Cryotherapy in Endodontics Chronic Disease Management










DECEMBER 2022 Vol 50 n Nº 12 Persistence and Commitment: Unparalleled Advocacy in 2022 — A Game Changer for Vulnerable Californians
Journa CALIFORNIA DENTAL ASSOCIATION December 2022



coverages
agent or broker
agreements with our partner insurance carriers. Eligibility, available coverage limits and discounts vary
carrier
carrier underwriting.
provided
overview of the referenced product and is not intended to be a complete description of all
states.
Street, 17th Floor, Sacramento, CA 95814 | TDIC IS CA Lic. #0652783 Insurance coverage
issued by Metropolitan Life Insurance Company, 200 Park Avenue, New York, NY 10166. Like most group benefits programs, benefit programs offered by
contain certain exclusions, exceptions, waiting periods, reductions, limitations and terms for keeping them in force. Ask your plan administrator for costs and complete details. Metropolitan Life Insurance Company |
Avenue
York, NY 10166 | L0522022773[exp0524][All States][DC,GU,MP,PR,VI] © 2022 MetLife Services and Solutions, LLC. Protection for every stage of life and practice. The coverage you need at affordable MetLife group rates. DISABILITY COVERAGE Protect your investment in your profession by preparing for unexpected injuries or illnesses. Plus coverage from leading carriers. HEALTH COVERAGE Keep yourself, your family and your whole team well. Find affordable Individual & Family and Small Group plans from trusted carriers. LIFE INSURANCE Easily add extra protection or change coverage levels to secure your loved ones’ peace of mind and future financial well-being. Benefits paid even if you can work but can’t practice dentistry Great rates for CDA members through a MetLife group plan INSURANCE SOLUTIONS Learn more online at tdicinsurance.com/solutions Call your local TDIC Insurance Solutions advisor at 800.733.0633 Scan here to get started: Flexible choice of benefit periods and maximum benefits Financial security with up to 60% of your income covered
TDIC Insurance Solutions offers other
as an
by
by
and are subject to
The information
here is an
terms, conditions and exclusions. Not available in all
TDIC Insurance Solutions | 1201 K
is
MetLife
200 Park
| New
departments
The Editor/Student Debt: American Dream or American Nightmare
Thank You to 2022 Journal Reviewers
Impressions
RM Matters/Digital Accessibility Lawsuits Are on the Rise: Is Your Website AwDA Compliant?
Regulatory Compliance/What Prescribers Should Know
Tech Trends
Index to 2022 Articles
Persistence and Commitment: Unparalleled Advocacy in 2022 — A Game Changer for Vulnerable Californians, a Commentary
CDA advocated tirelessly for targeted investments to improve dental pipeline opportunities and expand apprenticeship programs to address the dental staff shortages being experienced across the state.
Jared I. Fine, DDS, MPH
Cryotherapy in Endodontics: A Critical Review
This paper reviews the applications of cryotherapy in endodontics including its effects on post-endodontic pain, effectiveness against endodontic infections, hazardous effects on dentin and efficacy on cutting efficiency of Ni-Ti rotary instruments.
Zahed Mohammadi, DDS, MSc; Sousan Shalavi, DDS; and Hamid Jafarzadeh, DDS, MSc
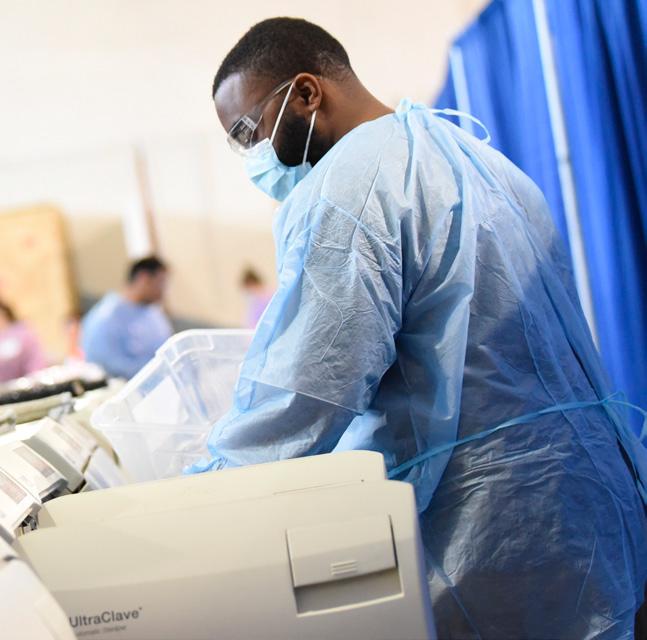
Integrated Approaches to Preventing and Managing Chronic Diseases: Colorado’s Diabetes Cardiovascular Disease Oral Health Integration Program
This paper describes Colorado’s integration strategies for leveraging clinical safety net and public health workforces to address the most pressing health care needs of underserved communities, with a focus on preventing and managing (pre)diabetes, (pre)hypertension and oral diseases.
Katya Mauritson, DMD, MPH(c); Sara Grassemeyer, MPH; Ian Danielson, MPA; and Abby Laib, MS
CDA JOURNAL, VOL 50 , Nº 12 DECEMBER 2022 711
DEC. 2022
719
features 717
715 727 733 C.E. Credit 745 719 753 755
749 723
published by the California Dental Association
1201 K St., 14th Floor Sacramento, CA 95814 800.232.7645 cda.org
CDA Officers
Ariane R. Terlet, DDS President president@cda.org
John L. Blake, DDS President-Elect presidentelect@cda.org Carliza Marcos, DDS Vice President vicepresident@cda.org
Max Martinez, DDS Secretary secretary@cda.org
Steven J. Kend, DDS Treasurer treasurer@cda.org
Debra S. Finney, MS, DDS Speaker of the House speaker@cda.org
Judee Tippett-Whyte, DDS Immediate Past President pastpresident@cda.org
Journa
CALIFORNIA DENTAL ASSOCIATION
Management
Peter A. DuBois Executive Director
Carrie E. Gordon Chief Strategy Officer
Alicia Malaby Communications Director
Editorial
Kerry K. Carney, DDS, CDE Editor-in-Chief Kerry.Carney@cda.org
Ruchi K. Sahota, DDS, CDE Associate Editor
Marisa Kawata Watanabe, DDS, MS Associate Editor
Gayle Mathe, RDH Senior Editor
Andrea LaMattina, CDE Publications Manager
Kristi Parker Johnson Communications Manager Blake Ellington Tech Trends Editor
Jack F. Conley, DDS Editor Emeritus
Robert E. Horseman, DDS Humorist Emeritus
Production Danielle Foster Production Designer
Upcoming Topics
January/Public Health Initiatives
February/General Topics March/Oral Appliances
Advertising Sue Gardner Advertising Sales Sue.Gardner@cda.org 916.554.4952
Volume 50 Number 12 December 2022
Permission and Reprints
Andrea LaMattina, CDE Publications Manager Andrea.LaMattina@cda.org 916.554.5950
Manuscript Submissions
www.editorialmanager. com/jcaldentassoc


Letters to the Editor www.editorialmanager. com/jcaldentassoc
Journal of the California Dental Association Editorial Board
Charles N. Bertolami, DDS, DMedSc, Herman Robert Fox dean, NYU College of Dentistry, New York
Steven W. Friedrichsen, DDS, professor and dean emeritus, Western University of Health Sciences College of Dental Medicine, Pomona, Calif.
Mina Habibian, DMD, MSc, PhD, associate professor of clinical dentistry, Herman Ostrow School of Dentistry of USC, Los Angeles
Robert Handysides, DDS, dean and associate professor, department of endodontics, Loma Linda University School of Dentistry, Loma Linda, Calif.
Bradley Henson, DDS, PhD, interim vice president research & biotechnology, associate dean for research and biomedical sciences and associate professor, Western University of Health Sciences College of Dental Medicine, Pomona, Calif.
Paul Krebsbach, DDS, PhD, dean and professor, section of periodontics, University of California, Los Angeles, School of Dentistry
Jayanth Kumar, DDS, MPH, state dental director, Sacramento, Calif.
Lucinda J. Lyon, BSDH, DDS, EdD, associate dean, oral health education, University of the Pacific, Arthur A. Dugoni School of Dentistry, San Francisco
Nader A. Nadershahi, DDS, MBA, EdD, dean, University of the Pacific, Arthur A. Dugoni School of Dentistry, San Francisco
The Journal of the California Dental Association (ISSN 1942-4396) is published monthly by the California Dental Association, 1201 K St., 14th Floor, Sacramento, CA 95814, 916.554.5950. The California Dental Association holds the copyright for all articles and artwork published herein.


The Journal of the California Dental Association is published under the supervision of CDA’s editorial staff. Neither the editorial staff, the editor, nor the association are responsible for any expression of opinion or statement of fact, all of which are published solely on the authority of the author whose name is indicated. The association reserves the right to illustrate, reduce, revise or reject any manuscript submitted. Articles are considered for publication on condition that they are contributed solely to the Journal of the California Dental Association. The association does not assume liability for the content of advertisements, nor do advertisements constitute endorsement or approval of advertised products or services.
Copyright 2022 by the California Dental Association. All rights reserved.
Visit cda.org/journal for the Journal of the California Dental Association’s policies and procedures, author instructions and aims and scope statement.
Connect to the CDA community by following and sharing on social channels
@cdadentists
Francisco Ramos-Gomez, DDS, MS, MPH, professor, section of pediatric dentistry and director, UCLA Center for Children’s Oral Health, University of California, Los Angeles, School of Dentistry
Michael Reddy, DMD, DMSc, dean, University of California, San Francisco, School of Dentistry
Avishai Sadan, DMD, dean, Herman Ostrow School of Dentistry of USC, Los Angeles
Harold Slavkin, DDS, dean and professor emeritus, division of biomedical sciences, Center for Craniofacial Molecular Biology, Herman Ostrow School of Dentistry of USC, Los Angeles
Brian J. Swann, DDS, MPH, chief, oral health services, Cambridge Health Alliance; assistant professor, oral health policy and epidemiology, Harvard School of Dental Medicine, Boston
Richard W. Valachovic, DMD, MPH, president emeritus, American Dental Education Association, Washington, D.C.
CDA JOURNAL, VOL 50 , Nº 12 712 DECEMBER 2022
Renew today at cda.org/renew renew EDUCATION RESOURCES RESEARCH ADVOCACY PROTECTION SUPPORT SAVINGS EXPERTISE CONNECTION EDUCATION RESOURCES RESEARCH ADVOCACY PROTECTION SUPPORT SAVINGS EXPERTISE Is your membership set for 2023? Don’t wait to lock in benefits built just for California dentists. Access one-on-one expert guidance, engaging C.E. across learning formats, tools that save time and money, and constant connection to trusted news and resources. It’s easy to pay dues online or choose convenient monthly payments. YOUR MEMBERSHIP ®
Create smiles. Change lives.
CDA Foundation volunteers and donors truly change the lives of others. Through your generosity, Californians in underserved communities gain access to dental treatment that relieves pain, restores dignity, creates smiles and opens more opportunities.


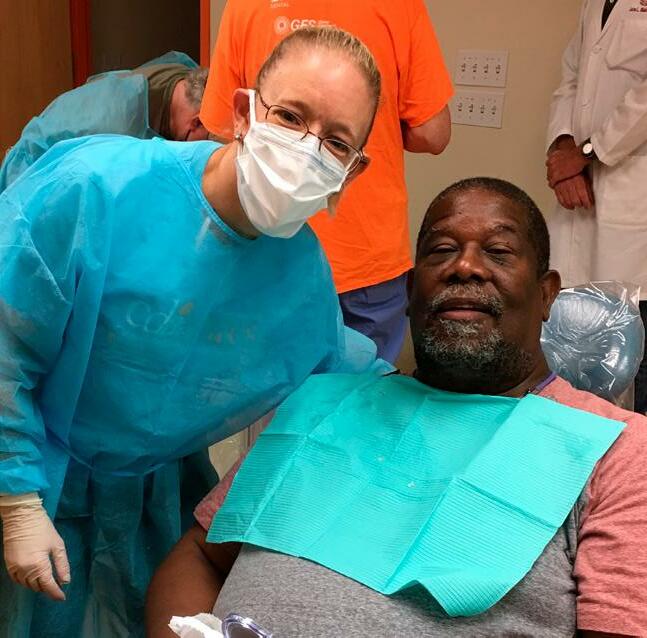



.
See ways to give at cdafoundation.org
Student Debt: American Dream or American Nightmare
Kerry K. Carney, DDS, CDE

Sometimes you can stew about something for a long time and never quite put your finger on the problem. That happened to me this weekend when I read an article by Ron Lieber about student loans and why they are so complicated.1 It made me wonder how paying for a dental education could have spiraled so completely out of control like a top that’s lost its momentum. It made me look at the world a generation ago and compare it with the world that new dentists graduate into now.
I remember chatting with a new dentist at a meeting more than 10 years ago. He told me his debt was over $250,000 and that he would be paying it off over 20 years. He was making payments of about $4,000 a month. That seemed like a mortgage payment to me, but after the loan was repaid, there would be no house, nothing tangible. Funds directed toward the repayment of student loans over 20-25 years diverts money that could have (should have) been invested or saved for retirement. (Where is that reverse mortgage for your dental education?)
It made me think about my motivations to pursue a degree in dentistry all those years ago. A degree in dentistry would require an investment of my time and my efforts in exchange for a profession that helped me to help others. Also, it would provide more financial stability than many other careers I had considered. Though the training was difficult, it was well worth my investment.
Committing to a huge debt that would take decades to pay off was not part of the decision-making then. If I were considering it today, it would give me pause. Many of us were brought up to avoid going into debt on
pain of death. Grants, scholarships, work/ study and side jobs were how some of us made it through school. The indebtedness hurdle can turn away good applicants who haven’t sufficient assets or access to assets or who just do not have the support system or confidence to overcome that barrier.
According to reports, the tremendous debt burden of new dentists influences many life decisions they may weigh: where they choose to practice, what kind of practice to join, whether to specialize, enter into public health or academia. Student loan debt even influences decisions about whether or when to begin a family. Buying a practice or starting a practice from scratch may not be possible for a new dentist already laboring to repay student debts.
There is so much money tied up with educational loans it should be a national embarrassment.
“Average educational debt for all indebted dental school graduates in the class of 2021 was $301,583, with the average for public and private schools at $261,226 and $354,901 respectively.”2 There are 70 accredited dental schools in the United States.3
In 2021, 6,665 students graduated from dental schools in the U.S. An American Dental Education Association (ADEA) report states that a little over 17% of the graduating students reported no debt. That seems to indicate the class of 2021 owed a
total of $1,668 million or $1.7 billion dollars. Does anyone else think something is wrong here?
New dentists in the ‘80s were beneficiaries of government programs that gave financial support to dental schools. We were seeking higher education in a time when there was a “general good” social contract. The idea was that those who improved themselves through higher education would eventually more than make up for the subsidies the country had provided for that education.
It was expected that we would provide increased services and pay higher taxes based on our higher incomes. We were encouraged and supported monetarily so that when we became contributing members of society, we would be part of the improvement of conditions for everyone. Later, these government subsidies were phased out as the burden of the cost of the education was shifted to the education consumer, the student.
In the 1980s and ‘90s, we started operating under a new set of questions: What is the cost of a dental education? What is the monetary return on the cost of one’s education? Who (or what entity) should be paying the cost of that education? How much can the consumer student invest based on the return on investment (ROI) model?
In order to help students finance their
CDA JOURNAL, VOL 50 , Nº 12 DECEMBER 2022 715 Editor
The idea of 'return on investment' has become the measuring stick and deciding metric for life choices and educational investment.
education, loans were designed to allow parents to take on more debt. These “PLUS loans” have become predatory in the sense that the amount borrowed is not aligned with the family’s income and ability to repay.4 Not only were new graduates mired in debt but families could be ensnared into unrepayable debts to help defray the debt burden on the student. The ROI was the rationale for indebtedness.
The idea of ROI has become the measuring stick and deciding metric for life choices and educational investment. So where did this ROI metric come from?
Frank Donaldson Brown was a brilliant electrical engineer who became an executive at DuPont and General Motors. He was the originator of the DuPont model of analysis. That model has become known as ROI analysis today. It was used to evaluate products, decide on new product investment and set the price for car models. It is now used in many environments as a basis for decisions. In dentistry, it is not only used when pitching the purchase of expensive equipment to dentists (“Your ROI on this $150,000 piece of equipment is less than 15 months. You would be foolish not to finance the purchase.”), but also as the basis for life decisions, like going to dental school.
In 2022, eight pieces of legislation that target dental school debt are being considered in Congress. All except one have to do with calculating or accumulating interest. Dental education cost reform is not addressed.
It made me think of my favorite quote from Thomas Pynchon, the author of “Gravity’s Rainbow:” “If they can get you asking the wrong questions, they don’t have to worry about answers.”
It feels like we keep asking the wrong questions when it comes to student debt. Instead of asking how can we make
borrowing easier? How can we make huge debts repayable over a lifetime? How can we provide more money in the form of loans to students and their families?
Why aren’t we asking:
■ How can we reduce the cost of education for the dental student?
■ How can we remove the financial restrictions on where and how new dentists practice?
■ How can we shift more financial support to the schools that provide dental education and thereby shift the education costs off the backs of students?
■ How can we provide more service commitment opportunities to allow all students who want to defray the cost of their education the chance to contract for their postgraduate service within areas or populations in need?
■ How can we remove the specter of decades of debt that discourage underrepresented categories of dental school applicants?
■ How do we keep from ensnaring the parents of students into committing to impossible-to-repay debt burdens?
■ Are we misappropriating Donaldson Brown’s ROI metric?
■ Exactly what is being invested and what are the returns?
Student debt is a complicated issue, but surely it deserves our utmost effort to ask the right questions. ■
REFERENCES
1. Lieber R. Why Aren’t Student Loans Simple? Because This Is America. The New York Times Sept. 3, 2022.
2. American Dental Education Association. Educational debt
3. Hanson M. Average Dental School Debt. EducationData.org Oct. 11, 2021.
4. Lieber R. The Subprime Loans for College Hiding in Plain Sight The New York Times Sept. 17, 2022.
The Journal welcomes letters
We reserve the right to edit all communications. Letters should discuss an item published in the Journal within the last two months or matters of general interest to our readership. Letters must be no more than 500 words and cite no more than five references. No illustrations will be accepted. Letters should be submitted at editorialmanager.com/ jcaldentassoc. By sending the letter, the author certifies that neither the letter nor one with substantially similar content under the writer’s authorship has been published or is being considered for publication elsewhere, and the author acknowledges and agrees that the letter and all rights with regard to the letter become the property of CDA.
716 DECEMBER 2022 CDA JOURNAL, VOL 50 , Nº 12
DEC. 2022 EDITOR
Reviewers
Thank You to the 2022 Reviewers
The Journal of the California Dental Association is grateful for the many professionals who formally reviewed manuscripts in 2022 and offered their recommendations. We extend our thanks to those who are instrumental in helping us produce this award-winning scientific publication.
Maha Ahmad, PhD
Tamer Alpagot, DDS, PhD
Pamela Arbuckle Alston, DDS, MPP
Baharak Amanzadeh, DDS, MPH
Clarisa Amarillas Gastelum, DDS, MS
Craig W. Amundson, DDS
Homayon Asadi, DDS
Phimon Atsawasuwan, DDS, MSc, MSc, MS, PhD
David M. Avenetti, DDS, MPH, MSD
Leif K. Bakland, DDS
Sepideh Banava, DDS, MSc, MBA, MPH, DABDPH
Nicole Barkhordar, DDS, MEd
Steven Bender, DDS
Beatriz Bezerra, DDS, PhD
Patrick Blahut, DDS, MPH
John L. Blake, DDS
Robert L. Boyd, DDS
Donald L. Branam, BS, PharmD
Carolyn Brown, DDS
Michael E. Cadra, DMD, MD
Paulo Camargo, DDS, MS, MBA
Tom Campbell, DDS
Hsun-Liang Chan, DDS, MS
Hubert Chan, DDS
Jennifer Chang, DDS, MSD
Kai Chiao Joe Chang, DDS, MS
Daniel Chavarria, DDS, PhD
Yo-wei Chen, DDS, MSc
Russell Christensen, DDS
Paul K. Chu, DDS
Stephen Cohen, DDS
Fadie T. Coleman, PhD
James J. Crall, DDS, ScD
Gerald E. Davis, DDS, MA, MS
Nancy Dewhirst, RDH
Evelyn Donate-Bartfield, PhD
Bruce Donoff, DMD, MD
Gary L. Dougan, DDS, MPH
Chad Edwards, DDS
Alec Eidelman, DMD, MPH
Jared Ira Fine, DDS ,MPH
Dana Fischer, MPH, CHES
Jason Flores, DDS, MHA, BSN-RN
David F. Fray, DDS, MBA
Steven Friedrichsen, DDS
Lawrence Gettleman, DMD, MSD
Alan H. Gluskin, DDS
Jay Golinveaux, DDS, MS
Anupama Grandhi, DDS
Richard J. Gray, DDS
Rishi Jay Gupta, DDS, MD, MBA
Mina Habibian, DMD, MS, PhD
Colin Haley, DDS, MEd
Yusuke Hamada, DDS, MSD
Lisa Anne Harpenau, DDS, MS, MBA, MA
Bradley Henson, DDS, PhD
Edmond Hewlett, DDS
Nicole Holland, DDS, MS
Katrina Holt, MPH, MS, RD
Nicola P.T. Innes, PhD, BDS, BSc, BMSc
Lisa Itaya, DDS
Parvati Iyer, DDS
Douglass Jackson, DMD, MS, PhD
Poonam Jain, BDS, MS, MPH
David E. Jaramillo, DDS
Dwight Jennings, DDS
Judith Ann Jones, DDS, MPH, DScD
Cristin E. Kearns, DDS, MBA
Reuben Kim, DDS, PhD
Gary D. Klasser, DMD
Jens Kreth, PhD
Max Kubitz, DDS Jayanth Kumar, DDS, MPH Satish Kumar, DMD, MDSc, MS Wey-Wey Kwok, JD Huong Le, DDS
Irving Lebovics, DDS Alexander Lee, DMD
Felix Lee, DMD
Stuart E. Lieblich, DMD Oariona Lowe, DDS
Cindy Lyon, RDH, DDS, EdD
Mark D. Macek, DDS, DrPH
Ilay Maden, BDS, MSc, PhD
Taraneh Maghsoodi, DDS, MS
Kristen Marchi, MPH
Malay Mathur, DDS
Melanie E. Mayberry, DDS, MS
Keith A. Mays, DDS, MS, PhD
Kevin McNeil, DDS
Diana Messadi, DDS, MMSc, DMSc
Peter Milgrom, DDS
Shelley Miyasaki, DDS, PhD
Mauricio Montero-Aguilar, DDS, MSc
Jean Moore, DrPH, MSN
Richard P. Mungo, DDS, MSD, MeD
Carol Anne Murdoch-Kinch, DDS, PhD
Theodore A. Murray Jr., DDS
Asma Muzaffar, DDS, MS, MPH
Richard J. Nagy, DDS
Mahvash Navazesh, DMD
Man Wai Ng, DDS, MPH
Carol Niforatos, DDS
Nooshin Noghreian, DDS
Enihomo Obadan-Udoh, DDS, MPH, DrMedSc
Heesoo Oh, DDS
David Ojeda, DDS
Joan Otomo-Corgel, DDS, MPH
Mariela Padilla, DDS, MEd
Robert J. Palmer Jr., PhD
Seena Patel, DMD, MPH
Kimberlie Payne, RDH, BA
Shakalpi Pendurkar, DDS, MPH
Steven Perlman, DDS, MScD, DHL
Patricia Podolak, DDS, MPH
Howard F. Pollick, BDS, MPH
Kiddee Poomprakobsri, DDS, MSD, MBA
CDA JOURNAL, VOL 50 , Nº 12 DECEMBER 2022 717
CONTINUED ON PAGE 718
Lori Rainchuso, DHSc, MS, RDH
Karen Raju, BDS, MPH
Diana E. Ramos, MD, MPH, MBA
Rajesh Raveendranathan, BDS,
Lindsay Rosenfeld, ScD, ScM
David Lawrence Rothman, DDS

Danielle Rulli, RDH, MS, DHSC
Mark Ryder, DMD
Elise Sarvas, DDS, MSD, MPH
Carlos S. Smith, DDS, MDiv
Hugo Sousa Dias, DDS
Leah Stein Duker, PhD
Charles Stewart, DMD
Piedad Suárez Durall, DDS


Tamanna Tiwari, MPH, MDS, BDS
Richard D. Trushkowsky, DDS
Philip Vassilopoulos, DDS, DMD
Timothy F. Walker, BS, MS, DDS
CDA JOURNAL, VOL 50 , Nº 12 CONTINUED FROM PAGE 717 DEC. 2022 REVIEWERS
*Take 15% off Premium and 5% off Basic Job Post or Resume Search. Scan QR code to apply savings. Offer expires 12/31/22 Trouble Hiring? We can help. Find more dental professionals with the #1 dental job board. SAVE 15% * Redeem Offer
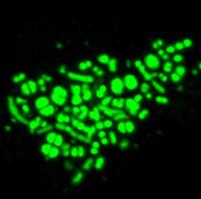
Microbes Form Superorganisms That Spread on Teeth

A cross-kingdom partnership between bacteria and fungi can result in the two joining to form a “superorganism” with unusual strength and resilience. These microbial groupings, found in the saliva of toddlers with severe childhood tooth decay, can effectively colonize teeth, according to a study by University of Pennsylvania School of Dental Medicine scientists. The study was published in Proceedings of the National Academy of Sciences. The research team discovered the assemblages were stickier, more resistant to antimicrobials and more difficult to remove from teeth than either the bacteria or the fungi alone. What’s more, the assemblages unexpectedly sprout “limbs” that propel them to “walk” and “leap” to quickly spread on the tooth surface, despite each microbe on its own being nonmotile.
“This started with a very simple, almost accidental discovery, while looking at saliva samples from toddlers who develop aggressive tooth decay,” said Hyun (Michel) Koo, DDS, MS, PhD, a professor at Penn Dental Medicine and co-corresponding author of the paper.
In the past, Dr. Koo’s lab has focused on the dental biofilm present in children with severe tooth decay, discovering that both bacteria – Streptococcus mutans – and fungi – Candida albicans – contribute to the disease. The discoveries came about when Zhi Ren, PhD, a postdoctoral fellow, was using microscopy that allows scientists to visualize the behavior of living microbes in real time.
After seeing the bacterial-fungal clusters present in the saliva samples, the researchers were curious how the groupings might behave once attached to the surface of a tooth. They created a laboratory system to recreate the formation of these assemblages, using the bacteria, fungi and a tooth-like material, all incubated in human saliva. The platform enabled the researchers to watch the groupings come together and to analyze the structure of the resulting assemblages. The team found a highly organized structure with bacterial clusters attached in a complex network of fungal yeast and filament-like projections called hyphae, all enmeshed in an extracellular polymer, a glue-like material.
Next, the researchers tested the properties of the assemblages once they had colonized the tooth surface and found surprising behaviors and emergent properties, including enhanced surface adhesion, making them very sticky, and increased mechanical and antimicrobial tolerance, making them tough to remove or kill.
Although the exact mechanisms are unknown, the assemblages’ ability to “move as they grow” enables them to quickly colonize and spread to new surfaces. When the research team allowed the assemblages to attach to and grow on real human teeth in a laboratory model, they found more extensive tooth decay as a result of a rapidly spreading biofilm.
Because these assemblages are found in saliva, targeting them early on could be a therapeutic strategy to prevent childhood tooth decay, said Dr. Koo. ■
CDA JOURNAL, VOL 50 , Nº 12 DECEMBER 2022 719 Impressions
Study Finds No Adverse Effects of Early Fluoride Exposure on Childhood Development
An Australian nationwide, populationbased, follow-up study published in the Journal of Dental Research has provided evidence that exposure to fluoridated water by young children was not negatively associated with child emotional, behavioral development and executive functioning in their adolescent years.
The study by Prof. Loc Do, PhD, of the University of Queensland Faculty of Health and Behavioural Sciences, School of Dentistry and colleagues examined the effect of early childhood exposures to water fluoridation on measures of schoolage executive functioning and emotional and behavioral development in a population-based sample. This longitudinal follow-up study used information from Australia’s National Child Oral Health Study of 2012-14. Children aged 5-10 years at the baseline were contacted again after seven to eight years, before they had turned 18.
Percent lifetime exposed to fluoridated water (% LEFW) from birth to the age of 5 years was estimated from residential history and postcode-level fluoride levels in public tap water. Measures of children’s emotional and behavioral development were assessed by the Strength and Difficulties Questionnaire (SDQ), and executive functioning was measured by the Behavior Inventory of Executive Functioning (BRIEF). Multivariable regression models were generated to
Genetic Defects Lead to Enamel Malformations

A team of researchers from the Center of Dental Medicine at the University of Zurich has identified a key gene network that is responsible for severe tooth enamel defects. The study was published in the journal iScience

Using various genetically modified mouse models, the scientists analyzed the effects of the Adam10 molecule, which is closely linked to the Notch signaling pathway. This signaling pathway enables communication between adjacent cells, is essential for embryonic development and plays a crucial role in the development of severe human pathologies such as stroke and cancer. To study the role of the Adam10/Notch signaling in the formation and pathology of tooth enamel in detail and to analyze cellular and enamel structure modifications in teeth upon gene mutation, the researchers used state-of-the-art genetic, molecular and imaging tools.
The scientists were able to demonstrate that a close link between impaired Adam10/ Notch function and enamel defects. “Mice carrying mutations of Adam10 have teeth with severe enamel defects,” said Thimios Mitsiadis, DDS, PhD, professor of oral biology at the Center of Dental Medicine and leader of this study. “Adam10 deletion causes disorganization of the ameloblasts, which then leads to severe defects in both the structure and mineral composition of the enamel.” Adam10-dependent Notch signaling is thus not only involved in severe pathological conditions, but also in the organization and structure of the developing tissues, such as teeth.
Understanding the genetic code that controls tooth development, the knowledge of the molecular connections during enamel formation and the impact of mutations leading to enamel malformations opens new horizons in the field of prevention and treatment, said Dr. Mitsiadis. “The requirements for enamel repair and de novo formation are extremely complex, but new genetic and pharmaceutical tools targeting impaired tooth enamel formation will enable us to considerably improve dental care in the future.”
compare the associations between the exposure and the primary outcomes, controlled for covariates. An equivalence test was also conducted to compare the primary outcomes of those who had 100% LEFW against those with 0% LEFW. Sensitivity analysis was also conducted. A total of 2,682 children completed SDQ and BRIEF, with mean scores of 7.0 (95% CI: 6.6, 7.4) and 45.3 (44.7, 45.8), respectively. Those with lower % LEFW tended to have poorer scores on the SDQ
and BRIEF. Multivariable regression models reported no association between exposure to fluoridated water and the SDQ and BRIEF scores. Low household income, identifying as Indigenous and having a neurodevelopmental diagnosis were associated with poorer SDQ/BRIEF scores.
The study concluded that exposure to fluoridated water during the first five years of life was not associated with altered measures of child emotional and behavioral development and executive functioning.
CDA JOURNAL, VOL 50 , Nº 12 720 DECEMBER 2022 DEC. 2022 IMPRESSIONS
Gel Treats Gum Disease by Fighting Inflammation
A topical gel that blocks the receptor for a metabolic byproduct called succinate treats gum disease by suppressing inflammation and changing the makeup of bacteria in the mouth, according to a new study led by researchers at NYU College of Dentistry. The research, conducted in mice and using human cells and plaque
Periodontal Care May Lead to Better Outcomes
After Heart Attack
samples, lays the groundwork for a noninvasive treatment for gum disease that people could apply to the gums at home to prevent or treat gum disease. The study was published in the journal Cell Reports.
The researchers started by examining dental plaque samples from humans and blood samples from mice. Using
University of Michigan researchers who studied patients receiving periodontal care, dental cleanings or no dental care during 2016-2018 and who had acute myocardial infarction (heart attack) in 2017 found that patients who had heart attacks and received periodontal maintenance care had the shortest hospital stays and more follow-up visits, while the longest hospital stays were experienced by the no-dental-care group. The study was published in the Journal of the American Dental Association

There was no statistically significant difference between the other groups (active periodontal care and regular care) compared to the no-care group.
“After controlling for several factors, the periodontal care group had higher odds of having post-hospital visits,” said study co-author Romesh Nalliah, DDS, associate dean for patient services at the U-M School of Dentistry.

The research team wanted to examine the association between periodontal care and heart attack hospitalization and follow-up visits in the 30 days after acute care. Using the MarketScan database, they found 2,370 patients who fit the study criteria. Of those, 47% percent received regular or other oral health care, 7% received active periodontal care (root planing and periodontal scaling) and 10% received controlled periodontal care (maintenance). More than 36% did not have oral health care before they were hospitalized after a heart attack.
“Dentistry is often practiced in isolation from overall health care,” Dr. Nalliah said. “Our results add weight to the evidence that medical and dental health are closely interrelated. More studies like ours are showing that it is a mistake to practice medicine without the thoughtful consideration of the patient’s oral health.”
Improved communication between medical and dental teams could help with early intervention to ensure stable periodontal health in patients who have risk factors for heart disease, Dr. Nalliah said.
metabolomic analyses, they found higher succinate levels in people and mice with gum disease compared to those with healthy gums, confirming what previous studies have found.
They also saw that the succinate receptor was expressed in human and mouse gums. To test the connection between the succinate receptor and the components of gum disease, they genetically altered mice to inactivate, or “knock out,” the succinate receptor.
In “knockout” mice with gum disease, the researchers measured lower levels of inflammation in both the gum tissue and blood, as well as less bone loss. They also found different bacteria in their mouths: Mice with gum disease had a greater imbalance of bacteria than did “knockout” mice.
This held true when the researchers administered extra succinate to both types of mice, which worsened gum disease in normal mice; however, “knockout” mice were protected against inflammation, increases in unhealthy bacteria and bone loss.
To see if blocking the succinate receptor could ameliorate gum disease, the researchers developed a gel formulation of a small compound that targets the succinate receptor and prevents it from being activated. In laboratory studies of human gum cells, the compound reduced inflammation and processes that lead to bone loss.
The compound was then applied as a topical gel to the gums of mice with gum disease, which reduced local and systemic inflammation and bone loss in a matter of days.
CDA JOURNAL, VOL 50 , Nº 12 DECEMBER 2022 721






AUTHOR Jared I. Fine, DDS, MPH, is the former director of Dental Public Health for Alameda County. He continues as a dental public health consultant to Alameda County.
Conflict of Interest Disclosure: None reported.
Persistence and Commitment: Unparalleled Advocacy in 2022 — A Game Changer for Vulnerable Californians


 Jared I. Fine, DDS, MPH
Jared I. Fine, DDS, MPH
The 2021-2022 California budget cycle might get little notice from the casual observer except for the record budget surplus. This surplus fueled significant financial commitment to address the seemingly unending needs of the nation’s most populous state, including battling COVID-19, destructive wildfires, homelessness and housing shortages, inflation, sky-rocking gasoline prices, the multiyear drought and more. Any of these important priorities could have eaten up the state’s additional resources, so it may seem surprising that, under the radar, dentistry achieved some big wins in the state budget, making significant gains and building on previous successes in new and unprecedented ways. This was not just another day at the office. Witnessing the extraordinary legislative successes is cause for celebration for the millions of Californians who will be the beneficiaries. Yes, a sizable budget surplus had a role, but that is far from the whole story. When I was studying the piano as a young adult, my teacher instructed me to repeat any measure in which I struck the wrong note. Striking the wrong note, he

explained, is not the issue. It’s learning the dance between the notes that accounts for a successful melody. When I think about CDA’s amazing successes this year, I think my teacher’s instructions apply. What were those successful notes? And what were the dance steps that achieved such success?


$1.7






Billion for Health Care Workforce, Staff Recruitment and Training

CDA has been advocating tirelessly for targeted investments to improve dental pipeline opportunities and expand apprenticeship programs to address the dental staff shortages being experienced across the state. Expanding and diversifying the health care workforce is in this budget with hundreds of millions invested in a wide range of health care provider scholarships and loan and grant programs for which many dentists and dental team members are eligible to apply. Among other things, funding will support the work of the Health Workforce Education and Training Council, which aims to build a diverse, culturally competent health care workforce as well as multilingual health initiatives to expand scholarship

DECEMBER 2022 723 CDA JOURNAL, VOL 50 , Nº 12 commentary
repayment for multilingual applicants.
CDA is particularly supportive of two new investments:
■ $45 million to develop and expand High Road Training Partnerships for Health and Human Services.
■ $175 million over three years to the Apprenticeship Innovation Program with a focus on nontraditional apprenticeships, including in health care.
The High Road Training Partnerships (HRTP) is a public-private partnership initiative of the California Workforce Development Board to provide training and career ladder opportunities, including in dental assisting. The new budget investment builds on the HRTP funding of $75 million in last year’s budget, and CDA is in the process of applying for some of those funds to expand the association’s own dental assisting pilot program Smile Crew California.
Expanding this training throughout the state would not only help alleviate dental staffing shortages exacerbated by the COVID-19 pandemic, but also create new job opportunities for workers who were displaced.
The Apprenticeship Innovation Program, which provides grants, reimbursements and other types of funding support to programs that train apprentices, is another opportunity for CDA to help address dental workforce shortages. Funds can be used, for example, for course development and classroom instruction. CDA is already working with the Newsom administration to explore opportunities to establish dental apprenticeships. A three-year investment of an additional $60 million in fiscal years 2023-24 and 2025 is part of Gov. Gavin Newsom’s stated goal of creating 500,000 new apprenticeships across the state by 2029.
$50 Million Investment Will Expedite Care for Patients With Special Health Care Needs
Even though California has made progress to increase access to dental care in the Medi-Cal Dental Program, lack of access to care for patients with special health care needs persists as a decades-long crisis. Only a few settings are equipped to provide care for this patient population, and most settings, including dental schools, have exceptionally long wait times. These delays, which have historically been up to a year or more, have been exacerbated
These additional dental care settings will significantly expand access to care for individuals who are otherwise unable to undergo dental procedures in traditional dental offices due to special health care needs or the complexity of the care needed, including people who need special accommodations for issues of mobility, stabilization or deep sedation. According to Allen Wong, DDS, EdD, American Academy of Developmental Medicine and Dentistry president and a professor at the University of the Pacific Arthur A. Dugoni School of Dentistry in the department of diagnostic sciences, “The growing attention on inequities in health care brought on by the pandemic has shined a light on dental care, a huge unmet need for those with intellectual and developmental disabilities.
Advocacy is giving a voice to the voiceless, and they need to be heard.
by the pandemic, often requiring families to travel for hours to find a location that can provide just routine care.
The 2022-23 state budget now includes an investment of $50 million to help alleviate the long wait times and the scarcity of settings throughout the state. The $50 million investment advocated by CDA and a coalition of special needs advocates, provider groups and dental schools will fund grants to build a network of new specialty dental clinics or expand existing settings that serve patients with physical, developmental or cognitive disabilities. Successful applicants will receive up to $5 million in grant funding, need to be Medi-Cal providers and agree to serve the special needs population for at least 10 years upon completion of construction.
“This funding will not solve all the problems,” he added, “but will help to lessen some of the barriers to care while we work on improving the knowledge and comfort level of all oral health providers for this population. Advocacy is giving a voice to the voiceless, and they need to be heard. I am thankful that California has listened and is responding.
$10 Million for Grants To Develop Dental Student Clinical Rotations
CDA successfully made a budget ask of a one-time $10 million allocation to create new and enhanced communitybased clinical education rotations for dental students to improve the health of California’s underserved populations. A newly developed consortia of California dental schools will be responsible for creating these rotations with the goals of improving access to quality health care and to foster a health care workforce that is able to address current and emerging needs. Nader Nadershahi, DDS, MBA, EdD, dean and vice provost of the University of the Pacific, Arthur A. Dugoni School
724 DECEMBER 2022 CDA JOURNAL, VOL 50 , Nº 12 commentary
of Dentistry and member of the consortia noted, “Hygiene students, dental students and residents come to our programs with a purpose to help members of their communities live healthy lives. Thanks to the CDA, we will now have the resources that allow our schools to collaborate and create sustainable rotations that do not put an additional cost burden on students, enabling them to achieve their purpose.”
CDA’s advocacy was spurred on by the findings of the 2018-2028 California Oral Health Plan advisory committee, which indicated “insufficient infrastructure to promote culturally sensitive communitybased oral health programs” was a key reason for the high prevalence of dental caries and untreated caries among California’s third grade children. The committee also recommended increased collaboration between various health care, academic and public health organizations to provide care to underserved Californians. These new, self-sustaining clinical rotations will give trainees real-world experience in various dental practice models, including federally qualified health centers, private offices and mobile dentistry programs, and enhance learning in patient engagement, practice management and team-based care delivery.
Expanded Medi-Cal Benefits and Backfilled Provider Payments
CDA’s successful advocacy efforts were rewarded by substantial improvements in dental benefits, rates and initiatives in the California Medi-Cal Dental Program. These efforts built on advocacy of past years that witnessed the installment of California’s first dental director and passage of the Proposition 56 tobacco tax, which helps fund medical and oral health care programs.
The 2022-23 budget support includes:
■ A caries risk assessment bundle that includes an examination,
nutrition counseling, prophy, topical fluoride application and SDF for children ages 0 to 6 years old.
■ Expanded coverage of the adult crown benefit to include laboratoryprocessed crowns for posterior teeth. Consistent with American Dental Association evidence-based practice, lab-processed crowns provide better protection for molars than prefabricated crowns and help avoid the need for costly root canal therapy later on.
■ Extension of the CalHealthCares
These new, self-sustaining clinical rotations will give trainees real-world experience in various dental practice models.
student loan repayment program indefinitely. This program has already funded 120 dentists and will serve to encourage more dentists to provide care to the Medi-Cal population.
■ Backfilling a $31.7 million deficit in the Dental Transformation Initiative (DTI) for preventive services for children. Dentists who provided preventive services under the DTI in 2021 will receive full incentive payments for services already rendered.
■ Backfilling Proposition 56 revenues that have dropped due to reduced tobacco sales, as intended by the tax. The 2022-2023 budget supports continuation of enhanced provider
reimbursement rates with general fund dollars, a policy that has contributed to a 25% increase in Medi-Cal provider enrollment since the inception of the tax and one CDA strongly supports for the longterm stability of the program.
How Did CDA Arrive at This Momentous Advocacy Success?
To understand how CDA’s advocacy was so profoundly rewarded in 2022 is to reflect on years, actually decades, of persistence and commitment to its mission of serving the success of its members in service to their patients and the public.
CDA’s investment in care for disenfranchised populations and all Californians goes back decades. Here are a few examples:
■ Advocating for the statewide school-based dental disease prevention program.
■ Advocating for statewide community water fluoridation.
■ Incentivizing local geriatric dental care initiatives.
■ Assisting with the development and adoption of bloodborne pathogen standards in California.
■ Supporting the Californiawide First Smiles educational initiative to slow the epidemic of early childhood caries.
■ Adopting a three-phase, sevenyear strategic plan to address the barriers in access to care for one-third of Californians.
■ Advocating for a state dental director.
■ Reinstating adult Medi-Cal dental benefits after their near total elimination in the Great Recession.
■ Providing leadership in the Proposition 56 tobacco tax funding campaign and for its funding for
DECEMBER 2022 725 CDA JOURNAL, VOL 50 , Nº 12
the State Office of Oral Health and a local oral health plan in every California county.
To address the persistent and complex challenge of barriers in access to care for literally millions of Californians, the CDA House of Delegates adopted resolutions in 2002 and 2008 recognizing and committing to understanding the problem of access. The 2008 House authorized workgroups that diligently researched the issues for two years and, in 2010, proposed evidenced-based recommendations. In 2011, the formulated recommendations were presented to the house. Key recommendations focused on building a statewide dental public health infrastructure including:
■ Hiring a director with dental public health experience.
■ Developing an oral health plan, building on what exists.
■ Working with existing
stakeholders and programs.
■ Seeking federal and private funding.
■ Developing new childhood prevention programs.
The three-phase, seven-year strategic plan to address barriers in access to care that resulted from this work was adopted nearly unanimously by the 2011 CDA House of Delegates. The plan laid the foundation for CDA’s leadership in the successful 2016 Proposition 56 tobacco tax coalition and resulted in unprecedented funding in the 2017-18 state budget for health care in California. This included $140 million for supplemental Medi-Cal provider payments, full restoration of Medi-Cal adult dental benefits and $30 million of protected, firsttime funding annually for the State Office of Oral Health and local oral health programs.
This recent history has unmistakably demonstrated the importance of long-term engagement, proactive leadership, building
relations for coalitions with those of shared goals and ultimately sustained commitment. And though there is still much work to do to maximize these opportunities, now is a perfect time to pause and celebrate.
CDA’s advocacy would not have hit all the right notes if not for years of dedication to mastering the pathways. The CDA plan to address barriers in access to care states that “ … it was conceived in the context of an association whose members are part of a healing profession and bound by a public covenant and as a collective association tasked with advancing the oral health of the public as well as the profession of dentistry.” The successful CDA advocacy we have witnessed in 2022 is nothing less than historic testimony to the highest ideals of our profession. ■
THE AUTHOR, Jared I. Fine, DDS, MPH, can be reached at jaredfine@comcast.net.
726 DECEMBER 2022 CDA JOURNAL, VOL 50 , Nº 12
commentary
C.E. Credit
Cryotherapy in Endodontics: A Critical Review
Zahed Mohammadi, DDS, MSc; Sousan Shalavi, DDS; and Hamid Jafarzadeh, DDS, MSc
abstract
In medicine, cryotherapy is used to destroy tissue of both benign and malignant lesions by the freezing and rethawing process. In dentistry, cold application has been frequently employed for postoperative pain control following intraoral surgical procedures. The purpose of this paper is to review the applications of cryotherapy in endodontics including its effects on post-endodontic pain, effectiveness against endodontic infections, hazardous effects on dentin and efficacy on cutting efficiency of Ni-Ti rotary instruments, etc.
Keywords: Root canal therapy, Enterococcus faecalis, cryotherapy, endodontic pain, successful local anesthesia, fracture resistance, dentin, root surface temperature
Zahed Mohammadi, DDS, MSc, is an adjunct distinguished clinical professor at the Iranian Center for Endodontic Research (ICER), Research Institute of Dental Sciences at the Shahid Beheshti University of Medical Sciences in Tehran, Iran.
Sousan Shalavi, DDS, is an endodontic researcher in Hamedan, Iran.
Conflict of Interest Disclosure: None reported for all authors.
The term cryotherapy is derived from the Greek word cryos, meaning “cold.” Although it refers to the local or general use of low temperatures in medical therapy, cryotherapy actually does not imply implementing cold but rather extracting heat. The magnitude of the change in temperature and biophysical alterations in the tissues depends upon the differences in the temperature of the object and the heat or cold application, exposure time, thermal conductivity of the tissues and type of heat or cold agents employed. The clinical implication of this type of therapy in human tissues causes changes in the host’s local temperature.1,2
Mechanism of Action of Cryotherapy
Cryotherapy is the use of extreme cold to freeze and remove abnormal
tissue. It works by reducing the blood flow to a particular area, which can significantly decrease the inflammation degree and swelling that causes pain, especially around a tendon or a joint. It can temporarily reduce the activity of sensory nerve fibers that can also relieve the pain. When the body is vulnerable to extreme cooling, the blood vessels are narrowed and flow less to swelling areas.3–5 Once outside the cryogenic chamber, the vessels expand and an increased presence of Interleukin-10 is established in the blood. The cryotherapy chamber involves exposing individuals to freezing dry air (below −100 C) for two to four minutes.4,6
The intense cold used in cryotherapy can be produced using different substances such as liquid nitrogen, liquid nitrous oxide and argon gas. During cryotherapy, liquid nitrogen
CDA JOURNAL, VOL 50 , Nº 12 DECEMBER 2022 727 cryotherapy
AUTHORS
Hamid Jafarzadeh, DDS, MSc, is on the faculty of dentistry at the University of Toronto in Ontario, Canada, and the Dental Research Center at Mashhad University of Medical Sciences in Mashhad, Iran.
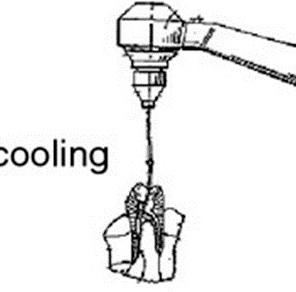
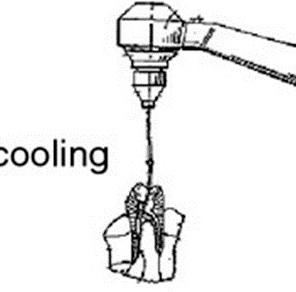
FIGURE. A dental instrument for treating teeth, provided with a needle cryogenic cooling, which receives the fluid from the refrigeration pipe conveyor. (Drawing courtesy of Giuliana Banche, PhD.)23
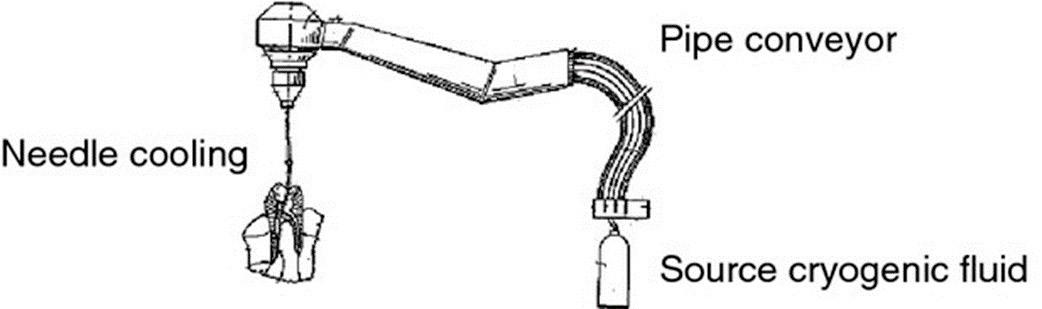
TABLE 1
Effect of Cryotherapy on Postoperative Pain
Authors
Vera et al.
Keskin et al.
Alharthi et al.
Gundogdu and Arslan
Nandakumar and Nasim
Al-Nahlawi et al.
Sadaf et al.
Monteiro et al.
or high-pressure argon gas flows into a needle-like applicator or cryoprobe.6
Cryotherapy in Medicine and Dentistry
In medicine, cryotherapy, sometimes referred to as cryosurgery, is a procedure used to destroy tissue of both benign and malignant lesions by the freezing and rethawing process. Examples of the uses of cryotherapy in medicine are the removal of various types of skin lesions, the treatment of dysplastic tissue of the uterine cervix and the treatment of some prostate cancers. Cryotherapy can also refer to the use of ice or cold packs applied to a part of the body after an injury to reduce inflammation.7
In dentistry, cold application has been frequently employed for postoperative pain control following intraoral surgical procedures.8 Although the mechanism of action and effectiveness of cryotherapy are well addressed in the literature, strong evidence to support its conclusions is lacking, except for the
Type of study
Randomized multicenter clinical trial
Effect on postoperative pain Year
Reduced the incidence of pain 2018
Reduced pain 2017 Clinical trial
Randomized controlled trial
Randomized prospective clinical trial
Randomized controlled clinical trial
Effect was not significant 2019
Reduced pain 2018
Reduced pain 2020
Reduced pain 2016 Clinical trial
Systematic review
Systematic review
Reduced pain at six and 24 hours after the procedure 2020
Reduced pain after six and 24 hours 2021
standardization of crucial factors such as the time period, duration, application mode and cold agent used. However, in recent years, a few studies were attempted and reported the intracanal use of cryotherapy in endodontics to reduce post-endodontic pain.9–12
Method Used To Apply Cryotherapy in the Root Canal
The dental instrument used for cryotherapy is equipped with a conduit of a conveyor capable of being connected to a source of fluid and a needle cryogenic cooling, which receives the fluid from the refrigeration pipe conveyor. The needle is made of a flexible material and has a smaller outer diameter (0.25 mm) than the size of the entrance inside a tooth canal so that it can be inserted into the canal tooth itself, where the cryogenic fluid is blown (FIGURE)
Cryotherapy in Endodontics Effect on Post-Endodontic Pain
In a randomized, multicenter clinical trial, Vera et al.12 showed that cryotherapy reduced the incidence of postoperative pain and the need for medication in patients presenting with a diagnosis of necrotic pulp and symptomatic apical periodontitis.
Keskin et al.11 revealed a significant reduction in postoperative pain in the cryotherapy group compared with the control group. Teeth with vital inflamed pulp were included in their study; however, they did not differentiate between asymptomatic and symptomatic pulpitis nor did they differentiate between cases with and without apical periodontitis.
In a randomized controlled trial, Alharthi et al.13 found that the roomtemperature saline as final irrigation showed comparable results to intracanal cryotherapy in previously asymptomatic cases without periapical pathosis.
CDA JOURNAL, VOL 50 , Nº 12 728 DECEMBER 2022 cryotherapy
Studies on Cryogenic Treatment of Ni-Ti Rotary Instruments Results Year Authors
2005 Kim et al.
Cryogenically treated specimens had a significantly higher microhardness than the controls.
2007 Vinothkumar et al.
Deep-dry cryogenic treatment increased the cutting efficiency of Ni-Ti instruments significantly.
2011 George et al.
A randomized prospective clinical trial showed that all the cryotherapy applications (intracanal, intraoral and extraoral) resulted in lower postoperative pain levels and lower visual analogue scale (VAS) scores of pain on percussion versus those of the control group.14 Another clinical trial compared the effect of intracanal cryotreated sodium hypochlorite and room-temperature sodium hypochlorite on postoperative pain after root canal treatment. Results demonstrated that the cryotherapy group showed a statistically significant reduction in postoperative pain levels at all tested time intervals and reduced analgesic intake at six hours postoperatively.15 In another study, Al-Nahlawi et al.6 indicated that the use of intracanal cryotherapy technique with negative pressure irrigation eliminates post-endodontic pain after single-visit root canal treatment (RCT).
In a systematic review, Sadaf et al.16 evaluated the effect of intracanal cryotherapy on postoperative pain after root canal therapy in patients with pulpal or periradicular pathosis. Findings showed that, compared with controls, intracanal cryotherapy significantly reduced postoperative pain at six and 24 hours after the procedure. However, there was no significant effect on pain at 48 and 72 hours and seven days after the procedure. In a recent systematic review, Monteiro et al.17 showed that intracanal cryotherapy application reduced postoperative endodontic pain after six and 24 hours (TABLE 1 ).
Deep cryogenic treatment improved the cyclic fatigue resistance of Ni-Ti rotary files significantly.
Effect on the Success of Local Anesthesia
Despite the fact that inferior alveolar nerve block (IANB) is the standardized injection technique used for achieving regional anesthesia for mandibular molar teeth, it does not always result in successful pulpal anesthesia, especially in patients with symptomatic irreversible pulpitis (SIP).18 Preoperative intraoral cryotherapy application after an IANB did not provide profound pulpal anesthesia for about 45% of mandibular molars with SIP. However, intraoral cryotherapy might be preferred as a simple and cheap auxiliary application to increase the success rate of IANBs in patients with SIP.19
Effect on Fracture Resistance of Endodontically Treated Teeth
Keskin et al.20 evaluated the effect of intracanal cryotherapy on the fracture resistance of endodontically treated teeth. Findings showed that application of intracanal cryotherapy as a final irrigant reduced the vertical fracture resistance of prepared roots when compared to the control group.
Effect on Reducing Root Surface Temperature
Vera et al.21 assessed a new methodology to reduce and maintain external root surface temperature for at least four minutes. Findings showed that although significant differences were found between the initial and lowest temperatures in both the control and experimental irrigation procedures, the experimental intervention reduced it almost 10 times that of the control.
When maintaining a −10 C temperature reduction over four minutes, the teeth in the experimental group also sustained significantly better results.
Effect on Enterococcus faecalis
Enterococcus faecalis is the species most often implicated in persistent root canal infections because of its several virulence factors that make it difficult to eradicate from the canals.22
Mandras et al.23 indicated that cryo-instrumentation after NaOCl irrigation significantly reduced the number of bacteria in the root canal compared to NaOCl alone, without the total elimination of Enterococcus faecalis. The cryogenic fluid (liquid nitrogen), by suitably varying the duration of the treatment, can reach the desired depth and provide immediate freezing of bacterial cells and their subsequent cryodestruction.
The process of freezing and thawing induces injury in microorganisms, in part, through membrane or cell wall disruption, leakage of intracellular constituents and changes in protein conformation.24 Yamamoto and Harris20 showed that in a test executed applying the freezing and thawing technique (30 s ‘ON’, 30 s ‘OFF’ and 30 s ‘ON’) using liquid nitrogen, the bacteria in vitro are significantly reduced with respect to the situation before the treatment.
Effect on Cutting Efficacy of Ni-Ti Rotary Instruments
Historically, the cold treatment of metals during manufacture had been advocated as a means of improving the surface hardness and thermal stability of the metal.25 The optimum cold treatment temperature range lies between −60 C and −80 C for tool steels depending upon the material and on the quenching parameters involved.25 For the past
DECEMBER 2022 729 CDA JOURNAL, VOL 50 , Nº 12
TABLE
2
30 years, researchers have reported substantial benefits from subjecting metals for industrial applications to a cryogenic process.25–27 Cryogenic treatment involves submersing metal in a super-cooled bath containing liquid nitrogen (−196 C/ −320 F)25,26 and then allowing the metal to slowly warm to room temperature. This cryogenic treatment is used to treat a wide range of metal components, including high-speed steel and hot-work tool steel.27,28 The cryogenic treatment was shown to have more beneficial effects than the traditional higher temperature cold treatment.29 The benefits include increasing cutting efficiency as well as the overall strength of the metal.25,27 Cryogenic treatment is an inexpensive treatment that affects the entire crosssection of the metal rather than just the surface in contrast to surface treatment techniques,26 such as ion implantation and vapor deposition. Currently, two mechanisms are believed to account for the change in the properties from cryogenic treatment for steel. The first is a more complete martensite transformation from the austenite phase following cryogenic treatment.28 The second is the precipitation of finer carbide particles within the crystalline structure.27 Controversy exists as to which mechanism is responsible.
There are few studies on the cryogenic treatment of Ni-Ti rotary files. Kim et al.30 evaluated the effects of cryogenic treatment on the composition, microhardness or cutting efficiency of Ni-Ti rotary instruments. According to their findings cryogenically treated specimens had a significantly higher microhardness than the controls. Furthermore, both cryogenically treated and control specimens were composed of 56% Ni, 44% Ti, 0% N (by weight) with a majority in the austenite phase. In another study, Vinothkumar et al.31 showed that deep
dry cryogenic treatment increased the cutting efficiency of Ni-Ti instruments significantly but not the wear resistance. George et al.32 found that deep cryogenic treatment improved the cyclic fatigue resistance of Ni-Ti rotary files significantly (TABLE 2 ).
Conclusion
In endodontics, cold has been used for multiple purposes including controlling postoperative endodontic pain, increasing the success rate of local anesthesia, enhancing the fracture resistance of the endodontically treated teeth, decreasing the temperature of the root surface, acting against specific bacteria like Enterococcus faecalis and enhancing the cutting efficiency of Ni-Ti rotary instruments. ■
REFERENCES
1. Chanliongo PM. Cold (cryo) therapy. In: Lennard TA, Walkowski S, Singla AK, Vivian DG, eds. Pain procedures in clinical practice. Philadelphia: Elsevier; 2011:555–558.
2. Newman R, Clebak KT, Croad J, Wile K, Cathcart E. Assorted skin procedures: Foreign body removal, cryotherapy, electrosurgery and treatment of keloids. Prim Care 2022 Mar;49(1):47–62 doi: 10.1016/j.pop.2021.10.003. Epub 2022 Jan 5.
3. Lombardi G, Ziemann E, Banfi G. Whole-body cryotherapy in athletes: From therapy to stimulation. An updated review of the literature. Front Physiol 2017 May 2;8:258 doi: 10.3389/fphys.2017.00258. eCollection 2017. PMCID: PMC5411446
4. Klimenko T, Ahvenainen S, Karvonen SL. Whole-body cryotherapy in atopic dermatitis. Arch Dermatol 2008 Jun;144(6):806–8 doi: 10.1001/archderm.144.6.806
5. Swenson C, Swärd L, Karlsson J. Cryotherapy in sports medicine. Scand J Med Sci Sport 1996 Aug;6(4):193–200 doi: 10.1111/j.1600-0838.1996.tb00090.x
6. Luethy D. Cryotherapy techniques: Best protocols to support the foot in health and disease. Vet Clin North Am Equine Pract 2021 Dec;37(3):685–693 doi: 10.1016/j. cveq.2021.07.005
7. Bouzigon R, Grappe F, Ravier G, Dugue B. Whole- and partial-body cryostimulation/cryotherapy: Current technologies and practical applications. J Therm Biol 2016 Oct;61:67–81 doi: 10.1016/j.jtherbio.2016.08.009. Epub 2016 Aug 27.
8. Whittaker DK. History of cryosurgery. In: Bradley PF ed. Cryosurgery of the maxillofacial region. Boca Raton, Florida: CRC Press; vol. 1 1986:2–13.
9. Pogrel MA. The use of liquid nitrogen cryotherapy in the management of locally aggressive bone lesions. J Oral Maxillofac Surg 1993 Mar;51(3):269–73; discussion 274 doi: 10.1016/s0278-2391(10)80172-7
10. Al-Nahlawi T, Hatab TA, Alrazak MA, Al-Abdullah
A. Effect of intracanal cryotherapy and negative irrigation technique on postendodontic pain. J Contemp Dent Pract 2016 Dec 1;17(12):990–996
11. Keskin C, Özdemir Ö, Uzun İ, Güler B. Effect of intracanal cryotherapy on pain after single-visit root canal treatment. Aust Endod J 2017 Aug;43(2):83–88 doi: 10.1111/aej.12175 Epub 2016 Oct 4.
12. Vera J, Ochoa J, Romero M, et al. Intracanal cryotherapy reduces postoperative pain in teeth with symptomatic apical periodontitis: A randomized multicenter clinical trial. J Endod 2018 Jan;44(1):4–8 doi: 10.1016/j.joen.2017.08.038 Epub 2017 Nov 1.
13. Alharthi AA, Aljoudi MH, Almaliki MN, Almalki MA, Sunbul MA. Effect of intra-canal cryotherapy on postendodontic pain in single-visit RCT: A randomized controlled trial. Saudi Dent J 2019 Jul;31(3):330–335 doi: 10.1016/j. sdentj.2019.03.004. Epub 2019 Mar 14. PMCID: PMC6626252
14. Gundogdu EC, Arslan H. Effects of various cryotherapy applications on postoperative pain in molar teeth with symptomatic apical periodontitis: A preliminary randomized prospective clinical trial. J Endod 2018 Mar;44(3):349–354 doi: 10.1016/j.joen.2017.11.002. Epub 2018 Feb 3.
15. Nandakumar M, Nasim I. Effect of intracanal cryotreated sodium hypochlorite on postoperative pain after root canal treatment - a randomized controlled clinical trial. J Conserv Dent 2020 Mar–Apr;23(2):131–136 doi: 10.4103/JCD. JCD_65_20. Epub 2020 Nov 5. PMCID: PMC7720754
16. Sadaf D, Ahmad MZ, Onakpoya IJ. Effectiveness of intracanal cryotherapy in root canal therapy: A systematic review and meta-analysis of randomized clinical trials. J Endod 2020 Dec;46(12):1811–1823.e1 doi: 10.1016/j. joen.2020.08.022. Epub 2020 Sep 8.
17. Monteiro LPB, Guerreiro MYR, de Castro Valino R, Magno MB, Maia LC, da Silva Brandão JM. Effect of intracanal cryotherapy application on postoperative endodontic pain: A systematic review and meta-analysis. Clin Oral Investig 2021 Jan;25(1):23–35 doi: 10.1007/s00784-020-03693-8. Epub 2020 Nov 21.
18. Mohammadi Z, Chavoshi M. Effect of needle bevel direction on the success rate of intra-ligament injection technique: A single-blinded clinical trial. Int J Clin Dent 2013;6:349–353
19. Topçuoglu HS, Arslan H, Topçuoglu G, Demirbuga S. The effect of cryotherapy application on the success rate of inferior alveolar nerve block in patients with symptomatic irreversible pulpitis. J Endod 2021 Jan;25(1):23–35 doi: 10.1007/ s00784-020-03693-8. Epub 2020 Nov 21.
20. Keskin C, Sariyilmaz E, Keleş A, Güler DH. Effect of intracanal cryotherapy on the fracture resistance of endodontically treated teeth. Acta Odontol Scand 2019 Mar;77(2):164–167 doi: 10.1080/00016357.2018.1549748. Epub 2019 Jan 9.
21. Vera J, Ochoa-Rivera J, Vazquez-Carcaño M, Romero M, Arias A, Sleiman P. Effect of intracanal cryotherapy on reducing root surface temperature. J Endod 2015 Nov;41(11):1884–7 doi: 10.1016/j.joen.2015.08.009. Epub 2015 Oct 1.
22. Mohammadi Z, Dummer PM. Properties and applications of calcium hydroxide in endodontics and dental traumatology. Int Endod J 2011 Aug;44(8):697–730 doi: 10.1111/j.1365-2591.2011.01886.x. Epub 2011 May 2.
730 DECEMBER 2022 CDA JOURNAL, VOL 50 , Nº 12 cryotherapy
23. Mandras N, Allizond V, Bianco A, et al. Antimicrobial efficacy of cryotreatment against Enterococcus faecalis in root canals. Lett Appl Microbiol 2013 Feb;56(2):95–8 doi: 10.1111/lam.12017. Epub 2012 Dec 27.
24. Yamamoto SA, Harris LJ. The effects of freezing and thawing on the survival of Escherichia coli O157:H7 in apple juice. Int J Food Microbiol 2001 Jul 20;67(1–2):89–96 doi: 10.1016/s0168-1605(01)00438-x
25. Huang HH, Hsu CH, Pan SJ, He JL, Chen CC, Lee TL. Corrosion and cell adhesion behavior of TiN-coated and ion nitrided titanium for dental applications. Appl Surf Sci 2005;244(1–4):252–256 doi.org/10.1016/j. apsusc.2004.10.144
26. Li UM, Chiang YC, Chang WH, et al. Study of the effects of thermal nitriding surface modification of nickel titanium rotary instruments on the wear resistance and cutting efficiency. J Dent
Sci 2006;1(1):53–58 doi:10.30086/JDS.200606.0001
27. Mohammadi Z, Soltani MK, Shalavi S, Asgary S. A review of the various surface treatments of Ni-Ti instruments. Iran Endod J 2014 Fall;9(4):235–240. Epub 2014 Oct 7. PMCID: PMC4224758
28. Shevchenko N, Pham MT, Maitz M. Studies of surface modified Ni-Ti alloy. Appl Surf Sci 2004;235(1–2):126–131 doi.org/10.1016/j.apsusc.2004.05.273
29. Conrad J, Dodd R, Worzala F, Qiu X. Plasma source ion implantation: A new, cost-effective, non-line-of-sight technique for ion implantation of materials. Surf Coat Technol 1988;36(3-4):927–937 doi.org/10.1016/02578972(88)90033-3
30. Kim JW, Griggs JA, Regan JD, Ellis RA, Cai Z. Effect of cryogenic treatment on nickel-titanium endodontic instruments. Int Endod J 2005 Jun;38(6):364–71 doi: 10.1111/j.1365-

2591.2005.00945.x PMCID: PMC1266290
31. Vinothkumar TS, Miglani R, Lakshminarayananan L. Influence of deep dry cryogenic treatment on cutting efficiency and wear resistance of nickel-titanium rotary endodontic instruments. J Endod 2007 Nov;33(11):1355–8 doi: 10.1016/j.joen.2007.07.017. Epub 2007 Aug 23.
32. George GK, Sanjeev K, Sekar M. An in vitro evaluation of the effect of deep dry cryotreatment on the cutting efficiency of three rotary nickel titanium instruments. J Conserv Dent 2011 Apr;14(2):169–72 doi: 10.4103/0972-0707.82627 PMCID: PMC3146111
THE CORRESPONDING AUTHOR, Hamid Jafarzadeh, DDS, MSc, can be reached at hamid_j365@yahoo.com.
DECEMBER 2022 731 CDA JOURNAL, VOL 50 , Nº 12
• Inexpensive • Disposable • Non-Toxic Package of 100 E-VAC INC.© CALL: (509) 448-2602 EMAIL: kenevac@hotmail.com Made in USA The Original E-VAC Tip PREVENT PAINFUL TISSUE PLUGS PROTECT YOUR EQUIPMENT FROM COSTLY REPAIRS FDA Registered Contact Your Local Dental Supply Company
December 2022 CDA Continuing Education Worksheet
This worksheet provides readers an opportunity to review C.E. questions for the article “Cryotherapy in Endodontics: A Critical Review” before taking the C.E. test online. You must first be registered at cdapresents360.com. To take the test online, click here. This activity counts as 0.5 of Core C.E.
1. True or False: Cryotherapy is the use of extreme cold to freeze and remove abnormal tissue.
2. The magnitude of tissue alteration during cryotherapy depends on all but which one of the following?
a. Thermal conductivity of the tissues.
b. Exposure time.
c. Type of heat or cold agents employed. d. Final temperature of the agent employed.
3. Which of the following describe cryotherapy? (mark all that apply)
a. Cryotherapy chamber exposes individuals to freezing dry air (below –100 C) for two to four minutes.
b. Blood vessels are narrowed by the extreme cooling.
c. Narrowed vessels reduce blood flow, which reduces inflammation and swelling.
d. Once outside the chamber, vessels expand and an increased presence of Interleukin-10 is established in the blood.
e. Sensory nerve fibers are stimulated, which may cause temporary painful sensations during and/or immediately following treatment.
4. Which one of the following substances is not commonly used during medical or dental cryotherapy?
a. Dry ice.
b. Liquid nitrogen.
c. Liquid nitrous oxide. d. Argon gas.
5. Which one of the following statements does not apply to the dental instrument used for cryotherapy?
a. It is equipped with a conduit of a conveyor capable of being connected to a needle and a source of cryogenic fluid.
b. The needle has a smaller outer diameter (0.25 mm) than the size of the entrance inside a tooth canal so that it can be inserted into the canal.
c. The needle is made of a rigid material to keep it from bending or breaking in the canal.
d. The cryogenic fluid is blown into the canal via the needle.
The authors cite the results of several studies that used cryotherapy for endodontic care. Which of the following are true and which are false?
6. True or False: A randomized prospective clinical trial showed that of all the cryotherapy applications (intracanal, intraoral and extraoral), only the intracanal application resulted in lower postoperative pain levels than those of the control group.
7. True or False: A clinical trial comparing the effect of intracanal cryotreated sodium hypochlorite and room-temperature sodium hypochlorite on postoperative pain after root canal treatment failed to demonstrate a difference in pain reduction between the cryotherapy group and the control group.
8. True or False: The authors posit that because inferior alveolar nerve blocks (IANBS) do not always result in successful pulpal anesthesia, especially in patients with symptomatic irreversible pulpitis, intraoral cryotherapy might be a useful auxiliary application to increase the success rate of IANBs in these patients.
9. True or False: A study evaluating the effect of intracanal cryotherapy on the fracture resistance of endodontically treated teeth showed that application of intracanal cryotherapy as a final irrigant reduced the vertical fracture resistance of prepared roots when compared to the control group.
10. True or False: A study on the effect of cryotherapy on Enterococcus faecalis, the bacterial species most often implicated in persistent root canal infections, indicated that cryo-instrumentation after NaOCl irrigation significantly reduced the number of bacteria in the root canal compared to NaOCl alone.
732 DECEMBER 2022 CDA JOURNAL, VOL 50 , Nº 12 C.E. CREDIT QUESTIONS
Integrated Approaches to Preventing and Managing Chronic Diseases: Colorado’s
Diabetes Cardiovascular Disease Oral Health Integration Program
Katya Mauritson, DMD, MPH(c); Sara Grassemeyer, MPH; Ian Danielson, MPA; and Abby Laib, MS
abstract
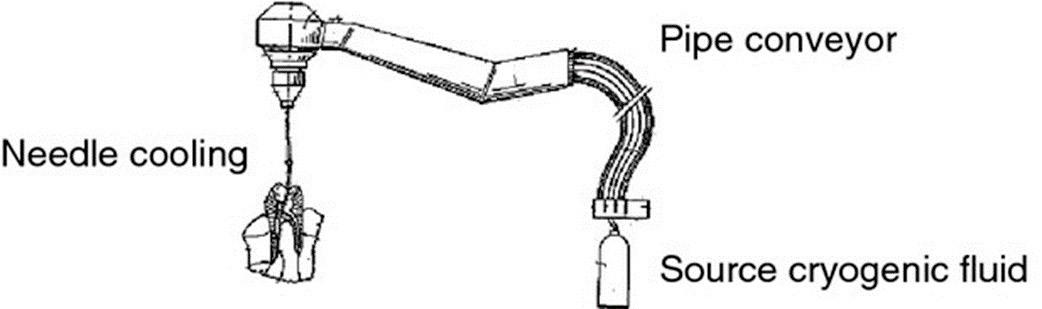
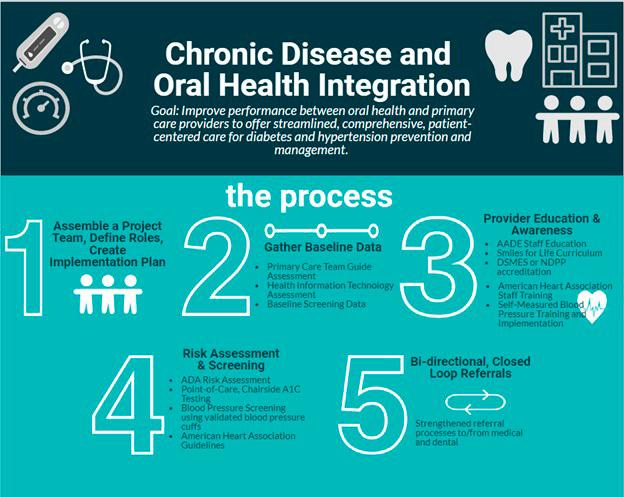
Research indicates that diabetes and hypertension are linked to worsening periodontal disease and uncontrolled oral diseases can make it difficult to prevent or manage other chronic diseases, creating deleterious cycles that can undermine overall health. Colorado continues to test integration strategies to leverage clinical safety net and public health workforces to address the most pressing health care needs of underserved communities, with a focus on preventing and managing (pre)diabetes, (pre)hypertension and oral diseases.
Keywords: Medical-dental integration, oral public health, diabetes, hypertension, oral health, dental, oral health equity, Colorado, Models of Collaboration

DECEMBER 2022 733 CDA JOURNAL, VOL 50 , Nº 12
chronic diseases
AUTHORS
Katya Mauritson, DMD, MPH(c), was Colorado’s state dental director and manager of the oral health unit at the Colorado Department of Public Health and Environment for 10 years. The oral health unit works to decrease oral health inequities across Colorado by integrating oral health strategies into public health and clinical systems across the state.
Conflict of Interest Disclosure: None reported.
Sara Grassmeyer, MPH, is the clinical quality improvement program manager for the Health Promotion Chronic Disease Prevention Branch, Prevention Services Division in the Colorado Department of Public Health and Environment for five years. In this role, she promotes effective use of health information technology and clinic quality improvement for oral and chronic disease prevention and management and more.
Conflict of Interest Disclosure: None reported.
Ian Danielson, MPA, is a chronic disease evaluator at the Colorado Department of Public Health and Environment. He led several evaluations for programs in the state of Colorado that focused on reducing the prevalence of and inequities in hypertension and diabetes.
Conflict of Interest
Disclosure: None reported.
Abby Laib, MS, is a program evaluator at the Colorado Department of Public Health and Environment. She has experience planning, implementing and managing public health evaluations as well as working with diverse stakeholders to effectively utilize their data to inform program decisions and improvements.
Conflict of Interest Disclosure: None reported.
Oral health is an often neglected but critical determinant of overall health, with physical1 and social2 impacts across the lifespan. Historical separation of medical, dental and behavioral health systems has led to often siloed clinical training programs, insurance coverage and delivery of primary health care services. Oral disease prevention and management programs regularly receive less attention and funding compared to chronic disease and behavioral health programs. Additionally, oral health services are considered part of the primary health care scope of services, and dental services are often perceived as cosmetic services. As a result, widespread access to evidencebased, individual and population-level interventions, which promote overall health and well-being, fall short of need, especially in communities of color and other underserved communities. Many dental clinicians do not have access to services that would help ensure delivery of culturally appropriate care, including interpretation and translation services. These and other systemic barriers perpetuate oral health inequities.
Historically, Colorado has had lower rates of obesity than most other states, with commensurate lower chronic disease rates. However, the 2018 statewide prevalences of obesity, diabetes and hypertension are trending upward since 2011, though only the increase in the prevalence of obesity is a significant increase (TABLE 1). The 2011 baseline was used due to a national change in the methodology used for the Behavioral Risk Factor Surveillance System between 2010 and 2011.
The Colorado Department of Public Health and Environment acknowledges that long-standing systemic racism, including economic and environmental injustice, has created conditions
that negatively affect marginalized communities, particularly people of color. These conditions, which limit opportunities for optimal health and influence individual behaviors, are critical predictors of health outcomes and have created health inequities for communities of color. Black and Hispanic communities experience a significant burden of obesity, diabetes and hypertension compared to white (non-Hispanic) communities (TABLE 2).
Given that obesity leads to an increased risk of developing diabetes4 and the projected growth of Hispanic populations in the state,5 the prevalence of Coloradans with obesity and obesityrelated diseases is likely to increase even more in the near future. Fortunately, the prevalence of oral diseases has been decreasing. However, according to Colorado’s 2018 Behavioral Risk Factor Surveillance System data,3 tooth loss due to decay or periodontal disease based on race/ethnicity is still significantly lower for non-Hispanic whites (33.2) versus Blacks, non-Hispanics (42.2) and Hispanics (38.9), respectively.
According to the Centers for Disease Control and Prevention’s (CDC) Chronic Disease Cost Calculator,6 diabetes and cardiovascular diseases cost Colorado approximately $10.6 billion each year in health care and lost productivity. Dental care costs in Colorado were approximately $1.5 billion in 2015. A substantial portion of these costs were out-of-pocket expenditures or paid by public insurances. The growth of historically underserved and never-served communities of color, along with the expected growth of older adults,6 will most likely lead to increased health care expenditures and an increase in the proportion of people with multiple chronic morbidities.
In order to address these looming and unsustainable health and financial
734 DECEMBER 2022 CDA JOURNAL, VOL 50 , Nº 12 chronic diseases
by
*Indicates significant difference compared to white, non-Hispanic based on comparison of confidence intervals.
crises, Colorado continues to seek innovative, effective ways to provide resources and opportunities to poorly and never-served communities.
For states that need more capacity to pursue the Quadruple Aim7 of health care (improved outcomes, patient experience, clinician experience and cost savings), the following information may be particularly relevant. The Colorado Department of Public Health and Environment is integrating dental clinical and oral public health workforces into efforts to prevent and manage diabetes and cardiovascular disease.
Facilitators of Current Work
Colorado’s Oral Health Unit is the only state organization in the U.S. that received two grants from the CDC’s Division of Oral Health to pilot and expand strategies to integrate medical and dental clinical services, with the supportive integration of oral health and chronic disease public health programs. In 2016, Colorado was one of six states to receive $250,000 per year for two years from the CDC DP-1609 Models of Collaboration grant.8 The Models of Collaboration grantees tested “innovative approaches to building communication between state chronic disease and oral health program staff, incorporating oral health into chronic disease management systems.”
Colorado focused its pilot grant on patients with a focus on prediabetes and clinical safety net programs. In 2018, Colorado was one of five states9 awarded enhanced funding via the CDC DP-1810 grant to continue its medical-dental chronic disease integration project, dubbed the Colorado Diabetes Cardiovascular Disease Oral Health Integration Program (DCVDOHI).
Colorado was well positioned to take on the critical work of integrating strategies to support oral health into chronic disease strategies and medical services for adults with diabetes and hypertension. Over a decade of innovative approaches in Colorado have increased access to oral health care and facilitated practice transformation in medical and dental settings. Colorado’s Oral Health Unit and partners built upon the following efforts, braiding promising strategies and programs to advance integrated care:
■ Colorado’s perinatal Cavity Free at Three10 program, established in 2007 by six local philanthropies, which has trained hundreds of medical providers to perform oral health assessments, provides fluoride varnish to young children and coaches caregivers in goal setting through motivational interviewing techniques.
■ The Health Resources and Services Administration’s Perinatal
and Infant Oral Health Quality Improvement grant.11 This grant supported 16 states, including Colorado and California. This grant provided additional funding, strategies and technical assistance that led to the development of the Cavity Free at Three program’s prenatal clinical change package, which integrated medical and dental services for pregnant people.
Colorado defines a clinical change package as an evidence-based or evidence-informed set of tools and strategies that improve clinical systems and patient outcomes.
Both of Colorado’s oral health change packages live within the Clinical Quality Improvement Portfolio12 are discussed below.
■ Delta Dental Foundation of Colorado’s Medical-Dental Integration Project,13 which spanned 2007-2019, co-located dental hygienists in medical practices in 39 locations across the state. This project enabled oral health preventive services and referrals in underserved areas while providing proof of sustainable co-location models.
■ The state’s Primary Care Association, Colorado Community Health Network, developed its “Oral Health Integration Manual”14 to support long-term integration of oral health services into care delivery systems. Released in 2015, the manual provides standardized “BITEs,” or Blueprints for Integrative Transformative Embodiment, for Colorado’s approximately 170 community health center clinical sites to implement on the path toward fully integrated systems. As Colorado’s Primary Care Association developed
DECEMBER 2022 735 CDA JOURNAL, VOL 50 , Nº 12
TABLE 1
Statewide Prevalences3 Hypertension Diabetes Obesity 25.0 6.7 20.7 2011 25.9 7.0 22.9 2018
%,
Diabetes %,
Obesity %,
TABLE 2 Chronic Disease Prevalence and Confidence Interval (CI)
Race/Ethnicity (2018)3 Hypertension
(95% CI)
(95% CI)
(95% CI) 33.9 (27.4 – 40.4) 9.7 (5.2 – 14.1) 31.0* (23.0 – 39.1) Black, non-Hispanic 22.6* (20.1 – 25.2) 8.9* (7.4 – 10.4) 29.8* (26.8 – 32.7) Hispanic 26.6 (25.4 – 27.7) 6.4 (5.7 – 7.0) 21.3 (20.1 – 22.5) White, non-Hispanic
its integration manual, it became a grantee of the Oral Health Unit to support public health strategies focused on boosting school sealant programs, water fluoridation and communications. The establishment of this contractual relationship for core oral public health functions facilitated the addition of current medical-dental activities.
■ The Colorado Department of Public Health and Environment’s Center for Health and Environmental data included oral health data and cross tabs to other diseases and risk factors in the department’s VISION dashboard: Visual Information System for Identifying Opportunities and Needs data dashboard.3 Data on oral disease and diabetes rates by race/ethnicity were used in Colorado’s successful application for the CDC DP-1609 Models of Collaboration grant. Data on oral disease, diabetes and cardiovascular disease rates and comorbidities were used in Colorado’s successful application for the CDC DP-1810 Medical-Dental Integration grant.
■ The Colorado Department of Public Health and Environment’s Health Promotion Chronic Disease Prevention Branch began planning integrated approaches to its health systems change work. The branch worked with multiple public health programs to develop a Clinical Quality Improvement team with funds from each contributing program. Colorado received its CDC Models of Collaboration DP-1609 award announcement early in the development of the Clinical Quality Improvement team, enabling the inclusion of oral health into this infrastructure.
■ In addition to receiving its core CDC DP-1815 grant, Colorado’s Diabetes/Cardiovascular Disease Unit was one of 29 grantees to receive a competitive grant, CDC DP-1817 Innovative State and Local Public Health Strategies to Prevent and Manage Diabetes, Heart Disease and Stroke. The state’s application included a strategy of funding at least two dental clinics for diabetes and cardiovascular disease activities.
the receipt of this grant, Colorado added cardiovascular disease prevention and management strategies to the Diabetes Oral Health Integration Project.
Colorado’s DCVDOHI program is the current iteration of its chronic disease-oral health/medical-dental integration work. For the remainder of this manuscript, Colorado’s past and current adult integration work will focus on the DCVDOHI program.
DCVDOHI Program Funding
The DCVDOHI program is financed by combining funds from the oral health and chronic disease state and federal funds (TABLE 3).
The branch worked with multiple public health programs to develop a Clinical Quality Improvement team
Program Strategies and Activities
The facilitators mentioned previously helped build infrastructure, expertise and momentum for Colorado to develop its current oral health-chronic disease/ medical-dental integration program. Colorado’s two-year pilot under the CDC’s DP-1609 grant focused on developing the Diabetes Oral Health Integration pilot program. This pilot program led to integration of the work of two Oral Health Unit staff with chronic disease staff and also led to integration of funding, contracting and other processes at the state health department. This integration led to the establishment of clinical contracts that allowed the expansion of oral health activities once Colorado received its five-year medical-dental integration grant CDC DP-1810. With
The DCVDOHI program and its funding are a piece of the larger Clinical Quality Improvement program. In addition to the Oral Health Unit and Diabetes Cardiovascular Disease Unit grants that fund the DCVDOHI program, the following programs contribute financial support to the Clinical Quality Improvement team’s activities:
■ Women’s Wellness Connection, supporting breast and cervical cancer screening and care coordination.
■ Colorectal Cancer Control Program supporting colorectal cancer prevention and screening.
■ WISEWOMAN (CDC’s Well-Integrated Screening and Evaluation for WOMen Across the Nation), supporting heart health screenings.
■ Tobacco Education, Prevention and Cessation Unit, supporting the integration of tobacco strategies across clinical systems.
DCVDOHI Program Processes
Staff from all of the programs contribute staff time to either serve as part of the core Clinical Quality Improvement team
736 DECEMBER 2022 CDA JOURNAL, VOL 50 , Nº 12 chronic diseases
DCVDOHI Program Funding Sources
CDC DP-1810 CDC DP-1815 and DP-1817
State general oral health funds
Oral health systems specialist .15 FTE Not applicable .10 FTE
Chronic disease coordinator .15 FTE .15 FTE .5 FTE
Clinical quality improvement/ health systems specialist .05 FTE .10 FTE .5 FTE
State dental director/oral health unit manager .10 FTE Not applicable .10 FTE
Pooled evaluation positions .20 FTE .10 FTE .5 FTE
Pooled fiscal, contracting and communications positions .15 FTE .10 FTE Not applicable
Grants to six federally qualified health centers 55% 15% 35%
Grant to one behavioral health organization 10% 25% 65%
Grant to Primary Care Association 75% Not applicable 25%
Operational costs (includes translation, supplies, travel, other)
Grant to regional and statewide Medicaid organizations
60% 15% 25%
50% Not applicable 50%
Approximate totals/year $200,000 $65,000 $120,000 or to provide subject matter expertise to inform the work of the team. For example, the Oral Health Unit’s health systems specialist is part of the core team while the state dental director serves as an advisor. The braiding of funds allows the DCVDOHI program to leverage internal state processes, including:
■ Requests for applications that include DCVDOHI and the Oral Health Unit’s prenatal clinical change packages. Once an applicant is awarded funding for any of the evidencebased interventions included in the request for applications opportunities, the awardee becomes eligible to add interventions to its future contract with the state, such as DCVDOHI strategies.
■ Contracting processes, with inclusion of strategies in contracts from DCVDOHI, diabetes, cardiovascular disease,
Women’s Wellness Connection, WISEWOMAN and tobacco programs. State staff share the burden of developing and monitoring contractors, which prevents overburdening individual staff members and shared clinical partners.
■ Collaborative monthly meetings between clinical grantees and the supportive state clinical quality improvement and contractual staff.
■ The development and regular enhancement of shared building blocks within the clinical change package that prepares clinics to include additional chronic disease and oral health strategies in the future, regardless of any focus on a specific disease topic during the request for application process.
■ Shared site visit activities including pooled costs for transportation and/or minimizing the number of
state staff conducting site visits.
Colorado plans to continue braiding funding, staff and processes to improve the sustainability and reach of all programmatic strategies. An additional benefit of the integration of public health programs is the decrease of duplicative efforts, and therefore costs, across public health programs.
DCVDOHI Collaborations
Several external partners inform the work and support the spread of the DCVDOHI program. These partners provide varying levels of support for the program and include unpaid, advisory positions.
The CDC DP-1609 Models of Collaboration for State Chronic Disease and Oral Health programs grant required collaborations with “key chronic disease and oral health personnel to provide oversight throughout the entire two-year project period.” Colorado
DECEMBER 2022 737 CDA JOURNAL, VOL 50 , Nº 12
TABLE 3
expanded this group into the current DCVDOHI advisory board, which continues to provide expertise on program development and implementation.
The advisory board also provided suggestions for policy changes and other strategies to enhance the effectiveness and reach of the DCVDOHI program. The advisory board consists of local and national chronic disease, oral health and clinical quality improvement experts. Representatives from the following organizations are currently on the DCVDOHI advisory board:
■ Colorado Community Health Network (Colorado’s Primary Care Association).
■ National Network for Oral Health Access.
■ National Association of Chronic Disease Directors.
■ American Diabetes Association.
■ American Heart Association.
■ University of Colorado’s medical and dental schools.
■ Delta Dental of Colorado.
■ Regional Oral Health Specialists
(local public health agencies contracted to implement Oral Health Unit strategies).
■ Medicaid office staff.
■ Colorado Department of Public Health and Environment staff. Colorado planned to include additional DCVDOHI advisory board members in order to explore partnerships to expand the program into private dental practices. However, the COVID-19 pandemic delayed those plans. Once Colorado is able to resume the majority of its core clinical and public health activities, the DCVDOHI program will reassess the ability to expand the advisory board to include representation from the following types of organizations:
■ Dental, medical and behavioral health membership associations.
■ Dental and medical board members or administrators.
■ Care coordination partners. An additional key group of partners that are currently not directly engaged in the DCVDOHI program includes Colorado’s regional accountability entities.
These entities coordinate care and provide other services to Medicaid enrollees. While the DCVDOHI program has not been able to engage the regional accountability entities as robustly as initially planned, the program was able to contract with Colorado Access during the CDC DP1609 Models of Collaboration grant cycle. The contract focused on data analyses, the results of which are described in the Results and Discussion sections below. The engagement of regional accountability entities in medical-dental activities should provide several future high-impact strategies for the DCVDOHI program. The DCVDOHI program is also planning to contract with Colorado’s Health Center Controlled Network, the Colorado Community Managed Care Network. This partner can help the DCVDOHI program and opportunities in the near future.
DCVDOHI Program Implementation
The Oral Health Unit, Chronic Disease Prevention and Health Promotion Branch and the Health Surveys and Evaluation Branch collaborated to develop the logic model (BOX) to guide DCVDOHI program implementation.
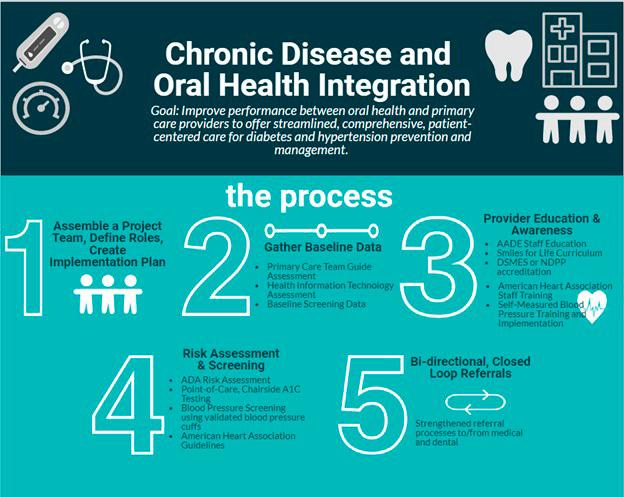
Staff from the state health department’s oral health, chronic disease, evaluation, budget, contracting and other teams collaborated to create a robust Clinical Quality Improvement Portfolio,11 which includes the DCVDOHI clinical change package. The portfolio guides health care systems and individual clinics, including those implementing the DCVDOHI clinical change package, to align activities around three foundational steps and several priority strategies:
Step 1: Building capacity and infrastructure focusing on the following foundational aspects of practice transformation: creating a culture of quality improvement, leveraging Health Information
738 DECEMBER 2022 CDA JOURNAL, VOL 50 , Nº 12
chronic diseases
FIGURE 1. These steps provide workflows, research and other relevant resources to enable implementation of best practices.
Technology (HIT) and implementing standard policies and workflows.
Step 2: Implementing one or more disease-specific evidence-based interventions, including cancer, diabetes, cardiovascular disease and oral disease screening, prevention and management activities.
Step 3: Tracking progress and evaluating outcomes, which includes: data visualization of electronic health record reports and trends, monthly check-ins with Clinical Quality Improvement staff, quarterly data reporting into data collection tools and annual evaluations.
In order to fully implement the DCVDOHI clinical change package within the medical-dental integration section of the Clinical Quality Improvement portfolio, the Oral Health Unit contracted with the State Primary Care Association, the Colorado Community Health Network. Staff from the Colorado Community Health Network’s Quality Initiatives Division ensured alignment of the DCVDOHI clinical change package with the aforementioned “Oral Health Integration Manual”14 BITEs. The change package provides best practices for medical and dental clinics to improve medical-dental
integration, demonstrated in fIGure 1
Each of the implementation steps provides workflows, research and other relevant resources to enable implementation of best practices. The DCVDOHI program utilizes a modified version of the Primary Care Team Guide Assessment, developed by the MacColl Center for Health Care Innovation at Group Health Research Institute,15 and is used to understand implementation of team-based care practices in grantee organizations. Assessment modification includes questions about the dental care team and medical-dental integration and allows care teams to identify how the organization utilizes team-based care practices, improve communication or change workflows to improve processes, ensure care team members are working to the top of their scope and better understand how medical and dental teams work together. The DCVDOHI program team uses scores from the modified Primary Care Team Guide Assessment to determine priority technical assistance needs of grantees.
The DCVDOHI program team meets monthly and consists of staff from the Oral Health Unit, the Clinical Quality Improvement team, Colorado
Community Health Network and the health department’s evaluation team. The Oral Health Unit provides logistical support and expertise on dental processes and oral disease prevention and management. The Clinical Quality Improvement team manages contracts with participating organizations and provides technical assistance on team-based care and quality improvement processes. The Colorado Community Health Network provides expertise in health systems processes and team-based care. The evaluation team conducts evaluation activities for the program. All members of the DCVDOHI program team provide coaching on program implementation and continuous quality improvement.
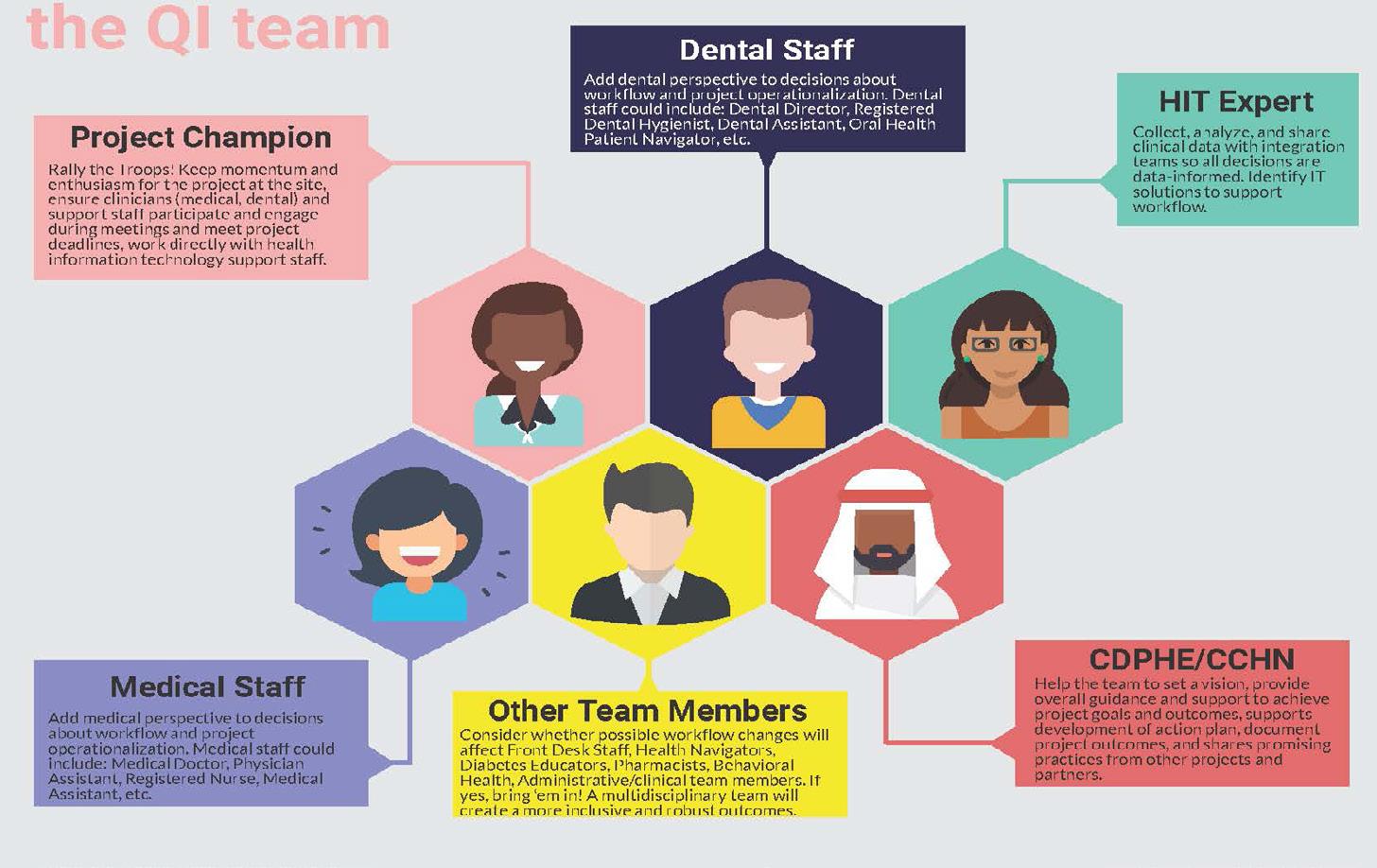
Each clinical grantee receives direct support from the DCVDOHI program team, while including additional clinical staff and partners. fIGure 2 demonstrates all of the roles required to successfully implement the DCVDOHI clinical change package.
Results and Discussion Clinical Outcomes
The DCVDOHI program has funded six organizations to work on integrating oral health with diabetes and/ or hypertension screening activities. While all six organizations have begun implementing the majority of DCVDOHI strategies, four are currently prioritizing hypertension control strategies and the other two diabetes control (all are working on strategies for oral health). Several factors distinguish each of the participating organizations, including geography, population served and colocation of dental and medical clinics. Therefore, the context of the project is unique for each organization. For instance, one clinic serves a population of people experiencing homelessness in a large metro area, whereas another clinic
DECEMBER 2022 739 CDA JOURNAL, VOL 50 , Nº 12
FIGURE 2. Roles required to successfully implement the DCVDOHI clinical change package.
Hypertension Control Rates
serves a large rural region of Colorado. This contextual diversity is important to understand when interpreting the data collection progress and preliminary results summarized in this update.
Although Colorado has been piloting clinical medical-dental integration activities since 2017, there have been significant barriers to collecting baseline data. It was only in 2019-2020, year two of the CDC DP-1810 grant, that baseline data were collected for all six funded organizations. In total, 9,565 dental patients were screened for chronic diseases. Three organizations were able to report hypertension screening rates, with an average of 60.2% (ranging between 25.0% and 99.7%) of eligible dental patients screened across organizations. Of those screened for hypertension, an average of 26% had blood pressure greater than 140/90. Two organizations were able to report on rates of diabetes risk assessment, with an average of 15.7% of eligible patients screened. These organizations also reported an average of 64% of patients with a high-risk assessment score received a Point of Care (PoC) diabetes screening. An average of 34% of those patients who received a screening had test values indicating possible diabetes.
Within the funded organizations, overall hypertension control rates averaged 62.4% in 2019 and 60.2% in 2020, for an average reduction of 2.2 percentage points between calendar years (TABLE 4). Changes in hypertension control rates varied across organizations, with two organizations experiencing reductions in hypertension control of approximately 9 percentage points, while
others improved hypertension control rates slightly. Observed reductions in hypertension control rates may be artifacts of the COVID-19 pandemic or other complicating factors, rather than actual reflections of changes in care. For instance, one clinic transitioned its electronic records around the time hypertension control data were submitted, and cleaning and validation of the data were not yet complete. Other health systems noted that hypertension control rates may decrease due to inability to see patients with high blood pressure in person, creating a situation in which patients who had high blood pressure prior to the pandemic may not have had a second blood pressure reading during the measurement period. Due to the lack of a second blood pressure reading, these patients would appear in the data as uncontrolled, even if they were able to reduce their blood pressure during the measurement period.
It is also worth noting that, with the exception of Clinic 3, these hypertension rates are health systemwide and do not solely reflect dental patients. Finally, the DCVDOHI program is designed to increase detection of high blood pressure. Therefore, during the initial stages of the program, health systems will be adding patients to the denominator of the hypertension control measure and may not be able to immediately move them to the numerator, reducing the overall rate of hypertension control.
Uncontrolled diabetes rates varied across funded organizations and between 2019 and 2020. On average, there was an increase of 3.1 percentage points in the rate of uncontrolled diabetes. Clinic 5 was
able to reduce uncontrolled diabetes by nearly 20 percentage points, while Clinic 3 saw a large increase of 29.3 percentage points (TABLE 5). In addition to the caveats listed previously in the discussion of hypertension control, it should be noted that Clinic 5 may experience more fluctuation in rates due to their small size relative to other organizations.
Before the CDC DP-1810 grant ends in fall 2024, Colorado plans to resolve many of the data collection challenges that inhibit the ability to demonstrate the impact of medical-dental integration strategies on patient health outcomes. However, the COVID-19 pandemic will most likely remain the largest challenge in understanding the outcomes of the short-term health outcomes of the DCVDOHI program.
Successes and Challenges
The DCVDOHI program has also identified the following organizational success and challenges of funded organizations.
Successes
■ Increased opportunity for quality improvement and oral health integration conversations with clinical partners and with internal/ external state and national partners.
■ Funding for an oral health patient navigator position. Navigator or care coordinator positions play critical roles in ensuring completion of patient referrals and treatment plans. The inability for this position to be reimbursed leads to gaps in funding,
740 DECEMBER 2022 CDA JOURNAL, VOL 50 , Nº 12 chronic diseases
TABLE 4
Measure Clinic 1* Clinic 2 Clinic 3 Clinic 4* Clinic 5* Clinic 6 Average Hypertension control rate 2019 56.2% 56.1% 71.0% 61.3% 64.3% 65.8% 62.4% Hypertension control rate 2020 60.3% 57.8% 61.4% 58.5% 66.8% 56.6% 60.2% Difference 4.1% 1.7% –9.6% –2.7% 2.5% –9.2% –2.2% *Fiscal reporting schedule (e.g., July 1–June 30).
Uncontrolled Diabetes Rates
Uncontrolled
requiring long-term funding from grants or other sources.
■ Buy-in from leadership and medical and dental teams. Leadership buy-in provides additional motivation, time and other resources to implement these and other systems change strategies.
■ Increased workforce satisfaction. Dental staff relay an increased sense of purpose and interest in their roles and an interest in remaining in their roles for longer, supporting retention of experienced clinicians.
■ Funding for electronic medical and dental record integration and other health IT (HIT) integration activities, including establishment of patient registries and dashboards to track patients and progress.
■ Implementation of prediabetes risk assessments in dental clinics.
■ Implementation of PoC HbA1c screenings by dental teams with results relayed to medical and potentially pharmacy teams.
■ Blood pressure monitoring training for dental staff by medical staff.
■ Use of Smiles for Life online modules16 to train medical staff and frontline workers in oral health.
■ Access to developed resources including CLIA waivers for HbA1c screenings.
■ Ability for dental clinics to bill Medicaid for HbA1c and blood glucose screenings.
Challenges
■ Staff turnover, lack of capacity and lack of buy-in. Some clinical
staff report that the oral health navigator/care coordination role is an often overburdened and underpaid role and may lead to higher turnover rates and a need for frequent and intensive onboarding processes for new coordinators.
■ Lack of compatible electronic medical and dental health records. This lack of integrated HIT infrastructure often requires costly changes supported by deep expertise to operationalize.
■ Lack of functionality in electronic records can lead to unintended outcomes, including inaccurate data reports, inability to track patient referrals from medical to dental and vice versa and to set and meet the goals of this project.
■ Data tracking issues including lack of patient demographic data.
■ Sensitivity issues with HbA1c testing machines and blood pressure wrist cuffs.
■ Cost of HbA1c testing machines.
■ Inability for dental clinics to bill insurances for blood pressure screenings and navigation to medical services.
■ Inability for medical providers to bill insurances for oral health risk assessments and preventive services.
■ Large costs but limited funding for clinics to realign systems of care, train staff in changes and maintain integration strategies requires more funding than most clinics can afford.
■ Shutdown and slowdown of services due to the COVID-19
pandemic, which continues to impact many safety net clinics.
■ Lack of capacity within safety net clinics and other organizations supporting the clinical safety net, especially during the COVID-19 pandemic. For example, both clinical and public health DCVDOHI staff were deployed to pandemic response activities.
■ High rates of white coat hypertension in dental patients.
Conclusion and Next Steps
Colorado’s DCVDOHI program has made progress developing and implementing its medical-dental integration strategies, with supportive integration of its chronic disease and oral health public health programs. The DCVDOHI program should eventually provide more evidence that integrated clinical systems can improve health outcomes for underserved populations.
As DCVDOHI clinical grantees rebound from the COVID-19 pandemic and strive to resume services at full capacity, the DCVDOHI program team will seek additional grantees. New grantees may include, but are not limited to, regional accountability entities, community safety net dental clinics, private practices, health care training programs, clinics serving children with high obesity and chronic disease rates and behavioral health systems. In order to focus on strategies to improve health equity and adopt promising practices from the pandemic, the DCVDOHI program team will work with its advisory board, grantees and others to update the
DECEMBER 2022 741 CDA JOURNAL, VOL 50 , Nº 12
TABLE 5
1*
2 Clinic 3 Clinic 4*
5*
6 Average
Measure Clinic
Clinic
Clinic
Clinic
diabetes rate 2019 30.3% 51.5% 26.2% 30.0% 42.3% 36.1% 36.1%
Uncontrolled diabetes rate 2020 30.3% 64.8% 55.5% 27.5% 22.7% 34.2% 39.2% Difference –0.03% 13.3% 29.3% –2.6% –19.6% –1.9% 3.1% *Fiscal reporting schedule (e.g., July 1–June 30)
DCVDOHI clinical change package.
The DCVDOHI program team plans to include telehealth, additional HIT and strategies to address patients’ food and housing security needs in the next update to the clinical change package. The Oral Health Unit is currently leading a workgroup focused on implementing and evaluating integrated telehealth and HIT strategies.
As mentioned in the partners section, promising data to support medical-dental integration programs was conducted by Colorado Access. In 2017, Colorado Access was the state’s largest regional accountability entity supporting Medicaid enrollees, covering the Denver metro area and the rural northeast corner of the state. The Colorado Department of Health and Environment provided funding to analyze data in an attempt to repeat the national United Concordia Jeffcoat1 study with Colorado data. Due to changes in the state Medicaid data vendor and other challenges, trend analyses like those conducted by Jeffcoat were not possible. Colorado Access found that the only significant finding was related to emergency department utilization for diabetics. In 2019, Colorado Access published its study,17 distributing its findings to clinics across the Denver metro area and to statewide partners. The publication demonstrated that for Medicaid “members with two or more diagnostic dental visits, the hazard of an ED visit is reduced nearly 60% (p < 0.0001). Additionally, there may be a potential dosage effect where individuals with two or more periodontal treatments had a 59% (p = 0.004) reduced hazard, where individuals with one periodontal treatment (after adjustment) did not have a reduced hazard over those who had no dental claims.”
The DCVDOHI program team continues to experience successes and
challenges implementing core strategies. In particular, Colorado has delayed its efforts to infuse strategies focused on alleviating the health inequities based on race, ethnicity, primary language and other factors. Colorado had planned several health equity strategies related to workforce development, such as focusing on delivery of culturally appropriate care, stratification of data for quality improvement and other activities that enable clinical and public health systems to better meet community needs.
The DCVDOHI program will continue
bi-directional referrals to local dental providers trained to support patients’ behavioral health needs. This and other efforts are priming Colorado to develop tridirectional strategies across dental, medical and behavioral health teams. Given the sharp rise in overdose deaths18 and suicidal ideation19 exacerbated by the COVID-19 pandemic, programs that include the dental and other workforces in substance use disorder and suicide prevention and referral strategies are critical.
Expanding medical-dental integration strategies to include behavioral health clinics is a promising practice that many health care partners are exploring. For example, a preliminary analysis20 of emergency room data by Mental Health Partners in Boulder, Colorado, found that before accessing services in the clinic’s Integrated Health Home,21 32% of patients visited an emergency department for health needs. After six months of accessing medical, dental and behavioral health care through an integrated model, only 13% of patients utilized an emergency department for their health needs.
to evolve, with a focus on mitigating the impact of the COVID-19 pandemic and addressing the challenges mentioned previously. In particular, once safety net clinics and other DCVDOHI partners return to full capacity, clinical metrics will continue to be monitored and enhanced to assess clinic quality improvement efforts and to improve outcomes.
For example, in order to support the integration of all primary health care services, the DCVDOHI program will soon add strategies and tools for bidirectional screenings and referrals between dental and mental health teams. The Oral Health Unit is testing oral health and behavioral health integration strategies and has contracted with one behavioral health organization to train its staff to conduct oral health screenings and plan
However, without whole health strategies, such as reimbursing dental, medical and behavioral health clinics for screening and referring for patients’ primary health care needs, it is unlikely that any private practice and most nonprofit safety net clinics can afford to sustain efforts without consistent grant funding. If insurance reimbursement policies are not viable options for some states, then increases in funding for state public health programs may enable more whole health programs. Value-based payment strategies that incentivize dental systems to collaborate or integrate with medical or mental health systems of care are being implemented in many dental settings.22 However, current payment strategies are most likely not robust or widespread
742 DECEMBER 2022 CDA JOURNAL, VOL 50 , Nº 12
chronic diseases
The DCVDOHI program team continues to experience successes and challenges implementing core strategies.
Inputs Activities
Evidence base for oral health promotion
Funding, technical assistance, resources, other
CDPHE staff: OHU, HSEB, CQI, DCVD, HPCDP, OPPI, Communications, Office of Health Equity
National/federallevel partners: CDC (oral health and chronic disease), ADA, AHA, NACDD, NNOHA, ASTDD, HRSA (workforce and PIOHQI)
State-level partners: CCHN, DCVDOHI Advisory Board, foundations, insurers, coalitions, dental and medical provider associations, University of Colorado and other training programs, individual contractors
Local partners: LPHAs, ROHS, FQHCs, COA and other RAEs
Local coalitions, NDPP/DSMES providers, other health systems
Other input: Existing EHR and HIT data systems
Medical-Dental Integration
• Convene and expand DCVDOHI advisory board to expand and incorporate CVD into DOHI model.
• Collaborate internally to leverage state and federal DCVD funding (CDC DP-181815) to integrate new DCVDOHI model into CQI portfolio, release RFA to recruit FQHC clinic sites and collaborate with key partners.
• Develop DCVDOHI model for private practices.
• Provide training and expand reach of Just Check It with dental providers, new medical offices and LPHAs.
• Enhance and develop new DCVDOHI tools, resources and workflows to support implementation in clinic sites.
• Develop academic detailing training for OHU, ROHS, LPHAs to include DCVD prevention and management.
• Develop and align communications about importance of oral health and chronic disease prevention and management efforts.
• Evaluate and conduct surveillance of medical-dental integration efforts.
Short-Term Outcomes
Intermediate Long-Term Outcomes Outcomes
Increased number of FQHC and clinic sites integrating medical and dental efforts related to diabetes, cardiovascular diseases and oral health.
Increased awareness of state oral health, diabetes and cardiovascular disease needs and priorities.
Increased collaboration between Oral Health Unit, chronic disease prevention and management and health systems units.
Increased percentage of adults screened for diabetes, high blood pressure and high cholesterol in funded clinics.
Increased percentage of patients with diabetes, high blood pressure and/or high cholesterol given referrals for medical or dental clinics.
Increased percentage of adults with diabetes who had a dental visit in past year.
Increased percentage of adults with high blood pressure who had a dental visit in past year.
Increased percentage of patients with history of high blood pressure who have achieved blood pressure control in funded clinics.
Decreased percentage of patients with HbA1C greater than 9 in funded clinics.
Increased referrals from medical to dental clinics.
enough to sustain or grow health system integration programs like DCVDOHI.
States like California, Colorado and others have enabled registered dental hygienists,23 physician assistants, nurses and/or other clinical staff to provide oral health and chronic disease prevention and management services outside of dental settings, but many states have not. While currently funded DCVDOHI clinics have not expanded their work
outside of clinical settings, a future strategy is to bring integrated health programs into community-based settings, such as worksites (especially worksites for lowwage-earning employees), housing facilities (e.g., long-term care facilities or shelters for people experiencing homelessness) and other sites with community members experiencing health inequities.
Another of Colorado’s future priorities includes continued work with safety net
and data partners to integrate oral health metrics and the dental workforce into HIT opportunities, including an upcoming update to Colorado’s HIT roadmap.24
The inclusion of oral health into HIT efforts may support clinical integration efforts. Integrated HIT systems may also eventually lead to opportunities for public health programs to have access to surveillance data, especially if diagnosis codes are implemented in dentistry.
DECEMBER 2022 743 CDA JOURNAL, VOL 50 , Nº 12
BOX
For example, if clinics are consistently documenting caries on recall in their electronic dental records, then public health programs can better understand communities that may need more resources for community-based fluoride varnish or outreach and education programs. The designation of Health Professional Shortage Areas can also be enhanced by HIT data by allowing primary care offices to analyze public health population data and access to primary health care services to identify which communities need more primary health care clinicians.
Finally, because of a recent steep rise in children with Type II diabetes,25 Colorado began discussions to explore modifying DCVDOHI tools for one school oral health partner. The COVID-19 pandemic and subsequent shutdown of school oral health programs derailed the plans. If Colorado receives future and/or additional funds to expand the DCVDOHI program, then staff will seek additional partnerships with child health experts to enhance DCVDOHI tools, enabling dental and other clinicians to address chronic diseases earlier in the lifespan of their patients. Regardless of future funding, Colorado’s Oral Health Unit plans to leverage its current integration work to encourage dental providers to regularly implement small changes in health history forms, intake processes and referral networks.
Colorado’s DCVDOHI program plans to add to the body of evidence that a well-trained and well-incentivized dental workforce can support the prevention and management of chronic diseases, including diabetes and hypertension. The dental workforce may also be leveraged to help mitigate the current behavioral health crises many communities are experiencing.
Additionally, as the DCVDOHI program is demonstrating, medical and behavioral health systems can also be trained and incentivized to improve oral health outcomes. The Colorado Department of Public Health and Environment’s DCVDOHI program provides more holistic strategies and supports clinical systems that are focused on improving population health outcomes and patient and clinical workforce satisfaction while decreasing health care expenditures. As the DCVDOHI program progresses, Colorado plans to include more supportive strategies across public health and clinical partners to sustain this work. ■
FUNDING This manuscript was supported by funding from the Centers for Disease Control and Prevention (CDC) and the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS) as part of awards totaling approximately $1.7 million with 0% financed with nongovernmental sources. The contents are those of the authors and do not necessarily represent the official views of nor an endorsement by HRSA, CDC, HHS, the U.S. government or the state of Colorado.
REFERENCES
1. Jeffcoat M, Jeffcoat R, Gladowski P, Bramson J, Blum J. Impact of periodontal therapy on general health: Evidence from insurance data for five systemic conditions. Am J Prev Med 2014 June;47(2):166–174 doi: 10.1016/j. amepre.2014.04.001. Epub 2014 Jun 18.
2. Baiju RM, Peter E, Varghese NO, Sivaram R. Oral Health and Quality of Life: Current Concepts. J Clin Diagn Res 2017 Jun;11(6):ZE21–ZE26 doi:10.7860/ JCDR/2017/25866.10110. Epub 2017 Jun 1. PMCID: PMC5535498
3. Colorado Department of Public Health and Environment, Center for Health Environmental Data. Vision Information System for Identifying Opportunities and Needs. 2017–2018. Accessed Dec. 1, 2020.
4. Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion. Diabetes and Prediabetes. Accessed Dec. 1, 2020.
5. The Bell Policy Center. Forces Demographics: A Changing Colorado. Accessed June 24, 2021.
6. Trogdon J, Murphy L, Khavjou O, Li R, Maylahn C, Tangka F, et al. Costs of chronic diseases at the state level: the chronic disease cost calculator. Prev Chronic Dis 2015 Sept;12:150131 doi: 10.5888/pcd12.150131
7. Agency for Healthcare Research and Quality. ACTS Supports
the Quadruple Aim. Accessed Aug. 14, 2021.
8. Association of State and Territorial Dental Directors. CDC Funded Grants to 6 States to Develop Models of Collaboration for State Chronic Disease and Oral Health Program: DP-161609. 2016. Accessed Dec. 1, 2020.
9. Centers for Disease Control and Prevention. CDC-Funded Programs: Cooperative Agreements. 2019. Accessed Dec. 1, 2020.
10. Colorado Department of Public Health and Environment. Cavity Free at Three Program. Accessed Dec. 1, 2020.
11. National Maternal and Child Oral Health Resource Center, Consortium for Oral Health Systems Improvement. Perinatal and Infant Oral Health Quality Improvement Initiative. 2019. Accessed Aug. 14, 2021.
12. Colorado Department of Public Health and Environment. Clinical Quality Improvement Portfolio. Accessed Aug. 16, 2021.
13. Delta Dental of Colorado Foundation. Initiatives CO MDI Accessed Dec. 1, 2021.
14. Colorado Community Health Network. Oral Health Integration: A manual for the Colorado Community Health Network. 2015. Accessed Dec. 1, 2020.
15. Accelerating Care Transformation Center. Improving Chronic Illness Care Primary Care Team Guide. Accessed Aug. 16, 2021.
16. Smiles for Life. A National Oral Health Curriculum. Smiles For Life produces educational resources to ensure the integration of oral health and primary care. Accessed Dec. 4, 2020.
17. Colorado Access. Association between dental care and reduced hazard of emergency department utilization in individuals with diabetes. Accessed Dec. 4, 2020.
18. Centers for Disease Control and Prevention. Overdose deaths accelerating during COVID-19: Expanded prevention efforts needed. Accessed Aug. 14, 2021.
19. Czeisler MÉ , Lane RI, Petrosky E, et al. Mental health, substance use and suicidal ideation during the COVID-19 pandemic — United States, June 24–30, 2020. MMWR Morb Mortal Wkly Rep 2020 Aug 14;69(32):1049–1057 doi: 10.15585/mmwr.mm6932a1 PMCID: PMC7440121 Accessed Aug. 15, 2021.
20. Colorado Department of Public Health and Environment, Oral Health Unit. Oral health partner spotlight. Accessed Aug. 13, 2021.
21. Mental Health Partners. Integrated Health Home. Accessed Aug. 13, 2021.
22. National Association of Community Health Centers and DentaQuest Partnership for Oral Health Advancement. Oral Health Value-Based Care: The Federally Qualified Health Center (FQHC) Story. Boston 2020. doi: 10.35565/DQP.2020.2013
23. American Dental Hygiene Association. Dental Hygiene Practice Act overview: Permitted functions and supervision level by state. Accessed Aug. 15, 2021.
24. State of Colorado, Office of eHealth and Innovation. Colorado Health IT Roadmap. Accessed Aug. 15, 2021.
25. Dabelea D, Mayer-Davis EJ, Saydah S, et al. Prevalence of Type 1 and Type 2 diabetes among children and adolescents from 2001 to 2009. JAMA 2014 May 7;311(17):1778–1786 doi:10.1001/jama.2014.3201
THE CORRESPONDING AUTHOR, Katya Mauritson, DMD, MPH(c), can be reached at vso9@cdc.gov.
744 DECEMBER 2022 CDA JOURNAL, VOL 50 , Nº 12
chronic diseases
Digital Accessibility Lawsuits Are on the Rise: Is Your Website AwDA Compliant?
TDIC Risk Management Staff
Dentists take professional and personal satisfaction in providing safe, effective care for patients of all ages and abilities. So, it can come as a shock when they are faced with a lawsuit for violations of the Americans with Disability Act (AwDA). This is especially disconcerting when the individual filing the lawsuit is not even an existing or prospective patient nor someone who has ever visited the office.
In recent years, a steadily rising wave of litigation based on infractions against the AwDA has impacted businesses of all types throughout the United States. While many of these suits are grounded in physical barriers to access, “click by” lawsuits are being filed in increasing numbers against businesses for digital violations.
More than 2,800 digital accessibility lawsuits were filed in federal courts in 2021, a 14% increase from those filed in 2020, according to Seyfarth Shaw, a firm that annually reports the number of lawsuits filed for Title III. Since 2013, more digital accessibility lawsuits have been filed in California than in any other state (5,930), with more than 500 of those being filed since the beginning of 2022.
The Dentists Insurance Company (TDIC) has noted an increase in calls to its Risk Management Advice Line from dentists who are facing AwDA digital accessibility lawsuits. TDIC’s risk management analysts offer guidance on accessibility law and compliance.
The Law and Reasonable Accessibility
If you are confused about the laws
regarding accessibility and compliance, you are not alone! Website compliance is notoriously complex. At a high level, the AwDA requires certain businesses to provide accommodations for people with disabilities. Dental offices fall under public accommodations requirements (Title I and Title III) and, in addition to physical accommodations on their premises, must have websites that offer “reasonable accessibility” to people with disabilities. These criteria include, but are not limited to:
■ Alternative text for images and nontext content.
■ Video closed captioning for the hearing impaired.
■ Compatibility with screen reader technology.
■ Colors, contrast and text sizing to facilitate readability.
■ Predictable page order and understandable navigation.
■ Ability for users to avoid or correct input mistakes.
Benefits and Risks of Digital Accessibility Compliance and Noncompliance
Dental practices that achieve compliance with Titles I and III of the AwDA benefit not only from reduced legal risk but also from improvements in user experience and the ability to reach a larger patient base. According to the Center on Disability at the Public Health Institute, over 10% of the population of California is considered disabled, with almost half of those individuals dealing with vision or hearing loss that affects their ability to fully utilize digital resources. An aging
population increases the likelihood of future users needing accessible digital formats. Website accessibility also helps those experiencing situational or temporary disabilities, such as injuries, which may affect how a person accesses information digitally.
Creating and maintaining an AwDA-compliant website helps protect your practice against lawsuits and fines, in addition to providing needed accommodations for current and potential patients. Failure to create an AwDAcompliant website could open your practice to lawsuits, financial liabilities and damage to your brand reputation.
Unfortunately, because compliance can be complicated, small business websites are low-hanging fruit for predatory litigation. In California, minimum damages for a first offense are $4,000 and can multiply for every site revisit — as much as $25,000 to $30,000 in legal fees or mediation if not covered by your dental business liability insurer. Dentists aren’t expected to be web experts nor have web content that is updated as often as e-commerce businesses, so their sites are less likely to be accessible, making them particularly vulnerable to anyone targeting noncompliant websites.
Example of a Noncompliant Dental Practice Website
A claim handled by TDIC illustrates the need to check website compliance with AwDA guidelines. A dentist was sued for unlawful discrimination by a man who claimed that he was completely deaf and accused the dental office of preventing him from fully and equally accessing video
DECEMBER 2022 745 CDA JOURNAL, VOL 50 , Nº 12
RM Matters
content on the practice’s website.
The plaintiff claimed that he was a prospective patient and was looking for information about the dental office online. According to the lawsuit, the website offered videos of patient reviews intended to attract new patients, but the plaintiff was unable to access the content fully and equally because it lacked closed captioning for the audio. The plaintiff alleged that his inability to access the video content caused him “difficulty and discomfort” and deterred him from pursuing oral health services with the dental office.
The dentist confirmed that the plaintiff was not a patient of record and had never scheduled an appointment with the dental office. The plaintiff claimed that although he was not a patient, he was visiting the website to potentially seek out services from the dental office. He also revealed that his visit to the office’s website was made in part in the capacity of a tester — someone who visits a public accommodation with the intent of establishing whether the public accommodation discriminates against people with disabilities. The courts in California currently allow “tester” litigation.
In this case, the dental office’s website was found to be noncompliant as alleged, and TDIC worked with the plaintiff’s attorney to settle the case.
“The majority of these lawsuits are filed without notice,” said Mark Gibson, an attorney who specializes in defending AwDA cases. “Many plaintiffs are targeting dental offices for profit and have no intention of becoming patients. They have little interest in giving the office notice or an opportunity to fix it before filing suit, as that may reduce the value of their case.” Gibson advises, “Since these suits can come without warning, the best defense is to be proactive in auditing and regularly updating the website.”
Making Your Web Content Accessible
Just like your dental practice, your site must be accessible to new and existing patients, and you can take steps to best represent your practice and minimize legal risks.
to the content they need.
■ A consistent, organized layout that can be easily navigated throughout the entire site.
CDA members can also log in to cda.org to access a helpful guide on AwDA and state laws regarding accessibility.
An aging population increases the likelihood of future users needing accessible digital formats.
Practice leaders should ensure that the individuals or companies hired to build or update the website are both aware of the accessibility standards and working to ensure your website adheres to those requirements for compliance. Look for a web designer experienced in Web Content Accessibility Guidelines (WCAG) or ask someone who specializes in website accessibility auditing to recommend a designer.
Some of the basic pieces to achieving compliance are:
■ Alt tags for all images, videos and audio files, which allow users with disabilities to read or hear alternative descriptions of content they might not otherwise be able to view.
■ Text transcripts for video and audio content, which help hearing-impaired users understand content that would otherwise be inaccessible to them.
■ Identifying the site’s language in the header code, which helps users who utilize text readers.
■ Alternatives and suggestions when users encounter input errors so visitors can better navigate
TDIC’s Risk Management experts recommend that dental practices update their websites yearly and whenever there is a significant change in staff, services or practice hours to ensure that their websites are a current representation of their practices. Regular website updates also help with Google search engine (SEO) rankings. This means if your website is regularly updated, you’ll have a better chance of showing up in a Google search when a potential patient searches for a dentist in your area.
The digital face of your practice can comply with federal web content standards to accommodate the needs of visitors while providing relevant information and resources for your patients. A best practice is to designate one member of the practice team to review the website on a regular basis (quarterly for large practices and semiannually for smaller practices) and verify:
■ All hyperlinks are active and accurate.
■ Practice information is current.
■ Staff listings are up to date.
■ Content is a true reflection of the practice.
■ Any inactive sites or pages have been taken down.
It is unfortunate that a growing number of plaintiffs and their attorneys are leveraging AwDA compliance to pursue personal profit; however, the trend underscores the need to make dental practices physically and digitally accessible and welcoming to patients with disabilities. Your website may be a prospective patient’s first impression of your practice and your team. Ensure it
746 DECEMBER 2022 CDA JOURNAL, VOL 50 , Nº 12
DEC. 2022 RM MATTERS
demonstrates your adherence to standards and commitment to inclusive experiences. ■

The Dentists Insurance Company’s Risk Management Advice Line is a benefit available at no cost to CDA members, as well as to policyholders protected by TDIC. To schedule a consultation, visit tdicinsurance.com/RMconsult or call 877.269.8844.
Expert

DECEMBER 2022 747 CDA JOURNAL, VOL 50 , Nº 12
• A
• One-on-one
• Ongoing
Visit us
tdicinsurance.com/RM Scan
explore: @TDICinsurance | CA Lic # 2361-4
support to manage your risks. TDIC is here to help you understand and navigate dentistry’s risks. Policyholders benefit from unique tools and expertise:
library of time-saving forms, guides and templates
guidance from dedicated Advice Line analysts
education on through live and online seminars
online:
here to
Control expenses.
More membership value from vendors dentists can trust.


The California Dental Association leverages the strength of our large membership to deliver more value to practices of every size. Benefit from member-exclusive pricing and expert support to control your practice expenses. Explore products and

Flex your cash flow with a card designed just for dentists and earn extra rewards points for your ADA, CDA and practice-related purchases.
Get smart guidance, competitive rates and reduced fees on practice financing solutions that help you purchase, restructure or grow.
Get competitive prices on dental supplies you love from brands you trust through membership’s collective purchasing power.
®
ENDORSED SERVICES
services for the business side of practice at cda.org/EndorsedServices
What Prescribers Should Know
CDA Practice Support

This article reviews what California prescribers should know about prescribing medicines in the state. Information on requirements for prescribers who dispense or administer controlled substances and other medication will be addressed in a future article. More information on prescribing and CURES is in two CDA Practice Support resources available on cda.org
What is required to prescribe in California?
A dentist must have an active dental license to prescribe medicines. No other state registration is required. To prescribe controlled substances, however, a dentist also must be registered with the U.S. Drug Enforcement Administration (DEA).
What are the rules for obtaining a DEA registration?
A DEA registration number is site specific. Before applying for a DEA number, a dentist should ensure their address in dental board records is the same address they are using on the DEA application. If a dentist administers a controlled substance at more than one office, the dentist must obtain separate DEA registration numbers for each location (the board requires that dentists report each place of practice). Additional DEA registrations are not required if a dentist only prescribes at other office locations within California and does not administer or dispense controlled substances there.
The DEA permits an individual practitioner, such as a locum tenens dentist, to use a home address as the
principal place of business. In such cases, the location is considered a “controlled premises” and is subject to unannounced inspections and administrative warrants. Recordkeeping and security requirements remain the same.1
Practitioners may not use a P.O. box or private mailing box address for DEA registration.

Does a dentist need a DEA registration if they do not prescribe, administer or dispense controlled substances?
The law does not require it. However, dental plans may require a dentist to be registered with the DEA as part of their credentialing process. Always check with each contracted plan prior to giving up a DEA registration.
DECEMBER 2022 749 CDA JOURNAL, VOL 50 , Nº 12
Regulatory
Compliance
LDM_CDA_Journal_1.3_Square_LindaBrown_05_23_17.indd 1 5/24/2017 9:21:40 PM
Is electronic prescribing required in California?
Electronic data transmission prescriptions are mandated in California as of Jan. 1, 2022. However, recent legislation expanded the following permitted exceptions to the mandate:
■ The prescription is issued for use by a patient with a terminal illness.
■ An electronic data transmission prescription is unavailable due to a temporary technological or electrical failure as defined by law.
■ The prescription is intended to be dispensed by a pharmacy located outside of California.
■ The prescription is issued in a hospital emergency department or urgent care clinic and one or more of the following conditions are present:
■ The patient resides outside the geographic area of the hospital.
• The patient is homeless or indigent and does not have a preferred pharmacy.
• The prescription is issued at a time when a patient’s regular or preferred pharmacy is likely to be closed.
• Under any of the conditions described above, a prescription must be electronically issued but does not require electronic transmission and may be provided directly to the patient.
■ The prescription is issued by a veterinarian.
■ The prescription is for eyeglasses or contact lenses.
■ The prescription is issued by a prescribing health care practitioner serving as a volunteer in a free clinic and receives no remuneration for their services.
■ The prescribing health care practitioner and the dispenser are the same entity.
■ The prescription is issued by a
prescribing health care practitioner under circumstances whereby the practitioner reasonably determines that it would be impractical for the patient to obtain substances prescribed by an electronic data transmission prescription in a timely manner and the delay would adversely impact the patient’s medical condition.
■ The issued prescription includes elements not covered by the latest version of the National Council for Prescription Drug Programs’ SCRIPT standard.
■ The prescriber registers with the California State Board of Pharmacy, stating that they meet one or more of the following criteria:
• Their practice is in the area of an emergency or disaster declared by a federal, state or local government.
• They issue 100 or fewer prescriptions per calendar year.
• They are unable to issue electronic data transmission prescriptions due to circumstances beyond their control.
To remain exempt, a prescriber must annually register with the pharmacy board and maintain documentation of the circumstances qualifying them for exemption. The pharmacy board will post a list of registered prescribers on its website.
Be aware of patients with prescription drug benefits under Medicare/Medicaid, as their prescriptions must be submitted by electronic data transmission in order for the program to pay for it.
What is required on a prescription form?
If a prescriber is exempt from using electronic data prescriptions, they must ensure paper prescriptions for controlled substances are on tamper-resistant forms
printed by state-approved printers with the following required elements detailed in Health & Safety Code §11162.1:
■ A latent, repetitive “void” pattern printed across the entire front of the form.
■ A watermark of “California Security Prescription” printed on the backside of the form.
■ A chemical void protection that prevents alteration by chemical washing.
■ A feature printed in thermochromic ink.
■ An area of opaque writing so that the writing disappears if the prescription is lightened.
■ A description of the security features included on each form.
■ Six quantity check-off boxes so that a prescriber may indicate quantity by checking the applicable box. A box should appear next to the following quantities: 1-24; 25-49; 50-74; 75-100; 101-150; 151 and over. Additionally, a space should be in the area to designate the units referenced in the quantity boxes when the drug is not in tablet or capsule form.
■ The statement “Prescription is void if the number of drugs prescribed is not noted” printed on the bottom of the form.
■ The preprinted name, license category, license number, DEA registration number and address of the prescriber. (Including the individual NPI number is recommended.)
■ Check boxes to indicate number of refills.
■ Space to indicate the date of origin of the prescription.
■ A check box indicating the prescriber’s order to not substitute.
■ The approved security printer’s identifying number.
■ If multiple prescriber names
750 DECEMBER 2022 CDA JOURNAL, VOL 50 , Nº 12
DEC. 2022 REG. COMPLIANCE
are printed on a form, a check box next to each name.
■ A uniquely serialized number as prescribed by the Department of Justice.
Each batch of controlled substance prescription forms must have a lot number printed on the form and each form within that batch numbered sequentially beginning with the numeral one.
Prescriptions for noncontrolled substances may be written on a tamperresistant form or orally transmitted to the pharmacy.
What are a prescriber’s obligations with respect to CURES?
CURES is the state’s prescription drug monitoring database. Every controlled substance prescriber is required to register with CURES to access its information and to report the dispensing of controlled substances (dispensing medication is different from
administering it).
A prescriber is required to check CURES for a patient’s prescription history before prescribing a Schedule II-IV drug. The intent of the requirement is to assist prescribers in making better prescribing decisions and to reduce prescription drug abuse. One exception to this requirement is: “… if a health care practitioner prescribes, orders, administers, furnishes or dispenses a controlled substance to a patient as part of the patient’s treatment for a surgical procedure, if the quantity of the controlled substance does not exceed a nonrefillable five-day supply of the controlled substance to be used in accordance with the directions for use …”
If the controlled substance remains part of the patient’s treatment, a prescriber must subsequently check CURES prior to writing another prescription and every four months while
the substance is part of the patient’s treatment. The patient activity report may not be pulled earlier than 24 hours prior to issuing a prescription. ■
Regulatory Compliance appears monthly and features resources about laws that impact dental practices. Visit cda.org/practicesupport for more than 600 practice support resources, including practice management, employment practices, dental benefit plans and regulatory compliance.
REFERENCE
1. U.S. Drug Enforcement Administration. Registration Q&A. Accessed Sept. 21, 2022.
DECEMBER 2022 751 CDA JOURNAL, VOL 50 , Nº 12
PROGRAM • Two
•
• All the resources you
• An
• Low-cost
more and register today at
. Set up your
to ensure
CDA PRESENTS Bloodborne pathogen and infection control are not the same. Did you know that Cal/OHSA requires annual bloodborne pathogen training for dental professionals, as well as annual review for practices’ exposure control plans? CDA has developed convenient, flexible and affordable training — available only to members and their practice teams. NEW! BLOODBORNE PATHOGENS AND EXPOSURE CONTROL PLAN
how-to courses to help dental practice leaders train others
Blended program with on-demand learning for current and future staff
need to complete an exposure plan with your team
easy path to achieve full Cal/OSHA compliance
options designed for every practice size Learn
cda.org/BBP
Online Learning account with the same email you use for cda.org
access to members-only learning options.
Is your practice fully in compliance?
A look into the latest dental and general technology on the market
iPhone 14 Pro ($999-$1,499, Apple)
Apple’s iPhone is an iconic, ubiquitous piece of gear that has set the standard for what should be expected from a mobile phone. While each component — camera, processor, display, battery, software — may not be the cutting edge in themselves, the sum of these parts is what makes the iPhone special. As was uttered by Steve Jobs year after year, “It just works.” Apple’s latest offering, the iPhone 14 Pro, strives to be the embodiment of this mantra as it addresses longstanding gripes like the camera quality, screen resolution and the infamous notch. The 512GB model was reviewed for this article.
From a physical appearance, the iPhone 14 Pro has similar dimensions to the iPhone X and is slightly heavier. The camera is quite considerable and does not allow the device to lay flat. The screen is responsive thanks to its 120Hz refresh rate and is easy to read even in broad daylight. The A16 processor is fast, handling everything from multitasking productivity tasks to gaming with ease. The biggest upgrades are reserved for the new 48MP camera and dynamic notch. Once the exclusive features of many Android devices, Apple implements them to great effect. The camera is capable for photography and videography while the dynamic notch space at the top of the screen displays relevant information based on what is occurring. Overall, the iPhone 14 Pro is a fantastic device because of its features, reliability and tight integration of features and is certainly among the best mobile phones on the market today.
— Alexander Lee, DMD
Belkin iPhone Mount ($29.95, Belkin)
Most built-in webcams on laptop computers deliver standard quality video. Because many laptops have displays with thin profiles, the webcam capabilities of these displays are severely limited. On the other hand, smartphone cameras are among the best in capturing video with incredible detail and quality. With the release of macOS Ventura (10.13) and iOS 16, MacBook and iPhone owners can take advantage of a feature known as Continuity Camera, which allows the rear cameras of a compatible iPhone to be used as a webcam on the MacBook. The Belkin iPhone Mount with MagSafe for Mac Notebooks lets users make use of Continuity Camera with their iPhone mounted to the top of their MacBook display.
The Belkin iPhone Mount with MagSafe for Mac Notebooks is a compact, low-profile, circular magnetic accessory that attaches to the back of a MagSafe-compatible iPhone. The base of the mount has a rubber-like texture that feels both soft and rugged. There are two attachments that can swivel out from the base. First is a metal ring that can be used either as an iPhone hand grip or a kickstand to prop the iPhone upright on a surface. The other is a clip that is designed to hang on the top edge of a MacBook display. The mount works as intended with Continuity Camera, but users will find their display tilt range severely limited because the iPhone is too heavy to be supported by the display hinge. As a result, users must keep their MacBook display tilted at an angle that can handle the weight of the iPhone or use a support to prop the display upright at the desired tilt. The clip is made of the same rubber-like material as the base of the mount, so it will not damage the MacBook display. This accessory has many useful purposes, but the main feature of using Continuity Camera can be awkward depending on the type of iPhone and MacBook it is being used on due to this limited display tilt range issue.
— Hubert Chan, DDS
CDA JOURNAL, VOL 50 , Nº 12 DECEMBER 2022 753
Tech Trends
Pursue smart employment practices.
As a CDA member, you have access to a full library of helpful resources for employers, plus the expertise of dedicated Practice Support analysts.
Better understand training requirements, paid sick leave, wage and hour laws, notices and more. And save time with our custom employee manual generator.
Explore your CDA member resources at cda.org/EmploymentPractices.
Dental Benefit Plans Employment Practices Regulatory Compliance Practice Management

® PRACTICE SUPPORT
Dr. Stephanie Sandretti Member since 2015
Index to 2022 Articles Journal of the California
Dental Association Vol. 50 Nos. 1–12
Author Index
Rachel Anderson
Oral Health Intervention Before Pregnancy: A Preconception Approach Vol. 50, No. 4:217
Pamela S. Arbuckle Alston
The Importance of Diversity, Equity and Inclusion From the Clinician’s Perspective

Vol. 50, No. 10:605
Anders Bjork
Impact of COVID-19 on Dentistry

Vol. 50, No. 2:103
California Department of Public Health, Office of Oral Health
Toolkit: When Sugar Is Not So Sweet Vol. 50, No. 5:277
Jean Calvo
Strategies To Reduce the Use of General Anesthesia for Children and Adolescents With Special Health Care Needs: Dental Desensitization and ‘Shorten the Line’ Models Vol. 50, No. 6:345
Kerry K. Carney
Connections, Redemption and Dentistry Vol. 50, No. 10:571
Secret Welcome Sign, Really? Vol. 50, No. 9:499
A Little Bit of Normal Vol. 50, No. 7:383
Student Debt: American Dream or American Nightmare Vol. 50, No. 12:715
When Bad Things Bring Good Lessons Vol. 50, No. 3:139
Paul S. Casamassimo Pain, Psyche and Protective Stabilization Vol. 50, No. 8:473
Benjamin W. Chaffee
A Dental Care Coordination System To Increase Access for Medicaid Dental Program Beneficiaries: Experiences in Alameda County, California Vol. 50, No. 3:147
David W. Chambers
Ethics Should Fit the Scope of Practice Vol. 50, No. 1:5
Elisa M. Chávez
Improving Access to Care and Patient Experience Through Diversity, Equity, Inclusion and Belonging Vol. 50, No. 109:589
One More Look at Medicare and Why a Dental Benefit Is Still Needed for All Vol. 50, No. 7:407
Eve Cuny
Safe Dental Care During the COVID-19 Pandemic Vol. 50, No. 2:97
Ellen Darius
Care Coordination: A Valuable Adjunct To Dental Practice — Lessons Learned in a Public Health Setting Vol. 50, No. 6:359
Amelia David
Evaluating the Effectiveness of Periodontal Data Collection Practices in Second-Year Dental Students Vol. 50, No. 11:663
Usha Dayanarayana
Allergic Manifestations in the Oral Cavity Vol. 50, No. 5:245
Emily Duong
Salivary and Plaque Microbiomes During Treatment With Different Orthodontic Appliances Vol. 50, No. 11:683
Jared I. Fine
Persistence and Commitment: Unparalleled Advocacy in 2022 — A Game Changer for Vulnerable Californians Vol. 50, No. 12:723
Steven W. Friedrichsen
DEIB: Looking to a Future of Equity and Excellence Vol. 50, No. 10:577
Kenneth J. Glenn
Childhood Adversity Correlates With Young Adult Health Dental Patient Behaviors Vol. 50, No. 11:693
Richard Graham
State of the CDA Foundation Vol. 50, No. 6:309



DECEMBER 2022 755 CDA JOURNAL, VOL 50 , Nº 12 2022 Index
Journa CALIFORNIA DENTAL ASSOCIATION Teledentistry Hybrid Learning Case-Based Discussions Community-Based Education January 2022 JANUARY 2022 Vol 50 Nº Dental Student Research Mariela Padilla, DDS, M.Ed Journa CALIFORNIA DENTAL ASSOCIATION Collective Strength Infection Control Impact of COVID-19 Oral Health Implications February 2022 Living and Practicing With COVID-19 Natasha A. Lee, DDS FEBRUARY 2022 Vol 50 Nº Journa CALIFORNIA DENTAL ASSOCIATION Adenomatoid Odontogenic Tumors Mouth-COVID-19 March 2022 A Dental Care Coordination System To Increase Access for Medicaid Dental Program Beneficiaries: Experiences in Alameda County, California MARCH 2022 Vol 50 Nº
Christine Y.W. Hao
Rollout of the Oral Health Literacy Toolkit in California: A Mixed-Methods Analysis Vol. 50, No. 11:671
Oussama Hefnawi
Impact of Hybrid Learning on Students’ Performance in Biomedical Sciences During COVID-19 Pandemic Vol. 50, No. 1:27
Katrina Holt
Improving Oral Health and Overall Health for Pregnant People and Infants

Vol. 50, No. 4:211
Jennifer Kent
Reshaping the Medi-Cal Dental Program — Evolving Oral Health Care in California Vol. 50, No. 7:401
Soh Yeun Kim
Management of Hypertensive Crisis in a Dental School: 10Year Retrospective Review of Medical Emergency Incidents With Recommendations Vol. 50, No. 11:653
Ronald W. Kosinski
NYU Dentistry Oral Health Center for People With Disabilities Vol. 50, No. 6:353
Jayanth Kumar
COVID-19 and Oral Health Care: Implications for Dental Practices Vol. 50, No. 2:119



Improving the Oral Health of Pregnant People: The Need for a Health Care-Public Health Partnership Vol. 50, No. 4:203
WHEN SUGAR IS NOT SO SWEET

Zahed Mohammadi
Cryotherapy in Endodontics: A Critical Review Vol. 50, No. 12:727
Shervin Molayem
The Mouth-COVID-19 Connection: Importance of the Oral Cavity for the Coronavirus — Part I Vol. 50, No. 3:165
Shervin Molayem
The Mouth-COVID-19 Connection: Importance of the Oral Cavity for the Coronavirus — Part II Vol. 50, No. 3:175
Tarun Mundluru
A Mandibular Adenomatoid Odontogenic Tumor With a Novel Treatment Utilizing Platelet-Rich Fibrin Vol. 50, No. 3:159
Richard J. Nagy
Dentistry’s Collective Strength During Unprecedented Times Vol. 50, No. 2:87
Nam Nguyen
Embracing Precision and Data Science in Dentistry Vol. 50, No. 8:441
Katherine Lambert
Informed Consent in the Older Adult Population: A MixedMethods Study Vol. 50, No. 5:257
Setareh Lavasani
Inadequate Dental Imaging Delays Diagnosis of Pathologic Le Fort I Fracture Secondary to Bisphosphonate Use Vol. 50, No. 9:513
Oral and Maxillofacial Radiology Diagnosis: The Role of Image Modality Selection, Interpretation Skills and Use of Cone Beam Computed Tomography Technology Vol. 50, No. 9:509

Natasha A. Lee
Living and Practicing With COVID-19 Vol. 50, No. 2:83
Mary J. Lomax-Ghirarduzzi
Humanizing Oral Health: Race, Representation and Equity in Dental Education and Oral Health Care Vol. 50, No. 10:581
Katya Mauritson
Integrated Approaches to Preventing and Managing Chronic Diseases: Colorado’s Diabetes Cardiovascular Disease Oral Health Integration Program Vol. 50, No. 12:733
Antranig Mesrobian
Evolution of Patient Care Post-Pandemic: Teledentistry the New Norm, a Narrative Review Vol. 50, No. 1:17
Mark Mintline
The Synergistic Role of 2D and 3D Imaging in Evaluating Tumors of the Jaws: A Case Report of Diffuse Large B-Cell Lymphoma of the Mandible Vol. 50, No. 9:519
Dennis Paul Nutter, DDS
How Do We Protect a Child’s Psychological Health During Procedures That Use Protective Stabilization? Vol. 50, No. 8:453
Viren R. Patel
Facing the Challenge of Dental Benefit Plans Vol. 50, No. 7:389
Christine I. Peters
Dental Student Community Clinic Placement in Australia and the United States: Systematic Review and Case Study Vol. 50, No. 1:49
756 DECEMBER 2022 CDA JOURNAL, VOL 50 , Nº 12 2022 Index
Journa CALIFORNIA DENTAL ASSOCIATION Dental Care During Pregnancy Adults and Infants Oral Health Preconception Intervention April 2022 Improving the Oral Health of Pregnant People The Need for a Health Care-Public Health Partnership APRIL 2022 Vol 50 Nº Jayanth V. Kumar, DDS, MPH and Renee Samelson, MD, MPH Journa CALIFORNIA DENTAL ASSOCIATION Allergic Manifestations Informed Consent in Older Adults Glycemic Index Management May 2022 MAY 2022 Vol 50 Nº
Journa CALIFORNIA DENTAL ASSOCIATION September 2022 Medication-Related Osteonecrosis of the Jaw Diffuse Large B-Cell Lymphoma Digital Workflows 2D and CBCT in Orthodontics SEPTEMBER 2022 Vol 50 Nº
Christian Pretto
Management of the Glycemic Index Through Periodontal Management With Pharmacological Agents Vol. 50, No. 5:265
Rafeeq N. Rahman
An Overview of Digital Workflows for Precision Implant Dentistry Vol. 50, No. 9:527
Karen Raju
Medical-Dental Integration: A Promising Approach To Address Unmet Dental Needs of Children and Youth With Special Health Care Needs Vol. 50, No. 6:331
Ruchi K. Sahota
The Great Resignation Vol. 50, No. 8:435
The Rise of Podcasts Vol. 50, No. 2:75
Charles D. Stewart
Commercial Dental Benefit Plans Vol. 50, No. 7:393



Ray E. Stewart
Oral Health Care for Californians With Special Health Care Needs: A Problem in Need of a Solution Vol. 50, No. 6:317
Oral Health Care for People With Special Health Care Needs: A Call To Action Vol. 50, No. 6:315
Nathan Suter
Benefit Design and Reimbursement Considerations for Teledentistry Vol. 50, No. 7:415
Ariane Terlet
Who We Are and Where We Are Going Vol. 50, No. 4:195
Zohra Tumur Dental Student Research Vol. 50, No. 11:651
Paula
Andrea Villa-Machado
The Role of CBCT and Guided Endodontics in Accessing a Calcified Maxillary Molar Using Computer-Assisted Dynamic Navigation: A Case Report Vol. 50, No. 9:551
Lynn Walton-Haynes
Dental Care in California During Pregnancy Vol. 50, No. 4:207
Marisa K. Watanabe
Innovative Approaches for Fostering DEI Development in Preclinical and Clinical Training Vol. 50, No. 10:613
Empowering Ourselves and Others Vol. 50, No. 5:237
MultiGen at Work Vol. 50, No. 11:643

Allen Wong
Billing for Extra Time Needed To Treat Individuals With Special Needs Vol. 50, No. 6:367

Predoctoral Curriculum Modifications in Caring for Patients With Special Health Care Needs Vol. 50, No. 6:325
Audrey Yoon
An Update on the Utilization of 2D and Cone Beam Computed Tomography Imaging in Orthodontics Vol. 50, No. 9:541

Brandon Zegarowski
Efficacy of Virtual Asynchronous Didactic Delivery and CaseBased Discussions for Predoctoral Orthodontic Education Vol. 50, No. 1:35
Title Index
A Dental Care Coordination System To Increase Access for Medicaid Dental Program Beneficiaries: Experiences in Alameda County, California
Benjamin W. Chaffee, Jared I. Fine, Yilak Fantaye, Kristin S. Hoeft, Rhodora Ursua, Ray Stewart, Suhaila Khan Vol. 50, No. 3:147
A Little Bit of Normal Kerry K. Carney Vol. 50, No. 7:383
A Mandibular Adenomatoid Odontogenic Tumor With a Novel Treatment Utilizing Platelet-Rich Fibrin
Tarun Mundluru, David Pilgrim, Reyes Enciso,Parish P. Sedghizadeh, Mohammad A. Khalifeh Vol. 50, No. 3:159
Allergic Manifestations in the Oral Cavity
Usha Dayanarayana, Shilpa Padar Shastry, Chetan Shankar, Naveen Kumar N, Rama Murthy TK, Mahesh BS Vol. 50, No. 5:245
An Overview of Digital Workflows for Precision Implant Dentistry
Rafeeq N. Rahman, Alexander Lee, Setareh Lavasani, Tobias Boehm Vol. 50, No. 9:527
DECEMBER 2022 757 CDA JOURNAL, VOL 50 , Nº 12
Journa CALIFORNIA DENTAL ASSOCIATION Commercial Dental Benefits Medi-Cal Dental Program Medicare Coding and Reimbursing for Teledentistry July 2022 JULY 2022 Vol 50 Nº dental
FACING THE CHALLENGES OF VIREN R. PATEL, DDS Journa CALIFORNIA DENTAL ASSOCIATION Protective Stabilization Medical Immobilization Missed Dental Appointments August 2022 AUGUST 2022 Vol 50 Nº EMBRACING PRECISION AND DATA SCIENCE IN DENTISTRY Journa CALIFORNIA DENTAL ASSOCIATION September 2022 Medication-Related Osteonecrosis of the Jaw Diffuse Large B-Cell Lymphoma Digital Workflows 2D and CBCT in Orthodontics SEPTEMBER 2022 Vol 50 Nº
benefit plans
An Update on the Utilization of 2D and Cone Beam Computed Tomography Imaging in Orthodontics
Audrey Yoon, Linda Phi, Joorok Park Vol. 50, No. 9:541
Benefit Design and Reimbursement Considerations for Teledentistry



Nathan Suter Vol. 50, No. 7:415
Billing for Extra Time Needed To Treat Individuals With Special Needs
Allen Wong, Ellen Darius Vol. 50, No. 6:367
Care Coordination: A Valuable Adjunct To Dental Practice
— Lessons Learned in a Public Health Setting
Ellen Darius, Huong Le, Sridevi Ponnala,Curtis Le Vol. 50, No. 6:359

Childhood Adversity Correlates With Young Adult Health Dental Patient Behaviors
Kenneth J. Glenn, Christina Light, Todd Franke, Shane N. White Vol. 50, No. 11:693
Commercial Dental Benefit Plans
Charles D. Stewart Vol. 50, No. 7:393
Connections, Redemption and Dentistry
Kerry K. Carney Vol. 50, No. 10:571
COVID-19 and Oral Health Care: Implications for Dental Practices



Jayanth Kumar Vol. 50, No. 2:119
Cryotherapy in Endodontics: A Critical Review
Zahed Mohammadi, Sousan Shalavi, Hamid Jafarzadeh Vol. 50, No. 12:727
DEIB: Looking to a Future of Equity and Excellence
Steven W. Friedrichsen, Nader A. Nadershahi Vol. 50, No. 10:577
Dental Care in California During Pregnancy
Lynn Walton-Haynes, Joanna Aalboe, Jayanth V. Kumar Vol. 50, No. 4:207



Dental Student Community Clinic Placement in Australia and the United States: Systematic Review and Case Study Anna Doan Bowers, Ove A. Peters, Paul Subar, Sandra March, Christine I. Peters Vol. 50, No. 1:49
Dental Student Research
Zohra Tumur Vol. 50, No. 11:651
Dentistry’s Collective Strength During Unprecedented Times
Richard J. Nagy Vol. 50, No. 2:87
Efficacy of Virtual Asynchronous Didactic Delivery and Case-Based Discussions for Predoctoral Orthodontic Education
James Chen, Brandon Zegarowski, Mandy Lam Vol. 50, No. 1:35

Embracing Precision and Data Science in Dentistry

Nam Nguyen, Andrew H. Jheon, Michael S. Reddy Vol. 50, No. 8:441
Empowering Ourselves and Others
Marisa Kawata Watanabe Vol. 50, No. 5:237
Ethics Should Fit the Scope of Practice
David W. Chambers Vol. 50, No. 1:5
Evaluating the Effectiveness of Periodontal Data
Collection Practices in Second-Year Dental Students
Amelia David, Soh Yeun Kim, Barnabas Kim, Hyun Il Kim Vol. 50, No. 11:663
Evolution of Patient Care Post-Pandemic: Teledentistry the New Norm, a Narrative Review
Antranig Mesrobian, Karam Korya, Kamal Al-Eryani Vol. 50, No. 1:17
Facing the Challenge of Dental Benefit Plans
Viren R. Patel
Vol. 50, No. 7:389
How Do We Protect a Child’s Psychological Health During Procedures That Use Protective Stabilization?
Dennis Paul Nutter Vol. 50, No. 8:453
Humanizing Oral Health: Race, Representation and Equity in Dental Education and Oral Health Care

Mary J. Lomax-Ghirarduzzi Vol. 50, No. 10:581
Impact of COVID-19 on Dentistry
Anders Bjork Vol. 50, No. 2:103
Impact of Hybrid Learning on Students’ Performance in Biomedical Sciences During COVID-19 Pandemic Oussama Hefnawi, Xi Chen, Mahvash Navazesh Vol. 50, No. 1:27

Improving Access to Care and Patient Experience Through Diversity, Equity, Inclusion and Belonging Elisa M. Chávez Vol. 50, No. 109:589

Improving Oral Health and Overall Health for Pregnant People and Infants
Katrina Holt, Ruth Barzel Vol. 50, No. 4:211
758 DECEMBER 2022 CDA JOURNAL, VOL 50 , Nº 12 Index Journa CALIFORNIA DENTAL ASSOCIATION December 2022 DECEMBER 2022 Vol 50 Nº 12
and
Unparalleled Advocacy in 2022 — A Game Changer for Vulnerable Californians Cryotherapy in Endodontics Chronic Disease Management
Persistence
Commitment:
Improving the Oral Health of Pregnant People: The Need for a Health Care-Public Health Partnership
Jayanth V. Kumar, Renee Samelson Vol. 50, No. 4:203
Inadequate Dental Imaging Delays Diagnosis of Pathologic Le Fort I Fracture Secondary to Bisphosphonate Use
Setareh Lavasani, Ho-Hyun (Brian) Sun, Jeffrey A. Elo Vol. 50, No. 9:513
Informed Consent in the Older Adult Population: A Mixed Methods Study
Katherine Lambert, Grace Yasewicz, Garrett Finney, Thomas Meuser, Regula Robnett, Yang Kang Vol. 50, No. 5:257
Innovative Approaches for Fostering DEI Development in Preclinical and Clinical Training
Marisa K. Watanabe, Lucian O’Connor, Keith R. Boyer, T. Jamie Parado, Paulina A. Saraza, Edmond R. Hewlett, George Taylor, Bradley S. Henson Vol. 50, No. 10:613
Integrated Approaches to Preventing and Managing Chronic Diseases: Colorado’s Diabetes Cardiovascular Disease Oral Health Integration Program
Katya Mauritson, Sara Grassemeyer, Ian Danielson, Abby Laib Vol. 50, No. 12:733
Living and Practicing With COVID-19
Natasha A. Lee Vol. 50, No. 2:83
Management of Hypertensive Crisis in a Dental School: 10 Retrospective Review of Medical Emergency Incidents With Recommendations
Soh Yeun Kim, Sarah Lim, Chanmee Esther Kim, Lauren Barlow, Adlene Chang, Holli Riter, Iris Nam, Heidi Christensen, Udochukwu Oyoyo Vol. 50, No. 11:653
Management of the Glycemic Index Through Periodontal Management With Pharmacological Agents
Christian Pretto, Joshua Tordjman, Aviv Ouanounou Vol. 50, No. 5:265
Medical-Dental Integration: A Promising Approach To Address Unmet Dental Needs of Children and Youth With Special Health Care Needs
Karen Raju, Yogita Butani Thakur, Cambria Garell, Irene V. Hilton Vol. 50, No. 6:331
MultiGen at Work
Marisa Kawata Watanabe Vol. 50, No. 11:643
NYU Dentistry Oral Health Center for People With Disabilities
Ronald W. Kosinski Vol. 50, No. 6:353
One More Look at Medicare and Why a Dental Benefit Is Still Needed for All
Elisa M. Chávez Vol. 50, No. 7:407
Oral and Maxillofacial Radiology Diagnosis: The Role of Image Modality Selection, Interpretation Skills and Use of Cone Beam Computed Tomography Technology Setareh Lavasani Vol. 50, No. 9:509
Oral Health Care for Californians With Special Health Care Needs: A Problem in Need of a Solution
Ray E. Stewart, Ben Meisel Vol. 50, No. 6:317
Oral Health Care for People With Special Health Care Needs: A Call To Action
Ray E. Stewart, Ben Meisel Vol. 50, No. 6:315
Oral Health Intervention Before Pregnancy: A Preconception Approach
Rachel Anderson, Hugh Silk Vol. 50, No. 4:217
Pain, Psyche and Protective Stabilization
Paul S. Casamassimo, Beau Meyer, Janice A. Townsend Vol. 50, No. 8:473
Persistence and Commitment: Unparalleled Advocacy in 2022 — A Game Changer for Vulnerable Californians Jared I. Fine Vol. 50, No. 12:723
Predoctoral Curriculum Modifications in Caring for Patients With Special Health Care Needs
Allen Wong, Paul Subar Vol. 50, No. 6:325
Reshaping the Medi-Cal Dental Program — Evolving Oral Health Care in California
Jennifer Kent Vol. 50, No. 7:401
Rollout of the Oral Health Literacy Toolkit in California: A Mixed-Methods Analysis
Christine Y.W. Hao, Karen Sokal-Gutierrez, Susan L. Ivey, Kristin S. Hoeft Vol. 50, No. 11:671
Safe Dental Care During the COVID-19 Pandemic Eve Cuny Vol. 50, No. 2:97
Salivary and Plaque Microbiomes During Treatment With Different Orthodontic Appliances
Emily Duong, Elaine Pham, Julia Esfandi, Kim-Sa Kelly, Arvin Pal, Masooma Rizvi, Nini Tran, Tingxi Wu, Bhumika Shokeen, Renate Lux Vol. 50, No. 11:683
Secret Welcome Sign, Really?
Kerry K. Carney Vol. 50, No. 9:499
State of the CDA Foundation
Richard Graham Vol. 50, No. 6:309
Strategies To Reduce the Use of General Anesthesia for Children and Adolescents With Special Health Care Needs: Dental Desensitization and ‘Shorten the Line’ Models
Jean Calvo, Paul Glassman, Tara Glavin, Helen Mo Vol. 50, No. 6:345
Student Debt: American Dream or American Nightmare Kerry K. Carney Vol. 50, No. 12:715
The Associate Editor: The Great Resignation
Ruchi K. Sahota Vol. 50, No. 8:435
The Importance of Diversity, Equity and Inclusion From the Clinician’s Perspective
Pamela S. Arbuckle Alston, Jessica Baisley, Andrea Akabike, Jack Luomanen Vol. 50, No. 10:605
The Mouth-COVID-19 Connection: Importance of the Oral Cavity for the Coronavirus — Part I Shervin Molayem, Carla Cruvinel Pontes Vol. 50, No. 3:165
The Mouth-COVID-19 Connection: Importance of the Oral Cavity for the Coronavirus — Part II Shervin Molayem, Carla Cruvinel Pontes Vol. 50, No. 3:175
The Rise of Podcasts
Ruchi K. Sahota Vol. 50, No. 2:75
The Role of CBCT and Guided Endodontics in Accessing a Calcified Maxillary Molar Using Computer-Assisted Dynamic Navigation: A Case Report
Paula Andrea Villa-Machado, Julián González-García, Felipe Augusto Restrepo-Restrepo Vol. 50, No. 9:551
The Synergistic Role of 2D and 3D Imaging in Evaluating Tumors of the Jaws: A Case Report of Diffuse Large B-Cell Lymphoma of the Mandible
Mark Mintline, Jeffrey A. Elo, Setareh Lavasani, James Ywom, Ashtin Alves, Ho-Hyun (Brian) Sun Vol. 50, No. 9:519
Toolkit: When Sugar Is Not So Sweet
California Department of Public Health, Office of Oral Health Vol. 50, No. 5:277
When Bad Things Bring Good Lessons
Kerry K. Carney Vol. 50, No. 3:139
Who We Are and Where We Are Going
Ariane Terlet Vol. 50, No. 4:195
DECEMBER 2022 759 CDA JOURNAL, VOL 50 , Nº 12
SIMPLY BRILLIANT. ®
SAVE THE DATE Connect with us California

Dental Association

Anaheim, California May 18–20, 2023 San Jose, California September 7–9, 2023 Like us @cdadentists Follow us @cdadentists Follow us @cdadentists
Learn together at CDA Presents. Keep connected to CDA for news on our next convention, including schedules, new courses, workshops, amazing speakers and special events at cda.org/cdapresents.
Build your skills online at any time. Explore a full catalog of on-demand courses and live learning events year-round, with expanded offerings and special benefits for CDA members at cda.org/learning
Journa CALIFORNIA DENTAL ASSOCIATION









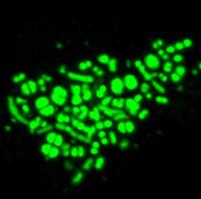







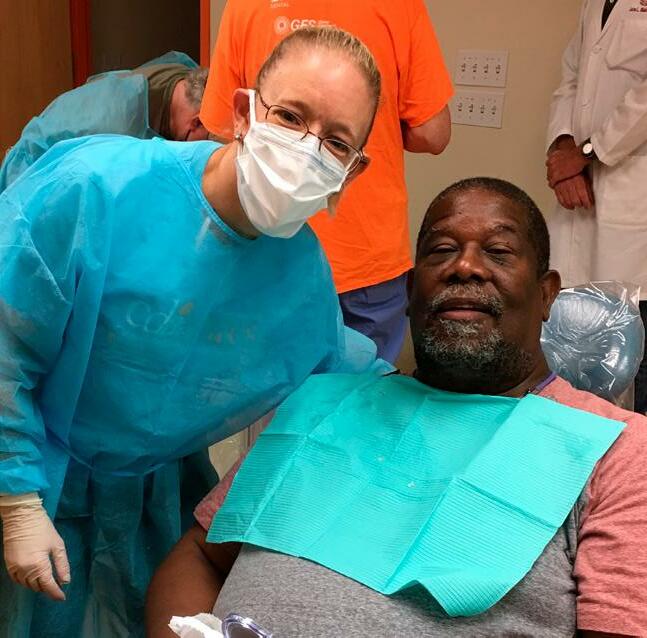



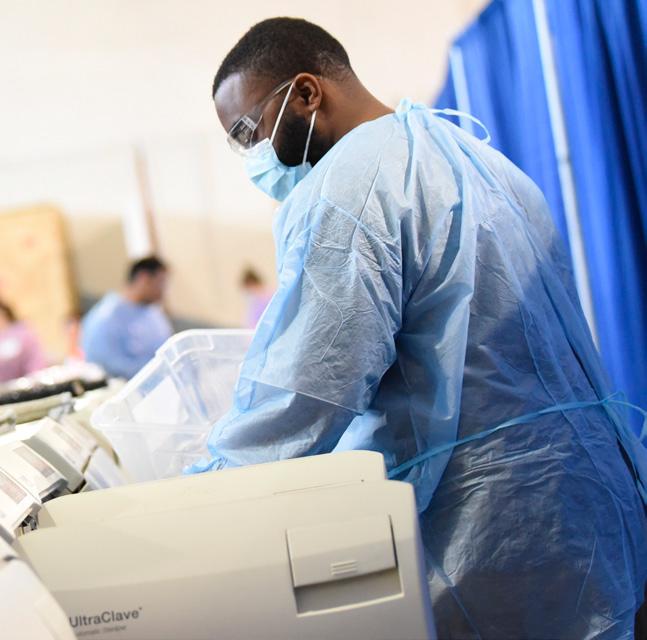












 Jared I. Fine, DDS, MPH
Jared I. Fine, DDS, MPH