
NEW TDIC SEMINAR





Through an engaging, self-guided course, learn how to sharpen your critical communication and documentation skills to lessen potential complaints, claims or lawsuits.
Take all the course modules at once or study them as time allows at your own pace from the comfort of your home or office. Upon course completion, earn 3.0 units ADA CERP C.E. and a 5% Professional Liability premium discount.*
Learn more and register online at tdicinsurance.com/seminars.
The Associate Editor/MultiGen at Work
RM Matters/Facing Reality: Communicating and Managing Achievable Aesthetic Outcomes Regulatory Compliance/How To Manage Patient Information Breach Assessment and Notification
Dental Student Research
An introduction to the issue.
Zohra Tumur, MD, PHD

Management of Hypertensive Crisis in a Dental School: 10-year Retrospective Review of Medical Emergency Incidents With Recommendations
This 10-year retrospective study analyzes the past medical emergency in-house calls at the Loma Linda University School of Dentistry.
Soh Yeun Kim, DDS; Sarah Lim, BA; Chanmee Esther Kim, BS; Lauren Barlow, BS; Adlene Chang, BA; Holli Riter, DDS; Iris Nam, DDS; Heidi Christensen, DDS; and Udochukwu Oyoyo, MPH
The objective of this study was to compare the time taken for second-year dental students to collect periodontal data and to assess their confidence level in preclinical activities.
Amelia David, BDS, MS; Soh Yeun Kim, DDS; Barnabas Kim, BS; and Hyan Il Kim, BS; and Udochukwu Oyoyo, MPH
Rollout of the Oral Health Literacy Toolkit in California: A Mixed-Methods Analysis
This study was intended to obtain user feedback and suggestions for improvement of the toolkit.
Christine Y.W. Hao, DMD, MPH; Karen Sokal-Gutierrez, MD, MPH; Susan L. Ivey, MD, MHSA; and Kristin S. Hoeft, PhD, MPH
published by the California Dental Association 1201 K St., 14th Floor Sacramento, CA 95814 800.232.7645 cda.org
CDA Officers
Ariane R. Terlet, DDS President president@cda.org
John L. Blake, DDS President-Elect presidentelect@cda.org Carliza Marcos, DDS Vice President vicepresident@cda.org
Max Martinez, DDS Secretary secretary@cda.org
Steven J. Kend, DDS Treasurer treasurer@cda.org
Debra S. Finney, MS, DDS Speaker of the House speaker@cda.org
Judee Tippett-Whyte, DDS Immediate Past President pastpresident@cda.org
CALIFORNIA DENTAL ASSOCIATION
Peter A. DuBois Executive Director
Carrie E. Gordon Chief Strategy Officer
Alicia Malaby Communications Director
Editorial
Kerry K. Carney, DDS, CDE Editor-in-Chief Kerry.Carney@cda.org
Ruchi K. Sahota, DDS, CDE Associate Editor
Marisa Kawata Watanabe, DDS, MS Associate Editor
Gayle Mathe, RDH Senior Editor
Zohra Tumur, MD, PhD Guest Editor
Andrea LaMattina, CDE Publications Manager
Kristi Parker Johnson Communications Manager
Blake Ellington Tech Trends Editor
Jack F. Conley, DDS Editor Emeritus
Robert E. Horseman, DDS Humorist Emeritus
Production
Danielle Foster Production Designer
Upcoming Topics December/General Topics January/Public Health Initiatives February/General Topics
Advertising
Sue Gardner Advertising Sales Sue.Gardner@cda.org 916.554.4952
Volume 50 Number 11 November 2022
Andrea LaMattina, CDE Publications Manager Andrea.LaMattina@cda.org 916.554.5950
www.editorialmanager. com/jcaldentassoc


Letters to the Editor www.editorialmanager. com/jcaldentassoc
Journal of the California Dental Association Editorial Board
Charles N. Bertolami, DDS, DMedSc, Herman Robert Fox dean, NYU College of Dentistry, New York
Steven W. Friedrichsen, DDS, professor and dean emeritus, Western University of Health Sciences College of Dental Medicine, Pomona, Calif.
Mina Habibian, DMD, MSc, PhD, associate professor of clinical dentistry, Herman Ostrow School of Dentistry of USC, Los Angeles
Robert Handysides, DDS, dean and associate professor, department of endodontics, Loma Linda University School of Dentistry, Loma Linda, Calif.
Bradley Henson, DDS, PhD, interim vice president research & biotechnology, associate dean for research and biomedical sciences and associate professor, Western University of Health Sciences College of Dental Medicine, Pomona, Calif.
Paul Krebsbach, DDS, PhD, dean and professor, section of periodontics, University of California, Los Angeles, School of Dentistry
Jayanth Kumar, DDS, MPH, state dental director, Sacramento, Calif.
Lucinda J. Lyon, BSDH, DDS, EdD, associate dean, oral health education, University of the Pacific, Arthur A. Dugoni School of Dentistry, San Francisco

Nader A. Nadershahi, DDS, MBA, EdD, dean, University of the Pacific, Arthur A. Dugoni School of Dentistry, San Francisco
The Journal of the California Dental Association (ISSN 1942-4396) is published monthly by the California Dental Association, 1201 K St., 14th Floor, Sacramento, CA 95814, 916.554.5950. The California Dental Association holds the copyright for all articles and artwork published herein.

The Journal of the California Dental Association is published under the supervision of CDA’s editorial staff. Neither the editorial staff, the editor, nor the association are responsible for any expression of opinion or statement of fact, all of which are published solely on the authority of the author whose name is indicated. The association reserves the right to illustrate, reduce, revise or reject any manuscript submitted. Articles are considered for publication on condition that they are contributed solely to the Journal of the California Dental Association. The association does not assume liability for the content of advertisements, nor do advertisements constitute endorsement or approval of advertised products or services.
Copyright 2022 by the California Dental Association. All rights reserved.
Visit cda.org/journal for the Journal of the California Dental Association’s policies and procedures, author instructions and aims and scope statement.
Connect to the CDA community by following and sharing on social channels
Francisco Ramos-Gomez, DDS, MS, MPH, professor, section of pediatric dentistry and director, UCLA Center for Children’s Oral Health, University of California, Los Angeles, School of Dentistry
Michael Reddy, DMD, DMSc, dean, University of California, San Francisco, School of Dentistry
Avishai Sadan, DMD, dean, Herman Ostrow School of Dentistry of USC, Los Angeles
Harold Slavkin, DDS, dean and professor emeritus, division of biomedical sciences, Center for Craniofacial Molecular Biology, Herman Ostrow School of Dentistry of USC, Los Angeles
Brian J. Swann, DDS, MPH, chief, oral health services, Cambridge Health Alliance; assistant professor, oral health policy and epidemiology, Harvard School of Dental Medicine, Boston
Richard W. Valachovic, DMD, MPH, president emeritus, American Dental Education Association, Washington, D.C.
This study investigated the microbial changes during treatment with clear aligners (CA) and fixed appliances (FA) and evaluated the utility of saliva as a diagnostic marker in orthodontic patients.
Emily Duong, BS; Elaine Pham, BS; Julia Esfandi, BS; Kim-Sa Kelly, BS; Arvin Pal, DDS; Masooma Rizvi, DDS; Nini Tran, DDS, PhD; Tingxi Wu, DDS, PhD; Bhumika Shokeen, PhD; and Renate Lux, PhD
The purpose of this study was to determine if childhood exposure to adverse experiences in a Los Angeles dental population was related to current young adult tobacco, alcohol and drug behaviors.
Kenneth J Glenn, BS; Christina Light, BS; Todd Franke, MSW, PhD; and Shane N. White, BDentSc, MS, MA, PhD
CDA Foundation volunteers and donors truly change the lives of others. Through your generosity, Californians in underserved communities gain access to dental treatment that relieves pain, restores dignity, creates smiles and opens more opportunities.








As I glanced at my bookshelf that houses some of my favorite childhood titles, it was quite nostalgic to reread “Mary Alice Operator Number 9, Miss Nelson is Missing” and the unforgettable “The Berenstain Bears Visit the Dentist.” My name is printed proudly in just-learnedto-write letters in the upper left corner, and I sat imagining when I first turned the crisp new pages to now gently turning the weathered pages — both giving me such satisfaction. Fast forward multiple decades later and with a quick search on the web, the very same book is at my fingertips as an e-book or an audio book to listen to during my drive to work. Growing up split between generations certainly created a blend of culture — playing vinyl records and LPs on my record player, using a Compaq computer to play Frogger on the green screen, listening to cassettes and CDs on a boombox, to the big introduction of AOL (“you’ve got mail!”), mini-disc and mp3 players and social media platforms no longer in existence. Technological advancements, social trends and generational gaps continue to bare their teeth and shape our present and future times.
With the Merriam-Webster Dictionary constantly adding new words I have yet to encounter, understanding the ever-changing slang has been a humorous and now annual ritual at our family gatherings. Previously proud to use slang abbreviations like YOLO (you only live once), IMHO (in my humble/honest opinion) and SMH (shaking my head), I realized each year that I have become so cheugy (out of date and no longer trendy) that I might end up tripping over these generational gaps. Instead, I rely on my next generation of cousins to “educate” me on the latest craze, social media
platforms and new ways for easy and instant gratifications. Whether or not I choose to follow the next trend, clear communication between providers and patients, among health care team members and between family members has always been, and remains, imperative in building trust, strong rapport and a successful practice.
Recently, Fortune Magazine published an article by Lambeth Hochwald regarding the growing generation gaps in the workplace and what changes are to come. According to Hochwald, 40% of Americans currently have a supervisor who is younger than they are and millennials will be the dominant demographic population by 2025.1 Companies and organizations comprised of Gen Z (1997-2012), millennials (1981-1996), Gen X (19651980), baby boomers (1946-1964) and the Silent Generation (1928-1945) working together are demonstrating the demographic shift of workforce composition.2 Noting the higher percentage of younger supervisors, the traditional hierarchical mindset of “older age equals higher position” has begun to wane.
With dental student indebtedness on the rise, a 2022 survey study regarding general perspectives of orthodontists in the United States and Canada found significant variability among different generations in practice.3 The results of the study described that more technologically advanced and
costly equipment were utilized more often by the younger generation (notably with higher student debt) of orthodontists versus the Silent Generation.3 In addition, another significant difference was noted in practice marketing, with the younger generation relying heavily on social media platforms and the older generation limiting the budget to more traditional marketing.3 In a multigenerational team, collaborating and marrying the strengths of digital media with personal word-of-mouth supports the success of the health care team and practice.
In “Promoting an Age-Inclusive Workforce; Living, Learning and Earning Longer,” the authors explored the rapid changes in population demographics, highlighting the strengths of generational diversity in the workforce. The authors noted that a “key advantage of a multigenerational workforce is that it enables effective synergies between experienced and less experienced staff to the benefit of employers and employees.”4 But to accomplish this synergistic multigenerational workforce, support is needed for the dental team to bridge communication and behavior gaps; this may start with building a practice or health care team whose goal is to eliminate stereotypical references to each generation.4 Other examples include incorporation and development of training geared toward team or practice goals rather than
Technological advancements, social trends and generational gaps continue to bare their teeth and shape our present and future times.
segregated or siloed groupings of experience as well as practicing incentivization of overall production to showcase the collective impact that involves the multigenerational workforce rather than individual incentivization.4
FWIW (for what it’s worth), maybe it’s about time we catch up with MerriamWebster — IYKYK (if you know, you know). Take courses on implicit bias, communication and ways to diversify your team. The times of using pager code such as 424 (call me back) and 43770 (hello) have passed, and sooner than we think, Gen Alpha (2013-2025) will join the workforce. Now, if someone tells you, “These dentures are snatched!” — celebrate — that means you are on fleek aka on point! n
1. Hochwald L. Generation gaps are a growing workplace headache. Brian Chesky’s mentor is on a mission to bridge them Fortune September 2022.
2. Dimock M. Defining Generations: Where Millennials End
and Generation Z Begins. Washington, D.C.: Pew Research Center; Jan. 17, 2019. Accessed Oct. 11, 2022.
3. Hussain SR, Jiang SS, Bosio JA. Generational perspectives of orthodontists in the U.S. and Canada: A survey study.
Am J Orthod Dentofacial Orthop 2022 Aug 30;S0889–5406(22)00476-0 doi: 10.1016/j.ajodo.2021.07.020 Online ahead of print.
4. Organisation for Economic Cooperation and Development (OECD) . Good for business: Age diversity in the workplace and productivity. In: Promoting an Age-Inclusive Workforce: Living, Learning and Earning Longer. Paris: OECD Publishing; 2021.
Marisa K. Watanabe, DDS, MS, is a professor and associate dean for community partnerships and access to care at the Western University of Health Sciences, College of Dental Medicine. She currently serves on the board of the Medicaid|Medicare|CHIP Services Dental Association as the academic director and is the chair of the Los Angeles County Department, Oral Health Program Community Oral Health Improvement Plan, Workforce Development and Capacity Workgroup.
We reserve the right to edit all communications. Letters should discuss an item published in the Journal within the last two months or matters of general interest to our readership. Letters must be no more than 500 words and cite no more than five references. No illustrations will be accepted. Letters should be submitted at editorialmanager.com/ jcaldentassoc. By sending the letter, the author certifies that neither the letter nor one with substantially similar content under the writer’s authorship has been published or is being considered for publication elsewhere, and the author acknowledges and agrees that the letter and all rights with regard to the letter become the property of CDA.
Editor’s note: The following tributes to Dr. Dennis Kalebjian were written by CDA past president Dr. Debra Finney, who followed him as president in 2004, and by CDA past president Dr. Steve Chan, who preceded him as president in 2002.

March 1, 1954 - July 23, 2022
Most of you reading this will relate to Dr. Dennis Kalebjian through his professional career in dentistry. However, Dennis was so much more and that is what made him a truly great man. Let me offer some insight . . .
Dennis had a highly successful dental practice for 43 years in his home town of Fresno. In addition to providing general dentistry services in his office, he also treated special needs and medically compromised patients at a local hospital. He was involved in his community, through his children’s activities in sports and music, through his church and by his charitable treatment of the underserved. He was appreciated and respected in a community that saw him as a dedicated family man and a generous provider for those in need.
Along with his dental practice and
community and family activities, Dennis had some talents not as well known by his dental colleagues. He was a musician from an early age and played the piano for many family and community events throughout his life. He was also a farmer. His parents had a raisin farm that had been started by his grandparents and later maintained by Dennis and his son.
He had quite a repertoire of skills — from dentistry to music to driving a tractor. But there’s more! Somehow, he found time to devote to leadership in his profession. First in his local Fresno-Madera Dental Society where he served as president. Continuing on with his involvement, he served in positions with the CDA and ADA. He was CDA president in 2003.
Dennis was a quiet leader, thoughtful and pensive. He studied and considered all aspects of an issue before making a decision. And yet, in that patient demeanor, there
was a mischievous side lurking behind an impish smile that would spurt out amusing comments and observations catching those around him off guard. Although he could appear serious and indifferent, he was anything but. He had a warm and kind heart and was gentle and caring. He was an educator and mentor in his community and with his family. He imparted his love of music and dentistry to his children. We lost a treasured friend and colleague, but his family lost much more. We all lost a great man.
Dennis Kalebjian’s Opus Dennis had a lifelong passion for music. We honor his life with a symphonic metaphor.
Dennis Kalebjian, son of a Fresno raisin farmer, rose to become president of the California Dental Association (2003). He could hear melodies from afar. He could hear the possible.
Hypnotic melodies drew him from the vineyards to the auditoriums of the University of Pacific to the halls of the ADA and beyond.
This is his symphony of life.
To aspire
Ever hear a melody that’s so compelling, you stop.
You turn your head. You listen.
Dennis was that rising star, the voice of clarity.
He was the youngest, at the time, to chair a CDA Council, to chair the multimillion-dollar ADA Business Enterprise Inc. to lead the search for: an ADA Executive Director a TDIC CEO a CDA Executive Director
He was listening. Those around him were listening to him.
Concert Performance
Community Medical Center (Fresno)
His audience. Postgrad residents thought they would only hear how to do hospital dentistry. He would teach a long line of neophytes the melodies he could hear.
“Be the Best.” “Practice, Practice. Practice.”
His vocal chorus tolled about character, about community and about relationships.
For over 40 years, postgrad-program alumni sought him out.
“You once told me the melodies. I hear your songs in my head.
Now I sing the melodies that Dennis shared with me.”
The Captain’s Chair Dennis was the youngest up to that time to ascend to the CDA President.
9-11 was still fresh. Changing the CDA management was fresh.
Anti-amalgamists and denturists were attacking. U.S. Supreme Court FTC vs. CDA meant we had to adjust. The CDA Foundation was realized.
It’s said that the test of leadership is when you are tested.
Raising a Family
Juggling debt from school, starting a practice with wife Paulette during a recession and raising a family with three babies. The profession’s clarion call summoned. Yet Family always came first.
His legacy is family. Daughter Bridgit is a dentist. Son Brad is a fourthgeneration farmer. Daughter Jamie is an attorney. Grandbabies’ hugs from Penelope, Presley, Piper, Glen, Eileen, Andre and Lucy are priceless.
On July 23, 2022, Dennis raised his baton one last time. Sforzando!
Pancreatic cancer silenced the music.
Members of St. Gregory Armenian Apostolic Church sang his praises.
Compadres from Chicago, North Carolina and distant California borders came.
The Processional brought residents, patients and special patients from 43 years ago.
They came to say Good Bye to the man who touched their lives
The man who taught them to hear the music that he heard.

Many studies have indicated that the health of teeth and gums can influence the body elsewhere, including the brain. But other studies have been less conclusive, and much uncertainty remains about the strength and direction of this relationship. It’s possible, for instance, that the link can be explained by people developing poor dental health as a result of their early dementia, instead of the other way around — an example of something scientists call reverse causality. However, a recent study from the University of Eastern Finland that reviewed existing evidence found that poor dental health was linked to a later higher risk of cognitive decline and dementia. This increased risk was especially apparent for those missing some or all of their teeth. The study was published in the Journal of the American Geriatrics Society.
The research team sought to conduct an updated meta-analysis of the evidence so far, one that would try to account for these gaps in knowledge. They collected and analyzed 47 longitudinal studies that tracked people’s oral and brain health over time, looking specifically at those who hadn’t been diagnosed with dementia at the start of the study. Ultimately, they found that people with poor oral health were 23% more likely to eventually develop some amount of cognitive decline and 21% more likely to develop dementia. And of the various measures of oral health studied, they also found that tooth loss in particular was independently associated with cognitive decline and dementia.
The researchers caution that the evidence they examined is still limited and has many caveats, so it’s hard to draw firm conclusions. Many of the studies reviewed looked at different groups of people (some only included people over 65) or tracked them for different time periods, while others may have had methodological problems in their design. But the authors say theirs is the largest review of its kind to date. They also tried to account for reverse causality in a separate analysis and found that it could explain some but not all of the connection seen here.
In other words, while there might be a real cause-and-effect link between poor oral health and dementia, it will take more well-done research to better understand the specifics of this relationship, including the exact mechanisms behind it. Some scientists theorize, for instance, that the bacteria found in people with gum disease can help trigger or accelerate the complex chain of events that leads to dementia. The team behind this paper also notes that losing teeth could harm the aging brain by depriving people of familiar sensations. And other factors likely can negatively affect both the mouth and brain at the same time, such as nutritional deficiencies. n
The percentage of smokers who attempted to quit cigarettes dropped for the first time in a decade, according to a study published in the JAMA Network Open. Researchers attributed the phenomenon to the COVID-19 pandemic.

The study is one of the first to offer insight into how smoking cessation changed during the pandemic. Some prior studies have suggested that the pandemic led to an increase in cigarette use among smokers as a stress-related coping mechanism. For other smokers, fears about the health risks of COVID-19 may have prompted a decision to reduce or quit tobacco products.
In the new cross-sectional study, researchers analyzed changes in smoking cessation-related behaviors throughout the COVID-19 pandemic using data from approximately 790,000 U.S. adult smokers. Researchers also gathered data from the nationally representative Behavioral Risk Factor Surveillance System survey and representative retail scanner sales data for nicotine replacement therapy universal product codes.
Researchers evaluated changes in the annual self-reported prevalence of past-year quit attempts and recent successful cessation before and during the COVID-19 pandemic. Sales volumes of nicotine gum, lozenges and patches before and during the pandemic were calculated.
The annual number of past-year
A recent study in the Pediatric Dental Journal provides evidence of strong relationships between acidic drinks and dental erosion. Researchers from Misr International University in Egypt analyzed the effects of common beverages on deciduous teeth enamel and got results that were perhaps not shocking — carbonated soft drinks and acidic juices resulted in drastic softening and a serious reduction in enamel surface hardness and loss of surface structure of deciduous teeth at two- and four-weeks erosive challenge.
For the study, the researchers subjected a total of 52 human extracted deciduous molars to erosive challenge by cyclic immersion in four liquids — artificial saliva, strawberry-flavored milk, orange juice and the carbonated soft drink Pepsi — for a 28-day pH cycling protocol. The enamel surface microhardness and surface topography using a scanning electron microscope were assessed at baseline after two- and four-weeks of the erosive challenge.
Analysis found that Pepsi and orange juice showed high erosive potentiality affecting the enamel surface of the teeth while the milk-based beverage showed no difference from the artificial saliva.

Citing a “drastic burst” of consumption of carbonated soft drinks and juice among children during the COVID-19 pandemic, the study authors noted that if dental erosion is not controlled or stabilized, affected children may suffer from severe tooth surface loss, tooth sensitivity, poor esthetics and eventually the risk of dental abscesses of the affected teeth.
cessation attempts decreased for the first time since 2011 from 65.2% to 63.2%. The largest decreases were among individuals between the ages of 45 and 64, those with two or more comorbidities and Black individuals. The rate of recent successful cessation remained unchanged. Simultaneously, sales of nicotine replacement therapy brands decreased across the U.S. Compared with expected sales, observed sales during the pandemic were lower by 13% for lozenges, 6.4% for patches and 1.2% for gum. Smoking cessation activity decreased amid the COVID-19 pandemic and remained
depressed for more than a year.
These findings suggest a decrease in smoking cessation activity during the COVID-19 pandemic and the need to reengage smokers in evidence-based quitting strategies, according to the researchers.
The Black Death was a bubonic plague in the 14th century and is known as the most fatal pandemic in history, killing millions across Europe, Africa and Asia. The cause of the bubonic plague comes from the bacterium Yersinia pestis, which is commonly spread by fleas.
Researchers for years have been
looking for where the pandemic originated and recently found DNA evidence of the bacteria inside of ancient teeth from the bodies of people buried in modern-day Kyrgyzstan. The ancient teeth DNA dates all the way back to 1338 when the plague was beginning to grow.
Johannes Krause, PhD, a professor at
the Max Planck Institute for Evolutionary Anthropology in Leipzig, Germany, and several other researchers co-authored the study that was published in the journal Nature.
A San Diego State University study found that more generous Medicaid payment policies were associated with significant but modest increases in children’s preventive dental visits and excellent oral health. The study was published in the JAMA Health Forum

In the cross-sectional study, researchers set out to evaluate the association between the ratio of Medicaid payment rates to dentist charges for an index of services (fee ratio) and children’s preventive dental visits, oral health and school absences. Relative to previous studies of children’s dental visits, the research team examined a more recent period after the major U.S. health care reform that included the Affordable Care Act’s Medicaid expansion and the inclusion of dental as an essential health benefit for children.
A difference-in-differences analysis was conducted between September 2021 and April 2022 of 15,738 Medicaid-enrolled children and a control group of 16,867 privately insured children aged 6 to 17 years who participated in the 2016-2019 National Survey of Children’s Health. Exploratory subgroup analyses by sex and race and ethnicity were also performed.
The study found that more generous Medicaid payment policies were associated with significant but modest increases in children’s preventive dental visits and excellent oral health. To the authors’ knowledge, their study is among the first to assess whether Medicaid dental payment rates are associated with improvements in children’s oral health and school absences and to document whether associations differ by sex and race and ethnicity. The authors noted that further research is needed to understand the potential association between policies that improve access to dental care and children’s academic success.
“What we found in this burial ground … was the ancestor of four of five of those lineages — so it’s really like the big bang of plague,” Dr. Krause said at a news conference. “So we have basically located this origin in time and space, which is really remarkable.”
Researchers believed for a long time that burial sites in Kyrgyzstan, which have 467 tombstones spanning nearly 900 years, could possibly have the remains of people who died from the plague. There are 118 graves dated between 1338 and 1339, and the high number in just two years caught researchers’ attention.
Researchers then examined seven teeth from seven different people buried and found evidence of the bacteria inside of dried blood vessels in the teeth. They then determined that the bacteria strain in the teeth “was an ancestor of genomes from victims of the Black Death about eight years later.”



Zohra Tumur, MD, PhD, is an assistant professor in the College of Dental Medicine at Western University of Health Sciences in Pomona, California.
Conflict of Interest Disclosure: None reported.
If at first, you don’t succeed, search, search again. That’s why they call it research. – Unknown

“How is research going?” I asked, and my friend replied, “research is research.” We both laughed. However, this conversation resonated with me for years.
The Oxford Dictionary defines research as “the systematic investigation into and study of materials and sources to establish facts and reach new conclusions.” Research takes years of hard work and dedication before it reaches its conclusion. Nevertheless, the new information and knowledge acquired contributes to the advancement of science and technology. In health care, research plays a crucial role in discovering new therapeutic approaches, making evidence-based decisions and establishing better health policies.
Albert Szent-Gyorgyi (winner of the Noble Prize in Medicine in 1937) said, “Research is to see what everybody else has seen, and to think what nobody else has thought.” Research is a process that starts with careful observation, critical analysis of the situation and developing research questions and hypotheses. Next comes the process of research design, data collection, analysis and interpretation. Finally, research ends disseminating findings to a greater audience. Actually, research does not end there; it opens doors for future research questions and opportunities, and it continues.1
Science and research played a crucial role in the development of the dental profession and dental education and have
become a core of modern dentistry. Dental research scientists and clinical scholars contributed tremendously to understanding complex human diseases and disorders beyond the diseases of the oral cavity during the last half of the 20th century.2

The January 2020 issue of the Journal highlighted the importance of research in dental education. Dr. Paul Krebsbach, dean of the University of California, Los Angeles, School of Dentistry, started his introduction by emphasizing the importance of generating new knowledge to build a vibrant dental professional future. The authors in that issue emphasized the crucial role of research in dental education by stating that research helps dental students to deeply understand the biosocial foundation of the dental profession and acquire critical thinking abilities. They also emphasized the importance of exposing students to advanced science and technology to create a competent dentistscientist workforce necessary to compete in today’s precision health care environment.3
To support student research, the Journal highlights students’ research work in special issues. Students from dental schools in California are encouraged to submit their research and share it with a greater audience.
Even with restricted access to research during the COVID-19 pandemic, dental schools adapted to the new changes and exhibited resilience and creativity to continue all parts of dental education, including research programs. In the January 2022 issue of the Journal, dental students shared their research on how
dental schools adapted to the pandemic. This Journal issue presents diverse research topics in dentistry. Students from the Loma Linda University School of Dentistry contributed “Management of Hypertensive Crisis in a Dental School: 10-year Retrospective Review of Medical Emergency Incidents With Recommendations,” which includes the opportunity to earn continuing education credit, and “Evaluating the Effectiveness of Periodontal Data Collection Practices in Second-Year Dental Students.” Students from the University of California, San
Francisco, analyzed user feedback in their article “Rollout of the Oral Health Literacy Toolkit in California: A Mixed-Method Analysis.” The articles “Salivary and Plaque Microbiomes During Treatment With Different Orthodontic Appliances” and “Childhood Adversity Correlates With Young Adult Health Dental Patient Behaviors” were submitted from the University of California, Los Angeles.
I am very pleased to work with the CDA team to support student research publications. We truly appreciate all the authors who submitted articles to CDA.
It shows their resilience, determination, commitment and dedication to scientific discovery and to creating safe and effective dental health services. We applaud all the students, mentors and CDA administration who brought this Journal issue to life. We hope readers enjoy it. n

1. Portney LG. Foundations of clinical research: Applications to evidence-based practice. 4th ed. Philadelphia: F.A. Davis; 2020.
2. Slavkin HC. The Impact of Research on the Future of Dental Education: How Research and Innovation Shape Dental Education and the Dental Profession. J Dent Educ 2017 Sep;81(9):eS108–eS127 doi: 10.21815/JDE.017.041
3. Krebsbach P. Ensuring a Vibrant Future for Dentistry Through Research and Discovery. J Calif Dent Assoc 2020 Jan;48(1)

Soh Yeun Kim, DDS; Sarah Lim, BA; Lauren Barlow, BS; Chanmee Esther Kim, BS; Adlene Chang, BA; Holli Riter, DDS; Iris Nam, DDS; Heidi Christensen, DDS; and Udochukwu Oyoyo, MPH
Background: The objective of this study was to analyze the type and frequency of medical emergency calls made at the Loma Linda University School of Dentistry (LLUSD) and to reinforce the guideline for the most frequent incident.

Methods: Emergency call data from the past 10 years at LLUSD were collected and categorized according to the type and frequency of medical emergencies. The most frequent emergency data was identified, and additional information was gathered using the patients’ electronic health records in the axiUm database.
Results: Emergency calls related to hypertension (HTN) were the most common emergency calls encountered at LLUSD and comprised 32.9% of the calls (95% confidence interval (CI): 29.1, 36.9). HTN-related calls peak at age groups 50 to 80 (P < 0.05). Seventy-seven percent of patients who had emergency calls had an existing HTN. Out of the total HTN incidences, 11% were transported to the emergency room (ER) (95% CI: 7.86, 12.2).
Conclusions: The most frequent medical emergency call at LLUSD was related to hypertension. A revised HTN guideline is recommended to guide dental providers to determine when to call emergency medical service (EMS) or when to consider a medical consultation with a patient’s physicians to minimize reports that do not require immediate management. Providers must also consider the patient’s individual health history, background and comorbidity.
Practical implications: The proposed updated HTN treatment guideline will guide dentists or staff on whether to call EMS for immediate treatment or refer to a patient’s physician for HTN care.
Keywords: Medical emergency, hypertension, hypertensive emergency, hypertensive urgency, guideline
Soh Yeun Kim, DDS, is an assistant professor and course director of patientcentered care II at the Loma Linda University School of Dentistry.
Sarah Lim, BA, is a fourthyear dental student at the Loma Linda University School of Dentistry.
Lauren Barlow, BS, is a fourth-year dental student at the Loma Linda University School of Dentistry.
Chanmee Esther Kim, BS, is a fourth-year dental student at the Loma Linda University School of Dentistry.
Adlene Chang, BA, is a fourth-year dental student at the Loma Linda University School of Dentistry.
Holli Riter, DDS, is an associate professor and a director for the special care dentistry department at the Loma Linda University School of Dentistry.
Iris Nam, DDS, is an assistant professor and clinician in the special care dentistry department at the Loma Linda University School of Dentistry.
Heidi Christensen, DDS, is a professor and patient care manager at the Loma Linda University School of Dentistry.
Udochukwu Oyoyo, MPH, is an assistant professor and statistician at the Loma Linda University School of Dentistry.
Conflict of Interest Disclosure: None reported for all authors.
Medical emergencies in a dental office setting are not unexpected. As the human lifespan increases, so does the incidence of chronic disease.1,2 This in turn means that the likelihood of having a serious medical emergency in the dental environment also increases.3 While there is limited data available as to the frequency of medical emergencies in dental settings, survey data showed that 3 in 4 dentists report having some kind of medical emergency in their office.4 Recent trends in the health care environment require that dental health professionals become more involved in the management of the general health of patients and address related emergencies when they arise.
Although the majority of the emergencies in a dental setting are not life threatening,5 the dental practitioner needs to be prepared for all types of emergencies. Proper training for medical emergencies is part of the dental school curriculum, but dentists and dental students often report that they feel underprepared to handle the emergencies in their practices.6 The Commission on Dental Accreditation (CODA) provides accreditation standards for dental education programs. CODA Standard 2-23 states that students “must be competent in providing oral health care within the scope of general dentistry, as defined by the school” including “dental emergencies,”7 which we define to include medical emergencies. Despite the preparation and education on emergencies taught in dental school, dealing with
medical emergencies often causes high anxiety among dental students and practicing dentists. In order to better educate students on ways to reduce potential risks and to improve the quality of care delivered, it is important that we identify the adverse events seen most commonly in the dental education setting. It is vital to improve the management process of medical emergencies, dental professionals’ awareness and education and reduction of the frequency of medical emergencies.8
Identifying ways to reduce dentalsetting emergencies and training dental students to look for prevention strategies is of high importance. A recent investigation found that 35% of dental patients who had an emergency in the dental office had a history of systemic disease, with about a third of those patients having a history of cardiovascular disease.9 The ability to collect and interpret a thorough health history as well as to correlate the health history with potential medical emergencies are vital to the improvement of the level of preparedness of the dental team and the reduction of anxiety related to managing emergencies during dental treatment.
This 10-year retrospective study analyzes the past medical emergency inhouse calls at the Loma Linda University School of Dentistry (LLUSD). The objective of this study was to analyze the type and frequency of emergency call reports made in LLUSD and to reinforce the guideline for the most frequent incident to aid in decision-making of the
Medical emergency is identified and x8333 is called.
Emergency response team shows up at the specified area.
Emergency response team evaluates the subject and scene.
If transportation to hospital (ER) is indicated
If transportation to hospital (ER) is NOT indicated
911 or EMS is called. Basic medical assistance or treatment will be provided in the meantime. Upon EMS arrival, subject will be transported to hospital (ER).
Emergency response team includes an RN, dental anesthesiologist, staff from clinic supply, dental maintenance and clinic manager’s office
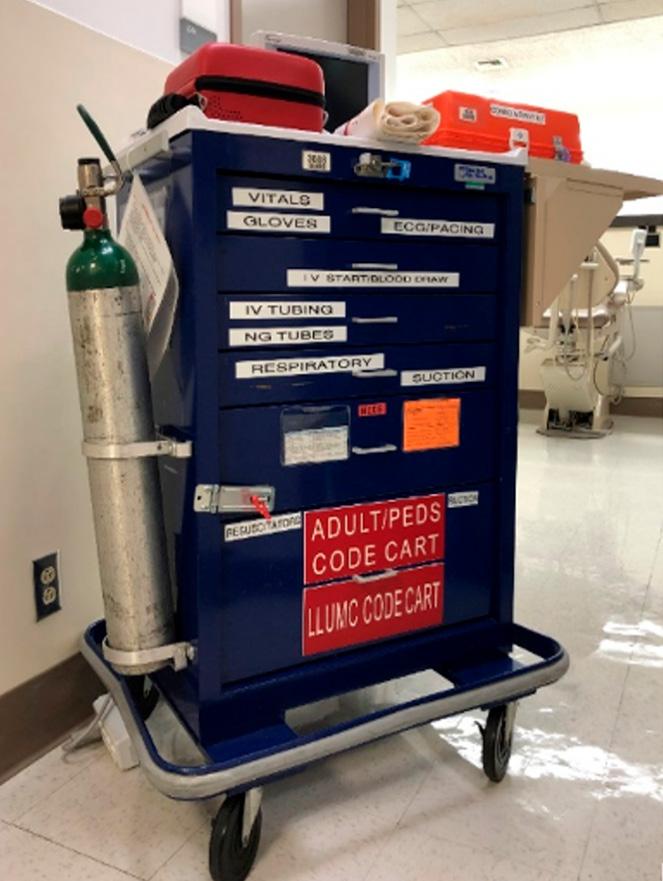
FIGURE 1. LLUSD in-house emergency call (8333) flow chart.
students, staff, faculty and other dental professionals. This study is unique in that the most common emergency call in a dental school setting is analyzed and the trend of the most common emergency is further investigated.
This retrospective study was reviewed and approved by the Loma Linda University Institutional Review Board (IRB #5210442). In order to manage medical emergencies at LLUSD, an immediate response protocol is in place for any medical emergencies that occur within the dental school building during regular business hours (f IG ure 1 ). All predoctoral and most postdoctoral dental clinics are located in this building. The emergency team responds to all emergencies called through an in-house emergency call number, 8333, whether the subject is a dental school patient, student, faculty member, staff or visitor. The response team includes a registered nurse and dentist anesthesiologist from the dental anesthesia department, a clinic
Basic medical assistance or treatment will be provided. It will be determined if the dental treatment will be continued or discontinued.
supply staff member who is responsible for the emergency code cart (f IG ure 2 ), a dental maintenance staff member for crowd control and a staff member from the dental clinic manager’s office. The latter is responsible for completion of the incident report of the emergency, using a medical emergency report and submitting an unusual occurrence report (UOR) form. These reports are compiled and stored in the dental clinic manager’s office and are reviewed at the request of the clinical quality assurance committee. Recommendations for changes, updates or other process improvements will then be given to the appropriate stakeholders.
Medical emergency incident data from January 2012 to October 2021 in which an internal or in-house medical emergency call was dialed was collected from the medical emergency reports compiled from the LLUSD clinic manager’s office. The data were analyzed after being summarized by type and frequency of medical emergency calls. The most frequent emergency data was identified, and additional information was gathered using
Incident report will be filled out in the dental manager’s office.
FIGURE 2. LLUSD emergency code cart.
the patients’ electronic health record in the axiUm database. This information included the subject’s age, gender and history of hypertension. The information regarding the necessity of transportation to an ER of the hospital was obtained from the compiled report stored in the LLUSD
Frequency 193 83 56 52 50 33 24 9 7 4 75 586
Groups 20-30 30 20 10 0 5 8 23 26 27
clinic manager’s office. Descriptive statistics including frequencies and proportions were used to characterize the cohort data; jamovi software was utilized for analysis, and 95% confidence intervals (CI) are reported where appropriate.
Overall, 586 in-house medical emergency calls were recorded during the duration of this study from January 2012 to October 2021. f IG ure 3 presents the types and frequency of emergency incidents in descending order. Emergency calls related to hypertension (HTN) were the most common emergency calls encountered at LLUSD. A total of 193 calls were made for HTN, which comprised 32.9% of the
calls (95% CI: 29.1, 36.9). The second most common type of medical emergency calls was dizziness, of which 83 incidents were recorded (95% CI: 11.4, 17.3). The frequency of falling was 56, syncope was 52 and swallowing objects such as crowns, burs or instruments was 50. Anxiety followed with a frequency of 33, allergy was 24, low blood glucose was nine, low blood pressure was seven and seizure was four. The category of “other” includes nausea, chest pain, nosebleed, throat irritation, high blood sugar, shortness of breath, stroke symptoms, presyncope (a feeling that you may faint but you do not), stomach pain, wheezing, swelling of ankles, knee pain, cold and shaking, pain, weakness, unresponsive, extensive
age
20–30 31–40 41–50 51–60 61–70 71–80 < 81 Totals (3 unknown) Female 2 1 5 23 27 26 10 94 Male 0 5 8 26 26 22 9 96 10 26 22 Female Male FIGURE 4. Frequencies of LLUSD in-house medical emergency calls (8333 calls) by age group. 2 1 5 26 9
bleeding, palpitations, headache and uncategorized. f IG ure 4 breaks down HTN incidences by age group and gender. Age was categorized into seven categories ranging from 20 to 81 and older and divided into 10-year intervals. Each age group contains a male and female bar, and female data is indicated by light blue color while male data is indicated by dark blue. There was no difference between incidences by gender, but the data indicated higher incidences with increasing age (p < 0.05). The difference of frequency between the genders varies no more than four, and the overall data creates a bell curve leaning to the right. The bell curve peaks at age groups 50-80 and the overall data
Prior diagnosis Undx+Unknown total
indicates higher incidences with age.
f IG ure 5 represents the percent of calls made for patients who lacked or had prior diagnosis of HTN. Seventyseven percent of patients who had emergency calls made reported that they have existing HTN conditions.
f IG ure 6 describes the frequency of yearly HTN calls and those that were transported to the ER upon evaluation from the in-house medical team. HTNrelated emergency calls were made the most in 2013 and 2019; 31 and 30 calls were made respectively. Out of the total HTN incidences from 2012 to 2021, 11% were transported to the ER, which shows 95% confidence intervals (95% CI: 7.86, 12.2).
In this retrospective study, we gathered data on the types and frequency of medical emergencies at LLUSD over a 10-year period. The most common type of medical emergency call at LLUSD in the past 10 years was high blood pressure-related calls comprising 32.9% of all calls. This finding was significant to focus on hypertensionrelated emergency calls. The second most common calls were dizziness, having been observed in 14.2% of emergency calls. HTN-related calls were observed more than twice as frequently as dizziness.
In May 2020, according to the American Heart Association (AHA), nearly half of U.S. adults — an estimated 116 million — have high blood pressure.10 High blood pressure is defined as a systolic reading of 130 or higher or diastolic of 80 or higher. AHA news also stated that the percentage of people who have hypertension in the U.S. increases as they age,10 and this trend was also found in HTN-related calls at LLUSD (P < 0.05). More calls were made for the 50-80 age groups.
The HTN treatment guidelines
23% 77%
Hypertension total 10 years Prior diagnosis Undx+Unknown total % diagnosed
FIGURE 5. HTN-related calls and existing HTN history.
developed at LLUSD in 2009 (TABLE 1 ) assert that any blood pressure (BP) over 180/110 mmHg is a contraindication for any dental treatment. According to the American College of Cardiology and AHA, the 2017 guidelines for hypertensive crisis is 180/120 mmHg or greater.11 HTN crisis can be defined as a hypertensive emergency or urgency depending on the involvement of organ damage. Hypertensive emergency is a rapid increase in blood pressure that can result in end-organ damage.12 Hypertensive urgency is characterized by an increase in blood pressure without showing signs or symptoms of acute organ damage and does not involve immediate risk; therefore, the treatment for hypertensive urgency can be done after the patient is dismissed within 24 to 48 hours, and oral antihypertensive therapy or medication is usually sufficient.13–16 Whelton et al. stated that these hypertensive urgency patients are not having a hypertensive emergency and therefore do not require immediate BP reduction in the emergency department.11 However, recognizing or identifying
193 149 46 77.20207254
hypertensive emergencies is very critical because end-organ damage can cause fatal medical situations12 that need hospital assistance.13 When organs are affected, immediate intervention in a hospital or intensive care setting is required to lower the blood pressure.12,14,17 Associated symptoms can include chest pain, headache, vision changes, shortness of breath, nausea, vomiting, confusion, etc. With these symptoms present, a patient should be referred to EMS to be transported to a high level of care in order to prevent further organ damage or other adverse sequelae.12 Associated examples of organ damage include acute ischemic stroke, acute myocardial infarction, unstable angina pectoris, acute renal failure and dissecting aortic aneurysm.11
A systematic review done by Astarita et al. regarding hypertensive emergencies and urgencies in the emergency department showed that both hypertensive emergencies and urgencies are frequent reasons of emergency room visits, and hypertensive urgencies were significantly more common than hypertensive emergencies.18 Hypertensive
Current LLUSD Hypertension Treatment Guideline
Systolic BP Diastolic BP
Medical risk factors present Recommendations 120–139 80–89 Yes or no (see examples in the caption below)
Routine dental care OK; discuss BP guidelines with patient 140–160 90–99 Yes/no
Routine dental care OK; consider stress reduction protocol; recommend medical consult 161–179 100–109 No
Routine dental care OK; consider stress reduction protocol; recommend medical consult 161–179 100–109 Yes
Urgent dental care only; consider stress reduction protocol; medical consult required before further treatment 180–209 110–119 No
No dental treatment without a medical consult; refer for prompt medical consult 180–209 110–119 Yes No dental treatment; refer for emergency medical treatment > 209 > 109 Yes/no No dental treatment; refer for emergency medical treatment
Examples of medical risk factors: medical history of myocardial infarction, angina pectoris, high coronary artery disease risk, recurrent stroke history, diabetes, chronic renal disease, pregnancy, patient age factor, etc.
120-129/ and /<80
130-160/ or /80-99
Yes/No
Yes/No
161-180/ or /100-120 No
161-180/ or /100-120 Yes
>180/ and/or />120 Yes/No
>209/ and/or />120
No contraindications to routine dental care. Discuss BP guidelines with patient.
Minimal risk to routine dental care. Stress reduction protocol; recommend medical consult.
Routine dental care with precautions. Stress reduction protocol, refer for medical consult.
Urgent dental care only. Stress reduction protocol; medical consult required for further treatment.
No dental treatment without a medical consult. Refer for medical consult. No dental treatment.
Refer immediately to patient’s primary care provider or urgent care.
If any symptoms of hypertensive crisis are present, call in-house medical emergency number (or call EMS if it is private practice setting).
HTN crisis signs or symptoms: Headache, altered mental status, blurred vision, numbness or weakness, pressure or tightness in the chest, chest discomfort or pain, difficulty breathing, diaphoresis, dizziness, nausea and vomiting, etc.
Risk factors or comorbidities: Medical history of myocardial infarction, angina pectoris, high coronary artery disease, recurrent stroke history, diabetes, chronic renal disease, patient age factor, seizure, anxiety, etc.
Pregnant patients: Any pregnant patient with a systolic blood pressure >160 or diastolic >110 should not receive routine care and should be referred to the patient’s prenatal care provider immediately.25
urgency was also the more common trend found in LLUSD. After analyzing the emergency call data at LLUSD, it was determined that the asymptomatic or nonemergent HTN calls were more prevalent than symptomatic calls. Among the HTN-related calls, 11% were transported to the emergency department, and these can be considered hypertensive emergencies (f IG ure 6 ). Many BP reading levels that prompted in-house medical emergency calls did not have to be considered a true emergency, as the patients could have been referred to a physician or urgent care facility with a medical consultation. In practice, this lack of distinction could result in an unnecessary call to EMS. Based on this study, additional education or proposed updated institutional guidelines (TABLE 2 ) regarding management of HTN patients would be beneficial to
students, faculty and staff to help make better decisions regarding emergency calls and disposition of patients with high blood pressure in a dental setting.
Hypertension is commonly seen in dental settings. One study done by Kellog and Gabetti showed that nearly one-third of the sample patients in their dental school clinic had high blood pressure and emphasized the importance of monitoring hypertensive patients and providing appropriate dental care.19 Seventy-seven percent of patients who had HTN-related emergency calls at LLUSD had a history of existing hypertension (f IG ure 5 ), and their HTN measurement at the time of their LLUSD dental appointment was high enough to make the calls. The prevalence study of hypertension at a dental school shows that HTN is often undiagnosed or uncontrolled;20 therefore, the role of
dental professionals is vital in that dental clinicians can help patients receive more managed treatment for their hypertension by sending a medical consultation or referring patients to physicians. Twentythree percent of patients who had HTNrelated emergency calls at LLUSD did not report a history of diagnosed hypertension (f IG ure 5 ), and they may have benefited from referral to a medical provider to evaluate their high blood pressure and possibly diagnose hypertension.
When hypertension is noted, several factors must be considered. Several measurements of blood pressure need to be done to confirm the finding, and potential high blood pressure triggers should be looked into.13 Errors in measurement of blood pressure are common; therefore, appropriate patient preparation and use of accurate measurement technique are vital parts of proper blood pressure evaluation.11
Clinicians must consider if a patient has dental anxiety as a trigger because anxiety is associated with blood pressure elevation.21 The possibility of white coat hypertension also needs to be screened at dental offices. The prevalence is higher with older patients, and 1% to 5% of white coat hypertension may convert to sustained hypertension, which shows elevated blood pressure both in-office and out-of-office settings.11 Clinicians must check if the patient took their scheduled blood pressure medications as well.
Comorbidity is also significantly important. Certain risk factors or comorbidities may limit the treatment guidelines and affect the decisionmaking process.11 When a patient has other medical risk factors, a patient’s cardiovascular disease can result in a very serious emergency situation. One case report done by Thoms et al. showed the case of a patient with a history of hypertension, angina, end-stage renal disease and other conditions who had a cardiovascular collapse during a routine dental procedure.22 This life-threatening situation can happen in any dental clinic. This case study also suggested that the emergency response plan needs to be developed to minimize serious events during the dental procedure. According to the study by Southerland et al., risk factors for hypertension include age, obesity, family history, race, diabetes, dyslipidemia, tobacco use, stress, high-sodium diet and depression.23
Providing dental students with appropriate education regarding how to manage hypertension patients in a dental setting is crucial. First-year dental students at LLUSD are introduced to the HTN treatment guideline with a lecture. Second-year dental students learn HTN in depth in the pathology class and are further trained with casebased scenarios regarding HTN patients.
They are also tested on how to measure blood pressure accurately and on the management of HTN patients with different scenarios during objective structured clinical examination (OSCE). Third- and fourth-year students apply the knowledge to their actual patient care setting. The students may need additional calibrations or training updates to make sure they are up to date with the guideline, as repeating simulation or scenario-based training has been shown to be beneficial. A study by Manton et al. showed the resident groups who received
utilized in any dental school settings to educate students, faculty and staff and aid the decision of providing patients with dental treatment or disposition of patients with HTN when the patients do not present emergent symptoms. It will also be useful in private-practice settings as it will guide dentists or staff on whether to call EMS or refer to a patient’s physician for HTN treatment. Patients with nonemergent hypertension can be seen safely in the clinic12 when clinicians follow the HTN management guidelines.
The possibility of white coat hypertension also needs to be screened at dental offices.
The limitation of this study is that only HTN-related calls and trends were the focus of this project. Because nearly one-third of the total emergency calls were HTN related, this was considered significant enough to investigate and make the project’s sole focus. However, addressing other common emergency calls (dizziness, falling, swallowing objects, etc.) in more detail could be future research projects.
simulation-based medical emergency curriculum performed significantly better than the residents in a control group.24
The significance of this study is that it identified the most common emergency calls in a dental school setting in the last 10 years with 95% confidence interval, and the trend emphasized the importance of following HTN guidelines to make decisions on HTN patient management. Members of LLUSD and readers in other dental-profession settings will gain knowledge from this project for the trend of hypertensive crisis and when it is appropriate to call EMS during hypertensive crisis. The proposed updated LLUSD HTN treatment guideline, which includes HTN emergency symptoms and updated HTN measurement readings (TABLE 2 ), can be
The most frequent medical emergency call at LLUSD was hypertension (HTN). A revised HTN treatment guideline is recommended to guide dental providers to determine when to call EMS or when to consider medical consultation of HTN patients. Providers must also consider the patient’s individual health history, background and comorbidity. n
1. Anders P, Comeau R, Hatton M, Neiders M. The nature and frequency of medical emergencies among patients in a dental school setting. J Dent Educ 2010;74(4):392–6
2. Niessen LC, Fedele DJ. Aging successfully: Oral health for the prime of life. Compend Contin Educ Dent 2002 Oct;23 Suppl 10:4–11
3. Dym H. Preparing the dental office for medical emergencies. Dent Clin North Am 2008 Jul;52(3):605–8, x doi: 10.1016/j.cden.2008.02.010
4. Collange O, Bildstein A, Samin J, et al. Letter to editor: Prevalence of medical emergencies in dental practice. Resuscitation 2010 Jul;81(7):915–6 doi: 10.1016/j. resuscitation.2010.03.039
5. Haas D. Management of medical emergencies in the dental
office: Conditions in each country, the extent of treatment by the dentist. Anesth Prog 2006 Spring;53(1):20–4 doi: 10.2344/0003-3006(2006)53[20:MOMEIT]2.0.CO;2 PMCID: PMC1586863
6. Clark M, Wall B, Tholström TC, et al. A 20-year follow-up survey of medical emergency education in U.S. dental schools. J Dent Educ 2006 Dec;70(12):1316–9
7. Commission on Dental Accreditation. Accreditation standards for dental education programs. Chicago: American Dental Association; 2017.
8. Sorenson AD, Marusko RM, Kennedy KS. Medical emergencies in the dental school setting. J Dent Educ 2021 Jul;85(7):1223–1227 doi: 10.1002/jdd.12590. Epub 2021 Mar 22. PMID: 33754336.
9. Alhamad M, Alnahwi T, Alshayeb H, et al. Medical emergencies encountered in dental clinics: A study from the Eastern Province of Saudi Arabia. J Fam Community Med 2015 Sep–Dec;22(3):175–9 doi: 10.4103/22308229.163038
10. American Heart Association. Is high blood pressure inevitable? Here’s how to keep it in check. 2020, May 18.
11. Whelton PK, Carey RM, Aronow WS, Casey DE Jr., Collins KJ, Dennison Himmelfarb C, DePalma SM, Gidding S, Jamerson KA, Jones DW, MacLaughlin EJ, Muntner P, Ovbiagele B, Smith SC Jr, Spencer CC, Stafford RS, Taler SJ, Thomas RJ, Williams KA Sr, Williamson JD, Wright JT Jr. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ ASPC/NMA/PCNA. Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/ American Heart Association Task Force on Clinical Practice Guidelines. Hypertension 2018 Jun;71(6):e13–e115. doi: 10.1161/HYP.0000000000000065. Epub 2017 Nov 13. Erratum in: Hypertension 2018 Jun;71(6):e140–e144. PMID: 29133356.
12. Suneja M, Sanders ML. Hypertensive emergency. Med Clin North Am 2017 May;101(3):465–478 doi: 10.1016/j. mcna.2016.12.007. Epub 2017 Mar 2. PMID: 28372707.
13. Sobrino Martínez J, Doménech Feria-Carot M, Morales Salinas A, Coca Payeras A. Crisis hipertensivas: Urgencia y emergencia hipertensiva [Hypertensive crisis: Urgency and hypertensive emergency]. Medwave 2016 Nov 18;16(Suppl4):e6612. Spanish. doi: 10.5867/ medwave.2016.6612. PMID: 28055998.
14. Henny-Fullin K, Buess D, Handschin A, Leuppi J, Dieterle T. Hypertensive Krise [Hypertensive urgency and emergency]. Ther Umsch 2015 Jun;72(6):405–11. German. doi: 10.1024/0040-5930/a000693. PMID: 26098191.
15. Maloberti A, Cassano G, Capsoni N, Gheda S, Magni G, Azin GM, Zacchino M, Rossi A, Campanella C, Beretta ALR, Bellone A, Giannattasio C. Therapeutic approach to hypertension urgencies and emergencies in the emergency room. High Blood Press Cardiovasc Prev 2018 Jun;25(2):177–189 doi: 10.1007/s40292-018-0261-4 Epub 2018 May 18. PMID: 29777395.
16. Bales A. Hypertensive crisis. How to tell if it’s an emergency or an urgency. Postgrad Med 1999 May 1;105(5):119–26, 130 doi: 10.3810/pgm.1999.05.1.735 PMID: 10335324.
17. Adebayo O, Rogers RL. Hypertensive emergencies in the emergency department. Emerg Med Clin North Am 2015 Aug;33(3):539–51 doi: 10.1016/j.emc.2015.04.005. Epub 2015 May 30. PMID: 26226865.
18. Astarita A, Covella M, Vallelonga F, Cesareo M, Totaro S, Ventre L, Aprà F, Veglio F, Milan A. Hypertensive emergencies and urgencies in emergency departments: A systematic review and meta-analysis. J Hypertens 2020 Jul;38(7):1203–1210 doi: 10.1097/HJH.0000000000002372. PMID: 32510905.
19. Kellogg SD, Gobetti JP. Hypertension in a dental school patient population. J Dent Educ 2004 Sep;68(9):956–64 PMID: 15342656.
20. Gordy FM, Le Jeune RC, Copeland LB. The prevalence of hypertension in a dental school patient population. Quintessence Int 2001 Oct;32(9):691–5. PMID: 11695137.
21. Ifeagwazi CM, Egberi HE, Chukwuorji JC. Emotional reactivity and blood pressure elevations: Anxiety as a mediator. Psychol Health Med 2018 Jun;23(5):585–592 doi: 10.1080/13548506.2017.1400670. Epub 2017 Nov 6. PMID: 29105504.
22. Thoms S, Cooke M, Crawford J. Cardiovascular collapse associated with irreversible cardiomyopathy, chronic renal failure and hypertension during routine dental care. Anesth Prog 2016 Spring;63(1):34–41. doi: 10.2344/0003-300663.1.34. PMID: 26866410; PMCID: PMC4751519.
23. Southerland JH, Gill DG, Gangula PR, et al. Dental management in patients with hypertension: Challenges and solutions. Clin Cosmet Investig Dent 2016 Oct 17;8:111–120 doi: 10.2147/CCIDE.S99446. eCollection 2016. PMCID: PMC5074706
24. Manton JW, Kennedy KS, Lipps JA, Pfeil SA, Cornelius BW. Medical emergency management in the dental office (MEMDO): A pilot study assessing a simulation-based training curriculum for dentists. Anesth Prog 2021 Jun 1;68(2):76–84 doi: 10.2344/anpr-67-04-04 PMID: 34185862; PMCID: PMC8258755
25. Brown MA, Magee LA, Kenny LC, Karumanchi SA, McCarthy FP, Saito S, Hall DR, Warren CE, Adoyi G, Ishaku S. International Society for the Study of Hypertension in Pregnancy (ISSHP). The hypertensive disorders of pregnancy: ISSHP classification, diagnosis and management recommendations for international practice. Hypertension 2018 Jul;13:291–310 doi: 10.1016/j.preghy.2018.05.004 Epub 2018 May 24. PMID: 29803330.
THE CORRESPONDING AUTHOR, Soh Yeun Kim, DDS, can be reached at sokim@llu.edu.
This worksheet provides readers an opportunity to review C.E. questions for the article “Management of Hypertensive Crisis in a Dental School: 10-year Retrospective Review of Medical Emergency Incidents With Recommendations” before taking the C.E. test online. You must first be registered at cdapresents360.com. To take the test online, click here. This activity counts as 0.5 of Core C.E..
1. Which of the following statements apply to this study? (mark all that apply)
a. It analyzed medical emergency calls made at Loma Linda University School of Dentistry over a 10-year period.
b. It identified hypertension (HTN) as the most common reason for an emergency call.
c. It proposed updated patient management guidelines for HTN.
d. It recommended that the revised HTN treatment guideline could assist dental providers to determine when to call EMS or when to consider medical consultation of HTN patients.
2. The authors used which of the following methods for their study? (mark all that apply)
a. Medical emergency incident data from January 2012 to October 2021 in which an internal or in-house medical emergency call was made.
b. Data was summarized by type and frequency of medical emergency calls and then analyzed.
c. Additional information was collected from patients’ electronic health records and analyzed, including age, gender, history of hypertension and whether they were transported to the ER.
d. All of the above.
3. True or False: Hypertension (HTN) was identified as the most common medical emergency at a rate of more than twice the next most common emergency complaint.
4. Which of the following emergencies was the second most frequent reason for an emergency call from the LLUSD clinic?
a. Anxiety.
b. Fainting.
c. Low blood sugar.
d. Dizziness.
e. Swallowing a foreign object.
5. What was the percentage of people who had an HTN-related emergency call at LLUSD but had not reported a history of HTN?
a. 12%
b. 17%
c. 23% d. 27%
e. 30%
6. The authors state that errors in measurement of blood pressure (BP) are common and note that which of the following should be evaluated for possible influence on BP readings (mark all that apply):
a. Poor measurement technique. b. Dental anxiety. c. White coat hypertension. d. Failure to take prescribed medication. e. All of the above.
7. True or False: Analysis of emergency call data determined that asymptomatic or nonemergent HTN calls were more prevalent than symptomatic calls.
8. Which of the following are risk factors for HTN? (mark all that apply):
a. Age. b. Gender. c. Obesity. d. Race. e. Diabetes. f. Tobacco use. g. Dyslipidemia.
9. True or False: A 2021 study evaluating the effectiveness of emergency training showed that there was no difference between the resident group who received simulation-based medical emergency curriculum and the resident group in a control.
10. True or False: The condition under which the authors’ proposed guidelines recommend that only emergency dental care be provided and a medical consult be obtained before proceeding with dental treatment is when a patient’s systolic BP is 161-180 or their diastolic BP is 100-120 and medical risk factors are present.
Amelia David, BDS, MS; Soh Yeun Kim, DDS; Barnabas Kim, BS; and Hyan Il Kim, BS; and Udochukwu Oyoyo, MPH

abstract
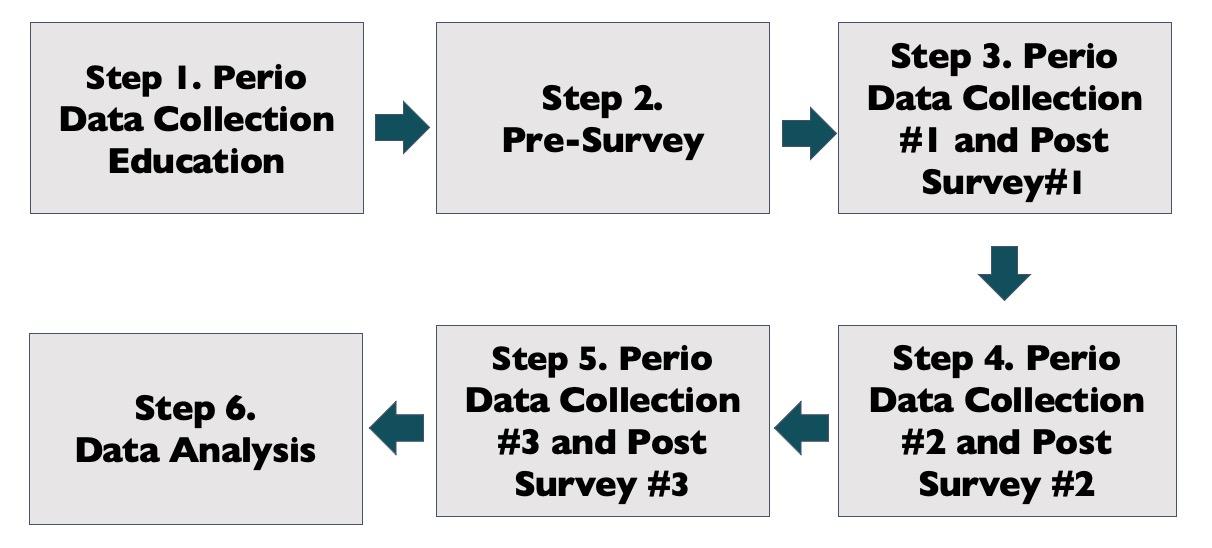
Background: The objective of this study was to compare the time taken for second-year dental students to collect periodontal data and to assess their confidence level in preclinical activities.

Methods: Second-year dental students at the Loma Linda University School of Dentistry (LLUSD) paired up as clinician and patient and participated in three periodontal data collection preclinical activities. A total of 91 sample data were included. The time that students spent on periodontal data collection was recorded. A presurvey and three postsurveys were conducted to evaluate students’ confidence. One sample t-test, the Freidman test, Pairwise comparisons and Kruskal-Wallis tests were used for statistical analysis.
Results: One sample t-test result showed that there was statistically significant time improvement between first and second data collection and between second and third data collection (p-values < 0.001). Results for postsurvey 2 with the Kruskal-Wallis test showed collection times were significantly lower among students who reported confidence in collecting data [H(1) = 5.60, p = .018)].
Conclusions: Statistically significant time improvement through periodontal data collection activities were seen. Students’ confidence level and improved data collection time were especially related during the second data collection.
Practical implications: This study signifies that multiple practice sessions in training can be a valuable learning tool to reduce the amount of time that students need to complete the task and increase students’ confidence level.
Keywords: Periodontal data collection, preclinical activity, time improvement, students’ confidence
Amelia David, BDS, MS, is an assistant professor and clinical instructor in the department of periodontics at the Loma Linda University School of Dentistry.
Conflict of Interest Disclosure: None reported.
Soh Yeun Kim, DDS, is an assistant professor and course director of PatientCentered Care II in the division of general dentistry at the Loma Linda University School of Dentistry.
Conflict of Interest Disclosure: None reported.
Barnabas Kim, BS, is a fourth-year dental student at the Loma Linda University School of Dentistry.
Conflict of Interest Disclosure: None reported.
Hyun Il Kim, BS, is a fourth-year dental student at the Loma Linda University School of Dentistry.
Conflict of Interest Disclosure: None reported.
Udochukwu Oyoyo, MPH, is an assistant professor and statistician at the Loma Linda University School of Dentistry.
Conflict of Interest Disclosure: None reported.
The goal of the preclinical dental curriculum at the Loma Linda University School of Dentistry (LLUSD) is to ensure students are well-prepared with dental knowledge and skills that will enable them to be competent to practice dentistry effectively and independently in providing patient care. Second-year dental students are trained in preclinical activities that guide their transition from didactic and preclinical settings into direct patient care. Dental students at LLUSD are introduced to periodontics in their first year in a classroom setting and didactic teaching continues in their second year. Preclinical periodontal hands-on practices are emphasized during their second year of dental school along with other preclinical hands-on activities such as patient examination and local anesthesia practice.
Students are paired up and take turns as providers and patients under faculty supervision. Students start actual patient care in the spring quarter of their second year. They perform comprehensive oral evaluations (COEs) and periodic oral evaluations (POEs) under faculty supervision.
In addition to evaluating and assessing their patients for caries and restorative needs, students must be able to evaluate periodontal health by collecting periodontal data during COEs and POEs. Periodontal health is the foundation of overall dental health and also has an impact on patients’ general health.1 Periodontal disease is associated with several medical conditions such as Type 2 diabetes, cardiovascular disease, pregnancy, chronic renal disease, etc.1 A study showed that treating periodontal disease can increase oral health-related quality of life (OHRQoL).1 Therefore, it is imperative to understand a patient’s periodontal condition, determine accurate periodontal diagnoses and provide appropriate
periodontal treatment for patients. It is important to collect accurate periodontal data to make a correct diagnosis. Dental students must master measuring periodontal pocket depths (PD), bleeding on probing (BOP), clinical attachment level (CAL), gingival recession (GR), mobility and furcation involvement.
There is a need for confirmation on whether repetition of preclinical practice can improve students’ confidence and performance in providing patient care. When predoctoral students are introduced to skills they have never encountered before, they are expected to underperform in terms of time management compared to experts. However, the speed and accuracy of data collection is expected to increase after repetition. Wang et al.2 conducted research on the surgical skill and confidence level of medical residents by providing repetitive practice during boot camp.2 At least five hours of skills training was assigned to the residents, and they were required to train at least 30 hours per month.2 They found that repetitive practice is imperative to learning new skills and behavior, and they concluded that repetition improved their confidence levels.2
An integrated review done by Gharibi and Arulappan showed that repeated simulation enhanced self-confidence, critical thinking, knowledge, competence and satisfaction of nursing students.3 Recipients of repetitive simulation reported that their ability to execute certain clinical skills was improved. In addition, they became more active in learning, which was directly linked to increased self-confidence, clinical competence and problem-solving.3 A study from Haleem et al. also showed the importance of repetition in education. Their study recruited a total of 935 adolescents and provided oral health education led by dentists, teachers and peer-leaders.
Regardless of the position of educators, they were able to conclude that repetition and reinforcement can play a vital role in school-based oral health education.4
Patients’ comfort during a dental procedure is also an important part of patient-centered care.5 Research shows that the “level of comfort” a patient perceives during dental care has an impact on the judgment of a dentist’s skill and quality of care.6 A patient’s comfort reflects their trust in the knowledge and experience of the provider. The study also showed that more experienced dentists have higher patient satisfaction levels compared to recent dental graduates, which is associated with their greater skill and speed.6 Another study showed that patients appreciate speed, experience and a feeling of ease and comfort when procedures are performed in a timely manner.7 Therefore, through repetitive practices, perceived patient comfort is expected to improve as the provider’s confidence level and speed in performing periodontal data collection increases.
There were few studies in the literature regarding students’ performance and measuring time on periodontal data collection. One study in Japan assessed the time needed to measure periodontal probing on a typodont among dental professionals and dental students.8 The study showed that probing time was much longer in the students’ group when it was compared to the dental professional group,
but the probing time decreased as they repeated the practice on the model.8
The objective of this study was to compare the time taken for novice second-year dental students to collect periodontal data and to assess their self-confidence levels through repeated practice of periodontal data collection during preclinical hands-on sessions. In a survey, student clinicians were also asked which component of the periodontal data collection was the most difficult or challenging to measure.
We hypothesized that repetitive practice of preclinical data collection will lead to second-year dental students being more efficient with periodontal examinations, thus leading to decreased time and increased confidence.
The study protocol was reviewed by the Loma Linda University Institutional Review Board (IRB), and the study is exempt from IRB (IRB# 5210456).
A total of 91 dental students from the DDS class of 2024 participated in three periodontal data collection activities (eight dental hygiene graduate dental students were excluded). These 91 students did not have prior periodontal data collection experience.
All students received didactic training on periodontal data collection that included lectures and instructional videos on measuring or determining
probing depth (PD), bleeding on probing (BOP), clinical attachment loss (CAL), gingival recession (GR), mobility and furcation. Techniques on how to accurately measure and collect the data were continuously emphasized.
A total of three periodontal data collection opportunities were given to each student. The first periodontal data collection was in August 2021, the second data collection was completed in October 2021 and the third was in January 2022 during their preclinical sessions in the dental clinic. Each student participated in periodontal data collection both as a clinician and as a patient. For each periodontal data collection activity, student clinicians were randomly assigned to different student patients. Students were instructed to record their data collection start and end times.
The Marquis periodontal probe was used to collect periodontal data. Students measured PD from the gingival margin to the base of the pocket on each of the tooth’s six surfaces: distofacial, facial, mesiofacial, distolingual, lingual and mesiolingual.9 Bleeding from the pocket was documented as BOP. GR was recorded as the measurement from the cementoenamel junction (CEJ) to the gingival margin.9 CAL was measured from the CEJ to the bottom of the pocket. Tooth mobility was checked by using the blunt end of two instruments. Mobility was then recorded according to the extent of the tooth movement.9 Furcation involvement was explored in multirooted teeth using the Nabers probe and then graded according to the extent of the furcation.9
Student clinicians recorded the amount of time spent to complete each periodontal data collection activity, and the recorded time for each activity was compared and analyzed.
In addition to recording the elapsed time during the periodontal
FIGURE 2. Mean time (minutes) spent on first and second perio data collection.
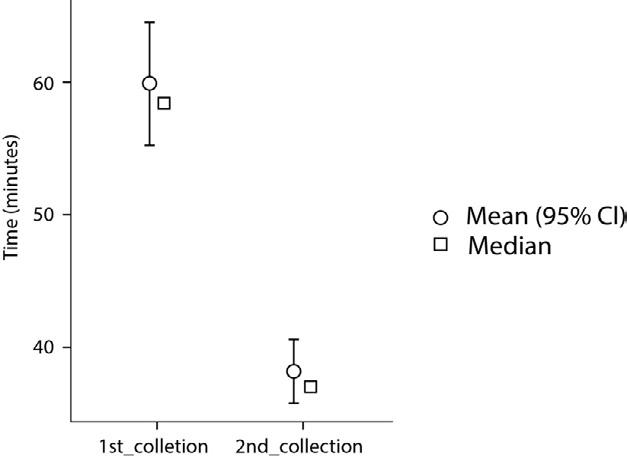

FIGURE 3. Mean time (minutes) spent on second and third perio data collection.
any significant difference in time lapse between first and second data collection and between second and third data collection. To evaluate if there was any correlation between time improvement and student clinicians’ confidence level, the Kruskal-Wallis test was utilized.
The mean completion time for the first periodontal data collection was found to be 60.5 minutes (min) and 38.2 min for second periodontal data collection (fIGure 2). The time difference or time improvement between first and second periodontal data collection was calculated to be 22.3 min. Between the second and third periodontal data collection activities, the mean time was reduced from 38.2 min to 33.3 min, which showed 4.9 min time improvement (fIGure 3). A paired sample t-test was used to analyze the statistical significance of the time difference or time improvement between each periodontal data collection. The P value for the 22.3 min time improvement between first and second periodontal data collection was found to be less than 0.001 (P < 0.001). Similarly, the P value for the time difference between the second and third periodontal data collection resulted in less than 0.001 (P < 0.001).
data collection, a total of four surveys were conducted. A presurvey before the first periodontal data collection and three postsurveys after each of the data collection activities were distributed to students using the Qualtrics system (fIGure 1).
In the presurvey and three postsurveys, a question about their confidence level as clinicians was asked using a 5-point
Likert scale ranging from “strongly agree” to “strongly disagree.” The surveys also asked about the most challenging components or concepts of periodontal data collection among PD, CAL, GR, mobility and furcation involvement.
In order to evaluate the hypothesis, one sample t-test, the Friedman test and Pairwise comparisons were used to statistically analyze whether there was

Students who spent longer time on their first periodontal data collection showed greater time improvement on their second periodontal data collection (fIGure 4). Similarly, student clinicians who spent more time during their second periodontal data collection showed greater time improvement on their third data collection (fIGure 5).
A Friedman test and Pairwise comparison were also conducted to determine whether collection times differ among the first, second and
third collections. The results showed statistically significant differences, X2(2) = 99.0, p < 0.001. We reject the null hypothesis and conclude that statistically significant differences exist among the three periodontal data collection periods (fIGure 6).
Kruskal-Wallis tests indicated that no statistically significant difference was present in periodontal data collection time between confidence groups at postsurvey 1 [H(1) = 2.09, p = .098)] and postsurvey 3 [H(1)= 1.65, p = .200)] (fIGure 7). However, in postsurvey 2, collection times were significantly lower among students who reported confidence in collecting data [H(1) = 5.60, p = .018)]. Thus, we fail to reject the null hypothesis for periodontal collection times 1 and 3 (fIGure 8).
Repeated clinical practice has been shown to reduce the time taken to complete a periodontal data collection as well as increase the clinicians’ confidence.2 As seen here with novice dental students given three periodontal data collection practice sessions, the time taken to gather periodontal data decreased significantly (p < 0.001).
After the first and third periodontal data collection, the student group who agreed or strongly agreed to confidence in postsurvey did not have a statistically significant difference in time they spent on periodontal data collection when compared to the student group who reported disagree or neutral response (mixed group). However, there was a statistically significant difference in the second postsurvey after second periodontal data collection, which showed that students who reported confidence spent
significantly less time on periodontal data collection. This data indicates that the second data collection time would be a meaningful time to intervene and provide additional educational support or resources to students to improve confidence.
Many students indicated that CAL was the most difficult periodontal data concept throughout the practice (fIGure 9). In the presurvey, about 60% of students responded that CAL was the most difficult periodontal data component, and about 78% responded the same way after they performed periodontal data collection. An increased number of students felt that CAL was a difficult concept to apply clinically. Periodontal disease is characterized by attachment loss, which is measured from the CEJ to the base of the probeable pocket. CAL can be misinterpreted and often hard to measure because the CEJ can be challenging to visualize and oftentimes may not be well defined.10 Identifying and measuring attachment loss on the interproximal surfaces can be a greater challenge as compared to direct buccal or lingual surfaces;10 therefore, more practice sessions with a focus on understanding and measuring CAL in the various scenarios would be beneficial for students. Additionally, short tutorial videos can be shown to students before their periodontal data collection and small group live demonstrations can be conducted by periodontal faculty in the clinic at the beginning of the clinic activity. It would be beneficial for students if they were able to practice CAL measurement on typodont with various periodontal health conditions and demonstrate their skills and understanding of CAL to instructors before they check CAL on their patients. It is imperative for students to have enough practice with good learning tools or equipment to maximize their learning.11 One study in Japan showed that the newly

developed model designed for pocket depth measurement training can be effective for students to practice.12 Second-year students can also pair up with upper classmates after their required preclinical periodontal data collection training. When upper classmates see patients during COEs or POEs, second-year students could participate in or observe periodontal data collection on actual patient cases with periodontitis.
One of the most common concerns in the student dental clinic at LLUSD is that it can take a significant amount of time to complete COE and POE, as collecting various data slows down the student clinician, one of them being periodontal data.
Students’ clinical abilities perceived
by patients reduce dental anxiety in patients, and the possibility of the patient being anxious increases with long dental appointments.13 Therefore, providing students with multiple practice opportunities can result in the student being more efficient and confident, thus reducing the time taken and ultimately reducing patients’ anxiety and increasing patients’ comfort level.
A limitation of this study is that the accuracy of the periodontal data collected by students was partially evaluated by faculty. Faculty reviewed the recorded data and radiographs in the clinic and spot-checked PD, CAL and other data when needed. Feedback was given to
students during the time of periodontal data collection. The full-mouth data verification was not feasible with a limited number of faculty and limited time allotted to the clinic sessions. However, after data collection activity, students had a separate case presentation session in the clinic for comprehensive oral evaluation treatment planning, and instructors were able to review the overall collected data and check certain areas as necessary to confirm periodontal diagnosis and periodontal treatment plans. Evaluation of the accuracy of the full periodontal data that students collected could be a future research project.
Another drawback of this study is that the patients with whom students worked were primarily their young and healthy classmates. Students were mainly working on healthy gingiva or healthy gingiva with reduced periodontium or gingivitis cases. Most of the students were not able to assess periodontal data collection on active periodontitis cases due to the nature of the patient pool. Examining or collecting data from a patient with periodontitis may be a much different experience for the students, and they may face some challenges compared to the practice sessions. However, one study that assessed students’ probing depth consistency with the use of audio-video method showed that there was no significant difference for the gingivitis and periodontitis patients.14
There was statistically significant time improvement between the first and second periodontal data collection and between the second and third periodontal data collection. Statistical significance was also seen between students’ confidence level and improved data collection time especially during the second data collection.
The results of this study are significant

FIGURE 7. First and third data collection time and student response group for postsurvey 1 and 3.

in proving that repetitive practice is a valuable method of learning to establish a foundation that will guide students in being efficient by decreasing chair time and being confident in patient care. n
1. Fischer RG, Lira Junior R, Retamal-Valdes B, Figueiredo LC, Malheiros Z, Stewart B, Feres M. Periodontal disease and its impact on general health in Latin America. Section V: Treatment of periodontitis. Braz Oral Res 2020 Apr 9;34(supp1 1):e026 doi: 10.1590/1807-3107bor-2020.vol34.0026. PMID:
32294679.
2. Wang W, Ma H, Ren H, Wang Z, Mao L, He N. The impact of surgical boot camp and subsequent repetitive practice on the surgical skills and confidence of residents. World J Surg 2020 Nov;44(11):3607–3615 doi: 10.1007/s00268-02005669-x. PMID: 32632643; PMCID: PMC7527321
3. Al Gharibi Msn KA, Arulappan MSc N PhD DNSc J. Repeated Simulation Experience on Self-Confidence, Critical Thinking, and Competence of Nurses and Nursing Students-An Integrative Review. SAGE Open Nurs 2020 Jun 1;6:2377960820927377 doi: 10.1177/2377960820927377. PMID: 33415282; PMCID: PMC7774432
4. Haleem A, Khan MK, Sufia S, et al. The role of repetition and reinforcement in school-based oral health education-a
cluster randomized controlled trial. BMC Public Health 2016 Jan 4;16:2 doi: 10.1186/s12889-015-2676-3. PMID: 26728002; PMCID: PMC4700643
5. Seleznev I, Alibekova R, Clementi A. Patient satisfaction in Kazakhstan: Looking through the prism of patient healthcare experience. Patient Educ Couns 2020 Nov;103(11):2368–2372 doi: 10.1016/j.pec.2020.05.004. Epub 2020 May 11. PMID: 32448625.
6. Riley JL 3rd, Gordan VV, Rindal DB, Fellows JL, Qvist V, Patel S, Foy P, Williams OD, Gilbert GH. Dental PracticeBased Research Network Collaborative Group. Components of patient satisfaction with a dental restorative visit: Results from the Dental Practice-Based Research Network. J Am Dent Assoc 2012 Sep;143(9):1002–10 doi: 10.14219/ jada.archive.2012.0329. PMID: 22942147; PMCID: PMC3432985
7. Carmagnola D, Filippucci L, Celestino S, Carrassi A, Delia S, Lodi G. A survey on the experience with dental tourism in a sample of Italian patients. Minerva Stomatol 2012 Jan–Feb;61(1–2):11–20. English, Italian. PMID: 22274306.
8. Sunaga M, Minabe M, Inagaki K, Kinoshita A. Effectiveness of a specially designed dental model for training, evaluation, and standardization of pocket probing. J Dent Educ 2016 Dec;80(12):1430–1439. PMID: 27934668.
9. Do JH, Takei HH, Carranza FA. Periodontal Examination and Diagnosis. In: Newman MG, Takei HH, Klokkevold PR, Carranza FA, eds. Newman and Carranza’s Clinical Periodontology. 13th ed. Philadelphia: Elsevier; 2019:378–396.
10. Fritz PC. Clinical attachment level - how to calculate and interpret this important measurement. Oral Health Group. Oct. 1, 2013.
11. Sahu PK, Chattu VK, Rewatkar A, Sakhamuri S. Best practices to impart clinical skills during preclinical years of medical curriculum. J Educ Health Promot 2019 Mar 14;8:57 doi: 10.4103/jehp.jehp_354_18. eCollection 2019 PMCID: PMC6442250
12. Sunaga M, Kondo K, Adachi T, Miura Y, Kinoshita A. Development and evaluation of a new dental model at Tokyo Medical and Dental University for the practice of periodontal pocket probing. J Dent Educ 2013 Sep;77(9):1185–92. PMID: 24002857
13. Caltabiano ML, Croker F, Page L, Sklavos A, Spiteri J, Hanrahan L, Choi R. Dental anxiety in patients attending a student dental clinic. BMC Oral Health 2018 Mar 20;18(1):48 doi: 10.1186/s12903-018-0507-5. PMID: 29558935; PMCID: PMC5859659
14. Prabhu S, John V, Blanchard S, Eckert GJ, Hamada Y. Assessing effectiveness of an audiovisual educational tool for improving dental students’ probing depth consistency. J Dent Educ 2019 Apr;83(4):429–436 doi: 10.21815/ JDE.019.052. Epub 2019 Feb 11. PMID: 30745343.
THE CORRESPONDING AUTHOR, Soh Yeun Kim, DDS, can be reached at sokim@llu.edu.
Presurvey Postsurvey 1 Postsurvey 2 Postsurvey 3
FIGURE 9. Percent of students identifying clinical attachment level (CAL) as the most difficult component of periodontal data collection.

Christine Y.W. Hao, DMD, MPH; Karen Sokal-Gutierrez, MD, MPH; Susan L. Ivey, MD, MHSA; and Kristin S. Hoeft, PhD, MPH
abstract
Background: Formative assessment of the rollout process of the California Oral Health Literacy (OHL) toolkit uses a mixed-methods approach. The OHL toolkit is an educational resource for dental professionals to improve communication with patients. This study was intended to obtain user feedback and suggestions for improvement.

Methods: This mixed-methods assessment of the OHL toolkit rollout included anonymous post-training surveys distributed at regional dental societies in California and 1:1 interviews with dental champions who would work with the research team on toolkit rollout. Anonymous and deidentified data were analyzed using R and Dedoose.
Results: From surveys (n = 37), the OHL toolkit components of highest interest to respondents were teach-back, increasing health literacy awareness among staff and learning to use plain language communication. Perceived implementation barriers were time constraints, insufficient staffing and a need for more training on communication techniques. Impressions, implementation prospects and recommendations for the OHL toolkit were obtained from qualitative interviews (n = 6). Overall, participants had positive impressions of the training presentation, OHL toolkit and implementation prospects.
Conclusion: This study identified interest areas and implementation barriers, data that can be used to further improve the OHL toolkit and reduce barriers faced by practitioners. Further assessments at clinician and patient levels will be helpful for outcomes evaluation.

Practical implications: The OHL toolkit is perceived positively by dental practitioners in California. Facilitators and barriers identified by dental providers and champions can be addressed through changes to the OHL toolkit and training. Rollout at the national level is being considered.
Keywords: Oral health, program evaluation, public health, California, United States
Christine Y.W. Hao, DMD, MPH, began her MPH-dental public health journey in the joint University of California, BerkeleyUniversity of California, San Francisco program in summer 2021. She is currently a dental public health resident at UCSF. As part of her MPH program, Dr. Hao completed a specialty area in maternal, child and adolescent health and earned a certificate in health management.
Conflict of Interest Disclosure: None reported.
Karen Sokal-Gutierrez, MD, MPH, is a clinical professor at the University of California, Berkeley, School of Public Health and a fellow of the American Academy of Pediatrics. She is a physician with training in pediatrics, preventive medicine and public health and has worked as a clinic physician, public health program administrator, child health policy consultant and an educator.
Conflict of Interest Disclosure: None reported.
Susan L. Ivey, MD, MHSA, is an adjunct professor in the University of California, Berkeley, School of Public Health and the director of research at Health Research for Action, an affiliated center of UCB’s School of Public Health. She has been conducting health disparities and health services research for over 20 years.
Conflict of Interest Disclosure: None reported.
Kristin Hoeft, PhD, MPH, is an assistant professor in the division of oral epidemiology and dental public health at the University of California, San Francisco, School of Dentistry. She has worked in dental public health since 2006, working as part of the Center to Address Children’s Oral Health (CAN DO) and the California Oral Health Technical Assistance Center (COHTAC).
Conflict of Interest Disclosure: None reported.
The burden of oral diseases is experienced globally and is accompanied by frequent disparities among low-income and low-literacy populations. This is particularly concerning considering that oral health is fundamental to general health and connected to all life and social functions.1,2 In “Oral Health in America: A Report of the Surgeon General,” oral diseases are described as a “silent epidemic” that disproportionately affects vulnerable populations including ethnic minorities, the elderly and children from lower socioeconomic backgrounds.3 Two decades later, as described in Oral Health in America, a follow-up to the surgeon general’s report, disparities in oral health status continue to exist.4 With consideration to strategies in oral health promotion and population health improvement, the significant role of oral health literacy (OHL) is highlighted in the report.4
Individual health literacy is defined as “the degree to which individuals have the ability to find, understand and use information and services to inform healthrelated decisions and actions for themselves and others.”5 OHL also includes aspects of care processes pertaining to the oral environment.2,6 The consequences of low health literacy are significant. Individuals with lower health literacy are less likely to utilize preventive care and are more likely to utilize emergency care.4,7 Further, among individuals with lower OHL, poorer periodontal health was observed.8 Low oral health knowledge is also associated with a lower perceived oral health-related quality of life.9 Among individuals who did not have a dental visit in the past year, their OHL was found to be lower.10
Recent conceptions of health literacy have expanded from perceptions of health literacy as an individual characteristic to a recognition that communication
occurs between multiple people within an organizational setting. Healthy People 2030 defines organizational health literacy as “the degree to which organizations equitably enable individuals to find, understand and use information and services to inform health-related decisions and actions for themselves and others.”5 This expansion in health literacy definition recognizes the important role that providers and organizations can play in communicating health information to patients, regardless of an individual’s health literacy level.
The emphasis on OHL improvement among providers and patients resonates at state and national levels. The American Dental Association established its National Oral Health Literacy Advisory Committee (NOHLAC) for Health Literacy in Dentistry to advance provider and patient OHL.11 A key part of that committee’s action plan has been the development of an OHL toolkit for dental professionals. Other dental professional and oral health organizations have also set goals to advance OHL.11 In collaboration, an OHL toolkit was developed by the California Department of Public Health Office of Oral Health (CDPH-OOH) and the University of California, Berkeley, School of Public Health’s Health Research for Action (HRA) center.12 The overall goal of the OHL toolkit is to increase OHL among providers and, by interactional influence, to increase OHL among patients and caregivers.12,13
The OHL toolkit consists of five major components: OHL in Practice, a guide book with communication strategies for oral health care providers; the practice assessment checklist, a tool for identification of OHL strengths and opportunities within a dental practice; the teach-back resource guide; the “Going to the Dentist” patient brochure; and the OHL action plan, a worksheet for setting OHL goals in practice. The
toolkit incorporates multiple strategies to create patient-friendly environments and improve provider-patient communication, thereby increasing patient understanding and participation in their care. The OHL toolkit is available to download free of charge from the California Oral Health Technical Assistance Center.14
Although OHL interventions by care providers have been shown to positively influence recipients’ oral health knowledge and skills,15,16 it is important to anticipate potential provider and patient barriers with respect to success. Among providers, perceived barriers include insufficient training in OHL in a professional setting and limited chairside time.17 Among patients, limited literacy skills are a barrier to achieving OHL.18 Common to both, clear communication is critical in improving OHL.17
This study evaluates the OHL toolkit rollout at dental societies in California. Specific objectives are: 1) Evaluate initial feedback from dental society participants on the OHL toolkit training, including impressions of the training and the OHL toolkit and perceived opportunities and barriers for implementation at their practices; 2) interview six dental champions who are also trainers at dental society presentations and collect qualitative data on the OHL toolkit impressions and implementation opportunities and barriers; and 3) identify focus areas for future programs and materials improvement using data collected.
The activities described are part of formative assessments for the rollout process of the OHL toolkit. The OHL toolkit training workshops, consisting of presentations with background about OHL and detailed information on toolkit components, were conducted at regional dental societies and local oral health
programs (LOHPs). Post-training surveys were created for the workshops. Trainings at LOHPs were not assessed as part of this study; this study and methods here pertain only to the activities conducted with dental providers at dental societies. Two main assessment modalities were used:
n Quantitative assessment that consisted of anonymous posttraining surveys at local dental society meetings. Surveys were inputted into Qualtrics survey software and survey links were
utilization to other dentists through dental society trainings.19 The champions received a modest stipend for their participation.
Prior to initiating interviews, verbal informed consent was obtained. Interviews were conducted virtually on Zoom and were audio recorded, transcribed verbatim and deidentified prior to analysis using Dedoose.20 Content analysis was used to examine interview data for common themes around implementation and training for the champion role these dentists would undertake.
It is important to anticipate potential provider and patient barriers with respect to success.
provided both during and after presentations to dental providers.
n As a qualitative element, 1:1 semistructured interviews were conducted with the dental champions. Dental champions are California general and pediatric dentists who already had an interest and/or experience in OHL and who were willing to take on the role of leaders in the OHL improvement process by agreeing to participate in an initial training and then partner with HRA staff to deliver trainings. The terminology “champion” was designated for their role as point persons and leaders in implementing components of the OHL toolkit in their respective organizations or practices as well as demonstrating OHL toolkit
Self-certification by the principal investigator indicated this project was a program evaluation and not considered human-subjects research; therefore, a separate IRB review was not required.
The OHL toolkit trainings were delivered via Zoom presentations at local dental societies, with presenter pairings of dental champions with HRA staff with OHL expertise. The presentations ranged from 60 to 120 minutes and consisted of a core 60-minute presentation used for all presentations. Where time allowed, additional information and practice activities were included. Session length was determined by the respective dental societies’ meeting time constraints. Presenter calibration was not performed. All dental champions, however, attended an OHL toolkit “dental champion” workshop hosted by HRA on Jan. 26, 2022, where detailed information on individual toolkit components was collectively reviewed. They observed the training materials and format, and all used the same standard-base training slide deck with some tailoring for extended-length trainings and for champions to discuss personalized implementation in their own practice.
An anonymous post-training survey link was distributed to attendees during and at the end of OHL toolkit presentations by dental societies in California. Upon opening the survey link, an informative paragraph describing the purpose of
the survey and intended data usage was presented to respondents (APPENDIX 2). The survey had 12 questions and covered basic demographic information, role and years in clinic, clinic type, impressions of the presentation and toolkit, components of interest and
implementation barriers (APPENDIX 2). Survey questions were reviewed by the co-authors for face and content validity. Surveys were hosted on UC Berkeley Qualtrics XM,21 and data analysis was performed using R (version 4.1.2).22,23
From trainings held Feb. 8, 16 and 17, 2022, at three dental societies with a total of 124 attendees consisting of dental practitioners and office staff members, 37 responses from post-training surveys were collected. Survey data collection began Feb. 8, 2022, and ended March 4, 2022, when no new responses were recorded for the next 30 days.24 The interquartile range for survey completion time was approximately two to three minutes.
TABLE 1 is a summary of respondents’ demographics and practice information including current role, years in current role, practice type, Medi-Cal (Medicaid) insurance acceptance, race/ethnicity and gender. Forty-one percent of respondents were dentists and 46% were dental hygienists; 84% of respondents had 10 or more years of experience; 73% of respondents were part of private practices and 16% were part of a federally qualified health center (FQHC); a majority of practices (70%) did not accept Medi-Cal; the highest three proportions of race/ethnic groups were white or Caucasian (49%), Asian (16%) and Hispanic or Latino (14%).
Feedback on the toolkit presentation, impression of the toolkit, toolkit components of interest and potential implementation barriers were identified and summarized. Over 90% of respondents “strongly agree” or “somewhat agree” that the presentation was well-organized
Percentage of respondents %, (n)
0 10 20 30 40 50 60 70
Increase health literacy awareness among staff
Plain language communication
Health literacy practice assessment checklist
Motivational interviewing
Identify translation/interpretation needs
Provide "Going to the Dentist" brochure to patients Plain language signs and forms
Develop health literacy improvement plan Choose a team leader Don’t know yet/undecided I do not intend to implement the toolkit
FIGURE 1. Toolkit components most likely to be utilized.
59 (n=22) 49 (n=18) 46 (n=17) 43 (n=16) 30 (n=11) 22 (n=8) 16 (n=6) 16 (n=6) 16 (n=6) 14 (n=5) 11 (n=4) 3 (n=1)
Percentage of respondents %, (n)
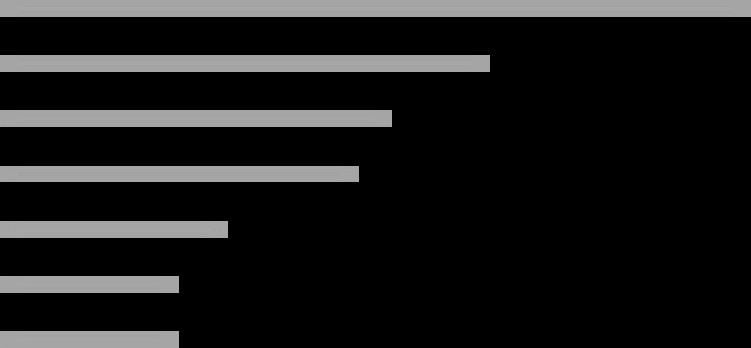
0 5 10 15 20 25 30 35 40 45 50
Time constraint
Insufficient staffing
Need more training on communication techniques
There are no perceived barriers in implementation
Other Need more information for implementation
Need additional materials for implementation
FIGURE 2. Potential toolkit implementation barriers.
increased understanding of OHL and that the training was a good investment of time. A lower but substantial proportion (67%) of respondents indicated they were “extremely likely” or “somewhat likely” to take on toolkit implementation, but 54% felt they needed more information to use the OHL toolkit.
Survey respondents also indicated toolkit components they were most likely to utilize. The top five components of
46 (n = 17) 30 (n = 11) 24 (n = 9) 22 (n = 8) 14 (n = 5) 11 (n = 4) 11 (n = 4)
interest (% respondents, n) were the teachback technique (59%, n = 22) (teach-back assesses patient understanding of their oral health conditions and recommended actions to take), increased health literacy awareness among staff (49%, n = 18), plain language communication (46%, n = 17), the health literacy practice assessment checklist (43%, n = 16) and motivational interviewing (30%, n = 11) (fIGure 1).
The top toolkit implementation
barriers (% respondents, n) were time constraint (46%, n = 17), insufficient staffing (30%, n = 11) and the need for more training on communication techniques (24%, n = 9) (fIGure 2).
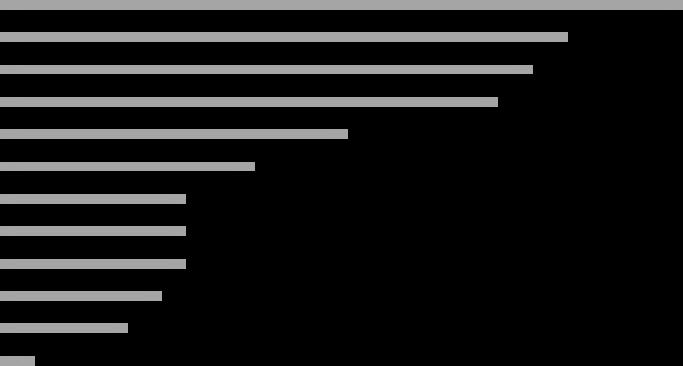
Semi-structured 1:1 interviews were conducted with the dental champions from Jan. 10, 2022, to Jan. 22, 2022. Among the dental champions, 83%
Feedback/impression
Extremely likely/ strongly agree % (n)
Somewhat likely/ somewhat agree % (n)
Neither likely nor unlikely/ neither agree nor disagree % (n)
Somewhat unlikely/ somewhat disagree % (n)
Extremely unlikely/ strongly disagree % (n)
Likelihood of toolkit implementation 32 (12) 35 (13) 22 (8) 3 (1) 8 (3)
Presentation was well-organized 86 (32) 8 (3) 3 (1) 3 (1) 0
N/A % (n)
Presenter is knowledgeable 84 (31) 11 (4) 3 (1) 0 0 3 (1)
I have an increased understanding of OHL 65 (24) 22 (8) 11 (4) 0 0 3 (1)
The training was a good investment of my time 59 (22) 24 (9) 11 (4) 0 3 (1) 3 (1)
Information from training is useful in my work 51 (19) 27 (10) 14 (5) 5 (2) 0 3 (1)
I need more information to be able to use toolkit 22 (8) 32 (12) 24 (9) 8 (3) 11 (4) 3 (1)
(n = 5) were pediatric dentists and 17% (n = 1) were general dentists; 50% (n = 3) were associated with an FQHC or academic clinics and 50% (n = 3) were associated with private practice.
Interview results with the dental champions are organized into key themes and summarized with representative quotes in TABLE 3.
Key themes are:
n Providers have varied OHL skills.
n Priority areas for OHL improvement are identified.
n Impression of the toolkit was mostly positive.
n Suggestions for the toolkit.
The five toolkit components of highest interest level are also compared directly with communication and behavior modification strategies that are used by the dental champions (TABLE 4).
Improving patient and provider OHL has emerged as an important priority of the American Dental Association and other oral health organizations.11 Improved OHL is critical to reduce dental disease and increase preventive care.4 Because dental professionals have a key responsibility
to communicate well with patients to improve their OHL and the ability to adopt positive oral health behaviors, provider communication training is essential.11,12 The California OHL toolkit and associated trainings are intended to advance providers’ OHL skills and, by extension, patients’ OHL abilities.12 This study was intended to provide initial feedback and recommendations in the first phase of the OHL toolkit rollout.
Data from quantitative and qualitative aspects were analyzed and results were contrasted. The overall impression of the toolkit rollout at dental societies was positive with positive implementation prospects (TABLE 2). The dental champions also perceived the toolkit mostly positively and provided suggestions for improvements (TABLE 3).
The top five toolkit components of interest were the teach-back technique, increased health literacy awareness among staff, plain-language communication, the health literacy practice assessment checklist and motivational interviewing (fIGure 1). This was compared with interview results on communication and behavior modification techniques utilized by the dental champions (TABLE 4). A complete
overlap between survey and interview results was observed; this alignment indicates the dental champions are wellpositioned as peer educators for the toolkit training sessions at dental societies.
Upon identification of the toolkit components of interest, adjustments can be made to increase uptake and/ or implementation. These results can be combined with specific recommendations from dental champions (TABLE 3) such as including more graphics, providing laminated physical copies or offering patient-facing materials at a lower literacy level and in different languages.
From post-training surveys, the top three perceived barriers in toolkit implementation were time constraint, insufficient staffing and the need for more training on communication techniques (fIGure 2). A significant overlap in barriers was observed in a three-way comparison among survey results, interview results and current literature (APPENDIX 1). Barriers identified by the dental champions included time constraint and lack of incentives or reimbursement. In a previous formative study by Tseng et al.17 prior to creation of the toolkit, barriers to promoting OHL among dental providers
“Oh, we have a lot to improve.”
“I guess I’ll be generous. I think that we have room for improvement, as we all do. You know the term practice means that you should be continually improving.”
“They [OHL skills] vary and it’s something that we’re constantly reevaluating to make sure we’re not bringing our own biases into our appointments.”
“I feel like in our office, because I’ve made such an emphasis on it and I’ve given lunch-and-learns to my staff, that we’re actually pretty well-equipped to do that [implement the toolkit]. But I kind of realize I may be an outlier because this has been what I’ve devoted much of my career towards.”
• “I’d say from a pediatric standpoint I think it’s really important to have a lot of visuals and signs that are easy to read. Always keeping it simple, and I think that just plays a role for children to read and understand things but also for families and parents too.“
• “Well, I’m always going to be a stickler for the interpreting services. One: Having that signage at the front of the office, systems to coordinate your visits. Second one would be actually using tools for the language and then the third one’s probably teach-back.”
• “I would say I think most providers need to understand the basics of best practices when you talk about health literacy. You know the basics, in pedo-land we do tell-show-do, which is similar to teach-back.”
• “I think it’s laid out very clearly in terms of which pages are for short-term goals and long-term goals. So I think it’s easy to understand and the pictures and the colors and layout is, overall, nice and easy to read.”
• “It looks great on paper, and it’d be nice to see how it’s actually implemented. I’m very curious about implementation.”
• “It’s actually a pretty fantastic toolkit. It’s there to help bring some of these tools into practices that either don’t have them in existence or don’t have them in existence fully.”
• “Maybe more graphics, it’s too wordy.”
• “If we receive the toolkit as more of like how we receive our CPR materials with laminated sheets, or a little kit of cards that are very well packaged, … that would be more engaging for the providers in the clinic and it’s easier to share.”
• “Having more [patient-facing] information at a lower literacy level in different languages … pamphlets or information cards readily available that are easy for the eye. Meaning lots of visuals, also in a language they can understand. Very few wording unless the wording is necessary.”
in California included inadequate clinical time, limited reimbursement and lack of OHL communication training and OHL proficiency requirements. A recurrence of these themes emphasizes priority areas to address to help dental providers overcome barriers in OHL toolkit implementation particularly in areas of communications training, staffing and reimbursement models. Information from this study is foundational in advancing the OHL toolkit rollout. To further evaluate the toolkit’s
effectiveness, subsequent studies on clinical implementation and patient perspectives are necessary. Interventions targeting adults and children continue to provide evidence for the need for OHL improvement. Several studies have shown associations between caregiver health literacy/OHL and the oral health status of children.25–27 A study by Dudovitz et al.16 evaluated the effects of an OHL intervention among parents whose children participated in the Head Start program. Participants had diverse backgrounds and initially had
increased caries risk. The study showed that an OHL intervention delivered by Head Start staff was successful in improving OHL among parents. Interventional activities included healthy meals for parents, hands-on demonstrations and oral health resources including low OHL books and oral hygiene tools. The study also showed positive changes in oral health knowledge and transfer of oral hygiene influences to the children of participants.
Kaur et al.15 studied OHL interventions by dental hygienists. The interventions
TABLE 4
Communication and behavior modification strategies in use by dental champions (from interviews)
• Teach-back
• Increase health literacy awareness among staff
• Clear (plain) language, no jargon
• HL practice assessment
• Motivational interviewing
• Multitasking
• Usage of interpretation services
• Choose a team leader
• Longer/split appointments
• Scripting
• ... and many more
APPENDIX 1
Top five OHL toolkit components most likely to utilize (from survey)
• Teach-back
• Increase health literacy awareness among staff
• Plain-language communication
• HL practice assessment checklist
• Motivational interviewing
Tseng et al.17 Barriers to promote OHL among dental providers in California
• Inadequate clinical time
• Limited reimbursement for patient education
• Lack of OHL communication training and proficiency requirements
• Insufficient high-quality patient education materials
• Logistical and financial difficulties in access to interpretation services
consisted of five elements: A photonovel written specifically for the target population; the teach-back technique; a concrete action plan made by participants; daily tracking of activities by participants; and monthly follow-ups
Top five OHL toolkit components most likely to utilize (from survey)
• Time constraint
• Lack of incentives or reimbursement
• Difficult to quantify improvements
• Bias and lack of passion in cultural competency
Potential barriers to toolkit implementation, from post-training surveys
• Time constraint
• Insufficient staffing
• Need more training on communication techniques
to reinforce behavior. The interventions resulted in improvement in oral hygiene practices among participants.
Because OHL improvement strategies in the OHL toolkit are similar to interventions utilized in the studies
mentioned previously, it is reasonable to anticipate positive OHL improvements among patients upon its implementation. To evaluate OHL impacts, patient-level OHL assessments will be necessary. Some challenges to those assessments are briefly
described here. An ongoing challenge is selection of an appropriate instrument for OHL evaluation among patients. There are several existing instruments with some based on medical or dental vocabulary recognition. The Rapid Estimate of Adult Literacy in Dentistry (REALD) system is based on an individual’s ability to recognize a word and read it aloud correctly.6,15 More recently, OHL evaluations have expanded to include more dimensions such as reading comprehension, decisionmaking and quantitative skills.6 There is also increasing effort in assessing functional aspects of OHL. In a study by Sun et al.,28 an evaluation instrument was developed to assess functional OHL, oral health knowledge, oral health skills and oral health beliefs. Therefore, when assessing OHL, it is important to recognize that different instruments measure various dimensions of OHL.10 One OHL toolkit-relevant way to evaluate improvement in patient OHL would be to assess before and after a provider uses the teach-back technique, which demonstrates a patient’s understanding of their provider’s description of their oral health condition and recommended actions to take. Likewise, case studies of the OHL toolkit implementation in dental practices over time would be valuable.
Strengths of the study include the use of mixed methods for formative assessment of implementation and the opportunity to increase sample size as more trainings are conducted. Limitations of this study include a small number of survey participants (n = 37) and risk of bias because the surveys were voluntary. To increase response rate, future survey completion can be linked to the receipt of continuing education credits.
With respect to qualitative interviews with the dental champions, it is important to recognize that five of the six champions were pediatric dentists, therefore
findings may not represent perspectives of general dentists. Future research should include more input from general dentists and other dental specialists.
In summary, three specific recommendations are to:
n Adjust toolkit components per feedback, interest level and suggestions.
n Take concrete steps in reducing identified barriers to toolkit implementation.
n Assess toolkit implementation at the clinical level and evaluate effects on patient OHL for a more formal outcomes evaluation.
For Future Students and/ or Researchers
Continuing from the three recommendations, multiple approaches are possible. One suggestion is to perform policy analysis on reimbursement models and identify possible reimbursement mechanisms for OHL improvement efforts. Another approach is to evaluate actual uptake/implementation of the OHL toolkit across dental clinics in California. Finally, to examine effects on patient OHL, a comparative study pre- and post-implementation in a sample of practices that plan to implement the OHL toolkit can be considered.
Due to the growing interest in OHL improvement, a nationwide version of the toolkit may also be considered. To facilitate the rollout of a nationwide OHL toolkit, adjustments will be necessary. For example, once a reimbursement model for OHL improvement is established in California, relevant information can be included as reference for other states. In addition to effective interventions and evaluations, multiple stakeholders need to
collaborate for OHL improvement; this involves multiple levels of organization including members of the public, health care providers and policymakers. n
Toolkit development and trainings were funded by the California Department of Public Health Office of Oral Health. We thank study participants and dental societies for their interest in bringing the OHL toolkit trainings to its members and the California Oral Health Technical Assistance Center for hosting the toolkit on its website.
This study was funded by the California Department of Public Health (CDPH) under Contract Number 21-10140.
1. Centers for Disease Control and Prevention. Basics of Oral Health. Jan. 4, 2021. Accessed April 18, 2022.
2. Ramos-Gomez F, Kinsler J, Askaryar H. Understanding oral health disparities in children as a global public health issue: How dental health professionals can make a difference. J Public Health Policy 2020;41(2):114–124 doi:10.1057/ s41271-020-00222-5
3. U.S. Department of Health and Human Services. Oral Health in America: A Report of the Surgeon General. Rockville, Md: U.S. Department of Health and Human Services, National Institute of Dental and Craniofacial, Research, National Institutes of Health; 2000.Accessed April 19, 2022.
4. U.S. Department of Health and Human Services Bethesda, MD: U.S. Department of Health and Human Services, National Institute of Dental and Craniofacial R National Institutes of Health. Oral Health in America: Advances and Challenges Bethesda, Md and National Institute of Dental and Craniofacial Research; 2021.
5. U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion. Health Literacy in Healthy People 2030 - Healthy People 2030. Accessed April 19, 2022.
6. Dickson-Swift V, Kenny A, Farmer J, Gussy M, Larkins
S. Measuring oral health literacy: A scoping review of existing tools. BMC Oral Health 2014;14(1):148 doi:10.1186/1472-6831-14-148 PMCID: PMC4417207
7. Horowitz AM, Kleinman DV. Oral health literacy: A pathway to reducing oral health disparities in Maryland. J Public Health Dent 2012 Winter;72 Suppl 1:S26–30 doi: 10.1111/j.1752-7325.2012.00316.x
8. Baskaradoss JK. Relationship between oral health literacy and oral health status. BMC Oral Health 2018;18(1):172 doi:10.1186/s12903-018-0640-1 PMCID: PMC6201552
9. Kwon SR, Lee S, Oyoyo U, et al. Oral health knowledge and oral health related quality of life of older adults. Clin Exp Dent Res 2021 Apr;7(2):211–218 doi:10.1002/cre2.350. Epub 2020 Nov 17. PMCID: PMC8019761
10. Henderson E, Dalawari P, Fitzgerald J, Hinyard L. Association of Oral Health Literacy and Dental Visitation in an Inner-City Emergency Department Population. Int J Environ Res Public Health 2018 Aug 15;15(8):1748 doi: 10.3390/ ijerph15081748 PMCID: PMC6121363
Thank you for participating in our OHL Toolkit training. Your feedback is very important in helping us improve future training. We appreciate your time and effort in completing this survey. All information collected is for program evaluation and quality improvement purposes only and will remain anonymous.
If you have questions or would like assistance, please contact Jessica at healthaction@berkeley.edu.
Thank you!
Q1. Which of the following best describes your role?
[Choices: dentist; dental hygienist; dental assistant; office manager; administration; dental director; other — please specify]
Q2. How many years have you been in this role? [numeric entry]
Q3. Which of the following best describes your dental practice? [select all that apply] [Choices: private practice; federally qualified health centers (FQHC); corporate/group practice; other — please specify]
Q4. [If in Q3, private practice, corporate/group practice or other is selected.] Does your practice accept patients on Medi-Cal Dental? [Yes/No]
Q5. What is your gender?
[Choices: male; female; other; prefer not to answer]
Q6. Which of the following best describes you?
[Choices: American Indian/Alaska Native; Asian; Black or African American; Hispanic or Latino; Native Hawaiian/Other Pacific Islander; white or Caucasian; biracial/multiracial; a race/ethnicity not listed above; prefer not to answer]
Q7. How likely are you to implement component(s) of the toolkit in your practice?
[Choices: extremely unlikely; somewhat unlikely; neither likely nor unlikely; somewhat likely; extremely likely]
Q8. Which, if any, from the following components in the toolkit are you most likely to utilize? Select up to five (5).
[Choices: Health literacy practice assessment checklist; increase health literacy awareness among staff; develop health literacy improvement plan; choose a team leader; plain language signs and forms; plain language communication; identify translation/ interpretation needs; teach-back technique; motivational interviewing; provide “Going to the Dentist” brochure to patients; other — please specify; I do not intend to implement the toolkit; don’t know yet/undecided]
Q9. If applicable, what are potential barriers in implementing the toolkit? [select all that apply]
[Choices: Need more information for implementation; need additional materials for implementation; need more training on communication techniques; time constraint; insufficient staffing; other — please specify; there are no perceived barriers in implementation]
Q10. For each question, please select the option you most identify with. [Choices: strongly disagree; somewhat disagree; neither agree nor disagree; somewhat agree; strongly agree] a) The presentation was well-organized.
b) The presenter is knowledgeable.
c) I have increased understanding in the topic of oral health literacy.
d) The training was a good investment of my time. e) Information from the training is useful in my work.
f) I need more information to be able to use the toolkit.
Q11. If you have additional questions or comments, please let us know here.
Q12. Please describe one aspect from the presentation that can be improved.
11. Clough SR. American Dental Association: Advancing health literacy within and by the dental profession. J Calif Dent Assoc 2020 Aug;48(8):383–387. Accessed Aug. 3, 2022.
12. Neuhauser L, Eleftherion A, Jackson R, et al. Development of the California Oral Health Literacy Toolkit. J Calif Dent Assoc 2021 Sep;49(9):587–593

13. Kumar J, Jackson R. California Department of Public Health. California Oral Health Plan 2018-2028. Published online January 2018. Accessed May 5, 2022.
14. California Oral Health Technical Assistance Center. Oral Health Literacy Toolkit. Accessed April 19, 2022.
15. Kaur N, Kandelman D, Potvin L. Effectiveness of “Safeguard Your Smile,” an oral health literacy intervention, on oral hygiene self-care behaviour among Punjabi immigrants: A randomized controlled trial. Can J Dent Hyg 2019;53(1):11 PMCID: PMC7533823
16. Dudovitz R, Teutsch C, Holt K, Herman A. Improving parent oral health literacy in Head Start programs. J Public Health Dent 2020;80(2):150–158 doi:10.1111/jphd.12361
17. Tseng W, Pleasants E, Ivey SL, et al. Barriers and Facilitators to Promoting Oral Health Literacy and Patient Communication among Dental Providers in California. Int J Environ Res Public Health 2020 Dec 30;18(1):216 doi: 10.3390/ ijerph18010216 PMCID: PMC7795206
18. Macek MD, Atchison KA, Wells W, Haynes D, Parker RM, Chen H. Did you know Medicare does not usually include a dental benefit? Findings from a multisite investigation of oral health literacy: Medicare does not usually include a dental benefit. J Public Health Dent 2017;77(2):95–98 doi:10.1111/jphd.12199 PMCID: PMC5557019
19. Shaw EK, Howard J, West DR, et al. The role of the champion in primary care change efforts: From
the State Networks of Colorado Ambulatory Practices and Partners (SNOCAP). J Am Board Fam Med 2012 Sep–Oct;25(5):676–685 doi:10.3122/ jabfm.2012.05.110281 PMCID: PMC3535479
20. Dedoose. Dedoose 9.0.46
21. Qualtrics. Qualtrics XM. March 2022.
22. R Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing: Vienna; 2020.
23. RStudio Team. RStudio: Integrated Development for R Boston; 2019.
24. Qualtrics. For how long should you accept survey responses? Accessed Aug. 2, 2022.
25. Miller E, Lee JY, DeWalt DA, Vann WF. Impact of caregiver literacy on children’s oral health outcomes. Pediatrics 2010;126(1):107–114 doi:10.1542/peds.2009-2887 PMCID: PMC2896459
26. Firmino RT, Ferreira FM, Martins CC, Granville-Garcia AF, Fraiz FC, Paiva SM. Is parental oral health literacy a predictor of children’s oral health outcomes? Systematic review of the literature. Int J Paediatr Dent 2018;28(5):459–471 doi:10.1111/ipd.12378. Online ahead of print.
27. Bridges SM, Parthasarathy DS, Wong HM, Yiu CKY, Au TK, McGrath CPJ. The relationship between caregiver functional oral health literacy and child oral health status. Patient Educ Couns 2014 Mar;94(3):411–416 doi:10.1016/j.pec.2013.10.018
28. Sun Y, Sun J, Zhao Y, Cheng A, Zhou J. A new comprehensive oral health literacy scale: Development and psychometric evaluation. BMC Oral Health 2021 Sep 5;21(1):429. doi:10.1186/s12903-021-01795-7 PMCID: PMC8419934

Emily Duong, BS; Elaine Pham, BS; Julia Esfandi, BS; Kim-Sa Kelly, BS; Arvin Pal, DDS; Masooma Rizvi, DDS; Nini Tran, DDS, PhD; Tingxi Wu, DDS, PhD; Bhumika Shokeen, PhD; and Renate Lux, PhD

Background: This study investigated the microbial changes during treatment with clear aligners (CA) and fixed appliances (FA) and evaluated the utility of saliva as a diagnostic marker in orthodontic patients.

Methods: Ten patients each were enrolled in the FA and CA groups. Plaque (PI) and gingival indices (GI) were measured at baseline, three, six and 12 months. Saliva and plaque samples were collected at each time point for determination of the respective microbial community composition via 16S rRNA sequencing.
Results: PI and GI increased significantly over time only in FA patients. While alpha diversity was similar for FA or CA patients, beta diversity and microbial community composition analysis revealed significant differences between saliva and plaque for both treatment groups. Further analysis of the relative abundance of certain health- and disease-associated genera present in the saliva and plaque of FA and CA patients correlated with the clinical parameters.
Conclusions: Clinical parameters significantly worsened during orthodontic treatment with FA but not CA. The microbial composition of plaque and saliva differed significantly between treatment groups. However, the changes in abundance of some individual genera were similar in both saliva and plaque in correlation with the corresponding clinical parameters. These genera show potential as biomarkers for health and disease.
Practical implications: Monitoring of the microbial community composition during orthodontic treatment could reduce the risk of oral disease development. While the microbial composition of saliva is not reflective of the plaque communities implicated in oral health and disease, individual marker genera show promise as biomarkers.
Keywords: Orthodontics, fixed appliances, clear aligners, microbiome, saliva, plaque, gingival inflammation
Emily Duong, BS, is a DDS candidate at the University of California, Los Angeles (UCLA), School of Dentistry. She and Ms. Pham contributed equally to this paper.
Elaine Pham, BS, is a fourth-year student in the department of molecular, cell and developmental biology at UCLA. She and Ms. Duong contributed equally to this paper
Julia Esfandi, BS, is a DDS candidate at UCLA.
Kim-Sa Kelly, BS, is a DDS candidate at UCLA.
Arvin Pal, DDS, is a thirdyear orthodontics resident at UCLA.
Masooma Rizvi, DDS, is a first-year periodontics resident at UCLA.
Nini Tran, DDS, PhD, is an assistant professor in the section of pediatric dentistry at UCLA.
Tingxi Wu, DDS, PhD, is the director of orthodontic and craniofacial development research at the Forsyth Institute in Cambridge, Massachusetts.
Bhumika Shokeen, PhD, is a project scientist in the section of periodontics at the UCLA School of Dentistry.
Renate Lux, PhD, is a professor in the section of periodontics at the UCLA School of Dentistry.
Conflict of Interest Disclosure: None reported for any of the authors.
Malocclusion has traditionally been treated with the use of orthodontic fixed appliances (FA) to correct tooth alignment. This treatment involves brackets and bands bonded onto the enamel and a flexible arch-wire ligated onto the brackets in order to produce light continuous forces to reposition teeth. However, FA can impede oral hygiene care and contribute to significant biofilm accumulation, resulting in a higher risk of caries and periodontal diseases.1 The introduction of clear aligners (CA) in the 1990s as a removable option to address malocclusion has facilitated proper oral hygiene practices. While correct usage of CA can be very beneficial for oral hygiene, CA patients still run the risk of developing dental plaque on tooth surfaces due to the full coverage design of the CA. Dental plaque is a sticky film of bacteria that layers itself onto oral surfaces in an intricate, well-organized manner.2,3 Accumulation of this dental plaque often leads to gingival inflammation and enamel demineralization, resulting in periodontal diseases and dental caries.1
Several earlier studies investigating the clinical health in patients treated with different types of orthodontic appliances reported that in comparison to FAs, treatment with CA resulted in improved periodontal health4–8 and reduction in plaque accumulation.9,10 Generally, clinical outcomes are closely interrelated with the associated microbial communities. Therefore, investigating the changes in microbiome composition after the introduction of orthodontic appliances is critical for understanding their impact on oral health.
Most of the earlier efforts to evaluate the changes in microbial composition after the introduction of orthodontic appliances in the oral cavity were targeted to a
few selected pathogens by quantitative methods.10–12 While these approaches yielded some interesting insights, they did not allow a deep understanding of the changes occurring at the community level. More recently, several studies have investigated the effect of clear aligners treatment on the oral microbial community as a whole,13,14 but only a selected few studies15–17 have compared the microbiomes between two different orthodontic treatments (CAs and FAs). Additionally, these studies either analyzed plaque15,16 or saliva to evaluate the microbial changes.17 Comprehensive studies comparing the clinical implications of the two different treatment modalities along with the longitudinal assessment of the microbial composition of saliva and plaque are still missing. This lack of inclusive studies evaluating the effects of treatment leaves a significant gap in our understanding of the microbial shift and the associated oral health implications.
In the oral cavity, saliva serves a variety of functions including lubrication of oral tissues and plays important roles in the host defense against pathogens. Additionally, saliva acts as a buffer and prevents the progression of tooth decay by remineralizing the tooth enamel layer and neutralizing the acidity of bacterial metabolic waste products. As saliva is a repository of microbes and multiple other biomarkers, numerous studies have explored the use of saliva as a diagnostic tool.18–20 Although, in periodontitis, some studies have demonstrated the potential of saliva as a reliable diagnostic tool,21,22 the use of saliva as a dependable diagnostic tool for patients undergoing orthodontic treatment remains unclear.
The few studies17,23 that have explored saliva for investigating changes in microbial composition during orthodontic treatment did not identify any significant changes in salivary microbial
composition post-treatment. Thus, our aims in this longitudinal study were to investigate the microbial changes in plaque and saliva of patients with FA or CA and assess the corresponding clinical parameters. Furthermore, we evaluated the utility of saliva as a diagnostic marker for oral microbiome changes during orthodontic treatment.
This study was approved by the Institutional Review Board (IRB) at the University of California, Los Angeles (UCLA) (IRB #16-001258). The subjects who were starting their treatment at the UCLA orthodontics clinic were screened and recruited in the study. Informed consent was obtained and subjects were grouped based on their treatment modality, with 10 subjects each in the FA or CA groups. Patients with active caries, periodontal disease and chronic systemic diseases were excluded, along with patients who took antibiotic medications within 30 days of starting treatment.
Saliva and plaque samples were collected from patients at four different time points: pretreatment baseline (T0), three months (T1), six months (T2) and 12 months (T3) after treatment start. At each appointment, plaque and gingival indices were measured. Plaque accumulation was quantified using the Turesky Modified QuigleyHein Plaque Index (TQHPI),24 which utilizes a scale from 0-5 to evaluate supragingival tooth plaque after the patient rinsed with a TRACE disclosing solution (Young Dental LLC, Earth City, Missouri). For gingival health, swelling and bleeding, the two signs of inflammation, were assessed and the level of gingival disease was qualitatively measured with the Löe-Silness gingival index (GI) on a scale from 0-3.25
Supragingival plaque samples were
collected from the gingival third of the central incisors and premolars using sterilized periodontal scalers. To obtain saliva samples, patients expectorated into 50 ml sterile falcon tubes. The saliva was then aliquoted into cryotubes with 15% glycerol in phosphate buffered saline (1X PBS) and stored in a freezer at – 80° C until further use. In addition, tray plaque was collected from the intaglio of the patients’ clear aligner trays using interproximal brushes. All plaque samples were collected into sterile 1X PBS and placed into a – 80° C freezer until further use.
We evaluated the utility of saliva as a diagnostic marker for oral microbiome changes during orthodontic treatment.
and reverse primers and 1X of the HF Taq polymerase Master mix (NEB, Ipswich, Massachusetts). The PCR cycles consisted of an initial denaturation step of 98° C for three minutes followed by 35 cycles of 98° C for 30 seconds, 55° C for 30 seconds, 72° C for 30 seconds with a final extension of 72° C for five minutes. The PCR products were then pooled and cleaned with AMPure XP beads (Beckman Coulter, A63881, Indianapolis) before adding indices using the Nextera XT Index kit (Illumina). After quantification of the amplicons with the DNA KAPPA kit (Roche Diagnostics, Indianapolis), equal amounts of each sample were pooled into a single library. The quality and quantity of the library were checked at the Technology Center of Genetics and Bioinformatics Core at UCLA before MiSeq sequencing on the Illumina platform.
DNA from the saliva and plaque samples was extracted using the MasterPure DNA Purification Kit (Epicentre, Biosearch Technologies, Middlesex, U.K.) based on manufacturer’s instructions with minor modifications.26 A nanodrop (Thermo Scientific, Waltham, Massachusetts) was used to measure DNA quality and quantity. Further, the 16S rRNA library was constructed according to the HOMINGS protocol using V1-V3 primers instead of V3-V4 primers. Briefly, the V1 to V3 region of the 16S rRNA gene was amplified using gene specific primers with Illumina overhang adapters (Illumina, San Diego). Three PCR reactions were carried out for each sample and pooled together to reduce bias. Each PCR reaction mixture (25 µl) contained 25 ng DNA, 0.4 µM each of the forward
Following the demultiplexing and trimming of barcodes, low-quality sequences containing bases with Phred quality values < 20 were trimmed and denoised using the DADA2 package (Callahan, McMurdie, et al. 2016). The amplicon sequence variants (ASVs) generated were taxonomically assigned by comparison to the HOMD database (Chen, Yu, et al. 2010). Alpha and beta diversity analyses were performed using the core metrics plug-in in QIIME 2. The Shannon’s index diversity measure was used for calculating alpha diversity, while weighted UniFrac was used for assessing beta diversity.
The power of the study was calculated using the G*Power statistical analysis program27,28 (version 3.1.9.4; Franz Faul, Christian-Albrechts-Universitat, Kiel, Germany). Data normality was determined using the Shapiro-Wilk analysis.29 Statistical significance was calculated using a two-tailed t-test for the TQHPI and the Mann-Whitney U test
TABLE 1
Fixed appliance (FA) Clear aligner (CA)
Patients 10 10 Female 6 7 Male 4 3
Average age (years) 23.0 30.9 SD (years) 13.6 12.3
TABLE 2
Shapiro-Wilk Statistical Analysis of Plaque Index (PI) and Gingival Index (GI)
Plaque index (PI) Gingival index (PI)
n 10 10 Mean 6 7 SD 4 3 W 23.0 30.9 Distribution 13.6 12.3
TABLE 2. The use of site-specific values in the calculation of each analysis resulted in two values per appointment per patient (n = 72).
for the GI scores at a level of p ≤ 0.05. GraphPad Prism (version 9.1.0; GraphPad Software Inc., San Diego) was used to assess significance of alpha diversity measures by the Kruskal-Wallis test.
A total of 20 patients participated in this study and were divided into two groups based on the treatment they received: FA, n=10 or CA, n = 10. The average age of the FA group was 23.0 ± 13.6 years, while the average age of the CA group was 30.9 ± 12.3 years (TABLE 1 ). The difference in age was not statistically significant (p = 0.201). The sex distribution between groups was similar but not identical: The FA group consisted of six females and four males, while the CA group was comprised of seven females and three males (TABLE 1 ). To analyze the normality of the clinical
data, the Shapiro-Wilk test29 was used. As shown in TABLE 2 , at a threshold of p = 0.05, it was determined that the plaque index (PI) followed a normal distribution, while the gingival index (GI) did not follow a normal distribution. Further, the G*Power statistical analysis program was used to calculate the implied and power of the study. The effect size for the PI data was 0.0670 and the calculated power was 0.9676. The effect size for the GI data was 0.1893 and the calculated power was 0.7105.
The assessment of clinical parameters such as PI showed a clear upward trend between baseline and 12 months in the FA group; however, no such increase was noted in the CA group (f IG ure 1 A ). A two-tailed t-test revealed a statistically significant difference in PI from baseline to six months and from baseline to 12 months (p < 0.05) in the FA group, while
no significant difference was observed in the CA group. Because the GI data did not follow a normal distribution, the Mann-Whitney U test was performed to calculate significance. Similar to the PI values, the FA but not the CA group demonstrated an increasing trend in GI scores between baseline and 12 months (f IG ure 1 B ). This increase in GI was significant between baseline to six months and baseline to 12 months in patients receiving FA treatment (P < 0.05).
Following the analysis of clinical parameters, changes at the microbial level were assessed. To observe the within sample diversity, alpha diversity using Shannon’s index measure was calculated for the saliva and plaque samples from both FA and CA patients. No significant changes in alpha diversities were found over time for any of the sample types from either CA or FA (f IG ures 2 A and 2B ). Furthermore, when comparing the groups against each other, no significant differences were observed between saliva, tooth-associated plaque and trayassociated plaque at any of the time points (f IG ures 2 A and 2B ). Although a small decrease in the alpha diversity of saliva was observed in comparison to plaque in both FA and CA, the difference was not statistically significant (f IG ures 2 A and 2B ). The similarities and dissimilarities in the communities were further evaluated using beta diversity analysis, which was measured by weighted UniFrac distances. The distances were plotted using principal coordinate analysis (PCoA) for each collection time point (f IG ure 3 ). The saliva communities were very different from plaque communities irrespective of the FA or CA group and exhibited a distinct cluster from plaque at all time points (f IG ures 3 A-3D ). Additionally, the tray plaque biofilm community was markedly different from plaque and demonstrated its own cluster at all
FIGURES 1. Graphical representation of the clinical parameters in the fixed appliances (FA) and the clear aligners (CA) group. 1A. The histogram represents plaque index (PI) scores at 0 months (T0), three months (T1), six months (T2) and 12 months (T4) visits in both the FA (blue bar) and the CA (orange bar) group. 1B. The bar graph represents gingival index (GI) assessment at 0 months (T0), three months (T1), six months (T2) and 12 months (T3) visits in both the FA (blue bar with black dots) and CA (orange bar with black dots) group. The data is represented as the mean of plaque index or gingival index with standard error of mean (SEM). * Indicates significant differences of p < 0.05.
1A 1B 2A 2B
FIGURES 2. Alpha diversity analysis by Shannon’s index of saliva and plaque collected from 2A. fixed appliances (FA) patients at 0 months (T0), three months (T1), six months (T2) and 12 months (T3) duration in plaque (purple bars) and saliva (blue bars); and 2B. Clear aligners (CA) patients at 0 months (T0), three months (T1), six months (T2) and 12 months (T3) duration in plaque (green bars), saliva (orange bars) and tray plaque (red bars). The data are represented as the mean of Shannon’s index with standard error of mean (SEM).

available time points (f IG ures 3 B-3D ). The greatest disparity in beta diversity analysis for saliva and plaque was observed at the 12-month time point for both the FA and CA groups (f IG ure 3D ).
Next, the microbial composition in the FA and the CA group was analyzed at the genus level for both plaque as well as saliva samples. The microbial compositions of saliva and plaque were distinct (f IG ures 4 ). While some variation was apparent, the overall microbial profiles for each treatment did not seem to change much over time. However, when comparing the bacterial compositions between
plaque and saliva at the individual genus level, saliva harbored a higher relative abundance of Streptococcus whereas plaque samples contained a greater abundance of Actinomyces in both FA and CA groups (f IG ures 4 A and 4B ). In CA patients, the tray plaque composition resembled the saliva community more than the tooth-associated plaque at all time points (f IG ure 4B ). Although the communities were very similar in the same treatment group at all time points, some genera exhibited differential increase or decrease in relative abundance over time in both FA and CA. Notably, the
relative abundance of Veillonella and Haemophilus varied throughout the course of treatment in both groups and correlated with the clinical parameters (f IG ure 5 ). In the FA group, the relative abundance of the disease-associated genus Veillonella increased in both plaque and saliva, whereas in the CA group, no change was observed. In contrast, the health-associated genus Haemophilus decreased in both saliva and plaque of the FA group, while in the CA group, relative abundance varied but no consistent trend was observed.

With the increased use of CA and the continued widespread use of FA, which has long been associated with white spot lesions and gingival inflammation, a more thorough investigation of how these treatment modalities affect microbial community composition in both saliva and plaque is warranted. Therefore, in this longitudinal study, we investigated how both plaque and salivary microbiomes are affected by treatment with fixed appliances (FA) and clear aligners (CA) and how they are correlated with the clinical parameters.
The analysis of clinical parameters revealed a significant increase in PI and GI indices over time only in the FA group (f IG ure 1 ). This observation was consistent with previous
research that showed higher levels of supragingival plaque accumulation in FA patients6,7,15,16,30–32 and better maintenance of periodontal health in the CA group.10,33 Consequently, FA treatment leads to increased gingival inflammation, whereas CA treatment poses no such risk to the periodontium. The stability of the PI and GI scores in the CA group throughout the 12 months of treatment suggests that the removable nature of such devices is advantageous by enabling better access for oral hygiene care and thus reducing plaque accumulation and gingival inflammation as compared to FA.32 Although insignificant, the average between the two groups may also have played a role, as the average age was higher in the CA group suggesting that this group was better in following the directions and maintaining better oral hygiene.
Alpha diversity analysis demonstrated that there were no significant differences in saliva and plaque in either of the treatment groups, indicating similar microbial diversities within samples (f IG ure 2 ). Furthermore, no changes in alpha diversity were found over time for all the sample types. In agreement with this observation, a study by Wang et al.17 as well as our own previous studies15,16 did not find any significant differences in alpha diversity between CA and FA. Additionally, studies focusing only on CA also reported similar alpha diversities before and after orthodontic treatment.13,14
Beta diversity is used to measure the similarity or dissimilarity of different microbial communities and can be defined as the variability in taxonomic composition among sampling units for a given area.34 Beta diversity analysis showed

4A 4B
that the microbial communities in plaque and tray plaque are highly distinct from each other (f IG ure 3 ). Interestingly, the tray plaque communities localize close to the salivary samples. Because saliva coats the entire oral cavity, it can act as an intermediary between supragingival tooth and tray plaque. Over time, plaque, tray plaque and saliva microbiomes gradually become more distinct in both the FA and CA groups, with the largest disparity seen at the 12-month time point.
Each group tested in this study (saliva, plaque and tray plaque) has a
unique bacterial community at baseline that fluctuates throughout orthodontic treatment as shown in f IG ures 4 A and 4B . However, if just plaque is considered, within the two groups, in accordance with our earlier study,16 Leptotrichia increased over time in plaque of FA but not in the CA patients. This trend was not observed in saliva. In between CA and tray plaque, consistent with earlier findings,16 Corynebacterium, Actinomyces and Selenomonas were higher in relative abundance in CA in comparison to tray plaque. Throughout treatment, changes
occur in the oral microbiome, which are evident in saliva, plaque and CA tray plaque. Furthermore, the higher relative abundance of Streptococcus in saliva compared to the higher relative abundance of Actinomyces in plaque could be a factor in the dissimilarity in microbial community compositions of saliva and plaque. This finding along with the differences in beta diversity revealed that saliva does not accurately reflect the microbiome changes in plaque. Although saliva can be representative of the entire oral microbiome, it may not be specific enough to identify the pathogenic changes occurring on the tooth and gingiva, unlike plaque, which is indicative of the clinical changes at distinct oral locations.

The genus-level analysis in correlation with the clinical parameters revealed that some genera exhibited a strong correlation with the PI and GI. In accordance with some earlier studies,16 Veillonella, previously associated with caries35,36 and periodontitis,37,38 showed a significant increase in the relative abundance with time in the FA group indicating correlation with higher PI and GI (fIGure 5). However, in the CA group, no such increased abundance was observed. In contrast, Haemophilus, a health-associated bacterial genus,16,39 exhibited decreased relative abundance with time in FA.16 The relative abundance of Haemophilus was, however, similar in the CA group. This correlation of Veillonella and Haemophilus with time was detected both for saliva and plaque samples in FA and thus holds potential as biomarkers for future orthodontic treatment studies.
In this study, patients undergoing orthodontic treatment with FA demonstrated significantly more plaque accumulation and poor gingival health, whereas no such difference was observed
FIGURES 5. Percentage relative abundance of 5A-5B Veillonella at 0 months (T0), three months (T1), six months (T2) and after 12 months (T3) duration for both FA and CA groups in plaque and saliva. 5C-5D Haemophilus at 0 months (baseline), three months (T1), six months (T2) and after 12 months (T3) duration for both FA and CA groups in plaque and saliva. The data are represented as the mean of relative abundance with standard error of mean (SEM).
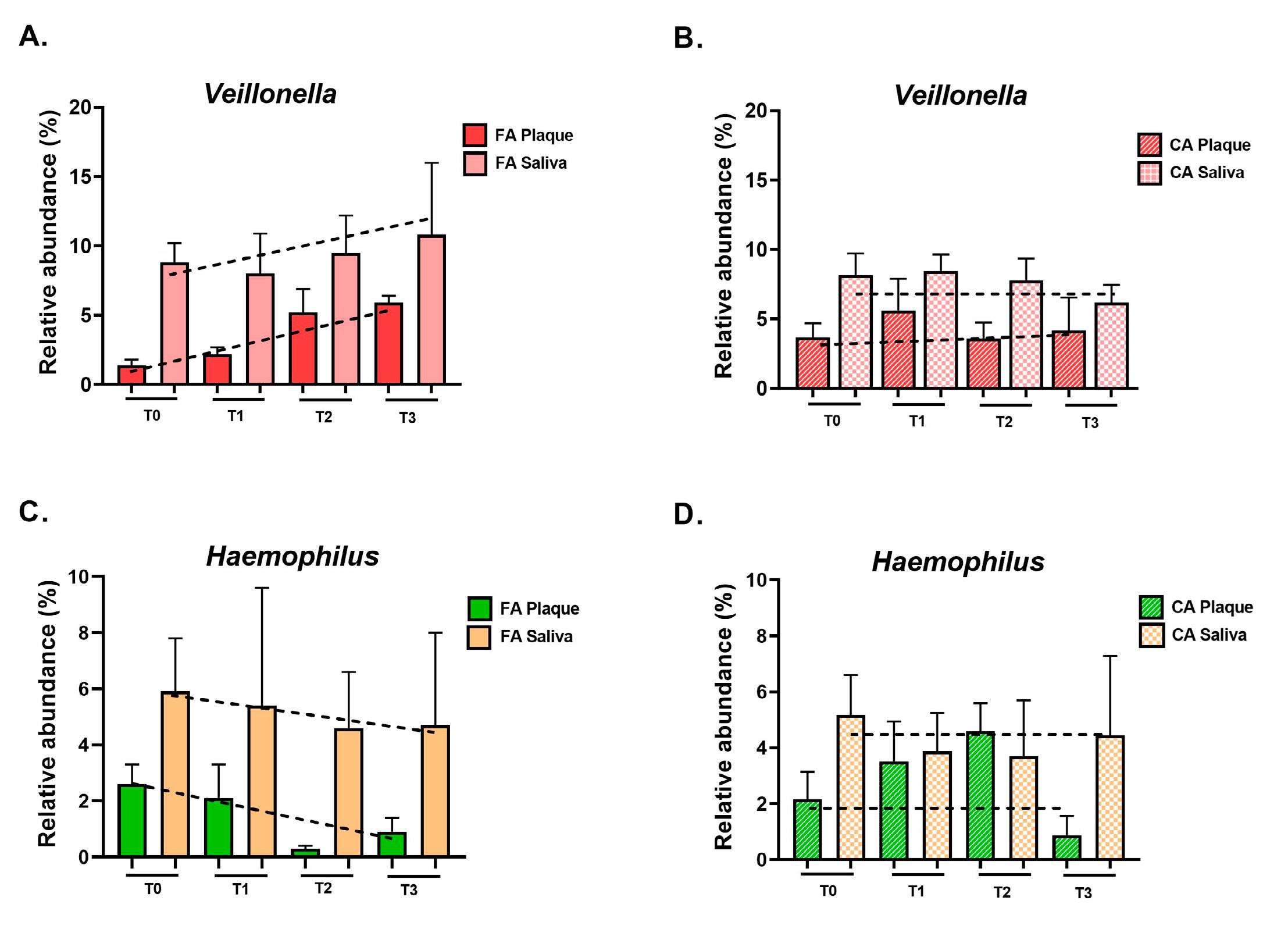
in patients with CA. Although the alpha diversities were similar in patients with FA and CA for both plaque and saliva, beta diversity analysis revealed that the compositions of these communities were different. Saliva failed to reflect the same microbial changes that occur in plaque and thus cannot be used as a diagnostic tool in orthodontic treatment, but individual genera within saliva show potential as biomarkers for health and disease. However, future studies are necessary to better understand the clinical relationship between plaque and saliva in both treatment groups and to independently validate the potential
utility of the identified genera as healthand disease-related biomarkers. n
The authors thank all of the study participants. This project was partially funded by the orthodontic faculty development fellowship award from the American Association of Orthodontist Foundation to Dr. Tingxi Wu.
1. Wade WG. The oral microbiome in health and disease. Pharmacol Res 2013 Mar;69(1):137–43 doi: 10.1016/j. phrs.2012.11.006. Epub 2012 Nov 28.
2. Dewhirst FE, Chen T, Izard J, et al. The human oral microbiome. J Bacteriol 2010 Oct;192(19):5002–17 doi: 10.1128/JB.00542-10. Epub 2010 Jul 23. PMCID: PMC2944498.
3. Marsh PD. Dental plaque as a biofilm and a microbial community — implications for health and disease. BMC Oral Health 2006 Jul;6 Suppl 1:S14 doi.org/10.1186/1472-
6831-6-S1-S14
4. Azaripour A, Weusmann J, Mahmoodi B, et al. Braces versus Invisalign: Gingival parameters and patients’ satisfaction during treatment: A cross-sectional study. BMC Oral Health 2015 Jun 24;15:69 doi: 10.1186/s12903-015-0060-4
5. Jiang Q, Li J, Mei L, et al. Periodontal health during orthodontic treatment with clear aligners and fixed appliances: A meta-analysis. J Am Dent Assoc 2018 Aug;149(8):712–720.e12 doi: 10.1016/j.adaj.2018.04.010 Epub 2018 Jun 18.
6. Lu H, Tang H, Zhou T, Kang N. Assessment of the periodontal health status in patients undergoing orthodontic treatment with fixed appliances and Invisalign system: A metaanalysis. Medicine (Baltimore) 2018 Mar;97(13):e0248 doi: 10.1097/MD.0000000000010248 PMCID: PMC5895427
7. Rossini G, Parrini S, Castroflorio T, Deregibus A, Debernardi CL. Periodontal health during clear aligners treatment: A systematic review. Eur J Orthod 2015 Oct;37(5):539–43 doi: 10.1093/ejo/cju083. Epub 2014 Dec 29.
8. Mulla Issa FHK, Mulla Issa ZHK, Rabah AF, Hu L.
Periodontal parameters in adult patients with clear aligners orthodontics treatment versus three other types of brackets: A cross-sectional study. J Orthod Sci 2020 Feb 12;9:4 doi: 10.4103/jos.JOS_54_17. eCollection 2020. PMCID: PMC7041336
9. Miethke RR, Vogt S. A comparison of the periodontal health of patients during treatment with the Invisalign system and with fixed orthodontic appliances. J Orofac Orthop 2005 May;66(3):219–29 doi: 10.1007/s00056-005-0436-1
10. Mummolo S, Nota A, Albani F, et al. Salivary levels of Streptococcus mutans and Lactobacilli and other salivary indices in patients wearing clear aligners versus fixed orthodontic appliances: An observational study. PLoS One 2020 Apr 24;15(4):e0228798 doi: 10.1371/journal. pone.0228798. eCollection 2020. PMCID: PMC7182227
11. Naranjo AA, Trivino ML, Jaramillo A, Betancourth M, Botero JE. Changes in the subgingival microbiota and periodontal parameters before and 3 months after bracket placement. Am J Orthod Dentofacial Orthop 2006 Sep;130(3):275.e17–22 doi: 10.1016/j. ajodo.2005.10.022
12. Lee SM, Yoo SY, Kim HS, et al. Prevalence of putative periodontopathogens in subgingival dental plaques from gingivitis lesions in Korean orthodontic patients. J Microbiol 2005 Jun;43(3):260–5
13. Guo R, Zheng Y, Liu H, et al. Profiling of subgingival plaque biofilm microbiota in female adult patients with clear aligners: A three-month prospective study. PeerJ 2018 Jan;6:e4207 doi: 10.7717/peerj.4207. eCollection 2018 PMCID: PMC5755484
14. Zhao R, Huang R, Long H, et al. The dynamics of the oral microbiome and oral health among patients receiving clear aligner orthodontic treatment. Oral Dis 2020 Aug;26(2):473–83 doi.org/10.1111/odi.13175
15. Mullen J, Agnello M, Viloria E, Chien KC, Duong E, Rizvi M, Hajian P, Li H, Shi B, Ting K, Shi W, Lux R, Wu T. Clinical and microbial changes in orthodontic patients using clear aligners vs. fixed appliances. J Calif Dent Assoc 2019 Dec;47(12):783–91
16. Shokeen B, Viloria E, Duong E, et al. The impact of fixed orthodontic appliances and clear aligners on the oral microbiome and the association with clinical parameters: A longitudinal comparative study. Am J Orthod Dentofacial Orthop 2022 May;161(5):e475–e485. doi: 10.1016/j. ajodo.2021.10.015. Epub 2022 Mar 2.
17. Wang Q, Ma JB, Wang B, et al. Alterations of the oral microbiome in patients treated with the Invisalign system or with fixed appliances. Am J Orthod Dentofacial Orthop 2019 Nov;156(5):633–640 doi: 10.1016/j.ajodo.2018.11.017
18. Eroglu AK, Baka ZM, Arslan U. Comparative evaluation of salivary microbial levels and periodontal status of patients
wearing fixed and removable orthodontic retainers. Am J Orthod Dentofacial Orthop 2019 Aug;156(2):186–192 doi: 10.1016/j.ajodo.2018.08.022
19. Buzalaf MAR, Ortiz AC, Carvalho TS, et al. Saliva as a diagnostic tool for dental caries, periodontal disease and cancer: Is there a need for more biomarkers? Expert Rev Mol Diagn 2020 May;20(5):543–555 doi: 10.1080/14737159.2020.1743686. Epub 2020 Mar 30.
20. Mandel ID. The diagnostic uses of saliva. J Oral Pathol Med 1990;19(3):119–25. doi. org/10.1111/j.1600-0714.1990.tb00809.x.
21. Lundmark A, Hu YOO, Huss M, et al. Identification of salivary microbiota and its association with host inflammatory mediators in periodontitis. Front Cell Infect Microbiol 2019 Jun 21;9:216 doi: 10.3389/fcimb.2019.00216. eCollection 2019. PMCID: PMC6598052
22. Diao J, Yuan C, Tong P, et al. Potential roles of the free salivary microbiome dysbiosis in periodontal diseases. Front Cell Infect Microbiol 2021 Sep 22;11:711282 doi: 10.3389/fcimb.2021.711282. eCollection 2021. PMCID: PMC8493099
23. Sifakakis I, Papaioannou W, Papadimitriou A, et al. Salivary levels of cariogenic bacterial species during orthodontic treatment with thermoplastic aligners or fixed appliances: A prospective cohort study. Prog Orthod 2018 Aug 1;19(1):25 doi: 10.1186/s40510-018-0230-4 PMCID: PMC6068060
24. Turesky S, Gilmore ND, Glickman I. Reduced plaque formation by the chloromethyl analogue of victamine C. J Periodontol 1970 Jan;41(1):41–3 doi: 10.1902/ jop.1970.41.41.41
25. Loe H, Silness J. Periodontal disease in pregnancy. I. Prevalence and severity. Acta Odontol Scand 1963 Dec;21:533–51 doi: 10.3109/00016356309011240
26. Agnello M, Marques J, Cen L, et al. Microbiome associated with severe caries in Canadian first nations children. J Dent Res 2017 Nov;96(12):1378–1385 doi: 10.1177/0022034517718819. Epub 2017 Jul 14. PMCID: PMC5652857
27. Faul F, Erdfelder E, Lang AG, Buchner A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods 2007 May;39(2):175–91 doi: 10.3758/bf03193146
28. Faul F, Erdfelder E, Buchner A, Lang AG. Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Behav Res Methods 2009 Nov;41(4):1149–60 doi: 10.3758/BRM.41.4.1149
29. Shapiro SS, Wilk MB. An analysis of variance test for normality (complete samples). Biometrika1965;52(3/4):591–611 doi.org/10.1093/ biomet/52.3-4.591
30. Levrini L, Mangano A, Montanari P, et al. Periodontal health status in patients treated with the Invisalign system and fixed orthodontic appliances: A three months clinical and microbiological evaluation. Eur J Dent 2015 Jul–Sep;9(3):404–410 doi: 10.4103/1305-7456.163218 PMCID: PMC4569994
31. Cerroni S, Pasquantonio G, Condo R, Cerroni L. Orthodontic fixed appliance and periodontal status: An updated systematic review. Open Dent J 2018 Sep 28;12:614–622 doi: 10.2174/1745017901814010614 eCollection 2018. PMCID: PMC6182882
32. Levrini L, Abbate GM, Migliori F, et al. Assessment of the periodontal health status in patients undergoing orthodontic treatment with fixed or removable appliances. A microbiological and preliminary clinical study. Cumhuriyet Dent J 2013;16(4):296–307 doi:10.7126/cdj.2013.1974
33. Karkhanechi M, Chow D, Sipkin J, et al. Periodontal status of adult patients treated with fixed buccal appliances and removable aligners over one year of active orthodontic therapy. Angle Orthod 2013;83(1):146–51 doi: 10.2319/031212217.1. Epub 2012 Jun 22. PMCID: PMC8805524.
34. Anderson MJ, Ellingsen KE, McArdle BH. Multivariate dispersion as a measure of beta diversity. Ecol Lett 2006;9(6):683–93 doi.org/10.1111/j.14610248.2006.00926.x
35. Kanasi E, Dewhirst FE, Chalmers NI, et al. Clonal analysis of the microbiota of severe early childhood caries. Caries Res 2010;44(5):485–97 doi: 10.1159/000320158. Epub 2010 Sep 23. PMCID: PMC2975730
36. Luo YX, Sun ML, Shi PL, et al. [Research progress in the relationship between Veillonella and oral diseases]. Hua Xi Kou Qiang Yi Xue Za Zhi 2020;38(5):576–82 doi: 10.7518/hxkq.2020.05.018 PMCID: PMC7573782
37. Kamma JJ, Nakou M, Manti FA. Predominant microflora of severe, moderate and minimal periodontal lesions in young adults with rapidly progressive periodontitis. J Periodontal Res 1995 Jan;30(1):66–72 doi: 10.1111/j.1600-0765.1995. tb01254.x
38. Tanner AC, Socransky SS, Goodson JM. Microbiota of periodontal pockets losing crestal alveolar bone. J Periodontal Res 1984 May;19(3):279–91 doi: 10.1111/j.16000765.1984.tb00819.x
39. Baraniya D, Jain V, Lucarelli R, et al. Screening of healthassociated oral bacteria for anticancer properties in vitro. Front Cell Infect Microbiol 2020 Oct 6;10:575656 doi: 10.3389/fcimb.2020.575656. eCollection 2020. PMCID: PMC7573156
THE CORRESPONDING AUTHORS, Renata Lux, PhD, and Bhumika Shokeen, PhD, can be reached at rlux@dentistry. ucla.edu and bhumikas@ucla.edu.
More membership value from vendors dentists can trust.


The California Dental Association leverages the strength of our large membership to deliver more value to practices of every size. Benefit from member-exclusive pricing and export support to achieve regulatory compliance in your practice.
Explore products and services for the business side of practice at cda.org/EndorsedServices
Exclusive pricing on e-prescribing software to keep in compliance and offer patient’s convenience.
Significant savings on e-prescribing software to comply with California’s latest requirements.
Take the guesswork out of HIPAA compliance with savings on software for any sized dental practice.
Discounts on human resources solutions designed for healthcare and risk-free assessments.

Kenneth J Glenn, BS; Christina Light, BS; Todd Franke, MSW, PhD; and Shane N. White, BDentSc, MS, MA, PhD
abstract

Background: This study related childhood adversity to current health behaviors in a young adult Los Angeles dental population presenting for wisdom tooth extraction.
Methods: Routine health questions relating to smoking, alcoholism, use of street drugs and addiction to drugs were correlated to childhood adversity.
Conclusions: People who suffer from high levels of childhood adversity are known to have unfavorable adult health trajectories.
Practical implications: Interpretation of routine health behavior questions can help to identify vulnerable and at-risk adults.
Keywords: Dental patient, vulnerability, adverse childhood exposure, health behavior
Kenneth J Glenn, BS, is a dental student at the University of California, Los Angeles, School of Dentistry.
Conflict of Interest Disclosure: None reported.
Christina Light, BS, is a dental student at the University of California, Los Angeles, School of Dentistry.
Conflict of Interest Disclosure: None reported.
Todd Franke, MSW, PhD, is a professor in the department of social welfare at the University of California, Los Angeles.
Conflict of Interest Disclosure: None reported.
Shane N. White, BDentSc, MS, MA, PhD, is a professor at the University of California, Los Angeles, School of Dentistry.
Conflict of Interest Disclosure: None reported.
Early life stress exposure and experience, including socioeconomic status and harsh or chaotic or nonnutritive environments, are known to lead to vulnerability and unfavorable adult health trajectories. Stress, or cumulative allostatic load, influences neural, physiological and physical development and long-term health. Allostatic load is the concept that cumulative stress, wear and tear on physiological regulatory systems over a lifetime, may predispose to disease and other vulnerabilities.1
The effects of childhood stress or adversity may not be visible or known to health care providers. However, childhood
adversity has been linked to increased risks of infection, multiple chronic conditions and cardiovascular disease in adulthood as well as earlier death.2–5
Adverse childhood experiences are associated with negative health behaviors in adults, including excessive alcohol use.6–8 However, to date, there is little knowledge of dental patients’ health trajectories.9
Only rarely has attention been directed to the impact of adverse childhood experience on oral health in adult life.10,11 However, associations have been found between childhood adversity and inadequate dental care, caries, tooth loss, restoration placement and periodontal disease in later life.10,12–14
Exposure to childhood adversity could be an important predictive factor for poor general and dental health.10 Given the growing role that dental professionals have in identifying vulnerable individuals, as well as victims of violence, abuse and neglect, awareness of the potential for individuals to have suffered adverse childhood experiences should be raised. Additionally, the mechanisms linking childhood adversity to poor dental and systemic health should be understood.10
Successive reports from the surgeon general and the Institute of Medicine (IOM) have highlighted the connections among overall health, oral health and vulnerability.15–17 Not much has changed since 2009 when IOM President Harvey V. Fineberg, MD, PhD, enjoined: Can you imagine a time when we fully incorporate mental and dental health into our thinking about health? What is it about problems above the neck that seems to exclude them so often from policy about health care? But this is a two-way street; dentistry must also embrace the challenges of overall, mental and behavioral health.
Identifying those patients who are broadly vulnerable and/or at risk of unhealthful behaviors would allow interventions that are capable of modifying maladaptive responses to adverse childhood experiences, such as drinking and smoking and substance abuse.18 Dentists have the opportunity to identify patients who may be at risk due to unhealthful behaviors. Are such adverse trajectories evident in dental populations, and how long does it take for childhood adversity to impact adult health behaviors?
The purpose of this study was to determine if childhood exposure to adverse experiences in a Los Angeles dental population was related to current young adult tobacco, alcohol and drug behaviors.
Patients presenting for extraction of lower wisdom teeth were recruited at the UCLA School of Dentistry Oral and Maxillofacial Surgery Clinic, a convenience sample.9,19 All consenting patients requiring third molar extractions between June 2011 and September 2013 and who completed questionnaires were included, whether or not they completed wisdom tooth extraction.
This clinic has a socioeconomically diverse patient population because it provides specialty services to patients
The mechanisms linking childhood adversity to poor dental and systemic health should be understood.
covered by Medi-Cal and is located in an extremely affluent part of Los Angeles. According to patient registration data, the UCLA School of Dentistry patient population for the 2012-13 financial year was: 50% male/female; < 1% transgender; and < 1% other. For the same year, patients described their race as Asian, 10%; African American, 11%; Caucasian, 50%; Hispanic, 20%; undescribed, 5%; Native American < 1%; other, 3%; Persian, 3%; and Pacific Islander, < 1%. Spanish speakers represent a significant part of the patient pool. This population was known to have spread among childhood experiences and current young adult health behaviors, so it was amenable to the purpose of this study.9
A sample size of 131 was attained.19 Subjects were aged 18 years or older and able to provide informed consent;
most wisdom teeth are extracted from adults aged 18 and older. Some selection biases may have occurred.
Institutional Review Board approval was obtained (UCLA IRB #10-001874). Subjects were recruited using a posted flyer; interested patients contacted the clinic receptionist. Next, recruiters used a short eligibility screening, according to a standardized script, to determine eligibility. Finally, completion of informed consent occurred in a private room. Subjects were given a $20 gift card upon consent, whether or not they completed the questionnaire or treatment.
In order to ensure absolute patient confidentiality, no personal identifiers were collected, so the questionnaires could never be related to an individual participant even if subpoenaed. The questionnaires were catalogued by unique random bar codes.
Questionnaires were used to identify and quantify childhood stressors. The questionnaire first directed subjects to the period of ages 8-11 years during their childhood and included questions adapted to these years. Five questions were used to create an overall composite index of childhood adversity on a scale that ranged from 0 to 37. The questions used were previously established for such purposes; they rated emotional and physical abuse, parental disharmony; parental educational attainment, childhood financial comparison and childhood parental income.20–22 The questions were derived from those developed in the ACE Study, a collaboration between Kaiser Permanente’s Health Appraisal Center (HAC) in San Diego and the U.S. Centers for Disease Control and Prevention, designed to assess the impact of numerous, interrelated, adverse childhood experiences on a wide variety of health behaviors and outcomes and on health care utilization.23 These questions have repeatedly demonstrated a strong, graded, dose-response relationship
TABLE 1
Correlations Between Childhood Adversity Index and Young Adult Health Behaviors
Correlation coefficient p value
Do you smoke? 0.46 0.000
Have you ever considered yourself an alcoholic? 0.45 0.000
Have you ever used street drugs? 0.41 0.000
Have you ever been addicted to drugs?
TABLE 2
0.22 0.01
Coefficient Standard error t p value
Do you smoke?
Have you ever considered yourself an alcoholic?
Have you ever used street drugs?
Have you ever been addicted to drugs?
3.39 1.13 2,99 0.004
5.68 1.97 2,89 0.005
4.02 1.63 2.47 0.015
1.78 1.68 1.06 0.293
to numerous health and social outcomes.24
Four routine questions from the standard UCLA School of Dentistry Health Questionnaire were used to measure current young adult health behaviors related to smoking, alcohol and drug use. These were: Do you smoke? Have you ever considered yourself an alcoholic? Have you ever used street drugs? and Have you ever been addicted to drugs? All four measures were dichotomous, with zero indicating “no” and one indicating “yes.”
The questionnaires were administered immediately after completion of the standard UCLA School of Dentistry Health Questionnaire, with a trained clinic staff member in attendance to assist subjects as needed, in a closed private room.
Bivariate Pearson correlations were calculated between the childhood adversity index for each of the four young adult health behavior questions. Additionally, a full multiple regression model was
used to assess the combined effect for the four young adult behavior questions as independent variables. Regression assumptions were checked including normality and heterogeneity of variance.
Correlations were found between the childhood adversity index score, describing the 8-11 age period and smoking, alcoholism, use of street drugs and addiction to drugs as young adults (TABLE 1). The correlations with smoking, alcoholism and use of street drugs were moderate; the correlation with addiction to drugs was weak. But all were highly statistically significant (TABLE 1).
Multiple regression using the four independent variables significantly predicted the childhood adversity index score, F (4,91) = 12.9. The R-squared value for this model was 0.36. In comparing the bivariate results (TABLE 1) to the full
model results (TABLE 2), three of the four independent variables remain significant in the full model. While the answer to the question “Have you ever been addicted to drugs?” was significantly correlated with the childhood adversity index in the bivariate in the model described above (TABLE 1), it was not a significant predictor in the regression analysis (TABLE 2). This is due to the fact that the other three variables in the model explained all of the variability that the question “Have you ever been addicted to drugs?” explained when alone in the bivariate model, making it a nonsignificant predictor in the presence of the other measures. This may be largely due to the relationship between having ever used street drugs and having been addicted to drugs. The observed range of scores on the childhood adversity index was 0 to 28. All three of the other independent variables seem to have a substantial impact on the change in the adversity index. For example, with a 1-point change on the response to “Have you ever considered yourself an alcoholic?” the model would predict over a 5-point change on the childhood adversity index. Likewise, a 1-point change in these measures accounted for a 4-point and 3.4-point change in the childhood adversity index with the questions “Have you ever used street drugs?” and Do you smoke?
While signs of childhood adversity may be invisible to dentists and other care providers, questions in a routine dental health questionnaire correlated with childhood adversity and predicted the adversity experienced. Responses to such questions not only tell us about current health behaviors, but the results of this study demonstrate that they also inform the care provider to the general likelihood of childhood adversity and overall negative adult health trajectories.
Given the known relationships
between childhood adversity and adult diseases, such routine questions may help to recognize the potentially vulnerable who are at heightened risk of a variety of adverse trajectories, from respiratory and cardiovascular disease to mental disease, periodontal disease and caries.
These routine health behavior questions may be a surrogate for the very personal questions needed to directly measure childhood adversity. Measuring childhood adversity is difficult because the patient may be unaware of the context of adverse childhood experiences, feel uncomfortable answering such questions, be embarrassed, afraid for themselves, protective of an abuser or scared of the legal implications of an answer. Self-report is the usual practice for identifying patients with exposure to adversity. However, the use of markers such as these health behavior questions may provide a more objective identification. Consideration by a caregiver to the broader context of questions relating to health behaviors could be useful and important.
However, it is important to remember that although the results of this study were moderately predictive of a population, they are not necessarily predictive of every individual within the population. The answers to the questions are not diagnostic of childhood adversity; instead, they suggest a significantly heightened risk of an individual having experienced childhood adversity.24
Although the impact of childhood adversity may take decades to manifest as respiratory or cardiovascular disease in middle age or late adulthood, the data in this study indicate that childhood adversity very quickly impacted young adult health behaviors, with this trajectory being manifested in less than a decade.
The correlations identified in this study were moderate. However, this should not be viewed as if childhood adversity is unimportant, but as a manifestation
of the multifactorial etiologies of smoking, alcohol and drug abuse.
Some selection bias may have occurred in that it is possible that those who were most disadvantaged as children did not or were not able to access the dental school clinic for wisdom tooth extractions.
Diseases that may appear completely unrelated, such as periodontal disease and ischemic heart disease, have been found to be similarly associated with the same indicators of allostatic load, suggesting a possible common stress pathway linking socioeconomic
appropriate oral hygiene techniques and diminished salivary flow.26 They explained that concurrent abuse of tobacco worsens dental disease and heightens the risk of developing oral cancer. Thus, identification of the alcohol-abusing patient, a cancerscreening examination, preventive dental education and use of saliva substitutes and anticaries agents are indicated. They added that special precautions must be taken when performing surgery and when prescribing or administering analgesics, antibiotics or sedative agents that are likely to have an adverse interaction with alcohol or psychiatric medications. Again, it is more than possible that disinterest in personal health may be a consequence of childhood adversity.
position to both conditions.11
In consideration of the questions relating to current health behaviors, Rossow has explained that people with drug use disorders have an elevated prevalence of oral diseases, in particular caries, periodontal disease and xerostomia.25 She adds that the other main drivers of oral diseases and their progression, poor oral hygiene, frequent sugar intake and infrequent dental visits, can be ascribed to the irregular lifestyle, fiscal disadvantages and mental health problems that often accompany drug use. However, it is possible that all these drivers of oral disease flow from childhood adversity.
In a similar vein, Friedlander et al. noted that the prevalence of dental disease in alcoholics is usually extensive because of a disinterest in performing
Holistic dental care recognizes the need to address behavioral, systemic and oral issues. To these things, we now add the need to consider allostatic load and early life adversity. The dental profession must identify, understand and support the vulnerable and guide patients to appropriate intercession by our health care partners. Dentists may not routinely probe for adverse childhood experiences or unhealthy behavior issues beyond the questions on a routine medical history form. However, the widely used routine questions “Do you smoke?” “Have you ever considered yourself an alcoholic?” and “Have you ever used street drugs?” can provide broader insight and direction to dentists than previously realized.
Recognizing, advising and referring to an appropriate caregiver are important for the success of current treatment, maintenance of oral health and overall health.
A dentist can implement the process of recognition and intervention to address health behaviors, such as reducing cigarette, alcohol or drug consumption, by including recommendation and referral in a treatment plan. This
Measuring childhood adversity is difficult because the patient may be unaware of the context.
would allow the dentist to present the change in an objective nonjudgmental manner. An awareness and expectation would be recorded, and the behavioral change would be framed in terms of the patients own presenting complaint and the overall treatment plan.
Answers to several routine health behavior questions from a dental clinic health questionnaire “Do you smoke?” “Have you ever considered yourself an alcoholic?” and “Have you ever used street drugs?” correlated with childhood adversity experienced by a group of young adult dental patients. Childhood adversity is known to be linked to a wide variety of adverse adult health trajectories. Broader interpretation of answers to routine adult health behavior questions can better inform care providers as to the possibility of patients’ vulnerability associated with childhood adversity. Dentists must identify, understand and consider vulnerabilities created by adverse childhood experiences when they provide comprehensive adult patient care. n
The authors are very grateful for support from NIH NIDA grant R21 DA031571. We are most appreciative of the efforts of all the faculty, staff and residents of the UCLA Oral and Maxillofacial Surgery Clinic in their gracious and invaluable support of this study.
1. McEwen BS, Stellar E. Stress and the individual. Mechanisms leading to disease. Arch Int Med 1993 Sep 27;153(18): 2093–2101
2. Cohen S, Doyle WJ, Turner RB, et al. Childhood socioeconomic status and host resistance to infectious illness in adulthood. Psychosom Med 2004 Jul–Aug;66(4):553–8 doi: 10.1097/01.psy.0000126200.05189.d3
3. Karlamangla AS, Singer BH, Williams DR, et al. Impact
of socioeconomic status on longitudinal accumulation of cardiovascular risk in young adults: The CARDIA Study (USA). Soc Sci Med 2005 Mar;60(5):999–1015 doi: 10.1016/j. socscimed.2004.06.056
4. Lehman BJ, Taylor SE, Kiefe CI, et al. Relation of childhood socioeconomic status and family environment to adult metabolic functioning in the CARDIA study. Psychosom Med 2005 Nov–Dec;67(6):846–54 doi: 10.1097/01. psy.0000188443.48405.eb
5. Danese A, McEwen BS. Adverse childhood experiences, allostasis, allostatic load and age-related disease. Physiol Behav 2012 Apr 12;106(1):29–39 doi: 10.1016/j. physbeh.2011.08.019. Epub 2011 Aug 25.
6. Lee RD, Chen J. Adverse childhood experiences, mental health and excessive alcohol use: Examination of race/ethnicity and sex differences. Child Abuse Negl 2017 Jul;69:40–48 doi: 10.1016/j.chiabu.2017.04.004. Epub 2017 Apr 28. PMCID: PMC5896758
7. Wiehn J, Hornberg C, Fischer F. How adverse childhood experiences relate to single and multiple health risk behaviours in German public university students: A cross-sectional analysis. BMC Public Health 2018:18(1):1005 doi.org/10.1186/ s12889-018-5926-3
8. Merrick MT, Ford DC, Ports KA, et al. Vital signs: Estimated proportion of adult health problems attributable to adverse childhood experiences and implications for prevention — 25 states, 2015–2017. Morb Mortal Wkly Rep 2019 Nov 8;68(44):999–1005 doi: 10.15585/mmwr.mm6844e1 PMCID: PMC6837472
9. Light C, Glenn KJ, Sharma R, Nguyen K, Chen H, Franke T, White SN. Vulnerability of a young adult dental population in Los Angeles. J Calif Dent Assoc 2020:48(12):689–694
10. Ford K, Brocklehurst P, Hughes K, Sharp CA, Bellis MA. Understanding the association between self-reported poor oral health and exposure to adverse childhood experiences: A retrospective study. BMC Oral Health 2020 Feb 14;20(1):51 doi: 10.1186/s12903-020-1028-6 PMCID: PMC7020341
11. Boyce WT. The lifelong effects of early childhood adversity and toxic stress. Pediatr Dent 2012 Jan;129(1):e232–46 doi: 10.1542/peds.2011-2663. Epub 2011 Dec 26.
12. Sabbah W, Watt RG, Sheiham A, Tsakos G. Effects of allostatic load on the social gradient in ischaemic heart disease and periodontal disease: Evidence from the Third National Health and Nutrition Examination Survey. J Epidemiol Community Health 2008 May;62(5):415–20 doi: 10.1136/ jech.2007.064188
13. Bright MA, Alford SM, Hinojosa MS, et al. Adverse childhood experiences and dental health in children and adolescents. Community Dent Oral Epidemiol 2015 Jun;43(3):193–9 doi: 10.1111/cdoe.12137. Epub 2014 Nov 21
14. Crouch E, Radcliff E, Nelson J, et al. The experience of adverse childhood experiences and dental care in childhood. Community Dent Oral Epidemiol 2018 Oct;46(5):442–448 doi: 10.1111/cdoe.12389. Epub 2018 Jun 6.
15. U.S. Department of Health and Human Services. Oral Health in America : A Report of the Surgeon General. Rockville, Md.: U.S. Department of Health and Human Services, National Institute of Dental and Craniofacial Research, National Institutes of Health; 2000.
16. Institute of Medicine. Advancing Oral Health in America Washington, D.C.: The National Academies Press; 2011.
17. Institute of Medicine and National Research Council. Improving access to oral health care for vulnerable and underserved populations. Washington, D.C.: The National Academies Press; 2011.
18. Chandler GE, Roberts SJ, Chiodo L. Resilience intervention for young adults with adverse childhood experiences. J Am Psychiatr Nurses Assoc 2015 Nov-Dec;21(6):406–16 doi: 10.1177/1078390315620609
19. Sharma R, Lohiya S, Rajabi P, et al. Prevalence of enamel markings on third molars. J Calif Dent Assoc 2016 Aug;44(8):499–505
20. Dube SR, Felitti VJ, Dong M, et al. Childhood abuse, neglect, and household dysfunction and the risk of illicit drug use: The adverse childhood experiences study. Pediatrics 2003 Mar;111(3):564–72. doi: 10.1542/peds.111.3.564.
21. Felitti VJ, Anda RF, Nordenberg D, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. Am J Prev Med 1998 May;14(4):245–58 doi: 10.1016/s0749-3797(98)00017-8
22. Kuh D, Mishra GD, Black S, et al. Offspring birth weight, gestational age and maternal characteristics in relation to glucose status at age 53 years: Evidence from a national birth cohort. Diabet Med 2008 May;25(5):530–5 doi: 10.1111/j.1464-5491.2008.02427.x PMCID: PMC3399089
23. Anda RF, Felitti VJ, Bremner JD, Walker JD, Whitfield C, Perry BD, Dube SR, Giles WH. The enduring effects of abuse and related adverse experiences in childhood. A convergence of evidence from neurobiology and epidemiology. Eur Arch Psychiatry Clin Neurosci 2006 Apr;256(3):174–86 doi: 10.1007/s00406-005-0624-4. Epub 2005 Nov 29. PMCID: PMC3232061
24. Anda RF, Porter LE, Brown DW. Inside the Adverse Childhood Experience Score: Strengths, Limitations, and Misapplications. Am J Prev Med 2020 Aug;59(2):293–295 doi: 10.1016/j.amepre.2020.01.009. Epub 2020 Mar 25.
25. Rossow I. Illicit drug use and oral health. Addiction 2021:116(11):3235–3242 doi: 10.1111/add.15360. Epub 2021 Jan 15.
26. Friedlander AH, Marder SR, Pisegna JR, Yagiela
JA. Alcohol abuse and dependence: psychopathology, medical management and dental implications. J Am Dent Assoc 2003 Jun;134(6):731–40 doi: 10.14219/jada. archive.2003.0260 PMCID: PMC6736549
THE CORRESPONDING AUTHOR, Shane N. White, BDentSc, MS, MA, PhD, can be reached at snwhite@dentistry.ucla.edu.
As a CDA member, you have access to a full library of helpful resources for employers, plus the expertise of dedicated Practice Support analysts.
Better understand training requirements, paid sick leave, wage and hour laws, notices and more. And save time with our custom employee manual generator.
Explore your CDA member resources at cda.org/EmploymentPractices.
Dental Benefit Plans Employment Practices Regulatory Compliance Practice Management


There is a great deal of satisfaction in seeing dramatic “before” and “after” images, and even more so when your efforts are responsible for positive change. The ability to create transformative improvements in oral health and appearance is frequently cited by dentists and orthodontists as the most satisfying aspect of their profession.
While many patients are just as pleased with their treatment outcomes as their provider is, occasionally there are patients who claim that the reconstructive work did not meet their expectations. Through thoughtful communication, dentists have opportunities to mitigate patient complaints and manage expectations for increased patient satisfaction.


The Dentists Insurance Company (TDIC) Risk Management Advice Line, which provides guidance to TDIC policyholders and dental association members, regularly receives calls regarding patients who have expressed dissatisfaction with the outcomes of their reconstructive treatments. The following case study illustrates how TDIC’s Risk Management analysts have advised callers to respond.
A dentist called the Advice Line with questions about how to manage a dissatisfied patient. After the dentist had completed Invisalign treatment, the adult patient insisted that the result was not representative of the outcome promised by the dentist.
The patient demanded that the dentist retreat the case at no charge. The dentist explained that it was unnecessary to spend
additional time and money to retreat the case when the outcome was both clinically acceptable and represented the original desired outcome expressed by the patient.

During the Advice Line call, the dentist shared their perspective that the patient’s expectations had changed over the course of treatment and became more specific regarding desired tooth rotation and position. The dentist sought advice on how to best communicate with the
patient. How could the dentist illustrate that the patient’s desired result changed over the course of treatment as well as explain that her expectations simply could not be clinically achieved with the original treatment plan? The result the patient desired would involve changing the size and shape of her natural teeth, but she refused to consider cosmetic options such as veneers.
The Risk Management analystrecommended that the dentist perform a review of the patient’s chart, assessing the documentation on file including a signed consent for treatment, the treatment plan and the stated potential outcome. These records should substantiate the dentist’s claim that the patient had been fully informed of the original treatment plan and had consented to treatment for the stated outcome.
The analyst also advised the dentist to suggest the patient seek a second opinion, including a report from the consulting provider. If another orthodontist expressed an opinion that was not in agreement with the treating dentist’s plan, then the dentist should reach out again to the Advice Line to discuss options for optimally managing the situation.
If the patient refused to seek a second opinion, then the dentist could choose to inform the patient that they were respectfully declining to retreat the case. The analyst agreed that despite the patients’ insistence that the result could and should be improved, the dentist should oversee the treatment and not be influenced by the patient’s statements. However, the dentist should still review the chart and be prepared to defend the case if the patient decided to take further action. Again, the Advice Line analyst offered to assist the dentist further if that occurred.
TDIC’s experts point to poor communication being the greatest cause of litigation, not poor dentistry. Complaints are best addressed and resolved when effective communication tools have been utilized before, during and after treatment through appropriate case selection, detailed treatment planning and thoughtful handling of crucial conversations.
Careful case selection is one of the most important aspects to consider when it comes to protecting against potential
risk. Barring discrimination, dentists are not obligated to accept all patients into their practices. It’s imperative to educate patients during the selection process by using pamphlets and before and after photos. Not every procedure is right for every patient; explaining that in a compassionate manner may be necessary.
Those cases you do select to treat should be with patients with whom you can form productive, healthy provider-patient relationships. The scope of treatment required should not
criticism of former dentists.
n Long, complex dental history with multiple providers.
n Inability to receive or convey constructive feedback.
n Requests for specific prescriptions.
n Overly rigid treatment controls and restrictions or citing research that is clinically unsupported.
n Unrealistic time or treatment expectations.
n Providing photos of celebrity’s or model’s smiles (or their own from years ago) that are unachievable outcomes.
Along with evaluating the patient’s personality, demeanor and treatment expectations, dentists should carefully consider what is an achievable outcome for each individual. In general, reconstructive results are affected by jaw size, musculature, variable biological responses and patient compliance. Share the most realistic potential outcome with the patient based upon known barriers to treatment.
exceed that which you can successfully, effectively and safely provide.
“We try to look at every possible angle when it comes to patient interactions, and a lot of issues can be traced back to patient selection,” said Taiba Solaiman, one of TDIC ‘s senior risk management analysts. “Patient demeanor is important information in patient selection.” Solaiman says dentists often have an uneasy feeling about certain patients but may put their instincts aside in favor of potential income or simply trying to make patients happy.
Take time to get to know potential patients and learn more about their motivation for seeking care. Some “red flags” that should indicate caution when accepting a patient for reconstructive treatment include:
n Excessive complaining or
Providing detailed treatment plans that outline the options discussed, the risks and the associated costs can help prevent miscommunication between patient and provider about anticipated outcomes. Communicate the scope and limitation of treatment to patients before reconstruction begins. This is most effectively documented when patients are given detailed treatment plans with copies included in the patient’s chart.
Additional documentation associated with the treatment plan should include the patient’s signed acknowledgment of their receipt and understanding of the plan and their consent for treatment. Include pretreatment records such as photos, study models and diagnostic wax-ups. If the treatment plan changes
Communicate the scope and limitation of treatment to patients before reconstruction begins.
course midtreatment, a revised treatment plan should be printed and signed by the patient before proceeding.
Despite your best efforts to offer patients realistic treatment outcomes and detailed treatment plans, some patients will still be dissatisfied. Whether or not you feel a patient’s complaint is reasonable or has merit, taking the time to listen and respond in a meaningful way is a personal touch that takes only a few minutes, but can make a world of difference.
Risk management analysts emphasize that a process of listening to and recognizing complaints does not mean that dentists are admitting liability. It is common for dentists to mistakenly believe that acknowledgement of a complaint equals agreement and therefore validates a patient’s claim. In actuality, documentation that a dentist responded to the patient’s complaint reflects that the dentist was responsive to the patient and viewed their concerns seriously.
Often these matters arise when a patient believes they didn’t receive adequate information about their treatment such as warnings about potential risks or other treatment options. Expressing concern for their frustration and attempting to address those specifics helps diminish the damage with both the patient and any source of resolution, such as the dental board. Also, referencing back to your treatment notes and informed consent forms that the patient signed can demonstrate the thoroughness of your
efforts to educate the patient. In the event of a claim, this will demonstrate to anyone who reviews the case that the patient was listened to and treated with respect, rather than ignored or dismissed.
TDIC experts offer these guidelines for handling patient complaints:
n Discussions about patients’ clinical concerns should not be left to staff. If the complaint is made via phone or email, the treating dentist should extend an invitation or make time for a face-to-face meeting with the patient as soon as possible to address the patient’s concerns.
n When meeting to discuss a patient complaint, active listening helps the patient feel respected. Practice active listening by avoiding distractions, establishing eye contact with the patient and adding comments that elicit additional information.
n Demonstrate comprehension by paraphrasing concerns in your own words. Restate what you understand the patient’s complaint to be. Avoid the tendency to include evaluations of what the patient is telling you.
n Provide education. Help patients understand the scope and feasible outcomes with educational tools such as pamphlets, models and other resources.
n Carefully document all the patient’s concerns and how they were addressed. TDIC recognizes that when faced with an unhappy patient, these conversations can be difficult and often come down to
thoughtful and considerate responses that avoid escalation of the matter.
TDIC’s current online seminar offers policyholders the opportunity to enhance communication and documentation skills to assist dentists with these difficult conversations.
Take time to review the patient’s case thoroughly before offering resolutions to the complaint. If necessary, explain to the patient that you need time to review and give a specific timeframe when you will be prepared to address their concern (for example, 48 hours).
Fortunately, most patients will be thrilled by their new smile and the likelihood of a dissatisfied patient can be mitigated through considerate patient selection, detailed treatment plans and documentation. When complaints do arise, take time to listen and respectfully consider the patient’s concerns. TDIC’s Risk Management analysts are available to help through the Risk Management Advice Line and can provide resources and suggestions on how to best resolve patient complaints.
The Dentists Insurance Company’s Risk Management Advice Line is a benefit available at no cost to CDA members, as well as to policyholders protected by TDIC. To schedule a consultation, visit tdicinsurance.com/RMconsult or call 877.269.8844.
BRENTWOOD: 4 Ops, professionally designed, Dentrix, Paperless, Laser, great location 2019 GR $520K on 2 5 day week #CA3008
CENTRAL VALLEY / MODESTO
AREA: GP, 8 Ops, 20+ Yrs Goodwill, Digital, 4 hyg days/wk Hi traffic area! 2021 GR $999K #2721
DANVILLE: 4 Ops+RE , Desirable location, 80 Yrs. Goodwill, Digital, with 5 ½ hyg days/wk 2021 GR $1 3M #3203
ELK GROVE / S. SACRAMENTO
AREA: 4 Op Ortho Practice, 21+ Yrs Goodwill, Digital, Highly Desirable Area! 2021 GR $724K #CA3250

FAIRFIELD AREA: High traffic area, 7 Ops Digital, Pano/CB, 23+ NP/ mo with 8+ Hyg. days/wk. Room to grow with specialties 2019 GR $1 7M and 2021. #CA1824
FAIRFIELD/VALLEJO AREA: 7 Ops, Paperless practice in a high traffic area. Digital, CEREC with 43 yrs Goodwill 2021 GR $1 5M. #3117
GREATER MODESTO AREA: New Listing! 7 Ops, Seller has 15 yrs. Goodwill, Seller open to working back, Digital, Desirable Area! 2021 GR $614K #3286
LAKE TAHOE AREA: 4 Ops, 37+ yrs Goodwill Rural lifestyle GP in growing resort community 2019 GR $760K #CA1715
LAKE TAHOE AREA WITH LAKE VIEWS: Well-established practice in magical Lake Tahoe! 4 Ops, Paperless practice, Digital 20 yrs Goodwill, 2021 GR $1 4M. #3100
NORTHERN CALIFORNIA PERIO: 4 Ops+RE, 33 yrs Goodwill 2021 GR $1 4M #3118
PLEASANTON: Great neighborhood, paperless, digital, 6 Ops, 5 equipped. Don’t miss opportunity in this great community. #CA3023
RED BLUFF/CORNING/ORLAND AREA: 6 Ops, 8 hyg days/wk w/ room to grow! 33+ yrs Goodwill, Paperless, Digital 2021 GR $826K RE for sale with practice #CA3161

ROCKLIN/GRANITE BAY: Hi end 4 Ops GP/Cosmetic practice in affluent area Paperless, digital, iTero scanner, 8+ hyg. Days/wk. 2019 GR $1.6M+, 2021 Prod projected at $2M+. RE for sale with practice #CA2793
ROSEVILLE/CITRUS HTS: 4 Ops with 18 yrs Goodwill, Digital, Laser, Strong hyg , Specialties Referred, 2021 est GR $775K #CA2897
SAN MATEO: 3 Ops, digital X-ray, great opportunity in this highly desirable area/busy retail strip center location. 2021 GR $381K with no advertising. #CA3044
SANTA CLARA COUNTY-WEST VALLEY: 5 Op OMS Practice, Affluent Area with room to Grow! 2021 GR $579K. #CA3239

SONOMA COUNTY: Price Adjustment! Large GP, 2019 GR $2.3M +. Stand-alone 3,000 sf prime Real Estate, 72 NP/mo. & 10 Hyg Days. 6 Ops, Pano, Dexis, Cameras, Laser, Dentrix. Both Business & RE for sale or Lease. Doctor Retiring. #CA544
SONOMA COUNTY: 4 Ops in spacious layout in heart of the area off main highway. Est 22 yrs with 5-star Google reviews, Paperless with CEREC, Scope, Laser, Strong hyg. Retiring seller. 2019 GR $782K with good post-COVID recovery. #CA2594
SONOMA COUNTY: 4 Ops, FFS GP Practice, 27 yrs Goodwill, 8 hyg days/ wk, Digital, Paperless, Eco-Friendly and Energy Efficient Solar Panels. 2021 GR $1.6M. #CA3165
S. SACRAMENTO/POCKET ROAD/ELK GROVE AREA: 5 Ops, Paperless, Digital X-ray, Soft Tissue Lase, Pano X-ray, CEREC. 73 yrs. Goodwill. 2021 GR $803K. #CA3093
S. SACRAMENTO METRO: 5 Ops Open Bay Chair, Ortho Specialty Practice, 10+ Yrs. Goodwill, Digital, Highly Desirable Area! 2021 GR $404K. #CA3149
GREATER MODESTO: 7 Ops, Desirable area, Dentrix, Digital, Laser, Digital Pano. RE for sale w/practice. Not a Delta Premier provider. 2020 GR $615K and 2021 should exceed it. #CA2795
SANTA CRUZ: 4 Ops, Minutes to beach! Digital, CEREC, Pano, CBCT. Bread and butter practice-room to grow with specialties. FFS and Delta PPO only. #CA2938
AGOURA HILLS/WESTLAKE VILLAGE/THOUSAND OAKS:
4 Ops plus 1 plumbed not equipped. 18 yrs. Goodwill. 2021 GR $1.1M. #3085
BAKERSFIELD: 7 Ops, 38 yrs Goodwill, Digital, RE or sale, Fee for Service, PPO, Delta Premier. 2021 GR $732K. #CA2945
CENTRAL VALLEY: Pediatric Practice. 10 chairs, Ortho and Oral Surgery services in-house. Digital Xray, Digital Pan/Ceph. 30+ yrs. Goodwill. Seller available to stay for transition. 2021 GR $2M. #2794
CENTRAL COAST: GP, 8 Ops, Digital, Paperless, 5 hyg days/wk. 2021 GR $2.4M. #3157
COASTAL ORANGE COUNTY: 5 Ops, 4 equipped, digital sensors & pano. Room to grow, in a wellestablished area. GR $735K. #CA2787
COASTAL ORANGE COUNTY: New Listing! 8 Ops, GP, 18 Yrs. Goodwill, Digital X-ray, Desirable Location, Seller Retiring! 2021 GR $881K. #3275


HESPERIA: Well-established GP practice, 5 Ops+RE, Digital, 22 Yrs. Goodwill. 2021 GR $500K. #1500



NORTH ORANGE COUNTY: 4 Ops, 30+ Yrs. Goodwill, Digital, Paperless, 3.25 hyg days/wk. 2021 GR $1M. #3262 ORANGE: 4 Ops+RE, 2 hygiene days/ wk. with room to add more days. Seller refers out all specialties. 2021 GR $590K. #3143

RANCHO SANTA MARGARITA: 4 Ops, 30+ yrs Goodwill, Modern and Bright Designed Office! Digital Laser, Pano, Strong hyg 2021 GR $665K. #CA3160
SAN BERNARDINO: 6 Ops, established 33 yrs, Cash, HMO, DentiCal. Busy area w/ parking. 2021 GR $960K+. Seller offering RE for sale w/ 2 lease tenants adjacent to practice. Room to expand with spec. #CA2843
SOUTH ORANGE COUNTY: 6 Ops, 25+ yrs. Goodwill, Digital, PPO/FFS Only, 5 hyg. days/wk. 2021 GR $1M. #CA3095

TORRANCE: 6 Ops, 40 yrs. Goodwill. Strong hygiene, in-house Perio and Endo specialists 2 days per month. Digital Xray, Intraoral Camera and Laser. 2021 GR $1.5M #CA3113
WHITTIER: 4 plumbed Ops, 3 equipped, Paperless, Digital X-ray, Intraoral Camera and Laser. Longestablished FFS/PPO Practice. 2021 GR $497K. #3150

CHULA VISTA: New Listing! 6 Ops +RE, GP, 52 Yrs. Goodwill, 4.5 Hyg. Per Wk., 44% FFS, 56%PPO, Room for Growth! 2021 GR $545K. #3195
ENCINITAS: GP practice. 6 Ops, Private parking lot. Great technology with a CBCT, 5 Microscopes, Scan X and SoftDent. 38 yrs. Goodwill. 2021 GR $960K. #CA3152
ESCONDIDO DENTAL REAL ESTATE: Stand alone building with 5 fully equipped Ops, 2 with brand-new equipment. On corner lot with private parking and spacious floor plan. #CA3031
LA JOLLA: 5 Ops, Well-established GP Practice, 35 Yrs. Goodwill, 9 Hygiene days per week, Digital, Soft Tissue Laser. 2021 GR $816K. #CA3190
OCEANSIDE: GP practice blocks from the beach! 40 yrs Goodwill, 7 ops, 4 equipped. 2021 GR $691K. #3151
SAN DIEGO: 6 Ops, 4 equipped, recently updated, Digital Pan, Microscopes, and Laser. Specialties referred, room for additional hours and dentistry. #CA3005
SAN DIEGO: Oral Surgery practice with 2 surgical rooms, 2 consult rooms in a standalone building. 46 yrs. Goodwill. 2021 GR $413K. #3115
SAN DIEGO: 4 Op Open Bay w/3 private Ops, Emergency Sale Pediatric Practice, 19 + Yrs. Goodwill, Digital. 2021 GR $1M. #CA3140
SAN DIEGO: CHART ONLY SALE! Seller retiring, 30 yrs Goodwill, 400 patients seen in the last 18 months. 50% Cash, 50% PPO, No Delta Premier #CA3188
SCRIPPS RANCH: 5 Ops, 3 equipped, strip mall location, bright, spacious office. CEREC, CBCT, Dexis, Soft tissue Laser, Implant Motor, I/O Camera. Specialties referred. #CA3054

Every health care provider in California should be aware of the procedures to provide notification to the affected parties of a patient information breach. The state data breach law applies to most businesses and government agencies and is applicable to certain types of electronic information. The HIPAA breach notification rule applies to covered entities and is applicable to “protected health information” in all formats. Although many health care providers have cyber liability insurance coverage that will assist in carrying out required notifications, providers should understand their obligations.

The state breach law requires notification when certain categories of unencrypted electronic information are accessed impermissibly. The information includes an individual’s first and last name, or first initial and last name, in combination with any of the following:
n Social Security number.
n Driver’s license number or California identification card number.
n Account number, credit/debit card number, in combination with any required security code, access code or password that would allow access to the person’s financial account.
n Medical information, defined as “any information regarding an individual’s medical history, mental or physical condition or medical treatment or diagnosis by a health care professional.”
n Health insurance information, defined as “an individual’s health insurance policy number or subscriber identification number, any unique identifier used by a health insurer to identify the individual or any information in an individual’s application and claims history, including any appeals records.”
n A username or email address in
combination with a password or security question and answer that would permit access to an online account.

n Information or data collected through the use or operation of an automated license plate recognition system.
The HIPAA breach notification rule applies to “protected health information”
in all forms — electronic, oral and hard copy. Personal health information (PHI) is individually identifiable health information held or transmitted by a covered entity or its business associate. HIPAA does not cover employee or education health records, as those are covered by different laws.
Any impermissible disclosure or use of PHI is automatically assumed to be a breach. HIPAA requires breach notification unless a covered entity determines the impermissible use or disclosure is either one of four allowable exceptions or there is a low probability the PHI was compromised after the covered entity performs a breach risk assessment. The four allowable exceptions are:
1. The unintentional acquisition, access, use or disclosure of PHI by a staff member or a business associate acting in good faith and with the scope of their job responsibility as long as the breach does not result in further impermissible use or disclosure.
2. The inadvertent disclosure of PHI to another person who is authorized to access PHI at the same business.
3. The covered entity determines that the unauthorized individual who received the PHI is unable to retain it.
4. Low probability that the PHI in question was compromised. Such a determination must be documented in conjunction with the logging of the impermissible use or disclosure. The finding of low risk of compromise also must be documented when a covered entity performs a breach risk assessment. The assessment must consider the following when determining whether PHI was compromised:
n Nature and extent of patient information involved.
n Who received/accessed the information.
n Potential that patient information was acquired or viewed.
n Extent to which risk to the data has been mitigated.
A three-point scale (high, medium, low) for each consideration can be used to assess overall risk. If a covered entity determines the risk of compromise is low, then the risk assessment must be documented. HIPAA documentation must be retained for at least six years from the incident date or, if it is a policy or procedure, the last effective date. Documentation of a breach risk assessment is not required if the covered entity proceeds with notifying the affected individuals.
Examples of impermissible uses and disclosures of PHI on which a HIPAA privacy officer may want to conduct a breach risk assessment include:
n Staff leaving a detailed message for a patient with someone the patient did not authorize to receive such information.
n Ransomware.
n Paper charts found in a dumpster or possessed by an unauthorized individual.
The state breach law requires data breach notification immediately following the discovery of the breach and can be provided by written or electronic notice. In the case of a breach of a username or email address in combination with a password or security question answer, electronic notification shall not be sent to an email address that was subject to the breach.
HIPAA-covered entities must provide notification “without unreasonable delay” and in no case later than 60 days after the breach is
discovered. If a business associate discovers the breach, the 60-day count starts on the day the business associate discovered it even if the business associate delays informing the covered entity.
Both state law and HIPAA require specific content for the notification. California also specifies the format of the notification, requiring the use of headers. If a business offers credit monitoring to affected individuals, the state requires that it be offered free of charge and for a duration of not less than 12 months.
If 500 or more individuals are affected, non-HIPAA-covered entities must notify the state attorney general’s office. HIPAA-covered entities must notify the U.S. Department of Health and Human Services and prominent local media outlets within 60 days of breach discovery. If fewer than 500 individuals are affected, a HIPAAcovered entity must notify HHS of the breach no later than 60 days into the following year (March 1 in non-leap years).
A breach notification checklist and sample notification letter are available in the Practice Support section of cda.org. n
Regulatory Compliance appears monthly and features resources about laws that impact dental practices. Visit cda.org/practicesupport for more than 600 practice support resources, including practice management, employment practices, dental benefit plans and regulatory compliance.
®

SIMPLY BRILLIANT.
SAVE THE DATE Connect with us California Dental Association


(Starts at $10/month, no charge to consumer, Corowell)
A major contributor in the fight against the pandemic is the ability to test for COVID-19. Test availability, accuracy, speed and ease of use are factors in evaluating which tests are appropriate to use. Throughout the pandemic, people have become familiar with either rapid antigen or PCR testing. Rapid antigen tests are popular because they can be performed at home with results typically available in 15 minutes but require an uncomfortable nasal swab. Corowell is a different type of test that utilizes a symptom screening app and “scratch and sniff” smell identification to determine in as little as 60 seconds if someone is infected with COVID-19. Corowell is U.S. Food and Drug Administration (FDA) approved as a COVID-19 symptom screening test. The test comes in a sealed packet the size of a standard index card. Patients download the Corowell app, enter their personal information including applicable health insurance details, open the test and scan the unique QR code on the card inside. After answering a series of symptom screening questions, patients are directed to “scratch and sniff” an area on the card to identify the scent. The identification is followed up with a question asking patients to rate their confidence in determining the scent. The app then takes the answers and applies machine learning from its global database of responses to determine whether the patient is infected with COVID-19. Patients who pass the test receive an “all clear” result that can be added to their Apple or Google Wallet. Patients who fail the test are encouraged to obtain further testing to rule out a COVID-19 infection. Each test contains a randomized scent, and its proper identification alone does not lead to a definitive diagnosis. Clinical data from the manufacturer has shown the test has a 90% sensitivity, 96% specificity and can detect COVID-19 as early as three days postinfection. The test is noninvasive, quick, easy and can be used anytime and anywhere. There are no out-of-pocket costs for patients, as the manufacturer bills insurance companies directly for testing.
Keeping offices and organizations healthy and safe from COVID-19 is important in helping to bring the pandemic to an end. The availability of faster and easier methods to test patients, providers and staff can lead to greater compliance and acceptance. With its unique
“scratch and sniff” method, Corowell has the potential to be the preferred method to efficiently screen individuals for COVID-19.
Tech Pack 2 ($210, Aer Designs LLC)
As travel and in-person work ramps up, people will need to (once again) haul their gear from one location to another. Whether it’s a consultant presenting at meetings or a dental specialist going to a general practitioner’s office, having a protective and comfortable backpack is essential for those on the move. Aer, a San Franciscobased company started in 2014 as a crowdfunding project that aimed to combine a gym and office bag into one design, specializes in creating minimalist, durable and functional travel gear. It’s latest offering, the Tech Pack 2, is billed as the “ultimate tech backpack.”
The Tech Pack 2 certainly lives up to Aer’s goals of minimalistic design. With a 17 L capacity, it is considered a medium to large bag and is twice the weight of many other competitors at 3.8 pounds. This all-black backpack hides nearly all of its features thanks to its waterproof, carbonate polyurethane face and YKK AquaGuard zippers, and it has a plethora of features. The Tech Pack 2 has three main compartments: a padded pouch for everyday items, two-side pouches and two handles. The Tech Pack 2 can comfortably and safely hold two 15-inch laptops, two tablets, all the peripherals for each device (e.g., power supplies, mouse, cables, connectors, etc.) and everyday items like a water bottle, pens and sunglasses. The padded, nylon straps are comfortable, and its structured design allows it to stand upright without falling over. Over the course of two cross-country flights, the Tech Pack 2 was a stalwart that held everything securely, fit in the smallest of airplane spaces and remained comfortable … albeit on the heavy side. For users who travel regularly with lots of gear, the Tech Pack 2 is an excellent choice, but most would be better served with a smaller, lighter backpack.
— Alexander Lee, DMD