 2015 Jul; 91(7):401-6. PMID: 25988992.
Hagadorn JI, Salikooti S, Pappagallo M, AriasCamison J, Weiner S, Alba J, Herson V. Postpartum triage, services provided, and length of stay for infants born at 35 weeks gestation. Am J Perinatol. Jul 2015; 32(8):747-54. PMID: 25535928.
Kaushik M, Bober B, Eisenfeld L, Hussain N. Hemophilus parainfluenzae sepsis in a newborn infant following water birth and a review of the literature. Am J Perinatol Rep. 2015 Oct. doi: http://dx.doi.org/10.1055/s-0035-1556068.
Braga MS, Kabbur P, Alur P, Goodstein MH, Roberts KD, Satrom K, Shivananda S, Goswami I, Pappagallo M, Briere CE, Suresh G. Current practice of neonatal resuscitation documentation in North America: a multi-center retrospective chart review. BMC Pediatr. 2015 Nov 14; 15:184. PMID: 26572859.
Smith AL, Alexander ML, Sadek ML, Rosenkrantz TS, Fitch RH. Sex differences in behavioral outcome following neonatal hypoxic ischemic brain injury: a female advantage? Int J Dev Neurosci. 2015 Dec; 47(Pt A):91-2. doi:10.1016/j.ijdevneu. 2015.04.250.
Smith AL, Alexander M, Chrobak JJ, Rosenkrantz TS, Fitch RH. Dissociation in the effects of induced neonatal hypoxiaischemia on rapid auditory processing and spatial working memory in male rats. Dev Neurosci. 2015; 37(4-5):440-52. PMID: 25791036.
Assad M, Elliott MJ, Abraham JH. Decreased cost and improved feeding tolerance in VLBW infants fed an exclusive human milk diet. J Perinatol. 2015; 36(3):216-20.
Bellini S. Post-resuscitation care and pre-transport stabilization of newborns using the principles of STABLE Transport. Nurs Women’s Health. 2015; 19(6): 533-6.
Bellini S. What parents need to know about vitamin K administration at birth. Nurs Women’s Health. 2015; 19(3):261-5.
Bellini S. Ensuring quality in online NNP programs. NANNCentral. 2015; 31(1):3. ISSN: 1544-3382.
Bellini S. A primer on updates to the Neonatal Resuscitation Program. Nurs Women’s Health. 2016; 20(3):305-8.
Fitzstevens JL, Smith KC, Hagadorn JI, Caimano MJ, Matson AP, Brownell EA. A systematic review of the human milk microbiota. Nutr Clin Pract. 2016 Sept 27.
Hagadorn JI, Brownell EA, Trzaski JM, Johnson KR, Lainwala S, Campbell BT, Herbst KW. Trends and variation in management and outcomes of very low birth
weight infants with patent ductus arteriosus. Pediatr Res. 2016 Sept 28.
Brownell EA, Smith KC, Cornell EL, Esposito PA, Wiley CC, Wang Z, Bushley AW, Lussier MM, Hagadorn JI. Five-year secular trends and predictors of non-consent to receive donor milk in the neonatal intensive care unit. Breastfeed Med. 2016 May 18.
Cornell EL, Lerer TJ, Hagadorn JI, Chapman DJ, Lussier MM, Brownell EA. A non-NICU-specific peer counseling program is not associated with human milk receipt at or following discharge. J Perinatol. 2016 May 26.
Briere CE, McGrath JM, Cong X, Brownell E, Cusson R. Direct-breastfeeding in the neonatal intensive care unit and breastfeeding duration for premature infants. Appl Nurs Res. 2016. doi: http://dx.doi.org/10.1016/j.apnr.2016.04.004.
Hagadorn JI, Sink DW, Buus-Frank M, Edwards E, Morrow K, Horbar J, Ferrelli, K, Soll R. Oximeter alarm safety and oxygen saturation targeting in the Vermont Oxford Network iNICQ 2015: Alarm Safety quality improvement collaborative. J Perinatol. 2016 Dec 15. doi: 10.1038/jp.2016.219.
Cornell E, Lerer T, Hagadorn JI, Chapman DJ, Lussier M, Brownell E. The effect of peer counselors on human milk receipt in the neonatal ICU. J Perinatol. 2016 May 26. doi: 10.1038/jp.2016.75. Epub ahead of print. PMID: 27228507.
Hagadorn JI, Brownell EA, Lussier MM, Parker MGK, Herson VC. Variability of criteria for pasteurized donor human milk use: a survey of US neonatal ICU medical directors. JPEN J Parenter Enteral Nutr. 2016 Mar; 40(3): 326-33.
Lainwala S, Hussain N. Treatment of patent ductus arteriosus with cylco-oxygenase inhibitors beyond 2 weeks of age in very low birth weight infants. Am J Perinatol. 2016; 33:584-9.
Bellini S, Beaulieu M, editors. Neonatal advanced practice nursing: a case-based learning approach. New York: Springer; 2016 Nov 28.
Bolam D, Duncan SD, Engle W, Gomez M, Grebe J, Hoffmeister C, Kanter DM, Martin GI, Molteni RA, Nemerofsky S, Pearlman SA, Rosen T, Rosenkrantz T, Weisberger S. Quick reference guide to neonatal coding and documentation. 2nd ed. Duncan SD, Martin GI, Pearlman SA, editors. American Academy of Pediatrics; 2015 Aug.
Chapters
Bellini S, Cusson RM. The role of the nurse practitioner. In: Dreher HM, Smith-Glasgow ME, editors. Role development for doctoral advanced nursing practice. 2nd ed. New York: Springer; 2016 Dec.
DeNisco S, Bellini S. When the DNP chair is a DNP graduate: the DNP in the academic role. In: Dreher HM, Smith-Glasgow ME, editors. Role development for doctoral advanced nursing practice. 2nd ed. New York: Springer; 2016 Dec.
Books
Adams-Chapman I, Carlton DP, Moore JE. Specialty board review neonatal-perinatal medicine. 1st ed. New York: McGraw-Hill; 2015.

Staff
James E. Moore, MD, PhD
Division Head
Jose Arias-Camison, MD
Tina Rita Bafumi, MD
Fadel Balawi, MD
Hema DeSilva, MD
Professor Emeritus
Leonard I. Eisenfeld, MD
James Hagadorn, MD
Victor C. Herson, MD
Naveed Hussain, MBBS, DCH
Carla Jacobson-Kiel, MD
Shabnam Lainwala, MD
Kathleen Marinelli, MD
Adam Matson, MD
Arpana Mohnani, MD
Sandra Motta, MD
Indira Panthagani, MD
Mariann Pappagallo, MD
Ted S. Rosenkrantz, MD
Saritha Salikooti, MD
Marilyn Sanders, MD
Shikha Sarkar, MD
David W. Sink, MD
Jennifer Trzaski, MD
Aniruddha Vidwans, MD
Leslie I. Wolkoff, MD
Jacqueline McGrath, PhD
Sandra Bellini, DNP, APRN, NNP-BC
Corey Champeau, PA-C
Sabrina Colangelo, PA-C
Allyson Dacruz, PA-C
Shivani Desai, PA-C
James Gerace, PA
Brian Landry, PA-C
Kristen Moore, PA
Lucia Onofrio, PA-C
Jessica Simao, PA
Stacy Voegeli, PA-C
Angela Boisseau, APRN
Mary Brennan-Centrella, APRN
Anna Camacho, APRN
Stephanie Capps, APRN
Jessica Cauchon, APRN
Karen Cleveland, APRN
Nicole Duguay, APRN
Maria Haar, APRN
Jill Herr, APRN
Lindsay Leighton, APRN
Michelle Letendre, APRN
Jennifer Long, APRN
Nick Markey, APRN
Stephanie McGuire, APRN
Suanne Menick, APRN
Karen O’Brien, APRN
Kim Oski, APRN
Wendy Petow, APRN
Karen Pietruszkiewicz, APRN
Laura Pittari, APRN
Terry Poppiti, APRN
Christine Raymond, APRN
Megan Richardson, APRN
Stacey Rubin, APRN
Babette Sternat, APRN
Patricia Trehey, APRN
Lindsay Tucker, APRN
Alyssa Weiss, APRN
Claudia Wittenzellnew, APRN
Erin Vlahakis, APRN
Mary Young, APRN
In 2015, for the first time, the Urology-Nephrology service line was able to provide a full year of comprehensive care for the children of Connecticut with complex genitourinary medical needs. In 2015 and 2016, joint service line clinics were in full swing with the continued success of both the ROCKS (Reduction of Childhood Kidney Stones) and CKD/PUV clinics. Satellite services are now fully established at Connecticut Children’s Shelton and Farmington locations, and we also have the ability to obtain joint visits with Urology at the Farmington site. Dialysis and transplant services grew with six transplant recipients during 2015 and 2016.
The year 2015 also marked the first time that our Pediatric Nephrology section became the largest in the state with four board-certified/eligible Pediatric Nephrologists, a dietitian, a physician assistant, two nurses, and a dedicated full-time social worker. As a service line, we have successfully integrated ancillary services for both the inpatient and outpatient areas, improving the patient and family experience. We are providing comprehensive care seamlessly for our patients regardless of
where they are located in our hospital.
In 2015 and 2016, the division increased care and completed more than 5,500 outpatient visits as well as increasing inpatient volumes. The visits were comprised of pre-transplant, post-transplant, inpatient and outpatient consults as well as acute and chronic dialysis. Our Renal Transplant service grew with five recipients for the academic year – an all-time high. The division continues to work closely with the ICU on a regular basis to provide continuous veno-venous hemodiafiltration for our sickest patients.
The section was one of 32 in the country to join the prestigious SCOPE (Standardizing Care to Improve Outcomes for Pediatric ESRD) Collaborative. This collaborative is a quality initiative organized by the Children’s Hospital Association to develop improved methods and best practice guidelines for children on dialysis. The division continued with multiple research initiatives and productivity with papers and abstract presentations at national meetings. The division has multiple

IRB-approved research studies active at this time as well as a joint research collaborative with the Division of Urology.
Locally, the staff exhibited continued excellence in teaching. Dr. Silva won the prestigious McNeill Teaching Award for resident didactic lectures. Multiple staff members created webinars, and also lectured at Grand Rounds in Danbury. Dr. Mason was an invited lecturer for the UConn Group on Women in Medicine (GWIMS) event in early 2015. She also spearheaded the Connecticut Children’s Transition Advisory Group in late 2015. Both Drs. Mason and Dogra had an invited poster presentation at Connecticut Children’s Illuminations Quality and Safety Annual Conference in October 2016.
As we look forward to the upcoming year, we expect to increase volume as we expand services towards Danbury and Fairfield, CT, and Baystate Medical Center in Springfield, MA. We also will continue our extensive research portfolio and move from IRB-approved research to funded studies.
Publications
Rheault MN, Zhang L, Selewski DT, Kallash M, Tran CL, D’Alessandri-Silva C, et al. AKI in children hospitalized with nephrotic syndrome. Clin J Am Soc Nephrol. 2015 Dec 7; 10(12):2110-8. Epub 2015 Oct 8. doi:10.2215/ CJN.06620615.
Sadowski CE, Lovric S, Ashraf S, Pabst WL, Gee HY, Kohl S, Silva C, et al. A single-gene cause in 29.5% of cases of steroid-resistant nephrotic syndrome. J Am Soc Nephrol. 2015 Jun;26(6):1279-89. doi: 10.1681/ASN.2014050489.
Band ME, Sheldon C, Brancato J, Parikh N, D’AlessandriSilva CJ. A 17-year-old with steroid resistant nephrotic syndrome. Pediatrics. 2016;137(5):e20153205.
Band ME, D’Alessandri-Silva C. Pediatrics: the forgotten stepchild of nephrology. Physician Assistant Clinics. 2016 Jan;1(1):175–85.
D’Alessandri-Silva C, Dorsey K. Week 38: enuresis. In: Yale primary care pediatrics curriculum. 6th ed. 2016.
Dogra S, Kaskel F. Steroid-resistant nephrotic syndrome: a persistent challenge for pediatric nephrology. Pediatr Nephrol. 2016. doi:10.1007/s00467-016-3459-5.
Staff
Cynthia D’Alessandri-Silva, MD, FAAP, Division Head
Sherene Mason, MD, FAAP, MBA
Bruce McDonald, MD, FAAP
Samriti Dogra, MD
Molly Band, PA-C

We continue to expand and provide comprehensive medical services for pediatric neurology patients. We have been involved in several clinical trials for epilepsy, spinal muscular atrophy and Duchenne muscular dystrophy.
Our patients with epilepsy receive comprehensive care that may include ketogenic diet and evaluations for epilepsy surgery in collaboration of the Neurosurgery Division. Additionally, the Autism Research Program, which is funded by the Affinity Research Collaborative (ARC) grant, has enrolled a substantial number of subjects. Our faculty continues to present their work at numerous national and international conferences.
Dr. Richard Young has received the Medal of Merit from the State of Connecticut Military Department as well as the Legion of Merit from the U.S. Army. Dr. Francis DiMario was presented with a Certificate of Appreciation by the Child Neurology Society.
The Pediatric Neurology Division welcomed Dr. Christine Matarese in January 2015, Dr. William Graf in May 2016, and Elizabeth Equi, APRN, in December 2016. Additionally, Dr. Cruz-Zeno transitioned from the Department of Developmental Pediatrics to Neurology in October 2016.
Since arriving at Connecticut Children’s, Dr. Mark Schomer has helped to establish a multi-institutional EEG database with collaborators at Boston Children’s Hospital and Columbia Medical Center with the goal of finding factors that may help in predicting outcomes following seizures in the neonatal period.
Dr. Louisa Kalsner (principal investigator) and Dr. Gyula Acsadi (co-investigator) are in a collaborative research program on autism founded by the joint UConn and Jackson Laboratory ARC Program. Dr. DiMario conducts a multicenter clinical study on tuberous sclerosis. Dr. Acsadi has collaborated with Sylvia Õunpuu and Dr. Kristan Pierz of the Center of Motion
Analysis to evaluate the gait patterns of CMT patients. Dr. Acsadi participates in the Tone Management program that helps to treat patients with spasticity as well as an adult neuromuscular fellowship with UConn and Hospital for Special Care. Dr. Jennifer Madan Cohen has collaborated with Neurosurgery and Hartford Hospital’s adult epilepsy program to evaluate patients with intractable focal epilepsy for epilepsy surgery.
Affinity Research Collaborative (ARC); the Institute for Systems Genomics at the University of Connecticut. Co-principal Investigator; Neural synaptic and circuit dysfunction in the autism spectrum disorders. $250,000 over 5 years. (Currently in year 3.)
Educational grant: from the Children’s Tumor Foundation ($6,000) to Dr. DiMario.
Koziol-Dube K, Burke G, DiMario FJ. Self-regulated learning of child neurology for medical students. Conn Med. 2016; 80(10):581-4.
DiMario FJ. [commentary] Schmidt et al. Breath-holding spells occur disproportionately more often in children with transient erythroblastopenia. Acta Paediatrica. 2016: 105(9):1088-93.
Miller G, Graf WD. Privacy, propriety, and the United States television media: “Watch this man die, and now we are going to sell you some detergent.” Am J Bioeth. 2016 Nov; 16(11):56-7.
Kim J, Liao YH, Ionita C, Bale AE, Darras B, Acsadi G. Mitochondrial membrane protein-associated neurodegeneration mimicking juvenile amyotrophic lateral sclerosis. Pediatr Neurol. 2016 Aug 24. Epub ahead of print.
Acsadi G. [editorial] Pediatric neurology in the era of genomics. Pediatr Clin North Am. 2015 Jun; 62(3).
Jani-Acsadi A, Õunpuu S, Pierz K, Acsadi G. Pediatric Charcot-Marie-Tooth disease. Pediatr Clin North Am. 2015 Jun; 62(3):767-86.
Viollet L, Glusman G, Murphy KJ, Newcomb TM, Reyna SP, Sweney M, Nelson B, Andermann F, Andermann E, Acsadi G, et al. Alternating hemiplegia of childhood: retrospective genetic study and genotype-phenotype correlations in 187 subjects from the US AHCF Registry. PLoS One. 2015 May 21; 10(5):e0127045.
DiMario FJ. [commentary] Williams J, Cain N. Case report of successful treatment of pallid breath-holding spells with glycopyrrolate. Pediatrics. 2015; 135(5):e1308-11. doi:10.1542/ peds.2014-2456. Yearbook Pediatrics 2015.
DiMario FJ Jr. Non-epileptic paroxysmal events of childhood. Pediatr Ther. 2015; 5(2):54.
DiMario FJ, Sahin M, Fakhari DE. Tuberous sclerosis complex. Pediatric Clin North Am. 2015; 62(3):633-48.
Roy B, DiMario FJ Jr. A case of refractory epilepsy; neuronal migration disorders. Ann Pediatr Child Health. 2015; 3(9):1091-4.
Kalsner L, Chamberlain S. Prader Willi, Angelman and 15q11-q13 Duplication Syndromes. Pediatr Clin North Am. 2015; 62(3):587-606.
Chapters
DiMario FJ. Tuberous sclerosis complex. In: Epocrates. London: BMJ. Revision and update, 2015 Jul.
Young RSK. Meningoencephalitis. In: McInerny T, Adam HM, Campbell DE, Foy JM, Kamat DM, DeWitt TG, editors. AAP textbook of pediatric care, 2nd ed. Elk Grove Village, IL: American Academy of Pediatrics; 2016.
Staff
Gyula Acsadi, MD
Division Head
Francis J. DiMario, Jr., MD
William Graf, MD
Louisa Kalsner, MD
Jennifer Madan-Cohen, MD
Christine Matarese, DO
Mark Schomer, MD
Richard Young, MD
Edwin Zalneraitis, MD
Edwin Cruz-Zeno, MD
Elizabeth Equi, APRN
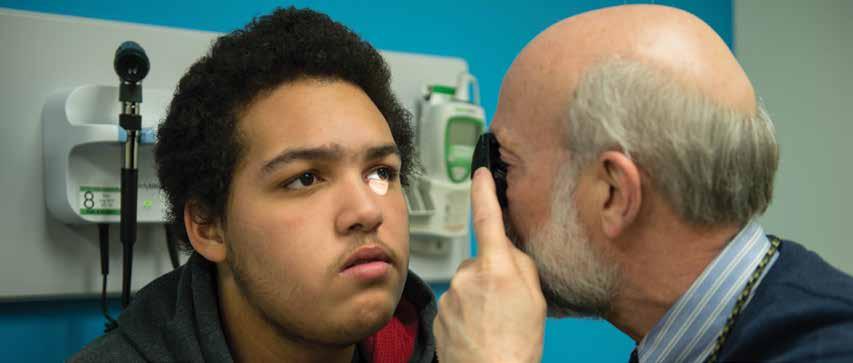
Our Pediatric Neurosurgery program has continued to consolidate its role as the leader in pediatric neurosurgical care in Western New England with expansion of services into Western Massachusetts.
Through a new partnership with Baystate Children’s Hospital in Springfield, MA, our program provides direct services to the children of Western Massachusetts. The program currently provides outpatient consultations and a defined scope of surgical services in Springfield, with aims to expand services over the next three to five years.
Our program in Hartford continues to provide comprehensive pediatric neurosurgical services for all ages. Through partnerships with Pediatric Oncology, Orthopaedics, Craniofacial Surgery, Otolaryngology, and Neuro-interventional Radiology, we provide unparalleled care for the children of Connecticut and Western Massachusetts. This includes minimally invasive approaches for the management of craniosynostosis, hydrocephalus, intracranial tumors, and anterior skull base disease. Our surgical epilepsy program has experienced continued growth, with plans for expansion of our inpatient epilepsy monitoring unit and the addition of a 3T MRI in the coming fiscal year.
Dr. Markus Bookland has rapidly established his lab at the University of Connecticut, securing $50,000 in private funding over the past year. His novel work with Dr. Min TangSchomer investigating pediatric malignant glioma cell lines and 3D silk scaffold tumor culture models has demonstrated promising preliminary results.
Publications
Brockmeyer DL, Oakes WJ, Rozzelle C, Johnston J, Rocque BG, Anderson RCE, Feldstein N, Martin J, Tuite GF, Rodriguez L, Wetjen N, Aldana P, Pincus D, Storm P, Proctor MR, Lew S. Chiari malformation Type 1 and atlantoaxial instability: a letter from the Pediatric Craniocervical Society. J Neurosurg Spine. 2015;17.
Linkov G, Kanev P, Isaacson G. Conservative management of typical pediatric postauricular dermoid cysts. Int J Pediatr Otorhinolaryngol. 2015;79(11):1810-13. Epub 2015 Aug 13.
Linov G, Kanev P, Isaacson G. Surgical management of temporal bone dermoid cysts. American Society of Pediatric Otolaryngology. 2015 May.
Weinerman B, Finck C, Kanev P. Epidermal cyst presenting in setting of prior myelomingocele: a pediatric case report. CTACSPA Annual, October 28, 2016.
Kellerman K, Stoltz N, Bookland M. Decreasing lumbosacral infection rates. 5th Annual Illuminations Quality and Patient Safety Conference; 2016 Oct; Hartford, CT.
Staff
Jonathan Martin, MD Division Head
Markus Bookland, MD
Paul Kanev, MD
Affiliated Faculty
Eileen Gillan, MD Neuro-oncology
Mark Lee, MD Orthopaedic Surgery
Charles Castiglione, MD Craniofacial Surgery
Belachew Tessema, MD
Otolaryngology/Endonasal Sinus Surgery
Katie Kellerman, PA-C Petronella Stolz, APRN, DNP
Marty Ollenschleger, MD Neurointerventional Radiology
Jennifer Madan-Cohen, MD Epilepsy/Neurology
The Orthopaedic Division continues to grow both clinically and academically. An all-star team ranging from surgeons to sports trainers to engineers provides quality care for the full spectrum of orthopaedic conditions to improve the quality of health for members of our community.
The Orthopaedic Division consists of three services: the pediatric orthopaedic service, a sports medicine service (Elite Sports Medicine), and the Center for Motion Analysis (CMA). The pediatric orthopaedic service has six fellowship-trained pediatric orthopaedic surgeons, one advanced-practice registered nurse, and two physician’s assistants. Together, our services provide the full spectrum of care for children and young adults with orthopaedic conditions such as scoliosis and spinal deformities, limb deformity, congenital dislocated hips, clubfeet, congenital hand deformities, children’s fractures, sports injuries, as well as neuromuscular conditions such as cerebral palsy, spina bifida and muscle diseases.
Orthopaedic Surgery residents are taken through a core curriculum of pediatric orthopaedic topics to supplement their clinical and surgical experience. An ACGME-accredited pediatric orthopaedic fellowship helps train the next generation of subspecialists. Journal clubs for the entire clinical staff keep the team up to date on the latest literature and promote a cohesive environment for the care team. Departmental and interdisciplinary conferences with radiology and neurosurgery promote multi-specialty collaboration. Dr. Kristan Pierz serves as editor of the POSNA Resident Review, and Dr. Matthew Milewski co-chairs the educational committee for the Pediatric Research in Sports Medicine (PRiSM) group.
The sports medicine service (Elite Sports Medicine) continues to grow under the guidance of four physicians, three physician’s assistants, three athletic trainers, and, in partnership with UConn, Dr. Carl Nissen oversees three sports medicine fellows. This group provides outstanding care for young athletes with injuries and oversees impressive sports injury prevention and concussion programs. Additionally, Dr. Milewski has joined Dr. Nissen on the executive board of the Research in Osteochondritis of the Knee (ROCK) group. They remain active in many leadership roles in groups including PRiSM, POSNA (Pediatric Orthopaedic Society of North America), Connecticut State Medical Society, New England Shoulder
and Elbow Society, CT Concussion Task Force, and AOSSM (American Orthopaedic Society for Sports Medicine).
The Center for Motion Analysis continues to expand its scope of practice, both clinically and in the area of research. Research in the CMA currently includes multiple collaborations such as outcomes for patients with cerebral palsy with the Functional Assessment Research Group with six other children’s hospitals, research on concussion with Children’s Hospital of Los Angeles and University of Oregon, and in pain management in young adult females with Cincinnati Children’s Hospital. Funded research also includes analysis of orthopaedic surgical outcomes using motion analysis techniques in patients with Charcot-Marie-Tooth and recurrent clubfoot deformity as well as evaluation of return-to-sport decision-making following ACL reconstruction.
Our research program, under the direction of Matthew Solomito, has been increasingly busy. Our three services have 47 active IRB studies underway with over 30 additional projects in progress. Collaboration in multicenter studies gives us access to the latest protocols for difficult diseases. Grants from Major League Baseball, Centers for Disease Control, and POSNA help us provide evidence-based guidelines for topics such as ideal pitching mechanics and return-to-play after ACL reconstruction. The Scoliosis Research Society has provided a two-year grant to study motion and quality of life following spinal fusion. Summer research programs educate college and medical students on the scientific process.
The Orthopaedics Division continues to benefit from generous fundraising, and this year’s Storybook Gala raised money to purchase a state-of-the-art low-dose X-ray system (EOS).
Publications
Acsadi AJ, Õunpuu S, Pierz K, Acsadi G. Pediatric CharcotMarie-Tooth Disease. Pediatr Clin North Am. 2015;62(3):4.
Brooks TM, Friedman LM, Silvis RM, Lerer T, Milewski MD. Are labs and imaging indicated in pediatric patients who present to the Emergency Department with back pain? Pediatr Emerg Care. 2015. Epub 2016.
Chaudhry S, Kang K, Lee MC. Reinforcing a spica cast with a fiberglass bar. Am J Orthop. Epub 2015 Nov;44(11):E423-6.
Chaudhry S. Pediatric posterior sternoclavicular joint injuries. J Am Acad Orthop Surg. 2015 Aug.
Heyworth B, Edmonds E, Minider K, Nissen C, et al. Variations in surgical treatment of knee osteochondritis dissecans among high volume OCD surgeons. Orthop J Sports Med. 2015 Aug; 3(7):2.
Kostyun R, Milewski MD, Hafeez I. Sleep disturbance and neurocognitive function during the recovery of sportsrelated concussions in adolescents. Am J Sports Med. 2015 Mar; 43(3):633-40.
Lee MC. To culture or not to culture. [commentary on]. Section J. Microbiological culture methods for pediatric musculoskeletal infection. A guideline for optimal use. J Bone Joint Surg Am. 2015 Mar 18;97(6): e32.
Manworren R, Pantaleao A, Bradshaw R, Lee M, Thomson J, Rader C, Misra M, Weiss R, Tsai A, Ruano G. Predicted pain in pediatric surgical procedures. J Pain. 2015 Apr; 16(4):S15.
Milewski MD, Booker JL. Tibial spine avulsion fractures: a focus on arthroscopic treatment and rehabilitation. Conn Med. 2015 March; 79(3):139-48.
Nissen CW. Anterior cruciate injuries in adolescent athletes. Conn Med. 2015 Mar; 79(3):149-153.
Nissen CW. Appropriate use criteria for the management of osteochondritis dissecans of the femoral condyle. Am Acad Orthop Surg. 2015 Dec 4.
O’Malley MP, Milewski MD, Solomito MS, Erwteman AS, Nissen CW. The association of tibial slope and anterior cruciate ligament rupture in skeletally immature patients. Arthroscopy. 2015; 31(1):77-82.
Õunpuu S, George G, Bagley A, Sison-Williamson M, Hassani S, Johnson B, et al. Variations in kinematic and spatiotemporal gait parameters by Gross Motor Function Classification System level in children and adolescents with cerebral palsy. Dev Med Child Neurol. 2015 Oct; 57(10):955-62.
Õunpuu S, Solomito MJ, Bell K, Deluca P, Pierz K. Longterm outcomes after multilevel surgery including rectus femoris, hamstring, and gastrocnemius procedures in children with cerebral palsy. Gait Posture. 2015 Sept; 42(3):365-72.
Rethlefsen SA, Nguyen DT, Wren TA, Milewski MD, Kay RM. Knee pain and patellofemoral symptoms in patients with cerebral palsy. J Pediatr Orthop. 2015 Jul-Aug; 35(5):519-22.
Solomito MJ, Garibay EJ, Woods JR, Õunpuu S, Nissen CW. Lateral trunk lean in pitchers affects both ball velocity and upper extremity joint moments. Am J Sports Med. 2015; 43(5):1235-40.
Solomito MJ. Lagrangian approach to modeling the biodynamics of the upper extremity: applications to collegiate baseball pitching. [doctoral dissertation] DigitalCommons@ UConn; 2015 Dec 16; 995.
Wall E, Polousky JD, Shea KG, Carey JL, Ganley TJ, Grimm NL, Jacobs JC, Edmonds EW, Eismann EA, Aderson A, Heyworth B, Lyon R, ROCK Study Group. Novel radiographic feature classification of knee OCD – a multicenter reliability study. Am J Sports Med. 2015; 43(2):303.
Nissen CW. [guest editor] Special issue: Sports Medicine –Conn Med. 2015 Mar; 79(3).
Pierz KA. CORR Insights(®): does exercise influence pediatric bone? A systematic review. Clin Orthop Relat Res. 2015 Nov.
Hyman JE, Trupia EP, Wright ML, Matsumoto H, Jo CH, Mulpuri K, Joseph B, Kim HK, Mack PW; International Perthes Study Group Members. Interobserver and intraobserver reliability of the modified Waldenström classification system for staging of Legg-Calvé-Perthes disease. J Bone Joint Surg Am. 2015 Apr.
Acsadi AJ, Õunpuu S, Pierz K, Acsadi G. Pediatric Charcot-Marie-Tooth Disease. Pediatr Clin North Am. 2015; 62(3):767-86.
Õunpuu S, Solomito MJ, Bell K, DeLuca P, Pierz K. Longterm outcomes after multilevel surgery including rectus femoris, hamstring and gastrocnemius procedures in children with cerebral palsy. Gait Posture. 2015; 42(3):365-72.
Nieuwenhuys A, Õunpuu S, Campenhout AV, et al. Identification of joint patterns during gait in children with cerebral palsy: a Delphi consensus study. Dev Med Child Neurol. 2015; 58(3): 306-13.
Õunpuu S, Gorton G, Bagley A, et al. Variations in kinematic and spatiotemporal gait parameters by Gross Motor Function Classification System level in children and adolescents with cerebral palsy. Dev Med Child Neurol. 2015; 57(10):955-62.
Heyworth B, Edmonds E, Minider K, Nissen C, et al. Variations in surgical treatment of knee osteochondritis dissecans among high volume OCD surgeons. Orthop J Sports Med. 2015 Aug; 3(7):suppl 2.
Kostyun RO, Hafeez I. Protracted recovery from a concussion: a focus on gender and treatment interventions in an adolescent population. Sports Health. 2015; 7(1):52-7.
O’Malley M, Solomito MJ, Milewski MD. The association of tibial slope and ACL rupture in skeletally immature patients. Arthroscopy. 2015; 31(1):77-82.
Milewski MD, Booker JL. Tibilar spine avulsion fractures: a focus on arthroscopic treatment and rehabilitation. Conn Med. 2015; 79(3):139-48.
Wang DH, Kostyun RO, Solomito MJ. The biomechanics of cranial forces during figure skating spinning elements. Conn Med. 2015; 79(3):133-7.
Kostyun RO. Sleep disturbances in concussed athletes: a review of the literature. Conn Med. 2015; 73(9):161-5.
Feyissa EA, Cornell E, Chandhok L, Wang D, Ionita C, Schwab J, Kostyun R, et al. Impact of co-management at the primarysubspecialty care interface on follow-up and referral patterns for patients with concussion. Clin Pediatr. 2015; 54(10):969-75.
Golan EJ, Thomson JD. When in doubt, examine the patient. [commentary] Baldwin KD, et al. Predictive factors for differentiating between septic arthritis and Lyme disease of the knee in children. J Bone Joint Surg Am. 2016 May.
LaPrade R, Agel J, Baker J, Brenner J, Cordasco F, Côté J, Engebretsen L, Feeley B, Gould D, Hainline B, Hewett T, Jay-
anthi N, Kocher M, Myer G, Nissen C, Philippon M, Provencher M. AOSSM Early sport specialization consensus statement. Orthop J Sports Med. 2016; 4(4).
Nieuwenhuys A, Õunpuu S, Campenhout AV, et al. Identification of joint patterns during gait in children with cerebral palsy: a Delphi consensus study. Dev Med Child Neurol. 2016 Mar; 58(3):306-13.
Carey J, Wall E, Grimm NL, Ganley TJ, Edmonds EW, et al., (Nissen C, 9/17). Novel arthroscopic classification of osteochondritis dissecans of the knee: a multicenter reliability study. AJSM. 2016; 44(7):1694-8.
Brooks TM, Friedman LM, Silvis RM, Milewski MD. Back pain in a pediatric emergency department: etiology and evaluation. Pediatr Emerg Care. 2016.
Solomito MJ, Ferreira JV, Nissen CW. Biomechanical differences between right- and left-handed pitchers. Sports Biomech. 2016 Jun 2:1-9.
Little RM, Milewski MD. Physeal fractures about the knee. Curr Rev Musculoskelet Med. 2016 Dec; 9(4):478-86.
Nepple JJ, Milewski MD, Shea KG. Research in osteochondritis dissecans of the knee: 2016 update. J Knee Surg. 2016; 29(7):533-8.
Shea KG, Styhl AC, Jacobs JC, Ganley TJ, Milewski MD, et al. The relationship of femoral physis and medial patellofemoral ligament in children: a cadaveric study. AJSM. 2016 Nov; 44(11):2833-7.
Chapters
Cruz AI, Milewski MD. Patellofemoral instability and other common knee issues in the skeletally immature athlete. In: Orthopaedic knowledge update (OKU) 5: sports medicine. Rosemont, IL: American Academy of Orthopaedic Surgeons (AAOS); 2015.
Milewski MD, Tompkins M, Ganley TJ, Shea KG. Osteochondritis dissecans of the knee. In: Orthopaedic knowledge update (OKU) 5: pediatrics. Rosemont, IL: American Academy of Orthopaedic Surgeons (AAOS). 2016.
Kostyun R, Nissen CW, Hafeez I. Special considerations in head injuries in adolescent athletes. In: Miller M, editor. Orthopaedic knowledge update (OKU) 5: sports medicine. Rosemont, IL: American Academy of Orthopaedic Surgeons (AAOS). 2015.
Socci A, Cruz AI, Little R, Milewski MD. Lower extremity and foot disorders. In: Orthopaedic knowledge update (OKU) 12: pediatrics. Rosemont, IL: American Academy of Orthopaedic Surgeons (AAOS). Pending publication in 2017.
Milewski MD. [two entries] Adolescent athlete, and Pediatric lower extremity trauma. In: Pocket orthopaedic surgery. Philadelphia, PA: Wolters Kluwer. 2015.
Thomson JD. [contributor] Spina bifida. In: Alexander M, Matthews D, editors. Pediatric rehabilitation, principles and practice. 5th ed. Demos Medical; 2015.
Õunpuu S, Pierz K. Hereditary motor sensory neuropathy: understanding function using motion analysis. In: Handbook of human motion. Miller F, editor. 2016.
Staff
Jeffrey D. Thomson, MD
Division Head
Sonia Chaudhry, MD
Imran Hafeez, MD
Mark C. Lee, MD
Philip W. Mack, MD
Matthew D. Milewski, MD
Carl W. Nissen, MD
Kristan Pierz, MD
David Wang, MD
Janet Zahradnik, MD
Amy Shannon, APRN
Bruce E. Bowman, PA-C, DFAAPA
Nicole Cottle, PA-C
Sylvia Õunpuu, MSc
Marta Jablonski, PA-C
Kevin Fitzsimmons, PA-C
A.J. Ricciuti, PA-C

Since the founding of the Division of Otolaryngology – Head and Neck Surgery in 1999, we have continued our impressive growth trajectory. In the last fiscal year, Connecticut Children’s Specialty Group division otolaryngologists performed 2,179 surgeries and logged 14,491 outpatient visits.
Clinically, our scope of practice has expanded with some new and exciting procedures. First, in the evaluation of pediatric obstructive sleep apnea in complex patients, Valerie Côté, MD, has introduced sleep endoscopy evaluation in the operating room. This diagnostic step enables the clinician to identify multiple potential sites of obstruction to tailor treatment options and appropriately counsel families. Second, Christopher Grindle, MD, and Scott Schoem, MD, have started performing totally implantable bone-anchored hearing devices. Families now have the option of choosing the standard system called the Baha Connect, or the newer, totally implantable system known as Baha Attract.
Specialty clinics have become much more popular for families to obtain comprehensive care for their children. Our voice, swallowing and cochlear implant clinics have thrived and increased their capacity to meet the growing demand. Our newest and perhaps most exciting clinical initiative this year is the development of a comprehensive aerodigestive team to treat laryngotracheal, pulmonary and gastrointestinal disorders. Although we have been already providing this service in a limited fashion, establishing a formal aerodigestive team allows for the space, equipment and resources to provide best-in-class comprehensive care. The Director of the Connecticut Children’s Airway Team (CCAT) is Nicole Murray, MD. The team includes Otolaryngology – Head and Neck Surgery, Pulmonary Medicine, Gastroenterology, and Speech Language Pathology.
Educationally, Katherine Kavanagh, MD, has increased our collaboration with the Division of Anesthesiology in resident education using medical simulation technology. Use of 3D imaging technology has rapidly changed our medical simulation capability and enhanced our ability to provide advanced, measurable instruction for trainees. On the cutting edge of this emerging technology, Tulio Valdez, MD, MSc, and his lab team are developing new 3D teaching models for airway, cleft lip, cleft palate, and ear medical simulation. His collaborators are Drs. Kavanagh, Côté, and Grindle.
On the research side, Dr. Valdez has transformed our division’s research program by developing a photonics and imaging laboratory. The center is a collaboration between the Massachusetts Institute of Technology and Connecticut Children’s Medical Center, and it focuses on the study of middle ear pathology using spectroscopic modalities and new generation imaging techniques. Dr. Valdez and his team have received $100,000 in funding through an MIT consortium grant. Moreover, Drs. Côté, Kavanagh and Valdez, and research assistant Jose Arbouin won the first place award for best poster presentation at the American Society of Pediatric Otolaryngology in Chicago in May 2016. Their award-winning poster was titled “3D Printed Haptic Simulation Model for the Surgical Repair of Incomplete Cleft Palate.”
Humanitarian missions demonstrate a desire to improve global health and bring our expertise to underserved areas. Both Drs. Côté and Schoem participate in otolaryngology mission work. This year Dr. Côté traveled to Ecuador to perform cleft lip and palate surgery through the Global Smile Foundation. Dr. Schoem performed complex ear surgery in Nicaragua through Mayflower Medical Outreach.
Publications
Côté V, Liang C, Perkins J, Ruiz A, Sillau S, Friedman NR. Characteristics of children under 2 years of age undergoing tonsillectomy for sleep-disordered breathing or obstructive sleep apnea. Int J Pediatr Otorhinolaryngol. 2015;79(6):903-8.
Côté V, Kus LH, Zhang X, Richardson K, Nguyen LHP. Advanced airway management teaching in otolaryngology residency: a survey of residents. Ear Nose Throat J. 2015 AprMay;94(4-5):187-92.
Valdez TA, Marvin K, Bennett NJ, Lerer T, Nolder AR, Buchinsky FJ. Current trends in perioperative antibiotic use: a survey of otolaryngologists. Otolaryngol Head Neck Surg. 2015 Jan;152(1):63-6. doi: 10.1177/0194599814554551. Epub 2014 Oct 10. PMID: 25305267.
Valdez TA, Spegazzini N, Pandey R, Longo K, Grindle C, Peterson D, Barman I. Multi-color reflectance imaging of middle ear pathology in vivo. Anal Bioanal Chem. 2015
May;407(12):3277-83. doi: 10.1007/s00216-015-8580-y.
Epub 2015 Mar 10. PMID: 25753015.
Ruiz JN, Belum VR, Boers-Doets CB, Kamboj M, Babady NE, Tang YW, Valdez TA, Lacouture ME. Nasal vestibulitis due to targeted therapies in cancer patients. Support Care Cancer. 2015 Jan 22. Epub ahead of print. PMID: 25876156.
Wang X, Valdez TA, Bi J. Detecting tympanostomy tubes from otoscopic images via offline and online training. Comput Biol Med. 2015 Jun 1;61:107-18. doi: 10.1016/j.compbiomed.2015.03.025. Epub 2015 Apr 4. PMID: 25889718.
Pandey R, Paidi SK, Kang JW, Spegazzini N, Dasari RR, Valdez TA, Barman I. Discerning the differential molecular pathology of proliferative middle ear lesions using Raman spectroscopy. Sci Rep. 2015 Aug 20;5:13305. doi: 10.1038/ srep13305.
O’Reilly RC, Soundar S, Tonb D, Bolling L, Yoo E, Nadal T, Grindle C, Field E, He Z. The role of gastric pepsin in the inflammatory cascade of pediatric otitis media. JAMA Otolaryngol Head Neck Surg. 2015 Apr;141(4):350-7. doi: 10.1001/ jamaoto.2014.3581. PMID: 25633964.
Books
Valdez TA, Vallejo J, editors. Infectious diseases in pediatric otolaryngology – a practical guide. Springer; 2015.
Chapters
Côté V, Bocchini C. Infected congenital neck lesions. In: Valdez TA, Vallejo J, editors. Infectious diseases in pediatric otolaryngology – a practical guide. Springer; 2015.
Schoem SR, Bennett N, Johnson K. Complications of otitis media. In: Valdez TA, Vallejo J, editors. Infectious diseases in pediatric otolaryngology – a practical guide. Springer, 2015.
Schoem SR. Neonatal nasal obstruction. In: Lioy J, Sobol SE, editors. Disorders of the neonatal airway: fundamentals for practice. Springer; 2015.
Grindle CR. Diagnosis of Otitis media. In: Preciado D, editor. Otitis media: state of the art concepts and treatment. Springer; 2015.
Staff
Scott Schoem, MD Division Head
Valerie Côté, MD, FRCSC
Christopher Grindle, MD
Katie Kavanagh, MD
Nicole Murray-Posner, MD
Tulio Valdez, MD
Rebecca Strong, APRN
Meaghan Krajewski, APRN
Christine Harrington, PA-C
Our mission is to utilize our multidisciplinary expertise to alleviate pain and stress in children afflicted with acute, chronic or terminal illness.
Highlighting our year has been the addition of new faculty members Eapen Mathew, MD, and Emily Wakefield, PsyD. After completing his anesthesia residency at UConn, Dr. Mathew spent the last two years at Cincinnati Children’s where he completed fellowships in Pediatric Anesthesia and Pediatric and Adult Pain Medicine. He joined the division part-time. A former research assistant in the division, Dr. Wakefield completed her PsyD at University of Hartford and then went on to do a Pediatric Psychology internship at SUNY Upstate Medical Center, and then completed her Postdoctoral Fellowship on the Consultative Liaison Service at Connecticut Children’s.
Other important highlights and milestones for the division for 2015 and 2016 included:
Kalyani Raghavan, MD, received a grant from the Autism Speaks Foundation entitled “Online modules to train medical staff in best practices for kids with ASD during medical procedures”
William T. Zempsky, MD, PMH, was appointed to the Senior Appointments and Promotions Committee at the University of Connecticut School of Medicine
Dr. Zempsky was elected as Chair of the Pediatric Special Interest Group of the American Pain Society
Dr. Zempsky was appointed to the State of Connecticut Medical Marijuana Board
New Grants
BAA-N01DA-15-4422 RFP – University of Connecticut (UConn) Center for the Advancement of Managing Pain (CAMP) NIH Center of Excellence in Pain Education (CoEPE). Site PI: Dr. William Zempsky. Co-Investigator: Dr. Ana Verissimo.
R01HD086978-01A1 – NIH/NICHD iCanCope with sickle cell disease. Co-Investigator: Dr. William Zempsky.
Donaghue Foundation Making Research Relevant and Ready: Seed greater understanding of sickle cell disease. PI: Dr. William Zempsky.
Autism Speaks Foundation: Online modules to train medical staff in best practices for kids with ASD during medical procedures. PI: Dr. Kalyani Raghavan.
Publications
Santos M, Murtaugh T, Pantaleao A, Zempsky WT, Guite JW. Chronic pain and obesity within a pediatric interdisciplinary pain clinic setting: a preliminary examination of current relationships and future directions. Clin J Pain. 2016 Nov 10. Epub ahead of print.
Tran ST, Guite JW, Pantaleao A, Pfeiffer M, Myer GD, Sil S, Thomas SM, Ting TV, Williams SE, Edelheit B, Õunpuu S, Rodriguez-MacClintic J, Zemel L, Zempsky W, Kashikar-Zuck S. Preliminary outcomes of a cross-site cognitive-behavioral and neuromuscular integrative training intervention for juvenile fibromyalgia. Arthritis Care Res (Hoboken). 2016 Jun 22. Epub ahead of print.
Zempsky WT, Wakefield EO, Santanelli JP, New T, Smith-Whitley K, Casella JF, Palermo TM. Widespread pain among youth with sickle cell disease hospitalized with vasoocclusive pain: a different clinical phenotype? Clin J Pain. 2016 Jun 17. Epub ahead of print.
Xiao L, Andemariam B, Taxel P, Adams DJ, Zempsky WT, Dorcelus V, Hurley MM. Loss of bone in sickle cell trait and sickle cell disease female mice is associated with reduced IGF-1 in bone and serum. Endocrinology. 2016 Aug; 157(8):3036-46.
Schmitz ML, Zempsky WT, Meyer JM. Safety and efficacy of a needle-free powder lidocaine delivery system in pediatric patients undergoing venipuncture or peripheral venous cannulation: randomized double-blind COMFORT-004 trial. Clin Ther. 2015 Aug; 37(8):1761-72.
Zempsky WT, Schmitz ML, Meyer JM. Safety and efficacy of needle-free powder lidocaine delivery system
in adult patients undergoing venipuncture or peripheral venous cannulation: a randomized, double-blind, placebocontrolled trial. Clin J Pain. 2016 Mar; 32(3):211-7.
Manworren RC, Jeffries L, Pantaleao A, Seip R, Zempsky WT, Ruaño G. Pharmacogenetic testing for analgesic adverse effects: pediatric case series. Clin J Pain. 2016 Feb; 32(2):109-15.
Manworren RC, McElligott CD, Deraska PV, Santanelli J, Blair S, Ruscher KA, Weiss R, Rader C, Finck C, Bourque M, Campbell B. Efficacy of analgesic treatments to manage children’s postoperative pain after laparoscopic appendectomy: retrospective medical record review. AORN J. 2016 Mar; 103(3):317.e1-11.
Chou R, Gordon DB, de Leon-Casasola OA, Rosenberg JM, Bickler S, Brennan T, Carter T, Cassidy CL, Chittenden EH, Degenhardt E, Griffith S, Manworren R, McCarberg B, Montgomery R, Murphy J, Perkal MF, Suresh S, Sluka K, Strassels S, Thirlby R, Viscusi E, Walco GA, Warner L, Weisman SJ, Wu CL. Management of postoperative pain: a clinical practice guideline from the American Pain Society, the American Society of Regional Anesthesia and Pain Medicine, and the American Society of Anesthesiologists’ Committee on Regional Anesthesia, Executive Committee, and Administrative Council. J Pain. 2016 Feb; 17(2):131-57. doi: 10.1016/j.jpain.2015.12.008.
Baumbauer KM, Young EE, Starkweather AR, Guite JW, Russell BS, Manworren RC. Managing chronic pain in special populations with emphasis on pediatric, geriatric, and drug abuser populations. Med Clin North Am. 2016 Jan; 100(1):183-97.
Manworren RC, Gilson AM. Nurses’ role in preventing prescription opioid diversion. Am J Nurs. 2015 Aug; 115(8):34-40.
Manworren RC, Ruaño G, Young E, St Marie B, McGrath JM. Translating the human genome to manage pediatric postoperative pain. J Pediatr Surg Nurs. 2015 Jan-Mar; 4(1):28-39.
Manworren RC. Multimodal pain management and the future of a personalized medicine approach to pain. AORN J. 2015 Mar; 101(3):308-14; quiz 315-8.
Manworren R, Girard E, Verissimo AM, Riccardino S, Ruscher KA, Weiss R, Hight D. Effectiveness of hypnosis for post-operative pain management of minimally invasive thorascopic approach to repair pectus excavatum: retrospective analysis. Pediatr Surg Nurs. 2015; 4.
Evans JR, Jastrowski Mano K, Guite JW, Weisman SJ, Hainsworth KR. Psychometric properties of the pain stages of change questionnaire: new insights on the measurement of readiness to change in adolescents, mothers, and fathers. J Pain. 2015 Jul; 16(7):645-56.
Staff
William T. Zempsky, MD, MPH Division Head
Len Comeau, MD
Eapen Mathew, MD
Kerry Moss, MD
Kalyani Raghavan, MD
Ana Verissimo, MD
Jessica Guite, PhD
Renee Manworren, PhD, APRN
Emily Wakefield, PsyD
Kim Kempner, APRN
In 2015 and 2016, the Department of Pathology and Laboratory Medicine continued its mission of providing the highest quality laboratory services through excellence, innovation, integrity and concern for quality care provided to patients.
Except for the retirement of Tom Ciesielski, MD, Director of the Autopsy Service, there were no physician or PhD staffing changes. Dr. Sarah Song assumed the role of Autopsy Service Director with Tom’s departure.
Although the majority of the members within the department provide services in Anatomic Pathology, there is a wide range of subspecialization within that division. The current MD/PhD staff in Anatomic Pathology have subspecialization in neuropathology (3), cytopathology (8), pediatric pathology (1), molecular pathology (1), and dermatopathology (1). Additional members within AP have specialty skills in organ systems for which there is no board certification. These include breast pathology, GI pathology, GU pathology, Gyn pathology, Pulmonary pathology, Head and Neck pathology, and soft tissue tumors. Additionally, there are six members of the department board certified in Hematopathology providing support in Hematology and Hematopathology. Two staff members provide support in Transfusion Medicine. One is board certified in Transfusion Medicine and the other has specialty expertise in Coagulation. There is one PhD board-certified member in each of the following disciplines: Microbiology, Chemistry, Molecular Pathology/Cytogenetics, and Immunopathology.
Local, regional and national trends in laboratory medicine are focused around laboratory consolidation within health care systems. Hospital labs partnering with commercial labs or selling their outreach programs to commercial labs is another trend. These are largely a response to the evolution of value-based health care with attempts to reduce costs and increase efficiencies. Fee-for-service outpatient laboratory reimbursement is expected to progressively decline with the value-based health care evolution.
Locally, we are experiencing this trend with the sale of Clinical Laboratory Partners (CLP) to Quest Diagnostics. With the health care system in need of capital and prospects of declining value for CLP through declining revenues with decreased utilization of laboratory services, now was the time for such a sale.
Another trend in laboratory medicine is the increasing application of molecular testing especially in the diagnosis and selection of therapy in neoplastic diseases.
Equipment for Next Generation Sequencing (NGS) was obtained in Molecular Diagnostics and is under development for applications in the Cancer Program.
The department’s 12 residencies in anatomic pathology and five fellowship positions continue to be filled with highly qualified individuals. Graduates of our educational program have continued to be successful in obtaining highly desirable fellowships on completion of their residency training program in Pathology at Hartford Hospital or have gone on to find attractive positions in the clinical practice of Pathology. The residency program continues as a Hartford Hospital-only program that is not integrated with the University of Connecticut. The program does rely on the university, however, for training residents in renal pathology and electromicroscopy. Now that the department has recruited a dermatopathologist, the program no longer relies on training in Dermatopathology at the university.
Publications
Agaronov M, Ratkiewicz I, Lawlor M, Cartun RW, Aslanzadeh J, Fiel-Gan M. Cokeromyces recurvatus identified in lung biopsy: case report of a non-pathogenic fungus highlighting its potential histologic mimics. Ann Clin Lab Sci. 2015 Mar; 45(2):209-14. PMID: 25887878.
Vrotsos E, Gorgan M, DiGiuseppe JA. Detection of small abnormal B-lymphoblast populations at diagnosis of chronic myelogenous leukemia, BCR-ABL1+: Incidence, phenotypic features, and clinical implications. Cytometry B Clin Cytom. 2015. doi: 10.1002/cyto.b.21250.
DiGiuseppe JA, Tadmor MD, Pe’er D. Detection of minimal residual disease in B lymphoblastic leukemia using viSNE. Cytometry B Clin Cytom. 2015; 88B:294-304.
Vrotsos E, Gillan E, Mnayer L, DiGiuseppe JA. Myeloid blast phase of chronic myelogenous leukemia, BCR-ABL1+, associated with a secondary translocation involving MLL. Case report and review of the literature. J Hematopathol. 2015. doi: 10.1007/s12308-015-0246-3.
Doss M, Araneta R 3rd, Fiel-Gan M, Edelheit B. Cranial nerve BI palsy as an initial presentation of necrotizing sarcoid granulomatosis in a 14-year-old female: case report and literature review. Semin Arthritis Rheum. 2015 Reb; 44(4); 450-60. doi:10.1016/j.semarthrit. 2014.07.004. Epub 2014 July 17. PMID: 25130755.
Lewis S, Aljarallah B, Trivedi A, Thung SN. Magnetic resonance imaging of a small vessel hepatic hemangioma in a cirrhotic patient with histopathologic correlation. Clin Imaging. 2015.
Marti J, Trivedi A, D’Alessandro V, Roayaie S, Rosen A, et al. Calcified telangiectatic hyperplastic nodule associated with vascular malformation in a child: a case report. Fetal Pediatr Pathol. 2015 Apr; 34(2):108-16. doi:10.3109/15513815.2 014.970264.
Roy B, Uphoff DF, Silverman IE. Rheumatoid meningitis presenting with multiple stroke-like episodes. JAMA Neurol. 2015 Sep 1; 72(9):1073-6. doi: 10.1001/jamaneurol.2015.1105.
Ghazi IM, DP Nicolau, MD Nailor, J Aslanzadeh, J Ross, Kuti JL. Antibiotic utilization and opportunities for stewardship among hospitalized patients with influenza respiratory tract infection. Infect Cont Hosp Epidemol. 2016; 37(5):583-9.
DiGiuseppe JA, Tadmor MD, Pe’er D. Detection of minimal residual disease in B lymphoblastic leukemia using viSNE. Cytometry B Clin Cytom. 2015; 88B:294-304.
Vrotsos E, Gorgan M, DiGiuseppe JA. Detection of small abnormal B-lymphoblast populations at diagnosis of chronic myelogenous leukemia, BCR-ABL1+: incidence, phenotypic features, and clinical implications. Cytometry B Clin Cytom. Epub 2015 Jul 3. doi: 10.1002/cyto.b.21250.
Vrotsos E, Gillan E, Mnayer L, DiGiuseppe JA. Myeloid blast phase of chronic myelogenous leukemia, BCR-ABL1+, associated with a secondary translocation involving MLL. Case report and review of the literature. J Hematopathol. 2016; 9:29-33.
Wang W, Cortes JE, Khoury JD, Wang S, DiGiuseppe JA, Bueso-Ramos CE, Chen Z, Kantarjian HM, Medeiros LJ, Hu
S. Risk stratification of additional chromosomal changes in chronic myelogenous leukemia in the era of tyrosine kinase inhibitors. Blood. 2016; 127:2742-50.
Mar N, DiGiuseppe JA, Dailey ME. Rubenstein-Taybi syndrome – a window into follicular lymphoma biology. Leuk Lymphoma. Epub: 2016 Apr 18. http://dx.doi.org/10.3109/ 10428194.2016.1165816.
Townsend M, Berke A, Elaba Z, Banki A, Murphy M. Recurrent CD4−/CD8− peripheral T-cell lymphoma with change in cytoarchitectural features and immunophenotype over the course of disease. J Cut Path. 2015 Dec; 1036–7.
Murphy MJ, Shahriari N, Payette M, Mnayer L, Elaba Z. Development of a curriculum in molecular diagnostics, genomics and personalized medicine for dermatology trainees. J Cutan Pathol. 2016 Jul 22. doi: 10.1111/cup.12760.
Huang T, Pope SJ, Volpe JP, Raj PS, Fiel-Gan MD. Pulmonary capillary hemangioma diagnosed by needle core biopsy: case report and review of the literature. Human Pathol. 2016. http://dx.doi.org/10.1016/j.ehpc.2016.09.004.
Ligato S, Valdes AY, Newcomb, P, Cartun R. Expression and utility of IMP3 in the differential diagnosis of atypical glandular cells and adenocarcinoma in liquid based cervical cytology. J Am Soc Cytopathol. 2016 Sep-Oct; 5(5):277-85. doi: http://dx.doi.org/10.1016/jasc.2016.02.002.
Gadara MR, Gonzalez M, Cartun RW, Ligato S. IMP3 immunoractivity is more sensitive than AMACR in detecting dysplastic epithelium and early adenocarcinoma in barret esophagus. Appl Immunohistochem Mol Morphol. 2016 Jan 13. Epub ahead of print.
Zhu Q, Ricci Jr A, Hegde P, et al. Assessment of functional differences in malignant and benign breast lesions and improvement of diagnostic accuracy by using US-guided diffuse optical tomography in conjunction with conventional US. Radiology. 2016: 1-11. PMID 26937708.
Symbol B, Ricci Jr A. Suggested management of breast sclerosing intraductal papilloma without atypia diagnosed on core biopsy: a semiquantitative approach. Mod Pathol. 2016; 29(1):Supp 74A.
Collins K, Ricci Jr A. Micropapillary mucinous breast carcinoma: an under-recognized variant. Mod Pathol. 2016; 29(1):Supp 37A.
Stretz C, Song X, Killory BD, Ollenschleger MD, Nouh AM. Rheumatoid meningitis: diagnostic and therapeutic observations. Conn Med. 2016 Mar; 80(3):163-6. PMID: 27169300.
Modak J, Song X, Finelli P, Prasad A. Herpes simplex encephalitis in an immunocompromised adult with novel MRI and pathology findings. Clin Neuroradiol. 2016 Aug 24. PubMed: 27557804.
J Marti, A Trivedi, A Rosen, R Arnon, SN Thung, M Schwartz. Idiopathic perinatal hepatic infarct as a cause of liver mass. Ann Pediatr Surg. 2016 Oct; 12(4):167-9.
Wang W, Cortes JE, Khoury JD, Wang S, DiGiuseppe JA, Bueso-Ramos CE, Chen Z, Kantarjian HM, Medeiros LJ, Hu S. Risk stratification of additional chromosomal changes in chronic myelogenous leukemia in the era of tyrosine kinase inhibitors. Blood. 2016 Jun 2; 127(22):2742-50.
Vrotsos E, Gorgan M, DiGiuseppe JA. Detection of small abnormal B-lymphoblast populations at diagnosis of chronic myelogenous leukemia, BCR-ABL1+: incidence, phenotypic features, and clinical implications. Cytometry B Clin Cytom. 2015. doi:10.1002/cyto.b.21250.
DiGiuseppe JA, Tadmor MD, Pe’er D. Detection of minimal residual disease in B lymphoblastic leukemia using viSNE. Cytometry B Clin Cytom. 2015; 88B:294-304.
Shapiro M, Ollenschleger MD, Baccin C, Becske T, Spiegel GR, Wang Y, Song X, Raz E, Zumofen D, Potts M, Nelson PK. Foreign body emboli following cerebrovascular interventions: clinical, radiographic, and histopathologic features. AJNR Am J Neuroradiol. 2015 Aug 20; 36(11):2121-6.
Lewis S, Aljarallah B, Trivedi A, Thung SN. Magnetic resonance imaging of a small vessel hepatic hemangioma in a cirrhotic patient with histopathologic correlation. Clin Imaging. 2015 Jul-Aug; 39(4):702-6.
Chapters
DiGiuseppe JA. Acute lymphoblastic leukemia/lymphoma: Diagnosis and minimal residual disease detection by flow cytometric immunophenotyping. In: Manual of molecular and clinical laboratory immunology. 8th ed. American Society for Microbiology; 2016. ISBN-13: 978-1555818715; p. 207-16.
Staff
William T.
Pastuszak, MD
Department Chief
Jaber Aslanzadeh, PhD
Margaret Assaad, MD
Fabiola Balarezo, MD
Richard Cartun, PhD
Joseph DiGiuseppe, MD, PhD
Jonathan Earle, MD
Zendee Elaba, MD
Mary Fiel-Gan, MD
Marilyn Kritzman, MD
Lisa Laird, MD
Saverio Ligato, MD
Bela Mandavilli, MD
Srinivas Mandavilli, MD
Richard Muller, MD
Laila Mnayer, MD
Nadia Nashid, MD
William Rezuke, MD
Andrew Ricci, MD
Donna Rose, MD
Peter Shen, MD
Bradford Sherburne, MD
Xianyuan Sarah Song, MD
Yanjun Su, MD
Anshu Trivedi, MD
Dean Uphoff, MD
Gregory Makowski, PhD
Terry Voytek, MD
In the years 2015 and 2016, Dr. Charles Castiglione was selected for the second and third consecutive years as a finalist for the Hartford Healthcare Heroes Award. During the same period, Dr. Alan Babigian was president of the New England Society of Plastic and Reconstructive Surgeons, and president-elect of the Connecticut Society of Plastic and Reconstructive Surgeons. Dr. Orlando Delucia was the president of the Connecticut Society of Plastic and Reconstructive Surgeons. Dr. Castiglione was chosen to co-edit a textbook, Complications in Maxillofacial Cosmetic Surgery
The Plastic Surgery Department provides clinical services at the Connecticut Children’s Medical Center and at Hartford Hospital. Our surgical volume has remained stable, and includes all types of plastic and reconstructive procedures. Our plastic surgeons frequently collaborate with other surgical specialists, providing state-of-the-art multidisciplinary surgical care. Common surgical procedures performed include: complex wound closures including flaps and grafts, craniofacial reconstruction, craniofacial fracture repair, cleft lip/palate reconstruction, breast surgery/reconstruction, body contouring, skin/soft tissue tumor excision/ repair, upper extremity/hand surgery/reconstruction, and cosmetic surgery/non-surgical cosmetic procedures.
The multidisciplinary Craniofacial Team at Connecticut Children’s, co-directed by Dr. Charles Castiglione of Plastic Surgery and Dr. Paul Kanev of Pediatric Neurosurgery, remains a center of excellence. The team provides comprehensive evaluation and treatment for patients of all ages with congenital or acquired deformities of the head and neck. Active team members come from many disciplines, including Plastic Surgery, Pediatric Neurosurgery, Pediatric Otolaryngology, Pediatric Dentistry, Orthodontics, Oral and Maxillofacial Surgery, Pediatric Development, Social Work, and Speech and Language Pathology. Surgeries for cleft lip and palate are most common. Craniosynostosis reconstruction, performed by Dr. Castiglione of Plastic Surgery, and Drs. Kanev, Jonathan Martin, and Markus Bookland of Pediatric Neurosurgery, are also common. In addition, the multidisciplinary Craniofacial Trauma Team, under the leadership of Drs. Castiglione and Norman Cavanagh, provides
cutting edge treatment for all craniomaxillofacial injuries at both Connecticut Children’s and Hartford Hospital.
In June 2016, Dr. James Piorkowski joined the Department of Plastic Surgery, having completed residencies in General Surgery, Plastic Surgery, and Orthopedic Surgery, as well as a Hand Surgery fellowship. Five plastic surgeons, Drs. Duff Ashmead, Alan Babigian, David Bass, James Piorkowski, and Steven Smith, are fellowship-trained hand surgeons, and perform all types of upper extremity and hand surgery. This includes trauma surgery, and reconstruction for acquired and congenital deformities. These surgeons also provide the majority of coverage for hand call at Hartford Hospital and Connecticut Children’s.
Plastic surgeons are very involved in volunteer activities, including surgical mission trips. Drs. Babigian and Castiglione are consultants for Iraq Star, providing surgical care to injured veterans of the Iraq and Afghanistan wars. Dr. Bass continues to make frequent mission trips to South America. Drs. Babigian and Castiglione travel to Ecuador and perform many surgeries, including burn reconstruction, hand surgery, ear reconstruction, and cleft lip/palate surgeries.
Education is a large component of the Plastic Surgery Department’s activities. Residents from General Surgery, Orthopedic Surgery, Urology, ENT, OMFS, and Emergency Medicine rotate on the service. Medical students also elect rotations on Plastic Surgery. Active teaching occurs during daily patient rounds, in the clinic/office setting, in the ER, in the OR, and during planned teaching conferences. Several residents and medical students also have expressed interest in a career in Plastic Surgery, and four residents matched at premier plastic surgery residency programs in the past two years. This brings the total to 48 of our residents and students who have moved on to Plastic Surgery since 1988 when Dr. Castiglione began practicing here. Several residents and medical students are involved in research projects with Drs. Babigian and Castiglione. In addition to publishing articles, Drs. Babigian and Castiglione have presented papers locally, regionally, and nationally. Dr. Castiglione is the Plastic Surgery editor for Connecticut
Medicine: The Journal of the Connecticut State Medical Society, and a reviewer for both The American Journal of Cosmetic Surgery, and Craniomaxillofacial Trauma & Reconstruction. Some department members are involved in local, regional and national professional societies. Drs. Castiglione and Delucia are members of the executive council of the Connecticut Society of Plastic and Reconstructive Surgeons, Dr. Delucia is president, and Dr. Babigian is president-elect. Drs. Babigian and Castiglione are members of the executive council of the New England Society of Plastic and Reconstructive Surgery, and Dr. Babigian is now the president of the NESPRS.
Publications
Banki M, Castiglione C, Ferneini E. Infections associated with aesthetic facial surgery: head, neck, and orofacial infections: an interdisciplinary approach. Elsevier; 2015. p. 366-72.
Lin R, Stevens P, Winninger M, Castiglione C. Orthotic management of deformational plagiocephaly: consensus clinical standards of care. Cleft Palate Craniofac J. 2016 Mar; 53(2).
Hughes C, Lobel B, Gilson A, Campbell J, Mukhopadhyay S, Babigian A, Ellner S, Shapiro D. Can a quality collaborative build value in global surgery? Results from a single state experience. Conn Med. 2015; 79(8):483-7.
Hughes C, Campbell J, Mukhopadhyay S, McCormick S, Silverman R, Lalikos J, Castiglione C, Babigian A. Remote digital preoperative assessments for cleft lip and palate may improve clinical and cost effectiveness for global plastic surgery. Cleft Palate Craniofac J. [accepted for publication April 2016]
Staff
Charles L. Castiglione, MD, MBA, FACS Division Chief
Brian Allen, MD
Duffield Ashmead, MD
Alan Babigian, MD
David Bass, MD
Alex Cech, MD
Orlando Delucia, MD
James Piorkowski, MD
Steven Smith, MD
M. Eileen Auclair, PA-C
Mindi Ceick, APRN
C. Paul Polzella, PA-C

The Division of Pulmonary Medicine strives to be a comprehensive regional resource for pediatric pulmonary disease, with commitments to expert patient care, professional and patient education, and clinical and basic research. Recent highlights include the expansion of our Pediatric Sleep Center and the development of a Severe Asthma Clinic.
The Division of Pulmonary Medicine provides care for infants, children and adolescents with a variety of pulmonary diseases including asthma, apnea, bronchopulmonary dysplasia, cystic fibrosis, interstitial lung disease, neuromuscular disease, sleep disorders, and chronic respiratory failure. The division oversees a state-of-the-art pulmonary function laboratory that is capable of performing spirometry, body plethysmography, impulse oscillometry, methacholine challenge, cardiorespiratory adaptation, and exercise provocation testing in children. Simple spirometry and bronchodilator assessment also are performed at our satellite clinics.
Our Pediatric Sleep Center has grown under the leadership of Dr. Jay Kenkare to 1,500 studies annually. The recruitment of a sleep-certified clinical psychologist, Dr. Lynelle Schneeberg, has allowed us to expand our evaluation and treatment of children with non-respiratory and behavioral sleep problems. Other specialty clinics include a joint Sickle Cell Pulmonary Clinic with Hematology/Oncology; a multispecialty Aerodigestive Clinic with ENT, Gastroenterology, and Speech Therapy; a joint Cystic Fibrosis–Infectious Disease Clinic; and a Severe Asthma Clinic, a collaborative venture with the Care Coordination Center and with school nurses. Our Central Connecticut Cystic Fibrosis Center continues to be one of the top CF centers in the country based on combined pulmonary and nutritional outcomes.
Members of the Pulmonary Division contributed to the education of medical students and residents, respiratory therapists, and nursing APRN students from Yale. Dr. Craig Schramm continued to serve on the Pediatric Chest Medicine Network Steering Committee of the American College of Chest Physicians and as a member of the University Center for Excellence in Developmental Disabilities at the University of Connecticut Health Center. Our Cystic Fibrosis Center Director, Dr. Craig Lapin, continued to serve on the Cystic Fibrosis Foundation Therapeutics Data Safety Monitoring Board, and
Center co-director, Dr. Melanie Collins, was the Connecticut representative to the Cystic Fibrosis Foundation Special Interest Group on newborn screening. Ms. Rosalyn Bravo, APRN, served as the program chair of the Connecticut chapter of the National Association of Pediatric Nurse Practitioners.
Two of our nurses received special recognition this year. Ms. Debby Foster, one of our clinical nurses and certified asthma educators, received a Nightingale Award for her dedication to patient care and education. Ms. Ginny Drapeau was named the prestigious 2016 Mary M. Kontos Care Champion by the Cystic Fibrosis Foundation, an award given to a member of a CF care team selected nationally for passion for excellence, commitment to care and advocacy for individuals with CF, a leadership role in the CF community, and in recognition of a lifetime dedicated to fighting CF.
Clinical research projects conducted over the past year included comparison of impulse oscillometry with clinical asthma scores and participation in multi-center trials involving ivacaftor and lumacaftor in children with cystic fibrosis. Collaborative research projects focused on microbiological research in cystic fibrosis with Quinnipiac Medical School, and weaning of supplemental oxygen in infants with bronchopulmonary dysplasia with Boston Children’s Hospital. Additional basic science research addressed mechanisms of airway immunological tolerance with the Department of Immunology and microRNA expression in asthmatic airways with the Jackson Laboratory for Genomic Medicine in Farmington.
Publications
Bracken SJ, Adami AJ, Szczepanek SM, Ehsan M, Natarajan P, Guernsey LA, Shahriari N, Rafti E, Matson AP, Schramm CM, Thrall RS. Long-term exposure to house dust mite leads to the suppression of allergic airway disease despite persistent lung inflammation. Int Arch Allergy Immunol. 2015; 166(4):243-58.
Carson WF 4th, Guernsey LA, Singh A, Secor ER Jr, Wohlfert EA, Clark RB, Schramm CM, Kunkel SL, Thrall RS. Cbl-b deficiency in mice results in exacerbation of acute and chronic stages of allergic asthma. Front Immunol. 2015 Nov 20; 6:592. doi: 10.3389/ fimmu.2015.00592. eCollection 2015.
Hopfer SM, Stalker HJ, Collins MS. Genetic counseling via telemedicine in a newborn screening program – a novel approach. Ann Clin Lab Sci. 2015; 45:467.
Kaleel M, Pascal M, O’Loughlin M, Schramm CM, Collins MS. Serial lung magnetic resonance imaging to monitor disease progression in a child with a diffuse alveolar hemorrhage syndrome. J Clin Med Res. 2015; 7(4):267-9.
Khincha PP, Bertuch AA, Agarwal S, Townsley DM, Young NS, Keel S, Shimamura A, Boulad F, Simoneau T, Justino H, Kuo C, Artandi S, McCaslin C, Cox DW, Chaffee S, Collins BF, Giri N, Alter BP, Raghu G, Savage SA. Pulmonary arteriovenous malformations: an uncharacterised phenotype of dyskeratosis congenita and related telomere biology disorders. Eur Respir J. 2016 Oct 20. doi: 10.1183/13993003.01640-2016. Epub ahead of print.
Kuti JL, Pettit RS, Neu N, Cies JJ, Lapin C, Muhlebach MS, Novak KJ, Nguyen JT, Saiman L, Nicolau DP. Microbiological activity of ceftolozane/tazobactam, ceftazidime, meropenem, and piperacillin/tazobactam against Pseudomonas aeruginosa isolated from children with cystic fibrosis. Diagn Microbiol Infect Dis. 2015 Sep; 83(1):53-5.
Lenehan PJ, Schramm CM, Collins MS. An evaluation strategy for potential QTc prolongation with chronic azithromycin therapy in cystic fibrosis. J Cyst Fibrosis. 2016; 15(2):192-5.
Lodha A, Ediger K, Rabi Y, Lodha S, Tang S, Bhandari A, Sauve R, Bhandari V. Does chronic oxygen dependency in preterm infants with bronchopulmonary dysplasia at NICU discharge predict respiratory outcomes at 3 years of age? J Perinatol. 2015; 35:530-6.
Sayej W, Collins MS. Failure to thrive in a teenage boy. Med News. 2015 Sept; p 2.
Schramm CM, Sala KA, Carroll CL. Clinical exam does not predict response to albuterol in ventilated infants with bronchiolitis. Pediatr Crit Care Med. 2016 Nov 1. E-pub ahead of print. doi: 10.1097/PCC.0000000000000999.
Simoneau T, Sawicki GS, Milliren CE, Feldman HA, Gordon CM. A randomized controlled trial of vitamin D replacement strategies in pediatric CF patients. J Cyst Fibros. 2016 Mar; 15(2):234-41.
Chapters
Bhandari A, Bhandari V. Bronchopulmonary dyplasia. In: Schwartz MW, editor. The 5-minute pediatric consult. 7th ed. Philadelphia, PA: Williams and Wilkins; 2015.
Bhandari A, Zinman R. Branchial cleft malformations. In: Schwartz MW, editor. The 5-minute pediatric consult. 7th ed. Philadelphia, PA: Lippincott, Williams and Wilkins; 2015.
Blechner M, Bhandari A. What do I need to know about sleep and breathing in children with underlying lung disease? In: Chidekel AS, editor. Curbside consultation in pediatric sleep disorders: 49 clinical questions. Thorofare, NJ: SLACK Inc; 2015.
Collins MS. Sinus disease in cystic fibrosis. In: Valdez T, Vallejo J, editors. Infectious diseases in pediatric otolaryngology. Switzerland: Springer International; 2016. p. 121-33.
Staff
Craig Schramm, MD Division Head
Anita Bhandari, MD
Melanie Sue Collins, MD
Umit Emre, MD
Jay Kenkare, MD
Craig Lapin, MD
Anne McLaughlin, MD
Lynelle Schneeberg, PsyD
Tregony Simoneau, MD
Rosalynn Bravo-Cavoli, APRN
Amanda Filippelli, APRN
The Division of Radiology provides a full spectrum of imaging services as well as minimally invasive image-guided procedures to all clinical divisions at Connecticut Children’s Medical Center. The department is an “Image Gently” facility using strategies to minimize radiation to our patients while utilizing best practice standards and appropriateness criteria to best evaluate children.
Imaging modalities range from computed radiography and digital radiography to complex magnetic resonance imaging. The department is accredited through the American College of Radiology in Ultrasound, CT and MRI. Nuclear Medicine services are provided through collaboration with Hartford Hospital. Image guided procedures are provided through collaboration with physicians from Jefferson Radiology and Hartford Hospital in Interventional Radiology and Interventional Neuroradiology. With support from the Divisions of Anesthesia and Sedation Services, more image guided procedures are being performed on site at Connecticut Children’s Medical Center allowing for less disruption of care in a safer environment.
The Department of Radiology has seen major replacements and upgrading of imaging equipment over the past several years. Most basic imaging is performed in state-of-the-art digital radiography rooms which allow for better plain film imaging with approximately 40 percent radiation dose reduction. Four new ultrasound units have been purchased and put into service allowing for superior imaging in a modality that is well suited to our pediatric population. Because of increasing demand for ultrasound services, hours of routine operation have been extended to midnight and weekends. A Siemen’s flat panel fluoroscopy unit was installed allowing for significant radiation dose reduction with improved image quality. These upgrades support the philosophy of the department as an “Image Gently” and “Step Gently” facility to provide appropriate imaging while reducing the effects of ionizing radiation as much as possible. Video goggles were provided by a donor through the Foundation. They can be worn by a child in the MR unit who can watch a movie while having a lengthy imaging procedure with less dependence on sedation. Child Life provides support in the department for children undergoing difficult procedures.
Dr. Douglas Moote is collaborating with Dr. Jeffrey Hyams in the Division of Gastrointestinal Diseases to support multicenter grant-funded research evaluating the impact of MR imaging of children with inflammatory bowel disease.
Dr. Michael Baldwin is involved in a COG multicenter collaborative assessing impact of pulmonary nodule detection in patients with sarcoma.
The Division of Radiology provides resident education in Pediatric Radiology to radiology residents from the University of Connecticut Health Center, Hartford Hospital, and the Hospital of St. Vincent’s in Bridgeport, CT. Pediatric residents and medical students from the University of Connecticut attend elective rotations in the department. The radiology attendings provide didactic lectures to the radiology and pediatric residents as well as case review sessions. Teaching and clinical care conferences are held in collaboration with the Divisions of Pulmonary Medicine, Digestive Diseases, Endocrinology, General Surgery, Hematology-Oncology, Orthopedic Surgery, and Urology, as well as the NICU and PICU. Work conferences are provided weekly to the Pediatric House Staff.
Publications
Kaleel M, Schramm C, Pascal M, O’Loughlin M, Collins MS. Serial lung magnetic resonance imaging to monitor disease progression in a child with a diffuse alveolar hemorrhage syndrome. J Clin Med Res. 2015 Apr;7(4):267-9. doi:10.14740/ jocmr1962w. Epub 2015 Feb 9. PMID: 25699125.
Dong H, Carlton M, Lerner A, Epstein PM. Effect of cAMP signaling on expression of glucocorticoid receptor, bim and bad in glucocorticoid-sensitive and resistant leukemic and multiple myeloma cells. Front Pharmacol. 2015 Oct 13; v.6.
Shapiro M, Ollenschleger MD, Baccin C, Becske T, Spiegel GR, Wang Y, Song X, Raz E, Zumofen D, Potts M, Nelson PK. Foreign body emboli following cerebrovascular interventions – clinical, radiographic, and histopathologic features. AJNR Am J Neuroradiol. 2015 Nov;36(11):2121-6.
Killory B, Kilbourn K, Ollenschleger M. A novel use of direct platelet application during surgery for clopidogrel-as-
sociated intracerebral hemorrhage. World Neurosurg. 2015 Dec;84(6):2078.e1-4.
Naples J, Grindle C, Zimmerman D. A rare cause of bilateral conductive hearing loss in a young boy. JAMA Otolaryngol –Head & Neck Surg. 2016 Feb 18. Epub 2016 Dec 18.
Stensby JD, Kaliney RW, Alford B, Shen FH, Patrie JT, Fox MG. Radiographic appearance of transforaminal lumbar interbody fusion performed with and without recombinant human morphogenetic protein–2. Am J Roentgenol. 2016 Mar;206(3):588-94. doi: 10.2214/AJR.15.14503.
Staff
R. Timothy Brown, MD Division Head
Michael Baldwin, MD
Frederick Conard, MD
Michael Hallisey, MD
Josh Kallen, MD
Douglas Moote, MD
Martin Ollenschleger, MD
Steven Poole, MD
Ron Rosenberg, MD
Margaret Szerejko, MD
Gregory Wrubel, MD
David Zimmerman, MD

The faculty members of the Division of Research conduct high quality clinical/translational research and clinical trials, provide expert statistical consultation to pediatric faculty, oversee research staff of clinical investigators, and prepare proposals for external funding to advance the overall research enterprise of Connecticut Children’s Medical Center.
They are assisted in this work by more than 30 professionals, including an expert group of master’s prepared research associates and divisional research managers, certified study coordinators and skilled sponsored-program administrators and analysts. The division also manages a unique Investigator Support program for new and established investigators that has yielded six NIH Mentored Scientist (K) awards and a 60 percent R01 funding rate.
Several important changes to the division occurred during 2015-2016. Dr. Georgine Burke stepped down as division head in April 2016, retiring after a 25-year career in which she led the creation of the division and research program at Connecticut Children’s. She is continuing to serve as a consultant to the program as well as statistical consultant to the Journal of Human Lactation. Biostatistician Trudy Lerer, MS, retired in September 2016, following 23 years of service in biostatistics. Bringing a new focus in bioengineering to the faculty are Dr. Min Tang-Schomer, PhD, whose work features novel approaches to neural tissue engineering (joint appointment in School of Engineering, University of Connecticut), Dr. Rishikesh Pandey, PhD, Technical Lead, Biophotonics Laboratory, and Dr. Matthew Solomito, PhD, specialist in biomechanics. Dr. Abigail Bushley, PhD, epidemiologist, joined the faculty in support of the Office of Community Child Health.
The latter half of 2016 saw the start of a Connecticut Children’s research innovation center, in partnership with the Technology Incubator Program of the University of Connecticut.
Dr. Elizabeth Brownell established the Connecticut Human Milk Research Center in 2015, a multidisciplinary group of investigators who seek to better understand the effect of human milk on preterm infant growth, clinical, and neurodevelopmental outcomes. A highlight has been a competitive summer internship program, beginning in 2015 with three
interns, with weekly journal clubs, shadowing Neonatology rounds, participation in Breastfeeding Grand Rounds, and social activities. Dr. Brownell continued her service on the editorial board of the Journal of Human Lactation, as a member of the Baby Friendly USA NICU task force, and as co-chair of the data and epidemiology committee of the maternal child health section of the American Public Health Association. To acknowledge her professional commitment and effort toward advancing human milk research and contributing to the health of all infants, Dr. Brownell was awarded the 2016 Connecticut Breastfeeding Coalition’s Annual Research and Surveillance Award. She also received a faculty appointment as an Assistant Professor of Pediatrics to the Quinnipiac University Frank H. Netter, MD, School of Medicine.
Dr. Tang-Schomer was invited to be a guest editor for Scientifica. Dr. Zhu Wang was appointed to the rank of Associate Professor in the School of Medicine.
Grants
University of Connecticut Stimulus Grant: “3D Brain Tissue Model.” Principle investigators: Min Tang-Schomer, PhD, and Joel Pachter, PhD, (Dept. of Cell Biology, UConn Health).
Publications
Ren M, Du C, Herrero Acero E, Tang-Schomer MD, Ozkucur N. A biofidelic 3D culture model to study the development of brain cellular systems. Sci Rep. 2016 Apr 26;6:24953. doi: 10.1038/scrp24953. PMID: 27112667.
Sood D, Chwalek K, Stuntz E, Pouli D, Du C, Tang-Schomer M, Georgakoudi I, Black LD, Kaplan DL. Fetal brain extracellular matrix boosts neuronal network formation in 3D bioengineered model of cortical brain tissue. ACS Biomater Sci Eng. 2016;2(1):131-40. doi: 10.1021/acsbiomaterials.5b00446.
An B, Tang-Schomer MD, Huang W, He J, Jones JA, Lewis RV, Kaplan DL. Physical and biological regulation of neuron regenerative growth and network formation on recombinant dragline silks. Biomaterials. 2015;48:137-46. NIHMS663832. PMID: 25701039. PMCID: PMC4353650.
Chwalek K, Tang-Schomer MD, Omenetto FG, Kaplan DL. In vitro bioengineered model of cortical brain tissue. Nat Protoc. 2015;10(9):1362-73. NIHMS780330. PMID: 26270395. PMCID: PMC4867028.
Chwalek K, Sood D, Cantley WL, White JD, Tang-Schomer M, Kaplan DL. Engineered 3D silk-collagen-based model of polarized neural tissue. J Visualized Exp. 2015;(105):e52970. PMID: 26555926. PMCID: PMC4692668.
Cloutier MM, Wiley J, Wang Z, Grant A, Gorin AA. The Early Childhood Obesity Prevention Program (ECHO): an ecologically based intervention delivered by home visitors for newborns and their mothers. BMC Public Health. 2015;15:584.
Wang Z, Ma S, Wang CY. Variable selection for zero-inflated and overdispersed data with application to health care demand in Germany. Biom J. 2015 Sep;57(5):867-84.
Sayej WN, Ménoret A, Maharjan AS, Fernandez M, Wang Z, Balarezo F, Hyams JS, Sylvester FA, Vella AT. Characterizing the inflammatory response in esophageal mucosal biopsies in children with eosinophilic esophagitis. Clin Transl Immunology. 2016;5:e88. doi: 10.1038/cti.2016.30. Epub 2016 Jul 1.
Lussier MM, Brownell EA, Proulx TA, Bielecki D, Marinelli KA, Bellini S, Hagadorn JI. Daily breast milk volume in mothers of very low birth weight neonates: a repeated measures randomized trial of hand expression versus electric breast pump expression. Breastfeed Med. 2015 Jul-Aug;(10):312-7.
Briere CE, McGrath JM, Cong X, Brownell EA, Cusson R. Direct-breastfeeding premature infants in the neonatal intensive care unit. J Hum Lact. 2015 Aug;31(3):386-92.
Briere CE, Lucas R, McGrath JM, Lussier M, Brownell E. Establishing breastfeeding with the late preterm infant in the NICU. J Obstet Gynecol Neonatal Nurs. 2015 Jan;44(1):10213.
Brownell EA, Hagadorn JI, Lussier MM, Goh G, ThevenetMorrison KN, Lerer TJ, Herson VC, Howard CR. Optimal periods of exclusive breastfeeding to predict any breastfeeding duration through one year. J Pediatr. 2015 Mar;166(3):566570.e1.
Brownell EA, Smith KC, Cornell EL, Esposito PA, Wiley CC, Wang Z, Bushley AW, Lussier MM, Hagadorn JI. Five-year secular trends and predictors of non-consent to receive donor milk in the neonatal intensive care unit. Breastfeed Med. 2016 May 18. PMID: 27191772.
Fitzstevens JL, Smith KC, Hagadorn JI, Caimano MJ, Matson AP, Brownell EA. A systematic review of the human milk microbiota. Nutr Clin Pract. 2016 Sept 27. Epub ahead of print.
Hagadorn JI, Brownell EA, Trzaski JM, Johnson KR, Lainwala S, Campbell BT, Herbst KW. Trends and variation in management and outcomes of very low birth weight infants with patent ductus arteriosus. Pediatr Res. 2016 Sept 28. Epub ahead of print.
Cornell EL, Lerer TJ, Hagadorn JI, Chapman DJ, Lussier MM, Brownell EA. A non-NICU-specific peer counseling program is not associated with human milk receipt at or following discharge. J Perinatol. 2016 May 26. Epub ahead of print.
Valdez TA, Marvin K, Bennett NJ, Lerer T, Nolder AR, Buchinsky FJ. Current trends in peri-operative antibiotic use: a survey of otolaryngologists. Otolaryngol Head Neck Surg. 2015 Jan;152(1):63-6.
Campbell BT, Austin DM, Kahn O, McCann MC, Lerer TJ, Lee K, et al. Current trends in the surgical treatment of pediatric ovarian torsion: we can do better. J Pediatr Surg. 2015 Aug;50(8):1374-7.
Oliva-Hemker M, Hutfless S, Al Kazzi ES, Lerer T, Mack D, LeLeiko N, et al. Clinical presentation and five-year therapeutic management of very early-onset inflammatory bowel disease in a large North American cohort. J Pediatr. 2015 Sep;167(3):527-32.
Grossi V, Lerer T, Griffiths A, LeLeiko N, Cabrera J, Otley A, et al. Concomitant use of immunomodulators affects the durability of infliximab therapy in children with Crohn’s disease. Clin Gastroenterol Hepatol. 2015 Oct;13(10):1748-56.
Brooks TM, Friedman LM, Silvis RM, Lerer T, Milewski MD. Back pain in a pediatric emergency department: etiology and evaluation. Pediatr Emerg Care. Epub ahead of print 2016 Jun.
Brooks TM, Smith MM, Silvis RM, Lerer T, Henry C, Maitland R, Dunn AL, Logan K, Smith SR. Symptom guided emergency department discharge instructions for children with concussion. Pediatr Emerg Care. Epub ahead of print 2016 Jun.
Casavant S, McGrath J, Burke G, Briere CE. Caregiving factors affecting breastfeeding duration within the NICU. Adv Neonatal Care. 2015 Dec;15(6):421-8. PMID: 26551792.
Trapp C, Burke G, Crowell RC, Gorin AA, Cloutier MM. The relationship between dietary patterns, BMI percentile and household food security in young urban children. Child Obes. 2015 Apr;11(2):148-55. Epub 2015 Feb 26.
Prasad R, Pandey R, Barman I. Engineering tailored nanoparticles with microbes: quo vadis? WIREs Nanomed Nanobiotechnol. 2016;8;316-30.
Pandey R, Valdez T. Chemical imaging in middle ear pathology: quo vadis? J Postdoc Res. 2016:4;7-12.
Õunpuu S, Solomito MJ, Bell K, DeLuca P, Pierz K. Longterm outcomes after multilevel surgery including rectus femoris, hamstring and gastrocnemius procedures in children with cerebral palsy. Gait Posture. 2015;42(3):365-72.
Solomito MJ, Garibay EJ, Woods JR, Õunpuu S, Nissen CW. Lateral trunk lean in pitchers affects both ball velocity and upper extremity joint moments. Am J Sports Med. 2015;43(5):1235-40.
O’Malley M, Solomito MJ, Milewski MD. The association of tibial slope and ACL rupture in skeletally immature patients. J Arthroscopic Rel Surg. 2015;31(1):77-82.
Wang DH, Kostyun RO, Solomito MJ. The biomechanics of cranial forces during figure skating spinning elements. Conn Med. 2015;79(3):133-7.
Solomito MJ. Lagrangian approach to modeling the biodynamics of the upper extremity: applications to collegiate baseball pitching. 2015. Doctoral Dissertations. Paper 995. http://digitalcommons.uconn.edu/dissertations/995
Solomito MJ, Ferreira JV, Nissen CW. Biomechanical differences between right and left handed pitchers. Sports Biomech. 2016 June;(2):1-9.
Nissen CW, Solomito MJ. Baseball injuries. In: Let’s discuss: adolescent sports injuries. American Academy of Orthopedic Surgeons. Retrieved from http://www.aaos.org/store/ product/?productid=9324662.
Wang Z. Cancer classification using mass spectrometrybased proteomics data. 2015. https://cran.r-project.org/ web/packages/bst/vignettes/pros.pdf
Wang Z. Classification of cancer types using gene expression data. 2015. https://cran.r-project.org/web/packages/ bst/vignettes/static_khan.pdf
Wang Z. Classification of UCI machine learning datasets. 2015. https://cran.r-project.org/web/packages/bst/vignettes/static_mcl.pdf
Wang Z. Survival prediction using gene expression data. 2015. https://cran.r-project.org/web/packages/bujar/vignettes/static_dlbcl.pdf
Wang Z. Analysis of cancer data with boosting algorithm for nonconvex loss. 2016. https://cran.r-project.org/web/packages/bst/vignettes/static_cancer.pdf
Faculty
Georgine S. Burke, PhD
Division Head
Zhu Wang, PhD
Elizabeth Brownell, PhD
Abigail Bushley, PhD
Rishikesh Pandey, PhD
Trudy Lerer, MS
Matthew J. Solomito, PhD
Min Tang-Schomer, PhD
Staff
Lisa Benson Senior Director of Research Administration and Sponsored Programs
Terry Dehnel Director, Office of Grants and Sponsored Programs
Kim Jennings Senior Manager, Clinical Trials Unit
Lisa Butler Grants Contracts Manager
Kimberly Davey, MS Grants Manager
Katherine Herbst, MS Clinical Research Manager
Shefali Thaker, MPH Research Associate II
Kathleen A. Sala, MPH Research Associate II

The Division of Rheumatology is the largest such program in Connecticut, taking pride in our ability to be accessible to all corners of the state. In 2015-16, referrals were received from 152 of the 169 towns in Connecticut.
The division is looking to expand and increase its academic standings. With that in mind, the division recruited an outstanding young physician, Dr. Heather Tory, who will be splitting her time between rheumatology and patient safety/quality, which will include ongoing research as well. She joins Drs. Lawrence Zemel and Barbara Edelheit.
The mission of the division is to provide the best clinical care possible to children with rheumatic disease, teach trainees the basics of the field, and to enroll patients in clinical trials or collaborative research projects when applicable.
We continue to run a high-volume practice; during 2015-16, we saw the following number of patients:
1). New outpatients – 822/year (additional 47 new patients at Shriner’s Hospitals for Children satellite)
2). Follow-up visits – 1,900/year (additional 194 follow-up patients at Shriner’s)
3). Inpatient admissions – 30/year
4). Inpatient consults – 35/year
5). Joint aspirations – 75/year
Rheumatology collaborates with the Sedation service around procedures, Orthopaedics for overlapping disorders, GI for infusions and drug toxicities, Hematology for disorders that span both specialties, Nephrology for lupus and vasculitis, Infectious Diseases for Lyme disease, and the Pain and Palliative service for children with amplified pain disorders such as fibromyalgia. The division fully utilizes the resources of the hospital, since many of the patients have multi-system disease or complex psycho-social problems.
The division provides critical education to trainees, since the outpatient rotation is often the only exposure pediatric residents have with rheumatic disease. Eleven of the 13 blocks were subscribed by pediatric residents or fourth-year medical students on elective. Space permitting, we occasionally ac-
commodate outside residents, third-year medical students, and even physician assistant students. We have an arrangement with the Division of (adult) Rheumatology at the University of Connecticut Health Center to provide their fellows with pediatric training.
Special Programs 2015-2016
1) Comprehensive Lyme disease program: collaborating with several other divisions, including Infectious Diseases, Orthopaedics, and Pain and Palliative; collecting longitudinal data.
2) Starting a diagnostic dilemma service, working with Infectious Diseases for initial outpatient contact with patients who meet inclusion criteria, such as unexplained fever or fatigue, and working with the inpatient MUPS (medically unexplained physical symptoms) team to coordinate further inpatient work-up. Prospective data will be collected, and outcomes analyzed.
Publications
Janow G, Schanberg LE, Setoguchi S, Hasselblad V, Mellins ED, Zemel L, et al. The Systemic Juvenile Idiopathic Arthritis Cohort of the Childhood Arthritis and Rheumatology Research Alliance Registry: 2010-2013. J Rheumatol. 2016 Sep 1; 43(9):1755-62.
Fitzpatrick L, Broadaway KA, Ponder L, Zemel L, AngelesHan ST, et al. Phenotypic characterization of juvenile idiopathic arthritis in African American children. J Rheumatol. 2016 April 1; 43(4):799-803.
Ombrello MJ, Remmers EF, Tachmazidou I, Grom A, Zemel L, et al. HLA-DRB111 and variants of the MHC class II locus are strong risk factors for systemic juvenile idiopathic arthritis. Proc Natl Acad Sci USA; 2015 Dec;112(52):15970.
Zemel L, Blier P. Juvenile fibromyalgia: a primary pain, or pain processing disorder. Semin Pediatr Neurol. 2016; 23:231-41.
Suter L, Barber CE, Herrin J, Leong A, Losina E, Miller A, Newman E, Robbins M, Tory H, Yazdany J. American College of Rheumatology White Paper on Performance Outcome Measures in Rheumatology. Arthritis Care Res. 2016; 68(10):1390-1401.
Staff
Lawrence Zemel, MD
Division Head
Barbara Edelheit, MD
Heather Tory, MD

The years 2015 and 2016 have been very busy and productive ones for the Division of Transplant at Connecticut Children’s. Working closely with the Division of Nephrology, the pediatric kidney transplant programs continue to grow, and successful kidney transplants have been performed. Our multidisciplinary approach has allowed us to successfully offer transplants to more pediatric patients. The program is recognized by UNOS.
The Transplant Division has a strong quality commitment. Each program has a quality indicator dashboard as well as a Process Improvement dashboard that tracks PI projects such as revisions of policies, decreasing infections, and developing algorithms to improve patient care. Specifically, a prednisonefree protocol was created to be on the cutting edge of therapies offered to children in the country.
We were named a Center of Excellence by Anthem and Aetna, attesting to the quality of our program.
Staff
Patricia Sheiner, MD, FACS Division Director
Caroline Rochon, MD
Brian Shames, MD

The mission of the Pediatric Urology Division is to provide the highest quality, family centered surgical care. We are continually reviewing our specific clinic wait times and offering same-day visits in an effort to improve patient access and experience.
Pediatric Urology provides comprehensive care as a combined service line with Pediatric Nephrology. The service line has remained busy with nearly 17,559 patient visits and over 1,963 operative cases. We continue to enhance specialty clinics at Connecticut Children’s Medical Center. These include: GUPPE clinic for patients with disorders of sexual development, ROCKS clinic for patients with kidney stones, PUV clinic for patients with posterior urethral valves, MVP clinic, managing voiding problems for patients with bladder and bowel dysfunction, and Prenatal Clinic for patients with known fetal urologic abnormalities.
In 2016, there were several changes to the list of providers in the division. Drs. Fernando Ferrer, Christina Kim, John Makari, Eric Nelson, and Miriam Harel pursued a private practice opportunity. We have welcomed new providers including Dr. Howard Hochman, an experienced pediatric urologist, who joined us from Hartford Hospital. Additionally, Dr. Adam Hittelman joined us in collaboration with Yale. He specializes in robotic surgery and complex reconstruction. Dr. Carlos Medina comes to us from New York Presbyterian Hospital/Weill Cornell Medical College and is the new medical director of the division. Dr. Angela Arlen will join the division in April in collaboration with Yale. She comes to us from Iowa University. Finally, Anne Dudley, MD, will be joining the team in August 2017. She is coming from Vanderbilt University and has a strong interest in spina bifida and complex reconstruction.
The new team is looking forward to working with the referring providers and providing comprehensive urologic care to the children of Connecticut.
Publications
Harel M, Ferrer FA, Shapiro LH, Makari JH. Future directions in risk stratification and therapy for advanced pediatric genitourinary rhabdomyosarcoma. In: Urologic oncology: seminars and original investigations. Elsevier; 2015. doi: 10.1016/j.urolonc.2015.09.013.
Gerber C, Harel M, Lynch ML, Herbst KW, Ferrer FA, Shapiro LH. Proximal tubule proteins are significantly elevated in bladder urine of patients with ureteropelvic junction obstruction and may represent novel biomarkers: a pilot study. J Ped Urol. Epub 2015 Oct. (10.1016/j.jpurol.2015.10.008).
Dangl PP, Akhavan A, Odeleye M, Avery D, Lendvay T, Koh C, Elder JS, Noh PH, Bansal D, Schulte M, MacDonald J, Shukla A, Kim C, Herbst K, Corbett S, Kearns J, Kunnavakkam R, Gundeti MS. Ninety-day perioperative complications of pediatric robotic urological surgery: a multi-institutional study. J Ped Urol. Epub 2015 Oct. (10.1016/j.jpurol.2015.08.015).
Zee RS, Herbst KW, Kim C, McKenna PH, Bently T, Cooper CS, Herndon CD. Urinary tract infections in children with prenatal hydronephrosis: a risk assessment from the Society for Fetal Urology Hydronephrosis Registry. J Ped Urol. Epub 2016 Apr. (10.1016/j. jpurol.2016.04.024).
Harel M, Herbst KW, Nelson E. Practice patterns in the surgical approach for adolescent varicocelectomy. SpringerPlus. 2015 Dec:4(1):1-6.
Wang HS, Herbst KW, Rothman JA, Shah NR, Weiner JS, Routh JC. Trends in sickle-cell-disease-related priapism in U.S. children’s hospitals. Urology. Epub 2015 Dec. (10.1016/j.urology.2015.11.023).
Smith PP, DeAngelis A, Simon R. Evidence of increased centrally enhanced bladder compliance with ageing in a mouse model. BJU Int. 2015;155(2): 322-9. doi: 10.1111/bju.12669. PMID: 25116343.
Smith PP, Kuchel GA, Griffiths D. Functional brain imaging and the neural basis for voiding dysfunction in older adults. Clin Geriatr Med. 2015;4:549-65.
Chapple CR, Osman NI, Birder L, van Koeveringe GA, Oelke M, Nitti VW, Drake MJ, Yamaguchi O, Abrams P, Smith PP. The underactive bladder: a new clinical concept? Eur Urol. 2015;68(3);351-3. PMID: 25770481.
Chapters
Pope JC 4th, Makari JH. Vesical neck reconstruction. In: Graham SD, Keane TE, editors. Glenn’s urologic surgery. 8th ed. Philadelphia: Lippincott Williams and Wilkins; 2016.
Boylan A, Murphy G, Nelson E. Enuresis algorithm. In: Domino FJ, editor. www.5minuteconsult.com. Philadelphia: Wolters Kluwer Health; 2016.
Staff
Fernando Ferrer, MD, FAAP, FACS
Division Head
Carlos Medina, MD
Medical Director
Jill Bernstein MD, FAAP
Adam Hittelman, MD
Howard Hochman, MD
Christina Kim, MD, FAAP
John Makari, MD, FAAP, FACS
Eric Nelson, MD
Phillip Smith, MD
Lauren Brennan, APRN
Katherine Herbst, MSc

The pediatric residency program continued with its uninterrupted record of full, continuing accreditation, with no areas of concern or citations from the Pediatric Review committee of the ACGME.
The program continued to successfully recruit high quality residents. Entering residents had an average of 2.9 scholarly activities and 7.9 community service activities prior to matching. Graduates were, once again, placed in competitive fellowship programs and outstanding practices. The program first-attempt pass rate on the American Board of Pediatrics certifying examination has increased once again, and it is comfortably meeting the required pass rate for accreditation. Resident participation research continues to increase as well, and more participation has been documented in the context of the now ongoing Research Methods rotation under the leadership of Dr. Sharon Smith, with the addition of greater direction in identifying collaborations for resident research projects. ACGME surveys and program surveys of faculty and residents were notably positive, but they also provided the identification of areas of focus for program development, including the following program improvement efforts:
The program continued to address meaningful assessment of learners with continued progress in providing evaluations in a more timely way, and efforts to improve the quality of the evaluations with greater authenticity and deliberateness using the milestone method of tracking resident progress and issues.
Through the continued leadership efforts of Dr. Christine Skurkis, additional efforts were made to improve the timeliness of evaluations. This was reviewed again at the Annual Faculty Meeting, open to all faculty and residents. Improved timeliness of assessment was accomplished by regular reporting of the information, by area of activity, so faculty and leadership could identify successes and areas for improvement. Actions to be taken for areas of need were identified.
Improved content of evaluations was addressed through a workshop for Core Faculty Leaders and an initial effort at dissemination of the expected approach to the
assessment of residents. This year’s workshop was an interactive session in which Core Faculty Leaders shared best practices and ways to meet challenges in the various areas of resident activities. A commitment was made to disseminate the methods identified in the faculty development session to all faculty members performing resident assessments. Leveraging technology to enhance the ability of faculty to evaluate residents through directly observed performance continued to evolve. The Pediatric Hospital Medicine faculty members, through the leadership of Dr. Richard Johnson, played a major role in moving this forward, with the engagement of Apple, Inc., and continued commitment to implementation of the application for smart phones that would allow faculty to do real-time evaluations efficiently and effectively.
The need to better balance service and education, and ensure access to opportunities to learn and master procedures, was identified and approached in a number of ways.
A multiple component plan was developed to begin addressing these problems that affect both residents and faculty. Efforts were begun to address inpatient rounding. This included smaller rounding teams, improved rounding processes, addition of more medical team assistants to do non-physician work in support of rounds and ongoing care, and improved distribution of patients. These initiatives are ongoing.
Enhancements for the electronic medical record (EMR) were begun, first by making it easy to use the discharge summary, requiring little additional effort and delivering needed information in a timely way. Discharge summary issues have virtually gone away! This creates more time to get away from the computer screen and get back to the bedside. Next steps include addressing other parts of this documentation and how it is implemented, for example, expanding the devices for accessing and using the EMR, so the ability to use them in mobile ways becomes a reality.
Procedural competence tracking, including criteria for documenting procedural competence, was revisited and
revised. Ways to ensure resident access to required procedures were identified. Competition for cases, in a number of settings, was addressed with the review and revision of the distribution methods for assigning patients to the primary providers.
Improving resident ability to identify potential research mentors, and enhancing the perception of environment of inquiry within the residency program were pursued in a number of ways.
To enhance the resident awareness of research opportunities and their ability to pursue them, Dr. Sharon Smith continued her efforts to forge ahead with resident scholarship. A searchable database is in development and will maintain a list of faculty willing to mentor resident research, and their area of interest. This creates a listing of rotation and division-specific scholarly activities that residents can access on our Blackboard curricular site. These also are disseminated through email and by “newsletter,” both of which highlight scholarly achieve-
Staff
Residency Program Director
Edwin L. Zalneraitis, MD Professor
Associate Program Directors Residency Program
Christine Skurkis, MD
Assistant Professor
Sharon Smith, MD Professor
Mark Greenstein, MD Professor
Patricia Joyce, MD
Associate Professor
ments to help stimulate interest and honor achievement. Research didactic instruction continues in the research basics rotation four times annually. Research-specific didactic instruction material was posted to Blackboard as well, to ensure access for all residents.
Strategic efforts to improve wellness for residents and faculty were continued and expanded.
In collaboration, Connecticut Children’s, the Department of Pediatrics, and the Pediatric Residency Program continued to plan and carry out key initiatives targeted at self-care, connectedness and the work environment in an effort to promote resilience and overall wellness among faculty and residents. Flexible vacation days, renewal options, modified retreats and the EMR efforts highlight the changes dedicated to this purpose so far. Faculty participated in resilience training as well, and the institution and the program have planned consultation with nationally recognized leaders to assess where we are currently and recommend next steps in the endeavor to capture, grow and sustain our personal and professional well-being.
Administrative Staff
Aida Velez
Manager Medical Education
Kristen Mangiafico
Medical Education Registrar
Barry Wagar
Program Administrator
Brian Lesmes
Program Assistant
Medical Education
Andrea Richardson
Pediatric Clerkship Administrator
Pediatric Residents by Level, 2015-16
PL-1
Caroline Amin, MD
Peggy Chen, MD
Roxanne Cheung, MD
Sigfus Kristinn
Gunnlaugsson, MD
Anjali Gupta, MD
Margaret Gloria Hilder, MD
Rebecca Kohlberg-Davis, MD
Jonah Mandell, DO
Justine Mrosak, MD
Dana Nezon, MD
John Norko, MD
Nisha Patel, MD
Jenny Petrauskas, MD
Agnes Reschke, MD
Sara Soshnick, DO
Jessica Tutolo, MD
Carolina Vega, MD
Emily Anne Sampino, MD
Caleb Wasser, DO
Jonathan Wong, DO
PL-2
Emily Biddick, MD
Abigail Bosk, DO
Crista Cerrone, MD
Elizabeth Chasse, MD, MPH
Katie Clouthier, DO
Tam Doan, MD
Sarah Germani, DO
Jilian Gormley, DO
Tuhina Joseph, DO, MS
AnnaMarie Koller, DO
Selena Levine, DO
Katrina Loh, MD
PL-1 Pediatric Residents 2016 - 17
Amy Blodgett, MD
Noah Buncher, DO
Jessica Fannell, MD
Nicole Fersa, DO
Joshua Goldman, MD
Erin Goode, DO
Shilpa Guntaka, MD
Kristin Hallett, MD
Owen Kahn, MD
Kaitlin Keenan, DO
Abraham Khorasani, MD
Danielle Klima, DO
Sarah Kollar, DO
Neetu Krishnan, DO
Faculty Education Coordinators
Nancy Miller, MD
Shailendra Upadhyay, MD
Laurie Scheiner, MD
Rebecca Moles, MD
Keri Wallace, MD
Allison Cowl, MD
Mark Greenstein, MD
Kristin Welch, MD
Lana Friedman, MD
Cem Demirci, MD
Bella Zeisler, MD
Richard Johnson, MD
Kerry Moss, MD
Melissa Held, MD
Core Faculty & Site Directors
Timothy Brown, MD
Francis DiMario, MD
Katherine Kavanaugh, MD
Nicole Murray-Posner, MD
David Muccino, MD, MPH
Shannon Oteri, DO
Carolina Quintana, MD
John Ramirez, MD
Amanda Silverio, MD
Kaitlin Strumph, DO
Whitney Trompeter, MD
Christine Yang, MD
Nancy Yip, DO, MS
Caroline Adegite, MD
Alyson Baker, MD
William Brucker, MD
Mary Ann De Banate, MD
Mona Doss, DO
Mark Gilroy, DO
Megan Griffiths, MD
Kunal Gupta, MD
Jane Im, MD
Rose Lee, MD
Laura McKay, MD
Brenda Prindle, MD
Louis Rigos, DO
Melanie Rudnick, MD
Jessica Shui, MD
Vaka Kristin Sigurjonsdottir, MD
Kristopher Teti, MD
Sussi Vivar, MD
Anna Weingarten, DO
Chief Residents
Paula Lucuara Revelo, MD
Wallis Molchen, DO
Christine Pulice, DO
Chelsea Lepus, DO
Catherine Paszek, DO
Usha Prasad, DO
Katarzyna Saar, DO
Jessica Sanchez, MD
Chelsea Wells, DO
Chief Residents
Mark Gilroy, DO
Megan Griffiths, MD
Laura McKay, MD
Christine Skurkis, MD
Leslie Wolkoff, MD
Sherene Mason, MD
Francis DiMario, MD
Kristan Pierz, MD
Craig Lapin, MD
Tregony Simoneau, MD
Carl Nissen, MD
Kristan Pierz, MD
Andrea Orsey, MD
Barbara Edelheit, MD
David Wang, MD
Richard Weiss, MD
David Sink, MD
Nicole Murray-Posner, MD
Richard Weiss, MD
Christine Welch, MD
The University of Connecticut School of Medicine-sponsored graduate medical education (fellowship) programs at Connecticut Children’s Medical Center continue to graduate very well trained specialty physicians who enter practice throughout the country. Our fellows continue to be awarded funding for exciting research projects, with numerous accepted presentations at national scientific meetings, and travel grants and awards. The success of our fellowship programs would not be possible without the dedication and tireless efforts of our fellowship coordinators: Jack Wakefield, Marianne Gonzalez, Opeyemi Aina, Lindsay Haythorn and Amanda Ross.
Led by Dr. Michael Archambault, the Pediatric Anesthesiology program was newly accredited in October 2015. The program successfully matched Dr. Thomas Manning from the University of Nebraska Medical Center. Dr. Manning will join the program in July 2017.
Led by Dr. Paola Palma Sisto and Associate Program Director Dr. Rebecca Riba-Wolman, the program continued to graduate fellows into academic programs. Drs. Paola Palma Sisto and Rebecca Riba-Wolman have been active with the Pediatric Endocrine Society fellowship group on new assessment tools for the ACGME’s Next Accreditation System requirements for fellowship. Fellows have had a 100 percent pass rate at first attempt on the pediatric endocrinology board. They also are engaged in meaningful research experiences mentored by well-published, NIH-funded investigators in basic and translational research. Our fellows continue to receive travel grants to attend national meetings to present their work.
Dr. Sasi Penukonda graduated from the program in June 2015 and went on to practice in Springfield, MA. He gave a platform presentation on his work at the Pediatric Academic Societies annual meeting. He also has received travel grants to national meetings to present his research. His work was titled “Vanilloid Receptor 1 Regulates Gut Immune Homeostasis.”
Dr. Sunitha Sura completed her research on “Characterization of
Immune Checkpoint Inhibitor LAG-3 in Peripheral Blood Mononuclear Cells of Subjects with High HDL-Cholesterol.” She also has received travel grants to national meetings to present her research. She graduated our program in June 2016 and has joined our faculty here at the Department of Pediatrics.
Dr. Shrinkhala Srivastava has been working on her research characterizing the polycystic ovarian syndrome (PCOS) population at the endocrine clinic. She presented her work at the Pediatric Endocrine Societies and the Endocrine Society national meetings. She is working on a prospective study involving depression assessment in new patients referred for PCOS.
Dr. Tricia Pinto joined us from Florida State University in Pensacola, FL, in July 2015 as our current second-year fellow. Her area of interest is in bone physiology in children. She has joined the lab of Dr. Marja Hurley to further investigate bone disease at the molecular level using a mouse model.
Dr. Massiel Mojica Sarmiento joined us from Lincoln Medical and Mental Health Center in Bronx, NY, as our first year fellow in July 2016. Her area of interest is in childhood obesity and prevention.
In December 2016, the program successfully matched Whei Ying Lim, MD, from Hurley Medical Center in Michigan. Dr. Lim will join the program in July 2017.
Led by Dr. Matt Laurich, the Pediatric Emergency Medicine Fellowship is now in its 17th year. Dr. Laurich assumed the role of program director in July 2015 after having served as associate program director under Dr. John Brancato. Dr. Brancato had served as program director for 14 years, building the fellowship from its infancy to the successful program it is today. The fellowship was approved in 2015 to expand to its new complement of six fellows.
Dr. Talia Brooks graduated from the fellowship in June 2015 and took a faculty position at Cohen Children’s Medical Center in New Hyde Park, NY. Her fellowship research resulted in two manuscripts that have been accepted for publication in Pediatric Emergency Care: “Back Pain in a Pediatric Emer-
gency Department: Etiology and Evaluation,” and “Symptom Guided Emergency Department Discharge Instructions for Children with Concussion.”
The program welcomed two excellent new fellows in 2015. Dr. Laurie Malia joined us after having completed her residency here at Connecticut Children’s Medical Center. Dr. Hannah Sneller joined us from Stony Brook Children’s Hospital in Stony Brook, NY, where she completed her pediatric residency and chief residency.
Dr. Malia participated in a research project here as a resident that was accepted for publication in January 2016 in Pediatric Emergency Care. It’s entitled, “Revisiting Appendiceal Diameter via Ultrasound for the Diagnosis of Acute Appendicitis.” In October 2016, Dr. Malia presented the results from one of her fellowship projects at the American Academy of Pediatrics National Conference in San Francisco, CA. Her project, “Fast and Sensitive: Automated Point of Care Urine Dips,” compared the performance characteristics of automated urine dips versus urinalysis and microscopy for diagnosing urinary tract infection in the Emergency Department.
Dr. Sneller presented her prior research at the American Academy of Pediatrics National Conference and Exhibition in Washington, DC, in October 2015. Her project was “Improvement in Compliance for Home Management Plan of Care on the Pediatric Inpatient Units Utilizing the Electronic Medical Record.”
Our current third-year fellows are Dr. Karl Hellstrand and Dr. Kathryn Kasmire. Dr. Hellstrand presented his research on “Prevalence of Cyberbullying in Patients Presenting to the Pediatric Emergency Department” at the Eastern Society for Pediatric Research in Philadelphia in March 2016 and the Pediatric Academic Societies in May 2016. In addition, Dr. Hellstrand published a case report on “Low Back and Leg Pain With Refusal to Ambulate in a 6-Year-Old Male” in Clinical Pediatrics in November 2015.
Dr. Kasmire presented the results of her research on “Trampoline Park and Home Trampoline Injuries” at the Eastern Society for Pediatric Research in Philadelphia in March 2016 and the Pediatric Academic Societies in May 2016. The study was subsequently published in Pediatrics in September 2016. This research garnered national media attention and
was covered in numerous news outlets including National Public Radio, USA Today, CBS News, NBC News, and U.S. News & World Report.
In January 2016, Connecticut Children’s hosted the 4th Annual New England Regional Pediatric Emergency Medicine Fellows’ Conference, which was attended by over 60 fellows and faculty from PEM Fellowships at Yale, Brown, Bay State Medical Center, Boston Medical Center, and Boston Children’s. Our own Dr. James Wiley delivered the keynote address.
The program welcomed two excellent new fellows in July 2016. Dr. Noah Jablow joined us from Stony Brook Children’s Hospital, and Dr. Tasha Desai joined us from the Children’s Hospital at Lehigh Valley Health Network in Allentown, PA.
In December 2016, the program successfully matched two future fellows who will start here in July 2017: Dr. Jacob Greenberg from Maimonides Infants’ and Children’s Hospital of Brooklyn, NY, and Dr. Prina Patel from Winthrop University Hospital in Mineola, NY.
Led by Dr. Wael Sayej since July 2014, the fellowship program in Pediatric Gastroenterology, Hepatology and Nutrition has had five fellows since it started five years ago. Dr. Sayej became the program director as of August 2014 after the departure of Dr. Francisco Sylvester. The program graduated its first fellow, Dr. Johanna G. Palmadottir, in June 2014, and second fellow, Dr. Ajay Rana in 2015. Dr. Palmadottir has been practicing as assistant professor of pediatrics at the Medical University of South Carolina in Charleston. Dr. Rana accepted a position at Eastern Maine Medical Center in Bangor, ME.
The program graduated its third fellow, Dr. Jasmeet Mokha, in June 2016. Dr. Mokha joined us as clinical faculty in our GI division at Connecticut Children’s. Dr. Mokha has been very successful and productive during his fellowship training. He has two first-author peer-reviewed publications and a third one in the works, he has a completed a book chapter with Division Head Dr. Jeffrey Hyams, and has been invited to present at national conferences. He was recently awarded the Oley Foundation HomePN Research Award for his paper,
“Effects of Ethanol Lock Therapy on Central Line Infections and Mechanical Problems in Children With Intestinal Failure,” and was invited to present it at the Oley Foundation national conference. Dr. Mokha is interested in intestinal rehabilitation in children with short bowel syndrome and in functional gastrointestinal disorders.
Our third year fellow, Dr. Victoria Grossi, is progressing very nicely and is showing great promise. She will be joining our group as clinical faculty when she completes her fellowship training in July 2017. Her current research is focused on pain genetics in patients with inflammatory bowel disease. She has submitted two abstracts to Digestive Diseases Week (DDW 2017), which is regarded as the most important annual gastroenterology conference in the world. Dr. Grossi has previously presented oral presentations at DDW. She also contributed two chapters in the new Pediatric GI review book that is sponsored by the North American Society for Pediatric Gastroenterology, Hepatology and Nutrition (NASPGHAN). Finally, Dr. Grossi is completing a master’s degree in Clinical and Translation Research at UConn.
Our second year fellow, Dr. Angela Pressley-Wallace, started her research experience in July 2016. Dr. Pressley-Wallace is interested in both clinical and translational research on eosinophilic esophagitis. She is currently working in the lab with patient samples to determine the role of the IL-10/IL-5 ratio in monitoring disease activity in Eosinophilic Esophagitis. She has recently submitted an abstract to the Eastern Society for Pediatric Research (March 2017) and the Pediatric Academic Society meeting (May 2017). Dr. Pressley-Wallace contributed a chapter in the new Pediatric GI review book sponsored by NASPGHAN.
Dr. Temara Hajjat joined the program in July 2016. She completed her pediatric residency at the University of Iowa Hospitals and Clinics in Iowa City, IA. She completed her medical school education at the Jordan University of Science and Technology Faculty of Medicine, Amman, Jordan, with a scholarship from the King of Jordan, received for achieving distinction in high school. Dr. Hajjat hit the ground running and has been well perceived by our faculty, residents, nurses and others throughout the hospital. She will be starting her
research rotation in February 2017 and will transition to working in the lab in July.
Dr. Sayej has been involved with the NASPGHAN training committee and worked on the EPA (Entrustable Professional Activity) curriculum for pediatric gastroenterology.
In December 2016, the program successfully matched Dr. Andrew Fondell who will join the program in July 2017. He is completing his residency at UnityPoint Health, Blank Children’s Hospital, Des Moines, IA, where he also served as a chief resident. He completed his medical school education at Rocky Vista University College of Osteopathic Medicine in Parker, CO.
Grossi V, Bezler N, Sayej WN. An ulcer of the duodenum in an adolescent caused by a pancreatic neuroendocrine tumor. Clin Gastroenterol Hepatol. 2016 Sep 6. PMID: 27613258.
Mokha JS, Davidovics ZH. Improved delivery of fat from human breast milk via continuous tube feeding. J Parenter Enteral Nutr. 2016 Feb 5. PMID: 26850740.
Mokha JS, Davidovics ZH, Samela K, Emerick K. Effects of ethanol lock therapy on central line infections and mechanical problems in children with intestinal failure. J Parenter Enteral Nutr. 2016 Jan 29. PMID: 26826261.
Samela K, Mokha J, Emerick K, Davidovics ZH. Transition to a tube feeding formula with real food ingredients in pediatric patients with intestinal failure. Nutr Clin Pract. 2016 Aug 4. pii: 0884533616661011. Epub ahead of print.
Grossi V, Lerer T, Griffiths A, LeLeiko N, Cabrera J, Otley A, Rick J, Mack D, Bousvaros A, Rosh J, Grossman A, Saeed S, Kay M, Boyle B, Oliva-Hemker M, Keljo D, Pfefferkorn M, Faubion W, Kappelman MD, Sudel B, Markowitz J, Hyams JS. Concomitant use of immunomodulators affects the durability of infliximab therapy in children with Crohn’s disease. Clin Gastroenterol Hepatol. 2015 Oct; 13(10):1748-56. PMID: 25911120.
Grossi V, Hyams JS. The safety of treatment options for pediatric Crohn’s disease. Expert Opin Drug Saf. 2016 Oct; 15(10):1383-90. doi: 10.1080/14740338.2016.1203418.
Epub 2016 Jul 1.
Fellows Book Chapters
Grossi V, Sayej WN. Colitis. In: The NASPGHAN fellows concise review of pediatric gastroenterology, hepatology and nutrition. 2nd ed. 2016.
Grossi V, Sayej WN. Radiation oncology. In: The NASPGHAN fellows concise review of pediatric gastroenterology, hepatology and nutrition. 2nd ed. 2016.
Mokha J, Sayej WN. Colic and gas. In: The NASPGHAN fellows concise review of pediatric gastroenterology, hepatology and nutrition. 2nd ed. 2016.
Mokha J, Sayej WN. Appendicitis. In: The NASPGHAN fellows concise review of pediatric gastroenterology, hepatology and nutrition. 2nd ed. 2016.
Pressley-Wallace A, Sayej WN. Chronic constipation and encopresis. In: The NASPGHAN fellows concise review of pediatric gastroenterology, hepatology and nutrition. 2nd ed. 2016.
Poster Presentations
Mokha J. Improved delivery of fat from human breast milk via continuous tube feeding. NASPGHAN; 2015 Oct; Washington, DC.
Mokha J. Gastric fluid microbiomes in children with and without Eosinophilic Esophagitis. NASPGHAN; 2015 Oct; Washington, DC.
Mokha J. Ethanol lock therapy in children with intestinal failure lowers infection rates but increases rates of mechanical problems. Digestive Diseases Week; 2015 May 20; Washington, DC.
Grossi V, Bezler N, Finck C, Sayej W. A rare cause of duodenal ulcer in an adolescent male. NASPGHAN; 2015 Oct; Washington, DC.
Rana A, Lerer T, Fernandez M, Hyams J, Sylvester FA, Sayej W. Routine premedicaiton with intravenous methylprednisolone can prevent the need for dose intensification of infliximab in children with Crohn’s disease. NASPGHAN; 2015 Oct; Washington, DC.
Led by Dr. Joseph Tucker and Robin Schwartz, MS, CGC, the Medical Genetics and Genomics Residency Training Program has been training clinical medical geneticists since the program was first accredited in 1997. Future development of the program involves plans to expand to allow for a fouryear combined Pediatrics and Genetics training program, and collaboration with Jackson Laboratories now located on the campus of the University of Connecticut School of Medicine. In November 2016, the program successfully matched Dr. Jaclyn Gordon from St. Joseph’s Regional Medical Center in Mishawaka, IN. Dr. Gordon will join the program in July 2017.
The Pediatric Infectious Diseases Fellowship Program is led by Dr. Nicholas Bennett and was newly accredited in September 2016.
Led by Drs. James Hagadorn, David Sink, and Jennifer Trzaski, the fellowship program in Neonatal-Perinatal Medicine continued its outstanding record of academic accomplishment and scholarly productivity. Arvin Bundhoo, MD, and Soji Varghese, MBBS, both completed the fellowship program successfully in June 2015.
Tristan Lindberg, MD, completed the fellowship program successfully in June 2016. Under the mentorship of Dr. Adam Matson, Dr. Lindberg presented his research to the New England Perinatal Society in Newport, RI, in March, the Eastern Society for Pediatric Research in Philadelphia in March, and the Pediatric Academic Societies in Baltimore in May.
Third-year fellow Kendall Johnson, MD, specializing in Quality Improvement, presented her work at the Vermont Oxford Network Quality Improvement Congress in Chicago in October
2015, at the Eastern Society for Pediatric Research in Philadelphia in March, and to the Pediatric Academic Societies in Baltimore in May.
Maushumi Assad, MD, MPH, joined us in July of 2015. She gave platform presentations to the New England Perinatal Society in March 2016 in Newport, RI, the Eastern Society for Pediatric Research in Philadelphia in March, and the Pediatric Academic Societies in Baltimore in May 2016.
Jennifer Caldwell, MD, MS, joined us in July 2016 as first year fellow. Dr. Caldwell holds a master’s degree in Medical Sciences from McMaster University in Hamilton, Ontario, and completed her residency in pediatrics at Albany Medical Center.
In December 2016, the program successfully matched Betté Ford, MD, from Morehouse School of Medicine in Atlanta, and Rachel Koski, DO, MS, from Albany Medical Center. Drs. Ford and Koski will join the program in July 2017.
Led by Dr. Mark Lee, the Orthopaedics fellowship was ACGME accredited in 2013.
Rhianna Little joined the program in July 2015 and completed a research project utilizing the division’s state-of-the-art Motion Analysis Laboratory on knee moments during ambulation for patients with varus deformities of the lower extremities. She graduated in June 2016 and accepted a position in San Antonio, TX, to practice pediatric orthopaedics with a particular focus on sports injuries.
In April 2016, the program successfully matched Alvin Su, MD, PhD, from National Yang-Ming University of Taiwan. Dr. Su will join the program in July 2017. He completed two prior ACGME-accredited clinical fellowships in adult and pediatric sports medicine at Washington University and University of Pennsylvania and has published extensively. He is excited to spend a year learning about general pediatric orthopaedics while further honing his skills in pediatric sports medicine.
Beginning in 2017, the Pediatric Orthopaedics Fellowship will
have a dual accreditation with the ACGME and the Pediatric Orthopaedic Society of North America (POSNA), in a national effort to standardize the fellowship curriculum.
Led by Dr. Anita Bhandari for nine years, the Pediatric Pulmonary Fellowship graduated Dr. Anne McLaughlin in June 2015. Dr. McLaughlin stayed on at Connecticut Children’s as a junior faculty member in the Division of Pulmonology. As a third year fellow, she presented a poster at the American Thoracic Society Meeting in Denver, CO, titled “Asthma Control Scores Correlate Better With Small Airway Than Large Airway Dysfunction.” Dr. McLaughlin received the McNeill Teaching Award for pulmonary didactic teaching, presented by the residents.
Dr. Craig Schramm, who had been the fellowship program director from 1994 to 1999, resumed directorship of the program in July 2016.
Led by Drs. Christine Finck and Richard Weiss, the fellowship program in Pediatric General Surgery began in July 2011. To date, two fellows have graduated from the program and have gone on to successful practices – one in Eugene, OR, and the other in Hershey, PA. The program’s newest fellow, Dr. Yue Yung Hu, joined Connecticut Children’s in August 2015 and has a strong interest in health services research.
The program successfully matched Dr. Michael James Healy from the School of Medicine at Yale New Haven. Dr. Healy will join the program in July 2017 after completing his residency.
The ACGME-accredited fellowship program in Pediatric Urology continues to attract and train top candidates in our field. Former program director Dr. Christina Kim left Connecticut Children’s to pursue a private practice opportunity, and we are pleased to announce that Dr. Carlos Medina will be the new fellowship director.
In June 2015, Liza Aguiar completed her two-year fellowship training. While here, she received her master’s degree in clinical and translational research at the University of Connecticut. She is now on the faculty at Brown University.
Gina Lockwood joined us in July 2015 after completing the residency program at Medical College of Wisconsin. She is currently obtaining her master’s degree in clinical and translational research at the University of Connecticut, and should be finished in July 2017.
Fellows
Endocrinology
Paola Palma-Sisto, MD
Program Director
Rebecca Riba-Wolman, MD
Associate Program Director
Sasi Penukonda, MBBS
Sunitha Sura, MBBS
Shrinkhala Srivastava, MD
Tricia Pinto, MD
Massiel Sarmiento, MD
Urology
Christina Kim, MD
Program Director
Liza Aguiar, MD
Paul “Trey” Smith, MD
Gina Lockwood, MD
Lily Wang, MD
Emergency Medicine
V. Matt Laurich, MD
Program Director
Talia Brooks, MD
Karl Hellstrand, DO
Kathryn Kasmire, MD
Laurie Malia, DO
Hannah Sneller, MD
Noah Jablow, MD
Tasha Desai, DO
General Surgery
Christine Finck, MD
Program Director
Anthony Tsai, MD
Yue-Yung Hu, MD
Paul Smith III graduated from our program in June 2016. During his nonclinical year, he focused on urodynamic evaluation in children. Since graduation he has joined the faculty at Penn State University in Hershey, PA.
Lily Wang joined us in July 2016 after completing the residency program at Cornell University, and is completing research in bio-informatics in collaboration with Jackson Laboratory
Gastroenterology
Wael Sayej, MD
Program Director
Ajay Rana, MBBS
Jasmeet Mokha, MBBS
Victoria Grossi, DO
Angela Pressley-Wallace, MD
Temara Hajjat, MD
Neonatology
James Hagadorn, MD
Program Director
Tristan Lindberg, MD
Kendall Johnson, MD
Maushumi Assad, MD
Susan Pitts, DO
Jennifer Caldwell, MD, PhD
Orthopaedics
Mark Lee, MD
Program Director
Rhianna Little, MD
Pulmonology
Anita Bhandari, MD (2015) Program Director
Craig Schramm, MD (2016) Program Director
Anne McLaughlin, MD
Fellowship Coordinators
Opeyemi Aina
Anesthesiology, Orthopaedic Surgery, General Surgery, Urology
Marianne Custer
Emergency Medicine, Endocrinology, Infectious Diseases, Pulmonology
Lindsay Haythorn
Emergency Medicine, Infectious Diseases, Pulmonology, Surgery
Amanda Ross
Anesthesiology, Endocrinology, Neonatology, Orthopaedic Surgery
Jack Wakefield
Gastroenterology, Genetics, Neonatology
180833 Acsadi, An Open-label, Multi-center, 48-week Study Sarepta 1/1/15
Gyula With a Concurrent Untreated Control Arm to Therapeutics, Inc. Evaluate the Efficacy and Safety of Eteplirsen in Duchenne Muscular Dystrophy
180840 Acsadi, A Phase 2, Randomized, Double-blind, Biogen Idec 9/1/15
Gyula Sham-procedure Controlled Study to Assess MA, Inc. the Safety and Tolerability and Explore the Efficacy of ISIS 396443 (BIIB058) Administered Intrathecally in Subjects with Spinal Muscular Atrophy Who Are Not Eligible to Participate in the Clinical Studies ISIS 396443-CS3B or ISIS 396443-CS4
Altman, Leukemia Research
Lea’s Foundation 11/1/15
Arnold for Leukemia Research, Inc.
Altman, Leukemia Research
Lea’s Foundation 6/1/16 n/a
Arnold for Leukemia Research, Inc.
179372 Bennett, A Registry of Patients With Primary United States 1/1/15 12/31/16
Nicholas Immune Deficiency Disorders Immunodeficiency Network
180821 Bennett, A Multicenter, Randomized, Double-blinded Cubist 1/1/15
Nicholas Comparative Study to Evaluate the Efficacy, PharmaceSafety, and Pharmacokinetics uticals, Inc. of Daptomycin Versus Active Comparator in Pediatric Subjects With Acute Hematogenous Osteomyelitis Due to Gram-Positive Organisms
180825 Bennett, Randomized, Parallel Dose, Phase 1/2 Safety Biota Scientific 1/1/15 12/31/16 $-
Nicholas and Pharmacokinetics Study of Inhaled Mgmt Pty, Ltd. Laninamivir Octanoate TwinCaps® Dry Powder Inhaler in Children With Naturally Acquired Influenza A or B
180831 Bennett, A Phase 1, Open-label, Single Dose Study to Durata 1/1/15 12/31/16
Nicholas Investigate the Pharmacokinetics, Safety and Therapeutics Tolerability of Dalbavancin in Hospitalized International, BV Children Aged 3 Months to 11 Years Receiving Standard Intravenous Anti-infective Treatment for Bacterial Infections
Bookland, Pediatric Brain Tumors Research Connecticut 10/1/15 n/a n/a n/a n/a
Marcus Brain Tumor Alliance
Bookland, Pediatric Brain Tumors Research Connecticut
Marcus Brain Tumor Alliance
Bookland, Pediatric Brain Tumors Research Marc A. Somberg 10/1/15
Marcus Memorial Foundation
Bookland, Pediatric Brain Tumors Research Marc A. Somberg 12/1/16
Marcus Memorial Foundation
179408 Boruchov, Community Counts: Public Health Surveillance DHHS/CDC/
Donna for Bleeding Disorders ATHN (UMASS)
Donna (Hospital for Special Care)
Donna
179663 Boruchov, Sickle Cell Disease Consortium CT/DPH
Donna (Hospital for Special Care) 180265 Boruchov, My Life Our Future Biogen Idec
Donna (ATHN)
Boruchov, Data Quality Counts
Donna 180348 Boruchov, Data Quality Counts
Donna
180800 Boruchov, A Phase I/III Open-label, Multi-center, CSL Behring, 1/1/15
Donna Crossover Safety, Efficacy and Pharmacokinetic LLC Study of Recombinant Coagulation Factor VIII (rFVIII) Compared to Recombinant Human Antihaemophilic Factor VIII (rFVIII; INN: octocog alfa) in Subjects with Hemophilia A, and a Repeat PK, Safety and Efficacy Study (Part 3)
180812 Boruchov, H7T MC TADO Phase 3, Double-blind, Eli Lilly
Donna Randomized, Efficacy and Safety Comparison of Prasugrel and Placebo in Pediatric Patients with Sickle Cell Disease.
180819 Boruchov, Single-dose Study to Evaluate the Bristol Myers 1/1/15
Donna Pharmacokenetics, Pharmacodynamics, Safety, Squibb and Tolerability of Apixaban in Pediatric Subjects at Risk for a Venous or Arterial Thrombotic Disorder
180827 Boruchov, A Phase III Open-label, Multi-center, Extension CSL Behring, 1/1/15
Donna Study to Assess the Safety & Efficacy of LLC Recombinant Coagulation Factor VII CSL627 in Subjects With Severe Hemophilia A
180832 Boruchov, A Phase III Open-label Pharmacokinetic, CSL Behring, 1/1/15
Donna Efficacy and Safety Study of rVIII-Single Chain LLC in a Pediatric Population With Severe Hemophilia A
Brock, Elks Safe Kids Project Connecticut Elks 6/1/15
Karen Association
Brock, Elks Safe Kids Project Connecticut 6/1/16
Karen Elks Association
Campbell, Intimate Partner Violence (IPV) Screening, Brief Connecticut
Brendan Intervention, and Referral for Services Institute for Clinical & Translational Science (CiCATS)
180836 Carroll, A Randomized, Open-label, Active Controlled, Bristol Meyers
Christopher Safety and Extrapolated Efficacy Study in Squibb /Pfizer, Pediatric Subjects Requiring Anticoagulation for Inc. the Treatment of a Venous Thromboembolic Event
Chaudhry, Simple Bone Cysts in Kids
Sonia Hospital for Sick Children
179399 Cloutier, The Asthma Neighborhood DHHS/NIH/ 7/1/15
Michelle NHBLI
Michelle
Cloutier, Easy Breathing Training & Consulting Community
Michelle Health Network, Connecticut
180334 Cloutier, Easy Breathing Training & Consulting
Michelle Community Health Network, Connecticut
180312 Davey, T-Cell Receptor Excision Circles: A Novel New England
Brooke Approach to Identify Immunodeficiency in Congenital Newborns with Congenital Heart Disease Cardiology Research Fdn.
180841 Davidovics, A Randomized, Double-blind, Controlled, Clinical Baxter
Zev Trial to Evaluate the Risk of Developing Essential Healthcare Corp Fatty Acid Deficiency in Pediatric Patients, Including Neonates, Receiving Either Clinolipid (Lipid Injectable Emulsion, USP) 20% or Standard-of-Care Soybean Oil-based Lipid Emulsion
180847 Davidovics, A Multi-center, Randomized, Double-blind, Nutrinia, Ltd.
Zev Three-arm, Parallel-group Trial to Assess the Efficacy and Safety of NTRA-9620 in Infants With Short Bowel Syndrome (SBS) Following Surgical Resection (GIFT-02)
179256 Demirci, Type 1 Diabetes TrialNet
DHHS/NIH/ 1/1/15 12/31/16
Cem NIDDK (Univ South Florida)
180814 DiMario, A Three-arm, Randomized, Double-blind, Novartis
Francis Placebo-controlled Study of the Efficacy and Pharmaceuticals Safety of Two Trough Ranges of Everolimus as Corp. Adjunctive Therapy in Patients With Tuberous Sclerosis Complex (TSC) Who Have Refractory Partial-onset Seizures
179381 DuMont- Early Detection of Autism DHHS/NIH 3/1/15 5/31/16
Mathieu, (Drexel Univ) Thyde
179406 DuMont- Teaching Skills to Toddlers
DHHS/NIH 8/1/15
Mathieu, (UCONN Storrs) Thyde
180333 DuMont- Strategies to Promote Culturally Effective Connecticut 1/1/16 12/31/16
Mathieu, Screening, Referral and Service Provision in Health Thyde Primary Care Practices and Birth to Three Foundation
179248 Dworkin, Regional Care Coordination Community DHHS/HRSA 7/1/16
Paul Collaborative (CT/DPH)
179390 Dworkin, Regional Care Coordination Community DHHS/HRSA 7/1/15 6/30/16
Paul Collaborative (CT/DPH) 180271 Dworkin, Use of a National Affiliate Network to Diffuse WK Kellogg
Paul System Innovation to Promote Vulnerable Foundation Children’s Optimal Healthy Development
Paul Public Giving
Paul Community Coordination Health Foundation
Dworkin, Enhancing Pediatric Capacity to Mitigate the JPB Foundation 1/1/15
Paul Impact of Toxic Stress
180322 Dworkin, The Feasibility of Using Protective Factors Tools Aetna Foundation 1/1/16
Paul to Inform System Building and Measure Impact in Promoting Children’s Optimal Healthy Development
180360 Dworkin, The Office for Community Child Health Hearst 11/1/16 12/31/16 $75,000.00
Paul (OCCH): A Model for Children’s Hospitals to Foundation Elevate Their Status as Critical Community Resources
179269 Edelheit, TNF Inhibition
DHHS/NIH 1/1/15
Barbara (CCHMC)
180278 Edelheit, Enteric Flora in Newly Diagnosed Friends of 1/1/15
Barbara Spondyloarthritis CARRA (Univ. Alabama)
180758 Edelheit, A Longterm Multi-center Longitudinal Abbott 1/1/15 12/31/15
Barbara Post-marketing Observational Registry of Laboratories Humira (Adalimumab) in Children with Active JIA. Phase 1.
180740 Emerick, Evaluation of the Pharmacokinetics, Safety, Bristol Myers 1/1/15
Karan Tolerability and Efficacy of Entecavir in Pediatric Squibb Subjects With Cronic Hepatitis B Virus Who Are HB3AG-positive
180780 Emerick, A Comperative Study of the Antiviral Efficacy Bristol Myers 1/1/15
Karan and Safety of Entecavir (ETV) Versus Placebo Squibb in Pediatric Subjects With Chronic Hepetitis B Virus Infection
180639 Estrada, KIGS Pfizer, Inc. 1/1/15 12/31/15
Elizabeth
180707 Estrada, Tercica Registry Agreement (MS 305) Tercica, Inc. 1/1/15
Elizabeth
179393 Ferrer, Sphingosine-1-Phosphate Pathway-based DHHS/NIH/ 7/1/15 6/30/16
Fernando Therapy for Neuroblastoma NCI (UCHC)
180318 Ferrer, Breakthrough Therapies Targeting Solid Tumors Strike 3
Fernando Foundation
Ferrer, Solid Tumor Research Mill Foundation 9/1/15 n/a n/a
Fernando for Kids, Inc. Ferrer, Solid Tumor Research Department of 6/1/15 n/a
Fernando Connecticut VFW of U.S., Inc.
179398 Finck, Immune Evasion in Embryonic Stem Cell-based DHHS/NIH 5/15/15
Christine Tissue Repair and Transplantation (UCHC)
180277 Finck, Use of Neonatal Human-induced Pluripotent CT Innovations/ 1/1/15
Christine Stem Cells and Human Embryonic Stem Cells Jackson in Hyperoxia-induced Lung Injury Laboratories (UCHC)
Finck, Use of Neonatal Human-induced Pluripotent CT Innovations 1/1/16
Christine Stem Cells and Human Embryonic Stem Cells in Hyperoxia-induced Lung Injury
180357 Finck, Engineering and Implantation of a Patient- Biostage, Inc.
Christine specific Esophageal Construct for the Treatment of Esophageal Defects and Disease
179437 Germain- The Role of G Protein-coupled Signaling in NIH/NICHD
Lee, Emily Neurocognitive and Psychosocial Abnormalities (UCHC)
180701 Greenstein, Hunter Outcome Survey Shire Human 1/1/15
Robert Genetic Therapies
180779 Hagadorn, Phase III, Inhaled Nitric Oxide for the Treatment INO 1/1/15
James of Bronchopulmonary Dysplasia (BPD) in Therapeutics, Preterm Infants Requiring Mechanical LLC Ventilation or Positive Pressure Support on Days 5 - 14 After Birth
Hawley, K Elucidating Innate and Adaptive Immune Patterson Trust 4/1/16 3/31/17
X X Interplay in Human Syphilis
180804 Heller, Adult Congenital Heart Disease Enhancement Actelion Pharma 1/1/15
Felice Clinical Research Initiative USA
179376 Hussain, Antibiotic Safety in Infants
DHHS/NIH 1/1/15
Naveed (Duke Univ.)
179846 Hussain, A Multi-center, Double-blind, Randomized, Chiesi
Naveed Single Dose, Active-controlled Study to Farmaceutici Investigate the Efficacy and Safety of Synthetic S.p.A. Surfactant (CHF 5633) in Comparison to Porcine Surfactant (Poractant Alfa, Curosurf) in the Treatment of Preterm Neonates With Respiratory Distress Syndrome S.p.A.
179296 Hyams, Predicting Response to Standard Pediatri DHHS/NIH/ 5/1/15
Jeffrey Colitis Therapy: The PROTECT study NIDDK
180317 Hyams, Validation and the Pediatric Rome IV Criteria - American 7/1/15
Jeffrey Pilot Award in Functional Gastroenterolgy and Gastroenterolgy Motility Association Research Fdn.
180332 Hyams, Anti-TNF Therapy for Refractory Colitis in CCFA (CCHMC) 11/1/15
Jeffrey Hospitalized Children (“ARCH”)
180361 Hyams, Development and Evaluation of the TUMMY Izaak Walton 10/27/16 12/31/16
Jeffrey CD-index: A Patient Reported Signs and Killam Health Symptoms Index for Pediatric Crohn’s Disease Centre
180368 Hyams, Causes and Consequences of Newutrophil DHHS/NIH/ 11/1/16 12/31/16 $-
Jeffrey Dysfunction in Early Onset Crohn’s Disease NIDDK (Emory Univ.)
180725 Hyams, A Multi-center, Prospective, Long-term, Janssen 1/1/15
Jeffrey Observational Registry of Pediatric Patients Services, LLC With Inflammatory Bowel Disease
180753 Hyams, Investigative Natalizumab Through Further Elan 1/1/15 12/31/16
Jeffrey Oberservational Research and Monitoring Pharmaceuticals Phase IV Registry
180756 Hyams, Risk Stratification and Identification of CCFA (Emory U)
Jeffrey Immunogenetic and Microbial Markers of Rapid Disease Progression in Children With Crohn’s Disease
180777 Hyams, A Multidisciplinary Human Study on the Genetic, CCFC (Mt. Sinai 1/1/15
Jeffrey Environmental, and Microbial Interactions That Hosp) Cause IBD
Hyams, The ImageKids Study Shaare Zekek
Jeffrey Medical Ctr
180815 Hyams, A Phase 1b Open-label Study to Assess the Janssen 1/1/15
Jeffrey Safety and Pharmacokinetics of Subcutaneously Research & Administered Golimumab, a Human Anti-TNFα Development Antibody, in Pediatric Subjects With Moderately LLC to Severely Active Ulcerative Colitis
180823 Hyams, CCFA Partners-Pediatrics CCFA (Emory 1/1/15 12/31/16
Jeffrey Univ.)
180830 Hyams, Safety, and Tolerability of Serum-derived Bovine Entera Health
Jeffrey Immunoglobulin in Children With DiarrheaPredominant Irritable Bowel Syndrome
180839 Hyams, A Long-term, Non-interventional Registry to AbbVie, Inc. 8/18/15 12/31/16
Jeffrey Assess Safety and Effectiveness of Humira® (Adalimumab) in Pediatric Patients With Moderately to Severely Active Crohn’s Disease (CD) - CAPE
180843 Hyams, A Phase 4, Multi-center, Open-label Study of Janssen 12/14/15 12/31/16 $10,000.00 1-2 of 3 n/a n/a
Jeffrey Serum Infliximab Concentrations and Efficacy Research & and Safety of Dose Escalation in Pediatric Development Patients With Inflammatory Bowel Disease LLC
179356 Isakoff, National Clinical Trials Network Grant “DHHS/NIH/ 1/1/15
Michael NCI/COG (CHOP)” 179357 Isakoff, Children’s Oncologh Group Federally
Michael Sponsored Studies - Per Case Reimbursement NCI/COG (CHOP)
179374 Isakoff, Study Chair National Clinical Trials Network “DHHS/NIH/ 1/1/15
Michael Grant NCI/COG (CHOP)” 180206 Isakoff, Neuroblastoma and Medulloblastoma Spectrum
Michael Translational Research Consortium Sponsored Studies
180213 Isakoff, Children’s Oncology Group Industry Sponsored COG (CHOP) 1/1/15
Michael Studies - Per Case Reimbursement
180250 Isakoff, Moffitt Institute Sponsored Studies - Per Case H. Lee Moffitt 1/1/15
Michael Reimbursement Cancer Center and Research Institute Hospital, Inc.
Isakoff, Adolescent and Young Adults Cancer Program Essex County 1/1/16
Michael Community Foundation
Isakoff, Hematology/Oncology Clinical Trials LPL Financial 11/1/16 n/a n/a
Michael Services
Isakoff, Hematology/Oncology Advanced Cancer Feld 5/1/16
Michael Entertainment 180325 Kalsner, Adaptive Clinical Genomics for Precision CBIF (The
Louisa Medicine Jackson Laboratories)
Kalsner, TSC2 Variants Without Clinical Findings of UCONN Storrs 7/1/16
Louisa Tuberous Sclerosis Complex as a Risk Factor for Idiopathic Autism Spectrum Disorder
Lapin, Cystic Fibrosis Therapeutic Development Center Cystic Fibrosis 1/1/15
Craig Therapeutics Fdn.
Craig Foundation
Craig Foundation
Lapin, Implementation of the Depression and Anxiety Cystic Fibrosis
Craig Guidelines: Award for a Mental Health Therapeutics Fdn. Coordinator
Lapin, Therapeutics Development Center Cystic Fibrosis
Craig
Craig Foundation 180770 Lapin, Controlled Trial of Two Adherence Promotion Novartis
Craig Interventions for Cystic Fibrosis, [I Change Pharmaceuticals Adherence and Raise Expectations (ICARE)] Corp. (Univ. Miami) 180796 Lapin, A Phase 3, Randomized, Double-blind, Placeb Vertex
Craig -controlled, Parallel-group Study to Evaluate the Pharmaceuticals Efficacy and Safety of Ivacaftor in Subjects With Cystic Fibrosis Who Have the R117H-CFTR Mutation
180801 Lapin, A Long-term Prospective Observational Safety Seattle Children’s 1/1/15
Craig Study of the Incidence of and Risk Factors for Hospital Fibrosing Colonopathy in U.S. Patients With Cystic Fibrosis Treated With Pancreatic Enzyme Replacement Therapy
180803 Lapin, A Phase 3, Two-arm, Rollover Study to Evaluate Vertex
Craig the Safety of Long-term Ivacaftor Treatment in Pharmaceuticals Subjects 6 Years of Age and Older With Cystic Fibrosis and a Non-G551D CFTR Mutation
180805 Lapin, An Open-label Study to Assess the Population Hartford Hospital 1/1/15
Craig Pharmacokinetics, Safety, and Practicality of Administering Meropenem as a Prolonged Infusion to Cystic Fibrosis Children Admitted With an Acute Pulmonary Exacerbation
180809 Lapin, REACT
Craig
180811 Lapin, A Phase 3, Randomized, Double-blind, Vertex
Craig Placebo-controlled, Parallel Group Study to Pharmaceuticals Evaluate the Efficacy and Safety of Lumacaftor in Combination With Ivacaftor in Subjects Aged 12 Years and Older With Cystic Fibrosis, Homozygous for the F508del-CFTR Mutation
180816 Lapin, A Point-prevalence Study to Evaluate the AbbVie, Inc. 1/1/15 12/31/16
Craig Prevalence of Antibodies to Selected Porcine Aptalis Pharma, Viruses in Patients With Cystic Fibrosis Who Inc., & Janssen Are Receiving Porcine-derived Pancreatic Research & Enzyme Replacement Therapy: A Harmonized Development Protocol Across Sponsors LLC
180820 Lapin, A Phase 3, Rollover Study to Evaluate the Vertex 1/1/15
Craig Safety and Efficacy of Long-term Treatment Pharmaceuticals With Lumacaftor in Combination With Ivacaftor in Subjects Aged 12 Years and Older With Cystic Fibrosis, Homozygous or Heterozygous for the F508del-CFTR Mutation
180848 Lapin, A Phase 4, Open-label Treatment, Randomized Vertex 7/15/16 12/31/16
Craig Multi-center, Two-arm, Parallel-group, Pilot Pharmaceuticals Study of Adherence to Lumacaftor/Ivacaftor in CF Subjects Homozygous for the F508delCFTR Mutation
Livingston, Greater Hartford Children’s Advocacy Center, VOCA – Justic 7/1/15 6/30/16
Nina Direct Services, Child Abuse Program Department
Livingston, Greater Hartford Children’s Advocacy Center, Dept. of Children 7/1/15
Nina Direct Services, Victims of Abuse and Families
Livingston, Greater Hartford Children’s Advocacy Center, CT. Department 7/1/15
Nina Child Sexual Abuse of Public Health
Livingston, Greater Hartford Children’s Advocacy Center Office of Victim 10/1/15 6/30/16
Nina Sexual Abuse Exams/Interviews Services –Justice Department
180837 Madan- An Open-Label, Phase I, Pharmacokinetic Upsher-Smith 5/20/15 12/31/16
Cohen, Study of Single Doses of Intranasal Midazolam Laboratories, Inc. Jennifer (USL261) in Pediatric Subjects With Epilepsy
180838 Madan- A Randomized, Double-blind, Placebo-controlled GW Research 5/22/15 12/31/16 $149,570.80
Cohen, Study to Investigate the Efficacy and Safety of Ltd. Jennifer Cannabidiol (GWP42003-P; CBD) as Adjunctive Treatment for Seizures Associated With Lennox-Gastaut Syndrome in Children and Adults
180842 Madan- A Randomized, Double-blind, Placebo-controlled GW Research
Cohen, Study to Investigate the Efficacy and Safety of Ltd. Jennifer Cannabidiol (GWP42003-P) in Children and Young Adults With Dravet Syndrome
180844 Madan- An Open-label Extension Study to Investigate GW Research
Cohen, the Safety of Cannabidiol (GWP42003-P; Ltd. Jennifer CBD) in Children and Adults with Inadequately Controlled Dravet or Lennox-Gastaut Syndromes
179343 Makari, Short-term Outcomes of Interventions for DHHS/NIH 5/1/15 4/30/16
John Reproductive Dysfunction NICHHD (Univ. of Oklahoma)
180798 Makari, A 12-week, Randomized, Open-label, Active Pfizer, Inc. 1/1/15
John Comparator Period Followed by a 12-week Safety Extension Period to Evaluate the Safety and Efficacy of Fesoterodine in Subjeccts Ages 6 to 16 Years and >25 kg w
179367 Ohannes- Adaptive Treatment for Cannabis Use Disorders DHHS/NIH 8/1/15 7/31/16
sian, (UCHC)
Christine
179368 Ohannes- Treatment of Co-occurring Alcohol Use DHHS/NIH 7/1/15 12/31/16
sian, Disorders and Depression/Anxiety Disorders (UCHC)
Christine 179392 Ohannes- Bidirectional Effects Between Parental DHHS/NSF 12/1/15
sian, Work-Family Conflict and Adolescent Christine Psychosocial Adjustment
Ohannes- Psycho-social Depression Study Alvord Family 9/1/15 n/a
sian, Foundation
Christine
179319 Orsey, SunCoast CCOP Research Base at the DHHS/NIH
Andrea University of South Florida /NCI (Univ. South Florida)
180273 Orsey, Improving Quality of Life for Pediatric Cancer CHIP (UCONN 1/1/15
Andrea Patients and Parents Through Yoga Storrs)
180279 Orsey, Development and Validation of Pediatric CIHR/Toronto
Andrea Cancer-specific Symptom Screening and Hospital for Sick Assessment Tool Children
180339 Orsey, Thrombotic Thrombocytopenic Purpura (TPP) Baxalta (Univ. 3/19/16
Andrea Registry Hosp of Bern)
180792 Orsey, An Open-label, Multi-center Study of the Safety Purdue Pharm 1/1/15
Andrea of Twice Daily Oxycodone Hydrochloride LP Controlled-release Tablets in Opioid Experienced Children From Ages 6 to 16 Years Old
180728 Parikh, A Multi-center, Prospective, Open-label, Clinical Grifols, Inc. 1/1/15
Nehal Trial to Assess the Safety and Efficacy of a New Intravenous Immune Globulin (IGIV31 Grifols 10%) in Patients With Idiopathic (Immune) Thrombocytopenic Purpura
179246 Phulwani, Studies to Treat or Prevent Pediatric Type 2 DHHS/NIH/ 1/1/15 12/31/15
Pria Diabetes NIDDK (George Washington Univ.)
180786 Phulwani, Colesevelam Oral Suspension as Monotherapy Daiichi Sankyo, 1/1/15 12/31/16 $11,248.00
Pria or Add-on to Metformin Therapy in Pediatric Inc. Subjects With Type 2 Diabetes Mellitus
180310 Raghavan, Online Modules to Train Medical Staff in Best Autism Speaks
Kalyani Practices for Kids With ASD During Medical Inc. Procedures
Rubin, The Genetics and Neuroendocrinology of Shor Eli Lilly
Karen Stature International Study
Karen
Girls Turner Syndrome Eli
Mechanism of Impaired Mycobacteria Sensing
Juan by TLR2 & TLR4 Polymorphic Variants NIAID (UCHC)
179377 Salazar, Ryan White A
Juan (City of Hartford)
179388 Salazar, Phagosomal Signals Shape Inflammatory DHHS/NIH 7/1/15
Juan Responses to Borrelia Burgdorferi (UCHC)
Salazar, Phagosomal Signals Shape Inflammatory NIH 7/1/16
Juan Responses to Borrelia Burgdorferi
179394 Salazar, Ryan White D DHHS/HRSA 8/1/15
Juan (UCHC)
Juan Consortium
Salazar, Ryan White A
Juan (City of Hartford) Salazar, Ryan White B DPH 4/1/16
Juan
Juan (UCHC)
Salazar, CT DPH HIV Prevention Interventions 2012 DPH
Juan Salazar, Hartford Teenage Pregnancy Prevention DHHS/City of 7/1/16
Juan Initiative (HTPPI) Hartford
Salazar, ARC - Use of Diversity Outbred Mice to Study Jackson
Olga Cardiotoxicity of Chemo Laboratory
180326 Salazar, Establishing Cardiac Magnetic Resonance Hartford
Olga Imaging as the Standard Care for Childhood Foundation for Cancer Patients Public Giving
180268 Santos, Pain & Weight Treatment CT Institute for 7/1/15
Melissa Clinical & Translational Science (CICATS)
180304 Santos, Creating Pain and Weight Treatment CHIP (UCONN 5/15/15 12/31/16
Melissa Storrs)
180824 Schoem, A Prospective, Randomized, Double-blind, Otonomy, Inc. 1/1/15
Scott Sham-controlled, Multi-center, Phase 3 Study of OTO-201 Given as a Single Intratympanic Injection for Intra-operative Treatment of Middle Ear Effusion in Pediatric Patients Requiring Tympanostomy Tube Replacement
179375 Silva, Integrative Proteomics & Metabolomics for “DHHS/NIH/ 1/1/15 12/31/26
Cynthia Pediatric Glomerula Disease Biomarkers NIAID (Nationwide Children’s Hospital)”
Primary/
Secondary
180337 Silva, NephCure Kidney Foundation - CureGN NephCure 1/21/15
Cynthia Kidney Foundation (Nationwide Children’s Hospital)
180328 Simoneau, Optimization of Home Oxygen Weaning in Patient-Centered 1/1/15
Tregony Premature Infants Outcomes Research Institute (Boston Children’s)
179649 Slivka, Childhood Lead Poisoning Program CT/DPH 7/1/15 6/30/16
Hilda Tang- Development of a Vascularized and Perfused Internal – 3/1/16
Schomer M D3-D Human Brain Model Stimulus
180845 Tory, Efficacy, Safety and Tolerability of Tofacitinib for Pfizer, Inc. 5/1/16
Heather Treatment of Polyarticular-course Juvenile Idiopathic Arthritis (JIA) in Children and Adolescent Subjects
180341 Valdez, Tulio Short Wave Infrared Otoscope for Otitis Media Connecticut 8/24/16
Diagnosis Innovation (UConn Storrs)
180365 Valdez, Tulio Technology Commerialization UCONN Spark 4/18/16 12/31/16
Fund
180810 Valdez, Tulio A Multi-center, Randomized, Double-blind Salvat, SA 1/1/15
Clinical Trial to Assess the Efficacy and Safety of Ciprofloxacin 0.3% Plus Fluocinolone Acetonide 0.025% Otic Solution Compared to Ciprofloxacin 0.3% Otic Solution and to Fluocinolone Acetonide 0.025% Otic Solution in the Treatment of Acute Otisis Media With Tympanostomy Tubes (AOMT) in Pediatric Patients
179439 Waynik, Airway Microbiome and Age 6y Asthma
DHHS/NIH 9/21/16
Ilana Phenotypes in Two Diverse Multi-center Cohorts (Mass General)
179379 Waynik, Infant-specific IgE, Rhinovirus C Bronchiolitis, DHHS/NIH 12/1/15 11/30/16
Illana and Incident Asthma in MARC-35 (Mass General)
180822 Waynik, Pediatric Intravenous Versus Oral Antibiotic Patient Centered 1/1/15
Illana Theory (PIVVOT) Outcomes Research Inst. (CHOP)
180852 Weinstein, A Comparison of Glycosade® and Uncooked (International) 12/29/16
David Cornstarch (UCCS) for the Dietary Limited, a Nestle Management of Hepatic Glycogen Storage Health Science Diseases (GSD), Glyde Trial company
180826 Weiss, Hirschsprung Disease Research Collaborative Johns Hopkins
Richard (HDRC Study) University
180828 Wolkoff, A Phase Ib/IIa Randomized, Placebo-controlled Sigma-Tau
Leslie Study of the Safety and Efficacy of Once Pharmaceuticals, Daily Dosing of STP206 in Premature Very Low Inc. Birth Weight and Extremely Low Birth Weight Neonates
180835 Wolkoff, Multi-center Observational Study Regarding the Astra Zeneca 3/6/15
Leslie Non-interventional Surveillance Study of Pharmaceuticals, Respiratory Syncytial Virus Hospitalizations LP Among Infants Born at 29 to 35 Weeks Gestational Age Not Receiving Immunoprophylaxis
180323 Zemel, Observational Study of Pediatric Rheumatic CARRA (Duke 11/1/15 12/31/16
Lawrence Diseases: The CARRA Registry University)
180742 Zemel, A 12-week Randomized, Double-blind, Roche 1/1/15
Lawrence Placebo-controlled, Parallel-group, Two-arm Laboratories, Inc. Study to Evaluate the Efficacy and Safety of Tocilizumab in Patients With Active Juvenile Idiopathic Arthritis: With 92-week Single-arm Open-label Extension to Examine the Long-term Use of Tocilizumab
180794 Zemel, Phase 3, Multi-center, Open-label Study to UCB, Inc. 1/1/15 12/31/16
Lawrence Assess the Pharmacokinetics, Safety and Efficacy of Certolizumab Pegol in Children and Adolescents With Moderately to Severely Active Polyarticular-course Juvenile Idiopathic Arthritis
180813 Zemel, A Phase 3 Multi-center, Open-Label Study to Bristol-Meyers 1/1/15
Lawrence Evaluate Pharmacokinetics, Efficacy and Safety Squibb of Abatacept Administered Subcutaneously (SC) in Children and Adolescents with Active Polyarticular Juvenile Idiopathic Arthritis (pJIA) and Inadequate Response (IR) to biologic or non biologic Disease Modifying Anti-rheumatic Drugs (DMARDs)
180817 Zemel, An Phase Ib Open Label Multi-Center Study to Genentech 1/1/15
Lawrence Investigate Pharmacokinetics, Pharmacodynamics, and Safety of Tocilizumab Following Subcutaneous Adminitration in Patients with Polyarticular-Course Juvenile Idiopathic Arthritis
180818 Zemel, A Phase Ib Open-label Multi-center Study to Genentech
Lawrence Investigate Pharmacokinetics, Pharmacodynamics, and Safety of Tocilizumab Following Subcutaneous Administration in Patients With Systemic Juvenile Idiopathic Arthritis
180834 Zemel, ß-SPECIFIC 4 Patients: Study of Pediatric Novartis 1/1/15 12/31/16
Lawrence Efficacy and Safety With First-line Use of Canakinumab. An Open-label Canakinumab (ACZ885) Dose Reduction or Dose Interval Prolongation Efficacy and Safety Study in Patients With Systemic Juvenile Idiopathic Arthritis (SJIA)
179434 Zempsky, iCanCope With Sickle Cell Disease
DHHS/NIH/ 9/1/2016 12/31/16
William /NICHD (Seattle Children’s Research Institute) 180358 Zempsky, Strategies for Education in the Emergency Donaghue
William Department (SEED) Foundation
180802 Zempsky, An Open-label, Multi-center Study of the Safety, Purdue Pharma, 1/1/15 12/31/16
William Pharmacokinetics, and Efficacy of LP Buprenorphine Transdermal System (BTDS) Opiod Analgesia for Moderate to Severe Pain

Wishing everyone a healthy, successful, positive 2017
‘They may forget your name, but they will never forget how you made them feel.’

Connecticut Children’s Medical Center complies with applicable Federal civil rights laws and does not discriminate on the basis of race, color, national origin, age, disability, or sex.
ATENCIÓN: si habla español, tiene a su disposición servicios gratuitos de asistencia lingüística. Llame al 1-800-234-0780 (TTY: 1-800-545-8330).
UWAGA: Jeżeli mówisz po polsku, możesz skorzystać z bezpłatnej pomocy językowej. Zadzwoń pod numer 1-800-234-0780 (TTY: 1-800-545-8330).
Connecticut Children’s Medical Center is the only hospital in Connecticut dedicated exclusively to the care of children. Connecticut Children’s is a nationally recognized not-for-profit with a medical staff of more than 1,000 providing comprehensive, world-class health care in more than 30 pediatric specialties and subspecialties. Connecticut Children’s Medical Center is the primary pediatric teaching hospital for the UConn School of Medicine, has a teaching partnership with the Frank H. Netter MD School of Medicine at Quinnipiac University and is a research partner of Jackson Laboratory. Connecticut Children’s Office for Community Child Health is a national leader in community-based prevention and wellness programs.
To learn more about Connecticut Children’s Medical Center, please visit connecticutchildrens.org.


