





Illustrations by Nathan Hackett
4 TIPPING THE SCALE IN FAVOR OF CHILDREN’S HEALTH
Allen Sánchez
11 MODERN MEDICINE, TIME-HONORED PRACTICES: A PERSONAL AND PROFESSIONAL JOURNEY IN PEDIATRIC INTEGRATIVE MEDICINE
Anu French, MD, FAAP, ABoIM
18 HELPING TEENS TO NAVIGATE STRESS
Elena Mikalsen, PhD, ABPP
21 DEBUNKING ONLINE INFORMATION TO KEEP TEENS SAFE
Kelly Bilodeau
27 PREVENTING TEEN SUICIDE: TAKING MEASURES TO ENSURE AN ATTEMPT NEVER OCCURS
Cecelia Horan, PsyD, and Rick Germann, MA, LCPC
31 ADVOCATES FOR AT-RISK STUDENTS EASE THE TRANSITION BACK TO SCHOOL
Amy Onofre, PhD, LPC
36 FINDING THE RIGHT FIT: PROGRAMS FOSTER STUDENT INTEREST IN HEALTH CARE, DIVERSIFY FUTURE WORKFORCE
Robin Roenker
44 REFLECTION: BUILDING A PLAYBOOK FOR LIFE TO INSPIRE JOY, OVERCOME CHALLENGES
Sr. Lisa Maurer, OSB
48 PROGRAMMING TO PAIR YOUNGER AND OLDER GENERATIONS BRINGS MEANINGFUL CONNECTIONS
David Lewellen
53 AUTISM, NEURODIVERGENCE AND TRANSITIONING TO ADULTHOOD: THE NEED FOR SUPPORTED DECISION-MAKING AND SUPPORTED ENGAGEMENT
Nanette Elster, JD, MPH, and Kayhan Parsi, JD, PhD, HEC-C
2 EDITOR’S NOTE CHARLOTTE KELLEY
57 COMMUNITY BENEFIT Flourishing Children Benefit All of Us — For Generations To Come ALEXANDER GARZA, MD, MPH
60 FORMATION
Hope Is Not a Strategy. Or Is It? DARREN M. HENSON, PhD, STL
63 ETHICS
Stumbling Stones: History at Our Feet to Honor Humanity, Confront the Past BRIAN M. KANE, PhD
66 THINKING GLOBALLY
Opening Our Ears and Welcoming In Bold Change — Staying In by Leaning Out BRUCE COMPTON and HEATHER BUESSELER, MPH
69 MISSION
Why You Need a Chaplain on Your Personal Board of Directors JILL FISK, MATM
35 FINDING GOD IN DAILY LIFE
72 PRAYER SERVICE

IN YOUR NEXT ISSUE FAITH AND MEDICINE
As a child, whenever Christmas drew near, I looked forward to watching A Charlie Brown Christmas on TV. In the holiday special, Charlie Brown is feeling down despite the Christmas season and bemoans its commercialism.

To lift his spirits, Charlie goes with his friend Linus to look for a tree for the school’s Christmas play. However, the small tree he selects doesn’t go over well with the other kids, who are all looking forward to a great big, shiny aluminum tree.
“I’ll show them,” Charlie says, bringing the little tree home to fix it up into something grand. But his attempts fail, and his little tree sags to the ground from just one ornament. “Everything I touch gets ruined,” he says, and walks away.
But Linus approaches the sad tree, and says, “I never thought it was such a bad little tree. … Maybe it just needs a little love.” He then takes his blanket and lovingly wraps it around the bottom of the tree, perking the sapling right up. The other kids follow suit, decorate the tree and within seconds, a glorious, thriving tree takes shape.
And that’s all it took: just one person who believed in that little tree to start the chain to bring it fully to life.
In this issue of Health Progress, themed on Helping Youth Thrive, I encountered stories throughout Catholic health care and community partners about how just one mentor or advocate in a young person’s life, someone who believes in them and their potential, can help them flourish.
In her article about the Community Advocacy Project for Students in Lubbock, Texas, Amy Onofre, the program’s director, explains how the initiative pairs advocates with at-risk students at their schools to help kids set goals and navigate academic and life struggles, letting them know their voices matter. In another article, Sr. Lisa Maurer, OSB, director of mission integration and formation for Duluth Benedictine Ministries, who also
serves as an assistant football coach at the College of St. Scholastica in Minnesota, talks about the importance of having a value-laden playbook for life, especially when working with young people. Having one, she notes, can encourage youth to think about the values most important to them so they can confidently make decisions.
In another story about career training and job shadowing in Catholic health care for middle and high school students, we learn how experiencing just one day imagining themselves as health care professionals can transform a child’s dreams. When asked if he had known what a physician assistant was before spending a day with one particular program, a student answers, “No, but I’m going to do it.”
Also, thriving doesn’t stop when we get older, it only continues, as evidenced by writer David Lewellen’s article about intergenerational programs to pair younger and older people together. Whether by connecting generations through housing, art collaborations or in children’s classrooms, both younger and older participants gain social connection and meaning in their lives. “We give them power; they give us power,” says one older resident about the young children she encounters daily in her intergenerational living facility.
Even as I started planning this issue, Health Progress Editor Betsy Taylor began an academic leave to pursue professional development. Her endeavor is just another example of how we continue to flourish in all stages of life.
So, as some of you may start to see your own Christmas trees close in on their final days in the New Year, look around to see if there are any opportunities where you can help spark new life and hope. After all, providing love and a listening ear to those around us never goes out of season.
VICE PRESIDENT, COMMUNICATIONS AND MARKETING
BRIAN P. REARDON
EDITOR
BETSY TAYLOR btaylor@chausa.org
INTERIM EDITOR
CHARLOTTE KELLEY ckelley@chausa.org
GRAPHIC DESIGNER
NORMA KLINGSICK
ADVERTISING Contact: Yvonne Stroder, 4455 Woodson Rd., St. Louis, MO 63134-3797, 314-253-3447; fax 314-427-0029; email ads@chausa.org.
SUBSCRIPTIONS/CIRCULATION Address all subscription orders, inquiries, address changes, etc., to Service Center, 4455 Woodson Rd., St. Louis, MO 63134-3797; phone 800-230-7823; email servicecenter@chausa.org. Annual subscription rates are: complimentary for those who work for CHA members in the United States; $29 for nonmembers (domestic and foreign).
ARTICLES AND BACK ISSUES Health Progress articles are available in their entirety in PDF format on the internet at www.chausa.org. Photocopies may be ordered through Copyright Clearance Center, Inc., 222 Rosewood Dr., Danvers, MA 01923. For back issues of the magazine, please contact the CHA Service Center at servicecenter@chausa.org or 800-230-7823.
REPRODUCTION No part of this publication may be reproduced or transmitted in any form or by any means, electronic or mechanical, including photocopying, recording or any information storage and retrieval system, without permission from CHA. For information, please contact copyright@chausa.org.
OPINIONS expressed by authors published in Health Progress do not necessarily reflect those of CHA. CHA assumes no responsibility for opinions or statements expressed by contributors to Health Progress.
2024 AWARDS FOR 2023 COVERAGE
Catholic Press Awards: Magazine of the Year — Professional and Special Interest Magazine, First Place; Best Special Section, First Place; Best Special Issue, First Place; Best Coverage — Political Issues, First Place; Best Essay, First and Second Place; Best Feature Article, Third Place; Best Reporting on Social Justice Issues — Dignity and Rights of the Workers, Second Place; Best Reporting on Social Justice Issues — Life and Dignity of the Human Person, First Place; Best Reporting on Social Justice Issues — Option for the Poor and the Vulnerable, Third Place; Best Reporting on Social Justice Issues — Rights and Responsibilities, Third Place; Best Writing — In-Depth, Honorable Mention.
American Society of Business Publication Editors Awards: All Content — Enterprise News Story, Regional Gold Award; All Content — Government Coverage, Regional Silver Award; All Content — Editor’s Letter, Regional Silver Award.
Produced in USA. Health Progress ISSN 0882-1577. Winter 2025 (Vol. 106, No. 1).
Copyright © by The Catholic Health Association of the United States. Published quarterly by The Catholic Health Association of the United States, 4455 Woodson Road, St. Louis, MO 63134-3797. Periodicals postage paid at St. Louis, MO, and additional mailing offices. Subscription prices per year: CHA members, free; nonmembers, $29 (domestic and foreign); single copies, $10.
POSTMASTER: Send address changes to Health Progress, The Catholic Health Association of the United States, 4455 Woodson Road, St. Louis, MO 63134-3797.



Trevor Bonat, MA, MS, chief mission integration officer, Ascension Saint Agnes, Baltimore
Sr. Rosemary Donley, SC, PhD, APRN-BC, professor of nursing, Duquesne University, Pittsburgh
Fr. Joseph J. Driscoll, DMin, director of ministry formation and organizational spirituality, Redeemer Health, Meadowbrook, Pennsylvania
Tracy Neary, regional vice president, mission integration, St. Vincent Healthcare, Billings, Montana
Gabriela Robles, MBA, MAHCM, president, St. Joseph Fund, Providence St. Joseph Health, Irvine, California
Jennifer Stanley, MD, physician formation leader and regional medical director, Ascension St. Vincent, North Vernon, Indiana
Rachelle Reyes Wenger, MPA, system vice president, public policy and advocacy engagement, CommonSpirit Health, Los Angeles
Nathan Ziegler, PhD, system vice president, diversity, leadership and performance excellence, CommonSpirit Health, Chicago
ADVOCACY AND PUBLIC POLICY: Lisa Smith, MPA; Kathy Curran, JD; Clay O’Dell, PhD; Paulo G. Pontemayor, MPH; Lucas Swanepoel, JD
COMMUNITY BENEFIT: Nancy Lim, RN, MPH
CONTINUUM OF CARE AND AGING SERVICES: Indu Spugnardi
ETHICS: Nathaniel Blanton Hibner, PhD; Brian Kane, PhD
FINANCE: Loren Chandler, CPA, MBA, FACHE
GLOBAL HEALTH: Bruce Compton
LEADERSHIP AND MINISTRY DEVELOPMENT: Diarmuid Rooney, MSPsych, MTS, DSocAdmin
LEGAL, GOVERNANCE AND COMPLIANCE: Catherine A. Hurley, JD
MINISTRY FORMATION: Darren Henson, PhD, STL
MISSION INTEGRATION: Dennis Gonzales, PhD; Jill Fisk, MATM
PRAYERS: Karla Keppel, MA; Lori Ashmore-Ruppel
THEOLOGY AND SPONSORSHIP: Sr. Teresa Maya, PhD, CCVI

HELPING YOUTH THRIVE

ALLEN SÁNCHEZ President and Mission Leader, CommonSpirit St. Joseph’s Children
New Mexico: The Land of Enchantment, where you can find many opportunities for adventure but very few opportunities for our children. In 2010, the Annie E. Casey Foundation reported that the children of New Mexico ranked 46th in children’s wellbeing in the country,1 with 63% graduating high school and 80% of fourth graders falling below the proficient reading level.2 Three years later, in 2013, New Mexico would fall even further, ranking 50th in the nation for children’s well-being.3 Horrific, high-profile deaths of children at the hands of their parents and caregivers made headlines in the local and national media.
New Mexico is one of the largest oil producers in the nation, holding the rights to the majority of this liquid gold. At the time, this ranking, of a state holding the third-largest sovereign wealth fund in the nation4 (which today ranks as the secondlargest), was not just a sign of inequity but of a contrast for a dismal future for the well-being of the children of New Mexico. The state neglected to make the human capital investment necessary to uplift its children.
Yet, in the state’s coffers, what is known as the Land Grant Permanent Fund, which benefits from the state’s gas and oil revenues, was bulging. The situation could be best described by an image of a scale, with one side of it representing gas and oil royalty revenue pouring into the third-largest sovereign wealth fund in the nation and, on the opposite side of the scale, the worst outcomes for children, with the state ranking 50th in the nation in health and well-being. The fulcrum of the scale had to be moved to tip in favor of the children.
It was obvious that for years, the state’s policymakers had neglected to invest in its residents’ social capital. Through close examination during a strategic planning process — which included CHI St. Joseph’s Children (now known as CommonSpirit St. Joseph’s Children), New Mexico Voices for Children, Partnership for Community Action and others — many of the answers to preventing negative health outcomes pointed to an early mitigator: early childhood education and care programs.
To help policymakers comprehend how dire the situation was, CHI St. Joseph’s Children in Albuquerque, New Mexico, used the image of a potter spinning clay to form a vessel. It is like a child in the last trimester of pregnancy and through the age of 3, when approximately 1 million neural connections per second are being created, building the architecture of the brain.5 As

that beautiful, wet clay is being formed, like the brain, the adrenaline of toxic stress and adverse childhood experiences (ACEs) can poke holes in it, slowing down or even diminishing the development of the brain’s synapses. When the state then takes the largest investment it makes, K-12 education, and tries to pour it into the vessel, the pot cannot hold the liquid. The child arrives at kindergarten already behind — and stays behind — and we wonder why the child is unable to take full advantage of the educational opportunities.
CHI St. Joseph’s Children led its advocacy effort by example, creating one of the largest home visiting programs in the nation. This was funded by an endowment created from the divestiture of St. Joseph’s Hospital in Albuquerque by Catholic Health Initiatives, resulting in the community health organization known as CHI St. Joseph’s Children in 2000. We knew that home visiting develops the relationships that are the mitigators of toxic stress, trauma and ACEs that, years later, manifest themselves into poor health
outcomes.
With the support of case managers, trained home visitors go into the homes of first-time parents once a week for three years with a curriculum of health, well-being and school readiness. The case managers, who we refer to as Enhanced Referral Navigators, connect the families to all the safety net services for which they’re eligible. The program is open to any first-time parents in New Mexico and is offered at no cost to the participants. It was this example of leadership that gave legislators and policymakers a vision that they could embrace.
As an anchor organization in the community, CHI St. Joseph’s Children took on the banner to advocate for full funding of early childhood programs, which would create systemic change and bring health and well-being to the current and future generations of the state. In 2010, the organization Invest in Kids NOW began and had a membership of more than 40 nonprofits — including Partnership for Community Action, New Mexico
Voices for Children, Youth Development, Inc., and Lutheran Advocacy Ministry-New Mexico — to bring the fight to the state legislature to support such programs.
Everything was on the table, including raising taxes or the reappropriation of funds. There was no political will for a tax; what became an obvious source was the state’s Land Grant Permanent Fund. This was going to require a change in the distribution formula of the fund, created in 1910 by the Enabling Act, the law required for later creating the state of New Mexico in 1912. The Enabling Act stated that it would require a constitutional amendment, approved by the voters, to redirect money to the youngest residents of the state. This meant having to pass through the state legislature a resolution to place the question on the ballot for voters and would require a 2/3 majority vote of the elected bodies of the New Mexico State House of Representatives and the Senate.
Although polling indicated that 72% of registered voters in New Mexico were in favor of placing this resolution on the ballot,6 what seemed to be a logical solution turned into a 10-year battle with the state Senate. Entrenched senators of the powerful Senate Finance Committee had deemed the Land Grant Permanent Fund a sacred idol that could not be touched. Many elusive influencers of the state, protecting special interests such as the stock market and oil companies, seemed to sway that small group of powerful senators away from overhauling the long-needed distribution formula.
What made the yearslong battle an even greater indignity was that the oil money was flowing from lands seized from Native peoples by the federal government; the very lands creating the wealth were not benefiting the poorest populations from whom that land was taken.
This was a battle to create health and wellbeing for the population of the state, 7 one that
included a direct confrontation with the status quo of institutional racism. The ugly arm of institutional racism reached all the way back to the U.S. Congress, in its creation of the Land Grant Permanent Fund, by placing a requirement on New Mexico and Arizona as the only states in the country that must return to Congress for ratification for any changes to be made in their constitution dealing with state lands.
Invest in Kids NOW sounded the alarm on the plight of the children of New Mexico. Their campaign created an annual rally called the 1,000 Kid March to raise awareness in support of boosting early childhood education programs through the fund; its inaugural march was held in 2014. Each year that the event occurred, the state capitol, known as the Roundhouse, would be brimming with parents pushing strollers, leading toddlers by the hand and marching around the iconic capitol.
Parents faced legislators who were armed with misinformation, denying the scientific evidence of the benefits of early childhood education and planting fears that the state’s sovereign wealth fund, which at the time was over $15 billion and is now more than $30 billion,8 could not stand the additional withdrawal. The arguments by the fiscal hawks became a debate of what was the reasonable percentage to be withdrawn from a trust fund. Advocates turned this question on its head and returned with an additional question: What was the reasonable number of children to be left behind?
To elevate the detrimental effects that ACEs were having on the children of the state, CHI St. Joseph’s Children implemented a campaign in 2016 that parodied the state’s popular and successful tourism media campaign known as New Mexico True. This parody was known as New Mexico Truth9 — not just to tell the natural wonders of the state but to expose the statistics that showed the detrimental social conditions in which its children were living. The campaign didn’t ask
The campaign didn’t ask readers and viewers to take any specific action. Rather, it served as an educational campaign, like good prophets, first calling on the community to acknowledge and grieve for the injustices that had placed its children in peril.


readers and viewers to take any specific action. Rather, it served as an educational campaign, like good prophets, first calling on the community to acknowledge and grieve for the injustices that had placed its children in peril.
The Land of Enchantment was being challenged to see itself in the light of decades of institutional racism. The campaign featured such messages as, “New Mexico and its glowing hot air balloons rising to new heights where you can find the highest rate of children living in poverty in the United States.” Others included, “New Mexico, with its magnificent vistas and its unique cuisine, where our people turn a blind eye to its hungry
Powerful senators not in favor of the campaign’s mission influenced the media to editorialize their opposition through op-eds and Sunday cartoons depicting early childhood advocates as robbers and thieves. They went as far as declaring the 1,000 Kid March the Pre-K Gang, ready to hold up the Wells Fargo stagecoach carrying the chest of the Land Grant Permanent Fund with a cartoon of one man stating to another, “Keep yer eyes peeled! I hear the Pre-K Gang hangs out in these parts!”10
By being the first state in the union to make early childhood services a constitutional right, the health of New Mexico’s population will be forever changed.
children who rank second highest in the nation for children experiencing hunger.”
But the truth set the state free, and, with the public educated about the statistical conditions of the children of New Mexico, the logjam was broken. After 10 years of battling with the state legislature, the constitutional amendment, known as the House Joint Resolution 1 Early Childhood Constitutional Amendment,
placed on the November 2022
ballot and was approved by the voters with a mandate vote of 70.33% in favor.11
The ballot initiative authorized an additional withdrawal of 1.25% of the Land Grant Permanent Fund, but the ugly head of institutional racism planted more than a century earlier, still required ratification by the U.S. Congress. In the final hours of the congressional session ending on December 31, 2022, with the help of Sen. Martin Heinrich, D-New Mexico, and Senate Majority Leader Chuck Schumer, D-New York, the ratification was placed in the omnibus budget package, approved and sent to President Joe Biden’s desk for his signature.
In the process of this battle, additional distribution was approved, and, in a political sidestep to try and derail the Land Grant Permanent Fund distribution, a separate Early Childhood Trust Fund was created in 2020, also receiving oil money from the oil severance tax. In addition, a new department known as the Early Childhood Education and Care Department, with a cabinet secretary overseeing its activities, became the deliverer of early childhood services. On July 1, 2023, the funds began to flow. Today, the department’s budget for delivering early childhood services is nearly $800 million in a state with a population of approximately 2 million people.12
In the process of this work, the Early Childhood Advisory Council was created to advise the newly appointed secretary, and, with the exposure of institutional racism, a state Council for Racial Justice was convened in 2020. This council works at the governor’s will to illuminate racism from state institutions.
By being the first state in the union to make early childhood services a constitutional right, the health of New Mexico’s population will be forever changed. The immediate impact on children’s health is evident: The first-of-its-kind universal child care in the nation places children in a safe environment, lifts their parents up by creating the ability to seek employment and raises the family out of poverty.13 In many cases, that employment brings health insurance coverage to the family. Universal Pre-K ensures that children reach kindergarten ready to learn, and home visiting connects parents to safety net service organizations, reassuring them that babies do come with instructions.
Home visitors, as part of CommonSpirit St. Joseph’s Children’s Joyful Parenting Partnership program, connect families and babies to a medical home and teach parents resilience and how to advocate for their child. They also bring access and connection to housing assistance, vaccinations, the Supplemental Nutrition Assistance Program and other food services. Furthermore, they build relationships in which parents feel safe to self-disclose their need for referral and follow through to address issues such as postpartum depression or alcohol or substance abuse. In fact, the state can attest to a decrease in visits to the emergency room in the first year of a child’s life.14 New Mexico is blessed to have a revenue stream from royalties on gas and oil, but all states can discern how they, too, can make this constitutional right for their youngest children and invest it in the fundamental foundation for their lifelong health. Prioritizing health is a battle worth fighting.
ALLEN SÁNCHEZ is president and mission leader of CommonSpirit St. Joseph’s Children in Albuquerque, New Mexico. He is also executive director of the New Mexico Conference of Catholic Bishops and a member of the New Mexico State Investment Council, which manages the nation’s current second-largest sovereign wealth fund.
1. “The Annie E. Casey Foundation 2010 Kids Count Data Book,” Annie E. Casey Foundation, 2010, https://assets.aecf.org/m/resourcedoc/AECF2010KIDSCOUNTDataBook-2010.pdf.
2. “Common Core of Data: America’s Public Schools,” National Center for Education Statistics, January 2015, https://nces.ed.gov/ccd/tables/acgr_2010-11_to_ 2012-13.asp; “Early Warning! Why Reading by the End of Third Grade Matters,” Annie E. Casey Foundation, 2010, https://assets.aecf.org/m/resourcedoc/AECF-Early_ Warning_Full_Report-2010.pdf.
3. “2013 Kids Count Data Book: State Trends in Child Well-Being,” Annie E. Casey Foundation, 2013, https://assets.aecf.org/m/resourcedoc/AECF2013KIDSCOUNTDataBook-2013.pdf.
4. The New Mexico State Investment Council is a sovereign wealth fund that manages the investments for New Mexico’s four permanent funds: the Land Grant Permanent Fund, the Severance Tax Permanent Fund, the Tobacco Settlement Permanent Fund and the Water Trust Fund. Tiziana Barghini, “Largest Sovereign Wealth

Funds (SWFs) 2015,” Global Finance, November 1, 2014, https://gfmag.com/features/largest-sovereignwealth-funds/.
5. “Why 0-3?,” Zero to Three, https://www.zerotothree. org/why-0-3/.
6. “2021 New Mexico Early Childhood Statewide Survey,” CHI St. Joseph’s Children, January 11, 2021, https://stjosephnm.org/wp-content/uploads/2021/01/ New-Mexico-Early-Childhood-Statewide-SurveyPresentation.pdf.
7. “New Mexico Could Not Hear the Train,” Century Lives, November 1, 2023, https://open.spotify.com/ episode/6eSsNu3xlWfxWcdjo2YGfa.
8. “Permanent Fund Investments to Surpass Oil and Gas Revenue, Securing New Mexico’s Future by 2039,” New Mexico Department of Finance and Administration, https://www.nmdfa.state. nm.us/2024/09/17/permanent-fund-investments-tosurpass-oil-and-gas-revenue-securing-new-mexicosfuture-by-2038/.
9. New Mexico Truth, https://newmexicotruth.org.
10. Andrew Oxford, “Kids March on Capitol for Early Education Funds,” Santa Fe New Mexican, January 2018, https://www.santafenewmexican.com/news/
education/kids-march-on-capitol-for-earlyeducation-funds/article_adca512e-024b-596f-8322ed67b37bc0b7.html.
11. Phill Casaus, “Sánchez’s Persistence Helps Turn a Pipe Dream Into Early Education Milestone,” CommonSpirit St. Joseph’s Children, November 12, 2022, https://stjosephnm.org/2024/05/24/sanchezspersistence-helps-turn-a-pipe-dream-into-earlyeducation-milestone/.
12. Susan Dunlap, “ECECD Expects Slightly Smaller Budget than Requested,” New Mexico Political Report, March 2, 2024, https://nmpoliticalreport.com/ nmleg/ececd-expects-slightly-smaller-budget-thanrequested/.
13. “With Costs of Child Cares Soaring, New Mexico Finds a Way to Make It Free for Many,” NBC Nightly News, October 29, 2024, https://www.nbcnews. com/nightly-news/video/with-costs-of-child-caressoaring-new-mexico-finds-a-way-to-make-it-free-formany-223008837777.
14. “New Parent Home Visiting Program Reduces Infants’ Need for Medical Care During First Year of Life,” RAND, December 15, 2016, https://www.rand.org/news/ press/2016/12/15.html.
Health Progress’ Diversity, Equity and Inclusion
Discussion Guide supports learning and dialogue to move toward a greater understanding of patients, care providers and ways to work together for improved diversity, equity and inclusion in Catholic health care settings.
GUIDE INCLUDES
Introduction on how to use the materials.
Health Progress articles for reflection, discussion and as a call to action.
Opening and closing prayer from CHA’s resources.
OR SCAN THE QR CODE
HELPING YOUTH THRIVE

ANU FRENCH, MD, FAAP, ABoIM SSM Health Cardinal Glennon Pediatrics and Integrative Medicine
As I approach 30 years in clinical practice, walking into our SSM Health Cardinal Glennon Pediatrics and Integrative Medicine office at SSM Health DePaul Hospital in St. Louis reminds me of the poem I wrote as my mission statement when I was only dreaming of such a possibility.
Holy Encounter:
As I step over the threshold, I ask to be blessed with kind usefulness each day.
As I wash my hands, I ask to be mindful and motivational each day.
As I brew my morning tea, I ask to be humble and receptive each day.
As I take the history, I ask to listen keenly to the story each day.
As I recognize the honor, I ask for the courage to be connected each day.
As I feel the healing, I ask for the clarity to see the wholeness in each day.
As I tend the mind-body-spirit, I ask for surrender to the sanctity of each day.
As I nourish and flourish, I offer deep gratitude for the privilege of each day.
My presence: holy moment. My journey: holy labyrinth.
My office: holy space. My patient: holy encounter.
Sometimes, I pinch myself because 15 years ago, I was in such a different space. I was professionally and personally burned out, disinterested in the revolving sickness door of primary care pediatrics, and exhausted from the merry-
go-round of home and work. I had just attended a weekend gathering of integrative healers committed to improving health care for children. In the therapeutic journaling session, we were asked to write about something that had changed who we were professionally and personally. As the room fell silent, I realized that the time had come for me to acknowledge that I was burned out.
AN INTEGRATED PATH TO HEALING
I had lived most of my adult life with chronic disease that had taken its toll on me. It was becoming apparent to me that I was not an effective resource unless I was truly committed to being on the journey to healing myself. Creating tools to build intergenerational resilience in myself, my children, my patients and their caregivers had to become a priority.
In 2011, I answered an email about a fellowship on integrative medicine at the Andrew Weil Center for Integrative Medicine at the University of Arizona. I took a leap of faith and completed the training and board certification in this fledgling specialty.1 It was a healing-oriented medicine that looked at the whole person/child, teaching appropriate use of both conventional and evidence-

informed complementary remedies. I learned about self-care and started to nourish myself and my family through music and art.
The graphic shown below from The National Center for Complementary and Integrative Health of the National Institutes of Health, which researches the use and safety of complementary health approaches, shows how these remedies can be integrated into a whole-person health framework.2
Dr. Kathi Kemper, a respected pioneer in this specialty and professor of pediatrics at The Ohio State University College of Medicine, defines pediatric integrative medicine (PIM) as caring for the whole child in the context of their values, their family’s beliefs, their family system and their culture in the larger community. The specialty also considers a range of therapies based on the evidence of their benefits and costs, which aligns with SSM Health’s mission and values.
In 2015, Dr. Kemper invited me to be part of the American Academy of Pediatrics (AAP) Section on Integrative Medicine PIM Leadership Summit. The white paper we wrote included compelling data that showed complementary therapies are of great interest to parents and that the use of these therapies in pediatrics is significant. The National Health Interview Survey, conducted by the Centers for Disease Control and Prevention’s National Center for Health Statistics in 2012, revealed that 12% of children use complementary therapies chosen by their families, and studies in specific
chronically ill populations have reported complementary therapy use in up to 80%. 3 More than 1,500 parents solicited through a survey answered questions regarding integrative therapies they’d like to see offered in a pediatric practice and their willingness to advocate for insurance coverage of PIM therapies.
In 2019, with the support of leadership at SSM Health Cardinal Glennon Children’s Hospital, the PIM office came into being after five years of planning. And, in the last five years, we have had the privilege of being on healing journeys with many courageous families that have children with medically complex illnesses, which has renewed my zest for medicine. Integrative medicine nudged me in a fresh direction and connected me with a vibrant community of healers and teachers, both globally and in my own backyard of St. Louis, who continue to show me how to bring mind-bodyspirit medicine into our office and into my home.
In her groundbreaking book The Deepest Well: Healing the Long-Term Effects of Childhood Adversity, Dr. Nadine Burke Harris, founder of the Center for Youth Wellness and former Surgeon General of California, writes: “Sleep, mental health, healthy relationships, exercise, nutrition and mindfulness — we saw in our patients that these six things were critical for healing [of adverse childhood experiences]. ... Fundamentally, they all targeted the underlying biological mechanism

Source: The National Center for Complementary and Integrative Health

Integrative medicine nudged me in a fresh direction and connected me with a vibrant community of healers and teachers, both globally and in my own backyard of St. Louis, who continue to show me how to bring mind-bodyspirit medicine into our office and into my home.
— a dysregulated stress-response system and the neurologic, endocrine and immune disruptions that ensued.”4 Integrative medicine is dedicated to looking at the whole person and using the latest science to improve health and well-being.
When 6-year-old Maya, whose name has been changed for privacy, and her family arrived at our office, they had seen multiple health care practitioners. They were tired, scared, frustrated and looking for answers. As a trauma-informed office, our first goal is always to make sure that we are creating a safe space where the child and family feel seen, heard and affirmed.5
The importance of providing this level of care and attention is especially true for a neurodivergent child such as Maya, who is on the autism spectrum with behavioral, sleep and focus concerns. As family physician and psychiatrist Dr. Lewis Mehl-Madrona says in his beautiful book, Narrative Medicine: The Use of History and Story in the Healing Process, “We need to develop an approach that will allow the patient and his or her family to be active collaborators in the healing process.”6 So, our next goal was to come up with a therapeutic plan — one that was culturally competent, economically affordable and guided by the family — which included all of pediatric integrative medicine’s pillars of health (shown in the graphic on page 15).
Building intergenerational resilience is one of the priorities of PIM, and luckily for us, Maya loved music, art and mindful movement. Research on yoga is expanding at the National Institutes of Health, which currently lists several studies on its benefits.7 In 2016, recognizing how important the holistic approach to shifting health care paradigms was, AAP’s Section on Integrative Medicine released a clinical policy statement on the use of mind-body therapies in children and youth.8 A review on the effectiveness of yoga as a comple-
mentary therapy for children and adolescents, which I was asked to co-author, was included in the statement.9 This inspired me to complete yoga teacher training for kids through the YoYo Yoga School in St Louis.
The practice of yoga has been shown to decrease stress via downregulation of the sympathetic nervous system, the fight or flight response. I enjoyed bringing some of these tools into our office for Maya’s treatment plan, including using our breath to hum and buzz like bees as we did our mindful yoga poses of a tree, a mountain and a butterfly.
The benefits of sound and music examined in a scoping review show a range of their effects on the neuro-immune-endocrine systems. 10 In ancient cultures, the use of sound for healing was a highly developed sacred science. In 2018, a pilot study conducted at our SSM Health Cardinal Glennon Pediatric Primary Care Clinic at SSM Health DePaul Hospital was funded and published through the AAP’s Section on Integrative Medicine, demonstrating calming brain wave patterns in 25 parent-child volunteers — including improved sleep — who listened to healing harp music. 11, 12 Music therapy became part of Maya’s bedtime routine, in addition to soothing guided imagery routines practiced with her parents.
Once we gained the trust of Maya and her parents, we moved on to discuss incorporating an anti-inflammatory diet into the family’s shopping and cooking schedule and adding highquality supplements and botanicals to support deficiencies we found in her lab work.13 In the integrative psychiatry fellowship I completed in 2020, we were taught about the emerging field of nutritional psychiatry, which uses nutrition to optimize brain health and treat and prevent mental health disorders.14 As noted in an EBioMedicine article, using food as medicine points to the “immune system, oxidative biology, brain plastic-



ity and the microbiome-gut-brain axis as key targets for nutritional interventions.”15
It is encouraging for me to see, as someone who has found her way back from it, that burnout prevention is being given priority. The Missouri Chapter of the AAP collaborated with the Missouri Child Psychiatry Access Project16 and the Missouri Department of Conservation to host a physician wellness retreat in September, where I spoke on the anti-inflammatory diet and how to incorporate it into our homes and offices.
The Care for the Caregiver program at SSM Health Cardinal Glennon Children’s Hospital, through the generosity of the SSM Health Cardinal Glennon Children’s Foundation, facilitates weekly sessions for all the hospital’s care team members that include meditation, breath work, yoga, pet therapy, art therapy, massage and more. I was grateful to be invited to share a virtual sound healing meditation at one of the sessions this past fall with my Tibetan bowls. The baby steps we suggest to our patients and their families for lifestyle modification become important steppingstones for our own healing journeys so that we can all find what brings pleasure and fulfillment in our lives.
Dr. Andrew Weil, a world-renowned leader
and pioneer in the field of integrative medicine, emphasizes that good medicine should be based on good science, be inquiry-driven and open to new paradigms where one should use natural, effective, less-invasive interventions whenever possible.17 Maya had been showing steady improvement in all her symptoms as we addressed her sleep, diet, relationships and physical environment. She was back in school and getting the full benefit of all her therapies while the burden of worry on her parents had lifted considerably. Our wonderful PIM team makes these success stories possible.
Dr. Weil also discusses how important it is to train the next generation of practitioners to be models of health and healing, committed to the process of self-exploration and self-development. The Academic Consortium for Integrative Medicine & Health includes more than 75 academic medical centers, nursing schools and health systems that advance integrative health care education, research and clinical care.18 The SSM Health Cardinal Glennon Children’s Foundation sponsored a grant in 2014 that supported our SSM Health Cardinal Glennon Pediatric Primary Care at SSM Health DePaul Hospital in offering an elective accredited by the Accreditation Council for Graduate Medical Education in integrative medicine for third-year Saint Louis University pediatric residents as part of the Pediatric Integrative Medicine in Residency pilot.19
When the Integrative Medicine for the Underserved policy committee went to Capitol Hill in 2018 to attend a bipartisan congressional caucus on integrative approaches to address the chronic pain epidemic, I went with them and saw firsthand how sharing information on rigorous scientific research and sustainable models of clinical care can inform current health care policy.20 I am honored to be a clinical mentor for pediatricians who are currently doing their fellowship training in integrative medicine at the Andrew Weil Center for Integrative Medicine and giving back to the program that started my own journey to better health.
As we enter the new year, it will be 25 years for me with the mission of SSM Health, and I look forward to the next five-year plan of expanding our integrative medicine services to continue to provide equitable, affordable, accessible and


Inspired by an “I Am Centered” artwork piece hanging in one of the exam rooms at SSM Health Cardinal Glennon Pediatrics and Integrative Medicine’s office in St. Louis (shown left), a 6-year-old patient created her own artistic interpretation of the piece and gifted it to integrative pediatrician Dr. Anu French (shown right). Art, music and mindful movement can play important parts in integrative medicine’s holistic approach to care.
holistic pediatric care to all children regardless of their social determinants of health. I continue to research how music, mindfulness and art can rebuild and rewire brains and hearts, and I look forward to going to work each day.
Many of us get defined by the diseases we are told that we have. I was labeled with so many, and I thought I would have to coexist with them for the rest of my life. Painting “I Am” affirmations became a joyful way to connect with my two beautiful daughters and my own inner child. The affirming art that I created to bring me back from the brink of burnout is now hanging in the waiting room and exam rooms of our SSM Health Cardinal Glennon PIM office.
Maya was inspired by my “I Am Centered” artwork hanging in one of our exam rooms and gifted me with her interpretation of it, which sits proudly on my desk at work. I have come full circle, helping children and families access their innate selfregulatory systems as I continue to learn how to access mine.
DR. ANU FRENCH is an integrative pediatrician with SSM Health Cardinal Glennon Pediatrics and Integrative Medicine in St. Louis and is also an artist, musician and author.
1. “Andrew Weil Center for Integrative Medicine,” The University of Arizona, https://awcim.arizona.edu.
2. “What Does NCCIH Do?,” National Center for Complementary and Integrative Health — National Institutes of Health, https://www.nccih.nih.gov.
3. Lindsey Black et al., “Use of Complementary Health Approaches Among Children Aged 4–17 Years in the United States: National Health Interview Survey, 2007–2012,” National Health Statistic Report 10, no. 78 (February 2015): 1-19; Anna Esparham et al., “Pediatric Integrative Medicine: Vision for the Future,” Children 5, no. 8 (August 2018): https://doi.org/10.3390/ children5080111.
4. Dr. Nadine Burke Harris, The Deepest Well: Healing the Long-Term Effects of Childhood Adversity (Mariner Books, 2018).

5. “Professional Tools and Resources for TraumaInformed Care,” American Academy of Pediatrics, https://www.aap.org/en/patient-care/ trauma-informed-care/professional-tools-resources.
6. Dr. Lewis Mehl-Madrona, Narrative Medicine: The Use of History and Story in the Healing Process (Bear & Company, 2007).
7. “Yoga: Effectiveness and Safety,” National Center for Complementary and Integrative Health — National Institutes of Health, August 2023, https://www.nccih. nih.gov/health/yoga-effectiveness-and-safety.
8. Section on Integrative Medicine, “Mind-Body Therapies in Children and Youth,” Pediatrics 138, No. 3 (2016): https://doi.org/10.1542/peds.2016-1896.
9. Dr. Lawrence Rosen, Dr. Anu French, and Grace Sullivan, “Complementary, Holistic, and Integrative Medicine: Yoga,” Pediatrics in Review 36, No. 10 (2015): https://doi.org/10.1542/pir.36-10-468.
10. Genevieve A. Dingle et al., “How Do Music Activities Affect Health and Well-Being? A Scoping Review of Studies Examining Psychosocial Mechanisms,” Frontiers in Psychology 12 (September 8, 2021): https://doi. org/10.3389/fpsyg.2021.713818.
11. Dr. Anu French and Kristy Shaughnessy, “Testing the Impact of the ‘The Magic Mirror’ Harp Music as a CostEffective Biofeedback/Neurofeedback Tool to Relieve Stress, Build Intergenerational Resilience and Teach SelfRegulation,” Pediatrics 144, No. 2 (August 2019): https://doi.org/10.1542/peds.144.2MA6.530.
12. “Pediatric Pilot Study: Presentation at the American Academy of Pediatrics National Conference,” Amy Camie: The Healing Harpist, https://www. amycamie.com/pediatricpilotstudy.html.
13. “Dr. Weil’s Anti-Inflammatory Diet,” Dr. Weil, https://www.drweil.com/diet-nutrition/ anti-inflammatory-diet-pyramid/dr-weilsanti-inflammatory-diet/.
14. Dr. Drew Ramsey, “What is Nutritional Psychiatry?,” Drew Ramsey, MD, July 7, 2022, https://drewramseymd .com/brain-food-nutrition/what-is-nutritionalpsychiatry/.
15. Felice N. Jacka, “Nutritional Psychiatry: Where to Next?,” EBioMedicine 17 (March 2017): http://dx.doi. org/10.1016/j.ebiom.2017.02.020.
16. “Missouri Child Psychiatry Access Project (MO-CPAP),” University of Missouri School of Medicine, https://medicine.missouri.edu/departments/ psychiatry/research/missouri-child-psychiatry -access-project.
17. “Meet Dr. Weil,” Dr. Weil, https://www.drweil.com/ health-wellness/balanced-living/meet-dr-weil/.
18. “Academic Consortium for Integrative Medicine & Health,” https://imconsortium.org.
19. “Integrative Medicine in Residency,” Andrew Weil Center for Integrative Medicine at the University of Arizona, https://awcim.arizona.edu/education/imr.html.
20. “IM4US: Integrative Medicine for the Underserved,” https://im4us.org.
Integrative medicine is dedicated to looking at the whole person and using the latest science to improve health and well-being. The discipline explores the role that music, mindfulness, art and other complementary therapies can play on the journey to healing and wellness.
1. How do you feel about adding complementary therapies to treatment plans for patients suffering from chronic or complex diseases? What complementary resources are available to your patients, or how could you encourage them and your colleagues to include these as part of a treatment plan?
2. In addition to explaining the benefits of integrative medicine for her patients, author Dr. Anu French shares in her article how it has helped on her personal healing journey and suggests that the discipline can be a tool in burnout prevention. Does your health system offer integrative medicine as part of its well-being program for staff? If so, how can you and your colleagues take advantage of this?
3. As a system administrator, how can you explore adding art, meditation or other integrative medicine tools into your well-being program for clinicians and staff?
4. As a faith-based health care ministry, what are some ways you can incorporate spirituality into an integrative approach to healing for your patients? How can you include a spiritual component in your organization’s well-being efforts for staff?
ELENA MIKALSEN, PhD, ABPP Chief, Division of Pediatric Psychology, CHRISTUS Children’s
Some parents may notice that their teens seem more stressed every school year. And they are correct. According to The American Institute of Stress, 27% of U.S. teens feel extreme stress during the school year, approximately 18% experience an anxiety disorder caused by stress, and almost 30% report feeling depressed.1
Parents of teens may remember feeling stressed when they were teens and expect their children to navigate the years successfully, as they did. Teens today still face the same normal developmental stressors, such as finding peer groups, navigating the highs and lows of team sports, and increasing academic pressure, according to experts. In addition, pediatricians and mental health practitioners are also concerned about the growing impact of unrestricted social media access, increasing academic pressures at school, climate change, gun violence and, finally, the still lingering effects of the COVID-19 pandemic on current teen mental health.
Prior to the pandemic, pediatricians and mental health professionals were already noticing increasing rates of stress and mental illness in adolescents. However, the pandemic caused a significant psychological impact on youth and families. A recent American Psychological Association survey on stress in America pointed out that our society continues to experience psychological impacts of stress and traumatic experiences in the aftermath of pandemic lockdowns, school closures and disruptions in family routines. 2 Additionally, families and experts are still seeing the aftereffects of social isolation and academic underachievement on teen stress levels.
Another new factor increasingly affecting teens is social media. Experts are warning parents that prolonged social media use is associated with low self-esteem, depression, anxiety, poor sleep, eating disorders and suicide risk. Teens who spend more than three hours on social media per day face double the risk of mental health difficulties, according to an advisory from the U.S. Surgeon General in 2023,3 but studies have emerged showing that teens spend on average 4.8 hours per day navigating different social media platforms.4
The risk of negative mental health consequences from social media overuse is particularly high for adolescent girls. Girls are prone to comparing themselves to peers and defining their identity via others’ opinions, making them more vulnerable to depression after repeated exposure to social media. Girls, ages 13-19, have been found to spend more than five hours per day on social media,5 which means they feel the pressure to be “clever, smart and popular” all day, first at school and then on social media. It also means teens are being judged and criticized all day long, exposing them to constant social pressure. A rumor spread on social media can reach thousands of people in a matter of seconds.
Daily stress is definitely part of life, and it is
important to teach children how to navigate it. Long-term stress, however, is a risk for a variety of mental health difficulties. Stress can also cause significant wear on the immune system and lead to poor physical health. While experiencing stress is not necessarily detrimental for teens, how they cope with it is important. From my observations, teens are more likely to report using passive coping strategies, such as taking a nap or listening to music. While these methods work, they often don’t allow for learning active coping strategies, which help embrace and navigate stress, rather than just distract from it.
The following are some active ways of coping that parents can easily discuss with and teach to their children.
Manage social media use. Ever-increasing social media use is worsening teens’ stress levels, mental health, social skills, sleep and academic performance. The U.S. Surgeon General’s recent advisory cautioned that social media use in adolescence interferes with learning self-control, emotional regulation, learning and social skills and recommends parents take steps to prevent negative and spiraling effects of social media on teen mental health and stress levels.6 The following are some strategies that parents can do:
1. Parents should not allow their teens to access social media until they are 16. If they do decide to let them use it, they should consider an Instagram Teen Account, which includes some safeguards and parental controls.
2. Parents can create boundaries around family social media use. Parents should not allow smartphones to be used during meals or family activities. They should also serve as a good example to their teens by putting their phones away when talking, listening and eating.
3. Parents can teach teens how to handle social comparisons forced on them by social media. They can discuss how influencers and algorithms can affect them and how social media posts don’t portray real-life experiences.
4. Parents can teach their children how social media is often used for cyberbullying. They can encourage them to block bullies and stay connected only to peers who are positive, fun and supportive. They should also report all cyberbullying and exploitation of their teen.
Engage in physical activity. Only 15% of teens get enough daily exercise.7 Exercise is one of the most effective stress and anxiety relievers. It can also work as well as antidepressants or cognitive-behavioral therapy to reduce symptoms of depression.8 Any of these activities are helpful: yoga, hiking, biking, walking, dancing, running, basketball, rock climbing and skateboarding. The best activity is one that involves a social component, but it doesn’t need to be a team sport.
Get enough sleep. The recommended amount of sleep for teens is eight to 10 hours, according to recommendations from the American Academy of Pediatrics.9 However, surveys find that most teens sleep, on average, less than eight hours per night.10 Lack of sleep is connected to increased levels of stress, anxiety, depression and decreased academic performance. Teens who don’t get enough sleep are four times as likely to develop depression as those who are well-rested.11
Resist academic pressure. Teens are pressured more than ever to make high-stakes choices, know exactly who they are, perform perfectly all the time and achieve more. There is competition, social judgment and pressure from parents, teachers and society. Parents can teach their teens that they don’t have to be perfect, don’t have to get it right at any age, and can always change their minds when they are older. What they do now academically will not determine their entire lives.
Parents should discuss the importance of sometimes saying no to academic pressure. Their teen does not need to take every AP class their school recommends and participate in every club, sport and leadership activity. I recommend no more than two organized after-school activities for teens to allow for more time socializing with peers and engaging in self-care activities.
Parents can encourage their teens to engage in social and fun activities, not just required school activities. They should also allow them enough time to participate in religious youth groups, craft and talent activities, camps and community events. It’s also important that they keep in mind that colleges look for happy and well-rounded students, not just students with good grades and a multitude of standard activities.
Engage in meditation and mindfulness. Mindfulness refers to paying attention to life in the

present, being fully aware of our surroundings and what we are doing, and being in the moment and enjoying it fully, rather than constantly being distracted by electronics, social media and text messages. When we don’t have the ability to be in the moment, anxiety grows, and we become too overwhelmed to solve problems.
Teens who are always distracted and worried about the future begin to struggle with chronic stress and anxiety. Parents can teach their teens to put away their phones at the dinner table and turn off the TV the next time their family is eating dinner. They can encourage them to focus on eating their food and enjoying its flavors. Or the next time their teen is watching a show, they can suggest they don’t chat about it on social media or text friends at the same time, and instead stay fully tuned in to the program. Parents can encourage their children to do activities that require calm concentration, such as crafts, prayer, reading, science experiments or playing a musical instrument.
Talk about stress. Parents can teach their teens to talk to them and other family members daily about their stress. Even if their teen seems unwilling to open up, they can try to ask about stress on a daily basis and discuss ways they can handle their own stress. When adults show teens how they actively cope with stress, they tend to repeat their good skills. Parents can encourage teens to set limits on how much they absorb peers’ stress. Teens listening to their friends is OK, but always feeling the pressure to solve their problems is not.
I advise parents that if they think their teen needs more help dealing with stress and anxiety, they should talk to their pediatrician or search for a mental health provider. While family is often the best place to learn coping skills for stress, sometimes teens’ mental health requires careful evaluation and psychotherapy. For example, cognitivebehavioral therapy has been demonstrated as an effective and quick intervention to help teens learn stress management.12
By teaching teens to be proactive in building the tools needed to live happier and more balanced lives, they can gain confidence to better manage everyday stress.
ELENA MIKALSEN is the chief of pediatric psychology at CHRISTUS Children’s in San Antonio
and an associate professor of pediatrics at Baylor College of Medicine.
1. “The Most Important Statistics About Teen Stress,” The American Institute of Stress, https://www.stress. org/more-stress-information/#teen-stats.
2. “Stress in America 2023: A Nation Grappling with Psychological Impacts of Collective Trauma,” American Psychological Association, November 1, 2023, https://www.apa.org/news/press/releases/2023/11/ psychological-impacts-collective-trauma.
3. “Social Media and Youth Mental Health: The U.S. Surgeon General’s Advisory,” U.S. Department of Health and Human Services, 2023, https://www.hhs.gov/sites/ default/files/sg-youth-mental-health-social-mediaadvisory.pdf.
4. Jonathan Rothwell, “Teens Spend Average of 4.8 Hours on Social Media Per Day,” Gallup, October 13, 2023, https://news.gallup.com/poll/512576/teensspend-average-hours-social-media-per-day.aspx.
5. Rothwell, “Teens Spend Average of 4.8 Hours on Social Media Per Day.”
6. “Social Media and Youth Mental Health: The U.S. Surgeon General’s Advisory.”
7. “The 2022 United States Report Card on Physical Activity for Children and Youth,” Physical Activity Alliance, 2022, https://paamovewithus.org/wp-content/ uploads/2022/10/2022-US-Report-Card-on-PhysicalActivity-for-Children-and-Youth.pdf.
8. Lynette L. Craft and Frank M. Perna, “The Benefits of Exercise for the Clinically Depressed,” Primary Care Companion to The Journal of Clinical Psychiatry 6, no. 3 (2004): https://doi.org/10.4088/pcc.v06n0301.
9. Melissa Jenco, “AAP Endorses New Recommendations on Sleep Times,” AAP News, June 13, 2016, https://publications.aap.org/aapnews/news/6630/ AAP-endorses-new-recommendations-on-sleep-times.
10. Anne G. Wheaton et al., “Short Sleep Duration Among Middle School and High School Students — United States, 2015,” Centers for Disease Control, January 16, 2018, https://www.cdc.gov/mmwr/volumes/67/wr/ mm6703a1.htm.
11. Maanvi Singh, “Less Sleep, More Time Online Raise Risk For Teen Depression,” Your Health, NPR, February 6, 2014, https://www.npr.org/sections/ health-shots/2014/02/06/272441146/less-sleep-moretime-online-amp-up-teen-depression-risk.
12. Stefan G. Hofmann et al., “The Efficacy of Cognitive Behavioral Therapy: A Review of Meta-Analyses,” Cognitive Therapy and Research 36, no. 5 (July 2012): 427-440.

KELLY BILODEAU Contributor to Health Progress
Medical misinformation used to arrive on the back of a magazine or matchbox cover. Ads for questionable, gimmicky products were often clunky, unsophisticated and met with an eye roll.
“I’m not going to be able to go buy a belt and put it around my waist and have it jiggle, and that’s going to suddenly make me have that beautiful hourglass figure,” said Robin Henderson, chief executive of behavioral health at Providence Oregon.
But thanks to social media, medical falsehoods are now served in quick digital bites that are entertaining, believable and ubiquitous. Nearly 30% of the information people encounter online is false, according to the American Psychological Association (APA).1 “It’s a lot more slick, credible and enticing,” Henderson said.
This deluge of false health information creates problems in the doctor’s office, where it’s a struggle to debunk erroneous information to keep teens healthy.
“It has made our jobs a little bit more difficult at times and required us to be way more intentional in the way that we approach our patients. We need to engage and search out what they may be thinking and seeing, and then replace that with trusted information,” said Dr. Benson Hsu, a pediatric critical care specialist at Avera McKennan Hospital & University Health Center in Sioux Falls, South Dakota.
Health professionals and organizations, such
as the APA and the American Academy of Pediatrics (AAP), have been studying this new media landscape to determine the best way to steer teens away from false facts. Health care providers are gaining ground in this fight using novel tools and an enhanced understanding of how misinformation spreads and how to combat it. But it’s still a sizable challenge. “We haven’t quite figured out the secret sauce in social media, how to debunk myths and get accurate information out there,” Henderson said.
More health care organizations need to start communicating online. There’s not enough reputable information to balance out the nonreputable sources, said Dr. Alisahah Jackson, president of CommonSpirit Health’s Lloyd H. Dean Institute for Humankindness & Health Justice.
The spread of misinformation online is insidious because it’s effective. Video shorts or influencer content may be emotionally charged and seemingly aimed at keeping people “safe,” which increases the urgency to share it.2 Social media algorithms reward engagement, not accuracy. A teen who shows interest by clicking on a fake story may be fed a steady diet of problematic content,

which can reinforce the information. Research shows people are more likely to believe the same false information when exposed to it multiple times, according to the APA.3
Not surprisingly, teens may have trouble telling the difference between reliable and questionable information. One study published in Frontiers in Psychology found that less than half of teens trusted accurate health messages more than phony ones, and 41% thought that fake and real messages were equally trustworthy.4 People are also more likely to believe fake information if it confirms already held beliefs, aligns with their identity or worldview, or they are feeling emotional when they see it, according to the APA.5 Compounding the problem, one study found people were 70% more likely to share a fake story than a real one.6
Information that teens encounter doesn’t only affect themselves. They may share the information with older relatives. A patient navigator at CommonSpirit Health sent a woman a text message to schedule a COVID-19 vaccine appointment. “She responded back and said, ‘My grandkids are telling me not to take this vaccine, so I’m going to hold off,’” said Brisa Hernandez, system director of operations at CommonSpirit’s Lloyd H. Dean Institute for Humankindness & Health Justice.
misinformation during aimless scrolling. In other instances, they’re looking for answers often on topics they’re embarrassed to ask about, such as sexual health, appearance, weight or dieting, Hsu said.
Parents or providers are often alerted during a casual conversation that a teen has encountered misinformation. For Dr. Anisha Abraham, a pediatrician and spokesperson for AAP, it was a strange request from her teenage son about shampoo that tipped her off. He asked to buy a pricey brand to avoid stripping the oils out of his hair. “And I said, ‘Why am I paying $30 for this bottle of shampoo, and where did the stripping your oils come from?’” she said. “It was just this really interesting conversation.”
“The average age that young people start dieting is age 9 in the United States, which is really disturbing. There’s so much targeting to young people that can lead to either disordered eating or binge eating or other eating-related issues.”
— DR. ANISHA ABRAHAM
Why is there so much misinformation online? The reasons vary. Some of it is misinformation or incorrect or misleading content often spread unwittingly. Some content is deliberately deceptive, defined as disinformation.7
“I do believe that the monetary aspect of things probably has affected the desire to put out clickbait, things that will attract attention and viewership,” Avera’s Hsu said. “There is definitely a financial incentive to do that.”
Teens, who spend an average of 4.8 hours a day on social media, are at high risk for exposure to misinformation, according to the APA.8 Nearly 90% of their time is spent on the three most popular social media channels: TikTok, Instagram and YouTube. Sometimes teens encounter medical
Another red flag is a change in habits. Some teens have been swearing off sunscreen or looking to take specific supplements, CommonSpirit’s Hernandez said. Or it could be a shift in eating habits. There is a huge market for weight loss products, and kids start to feel the pressure to be slim early. “The average age that young people start dieting is age 9 in the United States, which is really disturbing,” Abraham said. “There’s so much targeting to young people that can lead to either disordered eating or binge eating or other eating-related issues.”
These topics prey on common insecurities, for example, the desire to build muscle, which can lead teens to seek out expensive, often unnecessary, and potentially dangerous supplements or steroids.
Helping kids become savvier about online risks also includes educating them about companies that may target them to make money. “The vaping industry very much targets young people,” Abraham said. “I’ve had conversations with kids and say, ‘Look, they don’t offer caramel-flavored

products for adults. It’s for you because they know that if a 13- or 14-year-old starts vaping, they have a lifelong vaper or smoker. Doesn’t that make you really angry that you’re being targeted and that they want your money and they want you hooked?’”
FINDING SOLUTIONS
Finding solutions and keeping kids on the right track isn’t easy. “Even as a parent and a pediatrician, I don’t always know what my kids are hearing and seeing,” Abraham said. However, health care providers can help ensure kids get accurate health information by using key strategies.
Become a trusted resource.
Doctors and nurses are among the most trusted professionals, CommonSpirit’s Jackson said. That can help make teens more receptive to taking their advice. “If you have a longitudinal relationship, if it’s somebody that you’ve seen as they’ve grown up, I think that’s an important way to build that trust as you engage them on topics,” Hsu said. That relationship should extend not only to the teen but to the family. Encourage parents to reach out with questions or concerns.
Study the media landscape.
It’s crucial to understand the information kids are being exposed to that might affect their health. For example, CommonSpirit Health embarked on a study in 2021 to understand vaccine hesitancy in their communities.9 They found that while many people were wary of vaccines, the reasons why they opted not to get the shot were very different between their study groups, Latinos in California’s Central Coast area and Black Americans in Little Rock, Arkansas. Don’t assume that patients are motivated by the same factors; ask.
Ask broad questions.
Go beyond the traditional screening topics when working with teens, which usually center around medical and safety-related topics such as selfharm, firearms, injury prevention and vaccines. “I think it’s important for providers to engage in things that may not necessarily fall under the umbrella of our usual health care topics, and to provoke discussion with teenagers and adolescents about things that they may be searching on their own, that they may be embarrassed to bring up in a clinic visit,” Avera’s Hsu said.
Tread lightly.
If a teen does believe misinformation, handle the discussion carefully.
Sometimes the best approach is to ask questions, allowing teens to come to their own conclusions. “It’s really creating a trusted, safe environment, and coming at it with a sense of curiosity, not judgment,” Hsu said. “Don’t say, ‘Well, obviously that’s wrong.’ Instead ask, ‘Why do you believe that?’”
The same approach can also apply to parents, who are paddling in the same sea of misinformation. “I don’t believe there are adults out there who intentionally want to mislead their kids,” Hsu said. “I think all adults are coming from a place of care and compassion. But they’re seeing their feed filled with information that I don’t necessarily agree with or that I believe is scientifically accurate.” Approach the discussion in good faith. “I think that’s way more effective than to come down and say, ‘Oh my gosh, I can’t believe you believe that that is so inaccurate and so wrong,’” he said.
Ultimately, patients have the right to make their own choices. “At the end of the day, we still have to be open to the fact that our patients and parents have opinions that may be different than ours, and we will have to agree to disagree,” AAP’s Abraham said.
Block and report. Don’t interact.
Let teens know they should respond to questionable information by unfollowing or blocking it. The same advice is also true for providers who may be tempted to comment on social media posts to debunk misinformation. Engaging with bad information can amplify it, expanding engagement.
“What we know is most effective is actually to report it,” Hsu said. This strategy can be frustrating because reporting may feel like playing WhacA-Mole. “It’s very easy to shut down an account and open another account to post the same thing again. But it’s just part of the battle,” Hsu said. “We have to just keep being engaged.”
Provide an alternative.
When teens encounter false information, doctors can debunk it by correcting the record with detailed factual information. Giving people accurate information up front, or “prebunking,” can also make them less likely to believe false facts, according to the APA.10 Some organizations are
prebunking by using online resource centers and educational outreach to schools, sports teams and even local media organizations.
“Providence has steeped themselves in this, especially when it comes to youth mental health,” Henderson said. “We’ve invested in developing a curriculum that’s free of charge, available to any district in the country.”
The organization collaborated on a free teen mental health website, Work2BeWell.org, which includes a host of validated resources to keep teens in safe corners of the internet, Henderson said. This information includes controversial topics.
Work2BeWell partnered with the documentary Hiding in Plain Sight: Youth Mental Illness to develop curriculum focused on youth mental health, including self-harm. “I heard from a parent recently who was saying, ‘Oh my gosh, if my kid watches this, they’re going to learn about self-harm,’” she said. But it’s far better for teens to learn about a challenging issue in a controlled environment rather than encountering risky content when scrolling alone online.
Establish an online presence.
There aren’t a lot of health care organizations with a strong online presence in the social media sphere aimed at addressing misinformation and disinformation. But that’s slowly changing.
CommonSpirit hopes to establish a foothold on social media channels, such as Instagram, Facebook and LinkedIn, to get evidence-based medicine and health-related information to patients, Jackson said. “It is still pretty new, but we have a social media communications platform strategy,” she said. “We’re really looking at making sure that people are aware of the science of kindness, compassion, empathy and trust.”
Amplify reliable sources.
Teens like to get information online, so providers can help ensure they get accurate information by recommending reliable material. “We verified everything that’s on our Work2BeWell site. Every resource we list has been verified, and we have a 50-state resource list, so there’s something for everybody in every state. It’s all clinically verified and free,” Henderson said. “A lot of sites that seem really credible, as you dig into them, they’re trying to sell you something. And that’s my first red flag.”
It’s far better for teens to learn about a challenging issue in a controlled environment rather than encountering risky content when scrolling alone online.
Speak out when dangerous misinformation arises. Appropriate organization leaders can reach out to local media if particularly troubling information starts to spread online. They’re usually willing to provide information that corrects the record and prevents harm.
Choose the right voice.
Kids tend to be more receptive to information when it comes from peers, so Henderson said they’ve developed tools that include teen voices, such as Work2BeWell’s podcast Talk2BeWell. “We have over 100 podcasts on Talk2BeWell that talk about different youth mental health issues of all shapes and sizes. Having them listen to other teens talk about something [is a] whole lot better than having them listen to a group of adults,” Henderson said.
Take a lesson from others.
Other countries are seeing some success with education initiatives designed to target online misinformation. “I think we can learn from other countries. Sweden and Denmark, for example, have implemented a curriculum in their schools for kids around how they can use social media, and how to discern what’s true and not true,” Jackson said.
MOVING THE NEEDLE TOGETHER
Ultimately, navigating online misinformation and disinformation is a huge challenge for the medical profession, and it’s a problem that won’t be solved anytime soon. However, a team approach can help move the needle.
“I think what we have to do is really work together within our communities, between health care and our educational system and with other parents to network, watch the trends and debunk these myths as a community together when we can,” Henderson said.

KELLY BILODEAU is a freelance writer who specializes in health care and the pharmaceutical industry. She is the former executive editor of Harvard Women’s Health Watch. Her work has also appeared in The Washington Post, Boston magazine and numerous health care publications.
1. “Using Psychological Science to Understand and Fight Health Misinformation: An APA Consensus Statement,” American Psychological Association, https:// www.apa.org/pubs/reports/misinformationrecommendations.pdf.
2. “Confronting Health Misinformation, The U.S. Surgeon General’s Advisory on Building a Healthy Information Environment,” U.S. Department of Health and Human Services, 2021, https://www.hhs.gov/sites/default/files/ surgeon-general-misinformation-advisory.pdf.
3. Tori DeAngelis, “Psychologists Are Taking Aim at Misinformation with These Powerful Strategies,” American Psychological Association, January 1, 2023, https://www.apa.org/monitor/2023/ 01/trends-taking-aim-misinformation.
4. Suzanna Burgelman, “41% of Teenagers Can’t Tell the Difference Between True and Fake Online Health Messages,” August 29, 2022, Frontiers, https://www.frontiersin.org/news/2022/08/29/ psychology-teenagers-health-fake-messages/.
5. DeAngelis, “Psychologists Are Taking Aim at Misinformation.”
6. “Confronting Health Misinformation.”
7. “Health Misinformation,” U.S. Department of Health and Human Services, https://www.hhs.gov/ surgeongeneral/priorities/health-misinformation/ index.html.
8. Tori DeAngelis, “Teens Are Spending Nearly 5 Hours Daily on Social Media. Here Are the Mental Health Outcomes,” American Psychological Association, April 1, 2024, https://www.apa.org/monitor/2024/04/ teen-social-use-mental-health.
9. Brisa Urquieta de Hernandez et al., “A Health System’s Approach to Using CBPR Principles with Multi-Sector Collaboration to Design and Implement a COVID-19 Vaccine Outreach Program,” Journal of Health Care for the Poor and Underserved 33, no. 4 (November 2022): https://dx.doi.org/10.1353/ hpu.2022.0172.
10. “Psychological Science Can Help Counter Spread of Misinformation, Says APA Report,” American Psychological Association, November 29, 2023, https://www.apa.org/news/press/releases/2023/11/ psychological-science-misinformation-disinformation.
With misinformation on the internet growing, so does the need for helping teens distinguish between truths and falsehoods. As health care ministries, we are simultaneously tasked with keeping them safe and giving them access to reliable information.
1. Author Kelly Bilodeau writes in her article that, according to the American Psychological Association, nearly 30% of the information people encounter online is false. This presents a huge challenge for everyone but especially for teens, who may be looking for quick answers and may not be as discriminating as adults when it comes to vetting sources. As health care providers, how can we help teens navigate such a difficult landscape and share reliable resources that they can use instead?
2. Bilodeau also mentions in her article that teens often turn to the internet for answers when the topic is something they are too embarrassed to ask about, such as sexual health, appearance, weight or dieting. What can health care providers do to make teens more comfortable in asking them for help with their most pressing questions, rather than leaning away from them and turning to unreliable sources?
3. According to the article, teens are spending 90% of their social media time on three main platforms: TikTok, Instagram and YouTube. The more these platforms learn about teens’ habits, the more their algorithms influence their choices and what they see on social media. How can we counteract this? As health care professionals, is there a way we can debunk misinformation, such as by creating online resource centers or conducting educational outreach to schools?

CECELIA HORAN, PsyD Director of Child & Adolescent Services, Ascension Illinois Alexian Brothers Behavioral Health Hospital
RICK GERMANN, MA, LCPC Vice President, Behavioral Health, Ascension Illinois
After a presentation on mental health awareness at a local high school in Chicago, a student approached the presenter and informed her that she was feeling suicidal. She even produced a letter she had written for her parents to find after a planned suicide attempt that afternoon. Thankfully, that attempt never occurred because of the mental health programs the school had in place.
In 2021, the Children’s Hospital Association, American Academy of Pediatrics and the American Academy of Child and Adolescent Psychiatry declared a state of emergency in child and adolescent mental health.1 That same year, U.S. Surgeon General Dr. Vivek H. Murthy said that we are facing an urgent mental health crisis in his Surgeon General’s Advisory, highlighting the urgent need to address the nation’s youth mental health crisis.2 In his advisory, he provided actionable recommendations for families, organizations, governments and others to take to improve the mental health of children, adolescents and young adults.
Most recently, in a June 17, 2024, opinion essay in The New York Times, Murthy re-emphasized that the mental health crisis in young people continues to be an emergency.3 Of particular concern is the rising number of young people who contemplate, attempt or die by suicide. The suicide rate among people aged 10 to 24 increased 62% from 2007 through 2021, according to the Centers for Disease Control and Prevention.4
Alarming statistics, published in 2023 by the Children’s Hospital Association,5 include:
More than 6,000 10- to 24-year-olds die by suicide each year.
Close to 2 million adolescents attempt suicide each year.
Among high schoolers, 20% report thinking seriously about suicide.
About 30% of girls said they seriously con-
sidered attempting suicide, double the rate among boys.
Suicide is the second leading cause of death for youth and young adults ages 10 to 24 (25% of all pediatric deaths).
Among LGBTQ+ students, 25% attempted suicide in 2023.
Suicide is the leading cause of death for Asian American youth.
When broken down further, other recent reports6 highlight the following alarming details: Between 2018 and 2021, suicide attempts by Black American youth increased by more than 36%.
Suicide is the third leading cause of death for Latinos aged 10 to 34.
One of the many recommendations from the
Surgeon General’s 2021 advisory was to “expand and strengthen suicide prevention and mental health crisis services.” The advisory specifically cited a need for intensive outpatient programs for children and adolescents.
According to a 2024 World Health Organization and UNICEF report,7 adolescents aged 10 to 19 and approximately 1 in 7 children are affected by mental health conditions, with anxiety, depression and behavioral disorders being the most prevalent.
The increased use of social media has resulted in the U.S. Surgeon General issuing a recent advisory about the impact it is having on youth mental health, indicating a growing body of research about the potential harms of social media.8 This advisory is due in large part to the exposure to inappropriate, violent and extreme content on social media platforms.
Providing screenings, early intervention and intensive outpatient services is key to suicide prevention. One effective model has been implemented at Ascension Illinois Alexian Brothers Behavioral Medicine in Hoffman Estates, Illinois, and has been in place for more than 25 years. Level-of-care screenings are conducted 24/7 for children, adolescents and their families who are in crisis to determine how to safely and effectively recommend and provide the services needed.
Based on presenting symptoms and safety risks, recommendations are given for the appropriate level of care and treatment. Inpatient hospitalization is recommended for youth at immediate and imminent risk of harming themselves or others. Partial hospitalization or intensive outpatient services are recommended for youth who can be kept safe at home but need intensive treatment. Outpatient therapy is recommended for youth who need weekly therapy.
Our Partial Hospitalization and Intensive Outpatient programs are day programs that typically operate for six hours, Monday through Friday. Intensive outpatient programs run three hours a day, three to five days per week. Patients are typically in a program for three to six weeks. The day is structured into a combination of groups focused on different areas, including learning skills to manage challenges, develop alternative actions, and increase motivation and cognitive flexibility.
We also have psychodynamic or process groups, which occur daily, are unstructured and focus on members discussing interpersonal struggles. To round out our holistic approach, we do spirituality and expressive groups. Expressive groups incorporate art, music, movement and drama.
A multidisciplinary team of psychiatrists, clinicians, registered nurses and nurse practitioners, chaplains, teachers and expressive therapists all work together to provide holistic and comprehensive treatment. In addition to medication management and group therapy, family therapy is provided as an integral part of fostering healthy communication and conflict resolution skills, which are necessary for positive growth and outcomes.
Our treatment model is the Ascension Behavioral Treatment Framework (ATF), which is an adaptation of David Barlow’s Unified Protocol9 for the treatment of emotional disorders. It brings together decades of clinical experience and research to provide treatment that is effective across numerous mental health disorders and conditions, including depression, bipolar disorder, anxiety, obsessive-compulsive disorder (OCD), eating disorders, nonsuicidal self-injury and suicide. It is effective because it addresses similar underlying problems in patients suffering from emotional disorders who experience strong and intense emotions, which often lead to negative reactions and behaviors.
These emotionally driven behaviors may temporarily alleviate distress in the moment but ultimately are not effective in the long term. The ATF includes modules that help patients identify emotions and negative thought patterns and how to develop skills to manage their challenges, develop alternative actions, increase motivation and foster cognitive flexibility.
While the ATF is the treatment model for all our partial hospitalization or intensive outpatient programs, we have found that treating our youth with specific diagnoses and symptoms in different programs is most effective. We have programs that specialize in eating disorders, OCD/anxiety and school anxiety/school refusal.
Additionally, within our general adolescent program, we have tracks that focus on chemical dependency, gender/sexual identity issues, communication/social skill deficits and generalized anxiety disorders. Our child programs incorporate a strong behavior management component based on a system where points are determined by
attendance, respectfulness, following directions and positive participation. We also teach parents/ guardians how to use the behavior management system at home. Our belief is that tailoring treatment interventions within our model provides the best outcomes.
In addition, bringing therapeutic interventions into school settings has offered an opportunity for mental health awareness, education and early intervention. Endorsed by leading mental health experts as an effective means to provide treatment to youth, 10 school-based counseling eliminates such barriers as treatment costs and transportation to a mental health center, as well as reduces the stigma of seeking help. Providing less intrusive treatment, such as individual and group counseling at school, results in significant progress, as evidenced by a 41% decrease in hospitalizations of students attending middle and high schools served by our school-based mental health programs.
situations, as often these are the only adults outside of the home who have frequent contact with the students.
In addition to suicide and crisis intervention, school personnel are offered refresher trainings on spotting the signs of abuse and neglect and understanding their responsibilities as mandated reporters when alarming signals appear.
In response to a survey of all school personnel involved in the program at the end of the 2023-2024 school year, 96% of respondents answered that the school program was “extremely valuable,” and 100% responded that they would recommend the program to other schools. One school principal shared this assessment of the program’s effectiveness: “Ascension’s program has had a profound impact on the mental well-being of our students, decreasing student absenteeism and number of psychiatric hospitalizations, while increasing student connections and support systems at school.”
Measuring the effectiveness of our programs and interventions is an integral part of continuing to shape and grow our services. We use standardized and evidence-based measures, which we administer weekly at admission, to guide treatment planning, and again at patients’ discharge. All our measures are self-reported.
This vital component of the service provides teachers and other school personnel with the skills needed to identify and intervene in crisis situations, as often these are the only adults outside of the home who have frequent contact with the students.
The program currently serves a total of 12 middle and high schools throughout the northwest suburbs of Chicago. With consent from students’ parents, services offered include individual and group counseling, crisis intervention and mental health awareness and education. Counselors placed in the schools provide Signs of Suicide training11 to the entire school, including school personnel, aimed at educating academic staff in identifying students at risk of suicide and offering seamless coordination of care to trained responders. This vital component of the service provides teachers and other school personnel with the skills needed to identify and intervene in crisis
While programs that serve children and adolescents have additional measures, the following four measures are standard across all our programs. We use the Brief Adjustment Scale-6 (BASE-6) to measure psychological adjustment; the General Anxiety Disorder-7 (GAD-7) to measure the presence and severity of anxiety; the Patient Health Questionnaire-9A (PHQ-9A) to measure the presence and severity of depression; and the World Health Organization Well-Being Index (WHO-5) to measure current well-being.
Recent data demonstrates the following improvements:
An increase of 39% in mental well-being and a 33% decrease in depression reported in youth participating in our School Anxiety/School Refusal program for the 2023-24 school year.

An increase of 31% in mental well-being and a 56% decrease in depression reported in youth enrolled in our Crystal Lake Child & Adolescent programs.
Clearly, there is a mental health crisis occurring among our youth. The prevalence of mental health issues is increasing. Suicidal ideation, suicide attempts and suicide are on the rise. Emergency room visits for mental health issues are also skyrocketing. Thankfully, there are effective solutions. An investment in continuing and widening treatment and services is warranted. We need to ensure that the attempt never occurs.
Regarding the student mentioned at the beginning of this article, after receiving immediate crisis intervention, she continued with therapy services and successfully worked through her situation. The attempt never occurred; however, what did occur was the opportunity to save a life due to having the right resources available at exactly the right time and place.
CECELIA HORAN is director of Child & Adolescent Services at Ascension Illinois Alexian Brothers Behavioral Health Hospital in Hoffman Estates and Crystal Lake, Illinois. RICK GERMANN is vice president of Behavioral Health at Ascension Illinois.
NOTES
1. “Children’s Hospitals Declare National Emergency in Children’s Mental Health,” Children’s Hospital Association, October 19, 2021, https://www.childrens hospitals.org/news/newsroom/2021/11/childrenshospitals-declare-national-emergency-in-childrensmental-health.
2. “Protecting Youth Mental Health: The U.S. Surgeon General’s Advisory,” U.S. Department of Health and Human Services, 2021, https://www.hhs.gov/sites/ default/files/surgeon-general-youth-mental-healthadvisory.pdf.
3. Dr. Vivek H. Murthy, “Surgeon General: Why I’m Calling for a Warning Label on Social Media Platforms,” The New York Times, June 17, 2024, https://www. nytimes.com/2024/06/17/opinion/social-media-health-
warning.html.
4. Sally C. Curtin and Matthew F. Garnett, “Suicide and Homicide Death Rates Among Youth and Young Adults Aged 10–24: United States, 2001–2021,” NCHS Data Brief, no. 471 (June 2023): https://dx.doi.org/10.15620/ cdc:128423.
5. “Addressing Pediatric Suicide,” Children’s Hospital Association, September 26, 2023, https://www. childrenshospitals.org/content/behavioral-health/ summary/the-state-of-pediatric-suicide.
6. Stephanie Pappas, “More than 20% of Teens Have Seriously Considered Suicide. Psychologists and Communities Can Help Tackle the Problem,” American Psychological Association, July 1, 2023, https://www. apa.org/monitor/2023/07/psychologists-preventingteen-suicide; Caroline Silva and Kimberly A. Van Orden, “Suicide Among Hispanics in the United States,” Current Opinion in Psychology 22 (August 2018): https://doi. org/10.1016/j.copsyc.2017.07.013.
7. “WHO and UNICEF Release Guidance to Improve Access to Mental Health Care for Children and Young People,” World Health Organization, October 9, 2024, https://www.who.int/news/item/09-10-2024-whoand-unicef-launch-guidance-to-improve-access-tomental-health-care-for-children-and-young-people.
8. “Social Media and Youth Mental Health: The U.S. Surgeon General’s Advisory,” U.S. Department of Health and Human Services, 2023, https://www.hhs.gov/sites/ default/files/sg-youth-mental-health-social-mediaadvisory.pdf.
9. David Barlow et al., Unified Protocol for Transdiagnostic Treatment of Emotional Disorders: Therapist Guide (Oxford University Press, 2017).
10. Amanda Sanchez et al., “The Effectiveness of School-Based Mental Health Services for ElementaryAged Children: A Meta-Analysis,” Journal of the American Academy of Child & Adolescent Psychiatry 57, no. 3 (March 2018): https://doi.org/10.1016/ j.jaac.2017.11.022.
11. “Some Secrets Should be Shared: Engaging the Entire School Community in Implementing Evidence-Based Suicide Prevention Programming,” National Center for School Mental Health, https://www.school mentalhealth.org/media/som/microsites/ncsmh/ documents/archives/PS-2.2--Shine--Some-SecretsShould-be-Shared.pdf.

AMY ONOFRE, PhD, LPC Director, Community Advocacy Project for Students, Center for Adolescent Resiliency, Texas Tech University
“Children require the presence of at least one caring person who can provide support for healthy development and learning, engender trust and love, and convey compassion, understanding, respect and interest.” 1
When the time comes to transition from an alternative school setting back to their original or traditional school, students at risk often struggle. Challenges include falling behind academically, returning to negative influences from peer groups, and difficulty readjusting to a less structured environment.2 These students often find themselves caught in a revolving door between the alternative educational setting and their original school.
To empower and advocate for these students, the Community Advocacy Project for Students (CAPS) in Lubbock, Texas, provides focused support through trained and caring adults.3 The vast majority of participants receiving services are secondary students recognized as at-risk, many of whom have been placed in alternative education due to disciplinary infractions.
Most of the young people that CAPS works with are encountered first in alternative placement, but others are referred by school counselors and administrators who believe that the student would benefit from additional support from another caring adult. CAPS trains volunteers to serve as advocates for the young participants and as liaisons for educators and administrators. By being a consistent and caring presence in their lives, advocates help demonstrate to students that their voices matter.
ROOTED IN MIND/BODY RESEARCH
CAPS is housed within the Center for Adoles-
cent Resiliency at Texas Tech University in Lubbock. From 2008 to 2018, the center partnered with Providence member Covenant Health on a project called the Covenant BodyMind Initiative to promote comprehensive adolescent wellness in schools. Covenant’s initiative began as an outreach project to address the prevalence of childhood obesity in Lubbock and the surrounding communities.
The project eventually produced multiple curricular platforms, which provided students in grades 6-12 in traditional school settings an allencompassing approach to what it means to be healthy — physically, mentally, emotionally and spiritually. Covenant BodyMind Initiative staff started teaching the curriculum in a couple of local schools while also providing the curriculum and training to area teachers who wanted to implement it in their classrooms. Through this holistic lens, the issues of a vulnerable population became evident, as staff witnessed some students struggling to get back on track in a traditional
school setting after transitioning there from alternative education, where they had been sent due to behavioral issues.
Based on these observations, the Center for Adolescent Resiliency built close working relationships with local secondary school leaders, who increasingly articulated struggles for students transitioning back to the traditional classroom. For some students, the alternative setting was (and is) a juvenile justice/correctional facility. As a result, CAPS grew from its original initiative of addressing childhood obesity to one focusing on an emergent need to help students transition back to a traditional educational setting.
With the approval and blessing of Covenant Health, the Covenant BodyMind Initiative staff developed an advocacy pilot using the project’s wellness curricula and adapted the program schedule to accommodate time to work one-onone with these students (with parents’ permission), starting with most at their alternative education setting before following them to their traditional schools later.
CAPS’ first program was a six-month pilot in 2018 during the fall semester, and it received additional support from a Wellness and Prevention Community grant from Covenant Community Health Outreach and the resiliency center. Since then, CAPS has paired advocates with nearly 340 students in grades 6-12 through one-on-one support and has additionally served more than 600 students through small group facilitation.
Grounded in a comprehensive wellness philosophy (as shown in the graphic on this page), CAPS programming addresses the whole child physically, socially, emotionally and behaviorally. With a focus on life skills development, the curriculum addresses topics such as healthy relationships, identity, emotional security, physical safety and belonging. It serves as a foundation for the development and adaptations necessary for CAPS’ skill-building program focus.
For students served through the program’s one-on-one advocacy, weekly meetings take place between the advocate and student at their traditional school during a time that works well with the student’s schedule and does not interfere with core classes. These meetings last 30 to 60 minutes and explore goal setting and obstacles through wellness lessons, activities and discus-
Safety and Security
Competence
Belonging
Relationships
Body Image
Physical Activity
Identity Nutrition
Mission and Purpose Perspective
Source: Used with permission from the Center for Adolescent Resiliency, Texas Tech University ©
sions. Advocates use this time to build rapport, explore struggles and offer support. Additionally, if advocates see that students are experiencing any personal challenges or barriers outside the classroom, they help serve as a conduit to relay those needs to the school counselor so students and their families can be connected to appropriate community resources. As shared through a CAPS survey about the program, one student wrote: “I hardly have people that will listen, but you guys listen.”
CAPS advocates also facilitate groups throughout the Lubbock Independent School District to support students struggling with issues such as grief and loss, emotional regulation and bullying. Activities are designed to meet the social-emotional needs of the students, helping them develop skills that empower and move them forward.
The idea of summer often brings thoughts of joy and excitement for children and families. However, this is not the reality for the many students that CAPS serves. It is not uncommon for advocates to eagerly return from the summer and reconnect with their students, only to discover they have either left the school district or their

whereabouts are unknown. For these students, summer may include a lack of extracurricular and relational involvement and resources, along with unsupervised time and increased access to risky situations and activities.
With the assistance of community partners, CAPS piloted programming in 2024 to keep students and volunteers connected through the summer break. CAPS Summer Site, hosted at a church’s gym in Lubbock, offered young people a safe place to connect with CAPS advocates and their peers by participating in art, sports and nutrition challenges. Each week had a wellness theme that influenced activities planned for the day, as well as allowing for free time. Whether painting, jewelry-making, basketball, pingpong or cornhole, students and advocates engaged in fun competitions, calming exercises and opportunities to gather during lunch.

End-of-summer reflections with participants offered valuable insight. Students learned new skills and had something to look forward to each week. Highlights identified by students were socialization, learning new skills, exploring emotional regulation, having access to an all-inclusive and supportive environment and being exposed to different types of physical activity. Based on the success of this pilot, CAPS plans to increase the frequency of meetings during the summer of 2025.
The program’s advocates include community members with diverse professional and personal backgrounds who share a desire to help adolescents reach their full potential. Serving as an approved practicum and internship site and service-learning partner for multiple programs, CAPS attracts many future practitioners from diverse areas of interest.
CAPS prepares and empowers advocates to effectively work within the school system and make a positive impact on their assigned stu -
dents. Advocates are required to pass background checks with both the Lubbock Independent School District and Texas Tech and successfully complete training led by the CAPS team. With financial support from Providence’s Well Being Trust, CAPS also enriches advocate experiences by hosting events that inspire discussion, offer additional training and provide new curricula.
Although CAPS is designed to impact youth participants, reflections with advocates show the impact is reciprocal. “My student truly has changed my life and shown me the power of patience, understanding and human connection,” one advocate shared in a CAPS program survey.
Advocates’ motivation to serve varies. Some get involved to gain professional experience; some want to be supportive adults to struggling young people; and others are fulfilling a class assignment. Some advocates were considered atrisk when young and realized the difference that one caring adult can make. Ultimately, all advocates report gaining something of value through their experience.
According to an African proverb, “It takes a village to raise a child.” CAPS has passionate partners, both internal and external, who create a powerful village for our students.
All young people deserve someone who believes in them, who sees their potential and is determined to help them see it as well. They need to know that their community values them and is rooting for their success. CAPS provides that support.
Collaborations are at the heart of the CAPS program. CAPS could not exist without the generosity and shared passion of others. Covenant Health’s initial grant allowed the program to begin its work and pursue its vision. Since then, Covenant Health has continued to offer counseling for participating students and their families free of charge to support the overall wellness of our community.
All young people deserve someone who believes in them, who sees their potential and is determined to help them see it as well. They need to know that their community values them and is rooting for their success. CAPS provides that support.
Because it is affiliated with Texas Tech, the project collaborates with several academic units, including Counselor Education (in the College of Education) and Nutritional Sciences and Human Development and Family Sciences (in the College of Health and Human Sciences). These collaborations provide curriculum and program evaluation expertise as well as educational experiences through internships, practica and communityengaged learning opportunities. The partnerships prepare future practitioners and provide the project with a steady stream of motivated volunteers to keep our impact strong and open the door to authentic engaged scholarship.
Collaborations allow CAPS to be a vital liaison between health experts, school personnel and highly trained and passionate volunteers. CAPS is proud to serve the youth of our community and to
be an avenue for passionate community members to get involved and learn from their experiences.
“I have never worked with a program that has provided more reliable, relevant, meaningful support of students than CAPS,” said Kristen Lewis, a counselor with Monterey High School in Lubbock who has collaborated with CAPS for several years. “[Advocates] quietly walk alongside these kids as they navigate life in a nonjudgmental and supportive way. They are authentic and genuine in the relationships that they build and they refuse to quit on a student.”
AMY ONOFRE is the director of the Community Advocacy Project for Students in the Center for Adolescent Resiliency at Texas Tech University in Lubbock, Texas.
1. Erik K. Laursen and Scott M. Birmingham, “Caring Relationships as a Protective Factor for At-Risk Youth: An Ethnographic Study,” Families in Society: The Journal of Contemporary Social Services 84, no. 2 (April 2003): 240-246, https://doi.org/10.1606/1044-3894.101.
2. Brianna L. Kennedy, Melanie M. Acosta, and Olivia Soutullo, “Counternarratives of Students’ Experiences Returning to Comprehensive Schools from an Involuntary Disciplinary Alternative School,” Race Ethnicity and Education 22, no. 1 (2017): https://doi.org/10.1080/1361 3324.2017.1376634.
3. “Community Advocacy Project for Students (CAPS),” Texas Tech University Center for Adolescent Resiliency, https://www.depts.ttu.edu/hs/car/caps/index.php.

Finding God in Daily Life
“Nothing
(3 JOHN 1:4) gives me greater joy than to hear that my children are
” walking in the truth.

HELPING YOUTH THRIVE

ROBIN ROENKER Contributor to Health Progress
Dr. Stacy Garrett-Ray will always remember the look of joy and wonder on a young girl’s face the first time she heard the human heart through a stethoscope.
“To let a child listen to your heart, it’s a very touching experience,” said GarrettRay, senior vice president and chief community impact officer for Ascension. The health system’s Foundation for Health Equity connects middle schoolers with a day of hands-on health care-related activities through its #GOALS (Go Out and Love Science) program.
The program’s hope is simple: to allow more kids from diverse socioeconomic and racial backgrounds to imagine themselves from an early age pursuing careers as doctors, nurses or other health care professionals.
As a Black woman physician, Garrett-Ray is keenly aware that she is an underrepresented demographic in medicine — currently just under 6% of U.S. doctors are Black,1 even though nearly 14% of the U.S. population is Black.2 Similarly, only 7% of American doctors and nurses are Latino, while Hispanic Americans account for roughly 19% of the U.S. population.3
Closing these representation gaps in medicine matters. Studies have repeatedly proven the value of a diverse health care workforce: Patients of color typically report greater trust and satisfac-
tion in their care — as well as better overall health outcomes — when matched with care providers who look like they do.4
But waiting to achieve better balance by tracking medical and nursing school enrollment numbers is too late. To effectively fill open jobs with qualified, diversified candidates, hospital administrators are increasingly realizing that they must start reaching kids from a broad range of backgrounds even earlier.
As a result, many Catholic health care systems, like Ascension, now sponsor or host programs aimed at fostering middle and high school students’ excitement about medicine as well as science, technology, engineering and mathematics (STEM), allowing them ample time to explore career pathways and find the right fit.

“You’ve got to think not just short-term, but also long-term, about how to really address the disparities,” Garrett-Ray said. “It’s got to be an investment that all organizations do together. It’s not just one of us that needs to be doing this in the community. It takes partners to be able to create this and invest in our future … to ensure that we have sustainable and high-quality care that is reflective of the communities in which we serve.”
Leaders say one key value of targeted outreach programming lies in its ability to open doors of
possibility — both in terms of higher education and career paths — that students otherwise might not have considered for themselves.
For example, Mercy Health has successfully partnered with Junior Achievement of Northwestern Ohio to offer high school students oneday job shadowing opportunities across its Toledo system footprint.
Students spend the morning following a Mercy staff member in their selected job track, from physicians, nurses, lab or imaging techs, and physical, occupational or speech therapists to administrative and support roles like social work, law

enforcement, facilities maintenance or information technology.
Then, during the afternoon, students visit Mercy College of Ohio in Toledo to learn about educational pathways and potential scholarship opportunities to pursue their fields of interest. Launched in 2022, the program has grown quickly and now serves more than 150 students over four event days each school year.
“One huge upside that we did not anticipate was the energy that these events bring to the employee side,” said Matt Sapara, vice president of business development and advocacy for Bon Secours Mercy Health. “Our employees see how hungry these kids are to learn about opportunities in health care, and it’s a real boost to our staff. We have never had an issue with getting enough volunteers to take these kids in and work a shift with them.”
In Buffalo, New York, Catholic Health offers a similar one-day exploration experience for high school students called Volunteer to Career. Offered two times each school year, the event lets a small group of six to eight students tour multiple hospital units, from the cath lab and radiology unit to surgery and physical therapy.
it elsewhere.
“We have some students who realize from this [job shadowing] event that they actually don’t like the sight of blood. From my perspective, I consider that an equal success,” he said. “In those cases, we’ve eliminated that student running down a path where they may spend a couple of years in college, otherwise, before getting to their clinicals and realizing this isn’t for them.”
In Ripon, Wisconsin, high school senior and certified nursing assistant Payton Ronson starts her day at 6:15 a.m. at SSM Health Ripon Community Hospital, where she works a three-hour shift before completing a full school day at nearby Laconia High School.
“I really like the environment in the emergency department, and the people are great to work with,” Ronson said. “If I don’t feel comfortable doing something, I’m not afraid to say, ‘I don’t know how to do this. Can you help me?’”
Ronson is just one of 60 Wisconsin high school students completing on-site health care training at SSM Health through its partnership with the Wisconsin Youth Apprenticeship Program. Supported by the Wisconsin Department of Workforce Development, the youth apprenticeship allows qualified juniors and seniors to earn high school course credit while completing a paid internship in their chosen career path.
“One huge upside that we did not anticipate was the energy that these events bring to the employee side. Our employees see how hungry these kids are to learn about opportunities in health care, and it’s a real boost to our staff.”
— MATT SAPARA
“I arrange the tour ahead of time with the various department managers,” explained Lisa Carey, supervisor of volunteer services for Catholic Health. “Each area gets about half an hour with the students, where they will go over the department, what role it plays in our hospital, and how it helps our patients.” At the end of the day, Carey shares information about volunteering or other training opportunities so students can pursue their health care interests.
Sapara believes that exploratory days are critically important, whether they solidify students’ excitement about health care careers or redirect
“They’re getting employability skills while they’re getting those academic and classroom skills,” explained Roderick Nunn, SSM Health’s vice president of diversity, equity and inclusion. “Students end up working 10 to 15 hours per week in our health ministries making $18 or more per hour. They have the opportunity to learn and earn, and, in the process, consider health care as a long-term career.”
“It’s a refreshing change of pace, in the ER especially, to get these young people on board, to show them what ER medicine is about, and to help them to use those skills,” said Ashley Kolberg, RN, emergency department nurse manager at Ripon Community Hospital.
Emma Hersey, a senior at Lincoln Academy in
Beloit, Wisconsin, is currently serving as an imaging intern with SSM Health St. Mary’s Hospital — Janesville. In that role, she spends every other school day at the hospital, where she transports patients for scans, sees their images and gains hands-on experience that has furthered her interest in a radiology career.
“It’s been fun to see how everything comes together to get a proper image,” Hersey said. “It requires a lot more work than I knew before.”
According to organizers, part of these programs’ power is their ability to tap into students’ innate curiosity about science and medicine.
In St. Louis, Mercy’s Teens Learning in the Community program offers 50 high school students the chance to spend seven weeks in the summer exploring at least four different health care sectors. Students attend twice-a-week, fullday experiences that include on-site visits and lunch-and-learn sessions with various departments at Mercy Hospital St. Louis. In the process, they come away with a deeper understanding of niche health care careers they may not have heard about before.
During past summers, for example, students have visited the hospital’s cancer center and learned about its new proton therapy machine, which uses precise, high-energy proton beams to treat cancer. They have learned about the surgical center’s CyberKnife and da Vinci surgical tools, and they’ve seen firsthand how teams at Mercy Hospital St. Louis’ Virtual Care Center use technology to provide telehealth services.
“During another session, we went to our helipad and met with a pilot and a couple of the nurses that work on the life flights [which transport critically ill or injured patients]. The students are always really inspired by getting to hear from people about what they do. It’s so great to see these experiences spark something within them about their own plans for their future career,” said Sarah Funaiole, manager of volunteer and guest services for Mercy Hospital St. Louis.
Ascension’s teams work to play up the fun aspects of STEM and health care careers during each #GOALS day, too. Every year, middle school students rotate through hands-on workshops where they experience lessons beyond those possible in a regular school classroom. During recent sessions, kids learned how to close a wound using

every other school day at SSM Health St. Mary’s Hospital — Janesville serving as an imaging intern in training offered through the health system’s partnered effort with the Wisconsin Youth Apprenticeship Program.
suture practice kits, simulated surgery using a 6-foot Operation game, and performed CPR to the beat of the famous Bee Gees song “Stayin’ Alive.”
Each year, the #GOALS program buses students from Nashville’s Haynes Middle School to Meharry Medical College, also in Nashville, where medical school staff and students, along with Ascension team members, help lead activities.
As a historically Black college, Meharry is responsible for training a large percentage of America’s Black doctors and dentists, and organizers with #GOALS say the opportunity for minority students to interact with medical students from similar backgrounds is what sets the program apart.
“It’s not that these students have never thought about health care. It is often that someone has actively told them it’s not something they should consider [perhaps due to doubts about access or
affordability]. … And we just want to reverse that narrative,” said Robyn Kress, senior vice president of Ascension Foundation.
Following the success of the annual program in Nashville, Ascension Foundation has partnered with other medical schools to bring #GOALS to other cities on a traveling basis, including Detroit and New Orleans. Before and after each #GOALS session, students are polled to determine how many may want to go into health care. The number always goes up after the event.
At a recent #GOALS session, a seventh-grade boy leaned over to Kress and said, “I’m really good at sutures. I’m going to be a PA [physician assistant] one day.” Kress asked if he had known what a PA was before that day.
“And he said, ‘No, but I’m going to do it.’ And it was just so cool,” Kress recalled.
Of course, youth outreach programming is just one piece of the puzzle when it comes to filling open jobs across the U.S. health care system. Initiatives to offer job training and placement incen-
tives for college-aged students and working adults are key as well.
Rather than operating such programs independently, most health care systems offer a combination of them.
For example, in addition to its long-standing student outreach, Catholic Health recently launched a new, formal internship focused on nonclinical roles at multiple hospitals throughout its system. The program gives participants a chance to hone marketable job skills during an eight-week, paid internship in areas such as hospital communications, legal support or finance.
“We developed this program to bridge the gap between finding talent for these nonclinical positions, but also the gap that students experience when they graduate of always needing experience in order to land that first job,” said Daniel Castelli, human resources corporate recruiter for Catholic Health.
With funding from a grant through the City of Buffalo, Catholic Health also recently launched a new apprenticeship program for existing employees. Through it, current staff members from

Middle school students learn how to close a wound using suture practice kits during a day of learning through Ascension’s #GOALS program.

“It’s not that these students have never thought about health care. It is often that someone has actively told them it’s not something they should consider [perhaps due to doubts about access or affordability]. … And we just want to reverse that narrative.”
— ROBYN KRESS
historically underserved ZIP codes can receive paid training toward new, higher-paying career trajectories within the hospital.
“In a paid, controlled environment, we’re letting them actively shadow departments that they have an interest in, such as nursing or radiology, and from there, they’re also doing professional leadership training classes so that they’re learning how to be an effective leader once they start to pursue their new career,” Castelli explained.
Since 2017, CommonSpirit Health has partnered with area community and vocational colleges to offer a range of health apprenticeships open to participants with at least a GED or high school diploma. These positions offer paid, on-the-job training in specialties for which CommonSpirit routinely has open positions, including certified medical assistants, sterile processing technicians and pharmacy technicians.
“Positions were sitting open for months on end, and it was easier for us to expand the population we could recruit from, bring people in, train them and get them certified in six months. In some cases, that was faster than sitting and waiting for someone with that certification to apply,” said Jaime Pearson, CommonSpirit Health’s senior recruiter for workforce development and talent acquisition.
Participants in the program typically attend classes one day a week and spend the other four workdays training in clinic. Their work time is paid, and they receive tuition support to offset the cost of their certification program.
The upside for CommonSpirit: Many apprentices stay on as full-time staff after they complete their training.
“They want to stay with our organization because they see that investment in them and
their growth,” Pearson said. “And the win for us is that once they’re certified, they hit the ground running because they’ve spent six months getting to know our processes and procedures.”
Collectively, hospital systems’ various outreach and training programs recognize that tomorrow’s health care workforce will be stronger — and more diverse — when people of all backgrounds can access a variety of pathways to explore health care as a career.
ROBIN ROENKER is a freelance writer based in Lexington, Kentucky. She has more than 15 years of experience reporting on health and wellness, higher education and business trends.
1. Patrick Boyle, “What’s Your Specialty? New Data Show the Choices of America’s Doctors by Gender, Race, and Age,” Association of American Medical Colleges, January 12, 2023, https://www.aamc.org/news/what-s-yourspecialty-new-data-show-choices-america-s-doctorsgender-race-and-age.
2. “Quick Facts,” United States Census Bureau, https://www.census.gov/quickfacts/.
3. Alec Tyson and Mark Hugo Lopez, “5 Facts About Hispanic Americans and Health Care,” Pew Research Center, October 30, 2023, https://www.pewresearch. org/short-reads/2023/10/30/5-facts-about-hispanicamericans-and-health-care/.
4. LaShyra Nolen, “Good Health Care Is Rooted in Evidence. So Is DEI.,” Harvard Public Health, June 25, 2024, https://harvardpublichealth.org/equity/ diversity-in-healthcare-is-good-for-physicians-andpatients-alike/; Dr. Monica E. Peek, “Increasing Representation of Black Primary Care Physicians — A Critical Strategy to Advance Racial Health Equity,” JAMA Network Open 6, no. 4 (April 2023): https:// doi.org/10.1001/jamanetworkopen.2023.6678.
Duquesne University offers an exciting graduate program in Healthcare Ethics to engage today’s complex issues.

Courses are taught face-to-face on campus or through online learning for busy professionals.
The curriculum provides expertise in clinical ethics, organizational ethics, public health ethics and research ethics, with clinical rotations in ethics consultation.
Doctoral students research pivotal topics in healthcare ethics and are mentored toward academic publishing and conference presentation.
MA in Healthcare Ethics (Tuition award of 25%)
This program requires 30 credits (10 courses). These credits may roll over into the Doctoral Degree that requires another 18 credits (6 courses) plus the dissertation.
Doctor of Philosophy (PhD) and Doctor of Healthcare Ethics (DHCE)
These research (PhD) and professional (DHCE) degrees prepare students for leadership roles in academia and clinical ethics.
MA Entrance – 12 courses
BA Entrance – 16 courses
Graduate Certificate in Healthcare Ethics
This flexible program requires 15 credits (5 courses). All courses may be taken from a distance. The credits may roll over into the MA or Doctoral Degree (PhD or DHCE).


SR. LISA MAURER, OSB Director of Mission Integration and Formation for Duluth Benedictine Ministries
Iknow from being an assistant football coach that there are endless formations, designs, schemes and combinations that can be part of an offensive playbook. Yet, it boils down to what a quarterback can do with a football, which is to run it, hand it off or throw it. Life, too, is full of a myriad of philosophies to follow. There are many ways you can run your life. You can fill your playbook with countless plays.
Having a playbook, as any good coach knows, is needed to be prepared to react to whatever comes your way. The middle of the game is not the time to come up with a plan and assess your options. The same is true in life. A personal playbook is needed to guide you as you travel life’s — and especially the health care landscape’s — winding and often uncertain road. Having a well-prepared, well-defined and refined playbook gives you a solid foundation and helps you to act with confidence. This playbook should be full of your fundamental values and guiding principles.
God has blessed us with the greatest playbook of all: the Bible. And God has given us Jesus to show us how to use that playbook. Jesus has demonstrated for us how to live, explained the plan, shown us the values, and taught us how to internalize God’s playbook. He instructed us to write it in our hearts so that it becomes who we are, rather than just something we do.
It is up to each of us to follow Jesus’ example and take God’s message and make it our own. As people created in the image and likeness of God,
we have it in ourselves to do just that. God wants us to live lives of holiness and goodness, and dreams for us to live life to the fullest.
Having a well-developed playbook is a good resource for ourselves and useful when working with others, especially young people. When working with student-athletes, I often talk to them about the values that not only make them good players and teammates but also good people. Being a person of good character, I remind them, is more important than the numbers on the scoreboard.
Encouraging young people to seriously build their own playbook is essential. If you don’t know what your values are, it is easy to go through life acting and reacting according to someone else’s moral compass, and that could lead you down the wrong path. Every person, no matter their age, has the light of life within them, the propensity for good and the longing for God. Building a valueladen playbook is where to start living a good life.
I offer you four plays from my personal playbook. These four values are the foundation of

how I strive to live my life. These values have proven to lead me to goodness and happiness. They have anchored my life in storms, inspired me in difficulties, and made any good day just a little bit brighter.
Maybe because I am a Benedictine, I think of hospitality as the first value to put in my playbook. As Benedictines, we think of hospitality all the time. It is one of our hallmarks. Now, when I say hospitality, I don’t simply mean offering coffee and cookies to a visitor. It is much more than that. It is about creating a welcoming atmosphere and extending acceptance to all.
Hospitality even goes beyond welcoming people. It calls for accepting all that God has to
offer you, the sun and the rain alike. Hospitality says that we welcome God’s gifts no matter how they come to us, whatever their disguise. Having the value of hospitality in your playbook allows you to be flexible and accepting of all people and situations.
No playbook is complete without the value of stewardship, taking care of what has been given to you and using it for the glory of God and the good of the Kingdom. Each of us has been entrusted with gifts, talents and the resources of time and treasure. Everything we have comes from and belongs to God, and we are responsible for being good stewards. Having the value of stewardship in your playbook invites you to take
Respect begins with cherishing and promoting the worth of all human life. It is treating people with dignity and wanting the best for them.

a count of your blessings and gives you reasons to trust in God.
PLAY #3: RESPECT
I don’t like to rank the values in my playbook, but if I did, I would put respect at the top. Even though you need a fully stacked and well-rounded playbook to live a full life, you can’t go wrong with having respect as your overarching value. I believe if you get respect right, then everything else will fall into place.
Respect begins with cherishing and promoting the worth of all human life. It is treating people with dignity and wanting the best for them. Respect is a way of thinking about or looking at people, places and things. Having respect in your playbook will keep you in right relationship with God, others and yourself.
PLAY #4: JUSTICE
One might not think of justice as a value that should be in a personal playbook. We might think it is only appropriate for lawyers, politicians or Superman (with his motto of truth, justice and a better tomorrow). Yet, we are called to be people of justice. When we live the value of justice, we are basing our decisions and actions not only on what is good for ourselves but also on how they affect the lives of others.
I know my mom told me more than once that I was intended to always do what I am meant to do
in the way I am supposed to do it. Having justice in your playbook will keep you in line with God’s dream for the world.
There you have it: my four plays for living a good life. With these four plays in my playbook, I can navigate anything life throws at me. They allow me to pivot and adjust. They keep me centered and on the right path. They help me become who and how God intends me to be.
Make a list of the four values that are most important to you. Define those values and think of practical ways to put them into action.
Reflect upon those people who have influenced you in developing your moral compass. What values did they teach you? How did they encourage you to find the values that are important to you?
How might you use values to help youth thrive? In what ways can you encourage youth to live a value-centered life?
With a value-laden playbook in place, the ability to spark the light of a good life within others is possible. Great players will inspire others.
SR. LISA MAURER, OSB, is the director of mission integration and formation for Duluth Benedictine Ministries. She is also the director of vocations and formation for her monastic community and serves as an assistant football coach at the College of St. Scholastica.
For just this moment, bring your attention to your breath.
For just this moment, bring your attention to your breath.
For just this moment, bring your attention to your breath.
INHALE deeply and settle yourself into your body.
For just this moment, bring your attention to your breath.
INHALE deeply and settle yourself into your body.
INHALE deeply and settle yourself into your body.
EXHALE the stress and tension you feel.
EXHALE the stress and tension you feel.
EXHALE the stress and tension you feel.
INHALE deeply and settle yourself into your body.
In these days of anxiety, a moment to pause is both a gift and a necessity.
In these days of anxiety, a moment to pause is both a gift and a necessity.
In these days of anxiety, a moment to pause is both a gift and a necessity.
EXHALE the stress and tension you feel.
For just this moment, bring your attention to your breath.
GENTLE YOUR BREATHING, your gaze and your heart as you consider: Where have I found peace in the past days?
GENTLE YOUR BREATHING, your gaze and your heart as you consider: Where have I found peace in the past days?
INHALE deeply and settle yourself into your body.
In these days of anxiety, a moment to pause is both a gift and a necessity.
GENTLE YOUR BREATHING, your gaze and your heart as you consider: Where have I found peace in the past days?
THINK FOR A MOMENT.
THINK FOR A MOMENT.
THINK FOR A MOMENT.
EXHALE the stress and tension you feel.
GENTLE YOUR BREATHING, your gaze and your heart as you consider:
In these days of anxiety where have I found peace?
In these days of anxiety where have I found peace?
In these days of anxiety where have I found peace?
In these days anxiety, a moment to pause is both a gift and a necessity.
Where have I found peace in the past days?
[Pause to consider]
[Pause to consider]
THINK FOR A MOMENT.
[Pause to consider]
GENTLE YOUR BREATHING, your gaze and your heart as you consider: Where have I found peace in the past days?
THINK FOR A MOMENT.
In these days of anxiety where have I found peace?
DWELL in the peace you have found and bring it with you into the rest of your day. Even now, God is with you, as near to you as your breath. Continue giving yourself the gift to pause, breathe and heal, knowing you are not alone.
DWELL in the peace you have found and bring it with you into the rest of your day. Even now, God is with you, as near to you as your breath. Continue giving yourself the gift to pause, breathe and heal, knowing you are not alone.
[Pause to consider]
In these days of anxiety where have I found peace?
DWELL in the peace you have found and bring it with you into the rest of your day. Even now, God is with you, as near to you as your breath. Continue giving yourself the gift to pause, breathe and heal, knowing you are not alone.
[Pause to consider]
DWELL in the peace you have found and bring it with you into the rest of your day.
Peace I leave with you; my peace I give you. I do not give to you as the world gives. Do not let your hearts be troubled and do not be afraid. JOHN 14:27 © Catholic Health Association of the
Peace I leave with you; my peace I give you. I do not give to you as the world gives. Do not let your hearts be troubled and do not be afraid. JOHN 14:27
DWELL in the peace you have found and bring it with you into the rest of your day. Even now, God is with you, as near to you as your breath. Continue giving yourself the gift to pause, breathe and heal, knowing you are not alone.
Peace I leave with you; my peace I give you. I do not give to you as the world gives. Do not let your hearts be troubled and do not be afraid. JOHN 14:27
Even now, God is with you, as near to you as your breath. Continue giving yourself the gift to pause, breathe and heal, knowing you are not alone.
© Catholic Health Association of the United States
© Catholic Health Association of the United States
Peace I leave with you; my peace I give you. I do not give to you as the world gives. Do not let your hearts be troubled and do not be afraid. JOHN 14:27
© Catholic Health Association of the United States
Peace I leave with you; my peace I give you. I do not give to you as the world gives. Do not let your hearts be troubled and do not be afraid. JOHN 14:27
© Catholic Health Association of the United States

DAVID LEWELLEN Contributor to Health Progress
Two high chairs stand next to an assortment of wheelchairs and walkers in the corner of the dining room at Trinity Woods. Mealtimes for the independent living residents at the facility, located on Mount Mary University’s campus in Milwaukee, are often shared with the school’s students, and some of the apartments are reserved for single mothers of young children.
“We love the little people running around,” said Sr. Martha Waligora, SSND, who has lived in the facility since it opened. “We give them power; they give us power. You can’t feel old in here, because so much is going on.”
Trinity Woods, which opened in 2021, is a collaboration among Trinity Senior Services, a longestablished management company that operates Catholic long-term care facilities; Mount Mary University; and the School Sisters of Notre Dame.1 Under one roof, the facility offers 90 independent living units; 54 assisted living units for aging sisters; 24 units of student housing; and a separately owned day care center that serves the community. It was designed from the ground up to meet the needs of aging populations, students and children, and it represents a hopeful new trend in housing policy.
The somber atmosphere of many senior living centers may result from the monoculture of age, in which young faces and outlooks are rare. But many programs are seeking to put the generations back together, whether through innovative living arrangements or pairing older and younger peo-
ple for social activities. In either case, participants talk about the resulting sense of social connection and meaning in their lives.
“We’ve artificially segregated generations for years,” said Donna Butts, executive director of Generations United, a Washington, D.C.-based advocacy group.2 “When we plan facilities, they’re stratified by age — school is for kids, senior centers are for seniors only.”
Shannon Jarrott, PhD, a professor of social work at Ohio State University, agreed that silos of funding and agencies keep the thinking separate, such as separate programs to provide meals for low-income students and low-income seniors.
At the level of national policy, “we wish change was quicker,” Butts said. “We have an aging population, and it’s not just about the last year of life anymore.” But she has noticed that new housing policies are tilting in favor of building “not a teen center and a (separate) senior center, but a community center.”
In the case of Trinity Senior Services, “we were blessed,” said CEO David Fulcher. “There was an opportunity and adjacent land, and we ran with it.” The biggest obstacle to such facilities, he said, is finding land directly beside a
university or other institution that’s oriented to younger people. But developers who are creating major new town centers from scratch have an opportunity to include senior housing as a natural part of the greater whole. “It’s meaningful, purposeful, natural interaction,” he said.
At Trinity Woods, the collaborations extend in many directions. Residents can audit courses for free at the university, and students come in to offer art therapy. The children at the day care center visit twice a month for “book nook,” pairing elders and kids for read-aloud time, and most major holidays feature a children’s parade through the retirement center’s hallways. “We call it, ‘Let’s go and wave hi to the grandmas and grandpas,’” said Jenele Baldwin, director of the day care center, “and they [the children] love it.”
For people who want social connection without moving, programs to put the generations back together need some structure. Butts said that once a week seems to work well, and so does a shared purpose, such as music, crafts or service projects. A one-shot visit to a nursing home could be “more harmful than helpful, if it’s not done well,” she said. “If kids see wheelchairs, smell things they haven’t smelled before, it can be terrifying.” But in regular visits with advanced preparation, young children become accustomed to disability in general and learn to process death as part of life.
Pairing one older person and one younger person is a best practice. Ohio State’s Jarrott said, “If you want to build relationships, you have to give people a chance to get to know each other.”
Jarrott has seen many programs falter or die because one person left or because funding dried up. But if intergenerational connection is explicitly part of the group’s mission, then new hires will
know that they are not just a day care teacher or a retirement home activities director.
In the bigger picture, Butts said, everyone needs meaning and purpose in their lives, and older people are vulnerable to loneliness and isolation, whether in retirement homes or not. She talks wistfully about a “prescription for purpose,” in which older people might also get a flyer with information about local intergenerational programs along with their medications. The recent surgeon general’s report on loneliness identified older adults and young adults as the most isolated groups, and Butts said, “It only makes sense to connect those two generations.”3
One program that tries to do just that is Perfect Pair, which matches long-term care residents with nearby college students.4 Founded in 2020 at the University of Michigan, the program now includes 20 colleges and has an average of 20 matches per school.
“We wanted this to be mutually beneficial,” said Kamryn Casey, the program’s national director of community engagement. College students may be offering their matches a glimpse of the busy outside world, but they also need a different kind of connection themselves. “It’s almost a grandparent-like figure,” Casey said. “They’ll ask for advice about roommates or classes. And the older people like to hear about their daily lives.”
“There’s an idea that older people need this more than young people do,” Jarrott said — and that idea is wrong. Children and youths may be in the center of a village that is raising them, “but we know that more kids need a bigger village.”
For Perfect Pair, older and younger generations who wish to be paired fill out a questionnaire, and the team matches them based on a shared interest. “Our student wait list is longer than our adult wait list,” Casey said.
“There’s an idea that older people need this more than young people do” — and that idea is wrong. Children and youths may be in the center of a village that is raising them, “but we know that more kids need a bigger village.”
— SHANNON JARROTT

Another program to link college students into the greater world is Opening Minds through Art (OMA), which encourages adults with dementia to create artwork. Since beginning at Miami University of Ohio in 2007, the program, which is headquartered at the university’s Scripps Gerontology Center, has spread to about 300 locations, pairing college students (or other volunteers) with residents of local retirement homes.5
Noelle Naccarato, a senior at Miami University who is now on her fourth match, said she has learned to “talk like a human,” resisting the impulse to speak too slowly and too loudly. “You have to be aware, but you also have to just be yourself.”
Naccarato already has contact with the older generation through her grandparents, but it’s a different feeling to interact with people who are meeting her as a young adult, without memories of her childhood. Her peers say that it has changed
their attitude toward older adults and improved their communication skills.
“In nursing homes, people feel like they’re care recipients,” said OMA Assistant Director Krysta Peterson. “There’s always someone telling them what to do, shuttling them around, saying, ‘it’s time to get up,’ or ‘it’s time to eat.’” But in the art setting, “choices are built in. They choose their paint, they very much direct their art project.”
In the bubble atmosphere of a college campus, meeting someone from a different age group has to be an intentional act. “If you’re participating, you’re already saying that you want to learn, and we train you to make the connection,” Peterson said. “Lots of participants will say, ‘I’m not an artist, I don’t know how to do this.’ Even facilitators will say, ‘I do bingo.’ But the art is there for the purpose of connection.”
Among the many locations that have modified the OMA program for their location is Richmond
Aging and Engaging, a new nonprofit that brings college students into three low-income senior housing complexes in Virginia’s capital. “A sense of purpose is important for health,” said Executive Director Jodi Winship, PhD, “and we’ve found that people in this community don’t have a lot of things to do.”
Winship recruits students to visit the units every week, doing activities that the residents have chosen. One site likes physical activities, such as cornhole and “balloon pickleball.” Another prefers crafts or board games.
Taking a break from academic work helps students’ mental health, too, Winship said. And students from the medical or pharmacy schools are “practicing their interpersonal skills and learning about future patients,” she said. “They can see why low-income patients can’t follow doctors’ instructions, or [they can see] the barriers of mental illness.”
Students are told beforehand that “you may see bugs on the floor, or you may be partnered with someone whose child has been murdered,” Winship said. “Don’t freak out.”
Older adults need a reason to get out of bed every day, Winship said, and meeting a blood sugar goal may not feel like much of a reason. “But if they can learn something new or do something engaging with students and friends, that’s a reason. They’re competitive at balloon pickleball. They’ll say, ‘I’m going to beat Gloria this week.’”
Older adults who live on their own also have options to keep in touch with the younger generation. In Billings, Montana, St. Vincent Regional Hospital sponsors the AmeriCorps Foster Grandparent program, which recruits low-income adults ages 55 and up for placement in schools and Head Start programs to serve as classroom helpers.6
“They’ve raised their own children, and they want to help with the next generation,” said Program Coordinator Lisa LaMere. “They don’t do it for the $4 an hour stipend. They do it for the kids. None of them see it as work.”
St. Vincent, and before it the Sisters of Charity of Leavenworth, has sponsored the federally funded program in the community since 1971. The
health system offers benefits to participants, such as free flu shots. The social connections with both their peers and children give senior participants “a reason to pay attention to their health,” LaMere said.
John Landry, who retired to Billings three years ago, has found fulfillment in a kindergarten classroom. “The kids call me Grandpa John,” he said. “Last year’s kids, who are in first grade now, they’ll see me in the hall and come running up and hug me.”
Landry is 60 and in his second year of working with a 23-year-old teacher, which has been another broadening experience. “I’m learning with the kindergartners how to do computers and iPads,” he said.
And of course, not everything happens under a formal program. Butts, of Generations United, said that the kids on her cul-de-sac enjoy hanging out with her 70-year-old husband. “We encourage people to dabble their toe,” she said. “Start with little things, and it will grow. Don’t be overwhelmed by a program. It could just be checking on an older neighbor.”
Ohio State’s Jarrott added: “The potential of these programs is only limited by our imagination. We need people in all disciplines — design, urban planning, you name it. We need each other.”
DAVID LEWELLEN is a freelance writer in Glendale, Wisconsin.
1. “Trinity Woods — An Intergenerational Community,” Trinity Senior Services, https://trinityseniorservices. org/trinity-woods/.
2. Generations United, https://www.gu.org.
3. “Our Epidemic of Loneliness and Isolation 2023: The U.S. Surgeon General’s Advisory on the Healing Effects of Social Connection and Community,” U.S. Department of Health and Human Services, https://www.hhs.gov/ sites/default/files/surgeon-general-social-connectionadvisory.pdf.
4. Perfect Pair, https://www.perfectpair.org.
5. Opening Minds Through Art, https://scrippsoma.org.
6. “St. Vincent Healthcare Foster Grandparent Program,” United Way of Yellowstone County, https://uwyellowstone.galaxydigital.com/agency/ detail/?agency_id=80353.
NANETTE ELSTER, JD, MPH, and KAYHAN PARSI, JD, PhD, HEC-C Neiswanger Institute for Bioethics, Loyola University Chicago Stritch School of Medicine
Transition is both a verb and a noun. In its most general sense, it means, according to The Merriam-Webster Dictionary, “a change or shift from one state, subject, place, etc. to another,” and the “period or phase in which such a change or shift is happening.”
A more medicalized definition of transition is “a purposeful, planned process that addresses the medical, psychosocial, educational and vocational needs of adolescents and young adults with chronic medical conditions, as they advance from a pediatric and family-centered to an adult, individual focused health care provider.”1
Transition, however, encompasses more than chronic medical conditions. We also recognize that various transitions occur throughout our lifetime, but the shift from adolescence to adulthood creates unique challenges and opportunities. This transition takes years and is a process, not an event. Key markers of transition include housing, employment, education, voting, driving, health care, marriage and contracting.
Critical to each of these markers of adulthood is the legal ability — and requirement, in many instances — to make these decisions for oneself, which can be both challenging and fortifying. Determining how such decisions are made — and who can make them — is essential during the transition period. The determination of who has the authority to make decisions is particularly pronounced for autistic and neurodivergent individuals. Some of them may have intellectual challenges, while others will not — but might be presumed to have limited capacity.
According to the latest data from the U.S. Centers for Disease Control and Prevention (CDC), approximately 1 in 36 children have been identified as autistic.2 Both data and services related to autism have focused primarily on children, and thus the transition to adulthood for autistic individuals and their families is often described as “falling off the cliff.” This metaphor describes the abrupt move from a model of entitlement with a full range of coordinated social and medical services to a model of mere eligibility for services at the state and federal levels.
Although a model of entitlement can pose challenges for autistic individuals in accessing services, a model of eligibility poses even greater barriers. As Anne Roux, director of Research and Policy Impact at A.J. Drexel Autism Institute, and her collaborators have stated:
Upon exiting secondary school, youth and
their families must navigate a complex and fragmented system of eligibility for adult services, which include Vocational Rehabilitation (VR), Developmental Disability (DD) services, safety net benefits like Supplemental Security Income (SSI), public health insurance like Medicaid, and Medicaid waivers, which cover services and supports not typically available through health insurance.3
While nearly 40% of autistic people have an intellectual disability (ID),4 according to the CDC, that alone does not necessarily render one incapable of making their own decisions. Even without an ID, an individual’s level of executive functioning can inhibit their ability to identify, apply for and access services. Additionally, the capacity for decision-making may wax and wane, and the types of decisions that must be made can range from minor to significant. For instance, the decision to consent to a flu shot may be less onerous than the ability to consent to major surgery.
Moreover, an autistic individual may have the ability to express their goals and values with certain clinicians but not others. Scheduling, planning and participating in medical and dental visits may be easier or more difficult, depending on one’s executive functioning skills. At all times, however, the autonomy and dignity of the autistic person must be respected. Therefore, a range of decision-making options are available to consider as one moves from childhood to adulthood and throughout one’s life span.
views of autistic adolescent and adult clients, especially those with co-occurring intellectual disability and/or language impairment. This harmful perspective may contribute to the assumption that these clients are unable to direct their own treatment and result in deriving treatment goals from caregivers’, rather than clients’, presenting concerns.5
Guardianship, however, is often seen as a last resort, as the guardian assumes all legal decisionmaking authority for the individual, and replacing a guardian involves a complex legal process. Additionally, guardianship may not respect the goals and values of the individual, especially if the individual can express, verbally or otherwise, their own values and preferences. Some of those values and preferences may not always be ideal. However, we afford discretion to neurotypical adults to make poor decisions. Poor decisions do not necessarily mean that an individual lacks capacity.
Supported decision-making is a way to further enhance autonomy, respect dignity, ensure a commitment to the individual’s best interests, and promote shared decision-making.
Measures that are more inclusive of an autistic individual’s autonomy (with or without an ID) include the following legal tools: a power of attorney for health care, a power of attorney for finances/property, and/or a newly emerging legal model of supported decision-making (SDM).
MECHANISMS FOR DECISION-MAKING
Being diagnosed with autism or as neurodivergent does not automatically render one incapable of making one’s own decisions. The presumption is often made, especially for those with an ID, that a parent or family member is the legal guardian when, in fact, they may not have taken the legal steps to become the person’s guardian. A recent Frontiers in Psychiatry article advises clinicians to be aware and cautious of any disability bias:
[C]linicians may hold implicit stigmatizing
SDM embodies the disability rights motto “nothing about us without us.” This seemingly simple statement captures the powerful notion that critical decisions, especially ones around health care, should not be made for autistic or neurodivergent individuals. Rather, as much as possible, they should be at the center of health care decision-making as well as other major life decisions, including where to work and where to live.
Currently, half of U.S. states have enacted supported decision-making laws, with Florida becoming the most recent state in July 2024.6 SDM
occurs when “people use trusted friends, family members and professionals to help them understand the situations and choices they face, so they may make their own decisions — [it] is a means for increasing self-determination by encouraging and empowering people to make decisions about their lives to the maximum extent possible.”7
This alternative to guardianship and other more formal legal interventions mirrors the way most adults make decisions: by consulting with friends, family and trusted advisors when facing serious health care decisions. SDM is a way to further enhance autonomy, respect dignity, ensure a commitment to the individual’s best interests, and promote shared decision-making.
For example, the law in Washington, D.C., defines SDM as:
[A] process of supporting and accommodating an adult with a disability in order to: (A) Assist the adult with a disability in understanding the options, responsibilities and consequences of life decisions; and (B) enable the adult with a disability to make life decisions, without impeding the self-determination of the adult with a disability or making decisions for the adult with a disability.8
While some variability exists from state to state on how supported decision-making works, including who can and cannot be named as a supported decision-maker, the general intent of such laws is not only to prioritize the preferences of the person for whom a decision is being made, but to allow that person to make decisions for themselves. A guardian, for example, may consider the preferences and views of a ward when making a decision, but the guardian is, by law, the ultimate decision-maker. Also of note is that in those states with SDM laws, “only Illinois limits the adult in an SDM agreement to a person with developmental or intellectual disabilities. All other states allow adults with disabilities … to receive support in SDM agreements.”9
SDM statutes lend formality to what are often informal arrangements, set parameters to ensure that exploitation is not occurring, and identify the range of decisions in which such agreements may be effectuated. An excellent resource for learning more about SDM is the Center for
Public Representation, which has extensive information on SDM and even has a sample SDM agreement form on its website. 10 Additionally, the American Bar Association has published a chart, current through 2023, of state statutes on SDM. The chart includes how states define SDM, what an SDM agreement is, how and when such agreements can be terminated, conflicts of interest and reporting requirements for third parties who suspect abuse.11 The goals are to demystify the process as much as possible and to make SDM more accessible for decision-makers and their supporters.
Supported decision-making is essential to respecting individual choices, and the growing attention to the voices of those for whom decision-making may be challenging is long overdue. Those decisions, however, must be effectuated. Therefore, we attest that we need to expand to a concept we refer to as supported engagement. 12 This is the next step in ensuring that “nothing about us without us” is operationalized beyond individual decisions.
This new conceptual framework acknowledges that supported decision-making is only the start. SDM recognizes that autistic and neurodivergent individuals may need the support of a trusted friend, parent or peer to help make health care and other important life decisions. Making such decisions is important, but the goal is to ensure that these individuals have flourishing lives.
Supported engagement argues that the need for support does not suddenly disappear when adolescents become adults. In fact, a greater need for support, or varying degrees of support, may arise in adulthood. Supported engagement recognizes the individual needs of autistic adults but also recognizes the obligation of the state and other organizations to provide services, as well as the right of autistic and neurodivergent individuals to participate in engaged ways to identify those services. As part of the community and the larger social fabric, their engagement in setting policy and legislation that impacts them is a matter of social justice.
Organizations such as the Autistic Self Advocacy Network emphasize self-advocacy but also recognize the need to have more just laws and policies. 13 Our conceptual framework of supported engagement recognizes that autistic and
neurodivergent individuals have differing needs for support. It recognizes the individuality of each person but also recognizes that the people living with these diagnoses need services that are accessible, coordinated and effective so they can enjoy and contribute to society as fully as possible.
NANETTE ELSTER and KAYHAN PARSI are professors at the Neiswanger Institute for Bioethics at Loyola University Chicago Stritch School of Medicine.
1. Amani Mohammed, Montasser Nadeem, and Taha Yousif, “Towards Safe and Effective Transition from Adolescence to Adult Care,” Sudanese Journal of Paediatrics 17, no. 1 (2017): 10-13.
2. “Data and Statistics on Autism Spectrum Disorder,” U.S. Centers for Disease Control and Prevention, May 16, 2024, https://www. cdc.gov/autism/data-research/index.html.
3. Anne M. Roux et al., “Evidence from the Autism Transitions Research Project (2017–2022): Capstone Review and Services Research Recommendations,” Autism Research 16, no. 3 (March 2023): 480–496, https://pubmed.ncbi.nlm.nih. gov/36622799/.
4. Matthew J. Maenner et al., “Prevalence and Characteristics of Autism Spectrum Disorder Among Children Aged 8 Years — Autism and Developmental Disabilities Monitoring Network, 11 Sites, United States, 2020,” MMWR Surveillance Summaries 72, no. 2 (March 2023): 1-14, http://dx. doi.org/10.15585/mmwr.ss7202a1.
5. Alana J. McVey et al., “The Ethical Imperative to Honor Autistic Clients’ Autonomy in Mental Health Treatment,” Frontiers in Psy-
chiatry 14 (September 2023): https:// doi.org/10.3389/fpsyt.2023.1259025.
6. Thaddeus Mason Pope, “Supported Decision Making — Now in 25 States,” Medical Futility Blog, July 5, 2024, https://medicalfutility.blogspot.com/2024/07/supporteddecision-making-now-in-25.html.
7. Peter Blanck and Jonathan G. Martinis, “‘The Right to Make Choices’: The National Resource Center for Supported DecisionMaking,” Inclusion 3, no. 1 (March 2015): 24-33, https://doi.org/10.1352/ 2326-6988-3.1.24.
8. “Code of the District of Columbia, Chapter 21B. Supported Decision-Making Agreements: § 7–2131. Definitions,” Council of the District of Columbia, https://code. dccouncil.gov/us/dc/council/code/titles/7/ chapters/21B.
9. “Supported Decision-Making: A Statutory Chart,” American Bar Association: Commission on Law and Aging, June 2023, https:// www.americanbar.org/content/dam/aba/ administrative/law_aging/2022-sdm-lstrstctd-altntvs.pdf.
10. “SDM Agreement Form,” Center for Public Representation: Supported DecisionMaking, https://supporteddecisions. org/getting-started-with-supporteddecision-making/sdm-agreement-form/.
11. American Bar Association, “Supported Decision-Making: A Statutory Chart.”
12. Nanette Elster and Kayhan Parsi, “Beyond Supported Decision-Making: The Need for Supported Engagement for Neurodivergent Adults,” The American Journal of Bioethics 24, no. 8 (2024): https://doi.org/10.1080/15 265161.2024.2370739.
13. “Self-Advocacy,” Autistic Self Advocacy Network, https://autisticadvocacy.org/ self-advocacy/; “Law & Justice,” Autistic Self Advocacy Network, https:// autisticadvocacy.org/law-justice/.


Issues are complimentary for those who work for CHA members in the United States.
ALEXANDER GARZA, MD, MPH
“And people were bringing children to him that he might touch them, but the disciples rebuked them. When Jesus saw this he became indignant and said to them, ‘Let the children come to me; do not prevent them, for the kingdom of God belongs to such as these.
Amen, I say to you, whoever does not accept the kingdom of God like a child will not enter it.’
Then he embraced them and blessed them, placing his hands on them.”
(Mark 10:13-16)
Childhood is a time of growth, learning, wonderment and hope, filled with the potential of a full and prosperous life ahead. Unfortunately, not all children and young people are given the opportunities and support required to flourish and reach their full potential.
The events and circumstances that shape children’s — and all people’s — lives take place in the homes and streets of their communities, far from the offices and examination rooms where health care teams try our best to help our patients overcome the sometimes daunting obstacles endemic in their neighborhoods.
In 2024, about 16% of America’s children lived in poverty, with 26% of children living with parents who lacked secure employment. In addition, 68% of fourth graders were not proficient in reading, and 74% of eighth graders were not proficient in math. Furthermore, 33% of children and teens (ages 10-17) were overweight or obese.1 And, approximately 64% of adults in the United States reported they had experienced at least one type of adverse childhood experience (ACE) before age 18. The Centers for Disease Control and Prevention describes ACEs as “potentially traumatic events that occur in childhood. … Also included are aspects of the child’s environment that can undermine their sense of safety, stability and bonding.”2
These statistics are alarming, but they are also related. Unhealthy environments can yield un-
healthy children. Collectively called the social determinants of health, these are the things that affect our patients beyond the walls of the hospital or clinic: economic opportunity, education, built environment, discrimination and pollution. They are far more pervasive and impactful than the few moments children spend in the hospital or doctor’s office.
What is more important about social determinants of health, however, is the cumulative effects of these experiences on the lives of children. Like a toxin, exposure to the social determinants — starting at an early age and compounding over time — likely increases the probability of a poor outcome in health and in life years later, at which point it will be difficult to repair.3
Working on issues related to these determinants is frequently described as working “upstream,” in the context of the root causes of poor health, such as food insecurity or housing. In addition to understanding this in the context of a disease, such as diabetes, we must also appreciate “upstream” in terms of the span of a lifetime. Failure to provide solutions early in life, whether they are material, such as housing or healthy food,
Like a toxin, exposure to the social determinants — starting at an early age and compounding over time — likely increases the probability of a poor outcome in health and in life years later, at which point it will be difficult to repair.
or societal, such as good schooling and family economic stability, places children on a perilous path from which it is more difficult to rescue later when they are downstream in disease and in life.
SSM Health’s vision is “Peace, hope and health for every person, family and community, especially those most in need.” In living out this vision, SSM Health, in addition to providing clinical care, recognizes the outsized effect intervention has on the health and well-being of the children we serve and how it is an investment in the future of our community.
SSM Health’s community benefit programs include initiatives specifically designed to help children and young people thrive. Some examples of this work in action include programs to support areas such as literacy, safety practices and nutrition.
Asthma inhalers: SSM Health St. Anthony Hospital in Oklahoma City has a first-in-the-nation partnership with the Brendon McLarty Memorial Foundation to help save the lives of Oklahoma K-12 public school students who experience asthma attacks at school.4 The foundation has begun supplying rescue inhalers and related medical supplies to every public school in Oklahoma, an effort sponsored in part by St. Anthony.
Cardinal Glennon Safety Program: SSM Health is the lead agency for Safe Kids St. Louis, a local chapter of the national Safe Kids program, which implements initiatives that help parents and caregivers prevent childhood injuries. There are safety initiatives for children and youth of all ages. These include safe sleep practices, car safety, and sports safety and injury prevention. It is open to the community and available all over the region; it provides education to first responders as well.5
Read, Talk & Play: SSM Health St. Mary’s Hospital — Janesville (Wisconsin) provides Read, Talk & Play kits to every birthing family at the
hospital to support early development. This is in partnership with the School District of Janesville to improve kindergarten readiness.
Period poverty: Menstruation is a major issue in education when girls don’t have access to feminine hygiene products, which can lead to school absences and embarrassment. St. Anthony Hospital in Oklahoma City awarded a grant to a local school district to provide these products for free in dispensers in every girls’ bathroom in the district’s elementary, middle and high schools.6
Improving Black infant mortality: The Saving Our Babies project is a collaboration with all health systems in Wisconsin’s Dane County to improve Black infant mortality. This initiative screens for social determinants in the prenatal setting and supports Black women with access to a doula and community health worker throughout pregnancy until the baby’s first birthday.
Drop-in center: SSM Health DePaul Hospital — St. Louis partners with the Epworth Drop-In Center in Normandy, Missouri, the Institute for Family Medicine and Operation Food Search to provide health care, food and nutrition education to homeless and at-risk teenagers and young adults seeking support at the drop-in center. The Institute for Family Medicine provides a nurse practitioner two days a week, and Operation Food Search provides healthy food bags and on-site cooking classes.7
Thrive by Five: Through a partnership with St. Mary’s Hospital — Janesville and the Rock County Public Health Department, the Thrive by Five coalition was launched in spring 2023 to support families and young children through coordinated resources, child development and literacy support. The coalition includes more than 15 partners across Wisconsin’s Rock County.
Food distribution for families: Through our regional Bread Basket program, SSM Health St. Louis conducts 18 food distribution events throughout the region annually. In 2023, we served more than 2,500 households consisting of
approximately 9,000 individuals, of which more than 3,800 were children under the age of 18. From January through early December 2024, we held 15 events serving more than 1,800 households consisting of more than 5,700 individuals, of which about 2,600 were children under the age of 18.
Vaping prevention: SSM Health teaches vaping prevention and provides mental health support to Marshall Middle School students in Janesville. Since 2022, more than 1,500 middle school students have been taught an evidencebased vaping prevention curriculum by staff at SSM Health.
‘Adopting’ a school: SSM Health St. Mary’s Hospital — Madison “adopted” Lincoln Elementary School, located in a low-income neighborhood in Madison, Wisconsin. This partnership allows hospital staff to conduct education in the school and provide access to socks, underwear and hygiene products for families.
Behavioral Health Urgent Care: During the height of the pandemic in 2020, SSM Health opened this walk-in facility in St. Louis, the firstof-its-kind in Missouri.8 Although the center was intended to serve adults, the need for youth mental health services was so great that we opened the urgent care to children and adolescents after a month of operation. Since then, SSM Health has opened a second behavioral health urgent care in the St. Louis region with high demand for services, particularly among children and teenagers.
While we acknowledge the value of what we have accomplished in trying to keep our children safe and healthy, we also know that it is not enough. The heavy burdens that inhibit children from their opportunity to flourish, particularly those who live in poverty, are beyond the capabilities of health care alone.
This is why, in addition to our clinical and social programs, we must partner with those in the community and, most importantly, be passionate advocates every day for those things outside of health care that we know impact our children and, by extension, our future. I encourage every person reading these words to join us in these crucial endeavors.
As abolitionist Frederick Douglass once pro-
fessed, “It is easier to build strong children than to repair broken men.”
DR. ALEXANDER GARZA is chief community health officer for St. Louis-based SSM Health. He is the winner of CHA’s 2022 Sister Carol Keehan Award.
1. “2024 Kids Count Data Book,” The Annie E. Casey Foundation, June 10, 2024, https://www.aecf.org/ resources/2024-kids-count-data-book.
2. “About Adverse Childhood Experiences,” U.S. Centers for Disease Control and Prevention, https://www.cdc. gov/aces/about/index.html.
3. Geoffrey R. Swain, “How Does Economic and Social Disadvantage Affect Health?,” Focus 33, no. 1 (Fall/Winter 2016/2017): https://www.irp.wisc.edu/ publications/focus/pdfs/foc331a.pdf; Dr. Paula Braveman and Dr. Laura Gottlieb, “The Social Determinants of Health: It’s Time to Consider the Causes of the Causes,” Public Health Reports 129, no. 1 (2014): https://doi.org/ 10.1177/00333549141291S206.
4. “Foundation Leads First-in-Nation Effort to Save Lives of Oklahoma Public School Children Suffering Asthma Emergencies,” SSM Health, November 18, 2022, https://www.ssmhealth.com/newsroom/2022/11/ foundation-leads-effort-save-children-with-asthma.
5. “SSM Health Cardinal Glennon Safety Program,” SSM Health Cardinal Glennon Children’s Hospital, https://www.ssmhealth.com/cardinal-glennon/ services/specialty-programs-for-patients-families/ safety-program.
6. Lisa Eisenhauer, “School District Gets a Hand from SSM Health Hospital to Take on ‘Period Poverty’” Catholic Health World 38, no. 19 (December 1, 2022): https:// www.chausa.org/publications/catholic-health-world/ archive/article/december-1-2022/school-district-getsa-hand-from-ssm-health-hospital-to-take-on-periodpoverty.
7. “Epworth Drop-In Center,” Epworth, https://www. epworth.org/services/epworth-drop-in-center/.
8. Andrea Smith, “SSM Health Opens Behavioral Health Urgent Care to Treat Depression, Anxiety and Other Mental Illnesses,” Ladue News, November 6, 2020, https://www.laduenews.com/health-and-wellness/ ssm-health-opens-behavioral-health-urgent-care-totreat-depression-anxiety-and-other-mental-illnesses/ article_9efce6d9-ac8a-54f6-be1a-7211c297e120.html.
“H
ope is not a strategy!” That refrain ricocheted across system leadership offices from a tough-as-nails executive, known for her grueling questioning of senior leaders. Parading into the conference room with improvement and growth plans, they often departed dejected.

The executive wanted solid evidence that assumptions were accurate, volumes were justified and capital requests would yield positive returns. She grilled leaders and prodded them to go two and three steps further, insisting on data and real-time facts. She rejected half-baked ideas. Anything remotely resembling the saying, “If we build it, they will come,” received the dreaded retort, “Hope is not a strategy!”
Hope may not play well in high-stakes operational meetings with tensions akin to entrepreneurs before a panel of notable venture capitalists on the TV show Shark Tank. Even so, it is a key strategy — or, rather, foundational to the spiritual life and a distinguishing mark of the Christian community. It is a prominent thread woven throughout the Christian tradition. It pops up across the scriptures and quite conspicuously in the writings of St. Paul’s letters to the earliest communities of believers. To the Hebrews, he posits hope in God’s promise as an anchor for the soul (1 Corinthians 6:19). To the Romans, he encourages their lives to overflow with hope (Romans 15:13). And to the Thessalonians, he inspires them not to grieve like others who do not have hope (1 Thessalonians 4:13).
backdrop of a world in tumult, Francis announced the Jubilee stating, “Everyone knows what it is to hope. In the heart of each person, hope dwells as the desire and expectation of good things to come, despite our not knowing what the future may bring.”1
This Jubilee provides at least four points of intersection for leaders of Catholic health care. First, hope is the desire and expectation of good things to come. It is an attentiveness, even a daily practice of mindful observation, of our desires that lead us to God, the source of all good things. Every leader desires good things for our ministries. Our desire for good outcomes and our expectation of higher quality or improved results or patient satisfaction scores are all fruits of human hope.
Francis’ letter suggests we walk into strategy meetings not just with slides and spreadsheets, but with the gifts that God has given us. The gifts
Our desire for good outcomes and our expectation of higher quality or improved results or patient satisfaction scores are all fruits of human hope.
Pope Francis pulls this thread from the tradition and hoists hope as the signature theme for the Jubilee Year 2025. Every quarter century, Roman Catholics mark the passage with a jubilee and an accompanying theme designated by the pontiff, in a practice stretching back to 1300. Against a
of intellect, insight, expertise and vision flow from God the Creator. Even given the challenges and obstacles of health care delivery and financing, the Spirit of God is urging us to recognize the tremendous giftedness endowed to us, especially the holistic vision Catholic health care offers.
Second, Francis writes that we “should be at the forefront in pointing out the need for a social covenant to support and foster hope, one that is
inclusive and not ideological.”2 This is a signature of Catholic health care, particularly in light of our community health and benefit activities.
Our partnerships are more than just good ideas and strategies that effectively address community health needs assessments. They are, in fact, actions that witness this social covenant to foster hope, particularly among populations whose conditions and situations may cause them to find hope fleeting. The pope’s vision that the Christian community is foremost in fostering social hope gives our ministries renewed confidence in our community partnerships and health strategies.
Third, Francis specifically articulates the Christian responsibility to offer hope to the sick, whether in our facilities or in their homes. He urges special effort to extend hope to the aging, who frequently feel abandoned and lonely. He also calls us to offer “tangible signs of hope” to persons with disabilities, migrants, exiles, refugees and the young, “for they are the joy and hope of the Church and of the world!”3
When St. Thomas Aquinas discussed hope in his extensive reflections on the virtues, he described it as a habit of the mind that is oriented toward a future good. Although it may be difficult, it is possible to obtain.5 This implies a degree of intention, focus and especially effort.
Our human efforts to be a wellspring of hope wane from day to day, week to week and project to project. Hope is not just a download permanently cached into our brains or being, and forevermore accessible. Hope is a gift from grace, mixed with our own exertion. We unlock and access it through our spiritual practices.
Hope is not just a download permanently cached into our brains or being, and forevermore accessible. Hope is a gift from grace, mixed with our own exertion. We unlock and access it through our spiritual practices.
For Catholic health care leaders, these ordinary activities are more than mere leading practices in public and community health. They are signs of a vibrant community acting as Christ for others today.
Fourth, Francis’ calling card has been to befriend and lift up those who are poor. CHA’s public commitment to those who are poor and vulnerable, enshrined in our Shared Statement of Identity for the Catholic Health Ministry, shares the pontiff’s heartfelt concern and love. This jubilee year offers Catholic health care the occasion to revisit this part of our identity with renewed focus.
In addition to the clinical, social and behavioral services we offer in solidarity with those who are poor, we can add hope to the top of our efforts this year. “I ask with all my heart that hope be granted to the billions of the poor, who often lack the essentials of life. … [W]e can easily grow inured and resigned. Yet we must not close our eyes to the dramatic situations that we now encounter all around us … Let us not forget: the poor are almost always the victims, not the ones to blame.”4
When Pope Benedict XVI wrote an encyclical letter on hope, he described prayer as the school of hope. Prayer is an action through which we commune with God in light of our own lives and current-day realities. Referencing Sts. Augustine and Paul, he noticed how hope entailed a straining toward things yet to come.
Cultivating hope entails preparing one’s heart to be enlarged and filled by God. Hence, prayer that fosters hope entails loosening our attachments and seeking the grace of God to soften and expand our hearts.6 Moreover, hope is nourished by prayer in the sense that when others no longer listen, God always awaits us in our prayer. And this, if nothing else, is the seed of hope.
A second spiritual practice is cultivating awareness of things for which we hope. Paying attention to longings and desires will lead to clarity on the things for which we hope. Routinely list the things you hope for. In this process, we will inevitably discover that some things that we hope for do not truly merit our attention. There are things of greater value to hope for.
Lastly, reading the scriptures or other sacred
texts, stories or poetry can shape our longing for what matters most. The scriptures reveal to us time and again a vision of the reign of God, where human flourishing will find its fullest expression. This becomes the fuel of human hope.
This Jubilee Year 2025, I find myself wondering about things to hope for as they relate to enlivening Jesus’ healing ministry today.
First, I hope that our zeal and love for our work in Catholic health care will grow, particularly as lay people are called to lead works of the Church. I pray that in time, the wider Church, and indeed all in society, will see our dedication as authentic and inspiring as it was when sisters nearly exclusively led our ministries.
Second, I hope the movement toward a synodal church will set root, first within each of us. This means genuinely seeing ourselves, individually and communally, as the living presence of the Risen Lord. This also means loosening mental attachments to portraying church primarily as something done by priests and bishops. When imagining church as a community of disciples, everyone has an integral role grounded in the image of God.
Third, I hope CHA sees the fruits of our labors in enacting the tactics enumerated in our strategic plan. This means that the building blocks of the reign of God are cemented into the structures of care and its provision of affordable and equitable access.
Fourth, I hope that every individual who seeks care from our ministries has an experience of being heard and accepted, cared for and deeply loved. I hope that every older adult living in a Catholic home for seniors shall know that he or she is cherished and invaluable, even as human
frailty and chronic conditions progress. I hope that the person burdened for years by mental health complications feels validated, seen and supported by our ministries. Ultimately, I hope that everyone who comes to a CHA ministry will find Christ welcoming them, embracing them and confidently sending them forth from an experience of healing — however simple or profound the gesture, treatment or intervention may be.
Lastly, I offer a postscript to the executive leader whose comment, “Hope is not a strategy!” sent a chill across a system’s operations. Understandably, she was exasperated by strategies she found lacking. The irony is that hope is inextricably intertwined with every strategy. Everyone knows what it is to hope — even that shrewd executive leader. “[A]nd hope does not disappoint.”
(Romans 5:5)
DARREN M. HENSON, PhD, STL, is senior director of ministry formation at the Catholic Health Association, St. Louis.
1. Pope Francis, “Spes Non Confundit, Bull of Indiction of the Ordinary Jubilee of the Year 2025,” The Holy See, section 1, https://www.vatican.va/content/francesco/ en/bulls/documents/20240509_spes-non-confundit_ bolla-giubileo2025.html.
2. Francis, “Spes Non Confundit,” section 9.
3. Francis, “Spes Non Confundit,” sections 10 and 12.
4. Francis, “Spes Non Confundit,” section 15.
5. Thomas Aquinas, Summa Theologica, Second Part of the Second Part, question 17, article 1.
6. Pope Benedict XVI, “Spe Salvi, Encyclical Letter on Christian Hope,” The Holy See, sections 33-34, https:// www.vatican.va/content/benedict-xvi/en/encyclicals/ documents/hf_ben-xvi_enc_20071130_spe-salvi.html.
In 1992, German artist Gunter Demnig conceived an art project as part of an initiative to honor Roma and Sinti victims of the Holocaust. In German, the project was called Stolpersteine, or “Stumbling Stones” in English.1 The idea was to give recognition to the lives of ordinary people who were killed as part of the Holocaust.

Memorials have been present for much of human history. In Rome, for example, there are memorials to events, to groups of people and to individuals, in that order. For Rome, the emphasis was on the social order and not the individual.
Christianity changed that slowly. The Christian emphasis on the dignity of the person took centuries to be rooted. Today, we reap the benefits of this emphasis when we talk about individual rights.
To understand Demnig’s memorial, we can look at it in the context of other remembrances of significant people we have experienced. From an American perspective, people who were influential in our history have been memorialized in lifelike and/or awe-inspiring sculptures. The examples that come to mind are in Washington, D.C.: the Lincoln Memorial and the Martin Luther King Jr. Memorial, both for individuals, and one for a group of people, the Vietnam Veterans Memorial by American architect, designer and sculptor Maya Lin.
These memorials are significant because they give us an invitation to understand other people. They are encounters. They ask us, “Why remember them? Why now?” They also ask us to ponder, “What do their lives have to do with ours?”
Demnig’s Stolpersteine try to directly answer these questions. In most of Europe, the city streets are made from cobblestones, which measure

There are Stolpersteine or “Stumbling Stones” in at least 1,200 places in Europe. This memorial in the Trastevere neighborhood in Rome remembers the Citoni family of five: a mother, father and three children aged 7, 5 and 3.
roughly 4 inches by 4 inches. Demnig’s project was designed to replace ordinary cobblestones with “stumbling stones” that are brass replicas of them.

The intention of the Stolpersteine is to disrupt our experience of the ordinary. Demnig wants to interrupt our attention as we walk along a street or plaza, causing us to think about the layers of history that are at our feet, quite literally.
Each of these brass “stones” is inscribed with the names of those who were arrested from their homes, and, the date of their death and final resting place, if those details were known. He uses the language of the stone’s location so that the memory resonates with those who live in that area and would ordinarily walk past it. An example from the Roman neighborhood Trastevere is shown on page 63.
Notice the words on each of these stones. “Qui abitava,” which means “Here lived.” Then follows the name of the person and their year of birth, “nato,” or “nata,” depending on whether they were male or female. This is followed by “arrestato(a),” the date of their arrest, and “deportato(a),” the location to which they were sent. In this case, this entire family was sent to Auschwitz. Lastly, a notation is included on where they died. Here, the parents are listed as “in lugo ignoto(a),” meaning
“no known place,” while their three children are remembered as being “assassinato(a),” murdered, at Auschwitz.
This memorial remembers the Citoni family of five: a mother, father and three children aged 7, 5 and 3. These stumbling stones are meant to make us think about the people inscribed on the stones, and the tragic circumstances of their lives and deaths. I am certain that without this memorial, none of us who have walked past this building in Rome would have known about these lives. So, we stumble on them and the memories of those lives as we continue to live.
Memorials invite us into other people’s lives so that our own experiences might be strengthened. A memorial makes the past present.2
Demnig’s vision for his project has some historical resonance, as those of us who have visited European churches might remember. In London’s Westminster Abbey, for example, the floor is covered in stones commemorating those buried there.3 Demnig transformed that experience
by honoring the forgotten, the people who were persecuted, rather than those who were famous. He remembered those who were dead but had no grave.
So where are the “stumbling stones” of Catholicism that remain true to Demnig’s vision? I have experienced many, and I am sure that there are many more that I have not yet encountered. I will mention one place that will serve to demonstrate the spirit of Demnig’s vision.
Starting in the mid-19th century, the Sisters of Charity of New York served the people of New York City. They cared for the poor, survivors of the Titanic, and more recently, those with AIDS at St. Vincent’s Hospital in New York City’s Greenwich Village until it closed in 2010.4 The sisters were a positive force for change in New York City.
One can find a “stumbling stone” to the Sisters of Charity at the New York City AIDS Memorial Park at St. Vincent’s Triangle (shown on page 64). The memorial recognizes the sisters’ contribution to the care of all New York City citizens.
This is a Catholic stumbling stone. It is a moment in time that should give us pause and a moment to remember these sisters. As you reflect on your past journeys and set out on any new ones ahead, ask yourself: What are the other stumbling stones of Catholic health care?
BRIAN M. KANE, PhD, is senior director, ethics, for the Catholic Health Association, St. Louis.
1. The Roma are colloquially known as “Travellers” or sometimes “Gypsies,” but these are considered derogatory terms. They are an itinerant population that originally migrated from India. They settled in Germany, then migrated to other parts of Europe. During the Holocaust,
they were one of the groups targeted by the Germans as being inferior. Adolf Eichmann often referred to the “Gypsy Problem” alongside the “Jewish Problem.” The Sinti are a subgroup of the Roma, most of who remained in Germany. See: Michael Burleigh and Wolfgang Wippermann, The Racial State: Germany 1933–1945 (Cambridge University Press, 1991), 122. Also, note that the word “Stolpersteine” refers to the plural “Stumbling Stones.” The singular is “Stolperstein.” Please see Gunter Demnig’s website on this project at https://www.stolpersteine.eu/en/home. I’d like to also recognize my daughter, Caitilin, who made me aware of this memorial.
2. Theologically, for Catholics, this description of making the past present is Eucharistic. The Mass makes Jesus’ sacrifice present for us today. It is the same gift to God, forever.
3. “Famous People/Organizations,” Westminster Abbey, https://www.westminster-abbey.org/history/ famous-people-organisations.
In a similar way, Demnig’s Stolpersteine recall the places where evil occurred by emphasizing the humanity of those who were murdered. This follows a long tradition of Jewish and Christian tradition that equates the speaking of words, and especially names, as a blessed act. Encountering the stones acknowledges their lives.
4. “NYC AIDS Memorial Park at St. Vincent’s Triangle,” NYC Parks, https://www.nycgovparks.org/parks/nycaids-memorial-park-at-st-vincent-s-triangle; Michael J. O’Loughlin, “The Secret History of Catholic Caregivers and the AIDS Epidemic,” America: The Jesuit Review, June 10, 2019, https://www.americamagazine.org/ faith/2019/05/31/catholic-hospital-pioneered-aidscare-podcast-plague-234101; Michael O’Loughlin, Hidden Mercy: AIDS, Catholics and the Untold Stories of Compassion in the Face of Fear (Broadleaf Books, 2021).
THINKING GLOBALLY
BRUCE COMPTON
Recent conversations with David Addiss and Heather Buesseler, from the Task Force for Global Health’s Focus Area for Compassion and Ethics (FACE), reminded me of the synodal process the Catholic Church has undertaken. It was great to hear how this secular organization embodies a similar process that Pope Francis describes as “a dynamism of mutual listening, conducted at all levels of the Church, involving the whole people of God.”1 As the saying goes, the shortest distance between two people is a story, so I have asked Buesseler to share hers.
HEATHER BUESSELER, MPH
At the end of a human-centered design workshop in Kampala, Uganda, that I facilitated more than a year ago with representatives from two East African health care organizations, I received some comments from participants that still resonate with me today:
“Sometimes you never know the potential you have until you have the opportunity to explore it.”
“You allowed us to contribute. And we came out with beautiful ideas.”
“Sometimes you go to these workshops and it is like a lecture, but the way you have structured this, we are required to participate. When you have to participate, you take ownership.”
As I took in this feedback, hot tears gathered in the corners of my eyes, and I tried to discern why this emotion was bubbling up.
In March 2020, I left my position as a senior global health advisor at an international humanitarian nongovernmental organization. A couple months later, George Floyd was murdered mere blocks from my house in South Minneapolis.
The social uprising and racial reckoning that
ensued prompted me to take a deeply critical look inward: What was my part, conscious or not, in perpetuating systems of oppression and White supremacy, both in America and as a global health professional? While I had always been conscious of my positionality as a White American woman and the geopolitical and postcolonial power dynamics at play, I found myself examining my place in this field anew.
Since leaving my job in early 2020, I began consulting with a focus on unblocking and embedding compassion in global health systems. One of the organizations I have been working with in this endeavor is FACE at the Task Force for Global Health.
At FACE, our working definition of compassion is: 1) an awareness of the suffering of another, coupled with 2) an emotional response to that suffering, and 3) a strong desire or action to alleviate and prevent suffering. In other words, awareness plus empathy plus action equals compassion. In this sense, global health is fundamentally a practice of compassion.
But global health is also historically rooted in the European colonial project. Its motivations,
while perhaps cloaked in an air of compassion, were often self-serving in nature. Tropical medicine was born of the desire to protect European colonizers from the health hazards encountered in the lands they had claimed. Offering health services to local populations was a means to introduce Western culture and to “civilize” native populations. In doing so, White Western “expertise” and systems of healing were elevated, displacing traditional knowledge and healing modalities.
Fast forward to the 21st century — the discipline of global health continues to center White knowledge, leadership and expertise. Global health funders, training institutions and decisionmakers are still largely concentrated in Europe and the United States. “Vulnerable populations” are still often treated as passive recipients of health programs. And local “partners” are frequently treated as infantry, given marching orders and then monitored for implementation “fidelity” and, of course, corruption.
Yes, global population health has improved over the past half-century by many objective measures: life expectancy has increased, maternal and child mortality has fallen, diseases like smallpox have been eradicated, and global hunger is abating. But if, as a global health professional, my compassionate actions to alleviate suffering in low- and middle-income countries (LMICs) are embedded in racialized epistemic and geopolitical systems of power that cause oppression and suffering, is it justified?
This dilemma is what I have been wrestling with when it comes to my place in global health. Do I lean out completely? Or is there something I can still meaningfully offer without displacing the skills, creativity and lived experiences of those I am supposedly helping? Particularly as I engage in the nascent domain of compassion in global health, I’m consciously trying to avoid shaping it within the same colonial power structures from which global health emerged.
In January 2022, FACE received funding from the IZUMI Foundation to test a novel approach to compassion cultivation with its existing grantee partners, using human-centered design to enhance compassion at the organizational, staff and/or
patient level. These partners, who deliver health programs and services in Africa and Latin America, are rightly regarded as exemplars of compassion despite the many challenges they face. Yet even exemplars need support, particularly when they work in resource-limited settings where human suffering can be severe and the causes of suffering complex.
After months of virtual relationship-building and an in-person discovery trip in May 2023 to Safari Doctors in Lamu, Kenya, and Nama Wellness Community Center in Mukono, Uganda, FACE hosted a human-centered design workshop in Kampala, Uganda. We brought together teams from both organizations to design solutions to the question: How might we codify a compassionate organizational culture?
The workshop wasn’t just participatory; it was engaged. We eschewed didactic trainings and instead facilitated fun, generative exercises to get the creative juices flowing and build on one another’s ideas. I saw people come alive. I saw people believe in themselves. I saw light bulb moments and lightning strikes. “You are tickling our brain!” one participant commented.
We emerged from the workshop with some fantastic concepts that we subsequently prototyped in each organization. But in my estimation, those prototypes and their outcomes only account for about 50% of the workshop’s impact. The other half was the way participants reconnected with their inner innovator, competence and worthiness. This format unlocked and unleashed something in them that has the potential to impact how they encounter any professional design challenge in the future.
Human-centered design flips the script in global health program design. It centers the end user of whatever service or product it aims to design. Most importantly, facilitators take off the “expert hat” and embody a beginner’s mindset. This means facilitators don’t show up with the solutions in mind — even if (like me) they are global health professionals. Instead, they create a space to draw out the ideas in the room and facilitate a process to move big, fuzzy idea buckets into testable, implementable concepts.
As I round out 20 years as a global health
professional, I am finding that shifting from the role of chief program designer to one of creating space and facilitating is not always easy. I’ve traveled to some of the world’s most far-flung places, been in the thick of responses to pandemics and horrific catastrophes, launched innovative projects and learned from the duds. Let’s just say I have many ideas about how to address the myriad health challenges facing communities in LMICs.
But as a White American global health professional, I’ve decided that the only way to stay in is to lean out. The hot tears in that workshop sprang forth because I realized that human-centered design facilitation might be just the way I can lean out and still stay in.
I’m not suggesting human-centered design is a panacea for “decolonization.” But it may be an opportunity to rewire global health partnerships
and redistribute power in a discipline seeking to break free from its colonial roots.
Human-centered design centers the lived experiences and ingenuities of the professionals and communities these programs intend to impact, making the solutions more resonant and more likely to stick. It is a format that allows the best of global health professionals from both LMICs and Western countries to shine as we co-create the most successful solutions. And it centers that which makes us most fully human: connection, meaning and compassion.
HEATHER BUESSELER is the founder and chief visionary officer of Humaniterra, a consulting firm dedicated to rehumanizing health systems, which partners with FACE at the Task Force for Global Health on its compassion programs.
As Catholic ministries, we are called to embody authentic listening and foster welcome and respect. Listening can be a difficult task when the harsh roots of global health include the challenging realities that Buesseler describes. The ongoing works of Catholic communities globally include many examples of amazing work on our journey of compassion.
The synodal process, along with the work of FACE, offers valuable lessons for our ongoing efforts to advance the healing ministry in the U.S. and worldwide. These insights emphasize the importance of authentic listening in fostering a sense of welcome, respect and a shared mission within our global health initiatives.
Through this work, I am reminded of a quote in CHA’s newly developed synodal conversation toolkit: “Listening is a bold contribution to human flourishing.”2
May we all go forth and listen boldly!
BRUCE COMPTON is senior director, global health, for the Catholic Health Association, St. Louis.
NOTES
1. Francesca Merlo, “Pope to Rome’s Faithful: Synodality Expresses the Nature of the Church,” Vatican News, September 18, 2021, https://www.vaticannews.va/en/pope/news/2021-09/pope-francis-discourse-rome-faithful-synodalprocess.html.
2. “Synodal Conversation Toolkit,” Catholic Health Association, https://www.chausa.org/prayers/the-synod-onsynodality/cha-synodal-conversation-toolkit/synodal-conversation-toolkit (CHA website login required to access).
For those who steward the Catholic health ministry, today’s leadership demands constant assessment of how decisions strengthen or limit the influence of our Catholic identity. Whether on behalf of patients, their families or their communities, the decisions leaders make are inescapable and carry lasting implications.

How does one appropriately decide how to care for all while maintaining financial sustainability? How does one empower teams to reimagine health care today while structural lethargy, political polarization and societal progress innovate at different speeds? What is the best approach to inspire those within your health system and/or community to unite as one ministry working toward a common mission? How can we support new generations of ministry leaders with the guidance and encouragement they need to steward the legacy that has been entrusted to them?
Consider the last big decision you made personally or professionally. I would venture to guess you were not alone in that choice. Whether you mulled it over with a colleague, called a family member, spoke to God or summoned inner stillness, at least one other guided your decision. Allow me to be so bold to say that for every good decision ever made, guidance was present. We don’t decide in a vacuum.
board does not actually convene, leaders establish relationships with a team of seasoned counsel to ensure they have access to wise voices to call upon and learn and grow from, a mentorship that is enriched through each guide’s respective gifts and talents.
What benefits would Catholic health leaders attain from establishing a personal board? Might there be denominators in the composition of a ministry leader’s board that would differ from other executive leaders’ boards? What is most needed, or better said, “who” is most needed to
Chaplains’ clinical and theological training sets them apart as moral exemplars in principle and behavior. They are experts in embodying a nonanxious presence as they listen, reflect, assess spiritual needs and propose appropriate interventions.
support a Catholic health leader’s decision-making? I have a suggestion that may be right under our noses.
A few years ago, through a leadership forum, I was introduced to the idea of establishing a “personal” board of directors — a network of four to six trusted colleagues to advise me in my personal and professional growth.1 On a personal board, the individuals who serve as guides offer wisdom and thought partnership regarding the choices and challenges a leader faces. While one’s personal
Chaplains are integral members of the interdisciplinary care team. They are professional partners who highly regard maintaining trusted relationships with co-workers across the continuum of care. They commit themselves day after day to honor the dignity of every person in their care with compassion and ethical service as they help others navigate life’s most existential questions, from birth to death.
Chaplains’ clinical and theological training sets them apart as moral exemplars in principle and behavior. They are experts in embodying a
nonanxious presence as they listen, reflect, assess spiritual needs and propose appropriate interventions.
Allow me to unpack how including a chaplain on a personal board of directors might profoundly serve growing leaders, guiding them in leadership capabilities and, at best, the larger Catholic health ministry. Let’s explore how this potential partnership can benefit leaders through some common questions they all face.
How do I determine priority needs?
Prioritizing tasks and decisions almost never turn out as cut and dried as they appear in a tool such as the Eisenhower Matrix, which classifies matters as urgent or not urgent, important or not important. For those of us who seemingly spend most of our time on urgent but unimportant matters,2 the work of a chaplain knows time through a different lens.
portant. While time itself cannot slow down, nor can many timelines for decision-making, the expertise of a chaplain can help reorient us to what is truly urgent and important, what is lasting and what is fleeting.
How do I lead like the founders?
In the swarm of daily turbulence, leaders can lose their bearings. One’s “why” — the why of the ministry’s mission and the legacy that leaders have been called to steward — can get lost. Chaplains are keen observers of what’s most important, helping one rediscover the anchor of vocational meaning and visionary focus. They astutely identify where one’s joy is operative and/or where vision is impeded, steadily offering questions to reorient one’s leadership back to the ministerial mission, vision and values.
While time itself cannot slow down, nor can many timelines for decision-making, the expertise of a chaplain can help reorient us to what is truly urgent and important, what is lasting and what is fleeting.
Day after day, the bulk of their work requires tending to existential, meaning-making questions around the quality of life and death, which are often also urgent. As they accompany patients facing decisions in serious illness or co-workers in crisis situations, chaplains have a skilled capacity to sort out what is eternal and what is temporal. They offer a solution to the ongoing quandary of the Eisenhower Matrix we know all too well.
Author and founder of the Center for Action and Contemplation, Fr. Richard Rohr, provides a perspective on time that also resonates with chaplains. He speaks of chronos time as a moment-bymoment, life-according-to-the-clock kind of time. In contrast, he offers an alternative: kairos time, the “eternal now” kind of time.3 Chaplains know kairos time well.
Forged through reflecting upon others’ experiences, chaplains operate from a deep sense of time that allows them to differentiate the urgent from the nonurgent, the important from the unim-
Like the founders, a chaplain’s spiritual life also informs their sense of community and their ability to perceive holiness in ordinary circumstances: sacramentality is their mainstay. Just as the community and rituals of religious life formed the attunement of the sisters, clinical pastoral education trains chaplains to perceive the constant presence of the Spirit. At its best, this awareness continually crosses the divides of denominations and/or spiritualities, opening one to receive the Holy in whomever or whatever form it may arrive.
Leading in the way of the founders empowers one to understand that the mystery of the Holy is among and within all as it heals, sustains and guides. Chaplains are expert ambassadors of sacramentality who can help leaders discover and embody what Sr. Mary Roch Rocklage, RSM, the late president and CEO of Mercy, called the “permeating presence” of Catholic health care.4
How do I maintain healthy boundaries?
The ministry of effective chaplains demonstrates appropriate boundaries to serve others sustainably.
Time: They practice the importance of sleep, personal and/or family time, and time away from pastoral duties. They know when to respond and when to delay a response.
Guidance: They regularly receive guidance from a ministerial supervisor or a spiritual di-
rector. A safe and loving listener can help them explore their own internal resistances and invitations. As they are listened to, they are better positioned to be listening guides to others.
Connection: They know and maximize their resources. They prioritize life-giving relationships and take time away from work to protect those connections. They don’t take on what’s outside of their capabilities but instead, refer out through a network of resources.
As we look to nurture our personal and professional growth and the ministries we steward, it would do us well to intentionally consider who surrounds us. Whose voices are in our ears and our hearts when we make decisions? Whose wise words will we recall as we guide others? Perhaps it is a chaplain you will consider.
The call to be a leader in the healing ministry of Catholic health care presents challenges that require the guidance and support of special, trusted advisors, however seasoned or fresh you are in a leadership role. Through their eternal perspective, sense of the Holy, practices to maintain healthy boundaries and a strong moral
compass, chaplains can be vital partners on your personal board of directors to shape you and the people, communities and generations within your reach.
JILL FISK, MATM, is director, mission services, for the Catholic Health Association, St. Louis.
1. Susan Stelter, “Want to Advance in Your Career? Build Your Own Board of Directors,” Harvard Business Review, May 9, 2022, https://hbr.org/2022/05/wantto-advance-in-your-career-build-your-own-board-ofdirectors.
2. Daniel Kennedy and Andrea Porter, “The Illusion of Urgency,” American Journal of Pharmaceutical Education 86, no. 7 (October 2022): https://doi.org/ 10.5688/ajpe8914.
3. Richard Rohr, “Growing Up Men,” On Being with Krista Tippett, June 13, 2019, https://onbeing.org/programs/ richard-rohr-growing-up-men/.
4. “Mercy’s Sister Mary Roch Rocklage Contributions Honored with Sculpture,” Mercy, August 24, 2023, https://www.mercy.net/newsroom/2023-08-24/mercys-sister-mary-roch-rocklage-contributions-honoredwith-scu/.



KARLA KEPPEL, MA, MISSION PROJECT COORDINATOR, CHA
In the face of academic, social and other stressors, young people can be especially burdened by the pressure to succeed. Add to these the pervasive demands of busyness, and well-being becomes an even more difficult topic to take seriously.
Leaders in Catholic health care are uniquely situated to lead younger generations by example. Ideally, through incorporating daily practices of well-being, personal connection with the Divine, and engagement in ministry formation they thoughtfully find meaning and purpose in their work. Through these everyday rituals, ministry leaders allow not only for their own flourishing, but for the flourishing of those they mentor.
Dr. Stuart Slavin, vice president for well-being at the Accreditation Council for Graduate Medical Education, suggests that when we think of our well-being as a continuum, taking small steps where we can, we are better situated and empowered to more intentionally integrate it into our routines. In doing so, we invite others into similar awareness.
The awareness that we have been named by God as beloved and worthy of love means that acting, even in small ways, toward our own flourishing becomes an important way to offer gratitude and praise back to the One who created us.
In his teachings around well-being, Slavin highlights a few key tools necessary for taking steps toward better well-being.1 One of these, metacognition, refers to the way we
“think about our thoughts.” That is, to notice distorted thinking, name it as such, and consider what other ways of thinking are possible. For example, is one grade (out of many) indicative of being a failure? What response would a loved one have to a declaration of failure? As one of God’s “Beloved,” what would a kinder response look like?
While many of us are likely familiar with these types of thought patterns, and perhaps even well-practiced in reframing them, Slavin suggests that these are practices that must be cultivated in younger generations if they are to experience well-being and fully flourish in their vocations.
Thus, while the practice of prayer and reframing may not be new, consider who in your life might benefit from being reminded of their own “belovedness.” As stated by the late spiritual writer Henri Nouwen, “Becoming the Beloved means letting the truth of our Belovedness become enfleshed in everything we think, say or do.”2
Starting from a place of love, we use our lived experiences as a path to the Divine. As you notice an invitation to reframe comes to the surface, can you pause, pray and consider other ways of thinking?
Take a deep breath. Then, another. As you settle into shifting your thinking, focus on the experience of it. What other perspectives can you take?
Incorporate into your breathing a simple two-part phrase that highlights your belovedness, your
God-given dignity, or a sense of belonging and being loved. A few examples:
Inhale: I am beloved.
Exhale: I belong.
Inhale: I am Your beloved.
Exhale: And so I am loved and love others as You do.
What do you notice? Does your thinking shift when you start from a place of belovedness, as one created in God’s image and likeness, to be infinitely loved by God for all eternity? How can you bring this reframing into your life daily whenever tensions or conflicting feelings arise?
CLOSING PRAYER
Boundless Love:
You embrace us with Your grace, know us deeply and love us unconditionally. Grant us the strength to love ourselves as You do and to share that love with others. In moments of doubt, may Your love be a steadfast anchor. May we find solace in the knowledge that we are cherished as Yours.
Let us always be aware that we are never alone. Your love surrounds us, supports us and leads us home. Amen.
1. “AWARE and Wellbeing Workshop,” Learn at ACGME, https://dl.acgme.org/ learn/course/aware-well-being-videoworkshop/aware-and-wellbeing-workshop/ introduction.
2. Henri Nouwen, Life of the Beloved: Spiritual Living in a Secular World (The Crossroad Publishing Company, 2002), 45.
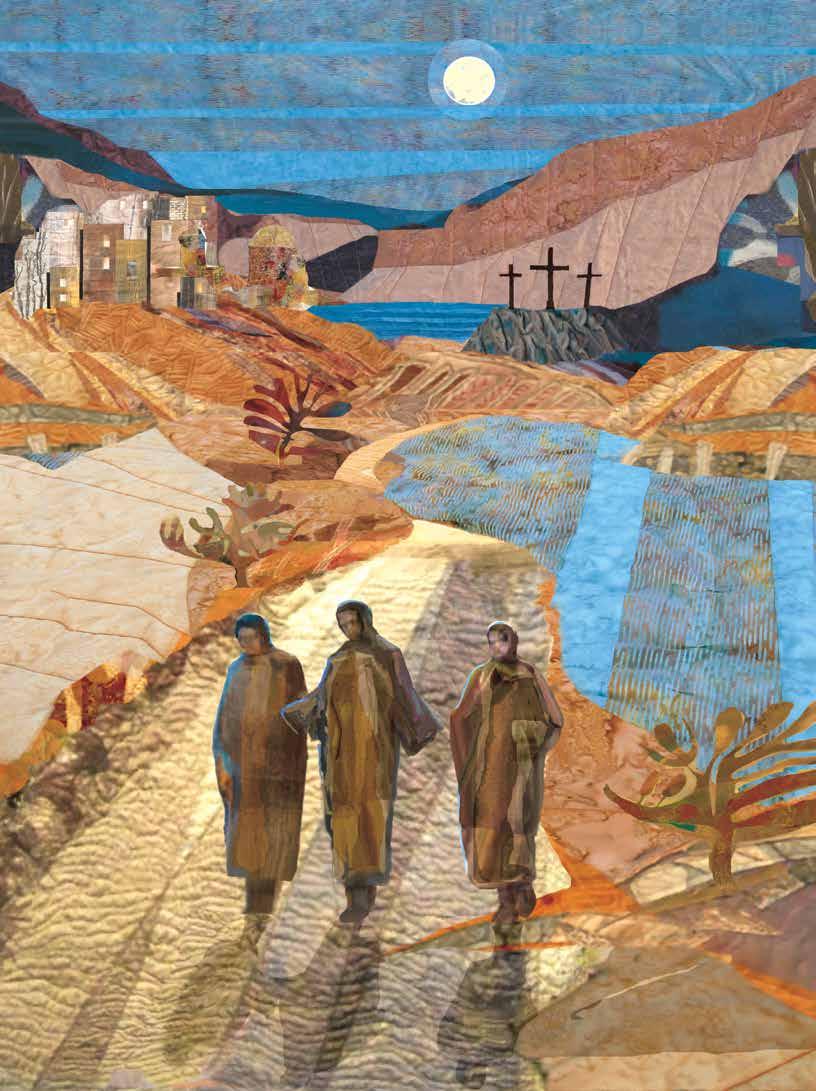


The Center for Theology and Ethics in Catholic Health aims at excellence in providing comprehensive resources for faithfully exploring how Catholic health can promote human flourishing by drawing on the Church’s teaching and the best expression of Catholic theological ethics.
“We promote dignity because we are Catholic, and we can encourage others to promote dignity as people of goodwill.”