CHRISTUS creates keystone document to ease advance care planning
By LISA EISENHAUER
CHRISTUS Health has created a onepage guide to help patients figure out where they are in the process of advance care planning and point them to resources so they can reach their goals.
Steven Squires, the system’s vice president of ethics, led the work that resulted in the keystone document called “Planning Your Path | Wishes and Health Care.” He wants the succinct reference to make it easier for care providers and patients to have oftendifficult conversations around planning for care in the event of a sudden illness or as the end of life nears.
“I hope that more people will start talking about what is often a taboo topic, I think, in American culture,” Squires says.

The document was the product of a “structured exercise” undertaken by CHRISTUS’ palliative care advisory council to figure out the best method the system could adopt to facilitate advance care
Continued on 4
Pathogens unit at Providence cared for some of country’s first patients with COVID-19
By VALERIE SCHREMP HAHN
In February 2020, when a cruise ship arrived at a California port carrying passengers with COVID-19, the workers in the special pathogens unit at Providence Sacred Heart Medical Center and Children’s Hospital in Spokane, Washington, were ready to help.

The unit is one of 13 spread throughout the country and designated by the federal government to treat high-consequence infectious diseases. They are known as Regional Emerging Special Pathogen Treatment Centers. Providence St. Joseph Health is the only Catholic health care system with a unit.
When the four COVID patients from the
SSM Health surgeon hopes book inspires Black girls to become doctors
By VALERIE SCHREMP HAHN
Dr. Jovita Ugochi Oruwari wants Black girls to see her.
She wants Black girls to see what’s possible, that they can be successful, live full lives and help Black patients facing sometimes drastic health disparities.
Oruwari, a breast surgeon at SSM Health DePaul Hospital — St. Louis, edited a book that published this spring called Black Girls in White Coats. The book profiles 60 female doctors from around the country in different medical disciplines.
Black physicians make up 5% of the physician workforce, according to the Association of American Medical Colleges. Black women account for just under 3%. The nation’s Black population is 14%.
Oruwari, 55, a native of Nigeria, attended college and medical school in the U.S. and has worked in St. Louis for more than 20 years. She was an oncologic breast surgeon for the Mercy St. Louis Cancer and Breast Institute, which is in a predominantly white area. When she moved to DePaul in 2020, and the majority of her patients were Black, she was struck by what she learned about disparities in medicine and the patients’
cruise ship who were under federal quarantine arrived at Sacred Heart’s unit in the early days of the virus’ spread, “There was a lot of response based out of fear,” said Christa Arguinchona, a nurse and Providence special pathogens program manager. “And so, it was challenging for sure, but it was also an opportunity to educate
CommonSpirit hospital programs acquaint minority students with health careers
By JULIE MINDA
Like many other health care facilities across the U.S., sites within CommonSpirit Health have been increasingly concerned that minority populations are underrepresented on their staffs.

Such introspection has led hospitals in two CommonSpirit regions to develop internships that invite high school and college students of minority backgrounds to experience firsthand what it is like working in a health profession. They also get support from on-staff clinicians and receive handholding and other help to get started in a health care career.
Though the programming at the hospitals is in its infancy, it already is showing strong potential to build minority students’
The value of palliative care
Incentivizing living organ donors 3 Executive changes 6
2
Continued on 7 Continued on 6
on 5
Continued
Emergency workers arrive at Providence Sacred Heart Medical Center and Children’s Hospital with a patient during a preparedness drill in March. The hospital in Spokane, Washington, has a special pathogens unit, one of 13 in the nation that treat people with high-consequence infectious diseases.
Squires
“
This happened to be an emerging novel pathogen that we really didn’t know much about yet. So, it was a perfect use of our space and our expertise.”
— Christa Arguinchona
AUGUST 15, 2023 VOLUME 39, NUMBER 13 PERIODICAL RATE PUBLICATION
Dr. Jovita Ugochi Oruwari meets with patient Dawn Patrick of St. Louis in July. Oruwari is a breast surgeon at SSM Health DePaul Hospital — St. Louis. She edited a book called Black Girls in White Coats, which features profiles of 60 Black female doctors.
Palliative care webinar focuses on giving quality care to the whole person
By VALERIE SCHREMP HAHN
Palliative care is core to the work of the Catholic health care ministry. By helping patients get relief from the symptoms, pain and stress of a serious illness, the care adds value beyond its ability to reduce health care costs, said speakers at a webinar hosted by CHA.
“It is better quality care. It’s the way we want to care for people,” said Sarah Hetue Hill, the regional vice president for mission integration for CHRISTUS Santa Rosa Health System and CHRISTUS Children’s.

Hill discussed palliative care along with Maria Gatto, chair of CHA’s Palliative Care Advisory Council and a palliative care consultant. The webinar on July 26 was called “Palliative Care: Connecting Catholic Health Care’s Mission & Today’s Quality and Business Imperatives.”
Palliative care treats the whole person — mind, body and spirit. It can be provided at any stage of the illness by a team of trained specialists that includes doctors, nurses, social workers, chaplains and other care specialists. Studies show that those who receive palliative care may spend fewer days in the hospital, have fewer emergency room visits, improve their quality of life, and may even live longer, according to the Center to Advance Palliative Care. The center offers health care professionals and organizations resources to provide highquality and equitable care for people living with serious illness.
“Those of us who are very passionate about palliative care like to say that it’s truly a hallmark of who we are, and that’s because it stems directly from our history and our legacy,” said Hill.
She pointed out that the word “palliative” comes from the Latin root of “palliare,” meaning to cloak — like extra protection to shield people from harm. She noted that Jesus cared for the mind, body and spirit of lepers and a hemorrhagic woman by healing them not only physically but also spiritually by returning them to their communities. Many other groups and religious orders have followed suit over the years by attending to the whole person, she said.
Pope John Paul II, Pope Benedict XVI and Pope Francis have all spoken out and supported palliative care, she pointed out. Pope Francis said palliative care recognizes “the value of the person.”
Who can use palliative care?
Gatto outlined case studies of those who
Palliative care ensures value
Palliative care is specialized medical care that focuses on relieving the symptoms and stress of any serious illness, ideally alongside curative treatment. A strong evidence base exists proving its impact on quality, satisfaction, consumer demand and cost. Because it focuses on the highest need and highest cost patient segment, palliative care is an essential strategy for population health management.
IMPROVES QUALITY OF LIFE AND SYMPTOM BURDEN
DRIVES HIGH SATISFACTION AND POSITIVE PATIENT EXPERIENCES
Reduces
with improvements lasting months after initial consultation
of people who received palliative care are likely to recommend it to others
CHA supports Palliative Care and Hospice Education and Training Act
In July, the Palliative Care and Hospice Education and Training Act was introduced in the U.S. Senate. The act aims to bolster the palliative care and hospice workforce and invest in training, education and research. The bill has changed over the years but the goal of offering more training for people to provide palliative care remains the same, and CHA has supported such efforts for the last decade.
Also in July, Sr. Mary Haddad, RSM, CHA president and CEO, and members of the United States Conference of Catholic Bishops sent a joint letter of support to leadership of the Senate Committee on Health, Education, Labor & Pensions.
could use palliative care:
Mike, a family man diagnosed with head and neck cancer, needs help coordinating care so he can receive pain management for his symptoms alongside curative treatment.
Anne, a young woman experiencing pain and disability after a mastectomy, needs coordination between close cancer monitoring and pain management so she can sleep through the night and return to the gym.
Martha, who has worsening dementia and arthritis, needs support alongside her husband Bernard, who wants to care for her at home. Her team is managing her symptoms, assessing her home for fall risks and coordinating her care.
“It’s an extra layer of support,” Gatto said.
“It doesn’t take over the care, but it adds more support. ... It’s about living well and being at home to get the best possible care to control your serious illness, and it helps to coordinate all your providers talking together.”
Coordinating to fill a need
She pointed out that the Palliative Care Quality Collaborative is the only unified national registry of specialty palliative care data. Care providers can use the data to look at other programs to see how their work measures up and where to focus resources, she said.
Palliative care is key to supporting an aging nation. The population of people aged 85 and older will more than triple by 2060, Gatto said. Surveys show that patients want palliative care once they are informed about it, she said.
“The Case for Hospital Palliative Care,” a publication from the Center to Advance Palliative Care, says the care improves patients’ quality of life and reduces health care costs, including by reducing the need for emergency and intensive care. For a midsized hospital conducting 500 palliative care consultations each year, the center says savings can add up to more than $1.6 million a year.
“So get out your calculator, because if you look at these numbers, that is the huge value of that business imperative,” Gatto
“The Catholic Church teaches that all people possess inherent dignity and worth, and as such human life is a gift from God that no one may dispose of at will,” the letter said in part. The letter also cited Pope Francis, who said: “Palliative care is an authentic expression of the human and Christian activity of providing care, the tangible symbol of the compassionate ‘remaining’ at the side of the suffering person.”
said.
She pointed out that more than 83% of U.S. hospitals with 50 or more beds had a palliative care program in 2020, up from just over 24% in 2000. Palliative care has been one of the fastest-growing fields as health care organizations, health plans and policymakers have recognized the improvement and quality that also reduces costs.
Gatto said health systems should focus on sustainability and growth strategies. Among the things they can do: work on quality standardization, improve financial coding and billing practices, identify patients sooner, improve staffing models, and focus on team health and resilience.
Hill said that while hospitals are struggling financially, it’s imperative to remind senior leaders of the hospital’s mission and the work of their founders. “This is the work that they started with. So, let’s bring it back to this,” she said.
Visit chausa.org/chw for a link to the webinar.
vhahn@chausa.org
Vice President Communications and Marketing
Brian P. Reardon
Editor Lisa Eisenhauer leisenhauer@chausa.org
314-253-3437
Associate Editor Julie Minda jminda@chausa.org
314-253-3412
Associate Editor Valerie Schremp Hahn vhahn@chausa.org
314-253-3410
Graphic Design
Norma Klingsick

Advertising ads@chausa.org
314-253-3477
Catholic Health World (ISSN 8756-4068) is published semimonthly, except monthly in January, April, July and October and copyrighted © by the Catholic Health Association of the United States.
POSTMASTER: Address all subscription orders, inquiries, address changes, etc., to CHA Service Center, 4455 Woodson Road, St. Louis, MO 63134-3797; phone: 800-230-7823; email: servicecenter@ chausa.org. Periodicals postage rate is paid at St. Louis and additional mailing offices. Annual subscription rates: CHA members free, others $29 and foreign $29. Opinions, quotes and views appearing in Catholic Health World do not necessarily reflect those of CHA and do not represent an endorsement by CHA. Acceptance of advertising for publication does not constitute approval or endorsement by the publication or CHA. All advertising is subject to review before acceptance.
Providence’s environmental efforts win top honors in Laudato Si’ awards
Catholic Climate Covenant named Providence St. Joseph Health as the health care winner in its 2023 U.S. Laudato Si’ Champions Awards.
In honoring Providence, Catholic Climate Covenant said the Renton, Washington-based health system “has been at the forefront of environmental sustainability for two decades. With a visionary pledge to become carbon negative by 2030, Providence implemented a comprehensive environmental sustainability framework across their network of hospitals, medical office buildings and business units.”
© Catholic Health Association of the United States, August 15, 2023
Catholic Climate Covenant is a nonprofit that partners with other organizations to inspire and equip U.S. Catholics to care for creation. Its Laudato Si’ awards honor organizations that embody the spirit of the encyclical written by Pope Francis calling on Catholics to care for the natural environ-
ment and all people.
The award winners were announced July 27 at the end of the 2023 Laudato Si’ and the U.S. Catholic Church Conference. The awards were given in 10 categories.
In addition to naming Providence as its top health care honoree, the covenant cited two Catholic health systems for honorable mentions. St. Louis-based Ascension was lauded in part for developing “a comprehensive Environmental Impact and Sustainability program that builds upon their existing efforts in energy conservation, waste management, recycling, and the use of renewable fuels.”
CommonSpirit Health won the other honorable mention. The convenant recognized that Chicago-based system for a commitment to the environment that “is deeply ingrained in its core values and strategic plan.”
Quality of life Symptom Burden REDUCES AVOIDABLE SPENDING AND UTILIZATION IN ALL SETTINGS 48% readmissions 28% cost/day 50% admissions 35% emergency department visits 43% hospital/ emergency department transfers 36% total costs INPATIENT OUTPATIENT SKILLED NURSING HOME-BASED
Center to Advance Palliative Care
symptom distress by 93% 66%
Source:
Hill
Gatto
“Those of us who are very passionate about palliative care like to say that it’s truly a hallmark of who we are, and that’s because it stems directly from our history and our legacy.”
2 CATHOLIC HEALTH WORLD August 15, 2023
— Sarah Hetue Hill
San Diego Padres
Sister takes the mound on Catholic Night
Sr. Candida Massabo tosses out the first pitch before the San Diego Padres game against the New York Mets at Petco Park in San Diego on July 7. The Padres declared the evening Catholic Night, an annual event since 2015. The purpose is to strengthen and encourage Catholic laity to witness their faith in a public setting. The team allotted 4,500 tickets to Catholic parishes across San Diego County. A sellout crowd of 42,000 fans was in attendance.

Sr. Massabo, a member of the congregation Saint Maria Goretti Sisters, is a chaplain at Scripps Mercy Hospital San Diego. Despite Sr. Massabo’s strong start on the mound, the Padres lost the game 7-5.
SSM Health improves benefits for employees who become living organ donors
SSM Health is striving to alleviate some of the disincentives and barriers living organ donors face by improving its pay and medical leave benefits for employees who choose to become donors.
It can be difficult for people to become living donors, partly because they may not get the needed medical leave time to recuperate during an estimated four- to sixweek recovery period. According to SSM Health, it is typical for people to use vacation time or take unpaid leave to make their organ donation.
The St. Louis-based system has changed its benefits policies “to support our colleagues who would consider such a self-
less act,” Sherry Ward, vice president of total rewards, said in a release on the new policies.
Employees serving as living donors are eligible for six weeks of medical leave at full pay and full coverage of their medical expenses under SSM Health’s employee health plan, WellFirst Health. Before the change, employees were eligible for 60% pay only for medically necessary time off.
Dr. Krista Lentine, medical director of living donation at SSM Health Saint Louis University Hospital and a nephrologist with the affiliated SLUCare Physician Group, said in the release that as a transplant physician she sees firsthand
the impact of providing living donors with support during recovery after donation surgery. She said the new SSM Health policies help “living donor employees recover without incurring financial loss in sharing the gift of life.”
She added that improving employee benefits for these staff members illustrates that SSM Health, its facilities and its transplant program are dedicated “to reducing barriers to living donation and living donor transplantation.”
According to the American Society of Transplantation, the most common organ donations are a kidney or a portion of the liver. The Health Resources and Services
Upcoming Events from The Catholic Health Association
Administration said more than 104,000 people are on the national organ transplant waiting list. As of January, nearly 89,000 people were waiting for a kidney and more than 10,000 were waiting for a liver. Each day, 17 people die waiting for an organ transplant.
SSM Health’s policy changes enabled the system to join the American Society of Transplantation’s “Circle of Excellence,” a designation given to organizations that support employees who donate an organ. This corporate recognition program “celebrates companies helping to eliminate barriers to living donation,” according to the transplantation society.
St. Michael in Northwest Washington to add patient tower to renovated campus
Building on a $540 million investment in Western Washington, St. Michael Medical Center plans to add a patient tower to its recently renovated Silverdale, Washington, campus, and to add a hybrid emergency room and urgent care facility in Bremerton, Washington.
The activity is part of expansion plans St. Michael announced in 2017, which include transferring inpatient beds from its Bremerton hospital campus to the Silverdale campus it acquired in 2014. St. Michael completed a renovation of the Silverdale campus in 2020. The expansion included a Level III trauma center, cancer center and medical pavilion.
The patient tower St. Michael is adding to the Silverdale campus will accommodate the beds from the Bremerton site. The tower is to open in 2025, and that facility will have 336 beds.
St. Michael is demolishing the Bremerton campus by summer 2024. It is adding the hybrid emergency room and urgent care to a clinic campus it has in Bremerton.
The medical center is part of Virginia Mason Franciscan Health, a system affiliated with CommonSpirit Health.
Catholic Ethics for Health Care Leaders Virtual Program Tuesdays Sept. 5 – Oct. 17 | 1 – 3 p.m. ET Mission in Long-Term Care Networking Zoom Call (Members only) Sept. 6 | 1 – 2 p.m. ET Deans of Catholic Colleges of Nursing Networking Zoom Call Oct. 3 | 1 – 2 p.m. ET United Against Human Trafficking Networking Zoom Call Oct. 4 | Noon – 1 p.m. ET Community Benefit 101: The Nuts and Bolts of Planning and Reporting Community Benefits Virtual Program Oct. 24 – 26 | 2 – 5 p.m. ET each day Mission Leader Seminar Virtual Program Tuesdays Nov. 7 – 28 | 1 – 2:30 p.m. ET
We Will Empower Bold Change to Elevate Human Flourishing. chausa.org/calendar
August 15, 2023 CATHOLIC HEALTH WORLD 3
Advance care planning
From page 1 planning.
The council of about 16 people evaluated several popular formats and identified the strengths and weaknesses of each. Among the weaknesses group members cited, Squires says, was that some of the formats focused so much on what medical interventions someone did or didn’t want that the person’s overall goals of care were ignored.
In the end, Squires says, the consensus was that CHRISTUS should develop its own format that lessened or eliminated the drawbacks of the other methods and capitalized on their strengths.
‘What are your wishes?’
One of the sources that informed the group’s work was a study titled “Common Items on a Bucket List” published in 2018 in the Journal of Palliative Medicine. That study concluded: “The bucket list is a simple framework that can be used to engage patients about their health care decision making. Knowing a patient’s bucket list can aid clinicians in relating each treatment option to its potential impact (if any) on the patient’s life and life goals to promote informed decision making.”
The printed guide CHRISTUS developed asks users at the start: “What are your wishes for your health care?” It notes that many people will face a time when they cannot communicate their wishes due to a sudden or long-term illness. It then asks: “Where are you in thinking about your advance care plans?”

Users get a choice of three answers, which each lead to a column of considerations, follow-up questions and QR codes. Those codes, when scanned with a smartphone camera, connect to various resources, such as a guide to having conversations about health care. The back of the guide covers frequently asked questions and has QR codes that link to additional resources.
Squires sees it as vital to the effective use of the guide that users have a “human touch point” — someone explaining the document’s importance and usefulness as it is presented to a patient.
“What we don’t want to do is leave something in a pile somewhere in the admissions process or in a physician’s office without having somebody who knows what it is and is able to dialogue with people about it,” he explains.

Relationship-building tool
Kathy Armijo Etre, vice president of mission integration at CHRISTUS St. Vincent Regional Medical Center in Sante Fe, New Mexico, introduced the guide to staff there this spring. She says the guide has been widely distributed among the nursing staff and to outpatient clinics.
Etre is on CHRISTUS’ palliative care advisory council and was one of those who supported the idea of the system developing a distinct and innovative approach to advance care planning. She says the guide is a big step in that direction.
“When Steven came up with this, I loved
it because it’s a way to begin the conversation and help people place where they are in their decision-making process,” Etre says.
Etre says the document aligns with the approach of Dr. Diane Portman, St. Vincent’s director of palliative care, who urges that end-of-life planning be an ongoing relationship-based process between care providers and patients, rather than a formbased process. “This (guide) is a tool to help initiate the relationship building with patients,” Etre says.
A member of St. Vincent’s supportive care team who is nearing graduation as a nurse practitioner is using the guide as part of a capstone project on advance care planning. That staffer plans to help the team, formerly known as the palliative
care team, create training on the use of guide. “It’s the next most important thing to be done,” Etre says.
Closing the gap
In Squires’s view, end-of-life care is an especially important aspect of Catholic health care. He points out that one of the directives in the Ethical and Religious Directives for Catholic Health Care Services is to provide patients in danger of death with “appropriate opportunities to prepare.”
Squires says the Catholic health care ministry can distinguish its end-of-life care by delivering it with more humaneness and compassion than other health care providers. It also can strive to close what he
sees as a disconnect: people want to have their end-of-life wishes followed but they often are not actually making those wishes known.

That gap was highlighted in a 2019 study commissioned by the California Health Care Foundation that found that most Californians supported advance care planning but only about a third had put their wishes in writing.
“Maybe the role of Catholic health care is to close the gap, to say, ‘What is it that’s making this so darn difficult, and how can we help?’” Squires says. “Maybe this document is just a start, like one individual piece to this larger societal issue.”
leisenhauer@chausa.org
COMMUNITY BENEFIT 101: THE NUTS AND BOLTS OF COMMUNITY BENEFIT


“The


the CHNA and CHIP was so essential and will be invaluable in my role.”
CHA’s Community Benefit 101: The Nuts and Bolts of Planning and Reporting Community Benefit, a virtual conference, will provide new community benefit professionals and others who want to learn about community benefit with the foundational knowledge and tools needed to run effective community benefit programs.
Attendees will receive a copy of CHA’s A Guide for Planning and Reporting Community Benefit
What you will learn:
Taught by community benefit leaders, the program will cover what counts as community benefit; how to plan, evaluate and report on community benefit programs; accounting principles and a public policy update.
Who should attend:
New community benefit professionals who want a comprehensive overview of all aspects of community benefit programming.
Staff in mission, finance/tax, population health, strategic planning, diversity and inclusion, communications, government relations, and compliance who want to learn about the important relationship of their work and community benefit/community health.
Veteran community benefit staff who want a refresher course to update them on current practices and inspire future activities.
View the full one-page guide created by CHRISTUS Health that helps patients figure out where they are in the process of advance care planning.
24, 25 & 26, 2023
day from 2
P.M. ET Join us for the virtual program!
were
and I can already use the information presented in my day to day activities.” LEARN MORE AT CHAUSA.ORG/COMMUNITYBENEFIT101 — Program Participant — Program Participant We Will Empower Bold Change to Elevate Human Flourishing. Thank you to our sponsor the American Hospital Association 4 CATHOLIC HEALTH WORLD August 15, 2023
information about
OCTOBER
Each
to 5
“CHA has great resources that
used as part of the program
Special pathogens unit
From page 1
everybody to our capability and to our preparedness level.”
None of the four COVID patients brought to the unit had severe symptoms. They were released within the 28 days that the unit was activated. As more people were hospitalized later with severe cases of COVID, the unit was used as treatment space for the overflow of patients.
Sharing their work
This spring, after the federal government lifted the public health emergency, Providence opened the doors to the highly specialized unit for media tours. The system wanted people to learn about how the unit works so they could understand how it was used, and how it may be used in the future.
Health leaders and federal partners look at specific criteria to determine when to activate and deactivate special pathogen units.

The units’ origins go back to the Ebola outbreak in 2014 and 2015, when Emory University Hospital in Atlanta, the University of Nebraska Medical Center/Nebraska Medicine, and NYC Health + Hospitals/ Bellevue in New York were tasked with caring for patients in the United States. Ebola first spread in parts of Africa, where more than 11,000 people died. Fewer than a dozen people were treated for it in the United States, where two people died.
The Ebola outbreak prompted the Centers for Disease Control and Prevention to partner with public health departments to create more regional facilities that would be able to respond in the event of a similar outbreak. Congress approved funding to establish the centers.
The Washington State Department of Health encouraged Sacred Heart to apply for funding. The hospital had the space and the willingness to invest in training and preparedness. Its unit opened in 2015, and generally serves Alaska, Idaho, Oregon and
Washington.
Special equipment
The unit is 14,000 square feet, with 12 ICU-level rooms with negative airflow to contain pathogens. There’s in-room video to help monitor and communicate with patients and caregivers, as well as a biosafety lab to contain potentially infectious samples. An isolated area stores dedicated supplies and personal protective equipment and has rooms for putting on and removing the gear.
The unit also has a San-I-Pak, which is a sterilizer that allows workers to inactivate waste that may carry an infectious substance. Without the sterilizer, the waste would have to be taken to an off-site
incinerator.
The number of patients the unit can hold at one time depends on the pathogen involved. The unit can hold only two patients with Ebola or viral hemorrhagic fever because of the space needed to isolate them at a high level. The unit can care for up to 12 patients who have a respiratory pathogen with a lower acuity.
Prepared for a pandemic
Arguinchona was at a meeting in January 2020 unrelated to COVID with colleagues from the other regional treatment centers when they started carefully monitoring the novel virus seen in Wuhan, China. Because the Spokane unit’s staff had been regularly training for years, preparations for their first patients went smoothly.
“This happened to be an emerging novel pathogen that we really didn’t know much about yet,” she said. “So, it was a perfect use of our space and our expertise.”
She said that no staffers contracted COVID during the unit’s activation — a testament to their preparedness.
About 90 staffers, who otherwise work elsewhere in the hospital, are specially trained to work in the unit. They include nurses, doctors, nurse practitioners, physician assistants, respiratory therapists, medical laboratory scientists and environmental services personnel. They get regular training and can mobilize within eight hours if they are asked to receive a patient with a high-consequence infectious disease. They all chose to work in the unit.

The unit’s staff partners with those in other regional centers to educate and train one another. This March, they completed a training exercise with another health care system in the Spokane area as well as with other local and state agencies. Now, they are working with the other regional centers to focus on prevention of disease spread.
Arguinchona called the time during the unit’s activation challenging, but not scary. “I would say we were confident, and we were ready,” she said. “And I’m confident that we would feel the same way again, if we were activated for another pathogen.”
Thomas Barnett is a nurse who joined the special pathogens team around the time it started and found it especially rewarding to be part of a new program at the hospital. He serves as a team leader and takes part in quarterly trainings.

“A lot of my colleagues I’ve worked with, I’ve tried to get them to join and they were like, ‘Do you really want to take care of an
Ebola patient if they come?’”
Barnett said his response is: “The way I look at it, I’m getting the best training to be safe. It’s not that I want to take care of somebody who is really contagious, but I know how to do it.”
When he and his colleagues in the unit learned in 2020 they would get some of the first COVID patients, they felt ready. “It was almost like a nervous excitement,” he said. “Like, OK, we don’t know what this virus is just yet, but I did feel very confident that we had all the right equipment. We’d had lots of training. We were familiar with the unit we were using.”
Preparing for the future
Leaders of the National Emerging Special Pathogens Training and Education Center, the coordinating body for the National Special Pathogens System, said in a statement that they are proud to have members of the Sacred Heart unit in its ranks. The leaders added that they “remain grateful that the Providence Sacred Heart special pathogens unit will continue to join NETEC and the nation’s 12 other RESPTCs (Regional Emerging Special Pathogen Treatment Centers) in setting the gold standard for special pathogens care, protecting the lives and security of millions of Americans in the process.”
“We
— Christa Arguinchona
Taking on the responsibility of the special pathogens unit is one way Sacred Heart fulfills its mission as a Catholic hospital, Arguinchona pointed out.

“We are very committed to our mission, and our mission is to care for our community and to care for those that are vulnerable,” especially those with infectious diseases, she said. “We can’t control who walks through our doors, and we want to be prepared for whoever is sent to us needing that care.”
vhahn@chausa.org
Nurse Sarah Emerson and other Providence Sacred Heart Medical Center and Children’s Hospital caregivers gather personal protective equipment before beginning a drill in the hospital’s special pathogens unit. The unit, one of 13 spread across the country, includes an isolated area that stores the equipment and includes rooms for putting it on and taking it off.
are very committed to our mission, and our mission is to care for our community and to care for those that are vulnerable. We can’t control who walks through our doors, and we want to be prepared for whoever is sent to us needing that care.”
Nurse Jessica Bruce with Providence Sacred Heart Medical Center and Children’s Hospital starts an IV during a preparedness drill. Staffers who work in the special pathogens unit, which opened in 2015, take part in regular drills to prepare for patients with a high-consequence infectious disease.
Arguinchona
August 15, 2023 CATHOLIC HEALTH WORLD 5
Barnett
PRESIDENTS/CEOS
Julie Lautt to interim president and CEO of Sioux Falls, South Dakota-based Avera Health. She also will continue in her role as Avera chief financial officer. In April Avera announced that President and CEO Bob Sutton would step down due to a serious medical condition.


Jackie Harris to president and CEO of Trinity Health Senior Communities. Previously she was president and CEO of Integrace, a senior living provider in the greater Washington, D.C., area. Prior to heading


Internships for minority students
From page 1 awareness of and to steer them toward those roles, while also providing a needed morale boost to the students’ mentors on staff, say executives heading the programs.
“From the student perspective, they’re exposed to the health care field, and seeing it in action … and this is showing them that this is within their reach,” says Dr. Lynn Jeffers, chief medical officer of CommonSpirit’s Dignity Health — St. John’s Regional Medical Center in Oxnard, California, and Dignity Health — St. John’s Hospital Camarillo in California. She says from the hospitals’ perspective, “We’re serving the community in a new way. And this is reinspiring the people involved about why they went into health care in the first place.”
Saida Selene Espinoza is the program director of a similar effort at a CommonSpirit hospital about 1,600 miles away at CHI Health Midlands hospital near Omaha, Nebraska. She says through that hospital’s internship programs, Hispanic students “are seeing it is possible to dream big, and they don’t have to let their background be a limiting factor” in their future careers.

Unequal access
Espinoza says there were several sources of inspiration for the Omaha-area program. For one, when she assisted with a COVID19 vaccination program at a local meatpacker, she saw a lack of Spanish-speaking health care professionals available to serve the majority-Hispanic workers getting the vaccine. In subsequent talks with others at CHI Health facilities and with the Latino Center of the Midlands, she learned there is a lack of diversity in staff across Omaha’s health care sector and that is causing a
Integrace, Harris had been president and CEO of Trinity Health Senior Communities from 2001 to 2009.
Kerry Alys Robinson to president and CEO of Catholic Charities USA. She had been a Leadership Roundtable executive partner.
ADMINISTRATIVE CHANGES
Dr. Kevin L. Lewis to senior vice president and chief physician executive of Hospital Sisters Health System of Springfield, Illinois, effective Aug. 28.

Sr. Lisa Maurer, OSB, to director of

mission integration and formation at Duluth Benedictine Ministries, the new ministerial public juridic person for the Benedictine Sisters of St. Scholastica Monastery in Duluth,
about topics prioritized by the workers.
The other internship, started in 2021 with another installment of mission and ministry funding, is the health career shadowing program. Hispanic high school and college students get an introduction to health care, are paired with mentors and spend time shadowing clinicians at CHI Health Midlands.
Students apply online for the programs, provide a letter of recommendation from their school, take part in a phone interview and then are selected for participation.
Students from both the community health worker and health care careers tracks can apply to move on to a certified nursing assistant program. It includes coursework at a local college, practical experience at CHI Health Midlands and assistance from a recruiter with job placement at CHI Health after the student is certified. Students have the opportunity to pursue other health care careers at CHI Health after becoming a CNA.
Minnesota.
Darren Henson to CHA senior director, ministry formation in the association’s Sponsorship and Mission Services department.

a yearlong internship. The interns go to the hospital for several hours once a week for two semesters. They spend the fall semester circulating among numerous hospital departments, including the intensive care unit, emergency department, physical therapy, respiratory therapy, pharmacy and radiology. They then focus on three preferred departments for the spring semester. All along they are paired with a physician mentor. The college students take a biology course at their school while participating in the hospital internship.
CommonSpirit hospitals in Camarillo and Oxnard replicated the program and began their own cohorts this past year. Another system facility, in Long Beach, is considering doing so.
Win-win-win-win
chasm between providers and patients.
Espinoza adds that populations have self-segregated in Omaha. She says students at high schools serving the mostly white areas traditionally have had much more access to health care career programs than students at high schools serving minority communities.
Collaborating with Omaha Public Schools and the nonprofit Latino Center, Espinoza and colleague Lucia Rodriguez Alvizo developed two paid internship programs designed to help increase CHI Health’s diversity. Rodriguez Alvizo is Healthier Communities & Community Benefit coordinator for CHI Health, Omaha. CHI has 14 hospital campuses in and around Omaha; most of the internship activity is at the CHI Health Midlands campus.
One internship program, started in 2019 with CHI Mission and Ministry Fund grant dollars, recruits Hispanic high school students to be community health interns, shadowing CHI Health Midlands community health workers. The interns communicate with, educate and provide resources to Hispanic community members, especially


Fewer than 20 students total can participate annually in the two internship programs. Espinoza says a goal is to increase the programs’ capacity.
From reflection to action
Similar programming in CommonSpirit’s Southern California region began at Dignity Health — Glendale Memorial Hospital and Health Center. In early 2021, colleagues there viewed the documentary Black Men in White Coats for Black History Month and were challenged to reflect on the lack of Black representation on clinical staffs in the U.S. and what they could do about it.
Rev. Cassie McCarty, the Glendale hospital’s director of mission integration and spiritual care services, explains that hospital leadership came up with the idea of an internship for students in underrepresented groups, including those of racial and ethnic minority status, those who identify as part of the LGBTQ+ population and those who are first in their family to go to college as well as those with lower socioeconomic status.
The resulting program that began in late 2021 has local high school and community college students applying to participate in
Those involved with the minority internship programs in the Omaha and Southern California regions say the initiatives are a win not just for the students but also for the facilities and their staffs, patients and community members.
Rev. McCarty in Glendale says many participating students had not previously known about the variety of roles available in a hospital. Jeffers in Oxnard and Camarillo notes that many students hadn’t considered that they could pursue hospital roles.


Espinoza in Omaha says that it’s important for minority students to have mentors whose backgrounds, life experiences, language, family life and faith are similar to their own. This helps them see themselves in the roles their mentors hold.
In Omaha, Gustavo Servin-Maciel is the Siembra Salud program coordinator at the Latino Center. Seimbra Salud translates to “sowing health.” He says through the shadowing programs, students are believing in themselves, getting out of their comfort zones and building the essential soft skills they’ll need throughout their future careers, whether or not they work in health care. Rodriguez Alvizo, with Omaha’s CHI Health, says students who are interested in health care roles are gaining career readiness through shadowing.
While the initiatives in both the Omaha and Southern California regions are new, both promise to in time boost the pipeline of candidates for health care positions at a time of widespread worker shortages.
And, facilities, patients and communities will benefit as staffs get more diverse, those interviewed say. Rev. McCarty notes the documentary that inspired the Southern California program shows that if patients don’t see themselves in their providers, they can lose trust in them. Conversely, when patients see themselves in their providers, they may develop more trusting relationships which can lead to better patient health, she says.
Jeffers in Southern California says a perhaps unanticipated benefit of the programming has been the positive impact on staff members who are mentoring the interns. Rev. McCarty agrees that the addition of fresh, young, motivated and curious minds has been energizing for the facilities. jminda@chausa.org
KEEPING UP
Lautt Harris Lewis Sr. Maurer Henson
Students who are part of the health career shadowing program at CHI Health Midlands get a chance to handle medical equipment during a demonstration. CHI Health Midlands is in Omaha, Nebraska.
Dr. Andrew Jeffers demonstrates orthopedic robots used for knee and hip replacements at Dignity Health — St. John’s Hospital Camarillo in California. His presentation was part of a “robot day” attended by local high school students who take part in the hospital’s shadowing program. The students had a chance to try out the robots. Jeffers is an orthopedic robotic surgeon and director of St. John’s Orthopaedic Center.
Jeffers
Espinoza
Rodriguez Alvizo
Rev. McCarty
6 CATHOLIC HEALTH WORLD August 15, 2023
Servin-Maciel
IN BRIEF
Ministry providers support AHA anti-violence campaign
The American Hospital Association hosted its annual Hospitals Against Violence “Have Hope Friday” to highlight how hospitals and health systems nationwide are combatting violence.
Have Hope Friday, promoted under the hashtag #HAVhope, invited health care systems and facilities to share how they are using partnerships, innovation, advocacy and creative thinking and solutions to foster a safer environment for patients, staff and community members. Among ministry organizations supporting Hospitals Against Violence in June on Twitter were CommonSpirit Health, CHA, Trinity Health and Trinitas Regional Medical Center of Elizabeth, New Jersey.
A focus of the Friday postings was health care organizations’ support of the Safety from Violence for Healthcare Employees Act, legislation that has been proposed in Congress to provide legal protections against assault and intimidation to health care workers.
Our Lady of the Lake offers virtual cardiac rehabilitation
Our Lady of the Lake Regional Medical Center in Baton Rouge, Louisiana, is now offering cardiac rehabilitation virtually.
The services are offered through a partnership between Our Lady of the Lake’s parent, Franciscan Missionaries of Our Lady Health System, and the telehealth company Recora. The virtual care offers heart disease patients the option to recover at home as they would at the cardiac rehab facility at Our Lady of the Lake Heart & Vascular Institute.
Francisican Missionaries of Our Lady Health System announced its partnership with Recora in February. Our Lady of the Lake is the first hospital in the health system to launch the virtual cardiac rehabilitation program.
Recora’s services remove issues patients often face with transportation and scheduling while providing on-demand support from care teams, 24/7 chat and additional resources.
Black female doctors
From page 1 experiences.
“It was a huge eye-opener for me,” she says. “A lot of data that I knew in the back of my head but I never really conceptualized was true.”
Book inspiration
She points out that Black women are 40% more likely than white women to die from breast cancer and are more likely to have advanced breast cancer. Many do not have access to mammography.
At the height of the COVID-19 pandemic, she saw Black patients’ mistrust of the vaccine, a fear rooted in a long history of the medical field mistreating and exploiting Black people.
When she talked to Black children about what they wanted to be when they grew up, they’d say Beyoncé or Jay-Z. “Nobody ever said health care, right?” she says.
She knew she could serve as an example. One white patient brought her two Black adopted children to meet Oruwari. “She wanted them to see someone of color who was practicing medicine just so that they
Mercy Cedar Rapids joins local Catholic partners for service project
Mercy Medical Center in Cedar Rapids, Iowa, completed its sixth annual service project with two other local Catholic organizations last month. The organizations call the one-day community service project Circle the City.

The tradition is a way for the sister ministries to mark the anniversary of the July 1875 arrival of the Sisters of Mercy in Cedar Rapids. The other partners are Mount Mercy University and the Catherine McAuley Center, a nonprofit social services organization.
This year, volunteers from all three organizations worked together to assemble 15,000 meals for the Take Away Hunger organization. That organization distributed the meals to community members who are in crisis.
SSM Health moves skilled nursing care from Mt. Calvary to Fond du Lac
SSM Health is moving Villa Loretto — which is the skilled nursing care facility at its eldercare campus in Mt. Calvary, Wisconsin — to an SSM Health eldercare campus in Fond du Lac, Wisconsin.
SSM Health said in a statement that the demand for skilled nursing beds has been declining at Villa Loretto and the facility
can see that this is a possibility,” the doctor says.
All of these things, Oruwari says, sparked the idea for this book.
Different paths to medicine
Oruwari knew some of the Black female doctors profiled in the book. Others she contacted through social media. They filled out a questionnaire, or, if they preferred, Oruwari interviewed them. Each profile reads like a short essay.
The doctors’ calls to medicine were different: Oruwari knew her career path since she was 3, when she sat in her grandfather’s hut in Nigeria and watched him give natural remedies to people as a traditional medicine man.
Dr. Jade James-Halpert, an obstetrician and gynecologist at SSM Health DePaul Hospital, writes that her mother used a lot of home remedies growing up, and she interpreted that to mean there was a shortage of Black doctors. “I decided I wanted to become one so I could help communities of color with their health,” she writes.
Many of the doctors are frank about struggles in medical school, or instructors not believing they should go into a certain field. Some have faced subtle or more overt
is at less than half its 50-bed capacity. The facility also has an aging physical plant. SSM Health said in the statement that after a period of rigorous discernment, “we determined it would be best to consolidate our skilled nursing operations to our nearby St. Francis Home in Fond du Lac.” St. Francis Home is attached to St. Agnes
Hospital.
SSM Health is helping Villa Loretto residents relocate to St. Francis Home or another location of their choice. SSM Health has invited Villa Loretto employees to transition to jobs at other SSM Health facilities. The Villa Rosa assisted living facility and the Cristo Rey Ranch petting zoo that are also on the Mt. Calvary campus remain open.
Back-to-school supply drive brings first responders to hospital campus
First responders from nearby police and fire departments took part in HSHS St. John’s Children’s Hospital’s Touch a Truck Back-to-School Supply Drive at the hospital in Springfield, Illinois.

The hospital invited the community to its campus to get a close-up look at police cruisers, fire engines and ambulances from various agencies. The event attracted dozens of people who in turn donated back-to-school supplies for children at local schools.
Some of the first responders who came for the event visited children getting care at St. John’s.
The hospital’s partners on the July 27 event were the Springfield police and fire departments; the Chatham, Illinois, Fire Department; Southern Illinois University School of Medicine; and America Ambulance.
discrimination from their peers, supervisors and patients. Some have struggled with their own mental health.
Women in general experience similar stresses, and they often think they are all alone, says Oruwari.
“We don’t really talk to each other because everybody’s trying to make it through,” she says. “And there’s this thing in medical training where you don’t show any sign of weakness. So you don’t complain, you don’t talk to each other, everybody’s doing just fantastic, right? So you don’t realize until you start talking to each other that you all probably had the same struggle.”
Beyond the white coats
Many of the women discuss their life outside of work, which includes time with family, mentoring and educating others through TikTok and other social media. Some of them have side businesses, such as providing financial consulting for women or marketing a line of fashion eyewear.
Many of the doctors write about the moment of recognition and joy when Black patients walk through an exam room door and are greeted by a doctor who looks like them. Studies show that this goes beyond simple recognition: Black doctors and patients listen to one another, resulting in better outcomes.
Writes Dr. Esther Ufot, who practices family medicine in Atlanta: “My proudest moment was a 90-year-old patient who had marched with Martin Luther King Jr. saying to me, ‘You are the first Black doctor I have
ever seen in my 90 years, and I am glad I am alive to see this.’”
That recollection gave Oruwari chills.
Oruwari asked the doctors to submit two types of photos: a professional one, maybe wearing a white coat or scrubs, and another as simply women, maybe glammed up for a night out.
“I know what appeals to the kids is glamour,” she says. “They don’t want to talk about going to school for eight years.”
Modeling possibilities
When Oruwari was in medical school, she was mentored by two female surgeons — even more of a rarity in those days — who specialized in breast cancer surgery. “Walking into the hospital and meeting these women who were surgeons was so inspiring to me, because, oh my gosh, they’re women,” she recalls. “And, I mean, they’re doing this. I can certainly do this.”
Oruwari knows she will retire someday and wants someone who looks like her to fill her shoes. As a Catholic, she is grateful SSM Health is on board with her mission and is helping her promote the book. She’s given away copies to local schools and youth organizations.
“This book is not only for every little Black girl out there who has dreamt of wearing a white coat and a stethoscope,” she writes in the book’s introduction. “It is also for all the little Black girls that have not dreamt of it because they have never thought it a possibility.”
vhahn@chausa.org
 Volunteers Deb Marlin, at left, and Paula Land prepare food for hungry people around Cedar Rapids, Iowa, during Circle the City, a daylong service project undertaken by volunteers.
Volunteers Deb Marlin, at left, and Paula Land prepare food for hungry people around Cedar Rapids, Iowa, during Circle the City, a daylong service project undertaken by volunteers.
March 1, 2022 CATHOLIC HEALTH WORLD 7 August 15, 2023
Firefighters help Jamari Isaiah Lee operate the hose on an engine during the Touch a Truck Back-to-School Supply Drive at HSHS St. John’s Children’s Hospital in Springfield, Illinois. First responders from several agencies took part.
Ever-evolving to meet new needs, St. Mary in Southern California marks centennial
Dignity Health — St. Mary Medical Center in Long Beach, California, is celebrating its centennial. The facility’s history includes an earthquake that once destroyed the hospital and the development of programming to help community members in need, including residents of Cambodian descent.
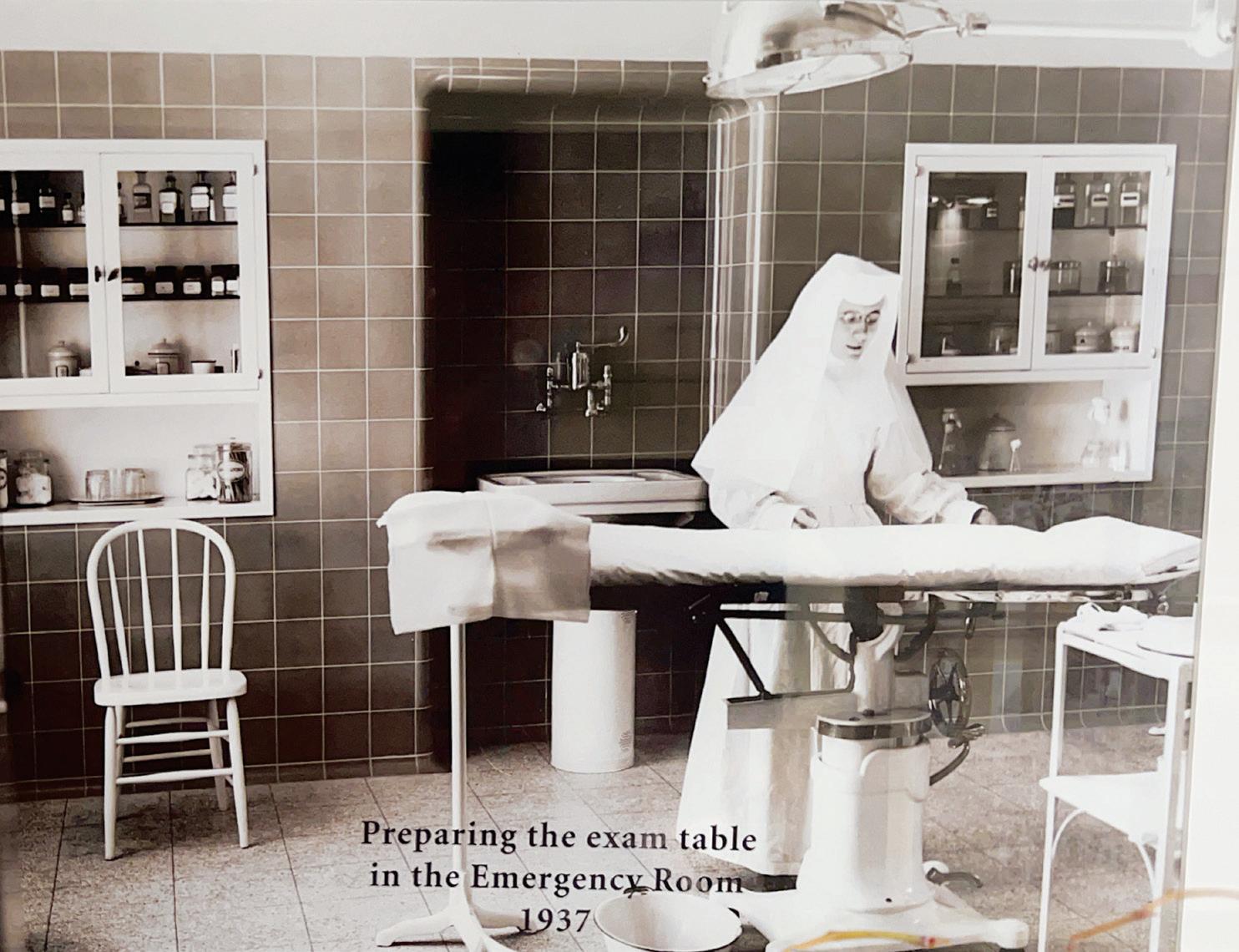
When it opened on August 26, 1923, St. Mary was the state’s first Catholic hospital south of Los Angeles. The Sisters of Charity of the Incarnate Word built the 70-bed hospital at a cost of about $160,000, and it included an emergency room, laboratory, pharmacy and operating room.


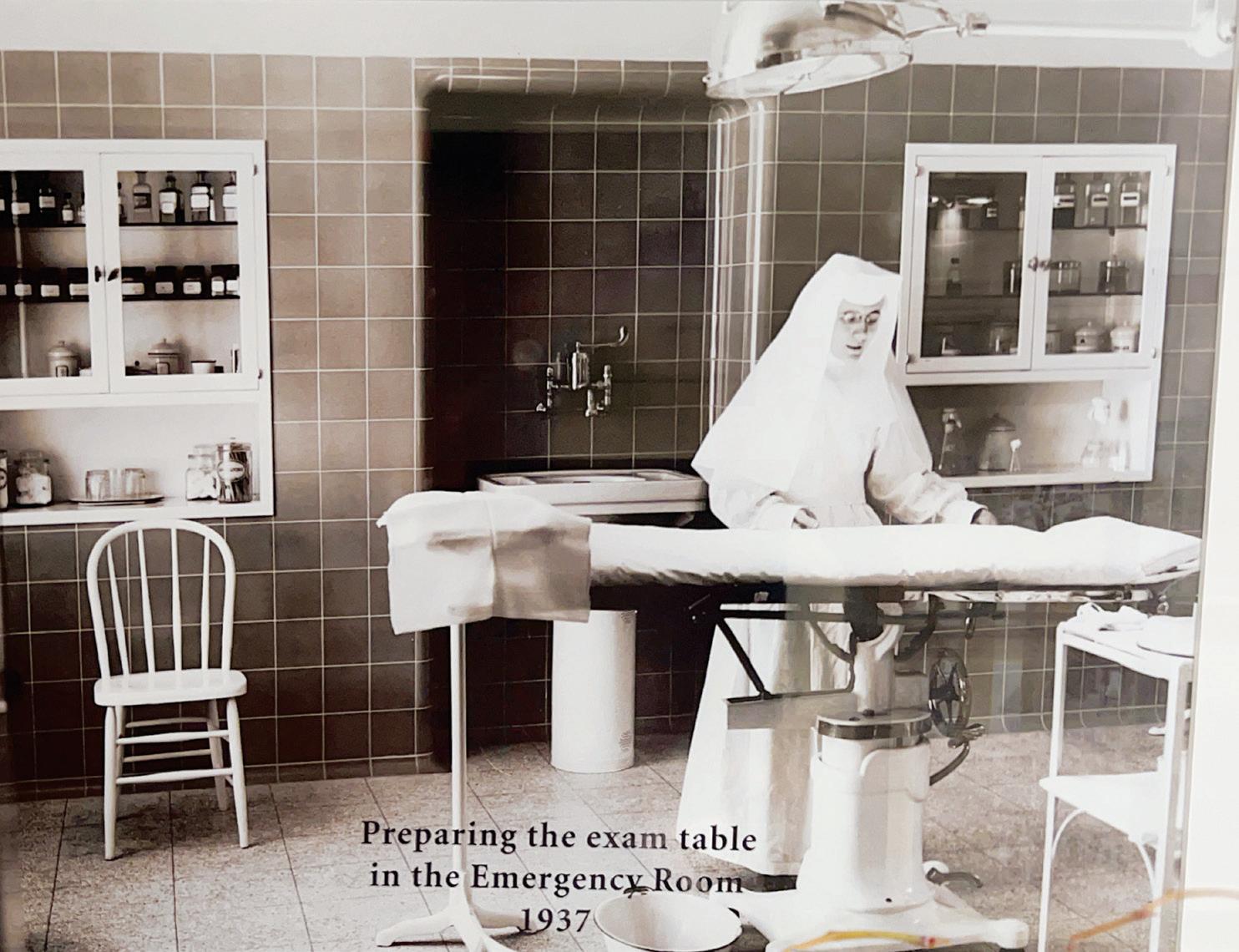
Just a decade after the hospital opened, a 6.4-magnitude earthquake destroyed the facility as well as the sisters’ convent and a chapel. With the assistance of the chairman of Hancock Oil, the sisters rebuilt the campus. It reopened in 1937.
The hospital has undergone multiple expansions, including a 1949 addition that doubled its capacity and a 1974 update that transitioned the facility to all private
Virtual gathering for ethicists to focus on innovations in Catholic health care
Registration is open for the Catholic Healthcare Innovation in Ethics Forum. The annual conference, known as CHIEF, provides a venue for ethicists working in Catholic health care to present innovative ideas or projects, receive critical feedback, and contribute to evolving how Catholic health care thinks about and implements ethics.
The virtual conference is Sept. 19-21 from 10 a.m. — 2 p.m. CST each day.
patient rooms and expanded the emergency department.
St. Mary currently has 360 beds. It is a Level II trauma center and it has a cardiac and vascular center, certified comprehensive stroke center, surgical weight loss center and maternity department. The facility now is part of CommonSpirit Health’s Dignity Health.
According to estimates from St. Mary, the hospital has provided services to 13% of Long Beach community members. Long Beach has a population of over 456,000. About 70% of St. Mary’s patient population is uninsured or is insured under MediCal, the state’s Medicaid program.
St. Mary established a clinic in 1986 that provides comprehensive care, social services, a food bank and other services to people with HIV. At the time the hospital opened this CARE Center, many hospitals were refusing to provide care to patients with HIV, according to St. Mary.
The hospital offers Families in Good Health, a multicultural health and social services program designed to meet the socioeconomic and wellness needs of people of Cambodian descent. That program served more than 8,000 people last year.
The hospital’s centennial celebration began in April with a kickoff event at the Museum of Latin American Art in Long Beach. The observances will continue with a festival Mass and picnic, a luncheon to honor the Sisters of Charity of the Incarnate Word, a birthday party that will be free to Long Beach community members as well as an end-of-the-year centennial ball.
St. Mary President and CEO Carolyn Caldwell said in a release that the centennial calls to mind “the strength and courage of our founding sisters.” She expressed hope that “St. Mary’s healing ministry will continue to thrive for another 100 years as it meets the growing health care needs of our community.”
CATHOLIC ETHICS for HEALTH CARE LEADERS
SEPTEMBER 5 TO OCTOBER 17, 2023
Consecutive Tuesdays from 1 to 3 P.M. ET
Seven-Week Virtual Course
Fr. Kopfensteiner
CHIEF is designed around short talks, a keynote address and time for networking. This year’s keynote address will be by Fr. Tom Kopfensteiner, senior executive vice president and chief mission officer with CommonSpirit Health.

Ethicists working in Catholic health care and students pursuing an ethicsrelated degree who have a desire to work in the Catholic health care ministry are invited to attend. The cost is $50. The fee is waived for students who are not employed full time.
To register, email Theresa McCruden at theresa.mccruden@mercy.net or Jenna Speckart at jenna.speckart@ mercy.net.
This online course is designed for mission leaders, chaplains/spiritual care leaders, clinicians, social workers and sponsors who want to deepen their understanding of Catholic health care ethics. Participants who complete the course will be better equipped to discern when to apply their learnings and when to seek the guidance of an ethicist.
WE HOPE TO SEE YOU THERE!
LEARN MORE AND REGISTER AT CHAUSA.ORG/CEHCL
A hospital staff member prepares an emergency room at Dignity Health — St. Mary Medical Center in 1937. That was the year the rebuilt Long Beach, California, hospital reopened after it had been destroyed in an earthquake.
Dignity Health — St. Mary Medical Center, at its 1923 grand opening. Present-day Dignity Health — St. Mary Medical Center of Long Beach.
8 CATHOLIC HEALTH WORLD August 15, 2023
































 Volunteers Deb Marlin, at left, and Paula Land prepare food for hungry people around Cedar Rapids, Iowa, during Circle the City, a daylong service project undertaken by volunteers.
Volunteers Deb Marlin, at left, and Paula Land prepare food for hungry people around Cedar Rapids, Iowa, during Circle the City, a daylong service project undertaken by volunteers.